- 1Department of Health Education, College of Military Preventive Medicine, Army Medical University, Chongqing, China
- 2Department of Basic Psychology, School of Psychology, Army Medical University, Chongqing, China
- 3College of Basic Medical Sciences, Army Medical University, Chongqing, China
- 4Department of Obstetrics and Gynecology, Chongqing Health Center for Women and Children, Chongqing, China
Objective: This study aims to explore the relationship between pregnancy stress (PS) and antenatal depression (AD) among Chinese pregnant women and to investigate whether maternal health literacy (MHL) and social support (SS) mediate the relationship between PS and AD.
Method: This cross-sectional study utilized a two-stage sampling approach, combining stratified random cluster sampling in the first stage with convenience sampling in the second stage, to enroll 1,391 pregnant women attending prenatal care at six hospitals in Chongqing between September 2023 and February 2024. Data were collected using structured scales, including general information questionnaire, Edinburgh Postnatal Depression Scale(EPDS), Pregnancy Stress Scale(PSS), Multidimensional Scale of Perceived Social Support(MSPSS) and Maternal health literacy questionnaire. We utilized Amos 22.0 to establish a structural equation model(SEM).
Results: 443 participants (31.85%) reported symptoms of depression, and 382 participants (27.46%) had moderate or above stress; in contrast, only 82 participants (5.90%) reached the level of MHL. Spearman correlation analysis revealed that all the variables were significantly correlated with AD (p < 0.01). SEM revealed several effects on AD, including PS (β = 0.470, p < 0.01), SS (β = -0.257, p < 0.01) and MHL (β = -0.095, p < 0.01), all of which were associated with higher depression scores. SS and MHL mediated the link between PS and AD. MHL and SS exerted a negative influence on PS (β =−0.236, -0.289; p < 0.01). There was no evidence of a mediating effect of MHL on the relationship between SS and AD.
Conclusion: PS, SS and MHL have a direct effect on AD. Moreover, MHL and SS play a mediating role between PS and AD. Health care providers should be aware of the potential threat of PS progressing to AD. Under the guidance of the principles of enhancing MHL and strengthening SS, in the short term, the focus should be on improving the MHL among Chinese population.
1 Introduction
Owing to changes in hormone levels and psychosocial factors (1), antepartum depression (AD) is becoming one of the most common complications during pregnancy (2). A comprehensive review of the global prevalence of AD reported that the overall prevalence of AD is 15–65% in low- and middle-income countries (3) and 5–30% in developed countries (4). In China, the prevalence of AD is approximately 10.3%~54.8% (1, 5). This proportion might, in fact, be significantly greater due to the stigma associated with depression, which makes women hesitate to share signs of sadness and irritability (6). Moreover, they may erroneously believe that hormonal protection during pregnancy shields them from psychological disturbances, leading to depression often being overlooked or underestimated (7). AD poses potential risks to both maternal and newborn health. Not only can it lead to miscarriage, premature delivery, low birth weight, and fetal distress (8), it may also predispose infants to later life issues such as temperament difficulties in infancy, emotional and behavioral problems in childhood, and mental health problems during adolescence (9, 10). Moreover, AD has also been recognized as the strongest predictor of postpartum depression in many studies (11–13). In summary, this evidence highlights the importance of focusing on the antenatal stage for the development of preventive and therapeutic interventions (11).
There are two possible mechanisms for explaining maternal depression: biological and psychosocial. From a psychosocial perspective, the strongest predictor is severe life stress (14). Pregnancy, as a potential stressor, is characterized mainly by changes and concerns in various aspects (15) which are collectively referred to as pregnancy stress (PS). PS is a triggering factor that exacerbates depression in pregnant women (16). A previous study revealed that 6.0–16.7% of pregnant women have high levels of perceived stress, whereas 13.6–91.86% of pregnant women have mild–moderate perceived stress (17, 18). The prevalence of PS can reach 94.2% in some regions of China (19), suggesting that a significant majority of pregnant women endure PS during gestation. PS may increase anxiety and disrupt sleep quality, thereby increasing the likelihood of AD (14, 20, 21). These findings underscore the importance of identifying methods to regulate stress and prevent depression (14).
Under the framework of stress process theory, mediating factors such as social support (SS), particular behavioral strategies, and cognitive strategies in coping are key factors (14, 22). These factors can influence individuals’ subjective PS experiences, thereby shaping their subsequent actions and efficiently regulating the impact of stress during pregnancy. This theory suggests that SS significantly shapes how we perceive and handle stress (23). When we feel supported and capable of coping, stress decreases. Research results have indicated a negative correlation between SS and PS (24, 25). Low SS plays a crucial predictive role in severe PS (17). Some studies have also suggested that there is a positive correlation between greater SS and improved AD (26, 27). SS is beneficial for both physical and mental health regardless of whether an individual is under pressure (25). However, whether SS plays a mediating role in the relationship between PS and AD has been less explored.
In addition, improving health literacy (HL) has become an important goal in the field of health in China. HL is generally defined as the ability of an individual to obtain, process, and understand basic health information and services to make appropriate health decisions. HL is an important factor in determining health (28), and this importance has driven an increasing amount of research on HL. Related studies have revealed a relationship between HL and perceived stress levels (29). People with high HL have lower perceptions of stress (30). HL is also related to the incidence rate of depression (31, 32). People with low HL may fail to recognize the symptoms and signs of depression and may not seek professional help (33, 34).
However, there is a lack of research on the correlation between maternal health literacy (MHL) and AD, as well as on the correlation between MHL and SS. There have been no reports on the mediating effect of MHL on the relationship between PS and AD. Given the limited understanding of the synergistic mechanism of AD and its related factors, this study aims to construct a structural equation model (SEM) to analyze the complex relationships among AD, MHL, PS, and SS and, in particular, to explore the impact pathway of PS on AD and the potential mediating roles of MHL and SS, which can provide a theoretical basis and intervention ideas to ameliorate AD.
2 Methods
2.1 Study design and participants
This cross-sectional survey was conducted from September 2023 to February 2024 among pregnant women in Chongqing, China, using a two-stage sampling approach. In the first stage, we implemented stratified random cluster sampling across three geographical regions (1): Two districts were randomly selected from ten in northeastern Chongqing (2); One district was randomly selected from six in southeastern Chongqing (3); Three districts were selected from twenty-one in the One-Hour Economic Circle region. In the second stage, convenience sampling was used to distribute questionnaires to pregnant women at hospitals in the six selected districts during the survey period, ensuring that each pregnant woman had an equal likelihood of being selected. The inclusion criteria were as follows (1): at least 18 years old (2), permanent residence in Chongqing (3), singleton pregnancy, and (4) no cognitive dysfunction or previous history of mental disorders. During this study, the investigators explained the objectives and importance of the questionnaire survey to all participants, who provided their written informed consent and were reminded of their right to withdraw at any stage of the study. Answers to the questionnaire were collected either through face-to-face interviews or through self-administered questionnaires completed by the literate participants. A total of 1422 pregnant women agreed to participate and returned questionnaires, of which 31 questionnaires were excluded because of invalid or incomplete responses. Ultimately, 1391 valid questionnaires were included in the analysis, representing a survey completion rate of 97.82%.
2.2 Instruments
2.2.1 General information questionnaire
A baseline questionnaire was designed to collect pregnant women’s general information, such as age, maternal and paternal education, monthly family income, occupation type, week of gestation, unplanned pregnancy status, sleep status, health status, marital relationship, and whether they had gone to maternity school.
2.2.2 Antepartum depression
AD was measured via the Edinburgh Postnatal Depression Scale (EPDS) developed by Cox et al. (35) and translated into Chinese by Lee et al. (36). It has also been validated for screening depression during pregnancy (37–39). The scale consists of 10 items. Each item is scored with a value from 0–3, with possible total scores ranging from 0–30. Previous studies have established that a cutoff score of 10 on the Chinese version of the EPDS demonstrates clinical utility in identifying probable depression (20, 39). In the present study, the Cronbach’s α of the EPDS was 0.851.
2.2.3 Pregnancy stress scale
The Pregnancy Stress Scale (PSS), a self-report assessment tool devised by Chen et al. in Taiwan (40), has been extensively utilized in relevant research among pregnant Chinese women to evaluate their PS status (1, 8, 19, 20). It consists of 30 items categorized into 4 factors: parenthood recognition (15 items), maternal and child health and safety (8 items), changes in body shape and physical activity (4 items), and other stressors (3 items), each using a 4-point Likert scale (17). The average score of all the items is calculated to assess the level of prenatal stress, and higher scores indicate higher levels. The Cronbach’s α internal consistency rating of the PS in this study was 0.94.
2.2.4 Multidimensional scale of perceived social support
The Multidimensional Scale of Perceived Social Support (MSPSS) is a 12-item instrument for measuring perceived SS that was developed by Zimet et al. (41). The Chinese version of the MSPSS has shown good reliability and validity in the literature (42, 43). Participants rated their responses on a seven-point Likert response scale (from 1 = very strongly disagree to 7 = very strongly agree). The scale was divided into 3 parts: family, friends, and significant others (43). The possible scores range from 4–28 for each subscale and from 12–84 for all items, with higher scores indicating greater total perceived social support. The MSPSS had a Cronbach’s α of 0.92 in the current study.
2.2.5 Maternal health literacy questionnaire
The MHL questionnaire, developed and compiled by the China Maternal and Child Health Care Association, is based on Article 55 of Basic Knowledge and Skills of Maternal and Child Health Literacy (44, 45). This questionnaire, which is designed to assess crucial health aspects, encompasses 35 inquiries into nutrition and physical activity during pregnancy, weight management strategies, childbirth modalities, breastfeeding practices, neonatal care techniques, and numerous other vital health concerns. It is categorized into three key domains: basic knowledge of mother and infant (BKMI), consisting of 22 items; behaviors and lifestyle (BAL), with 8 items; and health-related skills (HRS), encompassing 5 items. A score of 0 denoted an incorrect answer, with the overall HL score ranging from 0–100. Participants who achieved 80% or more of the total score (≥80) were considered to have adequate HL. This threshold was established based on scientific consensus and practical considerations (1): It has been widely adopted in prior research, effectively distinguishing between individuals with strong health skills from those with limited skills (46, 47) (2); This standard was developed by adapting international practices (where 75% is commonly used for scientific literacy assessments) to China’s specific context. The slightly higher threshold reflects both the increased emphasis on fundamental health knowledge and alignment with national policy priorities, particularly the health literacy improvement goals outlined in China’s Healthy China Initiative.
2.3 Statistical analyses
EpiData 3.02 was used for double entry of questionnaires, and data processing and analysis were performed with SPSS 26.0. The general characteristics of the participants were assessed using descriptive statistics. Continuous variables are presented as the means and standard deviations, and categorical variables are presented as frequencies/percentages. Comparisons were tested using t tests, analysis of variance (ANOVA), or nonparametric tests. An IBM SPSS Amos22.0 modeling and analysis system was used to establish a path analysis diagram of the relationships among the factors. The following indices were used to evaluate the goodness of fit of the model: the comparative fit index (CFI) >0.9, adjusted goodness-of-fit index (AGFI) >0.9, goodness-of-fit index (GFI)>0.9, normed fit index (NFI) >0.9, incremental fit index (IFI) >0.9, and root mean square error of approximation (RMSEA) <0.08. P < 0.05 was considered statistically significant.
3 Results
3.1 Baseline characteristics
Among the 1422 questionnaires collected, 31 had invalid or incomplete responses and were excluded from the study. Therefore, a total of 1391 pregnant women aged between 18~44 (29.63 ± 4.15) were included in the study. The sociodemographic characteristics of the study participants are displayed in Table 1. Among the participants, 1196 (85.98%) were between 18–35 years old, and 195 (14.02%) were older than 35 years old. A total of 1213 (87.20%) lived in central urban districts, and 195 (14.02%) lived in urban areas. Most of them were Han (87.20%). In total, 1020 (73.33%) were employed, and 371 (26.67%) were housewives. The proportions of primigravidas and multiparous women were 55.72% and 44.28%, respectively. Most of them had not attended maternity school (61.68%). More than half of the participants had good sleep (67.29%), and most of the participants were in good health (72.32%).
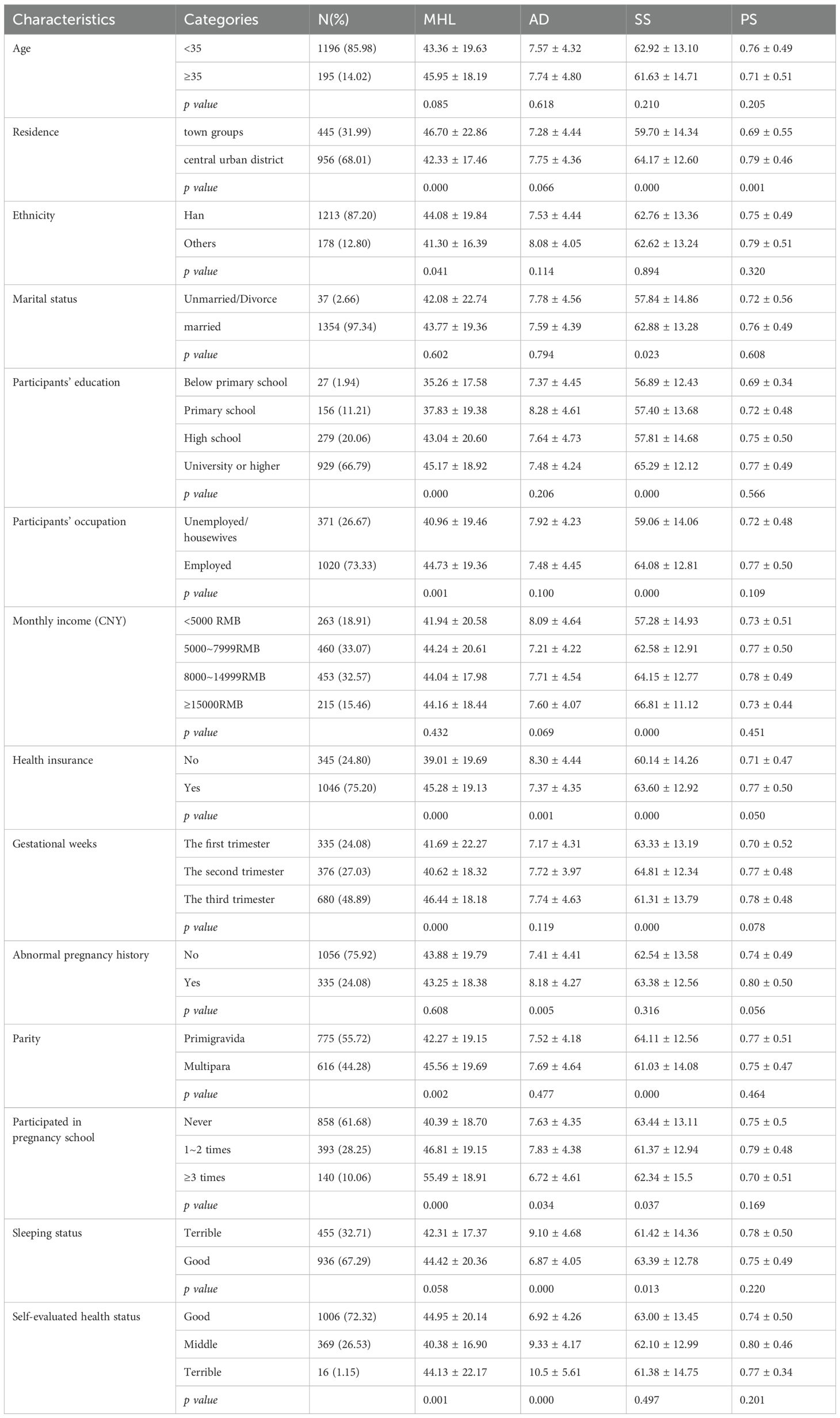
Table 1. MHL, AD, SS and PS scores of pregnant women with different demographic characteristics (n = 1391).
3.2 Maternal health literacy, antepartum depression, social support, pregnancy stress level and population distribution of scores
In this study, 82 participants (5.90%) reached the level of MHL, and 443 participants (31.85%) exhibited symptoms of AD. A total of 1287 participants (92.52%) reported stress, of which 382 (27.46%) had moderate or above stress. There were statistically significant differences in the MHL score among pregnant women, with differences in places of residence, nationality, educational level, occupation, health insurance, different gestational weeks, primigravida status, participation in maternity schools and self-evaluated health status(p < 0.05). There were statistically significant differences in AD among pregnant women with insurance, abnormal pregnancy history, participation in maternity schools, sleeping status and self-evaluated health status(p < 0.05). In addition to age, ethnicity, abnormal pregnancy history and self-evaluated health status, SS was significantly different across different demographics(p < 0.05). In contrast, PS was significantly different only in residential areas(p < 0.05), as shown in Table 1.
3.3 Description of MHL, SS, and PS with and without depression symptoms
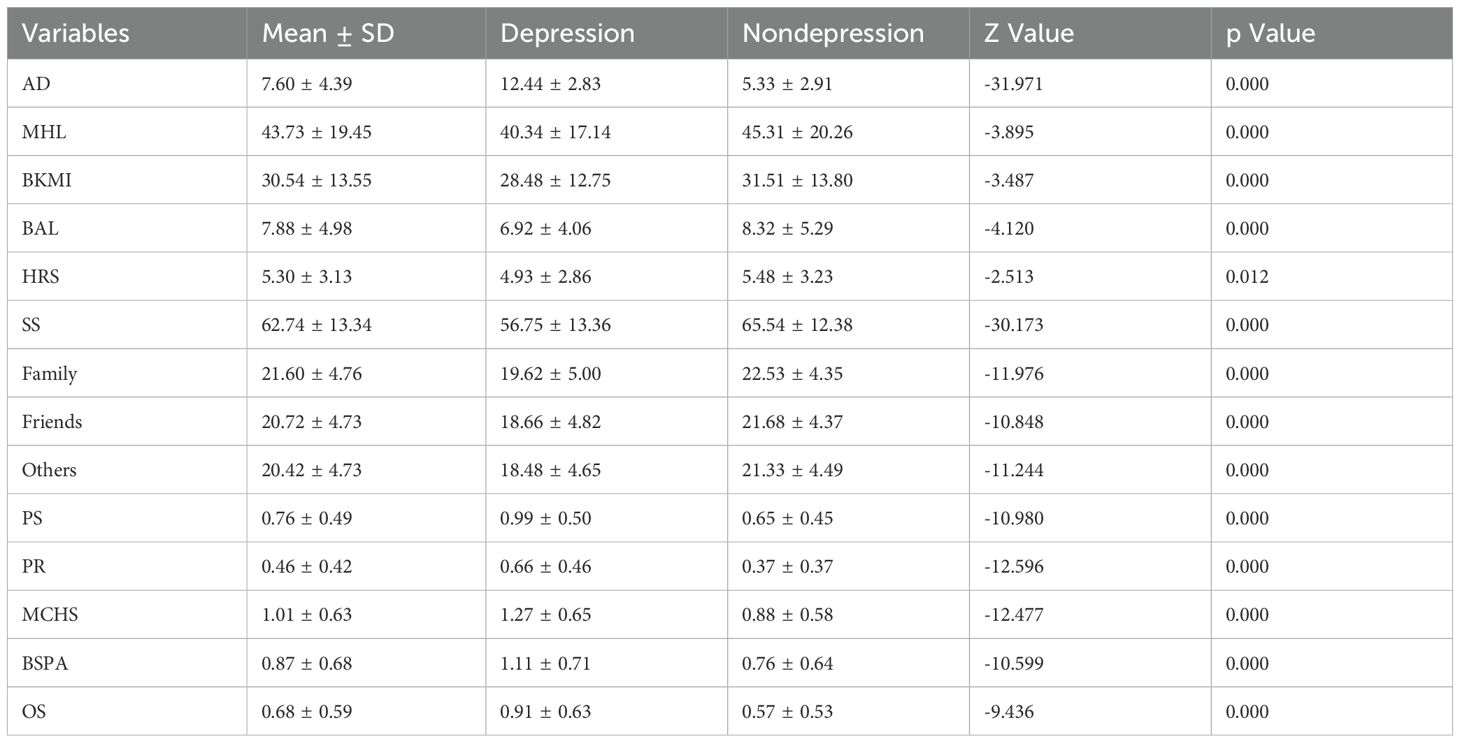
In this study, the AD score was (7.60 ± 4.39). The MHL score of pregnant women was (43.73 ± 19.45), with scores for BKMI, BAL, and HRS being (30.54 ± 13.55; 7.88 ± 4.98; 5.30 ± 3.13). The SS score was (62.74 ± 13.34), with family support, friend support, and other support scores being (21.60 ± 4.76; 20.72 ± 4.73; 20.42 ± 4.72). The PS score was (0.76 ± 0.79), with scores for PR, MCHS, BSPA and OS being (0.46 ± 0.42; 1.01 ± 0.63; 0.87 ± 0.68; 0.68 ± 0.59). Among all the variables, the difference in scores between depressed and non-depressed patients was statistically significant(p < 0.05), as shown in Table 2.
3.4 Correlations among MHL, SS, PS and AD
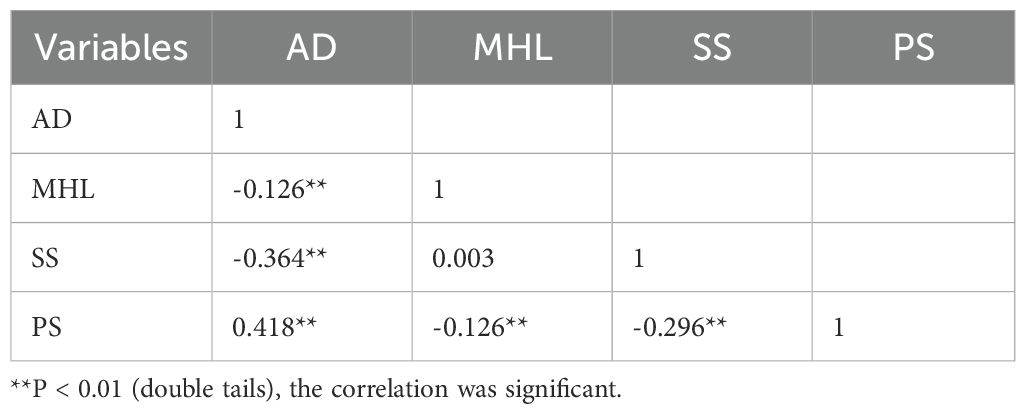
Table 3 shows the results of the spearman correlation analyses of MHL, SS, PS and AD. AD was negatively correlated with MHL and SS (p < 0.05). MHL was negatively correlated with PS (p < 0.05) but not with SS (p > 0.05). There was a positive correlation between PS and AD (p < 0.05).
3.5 Pathway analysis of AD in pregnant women
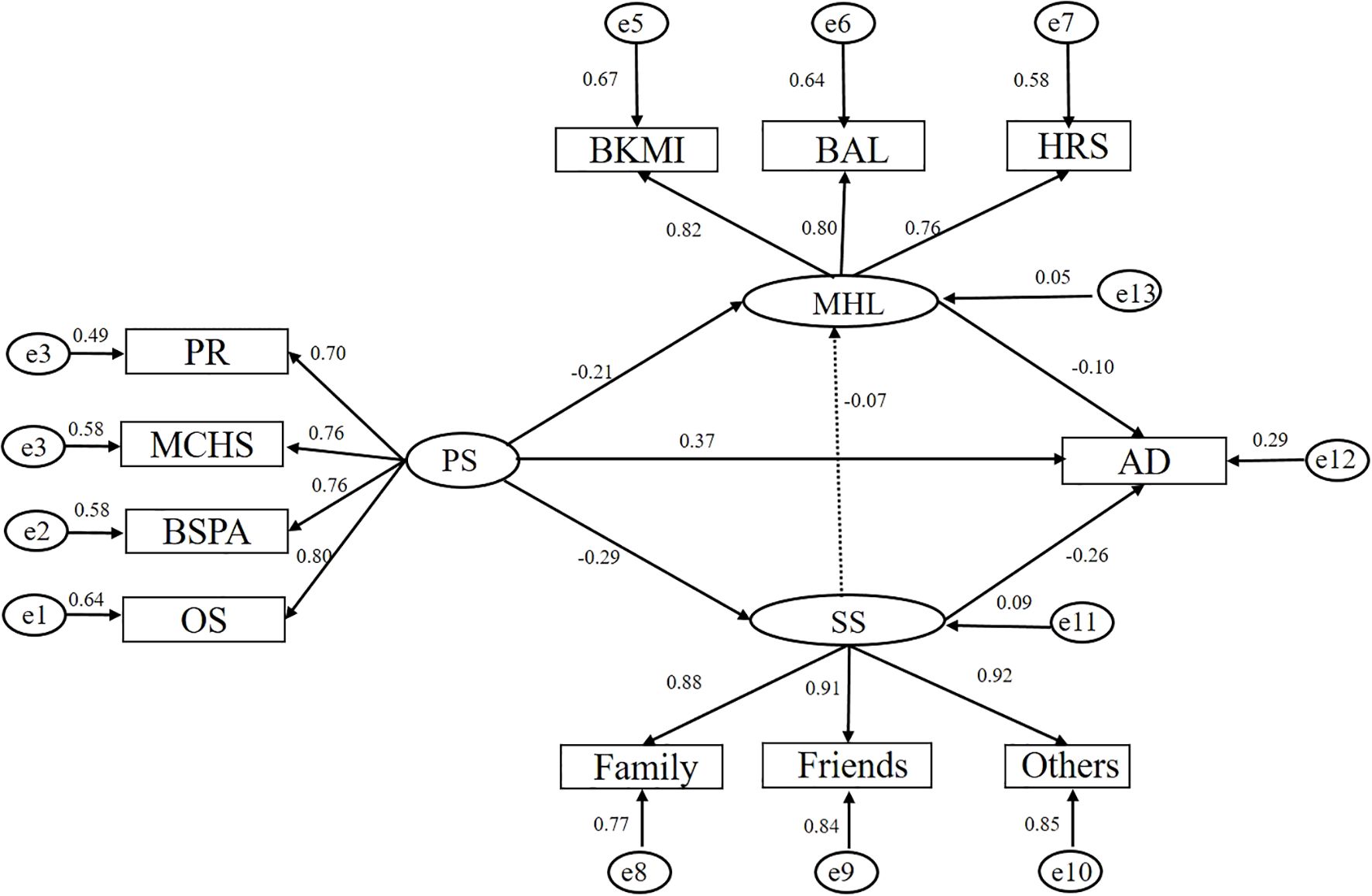
On the basis of the relevant literature and professional knowledge, a preliminary theoretical model was constructed by using the Bootstrap mediating effect test. After the analysis of the mediating effect, it was found that there was no statistically significant difference between MHL and SS(p > 0.05). Therefore, to better fit the structural model, we eliminated the direct path. Figure 1 shows the final model with standardized path coefficients that have sufficient fit. The overall fit of this model was as follows: CFI = 0.991, GFI = 0.986, NFI = 0.986, IFI = 0.991, AGFI = 0.976, RMSEA = 0.036. There were significant correlations between the observed variables and their respective latent variables, with the majority of regression weights exceeding 0.7, suggesting a strong linkage.
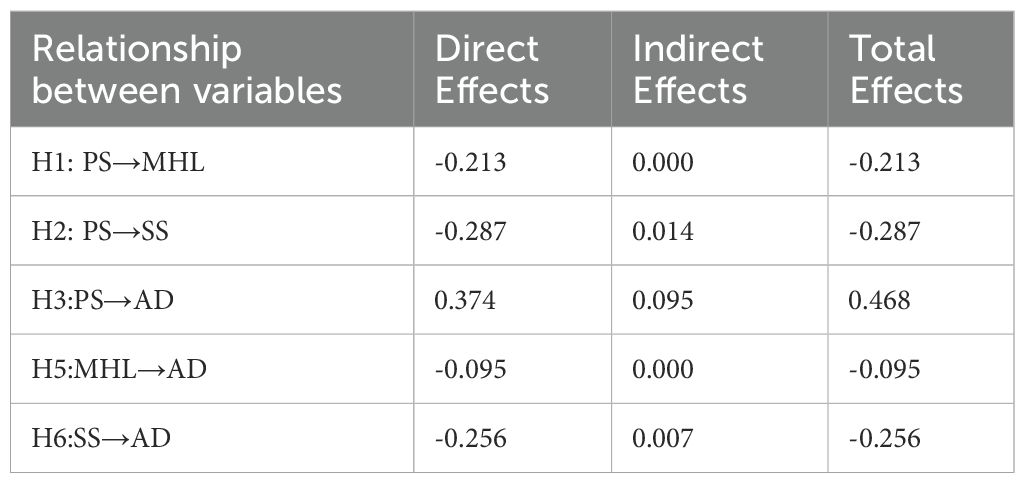
Table 4 presents the standardized coefficients of the path analysis. The results of the path analysis revealed that PS had a positive influence on AD (β = 0.375, p < 0.05) and a negative influence on MHL and SS (β =−0.236, -0.289; p < 0.05). SS had a negative effect on AD (β = -0.257, p < 0.05) but had no statistically significant effect on MHL (p > 0.05). MHL had a negative influence on AD (β =−0.095, p < 0.05). According to the analysis conducted with the latent variables, it revealed two significant mediating pathways (1): The PS→MHL→AD pathway showed an indirect effect of 0.020 (β = -0.213 × -0.095), accounting for 4.3% of the total effect (2); The PS→SS→AD pathway demonstrated an indirect effect of 0.074 (β = 0.287 × 0.257), representing 15.8% of the total effect (0.468). These findings indicate that both MHL and SS serve as partial mediators in the relationship between PS and AD, with SS exhibiting a relatively stronger mediating effect than MHL.
4 Discussion
The prevalence of AD in this study was 31.85%, which was slightly higher than that reported in a multisite survey in China (28.4%) (48) and lower than that reported in Nigeria (45.2%) (49) and Afghanistan (42.8%) (50). Experiencing major events can have significant psychological impacts (50). During a survey conducted in Urumqi, Xinjiang, China, during the COVID-19 pandemic, researchers reported that the prevalence rate of AD was 58.9% (51). Therefore, when dealing with major public health emergencies, it is imperative not only to properly execute various response efforts but also to pay attention to addressing the impact on the population’s mental health as the timely detection of and effective intervention in AD are crucial.
According to the absolute value of the path coefficient, the most important factor affecting AD was PS, which is consistent with relevant reports. Some studies in China have confirmed that the psychological stress experienced by pregnant women is a major factor in prenatal depression (14, 51). In our study, the prevalence of stress was 92.52%, of which 27.46% of participants had moderate or greater stress. The reason behind the higher PS among our study participants, compared with many similar studies conducted elsewhere, may be attributed to their heightened concerns about the impact of the COVID-19 pandemic on their own health and the well-being of their babies, especially following the comprehensive lifting of restrictions related to the pandemic in our country. Among the several dimensions of stress in our study, the scores for maternal and child health and safety were the highest. This finding also suggests that when confronted with the stressful experience of pregnancy, women inevitably harbor concerns for both their own well-being and that of the fetus, and these concerns serve as the main factors influencing pregnancy-related stress, which is consistent with the results of previous studies in China and Japan (51, 52). Hence, alleviating the psychological stress of women during pregnancy is an important factor in preventing AD.
In this research, there was a significant negative correlation between PS and SS. Previous study in China had indicated that SS not only effectively alleviates the negative emotions of pregnant women caused by adverse events but also strengthens their personal coping capabilities (11). SS plays an important mediating role between PS and AD. PS has an indirect effect on AD through SS, that is, PS may reduce an individual’s perceived SS, which in turn increases the risk of anxiety and AD. In the study, PS is negatively correlated with SS, while a lower SS is positively correlated with an increased severity of AD, indicating that PS can also indirectly affect the risk of AD. These results are consistent with existing evidence in China that inadequate social support, including lack of emotional support, or practical assistance, serves as a critical pathway linking PS to AD development (53). Moreover, the level of SS serves as a protective factor against AD; that is, the more SS that pregnant women perceive, the less severe their AD will be. This finding is inconsistent with the results reported in a previous study in China (20), but similar to those found in other studies in China as well (11). In this study, those pregnant women who did not report AD had higher scores than those of the depressed group in all three dimensions of SS. Furthermore, although family members remain the primary source of SS for pregnant women, support from friends and colleagues should not be overlooked. Relevant studies have shown that family support significantly influences the mental health of pregnant women, whereas friends and colleagues can offer additional emotional and informational support (20). Therefore, medical staff can commence from the perspective of social support; focus on the demographic characteristics that affect SS; and make full use of SS from family members, peers, medical staff, etc. These staff should provide high-risk pregnant women with information, materials, companionship, and emotional support; adjust their perception of stressors; help relieve PS; and prevent the occurrence of AD.
The results of this study indicated a negative correlation between MHL and PS. In other words, the higher the MHL is, the weaker the perception of stress. Similar findings have been reported in Greece and Iran (29, 30). Pregnant women with higher MHL tend to better understand and cope with various physiological and psychological changes during pregnancy, which enables them to effectively reduce PS. In contrast, MHL was significantly negatively associated with AD, which is inconsistent with the findings of individual study in Iran (30); nevertheless, most studies from the United States, China and Taiwan still support the idea that there is a negative correlation between HL and depression (8, 54, 55). This correlation may be because individuals with higher HL levels are able to recognize their own emotional problems or stress and actively access health information or receive help from health care providers. Additionally, path analysis revealed that MHL plays an intermediary role in PS and AD. In other words, people with HL can regulate stress in a timely manner and thus reduce the risk of depression. Therefore, health care workers during pregnancy should pay attention to improving the HL of pregnant women. Strengthening health education facilitates the provision of scientific pregnancy knowledge and psychological adjustment skills to help pregnant women establish appropriate health concepts and improve their ability to manage themselves and cope with stress.
In our research, there was no significant correlation between MHL and SS. This result is inconsistent with previous studies in China (56, 57). Prior literature suggests two possible explanations for why a correlation might be expected: first, when MHL is low, SS may compensate by filling knowledge gaps. Second, mothers with high MHL may be more adept at recognizing and utilizing SS resources, making them more likely to seek help when needed. While these mechanisms might theoretically explain a potential correlation, our findings showed no such correlation. This lack of correlation may be due to differences in the HL assessment scale. The scale used in this study was specifically designed for maternal and infant HL, which reflects the nutritional, safety, first aid and medical knowledge of pregnant women, all of which were obtained from health care professionals. However, most family members do not have a medical background in China (58). It is worth noting that in certain cultural contexts (such as Asian), the influence of social support on pregnant women may be more reflected in emotional support and practical care (e.g., specific behaviors like dietary adjustment and sharing of household chores), rather than in health information acquisition or participation in medical decision-making. These differences in support mechanisms may result in a more direct impact on behavioral compliance and psychological adaptability rather than directly enhancing health literacy. To some extent, this explains the possible reasons for the lack of a significant correlation between social support and the level of health literacy in this study. Although this study found no direct association between social support and health literacy, family support remains an important part of prenatal care. Future studies can further distinguish the types of support (such as emotional support vs. information support) and their impacts on health literacy in different dimensions. In addition, the overall level of MHL in this survey was relatively low. Follow-up studies can be grouped according to the level of MHL to further analyze the correlations among them. In light of these considerations, we plan to continue to explore the relationship between MHL and SS in future studies to reveal the intrinsic relationship more comprehensively.
5 Strengths and limitations
This study focused on multiple variables related to AD in pregnant women, including MHL, SS, and PS. Its main contribution is its groundbreaking establishment of the relationships among these variables, providing a theoretical basis and intervention directions for improving the AD situation of pregnant women. Moreover, the study adopted a standardized questionnaire to comprehensively evaluate MHL, SS, AD, and PS. This approach has created a replicable framework for future research in similar fields. However, this study also has certain limitations. First, owing to the adoption of a cross-sectional research method, this makes it difficult for us to determine the causal relationship among PS, MHL, SS and AD. It is particularly necessary to point out that when examining the mediating variables, since all the variables are measured at the same time point, we cannot clearly define the temporal sequence and dynamic change process among the variables. Future research can conduct longitudinal studies, measuring these variables multiple times at different stages of pregnancy to verify the mediating mechanism more accurately. Second, owing to the numerous questions in the questionnaire, it took a long time to obtain results. In the future, shorter versions of the questionnaires can be used. Additionally, this study relied only on one administration of the EPDS scale to assess AD and had no participation from psychiatrists in the diagnosis; since only presenting depressive symptoms were assessed, this approach may have overlooked some women with depressive symptoms, resulting in false negatives. In future research, secondary verification can be conducted in combination with clinical interviews.
6 Conclusions
In this study, we explored several factors related to AD in pregnant women. It was determined that PS, SS, and MHL directly influence AD, with PS having the most important impact and thus emerging as a pivotal factor in AD. Our research also revealed the regulatory functions of MHL and SS between PS and AD, further enriching our understanding of the intricate mechanisms underlying the mental health of pregnant women. On the basis of these findings, we provide targeted recommendations for health care providers. First, health care workers should be aware of the potential threat posed by the progression of PS to AD among pregnant women. Second, it is proposed to adopt the enhancement of MHL and the reinforcement of SS as guiding principles. Considering that SS is difficult to change in a short period, this study suggests that professional medical staff should pay attention to improving the MHL of pregnant women.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Informed written consent was obtained from all participants prior to data collection. This study was conducted according to the Helsinki Declaration and approved by the Ethics Committee of the Chongqing Health Center for Women.
Author contributions
LZ: Data curation, Formal Analysis, Investigation, Methodology, Supervision, Writing – original draft. FW: Investigation, Writing – original draft. FL: Data curation, Investigation, Writing – original draft, Writing – review & editing. XF: Investigation, Writing – original draft. HY: Investigation, Supervision, Writing – original draft. TZ: Investigation, Writing – original draft. HR: Data curation, Methodology, Writing – review & editing. CZ: Investigation, Visualization, Writing – review & editing. TL: Investigation, Project administration, Writing – original draft. LL: Project administration, Supervision, Writing – review & editing. EL: Data curation, Investigation, Writing – original draft. GD: Investigation, Writing – original draft. LR: Conceptualization, Project administration, Writing – review & editing. J-AC: Conceptualization, Project administration, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the medical research project of the Chongqing Health Commission (Grant No. 2024WSJK101).
Acknowledgments
We would like to thank the staff of the Chongqing Health Center for Women and Children, the Army Medical University affiliated hospital, Yunyang Maternal and Child Health Hospital, Xiushan Maternal and Child Health Hospital and Zhongxian Maternal and Child Health Hospital, which participated in this investigation, and the pregnant women who supported this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1600448/full#supplementary-material
Abbreviations
AD, antepartum depression; SS, social support; HL, health literacy; MHL, maternal health literacy; BKMI, basic knowledge of mothers and infants; BAL, behaviors and lifestyle; HRS, health-related skills; PS, pregnancy stress; PSS, pregnancy stress scale; MSPSS, The Multidimensional Scale of Perceived Social Support; EPDS, Edinburgh Postnatal Depression Scale; SEM, structural equation model; CFI, comparative fit index; GFI, goodness-of-fit index; NFI, normed fit index; RMSEA, root mean square error of approximation; PGFI, parsimonious goodness-of-fit index; PNFI, parsimonious normed fit index; AGFI, adjusted goodness-of-fit index; RFI, relative fitting index; IFI, incremental fit index; TLI, Tucker–Lewis index.
References
1. Gao Y, Tang X, Deng R, Liu J, and Zhong X. Latent trajectories and risk factors of prenatal stress, anxiety, and depression in southwestern China-A longitudinal study. Int J Environ Res Public Health. (2023) 20:3818. doi: 10.3390/ijerph20053818
2. Wei DM, Au Yeung SL, He JR, Xiao WQ, Lu JH, Tu S, et al. The role of social support in family socio-economic disparities in depressive symptoms during early pregnancy: Evidence from a Chinese birth cohort. J Affect Disord. (2018) 238:418–23. doi: 10.1016/j.jad.2018.06.014
3. Dadi AF, Miller ER, Bisetegn TA, and Mwanri L. Global burden of antenatal depression and its association with adverse birth outcomes: an umbrella review. BMC Public Health. (2020) 20:173. doi: 10.1186/s12889-020-8293-9
4. Mukherjee S, Trepka MJ, Pierre-Victor D, Bahelah R, and Avent T. Racial/ethnic disparities in antenatal depression in the United States: A systematic review. Maternal Child Health J. (2016) 20:1780–97. doi: 10.1007/s10995-016-1989-x
5. Ru YC. Prenatal anxiety and depression symptoms and influencing factors of pregnant women in Shenyang during Omicron virus epidemic. Master’s thesisChina Med University,Liaoning. (2023), 1–54. doi: 10.27652/d.cnki.gzyku.2023.000807
6. Marcus SM. Depression during pregnancy: rates, risks and consequences–Motherisk Update 2008. Can J Clin Pharmacol = J canadien pharmacologie clinique. (2009) 16:e15–22.
7. Bennett HA, Einarson A, Taddio A, Koren G, and Einarson TR. Prevalence of depression during pregnancy: systematic review. Obstetrics gynecology. (2004) 103:698–709. doi: 10.1097/01.AOG.0000116689.75396.5f
8. Jiang T, Tuxunjiang X, Wumaier G, Li X, and Li L. Path analysis of influencing factors for prenatal depressive symptoms in pregnant women. J Affect Disord. (2022) 317:397–402. doi: 10.1016/j.jad.2022.08.076
9. Field T, Diego M, Hernandez-Reif M, Figueiredo B, Deeds O, Ascencio A, et al. Comorbid depression and anxiety effects on pregnancy and neonatal outcome. Infant Behav Dev. (2010) 33:23–9. doi: 10.1016/j.infbeh.2009.10.004
10. Verbeek T, Bockting CL, van Pampus MG, Ormel J, Meijer JL, Hartman CA, et al. Postpartum depression predicts offspring mental health problems in adolescence independently of parental lifetime psychopathology. J Affect Disord. (2012) 136:948–54. doi: 10.1016/j.jad.2011.08.035
11. Biaggi A, Conroy S, Pawlby S, and Pariante CM. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J Affect Disord. (2016) 191:62–77. doi: 10.1016/j.jad.2015.11.014
12. Pampaka D, Papatheodorou SI, AlSeaidan M, Al Wotayan R, Wright RJ, Buring JE, et al. Postnatal depressive symptoms in women with and without antenatal depressive symptoms: results from a prospective cohort study. Arch women’s Ment Health. (2019) 22:93–103. doi: 10.1007/s00737-018-0880-8
13. Al-Abri K, Edge D, and Armitage CJ. Prospective analysis of factors associated with perinatal depression. Midwifery. (2024) 128:103871. doi: 10.1016/j.midw.2023.103871
14. Zhao H, Shi H, Chen C, Ren Z, He M, Li X, et al. Association between pregnant specific stress and depressive symptoms in the late pregnancy of Chinese women: the moderate role of family relationship and leisure hobbies. J Public Health. (2022) 28:1–12. doi: 10.1007/s10389-022-01806-z
15. Bjelica A, Cetkovic N, Trninic-Pjevic A, and Mladenovic-Segedi L. The phenomenon of pregnancy - a psychological view. Ginekologia polska. (2018) 89:102–06. doi: 10.5603/GP.a2018.0017
16. Luong TC, Pham TTM, Nguyen MH, Do AQ, Pham LV, Nguyen HC, et al. Fear, anxiety and depression among pregnant women during COVID-19 pandemic: impacts of healthy eating behaviour and health literacy. Ann Med. (2021) 53:2120–31. doi: 10.1080/07853890.2021.2001044
17. Zhang L, Huang R, Lei J, Liu Y, and Liu D. Factors associated with stress among pregnant women with a second child in Hunan province under China’s two-child policy: a mixed-method study. BMC Psychiatry. (2024) 24:157. doi: 10.1186/s12888-024-05604-7
18. Kingston D, Heaman M, Fell D, Dzakpasu S, and Chalmers B. Factors associated with perceived stress and stressful life events in pregnant women: findings from the Canadian Maternity Experiences Survey. Maternal Child Health J. (2012) 16:158–68. doi: 10.1007/s10995-010-0732-2
19. Zhang S. The course of maternal pregnancy-specific stress across pregnancy and effects on primary pregnancy outcomes: a prospective study. Master’s thesis Chinese Center Dis Control Prevention Beijing. (2017).
20. Wang Y, Gu J, Zhang F, and Xu X. Path analysis of influencing factors for maternal antenatal depression in the third trimester. Sci Rep. (2024) 14:4742. doi: 10.1038/s41598-024-55355-4
21. Faramarzi M, Kheirkhah F, Barat S, Cuijpers P, O’Connor E, Ghadimi R, et al. Prevalence and factors related to psychiatric symptoms in low risk pregnancy. Caspian J Internal Med. (2020) 11:211–18. doi: 10.22088/cjim.11.2.211
22. Wheaton B. Models for the stress-buffering functions of coping resources. J Health Soc behavior. (1985) 26:352–64. doi: 10.2307/2136658
23. Acoba EF. Social support and mental health: the mediating role of perceived stress. Front Psychol. (2024) 15:1330720. doi: 10.3389/fpsyg.2024.1330720
24. Dadi AF, Miller ER, Woodman R, Bisetegn TA, and Mwanri L. Antenatal depression and its potential causal mechanisms among pregnant mothers in Gondar town: application of structural equation model. BMC pregnancy childbirth. (2020) 20:168. doi: 10.1186/s12884-020-02859-2
25. Cohen S and Wills TA. Stress, social support, and the buffering hypothesis. psychol Bull. (1985) 98:310–57. doi: 10.1037/0033-2909.98.2.310
26. Bedaso A, Adams J, Peng W, and Sibbritt D. The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Reprod Health. (2021) 18:162. doi: 10.1186/s12978-021-01209-5
27. Khazaeian S, Kariman N, Ebadi A, and Nasiri M. The impact of social capital and social support on the health of female-headed households: a systematic review. Electronic physician. (2017) 9:6027–34. doi: 10.19082/6027
28. Health literacy: report of the Council on Scientific Affairs. Ad hoc committee on health literacy for the council on scientific affairs, american medical association. Jama. (1999) 281:552–7. doi: 10.1001/jama.281.6.552
29. Michou M, Panagiotakos DB, Lionis C, and Costarelli V. Low health literacy and perceived stress in adults: is there a link? Cent Eur J Public Health. (2021) 29:195–200. doi: 10.21101/cejph.a6692
30. Dehghani A. Association between health literacy with stress, anxiety and depression in multiple sclerosis patients: A cross sectional analytical study. Acta neurologica Taiwanica. (2024) 33:146–52. doi: 10.4103/ANT.33-4_112_0063
31. Hsu YL, Su DH, and Kuo SC. Health literacy and depression in women with type 2 diabetes mellitus. Clinics (Sao Paulo Brazil). (2020) 75:e1436. doi: 10.6061/clinics/2020/e1436
32. Zou H, Chen Y, Fang W, Zhang Y, and Fan X. The mediation effect of health literacy between subjective social status and depressive symptoms in patients with heart failure. J psychosomatic Res. (2016) 91:33–9. doi: 10.1016/j.jpsychores.2016.10.006
33. Poreddi V, Sundaram V, Reddy SN, Bidadi K, and Thimmaiah R. Postpartum depression: Mental health literacy of Indian mothers. Arch Psychiatr Nurs. (2021) 35:631–37. doi: 10.1016/j.apnu.2021.09.003
34. Fonseca A, Gorayeb R, and Canavarro MC. Women׳s help-seeking behaviours for depressive symptoms during the perinatal period: Socio-demographic and clinical correlates and perceived barriers to seeking professional help. Midwifery. (2015) 31:1177–85. doi: 10.1016/j.midw.2015.09.002
35. Cox JL, Holden JM, and Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J psychiatry: J Ment Sci. (1987) 150:782–6. doi: 10.1192/bjp.150.6.782
36. Lee DT, Yip SK, Chiu HF, Leung TY, Chan KP, Chau IO, et al. Detecting postnatal depression in Chinese women. Validation of the Chinese version of the Edinburgh Postnatal Depression Scale. Br J psychiatry: J Ment science. (1998) 172:433–7. doi: 10.1192/bjp.172.5.433
37. Zhang ZY, Yu JJ, Zeng WT, Zhou MC, Duan CC, and Zhu LL. Association between antenatal depression and adverse perinatal outcomes: a prospective cohort study. J Affect Disord. (2023) 323:490–95. doi: 10.1016/j.jad.2022.12.008
38. Choi SK, Kim JJ, Park YG, Ko HS, Park IY, and Shin JC. The simplified Edinburgh Postnatal Depression Scale (EPDS) for antenatal depression: is it a valid measure for pre-screening? Int J Med Sci. (2012) 9:40–6. doi: 10.7150/ijms.9.40
39. Lau Y, Wang Y, Yin L, Chan KS, and Guo X. Validation of the Mainland Chinese version of the Edinburgh Postnatal Depression Scale in Chengdu mothers. Int J Nurs Stud. (2010) 47:1139–51. doi: 10.1016/j.ijnurstu.2010.02.005
40. Chen CH, Chen HM, and Huang TH. Stressors associated with pregnancy as perceived by pregnant women during three trimesters. Gaoxiong yi xue ke xue za zhi = Kaohsiung J Med Sci. (1989) 5:505–9.
41. Zimet GD, Powell SS, Farley GK, Werkman S, and Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers assessment. (1990) 55:610–7. doi: 10.1080/00223891.1990.9674095
42. Wang F, Huang L, Zhang H, Jiang H, Chang X, and Chu Y. The mediating role of perceived stress on the relationship between perceived social support and self-care ability among Chinese enterostomy patients. Supportive Care cancer: Off J Multinational Assoc Supportive Care Cancer. (2021) 29:3155–62. doi: 10.1007/s00520-020-05829-8
43. Huang W, Li G, Wang D, Qu H, Tian M, and Wang Y. Postpartum depression literacy in Chinese perinatal women: a cross-sectional study. Front Psychiatry. (2023) 14:1117332. doi: 10.3389/fpsyt.2023.1117332
44. Chen J. Study on the status of maternal and infant health literacy and its impact on pregnancy outcomes in Gansu Province. Master Dissertation. Lanzhou University (2020), 1–59. doi: 10.27204/d.cnki.glzhu.2020.000973
45. Liu X. Correlation study of perinatal pregnant women’s health literacy and self-care ability. Master dissertation. Hunan Normal University (2018), 1–74.
46. Li Z, Tian Y, Gong Z, and Qian L. Health literacy and regional heterogeneities in China: A population-based study. Front Public Health. (2021) 9:603325. doi: 10.3389/fpubh.2021.603325
47. Rong H, Lu L, Wang L, Liu C, Zhang L, Li F, et al. Investigation of health literacy status and related influencing factors in military health providers of Chinese People’s liberation Army, a cross-sectional study. BMC Public Health. (2023) 23:4. doi: 10.1186/s12889-022-14958-0
48. Zhang L, Yang X, Zhao J, Zhang W, Cui C, Yang F, et al. Prevalence of prenatal depression among pregnant women and the importance of resilience: A multi-site questionnaire-based survey in mainland China. Front Psychiatry. (2020) 11:374. doi: 10.3389/fpsyt.2020.00374
49. Nwafor JI, Okedo-Alex IN, and Ikeotuonye AC. Prevalence and predictors of depression, anxiety, and stress symptoms among pregnant women during COVID-19-related lockdown in Abakaliki, Nigeria. Malawi Med journal: J Med Assoc Malawi. (2021) 33:54–8. doi: 10.4314/mmj.v33i1.8
50. Niazi AU, Alekozay M, Osmani K, and Najm AF. Prevalence and associated factors of depression, anxiety, and stress among pregnant women in Herat, Afghanistan: A cross-sectional study. Health Sci Rep. (2023) 6:e1490. doi: 10.1002/hsr2.1490
51. Tuxunjiang X, Wumaier G, Zhang W, Sailike B, Wang X, and Jiang T. The relationship between positive psychological qualities and prenatal negative emotion in pregnant women: A path analysis. Front Psychol. (2022) 13:1067757. doi: 10.3389/fpsyg.2022.1067757
52. Nakamura Y, Sato M, and Watanabe I. Positive Emotion and its Changes during Pregnancy: Adjunct Study of Japan Environment and Children’s Study in Miyagi Prefecture. Tohoku J Exp Med. (2018) 245:223–30. doi: 10.1620/tjem.245.223
53. Wang L, Yu J, Diao X, Zhang Y, Miao Y, and He W. The chain mediating effects of resilience and perceived social support in the relationship between perceived stress and depression in patients with COVID-19. Front Psychol. (2024) 15:1400267. doi: 10.3389/fpsyg.2024.1400267
54. Nutakor JA, Zhou L, Larnyo E, Addai-Dansoh S, and Cui Y. Impact of health information seeking behavior and digital health literacy on self-perceived health and depression symptoms among older adults in the United States. Sci Rep. (2024) 14:31080. doi: 10.1038/s41598-024-82187-z
55. Duong TV, Nguyen MH, Lai CF, Chen SC, Dadaczynski K, Okan O, et al. COVID-19-related fear, stress and depression in school principals: impacts of symptoms like COVID-19, information confusion, health-related activity limitations, working hours, sense of coherence and health literacy. Ann Med. (2022) 54:2064–77. doi: 10.1080/07853890.2022.2101688
56. Tang F, Zhong X, Liu S, Guo X, and Li D. Pathway analysis of the impact of health literacy, social support and self-efficacy on self-management behaviors in pregnant women with gestational diabetes mellitus. Front Public Health. (2023) 11:1188072. doi: 10.3389/fpubh.2023.1188072
57. Yumei P, Huiying K, Liqin S, Xiaoshan Z, Meijing Z, Yaping X, et al. The mediating effect of e-health literacy on social support and behavioral decision-making on glycemic management in pregnant women with gestational diabetes: a cross-sectional study. Front Public Health. (2024) 12:1416620. doi: 10.3389/fpubh.2024.1416620
Keywords: depression, stress, social support, health literacy, structural equation modeling
Citation: Zhang L, Wu F, Li F, Feng X, Yang H, Zhou T, Rong H, Zheng C, Luo T, Lu L, Lei E, Deng G, Ren L and Chen J-A (2025) The relationship between pregnancy stress and antepartum depression in Chinese pregnant women: the mediating effect of social support and maternal health literacy. Front. Psychiatry 16:1600448. doi: 10.3389/fpsyt.2025.1600448
Received: 26 March 2025; Accepted: 03 June 2025;
Published: 23 June 2025.
Edited by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranReviewed by:
Bayu Anggileo Pramesona, Lampung University, IndonesiaRania AlSabi, Putra Malaysia University, Malaysia
Copyright © 2025 Zhang, Wu, Li, Feng, Yang, Zhou, Rong, Zheng, Luo, Lu, Lei, Deng, Ren and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Ren, MTE5ODY2MDVAcXEuY29t; Ji-An Chen, Y2phdG1tdUBob3RtYWlsLmNvbQ==
†These authors have contributed equally to this work
 Ling Zhang
Ling Zhang Fanghui Wu2†
Fanghui Wu2†