- 1School of Medicine, Tongji University, Shanghai, China
- 2Affiliated Mental Health Center & Hangzhou Seventh People’s Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 3Clinical Research Center for Mental Disorders, Shanghai Pudong New Area Mental Health Center, School of Medicine, Tongji University, Shanghai, China
Background: Adolescent depression and non-suicidal self-injury (NSSI) represent significant global public health challenges, with high comorbidity rates and multidimensional adverse outcomes. Despite growing evidence on interventions, a comprehensive synthesis of strategies targeting this co-occurrence remains limited.
Aim: This scoping review systematically maps evidence-based interventions for adolescents with comorbid depression and NSSI, focusing on efficacy, mechanisms, and implementation challenges.
Methods: Following Arksey and O’Malley’s framework and PRISMA-ScR guidelines, a systematic search of English and Chinese databases (2000–2025) identified 18 studies (13 randomized controlled trials [RCTs], 3 quasi-experimental studies, and 2 other study designs). Data were extracted and synthesized to characterize intervention types, outcomes, and contextual factors.
Results: Psychotherapies, particularly dialectical behavior therapy for Adolescents (DBT-A), demonstrated robust efficacy, reducing NSSI frequency by 50% and relapse rates through enhanced emotion regulation. Family-system approaches (e.g., Satir therapy) improved family cohesion and reduced comorbid behaviors. Pharmacological agents (e.g., Selective Serotonin Reuptake Inhibitors) showed synergistic effects when combined with psychotherapy, while neuromodulation (e.g., Repetitive Transcranial Magnetic Stimulation) normalized neuroinflammatory markers. Innovations like narrative therapy facilitated identity reconstruction by externalizing NSSI as a separate entity from self-concept. Key challenges included cultural adaptability, limited long-term follow-up (≥1 year), and understudied digital intervention roles.
Conclusions: Integrated biological-behavioral interventions, culturally tailored protocols, and family-system strategies are pivotal for managing NSSI-depression comorbidity. Future research should prioritize rigorous RCTs with extended follow-up periods, community-based implementation, and digital mental health solutions to address scalability and sustainability gaps.
1 Introduction
Depressive disorders and non-suicidal self-injury (NSSI) among adolescents have emerged as pressing global public health challenges in recent decades. Major depressive disorder, characterized by persistent low mood, anhedonia, and reduced volitional activity, demonstrates particular clinical significance during the critical developmental transition of adolescence (1). According to the World Health Organization (WHO) – encompassing 194 member states across all regions – depressive disorders constitute the leading cause of disability-adjusted life years (DALYs) in adolescents worldwide, with current prevalence estimates ranging from 10% to 20% in community samples (2). A meta-analysis synthesizing 72 studies further substantiates these concerns, reporting a global point prevalence of 34% for clinically significant self-reported depressive symptoms in adolescent populations, with epidemiological trends indicating progressive escalation (3). Notably, female adolescents and those residing in Middle Eastern, African, and Asian regions demonstrate particularly elevated prevalence rates (3, 4). The clinical trajectory of adolescent depression is characterized by multidimensional impairment, including psychological distress, social dysfunction, academic decline, and reduced quality of life. Critically, this condition significantly increases suicide risk, causing substantial individual suffering and imposing considerable socioeconomic burdens on families and society (5).
Non-suicidal self-injury (NSSI) is defined as deliberate self-inflicted physical harm without suicidal intent, typically manifested through cutting, burning, or self-impact behaviors (6). Recognized as a critical clinical concern, NSSI has been included in the ‘Conditions for Further Study’ section of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), accompanied by provisional diagnostic criteria to facilitate systematic investigation (7). Epidemiological evidence highlights the elevated prevalence of NSSI among adolescents globally, with a lifetime prevalence of 19.3% (8)and 15-20% of adolescents reporting at least one self-injury episode (9). Notably, Chinese adolescents exhibit an even higher prevalence rate of 27.4% (10). Emerging data reveal significant psychiatric comorbidity patterns, particularly bidirectional associations between NSSI and depressive symptoms. A nationwide Chinese study involving 8,102 adolescents demonstrated that the NSSI group had a markedly higher depression detection rate (49.7%) compared to non-NSSI counterparts (17.7%), with females and high school students constituting vulnerable subgroups (11). Strikingly, 40% of adolescents diagnosed with major depressive disorder engage in NSSI behaviors (12), substantially exceeding population baselines.
Critically, NSSI functions not merely as a behavioral marker but as an active contributor to psychopathological progression. A multi-wave prospective study confirms that NSSI exacerbates depressive symptomatology through maladaptive feedback loops while serving as a robust predictor of subsequent suicide attempts (13). Furthermore, NSSI demonstrates strong comorbidity with anxiety disorders, post-traumatic stress disorder (PTSD), and borderline personality disorder (14, 15), collectively amplifying its burden across multiple mental health domains. These findings underscore the dual disease burden arising from the NSSI-depression syndemic and emphasize the imperative for targeted clinical interventions.
Existing interventions exhibit substantial heterogeneity (16–18). Dialectical Behavior Therapy for Adolescents (DBT-A) has demonstrated robust efficacy in reducing NSSI recurrence through emotion regulation skills (19, 20). Internet-based interventions show promise in overcoming geographical barriers, though their effectiveness in severe cases remains understudied and limited by digital divides (21, 22). A prospective randomized controlled trial revealed that individual narrative therapy maintained significant reductions in NSSI behaviors at 1-month follow-up, though therapeutic effects were moderated by familial support levels and patients’ cognitive flexibility (23). Pharmacological interventions, particularly selective serotonin reuptake inhibitors (SSRIs) and second-generation antipsychotics (SGAs), show limited target-specific evidence for NSSI reduction despite their antidepressant properties, with additional concerns regarding treatment response fluctuations and adverse effect profiles (24, 25).
Cross-cultural analyses further indicate that racial disparities in depression attribution models and treatment preferences may substantially influence intervention adherence. For instance, African American families demonstrate greater receptivity to cognitive behavioral approaches than biomedical explanations, underscoring the necessity for culturally adaptive modifications in standardized protocols (26). Notably, the social contagion effects of digital platforms on NSSI propagation remain inadequately addressed, with emerging evidence suggesting online communities may normalize self-injurious behaviors (27). Although prior systematic reviews have extensively investigated interventions for suicidal behavior (28), a significant gap persists in evidence-based strategies specifically targeting depression with NSSI behavior. Therefore, our scoping review systematically maps evidence-based interventions for adolescent depression with comorbid NSSI, employing rigorous methodology to characterize outcome measures, treatment efficacy, and implementation challenges through an interdisciplinary lens.
2 Methods
2.1 Aim
The aim of this scoping review is to systematically map evidence-based interventions for adolescent depression with comorbid non-suicidal self-injury (NSSI) and address three key research questions:
a. What interventions demonstrate efficacy in reducing depressive symptoms and NSSI behaviors?
b. How do contextual factors (e.g., cultural adaptability, interdisciplinary collaboration) influence intervention effectiveness?
c. What gaps persist in long-term outcomes, scalability, and digital health integration?
This synthesis seeks to inform translational research and optimize precision intervention frameworks through rigorous characterization of outcome measures, efficacy evidence, and implementation challenges.
2.2 Design
A scoping review is a comprehensive method following evidence-based practice principles. This methodology was selected as it allows for systematic mapping of emerging evidence in adolescent mental health interventions, particularly given the heterogeneous nature of existing studies in terms of design, population, and intervention types. Scoping reviews are uniquely suited to identify research gaps and clarify conceptual boundaries in complex, multidisciplinary fields—a critical need in this domain. It quickly helps researchers grasp the research status in a specific field, clarify the sources and types of existing evidence, summarize and analyze relevant outcomes, and identify research gaps (29). This scoping review adhered to (30) methodological framework, which comprises four core phases: a) systematically identifying relevant studies through database searches, b) applying predefined inclusion criteria for study selection, c)organizing extracted data in a structured format, and d) synthesizing findings via comprehensive thematic analysis. To ensure methodological rigor and reporting standardization, the investigation strictly adhered to the PRISMA-ScR guidelines (31), a recognized reporting framework specifically designed for scoping reviews. To enhance methodological transparency, we incorporated a brief critical appraisal of study heterogeneity (e.g., variability in sample sizes, intervention durations, and outcome measurement tools) and explicitly acknowledged limitations related to risk of bias across studies (e.g., lack of blinding in quasi-experimental designs). Given the nature of this secondary analysis which exclusively involved synthesizing published research findings, ethical committee approval was formally waived throughout the review process. The protocol for this scoping review is registered on the Open Science Framework (OSF; https://osf.io/kdb7x) with DOI: https://doi.org/10.17605/OSF.IO/QTFMZ.
2.3 Search strategy
Our search strategy spanned both English and Chinese scholarly databases to ensure comprehensive coverage of research on adolescent mental health interventions. Specifically, we queried English databases—PubMed, PsycINFO, CINAHL, Web of Science, and Scopus—as well as Chinese repositories such as CNKI and Wanfang. Moreover, by restricting our search to publications from January 2000 to January 2025, we captured a critical period marked by significant advances and evolving paradigms in adolescent mental health intervention strategies.
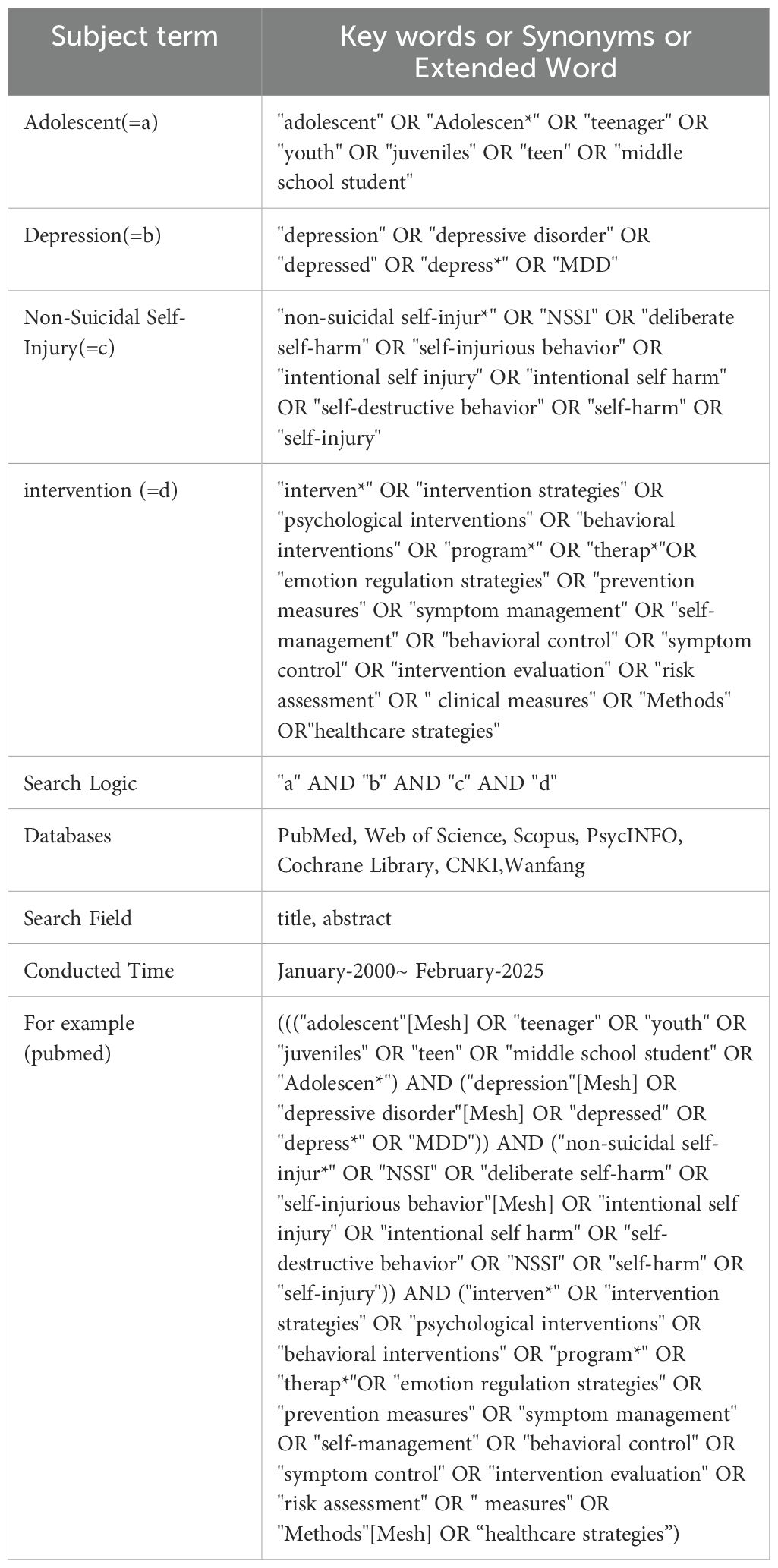
A search was conducted using both subject headings and free-text terms, and the references of the included studies were tracked. The subject headings comprised ‘adolescents’ ‘depression’ ‘non-suicidal self-injury’ and ‘intervention’. Keywords were selected by integrating MeSH terms, free-text terms, truncation, and synonyms. Boolean operators (AND, OR, NOT) were employed to construct the search strategy, ensuring both its comprehensiveness and accuracy. The detailed search strategy and the final search strategy for Web of Science are shown in Table 1. The search strategies for other databases are available from the authors on request.
2.4 Study selection
Study screening was conducted in two steps: 1) title and abstract screening and 2) full text screening. Prior to each step, the Program Manager (YBW) trains researchers to pilot test a sample of 30 studies to ensure consistency in screening. Thereafter, the project manager (FZC) rigorously monitors the screening process and provides feedback to the researchers to further improve the accuracy of the screening.
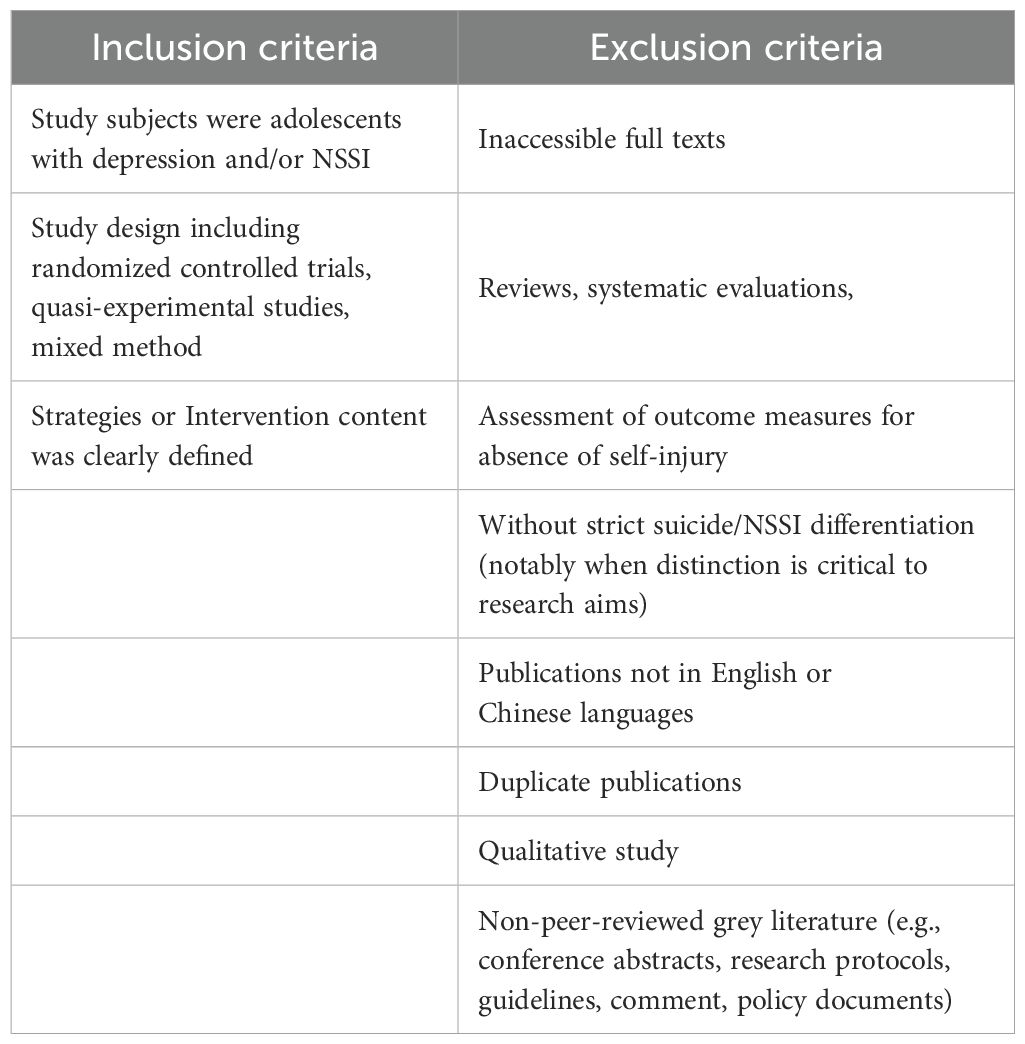
The inclusion and exclusion criteria for screening the literature are detailed in Table 2. It is important to note that a clear description of the intervention content and implementation process means that selected papers need to include specific measures and outcome indicators. If the description of the intervention is incomplete (e.g., lack of specific implementation steps or failure to report outcome indicators), the literature should be excluded. Regarding the classification of adolescent age, given the World Health Organization’s definition of adolescence as ages 10 to 19 (32), any study whose subjects fall outside this age range should be excluded. Non-peer-reviewed grey literature (for example, conference abstracts, research protocols, guidelines, opinions, case studies, policy documents) was excluded. It is methodologically justifiable to permit the inclusion of studies without strict differentiation between suicide and NSSI, particularly when the research objectives have limited relevance to the necessity of distinguishing these behavioral manifestations.
Firstly, the retrieved literature was imported into Covidence to remove duplicates. After deduplication, the initial screening of titles and abstracts was conducted. Following this initial screening, a second round of full-text screening was performed to confirm eligibility. The preliminary screening of titles and abstracts was systematically executed by four principal investigators (SHF, JB, LZ, YBW) employing a dual-reviewer verification protocol. Utilizing a paired evaluation framework, each dyad operated through coordinated workflows: the primary reviewer conducted initial eligibility assessments while the secondary researcher performed independent cross-verification, thereby maintaining methodological rigor in applying inclusion criteria. All retrieved studies received tripartite classification (‘include’; ‘exclude’; or ‘requiring further scrutiny’) through this collaborative process. Inter-rater discrepancies were addressed through structured deliberation during consensus-building sessions. For studies designated as requiring additional evaluation, the review team conducted iterative re-examinations of methodological details. When persistent interpretative variances occurred, arbitration by a senior third reviewer (with more than 5 years of systematic review experience) ensured conclusive resolution through evidence-based adjudication. A PRISMA flow chart detailing the selection process is presented in Figure 1.
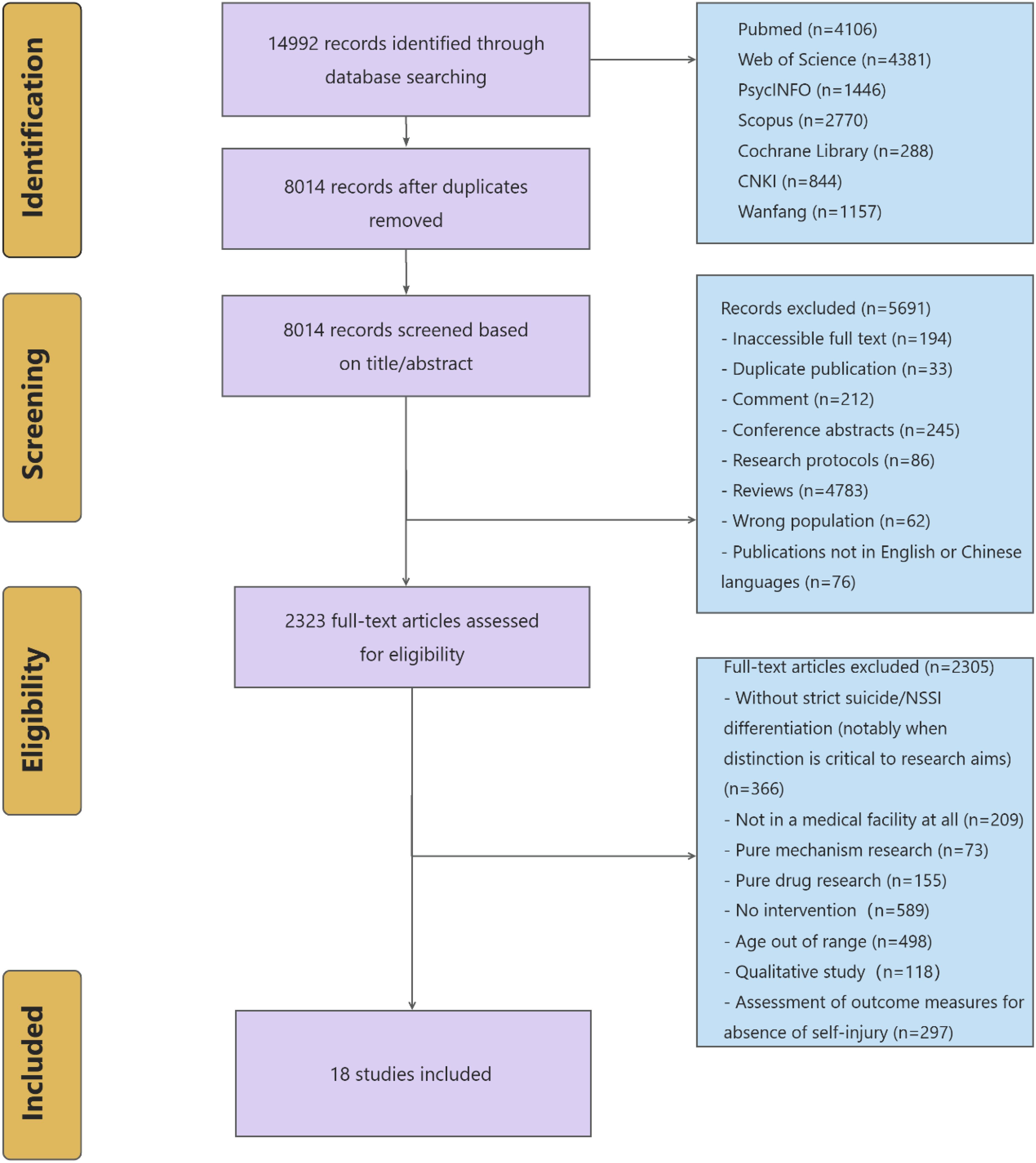
Figure 1. PRISMA flowchart of intervention of adolescent depression patients with non-suicidal self-injury behavior.
2.5 Data extraction process
A pre-pilot extraction form was implemented using Microsoft Excel to systematically document study attributes and essential details from the reviewed literature. Key variables captured encompassed bibliographic information (author, publication year, country), study design characteristics (research objectives, methodological approach, participant demographics, outcome index), risk of bias indicators (e.g., randomization procedures, blinding status, attrition rates), and intervention effect.
The extraction framework underwent iterative refinement through a preliminary testing phase led by the primary investigator, ensuring standardization of data collection parameters across all included studies. To enhance methodological rigor, the principal researcher conducted initial data extraction, followed by a cross-verification process where co-authors independently validated the accuracy and completeness of recorded information through random sampling audits. This dual-phase approach maintained consistency in data capture while minimizing procedural bias.
Additionally, while formal quality appraisal is not mandated in scoping reviews, we conducted a targeted assessment of methodological rigor using the Downs & Black checklist (33) to provide readers with insights into the strengths and limitations of included studies. The checklist assesses study quality across five subscales: reporting, external validity, bias, confounding, and power. Raters answer specific questions, with scores reflecting the study’s methodological quality. The scoping review included all studies scoring above 18, a threshold established by the tool’s authors to indicate medium to high quality (see Appendix 1).
3 Results
3.1 Selection process
The systematic search initially yielded 14992 records, with 8014 remaining following duplicate removal. Title and abstract screening identified 2323 potentially eligible articles, of which 18 studies (20, 23, 34–49) met full inclusion criteria after rigorous full-text evaluation (Figure 1).
3.2 Study characteristics
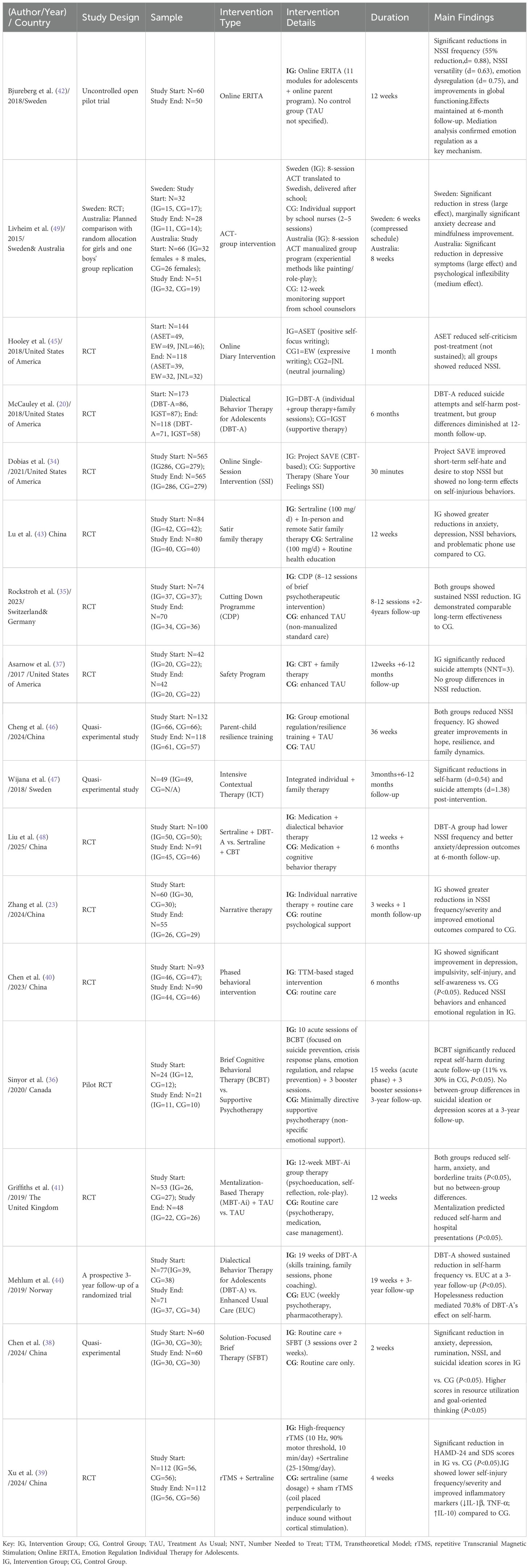
The final corpus comprised 13 randomized controlled trials (20, 23, 34–37, 39–41, 43–45, 48), three quasi-experimental investigations (38, 46, 47), and two other studies (42, 49), collectively evaluating three intervention categories: cognitive-behavioral oriented interventions (n=5), emotion regulation and acceptance-oriented intervention (n=4), family-systemic oriented intervention (n=4), postmodern/constructivist-oriented intervention (n=1), resource-oriented and goal-focused intervention (n=1), pharmacological-behavioral combined intervention (n=2), and other interventions (n=1). Sample sizes ranged from 24 to 565 participants, with longitudinal follow-up durations spanning 1 month to 4 years (Table 3).
3.2.1 Intervention providers
Clinical interventions were predominantly delivered by multidisciplinary teams (n=8, 44%) integrating psychiatrists, clinical psychologists, nurses, and social workers (e.g., DBT-A, MBT-Ai, ICT). Licensed clinical psychologists independently delivered interventions in 28% of studies (n=5), while psychiatric physician-nurse teams accounted for 22% (n=4). A minority employed single-provider models (n=1, 6%) (e.g., narrative therapy).
3.2.2 Intervention settings
Most interventions were hospital-based (n=10, 56%), primarily in outpatient clinics or inpatient wards. Community health centers supplemented delivery in 17% of studies (n=3), while 22% (n=4) utilized hybrid models combining in-person and teletherapy (e.g., remote Satir family therapy, web-based ERITA).
3.2.3 Control group configurations
Comparator arms predominantly featured treatment-as-usual (TAU) protocols (n=10, 56%), encompassing standard pharmacotherapy, health education, or supportive therapy. Sham stimulation controls (e.g., rTMS placebo) and routine psychological support accounted for 11% (n=2) and 33% (n=6) of studies, respectively.
3.3 Classification and content of intervention strategies
Based on the core theoretical framework and operational mechanisms of interventions, this study classifies the interventions as follows:
3.3.1 Cognitive-behavioral oriented interventions
Cognitive Behavioral Therapy (CBT) is a goal-oriented, systematic psychological intervention that integrates cognitive processes with behavioral strategies to help individuals modify maladaptive cognitive patterns and habitual behaviors, thereby alleviating emotional distress and mental health issues.
Short-term structured interventions grounded in CBT have gained widespread adoption due to their demonstrated efficacy and cost-effectiveness. The “Cutting Down Programme” (CDP), developed by Professor Rockstroh, employs a 10-session protocol that integrates crisis management planning with cognitive flexibility training. This intervention specifically targets maladaptive cognitive schemas and behavioral patterns associated with NSSI in adolescents, while simultaneously enhancing coping strategies and social support systems. The study found that both CDP and Treatment As Usual (TAU) showed comparable long-term effectiveness in reducing NSSI frequency (IRR=0.16), suicide attempts (IRR=0.27), and depressive symptoms (mean difference=-3.97), with no significant group differences observed (35).
Similarly, Brief Cognitive Behavioral Therapy (BCBT) (36) employs a structured protocol comprising 10 acute-phase sessions followed by 3 booster sessions. This intervention specifically targets the identification and modification of cognitive distortions and maladaptive behavioral patterns underlying self-injury, while systematically training patients in emotion regulation strategies and problem-solving skills. Empirical evidence from randomized controlled trials demonstrates that BCBT recipients exhibited significantly lower rates of recurrent self-injury during the acute treatment phase compared to control groups (OR=0.34, 95% CI [0.13–0.92]).
Chen implemented a stage-matched intervention guided by the Transtheoretical Model (TTM), deploying phase-specific strategies to address self-injurious behaviors (40). During the pre-contemplation phase, psychoeducational modules (e.g., video-based case studies illustrating long-term consequences of self-harm) were used to enhance risk perception. The contemplation phase incorporated motivational interviewing to resolve ambivalence by systematically weighing the pros/cons of behavioral change. In the preparation phase, clinicians co-developed individualized substitution behavior protocols (e.g., rubber band snapping to replace cutting) while addressing environmental triggers. The action/maintenance phase integrated family-monitored safety plans and mobile app prompts to reinforce adherence. This multi-tiered approach, combined with stage-contingent strategies (e.g., hazard restriction, family-involved contingency management), demonstrated efficacy in attenuating impulsivity and enhancing self-regulatory capacity through cognitive restructuring.
Moreover, the online single-session intervention (Project SAVE), targeting adolescents with recent self-injury, incorporates CBT principles through a 30-minute web-based program. It combines psychoeducation decoupling self-hatred from self-harm, peer testimonials on reduced self-injury, evidence-based alternative coping strategies (e.g., sensory substitution, cognitive reappraisal), and opportunities for participants to share personalized coping advice. While no significant effects on 3-month NSSI frequency were observed, short-term improvements in self-hatred (d=-0.35) and desire to stop self-harm (d=0.25) post-intervention surpassed control groups (34).
Additionally, Autobiographical Self-Enhancement Training (ASET) (45), a 28-day daily cognitive intervention, requires participants to document positive self-attributes (e.g., “I helped my neighbor today”) to reinforce self-worth and reduce self-criticism. Results show significantly lower self-criticism in ASET compared to neutral journaling (JNL) at treatment end (B=-4.31, p=0.047), with a trend toward reduced suicidal ideation at 3-month follow-up (B=-0.50, p=0.048).
3.3.2 Emotion regulation and acceptance-oriented intervention
Dialectical Behavior Therapy for Adolescents (DBT-A) integrates individual and group-based therapeutic modalities to address emotion dysregulation and maladaptive coping behaviors. Individual therapy prioritizes crisis management by collaboratively developing personalized alternative self-soothing strategies (e.g., substituting self-harm with ice-cold stimulation for physiological grounding).
Concurrently, group therapy employs a structured four-step emotion regulation protocol—comprising emotion identification, nonjudgmental acceptance of present-moment experiences, adaptive behavioral selection, and reinforcement of positive outcomes—to cultivate metacognitive awareness. Role-playing simulations are systematically integrated to enhance interpersonal efficacy and conflict resolution skills, particularly in high-stakes social contexts. Two recent randomized controlled trials (20, 44) demonstrate DBT-A’s robust efficacy: intervention cohorts exhibited a 50% reduction in self-harm frequency compared to treatment-as-usual controls, with longitudinal follow-up (3-year) data revealing 50% lower relapse rates in self-injurious behaviors. Mechanistic analyses indicate these outcomes are mediated by enhanced emotion regulation capacity (e.g., reduced physiological hyperarousal during distress) and mitigated hopelessness through value-driven behavioral activation. This evidence underscores DBT-A’s dual focus on acceptance-based validation and skills-based behavioral change, positioning it as a first-line intervention for chronic emotion dysregulation and self-injurious phenotypes.
Acceptance and Commitment Therapy (ACT) (50)targets emotion dysregulation by fostering cognitive flexibility and values-driven behavioral commitment. Core interventions include: a) mindfulness practices to enhance present-moment emotional awareness; b) cognitive defusion techniques to reduce overidentification with negative emotions; and c) values-based behavioral activation. ACT utilizes cognitive defusion and values clarification to reduce adolescent avoidance of negative emotions and enhance engagement in value-driven behaviors. In an Australian quasi-randomized trial (N = 66; females randomized to ACT or control, males non-randomized), an 8-week ACT group intervention (using experiential methods like art and role-play) significantly reduced depressive symptoms and improved psychological flexibility (49).
In addition, the Emotion Regulation and Inclusion-Based Therapeutic Approach (ERITA) is a family-system intervention combining emotion identification training with bidirectional acceptance-oriented dialogue to disrupt intergenerational cycles of emotional suppression. Its framework includes: a) emotion diary exercises for precise labeling of complex emotions (e.g., “anger mixed with disappointment”), b) family workshops teaching nonjudgmental communication (e.g., replacing “You shouldn’t feel this way” with “I notice you’ve been tired lately” to reduce shame), and c) community partnerships (e.g., school-based stress-reduction groups). A pilot study (42) showed ERITA reduced Difficulties in Emotion Regulation Scale (DERS) scores by 42% versus controls, with mechanism analyses revealing its “bidirectional acceptance” model: Parents ceased suppressing adolescents’ emotions (e.g., “Don’t cry”) and actively reshaped dialogues (e.g., shifting “Why do you fail?” to “What did this setback make you feel?”). This dual transformation resulted in a 2.1-fold reduction in severe emotion regulation deficits (baseline DERS score>35; 95% CI:1.4–3.0; p<0.01), suggesting that family-systems approaches may be particularly effective for individuals with high-severity conditions.
3.3.3 Family-systemic-oriented intervention
Family Function Training (46), involving parent-child group emotion regulation and resilience training (e.g., a 12-week modular course with gratitude, acceptance, and meaning-exploration units), positively affects adolescents’ hope, resilience, and family function. Strengthening parent-child bonds and building resilience in both adolescents and parents is a strategy that shows potential to reduce adolescents’ NSSI behavior.
Furthermore, Satir family therapy (43) utilizes role-playing and family sculpting to visualize emotional disconnections (e.g., simulating parental helplessness during self-injury), combined with non-accusatory communication protocols (e.g., reframing “you disappoint me” into “I need trust”) and crisis management strategies (e.g., collaborative “safe pause zones”). This approach not only reduces depressive/anxiety symptoms but also decreases comorbid smartphone dependency, highlighting multidimensional behavioral improvements.
Notably, the Safe Alternatives for Teens and Youths (SAFETY) program (37), a family-centered cognitive-behavioral intervention, represents the second psychosocial treatment (after I-CBT) with RCT-validated efficacy in reducing self-harm. Its framework integrates personalized safety planning, trigger identification, skill-building for adolescents and caregivers, and therapeutic consolidation, effectively enhancing family communication while lowering suicide risks. These findings underscore the multidimensional benefits of family-system approaches targeting both individual psychopathology and relational dynamics in NSSI management.
Grounded in ecological systems theory, Intensive Contextual Treatment (ICT) (47) integrates three intervention tiers:
a. Individual: Weekly CBT sessions targeting emotional regulation and cognitive flexibility;
b. Familial: Biweekly emotion-focused family therapy employing “I-statements” to replace accusatory communication;
c. Social: School-based safety plans co-developed with counselors to mitigate environmental triggers (e.g., bullying response protocols).
The trial demonstrated a 46% reduction in non-suicidal self-injury frequency (p<0.001) with moderate effect size (d=0.71), alongside improved school adaptation correlating with reduced hospitalization days. Longitudinal data revealed symptom resurgence at 12-month follow-up, highlighting the necessity for enhanced continuity of care. ICT uniquely synthesizes principles from family therapy, dialectical behavior therapy (DBT-A), and CBT through structured modules addressing emotional dysregulation, familial communication, and social functioning. Its efficacy in reducing self-harm, suicide attempts, and internalizing symptoms remains supported across extended follow-up periods, underscoring its community applicability for adolescents with suicidality.
3.3.4 Postmodern/constructivist-oriented intervention
Narrative therapy (NT), a postmodern psychotherapeutic approach, empowers adolescents with depression to deconstruct cultural oppression and rebuild self-identity by externalizing problems (e.g., reframing non-suicidal self-injury as “the pain controls you”) and reconstructing life narratives (23). Through “unique outcome” exploration, NT guides patients to recall successful non-self-injurious moments (e.g., “I managed stress without self-harm”) and reframe “exception events” (e.g., “I release emotions through exercise”), thereby enhancing self-efficacy and disrupting maladaptive identity-NSSI linkages.
3.3.5 Resource-oriented and goal-focused intervention
In addition, Solution-Focused Brief Therapy (SFBT) is a therapeutic approach that facilitates individual change through structured conversations. Core techniques include: a) normalization techniques to depathologize distress, b) empowerment techniques to amplify self-efficacy beliefs, c) exception-seeking inquiry to identify preexisting adaptive behaviors, and d) miracle question exercises to visualize goal-directed futures. By redirecting patients’ focus toward intrinsic strengths and preexisting adaptive behaviors, SFBT facilitated co-constructing solution-oriented goals (e.g., “What small step aligns with your values today?”), which catalyzed sustained improvements in affective states and behavioral patterns (38).
3.3.6 Pharmacological-behavioral combined intervention
A recent randomized trial (48) demonstrated the superior efficacy of sertraline combined with dialectical behavior therapy (DBT-A) versus cognitive-behavioral therapy (CBT) in reducing non-suicidal self-injury among adolescents with depression. The DBT-A cohort received weekly individual sessions, multifamily skills training, telephone coaching, and family therapy, while the CBT group underwent psychoeducation, emotion recognition, and behavioral activation. At 6-month follow-up, the DBT-A-sertraline group exhibited significantly greater reductions in NSSI frequency (42% vs. 28%, p<0.05) and comorbid anxiety/depressive symptoms compared to CBT-sertraline. This enhanced efficacy is attributed to DBT-A’s structured focus on emotion regulation and crisis management, synergizing with sertraline’s neurobiological effects to sustain long-term clinical improvements. The findings highlight the critical role of biological-behavioral synergy in optimizing NSSI treatment outcomes.
A study (39) demonstrated that high-frequency repetitive transcranial magnetic stimulation (HF-rTMS) combined with sertraline significantly reduced depressive symptoms and non-suicidal self-injury frequency in adolescents, concurrent with normalized inflammatory markers (↓IL-1β/TNF-α,↑IL-10; p<0.01). This dual intervention synergistically targets neuroinflammatory pathways and mood regulation circuits: HF-rTMS modulates dysfunctional neural circuitry while sertraline regulates serotonergic neurotransmission. The observed clinical improvements correlate with inflammatory rebalancing, suggesting a potential mechanistic link between cytokine modulation and behavioral outcomes. These findings highlight the therapeutic advantage of combined neuromodulatory and pharmacological approaches for NSSI-associated depression.
3.3.7 Other interventions
Mentalization-Based Therapy for Adolescents (MBT-Ai) is a specialized group therapy adapted from the original MBT introductory manual. It focuses on enhancing adolescents’ mentalizing capacity by interpreting emotions, needs, and intentions through reflective dialogues (e.g., “How did you expect others to respond to your self-injury?”) and emotion-labeling exercises. By improving psychological understanding, it aims to replace self-harm with verbal expression. The intervention covers emotional literacy, mentalization principles, and attachment patterns.
MBT-Ai consists of 12 weekly 1.25-hour sessions. It was tested in a single-blind randomized trial involving adolescents with high interpersonal conflict. Results showed that the MBT-Ai group exhibited a 42% reduction in NSSI frequency and 60% fewer emergency visits compared to the control group at 12 weeks. Improved mentalization capacity was found to mediate therapeutic effects (β=0.32, p=0.02), underscoring its pivotal role in behavioral regulation (41).
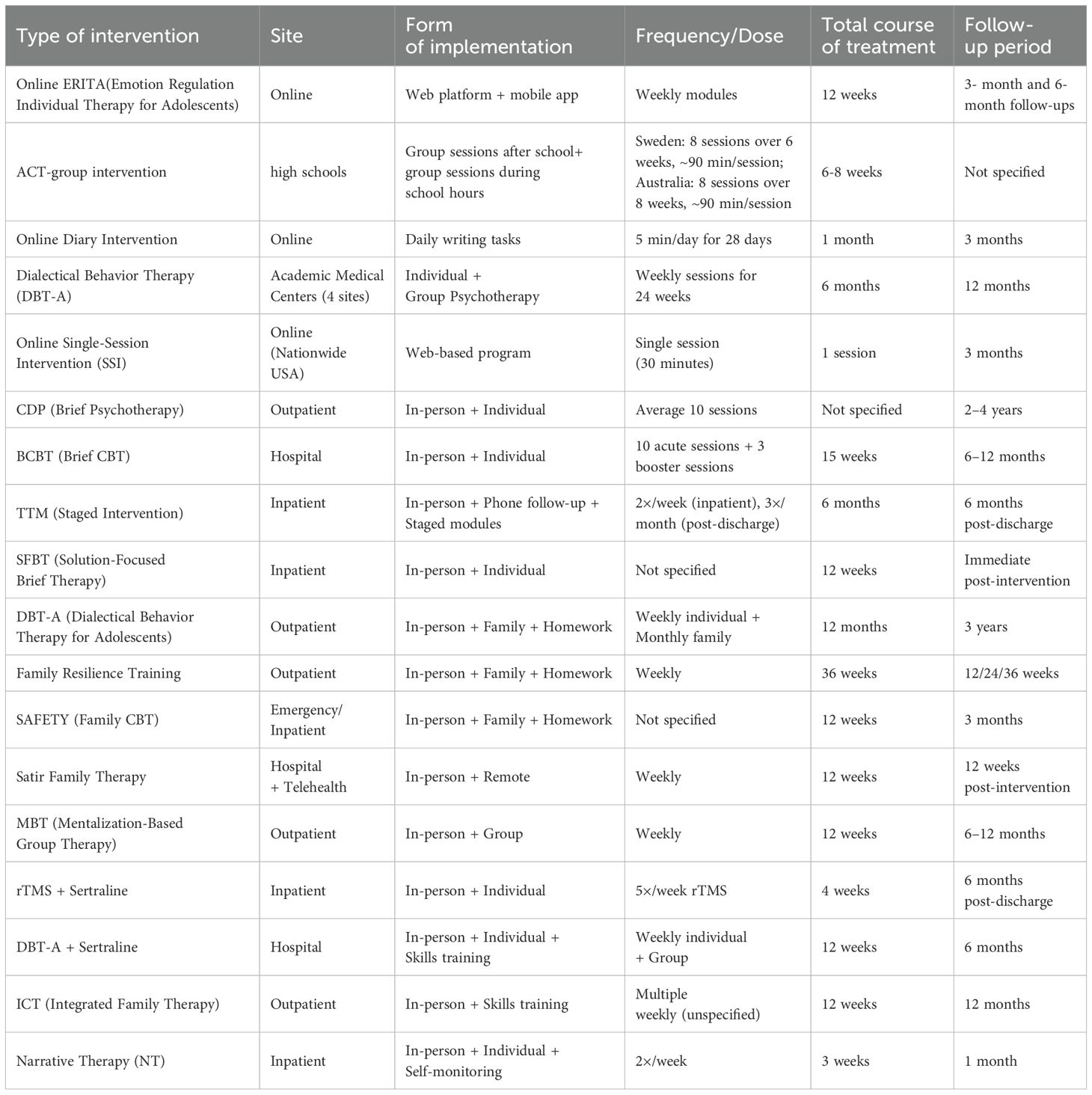
3.4 Form and dosage of implementation
Implementation modalities predominantly employ in-person formats (Table 4), including individual psychotherapy, group sessions, family interventions, and neurostimulation techniques, with limited integration of telemedicine components (43). Self-monitoring strategies utilize structured diary-keeping to document daily emotional events and positive experiences, as seen in introspective and narrative-based approaches. Family-system interventions incorporate skill-building exercises such as emotion-focused communication drills, parent-adolescent dyadic regulation training, and collaborative problem-solving tasks.
Intervention duration varies by modality: Psychosocial protocols typically adopt 8–12-week frameworks with 1–2 weekly sessions (e.g., 12-session Mentalization-Based Therapy for Adolescents, 90 minutes/session). Pharmaco-behavioral combinations maintain comparable timelines (e.g., 12-week sertraline plus DBT-A) (48). Innovative models demonstrate compressed therapeutic cycles. This structured yet flexible implementation balances therapeutic intensity, familial engagement, and clinical pragmatism.
3.5 Outcome indicators and effects
The primary outcome measures were categorized into the following domains: clinical symptoms (including depression/anxiety, impulsivity, and related psychopathologies), self-injurious behaviors (encompassing frequency/severity and recurrence rates), psychosocial functioning (assessing self-perception and social adaptation), neurophysiological biomarkers (specifically neuroinflammation-associated markers such as TNF-α, IL-1β, and related cytokine profiles), along with other therapeutic-specific parameters (Table 5).
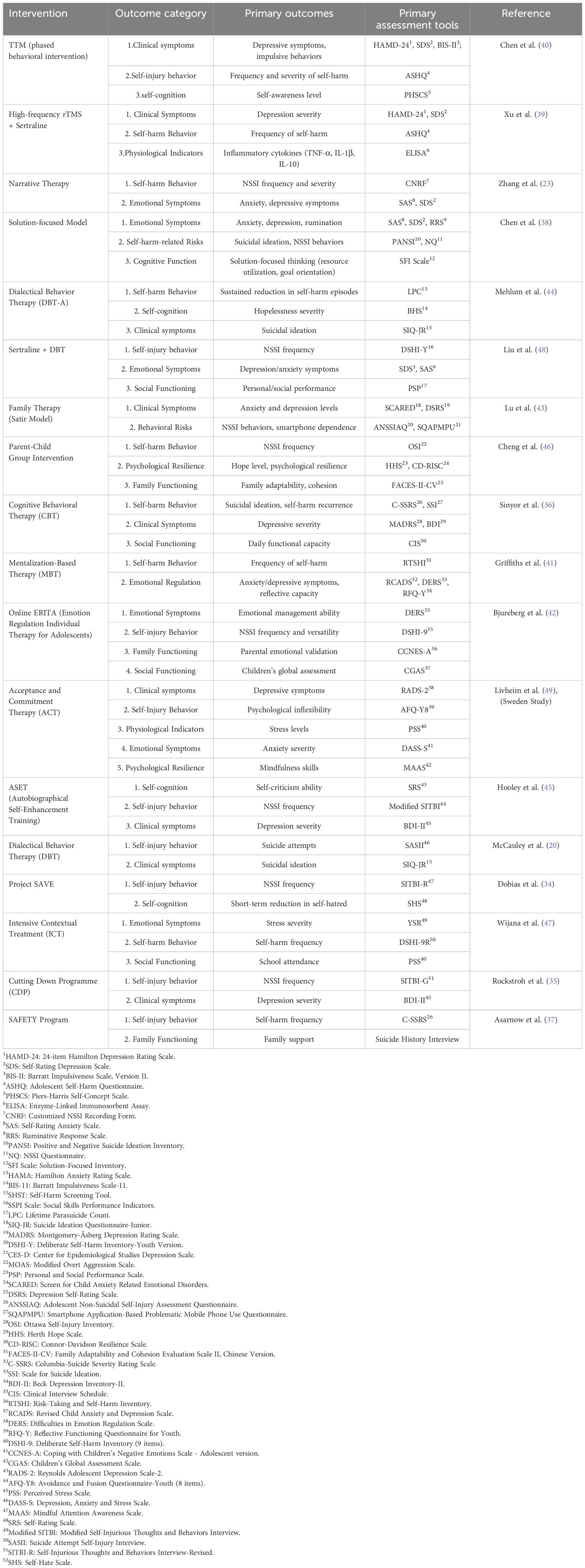
Table 5. Outcome indicators and effects of NSSI intervention strategies in adolescents with depression.
4 Discussion
This scoping review systematically synthesizes evidence on interventions targeting adolescents with comorbid depression and non-suicidal self-injury (NSSI), addressing efficacy, contextual influences, and translational gaps. Our findings reveal three key themes aligned with the research questions (RQ).
4.1 Efficacy of interventions (RQ 1)
Dialectical Behavior Therapy for Adolescents (DBT-A) emerged as a cornerstone intervention, demonstrating sustained reductions in NSSI frequency (50% reduction vs. controls) and depressive symptoms through its dual focus on emotion regulation and crisis management (20, 44). Longitudinal trials highlight DBT-A’s capacity to reduce relapse rates by 50% over three years, mediated by enhanced physiological regulation (e.g., reduced hyperarousal) and mitigated hopelessness through value-driven behavioral activation (44, 48). However, the predominance of female participants in DBT-A trials (e.g., 94.8% female in McCauley et al., 2018) limits generalizability to males, who face higher suicide mortality rates—a critical limitation noted across studies.
Family-systemic interventions, such as Satir therapy and parent-child resilience training, improved family cohesion (FACES-II-CV scores: d=0.63) and reduced comorbid behaviors like smartphone dependency (43, 46). Pharmacological agents, particularly SSRIs, exhibited limited standalone efficacy for NSSI but demonstrated synergistic potential when combined with psychotherapy (48). For instance, neuromodulation-pharmacotherapy hybrids (e.g., rTMS + sertraline) achieved inflammatory cytokine normalization alongside behavioral improvements, implicating neuroimmune pathways in NSSI-depression comorbidity (39).
4.2 Contextual influences (RQ 2)
Cultural specificity remains a barrier: Studies like Lu et al. (43) were conducted in single-center Chinese hospitals, limiting applicability to Western or diverse contexts. Cross-cultural disparities in adherence (e.g., higher dropout rates in Western online interventions vs. Asian family therapies) highlight the need for localized protocols. Narrative therapy (23), reduced NSSI severity by externalizing self-injury as a “controllable adversary” (d=0.88). However, compressed intervention durations (e.g., 3-week protocols) and reliance on hospital-based settings (56% of studies) limit generalizability to community contexts.
4.3 Critical gaps (RQ 3)
Long-term follow-up data: Only 22% of studies tracked outcomes beyond 1 year, hindering insights into sustained efficacy. Digital health integration: Despite emerging evidence for telehealth (e.g., hybrid Satir therapy in Lu et al.) (43), only 17% of studies utilized digital platforms. The social contagion effects of online communities and the efficacy of app-based interventions (e.g., Project SAVE) (34) remain underexplored.
4.4 Strengths and limitations
4.4.1 Strengths
4.4.1.1 Methodological rigor
This review strictly adhered to the PRISMA-ScR guidelines, ensuring transparency in reporting and minimizing selection bias. Dual independent screening by four researchers (with cross-verification and arbitration by a senior reviewer) was implemented during study selection, enhancing reliability in applying inclusion criteria. Multi-database coverage (PubMed, PsycINFO, CNKI, Wanfang) and dual-language screening (Chinese/English) reduced regional bias and expanded evidence capture, particularly for non-Western interventions.
4.4.1.2 Comprehensive scope
The inclusion of diverse intervention modalities (e.g., DBT-A, family therapy, pharmacotherapy) reflects real-world clinical complexity, aligning with the review’s aim to map heterogeneous evidence.
4.4.2 Limitations
4.4.2.1 Publication bias
The exclusion of grey literature (e.g., conference abstracts, unpublished trials) and non-English/Chinese studies may have omitted negative or region-specific findings, potentially skewing efficacy conclusions.
4.4.2.2 Intervention heterogeneity
Variability in intervention designs (e.g., 3-week protocols vs. longitudinal family therapies) complicates direct comparisons. While this reflects clinical diversity, it underscores the need for replication studies to establish generalizable efficacy.
4.4.2.3 Cultural and contextual gaps
Despite dual-language screening, 78% of family-system interventions were tested in East Asia (e.g., China), limiting insights into cultural adaptability for Western or low-resource settings. Notably, rural-urban disparities—particularly in mental health service accessibility—were not addressed in these trials.
4.5 Future directions
To address these gaps, we propose:
a. Longitudinal, multi-center trials prioritizing male participants and culturally adapted protocols (e.g., DBT-A modules co-designed with local communities).
b. Digital mental health frameworks integrating AI-driven chatbots for relapse prevention and blockchain-secured telehealth platforms.
c. Interdisciplinary collaboration models (e.g., psychiatrist-educator partnerships) to bridge hospital-community divides.
5 Conclusion
This scoping review advances current understanding by systematically mapping interventions for adolescent depression with comorbid NSSI across diverse cultural and methodological contexts, addressing critical translational gaps. Psychotherapy, particularly dialectical behavior therapy for adolescents (DBT-A) and family-system approaches, demonstrates robust efficacy in reducing both depressive symptoms and NSSI behaviors. Novel findings include the synergistic potential of pharmacological-behavioral hybrids (e.g., rTMS + sertraline) in modulating neuroinflammatory pathways and the culturally adaptive benefits of family-system interventions in East Asian populations. However, real-world implementation readiness varies: DBT-A and digitally hybrid models (e.g., online ERITA) show immediate scalability in clinical settings, whereas compressed protocols (e.g., 3-week narrative therapy) require further validation. Critical gaps persist in long-term outcomes (only 22% of studies tracked more than 1-year effects), equitable digital health integration (only 17% utilized telehealth), and male-inclusive trials (94.8% female in DBT-A studies). To optimize precision frameworks, clinical priorities should prioritize DBT-A and family therapies; policy efforts must address digital divides and cultural adaptation; research agendas require longitudinal, community-based trials and AI-driven relapse prevention tools. Study limitations, including publication bias toward hospital-based interventions and underrepresentation of low-resource settings, underscore the need for systematic reviews to consolidate global evidence.
Author contributions
SF: Writing – review & editing, Validation, Writing – original draft, Funding acquisition, Software, Investigation, Resources, Conceptualization, Project administration, Formal analysis, Visualization, Methodology, Supervision, Data curation. FC: Writing – review & editing, Data curation, Methodology, Supervision, Formal analysis, Project administration, Validation, Investigation, Funding acquisition, Resources. JB: Conceptualization, Resources, Validation, Investigation, Project administration, Writing – review & editing, Data curation, Methodology, Formal analysis, Writing – original draft, Software. LZ: Conceptualization, Software, Investigation, Writing – review & editing, Writing – original draft, Data curation, Project administration, Validation, Methodology. YW: Software, Validation, Writing – review & editing, Funding acquisition, Methodology, Resources, Formal analysis, Data curation, Writing – original draft, Project administration, Supervision, Conceptualization, Investigation, Visualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the STI2030-Major Projects, 2021ZD0202000 and the Shanghai Key Medical Discipline Construction Fund (No. 2024ZDXK0011) and the 2025 Shanghai Pudong New Area Health Talent Training Plan (2025PDWSYCBJ-09).
Acknowledgments
We thank all of the persons who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1601073/full#supplementary-material
Abbreviations
NSSI, Non-suicidal self-injury; DALYs, Disability-adjusted life years; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; SSRIs, Selective serotonin reuptake inhibitors; SGAs, Second-generation antipsychotics; CBT, Cognitive Behavioral Therapy; CDP, Cutting Down Programme; BCBT, Brief Cognitive Behavioral Therapy; DBT, Dialectical Behavior Therapy; TTM, Transtheoretical Model; SFBT, Solution-Focused Brief Therapy; HF-rTMS, High-frequency repetitive transcranial magnetic stimulation; ICT, Intensive Contextual Treatment; NT, Narrative therapy; MBT-Ai, Mentalization-Based Therapy for Adolescents.
References
1. Trasolini M, Serra G, Iannoni ME, Andracchio E, Apicella M, Maglio G, et al. Depression severity and verbal comprehension in children and adolescents with a major depressive episode. Front Psychiatry. (2024) 15:1395391. doi: 10.3389/fpsyt.2024.1395391
2. World Health Organization. Mental health of adolescents (2024). Available online at: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (Accessed January 23, 2025).
3. Shorey S, Ng ED, and Wong CHJ. Global prevalence of depression and elevated depressive symptoms among adolescents: A systematic review and meta-analysis. Br J Clin Psychol. (2022) 61:287–305. doi: 10.1111/bjc.12333
4. Salk RH, Hyde JS, and Abramson LY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol Bull. (2017) 143:783–822. doi: 10.1037/bul0000102
5. Rice F, Riglin L, Lomax T, Souter E, Potter R, Smith DJ, et al. Adolescent and adult differences in major depression symptom profiles. J Affect Disord. (2019) 243:175–81. doi: 10.1016/j.jad.2018.09.015
6. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th edition. Washington: American Psychiatric Publishing (2013). p. 947.
7. Buelens T, Luyckx K, Kiekens G, Gandhi A, Muehlenkamp JJ, and Claes L. Investigating the DSM-5 criteria for non-suicidal self-injury disorder in a community sample of adolescents. J Affect Disord. (2020) 260:314–22. doi: 10.1016/j.jad.2019.09.009
8. Voss C, Hoyer J, Venz J, Pieper L, and Beesdo-Baum K. Non-suicidal self-injury and its co-occurrence with suicidal behavior: An epidemiological-study among adolescents and young adults. Acta Psychiatr Scand. (2020) 142:496–508. doi: 10.1111/acps.13237
9. Moloney F, Amini J, Sinyor M, Schaffer A, Lanctôt KL, and Mitchell RHB. Sex differences in the global prevalence of nonsuicidal self-injury in adolescents: A meta-analysis. JAMA Netw Open. (2024) 7:e2415436. doi: 10.1001/jamanetworkopen.2024.15436
10. Han A, Xu G, and Su P. A Meta-analysis of characteristics of non-suicidal self-injury among middle school students in mainland China. . Chin J School Health. (2017) 38:1665–70. doi: 10.16835/j.cnki.1000-9817.2017.11.019
11. Yuan Y, Gan M, Yin X, Wu H, and Shen J. Correlation analysis between non-suicidal self-injury behavior and depressive symptoms in adolescents. Chin J School Health. (2023) 44:659–63. doi: 10.16835/j.cnki.1000-9817.2023.05.005
12. Zhong Y, Yang Y, and Liu H. Childhood trauma experiences and their impact on non-suicidal self-injury in adolescents with first episode depressive disorder. Chin J Psychiatry. (2020) 53:520–6. doi: 10.3760/cma.j.cn113661-20200107-00004
13. Scott LN, Pilkonis PA, Hipwell AE, Keenan K, and Stepp SD. Non-suicidal self-injury and suicidal ideation as predictors of suicide attempts in adolescent girls: a multi-wave prospective study. Compr Psychiatry. (2015) 58:1–10. doi: 10.1016/j.comppsych.2014.12.011
14. Cipriano A, Cella S, and Cotrufo P. Nonsuicidal self-injury: A systematic review. Front Psychol. (2017) 8:1946. doi: 10.3389/fpsyg.2017.01946
15. Reichl C and Kaess M. Self-harm in the context of borderline personality disorder. Curr Opin Psychol. (2021) 37:139–44. doi: 10.1016/j.copsyc.2020.12.007
16. Chen H, Zhou M, Han L, Manoharasetty A, Yu Z, and Luo H. Efficacy and executive function of solution-focused brief therapy on adolescent depression. Front Psychiatry. (2024) 15:1246986. doi: 10.3389/fpsyt.2024.1246986
17. English O, Wellings C, Banerjea P, and Ougrin D. Specialized therapeutic assessment-based recovery-focused treatment for young people with self-harm: Pilot study. Front Psychiatry. (2019) 10:895. doi: 10.3389/fpsyt.2019.00895
18. Dundon EL. A brief motivational intervention for adolescent depression in school based health centers. University of Connecticut, United States – Connecticut (2010). p. 138. Available at: https://www.proquest.com/docview/578521957/abstract/991EEAA998234825PQ/1 (Accessed May 18, 2025).
19. DeCou CR, Comtois KA, and Landes SJ. Dialectical behavior therapy is effective for the treatment of suicidal behavior: A meta-analysis. Behav Ther. (2019) 50:60–72. doi: 10.1016/j.beth.2018.03.009
20. McCauley E, Berk MS, Asarnow JR, Adrian M, Cohen J, Korslund K, et al. Efficacy of dialectical behavior therapy for adolescents at high risk for suicide A randomized clinical trial. JAMA Psychiatry. (2018) 75:777–85. doi: 10.1001/jamapsychiatry.2018.1109
21. Räsänen P, Lappalainen P, Muotka J, Tolvanen A, and Lappalainen R. An online guided ACT intervention for enhancing the psychological wellbeing of university students: A randomized controlled clinical trial. Behav Res Ther. (2016) 78:30–42. doi: 10.1016/j.brat.2016.01.001
22. Ma Q, Shi Y, Zhao W, Zhang H, Tan D, Ji C, et al. Effectiveness of internet-based self-help interventions for depression in adolescents and young adults: A systematic review and meta-analysis. BMC Psychiatry. (2024) 24:604. doi: 10.1186/s12888-024-06046-x
23. Zhang Y, Li X, Li M, Gao X, and Huang L. intervention effect of narrative therapy on non-suicidal self-injury in adolescents with depressive disorder: A prospective randomized controlled study. Chin J Contemp Pediatr. (2024) 26:124–30. doi: 10.7499/j.issn.1008-8830.2308030
24. Davey CG, Chanen AM, Hetrick SE, Cotton SM, Ratheesh A, Amminger GP, et al. The addition of fluoxetine to cognitive behavioural therapy for youth depression (YoDA-C): A randomised, double-blind, placebo-controlled, multicentre clinical trial. Lancet Psychiatry. (2019) 6:735–44. doi: 10.1016/S2215-0366(19)30215-9
25. Hetrick SE, McKenzie JE, Bailey AP, Sharma V, Moller CI, Badcock PB, et al. New generation antidepressants for depression in children and adolescents: A network meta-analysis. Cochrane Database Syst Rev. (2021) 5:CD013674. doi: 10.1002/14651858.CD013674.pub2
26. “Psychopharmacological treatment for depression in children and adolescents: Promoting recovery and resilience.” Positive Mental Health, Fighting Stigma and Promoting Resiliency for Children and Adolescents. (Academic Press) (2016). p. 205–35. doi: 10.1016/B978-0-12-804394-3.00011-5
27. Nesi J, Burke TA, Bettis AH, Kudinova AY, Thompson EC, MacPherson HA, et al. Social media use and self-injurious thoughts and behaviors: A systematic review and meta-analysis. Clin Psychol Rev. (2021) 87:102038. doi: 10.1016/j.cpr.2021.102038
28. Harris LM, Huang X, Funsch KM, Fox KR, and Ribeiro JD. Efficacy of interventions for suicide and self-injury in children and adolescents: a meta-analysis. Sci Rep. (2022) 12:12313. doi: 10.1038/s41598-022-16567-8
29. Riegel B, Westland H, Iovino P, Barelds I, Bruins Slot J, Stawnychy MA, et al. Characteristics of self-care interventions for patients with a chronic condition: A scoping review. Int J Nurs Stud. (2021) 116:103713. doi: 10.1016/j.ijnurstu.2020.103713
30. Arksey H and O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method. (2005) 8:19–32. doi: 10.1080/1364557032000119616
31. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
32. World Health Organization. Adolescent health (2024). Available online at: https://www.who.int/health-topics/adolescent-health (Accessed March 16, 2025).
33. Downs SH and Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. (1998) 52:377–84. doi: 10.1136/jech.52.6.377
34. Dobias ML, Schleider JL, Jans L, and Fox KR. An online, single-session intervention for adolescent self-injurious thoughts and behaviors: Results from a randomized trial. Behav Res Ther. (2021) 147:103983. doi: 10.1016/j.brat.2021.103983
35. Rockstroh F, Edinger A, Josi J, Fischer-Waldschmidt G, Brunner R, Resch F, et al. Brief psychotherapeutic intervention compared with treatment as usual for adolescents with nonsuicidal self-injury: outcomes over a 2-4-year follow-up. Psychother Psychosom. (2023) 92:243–54. doi: 10.1159/000531092
36. Sinyor M, Williams M, Mitchell R, Zaheer R, Bryan CJ, Schaffer A, et al. Cognitive behavioral therapy for suicide prevention in youth admitted to hospital following an episode of self-harm: A pilot randomized controlled trial. J Affect Disord. (2020) 266:686–94. doi: 10.1016/j.jad.2020.01.178
37. Asarnow JR, Hughes JL, Babeva KN, and Sugar CA. Cognitive-behavioral family treatment for suicide attempt prevention: A randomized controlled trial. J Am Acad Child Adolesc Psychiatry. (2017) 56:506–14. doi: 10.1016/j.jaac.2017.03.015
38. Chen H, Kang F, Li S, Bai L, Yao R, and Dong Y. Effect evaluation of a nursing intervention based on the solution-focused brief therapy in adolescents with depression. J Nurs Sci. (2024) 39:81–5. doi: 10.3870/j.issn.1001-4152.2024.07.081
39. Xu P, Wang Y, and Mao L. Effect of high-frequency repetitive transcranial magnetic stimulation combined with sertraline on depressive symptoms and self-injurious behaviors in adolescents with depression and nonsuicidal self-injury. Chin J Primary Med Pharm. (2024) 31:1149–53. doi: 10.3760/cma.j.cn341190-20230927-00238
40. Chen L, Li Y, and Li S. Effect of phased intervention to improve non⁃suicidal self⁃injury behavior in adolescents with depression. Chin Nurs Res. (2023) 37:2794–9. doi: 10.12102/j.issn.1009-6493.2023.15.022
41. Griffiths H, Duffy F, Duffy L, Brown S, Hockaday H, Eliasson E, et al. Efficacy of mentalization-based group therapy for adolescents: The results of a pilot randomised controlled trial. BMC Psychiatry. (2019) 19:167. doi: 10.1186/s12888-019-2158-8
42. Bjureberg J, Sahlin H, Hedman-Lagerlof E, Gratz KL, Tull MT, Jokinen J, et al. Extending research on emotion regulation individual therapy for adolescents (ERITA) with nonsuicidal self-injury disorder: Open pilot trial and mediation analysis of a novel online version. BMC Psychiatry. (2018) 18:326. doi: 10.1186/s12888-018-1885-6
43. Lu H, Huang Z, Zhang L, Huang X, and Li X. Influence of on emotions and behavior of adolescents with major depressive disorder. Heliyon. (2023) 9:e15890. doi: 10.1016/j.heliyon.2023.e15890
44. Mehlum L, Ramleth R-K, Tormoen AJ, Haga E, Diep LM, Stanley BH, et al. Long term effectiveness of dialectical behavior therapy versus enhanced usual care for adolescents with self-harming and suicidal behavior. J OF Child Psychol AND Psychiatry. (2019) 60:1112–22. doi: 10.1111/jcpp.13077
45. Hooley JM, Fox KR, Wang SB, and Kwashie AND. Novel online daily diary interventions for nonsuicidal self-injury: A randomized controlled trial. BMC Psychiatry. (2018) 18:264. doi: 10.1186/s12888-018-1840-6
46. Cheng J, Zhao J, Song B, Han H, Liu N, Chen Y, et al. Positive effects of parent-child group emotional regulation and resilience training on nonsuicidal self-injury behavior in adolescents: a quasi-experimental study. Front Psychiatry. (2024) 15:1343792. doi: 10.3389/fpsyt.2024.1343792
47. Wijana MB, Enebrink P, Liljedahl SI, and Ghaderi A. Preliminary evaluation of an intensive integrated individual and family therapy model for self-harming adolescents. BMC Psychiatry. (2018) 18:371. doi: 10.1186/s12888-018-1947-9
48. Liu C, Ye X, and Chen M. Sertraline medications plus dialectical behavior therapy for depressed adolescents with nonsuicidal self-injury behaviors. Suicide Life Threat Behav. (2025) 55:e13132. doi: 10.1111/sltb.13132
49. Livheim F, Hayes L, Ghaderi A, Magnusdottir T, Hogfeldt A, Rowse J, et al. The effectiveness of acceptance and commitment therapy for adolescent mental health: Swedish and Australian pilot outcomes. J Child Fam Stud. (2015) 24:1016–30. doi: 10.1007/s10826-014-9912-9
Keywords: adolescent depression, non-suicidal self-injury, scoping review, dialectical behavior therapy, family-system intervention, combined therapy, emotion regulation, neuroinflammatory pathways
Citation: Fang S, Chen F, Bian J, Zhang L and Wang Y (2025) Interventions for adolescent depression comorbid with non-suicidal self-injury: a scoping review. Front. Psychiatry 16:1601073. doi: 10.3389/fpsyt.2025.1601073
Received: 27 March 2025; Accepted: 06 June 2025;
Published: 26 June 2025.
Edited by:
Wen-Wang Rao, McGill University, CanadaReviewed by:
Say How Ong, Institute of Mental Health, SingaporeMehmet Hakan Turkcapar, Social Sciences University of Ankara, Türkiye
Britt Morthorst, University of Copenhagen, Denmark
Flávia Porto, Rio de Janeiro State University, Brazil
Trihaningsih Puji Astuti, Stikes Bhakti Mulia, Indonesia
Copyright © 2025 Fang, Chen, Bian, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanbo Wang, d2FuZ195YkB0b25namkuZWR1LmNu
†These authors share first authorship
 Shihan Fang
Shihan Fang Fazhan Chen3†
Fazhan Chen3† Yanbo Wang
Yanbo Wang