- 1Department of Psychology, East Carolina University, Greenville, NC, United States
- 2Department of Psychology, Ohio University, Athens, OH, United States
Content analysis is a critical step in understanding any mental health treatment, but these details are absent in the serious video games for ADHD literature. To better understand specific ADHD game elements, we conducted a systematic review and identified 37 seminal studies, published between February 2005 and March 2021, investigating 22 distinct ADHD games (final search on January 16, 2025) designed for children and adolescents. We coded those studies and supplementary game descriptions for therapeutic game content, then calculated effect sizes for immediate post-treatment effects on parent ratings of ADHD symptoms (i.e., far transfer), where available. There appeared to be considerable content variability across titles, but most games in this review (55%) attempt cognitive training, with pluralities deploying the go/no-go, continuous performance, and Corsi block tapping task paradigms. Nearly one-fifth (18%) of the games include theta/beta ratio neurofeedback, and more than one-quarter (27%) of the games include novel content (e.g., physical exercise, eye gaze training). Changes in parent ratings of ADHD symptoms range widely (ds = -0.55 to 1.26) without an obvious pattern of advantage for any game element. The largest far transfer effects for ADHD games are found in study results at highest risk of bias, seemingly irrespective of game content. Our findings suggest that far transfer effects are unconvincing for seminal game elements, and that new directions in ADHD game design and delivery are warranted.
1 Introduction
Serious games are designed to alter player knowledge, abilities, or behavior, rather than to simply entertain (1). In recent decades, serious video games have been designed to evaluate and treat mental illnesses, with emerging research showing some clinical benefits (e.g., 2). The most consistent finding is that serious games appeal to consumers (3) and are safe, with one product recently receiving safety clearance by the U.S. Food and Drug Administration (4). But the extent to which digital products use proven therapeutic elements is unclear. Like other treatments, the research on serious games warrants careful review and analyses before assuming any are appropriate for clinical care. To this end, we conducted a systematic review and content analysis of serious games for a high-incidence disorder to assess the clinical benefits of specific game elements.
1.1 Gamified ADHD treatments
A subset of mental health games is targeted to the symptoms, impairments, or deficits of children and adolescents with attention-deficit/hyperactivity disorder (ADHD). ADHD is a neurodevelopmental disorder characterized by persistent patterns of inattention and/or hyperactivity-impulsivity that interfere with academic, vocational, or social functioning. Serious video games for youth with ADHD (hereafter, ADHD games) might be designed to provide established assessment and psychosocial treatment (see 5), or ADHD games might deploy experimental elements, giving rise to new interventions. In either case, an ADHD game and its attributes can be contrasted with professional guidelines to determine its alignment with current best practices. Powell and colleagues (6) conducted such an analysis with popular mobile apps for ADHD by inviting children and clinicians to review app content. Interestingly, clinicians raised concerns about the lack of research support for elements within the apps and expressed disappointment that the apps were not targeted to practical needs. But this examination was limited to popular commercial products, which are not necessarily informed by scholarly research.
To assess the degree to which research-based ADHD games build on professional guidelines, it is important to contrast game content with evidence-based practices (EBPs). Treatment guidelines for ADHD have been produced by the American Academy of Pediatrics (AAP; 7), the Society for Developmental and Behavioral Pediatrics (SDBP; 8), and the Society of Clinical Child and Adolescent Psychology (SCCAP; 9). Among non-pharmacological treatments, behavioral approaches—including parent training, classroom management, and peer interventions—are strongly supported (i.e., “well-established”). Skill training interventions, like organization training, are also well established, provided those strategies target pertinent skills, provide practice over time, and include performance feedback. At lower levels of support, the professional guidelines diverge; the SCCAP identifies neurofeedback (and biofeedback more broadly) as possibly efficacious and cognitive training as experimental, whereas the AAP and SDBP withhold recommendation. In short, behavior therapy (BT) and training interventions are strongly supported, whereas neurofeedback (NF) and cognitive training (CT) may hold promise but are not as substantiated.
It appears most ADHD games in the empirical literature deliver CT and/or NF (10, 11) which warrants special consideration given the limitations in the literature. ADHD is associated with neurocognitive deficits in reaction time, sustained attention/vigilance, working memory, and response inhibition, often assessed using computerized laboratory tasks (12). Discoveries in neuroplasticity imply these deficits are corrigible (13), and that improvements in these domains can alleviate ADHD symptoms and impairments. To that end, CT and NF have been designed to engage and strengthen specific neurocognitive functions. In the case of CT, treatments typically use laboratory assessment tasks repurposed as training exercises. The challenge is that training activities that are identical to the original laboratory tasks might lead to skill improvement (e.g., digit span performance) but not neurorehabilitation in a broader sense (e.g., improved working memory). Thus, CT developers often create training experiences using modified laboratory tasks that theoretically increase the transfer of training, but the degree to which a validated laboratory task can or should be modified for training purposes is unknown (14).
In recent decades researchers have attempted to gamify both CT and NF tools to increase user engagement and motivation. The resulting tools mostly improve user performance on laboratory measures, but rarely produce real-world outcomes observable by parents or teachers (15, 16)—a distinction referred to as near versus far transfer. In short, behavior changes in domains that closely resemble a training task are considered “near” transfer, and behavior changes in domains unlike a training task are considered “far” transfer (17). The failure for ADHD games to consistently achieve far transfer beyond game-like situations is still not understood. One potential explanation is that, despite an association with ADHD, neurocognitive deficits may be irrelevant to clinical outcomes (i.e., correlation ≠ causation) (18). Alternatively, because neurocognitive dysfunction varies considerably between individuals (19), each tool may only benefit specific ADHD subpopulations. Or current tools may not effectively target the core processes impaired in ADHD. Games billed as “cognitive training” or “brain training” for ADHD could be comprised of activities targeting secondary or even unrelated processes (20). In any event, it is critical that treatments deliver meaningful, real-world behavior change at home or school, and CT/NF efforts generally appear to fall short.
1.2 ADHD game elements
By operationalizing practices like CT, NF, and BT, it is possible to categorize ADHD game content. Clearly not all BT lend themselves to easy gamification (e.g., parent training), but training interventions (5, p. 730), like time management and organization skills coaching for children, seem particularly well-suited to gameplay. Training interventions target the functional impairments associated with ADHD and can be readily operationalized based on the skills taught (e.g., organization training). NF is also relatively straightforward to operationalize given its distinguishing targets and instrumentation (e.g., electroencephalography) (21). But the cognitive abilities targeted by CT, like working memory and response inhibition, are subjectively categorized. Moreover, it is difficult, if not impossible, to examine or remediate a cognitive process in isolation (12). So, rather than identifying the latent processes that CT games putatively target, we believe it is most useful to identify the laboratory task paradigms deployed in each. For example, “visuospatial memory” is ambiguously defined, but the Corsi block tapping task, often used to measure it, is readily identifiable. Game elements approximating these tasks are informed by the research literature, whereas unique and innovative content can be judged novel (i.e., untested prior to gamification).
ADHD games have been reviewed many times, but there are two major limitations with these previous efforts. First, most ADHD games do not advance beyond early development stages (e.g., proof-of-concept), and yet reviewers rarely distinguish between nascent efforts and influential games that garner widespread scholarly attention. And second, only one study to date has attempted to examine game content (6), and that effort was limited to popular mobile apps. A content analysis is consistent with the experimental therapeutics approach to treatment development promoted by the National Institute of Mental Health because it provides clarity regarding both target mechanisms (e.g., working memory) and their associated clinical effects (e.g., symptom reduction) (22). Content analysis is a critical step in understanding any mental health treatment (23), but this information is conspicuously lacking in the ADHD games literature.
1.3 The present study
We pursued three primary aims (1): identify seminal ADHD games repeatedly cited in published, systematic reviews (2); categorize the therapeutic content within these games; and (3) determine the game elements associated with the most promising effects on parent ratings of ADHD symptoms (i.e., far transfer). Many of the games reviewed are proprietary or limited to use outside the United States, so we were unable to play most ourselves. Instead, we relied on a systematic review to identify the games, then synthesized the data from repeatedly cited studies, and corroborated our results with the study authors. We discuss what our results suggest about the ADHD games literature and then offer our recommendations for advancing this research, particularly as it applies to school-based intervention efforts.
2 Method
The current project was supported in part by a grant to East Carolina University and Ohio University (R324A180219), and we adhered to the most recent Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA; 24) for systematic reviews (see Supplementary 1). Data generated from this review, including details regarding our inclusion/exclusion decisions, are available at https://osf.io/x4e6f/.
2.1 Search strategy
To identify seminal ADHD games in the research literature, we first searched for systematic reviews and meta-analyses using OneSearch. OneSearch is a library search engine that scans dozens of interprofessional databases and local digital library materials simultaneously, while minimizing duplications. Our search phrase specified the diagnosis (“ADHD”), clinical focus (“intervention OR treatment OR training OR therap*”), delivery mechanism (“computer* OR digital* OR technolog*”), format (“game OR gamification”), and study type (“meta-analysis OR systematic review”).1 We noted a three-year gap between reviews from 2015 to 2018 (cf. 11), followed by a surge that seemed to mark new interest in ADHD games. As a result, we limited our search to the period from January 1, 2018, to December 31, 2024, to capture the recent spate of systematic reviews and meta-analyses (but did not apply any date restrictions to constituent studies).
The first author screened all candidate reviews using the titles and abstracts and omitted reviews clearly unrelated to our topic. The retained papers were then read by two or more co-authors and selected based on the following inclusion/exclusion criteria: (a) published in a peer-reviewed journal; (b) reports a unique systematic review and/or meta-analysis; (c) focuses specifically on ADHD rather than a range of conditions; and (d) focuses on studies of game-based interventions for children or adolescents. Once a set of suitable reviews was identified, all constituent studies were listed. We then excluded individual studies that (e) appear in only one review; (f) are not an efficacy, effectiveness, nor feasibility study of an intervention; (g) do not involve a computer-delivered game; (h) do not include school-age participants with ADHD; or (i) was not published in a peer-reviewed journal. We focused on repeatedly cited studies (criterion e) to ensure that the publications are seminal within this literature. Citation analysis is a common bibliometric technique for identifying key publications (25), which was vital in this case because game studies often involve exploratory and transitory technologies. By relying on citation across multiple, independent review teams, we also avoided definitional challenges around disputed terms like “serious games” and “gamification” (see 26). Dyads of co-authors then independently read each candidate study and applied the remaining criteria (f-i) to remove irrelevant or non-refereed sources. Disagreements were settled by the first author.
2.2 Game content
When necessary, we collected supplemental game descriptions from additional sources referenced in the articles or by searching scholarly databases for product descriptions, game overviews, or secondary publications using the game title as a search term (see Supplementary 2). For clarity, games that have undergone title changes were combined and attributed to the most recent title (e.g., EndeavorRx). We then coded the specific game elements intended to have clinical impact based on definitions of established assessment and treatment practices. To guide this work, we iteratively developed a codebook that functioned as a review protocol (see Supplementary 3). The most challenging step was operationalizing CT tasks. As a starting point, we relied on the review by Molitor and Langberg (27) to identify the task paradigms in the ADHD literature, and then operationally defined the tasks tested most often. When gamified, laboratory tasks are often altered (e.g., moving targets in the Corsi block-tapping paradigm), so in addition to our definitions we listed likely modifications. Game elements asserted to be therapeutic that were unlike our codes were reviewed by the team, compared to the relevant literature, and either added to our codebook or deemed “novel” if no precedent could be identified.
Interrater agreement was assessed using the AC1 statistic, given our two-rater design and anticipated marginal heterogeneity (28), as estimated by the irrCAC package (29) in R (30). The AC1 statistic is a chance-adjusted coefficient that can be interpreted similarly to a generalized kappa, with values > 0.80 indicating strong agreement. We then emailed the corresponding author for each CT study in our review to corroborate our findings, given the challenges defining those elements. We were prepared to update our findings if authors provided a compelling rationale; otherwise, we report our conclusions based on our reading of the published game descriptions (author response rate and feedback described below).
2.3 Magnitude of effects
To identify promising game content, we converted outcomes into a standardized metric (Cohen’s d). A wide variety of instruments are reported in the ADHD games literature (e.g., CT lab measures, rating scales, actigraphy measures) from a mix of within- and between-subjects designs, but parent ratings of ADHD symptoms are commonly used to measure far transfer. Hence, we focused on parent ADHD ratings and report d-family effect sizes where sufficient data were available. In two instances, researchers report parent ratings using the original Behavior Rating Inventory of Executive Function (BRIEF; 31) instead of ADHD symptoms. The BRIEF can discriminate between children with inattentive and hyperactive-impulsive symptoms (32), so we included those findings in cases where no ADHD symptom measure was reported.
To compute d, we used the tools provided by Lenhard and Lenhard (33). 2 For single-group or nonequivalent groups pre-post designs we calculated a repeated measures effect, and for pre-post control designs we calculated the Time × Treatment interaction effect. In some instances, effect sizes were only depicted in graphs, and we used a data extraction tool to inform those calculations (WebPlotDigitizer; 35). In all cases, we focused on groups with ADHD and ignored non-ADHD comparison groups, if included. We limited our calculations to immediate pre-post treatment effects, ignoring follow-up measurement occasions, given the variety of designs and follow-up times in this literature. As part of these efforts, we also assessed the risk of bias specific to parent rating outcomes, using tools provided by Cochrane. Specifically, we used the Revised Risk of Bias tool (RoB2; 36) for randomized trials, and the Risk of Bias in Non-randomized Studies of Interventions tool (ROBINS-I; 37) for non-randomized studies. RoB2 ratings were supported using spreadsheet applications that apply the standard scoring algorithms, as provided by Cochrane (beta ver. 7). To make the results of the RoB2 and ROBINS-I instruments directly comparable, we relabeled the “serious” and “critical” risk of bias determinations on the latter as “high” risk but provide our original determinations in the Supplementary Materials. Following online training on the instruments, the first author rated all studies reporting parent ratings and the last author independently rated a randomly selected subset of articles to assess consistency.
3 Results
Our search for literature reviews and meta-analyses, last conducted on January 16, 2025, returned 87 publications (see Figure 1), with most cross-listed in the Scopus (n = 53), PubMed (n = 31), and IngentaConnect (n = 30) databases. In the title screening process, we were able to exclude five duplicates and another 29 articles that were unavailable in English or clearly unrelated to ADHD games (e.g., focused on other medical conditions, game addiction). We then evaluated the remaining 53 articles using our inclusion/exclusion criteria (a-d) to identify reviews of ADHD games for children and adolescents (exclusion decisions are detailed in Supplementary 5). Our efforts identified five meta-analyses (38–42), six systematic reviews (10, 43–47), one scoping review (48), one mapping review (49), and one quasi-systematic review (50), for a total of 14 reviews reporting on 487 partially overlapping studies. The systematic review by Zheng and colleagues (47) appears in arXiv, an online repository for preprint manuscripts and was not peer-reviewed, but we included this manuscript because it appeared to be high-quality, potentially publishable, and already cited 29 times at the time of our review.
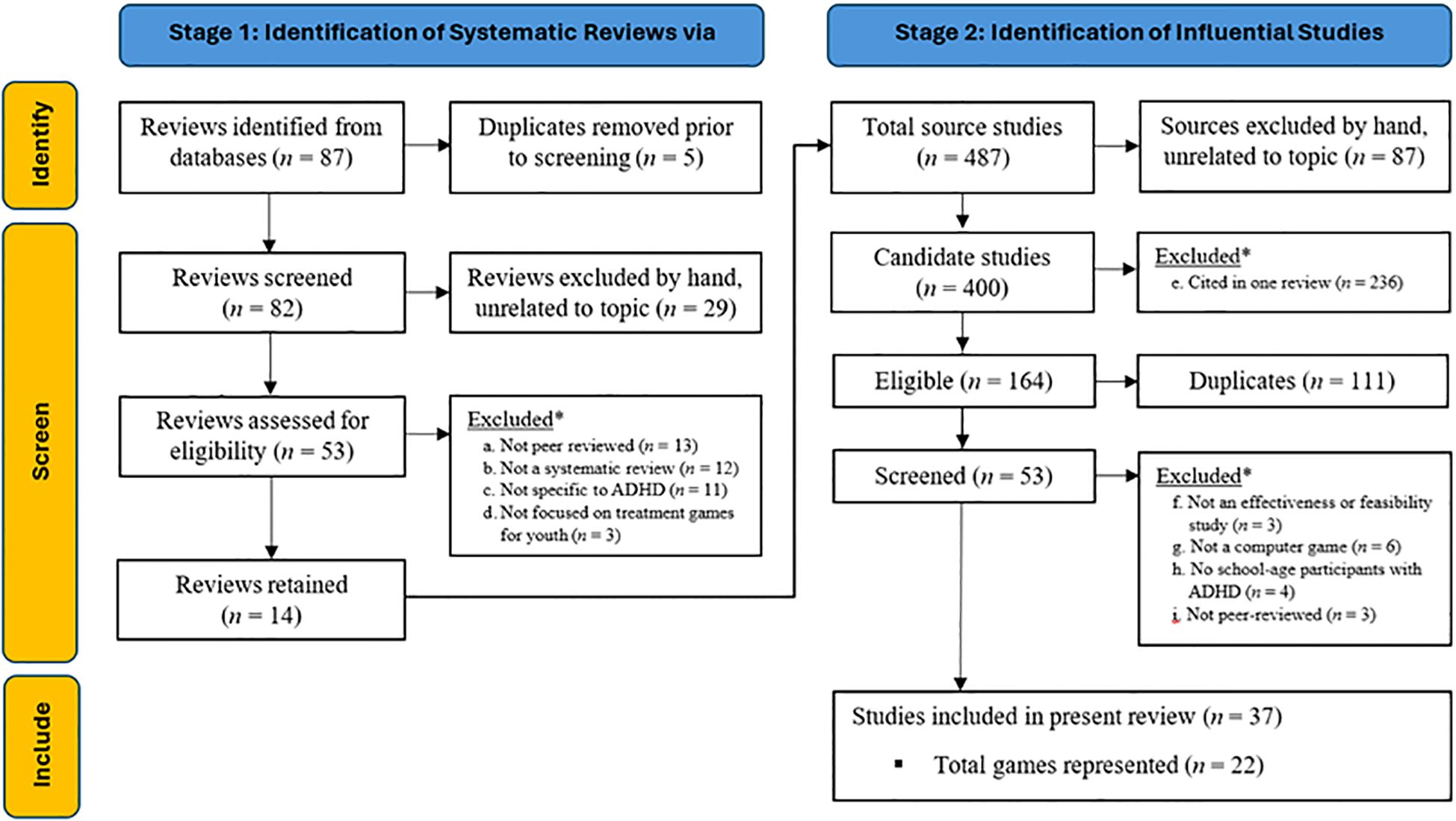
Figure 1. Flow Diagram of Two-stage Literature Review Process to Identify Influential Studies of ADHD Games.
We were able to remove 87 constituent studies based on reviewers’ descriptions; specifically, Rodrigo-Yanguas and colleagues’ (50) “quasi-systematic” review included expert opinion papers, narrative texts, case reports, and review articles that we omitted (and that did not overlap the other reviews). In the remaining 400 candidate studies, we excluded another 236 sources that were only cited in a single review (criterion e). We then applied our final exclusion criteria (f-i) as shown in Figure 1 to arrive at 37 repeatedly cited studies, published between February 2005 and March 2021, describing 22 games (51–87; all decisions and reviewer notes are provided in the accompanying dataset).
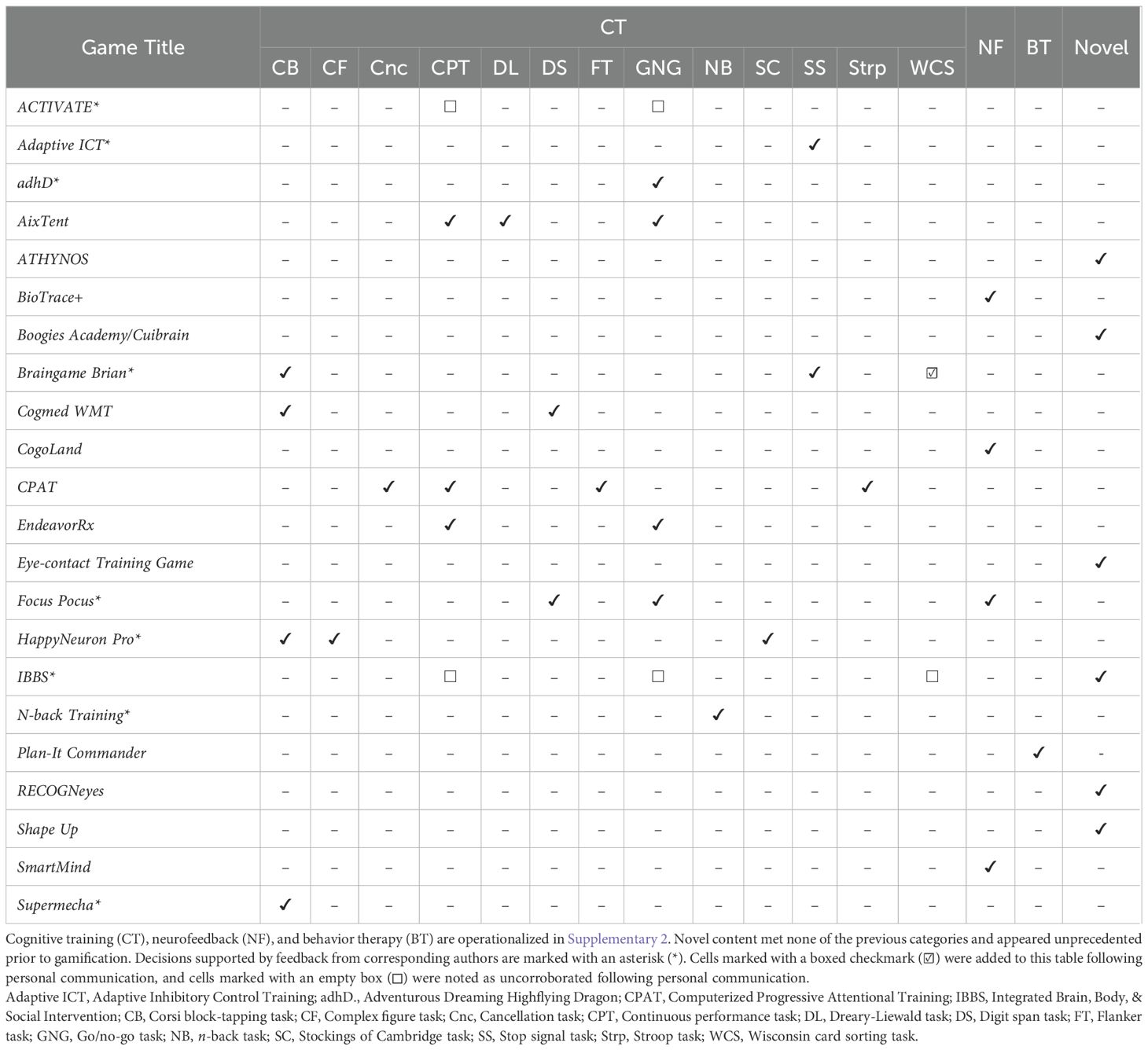
The games and the source studies are summarized in Table 1. For the content analysis, teams of two co-authors working independently coded games using the primary studies identified through our literature review and supplemental sources. The codebook began with 14 operationalized codes, and another seven were added based on follow-up discussions and iterative feedback from the coders. The coders were largely unfamiliar with neurocognitive assessment and relied solely on the codebook for their determinations. Initial calibration efforts with a subsample of four games resulted in an unacceptable range of interrater reliability estimates (AC1 = 0.68 to 1.00). In response, we revised the operational definitions that led to disagreement by adding clarifying language and links to online video demonstrations of the neurocognitive tasks. In a third round of coding with the same four games, interrater reliability increased to an acceptable level (AC1 = 0.93 to 1.00). We then used that version of the codebook for all games, with any remaining disagreements settled by the first author. Initial coder agreement remained acceptable (AC1 = 0.78 to 1.00), and instances of disagreement were resolved in follow-up communications. See Table 2 for our final content determinations. As part of these efforts, we also assessed interrater agreement for the risk-of-bias analyses. Double coding was completed in a randomly selected subset of eight articles (31%), resulting in an acceptable interrater agreement rate (87.5%), with only one discrepancy that required revised ratings (i.e., overlooked trial registration date).
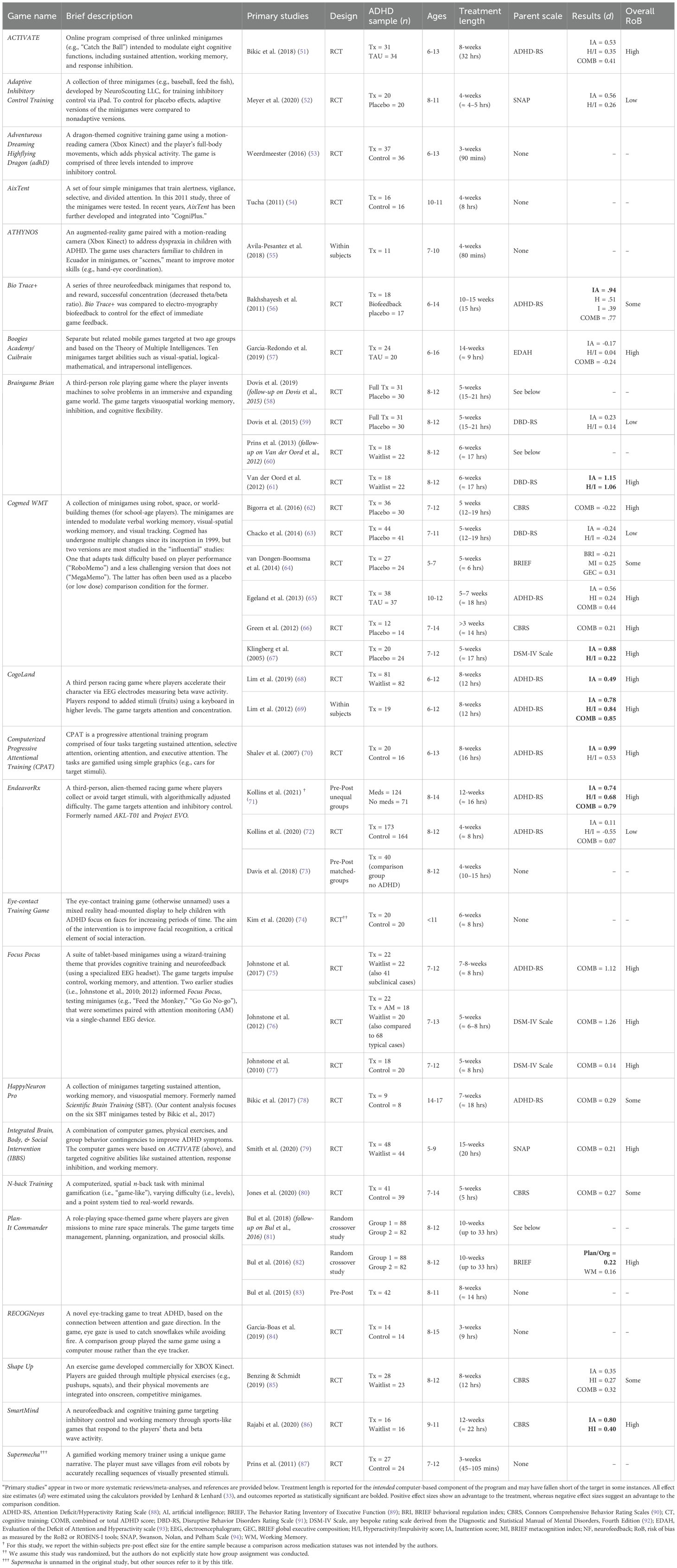
Table 1. Summary of influential game studies for children with ADHD and immediate parent-reported treatment effects.
As anticipated, most games (55%) in our sample provide at least one element of CT. Among those games, there are one to four recognizable neurocognitive tasks found in the assessment literature, but there is no single task used in most or all games. Rather, a plurality of CT games deploys variations of the go/no-go, continuous performance, and Corsi block-tapping task paradigms. Another four games (18%) attempt neurofeedback (including one combined with CT), and one game (5%) attempts behavior therapy. Six games (27%) deliver one or more novel elements, including one that targets dyspraxia (ATHYNOS), one game based on the theory of multiple intelligences (Boogie’s Academy/Cuibrain), three games that deliver physical exercise as a primary or secondary element (e.g., Shape Up), and two that are intended to improve eye gaze direction (RECOGNeyes) or facial recognition (Eye-contact Training Game).
We emailed our findings to corresponding authors for the 12 CT games and received feedback for nine of the games (75% response rate). This personal communication led to us adding one game element and recording five other category decisions as uncorroborated (see Table 2). Specifically, we added a game element in one instance (Braingame Brian) where the corresponding author provided unpublished design materials providing additional game detail. In the other instances, a developer responsible for two games (ACTIVATE and IBBS) disagreed with our characterization of their game elements, despite consensus among our coders. We report those elements as uncorroborated in deference to the developer’s feedback. Otherwise, all responding authors agreed with our conclusions. Note that these final determinations are reflected in the descriptive statistics reported above.
We then calculated effect size estimates (d) of change in parent ratings of ADHD symptoms, where available. Parent ratings were often identified as a primary or secondary outcome, and sufficient data or graphs were provided to estimate at least one effect size for 16 of the 22 games. Estimates range from -0.55 to 1.26. We then examined the relationships between game content and effect sizes on parent ratings of ADHD symptoms. Given the number of unique game elements identified, there was limited data for each. For this reason, our synthesis strategy was to summarize effect size estimate and display those results in a bubble plot (Figure 2), consistent with recommendations by McKenzie and Brennan (95). The result does not suggest clear relationships between game content and positive far transfer effects. Instead, the largest effects seem to be associated with the highest risk of bias (for full risk of bias result, see Supplementary 6). The risk was most often due to the parent raters’ awareness of their child’s treatment condition (e.g., Domain 4 of the RoB2). No effects from low-risk assessments exceeded d = 0.56, with a general pattern of the largest effects associated with the highest risk of bias. Although no game elements were clearly superior, the most promising may be the stop signal task paradigm, based on two low-risk of bias RCTs (d range = 0.14 to 0.56).
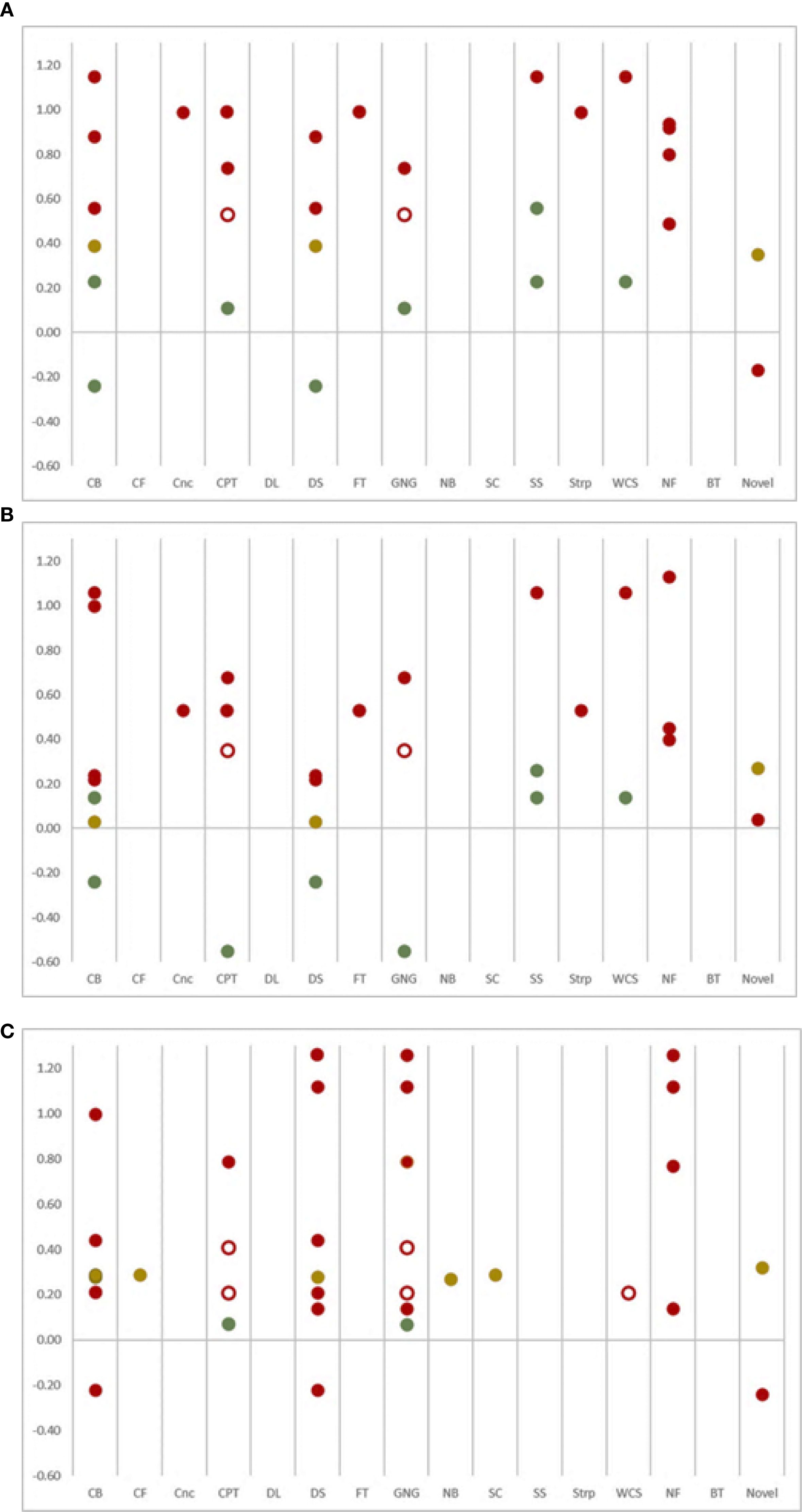
Figure 2. Bubble Plots of Effect Sizes for (A) Inattention, (B) Hyperactivity-Impulsivity, and (C) Combined ADHD Symptoms as Rated by Parents, by Game Content from Low Risk (Green), Some Risk (Yellow) and High Risk (Red) results. Category determinations that were not corroborated by the corresponding authors are indicated with empty bubbles. CB, Corsi block-tapping task; CF, Complex figure task; Cnc, Cancellation task; CPT, Continuous performance task; DL, Dreary-Liewald task; DS, Digit span task; FT, Flanker task; GNG, Go/no-go task; NB, n-back task; SC, Stockings of Cambridge task; SS, Stop signal task; Strp, Stroop task; WCS, Wisconsin card sorting task; NF, Neurofeedback; BT, Behavior therapy.
4 Discussion
We identified 22 ADHD games that have appeared in two or more recent systematic reviews or meta-analyses and examined the therapeutic content. Consistent with an experimental therapeutics approach, we were interested in categorizing intervention elements and identifying which are associated with the largest changes in child behavior. We found that ADHD game elements vary widely, even among games with similar objectives (e.g., improved working memory). For example, we uncovered 13 separate cognitive training (CT) mechanisms, with pluralities of CT games deploying content based on the go/no-go, continuous performance, and Corsi block tapping task paradigms. Those tasks ostensibly target sustained attention/response inhibition and visuospatial working memory. But even when successful on lab measures (i.e., near transfer) there is no guarantee these interventions lead to improved behavior elsewhere (i.e., far transfer). So, we examined the relationship between individual game elements and parent ratings of ADHD symptoms.
Our analysis extends previous reviews by showing that no individual game component is clearly superior to any other. In other words, no obvious pattern emerged between the purported mechanisms of action in ADHD games and far transfer outcomes, especially when considering possible sources of bias as depicted in Figure 2. Rater expectation bias is a clear confound in this literature that is difficult to avoid in common study designs (e.g., waitlist control); parent raters are often aware of their child’s treatment allocation (i.e., unblinded), which raises the risk assessment to high when using standard risk-of-bias scoring algorithms (see 36). Consistent with expectation bias, effect sizes in the present study tended to be relatively small in the few studies that blinded parent raters to treatment condition, and none were statistically significant. In other instances, studies suffered from attrition problems (e.g., children refused to play the game), which also raises the risk of bias (e.g., Domain 3 of the RoB2). In the end, there are too few high-quality studies using trustworthy far-transfer evaluations to draw definitive conclusions about the ADHD games literature. The available data suggest that bias likely explains those instances when statistically significant and meaningful results are reported. Importantly, this pattern holds true regardless of game content, and no element used in seminal games has demonstrated convincing far transfer effects. It is also critical to note that our data synthesis method does not account for study size, and one potentially promising finding for the stop signal task paradigm is based on only 101 study participants.
4.1 Why is far transfer so elusive?
As mentioned previously, there are several hypotheses for why ADHD games fail to achieve far transfer. Our results suggest that at least two of these hypotheses are unlikely. First, the hypothesis that each tool only benefits specific subpopulations of individuals with ADHD is partially unsupported because the same pattern of findings emerged for inattentive, hyperactive-impulsive, and combined presentation domains. But our results do not speak to subpopulations defined by other factors (e.g., working memory deficits), so that possibility is still plausible. Second, the hypothesis that ADHD games do not effectively target the core processes impaired in ADHD (i.e., misspecification) is also challenged because we found a wide range of attempted elements with no clear winners; rather, all results were unconvincing. Misspecification remains plausible only if interventions targeting the correct core processes have yet to be tested, published, and reviewed. To completely rule out this possibility, high quality studies with trustworthy measures of far transfer (e.g., blinded parent and/or teacher ratings) are still needed.
We believe the most likely explanation for why ADHD games fail to achieve far transfer is that neurocognitive deficits—the target for most of the games in the present review—are irrelevant to clinical outcomes (i.e., correlation ≠ causation) (18). If true, the most promising future direction is game content based on established psychosocial research. For example, behavior therapy and training interventions are the most established non-medicinal intervention domain, yet only one game in our review, Plan-It Commander (82, 83), delivers behavior interventions. In this case, parent ratings of executive functions suggested significant improvements and small effects on planning-organization and working memory (ds = 0.16 to 0.22), albeit with high risk of bias. More research is needed to determine whether serious games targeted to these domains can be effective in schools, but planning and organization interventions are well established in the treatment literature (5).
4.2 Limitations
There are several limitations to consider when interpreting our results. First, the studies captured in this review are not exhaustive of the ADHD games literature and do not reflect all games marketed directly to schools and families. Our conclusions are limited to those games that have been studied and then reviewed multiple times in the scholarly literature prior to 2025. Second, we did not play most of the games under investigation and may have miscategorized content based on our reading of the published literature. We tried to avoid error by contacting the authors of the CT studies in our review to verify our conclusions, but not all responded (75% response rate), perhaps due in part to language barriers. Third, we calculated effect size estimates for parent ratings of ADHD symptoms, given the clinical relevance and widespread use of those measures, but these data are not necessarily the best way to judge ADHD game efficacy. Multimethod, multisource measures of ADHD-related impairment would be far more informative, but unfortunately impairment measures are rare in this literature. Readers should also note that d estimates for within-subjects designs tend to be larger than for between-subject designs; for this reason, readers are cautioned to also consider statistical significance (bolded in Table 1) and the risk of bias when considering our results. Fourth, all neurofeedback games in the present review use some version of theta/beta ratio feedback, but other neurofeedback protocols exist (e.g., sensorimotor rhythm training, slow cortical potential training) that were not captured in the current overview. And fifth, we caution readers not to confuse our use of the term “novel” with “ineffective.” Game elements not appearing in the assessment or treatment literatures may indeed hold promise as interventions for ADHD. Similarly, game design elements, including game mechanics, narratives, and user experiences, might also influence user outcomes, but those factors were beyond the scope of this review.
4.3 Recommendations
To our knowledge, this is the first attempt to document and assess the potential promise of specific ADHD game elements. Based on our findings, we offer three recommendations to advance the research and development of these tools. First, content reporting standards would greatly advance this field and render coding efforts, like those attempted here, unnecessary. The lack of reporting standards is particularly problematic in the case of CT games. It is critical that developers cite the laboratory tasks or other source materials that inspire their training elements. Some authors report these details, albeit in companion articles or Supplementary Materials, whereas others offer few clues—even in widely cited, peer-reviewed studies. Likewise, novel therapeutic elements must be identified as such, ideally with a rationale for why developers believe this innovation is warranted and how it is intended to work. Therapeutically inert content meant to entertain and motivate players might be identified as “recreational” to avoid confusion with active elements. In our view, purely recreational content that thematically connects therapeutic elements may be necessary to enhance the appeal of ADHD games and engage otherwise reticent children and adolescents.
Second, the ADHD games reviewed here only included clinician support in a few cases. In fact, most games appear to have been developed as standalone interventions, available directly to consumers without the support of coaches, clinicians, trainers, or physicians. Based on our work with adolescents with ADHD, we believe this is impractical. We recommend that any games intended to change behavior are supported by real-world interventionists who coach players as they attempt new skills in their daily lives. Just as homework assignments are common in modern psychotherapies, children provided with a serious game must try the skills trained in the game in non-game settings, ideally structured and monitored by an adult. Game developers might consider parent, teacher, or clinician treatment manuals, and possibly player workbooks, that describe the game and prescribe activities to support transfer of learning. Planned transfer activities might address some of the difficulties to achieve far transfer effects (see 96), but this is an empirical question that has yet to be addressed. We believe this is particularly critical for games targeted to children with ADHD, given the chronic, neurodevelopmental nature of the disorder. But ADHD game design to date appears to be largely driven by market concerns, with priority given to self-contained and readily downloadable products. It would be informative to compare ADHD games across delivery models, where products are either delivered as standalone interventions or as part of a broader intervention package with real-world adult support.
Finally, behavior therapy and skill training interventions appear to be underrepresented in the ADHD games literature and warrant additional research. Traditional behavior therapy is strongly supported in the research literature, and successful efforts to gamify those approaches could expand treatments in homes, schools, and clinics. It is unclear whether games focused on training skills (e.g., organization strategies) could achieve replicable far transfer effects, but this domain may be ripe for development, given the growing literature on training interventions and what seems like a clear potential for gamifying those strategies. But until far transfer is convincingly demonstrated on trustworthy measures of ADHD-related impairments (e.g., organization, classroom performance) across multiple randomized control trials, we cannot safely conclude that any ADHD game—regardless of its content—is an effective treatment option.
Author contributions
BS: Methodology, Investigation, Data curation, Conceptualization, Resources, Writing – review & editing, Visualization, Validation, Project administration, Writing – original draft, Funding acquisition, Supervision, Formal analysis. SE: Funding acquisition, Supervision, Writing – review & editing, Writing – original draft, Investigation, Methodology. KC: Formal analysis, Data curation, Writing – original draft, Writing – review & editing. AD: Formal analysis, Methodology, Writing – review & editing. KL: Methodology, Formal analysis, Writing – review & editing. EM: Methodology, Writing – review & editing, Formal analysis. CW: Methodology, Writing – review & editing, Formal analysis, Validation.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. The research reported here was supported in part by the Institute of Education Sciences, U.S. Department of Education, through Grant R324A180219 to East Carolina University and Ohio University. The opinions expressed are those of the authors and do not represent views of the Institute or the U.S. Department of Education.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1605744/full#supplementary-material
Footnotes
- ^ We used wildcard characters (*) to capture common variations like “digital heath interventions.” We did not use wildcard characters with the search terms “game” and “gamification” to avoid capturing classroom and other real-world activities, like token economies, that have been referred to loosely as “gamified.” We also avoided variations of “ADHD” to exclude antiquated conceptions of the disorder (e.g., “hyperkinetic disorder”); but this only affected the search for systematic reviews/meta-analyses, not the constituent studies used for data synthesis.
- ^ To calculate d, we relied on the online calculators provided by Lenhard & Lenhard (33). Most often we used the calculator based on the formula attributed to Morris (2008) for pretest-posttest control group designs, which is sometimes denoted as dppc2. Alternatively, when eta squared (η2) was reported, we used Lenhard and Lenhard’s online calculator to directly transform to Cohen’s d. In other instances when standard deviation (SD) was provided for two groups or two measurement occasions separately without an effect size estimate, we used Lenhard and Lenhard’s online calculator to estimate pooled SD and added that into the standard formula for Cohen’s d (often denoted as ds). When only partial eta squared () was provided, we converted to Cohen’s f, and then multiplied f × 2 to get an estimate of Cohen’s d (34). Note that this approach was used in only one instance, where two groups of equal sizes were compared (Johnstone et al., 2017).
References
1. Cheng VWS, Davenport T, Johnson D, Vella K, and Hickie IB. Gamification in apps and technologies for improving mental health and well-being: Systematic review. JMIR Ment Health. (2019) 6:e13717. doi: 10.2196/1371
2. Fitzgerald M and Ratcliffe G. Serious games, gamification, and serious mental illness: A scoping review. Psychiatr Serv. (2020) 71:170–83. doi: 10.1176/appi.ps.201800567
3. Aschbrenner KA, Naslund JA, Tomlinson EF, Kinney A, Pratt SI, and Brunette MF. Adolescents’ use of digital technologies and preferences for mobile health coaching in public mental health settings. Front Public Health. (2019) 7:178. doi: 10.3389/fpubh.2019.00178
4. Evans SW, Beauchaine TP, Chronis-Tuscano A, Becker SP, Chacko A, Gallagher R, et al. The efficacy of cognitive videogame training for ADHD and what FDA clearance means for clinicians. Evid Based Pract Child Adolesc Ment Health. (2021) 6:116–30. doi: 10.1080/23794925.2020.1859960
5. Fabiano GA, Schatz NK, Aloe AM, Pelham WE, Smyth AC, Zhan Z, et al. Comprehensive meta-analysis of attention-deficit/hyperactivity disorder psychosocial treatments investigated within between group studies. Rev Educ Res. (2021) 91:718–60. doi: 10.3102/00346543211025092
6. Powell L, Parker J, Robertson N, and Harpin V. Attention deficit hyperactivity disorder: Is there an app for that? Suitability assessment of apps for children and young people with ADHD. JMIR mHealth uHealth. (2017) 5:e145. doi: 10.2196/mhealth.7371
7. Wolraich ML, Hagan JF, Allan C, Chan E, Davison D, Earls M, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. (2019) 144:e20192528. doi: 10.1542/peds.2019-2528
8. Barbaresi WJ, Campbell L, Diekroger EA, Froehlich TE, Liu YH, O’Malley E, et al. The Society for Developmental and Behavioral Pediatrics clinical practice guideline for the assessment and treatment of children and adolescents with complex Attention-Deficit/Hyperactivity Disorder: Process of care algorithms. J Dev Behav Pediatr. (2020) 41:S58–74. doi: 10.1097/DBP.0000000000000781
9. Evans SW, Owens JS, and Bunford N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. (2018) 43:527–51. doi: 10.1080/15374416.2013.850700
10. Peñuelas-Calvo I, Jiang-Lin LK, Girela-Serrano B, Delgado-Gomez D, Navarro-Jimenez R, Baca-Garcia E, et al. Video games for the assessment and treatment of attention-deficit/hyperactivity disorder: a systematic review. Eur Child Adolesc Psychiatry. (2022) 31:5–20. doi: 10.1007/s00787-020-01557-w
11. Rivero TS, Herrera Nunez LM, Pires EU, and Amodeo Bueno OF. ADHD rehabilitation through video gaming: A systematic review using PRISMA guidelines of the current findings and the associated risk of bias. Front Psychiatry. (2015) 6:151. doi: 10.3389/fpsyt.2015.00151
12. Pievsky MA and McGrath RE. The neurocognitive profile of attention-deficit/hyperactivity disorder: A review of meta-analyses. Arch Clin Neuropsychol. (2018) 33:143–57. doi: 10.1093/arclin/acx055
13. Raz N and Lindenberger U. Life-span plasticity of the brain and cognition: From questions to evidence and back. Neurosci Biobehav Rev. (2013) 37:2195–200. doi: 10.1016/jneubeorev.2013.10.003
14. Schmiedek F. Methods and designs. In: Strobach T and Karbach J, editors. Cognitive training: An overview of features and applications, 2nd ed. Berlin: Springer (2016). p. 11–22. doi: 10.1007/978-3-030-39292-5
15. Rubia K. Neurotherapeutics for ADHD: Do they work? Psych J. (2022) 11:419–27. doi: 10.1002/pchj.544
16. Simons DJ, Boot WR, Charness N, Gathercole SE, Chabris CF, Hambrick DZ, et al. Do “brain training” programs work? Psychol Sci Public Interest. (2016) 17:103–86. doi: 10.1177/1529100616661983
17. Redick TS. The hype cycle of working memory training. Curr Dir Psychol Sci. (2019) 28:423–9. doi: 10.1177/09637214198486
18. Smid CR, Karbach J, and Steinbeis N. Toward a science of effective cognitive training. Curr Dir Psychol Sci. (2020) 29:531–7. doi: 10.1177/0963721420951599
19. Kofler MJ, Irwin LN, Soto EF, Groves NB, Harmon SL, and Sarver DE. Executive functioning heterogeneity in pediatric ADHD. J Abnorm Child Psychol. (2019) 47:273–86. doi: 10.1007/s10802-018-0438-2
20. Rapport MD, Orban SA, Kofler MJ, and Friedman LM. Do programs designed to train working memory, other executive functions, and attention benefit children with ADHD? A meta-analytic review of cognitive, academic, and behavioral outcomes. Clin Psychol Rev. (2013) 33:1237–52. doi: 10.1016/j.cpr.2013.08.005
21. Lee CS, Chen T, Gao Q, Jua C, Song R, and Huang X. The effects of theta/beta-based neurofeedback training on attention in children with attention deficit hyperactivity disorder: A systematic review and meta-analysis. Child Psychiatry Hum Dev. (2022) 54:1577–606. doi: 10.1007/s10578-022-01361-4
22. Insel TR and Gogtay N. National Institute of Mental Health clinical trials: New opportunities, new expectations. JAMA Psychiatry. (2014) 71:745–6. doi: 10.1001/jamapsychiatry.2014.426
23. Raghavan R, Munson MR, and Le C. Toward an experimental therapeutics approach in human services research. Psychiatr Serv. (2019) 70:1130–7. doi: 10.1176/appi.ps.201800577
24. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
25. Passas I. Bibliometric analysis: the main steps. Encyclopedia (Basel Switzerland). (2024) 4:1014–25. doi: 10.3390/encyclopedia4020065
26. Stenros J. The game definition game: A review. Games Cult. (2016) 12:499–520. doi: 10.1177/1555412016655679
27. Molitor SJ and Langberg JM. Using task performance to inform treatment planning for youth with ADHD: A systematic review. Clin Psychol Rev. (2017) 58:157–73. doi: 10.1016/j.cpr.2017.10.007
28. Gwet KL. Computing inter-rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol. (2008) 61:29–48. doi: 10.1348/000711006X126600
29. Gwet KL. irrCAC: Computing chance-corrected agreement coefficients (CAC) (R package version 1.0) [computer software]. The Comprehensive R Archive Network (2019). Available online at: https://cran.r-project.org/src/contrib/irrCAC_1.0.tar.gz (Accessed January 15, 2025).
30. R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing (2021). Available online at: https://www.R-project.org/ (Accessed January 15, 2025).
31. Gioia GA, Isquith PK, Guy SC, and Kenworthy L. Behavior Rating Inventory of Executive Function (BRIEF) [Database record]. APA PsycTests. (2000). doi: 10.1037/t73087-000
32. Jacobson LA, Pritchard AE, Koriakin TA, Jones KE, and Mahone EM. Initial examination of the BRIEF-2 in clinically referred children with and without ADHD symptoms. J Atten Disord. (2020) 24:1775–84. doi: 10.1177/1087054716663632
33. Lenhard W and Lenhard A. Computation of effect sizes. Psychometrica. (2016). doi: 10.13140/RG.2.2.17823.92329
34. Cohen J. Statistical power Analysis for the Behavioral Sciences. 2nd ed. New York: Lawrence Erlbaum Associates, Inc (1988).
35. Rohatgi A. WebPlotDigitizer (Version 5) (2024). Available online at: https://automeris.io/ (Accessed January 15, 2025).
36. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
37. Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: A tool for assessing risk of bias in non-randomized studies of interventions. BMJ. (2016) 355:i4919. doi: 10.1136/bmj.i4919
38. Oh S, Choi J, Han DH, and Kim E. Effects of game-based digital therapeutics on attention deficit hyperactivity disorder in children and adolescents as assessed by parents or teachers: A systematic review and meta-analysis. Eur Child Adolesc Psychiatry. (2024) 33:481–93. doi: 10.1007/s00787-023-02174-z
39. Qiu H, Liang X, Wang P, Zhang H, and Shum DHK. Efficacy of non-pharmacological interventions on executive functions in children and adolescents with ADHD: A systematic review and meta-analysis. Asian J Psychiatr. (2023) 87. doi: 10.1016/j.ajp.2023.103692\
40. Westwood SJ, Parlatini V, Rubia K, Cortese S, and Sonuga-Barke EJ. Computerized cognitive training in attention-deficit/hyperactivity disorder (ADHD): A meta-analysis of randomized controlled trials with blinded and objective outcomes. Mol Psychiatry. (2023) 28:1402–14. doi: 10.1038/s41380-023-02000-7
41. Yu C, Wang C, Xie Q, and Wang C. Effect of virtual reality technology on attention and motor ability in children with attention-deficit/hyperactivity disorder: Systematic review and meta-analysis. JMIR Serious Games. (2024) 12:e5691281. doi: 10.2196/56918
42. Zhang W, Li H, and Sheng Y. A study of the effects of virtual reality-based sports games on improving executive and cognitive functions in minors with ADHD—A meta-analysis of randomized controlled trials. Behav Sci. (2024) 14:1141. doi: 10.3390/bs14121141
43. Caselles-Pina L, Sújar A, Quesada-López A, and Delgado-Gómez D. Adherence, frequency, and long-term follow-up of video game-based treatments in patients with attention-deficit/hyperactivity disorder: A systematic review. Brain Behav. (2023) 13:e3265. doi: 10.1002/brb3.3265
44. Cervantes JA, López S, Cervantes S, Hernández A, and Duarte H. Social robots and brain–computer interface video games for dealing with attention deficit hyperactivity disorder: A systematic review. Brain Sci. (2023) 13:1172. doi: 10.3390/brainsci13081172
45. Lim CG, Lim-Ashworth NS, and Fung DS. Updates in technology-based interventions for attention deficit hyperactivity disorder. Curr Opin Psychiatry. (2020) 33:577–85. doi: 10.1097/YCO.0000000000000643
46. Powell L, Parker J, and Harpin V. What is the level of evidence for the use of currently available technologies in facilitating the self-management of difficulties associated with ADHD in children and young people? A systematic review. Eur Child Adolesc Psychiatry. (2018) 27:1391–412. doi: 10.1007/s00787-017-1092-x
47. Zheng Y, Li R, Li S, Zhang Y, Yang S, and Ning H. A review on serious games for ADHD. arXiv preprint arXiv:2105.02970. (2021). https://arxiv.org/abs/2105.02970 (Accessed January 15, 2025).
48. Jiang H, Natarajan R, Shuy YK, Rong L, Zhang MW, and Vallabhajosyula R. The use of mobile games in the management of patients with attention deficit hyperactive disorder: A scoping review. Front Psychiatry. (2022) 13:792402. doi: 10.3389/fpsyt.2022.792402
49. Lakes KD, Cibrian FL, Schuck SE, Nelson M, and Hayes GR. Digital health interventions for youth with ADHD: A mapping review. Comput Hum Behav Rep. (2022) 6:100174. doi: 10.1016/j.chbr.2022.100174
50. Rodrigo-Yanguas M, González-Tardón C, Bella-Fernández M, and Blasco-Fontecilla H. Serious video games: Angels or demons in patients with attention-deficit hyperactivity disorder? A quasi-systematic review. Front Psychiatry. (2022) 13:798480. doi: 10.3389/fpsyt.2022.798480
51. Bikic A, Leckman JF, Christensen TØ, Bilenberg N, and Dalsgaard S. Attention and executive functions computer training for attention-deficit/hyperactivity disorder (ADHD): Results from a randomized, controlled trial. Eur Child Adolesc Psychiatry. (2018) 27:1563–74. doi: 10.1007/s00787-018-1151-y
52. Meyer KN, Santillana R, Miller B, Clapp W, Way M, Bridgman-Goines K, et al. Computer-based inhibitory control training in children with Attention-Deficit/Hyperactivity Disorder (ADHD): Evidence for behavioral and neural impact. PloS One. (2020) 15:e0241352. doi: 10.1371/journal.pone.0241352
53. Weerdmeester J, Cima M, Granic I, Hashemian Y, and Gotsis M. A feasibility study on the effectiveness of a full-body videogame intervention for decreasing attention deficit hyperactivity disorder symptoms. Games Health J. (2016) 5:258–69. doi: 10.1089/g4h.2015.0103
54. Tucha O, Tucha L, Kaumann G, König S, Lange KM, Stasik D, et al. Training of attention functions in children with attention deficit hyperactivity disorder. ADHD Atten Defic Hyperact Disord. (2011) 3:271–83. doi: 10.1007/s12402-011-0059-x
55. Avila-Pesantez D, Rivera LA, Vaca-Cardenas L, Aguayo S, and Zuñiga L. (2018). Towards the improvement of ADHD children through augmented reality serious games: Preliminary results, in: 2018 IEEE Global Engineering Education Conference (EDUCON), (2018) pp. 843–8. IEEE. doi: 10.1109/EDUCON.2018.8363318
56. Bakhshayesh AR, Hänsch S, Wyschkon A, Rezai MJ, and Esser G. Neurofeedback in ADHD: A single-blind randomized controlled trial. Eur Child Adolesc Psychiatry. (2011) 20:481–91. doi: 10.1007/s00787-011-0208-y
57. García-Redondo P, García T, Areces D, Núñez JC, and Rodríguez C. Serious games and their effect improving attention in students with learning disabilities. Int J Environ Res Public Health. (2019) 16:2480. doi: 10.3390/ijerph16142480
58. Dovis S, Maric M, Prins PJ, and van der Oord S. Does executive function capacity moderate the outcome of executive function training in children with ADHD? ADHD Atten Defic Hyperact Disord. (2019) 11:445–60. doi: 10.1007/s12402-019-00308-5
59. Dovis S, van der Oord S, Wiers RW, and Prins PJ. Improving executive functioning in children with ADHD: Training multiple executive functions within the context of a computer game. A randomized double-blind placebo controlled trial. PloS One. (2015) 10:e0121651. doi: 10.1371/journal.pone.0121651
60. Prins PJ, Brink ET, Dovis S, Ponsioen A, Geurts HM, De Vries M, et al. Braingame Brian”: Toward an executive function training program with game elements for children with ADHD and cognitive control problems. Games Health J. (2013) 2:44–9. doi: 10.1089/g4h.2013.0004
61. Van der Oord S, Ponsioen AJ, Guerts HM, Ten Brink EL, and Prins PJ. A pilot study of the efficacy of a computerized executive functioning remediation training with game elements for children with ADHD in an outpatient setting: Outcome on parent- and teacher-rated executive functioning and ADHD behavior. J Atten Disord. (2012) 18:699–712. doi: 10.1177/1087054712453167
62. Bigorra A, Garolera M, Guijarro S, and Hervás A. Long-term far-transfer effects of working memory training in children with ADHD: A randomized controlled trial. Eur Child Adolesc Psychiatry. (2016) 25:853–67. doi: 10.1007/s00787-015-0804-3
63. Chacko A, Bedard AC, Marks DJ, Feirsen N, Uderman JZ, Chimiklis A, et al. A randomized clinical trial of Cogmed working memory training in school-age children with ADHD: A replication in a diverse sample using a control condition. J Child Psychol Psychiatry. (2014) 55:247–55. doi: 10.1111/jcpp.12146
64. van Dongen-Boomsma M, Vollebregt MA, Buitelaar JK, and Slaats-Willemse D. Working memory training in young children with ADHD: A randomized placebo-controlled trial. J Child Psychol Psychiatry. (2014) 55:886–96. doi: 10.1111/jcpp.12218
65. Egeland J, Aarlien AK, and Saunes BK. Few effects of far transfer of working memory training in ADHD: A randomized controlled trial. PloS One. (2013) 8:e75660. doi: 10.1371/journal.pone.0075660
66. Green CT, Long DL, Green D, Iosif AM, Dixon JF, Miller MR, et al. Will working memory training generalize to improve off-task behavior in children with attention-deficit/hyperactivity disorder? Neurotherapeutics. (2012) 9:639–48. doi: 10.1007/s13311-012-0124-y
67. Klingberg T, Fernell E, Olesen PJ, Johnson M, Gustafsson P, Dahlström K, et al. Computerized training of working memory in children with ADHD-a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry. (2005) 44:177–86. doi: 10.1097/00004583-200502000-00010
68. Lim CG, Poh XWW, Fung SSD, Guan C, Bautista D, Cheung YB, et al. A randomized controlled trial of a brain-computer interface based attention training program for ADHD. PloS One. (2019) 14:e0216225. doi: 10.1371/journal.pone.0216225
69. Lim CG, Lee TS, Guan C, Fung DS, Zhao Y, Teng SS, et al. A brain-computer interface based attention training program for treating attention deficit hyperactivity disorder. PloS One. (2012) 7:1–8. doi: 10.1371/journal.pone.0046692
70. Shalev L, Tsal Y, and Mevorach C. Computerized progressive attentional training (CPAT) program: Effective direct intervention for children with ADHD. Child Neuropsychol. (2007) 13:382–8. doi: 10.1080/09297040600770787
71. Kollins SH, Childress A, Heusser AC, and Lutz J. Effectiveness of a digital therapeutic as adjunct to treatment with medication in pediatric ADHD. NPJ Digit Med. (2021) 4:1–8. doi: 10.1038/s41746-021-00429-0
72. Kollins SH, DeLoss DJ, Cañadas E, Lutz J, Findling RL, Keefe RS, et al. A novel digital intervention for actively reducing severity of paediatric ADHD (STARS-ADHD): A randomised controlled trial. Lancet Digit Health. (2020) 2:e168–78. doi: 10.1016/S2589-7500(20)30017-0
73. Davis NO, Bower J, and Kollins SH. Proof-of-concept study of an at-home, engaging, digital intervention for pediatric ADHD. PloS One. (2018) 13:e0189749. doi: 10.1371/journal.pone.0189749
74. Kim S, Ryu J, Choi Y, Kang Y, Li H, and Kim K. Eye-contact game using mixed reality for the treatment of children with attention deficit hyperactivity disorder. IEEE Access. (2020) 8:45996–6006. doi: 10.1109/ACCESS.2020.2977688
75. Johnstone SJ, Roodenrys SJ, Johnson K, Bonfield R, and Bennett SJ. Game-based combined cognitive and neurofeedback training using Focus Pocus reduces symptom severity in children with diagnosed AD/HD and subclinical AD/HD. Int J Psychophysiol. (2017) 116:32–44. doi: 10.1016/j.ijpsycho.2017.02.015
76. Johnstone SJ, Roodenrys S, Blackman R, Johnston E, Loveday K, Mantz S, et al. Neurocognitive training for children with and without AD/HD. ADHD Atten Defic Hyperact Disord. (2012) 4:11–23. doi: 10.1007/s12402-011-0069-8
77. Johnstone SJ, Roodenrys S, Phillips E, Watt AJ, and Mantz S. A pilot study of combined working memory and inhibition training for children with AD/HD. ADHD Atten Defic Hyperact Disord. (2010) 2:31–42. doi: 10.1007/s12402-009-0017-z
78. Bikic A, Christensen TØ, Leckman JF, Bilenberg N, and Dalsgaard S. A double-blind randomized pilot trial comparing computerized cognitive exercises to Tetris in adolescents with attention-deficit/hyperactivity disorder. Nord J Psychiatry. (2017) 71:455–64. doi: 10.1080/08039488.2017.1328070
79. Smith SD, Vitulano LA, Katsovich L, Li S, Moore C, Li F, et al. A randomized controlled trial of an integrated brain, body, and social intervention for children with ADHD. J Atten Disord. (2020) 24:780–94. doi: 10.1177/1087054716647490
80. Jones MR, Katz B, Buschkuehl M, Jaeggi SM, and Shah P. Exploring n-back cognitive training for children with ADHD. J Atten Disord. (2020) 24:704–19. doi: 10.1177/1087054718779230
81. Bul KC, Doove LL, Franken IH, van der Oord S, Kato PM, and Maras A. A serious game for children with attention deficit hyperactivity disorder: Who benefits the most? PloS One. (2018) 13:e0193681. doi: 10.1371/journal.pone.0193681
82. Bul KC, Kato PM, van der Oord S, Danckaerts M, Vreeke LJ, Willems A, et al. Behavioral outcome effects of serious gaming as an adjunct to treatment of children with attention-deficit/hyperactivity disorder: A randomized controlled trial. J Med Internet Res. (2016) 18:e26. doi: 10.2196/jmir.5173
83. Bul KC, Franken IH, van der Oord S, Kato PM, Danckaerts M, Vreeke LJ, et al. Development and user satisfaction of “Plan-It Commander,” a serious game for ADHD. Games Health J. (2015) 4:502–12. doi: 10.1089/g4h.2015.0021
84. García-Boas A, D’Amelio TD, Oliveira I, Collins P, Echevarria C, Zapata LP, et al. Novel interactive eye-tracking game for training attention in children with attention-deficit/hyperactivity disorder. Prim Care Companion CNS Disord. (2019) 21:19m02428. doi: 10.4088/PCC.19m02428
85. Benzing V and Schmidt M. The effect of exergaming on executive functions in children with ADHD: A randomized clinical trial. Scand J Med Sci Sports. (2019) 29:1243–53. doi: 10.1111/sms.13446
86. Rajabi S, Pakize A, and Moradi N. Effect of combined neurofeedback and game-based cognitive training on the treatment of ADHD: A randomized controlled study. Appl Neuropsychol Child. (2020) 9:193–205. doi: 10.1080/21622965.2018.1556101
87. Prins PJ, Dovis S, Ponsioen A, Ten Brink E, and van der Oord S. Does computerized working memory training with game elements enhance motivation and training efficacy in children with ADHD? Cyberpsychol Behav Soc Netw. (2011) 14:115–22. doi: 10.1089/cyber.2009.0206
88. DuPaul GJ, Power TJ, Anastopoulos AD, and Reid R. ADHA Rating Scale-IV: Checklists, norms, and clinical interpretation. New York: Guilford (1998).
89. Gioia GA, Isquith PK, Guy SC, and Kenworthy L. Behavior Rating Inventory of Executive Functions. Lutz: PAR (2000).
91. Fosco WD, Babinski DE, and Waschbusch DA. The disruptive behavior disorders rating scale: Updated factor structure, measurement invariance, and national caregiver norms. J Pediatr Psychol. (2023) 48:468–78. doi: 10.1093/jpepsy/jsad006
92. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th edition. Washington DC: DSM-IV (1994).
93. Farré A and Narbona J. EDAH: Scale for the assessment of attention deficit hyperactivity disorder. Madrid, Spain: TEA Ediciones (2001).
94. Swanson JM. SNAP-IV Teacher and parent ratings scale. In: Aykr F, editor. Therapist’s Guide to Learning and Attention Disorders. Academic Press (2003). p. 487–500.
95. McKenzie JE and Brennan SE. Chapter 12: Synthesizing and presenting findings using other methods. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors. Cochrane handbook for systematic reviews of interventions (ver. 6.4). Cochrane (2023). Available online at: www.training.cochrane.org/handbook (Accessed January 15, 2025).
Keywords: ADHD, digital health, serious games, systematic review, content analysis
Citation: Schultz BK, Evans SW, Carter KM, Dembowski A, Lojinger K, Murray ER and Walcott C (2025) A systematic review and content analysis of serious video games for children with ADHD. Front. Psychiatry 16:1605744. doi: 10.3389/fpsyt.2025.1605744
Received: 03 April 2025; Accepted: 11 August 2025;
Published: 06 October 2025.
Edited by:
Stefan Borgwardt, University of Lübeck, GermanyReviewed by:
James Hugo Smith-Spark, London South Bank University, United KingdomCharline Grossard, Assistance Publique Hopitaux De Paris, France
Copyright © 2025 Schultz, Evans, Carter, Dembowski, Lojinger, Murray and Walcott. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brandon K. Schultz, c2NodWx0emJAZWN1LmVkdQ==
 Brandon K. Schultz
Brandon K. Schultz Steven W. Evans
Steven W. Evans Kaitlynn M. Carter
Kaitlynn M. Carter Allison Dembowski1
Allison Dembowski1