- 1Population Health Sciences Institute, Newcastle University, Newcastle upon Tyne, United Kingdom
- 2Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust, Newcastle upon Tyne, United Kingdom
Background: Excessive alcohol use is common among people presenting to emergency departments with self-harm; however, this group face barriers accessing appropriate support. This study aimed to evaluate a rapid access personalised face-to-face service developed to address this gap and explore wider implementation opportunities.
Methods: We conducted a service evaluation with a mixed methods convergent design. An NHS data custodian extracted and anonymised electronic health records data prior to sharing with the research team for analysis using descriptive statistics and non-parametric tests. Qualitative semi-structured interviews were conducted with patients and clinicians and analysed thematically. Quantitative and qualitative data were integrated, and meta-inferences drawn.
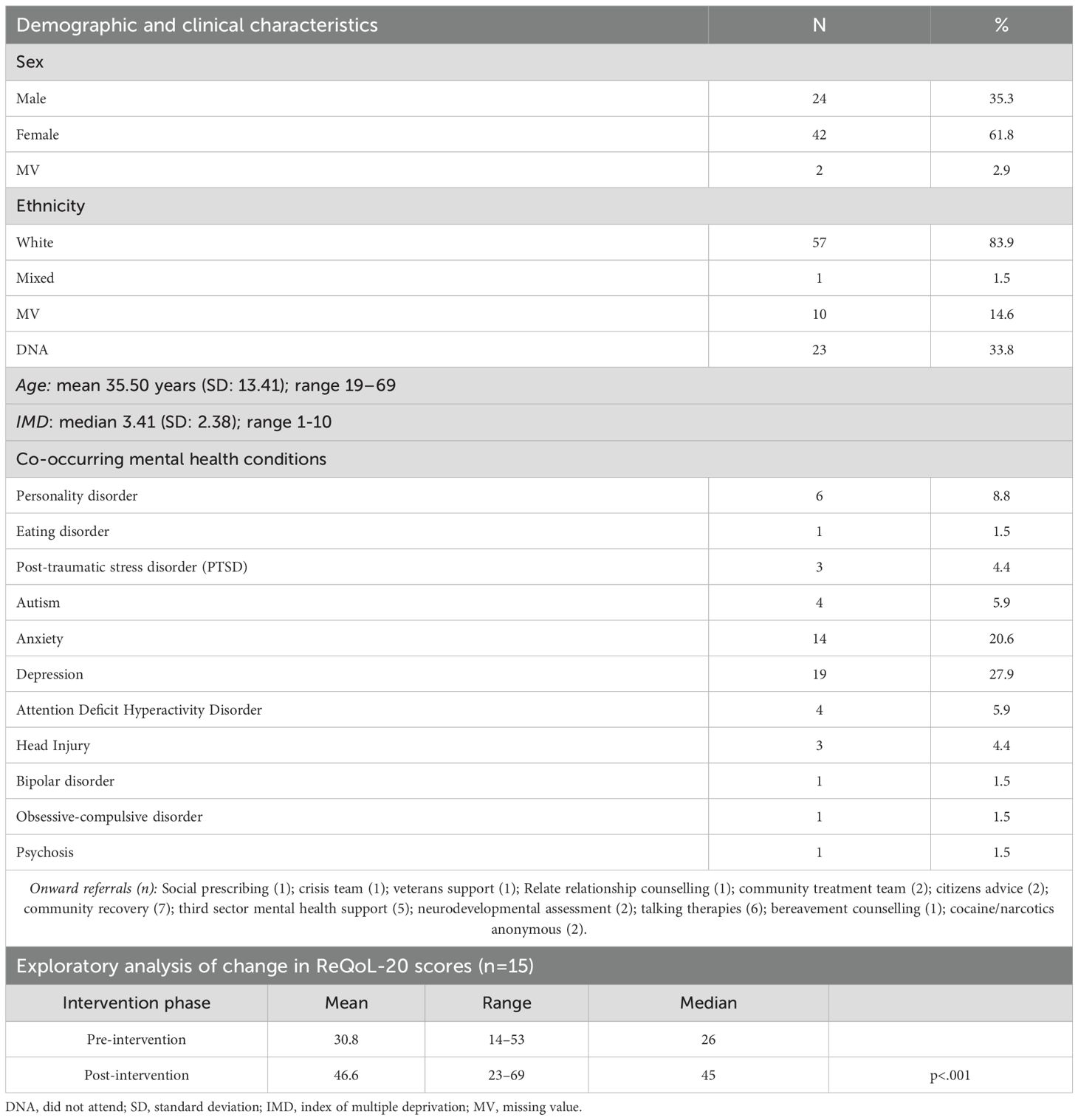
Results: Patients accessing the service (n=68) were mostly female (61.8%), white (83.9%), mean age 35 years (range 19-69), and most experienced additional mental health conditions alongside excessive alcohol use. Preliminary exploratory calculations comparing baseline to follow-up Recovery Quality of Life (ReQoL-20) scores suggested positive change. Three themes were identified from interviews with patients (n=11) and clinicians (n=7): (1) what the service added: rapidly plugging a recognised care gap for people using alcohol excessively but who are non-dependent and have poor mental health (2) what worked well: tailored relational support that builds recovery positive social networks and personal coping strategies (3) what could be improved: opportunities/challenges to sustaining and scaling-up the service.
Conclusions: The findings contribute to an evidence gap in appropriate care for patients with excessive alcohol use, self-harm and poor mental health. Whilst limited to one service, the findings highlight what patients valued, opportunities for implementation in other contexts, and thus have relevance internationally.
1 Introduction
Evidence suggests excessive alcohol consumption (defined in the UK as >14 units a week: a unit equating to eight grams of pure alcohol) (1), and mental health conditions commonly co-occur (2–6). Around a third of people who meet diagnostic criteria for major depressive disorder drink alcohol excessively (6–8). Experiencing excessive drinking and mental ill-health concurrently is associated with increased self-harm risks (9–13). Excessive drinking is highly prevalent amongst emergency department attenders in the UK and internationally (13, 14). A UK study showed alcohol involvement in 58.4% (n=11,556) of emergency department attenders with self-harm (14). UK prevalence of non-suicidal self-harm is 6.4% of the general adult population (15). Clinical guidelines define self-harm as intentional self-poisoning or self-injury regardless of the purpose (suicidal or non-suicidal) (16).
Research suggests treating excessive alcohol use and mental ill-health in parallel is important to ensure positive outcomes (4, 17). Further people with excessive alcohol use and mental ill-health frequently have multiple and complex needs, meaning that holistic approaches, that are coordinated across different health and care service providers and are responsive to local contexts are required (18–21). Evidence shows that people with excessive alcohol use and self-harm often face barriers to appropriate support, including gaps in service provision and limited understanding by services of their wider socio-economic circumstances (17, 22–25). Preventative approaches are also required for those who may not actively seek support for excessive drinking or who do not meet eligibility criteria for specialist addictions services (26–28).
1.1 Context
Research suggests alcohol brief interventions in the emergency department are beneficial and cost effective (29–31) however less research has specifically explored the use of brief interventions for people with alcohol misuse and self-harm and the findings from these studies are mixed. Previous research showed that a brief intervention for alcohol misuse following self-harm did not significantly reduce alcohol consumption or subsequent self-harm (32). The intervention was a 30-minutes interview with an alcohol specialist nurse and the authors suggested that longer interventions may be required. A systematic review of psychological interventions to reduce alcohol use found they led to reduced self-harm but had no impact on suicidal ideation (20). A Delphi consultation was conducted to identify core components of a brief intervention for emergency department attendees with self-harm and substance use difficulties; the authors planned feasibility testing of the intervention which comprised weekly phone calls for one month (33).
To address the care gap faced by people with excessive alcohol use who self-harm, a rapid access service (RAS) was developed and provided by the Psychiatric Liaison Service of a large NHS trust in North East England. This region has high levels of alcohol-related morbidity and mortality (34), above average deprivation (35), high numbers of people seeking mental health support (36) and high suicide rates compared to other parts of England [14.5 suicides per 100,000 people in the North East compared to 7.3 in London (37)]. The RAS clinic provided rapid access to short-term personalised face-to-face care for people identified as drinking excessively and accessing emergency services after a self-harm episode.
The RAS service was delivered at a community venue by a specialist substance use nurse with mental health experience. Patients presenting in emergency care at a local hospital following an episode of self-harm, were reviewed by RAS clinicians and those with excessive but not dependent level alcohol use (i.e. who psychiatric liaison clinicians did not consider suitable for or who did not meet criteria for referral to specialist addictions services) were eligible for RAS rapid access support. Care typically consisted of the offer of three personalised face-to-face sessions, including psychoeducation, and motivational interviewing-based alcohol and mental health support. Sessions were held weekly, with patients offered the next available session following the self-harm episode, usually the following week. After three sessions, patients were referred or signposted to sources of longer-term care as needed e.g. counselling or support from third sector organisations. This study aimed to (1): understand the care journeys of patients accessing the RAS service; and (2) explore implementation experiences and identify opportunities for transfer to other settings.
2 Methods
This mixed methods service evaluation used a convergent approach collecting and analysing quantitative and qualitative data in two parallel parts. Part 1: collection and analysis of quantitative electronic health record data. Part 2: qualitative interviews with patients and clinicians. The quantitative and qualitative data were then integrated, to generate deeper understanding of how the RAS service supported people (38).
2.1 Part 1
Electronic health data were accessed via the UK NHS Clinical Record Interactive Search system (CRIS). The research team provided an NHS data custodian with instructions regarding specific data needs, and the custodian conducted searches, extracting relevant data on their behalf and ensuring anonymisation before sharing with the research team for analysis. Data were extracted for all patients referred to the RAS from 23/2/23 (when the service started) to 31/8/24. The RAS ran one day a week and only when the specialist substance use nurse was available, so for some weeks during this period the service was not operational.
Extracted data included socio-demographic characteristics and postcode to calculate Indices of Multiple Deprivation (IMD), a measure of deprivation across seven domains (income, employment, education/skills/training, health/disability, crime, housing/services and living environment) (39). Data were also extracted on mental health or neurodevelopmental diagnoses, referrals to follow-up organisations, and Recovering Quality of Life (ReQoL-20) scores. The ReQoL-20 is a 20-item self-report measure of outcomes identified by respondents as important to recovering their quality of life (40). Reliable improvement is indicated by increases of ≥10 points while decreases of ≥10 points indicate reliable deterioration (40). Patients accessing the RAS were assessed with the ReQoL-20 at baseline (week 1) and intervention end (week 3).
Quantitative data including patient demographic and clinical characteristics, baseline and post-intervention ReQoL-20 scores and post-intervention service referrals were analysed with descriptive statistics and exploratory non-parametric tests. Pre/post-intervention ReQoL-20 scores were compared with Wilcoxon signed rank test using SPSS statistical software (41).
2.2 Part 2
Semi-structured interviews were conducted with patients accessing the RAS and clinicians involved in the design, commissioning, and delivery of the clinic.
2.2.1 Recruitment
Patients. Inclusion criteria were patients >18 years of age with excessive alcohol use who had accessed the RAS after presenting to the emergency department with self-harm. Patients were screened for eligibility by a RAS clinician, provided with information about the service evaluation, and asked if they were interested in taking part and agreeable to their contact details being provided to the research team. Those expressing interest were then contacted by the research team. Patient participants were provided with support organisation contact details and a £20 voucher.
Clinicians. A range of clinicians directly and indirectly involved in the delivery, management, referral to and commissioning of the RAS clinic were recruited through purposive sampling. A RAS clinician facilitated contact between the researchers and potential clinician participants who were then contacted directly by the research team.
2.2.2 Data collection
Semi-structured interview topic schedules were developed for patients and clinicians (see online Supplementary Materials: OS1, 2). Interviews with patients who had accessed the RAS explored their experiences including what worked well, and barriers/facilitators to their engagement. Patient demographic information was gathered using a structured form (OS3). Clinicians’ interviews covered the design and scope of the clinic, what worked well, challenges to delivery, and potential to transfer the service to other settings.
Interviews with all participants were conducted via MS Teams, audio-recorded and transcribed; transcripts were anonymised, and participants allocated a pseudonym. All participants provided informed consent before taking part in an interview.
2.2.3 Analysis
Interview data were analysed using thematic analysis combining deductive and inductive approaches during four iterative phases: (i) data familiarization; (ii) defining a coding framework; (iii) identifying themes/subthemes; and (iv) refining themes/subthemes (42, 43). We defined a-priori themes based on the evaluation questions, then inductively derived codes and subthemes from the data, mapping these onto the a-priori themes. Patient and clinician interview data were analysed together with between-group similarities and differences explored. Two researchers completed data analysis, meeting regularly to discuss coding, with 20% of transcripts double-coded independently. NVivo software was used to support data management and analysis.
Key findings from both Part 1 and 2 were combined: descriptive statistics from the quantitative data and quotes from the qualitative data were integrated in tables, allowing comparison, discussion of convergence and divergence and drawing meta-inferences (38).
2.3 Approvals
A service evaluation application was approved by the NHS Trust Research and Development Department (23/5/24: SER-24-277). The local NHS CRIS database oversight committee reviewed the service evaluation protocol and approved collection of retrospective quantitative health record data.
3 Results
3.1 Exploratory quantitative analysis of health data
Health record data were gathered for 68 patients referred to the clinic from 23/2/23 to 31/8/24. The characteristics of those people attending one or more of the RAS sessions offered are shown in Table 1. Thirty-eight patients (55.9%) had one or more co-occurring mental health condition (Table 1). Being a new service, the team were consolidating service protocols, and ReQoL-20 scores were not always completed, and some participants did not attend all appointments, meaning follow-up scores were sometimes unavailable: ReQoL-20 scores at baseline and follow-up were available for fifteen people. Mean ReQoL-20 score at baseline was 30.8 (range 14-53) and 46.6 (range 23–69) at follow-up (final session), suggesting improvement across the cohort (40). The mean change in scores from baseline to follow-up was 15.8 (range 6 - 39). Of these 15 patients, four (26%) moved from the clinical (0-49) to non-clinical range (≥50). A Wilcoxon’s signed rank test showed improvements in median ReQoL-20 scores from baseline to follow-up (p<.001).
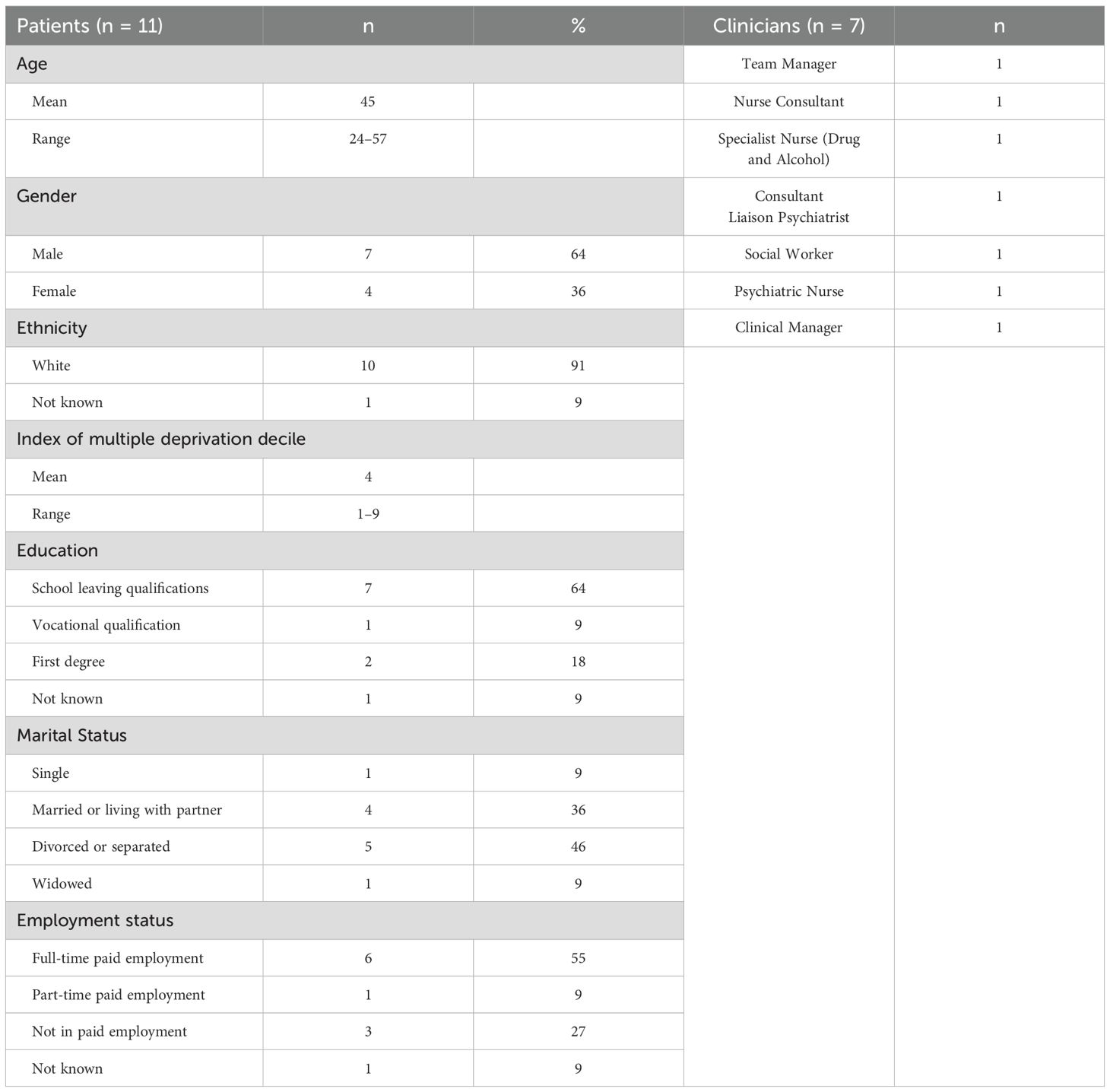
3.2 Qualitative interviews
Eleven patients and seven clinicians accessing/involved in operation of the RAS participated in an interview (Table 2). Clinician participants included a specialist drug and alcohol nurse who delivered RAS sessions and other members of the psychiatric liaison multidisciplinary team, representing those with different levels of involvement in the RAS so facilitating different perspectives. For example, participants included a psychiatrist and a psychiatric nurse who while not involved in delivering RAS sessions, were involved in the clinical care of patients accessing the RAS and decisions on their referral to the RAS. Other clinicians interviewed included those who were involved in managing the operational aspects of the RAS clinic for example facilitating organisational processes required for setting up the new service within the pathway and developing service protocols. Data analysis identified three themes: (1) What the service added: rapidly plugging a recognised care gap for people using alcohol excessively but who are non-dependent, who self-harm and have poor mental health; (2) What worked well: tailored relational support that builds recovery positive social networks and personal coping strategies; and (3) What could be improved: opportunities and challenges to sustaining and scaling-up the RAS service. Quotes are annotated (P: patient or C: clinician).
3.2.1 Theme 1. What the service added: rapidly plugging a recognised care gap for people using alcohol excessively but who are non-dependent and have poor mental health
Patients eligible for RAS support were drinking excessively, but not currently dependent on alcohol and had accessed accident and emergency with self-harm. By supporting this specific population, clinicians and patients highlighted the novel contribution to care provision:
‘Especially for people that fall down the gap, so don’t quite belong in the specialist drug and alcohol services. They don’t quite belong in mental health services. But they need help and it’s an unmet need’ (C2).
Participants indicated the community-based location differentiated the offer from existing clinical services, important for this group who may not feel comfortable attending specialist addictions services due to stigma or not feeling they required that level of support. One patient said: ‘I didn’t particularly want to see people who were in worse positions’ (P2). Another patient expanded on this:
‘I found … it was quite a quiet place; so I go to [addictions service] which is very clearly marked what it is … and I sometimes get anxious that when I’m going in I might be seen; everybody knows what sort of place it is.’ (P6).
A clinician highlighted the need to keep the clinic ‘out of drug and alcohol services’ (C1):
‘…didn’t have signs up and it wasn’t so noticeable so [patients] were given anonymity around why they were there. [Addictions service] is in the middle of the city centre. Yes, it’s great for accessibility, but for other clients it’s not. It’s too busy. Too many people stand around outside. There’s the pub opposite.’ (C1).
Participants suggested the combined support for mental health and excessive alcohol use provided by RAS distinguished it from existing services:
‘A lot of people feel that they have mental health difficulties, and they won’t be touched, or they’ll be excluded, because of their alcohol use, and that isn’t the case here. We’ll carry out mental health interventions and substance misuse interventions, not one or the other, we do both for the individual’ (C3).
One patient described being admitted to hospital prior to accessing RAS but felt their full needs were not addressed:
‘The doctors treated the physical symptoms, which obviously was to stop the alcohol which I did successfully … I was sent home from hospital … but they hadn’t dealt with the mental side of things’ (P10)
Patients and clinicians valued the rapid support the service provided. One patient said: ‘it meant that I had access to … support very quickly’ (P10). An emergency department clinician valued being able to offer timely appointments:
‘As a clinician, it’s an incredibly valuable resource to be able to offer someone something tangible in the ED [emergency department], because there’s so little to, often, offer people. Obviously, you’ve done your intervention in the ED. You’ve done your psychosocial assessment, which has, hopefully, left the person feeling safer to leave and with a safe plan in place. But there’s something incredibly validating to be able to give somebody an appointment there and then’ (C2).
3.2.2 Theme 2. What worked well: tailored relational support that builds recovery, positive social networks and personal coping strategies
Patients described characteristics of the RAS provider (a specialist substance use nurse) that helped them open-up about their difficulties with alcohol, mental health, and reasons for drinking including being approachable, able to establish rapport, and having active listening skills:
‘The way he spoke to you; it was like talking to one of your mates. Like he didn’t think anything bad of you … when I was telling him about flying my drone and things like that, when I went in for my next session … he’d ask me how that was going’ (P8)
‘He just got it and understood that … what I was doing and why I was doing it and that was comforting because it was tough, at the time and he sort of helped me get to the bottom of a few things which maybe I wouldn’t have got there by myself, or it would have took me a long time’ (P2).
Patients valued the pragmatic approach taken by the clinic who did not suggest people stop drinking rather break recovery down into small achievable goals. One patient explained:
‘He made it very clear that he didn’t believe that me going tee-total was the right thing. We discussed that I needed to improve my relationship with alcohol. But he made it very clear to me, he took away, well, the fear, if you like’ (P2).
RAS sessions employed a holistic approach to co-occurring excessive alcohol use and mental ill-health that recognised the impact on all areas of patients’ lives, one patient commenting: ‘We covered everything, my state of mind, my girlfriend, my drinking, what I can do to improve myself, what I can do to stop the drinking’ (P1). The RAS provider facilitated discussing what had been going on for patients before and after a self-harm episode, to help them develop insight:
‘Was there an increase in self-harm? What was the trigger for that? And allowing the individual to understand their emotions a lot better, and what potentially triggered them … we’re always talking about what they feel, what they want, and how they can achieve that’ (C3).
RAS patients described learning techniques to manage responses to potential risk events (‘giving me situations and scenarios, so I don’t react quickly’: P4) and coping strategies to manage alcohol use and mental health, including keeping an alcohol diary, activity schedule, and goal setting. Participants accounts suggested the sessions helped build social and recovery capital, a clinician explained:
‘Because if nothing changes in that context, what is going to keep that individual from relapsing? Because we want to build up on that for the individual, to try to stop them from relapsing, and lay some foundations’ (C3).
Patients described being encouraged to pick-up past hobbies and interests like reading and art and craft possibly neglected while drinking:
‘I used to be a long-distance runner, a lot of years ago. [RAS nurse] told me to start focusing on that, if I could, and I did. I’ve started to keep myself fit, take my mind off the drinking, take my mind off negative thoughts’ (P1)
3.2.3 Theme 3. What could be improved: opportunities and challenges to sustaining and scaling-up the RAS
The RAS clinic provided short-term support, and whilst patients were positive about care received, several would have liked more sessions, one patient explaining:
‘I just had three hours. I think I probably could’ve done with another three sessions because we’d just got to a point where we’d actually … it’s almost like if you imagine you’ve got a jumper, and you start to unpick the hem on the sleeve. I feel like I’d just started to unravel the sleeve when the sessions stopped’ (P10).
Clinicians recognised the shortcomings of the time-limited-support offer, but this allowed them to address immediate safety concerns: ‘…we can’t fix everything, we can’t solve everything in such a short period of time, but if an individual has presented in services in a mental health crisis, we are able to support them through that period quite safely and effectively’ (C3). Participants also highlighted the limited capacity of the RAS, being delivered by a single clinician it had to be paused during periods of absence:
‘If [RAS nurse’s] off we have nobody else to run that clinic. From an operational perspective that’s difficult and [RAS nurse’s] very aware of that … it’s really unfortunate that we have nobody else to run it’ (C1).
It was clear that any new clinicians would need to combine a positive relational and holistic approach, with awareness of underlying mechanisms driving excessive drinking:
‘Mental health knowledge and experience, as well, comes into play with that, to try and look at the interventions from a life planning, goal setting point of view. What are they doing within their life to change these issues that are ongoing? What’s their motivation? What’s their goal? And having that out with the service user, creating that conversation, and motivational interviewing, really, that identify what their specific treatment requirement is’ (C3).
A patient expanded highlighting that clinicians would require a pragmatic approach:
‘Not feeling embarrassed to write down “I’ve had a drink today”. Because at the last one [service] you weren’t supposed to drink at all and you couldn’t talk about alcohol in that way. You couldn’t say, “I’ve had a drink”. This was different, it allowed you to speak about it without feeling guilty. And if you’d had a drink, to work through why you had a drink’(P9).
Participants stressed the need for a full-time dedicated clinician, without management responsibilities, and graded at an appropriate level of seniority. Clinicians described challenges to service delivery included limited awareness of the RAS’s specific role and place within local care infrastructures, and that some colleagues were unclear about the referral criteria, potentially causing delays in care provision. To address this, clinicians suggested a designated contact be strategically embedded within the care pathway:
‘Educating the access services, educating the psychiatric liaison teams, educating the crisis teams, in every locality, in having that consistent pathway there … being able to explain that to services, I feel, really links the gap nicely. Because generic services, I suppose, you put a referral in, you discuss the referral, and you come up with an opinion or an assumption. However, having that additional person there to advocate for the service user really supports them’ (C3).
The existing RAS team were preparing to set up a new clinic in another location and reflected on other requirements, including integration with existing health services:
‘It would be linking with other services around us to identify what the need is, and getting a clinic sorted by identifying the room, identifying the population you want to work with, and the inclusion criteria, look at the exclusion criteria, and then get the ball rolling. But I suppose that would be linking in with different psychiatric liaison services, and looking at what they’ve used historically, and currently … more services, such as, like, blood borne virus screening, making sure that people’s physical health needs are being adhered to, as well as their mental health needs’ (C3).
Clinicians described practical ‘lessons learned’ from setting up the RAS that could inform scale-up to other locations including developing session content, guidance for measuring core outcomes, and protocols that would need to be established for e.g. referral criteria, non-attenders, lone working, and record-keeping.
Quantitative and qualitative data on co-occurring mental health conditions and quality of life are presented side-by-side in Tables 3 and 4 and compared in the discussion.
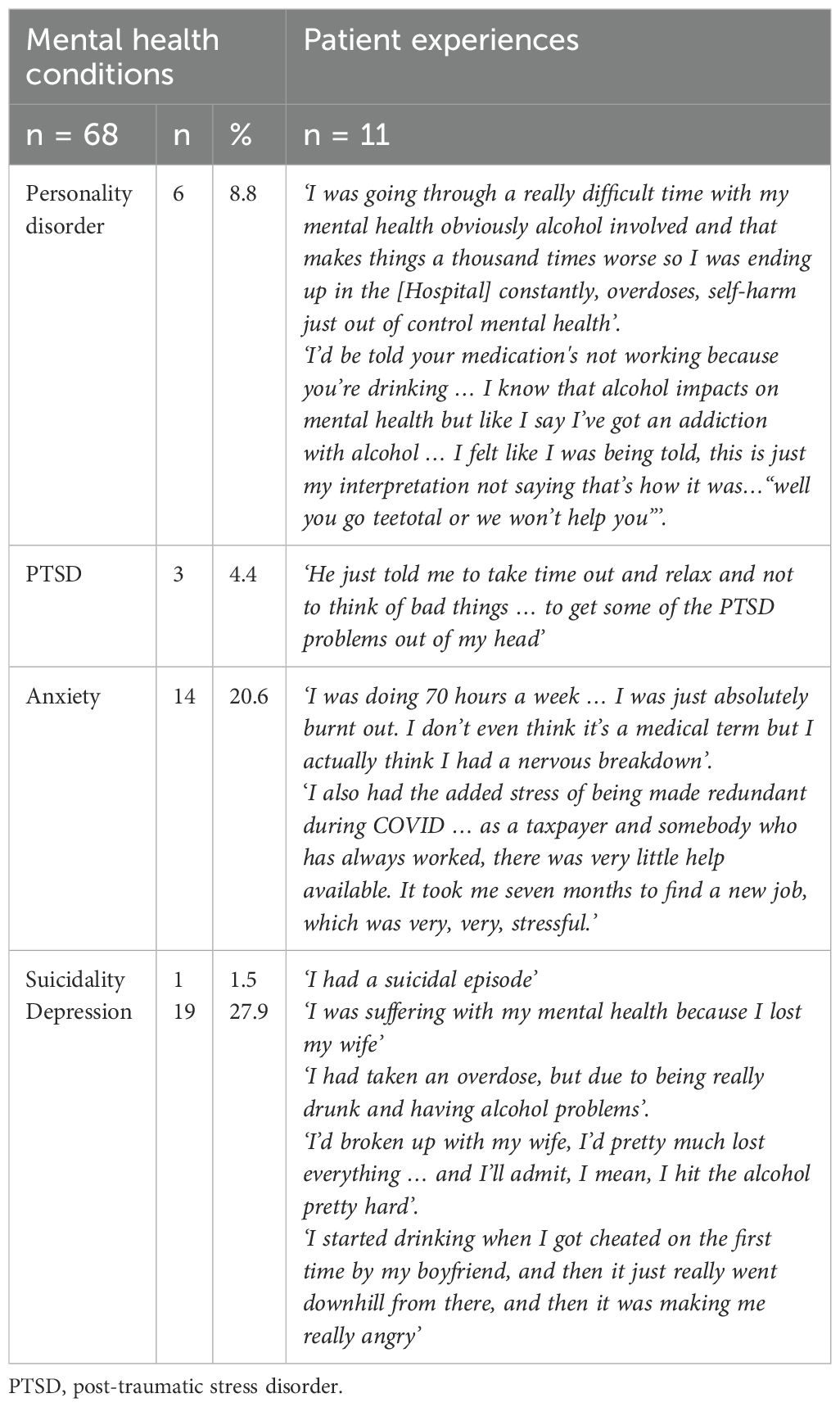
Table 3. Co-occurring mental health conditions identified in the quantitative health data alongside patient quotes.
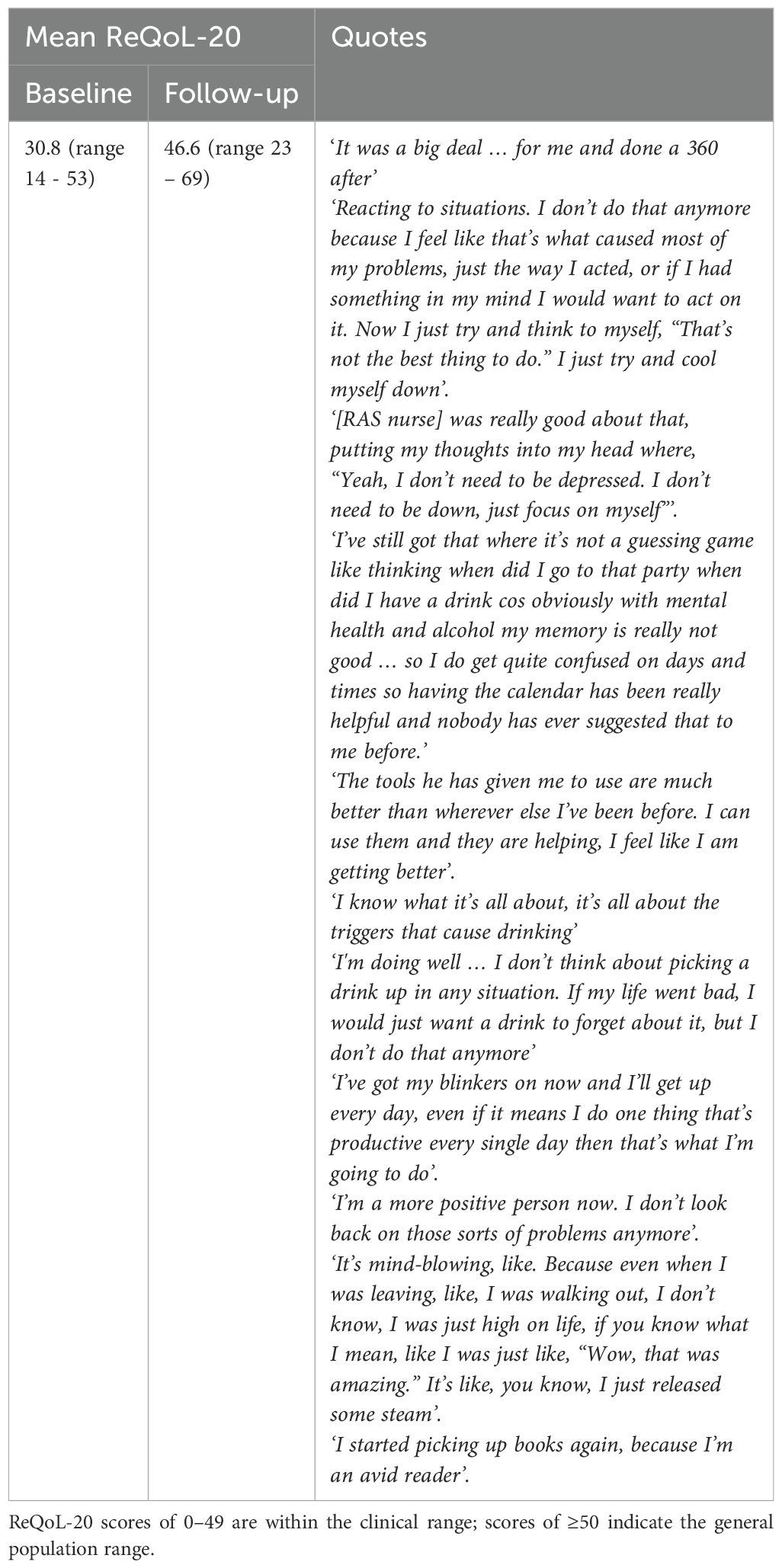
Table 4. Changes in quality-of-life scores from baseline to follow-up and illustrative patient quotes describing coping strategies found helpful.
4 Discussion
Despite the well-evidenced relationship between alcohol use and self-harm, and poor outcomes experienced by many people experiencing these concurrently, research shows persistent care gaps for people affected in the UK and internationally (13, 17, 22–24). We evaluated a new rapid access personalised face-to-face service in North East England for patients with excessive alcohol use, who self-harm, many with co-occurring mental health conditions but deemed unsuitable for specialist alcohol treatment services. Triangulating lived experience of the service with quantitative patient data, we found evidence of positive experiences of care, and health improvements in patients accessing the RAS. Patients described how the intervention enabled them to acquire new coping strategies to better manage their alcohol use and self-harm, and this was further evidenced by improved quality of life scores.
Our findings reflect and build on those of other studies, highlighting the need for tailored support to address the complex overlapping psycho-social factors impacting the behaviour of patients who self-harm and drink alcohol excessively (17, 25, 44, 45). Our data highlight the clinical complexity of this population; many patients accessing the RAS clinic had a co-occurring mental health condition (Tables 1, 3) and were experiencing adverse life events (e.g. relationship breakdown, housing, family and financial concerns, unemployment, bereavement). To address patients’ needs, sessions utilised different therapeutic techniques (e.g. motivational interviewing and psychoeducation) and advice on resuming interests e.g. running. This aligns with research showing the relationship between physical activity, alcohol consumption and distress (46). Other research also found motivational interviewing, cognitive behavioural and psychoeducational approaches helpful for people with excessive alcohol use including those with co-occurring mental ill-health (47–49) though research is required into effectiveness of digital interventions for this group (50).
Patients reported the holistic personalised approach contrasted with previous difficulties accessing care. Despite the ‘no wrong door’ policy for individuals with multiple co-occurring conditions (51, 52), healthcare still focusses primarily on identifying and managing single diagnoses (53, 54). Narrow eligibility criteria can mean individuals face barriers to accessing appropriate mental health care, despite guidance recommending access to preventative psychological interventions (55). Participants in our study described experiencing being ‘blocked’ from or ineligible for mental health support services unless they stopped drinking alcohol. Research with people experiencing excessive alcohol use and depression in North East England also found many encountered a lack of awareness/acknowledgment among providers, of the relationship between alcohol and mental ill-health, and the adverse impact of socio-economic factors on capacity to access support and recovery (22).
Our study demonstrates the potential contribution the RAS, designed for people who drink alcohol excessively but are not dependent, could make to existing healthcare provision. Stakeholders have called for a UK national alcohol strategy and development of secondary preventative interventions for clinical populations which are currently lacking (56, 57). Whilst the patients we spoke with would not meet existing criteria for specialist alcohol services, their alcohol use and mental ill-health were clearly a significant cause of risk and negatively impacted their day-to-day lives and quality of life.
Study strengths include combining quantitative and qualitative data to help understand how the RAS service supports people with excessive alcohol use who present to emergency services following an episode of self-harm; this mixed methods approach facilitates triangulating insights from different perspectives (38, 58). Also focussing on a service innovation which responds to an unmet care need identified in the UK and internationally (11, 13). Focussing on one geographical area could be construed as a limitation, however we gathered data exploring what would be required for transferability to other settings.
This preventative response to alcohol use disorder and mental health aligns with the NHS Long Term Plan’s aim to support people to address harmful lifestyle behaviours, identify and treat avoidable illness early, and exploiting opportunities for intervention during hospital admissions (59). Evidence shows the group targeted by the RAS service are likely to have repeat attendances at the emergency department (60), and in the context of rising numbers of alcohol-related deaths, particularly in North East England (61), the RAS service provides a promising approach for these patients. Our evaluation suggests key ingredients of the service potentially include rapid access to support, personalised holistic sessions considering mental health and alcohol use in parallel and delivered by non-judgemental clinicians. The findings suggest it would be important to explore opportunities to scale-out implementation into other clinical settings; for example, these could include alcohol nurses delivering the service in primary care with appropriate support. This is an innovative service, albeit based on delivery by one therapist. Future research should consider a wider staff base to ensure positive outcomes can be replicated and are not linked to the skills of individual clinicians.
A study strength was completing exploratory analysis using a standardised quality of life measure (ReQOL-20). However, scores at both baseline and follow-up were only available for fifteen people and this potentially introduces bias. It may be that those people who completed treatment sessions were more positive about the service compared with those people who disengaged early, and our findings would not capture or reflect the perspectives of those people in the latter group. We completed exploratory statistical significance testing; however, this is a small-scale study and there was no control group. Furthermore, patients in the interviews were invited to participate by the RAS clinician and we cannot assume the views of the eleven people interviewed would be the same as RAS patients who did not participate in the study. Moreover, while participant feedback was positive, the sample was again relatively small. We did not have data on the proportion of the patients accessing RAS who received concurrent aftercare from other sources e.g. the crisis team, or on the numbers of patients who would previously have been referred directly to the crisis team but were instead referred to the RAS and this is an area for future research. Future research is needed regarding implementation of similar clinics and any barriers in the context of changes to UK NHS mental health commissioning and the role of UK local integrated care boards who are tasked with commissioning and planning services for regional populations (59, 62, 63).
5 Conclusion
The findings contribute to an acute evidence gap in appropriate models of care for patients with co-occurring excessive alcohol use, self-harm and poor mental health. The data shed light on what was valued by patients and clinicians and how the approach could be implemented in other settings. The findings have potential to inform future commissioning decisions, innovation and service development in mental health and other clinical settings in the UK and internationally.
Data availability statement
The datasets generated and/or analysed during the current study are not publicly available due to confidentiality but are available from the corresponding author on reasonable request. Requests to access the datasets should be directed to YW15Lm9kb25uZWxsQG5jbC5hYy51aw==.
Ethics statement
The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written or verbal audio-recorded informed consent to participate in the study. Ethical approvals were not required as the study was a service evaluation. A service evaluation application was approved by the NHS Trust Research and Development department (23/5/24:SER-24-277). The local NHS CRIS database oversight committee reviewed the service evaluation and approved collection of retrospective anonymised quantitative health record data.
Author contributions
SW: Writing – review & editing, Project administration, Formal analysis, Writing – original draft, Data curation, Supervision, Investigation, Methodology, Software. ET: Conceptualization, Project administration, Validation, Writing – review & editing, Software, Writing – original draft, Formal analysis, Visualization. KJ: Visualization, Investigation, Conceptualization, Methodology, Writing – review & editing, Writing – original draft. EK: Conceptualization, Visualization, Writing – review & editing, Supervision. EG: Conceptualization, Writing – review & editing, Visualization. AO: Funding acquisition, Project administration, Writing – review & editing, Supervision, Data curation, Writing – original draft, Visualization, Methodology, Formal analysis, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The ADEPT Study was funded by a National Institute for Health and Care Research (NIHR) Advanced Fellowship (ADEPT: Alcohol use disorder and DEpression Prevention and Treatment, Grant: NIHR300616). The NIHR have not had any role in the design, implementation, analysis, write-up and/or dissemination of the research.
Acknowledgments
We are grateful to the research participants to those who helped with study recruitment and the NHS Trust Research and Development Informatics and CRIS team.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1608804/full#supplementary-material
References
1. Department of Health. UK Chief Medical Officers’ Low Risk Drinking Guidelines. London: Department of Health (2016).
2. Davis KA, Coleman JR, Adams M, Allen N, Breen G, Cullen B, et al. Mental health in UK Biobank–development, implementation and results from an online questionnaire completed by 157–366 participants: a reanalysis. BJPsych Open. (2020) 6:e18. doi: 10.1192/bjo.2019.100
3. Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. (2004) 61:807–16. doi: 10.1001/archpsyc.61.8.807
4. Puddephatt JA, Irizar P, Jones A, Gage SH, and Goodwin L. Associations of common mental disorder with alcohol use in the adult general population: a systematic review and meta-analysis. Addiction. (2022) 117:1543–72. doi: 10.1111/add.15735
5. Salokangas RK and Poutanen O. Risk factors for depression in primary care: Findings of the TADEP project. J Affect Disord. (1998) 48:171–80. doi: 10.1016/S0165-0327(97)00171-7
6. Sullivan LE, Fiellin DA, and O’Connor PG. The prevalence and impact of alcohol problems in major depression: a systematic review. Am J Med. (2005) 118:330–41. doi: 10.1016/j.amjmed.2005.01.007
7. Diagnostic and statistical manual of mental disorders: DSM-5. 5th edn. Washington, D.C: American Psychiatric Association (2013).
8. Lai HMX, Cleary M, Sitharthan T, and Hunt GE. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug Alcohol dependence. (2015) 154:1–13. doi: 10.1016/j.drugalcdep.2015.05.031
9. Cornelius JR, Salloum IM, Mezzich J, Cornelius MD, Fabrega H, Ehler JG, et al. Disproportionate suicidality in patients with comorbid major depression and alcoholism. Am J Psychiatry. (1995) 152:358–64. doi: 10.1176/ajp.152.3.358
10. Hjorthøj C, Østergaard MLD, Benros ME, Toftdahl NG, Erlangsen A, Andersen JT, et al. Association between alcohol and substance use disorders and all-cause and cause-specific mortality in schizophrenia, bipolar disorder, and unipolar depression: a nationwide, prospective, register-based study. Lancet Psychiatry. (2015) 2:801–8. doi: 10.1016/S2215-0366(15)00207-2
11. Kelly LM, Liu RT, and Zajac K. Comorbid alcohol-related problems and suicidality disproportionately impact men and emerging adults among individuals with depressive symptoms. J Affect Disord. (2021) 293:329–37. doi: 10.1016/j.jad.2021.06.043
12. Kingsbury M, Sucha E, Horton N, Sampasa-Kanyinga H, Murphy J, Gilman S, et al. Lifetime experience of multiple common mental disorders and 19-year mortality: results from a Canadian population-based cohort. Epidemiol Psychiatr Sci. (2020) 29:e18. doi: 10.1017/S2045796018000859
13. Ogeil RP, McGrath M, Grigg J, Peart A, Meddings JI, Greenwood CJ, et al. Diverging trends in alcohol-related harms: The role of comorbid mental health, suicide and self-harm behaviours in ambulance attendances for alcohol intoxication during the COVID-19 pandemic in Victoria, Australia. J Affect Disord. (2025) 371:170–6. doi: 10.1016/j.jad.2024.11.012
14. Ness J, Hawton K, Bergen H, Cooper J, Steeg S, Kapur N, et al. Alcohol use and misuse, self-harm and subsequent mortality: an epidemiological and longitudinal study from the multicentre study of self-harm in England. Emergency Med J. (2015) 32:793–9. doi: 10.1136/emermed-2013-202753
15. McManus S, Gunnell D, Cooper C, Bebbington PE, Howard LM, Brugha T, et al. Prevalence of non-suicidal self-harm and service contact in England, 2000–14: repeated cross-sectional surveys of the general population. Lancet Psychiatry. (2019) 6:573–81. doi: 10.1016/S2215-0366(19)30188-9
16. Self-harm: assessment, management and preventing recurrence. UK: National Institute for Health and Care Excellence. (NG225 (2022).
17. Connery HS, McHugh RK, Reilly M, Shin S, and Greenfield SF. Substance use disorders in global mental health delivery: epidemiology, treatment gap, and implementation of evidence-based treatments. Harvard Rev Psychiatry. (2020) 28:316–27. doi: 10.1097/HRP.0000000000000271
18. Norström T and Rossow I. Alcohol consumption as a risk factor for suicidal behaviour: a systematic review of associations at the individual and at the population level. Arch Suicide Res. (2016) 20:489–506.
19. Whiteford M and Byrne P. Talking about alcohol: Communities of practice and patient pathways. J Res Nursing. (2015) 20:12–25. doi: 10.1177/1744987114548744
20. Witt K, Chitty KM, Wardhani R, Värnik A, De Leo D, and Kolves K. Effect of alcohol interventions on suicidal ideation and behaviour: A systematic review and meta-analysis. Drug Alcohol dependence. (2021) 226:108885. doi: 10.1016/j.drugalcdep.2021.108885
21. Yang P, Tao R, He C, Liu S, Wang Y, and Zhang X. The risk factors of the alcohol use disorders—through review of its comorbidities. Front Neurosci. (2018) 12:303. doi: 10.3389/fnins.2018.00303
22. Jackson K, Kaner E, Hanratty B, Gilvarry E, Yardley L, and O’Donnell A. Understanding people’s experiences of the formal health and social care system for co-occurring heavy alcohol use and depression through the lens of relational autonomy: A qualitative study. Addiction. (2024) 119:268–80. doi: 10.1111/add.16350
23. Kaufmann CN, Chen L-Y, Crum RM, and Mojtabai R. Treatment seeking and barriers to treatment for alcohol use in persons with alcohol use disorders and comorbid mood or anxiety disorders. Soc Psychiatry Psychiatr Epidemiol. (2014) 49:1489–99. doi: 10.1007/s00127-013-0740-9
24. Powell SK. Handoffs and transitions of care: where is the Lone Ranger’s silver bullet? Professional Case Management (2006) 11:235–7. doi: 10.1097/00129234-200609000-00001
25. Priester MA, Browne T, Iachini A, Clone S, DeHart D, and Seay KD. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: an integrative literature review. J Subst Abuse Treat. (2016) 61:47–59. doi: 10.1016/j.jsat.2015.09.006
26. Finn SW, Mejldal A, and Nielsen AS. Perceived barriers to seeking treatment for alcohol use disorders among the general Danish population–a cross sectional study on the role of severity of alcohol use and gender. Arch Public Health. (2023) 81:65. doi: 10.1186/s13690-023-01085-4
27. Schuler MS, Puttaiah S, Mojtabai R, and Crum RM. Perceived barriers to treatment for alcohol problems: a latent class analysis. Psychiatr Services. (2015) 66:1221–8. doi: 10.1176/appi.ps.201400160
28. DiMartini AF, Leggio L, and Singal AK. Barriers to the management of alcohol use disorder and alcohol-associated liver disease: strategies to implement integrated care models. Lancet Gastroenterol hepatol. (2022) 7:186–95. doi: 10.1016/S2468-1253(21)00191-6
29. Landy MS, Davey CJ, Quintero D, Pecora A, and McShane KE. A systematic review on the effectiveness of brief interventions for alcohol misuse among adults in emergency departments. J Subst Abuse Treat. (2016) 61:1–12. doi: 10.1016/j.jsat.2015.08.004
30. Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, and Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT): toward a public health approach to the management of substance abuse. Alcohol/Drug Screening and Brief Intervention. Boca Raton: CRC Press. (2023). pp. 7–30.
31. Barbosa C, McKnight-Eily LR, Grosse SD, and Bray J. Alcohol screening and brief intervention in emergency departments: review of the impact on healthcare costs and utilization. J Subst Abuse Treat. (2020) 117:108096. doi: 10.1016/j.jsat.2020.108096
32. Crawford M, Csipke E, Brown A, Reid S, Nilsen K, Redhead J, et al. The effect of referral for brief intervention for alcohol misuse on repetition of deliberate self-harm: an exploratory randomized controlled trial. psychol Med. (2010) 40:1821–8. doi: 10.1017/S0033291709991899
33. Padmanathan P, Cohen R, Gunnell D, Biddle L, Griffith E, Breheny K, et al. Development of a brief intervention for emergency department attendees presenting with self-harm and co-occurring substance use problems: A Delphi method study. Crisis: J Crisis Intervention Suicide Prev. (2024) 45:254. doi: 10.1027/0227-5910/a000933
34. Alcohol-specific deaths in the UK: registered in 2020. Deaths caused by diseases known to be a direct consequence of alcohol misuse by sex, age, region and deprivation. London: Office for National Statistics (2021).
35. Corris V, Dormer E, Brown A, Whitty P, Collingwood P, Bambra C, et al. Health inequalities are worsening in the North East of England. Br Med Bulletin. (2020) 134:63–72. doi: 10.1093/bmb/ldaa008
36. Baker C and Kirk-Wade E. Mental health statistics: prevalence, services and funding in England. UK: House of Commons Library. (2023).
39. Noble M, Wright G, Smith G, and Dibben C. Measuring multiple deprivation at the small-area level. Environ Plann A. (2006) 38:169–85. doi: 10.1068/a37168
40. Keetharuth AD, Brazier J, Connell J, Bjorner JB, Carlton J, Buck ET, et al. Recovering Quality of Life (ReQoL): a new generic self-reported outcome measure for use with people experiencing mental health difficulties. Br J Psychiatry. (2018) 212:42–9. doi: 10.1192/bjp.2017.10
41. Field A. Discovering statistics using IBM SPSS statistics. UK: Sage publications limited (2024).
42. Proudfoot K. Inductive/deductive hybrid thematic analysis in mixed methods research. J mixed Methods Res. (2023) 17:308–26. doi: 10.1177/15586898221126816
43. Clarke V and Braun V. Thematic analysis. J Positive Psychol. (2017) 12:297–8. doi: 10.1080/17439760.2016.1262613
44. Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, et al. Addressing the burden of mental, neurological and substance use disorders: Key messages from Disease Control Priorities. Lancet. (2016) 387:1672–85.
45. Steeg S, Bickley H, Clements C, Quinlivan LM, Barlow S, Monaghan E, et al. Care gaps among people presenting to the hospital following self-harm: observational study of three emergency departments in England. BMJ Open. (2024) 14:e085672. doi: 10.1136/bmjopen-2024-085672
46. Alpers SE, Pallesen S, Vold JH, Haug E, Lunde L-H, Skogen JC, et al. The association between psychological distress and alcohol consumption and physical activity: a population-based cohort study. Front Psychiatry. (2023) 14:1181046. doi: 10.3389/fpsyt.2023.1181046
47. Oldham M, Beard E, Loebenberg G, Dinu L, Angus C, Burton R, et al. Effectiveness of a smartphone app (Drink Less) versus usual digital care for reducing alcohol consumption among increasing-and-higher-risk adult drinkers in the UK: a two-arm, parallel-group, double-blind, randomised controlled trial. EClinicalMedicine. (2024) 70. doi: 10.1016/j.eclinm.2024.102534
48. Csillik A, Devulder L, Fenouillet F, and Louville P. A pilot study on the efficacy of motivational interviewing groups in alcohol use disorders. J Clin Psychol. (2021) 77:2746–64. doi: 10.1002/jclp.23265
49. Curtiss JE, Wallace B, Fisher LB, Nyer M, Jain F, Cusin C, et al. Change processes in cognitive behavioural therapy and motivational interviewing for depression and heavy alcohol use: A network approach. J Affect Disord Rep. (2021) 3:100040.
50. O’Donnell A, Schmidt CS, Beyer F, Schrietter M, Anderson P, Jane-Llopis E, et al. Effectiveness of digital interventions for people with comorbid heavy drinking and depression: A systematic review and narrative synthesis. J Affect Disord. (2022) 298:10–23. doi: 10.1016/j.jad.2021.11.039
51. Coexisting severe mental illness and substance misuse: community health and social care services. UK: National Institute for Health and Care Excellence (NG58 (2016).
52. Better care for people with co-occurring mental health and alcohol/drug use conditions. A guide for commissioners and service providers. England: Public Health (2017).
53. Alcohol and Mental Health: Policy and practice in England. London: Institute for Alcohol Studies & Centre for Mental health (2018).
54. Stott A and Priest H. Narratives of recovery in people with coexisting mental health and alcohol misuse difficulties. Adv Dual Diagnosis. (2018) 11:16–29. doi: 10.1108/ADD-08-2017-0012
55. Duncan G, Saunders A, Gadsby B, and Hazard A. The Bradley Report five years on. London, England: Centre for Mental Health (2014).
57. Sinclair JM, King M, Masson S, and Gilmore I. UK needs national strategy to tackle alcohol related harms. UK: British Medical Journal Publishing Group (2025).
58. Guest G. Describing mixed methods research: An alternative to typologies. J mixed Methods Res. (2013) 7:141–51. doi: 10.1177/1558689812461179
59. NHS. 10 Year Health Plan for England: fit for the future. UK: National Health Service England (2025).
60. Pandian H and Kar N. Profile, referral pathways and re-attendance of psychiatric patients attending the emergency department: focus on suicidality & self-harm. BJPsych Open. (2021) 7:S339–S40. doi: 10.1192/bjo.2021.890
61. Alcohol-specific deaths in the UK: registered in 2023. UK: Office for National Statistics (2025). Available online at: https://www.ons.gov.uk/releases/alcoholspecificdeathsintheukregisteredin2023 (Accessed August 6, 2025).
Keywords: alcohol, non-dependent, rapid access, intervention, self-harm
Citation: Wigham S, Titchener E, Jackson K, Kaner E, Gilvarry E and O’Donnell A (2025) Personalised care for people with excessive alcohol use following an episode of self-harm: a mixed methods community case study in a psychiatric liaison team. Front. Psychiatry 16:1608804. doi: 10.3389/fpsyt.2025.1608804
Received: 09 April 2025; Accepted: 28 July 2025;
Published: 22 August 2025.
Edited by:
Alexander Michael Ponizovsky, Ministry of Health, IsraelReviewed by:
Liza Hopkins, The Alfred Hospital, AustraliaPrianka Padmanathan, University of Bristol, United Kingdom
Copyright © 2025 Wigham, Titchener, Jackson, Kaner, Gilvarry and O’Donnell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amy O’Donnell, YW15Lm9kb25uZWxsQG5ld2Nhc3RsZS5hYy51aw==
 Sarah Wigham
Sarah Wigham Elizabeth Titchener1
Elizabeth Titchener1