- 1Department of Otolaryngology, Affiliated Hospital of Nantong University, Medical School of Nantong University, Nantong, Jiangsu, China
- 2Department of Otolaryngology, Rugao Branch Institute, Affiliated Hospital of Nantong University, Nantong, Jiangsu, China
Introduction: Sleep plays an important role in maintaining physical and mental health, and it is important to study the relationship between sleep duration and new-onset emotional, nervous, or psychiatric problems (ENP).
Methods: A prospective cohort study was performed based on data from Wave 2011, 2013,2015 and 2018 in the China Health and Retirement Longitudinal Study (CHARLS) databases. Sleep duration was assessed by self-reported nighttime sleep and daytime nap duration. Self-reported diagnoses were used to identify the new-onset emotional, nervous, or psychiatric problems (ENP). We used different logistic regression models to explore the potential effects of sleep duration on ENP and performed mediation analyses to assess the mediating roles of BMI, hypertension, and diabetes(DM).
Results: Among 10,225 participants, 221 (2.16%) developed ENP during follow-up. The mean nighttime sleep duration was significantly shorter in the ENP group than in the non-ENP group. A restricted cubic spline regression model revealed a U-shaped relationship between nighttime sleep duration and ENP risk, with the lowest risk at 6.5 hours. Mediation analyses showed that BMI, hypertension, and diabetes did not significantly mediate this association (P values for ACME were all greater than 0.05).
Conclusion: A U-shaped association was observed between nighttime sleep duration and new-onset ENP, suggesting that both insufficient and excessive sleep may increase the risk of ENP. These findings highlight the importance of maintaining an optimal sleep duration for mental well-being.
1 Introduction
Anxiety and other mental health problems are prevalent worldwide and have become a major public health challenge (1, 2). Recent statistics show that one in four to five people suffer from common mental illnesses, and 29.2% have experienced an episode of a common mental disorder in their lifetime (3, 4). Meanwhile, the overlap of somatic symptoms, anxiety, and depressive symptoms are common in the general population (3). It is well known that sleep plays a crucial role in maintaining physical and mental health (5). Sleep deprivation is recognized as a common symptom and risk factor for a variety of psychiatric disorders and is strongly associated with anxiety and mood disorders (6). Sleep deprivation can lead to a variety of adverse outcomes, such as insomnia that can lead to depressive symptoms, suicidal ideation, metabolic syndrome, and unexpected work-related deaths (7). Sleep deprivation can significantly impair an individual’s emotional regulation, leading to an amplification of negative emotional experiences (such as anxiety, depression, and irritability) and a reduction in positive emotional experiences (8). Sleep deprivation is also considered a significant risk factor in the onset and development of anxiety symptoms (9). Long-term sleep deprivation itself is an important risk factor for the onset of depression and may exacerbate existing depressive symptoms (10). Therefore, studying the impact of sleep duration on emotional, nervous, or psychiatric problems (ENP) is of great significance.
However, previous studies have mostly employed cross-sectional designs or short-term experimental sleep deprivation (11), making it difficult to reveal the long-term dynamic relationship and causal link between sleep and ENP. Therefore, there is an urgent need to design rigorous prospective cohort studies for further investigation.
To the best of our knowledge, no studies have reported on the relationship between sleep duration and new-onset ENP in Chinese middle-aged and elderly populations. Therefore, the present study aimed to investigate the potential association between the two and to provide scientific evidence and feasible suggestions for reducing the incidence of ENP from the perspective of sleep duration.
2 Materials and methods
2.1 Study population
This study used data from the China Health and Retirement Longitudinal Study (CHARLS) database (https://charls.pku.edu.cn/), a nationally representative survey established in 2011 to assess the aging population in China. The CHARLS project utilizes multistage stratified probability sampling and collects detailed demographic, health, and psychosocial information through face-to-face interviews. The cohort includes individuals aged 45 and older, making it an ideal dataset for examining the temporal relationship between sleep duration and the onset of emotional, nervous, or psychiatric problems (ENP) in middle-aged and elderly populations.
We performed a prospective cohort analysis using data from four waves: 2011 (baseline), 2013, 2015, and 2018. Participants were included if they had available sleep and ENP data and no ENP at baseline (2011). Those lost to follow-up or with incomplete covariate data were excluded. The baseline sample consisted of 10,225 participants, with an overall retention rate of 80.5% for the first wave (12). This high retention supports the robustness and internal validity of the study design.
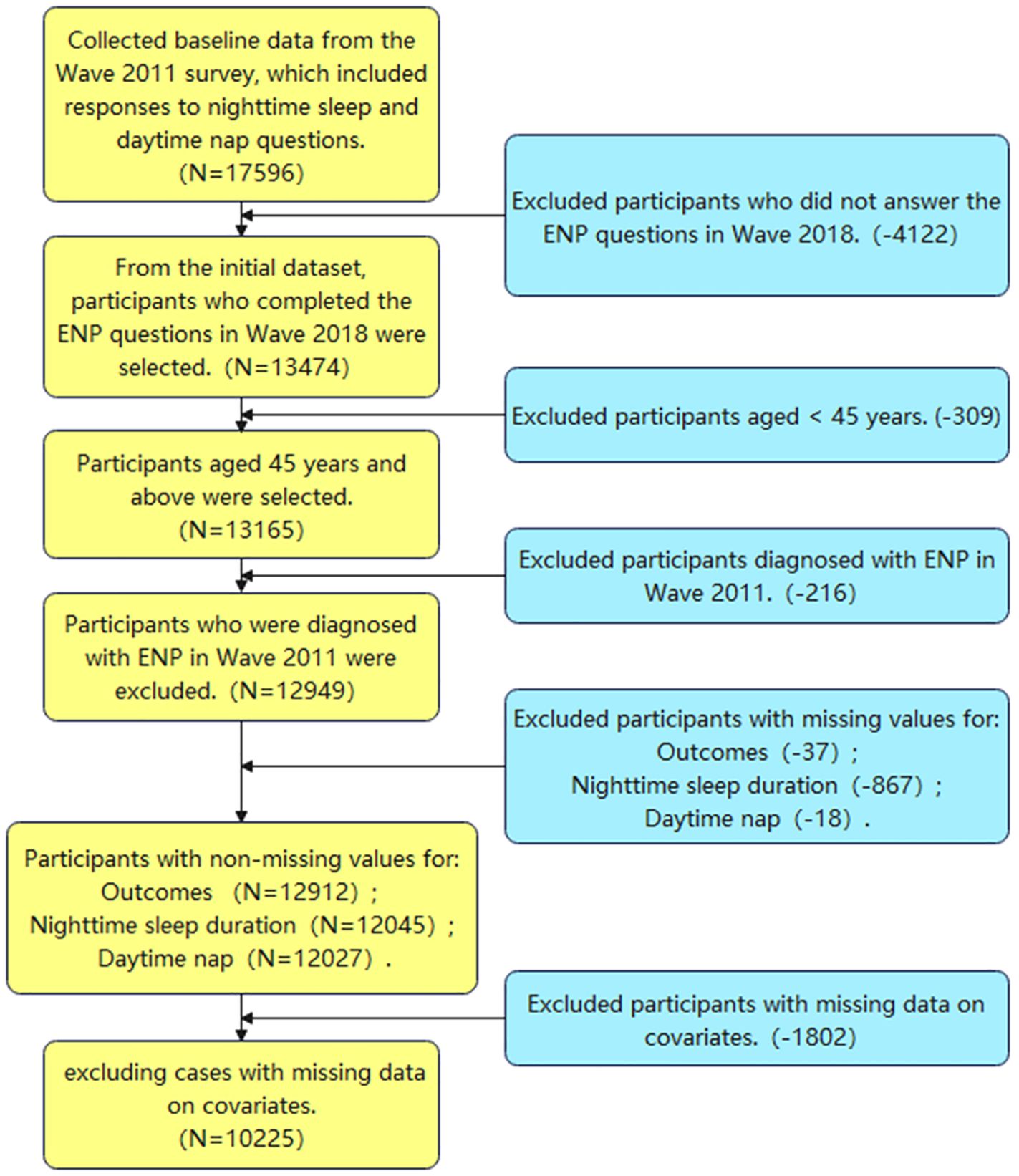
Figure 1 illustrates the screening process, starting with an initial inclusion population of 17,596. Following the process, we excluded 7,371 individuals, culminating in a final baseline data population of 10,225.
2.2 Sleep duration assessment
Sleep duration (hours) includes both nighttime sleep and daytime nap, as reported by respondents in the self-report questionnaire. The nighttime sleep duration (hours) was assessed using the question “DA049. During the past month, how many hours of actual sleep did you get at night (average hours for one night)?”. The daytime nap (minutes) was assessed based on responses to the question “DA050. During the past month, how long did you take a nap after lunch?”
2.3 Assessment of new-onset ENP
New-onset ENP was diagnosed using self-report data DA007 (11). When the interviewer inquired, “Have you received a diagnosis from a doctor for emotional, nervous, or psychiatric issues?” and the respondent responded in the affirmative, we recognized them as having an ENP. We eliminated subjects who received an ENP diagnosis in 2011, but included individuals diagnosed with an ENP after that until the 2018 follow-up period, according to our criteria for a new-onset ENP.
2.4 Assessment of covariates
Socio-demographic characteristics such as age, gender, marital status, education level (primary, below high school, or university and above) and place of residence (rural/urban) were included in this study. Lifestyle factors included smoking and alcohol consumption status. Current diseases included hypertension and diabetes. In addition, different weight statuses defined according to body mass index (BMI) criteria were important covariates, including underweight (BMI < 18.5), healthy weight (18.5 ≤ BMI < 24), overweight (24 ≤ BMI < 28), and obesity (BMI ≥ 28), which we considered categorical variables in our stratified analyses, but for logistic regression and mediation analyses, BMI was treated as a continuous variable.
2.5 Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD) and categorical variables as percentages. We used multivariate logistic regression analysis to investigate the association between sleep duration and new-onset ENP in depth. We used three models to calculate the ratio (OR) and 95% confidence intervals (CI) of the association between sleep duration and the risk of new-onset ENP: crude model, an unadjusted model; model 1, which was adjusted for sociodemographic variables including age, gender, education, location of residence, BMI, and marital status; and model 2, which was further adjusted for the confounding factors such as smoking status, alcohol consumption status, hypertension, and DM. We also conducted interaction analyses to explore the effects of covariate factors on the sleep-ENP association and restricted cubic spline analysis to visually elucidate the dose-response relationship between sleep duration and the risk of new-onset ENP. Data analysis was performed with R software (Version 4.2.2).
3 Results
3.1 Characteristics of the study population
Subgroups were compared in this study based on the presence or absence of ENP (221 with ENP (2.16%) and 10,004 without ENP). The overall sample size was 10,225 people, and there were significant differences between the diseased and non-diseased groups in terms of age, gender, education level, alcohol consumption, and hours of sleep (Table 1). First, the mean age of the diseased group was significantly higher than that of the non-diseased group (59.50 ± 8.56 vs. 58.29 ± 8.77, P = 0.04). There was also a difference in gender composition, with 65.61% females in the diseased group, which was significantly higher than 53.31% in the non-diseased group (P < 0.001). In addition, in terms of education level, the proportion of those who received high school and below education was significantly higher in the diseased group than in the non-diseased group (76.47% vs. 67.92%, P = 0.02), whereas the proportion of those who received university and above education was lower. Smoking status showed a tendency to be significantly different between the two groups (P = 0.05), and drinking habits also showed a significant difference, with a significantly higher proportion of those who had been drinking for more than 1 month in the diseased group than in the non-diseased group (17.19% vs. 25.30%, P = 0.01). Regarding sleep duration, the mean sleep duration was shorter in the diseased group (5.98 ± 2.21 hours vs. 6.39 ± 1.84 hours, P < 0.01), but there was no significant difference in nap time (P = 0.99). Hypertension and diabetes mellitus (DM) were both higher in the prevalent group, but did not reach significant levels (P = 0.07 and P = 0.09). Finally, BMI was not significantly different between the two groups (P = 0.79).
3.2 Relationship between sleep duration and risk of new-onset ENP
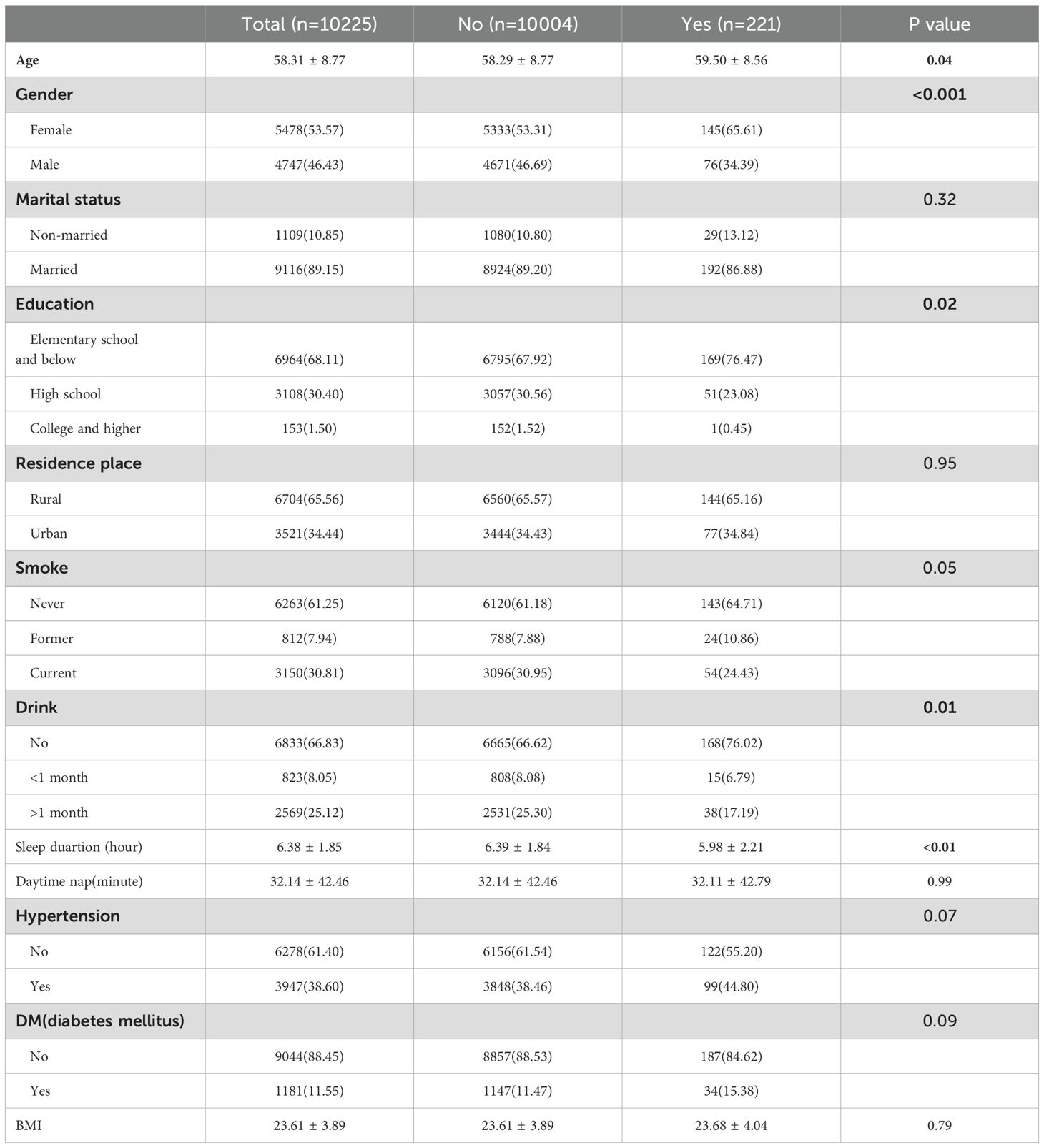
Three models were used in this investigation to comprehensively examine the impact of sleep duration on the risk of new-onset ENP (Table 2, Figure 2). A substantial reduction in the risk of new-onset ENP was linked to longer overnight sleep duration in Crude, Model 1, and Model 2 (P<0.05). In particular, after controlling for all factors, the incidence of ENP decreased by almost 24% with every inter-quartile range (IQR) increase in sleep duration, OR = 0.76 (95% CI: 0.62, 0.94, p = 0.01). Using Q1 as the reference group, we evaluated the relationship between longer sleep duration and new-onset ENP after stratifying nocturnal sleep duration into quartile (Q1, Q2, Q3, Q4). Q3 showed a considerably reduced risk in all three models, and the trend test revealed a significant trend impact of sleep length in all three models (P<0.05), suggesting that the risk of ENP gradually decreased as sleep duration increased.
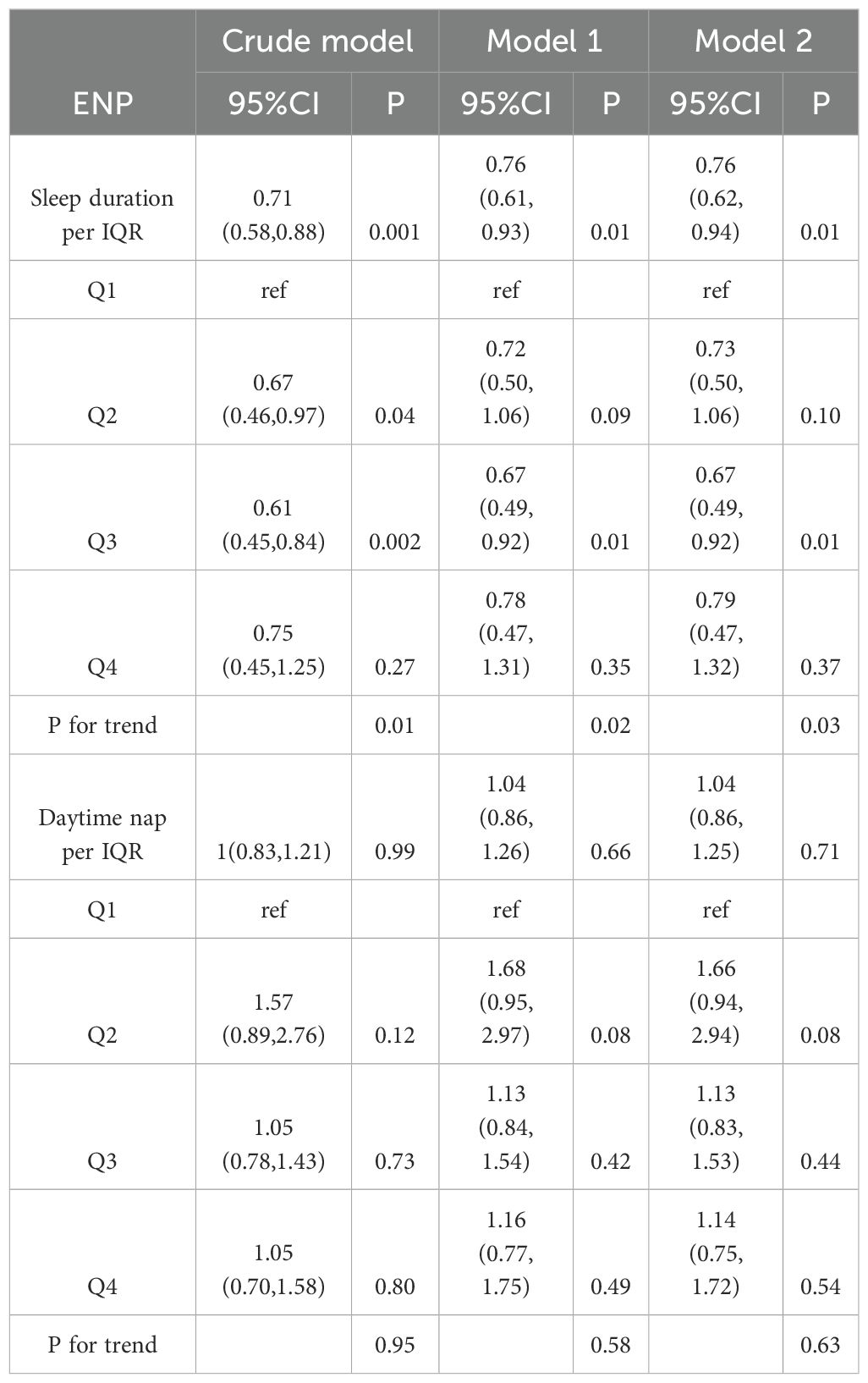
Table 2. Prospective associations between baseline sleep duration and daytime naps with follow-up new-onset ENP.
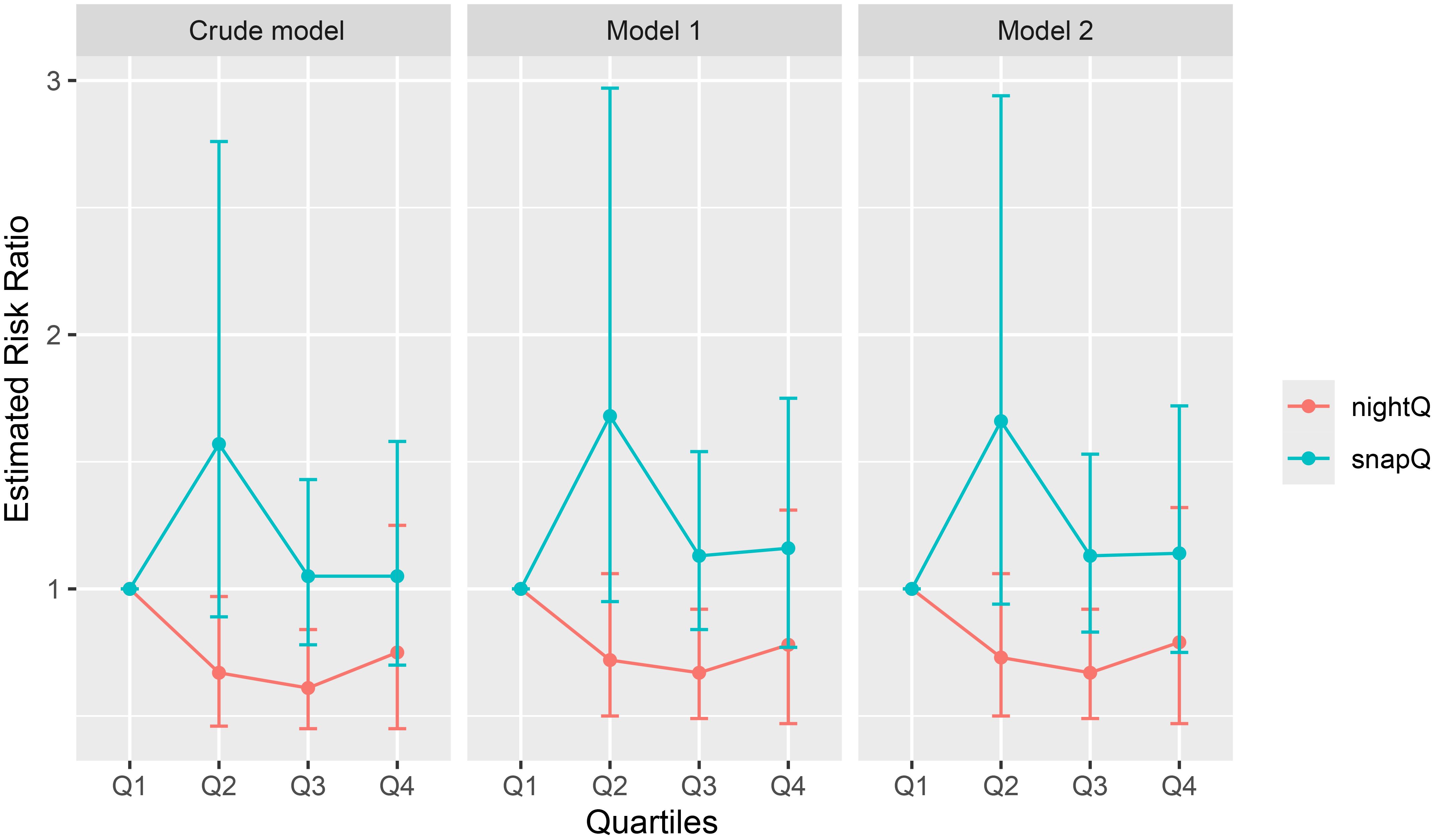
Figure 2. Effects of nighttime sleep duration quartile (nightQ) and nap duration quartile (napQ) on ENP in three different models (Crude model: an unadjusted model; Model 1: adjusted for age, gender, education, location of residence, BMI, and marital status; Model 2: further adjusted for smoking status, alcohol consumption status, hypertension, and DM).
The Restricted Cubic Splines (RCS) regression model was used to examine the link between overnight sleep duration and new-onset ENP risk (Figure 3). In all models, nighttime sleep duration and ENP risk showed a U-shaped curve relationship: shorter sleep duration (less than 6.5 hours) was associated with a significantly higher risk of ENP, and the risk gradually decreased with increasing sleep duration, reaching the lowest point after 6.5 hours, and then increased. At the ideal sleep duration (6.5 hours), new-onset ENP risk was the lowest.The relationship between sleep duration and new-onset ENP was significant (P-overall < 0.05) and non-linear (P-non-linear < 0.05) across all models (Figure 3A).
We also performed research on relationship between daytime naps and new-onset ENP, which found no significant connection and no significant trend across models and subgroups (Figure 3B). The P-value for each model was larger than 0.05 (P-overall > 0.8), and the non-linear test (P-non-linear) was likewise greater than 0.05, showing that there was no significant linear or non-linear relationship between daytime naps and new-onset ENP.
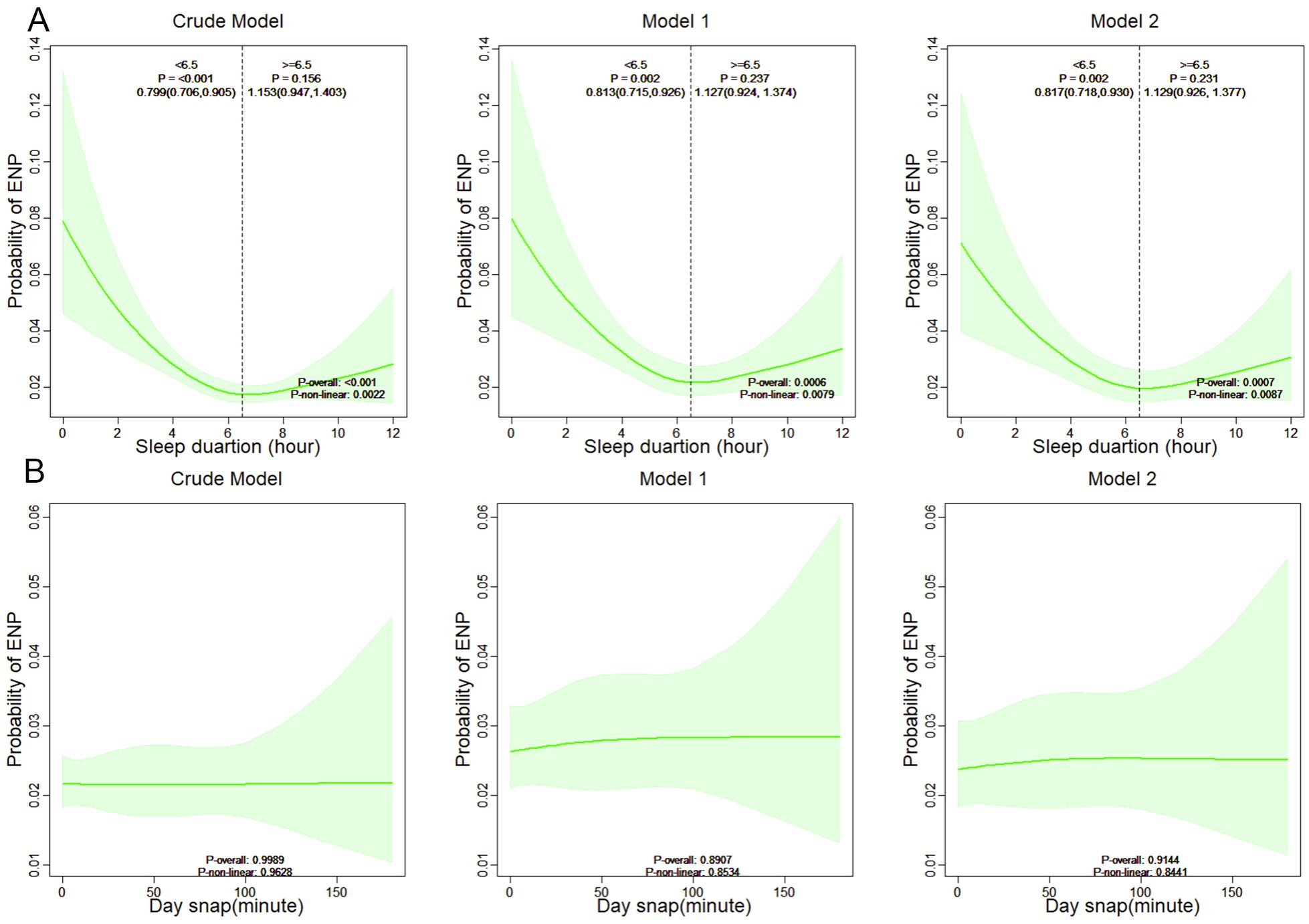
Figure 3. Association between sleep duration (A), daytime nap (B) and risk of new-onset ENP in restricted cubic spline analysis.
3.3 Subgroup analysis
Further subgroup analyses were conducted to investigate the variability of effects across groups, evaluate the stability of effects, and identify potential interactions (Figure 4). The results indicated that the risk of new-onset ENP was significantly reduced by increased nighttime sleep duration in the following subgroups: age, sex, married, high school education, living in the countryside, never-smokers, those with a BMI between 18.5-24, those without diabetes, and those without hypertension. The interaction analysis revealed that the effect of sleep on new-onset ENP was influenced by education and alcohol consumption factors.
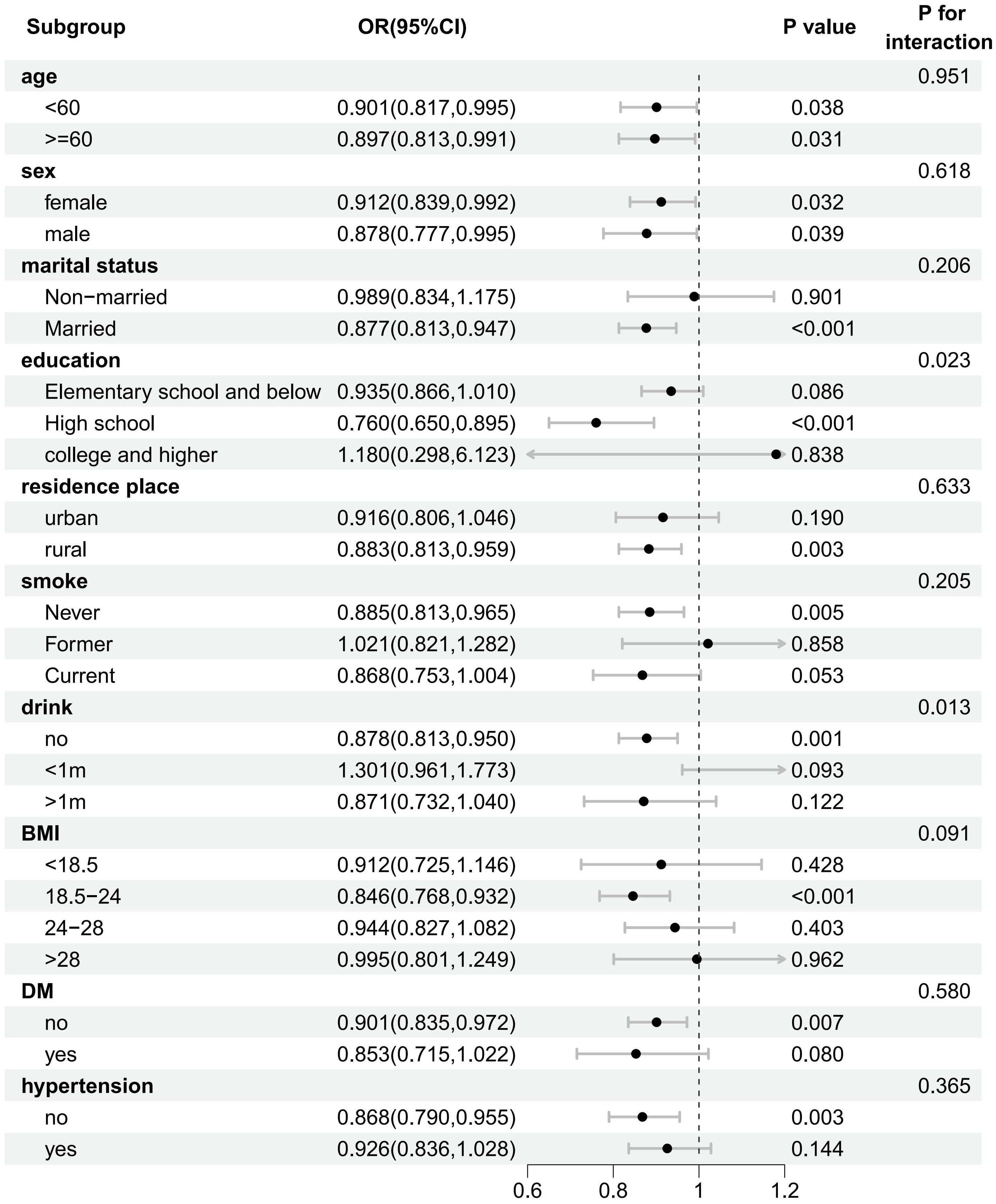
Figure 4. Forest plot of the stratified analysis of the association between sleep duration and risk of new-onset ENP.
3.4 Mediation analysis
In this study, we assessed the mediating effects of BMI, hypertension, and DM on the risk of new-onset ENP by mediation effect analysis of sleep duration at night (Table 3). The results showed that BMI, hypertension, and DM as mediating variables did not show significant mediating effects (P values of ACME were all greater than 0.05), suggesting that the indirect effects of sleep duration on ENP through BMI, hypertension, and DM were weak. However, the direct effect of nocturnal sleep duration on ENP was significant (all P values for ADE <0.05), indicating that nocturnal sleep duration was still significantly associated with new-onset ENP even after controlling for the effects of BMI, hypertension, and DM. Overall, the mediating role of BMI between nocturnal sleep duration and new-onset ENP was limited, and the effect of nocturnal sleep duration on the risk of new-onset ENP was mainly direct.
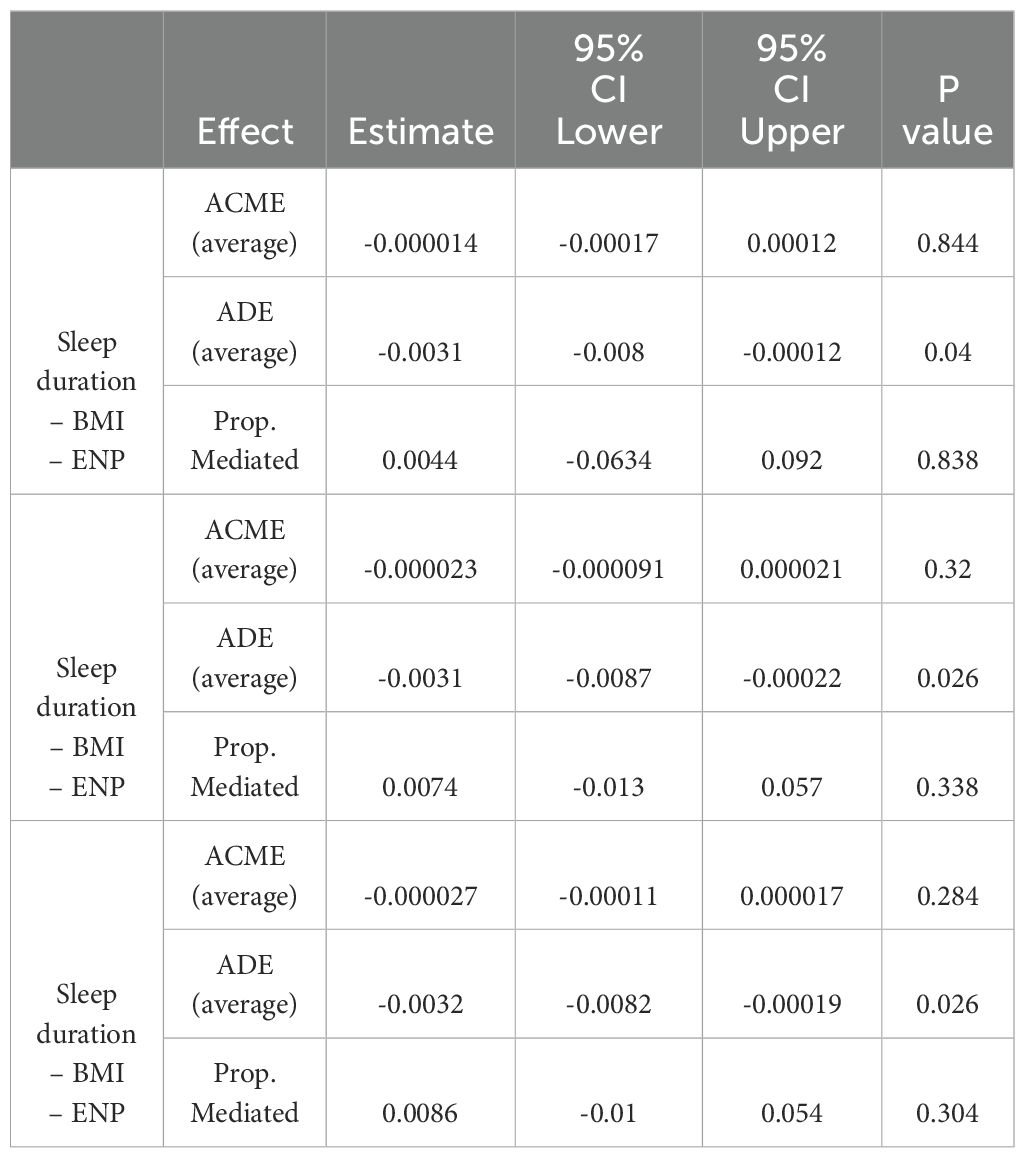
Table 3. Mediation effect of BMI, hypertension, and diabetes mellitus in the association between sleep duration and new-onset ENP.
4 Discussion
This study analyzed the association between total sleep duration (including nighttime sleep duration and daytime nap) and new-onset ENP using survey data from WAVE 2011, WAVE 2013, WAVE 2015, and WAVE 2018. After adjusting for the effects of covariates such as sex, age, BMI, hypertension and DM, the longer the total nighttime sleep duration, the lower the risk of ENP. Further analysis revealed a U-shaped relationship between nighttime sleep duration and the risk of new-onset ENP: When nighttime sleep duration was less than 6.5 hours, the risk of ENP gradually decreased with increasing sleep duration, reached a lowest point (6.5 hours), and then began to increase with further increases in sleep duration. This suggests that too little or too much sleep may increase the risk of ENP, and that an appropriate amount of sleep (6.5 hours) is ideal for mental health.
A substantial body of research has demonstrated the strong correlation between sleep and mental health, with sleep deprivation being identified as a significant risk factor for the development of mental health disorders (13). Adequate and high-quality sleep is not only essential for physiological recovery but also confers benefits with respect to cognitive function, mood regulation, immune system function and metabolic processes (14). During sleep, there is a notable increase in the convective exchange of cerebrospinal and interstitial fluids, which facilitates the removal of potentially neurotoxic waste products that may accumulate in the central nervous system during waking hours (15). The issue of sleep deprivation has been identified as a significant public health concern (16). Furthermore, research indicates that variations in sleep duration may be influenced by gender and ethnicity (17). The risk of adverse metabolic effects associated with sleep deprivation is also age-dependent (18). Nighttime sleep deprivation is a direct contributor to daytime sleepiness and impaired mood regulation, which in turn gives rise to more negative emotions and an increased risk of psychiatric disorders (19). From a mechanistic perspective, sleep deprivation may contribute to the development of age-related endothelial dysfunction, thereby accelerating the onset and progression of cardiovascular disease (20). Concurrently, diminished sleep duration is linked to elevated concentrations of growth hormone-releasing peptide, which influences energy metabolism by stimulating gastrointestinal motility and reducing insulin secretion (21). Furthermore, sleep deprivation may also serve to exacerbate the severity of mental health problems by increasing inflammatory responses (22). The results of the present study corroborate those of previous studies, confirming that a reduction in sleep duration is associated with an increased risk of new-onset ENP. In the present study, for each inter-quartile range (IQR) increase in sleep duration, the risk of psychiatric disorders was observed to decrease by approximately 29% (OR = 0.71, 95% CI: 0.58-0.88, P = 0.001). The present study also found, through further analysis, that an optimal sleep duration minimizes the risk of ENP, and in the present study this optimal sleep duration was 6.5 hours. Similar studies have previously provided support for this hypothesis. For example, Sun et al. identified a ‘U-shaped’ association between sleep duration and the risk of chronic kidney disease (CKD). Specifically, those who slept ≤4 or >10 hours per night exhibited an elevated risk of developing CKD compared to individuals who slept 6–8 hours per night (23). Similarly, Chen et al. found that an optimal sleep duration of 6–8 hours resulted in the lowest risk of developing atrial fibrillation compared to shorter or longer sleep duration (24).
The controversy over the relation between BMI and psychiatric disorders has not yet reached a consensus. Some studies have suggested that high BMI may affect mental health and emotional stability, and even depression, through biological mechanisms such as inflammation or endocrine dysregulation (25). However, some of the literature suggests that there is no significant association between BMI and mental disorders (26). The association between hypertension and mental disorders is also controversial. One study found that the prevalence of psychiatric disorders was significantly higher in hypertensive patients than in controls, with depression and anxiety being the most common symptoms (27). However, it has also been reported that there is no direct relationship between hypertension as part of metabolic dysfunction and depressed mood (28). The relationship between diabetes mellitus (DM) and ENP is similarly controversial. A cohort study of 1691 patients with type 2 diabetes showed that depressive symptoms may exacerbate diabetes distress, which in turn affects the severity of depressive symptoms (29). However, it has also been suggested that regardless of whether there is an association between diabetes and mental illness, the relationship may be confounded by socioeconomic status, lifestyle and genetic factors, among others. The development of mental health problems may not be a direct result of diabetes, but may be triggered by these common risk factors (30). In the present study, we explored the mediation roles of BMI, hypertension and diabetes in the relationship between nighttime sleep and the onset of ENP. The results of the mediation analyses showed that BMI, hypertension and diabetes did not have a significant mediating effect and that the effect of nighttime sleep duration on ENP was mainly direct rather than indirect through these covariates.
Furthermore, this study examined the influence of additional prevalent covariates on ENP, including age, gender, marital status, smoking, alcohol consumption, place of residence, and level of education. Among the factors exhibiting a significant effect were age, gender, education, and alcohol consumption. The results of our study indicate that females and older age groups are more susceptible to ENP symptoms. Additionally, individuals with lower levels of education may be at an elevated risk of developing ENP due to their exposure to life stressors and limited access to health resources. These findings are consistent with previously reported observations in the literature (31, 32). Additionally, our findings indicate an elevated risk of ENP among individuals who have never consumed alcohol. This observation contrasts with the majority of previous studies, which have concluded that alcohol consumption is significantly associated with psychiatric symptoms (33, 34). However, our results align with those of a survey study from rural China, which revealed a notable correlation between alcohol consumption and farmers’ mental well-being. Farmers who consumed alcohol exhibited a 19.7% higher mental health index compared to those who abstained from alcohol (35). We infer that the distinctive characteristics of the Chinese population may be the cause of these discrepancies.
Although the present study provides valuable insights into the relationship between nighttime sleep duration and new-onset ENP, it has several limitations. Firstly, the study primarily relied on participant self-reports for data, potentially leading to recall bias and compromising data accuracy. Secondly, this study did not measure sleep quality in detail, and future studies should incorporate objective sleep monitoring data to enhance data accuracy and further distinguish the effects of sleep duration and sleep quality. Thirdly, while we analyzed the effects of covariates such as BMI, hypertension, DM, smoking, and alcohol consumption and their mediating roles, we neglected to explore the underlying biological mechanisms, such as inflammation, neurotransmitters, or changes in hormone levels, that could significantly influence the relationship between sleep duration and the occurrence of ENP. Therefore, future studies should include the measurement of biomarkers to further elucidate the biological mechanisms of sleep duration on ENP.
5 Conclusion
Nighttime sleep duration showed a U-shaped relationship with the risk of new-onset ENP, with the most appropriate nighttime sleep duration (6.5 hours in this study) being associated with the lowest incidence of ENP. This finding provides new insights into our understanding of the relationship between sleep and mental health and highlights the need to consider sleep as an important intervention point when developing public health strategies and mental health interventions.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
The studies involving humans were approved by The Ethical Review Committee of Peking University(IRB approval number: IRB00001052-11015). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HW: Writing – original draft. SW: Writing – review & editing. BZ: Writing – review & editing. HN: Conceptualization, Software, Formal Analysis, Data curation, Resources, Writing – original draft, Project administration.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank the China Health and Retirement Longitudinal Study team for providing data and training in using the datasets. We thank all volunteers and staff involved in this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1609865/full#supplementary-material
References
1. Bakhtiari-Dovvombaygi H, Izadi S, Zare M, Asgari Hassanlouei E, Dinpanah H, Ahmadi-Soleimani SM, et al. Vitamin D3 administration prevents memory deficit and alteration of biochemical parameters induced by unpredictable chronic mild stress in rats. Sci Rep. (2021) 11:16271. doi: 10.1038/s41598-021-95850-6
2. Edmealem A and Olis CS. Factors Associated with Anxiety and Depression among Diabetes, Hypertension, and Heart Failure Patients at Dessie Referral Hospital, Northeast Ethiopia. Behav Neurol. (2020) 2020:3609873. doi: 10.1155/2020/3609873
3. Belete A, Abate MW, Nigat AB, Tigabu A, Bantie B, Yirga GK, et al. The magnitude of common mental illness and associated factors among adult holy water users in Amhara regional state Orthodox Tewahido churches, Ethiopia, 2021. BMC Psychiatry. (2023) 23:53. doi: 10.1186/s12888-023-04524-2
4. Faris N, Baroud E, Al Hariri M, Bachir R, El-Khoury J, and Batley NJ. Characteristics and dispositional determinants of psychiatric emergencies in a University Hospital in Beirut. Asian J Psychiatr. (2019) 42:42–7. doi: 10.1016/j.ajp.2019.03.024
5. Yi SJ, Jeong YM, and Kim JH. Relationship between sleep duration trajectories and self-rated depressive symptoms in South Koreans with physical disabilities. Healthcare (Basel). (2021) 9(3):361. doi: 10.3390/healthcare9030361
6. Mu FZ, Liu J, Lou H, Zhu WD, Wang ZC, and Li B. Influence of physical exercise on negative emotions in college students: chain mediating role of sleep quality and self-rated health. Front Public Health. (2024) 12:1402801. doi: 10.3389/fpubh.2024.1402801
7. Takano Y, Iwano S, Aoki S, Nakano N, and Sakano Y. A systematic review of the effect of sleep interventions on presenteeism. Biopsychosoc Med. (2021) 15:21. doi: 10.1186/s13030-021-00224-z
8. Meneo D, Samea F, Tahmasian M, and Baglioni C. The emotional component of insomnia disorder: A focus on emotion regulation and affect dynamics in relation to sleep quality and insomnia. J Sleep Res. (2023) 32:e13983. doi: 10.1111/jsr.13983
9. Singh A. A critical analysis of impact of sleep deprivation on emotional regulation. Int J Psychol. (2024) 9:64–71. doi: 10.47604/ijp.2852
10. Irwin MR, Olmstead R, Carrillo C, Sadeghi N, Fitzgerald JD, Ranganath VK, et al. Sleep loss exacerbates fatigue, depression, and pain in rheumatoid arthritis. Sleep. (2012) 35:537–43. doi: 10.5665/sleep.1742
11. Da SA, Vieira BA, and Dos SJ. The relationship between sleep deprivation and the worsening of mood disorders in health professionals working night shifts. Dement Neuropsychol. (2025) 19:e20240186. doi: 10.1590/1980-5764-DN-2024-0186
12. Zhao Y, Hu Y, and Smith JP. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
13. Dagani J, Buizza C, Cela H, Sbravati G, Rainieri G, Ghilardi A, et al. The interplay of sleep quality, mental health, and sociodemographic and clinical factors among italian college freshmen. J Clin Med. (2024) 13(9):2626. doi: 10.3390/jcm13092626
14. Gong M, Sun M, Sun Y, Jin L, and Li S. Effects of acute sleep deprivation on sporting performance in athletes: A comprehensive systematic review and meta-analysis. Nat Sci Sleep. (2024) 16:935–48. doi: 10.2147/NSS.S467531
15. Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, et al. Sleep drives metabolite clearance from the adult brain. Science. (2013) 342:373–7. doi: 10.1126/science.1241224
16. Seow LSE, Tan XW, Chong SA, Vaingankar JA, Abdin E, Shafie S, et al. Independent and combined associations of sleep duration and sleep quality with common physical and mental disorders: Results from a multi-ethnic population-based study. PloS One. (2020) 15:e0235816. doi: 10.1371/journal.pone.0235816
17. Dietch JR, Taylor DJ, Smyth JM, Ahn C, Smith TW, Uchino BN, et al. Gender and racial/ethnic differences in sleep duration in the North Texas heart study. Sleep Health. (2017) 3:324–7. doi: 10.1016/j.sleh.2017.07.002
18. Arora A, Pell D, van Sluijs EMF, and Winpenny EM. How do associations between sleep duration and metabolic health differ with age in the UK general population? PloS One. (2020) 15:e0242852. doi: 10.1371/journal.pone.0242852
19. Palmer CA and Alfano CA. Sleep and emotion regulation: An organizing, integrative review. Sleep Med Rev. (2017) 31:6–16. doi: 10.1016/j.smrv.2015.12.006
20. Matsuzawa Y, Kwon TG, Lennon RJ, Lerman LO, and Lerman A. Prognostic value of flow-mediated vasodilation in brachial artery and fingertip artery for cardiovascular events: A systematic review and meta-analysis. J Am Heart Assoc. (2015) 4(11):e002270. doi: 10.1161/JAHA.115.002270
21. Lin J, Jiang Y, Wang G, Meng M, Zhu Q, Mei H, et al. Associations of short sleep duration with appetite-regulating hormones and adipokines: A systematic review and meta-analysis. Obes Rev. (2020) 21:e13051. doi: 10.1111/obr.13051
22. Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol. (2015) 66:143–72. doi: 10.1146/annurev-psych-010213-115205
23. Sun H, Qin K, Zou C, Wang HH, Lu C, Chen W, et al. The association of nighttime sleep duration and quality with chronic kidney disease in middle-aged and older Chinese: a cohort study. Sleep Med. (2021) 86:25–31. doi: 10.1016/j.sleep.2021.08.007
24. Sun H, Qin K, Zou C, Wang HH, Lu C, Chen W, et al. Increased susceptibility to new-onset atrial fibrillation in diabetic women with poor sleep behaviour traits: findings from the prospective cohort study in the UK Biobank. Diabetol Metab Syndr. (2024) 16:51. doi: 10.1186/s13098-024-01292-1
25. Forte G, Favieri F, Pazzaglia M, and Casagrande M. Mental and body health: the association between psychological factors, overweight, and blood pressure in young adults. J Clin Med. (2022) 11(7):1999. doi: 10.3390/jcm11071999
26. Elia C, Karamanos A, Silva MJ, O'Connor M, Lu Y, Dregan A, et al. Weight misperception and psychological symptoms from adolescence to young adulthood: longitudinal study of an ethnically diverse UK cohort. BMC Public Health. (2020) 20:712. doi: 10.1186/s12889-020-08823-1
27. Kaya T and Demir N. Evaluation of patients diagnosed with essential hypertension in terms of mental and personality disorders. Alpha Psychiatry. (2024) 25:54–62. doi: 10.5152/alphapsychiatry.2024.231363
28. Portugal-Nunes C, Reis J, Coelho A, Moreira PS, Castanho TC, Magalhães R, et al. The association of metabolic dysfunction and mood across lifespan interacts with the default mode network functional connectivity. Front Aging Neurosci. (2021) 13:618623. doi: 10.3389/fnagi.2021.618623
29. Burns RJ, Deschenes SS, and Schmitz N. Cyclical relationship between depressive symptoms and diabetes distress in people with Type 2 diabetes mellitus: results from the Montreal Evaluation of Diabetes Treatment Cohort Study. Diabetes Med. (2015) 32:1272–8. doi: 10.1111/dme.12860
30. Roy T and Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. (2012) 142 Suppl:S8–21. doi: 10.1016/S0165-0327(12)70004-6
31. Sarokhani D, Parvareh M, Hasanpour Dehkordi A, Sayehmiri K, and Moghimbeigi A. Prevalence of depression among Iranian elderly: systematic review and meta-analysis. Iran J Psychiatry. (2018) 13:55–64.
32. Kurspahic MA and Mujcic A. The relationship between education and self-reported mental and physical health. Med Glas (Zenica). (2019) 16:102–7. doi: 10.17392/969-19
33. Armstrong N, Fu Z, and Woolf K. The relationship between lifestyle behaviors and mental illness in women in college. Nutrients. (2024) 16(14):2211. doi: 10.3390/nu16142211
34. Kim Y, Kim J, Oh JW, and Lee S. Association between drinking behaviors, sleep duration, and depressive symptoms. Sci Rep. (2024) 14:5992. doi: 10.1038/s41598-024-56625-x
Keywords: sleep duration, ENP(new-onset emotional, nervous, or psychiatric problems), CHARLS, mediating effect, prospective cohort study
Citation: Wu H, Wang S, Zhao B and Ni H (2025) A U-shaped relationship between nighttime sleep duration and new-onset emotional, nervous, or psychiatric problems: a prospective cohort study from China. Front. Psychiatry 16:1609865. doi: 10.3389/fpsyt.2025.1609865
Received: 11 April 2025; Accepted: 08 July 2025;
Published: 28 July 2025.
Edited by:
Jason H. Huang, Baylor Scott and White Health, United StatesReviewed by:
Arcady A. Putilov, Institute of Higher Nervous Activity and Neurophysiology (RAS), RussiaHui Liew, University of Nebraska at Kearney, United States
Copyright © 2025 Wu, Wang, Zhao and Ni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haosheng Ni, ZW50bmhzQG50dS5lZHUuY24=
†These authors have contributed equally to this work
 Hao Wu
Hao Wu Shuzheng Wang1†
Shuzheng Wang1† Haosheng Ni
Haosheng Ni