Abstract
Introduction:
Depression ranks as the second leading cause of the global health burden; therefore, identification of its risk and influencing factors is essential to develop more effective multidimensional interventions. The aim of the present study was to analyze the mediating role of family adaptability (FA) on the relationship between insecure attachment (IA) and family functioning (FF) in patients with major depressive disorder (MDD), which currently remains unclear. It also aims to provide a theoretical reference for optimizing rehabilitation interventions.
Methods:
This cross-sectional study enrolled 62 patients with MDD who were admitted to a tertiary hospital in Beijing from March 2024 to December 2024. Participants completed the General Information Questionnaire, Family Assessment Device, Family Adaptability and Cohesion Evaluation Scale, and the Experiences in Close Relationships Relationship Structures Scale. The 17-item Hamilton Depression Rating Scale was also administered. Subsequently, association analysis was performed.
Results:
Notable correlations were observed among IA, FA, and FF in adults with MDD. Regression analysis established both IA and FA as reliable predictors of FF. Bootstrap-mediated analysis revealed that FA partially mediated the relationship between IA and FF, accounting for 35.47% of the total association. Further analysis demonstrated differential mediation proportions; FA mediated 39.36% of the association between anxious IA and FF and 42.61% of the association between avoidant IA and FF, with all mediation pathways meeting conventional thresholds for statistical significance.
Conclusions:
IA in adult patients with MDD negatively impacts FF, with both anxious and avoidant IA subtypes showing independent negative associations partially linked by FA. Rehabilitation strategies should prioritize multidimensional interventions targeting the enhancement of FA to improve FF and facilitate clinical recovery.
1 Introduction
Major depressive disorder (MDD) was ranked as the world’s second leading level-4 cause of disability (by years lived with disability) in the 2021 Global Burden of Disease study (1). Effective first-line treatments for MDD include pharmacotherapy and psychotherapy (2, 3). Commonly used clinical psychotherapies include cognitive behavioral therapy, dialectical behavior therapy, emotion-focused therapy, and various other approaches (4). Most psychotherapies are not tailored to an individual’s living environment even though empirical evidence suggests a correlation between the characteristics of one’s living environment and the onset and persistence of depression (5). Family functioning (FF) can predict clinical outcomes in patients with MDD (6, 7). Therefore, investigating the factors and mechanisms influencing FF in adult patients with MDD has meaningful theoretical and practical relevance.
Previous studies have demonstrated a negative correlation between depression and FF (8–10). Based on McMaster’s model, FF refers to the ability of family members to fulfill their roles, appropriately engage in and respond to emotional stimuli within the family, maintain mutual cohesion, address and resolve family issues, and communicate effectively with one another (11). FF is strongly associated with depression (12–14) and quality of family attachment (15). From the perspectives of attachment and family system theories, FF appears to be related to a secure base of attachment among family members (16).
According to Bowlby’s attachment theory (17), an individual’s attachment style develops from early childhood experiences with caregivers (18). Prototype working models formed during infancy unconsciously influence expectations, fears, defenses, and behaviors, creating interpersonal experiences that persist as stable core elements throughout life and shape attachment patterns (19). Ainsworth and Bell categorized attachment into three primary types: secure, anxious, and avoidant, with the latter two classified as insecure attachment (IA) (20). Children with insufficient caregiver responsiveness tend to develop maladaptive strategies to maintain proximity to attachment figures or for self-protection, resulting in the hyperactivation (attachment anxiety) or deactivation (attachment avoidance) of the attachment system (21). Previous studies have confirmed a negative correlation between IA and FF (22), although current research has primarily focused on child and adolescent populations with limited attention to adult groups. Several meta-analyses have demonstrated associations between IA and the development, severity, chronicity, and functional impairment of MDD (23, 24). However, the specific pathways linking IA to FF and depression recovery in adults remain unclear. Therefore, the first hypothesis proposed was:
Hypothesis 1: IA is negatively associated with FF in adult patients with MDD.
According to the Circumplex Model theory, family adaptability (FA) is the ability of a family system to alter its power structure, role relationships, and relational rules in response to new situations and developmental demands (25). FA, a central characteristic of family systems, has been established to show measurable associations with depression (26), FF (27), and IA (28), with consistent evidence demonstrating predictable relationships among FA, cohesion evaluation scale outcomes, and FF (29). Clarifying the operational pathways through which IA affects FF in adult patients with depression and determining whether FA contributes to these mechanisms represents a clinically meaningful area of investigation that has received insufficient research attention. Accordingly, the second hypothesis proposed was:
Hypothesis 2: FA is associated with the IA–FF relationship, where IA correlates with lower FA, which in turn corresponds with poorer FF.
In summary, this study hypothesized that FF is associated with IA, and that this relationship involves FA. Consequently, we propose a mediation model (Figure 1) to examine the impact of IA on FF and verify the mediating role of FA, thereby providing evidence-based guidance for enhancing FF and facilitating recovery in patients with MDD.
Figure 1
Hypothesized mediation model of family adaptability.
2 Materials and Methods
2.1 Participants
From March to December 2024, inpatients at a tertiary psychiatric hospital in Beijing, China were selected as study participants. The inclusion criteria were as follows: (i) age between 18 and 60 years, (ii) diagnosis of MDD according to the International Classification of Diseases 10th Revision Classification of Mental and Behavioral Disorders (30), (iii) voluntary participation in the study, and (iv) ability to comprehend and independently complete the questionnaires. The exclusion criteria were as follows: (i) organic mental disorders, mental disorders due to psychoactive substances, bipolar affective disorder, and depressive disorder with psychotic symptoms; (ii) non-completion of the questionnaire; and (iii) substantial missing data. All the participants provided informed consent. This study was approved by the ethics committee of our hospital, (Approval No: (2023) Scientific Research No. 322). And this study was registered with the Chinese Clinical Trial Registry (registration number: ChiCTR2500101417; website: https://www.chictr.org.cn). The current manuscript introduces a sub study of this registered research project.
2.2 Measurements
2.2.1 17-item Hamilton Depression Rating Scale
The HAMD-17 (31) is the most widely used clinical instrument for assessing depression severity. It comprises 17 items, including feelings of guilt, suicide, difficulty falling asleep, and insight. Each item is scored on a 0–2 or 0–4 scale, with the total score ranging from 0 to 54. Higher scores indicate greater depressive severity. The scoring criteria were as follows: 0–7 indicates no depression or remission period, 8–17 indicates mild depression, 18–24 indicates moderate depression, and ≥25 indicates severe depression. In this study, the scale demonstrated good reliability with a Cronbach’s α coefficient of 0.74. Owing to its dependable diagnostic accuracy and proven validity, the HAMD-17 has become widely recognized and utilized in clinical settings, as well as in research.
2.2.2 Family Adaptability and Cohesion Scale, second edition
The FACES II (Chinese version) (32) is a self-administered measure that evaluates the cohesion and adaptability of families. It consists of 30 items, with each scored on a 5-point response option that ranges from 1 (“not at all”) to 5 (“always”). It includes two subscales: family cohesion (16 items) and FA (14 items). According to Olson’s theory, a higher score indicates a better FA. In this study, the scale demonstrated good reliability, with a Cronbach’s α of 0.80.
2.2.3 Experiences in Close Relationships-Relationship Structures Scale
The ECR-RS (33) consists of nine items and is concise in content, comprising two dimensions—attachment avoidance (items 1–6) and attachment anxiety (items 7–9)—which align with the theoretical framework of attachment. The ECR-RS items apply to three life stages—infancy, childhood/adolescence, and adulthood–and accommodate various attachment figures. A 7-point scale from 1 (strongly disagree) to 7 (strongly agree) was used, with the first four entries reverse-scored. Higher scores indicate greater levels of attachment anxiety and avoidance. In this study, the scale demonstrated good reliability with a Cronbach’s α coefficient of 0.77.
2.2.4 Family Assessment Device
The FAD (34, 35) is used to collect data on various aspects of the entire family system and can effectively identify potential problems within it. The scale consists of seven subscales: communication, roles, problem solving, affective responsiveness, affective involvement, behavioral control, and general functioning, totaling 30 items. Each item contains 4 response options (1=“Very much like my family” to 4=“Not at all like my family”). For health-positive items (Items 9–13 and 20-25), we applied reverse scoring (5 minus the actual score). All items were ultimately standardized such that 1=unhealthy and 4=healthy. Higher scores indicate a healthier FF. In this study, the scale demonstrated good reliability, with a Cronbach’s α of 0.79.
2.3 Data collection
Adult patients with MDD provided detailed information regarding their age, sex, marital status, family members, disease diagnosis, and depression severity. Data were collected using online questionnaires completed via mobile scanning. Researchers addressed related inquiries, and clinical information was retrieved from the patients’ medical records.
2.4 Statistical analysis
To address concerns regarding statistical power, we conducted a Monte Carlo power analysis for mediation using the online tool developed by Schoemann et al. (36) (https://schoemanna.shinyapps.io/mc_power_med/). We conducted 5,000 replications with a fixed sample size of 62. Based on the observed correlations among the independent variable, mediator, and dependent variable, and using a significance level of α = 0.05, the estimated power for detecting the indirect effect ranged from 0.89 to 0.99.
This study employed SPSS 23.0 statistical software to perform confirmatory factor analysis, descriptive statistics, independent samples t-tests, common method bias testing, correlation analysis, and regression analysis on normally distributed data. To assess the significance of mediation pathways, we conducted mediation model analysis using the SPSS PROCESS macro and applied the bias-corrected nonparametric percentile Bootstrap method for validation. Associations were considered statistically significant when the Bootstrap confidence intervals excluded zero.
Model 4 was used to test the mediating role of family adaptability (FA) between insecure attachment (IA) and family functioning (FF), while controlling for covariates including gender, age, education level, marital status, family composition, clinical diagnosis, and depression severity. Prior to formal analysis, we evaluated the assumptions of the linear regression model.
To further investigate the independent mediating associations of FA between anxious IA and FF, as well as between avoidant IA and FF, we re-validated the linear regression model assumptions before conducting additional analyses, followed by separate analyses using Model 4 for each relationship. To enhance the robustness of our findings, we implemented Bootstrap resampling (5,000 repetitions) to estimate coefficient distributions, assess bias and standard errors, and validate the mediation models.
3 Results
3.1 Demographics
We enrolled 62 patients with MDD (31 females and 31 males), with a mean age of 45 years. Half of the participants were married (50.0%) and almost half were mildly depressed (41.94%) (Table 1).
Table 1
| Variables | N | % |
|---|---|---|
| Sex | ||
| Male | 31 | 50.0% |
| Female | 31 | 50.0% |
| Age | ||
| 18–39 years | 34 | 54.8% |
| 40–60 years | 28 | 45.2% |
| Marital status | ||
| Single | 25 | 40.3% |
| Married | 31 | 50.0% |
| Divorced | 6 | 9.7% |
| Family members | ||
| Spouse | 26 | 41.9% |
| Parents | 31 | 50.0% |
| Children | 3 | 4.8% |
| Others | 2 | 3.2% |
| Diagnosis | ||
| Depressive episodes | 24 | 38.7% |
| Recurrent depressive disorder | 38 | 61.3% |
| Severity of disease | ||
| Remission period | 19 | 30.65% |
| Mild | 26 | 41.94% |
| Moderate | 13 | 20.96% |
| Severe | 4 | 6.45% |
Demographic, sociodemographic, and clinical characteristics of patients with major depressive disorders (N = 62).
3.2 Common method bias
To address the potential common method bias, we conducted an unrotated principal component factor analysis on all scale items and performed a Harman’s single-factor test. The results revealed 21 factors with eigenvalues greater than 1, with the first factor accounting for 27.57% of the variance. This proportion was below the critical threshold of 40%, indicating the absence of significant common method bias in the study data.
3.3 Correlations between variables
Our analysis revealed statistically robust associations among IA, FA, and FF. The findings showed inverse relationships between IA and both FA (r = -0.512, p < 0.001) and FF (r = -0.593, p < 0.001). In contrast, a strong positive relationship was observed between the FA and FF (r = 0.659, p < 0.001) (Table 2).
Table 2
| Variables | M | SD | 1 | 2 | 3 |
|---|---|---|---|---|---|
| 1. Insecure Attachment | 30.08 | 12.35 | 1 | ||
| 2. Family Adaptability | 45.00 | 11.87 | -0.512*** | 2 | |
| 3. Family Functioning | 83.32 | 16.11 | -0.593*** | 0.659*** | 3 |
Correlation between insecure attachment, family adaptability, and family functioning.
*p < 0.05, **p < 0.01, ***p < 0.001.
After categorizing the IA subtypes, Pearson analyses were performed to examine the association between attachment and FF. Anxious IA was inversely correlated to FA (r = -0.378, p < 0.01) and FF (r = -0.458, p < 0.001), whereas avoidant IA showed a comparable negative correlation with FA (r = -0.470, p < 0.001) and FF (r = -0.458, p < 0.001). FA and FF remained positively correlated (r = 0.659, p < 0.001) (Table 3).
Table 3
| Variables | M | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. Anxious Insecure Attachment | 16.34 | 7.27 | 1 | |||
| 2. Avoidant Insecure Attachment | 13.74 | 7.63 | 0.375** | 2 | ||
| 3. Family Adaptability | 45.00 | 11.87 | -0.378** | -0.470*** | 3 | |
| 4. Family Functioning | 83.32 | 16.11 | -0.458*** | -0.524*** | 0.659*** | 4 |
Correlation between anxious insecure attachment, avoidant insecure attachment, family adaptability, and family functioning.
*p < 0.05, **p < 0.01, ***p < 0.001.
Model 4 examined the mediating associations of FA on IA and FF. The analysis was controlled for sex, age, marital status, family members, disease diagnosis, and severity of depression. Prior to analysis, we evaluated the assumptions of the linear regression. To further investigate whether FA accounts for the associations between anxious/avoidant IA and FF, we revalidated the assumptions of the linear regression model before conducting additional mediation analyses. The results indicated that IA was inversely associated with FA and negatively correlated with FF, while FA showed a positive association with FF (Table 4). Specifically, anxious and avoidant IA reduced FA and directly worsened FF, whereas FA consistently enhanced it (Table 4).
Table 4
| Outcome variable | Predictor variable | Coefficient significance | Fit indices | ||||
|---|---|---|---|---|---|---|---|
| β | t | p | R | R2 | F | ||
| Family Functioning |
Family adaptability | 0.591 | 3.326 | 0.002** | 0.761 | 0.580 | 7.962 |
| IA | -0.433 | -2.848 | 0.006** | ||||
| Sex | -0.051 | -0.015 | 0.988 | ||||
| Age | -6.046 | -1.570 | 0.122 | ||||
| Marital status | 5.491 | 1.961 | 0.055 | ||||
| Family members | -0.450 | -0.194 | 0.847 | ||||
| Diagnosis | 2.204 | 0.623 | 0.536 | ||||
| Severity of disease | -0.206 | -0.989 | 0.327 | ||||
| Family Functioning |
Family adaptability | 0.689 | 3.982 | < 0.001*** | 0.746 | 0.556 | 7.244 |
| Anxiety IA | -0.549 | -2.230 | 0.030* | ||||
| Sex | -0.128 | -0.037 | 0.970 | ||||
| Age | -7.630 | -1.919 | 0.060 | ||||
| Marital status | 5.840 | 2.031 | 0.047 | ||||
| Family members | -0.615 | -0.258 | 0.798 | ||||
| Diagnosis | 3.402 | 0.899 | 0.373 | ||||
| Severity of disease | -0.271 | -1.290 | 0.203 | ||||
| Family Functioning |
Family adaptability | 0.681 | 3.847 | < 0.001*** | 0.743 | 0.551 | 7.101 |
| Avoidant IA | -0.505 | -2.085 | 0.042* | ||||
| Sex | 0.650 | 0.191 | 0.849 | ||||
| Age | -5.017 | -1.240 | 0.220 | ||||
| Marital status | 5.319 | 1.836 | 0.072 | ||||
| Family members | -0.095 | -0.039 | 0.969 | ||||
| Diagnosis | -0.009 | -0.002 | 0.998 | ||||
| Severity of disease | -0.283 | -1.343 | 0.185 | ||||
Multiple linear regression to identify predictors of family functioning.
*p < 0.05; **p < 0.01; ***p < 0.001. IA, insecure attachment.
3.4 Mediation association analysis
Model 4 examined the mediating role of FA on IA and FF. To enhance the robustness of our findings, the bootstrap function of the boot package was applied with 5,000 resamples to estimate the coefficient distributions, assess bias and standard errors, and evaluate the mediation model. Version 4.1 of the PROCESS macro in SPSS was used for mediation analysis, with associations considered statistically significant if bootstrap confidence intervals excluded zero. To assess whether FA differentially accounts for the associations between attachment subtypes and FF, separate analyses were conducted for anxious and avoidant IA using Model 4. These results indicated that FA mediated the association between IA and FF. IA showed significant associations with FF through both direct and indirect pathways involving FA, with mediation accounting for 35.47% of the total observed association. Furthermore, FA partially mediated the relationship between the anxious and avoidant IA subtypes and FF. For both attachment patterns, the total, direct, and indirect association on FF reached the conventional thresholds for interpretation, with mediation proportions of 39.40% for anxious IA, and 42.61% for avoidant IA (Figure 2, Table 5).
Figure 2
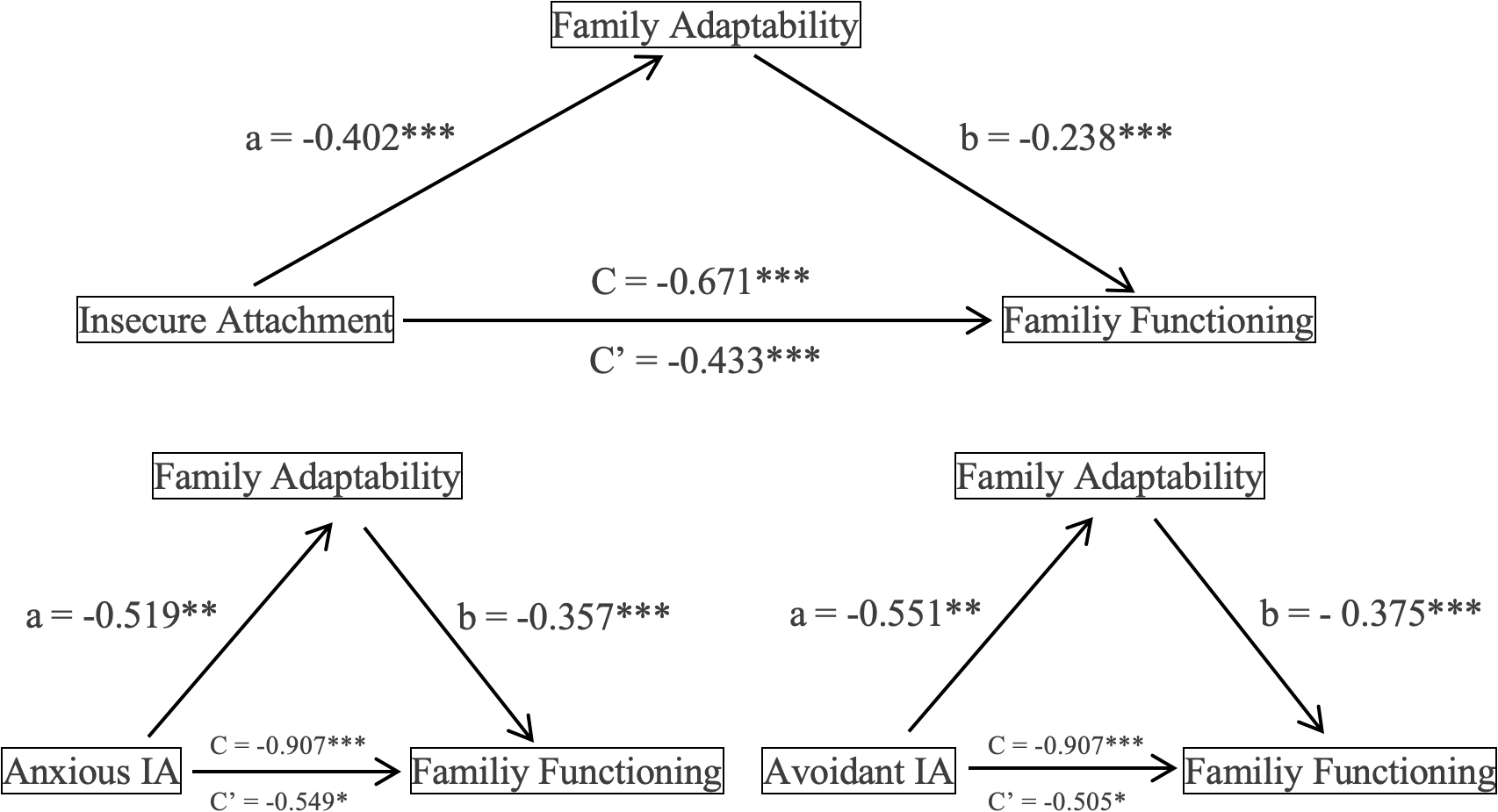
Intermediary role of family adaptability. Nonstandardized coefficients are reported. N = 62. *p < 0.05, **p < 0.01, ***p < 0.001. C indicates total effect; C’ indicates direct effect. IA, Insecure Attachment. Arrows only represent statistical associations,not causal direction.
Table 5
| Model | Effect | Boot SE | Bootstrap 95%CI | Ratio of indirect to total effect | ||
|---|---|---|---|---|---|---|
| Boot LLCI | Boot ULCI | |||||
| IA-FA-FF | Total effect | -0.671 | 0.146 | -0.964 | -0.377 | |
| Direct effect | -0.433 | 0.152 | -0.738 | -0.128 | ||
| Indirect effect | -0.238 | 0.104 | -0.463 | -0.060 | 35.47% | |
| Anxious IA-FA-FF |
Total effect | -0.906 | 0.259 | -1.427 | -0.386 | |
| Direct effect | -0.549 | 0.246 | -1.043 | -0.055 | ||
| Indirect effect | -0.357 | 0.158 | -0.690 | -0.065 | 39.40% | |
| Avoidant IA-FA-FF |
Total effect | -0.880 | 0.249 | -1.380 | -0.381 | |
| Direct effect | -0.505 | 0.242 | -0.991 | -0.019 | ||
| Indirect effect | -0.375 | 0.161 | -0.728 | -0.097 | 42.61% | |
The intermediary role of family adaptability in the insecure attachment-family functioning association.
*p < 0.05, **p < 0.01, ***p < 0.001. IA, insecure attachment; FA, family adaptability; FF, family functioning; LLCI, lower limit confidence interval; SE, standard error; ULCI, upper limit confidence interval.
4 Discussion
4.1 Predictive role of IA on FF in adult patients with MDD
This study confirmed that IA negatively predicts FF in adult patients with MDD, which is consistent with previous research on attachment patterns and FF (22, 37). Higher IA levels are associated with greater communication barriers, more rigid family interactions, and poorer FF.
First, individuals with anxious IA tend to engage in excessive rumination during family communication and emotional engagement, persistently seek reassurance about their worth and partner availability (38), and frequently exhibit jealousy and emotional instability in close relationships (39). Their heightened vigilance and overreactions to perceived threats impair their capacity to adaptively fulfill family roles when facing new situational demands (40). Consequently, their problem-solving abilities deteriorate, which ultimately compromises FF. In contrast, individuals with avoidant IA tend to avoid attachment-related thoughts and feelings predominantly by employing deactivating emotion regulation strategies (41, 42). When facing family conflicts or problems, they more frequently choose silence or withdrawal rather than active problem solving to avoid confrontation (43). This avoidance behavior leads to failure to fulfill family responsibilities, ultimately resulting in impaired FF.
We discovered that IA negatively predicted FF, whereas FF showed an inverse relationship with MDD. Dysfunctional family environments hinder recovery from depression (44, 45), indicating that IA is not only related to depression onset, progression, and severity (45–48), but also complicates treatment outcomes. These findings suggest that future research should develop individualized family interventions tailored to different attachment patterns to reduce IA, improve FF, and facilitate long-term recovery. These results underscore the importance of interdisciplinary collaboration, particularly between psychiatry and psychology, in establishing comprehensive long-term management strategies for adult patients with chronic depressive disorder.
4.2 FA’s intermediary role in the IA-FF association in adult patients with MDD
This study identified FA as a critical mediator between IA and FF in adult patients with MDD, establishing a sequential pathway from IA to impaired FA, and ultimately to poorer FF. Specifically, higher levels of IA were associated with reduced FA levels, which in turn led to poorer FF. FA’s intermediary role showed a substantial association with this complex process. These findings align with those of previous studies on child and adolescent populations (28, 49), further confirming the universal negative impact of IA on both FA and FF across different age groups and clinical/non-clinical populations.
Notably, the results further revealed differential mediation patterns. FA mediated the relationship between FF and both anxious and avoidant IA, but with distinct effect magnitudes, demonstrating attachment-specific mediation mechanisms. These findings offer a refined perspective on the relationship between IA and FF in adults with MDD.
Individuals with anxious and avoidant IA demonstrate substantial differences in emotional interactions, communication patterns, and problem-solving capacities within their family systems. Research indicates that when distressed, anxiously attached individuals often amplify their suffering (attachment hyperactivation) to elicit caregiver attention, predominantly employing over-activating emotion regulation strategies characterized by catastrophizing and rumination (50). This pattern reduces FF, promotes maladaptive coping, undermines consistent emotional support and security, and ultimately impairs FF. Individuals with avoidant attachment typically distrust others’ responsiveness, maintain emotional distance from attachment figures, and reject intimacy to prevent disappointment. Their characteristic pain suppression (attachment deactivation) and predominant use of deactivating emotion regulation strategies hinder meaningful emotional exchanges with family members (51, 52). This impairment in FA manifests as difficulty in open discussions during new family challenges and the inability to adjust relational rules or role allocations, ultimately degrading FF.
Attachment patterns are established during early childhood (53) and demonstrate considerable stability in adulthood, typically requiring prolonged systematic intervention for modification (18, 19) and presenting substantial treatment challenges for depression. This study revealed the mediating role of FA in the relationship between IA and FF in adult patients with depression, identifying FA as a crucial factor in the observed relationship between IA and FF. These findings suggest that therapeutic interventions targeting FA, particularly those that improve communication patterns, enhance emotional expression, and strengthen problem-solving skills within family systems, may effectively mitigate the negative association between IA and FF. Such approaches could optimize the living environment of patients with depression and create more favorable conditions for clinical recovery.
4.3 Study limitations and future directions
This study investigated the impact of IA on FF and its underlying mechanisms in patients with MDD to provide a reference for the development of rehabilitation plans. However, the study design incorporated the following limitations. First, this study explored the mediating role of family adaptability between insecure attachment and family functioning in patients with depressive disorder. Although the sample size was relatively small, future studies with larger samples are warranted to validate these findings. Second, this study employed a cross-sectional design that only permitted path analysis among variables without establishing causal inferences. Future longitudinal studies with expanded sample sizes could stratify depression severity and reassess patients after family therapy interventions. Subsequent evaluations of changes in attachment styles, family adaptability, and family functioning would yield additional data for analysis. Such approaches may elucidate more pathways and mechanisms between insecure attachment and family functioning, thereby providing theoretical references for depression rehabilitation.
5 Conclusion
In summary, this study elucidated the impact of IA on FF and its underlying mechanisms in patients with MDD. This supports the direct negative association between IA and FF, and identifies the mediating role of FA between IA and FF. Further analysis identified distinct intermediary pathways and association patterns. That is, FA differentially mediated the relationship between anxious IA and FF versus avoidant IA and FF. Consequently, when developing rehabilitation plans for depressive disorders, clinicians should focus on improving the family environment through the active implementation of family therapy. Particular attention should be paid to tailoring treatment strategies according to attachment characteristics, enhancing FA, and improving FF to facilitate patient recovery.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Beijing Anding Hospital Affiliated to Capital Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XC: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. XL: Data curation, Methodology, Supervision, Writing – review & editing. JZ: Investigation, Project administration, Writing – review & editing. LW: Investigation, Project administration, Writing – review & editing. XS: Funding acquisition, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We acknowledge everyone who contributed towards the article who does not meet the criteria for authorship. We thank Editage for ensuring language and grammar accuracy and for checking the logical presentation of ideas and the structure of the paper. The authors core research ideas were not altered in any way during the editing process.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Ferrari AJ Santomauro DF Aali A Abate YH Abbafati C Abbastabar H et al . Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:2133–61. doi: 10.1016/S0140-6736(24)00757-8
2
Santomauro DF Vos T Whiteford HA Chisholm D Saxena S Ferrari AJ . Service coverage for major depressive disorder: estimated rates of minimally adequate treatment for 204 countries and territories in 2021. Lancet Psychiatry. (2024) 11:1012–21. doi: 10.1016/S2215-0366(24)00317-1
3
Campbell LF Norcross JC Vasquez MJT Kaslow NJ . Recognition of psychotherapy effectiveness: the APA resolution. Psychotherapy. (2013) 50:98–101. doi: 10.1037/a0031817
4
Cuijpers P Noma H Karyotaki E Vinkers CH Cipriani A Furukawa TA . A network meta-analysis of the effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression. World Psychiatry. (2020) 19:92–107. doi: 10.1002/wps.20701
5
Rautio N Filatova S Lehtiniemi H Miettunen J . Living environment and its relationship to depressive mood: a systematic review. Int J Soc Psychiatry. (2018) 64:92–103. doi: 10.1177/0020764017744582
6
Bian Y Jin K Zhang Y . The association between family cohesion and depression: a systematic review and meta-analysis. J Affect Disord. (2024) 355:220–30. doi: 10.1016/j.jad.2024.03.138
7
Barzoki MH Toikko T . Family intimacy and depression: a comparative study among adolescents in Finland. Nord J Psychiatry. (2025) 79:70–8. doi: 10.1080/08039488.2024.2436986
8
Keitner GI Ryan CE Miller IW Kohn R Bishop DS Epstein NB . Role of the family in recovery and major depression. Am J Psychiatry. (1995) 152:1002–8. doi: 10.1176/ajp.152.7.1002
9
Goodyer IM Herbert J Tamplin A Secher SM Pearson J . Short-term outcome of major depression: II. Life events, family dysfunction, and friendship difficulties as predictors of persistent disorder. J Am Acad Child Adolesc Psychiatry. (1997) 36:474–80. doi: 10.1097/00004583-199704000-00009
10
Weinstock LM Keitner GI Ryan CE Solomon DA Miller IW . Family functioning and mood disorders: A comparison between patients with major depressive disorder and bipolar I disorder. J Consult Clin Psychol. (2006) 74:1192–202. doi: 10.1037/0022-006X.74.6.1192
11
Miller IW Kabacoff RI Epstein NB Bishop DS Keitner GI Baldwin LM et al . The development of a clinical rating scale the McMaster model of family functioning. Fam Process. (1994) 33:53–69. doi: 10.1111/j.1545-5300.1994.00053.x
12
Huang X Hu N Yao Z Peng B . Family functioning and adolescent depression: A moderated mediation model of self-esteem and peer relationships. Front Psychol. (2022) 13:962147. doi: 10.3389/fpsyg.2022.962147
13
Li M Li L Wu F Cao Y Zhang H Li X et al . Perceived family adaptability and cohesion and depressive symptoms: a comparison of adolescents and parents during COVID-19 pandemic. J Affect Disord. (2021) 287:255–60. doi: 10.1016/j.jad.2021.03.048
14
Zhang C Zhang Q Zhuang H Xu W . The reciprocal relationship between depression, social anxiety and aggression in Chinese adolescents: the moderating effects of family functioning. J Affect Disord. (2023) 329:379–84. doi: 10.1016/j.jad.2023.02.134
15
Thompson RA Simpson JA Berlin LJ . Taking perspective on attachment theory and research: nine fundamental questions. Attach Hum Dev. (2022) 24:543–60. doi: 10.1080/14616734.2022.2030132
16
Smrtnik Vitulić H Gosar D Prosen S . Attachment and family functioning across three generations. Fam Process. (2023) 62:775–94. doi: 10.1111/famp.12787
17
Bowlby J . Attachment and Loss: Vol. 3. Sadness and Depression. 2nd. New York: Basic Books (1980).
18
Waters E Hamilton CE Weinfield NS . The stability of attachment security from infancy to adolescence and early adulthood: general introduction. Child Dev. (2000) 71:678–83. doi: 10.1111/1467-8624.00175
19
Fraley RC Roisman GI . The development of adult attachment styles: four lessons. Curr Opin Psychol. (2019) 25:26–30. doi: 10.1016/j.copsyc.2018.02.008
20
Ainsworth MD Bell SM . Attachment, exploration, and separation: illustrated by the behaviour of one-year-olds in a strange situation. Child Dev. (1970) 41:49–67. doi: 10.2307/1127388
21
Nolte T Guiney J Fonagy P Mayes LC Luyten P . Interpersonal stress regulation and the development of anxiety disorders: an attachment-based developmental framework. Front Behav Neurosci. (2011) 5:55. doi: 10.3389/fnbeh.2011.00055
22
Brandão T Brites R Hipólito J Nunes O . Attachment orientations and family functioning: the mediating role of emotion regulation. J Psychol. (2022) 157:1–12. doi: 10.1080/00223980.2022.2128284
23
Fan AP Buka SL Kosik RO Chen Y-S Wang S-J Su T-P et al . Association between maternal behavior in infancy and adult mental health: a 30-year prospective study. Compr Psychiatry. (2014) 55:283–9. doi: 10.1016/j.comppsych.2013.08.024
24
Abdul Kadir NB Bifulco A . Insecure attachment style as a vulnerability factor for depression: recent findings in a community-based study of Malay single and married mothers. Psychiatry Res. (2013) 210:919–24. doi: 10.1016/j.psychres.2013.08.034
25
Olson DH . Circumplex model of marital and family systems. J Fam Ther. (2000) 22:144–67. doi: 10.1111/1467-6427.00144
26
Rahman A Sanchez M Bursac Z Whiting CY Piña-Watson B Taskin T et al . Depressive symptoms, family cohesion, and acculturation gap conflicts among Latinx emerging adults living in the United States. Fam Relat. (2023) 72:932–47. doi: 10.1111/fare.12722
27
Olson DHL . Family Inventories: Inventories Used in a National Survey of Families Across the Family Life Cycle. Rev. ed. St. Paul: Family Social Science, University of MinnesotaSt. Paul, Minn.: Family Social Science, University of Minnesota). (1985).
28
Alavi M Latif AA Ninggal MT Mustaffa MS Amini M . Family functioning and attachment among young adults in Western and non-Western societies. J Psychol. (2020) 154:346–66. doi: 10.1080/00223980.2020.1754153
29
Olson D . FACES IV and the Circumplex Model: validation study. J Marital Fam Ther. (2011) 37:64–80. doi: 10.1111/j.1752-0606.2009.00175.x
30
International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders . A conceptual framework for the revision of the ICD-10 classification of mental and behavioural disorders. World Psychiatry. (2011) 10:86–92. doi: 10.1002/j.2051-5545.2011.tb00022.x
31
Tang Y . Hamilton depression scale. Chin Ment Health J. (1999) Suppl):220–3.
32
Zhang S Lu X Du L Du J Wang W Guo A et al . Research on the development and application of family adaptability and cohesion evaluation scales as a family function evaluation tool. Chin Gen Pract. (2010) 13:725–8. doi: 10.3969/j.issn.1007-9572.2010.07.013
33
Peng X Luo C Wang Y Yin G . The Chinese version of the Experiences in Close Relationships-Relationship Structures Scale(ECR-RS) assesses the validity and reliability for middle school and college students. Chin Ment Health J. (2020) 34:957–63. doi: 10.3969/j.issn.1000-6729.2020.11.012
34
Li R Xu F Ji L . Preliminary revision of the family function assessment scale. J Health Psychol. (2013) 21:996–9. doi: CNKI:SUN:JKXL.0.2013-07-018
35
Liu L Zhao L . The effect of family functioning on anger: the mediating role of self-esteem. J Shanxi Univ (Philosophy Soc Science). (2018) 41:139–44. doi: CNKI:SUN:SXDD.0.2018-05-020
36
Schoemann AM Boulton AJ Short SD . Determining power and sample size for simple and complex mediation models. Soc psychol Pers Sci. (2017) 8:379–86. doi: 10.1177/1948550617715068
37
Mangialavori S Russo C Jimeno MV Ricarte JJ D’Urso G Barni D et al . Insecure attachment styles and unbalanced family functioning as risk factors of problematic smartphone use in Spanish young adults: a relative weight analysis. Eur J Investig Health Psychol Educ. (2021) 11:1011–21. doi: 10.3390/ejihpe11030075
38
Zhang M Wang J Li Q Li S Bao X Chen X . Temporal characteristics of emotional conflict processing: the modulation role of attachment styles. Int J Psychophysiol. (2023) 193:112243. doi: 10.1016/j.ijpsycho.2023.112243
39
Smith M South S . Romantic attachment style and borderline personality pathology: a meta-analysis. Clin Psychol Rev. (2020) 75:101781. doi: 10.1016/j.cpr.2019.101781
40
Huang Y-L Chen S-H Tseng H-H . Attachment avoidance and fearful prosodic emotion recognition predict depression maintenance. Psychiatry Res. (2019) 272:649–54. doi: 10.1016/j.psychres.2018.12.119
41
Woerner J Kopetz C Arriaga X . Intimate partner violence and sexual risk-taking: attachment avoidance as a linking mechanism. Behav Sci. (2025) 15:239. doi: 10.3390/bs15020239
42
Sood M Carnelley KB Newman-Taylor K . How does insecure attachment lead to paranoia? A systematic critical review of cognitive, affective, and behavioural mechanisms. Br J Clin Psychol. (2022) 61:781–815. doi: 10.1111/bjc.12361
43
Lutzman M Sommerfeld E . Mental pain as a mediator in the association between avoidant attachment and suicidal ideation among older men. Aging Ment Health. (2024) 28:1278–85. doi: 10.1080/13607863.2024.2323957
44
Chen P Harris KM . Association of positive family relationships with mental health trajectories from adolescence to midlife. JAMA Pediatr. (2019) 173:e193336. doi: 10.1001/jamapediatrics.2019.3336
45
Urbańska-Grosz J Sitek EJ Pakalska A Pietraszczyk-Kędziora B Skwarska K Walkiewicz M . Family functioning, maternal depression, and adolescent cognitive flexibility and its associations with adolescent depression: a cross-sectional study. Children. (2024) 11:131. doi: 10.3390/children11010131
46
Cicchetti D Doyle C . Child maltreatment, attachment and psychopathology: mediating relations. World Psychiatry. (2016) 15:89–90. doi: 10.1002/wps.20337
47
Brumariu LE Kerns KA . Parent–child attachment and internalizing symptoms in childhood and adolescence: a review of empirical findings and future directions. Dev Psychopathol. (2010) 22:177–203. doi: 10.1017/S0954579409990344
48
Brenning KM Soenens B Braet C Bosmans G . Attachment and depressive symptoms in middle childhood and early adolescence: testing the validity of the emotion regulation model of attachment. Pers Relatsh. (2012) 19:445–64. doi: 10.1111/j.1475-6811.2011.01372.x
49
Finklestein M Pagorek-Eshel S Laufer A . Adolescents’ individual resilience and its association with security threats, anxiety and family resilience. J Fam Stud. (2022) 28:1023–39. doi: 10.1080/13229400.2020.1778504
50
Benoit D . Infant-parent attachment: definition, types, antecedents, measurement and outcome. Paediatr Child Health. (2004) 9:541–5. doi: 10.1093/pch/9.8.541
51
Coyle P Van Doorn G Teese R Dye J . Adverse childhood experiences and infidelity: the mediating roles of anxious and avoidant attachment styles. Fam Process. (2025) 64:e13088. doi: 10.1111/famp.13088
52
Allen ES Baucom DH . Adult attachment and patterns of extradyadic involvement. Fam Process. (2004) 43:467–88. doi: 10.1111/j.1545-5300.2004.00035.x
53
Slade A Holmes J . Attachment and psychotherapy. Curr Opin Psychol. (2019) 25:152–6. doi: 10.1016/j.copsyc.2018.06.008
Summary
Keywords
major depressive disorders, insecure attachment, family functioning, family adaptability, mediating
Citation
Cheng X, Li X, Zhao J, Wang L and Shi X (2025) The mediating role of family adaptability in the relationship between insecure attachment and family functioning in patients with major depression disorder: a cross-sectional study. Front. Psychiatry 16:1611258. doi: 10.3389/fpsyt.2025.1611258
Received
14 April 2025
Accepted
30 July 2025
Published
20 August 2025
Volume
16 - 2025
Edited by
Maj Vinberg, University Hospital of Copenhagen, Denmark
Reviewed by
Xiao Wang, First Hospital of Shanxi Medical University, China
Andrei Gabriel Mangalagiu, Dr. Carol Davila Central Military Emergency University Hospital, Romania
Updates
Copyright
© 2025 Cheng, Li, Zhao, Wang and Shi.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinlei Cheng, shealia@aliyun.com; Xiaoning Shi, 13691412420@139.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.