- Division of Child and Adolescent Health, Shanghai Municipal Center for Disease Control and Prevention, Shanghai, China
Objective: To investigate the association between using screen in the dark—a predominant source of LAN—and depressive symptoms in Chinese adolescents.
Methods: This study utilized a sample of 3659 adolescents (51.87% boy, mean age 14.41 ± 1.55 years) from the 2020-2022 Surveillance of Students’ Common Diseases and Health Influencing Factors in Shanghai, China. Baseline screen usage was collected by self-reported questionnaire. Depressive symptoms at baseline, 1- and 2-year follow-up were assessed using the Center for Epidemiology Scale. Generalized estimating equations were used to evaluate the association of using screen in the dark with depressive symptoms.
Results: The prevalence of depressive symptoms and severe depressive symptoms in this study was 23.59% and 5.25% respectively at baseline. 15.76% adolescents who had depressive symptoms in 2020 aggravated to severe depressive symptoms in 2021 or 2022. 12.38% of the participants reported using screen in the dark. Using screen in the dark was associated with higher likelihood of depressive symptoms (OR = 1.89, 95%CI: 1.67, 2.15) and severe depressive symptoms (OR = 1.89, 95%CI: 1.54, 2.31). The adverse effect of using screen in the dark and screen time > 2 hours/day on depressive symptoms was slightly higher than only screen time > 2 hours/day (OR = 1.24, 95%CI: 1.12, 1.37) or only using screen in the dark (OR = 2.15, 95%CI: 1.73, 2.67). Additionally, those who using screen in the dark combination with screen time > 2 hours/day or insufficient sleep have the highest likelihood of depressive symptoms.
Conclusions: Screen use in dark environments independently related to depressive symptoms in adolescents, with compounded associations from excessive screen time and sleep deprivation. These findings underscore the need for public health interventions targeting nighttime digital behaviors.
1 Introduction
Adolescent depression is increasingly recognized as a significant public health concern. According to World Health Organization, depression is estimated to occur among 1.1% of adolescents aged 10–14 years old, and 2.8% of those 15–19 years old (1). Recent research demonstrates an increasing prevalence of depression among adolescents aged 10 to 14 years in various countries (2). Furthermore, depression is one of the leading causes of illness and disability among adolescents (1). Depression can significantly affect school attendance and academic performance, exacerbate feeling of isolation and loneliness, and may ultimately lead to suicide (3). Despite these serious implications, the etiology of depression remains insufficiently understood. Multiple factors are implicated in the development of depression, including stress, bullying, harsh parenting, socioeconomic problems, disruptions to daily rhythms (4–6).
Depression is frequently accompanied by sleep disorders and circadian misalignment (7, 8). Notably, exposure to light at night (LAN) is the strongest disruptor of circadian physiology and behavior (9, 10). Technological advancements have led adolescents to devote more time to self-luminous electronic devices, including computers, smartphones, tablets, and televisions, for both educational and recreational activities. Consequently, there has been a notable increase in both the frequency and duration of electronic device usage during pre-sleep hours. A survey involving 3,749 Chinese middle school students indicated that 63.2% of 7th-grade students engage in mobile phone use while in bed (11). Comparable patterns were identified in other Asian countries, where 81.1% of Korean adolescents (12) and 25.9% of Japanese adolescents (13) reported utilizing electronic devices post-lights out. In contrast to other sources of dim ambient light, self-luminous electronic screens often emit higher levels of short-wavelength (blue) light (14). This type of light exposure is more prone to disrupting circadian rhythms and may elevate the risk of mood disorders, such as depression (4, 15).
With the widespread use of screens, numerous studies have documented the association between screen time or content and depression (16–18). However, there is a paucity of research explicitly examining the role of high levels of light at night (LAN), particularly using screen in the dark, on depressive symptoms. Understanding this relationship could inform interventions and policy-making aimed at promoting healthier lifestyles among youth.
Building on the analysis of a previous study, this research employed a dataset spanning three years (2020–2022) from the Surveillance of Students’ Common Diseases and Health Influencing Factors in Shanghai, China. The primary objective was to assess the prevalence of depressive symptoms among adolescents and to explore its correlation with the use of screens in dark environments. Additionally, the study investigated whether screen time and insufficient sleep collectively exacerbate depressive symptoms.
2 Materials and methods
2.1 Research procedures and participants
The current study was conducted as a part of the Surveillance of Students’ Common Diseases and Health Influencing Factors (SSCDHIF) in Shanghai, China, during September to November from 2020 to 2022.
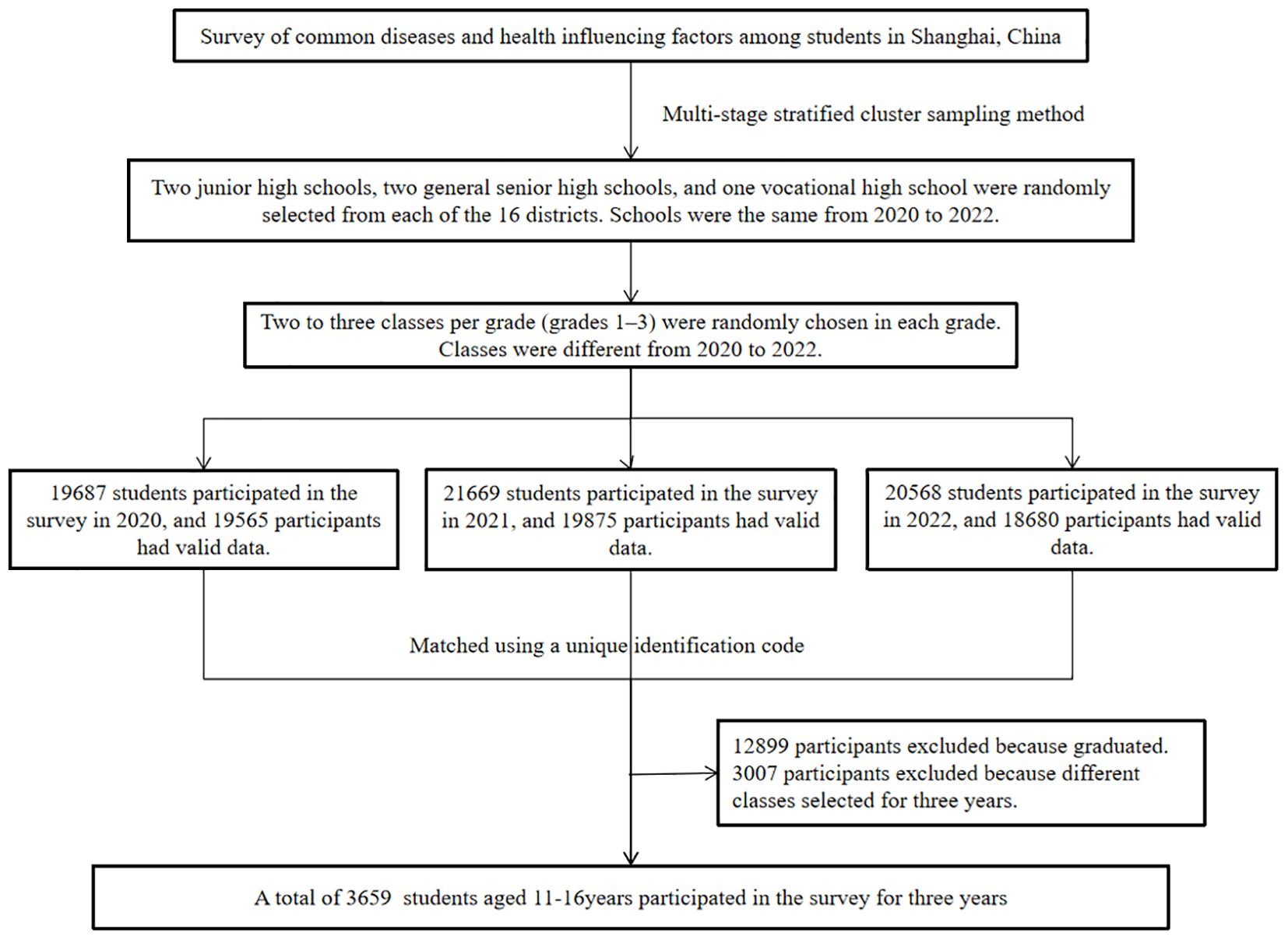
A multi-stage stratified cluster sampling method was employed to create a representative sample of middle school students in Shanghai. From each of the 16 districts, two junior high schools, two general senior high schools, and one vocational high school were randomly selected. Within each selected school, two to three classes per grade (grades 1–3) were randomly chosen, and all students in these classes completed an annual questionnaire survey. 19687 students participated in the survey in 2020, and 19565 participants had valid data. 21669 students participated in the survey in 2021, and 19875 participants had valid data. 20568 students participated in the survey in 2022, and 18680 participants had valid data. After matching with a unique identification code, a total of 3659 students who participated in the surveillance program for 3 consecutive years (2020–2022) were included in this study (Figure 1). These students progressed from first grade in 2020 to third grade in 2022. All participants and their parents/guardians have obtained informed consent before participation. The study protocol received ethical approval from the Shanghai Municipal Center for Disease Control and Prevention Ethics Committee (Approval No. 2022-13).
2.2 Measurement tools
2.2.1 Measurement of depression
Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression Scale (CES-D), a validated instrument for assessing depressive symptomatology in adolescent populations across diverse cultural contexts (19), including demonstrated reliability in Chinese cohorts (20). The CES-D contains 20 items with 4 response options: 1) not at all or rarely (< 1 day); 2) occasionally (1–2 days); 3) often or half of the days (3–4 days); and 4) most or all of the time (5–7 days). The values of the 4 options range from 0 to 3 successively. The total score ranges from 0 to 60, with higher scores indicating higher levels of depressive symptoms. A cut-off score ≥ 16 and ≥ 28 was used to identify the depressive symptoms and severe depressive symptoms respectively (21). The Cronbach’s alpha coefficient for this survey were 0.901, 0.887, 0.866.
2.2.2 Measurement of screen use in the dark
Using screen in the dark was measured as a binary variable. The original question asked respondents “Did you turn off the lights when using electronic screen after dark?” with the following response “never”, “occasionally”, “often”, “always”. Who responded “often”, “always” were recoded as 1, and who responded “never”, “occasionally” were recoded as 0.
2.2.3 Measurement of screen time
Participants were asked “How long did you use electronic screen per day in the last week?”. Screen time was categorized as a binary variable with the cutoff of 2 hours/day (1= “>2 hours/day”, 0= “≤2 hours/day”).
2.2.4 Measurement of sleep duration
Participants were asked “How much sleep did you get on an average day?”. According to the Health China 2030 Plan and the National Sleep Foundation’s updated sleep duration recommendations (22), adolescents who aged less than 14 years had less than 9 h of sleep on an average night; who aged 14–17 had less than 8 h of sleep; who aged over 18 had less than 7 h of sleep were considered as having an insufficient sleep, and were recoded as 1, the others had sufficient sleep were recoded as 0.
2.2.5 Covariates
In this study, the sociodemographic characteristics included district, age, gender (1 = boy, 2 = girl). District was categorized as urban areas (district of Huangpu, Xuhui, Jing’an, Changning, Putuo, Hongkou, and Yangpu) and suburbs (district of Pudong, Jinshan, Minhang, Fengxian, Songjiang, Qingpu, Jiading, Baoshan, and Chongming).
We controlled for other potential risk factors which were self-reported: one-child status (1 = yes, 0 = no), family economic status (1 = good, 2 = general, 3 = poor), drinking history (1 = yes, 0 = no), academic performance (1 = good, 2 = general, 3 = poor), school bullying (1 = yes, 0 = no).
School bullying was measured based on six questions, “During the past 30 days, have you ever been bullied in the following forms? (1) Being teased in a bad way; (2) Being robed; (3) Being intentionally excluded from group activity or isolated; (4) Being threatened; (5) Being physically beaten, kicked, attacked, or squeezed; (6) Being teased of physical defects or looks”. Every question followed three responses: never, occasionally, or often. Who chose “often” for any of the six questions were categorized as having school bullying.
2.3 Data analysis
All the analyses were performed using R Language (V4.4.1) and SPSS 29.0. A two-tailed p value of < 0.05 was considered statistically significant. Quantitative variables were analyzed as means (standard deviation) according to the normality of distribution, and qualitative variables were analyzed as numbers (percentages). The t-test and chi-squared test were used to compare difference between sub-groups. The analytic data included depressive symptoms, using screen in the dark and other variables in each assessed interval from 2020 to 2022, and was converted to long data before Generalized Estimating Equation (GEE) analysis. Associations between using screen in the dark, screen time, sleep duration and depressive symptoms were assessed using GEE for repeated measures analysis. Model 1 was crude model. Model 2 was adjusted for district, gender, age. Model 3 was further adjusted for one-child status, family economic status, drinking history, academic performance, school bullying. The joint effect between using screen in the dark and screen time or sleep duration was also assessed.
3 Results
3.1 Participant characteristics at baseline
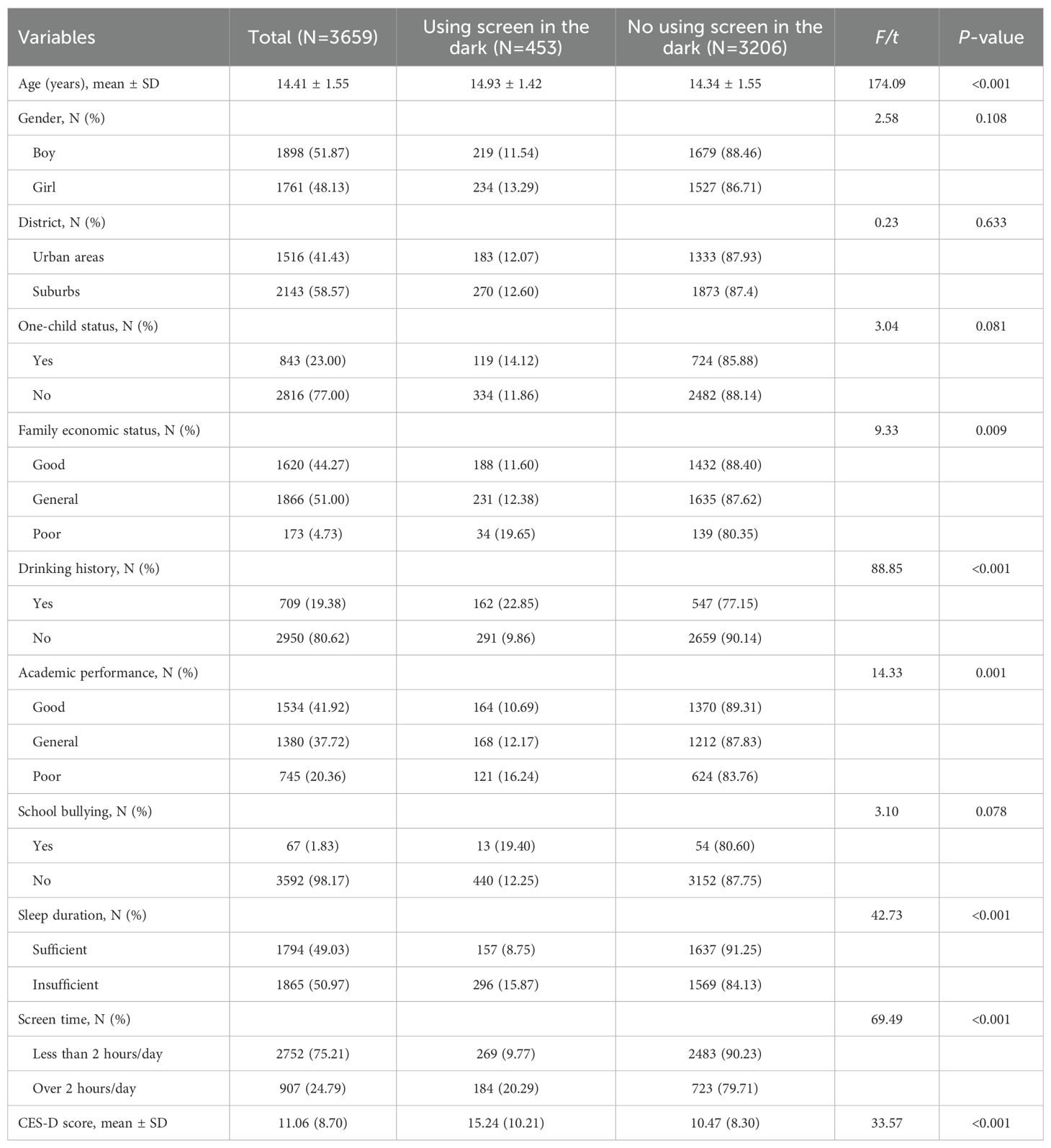
A total of 3659 participants were included in the analysis. Their age ranged from 11 to 19 years, and the mean age was 14.41(SD =1.55) years, 51.87% (1898) were boys and 48.13% (1761) were girls. The average score of CES-D was 11.06 (SD = 8.7). Adolescents who used screen in the dark exhibited higher CES-D scores compared to those who did not. A total of 453 participants (12.38%) reported using screens in the dark. They were more likely to have drinking history, poor family economic status, poor academic performance, insufficient sleep and screen time >2 hours/day. The demographic and behavior characteristics of adolescents at baseline are shown in Table 1.
3.2 Prevalence of depressive symptoms among adolescents from 2020 to 2022
Table 2 shows nearly a quarter of adolescents had depressive symptoms (CES-D score >16), and 5.25% had severe depressive symptoms (CES-D score >28) at baseline. The percentage of the participants had severe depressive symptoms increased to 5.90% in 2021 and 6.94% in 2022. The prevalence of persistent depressive symptoms and severe depressive symptoms were 7.46% and 0.74%. Furthermore, 15.76% adolescents who had depressive symptoms in 2020 aggravated to severe depressive symptoms in 2021 or 2022. Adolescents from urban areas were more likely to have depressive symptoms progression than those from suburbs. The incidence of (severe) depressive symptoms among senior high school students was higher than other students. Girls and adolescents who used screen in the dark, screen time >2 hours/day, and had insufficient sleep were more likely to have depressive symptoms in various outcomes.
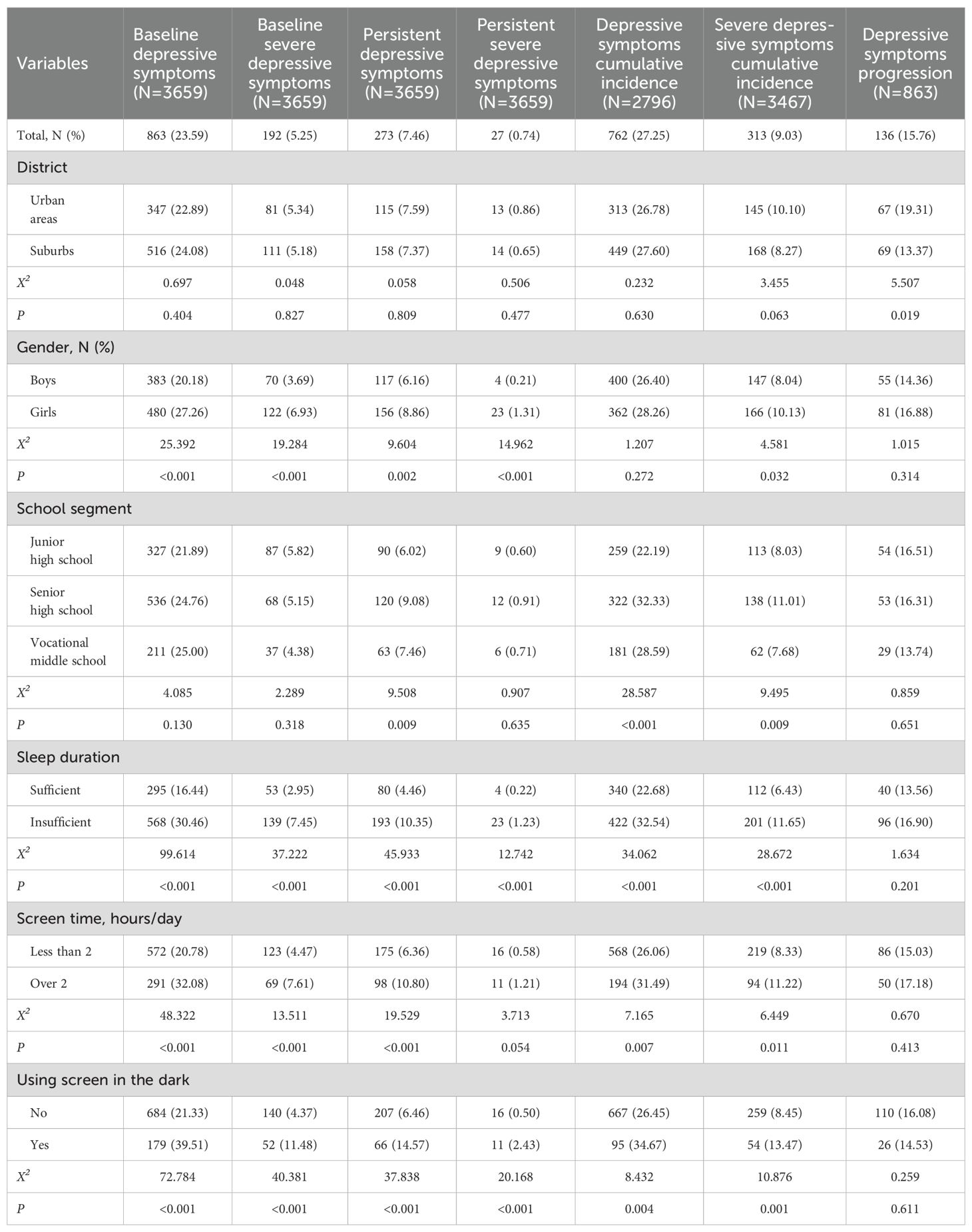
Table 2. The prevalence of depressive symptoms in adolescents in the follow-up survey from 2020 to 2022.
3.3 Associations between using screen in the dark, screen time, sleep duration and depressive symptoms
In the fully adjusted model, using screen in the dark was significantly associated with higher likelihood of depressive symptoms (OR = 1.89, 95%CI: 1.67, 2.15; P < 0.001) and severe depressive symptoms (OR = 1.89, 95%CI: 1.54, 2.31; P < 0.001) (Figure 2). Compared to screen time ≤ 2 hours/day group, screen time >2 hours/day group was associated with higher likelihood of depressive symptoms (OR = 1.28, 95%CI: 1.15, 1.42; P = 0.002) and severe depressive symptoms (OR = 1.24, 95%CI: 1.03, 1.49; P = 0.025). In addition, insufficient sleep group was associated with higher likelihood of depressive symptoms (OR = 1.56, 95%CI: 1.40, 1.72; P < 0.001) and severe depressive symptoms (OR = 1.84, 95%CI: 1.50, 2.27; P < 0.001) compared with adequate sleep group. Results from unadjusted and adjusted models were generally consistent (Figure 2).
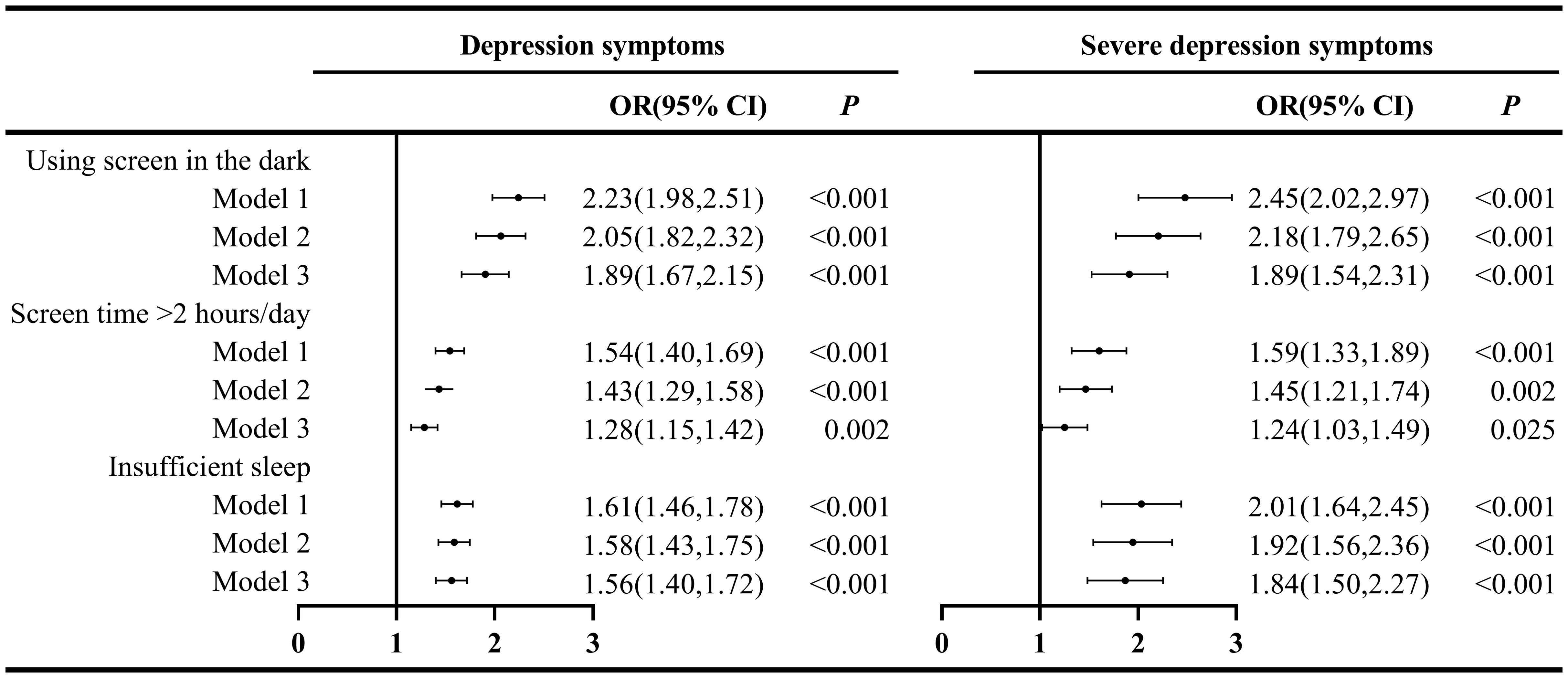
Figure 2. Association between using screen in the dark, screen time, sleep duration and depressive symptoms in adolescents from 2020 to 2022. Note: Model 1, crude model; Model 2, adjusted for district, gender, age; Model 3, Model 2 further adjusted for one-child status, family economic status, drinking history, academic performance, school bullying.
Table 3 illustrates the joint effect of using screen in the dark and screen time > 2 hours/day or insufficient sleep on depressive symptoms. We combined “using screen in the dark + insufficient sleep” and “using screen in the dark + screen time > 2 hours/day” into four groups respectively. Group 1 was the reference group, while Group 4 represented the joint effect. After adjusting for covariates, we found that OR of using screen in the dark and screen time >2 hours/day (OR = 2.22, 95%CI: 1.90, 2.60) on depressive symptoms was slightly higher than only screen time >2 hours/day (OR = 1.24, 95%CI: 1.12, 1.37) or only using screen in the dark (OR = 2.15, 95%CI: 1.73, 2.67). Furthermore, the OR for the combination of using screen in the dark and insufficient sleep (OR = 3.72, 95%CI: 2.79, 4.95) showed a substantial increase in relation to severe depressive symptoms when compared to using screen in the dark alone (OR = 2.09, 95%CI: 1.39, 3.14) or insufficient sleep alone (OR = 2.06, 95%CI: 1.65, 2.57). Likewise, the joint effects of using screen in the dark and screen time > 2 hours/day or insufficient sleep on severe depressive symptoms were consistent with depressive symptoms (Table 3).
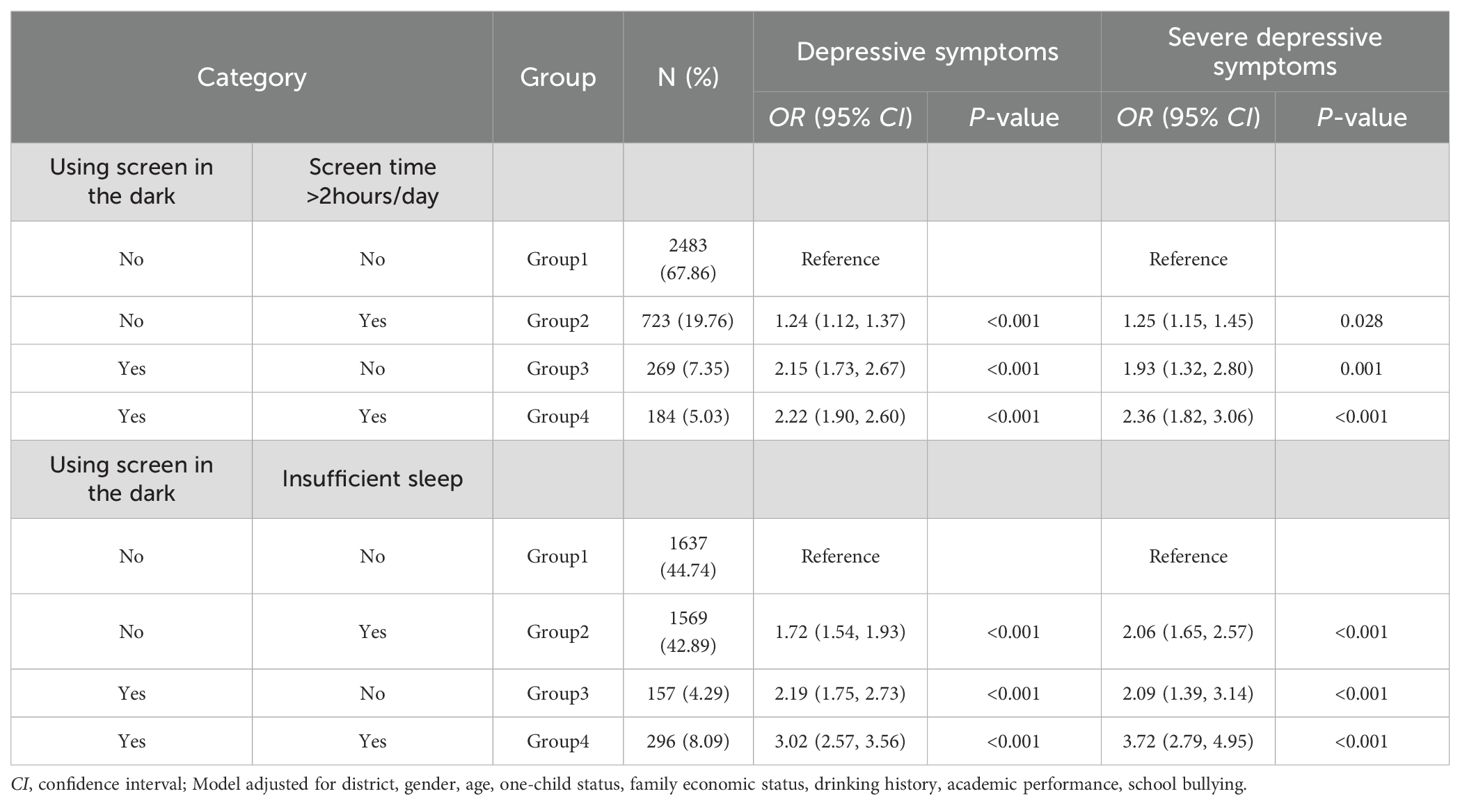
Table 3. Joint effect of using screen in the dark and screen time > 2hours/day or insufficient sleep on depressive symptoms.
4 Discussion
4.1 Main findings of this study
In this population-based, three-year longitudinal study conducted among 3,659 adolescents in Shanghai, China, it was found that 23.59% of participants exhibited depressive symptoms, while 5.25% experienced severe depressive symptoms in 2020. 15.76% adolescents who had depressive symptoms in 2020 aggravated to severe depressive symptoms in 2021 or 2022. Female adolescents and senior high school students were more susceptible to depression. Notably, over 10% of the adolescents reported using screens in the dark, a behavior significantly associated with depressive symptoms. Moreover, a robust association was observed between adolescents who used screens in the dark and those who experienced depressive symptoms, particularly when screen time exceeded two hours per day or when there was insufficient sleep, with the association being especially pronounced in cases of severe depressive symptoms.
The prevalence of depressive symptoms among adolescents observed in our study aligns with findings from a global meta-analysis (23), but lower than a national survey conducted at the early stage of the COVID-19 outbreak (24). The reasons might be that the epidemic has a greater impact on adolescents’ mental health, as well as the measurement instruments and cut-off scores were different in these studies. The CES-D, which was utilized in our research, is acknowledged as one of the most extensively used self-assessment tools in psychiatric epidemiology. It has also been widely applied in subsequent studies to screen for depression in adolescents. Previous studies have reported cut-off scores ranging from 14 to 30, exhibiting considerable variability without a consistent pattern (19). This variability complicates comparisons of prevalence rates across studies. Future research should focus on establishing standardized cut-off values to improve cross-study comparability.
Univariate analyses indicated that female students, screen use in dark environments, and inadequate sleep were correlated with depressive symptoms, including severe and persistent forms. High school seniors were at a heightened risk for persistent and cumulative depressive symptoms. This increased risk is attributed to the substantial academic pressure faced by high school seniors while preparing for the National College Entrance Examination, which is considered the most critical examination in their academic careers. In contrast, junior high school and vocational middle school students are exposed to comparatively lower academic demands. Consistent with previous research, our study identified a higher prevalence of depression among female adolescents (27.26%) compared to males (20.18%) in 2020. A national survey indicated that 39.5% (25) of female adolescents aged 11–18 years experienced depression, a figure exceeding that of our study, likely due to its timing during the COVID-19 outbreak in February 2020. The gender disparity in adolescent depression is a well-established phenomenon. Depression arises through multiple pathways, including biological vulnerabilities [e.g., hormonal and neurodevelopmental changes (26)] and psychosocial risk factors [e.g., low self-esteem, exposure to stress and violence (5, 27)]. Nonetheless, depression in males should not be overlooked, as the gender disparity in prevalence diminishes and stabilizes in adulthood (28). Furthermore, additional research is warranted to elucidate the genetic and social determinants underlying these gender differences in depression.
Our study identified an independent association between screen use in dark environments and depressive symptoms in adolescents. As previously mentioned, screen use in the dark may lead to increased LAN exposure. Animal studies (29–31) have demonstrated that LAN exposure can induce anti-social, anxiogenic, and depressive behaviors, even at minimal light levels as low as 5 lux. Human studies further support the LAN-depression link (32–34). A recent study confirmed that LAN is associated with mood and anxiety disorders among adolescents in the United States (4). While, the mechanisms underlying the association between screen use in dark environments and depression remain uncertain. Numerous studies have indicated that exposure to screen light during nighttime may diminish the secretion of melatonin, a hormone integral to sleep regulation, thereby disrupting the circadian timing system (35, 36). Recent research suggests that even brief exposure to light at night (0.5-3 hours) can increase levels of corticotropin-releasing hormone (CRH) and cortisol, potentially leading to heightened anxiety (37). In summary, nighttime light exposure may contribute to emotional disorders through multiple pathways: (1) dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, (2) suppression of melatonin secretion, and (3) impaired function of mood-related brain regions. Notably, adolescents show greater physiological sensitivity to LAN than adults (38, 39). The delayed melatonin rhythms and stronger suppression of melatonin by nighttime light may explain the higher prevalence of depression and anxiety in adolescents compared to adults.
More than 20% of adolescents reported engaging with electronic devices for several hours daily, a prevalence rate consistent with a study conducted in Guangzhou (6). Many studies (18, 40) have documented the adverse effects of prolonged internet use on adolescent depression. Excessive screen time has been associated with various psychological issues, including low self-esteem, stress, anxiety, depression, insecurity, and loneliness (16, 41). Several researchers have demonstrated that time spent on screens can displace participation in critical activities that may mitigate symptoms of depression, including adequate sleep (6, 42), physical exercise (43), and interpersonal communication with parents and peers. Empirical studies have confirmed the significant mediating role of these factors in the relationship between screen time and depression. Furthermore, excessive use of digital media screens may lead to various adverse effects, such as unhealthy eating behaviors, addiction, poor academic performance, cyber victimization, substance abuse, and diminished social interactions with others (44–46). These adverse effects may also contribute to mental health issues. Conversely, certain studies have indicated that internet use may alleviate depression in adolescents (47), potentially due to participation in recreational activities such as gaming, watching films or short videos, and listening to music, which can aid in stress relief and relaxation (48). Further research Future research should delineate the dual roles of screen media by jointly analyzing usage duration, content type, and contextual factors in adolescent mental health outcomes.
The current study suggests that adolescents who engage in screen use in dark environments coupled with insufficient sleep or prolonged screen time (> 2 hours/day) exhibit a higher likelihood of experiencing depressive symptoms. Notably, the combined effect of screen use in the dark and inadequate sleep significantly related to the severity of depressive symptoms. Furthermore, sleep disorders have been identified as definitive risk factors for depressive symptoms (42, 49). Numerous additional factors may indirectly influence depression by impacting sleep. A mediation analysis study indicated that electronic devices use exerted indirect effects on depressive symptoms through sleep duration reduction among adolescents (50). Nevertheless, the underlying pathophysiological mechanisms linking the combined effects of screen use in dark environments with insufficient sleep or extended screen time to depression remain inadequately understood. Additional high-quality research is required to elucidate these mechanisms.
This study has several limitations. Firstly, residual confounding may persist due to unmeasured variables such as dynamic parenting styles and fluctuating academic stress, which should be modeled as time-varying covariates in longitudinal designs. However, we adjusted for key confounders (e.g., one-child status and academic performance), strengthening the internal validity of our conclusions. Additionally, chronotype misalignment in adolescents may lead to circadian disruption, which could result in the emergence of more severe mood symptoms. It’s needed to investigate chronotype of adolescents and explore the relationship between using screen and depression. Secondly, the data utilized in this study were derived from the Surveillance of Students’ Common Diseases and Health Influencing Factors in Shanghai, China, which was not originally designed as a cohort study. We extracted data spanning from 2020 to 2022. Therefore, the representation of the samples and the resulting findings should be interpreted with caution. Because the economic level of Shanghai is higher, the results may not represent adolescents from cities with lower economic level. What’s more, the causal association and the moderate effect need to explore in the future. Thirdly, the data concerning screen use in low-light conditions were not collected with high precision. It would be advantageous to employ devices to measure screen luminance and to gather detailed information regarding screen types and the content viewed by adolescents in such conditions. The primary challenge was the large-scale nature of the survey, coupled with the fact that the participants were students, which rendered precise measurement difficult. In our future research, we aim to optimize the study design to address these limitations.
4.2 Conclusions
In conclusion, this longitudinal study establishes screen use in dark environments—a behaviorally modifiable source of nighttime light exposure—as an independent influencing factor for adolescent depressive symptoms. Adolescents engaging in screen use in the dark, particularly those experiencing insufficient sleep or exceeding two hours of screen time per day, exhibit a higher likelihood of developing depressive symptoms. Concurrently, there is a need for high-quality research to elucidate the causal association and its mechanisms. If these findings hold true, minimizing screen exposure in dark settings may represent a practical strategy for mitigating depression risk. It is imperative for governmental bodies to implement policy measures aimed at reducing nighttime light exposure and enhancing the mental health of adolescents. Greater attention should be directed by educational institutions and society towards addressing depression among female and senior high school students.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Shanghai Municipal Center for Disease Control and Prevention. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
SQ: Writing – review & editing, Funding acquisition, Formal analysis, Writing – original draft, Conceptualization. FZ: Writing – review & editing, Methodology, Project administration. XW: Writing – original draft, Resources, Methodology. SH: Writing – original draft, Resources, Data curation. KZ: Writing – original draft, Data curation, Software. LC: Software, Writing – original draft, Data curation. YH: Investigation, Writing – original draft. YY: Investigation, Writing – original draft. DY: Conceptualization, Writing – review & editing, Project administration, Validation. CL: Conceptualization, Writing – review & editing, Funding acquisition, Supervision.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was funded by the Three-year Action Plan for Strengthening the Construction of Public Health System in Shanghai (2023-2025) (GWVI-11.2-YQ26, GWVI-11.1-31, GWVI-7). The funders had no role in the study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
The authors wish to thank the study participants for their contribution to the research, as well as investigators and staff.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Adolescent mental health: Fact sheet(2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (Accessed March 15, 2025).
2. Li ZB, Lv JJ, Lu W, Yin MY, Li XY, and Yang CH. Burden of depression in adolescents in the Western Pacific Region from 1990 to 2019: An age-period-cohort analysis of the Global Burden of Disease study. Psychiatry Res. (2024) 336:115889. doi: 10.1016/j.psychres.2024.115889
3. Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10-24 years: a systematic analysis. Lancet. (2011) 377:2093–102. doi: 10.1016/S0140-6736(11)60512-6
4. Paksarian D, Rudolph KE, Stapp EK, Dunster GP, He J, Mennitt D, et al. Association of outdoor artificial light at night with mental disorders and sleep patterns among US adolescents. JAMA Psychiatry. (2020) 77:1266–75. doi: 10.1001/jamapsychiatry.2020.1935
5. Potter JR and Yoon KL. Interpersonal factors, peer relationship stressors, and gender differences in adolescent depression. Curr Psychiatry Rep. (2023) 25:759–67. doi: 10.1007/s11920-023-01465-1
6. Wang W, Du X, Guo Y, Li W, Zhang S, Zhang W, et al. Associations among screen time, sleep duration and depressive symptoms among Chinese adolescents. J Affect Disord. (2021) 284:69–74. doi: 10.1016/j.jad.2021.01.082
7. Pandi-Perumal SR, Monti JM, Burman D, Karthikeyan R, BaHammam AS, Spence DW, et al. Clarifying the role of sleep in depression: A narrative review. Psychiatry Res. (2020) 291:113239. doi: 10.1016/j.psychres.2020.113239
8. Won E, Na KS, and Kim YK. Associations between melatonin, neuroinflammation, and brain alterations in depression. Int J Mol Sci. (2021) 23:305. doi: 10.3390/ijms23010305
9. Bumgarner JR and Nelson RJ. Light at night and disrupted circadian rhythms alter physiology and behavior. Integr Comp Biol. (2021) 61:1160–9. doi: 10.1093/icb/icab017
10. Czeisler CA, Kronauer RE, Allan JS, Duffy JF, Jewett ME, Brown EN, et al. Bright light induction of strong (type 0) resetting of the human circadian pacemaker. Science. (1989) 244:1328–33. doi: 10.1126/science.2734611
11. Wang B, Pengcheng YI, Pan JING, Fang C.H.E.N.G., and Zhang W. Relationships between sleep quality and smart phone usage before bed among middle school students in Ningbo. Chin J Sch Health. (2019) 40:58–61. doi: 10.16835/j.cnki.1000-9817.2019.01.015
12. Seo JH, Kim JH, Yang KI, and Hong SB. Late use of electronic media and its association with sleep, depression, and suicidality among Korean adolescents. Sleep Med. (2017) 29:76–80. doi: 10.1016/j.sleep.2016.06.022
13. Munezawa T, Kaneita Y, Osaki Y, Kanda H, Minowa M, Suzuki K, et al. The association between use of mobile phones after lights out and sleep disturbances among Japanese adolescents: a nationwide cross-sectional survey. Sleep. (2011) 34:1013–20. doi: 10.5665/SLEEP.1152
14. Shechter A, Quispe KA, Mizhquiri Barbecho JS, Slater C, and Falzon L. Interventions to reduce short-wavelength (“blue”) light exposure at night and their effects on sleep: A systematic review and meta-analysis. Sleep Adv: J Sleep Res Society. (2020) 1:zpaa002. doi: 10.1093/sleepadvances/zpaa002
15. Obayashi K, Saeki K, Iwamoto J, Ikada Y, and Kurumatani N. Exposure to light at night and risk of depression in the elderly. J Affect Disord. (2013) 151:331–6. doi: 10.1016/j.jad.2013.06.018
16. Augner C, Vlasak T, Aichhorn W, and Barth A. The association between problematic smartphone use and symptoms of anxiety and depression—a meta-analysis. J Public Health. (2021) 45:193–201. doi: 10.1093/pubmed/fdab350
17. Ma L, Evans B, Kleppang AL, and Hagquist C. The association between screen time and reported depressive symptoms among adolescents in Sweden. Fam Pract. (2021) 38:773–9. doi: 10.1093/fampra/cmab029
18. Wu H, Ji JM, Qian Y, Jin XH, Yu HR, Liu XM, et al. Relationship between depressive symptoms and internet usage time among adolescents: Results from a nationwide survey. Psychiatry Res. (2022) 313:114603. doi: 10.1016/j.psychres.2022.114603
19. Park SH and Kwon YM. Can the center for epidemiologic studies depression scale be used to screen for depression in children and adolescents? An updated systematic review. Child Psychiatry Hum Dev. (2023) 56:277–87. doi: 10.1007/s10578-023-01553-6
20. Yang W, Xiong G, Garrido LE, Zhang JX, Wang MC, and Wang C. Factor structure and criterion validity across the full scale and ten short forms of the CES-D among Chinese adolescents. Psychol Assess. (2018) 30:1186–98. doi: 10.1037/pas0000559
21. Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. (1991) 20:149–66. doi: 10.1007/BF01537606
22. Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health. (2015) 1:233–43. doi: 10.1016/j.sleh.2015.10.004
23. Cuijpers P, Karyotaki E, Eckshtain D, Ng MY, Corteselli KA, Noma H, et al. Psychotherapy for depression across different age groups: A systematic review and meta-analysis. JAMA Psychiatry. (2020) 77:694–702. doi: 10.1001/jamapsychiatry.2020.0164
24. Qi H, Liu R, Feng Y, Luo J, Lei SM, Cheung T, et al. Prevalence of depression and its associated factors among adolescents in China during the early stage of the COVID-19 outbreak. Peer J. (2021) 9:e12223. doi: 10.7717/peerj.12223
25. Zhou J, Yuan X, Qi H, Liu R, Li Y, Huang H, et al. Prevalence of depression and its correlative factors among female adolescents in China during the coronavirus disease 2019 outbreak. Global Health. (2020) 16:69. doi: 10.1186/s12992-020-00601-3
26. Uddin M, Koenen KC, de Los Santos R, Bakshis E, Aiello AE, and Galea S. Gender differences in the genetic and environmental determinants of adolescent depression. Depress Anxiety. (2010) 27:658–66. doi: 10.1002/da.20692
27. Vucenovic D, Sipek G, and Jelic K. The role of emotional skills (Competence) and coping strategies in adolescent depression. Eur J Invest Health Psychol Education. (2023) 13:540–52. doi: 10.3390/ejihpe13030041
28. Salk RH, Hyde JS, and Abramson LY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol Bull. (2017) 143:783–822. doi: 10.1037/bul0000102
29. Li Z, Lee CS, Peng HY, Lin TB, Hsieh MC, Lai CY, et al. Lights at night mediate depression-like behavioral and molecular phenotypes in a glucocorticoid-dependent manner in male rats. Neuropharmacology. (2024) 248:109888. doi: 10.1016/j.neuropharm.2024.109888
30. Medeiros Contini F and Seggio JA. Constant light and single housing alter novelty-induced locomotor activity and sociability in female Swiss Webster mice. Neuro Endocrinol Lett. (2023) 44:117–22.
31. Wu F, Wu S, Gui Q, Tang K, Xu Q, Tao Y, et al. Blue light insertion at night is involved in sleep and arousal-promoting response delays and depressive-like emotion in mice. Biosci Rep. (2021) 41:BSR20204033. doi: 10.1042/BSR20204033
32. Helbich M, Browning M, and Huss A. Outdoor light at night, air pollution and depressive symptoms: A cross-sectional study in the Netherlands. Sci Total Environ. (2020) 744:140914. doi: 10.1016/j.scitotenv.2020.140914
33. Obayashi K, Saeki K, and Kurumatani N. Bedroom light exposure at night and the incidence of depressive symptoms: A longitudinal study of the HEIJO-KYO cohort. Am J Epidemiol. (2018) 187:427–34. doi: 10.1093/aje/kwx290
34. Tonon AC, Constantino DB, Amando GR, Abreu AC, Francisco AP, de Oliveira MAB, et al. Sleep disturbances, circadian activity, and nocturnal light exposure characterize high risk for and current depression in adolescence. Sleep. (2022) 45:zsac104. doi: 10.1093/sleep/zsac104
35. Nagare R, Plitnick B, and Figueiro MG. Does the iPad Night Shift mode reduce melatonin suppression? Light Res Technol. (2019) 51:373–83. doi: 10.1177/1477153517748189
36. Rahman SA, Wright KP Jr., Lockley SW, Czeisler CA, and Gronfier C. Characterizing the temporal dynamics of melatonin and cortisol changes in response to nocturnal light exposure. Sci Rep. (2019) 9:19720. doi: 10.1038/s41598-019-54806-7
37. Wang G, Liu YF, Yang Z, Yu CX, Tong Q, Tang YL, et al. Short-term acute bright light exposure induces a prolonged anxiogenic effect in mice via a retinal ipRGC-CeA circuit. Sci Adv. (2023) 9:eadf4651. doi: 10.1126/sciadv.adf4651
38. Bonilla P, Shanks A, Nerella Y, and Porcu A. Effects of chronic light cycle disruption during adolescence on circadian clock, neuronal activity rhythms, and behavior in mice. Front Neurosci. (2024) 18:1418694. doi: 10.3389/fnins.2024.1418694
39. Crowley SJ, Cain SW, Burns AC, Acebo C, and Carskadon MA. Increased sensitivity of the circadian system to light in early/mid-puberty. J Clin Endocrinol Metab. (2015) 100:4067–73. doi: 10.1210/jc.2015-2775
40. Vidal C, Lhaksampa T, Miller L, and Platt R. Social media use and depression in adolescents: a scoping review. Int Rev Psychiatry. (2020) 32:235–53. doi: 10.1080/09540261.2020.1720623
41. Huang XC, Zhang YN, Wu XY, Jiang Y, Cai H, Deng YQ, et al. Correction: A cross-sectional study: family communication, anxiety, and depression in adolescents: the mediating role of family violence and problematic internet use. BMC Public Health. (2023) 23:2345. doi: 10.1186/s12889-023-17226-x
42. Plante DT. The evolving nexus of sleep and depression. Am J Psychiatry. (2021) 178:896–902. doi: 10.1176/appi.ajp.2021.21080821
43. Almaqhawi A and Albarqi M. The effects of technology use on children’s physical activity: a cross-sectional study in the Eastern province of Saudi Arabia. J Med Life. (2022) 15:1240–5. doi: 10.25122/jml-2022-0148
44. Li G, Conti AA, Qiu C, and Tang W. Adolescent mobile phone addiction during the COVID-19 pandemic predicts subsequent suicide risk: a two-wave longitudinal study. BMC Public Health. (2022) 22:1537. doi: 10.1186/s12889-022-13931-1
45. Cuong VM, Assanangkornchai S, Wichaidit W, Minh Hanh VT, and My Hanh HT. Associations between gaming disorder, parent-child relationship, parental supervision, and discipline styles: Findings from a school-based survey during the COVID-19 pandemic in Vietnam. J Behav Addict. (2021) 10:722–30. doi: 10.1556/2006.2021.00064
46. Maurer BT and Taylor LC. The effect of digital media on children in their formative years. Jaapa. (2020) 33:46–51. doi: 10.1097/01.JAA.0000660180.96512.70
47. Pea R, Nass C, Meheula L, Rance M, Kumar A, Bamford H, et al. Media use, face-to-face communication, media multitasking, and social well-being among 8- to 12-year-old girls. Dev Psychol. (2012) 48:327–36. doi: 10.1037/a0027030
48. Padillah R, Setyosari P, Hambali IM, and Indreswari H. Combining music and film as therapy: how to reduce adolescent anxiety symptoms in digital era. J Public Health. (2023) 45:e779–80. doi: 10.1093/pubmed/fdad072
49. Luo X, Zhou Y, Zheng R, Li X, Dai Y, Narayan A, et al. Association of health-risk behaviors and depressive symptoms and anxiety symptoms: a school-based sample of Chinese adolescents. J Public Health. (2019) 42:e189–98. doi: 10.1093/pubmed/fdz115
Keywords: screen time, insufficient sleep, depressive symptoms, light at night, adolescents
Citation: Qu S, Zhang F, Wang X, Huang S, Zheng K, Chu L, Huang Y, Yang Y, Yang D and Luo C (2025) The association between using screen in the dark and depressive symptoms: a longitudinal study among Chinese adolescents. Front. Psychiatry 16:1618965. doi: 10.3389/fpsyt.2025.1618965
Received: 27 April 2025; Accepted: 29 July 2025;
Published: 20 August 2025.
Edited by:
André Comiran Tonon, Federal University of Rio Grande do Sul, BrazilReviewed by:
Lijuan Gao, Tianjin Xiqing Hospital, ChinaGuilherme Amando, Federal University of Rio Grande do Sul, Brazil
Copyright © 2025 Qu, Zhang, Wang, Huang, Zheng, Chu, Huang, Yang, Yang and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dongling Yang, eWFuZ2RvbmdsaW5nQHNjZGMuc2guY24=; Chunyan Luo, bHVvY2h1bnlhbl9lc3NAMTYzLmNvbQ==
†Present address: Chunyan Luo, Shanghai Municipal Center for Disease Control and Prevention, Shanghai, China
 Shuangxiao Qu
Shuangxiao Qu Fengyun Zhang
Fengyun Zhang Xuelai Wang
Xuelai Wang Liting Chu
Liting Chu