Abstract
Background:
Overt aggression may be associated with childhood maltreatment (CM), insomnia, and alexithymia, but the underlying mechanisms of these associations have not been fully explored in adolescents with major depressive disorder (MDD). Therefore, the present study aimed to deeply analyze the relationships between overt aggression and CM, insomnia, and alexithymia in adolescents with MDD, to reveal the mediating mechanisms, and to provide a theoretical basis for clinical interventions.
Methods:
From January 2024 to March 2025, this study included 251 adolescents with MDD. The Modified Overt Aggression Scale (MOAS), the 17-item Hamilton Depression Rating Scale (HAMD-17), the Childhood Trauma Questionnaire (CTQ), the Insomnia Severity Index Scale (ISI), and the Toronto Alexithymia Scale (TAS-20) were used to assess the adolescents’ overt aggression, depression, CM, insomnia, and alexithymia. Additionally, we employed the PROCESS macro program to examine the mediating role of insomnia and alexithymia between CM and overt aggression.
Results:
The prevalence of overt aggression in adolescents with MDD was 66.1%. The regression analyses showed that age (Beta = -0.761, t = -2.967, P = 0.003), depression (Beta = 0.183, t = 2.676, P = 0.008), CM (Beta = 0.132, t = 4.048, P < 0.001), and alexithymia (Beta = 0.092, t = 1.990, P = 0.048) were independent correlates of overt aggression. When CTQ subscale scores involved in the regression model, age (Beta = -0.829, t = -3.257, P = 0.001), depression (Beta = 0.184, t = 2.618, P = 0.009), emotional abuse (Beta = 0.372, t = 4.081, P < 0.001), and insomnia (Beta = 0.170, t = 2.054, P = 0.041) were independent correlates. Moreover, alexithymia and insomnia played a chain mediating role between CM and overt aggression.
Conclusion:
The risk of overt aggression is significantly higher in depressed adolescents and is significantly associated with CM, insomnia, and alexithymia. Additionally, insomnia and alexithymia may play a mediating role between CM and overt aggression. Given these findings, comprehensive interventions for depressed adolescents with adverse childhood experiences, insomnia, and alexithymia, should be emphasized in clinical practice to effectively reduce their risk of overt aggression.
1 Introduction
Major depressive disorder (MDD) is one of the most prevalent affective disorders in the adolescent population (1). In recent years, with rapid societal changes and transformations, the prevalence of MDD in adolescents has significantly increased (2). According to data from a national epidemiological survey in China, the prevalence of MDD in children and adolescents has been reported to be 2.0% (3). Not only does this disorder significantly impact adolescents’ schooling and daily lives, but it also markedly increases the risk of self-injury and suicide (4). Moreover, MDD is significantly associated with increased aggressive behaviors. For example, studies have shown that among adolescents with MDD, there is a high prevalence of aggressive behaviors, which are closely related to the severity of depressive symptoms (5). More importantly, individuals’ aggressive behaviors have been shown to significantly predict suicide attempts and deaths by suicide (6, 7). However, research on aggressive behaviors in adolescents with MDD remains limited. Therefore, it is particularly important and urgent to thoroughly investigate the current status and underlying mechanisms of aggression in this population.
Childhood maltreatment (CM) is typically defined as a serious adverse experience that an individual encounters during childhood, primarily including abuse and neglect (8). The prevalence of CM varies significantly across different populations. A large-scale survey conducted in 17 secondary schools in China found that the prevalence of CM among the general adolescent population was 34.8% (9). In contrast, the detection rate of CM in adolescents with MDD exceeds 80% (10). And, patients with MDD who have experienced traumatic childhood events tend to present a more complex set of clinical features, including an earlier age of onset of depressive symptoms, a higher frequency of relapses, a more severe and prolonged course of symptoms, and a generally poorer prognosis (11–13). Additionally, there may be connections between CM and individuals’ aggressive behaviors. For example, a cross-sectional study of Chinese children showed that psychological abuse in childhood was significantly associated with increased aggressive behaviors (14). At the physiological level, CM can disrupt specific brain structures and functions, increasing an individual’s susceptibility to aggression (15). This, in turn, can lead to adverse health outcomes and behavioral problems in adolescents, such as impulsive behaviors and violent tendencies. Nevertheless, the underlying mechanisms of the association between CM and aggression in adolescents with MDD remain incompletely understood. Given the high prevalence of CM and aggression in this population, examining the psychological and behavioral mechanisms underlying this link is crucial. Such research will help provide more specific targets for clinical practitioners to better identify and intervene in aggressive behaviors, ultimately improving outcomes for these adolescents.
Alexithymia and insomnia may play a significant role in the association between CM and aggression. Alexithymia, as an emotional processing deficit, is characterized by an individual’s difficulty in accurately identifying, differentiating, and expressing their emotional states (16). Notably, the prevalence of alexithymia is significantly higher in patients with psychiatric disorders, particularly those with depression (17). The development of alexithymia is a complex process whose roots can be traced back to an individual’s childhood. According to the Emotion Regulation Theory, traumatic childhood events may severely impair an individual’s ability to recognize and express emotions, and interfere with the normal development of the brain’s emotional center, thereby contributing to the development of alexithymia (18, 19). Emotion Regulation Theory further suggests that individuals with alexithymia are often unable to effectively use adaptive emotion regulation strategies (e.g., cognitive reappraisal) to alleviate internalized anger and tension when facing with stress or conflict (20). This emotion dysregulation may increase the likelihood of individuals adopting aggressive behaviors to cope with problems, thereby increasing adolescents’ susceptibility to aggression (21).
Additionally, insomnia may also play a mediating role in the association between CM and aggression. Previous studies have demonstrated that comorbid CM significantly increases the risk of insomnia in adolescents (22, 23). Insomnia not only impairs an individual’s ability to regulate their emotions, but may also contribute to increased emotional instability and irritability (24, 25). For example, a meta-analysis integrating 74 studies showed that poorer sleep quality was significantly associated with higher aggression in both children and adolescents, as well as in adults (26). Of interest, previous research has also found that alexithymia may contribute to the occurrence of insomnia in individuals (27). This suggests that alexithymia → insomnia may constitute a chain-mediated pathway in the association between CM and aggressive behaviors. However, this mechanism has not been fully explored in the population of adolescents with MDD.
Therefore, the aim of the present study was to analyze factors associated with overt aggression (including socio-demographic characteristics, depressive symptoms, CM, insomnia, and alexithymia) in adolescents with MDD, focusing on whether alexithymia and insomnia mediate the relationship between CM and overt aggression. Based on the above aims, we hypothesized that: (a) there are strong associations between overt aggression and socio-demographic characteristics, depressive symptoms, CM, insomnia, and alexithymia in adolescents with MDD, and (b) alexithymia and insomnia play a chain-mediated effect in the relationship between CM and overt aggression.
2 Methods
2.1 Study design and participants
This cross-sectional study was conducted from January 2024 to March 2025 at Bozhou People’s Hospital, Bozhou, Anhui Province, China, targeting adolescent psychiatric patients.. Inclusion criteria were: (1) age 12–18 years; (2) diagnosis of MDD according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5); and (3) willingness to participate fully in the study. Exclusion criteria included: (1) presence of other psychiatric disorders (e.g., schizophrenia, bipolar disorder); (2) significant medical conditions (e.g., major infections, autoimmune diseases); and (3) inability to complete assessments. Ultimately, a total of 251 adolescents with MDD were included, of whom 185 (73.7%) were female. The mean age of the participants was (15.42 ± 1.55) years, the mean age at onset was (13.84 ± 1.78) years, and the mean duration of illness was (18.35 ± 16.63) months (Table 1).
Table 1
| Variables | MDD (n = 251) |
|---|---|
| Females, n (%) | 185 (73.71) |
| Age (years), mean (SD) | 15.42 (1.55) |
| BMI (kg/m2), mean (SD) | 20.96 (3.84) |
| Age at onset (years), mean (SD) | 13.84 (1.78) |
| Duration of illness (months), median (P25, P75) | 12.00 (6.00, 24.00) |
| Antidepressants, n (%) | |
| None | 116 (46.21) |
| SSRIs | 120 (47.81) |
| Others | 15 (5.98) |
| MOAS total score, mean (SD) | 8.29 (6.88) |
| Overt aggression, n (%) | |
| No | 85 (32.57) |
| Yes | 166 (66.13) |
| HAMD-17 total score, mean (SD) | 21.34 (6.28) |
| CTQ total score, mean (SD) | 52.67 (12.88) |
| Sexual abuse, mean (SD) | 5.94 (2.37) |
| Emotional abuse, mean (SD) | 11.72 (4.49) |
| Physical abuse, mean (SD) | 7.36 (2.90) |
| Emotional neglect, mean (SD) | 16.51 (4.89) |
| Physical neglect, mean (SD) | 11.13 (3.54) |
| TAS-20 total score, mean (SD) | 69.03 (9.02) |
| ISI total score, mean (SD) | 13.43 (5.17) |
Socio-demographic and clinical characteristics of adolescents with MDD.
MDD, major depressive disorder; BMI, body mass index; SSRIs, selective serotonin reuptake inhibitors; MOAS, modified overt aggression scale; HAMD-17, 17-item hamilton depression scale; CTQ, childhood trauma questionnaire; TAS-20, toronto alexithymia scale; ISI, insomnia severity index scale.
SD, standard deviation.
The study was approved by the Ethics Committee of Bozhou People’s Hospital (No. 126, 2024), and written informed consent was obtained from all participants and their parents. Furthermore, all procedures conformed to the ethical standards of the 2013 version of the Helsinki Declaration (https://www.wma.net/policies-post/wma-declaration-of-helsinki/).
2.2 Measuring instruments
2.2.1 Socio-demographic characteristics
Socio-demographic data were obtained via a self-administered questionnaire, covering variables such as gender, age, body mass index (BMI), age at onset, duration of illness, and use of antidepressant medication.
2.2.2 Overt aggression
The Modified Overt Aggression Scale (MOAS) was utilized to assess overt aggression (28). The MOAS consists of four subscales: verbal attacks, assaults against objects, assaults against self, and physical aggression toward others. Higher total score indicates more severe aggression. Based on previous studies, the MOAS total score ≥ 4 was defined as the presence of overt aggression (28, 29). Currently, the MOAS is extensively validated and widely applied among adolescents (30, 31). In our study, the standardized Cronbach’s alpha coefficient for this scale was 0.723, which suggests satisfactory reliability for this measure.
2.2.3 Depressive symptoms
The severity of depressive symptoms was assessed using the 17-item Hamilton Depression Rating Scale (HAMD-17) (32). This scale comprises 17 items, scored from 0 to 76, with higher total score reflecting more severe depressive symptoms. The HAMD-17 has demonstrated strong reliability and validity, and has been widely adopted in Chinese adolescents with MDD (33, 34). In our study, the standardized Cronbach’s alpha coefficient for this scale was 0.714.
2.2.4 Childhood maltreatment
The Childhood Trauma Questionnaire (CTQ) was employed to evaluate CM in patients (35). The CTQ includes 28 items: 25 clinical items and 3 validity items, divided into five subscales: sexual abuse, emotional abuse, physical abuse, emotional neglect, and physical neglect. Each subscale comprises 5 items scored on a 5-point scale, yielding a subscale score range of 5 - 25. The CTQ total score is the sum of all subscale scores, with higher values indicating more severe childhood trauma. The Chinese version of the CTQ demonstrates robust reliability, validity, and internal consistency (36). In this study, the standardized Cronbach’s alpha coefficient for the CTQ was 0.741.
2.2.5 Insomnia symptoms
The Insomnia Severity Index (ISI) was utilized to assess the severity of insomnia symptoms over the past two weeks (37, 38). This scale consists of 7 items scored on a 5-point scale. The ISI total score ranges from 0 to 28, with higher scores indicating more severe insomnia. In this study, the standardized Cronbach’s alpha coefficient for the ISI was 0.795.
2.2.6 Alexithymia
The Toronto Alexithymia Scale (TAS-20) was utilized to assess difficulties in identifying and expressing emotions (39). The scale consists of 20 items scored on a 5-point scale, and the total score ranges from 20 to 100, with a higher total score indicating greater difficulties in emotional expression. The Chinese version of TAS-20 is extensively validated and widely used among Chinese adolescents with MDD (40, 41). In this study, the standardized Cronbach’s alpha coefficient for this scale was 0.731, indicating acceptable internal consistency.
2.3 Statistical analysis
Statistical analyses were performed using SPSS 23.0. Categorical variables were described using frequency (%). Continuous variables were assessed for normality using the Kolmogorov-Smirnov test. Normally distributed data were described as mean ± standard deviation (SD), while non-normally distributed data were described using the median (quartiles) [M (P25, P75)]. In univariate analyses, Pearson or Spearman correlation analyses were used to examine the correlations between MOAS total score with socio-demographic and clinical characteristics. In multivariate analyses, the linear regression model using the “Stepwise” method was applied to identify which factors (variables with P < 0.05 in the univariate analyses) were independent correlates of overt aggression (the dependent variable). In addition, Pearson correlation analyses were used to explore correlations between CM, overt aggression, insomnia and alexithymia. Finally, the mediating effects of insomnia and alexithymia in the associations between CM and overt aggression was analyzed using model 6 of the PROCESS macro program. And we performed 5,000 bootstrapped samples to assess the significance of the mediation effect, and a 95% confidence interval (CI) that did not contain zero indicated that the effect was statistically significant. In the mediation analyses, we controlled for multiple potential covariates, including age, sex, and depressive symptoms. All statistical tests were considered statistically significant at P < 0.05 (two-sided).
3 Results
3.1 Correlations between overt aggression with socio-demographic and clinical characteristics in adolescents with MDD
In this cross-sectional study, the prevalence of overt aggression in adolescents with MDD was 66.1% (Table 1). Pearson correlation analyses showed that overt aggression was negatively correlated with age (r = -0.242, P < 0.001) and age at onset (r = -0.209, P = 0.001), and positively correlated with depression (r = 0.305, P < 0.001), CTQ total score (r = 0.350, P < 0.001), emotional abuse (r = 0.333, P < 0.001), physical abuse (r = 0.217, P = 0.001), emotional neglect (r = 0.243, P < 0.001), physical neglect (r = 0.258, P < 0.001), alexithymia (r = 0.246, P < 0.001), and insomnia (r = 0.232, P < 0.001) (Table 2).
Table 2
| Variables | MDD (n = 251) | |
|---|---|---|
| r | P | |
| Gender | -0.127 a | 0.045 |
| Age | -0.242 | <0.001 |
| BMI | -0.110 | 0.081 |
| Age at onset | -0.209 | 0.001 |
| Duration of illness | 0.050 a | 0.430 |
| Antidepressants | -0.035 a | 0.577 |
| HAMD-17 total score | 0.305 | <0.001 |
| CTQ total score | 0.350 | <0.001 |
| Sexual abuse | 0.120 | 0.057 |
| Emotional abuse | 0.333 | <0.001 |
| Physical abuse | 0.217 | 0.001 |
| Emotional neglect | 0.243 | <0.001 |
| Physical neglect | 0.258 | <0.001 |
| TAS-20 total score | 0.246 | <0.001 |
| ISI total score | 0.232 | <0.001 |
Correlations between MOAS total score with socio-demographic and clinical characteristics in adolescents with MDD.
MDD, major depressive disorder; BMI, body mass index; SSRIs, selective serotonin reuptake inhibitors; MOAS, modified overt aggression scale; HAMD-17, 17-item hamilton depression scale; CTQ, childhood trauma questionnaire; TAS-20, toronto alexithymia scale; ISI, insomnia severity index scale.
Bolded P value: < 0.05.
Spearman correlation analysis.
3.2 Independent factors associated with overt aggression by multivariate linear stepwise regression analyses
The results of multivariate linear stepwise regression analyses were summarized in Table 3. When CTQ total score involved in the regression model, age (Beta = -0.761, t = -2.967, P = 0.003), depression (Beta = 0.183, t = 2.676, P = 0.008), CM (Beta = 0.132, t = 4.048, P < 0.001), and alexithymia (Beta = 0.092, t = 1.990, P = 0.048) were independent correlates of overt aggression. When CTQ subscale scores (including emotional abuse, physical abuse, emotional neglect, and physical neglect) involved in the regression model, age (Beta = -0.829, t = -3.257, P = 0.001), depression (Beta = 0.184, t = 2.618, P = 0.009), emotional abuse (Beta = 0.372, t = 4.081, P < 0.001), and insomnia (Beta = 0.170, t = 2.054, P = 0.041) were independent correlates of overt aggression. In contrast, none of the other CTQ subscales reached statistical significance (P > 0.05) and were therefore progressively excluded from the final regression model.
Table 3
| Variables | Beta | t | P |
|---|---|---|---|
| Model 1 b | |||
| Age | -0.761 | -2.967 | 0.003 |
| HAMD-17 total score | 0.183 | 2.676 | 0.008 |
| CTQ total score | 0.132 | 4.048 | <0.001 |
| TAS-20 total score | 0.092 | 1.990 | 0.048 |
| Model 2 c | |||
| Age | -0.829 | -3.257 | 0.001 |
| HAMD-17 total score | 0.184 | 2.618 | 0.009 |
| Emotional abuse | 0.372 | 4.081 | <0.001 |
| ISI total score | 0.170 | 2.054 | 0.041 |
Independent factors associated with MOAS total score by multivariate linear stepwise regression analysis.
MOAS, modified overt aggression scale; HAMD-17, 17-item hamilton depression scale; CTQ, childhood trauma questionnaire; TAS-20, toronto alexithymia scale; ISI, insomnia severity index scale.
Bolded P value: < 0.05.
, CTQ total score involved in the regression model;
, CTQ subscale scores involved in the regression model.
3.3 Correlations between CM, overt aggression, insomnia and alexithymia in adolescents with MDD
Correlation analyses showed that overt aggression was positively correlated with depressive symptoms, CM (including emotional abuse, physical abuse, emotional neglect, and physical neglect), insomnia, and alexithymia in adolescents with MDD (all P < 0.05) (Table 4). Furthermore, CTQ total score, emotional abuse and physical neglect were significantly positively correlated with insomnia as well as alexithymia (all P < 0.05) (Table 4).
Table 4
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. MOAS total score | 1.00 | |||||||||
| 2. HAMD-17 total score | 0.305 *** | 1.00 | ||||||||
| 3. CTQ total score | 0.350 *** | 0.345 *** | 1.00 | |||||||
| 4. Sexual abuse | 0.120 | 0.121 | 0.447 *** | 1.00 | ||||||
| 5. Emotional abuse | 0.333 *** | 0.280 *** | 0.798 *** | 0.300 *** | 1.00 | |||||
| 6. Physical abuse | 0.217 ** | 0.222 *** | 0.639 *** | 0.309 *** | 0.437 *** | 1.00 | ||||
| 7. Emotional neglect | 0.243 *** | 0.253 *** | 0.786 *** | 0.098 | 0.510 *** | 0.288 *** | 1.00 | |||
| 8. Physical neglect | 0.258 *** | 0.286 *** | 0.717 *** | 0.186 ** | 0.369 *** | 0.345 *** | 0.530 *** | 1.00 | ||
| 9. TAS-20 total score | 0.246 *** | 0.300 *** | 0.188 ** | 0.046 | 0.254 *** | -0.001 | 0.138 * | 0.141 * | 1.00 | |
| 10. ISI total score | 0.232 *** | 0.400 *** | 0.174 ** | 0.094 | 0.130 * | 0.162 * | -0.001 | 0.274 *** | 0.204 ** | 1.00 |
Correlations between childhood maltreatment, overt aggression, insomnia and alexithymia in patients.
MOAS, modified overt aggression scale; HAMD-17, 17-item hamilton depression scale; CTQ, childhood trauma questionnaire; TAS, toronto alexithymia scale; ISI, insomnia severity index scale.
*, P < 0.05; **, P < 0.01; ***, P < 0.001.
3.4 Mediating effects of alexithymia and insomnia in the associations of CM and overt aggression
The results of the mediation analyses were summarized in Table 5, Figures 1–3. Following the PROCESS procedure, the mediating roles of insomnia and alexithymia in the associations between CM and overt aggression were analyzed, resulting in six models. In these models, overt aggression was the dependent variable, with insomnia and alexithymia as mediating variables. The independent variables were: (1) CTQ total score in Model 1, (2) sexual abuse in Model 2, (3) emotional abuse in Model 3, (4) physical abuse in Model 4, (5) emotional neglect in Model 5, and (6) physical neglect in Model 6. The results showed statistically significant indirect effects only for Models 1, 3, and 6. In Model 1, the direct effect value was 0.147 [95% CI (0.085 - 0.209)] and the indirect effect value was 0.026 [95% CI (0.008 - 0.047)]. In model 3, the direct effect value was 0.392 [95% CI (0.213 - 0.572)] and the indirect effect value was 0.075 [95% CI (0.020 - 0.143)]. In model 6, the direct effect value was 0.346 [95% CI (0.112 - 0.580)] and the indirect effect value was 0.116 [95% CI (0.035 - 0.209)]. Of note, although the indirect effect of Model 4 was not significant. However, the mediation pathway from physical abuse to insomnia to overt aggression (Model 4) appeared to be statistically significant.
Table 5
| Models | Effect | Estimate | SE | 95% CI | Effect size (%) |
|---|---|---|---|---|---|
| Model 1 d | Total effect | 0.173 | 0.031 | 0.111 - 0.235 | – |
| Direct effect | 0.147 | 0.031 | 0.085 - 0.209 | 84.97 | |
| Indirect effect | 0.026 | 0.010 | 0.008 - 0.047 | 15.03 | |
| CTQ total score - Alexithymia - Overt aggression | 0.012 | 0.006 | 0.001 - 0.025 | 6.94 | |
| CTQ total score - Insomnia - Overt aggression | 0.012 | 0.007 | 0.001 - 0.027 | 6.94 | |
| CTQ total score - Alexithymia - Insomnia - Overt aggression | 0.003 | 0.002 | 0.001 - 0.006 | 1.15 | |
| Model 2 e | Total effect | 0.342 | 0.177 | -0.007 - 0.692 | – |
| Direct effect | 0.272 | 0.172 | -0.067 - 0.610 | – | |
| Indirect effect | 0.071 | 0.058 | -0.041 - 0.193 | – | |
| Sexual abuse - Alexithymia - Overt aggression | 0.022 | 0.041 | -0.065 - 0.103 | – | |
| Sexual abuse - Insomnia - Overt aggression | 0.045 | 0.031 | -0.002 - 0.119 | – | |
| Sexual abuse - Alexithymia - Insomnia - Overt aggression | 0.005 | 0.009 | -0.015 - 0.023 | – | |
| Model 3 f | Total effect | 0.467 | 0.091 | 0.289 - 0.646 | – |
| Direct effect | 0.393 | 0.091 | 0.213 - 0.572 | 84.15 | |
| Indirect effect | 0.075 | 0.031 | 0.020 - 0.143 | 16.06 | |
| Emotional abuse - Alexithymia - Overt aggression | 0.042 | 0.022 | 0.004 - 0.089 | 8.99 | |
| Emotional abuse - Insomnia - Overt aggression | 0.022 | 0.020 | -0.010 - 0.067 | 4.71 | |
| Emotional abuse - Alexithymia - Insomnia - Overt aggression | 0.011 | 0.006 | 0.002 - 0.025 | 2.36 | |
| Model 4 g | Total effect | 0.533 | 0.142 | 0.253 - 0.813 | – |
| Direct effect | 0.470 | 0.139 | 0.196 - 0.745 | – | |
| Indirect effect | 0.062 | 0.045 | -0.024 - 0.156 | – | |
| Physical abuse - Alexithymia - Overt aggression | 0.002 | 0.029 | -0.060 - 0.056 | – | |
| Physical abuse - Insomnia - Overt aggression | 0.060 | 0.034 | 0.007 - 0.136 | – | |
| Physical abuse - Alexithymia - Insomnia - Overt aggression | 0.000 | 0.006 | -0.012 - 0.012 | – | |
| Model 5 h | Total effect | 0.291 | 0.086 | 0.122 - 0.461 | – |
| Direct effect | 0.270 | 0.083 | 0.105 - 0.434 | – | |
| Indirect effect | 0.022 | 0.028 | -0.032 - 0.079 | – | |
| Emotional neglect - Alexithymia - Overt aggression | 0.024 | 0.016 | -0.004 - 0.059 | – | |
| Emotional neglect - Insomnia - Overt aggression | -0.008 | 0.020 | -0.048 - 0.031 | – | |
| Emotional neglect - Alexithymia - Insomnia - Overt aggression | 0.007 | 0.005 | -0.001 - 0.017 | – | |
| Model 6 i | Total effect | 0.462 | 0.117 | 0.232 - 0.692 | – |
| Direct effect | 0.346 | 0.119 | 0.112 - 0.580 | 74.89 | |
| Indirect effect | 0.116 | 0.044 | 0.035 - 0.209 | 25.11 | |
| Physical neglect - Alexithymia - Overt aggression | 0.039 | 0.023 | -0.006 - 0.088 | 8.44 | |
| Physical neglect - Insomnia - Overt aggression | 0.071 | 0.035 | 0.008 - 0.147 | 15.37 | |
| Physical neglect - Alexithymia - Insomnia - Overt aggression | 0.006 | 0.005 | -0.002 - 0.018 | 1.30 |
Mediating effects of insomnia and alexithymia in the associations of childhood maltreatment and overt aggression.
CTQ, childhood trauma questionnaire.
SE, standard error; CI, confidence interval; Bolded P value: < 0.05.
, CTQ total score - Alexithymia/Insomnia - Overt aggression;
, Sexual abuse - Alexithymia/Insomnia - Overt aggression;
, Emotional abuse - Alexithymia/Insomnia - Overt aggression;
, Physical abuse - Alexithymia/Insomnia - Overt aggression;
, Emotional neglect - Alexithymia/Insomnia - Overt aggression;
, Physical neglect - Alexithymia/Insomnia - Overt aggression.
Figure 1

Direct and indirect relationship models of CTQ total score, alexithymia, insomnia on overt aggression. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Figure 2
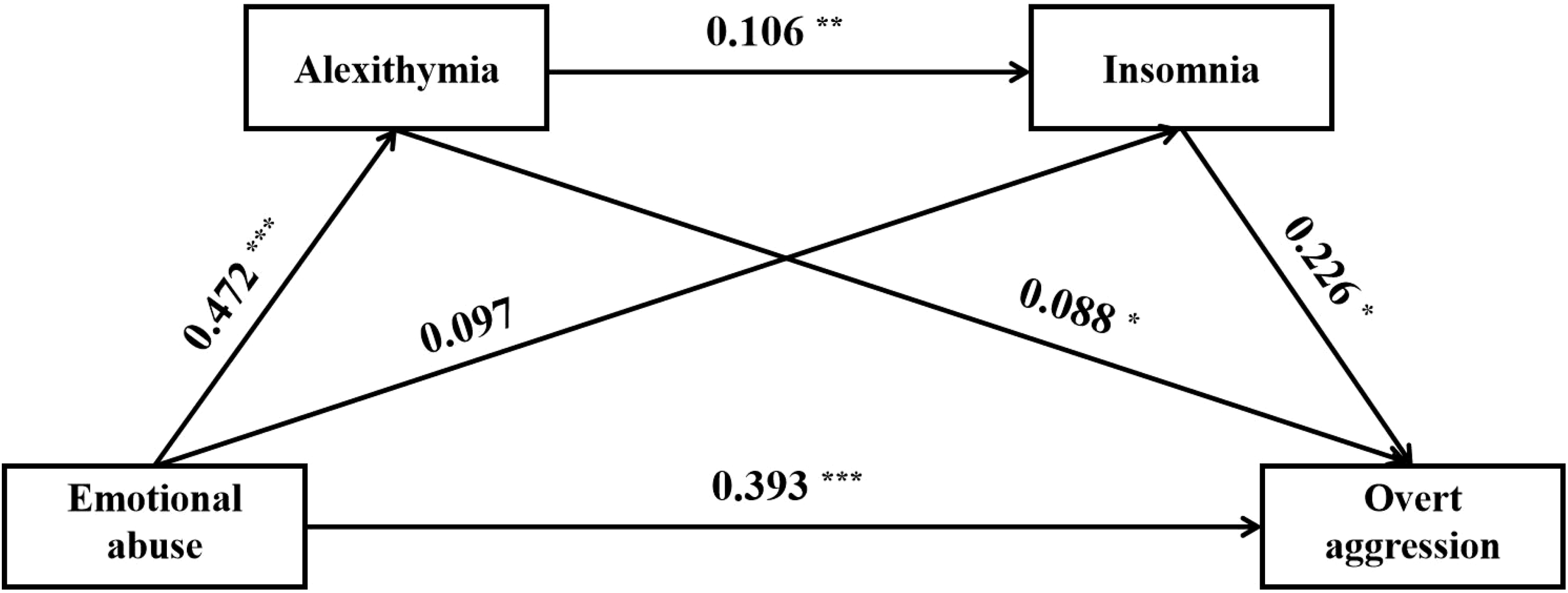
Direct and indirect relationship models of emotional abuse, insomnia, alexithymia on overt aggression. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Figure 3
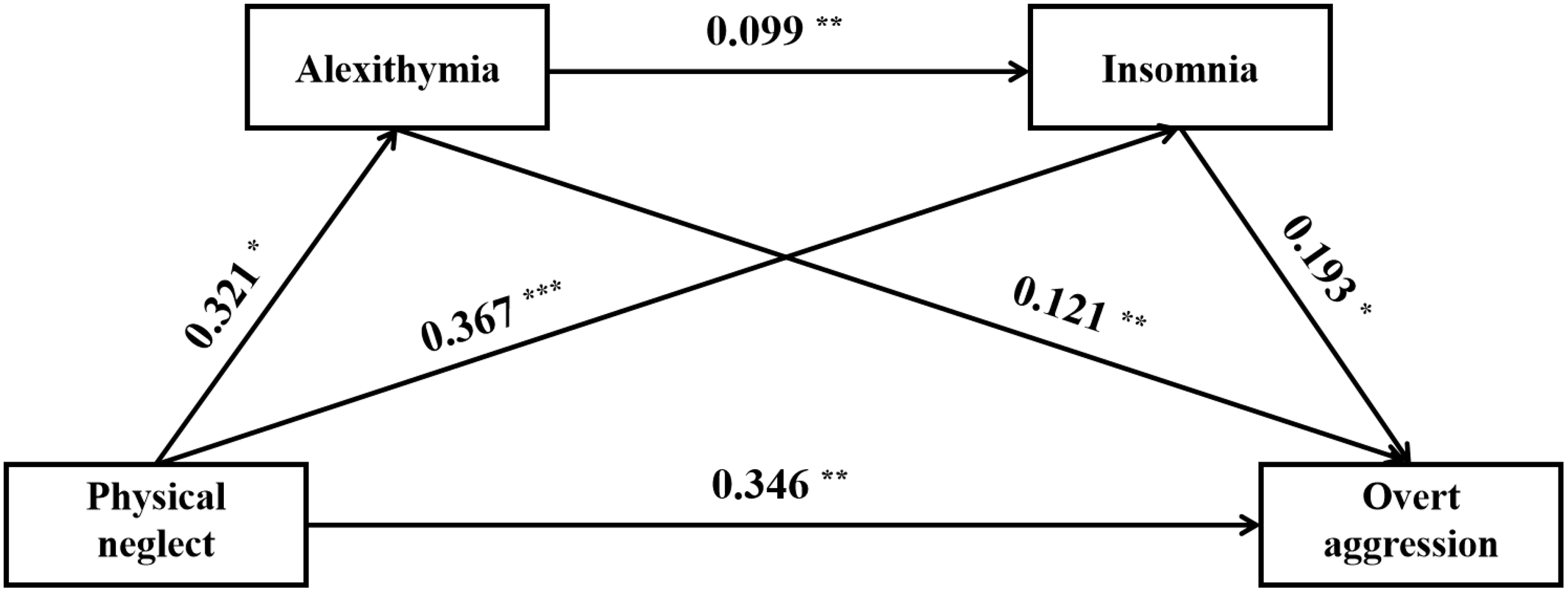
Direct and indirect relationship models of physical neglect, insomnia, alexithymia on overt aggression. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
4 Discussion
To our knowledge, this study was the first to examine the mediating roles of insomnia and alexithymia in the relationship between CM and overt aggression in adolescents with MDD. This finding enhanced our understanding of the underlying mechanisms of aggressive behaviors in this population and provided novel theoretical insights and directions for future clinical interventions and research.
In our study, the prevalence of overt aggression in adolescents with MDD was found to be 66.1%. This finding was consistent with previous research. For example, an epidemiological survey of adult patients with MDD reported that 58.7% exhibited aggressive behavior, which was strongly associated with higher depression severity and earlier age of onset (42). These observations suggested that aggression may be an important clinical feature of depression. Because of their immature psychological and cognitive development and limited self-regulation abilities, adolescents with MDD are more likely to exhibit aggressive behaviors (43). In addition, we found that the age of patients was negatively correlated with overt aggression. On the one hand, younger patients are more likely to exhibit aggressive behaviors because the brain regions responsible for emotion regulation and behavioral control, such as the prefrontal cortex, are not yet fully developed, and this underdevelopment makes it difficult for them to effectively inhibit impulsive behaviors (44). On the other hand, young patients often lack adequate psychological coping strategies and emotional expression abilities when facing depressive moods (45). As a result, they are more likely to express their distress and frustration through aggressive behaviors. In summary, overt aggression is more common in patients with MDD, particularly among adolescents. Therefore, this phenomenon warrants clinical attention, and further research into the assessment and mechanisms of aggressive behaviors in adolescents with MDD is needed.
Further analyses indicated that CM was a significant risk factor for the development of overt aggression in adolescents with MDD. Previous studies have established the strong and complex association between CM and aggression. For example, a study of Chinese adolescents found that CM has a bi-directional predictive relationship with aggression (46). Li et al.’s study based on resting-state functional magnetic resonance imaging also found that CM leads to aggressive behaviors by affecting functional connectivity between the default mode network (DMN), the cerebellar network (CON), and the dorsal attentional network (DAN) (15). Such close associations may involve complex mechanisms. On a biological level, studies have shown that CM may affect specific gene polymorphisms (e.g., the CREB1 rs4675690 T allele and the SIRT1 rs4746720 allele), which may in turn increase levels of aggression in adolescents by influencing neurobiological pathways (47, 48). A study of general adolescents also found that adverse childhood experiences may affect levels of cortisol and dehydroepiandrosterone (DHEA), which, in turn, may trigger a range of externalizing problems, such as aggressive behaviors and depression (49). Moreover, CM may also impair neuroplasticity and neurogenesis in brain circuits that regulate emotion and motivation, and this altered neurobiological basis may contribute to the increased risk of aggression in adolescents (21, 50). On a psychosocial level, Curtis et al. found that CM could influence aggressive behaviors by impairing an individual’s neurocognitive abilities (e.g., response inhibition) (51). Additionally, CM can increase the risk of aggressive behaviors in adolescents by promoting the development of specific personality traits (52, 53). A study of Chinese secondary school students found that borderline personality features were more pronounced in adolescents experiencing CM, and that these personality features were strongly associated with subsequent high levels of aggression (52). Li et al. revealed that CM significantly increased the risk of aggression in adolescents by promoting the development of callous traits (53). Additionally, another cross-sectional study conducted in China found that adolescents who had experienced childhood trauma exhibited poorer self-control, which significantly increased their susceptibility to aggressive behavior (54). Finally, of interest, the present study also found a more significant correlation between emotional abuse and overt aggression in adolescents with MDD. This finding may suggest that emotional abuse has a unique pathogenic mechanism in the development of adolescent aggression. For example, emotional abuse may more directly impair adolescents’ emotion regulation abilities and disrupt their interpersonal patterns (55, 56), thereby exacerbating the emergence of aggressive behaviors. However, this hypothesis still needs to be tested by further longitudinal studies to clarify the specific mechanisms of emotional abuse’s role in adolescent aggressive behaviors. In addition, other mediators may also play a bridging role between CM and aggression in adolescents with MDD, such as alexithymia and insomnia, which were explored in this study.
Alexithymia was shown to be a significant mediator between CM and overt aggression in adolescents with MDD in the present study. Indeed, the development of alexithymia is a long-term dynamic process whose origins can be traced back to childhood experiences, particularly those involving emotional neglect or trauma. Early adverse childhood experiences, such as emotional abuse, physical abuse, or neglect, can disrupt an individual’s normal emotional development and cognitive functioning, which can increase the risk of developing alexithymia (57, 58). For example, a prospective study in Finland found a significant correlation between adverse childhood experiences and the presence of alexithymia (59). And the association between alexithymia and aggression has also been supported by previous research. A study of young people found that alexithymia can significantly predict individuals’ aggressive behaviors (60). Individuals with alexithymia often have deficits in cognitive processing and emotion regulation, as evidenced by difficulties in recognizing and expressing their emotions, heightened reactivity to emotional stimuli, and a lack of effective emotion regulation strategies (20, 61), which may increase the risk of aggression. In addition, patients with MDD who have comorbid alexithymia are also likely to present with more severe psychopathological features, such as higher levels of anxiety, more frequent impulsive behaviors, and poorer social functioning (62, 63). These psychopathological traits not only exacerbate difficulties in emotion regulation, but also further weaken the individual’s ability to inhibit aggressive impulses, thereby contributing to the expression of aggressive behaviors in adolescents with MDD (64). Similarly, a survey of Chinese youths found that alexithymia mediated a positive association between CM and aggression (65), which further supports the findings of the present study. In conclusion, the results of the present study highlight the need to comprehensively consider the potential impact of alexithymia when intervening in adolescents’ aggressive behaviors and to develop targeted psychological interventions.
Also, the present study identified insomnia as another mediator of the link between CM and overt aggression. This finding was widely supported by existing studies. First, the association between CM and insomnia has been well established in several studies. A meta-analysis that included 26 studies noted the significant associations between CM and a range of sleep problems, including insomnia symptoms, shorter sleep duration and nightmares (66). On the one hand, adolescents experiencing CM often face many psychological stresses. For example, they may experience chronic high levels of stress and exhibit hypervigilance, anxiety, or depression, and these psychological states can significantly disrupt normal sleep rhythms, thereby increasing the risk of insomnia (67, 68). On the other hand, CM has been shown to affect the balance of neurotransmitters, such as decreasing the levels of serotonin and dopamine, which play a key role in regulating sleep-wake cycles and promoting restful sleep (69, 70). In our study, insomnia was shown to be an independent risk factor for overt aggression in adolescents with MDD, which is highly consistent with previous research. For example, a longitudinal study found that the persistence of insomnia symptoms significantly increased the likelihood of individuals developing aggressive behaviors (71). In addition, neuroimaging-based studies have further revealed the underlying neurobiological mechanisms between insomnia and aggressive behaviors. It has been found that adolescents with MDD who suffer from insomnia tend to have altered functional connectivity between the prefrontal cortex and the amygdala (72). The prefrontal cortex plays a key role in emotion regulation and behavioral inhibition, while the amygdala is strongly associated with the intensity of emotional responses (73). Abnormalities in this functional connectivity may lead to impaired emotion regulation and increased impulsive behavior, thereby increasing an individual’s susceptibility to aggressive behaviors (71).
Finally, and more critically, the present study initially revealed the chain-mediated role of narrative disorders and insomnia in the association between CM and overt aggression. This chained pathway is highly compatible with theoretical models of emotion regulation (74). Specifically, individuals who experience CM tend to have significantly weakened emotion regulation, which not only increases the risk of developing alexithymia but also exacerbates the negative accumulation of emotions, making them more susceptible to insomnia during times of stress (18, 19). Insomnia, in turn, further elevates the probability of overt aggression through the neuropsychological mechanisms described above. This finding provides new insights into the complex relationship between CM and overt aggression in patients with MDD. However, when analyzing specific sub-dimensions of CM, the results showed that only emotional abuse and physical neglect were statistically significant in mediating the effects. This finding suggested that emotional abuse and physical neglect may have a more significant impact on individuals, while the roles of other sub-dimensions may be relatively minor or not yet fully revealed. In addition, other dimensions of CM may only influence overt aggression in adolescents with MDD through a single pathway (e.g., alexithymia or insomnia). For example, in Model 4 of the present study, the mediating pathway from physical abuse to insomnia to overt aggression was found to be statistically significant, even though the overall indirect effect did not reach statistical significance. However, these findings should be interpreted with caution due to the limited number of relevant studies and the relatively small sample size of this study. Further in-depth explorations are needed in the future to more fully elucidate the mechanisms of action of these sub-dimensions and their long-term effects on individual aggression.
The limitations of our study were as follows: (1) The cross-sectional study design did not allow for causal inferences. Future studies should explore the mediating roles of insomnia and alexithymia in the relationship between CM and overt aggression using a longitudinal design. (2) The study was conducted in a single hospital in Anhui Province, China, with a small sample size, limiting the generalizability of the results. It is recommended that subsequent large-sample surveys be conducted in different regions and cultural contexts to validate the robustness of the mediation model. Additionally, future studies could consider more detailed stratified analyses of the sample based on factors such as patients’ sex, age, and disease severity to explore their potential impact. (3) Some data were based on patients’ self-reports, which may introduce recall bias, and the findings should therefore be interpreted with caution. (4) There may be other unmeasured variables that mediate the relationship between CM and overt aggression, and their omission may affect the accurate estimation of the mediating effect.
5 Conclusion
In this study, adolescents with MDD were found to exhibit a higher risk of overt aggression, which was significantly associated with CM, insomnia, and alexithymia. Further analyses showed that alexithymia and insomnia mediated the association between CM and overt aggression. Therefore, in clinical practice, clinicians and parents should pay attention to the adverse childhood experiences of adolescents with MDD and implement timely and targeted psychological interventions to prevent the development of alexithymia and insomnia. Through multidimensional interventions, the risk of overt aggression in adolescents with MDD may be reduced, and their psychological health and behavioral performance may be improved.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Bozhou People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
JW: Conceptualization, Investigation, Methodology, Formal Analysis, Project administration, Funding acquisition, Writing – original draft, Data curation. LL: Methodology, Formal Analysis, Data curation, Writing – original draft, Conceptualization, Investigation. SZ: Writing – original draft, Formal Analysis, Methodology, Investigation, Data curation, Conceptualization. LZ: Conceptualization, Investigation, Writing – review & editing, Methodology, Data curation. QW: Writing – review & editing, Data curation, Investigation, Methodology, Conceptualization. TS: Data curation, Methodology, Conceptualization, Writing – review & editing, Investigation. NZ: Investigation, Writing – review & editing, Conceptualization, Methodology, Data curation. XW: Investigation, Conceptualization, Writing – review & editing, Data curation, Methodology. LX: Methodology, Conceptualization, Data curation, Writing – review & editing, Formal Analysis, Supervision, Validation. FZ: Conceptualization, Investigation, Project administration, Supervision, Writing – review & editing, Data curation, Methodology, Formal Analysis.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by Bozhou Health Research Project (Grant No. bzwj2024b020) and Bozhou Children’s Hospital 2024 Hospital-level Research Project (Grant No. 2024LQN-02).
Acknowledgments
We sincerely thank all the study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Correction note
A correction has been made to this article. Details can be found at: 10.3389/fpsyt.2025.1734316.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Thapar A Collishaw S Pine DS Thapar AK . Depression in adolescence. Lancet (London England). (2012) 379:1056–67. doi: 10.1016/S0140-6736(11)60871-4
2
Daly M . Prevalence of depression among adolescents in the U.S. From 2009 to 2019: analysis of trends by sex, race/ethnicity, and income. J Adolesc Health: Off Publ Soc For Adolesc Med. (2022) 70:496–9. doi: 10.1016/j.jadohealth.2021.08.026
3
Li F Cui Y Li Y Guo L Ke X Liu J et al . Prevalence of mental disorders in school children and adolescents in China: diagnostic data from detailed clinical assessments of 17,524 individuals. J Child Psychol Psychiatry Allied Disciplines. (2022) 63:34–46. doi: 10.1111/jcpp.13445
4
Dong W Liu Y Bai R Zhang L Zhou M . The prevalence and associated disability burden of mental disorders in children and adolescents in China: a systematic analysis of data from the Global Burden of Disease Study. Lancet Regional Health Western Pacific. (2025) 55:101486. doi: 10.1016/j.lanwpc.2025.101486
5
Knox M King C Hanna GL Logan D Ghaziuddin N . Aggressive behavior in clinically depressed adolescents. J Am Acad Child Adolesc Psychiatry. (2000) 39:611–8. doi: 10.1097/00004583-200005000-00015
6
Coryell W Wilcox H Evans SJ Pandey GN Jones-Brando L Dickerson F et al . Aggression, impulsivity and inflammatory markers as risk factors for suicidal behavior. J Psychiatr Res. (2018) 106:38–42. doi: 10.1016/j.jpsychires.2018.09.004
7
Oquendo MA Galfalvy H Russo S Ellis SP Grunebaum MF Burke A et al . Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am J Psychiatry. (2004) 161:1433–41. doi: 10.1176/appi.ajp.161.8.1433
8
Teicher MH Gordon JB Nemeroff CB . Recognizing the importance of childhood maltreatment as a critical factor in psychiatric diagnoses, treatment, research, prevention, and education. Mol Psychiatry. (2022) 27:1331–8. doi: 10.1038/s41380-021-01367-9
9
Cen Y He J Zhong Y Zhou J Zeng J Huang G et al . The mediating role of sleep problems and depressed mood between psychological abuse/neglect and suicidal ideation in adolescent childhood: a multicentred, large sample survey in Western China. BMC Psychiatry. (2024) 24:64. doi: 10.1186/s12888-024-05503-x
10
Li X Wang X Sun L Hu Y Xia L Wang S et al . Associations between childhood maltreatment and suicidal ideation in depressed adolescents: The mediating effect of alexithymia and insomnia. Child Abuse Negl. (2023) 135:105990. doi: 10.1016/j.chiabu.2022.105990
11
Hovens JG Giltay EJ van Hemert AM Penninx BW . Childhood maltreatment and the course of depressive and anxiety disorders: the contribution of personality characteristics. Depression Anxiety. (2016) 33:27–34. doi: 10.1002/da.2016.33.issue-1
12
Dong C Wang Z Jia F Tian H Zhang Y Liu H et al . Gender differences in the association between childhood maltreatment and the onset of major depressive disorder. J Affect Disord. (2024) 351:111–9. doi: 10.1016/j.jad.2024.01.249
13
Medeiros GC Prueitt WL Minhajuddin A Patel SS Czysz AH Furman JL et al . Childhood maltreatment and impact on clinical features of major depression in adults. Psychiatry Res. (2020) 293:113412. doi: 10.1016/j.psychres.2020.113412
14
Liu F Yu T Xu Y Che H . Psychological maltreatment and aggression in preadolescence: Roles of temperamental effortful control and maladaptive cognitive emotion regulation strategies. Child Abuse Negl. (2023) 135:105996. doi: 10.1016/j.chiabu.2022.105996
15
Li Y Zhang T Hou X Chen X Mao Y . Common and distinct neural underpinnings of the association between childhood maltreatment and depression and aggressive behavior. BMC Psychiatry. (2025) 25:43. doi: 10.1186/s12888-025-06485-0
16
Taylor GJ . Alexithymia: concept, measurement, and implications for treatment. Am J Psychiatry. (1984) 141:725–32. doi: 10.1176/ajp.141.6.725
17
Li S Zhang B Guo Y Zhang J . The association between alexithymia as assessed by the 20-item Toronto Alexithymia Scale and depression: A meta-analysis. Psychiatry Res. (2015) 227:1–9. doi: 10.1016/j.psychres.2015.02.006
18
Chung MC Chen ZS . The interrelationship between child abuse, emotional processing difficulties, alexithymia and psychological symptoms among chinese adolescents. J Trauma Dissociation: Off J Int Soc For Study Dissociation (ISSD). (2021) 22:107–21. doi: 10.1080/15299732.2020.1788689
19
Rinne-Albers MA Pannekoek JN van Hoof MJ van Lang ND Lamers-Winkelman F Rombouts SA et al . Anterior cingulate cortex grey matter volume abnormalities in adolescents with PTSD after childhood sexual abuse. Eur Neuropsychopharmacology: J Eur Coll Neuropsychopharmacol. (2017) 27:1163–71. doi: 10.1016/j.euroneuro.2017.08.432
20
Preece DA Mehta A Petrova K Sikka P Bjureberg J Becerra R et al . Alexithymia and emotion regulation. J Affect Disord. (2023) 324:232–8. doi: 10.1016/j.jad.2022.12.065
21
Lee V Hoaken PNS . Cognition, emotion, and neurobiological development: mediating the relation between maltreatment and aggression. Child Maltreatment. (2007) 12:281–98. doi: 10.1177/1077559507303778
22
Schønning V Hysing M Dovran A Nilsen SA Hafstad GS Vedaa Ø et al . Sleep and childhood maltreatment: A matched-control study of sleep characteristics in Norwegian 16-19-year-olds. Scandinavian J Psychol. (2024) 65:119–28. doi: 10.1111/sjop.12960
23
Zhou SJ Wang LL Wang TT Wang JQ Chen JX . Associations between experienced aggression, poor sleep, and suicide risk among Chinese adolescents. Sleep. (2022) 45:zsac048. doi: 10.1093/sleep/zsac048
24
Vanek J Prasko J Genzor S Ociskova M Holubova M Sova M et al . Insomnia and emotion regulation. Neuro Endocrinol Lett. (2020) 41:255–69. doi: 10.1146/annurev-clinpsy-032814-112739
25
Sisman FN Basakci D Ergun A . The relationship between insomnia and trait anger and anger expression among adolescents. J Child Adolesc Psychiatr Nursing: Off Publ Assoc Child Adolesc Psychiatr Nurses Inc. (2021) 34:50–6. doi: 10.1111/jcap.12294
26
Van Veen MM Lancel M Beijer E Remmelzwaal S Rutters F . The association of sleep quality and aggression: A systematic review and meta-analysis of observational studies. Sleep Med Rev. (2021) 59:101500. doi: 10.1016/j.smrv.2021.101500
27
Li M Yuan Y Cheng X Wang Y Xu Z . Childhood maltreatment and insomnia in college students: The role of alexithymia and psychological distress. Acta Psychologica. (2024) 243:104149. doi: 10.1016/j.actpsy.2024.104149
28
Kay SR Wolkenfeld F Murrill LM . Profiles of aggression among psychiatric patients. I. Nature and prevalence. J Nervous Ment Dis. (1988) 176:539–46. doi: 10.1097/00005053-198809000-00007
29
Xu C Wang F Huang Q Lyu D Wu C Cao T et al . Association between overt aggression and anhedonia in patients with major depressive disorder during the acute phase. J Psychiatr Res. (2023) 165:41–7. doi: 10.1016/j.jpsychires.2023.07.013
30
Simonetti A Kurian S Saxena J Verrico CD Soares JC Sani G et al . Cognitive correlates of impulsive aggression in youth with pediatric bipolar disorder and bipolar offspring. J Affect Disord. (2021) 287:387–96. doi: 10.1016/j.jad.2021.03.044
31
Liu C Ye X Chen M . Sertraline medications plus dialectical behavior therapy for depressed adolescents with nonsuicidal self-injury behaviors. Suicide Life-threatening Behav. (2025) 55:e13132. doi: 10.1111/sltb.13132
32
Zimmerman M Martinez JH Young D Chelminski I Dalrymple K . Severity classification on the hamilton depression rating scale. J Affect Disord. (2013) 150:384–8. doi: 10.1016/j.jad.2013.04.028
33
Gu LM Deng CJ Shang DW Huang SQ Nie S Yang XH et al . Efficacy and safety of low-frequency repetitive transcranial magnetic stimulation in adolescents with first-episode major depressive disorder: A randomized, double-blind, sham-controlled pilot trial. J Affect Disord. (2025) 370:190–7. doi: 10.1016/j.jad.2024.11.001
34
Fu YJ Liu X Wang XY Li X Dai LQ Ren WY et al . Abnormal volumetric brain morphometry and cerebral blood flow in adolescents with depression. World J Psychiatry. (2023) 13:386–96. doi: 10.5498/wjp.v13.i6.386
35
Bernstein DP Stein JA Newcomb MD Walker E Pogge D Ahluvalia T et al . Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/S0145-2134(02)00541-0
36
Wang X Ding F Cheng C He J Wang X Yao S . Psychometric properties and measurement invariance of the childhood trauma questionnaire (Short form) across genders, time points and presence of major depressive disorder among chinese adolescents. Front In Psychol. (2022) 13:816051. doi: 10.3389/fpsyg.2022.816051
37
Bastien CH Vallières A Morin CM . Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
38
Chung KF Kan KKK Yeung WF . Assessing insomnia in adolescents: comparison of Insomnia Severity Index, Athens Insomnia Scale and Sleep Quality Index. Sleep Med. (2011) 12:463–70. doi: 10.1016/j.sleep.2010.09.019
39
Bagby RM Parker JD Taylor GJ . The twenty-item toronto alexithymia scale–I. Item selection cross-validation factor Struct J Psychosomatic Res. (1994) 38:23–32. 10.1016/0022-3999(94)90005-1
40
Zhang B Zhang W Sun L Jiang C Zhou Y He K . Relationship between alexithymia, loneliness, resilience and non-suicidal self-injury in adolescents with depression: a multi-center study. BMC Psychiatry. (2023) 23:445. doi: 10.1186/s12888-023-04938-y
41
Ling Y Zeng Y Yuan H Zhong M . Cross-cultural validation of the 20-item Toronto Alexithymia Scale in Chinese adolescents. J Psychiatr Ment Health Nurs. (2016) 23:179–87. doi: 10.1111/jpm.2016.23.issue-3pt4
42
Liu Q Cole DA . Aggressive outbursts among adults with major depressive disorder: Results from the Collaborative Psychiatric Epidemiological Surveys. J Psychiatr Res. (2021) 135:325–31. doi: 10.1016/j.jpsychires.2021.01.040
43
Harmon SL Stephens HF Repper KK Driscoll KA Kistner JA . Children’s rumination to sadness and anger: implications for the development of depression and aggression. J Clin Child Adolesc Psychology: Off J For Soc Clin Child Adolesc Psychology Am psychol Association Division. (2019) 48:622–32. doi: 10.1080/15374416.2017.1359788
44
Dahl RE . Adolescent brain development: a period of vulnerabilities and opportunities. Keynote address. Ann New York Acad Sci. (2004) 1021:1–22. doi: 10.1196/annals.1308.001
45
Cole PM Luby J Sullivan MW . Emotions and the development of childhood depression: bridging the gap. Child Dev Perspect. (2008) 2:141–8. doi: 10.1111/j.1750-8606.2008.00056.x
46
Yang J Huebner ES Tian L . Transactional processes among childhood maltreatment, self-control and aggression in early adolescence: disentangling between- and within-person associations. Res On Child Adolesc Psychopathol. (2022) 50:321–34. doi: 10.1007/s10802-021-00863-4
47
Zhang Y Kang C Yang H Yang M Wei S Wang Y et al . Gene-environment interactions between CREB1 and childhood maltreatment on aggression among male Chinese adolescents. Sci Rep. (2022) 12:1326. doi: 10.1038/s41598-022-05137-7
48
Wang M Peng C Chang H Yu M Rong F Yu Y . Interaction between Sirtuin 1 (SIRT1) polymorphisms and childhood maltreatment on aggression risk in Chinese male adolescents. J Affect Disord. (2022) 309:37–44. doi: 10.1016/j.jad.2022.04.063
49
Lee Y Donahue GZ Buthmann JL Uy JP Gotlib IH . The cortisol/DHEA ratio mediates the association between early life stress and externalizing problems in adolescent boys. Psychoneuroendocrinology. (2024) 165:107034. doi: 10.1016/j.psyneuen.2024.107034
50
Bounoua N Miglin R Spielberg JM Sadeh N . Childhood assaultive trauma and physical aggression: Links with cortical thickness in prefrontal and occipital cortices. NeuroImage. Clin. (2020) 27:102321. doi: 10.1016/j.nicl.2020.102321
51
Curtis A Harries T Skvarc D Guala T Enticott PG Miller PG . Childhood maltreatment and adult aggression: The moderating role of neurocognitive ability and substance use. Child Abuse Negl. (2024) 158:107094. doi: 10.1016/j.chiabu.2024.107094
52
Li Y Huang X Yuan M Chang J Zhang T Wang G et al . Childhood maltreatment and homicidal ideation among Chinese early adolescents: The serial mediating role of borderline personality features and aggression. Aggressive Behav. (2023) 49:536–46. doi: 10.1002/ab.22091
53
Li W Yang J Gao L Wang X . Childhood maltreatment and adolescents’ Aggression: A moderated mediation model of callous-unemotional traits and friendship quality. Child Maltreatment. (2022) 27:683–92. doi: 10.1177/10775595211046550
54
Xie Q Bi T Du Y Kou H Yang B . Childhood maltreatment is associated with aggression among male juvenile delinquents in China: the mediating effects of callous-unemotional traits and self-control. Front In Psychol. (2020) 11:1373. doi: 10.3389/fpsyg.2020.01373
55
Kim SG Weissman DG Sheridan MA McLaughlin KA . Child abuse and automatic emotion regulation in children and adolescents. Dev Psychopathol. (2023) 35:157–67. doi: 10.1017/S0954579421000663
56
Hernandez EM Trout ZM Liu RT . Vulnerability-specific stress generation: Childhood emotional abuse and the mediating role of depressogenic interpersonal processes. Child Abuse Negl. (2016) 62:132–41. doi: 10.1016/j.chiabu.2016.10.019
57
Khan AN Jaffee SR . Alexithymia in individuals maltreated as children and adolescents: a meta-analysis. J Child Psychol Psychiatry Allied Disciplines. (2022) 63:963–72. doi: 10.1111/jcpp.13616
58
Jaffee SR . Child maltreatment and risk for psychopathology in childhood and adulthood. Annu Rev Clin Psychol. (2017) 13:525–51. doi: 10.1146/annurev-clinpsy-032816-045005
59
Salokangas RKR From T Salokangas HRW Lehtoranta L Suvisaari J Koskinen S et al . Effects of childhood adversities on alexithymia features vary between sexes. Results of a prospective population study. Eur J Psychotraumatol. (2024) 15:2407256. doi: 10.1080/20008066.2024.2407256
60
Hahn AM Simons RM Simons JS Welker LE . Prediction of verbal and physical aggression among young adults: A path analysis of alexithymia, impulsivity, and aggression. Psychiatry Res. (2019) 273:653–6. doi: 10.1016/j.psychres.2019.01.099
61
Chen J Xu T Jing J Chan RC . Alexithymia and emotional regulation: A cluster analytical approach. BMC Psychiatry. (2011) 11:33. doi: 10.1186/1471-244X-11-33
62
Preece DA Mehta A Petrova K Sikka P Pemberton E Gross JJ . Alexithymia profiles and depression, anxiety, and stress. J Affect Disord. (2024) 357:116–25. doi: 10.1016/j.jad.2024.02.071
63
Celikel FC Kose S Erkorkmaz U Sayar K Cumurcu BE Cloninger CR . Alexithymia and temperament and character model of personality in patients with major depressive disorder. Compr Psychiatry. (2010) 51:64–70. doi: 10.1016/j.comppsych.2009.02.004
64
Velotti P Garofalo C Petrocchi C Cavallo F Popolo R Dimaggio G . Alexithymia, emotion dysregulation, impulsivity and aggression: A multiple mediation model. Psychiatry Res. (2016) 237:296–303. doi: 10.1016/j.psychres.2016.01.025
65
Zhou J Wei M Xie Q . Childhood maltreatment and aggressive behavior among college students: a serial mediation model of authenticity and alexithymia. Front In Psychiatry. (2024) 15:1478127. doi: 10.3389/fpsyt.2024.1478127
66
Schønning V Sivertsen B Hysing M Dovran A Askeland KG . Childhood maltreatment and sleep in children and adolescents: A systematic review and meta-analysis. Sleep Med Rev. (2022) 63:101617. doi: 10.1016/j.smrv.2022.101617
67
Agorastos A Olff M . Traumatic stress and the circadian system: neurobiology, timing and treatment of posttraumatic chronodisruption. Eur J Psychotraumatol. (2020) 11:1833644. doi: 10.1080/20008198.2020.1833644
68
Trompeter N Testa A Raney JH Jackson DB Al-Shoaibi AAA Ganson KT et al . The association between adverse childhood experiences (ACEs), bullying victimization, and internalizing and externalizing problems among early adolescents: examining cumulative and interactive associations. J Youth Adolescence. (2024) 53:744–52. doi: 10.1007/s10964-023-01907-2
69
Cicchetti D Rogosch FA . Gene × Environment interaction and resilience: effects of child maltreatment and serotonin, corticotropin releasing hormone, dopamine, and oxytocin genes. Dev Psychopathol. (2012) 24:411–27. doi: 10.1017/S0954579412000077
70
Monti JM . Serotonin control of sleep-wake behavior. Sleep Med Rev. (2011) 15:269–81. doi: 10.1016/j.smrv.2010.11.003
71
Zhang H Lei X . Effect of subjective sleep quality on aggression: A two-year longitudinal and fMRI pilot study. Biol Psychol. (2023) 176:108454. doi: 10.1016/j.biopsycho.2022.108454
72
Bao W Gao Y Feng R Li X Li H Cao L et al . Abnormal intrinsic functional network connectivity in adolescent major depressive disorder related to severity of insomnia. Prog In Neuropsychopharmacol Biol Psychiatry. (2025) 138:111357. doi: 10.1016/j.pnpbp.2025.111357
73
Andrewes DG Jenkins LM . The role of the amygdala and the ventromedial prefrontal cortex in emotional regulation: implications for post-traumatic stress disorder. Neuropsychol Rev. (2019) 29:220–43. doi: 10.1007/s11065-019-09398-4
74
Cole PM Michel MK Teti LO . The development of emotion regulation and dysregulation: a clinical perspective. Monogr Soc For Res In Child Dev. (1994) 59:73–100. doi: 10.1111/j.1540-5834.1994.tb01278.x
Summary
Keywords
overt aggression, childhood maltreatment, insomnia, alexithymia, adolescents, major depressive disorder
Citation
Wang J, Liu L, Zhou S, Zhao L, Wu Q, Sun T, Zhang N, Wei X, Xia L and Zhao F (2025) Associations between childhood maltreatment and overt aggression in depressed adolescents: the mediating effect of alexithymia and insomnia. Front. Psychiatry 16:1619353. doi: 10.3389/fpsyt.2025.1619353
Received
28 April 2025
Accepted
09 June 2025
Published
24 June 2025
Corrected
20 November 2025
Volume
16 - 2025
Edited by
Luca Steardo Jr., University Magna Graecia of Catanzaro, Italy
Reviewed by
Yingyan Zhong, Shanghai Jiao Tong University, China
Zhengqian Yang, Beijing Normal University, China
Updates
Copyright
© 2025 Wang, Liu, Zhou, Zhao, Wu, Sun, Zhang, Wei, Xia and Zhao.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Zhao, 214918725@qq.com; Lei Xia, xialei@ahmu.edu.cn
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.