- 1Department of Occupational Therapy, Faculty of Social Welfare and Health Sciences, University of Haifa, Haifa, Israel
- 2Department of Psychiatry, Rambam Medical Center, Haifa, Israel
- 3Eye Movement Desensitization and Reprocessing (EMDR) Israel Association, Ra’anana, Israel
- 4Presence & Innovation Laboratory, Laval, France
Background: Executive function difficulties may be prevalent in people with PTSD, and they might negatively affect their behavior and daily functioning. However, knowledge about the implications of executive function deficits on daily functioning and the assessments that reflect functional limitations is limited. This study aimed to measure how executive function difficulties affect daily functioning in PTSD using ecologically valid assessments that imitate daily activities.
Methods: The participants were 66 individuals aged 18–65 years: 26 diagnosed with PTSD and 40 healthy controls. All participants completed a socio-demographic questionnaire, the Clinician-Administered PTSD Scale, and the Behavior Rating Inventory of Executive Functions—BRIEF-A, a self-reported tool to assess the impact of executive functions on daily activities. The participants also performed a virtual shopping activity to assess executive functions while performing in a daily activity using the Virtual Action Planning Supermarket (VAP-S 2), a novel, ecologically valid, performance-based tool.
Results: Difficulties in executive functions were significantly more prevalent in PTSD patients: the BRIEF-A reflected how executive function difficulties manifested in behavioral dysregulation, restricting daily functioning. The VAP-S 2 revealed difficulties in executive functions, expressed as higher impulsivity, lower strategy use, and decreased performance efficiency while shopping in the virtual supermarket. Correlations were found between BRIEF-A and VAP-S 2: more collisions and lower inhibition in VAP-S 2 were correlated with worse BRIEF-A scores. Difficulties in executive functions correlated with PTSD severity.
Conclusions: Executive function difficulties in PTSD may correlate with PTSD severity and restrict daily functioning. Therefore, executive functions in PTSD should be evaluated using ecologically valid assessments to illuminate the implications of real-life activities. VAP-S 2 uniquely enables an objective assessment of executive functions in real-life scenarios for PTSD, complementing self-report and enhancing the ecological validity of findings. It is recommended to combine self-reports that reflect the person’s authentic perspective with performance-based assessments, such as the VAP-S 2, to focus intervention on people’s real-life context and, by that, improve their function and well-being.
1 Introduction
Posttraumatic stress disorder (PTSD) may arise following a trauma resulting from experiencing, witnessing, or learning of actual or threatened death, serious injury, or sexual violence. The global PTSD prevalence is estimated at 4%–11%, with higher rates among veterans and high-risk professionals like emergency medical personnel and firefighters (1). PTSD is a chronic and progressive condition. The symptoms include re-experiencing, avoidance, and increased arousal, such as hypervigilance and irritability. As a result, PTSD interferes with daily activities, social and family relationships, work attendance, income, and lower educational and occupational success (1) and may significantly reduce people’s quality of life (QOL) (2, 3). Intervention efficiency is frequently limited, and the suffering that people with PTSD experience severely affects their life experience, inclusion in society, self-efficacy, and well-being (4, 5). Therefore, knowledge about PTSD symptoms and their implications on daily life should be elaborated to improve intervention success and enable people to experience better function and QOL. There is a need for new evaluation and intervention approaches that reflect the implications of PTSD symptoms on people’s daily lives (6, 7).
It is crucial to recognize the significant influence of executive functions (EF) on PTSD symptoms and their effects on daily life. EF difficulties in PTSD may contribute to the prevalent and dominant symptoms of PTSD—hyperarousability, attention deficits, and regulation difficulties (8–13). EF include planning, cognitive flexibility, problem-solving, inhibitory and emotional control, working memory, initiation, organization, self-monitoring, and task-monitoring (10, 14). Hence, EF allow the person to control goal-directed thoughts and behavior. EF are required to perform and participate in self-directed activities effectively, and they are essential for almost all activities in various daily situations and environments (15). In PTSD, the prevalent EF difficulties include, for example, difficulties in divided and selective attention, cognitive flexibility, inhibition, working memory, and planning (10, 14).
Studies also highlight that EF difficulties in PTSD correlate with PTSD severity (6) and enhance it—for example, impaired attention and inhibition contribute to hypervigilance and arousal symptoms (8, 16). EF difficulties in PTSD may also deteriorate emotional status (14), an individual’s healthcare maintenance, involvement in the intervention (14, 17, 18), and most importantly, reduced daily function and inclusion in society (2, 14, 17, 18).
According to the International Classification of Functioning, Disability, and Health (ICF) framework of the World Health Organization (19), the primary outcome measures of intervention efficiency are the person’s ability to perform daily activities and participate in life settings. However, evaluation and intervention for PTSD are mainly performed in clinical settings and focused on psychological and pharmacological treatment. Although intervention may reduce PTSD symptoms, in many cases, there is no complete remission (7, 20), and intervention does not fully address the implications on daily life functioning.
Based on the ICF and the significant negative impacts of EF difficulties on the daily function of people with PTSD (18, 21, 22), greater attention should be given to the role of EF in PTSD pathology and implications on daily function. Nonetheless, studies on EF difficulties data about EF in PTSD have been mainly gathered by neuropsychological evaluations with a focus on specific EF components, such as working memory, inhibition (for example, go/no-go) (18, 23), as measured in laboratory settings. Studies with ecologically valid assessments that reflect implications on daily life are scarce (24–26). Several studies on the daily activities of people with PTSD include self-report tools like the Canadian Occupational Performance Measure (COPM), Short Form (SF-36), and Activity Card Sort (ACS) (2, 25, 27). Self-report tools can increase the awareness of performance and challenges (28). However, they may not fully capture real-life task performance or daily functional impairments and may be influenced by self-awareness, mood, or bias. Applying ecological evaluation to assess the implications of EF in daily life may facilitate a deeper understanding of the daily challenges faced by PTSD patients, support the development of personalized interventions to enhance daily functioning in real-life settings, and elevate overall well-being.
One effective ecological platform for treating PTSD is virtual reality (VR), which is considered a highly motivated, safe, and readily available environment (29–32). Previous studies that employed VR, whether as an exposure therapy or evaluation tool, have primarily demonstrated VR’s utility in assessing and diagnosing PTSD symptoms (33, 34). Applying VR to PTSD assessment can be a convenient experience, reducing the sense of threat and optimizing emotional engagement for treatment with fewer side effects (33, 35, 36). However, studies utilizing VR to address everyday activities in PTSD, such as shopping or driving, as an objective and ecological tool are limited. Existing studies primarily focus on the relationship between performance and symptoms (24, 36, 37). Research lacks information about objective and ecological assessments that reflect how PTSD characteristics, such as difficulties in EF, affect daily activity performance.
The Virtual Action Planning Supermarket (VAP-S 2) (38) aims to answer this need and bridges the gap between laboratory assessment and daily life demands. VAP-S 2 offers an innovative, virtual, ecologically valid VR platform that simulates everyday activities, such as shopping, providing objective, performance-based data that have not previously been explored in PTSD populations. By combining BRIEF-A and VAP-S 2, this study captures both the perceived and actual executive function difficulties, thereby enhancing the ecological validity and clinical relevance of findings in PTSD.
The VAP-S 2 is used in rehabilitation to assess instrumental activities of daily living (IADL). It provides a comprehensive record of temporal and spatial aspects that reflect performance, while depending on EF, and therefore elucidates how EF support and interfere with activity performance (39, 40). Studies have shown its effectiveness in assessing performance differences in conditions like Parkinson’s disease, stroke, mild cognitive impairment, and schizophrenia (38, 41–43). These studies described the potential advantages of the VAP-S for rehabilitating people with deficits in EF (40). Nevertheless, studies utilizing the VAP-S 2 in PTSD are scarce.
This study aimed to elaborate on the knowledge about EF difficulties in people with PTSD and their implications on daily functioning. The specific aims are as follows: (1) to compare EF between people with PTSD and healthy controls using ecological evaluation tools: a self-report about EF in daily scenarios and the actual performance-based virtual assessment—the VAP-S 2 shopping task; among people with PTSD, (2) to examine the correlations between EF as measured in a self-report and the actual performance-based daily activities (shopping in a supermarket) using the virtual reality platform; and (3) to examine the relationship between EF and PTSD severity.
The study hypotheses are as follows: (1) EF difficulties would be significantly more prevalent in people with PTSD; among people with PTSD, (2) greater difficulties in EF would significantly correlate with lower efficiency while performing a shopping activity in the virtual supermarket; and (3) difficulties in EF would significantly correlate with symptom severity.
2 Method
2.1 Participants
This study included 66 participants aged 18–65 years: 26 participants with a diagnosis of PTSD who were outpatients in the Psychiatry Unit and 40 healthy participants recruited by snowball sampling and advertisements published in the same geographic area as the study group. The exclusion criteria (based on the medical records) were physical/psychiatric diagnosis that is not PTSD, severe health condition (such as cancer, cerebrovascular accident (CVA)), cognitive decline diagnosis, use of drugs/substances in the study group (except the use of prescription drugs for PTSD), and ADHD symptoms in the control group (a T-score higher than 65 in the CAARS™) (44). Because of the high prevalence of ADHD in people with PTSD, ADHD was not an exclusion criterion in the PTSD group (6, 45, 46). However, it was considered a covariate in the data analysis.
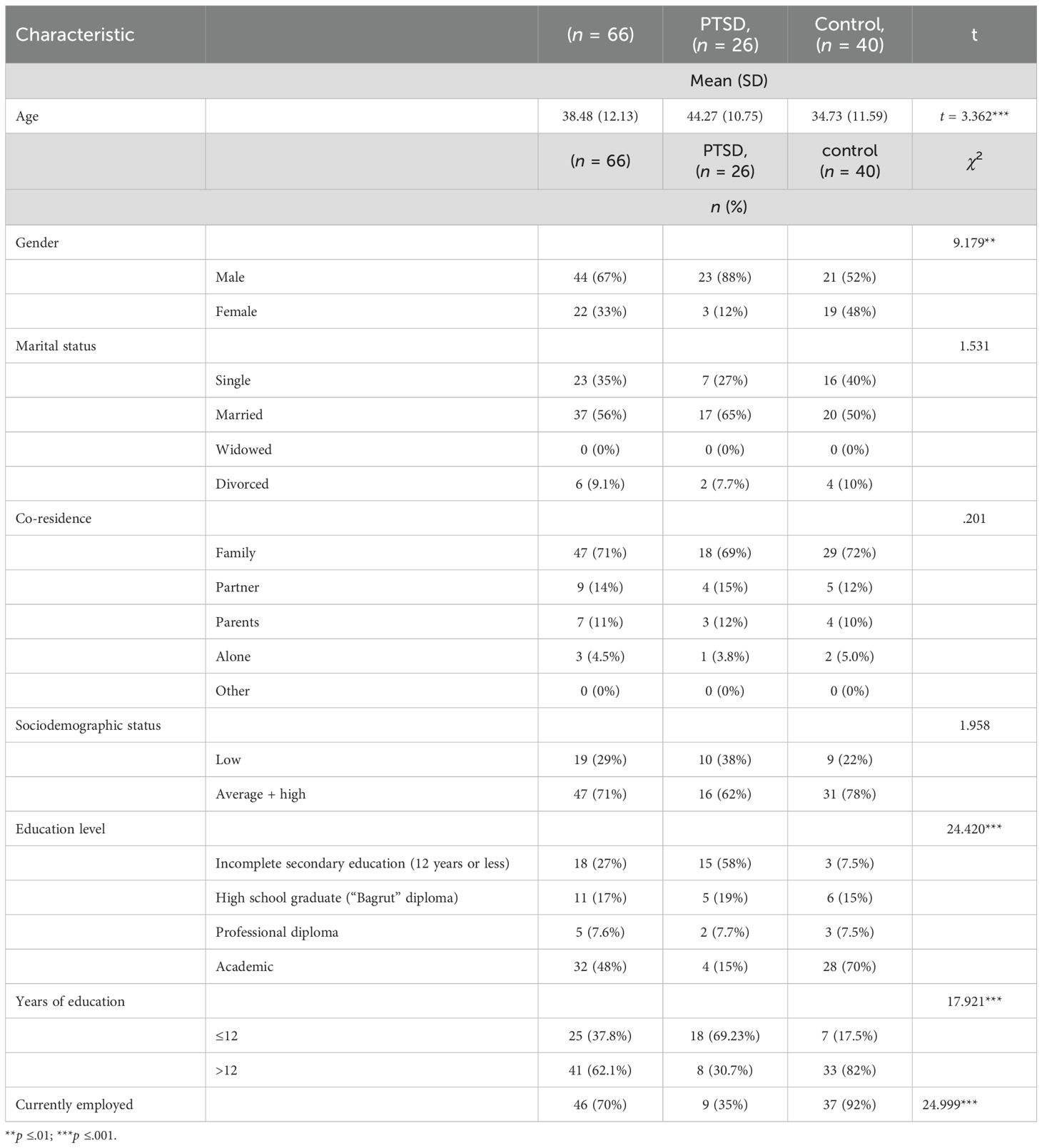
Table 1 presents the participants’ socio-demographic data. No significant differences were found between the groups regarding marital status, co-residence, and socio-demographic status (Table 1). However, there was a significant uneven gender distribution, with a higher prevalence of men in the study group. There were also differences between groups in age (the mean age of the control group is nearly a decade lower than that of the study group), in education (70% of the controls have an academic degree, compared to 15% among the study group), and in employment (only 27% of the study group participants are employed, compared to 95% of controls). It is worth noting that since the study group comprised chronic PTSD outpatients, the differences in education and employment are important as PTSD can impact participation in these areas (3, 47). Variances regarding age, gender, and education were considered in the statistical analysis process.
2.2 Instruments
The sociodemographic health questionnaire included information about participants’ health status, sociodemographic status, medications, and treatments.
The Conner’s Adult ADHD Rating Scales (CAARS-S:S) (44) is a self-report questionnaire designed to evaluate and screen ADHD in everyday life. The CAARS-S:S includes 26 items. For each item, the respondents indicate whether the described behavior occurred “never = 0”, “once in a while = 1”, “often = 2”, or “very frequently = 3” recently. Based on the sum of the scale, norms by age and gender (adjusted T-scores) were calculated. Higher scores indicate greater symptoms of ADHD. In this research, the CAARS-S:S was used to screen for symptoms of ADHD (when found, ADHD was held as a covariate). The cutoff for the abnormal ADHD performance range is higher than 65. Differences in ADHD symptoms between groups were taken into consideration in the statistical analysis.
The Clinician-Administered PTSD Scale CAPS (48) is the gold standard in PTSD assessment. The CAPS-5 is a 30-item structured interview that can be used to assess the DSM-5 PTSD symptoms. The questions cover the onset and duration of symptoms, subjective distress, impact on functioning, improvement since the last assessment, overall PTSD severity, and specifications for the dissociative subtype. A specific traumatic event must be identified for symptom inquiry, and standardized questions are used for each symptom. The full interview takes 45–60 min. In this study, the CAPS was administered by a trained psychiatric professional.
The Behavior Rating Inventory of Executive Function–Adult Version (BRIEF-A) (49) is a self-report questionnaire that was designed to assess EF in everyday life. The BRIEF-A includes 75 items. For each item, the respondents indicate whether the described behavior occurred “never = 1”, “sometimes = 2”, or “often = 3” in the past month. It includes nine clinical scales (inhibition, shift, emotional control, self-monitoring, initiation, working memory, plan, task-monitoring, organization) divided into two indices (the behavior regulation index (BRI) and metacognition index (MI)), which together make up the global executive composite (GEC) score. Adjusted T-scores (norms by age) are calculated based on the sum of each subscale and the general subscales. Higher scores indicate greater difficulties in EF. The abnormal EF performance range cutoff is a GEC score of 65 and above (49). The questionnaire was translated into Hebrew and adapted to fit the cultural context (50).
The Virtual Action Planning Supermarket (VAP-S 2) (38) is an upgraded version of the VAPS, with new graphic software that enables an adjustable environment designed to assess EF while shopping in a supermarket. The VAP-S 2 simulates a fully textured, medium-sized supermarket with multiple aisles. The task is to purchase seven items from a clearly marked products list displayed on the computer screen while facing multiple distractions commonly present in a daily environment, such as a supermarket (for example, a virtual buyer and randomized background noises) (51, 52). Then, the person has to proceed to the cashier’s desk and pay for the purchased products. A training task, similar but not identical to the test, is also available to enable users to become acquainted with the virtual environment. The VAP-S 2 yields 21 outcome measures: i.e., time (s) (initialization time, time to collect, checkout time, time to pay, exit time, stops time, session time), distance (in meters) (distance covered, distance in collecting, number of stops, collisions), and incorrect actions including checkout errors, other errors, perseverations, view the cart, need assistance, and intrusions (52). In this study, the outcome measures were conceptualized in terms of executive functioning into two categories, namely: (1) activity performance (mission completion)—measured by the number of purchased products and correct actions and (2) efficiency—the ability to complete the task with minimum expenditure of time and effort, measured by time, distance, and incorrect actions (25, 39). Additional outcome measures included impulsivity—a higher score indicated a higher level of impulsivity, strategy use (range 0–6)—a higher score indicated a greater ability to use strategies, and categorization (0/1/2 scores; categorizing the products that share a similar quality, e.g., banana and tomato are fruits)—a higher score indicates better categorization ability. Studies found that VAP-S 2 significantly differed between clinical populations and healthy adults (39, 40, 42). The VAP-S 2 displays culturally adjusted grocery items. The VAP-S 2 records the session and displays the task trajectory in upper or first-person view, providing an additional perspective of the track used during the activity.
2.3 Procedure
Ethical approval was obtained from the Helsinki Committee at Rambam Medical Center and the Institutional Review Board of the Faculty of Social Welfare and Health Sciences, University of Haifa. Data collection began on September 20, 2020 and continued until June 27, 2022. Individuals who were interested in participating in this study contacted the research coordinator. After approving the inclusion criteria, one or two meetings (in cases of fatigue impact) were scheduled in a quiet room at the psychiatric department (for the PTSD group) or at the participant’s home (for the control group). The participants signed a consent form in this meeting, completed the clinical questionnaires and the BRIEF-A, and performed the VAP-S 2.
2.4 Data analysis
Data were analyzed using SPSS (version 27). Descriptive statistics were performed to characterize the demographic data and the outcome measures. Tests of normality found a normal distribution in BRIEF-A scores, whereas the VAP-S 2 measures were not normally distributed. We used the MANCOVA test for the comparison hypotheses regarding the BRIEF-A while controlling for age, gender, and the number of education years as covariates. The effect size was determined according to Becker (53) and Richardson (53, 54). For the VAP-S 2 measures, we used the Mann–Whitney test. The correlations were examined using Pearson’s and Spearman’s correlation tests while controlling for the ADHD index and the symptoms’ severity variances. Due to multiple comparisons, the significance level was adjusted accordingly, and the tests were corrected for all pairwise comparisons using the Bonferroni correction. This resulted in a corrected significance threshold of p < 0.005 for the BRIEF-A analysis (MANCOVA test) and p < 0.004 for the VAP-S 2 analysis (Mann–Whitney test). This correction controls the family-wise error rate, reducing the risk of false positives that can occur when conducting multiple statistical tests.
3 Results
3.1 Participants’ clinical profile in the PTSD group
Based on the CAPS measure, 84.6% of the participants reported severe PTSD symptoms. Additionally, 87.5% reported severe symptoms in cluster B (intrusive thoughts and re-experiencing), 95.8% in cluster C (avoidance), 91.7% in cluster D (negative alteration in cognitions and mood), and 66.66% in cluster E (arousability). The most prevalent trauma type in the study group was war-related PTSD—including cases among veterans and combatants—accounting for 46% of the participants (Table 2a).
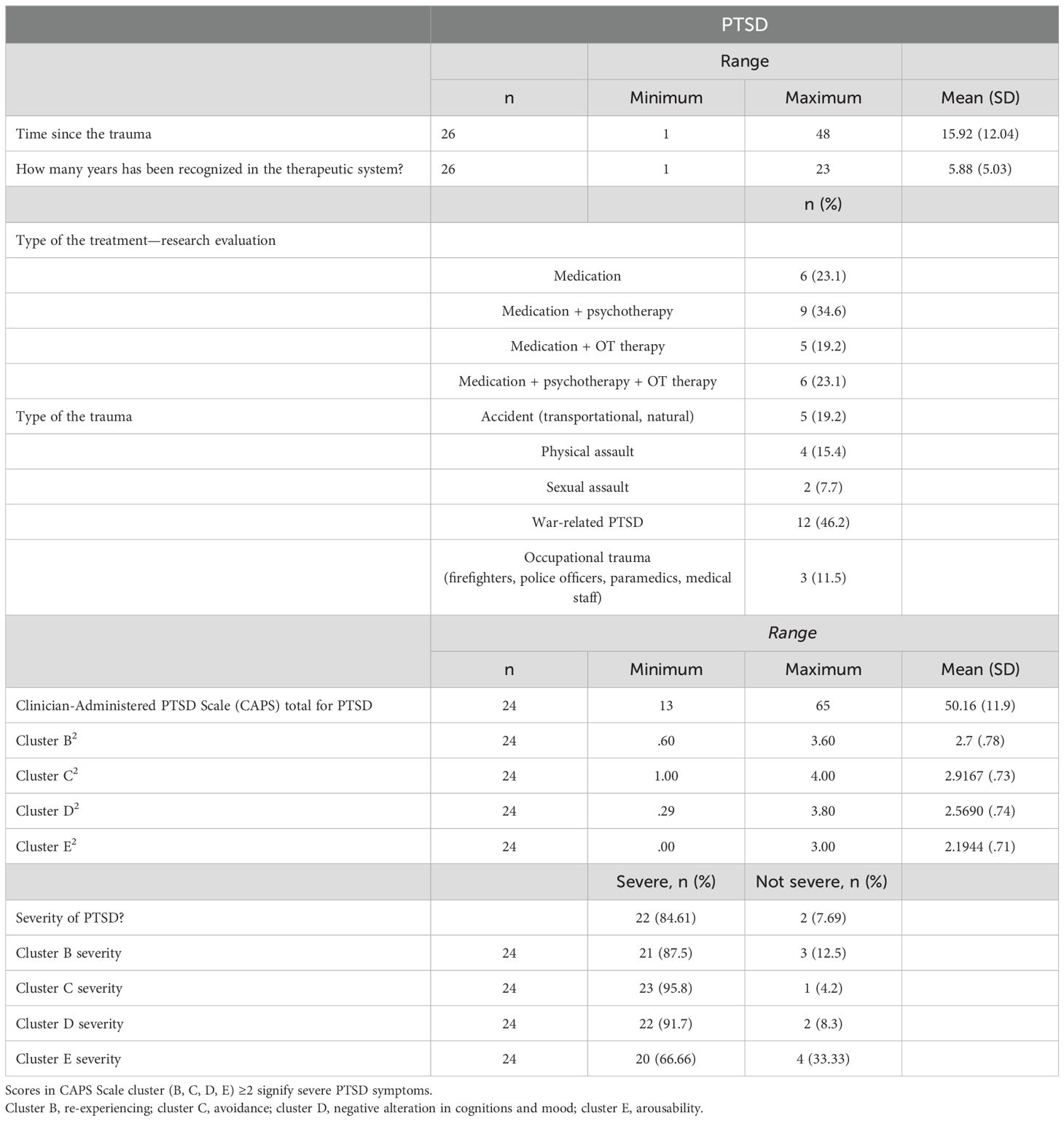
Table 2a. Descriptive statistics, means, and standard deviations of the characteristics of the PTSD group.
Conner’s ADHD index indicated a significant difference between the groups, with a higher prevalence of ADHD symptoms in the PTSD group (about 1.5 times higher than among the control group). The participants in the control group had normal range scores in Conner’s ADHD index test (Table 2b).
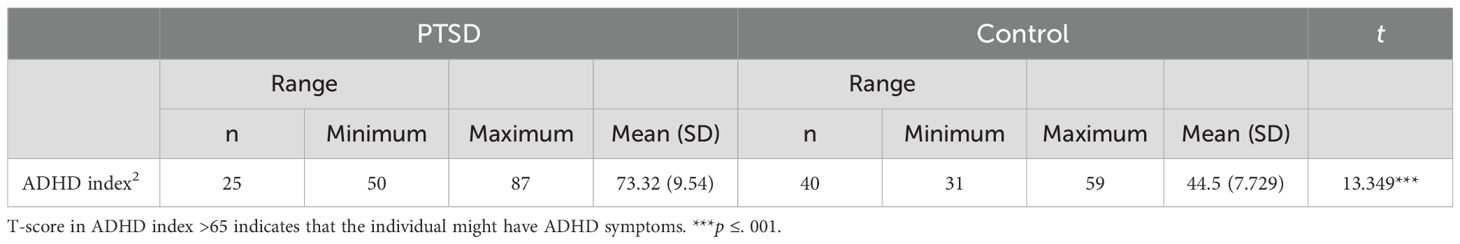
Table 2b. Descriptive statistics, means, and standard deviations of the Conner`s ADHD index between the groups.
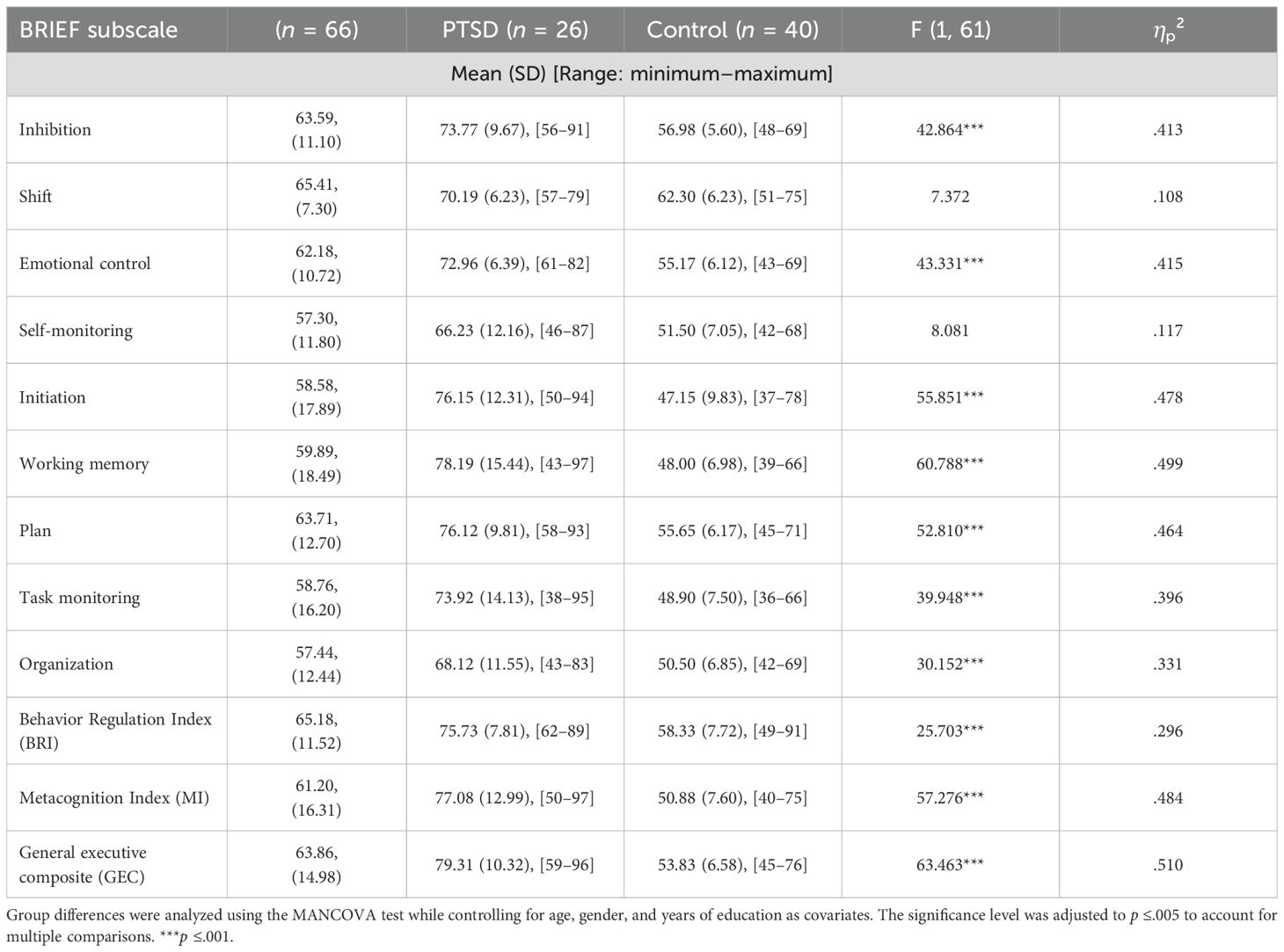
3.2 Differences in executive functions between groups based on BRIEF-A
Differences between groups were examined by the MANCOVA test controlling for age, gender, and the number of education years as covariates. The significance level was set at p ≤. 005 to account for multiple comparisons (Table 3).
The prevalence of EF difficulties based on the GEC cutoff score was significantly higher among the PTSD group (T-score ≥65), 88.5%, compared to the control group, 5%. When examining the differences between groups in BRIEF-A scales, lower EF abilities were found in the PTSD group in most scales (Table 3). Additional predictive analyses are provided in the Supplementary Material.
3.3 Differences between groups in EF based on VAP-S 2
Differences between groups were examined by the Mann–Whitney test (Table 4). The significance level was set at p ≤. 004 to account for multiple comparisons.
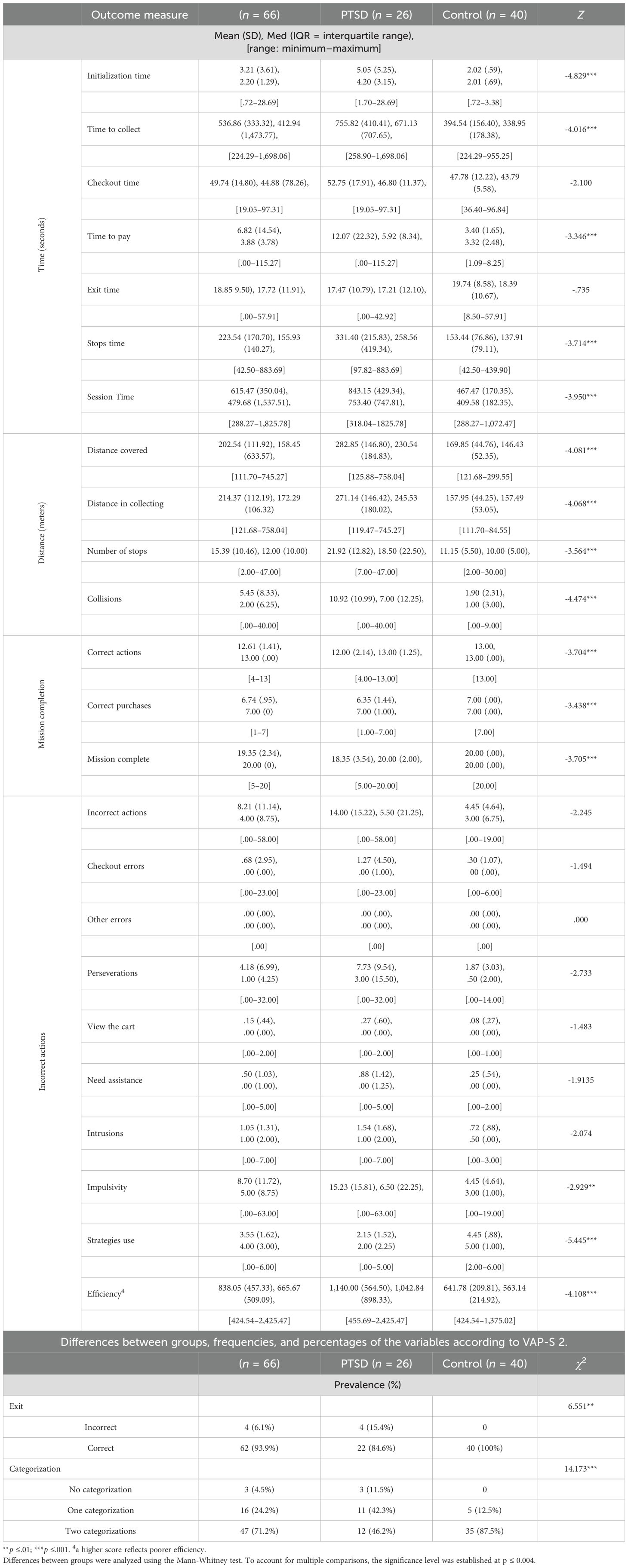
Table 4. Executive function differences between groups based on their performance in the Virtual Action Planning Supermarket (VAP-S 2).
When examining EF during VAP-S 2 performance, the participants with PTSD showed higher impulsivity, low strategy, and categorization use. They also showed interruptions in maintaining the sequence and continuity of the performance with higher mean scores in intrusions (sensory and visual interruptions), preservations (repeated actions), check-out errors, and longer exit time, although these differences were not statistically significant. All of these outcomes result in a longer time to complete the activity, longer trajectory distance, and more incorrect actions, leading to a significantly lower efficiency in completing the task (Table 4).
Figures 1–3 present differences in performance in VAP-S 2 between PTSD patients and healthy participants. As shown in Figure 1A, the trajectory of a 32-year-old man with PTSD performing the VAP-S 2 indicates less efficient performance with longer time to complete the activity, longer trajectory distance, and more incorrect actions compared to Figure 1B, the trajectory of a 33-year-old healthy man performing the VAP-S 2.
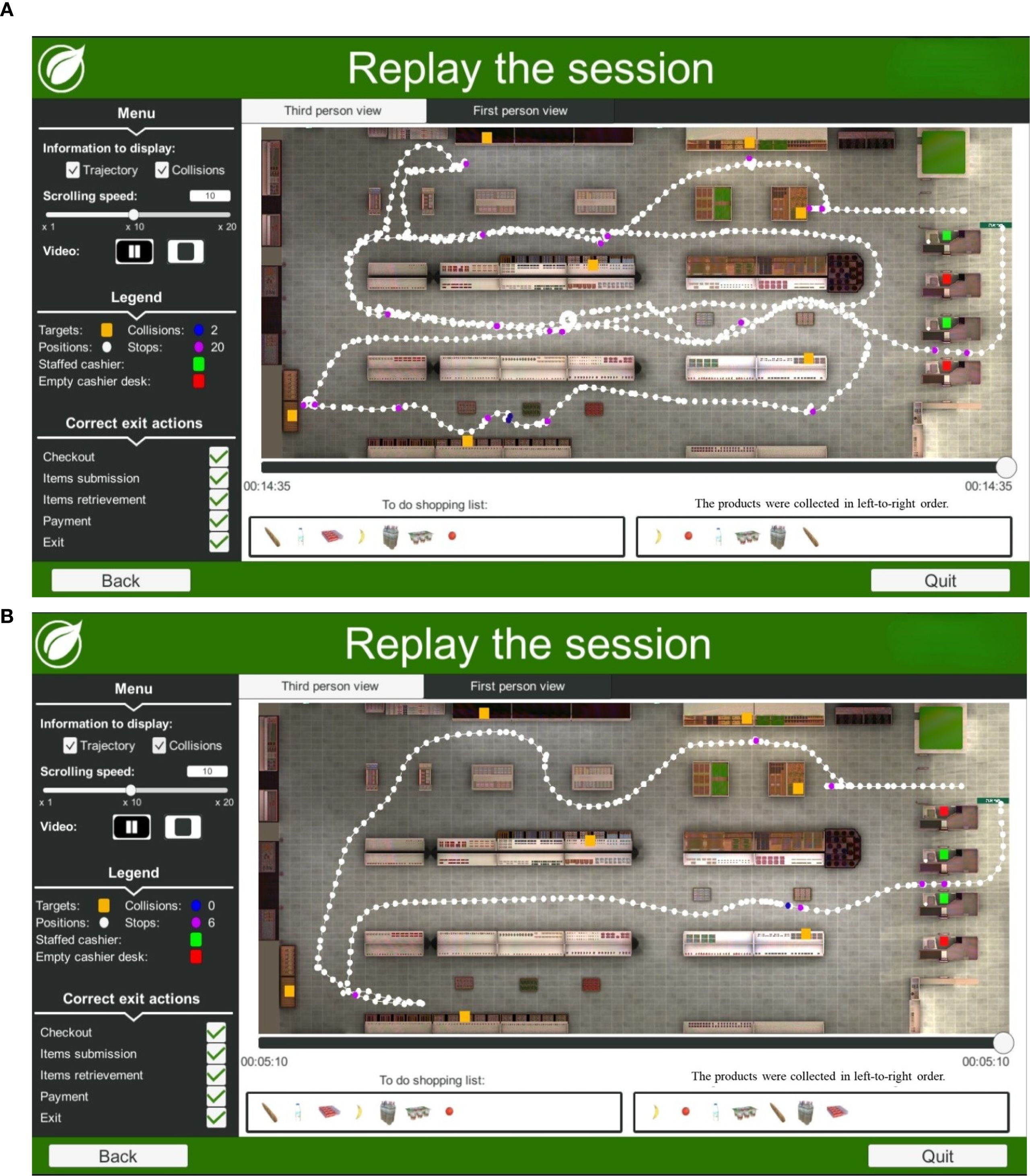
Figure 1. (A) Example trajectory of a 32-year-old man with PTSD performing the Virtual Action Planning Supermarket (VAP-S 2). This participant had an incomplete secondary education (12 or fewer education years) and completed the task in 14:35 min. An examination of the purchased items from the shopping list suggests that the participant categorized the groceries into dairy and fruit products and missed one product. (B) Example trajectory of a 33-year-old healthy man performing the Virtual Action Planning Supermarket (VAP-S 2). This participant had an incomplete secondary education (12 or fewer education years) and completed the task in 05:10 min. An examination of the purchased items from the shopping list suggests that the participant categorized the groceries into dairy and fruit products and collected all of the products.
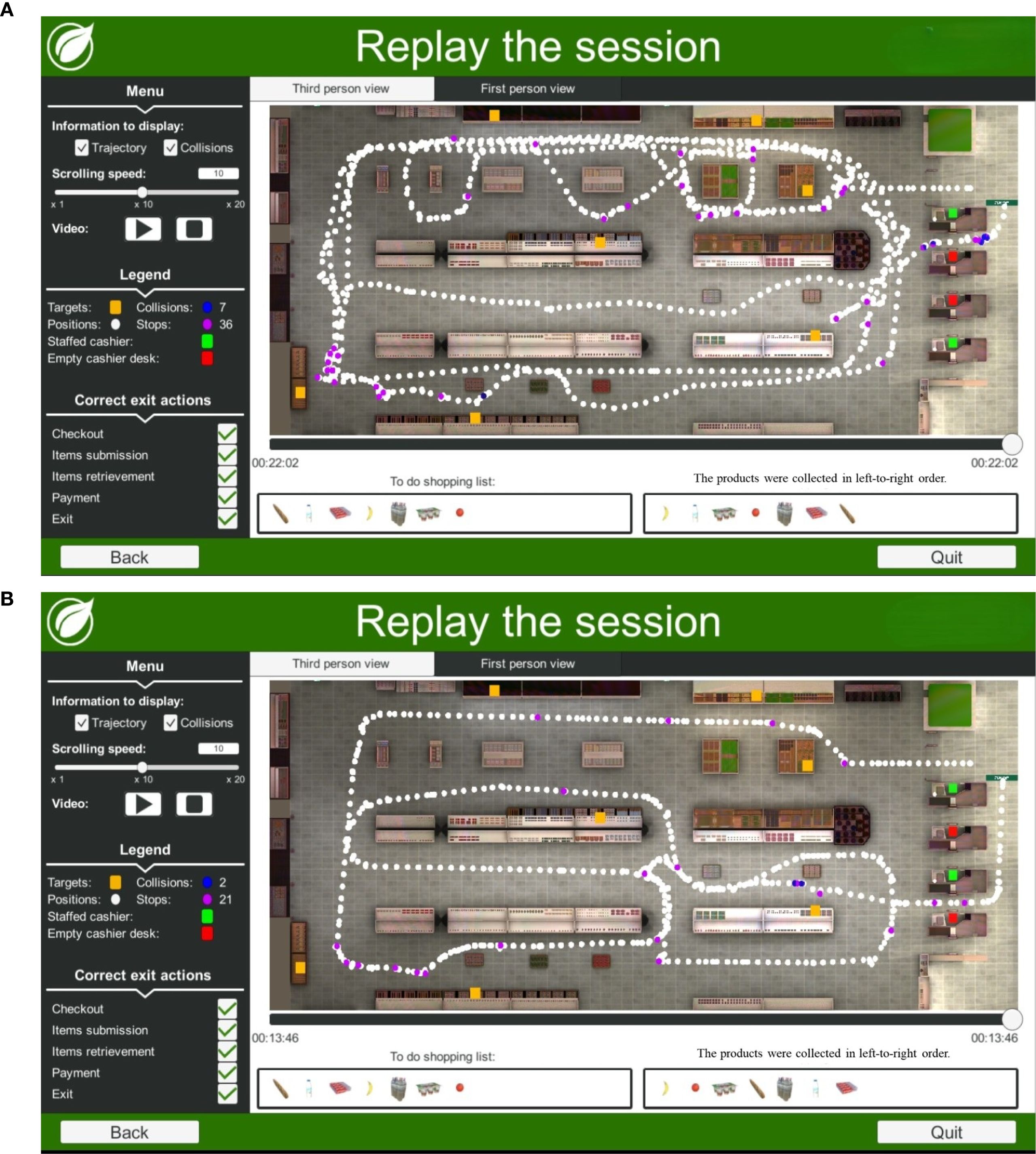
Figure 2. (A) Example trajectory of a 52-year-old man with PTSD while performing the Virtual Action Planning Supermarket (VAP-S 2). This participant had a professional diploma (12 to 13 years of education) and completed the task in 22:02 min. An examination of the purchased items from the shopping list suggests that the participant categorized the groceries into dairy products only and collected all of the products. (B) Example trajectory of a 52-year-old healthy man performing the Virtual Action Planning Supermarket (VAP-S 2). This participant had a high school graduate (“Bagrut” diploma) (12 education years). The total time to complete the task was 13:46 min. An examination of the purchased items from the shopping list suggests that the participant categorized the groceries into fruit products only and collected all of the products.
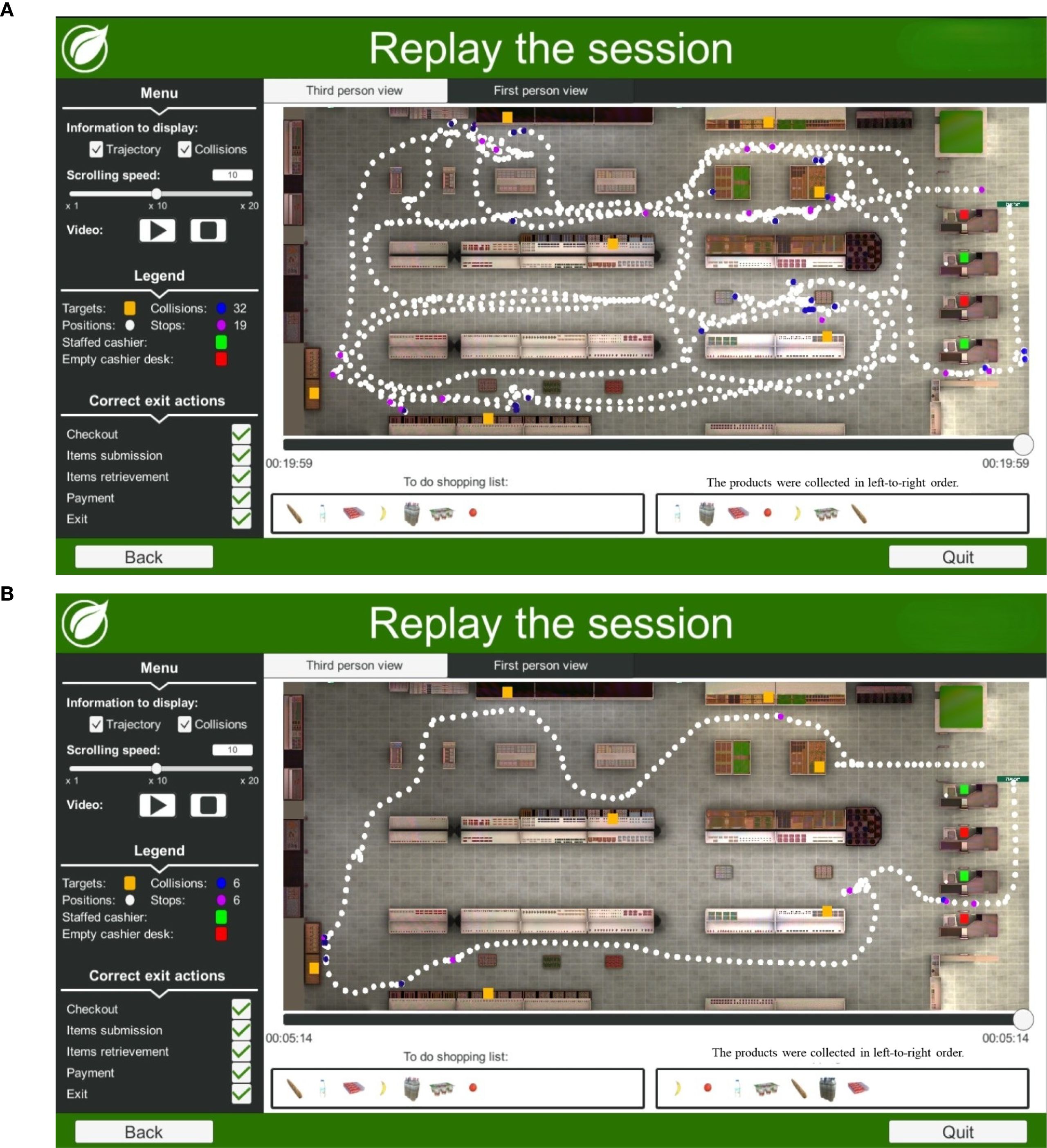
Figure 3. (A) Example trajectory of a 39-year-old man with PTSD while performing the Virtual Action Planning Supermarket (VAP-S 2). This participant had an incomplete secondary education (12 years or less) and completed the task in 19:59 min. An examination of the purchased items from the shopping list suggests that the participant categorized the groceries into fruit products only and collected all of the products. (B) Example trajectory of a 37-year-old healthy man performing the Virtual Action Planning Supermarket (VAP-S 2). This participant had an academic education (15 years of education or more) and completed the task in 05:14 min. An examination of the purchased items from the shopping list suggests that the participant categorized the groceries into dairy and fruit products and collected all of the products.
In Figure 2A, the trajectory of a 52-year-old man with PTSD performing the VAP-S 2 task indicates less efficient performance characterized by a longer time to complete the activity, greater trajectory distance, and more incorrect actions compared to Figure 2B, which shows the trajectory of a 52-year-old healthy man performing the VAP-S 2.
In Figure 3A, the trajectory of a 39-year-old man with PTSD performing the VAP-S 2 task indicates less efficient performance, characterized by a longer time to complete the activity, greater trajectory distance, and more incorrect actions compared to Figure 1B, the trajectory of a 37-year-old healthy man performing the VAP-S 2.
3.4 Correlations between EF as measured by the self-report (BRIEF-A) and actual performance-based assessment (VAPS 2) among the study group
Controlling for PTSD severity and ADHD, significant correlations were found between BRIEF-A scores and VAP-S 2 performance. Higher BRIEF-A general executive composite (GEC) and emotional control scores correlated with more collisions in the VAP-S 2 shopping task [rs(19) = 0.478, p < 0.05; rs(19) = 0.548, p < 0.01]. Poorer self-monitoring and organization correlated with more errors at checkout and exit selection [rs(19) = 0.446, p < 0.05; rs(19) = 0.457, p < 0.05]. Worse planning related to increased intrusions, reflecting difficulty ignoring distractions during task performance [rs(19) = 0.436, p < 0.05]. Additionally, lower inhibition and organization scores were associated with a greater need for assistance to perform [rs(19) = -0.6, p < 0.01; rs(19) = ;-0.435, p < 0.05]. Note that higher BRIEF-A scores indicate worse performance.
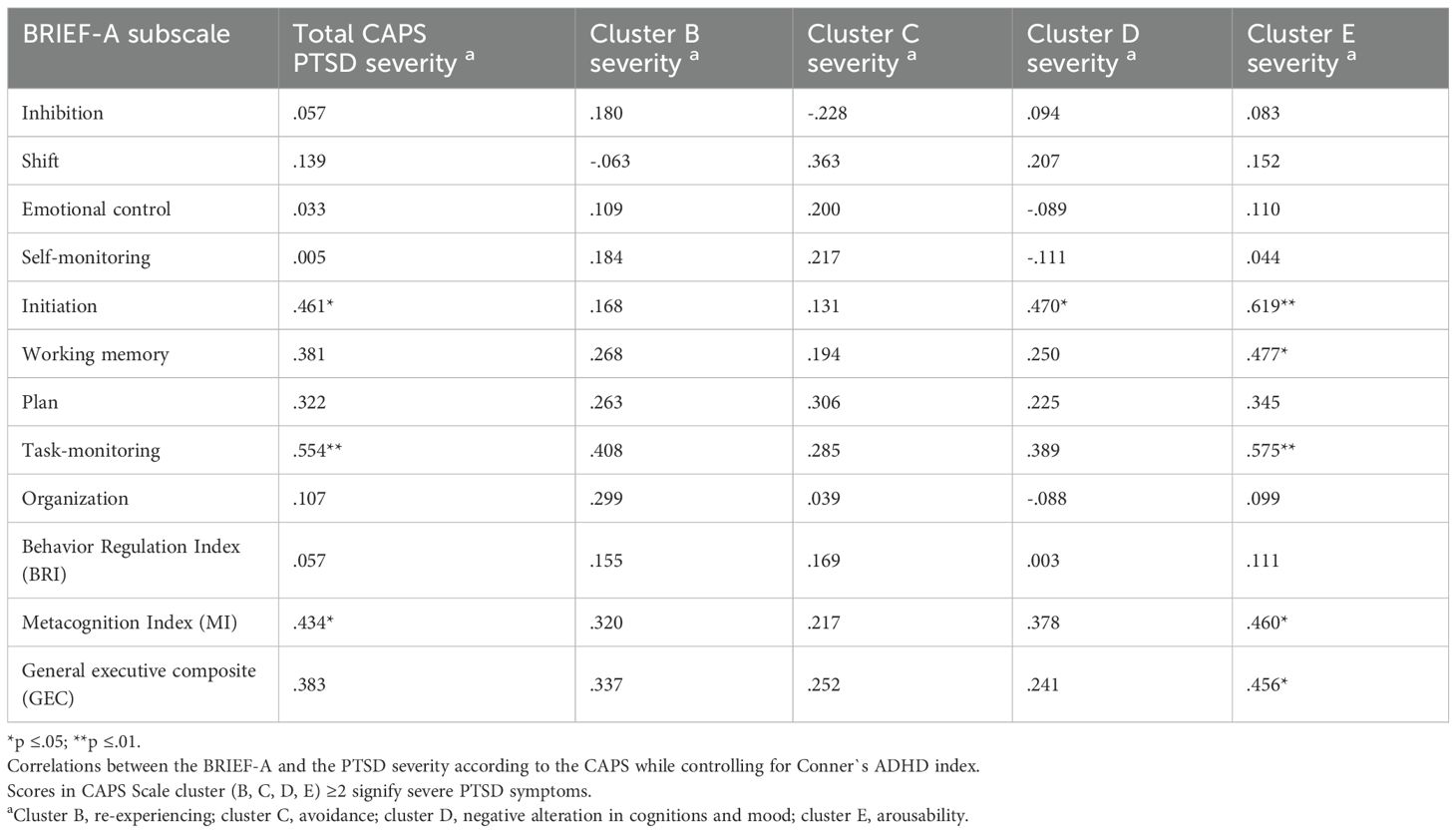
3.5 Correlations between EF and PTSD severity among the study group
Controlling for ADHD, PTSD severity significantly correlated with lower EF on the BRIEF-A—initiation, task-monitoring, and metacognition index (MI). Specifically, arousability (cluster E) significantly correlated with lower initiation, working memory, task-monitoring, MI, and GEC. In addition, negative alteration in cognition and mood (cluster D) significantly correlated with lower initiation (Table 5).
4 Discussion
This study focused on EF difficulties in people with PTSD, their relation to PTSD severity, and their implications on daily functioning. The study also highlighted the relevance of combining self-reports and performance-based ecologically valid evaluations to reflect EF difficulties in daily life scenarios. This significant information may optimize intervention efficiency.
The study’s first aim was to compare EF between participants with PTSD and healthy controls using the BRIEF-A self-report and an actual performance-based evaluation via a VR platform—the first hypothesis was confirmed. A higher prevalence of EF difficulties was found in the PTSD group in both measures—in most BRIEF-A scales as well as the behavioral regulation scale. The virtual shopping task highlighted that EF difficulties were expressed in higher impulsivity and lower strategy use, which affected performance efficiency. Previous reports exist regarding EF difficulties in PTSD and note, for example, how impulsivity impacts the ability to stop and monitor and how reduced inhibitory control affects the ability to deal with internal and external distractions (10, 11, 18) as manifested in the present study results of the VAPS 2 when distractions such as a virtual buyer and randomized noises appear while performing the VR shopping task. Impaired ability to manage distractions in PTSD can be associated with hyperactivity in the salience network (SN)—a circuit that detects and prioritizes significant internal and external stimuli. In PTSD, the SN (including the amygdala, anterior insula, and dorsal anterior cingulate cortex) shows heightened activation, lowering the threshold for perceiving stimuli as salient. This leads to exaggerated responses to distractions and increased sensitivity to environmental cues. Such neural alterations underlie core symptoms of hypervigilance and may contribute to the executive dysfunction observed in PTSD (55–58). The BRIEF-A used in the present study also provided a detailed profile of the various EF components affected in PTSD. This is important since many previous studies have used assessments that measure a specific EF component (for example, Trail Making Test B (TMT B) or Digit Span total (DS-tot)) (14, 59, 60), lacking a general picture that reflects daily life.
The present study used both a self-report and an actual performance of a daily activity to illuminate the functional implications of EF deficits in people with PTSD. This is one of the first studies to apply the VAP-S 2. Both BRIEF-A and VAP-S 2 were found to be feasible for profiling EF difficulties in people with PTSD. The few previous studies that used the BRIEF-A with people with PTSD (61) also found BRIEF-A to be a sensitive assessment to manifest EF difficulties and recommended using it in intervention and rehabilitation. The present study highlights the relevance of adding an assessment of the actual performance of a daily activity, such as shopping in the supermarket via the VAP-S 2.
The results of the VAP-S 2 confirmed that people with PTSD might have lower performance efficiency than healthy controls. Studies that used the VAP-S 2 in PTSD are scarce. This emphasizes the relevance of the present study and the VAP-S 2 in elaborating ways to evaluate how EF difficulties in people with PTSD impact their daily function and activity performance. The results showed that even a frequent and common activity, such as shopping in a supermarket, may be challenging for people with PTSD (22, 62, 63), placing significant demands on their executive functions. VAP-S 2 succeeded in depicting how, in this instrumental ADL activity, various EF components such as initiation, planning, attention, selection, working memory, sequencing, and monitoring are impaired in PTSD. This might explain their lower efficiency, lower ability to complete the task, higher impulsivity, incorrect actions, and lower use of strategies while performing the VAP-S 2. However, it is important to acknowledge that ADHD comorbidity may influence EF outcomes (6, 45, 46), and further research is needed to explore how EF affects daily activity performance in PTSD.
With regard to the second hypothesis, the VAP-S 2 also correlated with the BRIEF-A scores, showing concurrent validity—for example, a higher number of collisions (i.e., participants bumping into objects/people while performing the virtual shopping task) correlated with greater difficulties in EF (GEC score) and lower emotional control; lower self-monitoring and organization abilities were related to a higher number of errors in VAP-S 2. Lower inhibition and organization correlated with a greater need for assistance when performing the shopping task. Hence, using both a self-report, such as BRIEF-A, and the actual activity performance via VAP-S 2 may reflect how difficulties in EF are expressed in real-life scenarios that require proper planning, strategy use, rule compliance, problem-solving, and precise regulation of distractive stimuli (39–42). Furthermore, these findings remain significant after controlling for the ADHD covariate, strengthening our results and aligning with prior research highlighting the overlapping, yet distinct, EF impairments such as inhibition seen in PTSD and ADHD (6, 46).
Interestingly, in the present study, BRIEF-A scores correlated with PTSD severity (mainly arousability). As opposed to BRIEF-A, none of the VAP-S 2 measures correlated with PTSD symptom severity. While some previous studies indicate that PTSD symptoms may worsen EF (12, 64) and daily activity performance (23, 65), others claim that EF difficulties in PTSD are not moderated by PTSD symptom severity. Once PTSD occurs, EF difficulties are presented and not necessarily related to PTSD severity (9, 18, 60). In our study, it may be suggested that VAP-S 2 requires integral complex cognitive abilities that do not necessarily correlate with PTSD severity but with PTSD existence. Furthermore, most of the study participants were war-related PTSD including veterans and combatants (46% of the participants) and men. This may contribute to the current results as a previous study found that poorer EF performance in PTSD was related to male gender, older patients, war trauma, and comorbidity with depression that restricted participation and inclusion into society (14). Further studies on men and women in larger samples should examine the relation between VAP-S 2 outcomes and its relation with BRIEF-A and PTSD severity.
Studies should also explore the potential advantage of evaluating EF while performing a daily life activity, such as shopping in VAP-S 2, which offers promising clinical advantages for PTSD care, particularly by enabling the evaluation and training of activities that require executive function (EF) within realistic, daily-life contexts, such as shopping. The VAP-S 2 seems to have several benefits, especially for people with PTSD: it is a user-friendly environment that can be customized to the patient and the intervention plan. It may decrease the patient’s sense of threat and optimize emotional engagement in treatment (33, 36). Through the practice of familiar, everyday tasks via VAP-S 2, individuals with PTSD can build confidence, increase functional independence, and strengthen the courage to participate actively in their communities. These advances can help reduce stigmatization and foster social inclusion (32–34). This aligns with the International Classification of Functioning Disability and Health of the World Health Organization (19), which includes measures that imitate daily life activities that may improve intervention outcomes in terms of better independence and participation in daily life activities. As VAP-S 2 and similar VR platforms become increasingly accessible and affordable, their integration into routine clinical practice creates new opportunities for personalized interventions, ongoing progress monitoring, and improved real-world functional outcomes.
5 Conclusion
EF difficulties are more prevalent in people with PTSD and may affect their daily functioning. These impairments may also correlate with the severity of the symptoms, which may also impede daily functioning. The Virtual Action Planning Supermarket (VAP-S 2) uniquely enhances EF assessment by offering an immersive virtual reality environment that mimics real-life tasks, such as shopping. This method complements traditional self-report measures, increasing ecological validity and sensitivity to functional impairments relevant to patients’ daily activities. EF evaluation should combine self-reports that provide an authentic perspective based on the person’s own voice with actual performance-based assessments that imitate activities in real-life settings. Furthermore, incorporating VAP-S 2 in clinical settings can improve the evaluation of EF, make better tailor rehabilitation efforts, and provide a secure environment for practicing daily life skills. This combined approach provides a thorough understanding of perceived and actual executive function challenges, guiding personalized clinical interventions and enhancing treatment outcomes.
6 Limitations
Given the challenges of recruiting and retaining participants with PTSD, this study involved a relatively small sample size, which may have limited the ability to detect some “true effects” or associations between PTSD and EF. The sample had a gender imbalance, with more men included, since the inclusion criteria and professional considerations led to the exclusion of several women with PTSD. This imbalance may limit the generalizability of the findings to broader populations. Additionally, unmeasured or uncontrolled variables may have influenced the findings, potentially masking relationships between PTSD symptoms and executive function outcomes. The cross-sectional nature of the study, with variability in participant characteristics—such as trauma type, which was not analyzed as a primary variable due to heterogeneity and sample size constraints—further limits the generalizability of the results. Future research with larger, more demographically balanced samples is necessary to strengthen these findings and enhance their applicability.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was obtained from the Helsinki Committee at Rambam Medical Center and The Institutional Review Board of the Faculty of Social Welfare & Health Sciences, University of Haifa. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NS: Writing – review & editing, Writing – original draft, Investigation, Project administration, Data curation, Formal Analysis. EJ: Investigation, Writing – review & editing. EB: Investigation, Writing – review & editing. YC: Conceptualization, Writing – review & editing. EF: Methodology, Conceptualization, Writing – review & editing. UO: Methodology, Conceptualization, Writing – review & editing. NJ: Writing – review & editing, Software, Resources. EK: Resources, Writing – review & editing, Software. BE-Y: Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was funded by a grant from the EMDR Research Foundation (Winner of the Francine Shapiro Memorial Fund Grant Award, 2020).
Acknowledgments
We want to thank all participants, the Perspectives Program (Ofek) at Rambam Health Care Campus, the Psychiatric Department, and the medical staff at Rambam Medical Center for their invaluable support in completing this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1620472/full#supplementary-material
References
1. Association AP. Posttraumatic stress disorder. In: Diagnostic and Statistical Manual of Mental Disorders, 5 ed. (Washington, DC, USA: American Psychiatric Association) (2022).
2. Edgelow MM, MacPherson MM, Arnaly F, Tam-Seto L, and Cramm HA. Occupational therapy and posttraumatic stress disorder: A scoping review. Can J Occup Ther. (2019) 86:148–57. doi: 10.1177/0008417419831438
3. Schnurr PP, Lunney CA, Bovin MJ, and Marx BP. Posttraumatic stress disorder and quality of life: extension of findings to veterans of the wars in Iraq and Afghanistan. Clin Psychol Rev. (2009) 29:727–35. doi: 10.1016/j.cpr.2009.08.006
4. Storm MP and Christensen KS. Comparing treatments for post-traumatic comparing treatments for post-traumatic stress disorder-a systematic review stress disorder-a systematic review. Dan Med J. (2021) 68:9200643.
5. Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, and Friedman MJ. Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. J Clin Psychiatry. (2013) 74:e1171. doi: 10.4088/JCP.12r08225
6. Punski-Hoogervorst JL, Engel-Yeger B, and Avital A. Attention deficits as a key player in the symptomatology of posttraumatic stress disorder: A review. J Neurosci Res. (2023) 101:1068–85. doi: 10.1002/jnr.25177
7. Punski-Hoogervorst JL, Avital A, and Engel-Yeger B. Challenges in basic and instrumental activities of daily living among adults with posttraumatic stress disorder: A scoping review. Occup Ther Ment Health. (2022) 39:184–210. doi: 10.1080/0164212X.2022.2094523
8. Smits FM, Geuze E, Schutter D, van Honk J, and Gladwin TE. Effects of tdcs during inhibitory control training on performance and ptsd, aggression and anxiety symptoms: A randomized-controlled trial in a military sample. Psychol Med. (2021) 52:1–11. doi: 10.1017/S0033291721000817
9. Liu J, Roberts AL, Lawn RB, Jha SC, Sampson L, Sumner JA, et al. Post-traumatic stress disorder symptom remission and cognition in a large cohort of civilian women. Psychol Med. (2024) 54:2312. doi: 10.1017/S0033291724001107
10. Jagger-Rickels A, Stumps A, Rothlein D, Park H, Fortenbaugh F, Zuberer A, et al. Impaired executive function exacerbates neural markers of posttraumatic stress disorder. Psychol Med. (2021) 52:3985–98. doi: 10.1017/S0033291721000842
11. Jagger-Rickels A, Rothlein D, Stumps A, Evans TC, Bernstein J, Milberg W, et al. An executive function subtype of ptsd with unique neural markers and clinical trajectories. Transl Psychiatry. (2022) 12:262. doi: 10.1038/s41398-022-02011-y
12. Liu SR, Moore TM, Gur RC, Nievergelt C, Baker DG, Risbrough V, et al. High Executive Functioning Is Associated with Reduced Posttraumatic Stress after Trauma Exposure among Male U.S. Military Personnel. Front Psychol. (2023) 14:1181055. doi: 10.3389/fpsyg.2023.1181055
13. Adrien V, Bosc N, Peccia Galletto C, Diot T, Claverie D, Reggente N, et al. Enhancing agency in posttraumatic stress disorder therapies through sensorimotor technologies. J Med Internet Res. (2024) 26:e58390. doi: 10.2196/58390
14. Polak AR, Witteveen AB, Reitsma JB, and Olff M. The role of executive function in posttraumatic stress disorder: A systematic review. J Affect Disord. (2012) 141:11–21. doi: 10.1016/j.jad.2012.01.001
15. Josman N and Meyer S. Conceptualisation and use of executive functions in paediatrics: A scoping review of occupational therapy literature. Aust Occup Ther J. (2019) 66:77–90. doi: 10.1111/1440-1630.12525
16. Aupperle RL, Melrose AJ, Stein MB, and Paulus MP. Executive function and ptsd: disengaging from trauma. Neuropharmacology. (2012) 62:686–94. doi: 10.1016/j.neuropharm.2011.02.008
17. Wrocklage KM, Schweinsburg BC, Krystal JH, Trejo M, Roy A, Weisser V, et al. Neuropsychological functioning in veterans with posttraumatic stress disorder: associations with performance validity, comorbidities, and functional outcomes. J Int Neuropsychol Soc. (2016) 22:399–411. doi: 10.1017/S1355617716000059
18. DeGutis J, Esterman M, McCulloch B, Rosenblatt A, Milberg W, and McGlinchey R. Posttraumatic psychological symptoms are associated with reduced inhibitory control. Not Gen Executive Dysfunction. (2015) 21:342–52. doi: 10.1017/S1355617715000235
19. World Health Organization (WHO). International Classification of Functioning, Disability and Health: Icf. Geneva: World Health Organization (2001). 299 p.
20. Shalev A, Liberzon I, and Marmar C. Post-traumatic stress disorder. N Engl J Med. (2017) 376:2459–69. doi: 10.1056/NEJMRA1612499
21. Falconer E, Allen A, Felmingham KL, Williams LM, and Bryant RA. Inhibitory neural activity predicts response to cognitive-behavioral therapy for posttraumatic stress disorder. J Clin Psychiatry. (2013) 74:895–901. doi: 10.4088/JCP.12m08020
22. Maguen S, Stalnaker M, Mccaslin S, and Litz BT. Ptsd subclusters and functional impairment in. Mil Med. (2009) 174:779–85. doi: 10.1037/e717692011-006
23. Rodriguez P, Holowka DW, and Marx BP. Assessment of posttraumatic stress disorder-related functional impairment: A review. J Rehabil Res Dev. (2012) 49:649–66. doi: 10.1682/JRRD.2011.09.0162
24. Amick MM, Kraft M, and Mcglinchey R. Driving simulator performance of veterans from the Iraq and Afghanistan wars. J Rehabil Res Dev. (2013) 50:463–70. doi: 10.1682/JRRD.2012.06.0108
25. Josman N, Somer E, Reisberg A, Weiss PL, Garcia-palacios A, Hoffman H, et al. Busworld: designing a virtual environment for post-traumatic stress disorder in Israel: A protocol. (2006) 9:. doi: 10.1089/cpb.2006.9.241
26. Myers CE, Radell ML, Shind C, Ebanks-Williams Y, Beck KD, Gilbertson MW, et al. Beyond symptom self-report: use of a computer “Avatar” to assess post-traumatic stress disorder (Ptsd) symptoms. Int J Psychiatry Clin Pract. (2016) 19:593–8. doi: 10.1080/10253890.2016.1232385
27. Samuelson KW, Abadjian L, Jordan JT, Bartel A, Vasterling J, and Seal K. The association between ptsd and functional outcome is mediated by perception of cognitive problems rather than objective neuropsychological test performance. J Trauma Stress. (2017) 30:521–30. doi: 10.1002/jts.22223
28. Engel-Yeger B, Palgy-Levin D, and Lev-Wiesel R. Predicting fears of intimacy among individuals with post-traumatic stress symptoms by their sensory profile. Br J Occup Ther. (2015) 78:51–7. doi: 10.1177/0308022614557628
29. Aubin G, Béliveau MF, and Klinger E. An exploration of the ecological validity of the virtual action planning–supermarket (Vap-S) with people with schizophrenia. J Intellect Disabil Res. (2018) 28:689–708. doi: 10.1080/09602011.2015.1074083
30. Rizzo AA, Schultheis M, Kerns KA, and Mateer C. Analysis of assets for virtual reality applications in neuropsychology. Neuropsychol Rehabil. (2004) 14:207–39. doi: 10.1080/09602010343000183
31. Romero-Ayuso D, Castillero-Perea Á, González P, Navarro E, Molina-Massó JP, Funes MJ, et al. Assessment of cognitive instrumental activities of daily living: A systematic review. Disabil Rehabil. (2021) 43:1342–58. doi: 10.1080/09638288.2019.1665720
32. Rothbaum BO, Malcoun E, As R, and Josman N. Virtual reality exposure therapy for combat-related posttraumatic stress disorder. Ann N Y Acad Sci. (2010) 1208:126–32. doi: 10.1111/j.1749-6632.2010.05691.x
33. Best P, McKenna A, Quinn P, Duffy M, and Van Daele T. Can virtual reality ever be implemented in routine clinical settings? A systematic narrative review of clinical procedures contained within case reports for the treatment of ptsd. (2020) 1:563739. doi: 10.3389/frvir.2020.563739
34. Vianez A, Marques A, and de Almeida RS. Virtual reality exposure therapy for armed forces veterans with post-traumatic stress disorder: A systematic review and focus group. Int J Environ Res Public Health. (2022) 19:464. doi: 10.3390/IJERPH19010464
35. Eshuis LV, Van Gelderen MJ, Van Zuiden M, Nijdam MJ, Vermetten E, Olff M, et al. Efficacy of immersive ptsd treatments: A systematic review of virtual and augmented reality exposure therapy and a meta-analysis of virtual reality exposure therapy. J Psychiatr Res. (2021) 143:516–27. doi: 10.1016/j.jpsychires.2020.11.030
36. Valmaggia LR, Latif L, Kempton MJ, and Rus-Calafell M. Virtual reality in the psychological treatment for mental health problems: an systematic review of recent evidence. Psychiatry Res. (2016) 236:189–95. doi: 10.1016/j.psychres.2016.01.015
37. Levy CE, Miller DM, Akande CA, Lok B, Marsiske M, and Halan S. V-mart, a virtual reality grocery store: A focus group study of a promising intervention for mild traumatic brain injury and posttraumatic stress disorder. Am J Phys Med Rehabil. (2019) 98:191–8. doi: 10.1097/PHM.0000000000001041
38. Klinger E, Chemin I, Lebreton S, and Marié R-M. Virtual action planning in parkinson’s disease: A control study. (2006). doi: 10.1089/cpb.2006.9.342
39. Borgnis F, Baglio F, Pedroli E, Rossetto F, Uccellatore L, Oliveira JAG, et al. Available virtual reality-based tools for executive functions: A systematic review. Front Psychol. (2022) 13:833136. doi: 10.3389/FPSYG.2022.833136
40. Josman N, Kizony R, Hof E, Goldenberg K, Weiss PL, and Klinger E. Using the virtual action planning-supermarket for evaluating executive functions in people with stroke. J Stroke Cerebrovasc Dis. (2014) 23:879–87. doi: 10.1016/j.jstrokecerebrovasdis.2013.07.013
41. Josman N, Reisberg A, Weiss PL, Garcia-Palacios A, and Hoffman HG. Busworld: an analog pilot test of a virtual environment designed to treat posttraumatic stress disorder originating from a terrorist suicide bomb attack. Cyberpsychol Behav. (2008) 11:775–7. doi: 10.1089/cpb.2008.0048
42. Josman N, Schenirderman AE, Klinger E, and Shevil E. Using virtual reality to evaluate executive functioning among persons with schizophrenia: A validity study. Schizophr Res. (2009) 115:270–7. doi: 10.1016/j.schres.2009.09.015
43. Werner P, Rabinowitz S, Klinger E, Korczyn AD, and Josman N. Use of the virtual action planning supermarket for the diagnosis of mild cognitive impairment. Dement Geriatr Cogn Disord. (2009) 27:301–9. doi: 10.1159/000204915
44. Conners CK, Erhardt D, and Sparrow EP. The Conner’s Adult Adhd Rating Scales (Caars-S:S) Technical Manual North Tonawanda, N.Y. (North Tonawanda, NY, USA: Multi-Health Systems Inc) (1999).
45. Howlett JR, Campbell-Sills L, Jain S, Heeringa SG, Nock MK, Sun X, et al. Attention deficit hyperactivity disorder and risk of posttraumatic stress and related disorders: A prospective longitudinal evaluation in U.S. Army soldiers. J Trauma Stress. (2018) 31:909–18. doi: 10.1002/jts.22347
46. Wilson J, Fida D, Maurer R, Wiley A, Rajasekera T, and Spagnolo P. Sex differences in the comorbidity between attention deficit-hyperactivity disorder and posttraumatic stress disorder: A systematic literature review and meta-analysis. Gen Hosp Psychiatry. (2025) 95:32–9. doi: 10.1016/j.genhosppsych.2025.04.003
47. Hoppen TH, Priebe S, Vetter I, and Morina N. Global burden of post-traumatic stress disorder and major depression in countries affected by war between 1989 and 2019: A systematic review and meta-analysis. BMJ Glob Health. (2021) 6:e006303. doi: 10.1136/bmjgh-2021-006303
48. Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Charney DS, Keane TM, et al. Clinician-Administered Ptsd Scale for Dsm-Iv. Boston (MA): National Center for PTSD, U.S. Department of Veterans Affairs, Boston VA Medical Center (1998). 1–19
49. Roth RM and Gioia GA. Behavior Rating Inventory of Executive Function (Brief-a) –Adult Version. Lutz, FL: Psychological Assessment Resources (2005).
50. Rotenberg-Shpigelman S, Rapaport R, Stern A, and Hartman-Maeir A. Content validity and internal consistency reliability of the behavior rating inventory of executive function-adult version (Brief-a) in Israeli adults with attention-deficit/hyperactivity disorder. Isr J Occup Ther. (2008) 17:77–96.
51. Josman N, Hof E, Klinger E, Marié RM, Goldenberg K, Weiss PL, et al. Performance Within A Virtual Supermarket and its Relationship to Executive Functions in Post-Stroke Patients. Boston, MA: IEEE (2006). 106–9. doi: 10.1109/iwvr.2006.1707536.
52. Klinger E and Josman N eds. Virtual Environments to Evaluate and Treat Cognitive Deficits in Every Days Function. (Tel Aviv, Israel: Presentation Presented at ICVR Workshop) (2019).
53. Becker LA. Effect Size (Es) (2000). Available online at: http://web.uccs.edu/lbecker/Psy590/es.htm.
54. Richardson JTE. Eta squared and partial eta squared as measures of effect size in educational research. Educ Res Rev. (2011) 6:135–47. doi: 10.1016/j.edurev.2010.12.001
55. Akiki TJ, Averill CL, and Abdallah CG. A network-based neurobiological model of ptsd: evidence from structural and functional neuroimaging studies. Curr Psychiatry Rep. (2017) 19:81. doi: 10.1007/s11920-017-0840-4
56. Liberzon I and Abelson JL. Context processing and the neurobiology of post-traumatic stress disorder. Neuron. (2016) 92:14–30. doi: 10.1016/j.neuron.2016.09.039
57. Malikowska-Racia N and Salat K. Recent advances in the neurobiology of posttraumatic stress disorder: A review of possible mechanisms underlying an effective pharmacotherapy. Pharmacol Res. (2019) 142:30–49. doi: 10.1016/j.phrs.2019.02.001
58. Ross DA, Arbuckle MR, Travis MJ, Dwyer JB, van Schalkwyk GI, and Ressler KJ. An integrated neuroscience perspective on formulation and treatment planning for posttraumatic stress disorder: an educational review. JAMA Psychiatry. (2017) 74:407–15. doi: 10.1001/jamapsychiatry.2016.3325
59. Scott JC, Matt GE, Wrocklage KM, Crnich C, Jordan J, Southwick SM, et al. Quantitative meta-analysis of neurocognitive functioning in posttraumatic stress disorder. Psychol Bull. (2015) 141:105–40. doi: 10.1037/a0038039
60. Woon FL, Farrer TJ, Braman CR, Mabey JK, and Hedges DW. A meta-analysis of the relationship between symptom severity of posttraumatic stress disorder and executive function. J Trauma Stress. (2017) 22:1–16. doi: 10.1080/13546805.2016.1255603
61. Li Y, Dong F, Cao F, Cui N, Li J, Long Z, et al. Poly-victimization and executive functions in junior college students. Scand J Psychol. (2013) 54:485–92. doi: 10.1111/sjop.12083
62. Lee W, Lee YR, Yoon JH, Lee HJ, and Kang MY. Occupational post-traumatic stress disorder: an updated systematic review. BMC Public Health. (2020) 20:768. doi: 10.1186/s12889-020-08903-2
63. Plach HL and Sells CH. Occupational performance needs of young veterans. Am J Occup Ther. (2013) 67:73–81. doi: 10.5014/ajot.2013.003871
64. Melara RD, Ruglass LM, Fertuck EA, and Hien DA. Regulation of threat in post-traumatic stress disorder: associations between inhibitory control and dissociative symptoms. Biol Psychol. (2018) 133:89–98. doi: 10.1016/j.biopsycho.2018.01.017
Keywords: posttraumatic stress disorder (PTSD), behavioral regulation, executive functions, daily functioning, virtual shopping task performance, and severity of PTSD symptoms
Citation: Safi N, Jahjah E, Bergmann E, Fruchter E, Caspi Y, Oren U, Josman N, Klinger E and Engel-Yeger B (2025) Executive functions in post-traumatic stress disorder: their relation to PTSD severity and daily functioning. Front. Psychiatry 16:1620472. doi: 10.3389/fpsyt.2025.1620472
Received: 29 April 2025; Accepted: 13 October 2025;
Published: 17 November 2025.
Edited by:
Vladimir Adrien, Assistance Publique Hopitaux De Paris, FranceReviewed by:
Mark Dust, California State University, Fullerton, United StatesMegan Edgelow, Queen’s University, Canada
Copyright © 2025 Safi, Jahjah, Bergmann, Fruchter, Caspi, Oren, Josman, Klinger and Engel-Yeger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Batya Engel-Yeger, YmVuZ2VsQHVuaXYuaGFpZmEuYWMuaWw=
 Nehal Safi
Nehal Safi Elias Jahjah2
Elias Jahjah2 Eyal Bergmann
Eyal Bergmann Udi Oren
Udi Oren Naomi Josman
Naomi Josman Batya Engel-Yeger
Batya Engel-Yeger