- 1Faculty of Nursing, Guangxi University of Chinese Medicine, Nanning, China
- 2Department of Gastrointestinal Endoscopy, Guangxi International Zhuang Medical Hospital, Nanning, China
Introduction: This study aimed to examine the impact of social-psychological factors on anxiety before gastrointestinal endoscopy and its effect on patients’ quality of life (QoL).
Methods: Patients scheduled for gastrointestinal endoscopy were recruited for the study. Demographic characteristics, social factors, lifestyle information and endoscopy-related data were obtained through self-reports and the hospital information system. The 7-item Generalized Anxiety Disorder Questionnaire (GAD-7) was used to assess anxiety, while depression and somatization were evaluated using the Patient Health Questionnaire-9 (PHQ-9) and PHQ-15, respectively. Sleep quality was measured with the Pittsburgh Sleep Quality Index (PSQI), social support was assessed using the Social Support Rating Scale (SSRS), and QoL was evaluated through the 12-item Short Form Survey (SF-12).
Results: The prevalence of anxiety before gastrointestinal endoscopy was 34.44%. Gender, age, sleep quality, social support, depression, and somatization were associated with anxiety (all P<0.05). Independent predictors of anxiety were gender, age, PSQI, SSRS, PHQ-9 and PHQ-15 scores (all P<0.05). Furthermore, PSQI, PHQ-9, and PHQ-15 scores were positively correlated with the severity of anxiety (all P<0.05). Patients with anxiety exhibited lower scores in domains of the SF-12, including general health (GH), physical functioning (PF), role-physical (RP), bodily pain (BP), role-emotional (RE), mental health (MH), vitality (VT), and social functioning (SF). Both physical component summary (PCS) and mental component summary (MCS) scores were reduced. Notably, GH, RP, RE, MH, VT, SF, and MCS scores were negatively correlated with varying levels of anxiety (all P<0.05).
Conclusion: Social-psychological factors play a role in anxiety before gastrointestinal endoscopy; anxiety can negatively affect patients’ QoL.
Introduction
Gastrointestinal endoscopy allows for direct visualization of the alimentary tract and remains one of the most effective methods for detecting, diagnosing, and treating gastroenterological diseases (1). Although recent advances, such as artificial intelligence-assisted endoscopy, have emerged rapidly, traditional gastrointestinal endoscopy continues to play a critical role in the detection of gastric and colorectal lesions. It is widely regarded as the gold standard for diagnosing gastric and colorectal cancer and precancerous conditions (2–4). Procedures such as gastroscopy and colonoscopy, although minimally invasive and generally considered safe and effective, are frequently associated with heightened patient anxiety (5, 6). The underlying contributions to this pre-procedural anxiety remain poorly understood. Importantly, anxiety prior to gastrointestinal endoscopy not only affects psychological well-being but may also influence the examination process, treatment compliance, and postoperative recovery (7, 8).
Quality of life (QoL) is a key measure in evaluating health status and effectiveness of clinical interventions (9). Recent research has demonstrated that symptoms of anxiety are negatively associated with Qol, with more severe anxiety corresponding to more significant Qol impairments (10, 11). Whether anxiety specifically related to gastrointestinal endoscopy similarly impacts QoL remains unclear. Therefore, understanding and addressing patients’ anxiety in the context of endoscopic procedures is of growing importance in both clinical and psychological care.
The Theory of Unpleasant Symptoms (TOUS), proposed in 1995, emphasizes that unpleasant symptoms are subjectively perceived experiences that reflect a disruption in an individual’s normal functioning. TOUS identifies three key categories of factors that influence the symptom experience: physiological, psychological, and environmental factors. Physiological factors pertain to bodily function and pathological conditions; psychological factors involve emotional states, coping mechanisms, and perceived uncertainty; and environmental factors encompass social contexts, including family dynamics and levels of social support, which shape how symptoms are perceived. Furthermore, unpleasant symptoms can lead to specific symptom outcomes, referring to the consequences or prognoses following the experience of these symptoms (12, 13). Our previous research has demonstrated that socio-psychological factors influence both physical and mental health outcomes (14–16).
Building on the TOUS, this study aimed to investigate the impact of socio-psychological factors on anxiety prior to gastrointestinal endoscopy, as well as their subsequent effect on patients’ QoL.
Materials and methods
Participants and study design
Patients who visited the Department of Gastrointestinal Endoscopy at the Affiliated Hospital of Guangxi University of Chinese Medicine and were scheduled to undergo gastrointestinal endoscopy were recruited using a snowball sampling strategy between July and December 2024.
The inclusion criteria were as follows: (1) patients scheduled to undergo gastrointestinal endoscopic procedures; (2) no prior history of mental or mood disorders; (3) without severe physical illness; (4) no prior use of anti-anxiety or antidepressant treatments; (5) no experience of major life events within the past three months; (6) without cognitive impairment; (7) ability to read and write in Chinese.
This study was approved by the Institutional Ethics Committee of the Affiliate Hospital of Guangxi University of Chinese Medicine (Approval No. KY 2024-198). All participants provided written informed consent prior to their inclusion in the study and participated voluntarily. All procedures were conducted in accordance with relevant ethical guidelines and regulations, including the Declaration of Helsinki.
Sample size calculation
According to standard clinical research sample size estimation formulas, the average prevalence of anxiety prior to gastrointestinal endoscopy is approximately 50%. Considering an estimated 10% attrition rate, the minimum required sample size for this study was determined to be 424 participants (17, 18).
Measures and questionnaires
Demographic features, including gender and age, were collected. Social features and lifestyle data were self-reported by all participants and included place of residence, educational level, marital status, smoking, and alcohol consumption.
Psychological and endoscopy-related data, including family history of digestive diseases, H pylori infection status, number of prior endoscopies, use of anesthesia during endoscopy, types of endoscopic procedures, and diagnoses from both gastroscopic and colonoscopy, were obtained through self-reports in the hospital information system.
The Chinese version of the 7-item Generalized Anxiety Disorder questionnaire (GAD-7) was used to assess whether participants experienced anxiety. Each item score was calculated, and a total score above 5 indicated the presence of anxiety. Scores between 5 and 9 indicated mild anxiety, 10 to 14 indicated moderate anxiety, and scores above 15 indicated severe anxiety. The Cronbach’s alpha for the GAD-7 in this study was 0.92 (19).
The Chinese version of the Patient Health Questionnaire-9 (PHQ-9) was used to screen for depression. Each item was scored and summed, with a total score above 5 indicating the presence of depression. Scores between 5 and 9 indicated mild depression, 10 to 14 indicated moderate depression, 15 to 19 indicated moderately severe depression, and scores above 20 indicated severe depression. The Cronbach’s alpha for the PHQ-9 was 0.88 (20).
The Chinese version of the Patient Health Questionnaire-15 (PHQ-15) was used to screen for somatization and assess the severity of somatic symptoms. Each item was scored, and the total score was used to determine symptom severity. A total score above 6 indicated the presence of somatization. Scores from 6 to 15 indicated mild somatization, scores from 16 to 25 indicated moderate somatization, and scores above 26 were classified as severe somatization (21). The Cronbach’s alpha for the PHQ-15 in this study was 0.79 (22).
Sleep quality was measured using the Chinese version of the Pittsburgh Sleep Quality Index (PSQI). The PSQI consists of 19 self-rated items and differentiates between good and poor sleep quality by evaluating seven components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction over the previous month. A total PSQI score above 5 indicates poor sleep quality (23). The Cronbach’s alpha for the PSQI was 0.71, and the intraclass correlation coefficient was 0.90 (24).
Social support was assessed using the Social Support Rating Scale (SSRS), which evaluates three components: objective social support, subjective social support, and utilization of social support. Each item was scored, and total scores below 20 indicated low-level social support, scores between 20 and 29 indicated medium-level social support, and scores above 30 indicated high-level social support (25, 26).
The Chinese version of the 12-item Short Form Survey (SF-12) was used to measure QoL. The SF-12 is a self-reported questionnaire that includes eight domains and two summary components. The domains assessed by the SF-12 include general health (GH), physical functioning (PF), role-physical (RP), bodily pain (BP), role-emotional (RE), mental health (MH), vitality (VT), and social functioning (SF). The two summary components are the physical component summary (PCS) and the mental component summary (MCS), respectively (27). The reliability and validity of the Chinese version of the SF-12 have been confirmed and found to be comparable to those of the Chinese version of the SF-36 (28).
Statistical analysis
A post-hoc power analysis was conducted to ensure statistical power for sample size calculation by G*power version 3.1. Statistical analyses were conducted using IBM SPSS Statistics version 25.0. Continuous variables were presented as mean ± standard deviation, and categorical variables were expressed as percentages. Associations between relevant factors and study outcomes were reported as odds ratios (OR) with 95% confidence intervals (95% C.I.). Continuous variables were compared using independent t-tests. Categorical variables were compared using the chi-square test or Fisher’s exact test as appropriate. Independent factors associated with anxiety prior to gastrointestinal endoscopy were analyzed using logistic regression analysis. P< 0.05 was considered statistically significant.
Results
Incidence of anxiety before gastrointestinal endoscopy
A total of 504 patients who underwent gastrointestinal endoscopy were enrolled in this study, of whom 482 completed the questionnaires (power is 0.9126). Among them, 236 (48.96%) were male and 246 (51.04%) were female. The participants’ age ranged from 18 to 80 years, with a mean age of 44.21 ± 13.751 years.
The overall prevalence of anxiety before gastrointestinal endoscopy was 34.44%. Among the patients who experienced anxiety prior to the procedure, 124 (74.70%) had mild anxiety, 30 (18.07%) had moderate anxiety, and 12 (7.23%) had severe anxiety.
Social factors, lifestyles, and anxiety before gastrointestinal endoscopy
Various demographic and social factors, including gender, age, and level of social support, were found to significantly influence the incidence of anxiety before gastrointestinal endoscopy (all P<0.05). In addition, unhealthy lifestyle factors such as poor sleep quality were also associated with higher anxiety levels (P< 0.05). However, smoking and alcohol consumption did not show a significant association with anxiety (all P> 0.05) (Table 1).
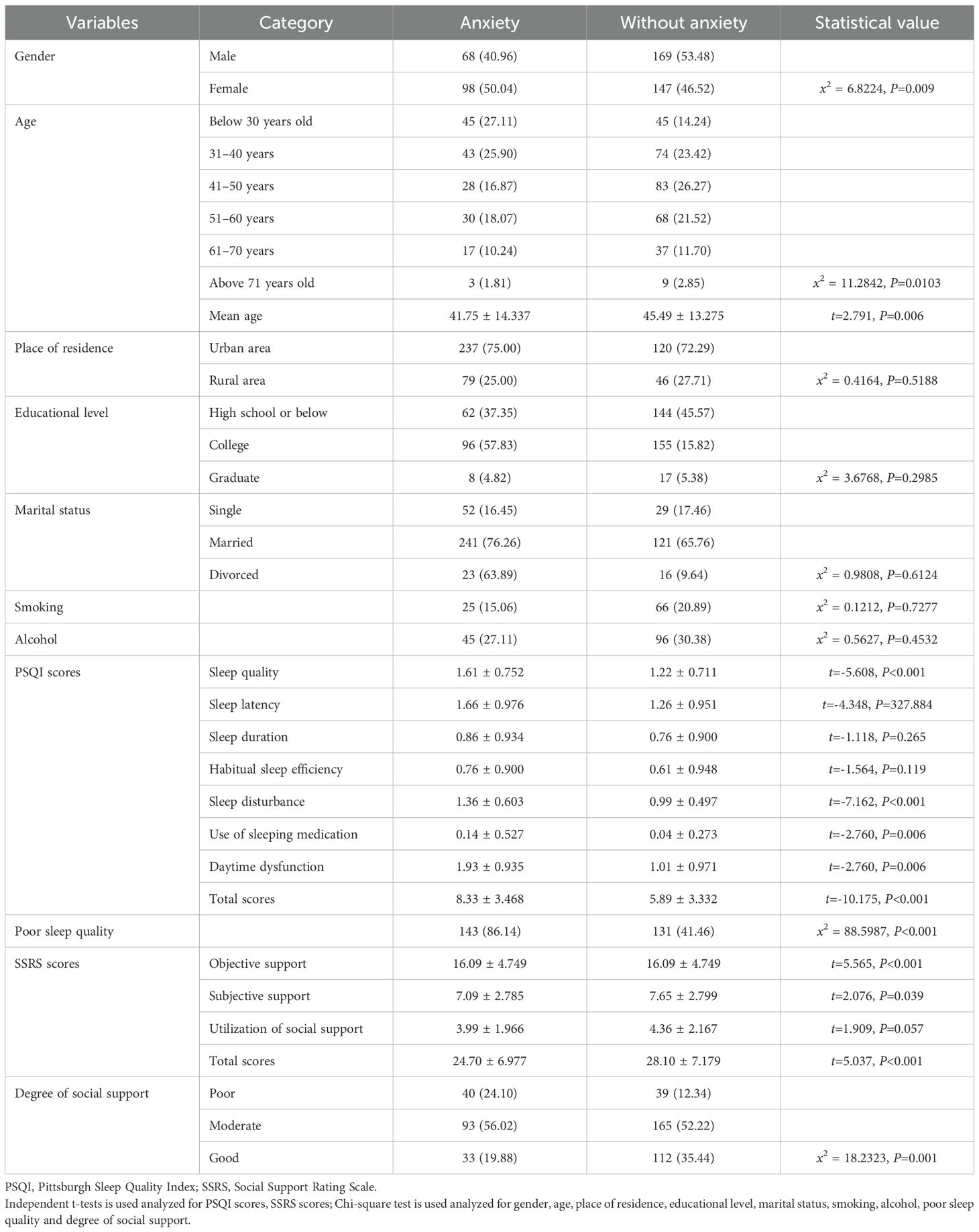
Table 1. Demographic, social factors and lifestyles in anxiety before gastrointestinal endoscopy [x ± s/n(%)].
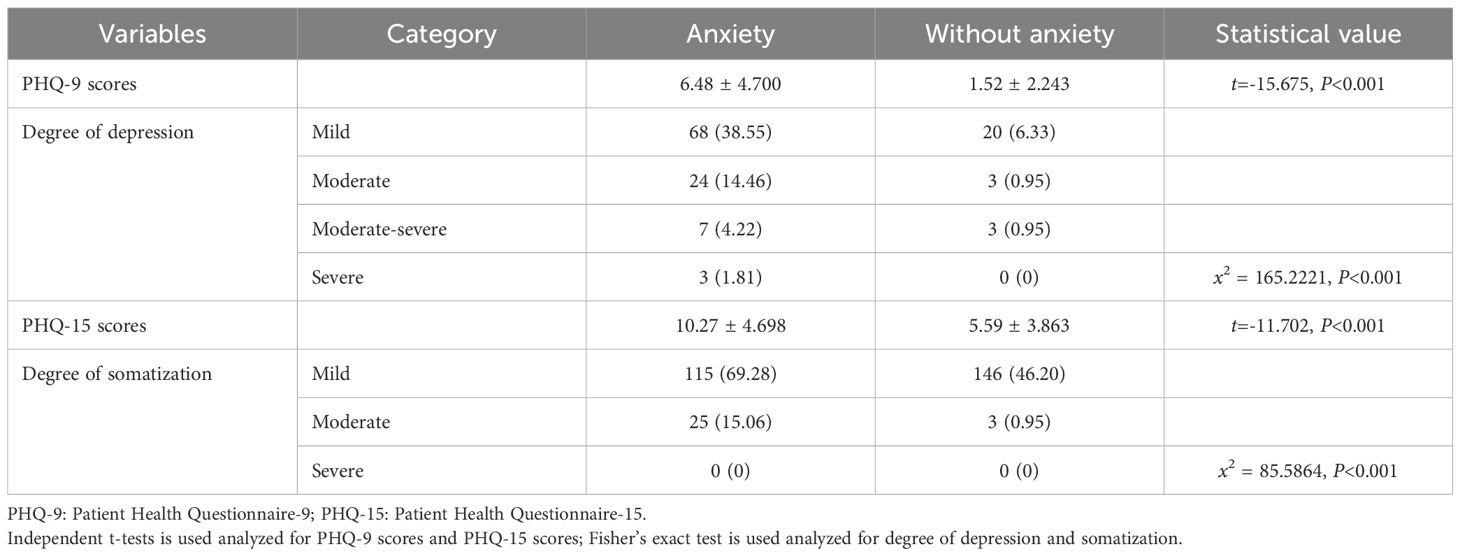
Psychological factors and anxiety before gastrointestinal endoscopy
This study confirmed that psychological factors, specifically depression and somatization, significantly affected the incidence of anxiety before gastrointestinal endoscopy (all P<0.05). Most patients who experienced anxiety were also found to suffer from mild depression and mild somatization (all P<0.05) (Table 2).
Physiological and endoscopy-related factors and anxiety before gastrointestinal endoscopy
In this study, physiological and endoscopy-related factors, including family history of digestive diseases, H. pylori infection, the number of previous endoscopies, whether the procedure was performed under sedation, type of endoscopy performed, and the endoscopic diagnosis, were not significantly associated with anxiety before gastrointestinal endoscopy (all P>0.05) (Table 3).
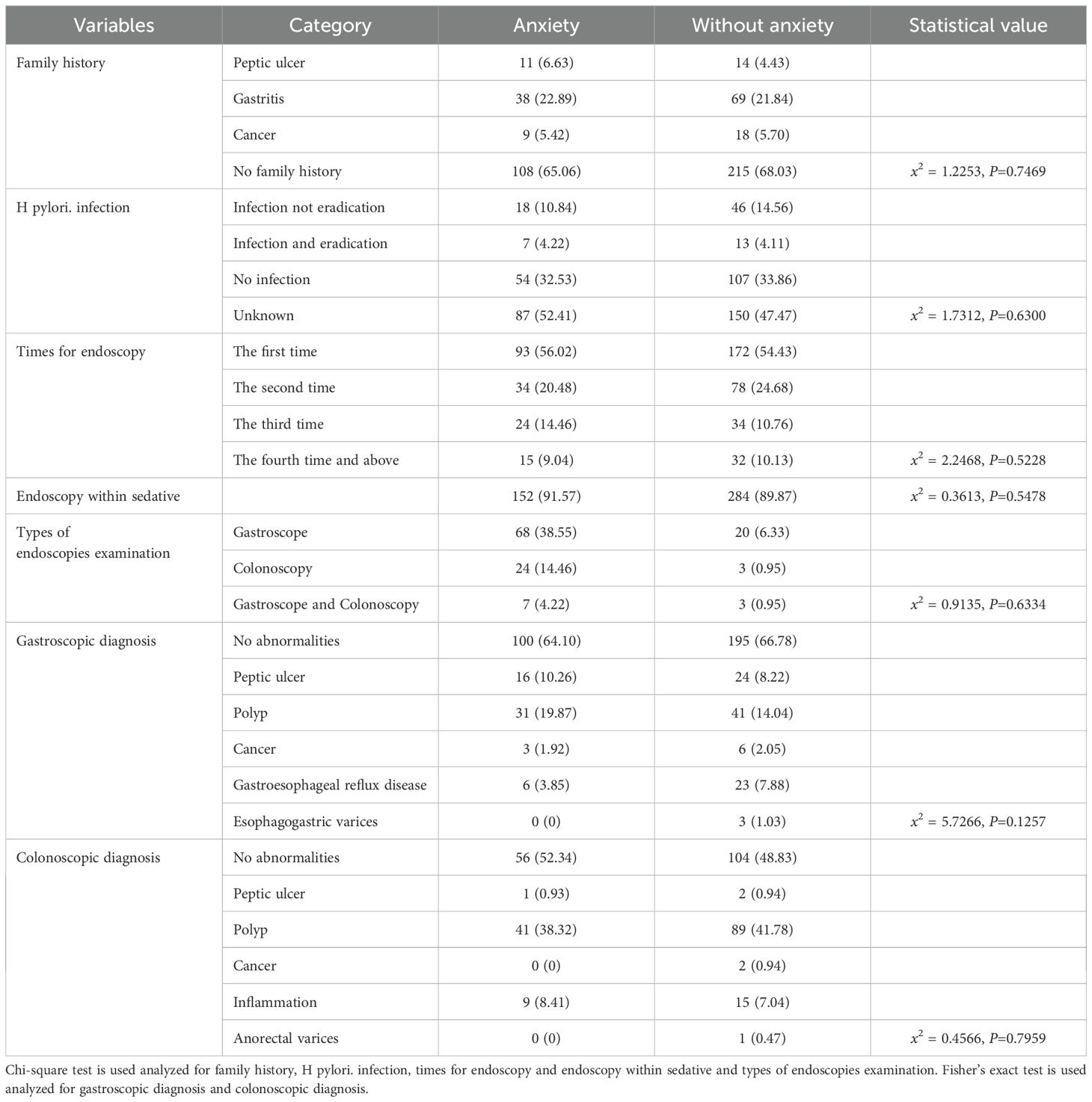
Table 3. Physiological and endoscopic related factors in anxiety before gastrointestinal endoscopy [n(%)].
Relevant independent factors for anxiety before gastrointestinal endoscopy
Gender (OR=1.657, 95%C.I. 1.133-2.423), age (OR=0.967, 95%C.I. 0.952-0.983), PSQI scores (OR=1.258, 95%C.I. 1.180-1.342), SSRS scores (OR=0.951, 95%C.I. 0.923-0.980), PHQ-9 scores (OR=1.115, 95%C.I. 1.045-1.188) and PHQ-15 scores (OR=1.490, 95%C.I. 1.350-1.645) were all identified as independent factors associated with anxiety before gastrointestinal endoscopy (all P<0.05) (Table 4).
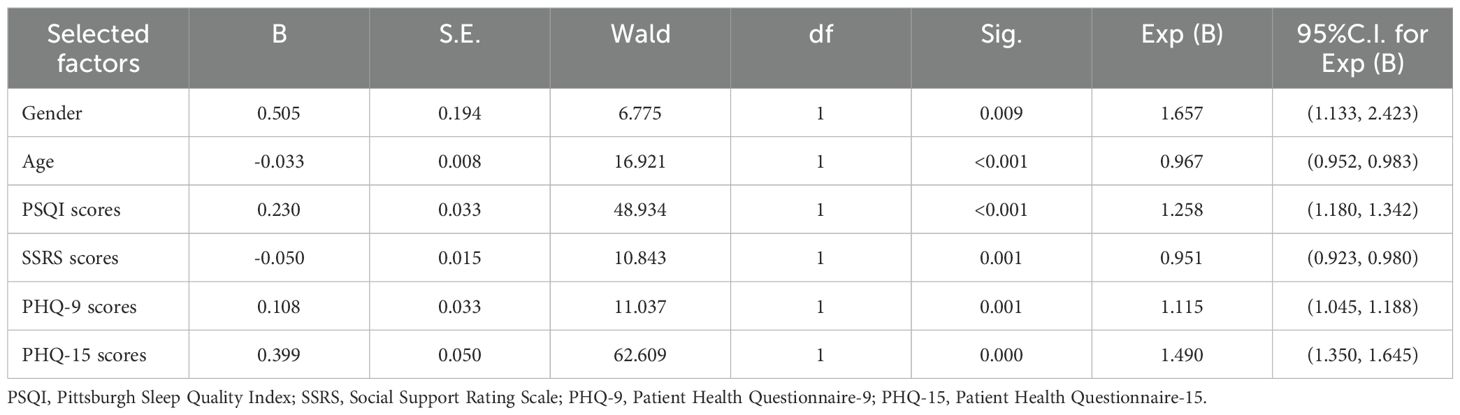
Table 4. Logistic regression analyses on selected factors associated with anxiety before gastrointestinal endoscopy.
Correlation between independent factors and varying levels of anxiety before gastrointestinal endoscopy
This study also demonstrated that age, PSQI scores, PHQ-9 scores, and PHQ-15 scores were all positively correlated with varying levels of anxiety among patients who underwent gastrointestinal endoscopy. The correlation coefficients (r) were -1.51, 0.173, 0.466, and 0.407, respectively, with corresponding P values of 0.001, 0.026, <0.001, and <0.001. However, there were no statistically significant correlations between anxiety levels and SSRS scores (r= -0.047, P= 0.448) (Figure 1).
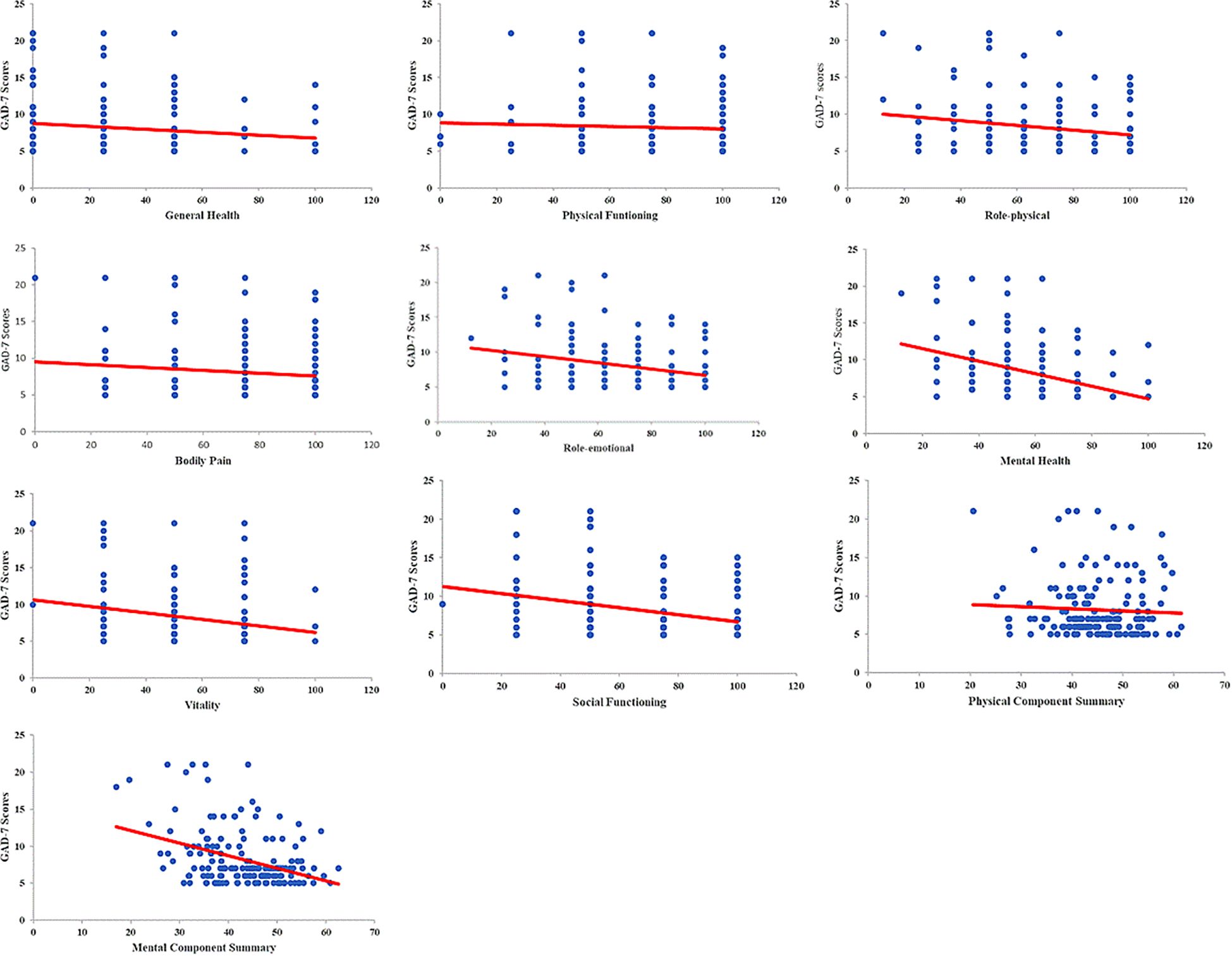
Figure 1. Correlation between QoL and varying levels of anxiety before gastrointestinal endoscopy. Scores among multiple domains of QoL, including GH, RP, RE, MH, VT, SF, and the scores of components in MCS, were negatively correlated with varying levels of anxiety among patients undergoing gastrointestinal endoscopy (r value were -0.164, -0.167, -0.192, -0.362, -0.216, -0.212 and -0.313, respectively; all P<0.05). There were no statistically significant correlations between anxiety levels among PF, BP and PCS (r value were -0.065, -0.049 and -0.039, respectively; all P>0.05).
Anxiety before gastrointestinal endoscopy and QoL
Patients who experienced anxiety prior to gastrointestinal endoscopy showed significantly lower QoL scores. All domains of QoL, including GH, PF, RP, BP, RE, MH, VT, SF, as well as the summary components PCS and MCS, were significantly reduced in patients with anxiety compared to those without (all P<0.05) (Table 5).
Correlation between QoL and varying levels of anxiety before gastrointestinal endoscopy
Scores among multiple domains of QoL, including GH, RP, RE, MH, VT, SF, and the scores of components in MCS, were negatively correlated with varying levels of anxiety among patients undergoing gastrointestinal endoscopy (all P<0.05). The more severe the anxiety, the lower the QoL scores observed (Figure 2).
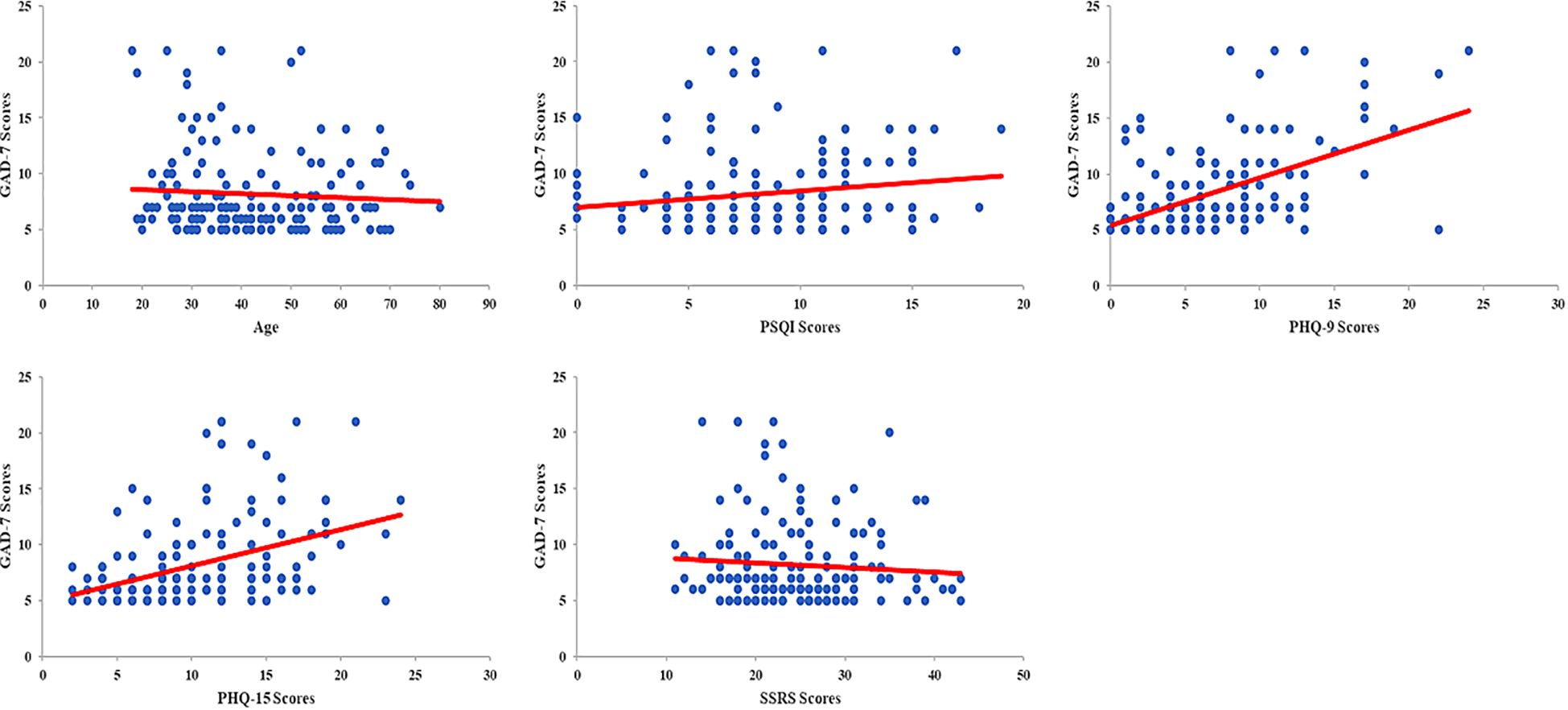
Figure 2. Correlation between independent factors and varying levels of anxiety before gastrointestinal endoscopy. Age, PSQI scores, PHQ-9 scores, and PHQ-15 scores were all positively correlated with varying levels of anxiety among patients who underwent gastrointestinal endoscopy (r value were -1.51, 0.173, 0.466, and 0.407, respectively; all P<0.05). There were no statistically significant correlations between anxiety levels and SSRS scores (r=-0.047, P= 0.448).
Discussion
Patients preparing to undergo invasive medical procedures such as gastrointestinal endoscopy frequently experience psychological distress, most commonly in the form of anxiety (29, 30). Globally, anxiety before gastrointestinal endoscopy is highly prevalent. Previous studies have reported rates ranging from 21.52% to over 50% among patients undergoing these procedures (17, 31). In this study, 34.44% of patients experienced anxiety before gastrointestinal endoscopy. Pre-procedural anxiety may reduce patient compliance and increase the risk of adverse events during or after the procedure (32). Therefore, identifying the contributing factors to this anxiety is critical to improving clinical outcomes.
Social-psychological factors are recognized as important pathogenic contributors to a wide range of diseases, particularly mental and mood disorders, such as bipolar disorder and suicidal behavior (33, 34). According to TOUS, psychological and environmental factors may induce the onset of unpleasant symptoms, including anxiety (12, 13, 35). In this study, we have confirmed that social-psychological factors such as social support, depression, and somatization had a significant impact on anxiety levels before gastrointestinal endoscopy. Furthermore, patients with unhealthy lifestyles, particularly those experiencing poor sleep quality, were more likely to suffer from pre-procedural anxiety. Recent research has suggested that sleep quality is closely associated with anxiety, potentially through mechanisms involving altered function of GABAergic neurons in the bed nucleus of the stria terminalis (36, 37).
According to the TOUS, physiological, psychological, and environmental factors all significantly contribute to the occurrence of unpleasant symptoms (12, 13, 35). In this study, we demonstrated that gender and age influenced the incidence of anxiety before undergoing gastrointestinal endoscopy. Differentiation of gender roles, disadvantage and disempowerment across the life course, and the coping styles of female that have an impact on female who was easy to suffer from anxiety (38). For the young age participants who underwent gastrointestinal endoscopy that were within negative health-related behaviors and would base on a false assumption with life-limiting conditions, that all would induce varying levels of anxiety (39, 40). However, other physiological and endoscopy-related factors, including family history of digestive diseases, H. pylori infection, number of previous endoscopies, use of sedation, type of endoscopic procedure, and diagnostic outcomes, did not show a significant impact on anxiety in this context, it may due to the sample homogeneity among participants. Anxiety, as a negative mood state, can be influenced by a range of physiological, psychological, and environmental factors (41–43). Additionally, individual differences in physiological, psychological, and social-environmental factors may shape one’s cognitive appraisal of invasive medical procedures. These differences in perceived acceptability may, in turn, lead to pre-procedural anxiety (44, 45). In this study, we identified gender, age, sleep quality, social support, depression, and somatization as independent predictors of anxiety before gastrointestinal endoscopy. Furthermore, PSQI, PHQ-9, and PHQ-15 scores were all positively correlated with varying levels of anxiety, confirming their relevance in evaluating psychological distress in this patient population.
Meanwhile, patients who experienced anxiety before undergoing gastrointestinal endoscopy also showed decreased QoL, representing one of the adverse outcomes associated with unpleasant symptoms (12, 13, 35). In this study, we confirmed that all QoL domains, both physical and mental components, were significantly lower in patients with anxiety. In particular, domains such as GH, RP, RE, MH, VT, SF, and MCS were negatively correlated with varying levels of anxiety prior to gastrointestinal endoscopy. Several studies have similarly reported that anxiety symptoms may impair physical functioning and that they are strongly associated with reduced QoL, especially in the physical dimensions. Moreover, as a negative mood state, anxiety tends to exert a more pronounced impact on the mental dimensions of QoL (46–48).
This study had several limitations. First, as a self-reported questionnaire-based survey, there is a possibility of memory bias or inaccuracies in the data provided by participants. Second, the study was conducted at a single center with a limited sample size, which may affect the generalizability of the findings. Further multicenter studies with larger samples are needed to validate these results.
In conclusion, this study confirmed a high prevalence of anxiety before gastrointestinal endoscopy. Socio-psychological factors played a significant role in the development of pre-procedural anxiety. Additionally, patients experiencing anxiety prior to endoscopy demonstrated reduced quality of life. These findings suggest that endoscopists, gastroenterologists, and GI nurses should pay close attention to patients at risk of anxiety before endoscopy in order to prevent adverse procedural outcomes and promote better recovery.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the institutional ethical committee of hospital affiliated to Guangxi University of Chinese medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
Z-PH: Formal analysis, Supervision, Writing – original draft, Methodology, Software, Data curation, Writing – review & editing, Project administration, Conceptualization, Resources, Visualization, Validation, Investigation, Funding acquisition. K-JQ: Data curation, Investigation, Writing – review & editing. B-BW: Data curation, Visualization, Validation, Supervision, Funding acquisition, Writing – review & editing, Software, Resources, Project administration. J-FL: Investigation, Writing – review & editing. TL: Investigation, Writing – review & editing. L-PY: Investigation, Writing – review & editing. L-PM: Writing – review & editing, Investigation.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study is supported by Guangxi University of Chinese Medicine Doctoral Research Funding Project (No. 2022BS015).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mezoff EA, Williams KC, and Erdman SH. Gastrointestinal endoscopy in the neonate. Clin Perinatol. (2020) 47:413–22. doi: 10.1016/j.clp.2020.02.012
2. Labaki C, Uche-Anya EN, and Berzin TM. Artificial intelligence in gastrointestinal endoscopy. Gastroenterol Clin North Am. (2024) 53:773–86. doi: 10.1016/j.gtc.2024.08.005
3. Manfredi G, Pedaci M, Iiritano E, Alicante S, Romeo S, Bertè R, et al. Impact of improved upper endoscopy quality on detection of gastric precancerous lesions. Eur J Gastroenterol Hepatol. (2023) 35:285–7. doi: 10.1097/MEG.0000000000002513
4. Sung JJ, Ng SC, Chan FK, Chiu HM, Kim HS, Matsuda T, et al. An updated Asia Pacific Consensus Recommendations on colorectal cancer screening. Gut. (2015) 64:121–32. doi: 10.1136/gutjnl-2013-306503
5. Albayrak T, Torun Göktaş A, Eyüpoğlu S, Muhtaroğlu A, and Dulger AC. Patient anxiety in endoscopy: A comparative analysis of single vs. Dual Procedure Effects. Cureus. (2024) 16:e57237. doi: 10.7759/cureus.57237
6. Yu X, Deng H, Xiong Z, Gong P, Ye M, Liu T, et al. A scale to measure the worry level in Gastrointestinal Endoscopy with sedation: Development, reliability, and validity. Int J Clin Health Psychol. (2023) 23:100410. doi: 10.1016/j.ijchp.2023.100410
7. Pontone S, Lauriola M, Palma R, Panetta C, Tomai M, and Baker R. Do difficulties in emotional processing predict procedure pain and shape the patient’s colonoscopy experience? BMJ Open. (2022) 12:e050544. doi: 10.1136/bmjopen-2021-050544
8. Sargin M, Uluer MS, Aydogan E, Hanedan B, Tepe Mİ, Eryılmaz MA, et al. Anxiety levels in patients undergoing sedation for elective upper gastrointestinal endoscopy and colonoscopy. Med Arch. (2016) 70:112–5. doi: 10.5455/medarh.2016.70.112-115
9. Fumincelli L, Mazzo A, Martins JCA, and Mendes IAC. Quality of life and ethics: A concept analysis. Nurs Ethics. (2019) 26:61–70. doi: 10.1177/0969733016689815
10. Freitas PHB, Meireles AL, Ribeiro IKDS, Abreu MNS, Paula W, and Cardoso CS. Symptoms of depression, anxiety and stress in health students and impact on quality of life. Rev Lat Am Enfermagem. (2023) 31:e3884. doi: 10.1590/1518-8345.6315.3885
11. Yang JP, Qu J, Sun K, and Gao LL. Anxiety symptoms and health-related quality of life in mainland Chinese pregnant women: a cross-sectional study. J Reprod Infant Psychol. (2023) 41:3–14. doi: 10.1080/02646838.2021.1952553
12. Lenz ER, Suppe F, Gift AG, Pugh LC, and Milligan RA. Collaborative development of middle-range nursing theories: toward a theory of unpleasant symptoms. ANS Adv Nurs Sci. (1995) 17:1–13. doi: 10.1097/00012272-199503000-00003
13. Lenz ER, Pugh LC, Milligan RA, Gift A, and Suppe F. The middle-range theory of unpleasant symptoms: an update. ANS Adv Nurs Sci. (1997) 19:14–27. doi: 10.1097/00012272-199703000-00003
14. Huang ZP, Wang K, Duan YH, and Yang G. Correlation between lifestyle and social factors in functional dyspepsia among college freshmen. J Int Med Res. (2020) 48:300060520939702. doi: 10.1177/0300060520939702
15. Huang ZP, Yang XF, Lan LS, Liu T, Liu CL, Li JL, et al. Correlation between social factors and anxiety-depression in function dyspepsia: do relationships exist? Prz Gastroenterol. (2014) 9:348–53. doi: 10.5114/pg.2014.47897
16. Huang ZP, Li SM, Shen T, and Zhang YY. Correlation between sleep impairment and functional dyspepsia. J Int Med Res. (2020) 48:300060520937164. doi: 10.1177/0300060520937164
17. Yang C, Sriranjan V, Abou-Setta AM, Poluha W, Walker JR, and Singh H. Anxiety associated with colonoscopy and flexible sigmoidoscopy: A systematic review. Am J Gastroenterol. (2018) 113:1810–8. doi: 10.1038/s41395-018-0398-8
18. Wang X and Ji X. Sample size estimation in clinical research: from randomized controlled trials to observational studies. Chest. (2020) 158:S12–20. doi: 10.1016/j.chest.2020.03.010
19. Spitzer RL, Kroenke K, Williams JB, and Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
20. Kroenke K, Spitzer RL, and Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
21. Kroenke K, Spitzer RL, and Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. (2002) 64:258–66. doi: 10.1097/00006842-200203000-00008
22. Lee S, Ma YL, and Tsang A. Psychometric properties of the Chinese 15-item patient health questionnaire in the general population of Hong Kong. J Psychosom Res. (2011) 71:69–73. doi: 10.1016/j.jpsychores.2011.01.016
23. Buysse DJ, Reynolds CF, Monk TH, Berman SR, and Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
24. Ho KY, Lam KKW, Xia W, Chung JOK, Cheung AT, Ho LLK, et al. Psychometric properties of the Chinese version of the Pittsburgh Sleep Quality Index (PSQI) among Hong Kong Chinese childhood cancer survivors. Health Qual Life Outcomes. (2021) 19:176. doi: 10.1186/s12955-021-01803-y
25. Qi M, Zhou SJ, Guo ZC, Zhang LG, Min HJ, Li XM, et al. The effect of social support on mental health in chinese adolescents during the outbreak of COVID-19. J Adolesc Health. (2020) 67:514–8. doi: 10.1016/j.jadohealth.2020.07.001
26. Wang L, Luo J, Li Y, Zhou Y, and Wang W. Social support, anxiety, and depression in patients with prostate cancer: complete mediation of self-efficacy. Support Care Cancer. (2022) 30:6851–6. doi: 10.1007/s00520-022-07065-8
27. Ware J, Kosinski M, and Keller SD. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care. (1996) 34:220–33. doi: 10.1097/00005650-199603000-00003
28. Lin Y, Yu Y, Zeng J, Zhao X, and Wan C. Comparing the reliability and validity of the SF-36 and SF-12 in measuring quality of life among adolescents in China: a large sample cross-sectional study. Health Qual Life Outcomes. (2020) 18:360. doi: 10.1186/s12955-020-01605-8
29. Jain A, Jain R, Nugent Z, Solati Z, Davidson D, Shafer LA, et al. Improving colonoscopy bowel preparation and reducing patient anxiety through recently developed online information resource: A cross-sectional study. J Can Assoc Gastroenterol. (2022) 5:161–8. doi: 10.1093/jcag/gwab047
30. Moline LR. Patient psychologic preparation for invasive procedures: an integrative review. J Vasc Nurs. (2000) 18:117–22. doi: 10.1067/mvn.2000.111640
31. Cheng Y, Zhong C, Wu W, Xi X, Luo M, Chen Y, et al. Association between anxiety, depression, and bowel air bubbles at colonoscopy: a prospective observational study. Ann Palliat Med. (2021) 10:3247–57. doi: 10.21037/apm-21-540
32. Chen YS, Feng GH, Yue QQ, Wang YF, Liu M, Zhao KH, et al. Effects of non-pharmacological interventions on anxiety in patients undergoing colonoscopy: A network meta-analysis of randomized controlled trials. J Psychosom Res. (2025) 191:112065. doi: 10.1016/j.jpsychores.2025.112065
33. Orhan M, Huijser J, Korten N, Paans N, Regeer E, Sonnenberg C, et al. The influence of social, psychological, and cognitive factors on the clinical course in older patients with bipolar disorder. Int J Geriatr Psychiatry. (2021) 36:342–8. doi: 10.1002/gps.5431
34. Wang JY, Chu J, Sun SH, Zhang J, Guo XL, and Jia CX. Social psychological factors and suicidal intent among suicide attempters in rural China: A path analysis. J Nerv Ment Dis. (2017) 205:48–53. doi: 10.1097/NMD.0000000000000628
35. Blakeman JR. An integrative review of the theory of unpleasant symptoms. J Adv Nurs. (2019) 75:946–61. doi: 10.1111/jan.13906
36. Li Y, Li G, Liu L, and Wu H. Correlations between mobile phone addiction and anxiety, depression, impulsivity, and poor sleep quality among college students: A systematic review and meta-analysis. J Behav Addict. (2020) 9:551–71. doi: 10.1556/2006.2020.00057
37. Kodani S, Soya S, and Sakurai T. Excitation of GABAergic neurons in the bed nucleus of the stria terminalis triggers immediate transition from non-rapid eye movement sleep to wakefulness in mice. J Neurosci. (2017) 37:7164–76. doi: 10.1523/JNEUROSCI.0245-17.2017
38. Kiely KM, Brady B, and Byles J. Gender, mental health and ageing. Maturitas. (2019) 129:76–84. doi: 10.1016/j.maturitas.2019.09.004
39. Barker MM, Beresford B, and Fraser LK. Incidence of anxiety and depression in children and young people with life-limiting conditions. Pediatr Res. (2023) 93:2081–90. doi: 10.1038/s41390-022-02370-8
40. Ramón-Arbués E, Sagarra-Romero L, Echániz-Serrano E, Granada-López JM, Cobos-Rincón A, Juárez-Vela R, et al. Health-related behaviors and symptoms of anxiety and depression in Spanish nursing students: an observational study. Front Public Health. (2023) 11:1265775. doi: 10.3389/fpubh.2023.1265775
41. Sharpley CF, Bitsika V, McMillan ME, and Agnew LL. Physiological, psychosocial, and environmental factors in depression among autistic girls. Int J Dev Neurosci. (2021) 81:502–9. doi: 10.1002/jdn.10122
42. Leyva-Vela B, Jesús Llorente-Cantarero F, Henarejos-Alarcón S, and Martínez-Rodríguez A. Psychosocial and physiological risks of shift work in nurses: a cross-sectional study. Cent Eur J Public Health. (2018) 26:183–9. doi: 10.21101/cejph.a4817
43. Engert V, Linz R, and Grant JA. Embodied stress: The physiological resonance of psychosocial stress. Psychoneuroendocrinology. (2019) 105:138–46. doi: 10.1016/j.psyneuen.2018.12.221
44. Profit DD. Describing and predicting preprocedural anxiety in patients scheduled for advanced gastrointestinal endoscopy during the COVID-19 pandemic. Gastroenterol Nurs. (2023) 46:475–88. doi: 10.1097/SGA.0000000000000766
45. Jones MP, Ebert CC, Sloan T, Spanier J, Bansal A, Howden CW, et al. Patient anxiety and elective gastrointestinal endoscopy. J Clin Gastroenterol. (2004) 38:35–40. doi: 10.1097/00004836-200401000-00009
46. Muthukrishnan A, Tayyib NA, Alsolami FJ, Ramaiah P, and Lathamangeswaric C. Anxiety and quality of life outcomes after coronary artery bypass graft surgery - A prospective cohort study. Curr Probl Cardiol. (2023) 48:101474. doi: 10.1016/j.cpcardiol.2022.101474
47. Roeper M, Hoermann H, Salimi Dafsari R, Koestner F, Mayatepek E, Kummer S, et al. Anxiety, depression, and quality of life in parents of children with congenital hyperinsulinism. Eur J Pediatr. (2022) 181:2779–88. doi: 10.1007/s00431-022-04486-9
Keywords: social factors, psychological factors, anxiety, gastrointestinal endoscopy, quality of life
Citation: Huang Z-p, Quan K-j, Wen B-b, Lin J-f, Liu T, Yang L-p and Meng L-p (2025) Impact of social-psychological factors on anxiety before gastrointestinal endoscopy and quality of life. Front. Psychiatry 16:1624437. doi: 10.3389/fpsyt.2025.1624437
Received: 07 May 2025; Accepted: 21 July 2025;
Published: 20 August 2025.
Edited by:
Guangxi Zhou, Jining Medical University, ChinaReviewed by:
Jian Liu, Renmin Hospital of Wuhan University, ChinaKunqiao Hong, The First People’s Hospital of Yunnan Province, China
Copyright © 2025 Huang, Quan, Wen, Lin, Liu, Yang and Meng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhen-peng Huang, aHVhbmdfemhlbnBlbmdAMTI2LmNvbQ==
†These authors have contributed equally to this work
 Zhen-peng Huang
Zhen-peng Huang Kong-jin Quan
Kong-jin Quan Bin-bin Wen1†
Bin-bin Wen1†