- Department of Psychology, Jeonbuk National University, Jeonju, Republic of Korea
Background: Interoception is the ability to perceive and integrate internal sensations. A key component of interoception, body trust, involves trusting internal sensations in daily life and feeling safe within one’s own body. Problems in body trust are linked to psychological disorders, including eating disorders and suicidal behaviors. However, existing tools for measuring body trust have several limitations, and the most recently developed promising instrument to address these issues is the Body Trust Scale (BTS). This study aimed to validate the Korean version of the BTS in a sample of Korean adults.
Methods: A total of 775 participants completed the BTS and other measures of positive body image, interoceptive sensibility, body investment, eating pathology, visceral sensitivity, self-harm behaviors, and suicidal ideation. The reliability, factor structure, invariance across age groups and gender, convergent validity, and discriminant validity of the BTS were examined.
Results: Results revealed that the Korean version of BTS has a three-factor structure consistent with the original scale. It also demonstrated good internal consistency, as well as convergent and discriminant validity. Partial scalar invariance across age groups and full measurement invariance across gender were also established.
Conclusion: The Korean version of the BTS is a reliable and valid instrument for measuring body trust in Korean adults. It is expected to have clinical utility for assessing body trust, with a specific focus on eating pathology and suicide risk.
1 Introduction
Interoception refers to the ability to perceive, attend to, and integrate internal bodily sensations (1), which occurs through communication between the body and brain (2). It includes various internal processes like heart rate, sensations of warmth, digestive signals (e.g., satiety, hunger), and pain experienced in the body (3). Interoception can be experienced both consciously and unconsciously (4, 5) and plays a crucial role in maintaining homeostasis (6). Garfinkel et al. (7) divided interoception into three dimensions: interoceptive accuracy, interoceptive sensibility, and interoceptive awareness. Interoceptive accuracy refers to the ability to objectively identify internal sensations. Recently, it has also been called interoceptive sensitivity (4). Interoceptive sensibility refers to the subjective belief in one’s ability to detect and process internal sensations, which can be measured through self-reports. Interoceptive awareness represents a metacognitive insight into one’s interoceptive accuracy, specifically the correspondence between physiological accuracy and subjective evaluation.
People experience interoception at every moment. However, some individuals have low interoceptive sensitivity that makes it difficult to recognize their bodily states, while others are overly sensitive and experience problems due to negatively interpreting bodily sensations (5). Such interoceptive dysfunction has been associated with various psychopathologies (2, 5, 8). For example, interoceptive dysfunction can lead to a disconnection from the body and a perception of it as an object rather than a human being, increasing the risk of self-harm behaviors (9, 10). Similarly, impairment in gastric interoception can distort the perception of satiety, potentially leading to binge eating or avoidance of food intake (11). Martin et al. (12) conducted a systematic review and revealed that interoceptive deficit is a commonly observed clinical feature in eating disorders. Thus, interoceptive dysfunction is considered a key mechanism underlying eating disorders and suicidality (13, 14).
Mehling et al. (4, 15) identified that interoceptive sensibility comprises eight dimensions, thereby demonstrating that interoception is a multidimensional construct. One of these dimensions, body trust, is particularly prominent in psychopathology (13, 16). Body trust refers to trusting one’s bodily sensations, feeling safe and comfortable in one’s body (4, 17), and valuing body ownership, which helps distinguish one’s own body from others and the external environment (16, 18).
Individuals with decreased body trust tend to rely on external cues over internal bodily signals for self-regulation (19), which may contribute to psychological problems. According to several empirical studies, diminished body trust has been associated with suicidal ideation and suicide attempts across various populations (10, 14) and has been shown to predict self-harming behaviors (9). Grunewald et al. (16) further confirmed the predictive validity of body trust in relation to suicidal ideation. Moreover, the Trusting subscale of the Multidimensional Assessment of Interoceptive Awareness (MAIA) (15) was identified as one of the factors negatively correlated with eating disorders (20, 21). Diminished body trust in eating disorder samples bridges the relationship between interoceptive awareness and eating disorder symptoms (22), and increases the severity of suicidal ideation, whether mediated by agitation or occurring independently (23). In summary, body trust emerges as a key dimension of interoception closely linked to both eating disorders and suicidality.
Despite the significance of body trust, existing tools for measuring it are limited. In studies on body trust, the Trusting subscale of the MAIA has been widely used. However, this subscale consists of only three items and does not fully capture the multidimensional aspects of body trust. Body trust is also closely associated with positive body image and sensitivity to internal sensations (16), which can be measured using the Body Appreciation Scale-2 (BAS-2) (24) and the Visceral Sensitivity Index (VSI) (25). Nonetheless, these scales focus on only partial aspects of body trust. To overcome these limitations, Grunewald et al. (16) developed the Body Trust Scale (BTS). BTS measures body trust across three dimensions: Comfort with One’s Body (CB), Physical Attractiveness (PA), and Comfort with Internal Sensations (CIS). CB refers to trusting and feeling supported by one’s body. PA assesses the perception of one’s body as appealing in both personal and social contexts. CIS represents the ability to comfortably accept internal bodily sensations. To evaluate psychometric properties of BTS, Grunewald et al. (16) examined its factor structure, internal consistency, test-retest reliability, convergent/divergent validity, predictive validity, and measurement invariance across gender using a sample of 479 U.S. adults. The results demonstrated that the BTS has a three-factor structure, strong internal consistency, and solid validity. Test-retest reliability of BTS was significant, and measurement invariance across gender was supported.
From a cultural perspective, individuals in non-Western cultures are reported to have lower interoceptive accuracy compared to those in Western cultures (26), which may be attributed to their collectivistic thinking and context-oriented information processing styles (26, 27). A study by Lee et al. (28) examining individuals with non-psychotic depression and anxiety disorders in South Korea found that, among the MAIA subscales, the Trusting subscale showed the strongest association with anxiety. Notably, suicide is a significant social issue across all age groups in Korea (29). These findings highlight the importance of exploring the relationship between body trust and mental health within the Korean cultural context. Nevertheless, research specifically focusing on body trust in Korea remains scarce.
In addition, interoceptive ability (e.g., accuracy, sensibility) has been shown to decline with age (30, 31). For instance, Dobrushina et al. (30) reported a negative correlation between age and the Trusting subscale of the MAIA-2. This suggests the need to investigate whether the BTS functions differently across age groups. Although previous research confirmed measurement invariance of the BTS across genders (16), its measurement invariance across age groups has yet to be investigated.
Thus, our study aimed to validate a Korean version of the BTS with a Korean adult sample. We administered the BTS and other measures to a sample of Korean adults and analyzed its factor structure, reliability, and convergent/discriminant validity. Measurement invariance across age groups and gender was also examined.
2 Methods
2.1 Participants/procedure
A sample of 800 Korean adults was recruited through an online research participant system. Balanced distribution was applied based on gender and age groups: young adults (20–34 years), middle-aged adults (35–49 years), older adults (50–64 years), and seniors (65 years and over). After excluding 25 multivariate outliers identified using Mahalanobis distance (p <.001) (32), the final sample comprised 775 participants, which exceeds the recommended sample size (32, 33). The sample consisted of 387 women (49.9%) and 388 men (50.1%), and was distributed across age groups as follows: 195 young adults (25.2%), 197 middle-aged adults (25.4%), 191 older adults (24.6%), and 192 seniors (24.8%). The mean age of the sample was 49.34 years (SD = 15.26; range: 20–80 years). Participants provided informed consent and completed the survey through an online research participation system.
2.2 Measures
2.2.1 Body Trust Scale
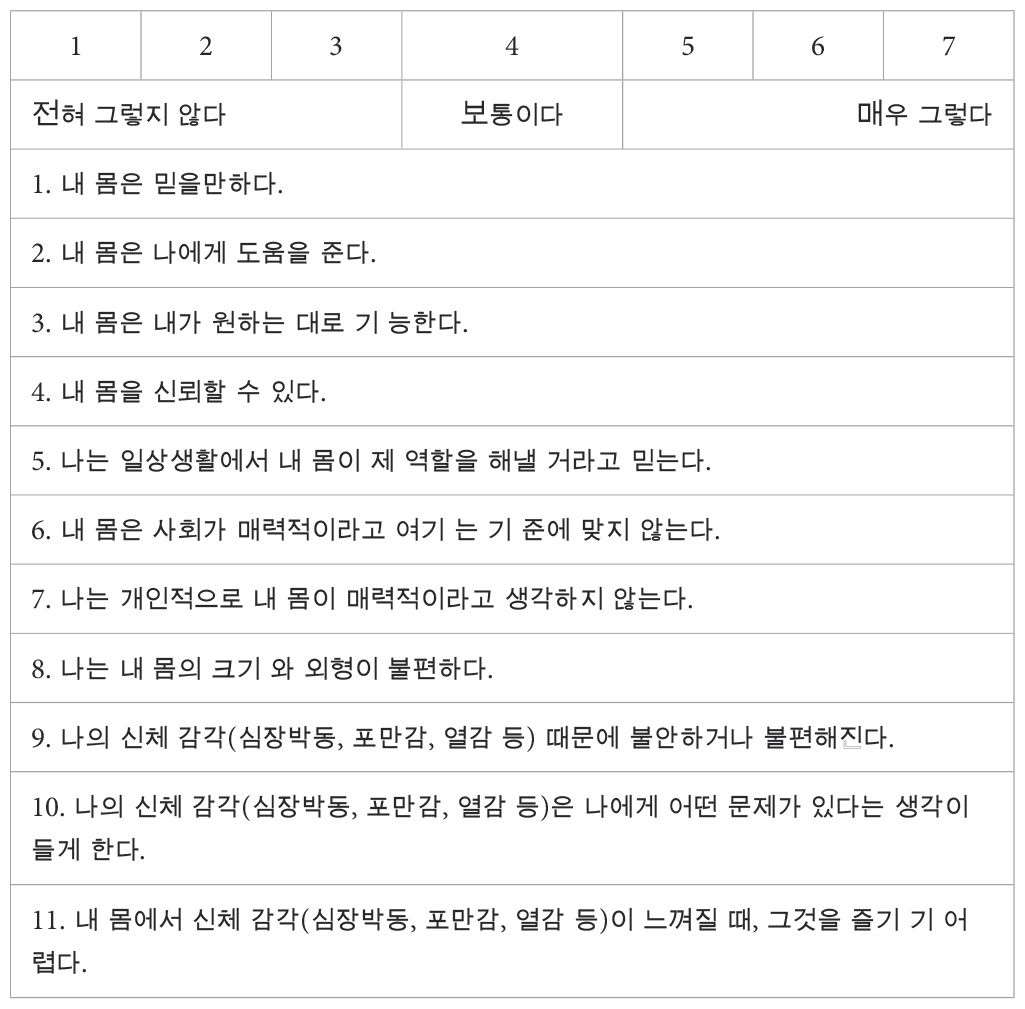
The Body Trust Scale (BTS) is an 11-item scale that assesses body trust across multiple dimensions (16). Each item is rated on a 7-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree). The original version of the BTS was translated into Korean and subsequently back-translated by the first author. Finally, the translation accuracy was verified by the authors. As part of the cultural adaptation process, the authors considered cultural characteristics of individuals in East Asian contexts, who may have difficulty attending to internal states due to their context-oriented attentional tendencies (26). To aid comprehension of physical sensations, examples such as heart rate, warmth, and satiety were included in the instructions and relevant items. These examples were based on those proposed by Grunewald et al. (3) to illustrate interoception (See Appendix).
2.2.2 Multidimensional Assessment of Interoceptive Awareness
The Multidimensional Assessment of Interoceptive Awareness (MAIA) is a 32-item measure assessing interoceptive sensibility (15). Mehling et al. (15) proposed that the MAIA has an eight-factor structure. However, Gim et al. (17) found that a six-factor structure was more suitable for the Korean version (K-MAIA) and validated its psychometric properties. The six subscales include Noticing, Accept, Attention regulation, Mind-body connection awareness, Return to body, and Trusting. Noticing captures the awareness of bodily sensations. Accept measures the tendency to accept rather than suppress or avoid negative emotions in response to unpleasant bodily sensations. Attention regulation reflects the ability to manage attention toward bodily sensations, and Mind-body connection awareness assesses the recognition of the relationship between bodily sensations and emotions. Return to body is associated with directing attention to bodily sensations to achieve functional outcomes. Finally, Trusting measures the degree to which one perceives their body as safe and reliable. The items are scored on a 7-point Likert scale (from 0 to 6), and each subscale score was calculated as the mean of its items. The internal consistency for the six subscales in this study ranged from α = .81-.92.
2.2.3 Body Appreciation Scale-2
The Body Appreciation Scale-2 (BAS-2) is a 10-item scale that assesses positive body image (24). Responses are scored using a 5-point Likert scale, ranging from 1 to 5. We used the Korean version of BAS-2, which has demonstrated good reliability and validity (34). In this study, the BAS-2 demonstrated high internal consistency (Cronbach’s α = .93).
2.2.4 Body Investment Scale
The Body Investment Scale (BIS) consists of 24 items that assess the level of emotional, cognitive, and behavioral engagement with one’s own body (35). Participants respond on a 5-point Likert scale ranging from 1 to 5. Mok (36) translated the BIS into Korean and validated its psychometric properties. In the current sample, the internal consistency for the BIS was good (Cronbach’s α = .84).
2.2.5 Visceral Sensitivity Index
The Visceral Sensitivity Index (VSI) is a 15-item self-reported measure that assesses gastrointestinal symptom-specific anxiety (25). Jang (37) translated the VSI into Korean. Items on the VSI are scored on a 6-point Likert scale, ranging from 1 (strongly agree) to 6 (strongly disagree), with total scores computed using reverse scoring. In this study, the VSI demonstrated high internal consistency (Cronbach’s α = .93).
2.2.6 Eating Disorder Inventory-Very Short
The EDI-VS is a brief 16-item version of the Eating Disorder Inventory (EDI) that assesses behaviors and personality traits associated with eating disorders (38). While the EDI-VS employs a Visual Analog Scale (VAS), we adapted it to a 6-point Likert scale (ranging from 1 = never to 6 = always) following the EDI response format (39) to ensure consistency across the measurement tools used. The adapted version was then translated into Korean. In this study, the Perfectionism (PF) subscale was excluded from the total EDI-VS score. The adjusted total score and the PF subscale were then analyzed separately to explore their distinct relationships with the BTS. The internal consistency of the EDI-VS in this study was α = .70, while the PF subscale showed α = .52. However, Maiano et al. (38) noted that each subscale consisted of only two items and was limited by its small number of items. To address this issue, they applied the Spearman-Brown prophecy formula. In line with their approach, this study also applied this formula and found that the estimated reliability for the PF subscale increased to 0.76.
2.2.7 Self-Harm Inventory
The Self-Harm Inventory (SHI) is a self-reported measure assessing various self-harm behaviors (40). We used a Korean version of the SHI, which was initially translated and validated by Kong (41) and subsequently modified by Lee (42) for use in the general population. The original SHI consists of 20 items, but item 13 was excluded as it overlapped conceptually with item 1 (43). Consequently, 19 items were used in this study. Responses are rated on a 4-point Likert scale, ranging from 1 (rarely) to 4 (always), and the internal consistency of the SHI in this study was high (Cronbach’s α = .93).
2.2.8 Depressive Symptom Inventory-Suicidality Subscale
The Depressive Symptom Inventory-Suicidality Subscale (DSI-SS) is a subscale of the Hopelessness Depression Symptom Questionnaire, consisting of 4 items (44). This scale assesses the frequency of suicidal ideation, suicide planning, perceived controllability of suicidal thoughts, and suicide-related impulses during the past two weeks. Psychometric properties of the Korean version of the DSI-SS were validated by Suh et al. (45). The DSI-SS is rated on a 4-point Likert scale (ranging from 0 to 3). For example, a score of 0 on item 4 corresponds to “I do not feel suicidal impulses (0 days)”, whereas a score of 3 corresponds to “I always feel suicidal impulses (10–14 days)”. The internal consistency for the DSI-SS in the current sample was high (Cronbach’s α = .93).
2.3 Statistical analyses
To examine the factor structure of the BTS, we conducted confirmatory factor analysis (CFA) using AMOS 22.0. Goodness of fit was tested with the root mean square error of approximation (RMSEA) and the standardized root mean square residual (SRMR) (46). According to the fit criteria proposed by Schermelleh-Engel et al. (47), an RMSEA ≤ 0.05 and an SRMR ≤ 0.05 indicate a good fit, whereas an RMSEA between 0.05 and 0.08 and an SRMR between 0.05 and 0.10 indicate an acceptable fit. The comparative fit index (CFI) (48) and the Tucker-Lewis index (TLI) (49) were also reported. According to Hu and Bentler (46), CFI and TLI values greater than 0.95 indicate a good fit. We additionally reported the goodness-of-fit index (GFI) and the adjusted goodness-of-fit index (AGFI) (50) as indicators of model fit. GFI values greater than 0.95 and AGFI values greater than 0.90 were interpreted as indicative of good fit (47). Although the chi-square test of model fit was reported, it was not considered a primary fit index due to its sensitivity to sample size (47). Further, average variance extracted (AVE) was calculated to examine convergent validity and discriminant validity within the factor structure. An AVE value of .50 or higher indicates adequate convergence, and discriminant validity is supported when the square root of the AVE for each factor exceeds its inter-factor correlations (51).
To examine whether the BTS factors were consistent across age groups and gender, we conducted a measurement invariance test using multiple-group confirmatory factor analysis. Measurement invariance was examined through the following sequential process: equivalence of factor structure, factor loadings, indicator intercepts, and latent means. At each step, the changes in CFI (ΔCFI) and RMSEA (ΔRMSEA) were examined. We followed the criteria proposed by Chen (52), who suggested that when total sample size is sufficiently large (N > 300) and the group sizes are approximately equal, measurement invariance can be inferred if ΔCFI ≤ 0.01 and ΔRMSEA ≤ 0.015. The chi-square statistics were reported but not used as a primary criterion due to its hypersensitivity and tendency to over-reject models (52).
Finally, the internal consistency of the BTS was assessed using Cronbach’s alpha, McDonald’s omega, and composite reliability (CR). Two-tailed Pearson correlations were used to analyze the relations between the BTS and the other measures in the current study. These analyses were conducted using SPSS 25.0 and jamovi 2.3.28.
3 Results
3.1 Reliability of the BTS
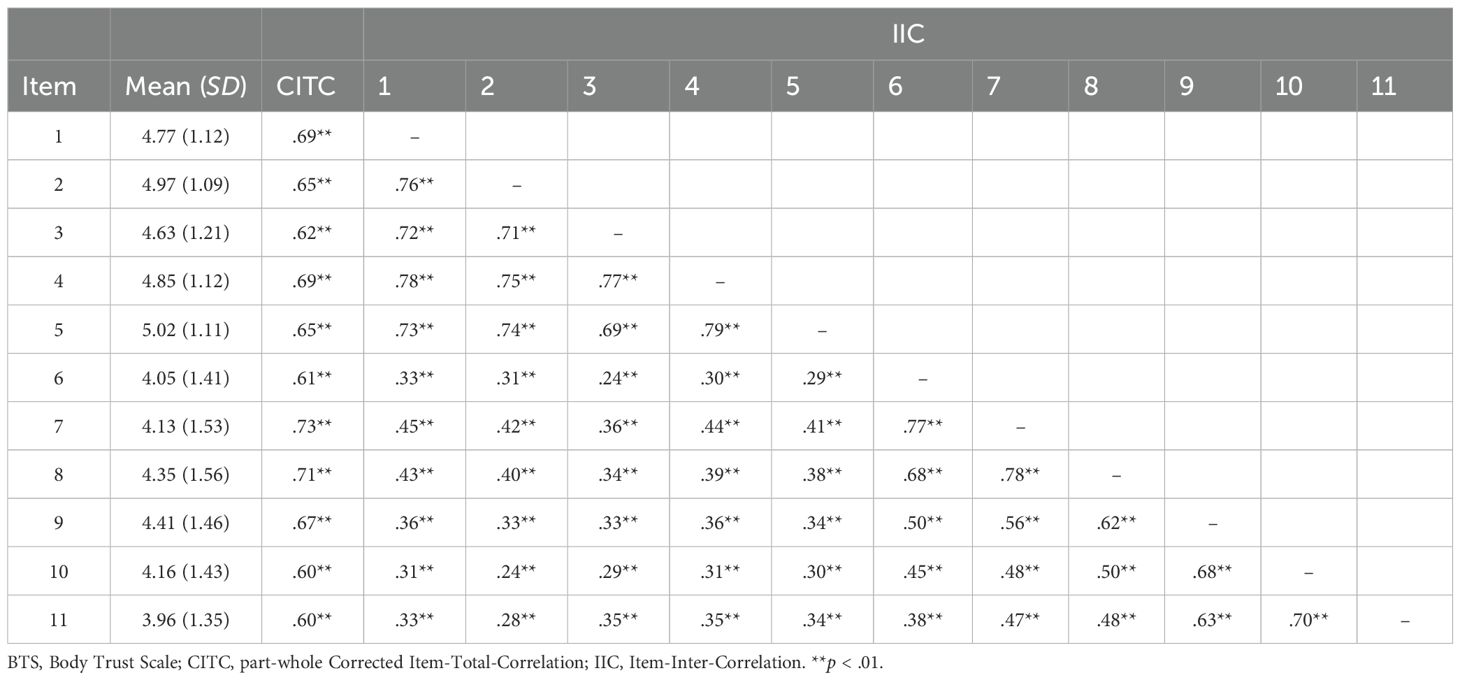
Basic psychometric properties of the BTS items are presented in Table 1. All items showed adequate part-whole corrected item-total correlations and inter-item correlations. The internal consistency of the total items of the BTS was high (Cronbach’s α = .91; McDonald’s ω = .91). The CB subscale, PA subscale, and CIS subscale of the BTS also showed overall good internal consistency (Cronbach’s α = .86 -.94; McDonald’s ω = .86 -.94; CR = .86 -.94).
3.2 Factor structure of the BTS
We conducted CFA to evaluate the original 3-factor model of the BTS proposed by Grunewald et al. (16). The model fit of the 3-factor model (N = 775) was acceptable [x2 (41) = 193.452, p <.001; CFI = 0.976; TLI = 0.968; RMSEA = 0.069; SRMR = 0.037; GFI = 0.956; AGFI = 0.929]. The measurement model of the BTS is presented in Figure 1. In addition, AVE values were calculated to assess convergent validity within the factor structure. All subscales demonstrated adequate convergent validity (CB = .744; PA = .753; CIS = .667). Discriminant validity was also supported, as the square root of the AVE for each factor (CB = .863; PA = .868; CIS = .817) was greater than inter-factor correlations, from .45 to .69 (Figure 1).
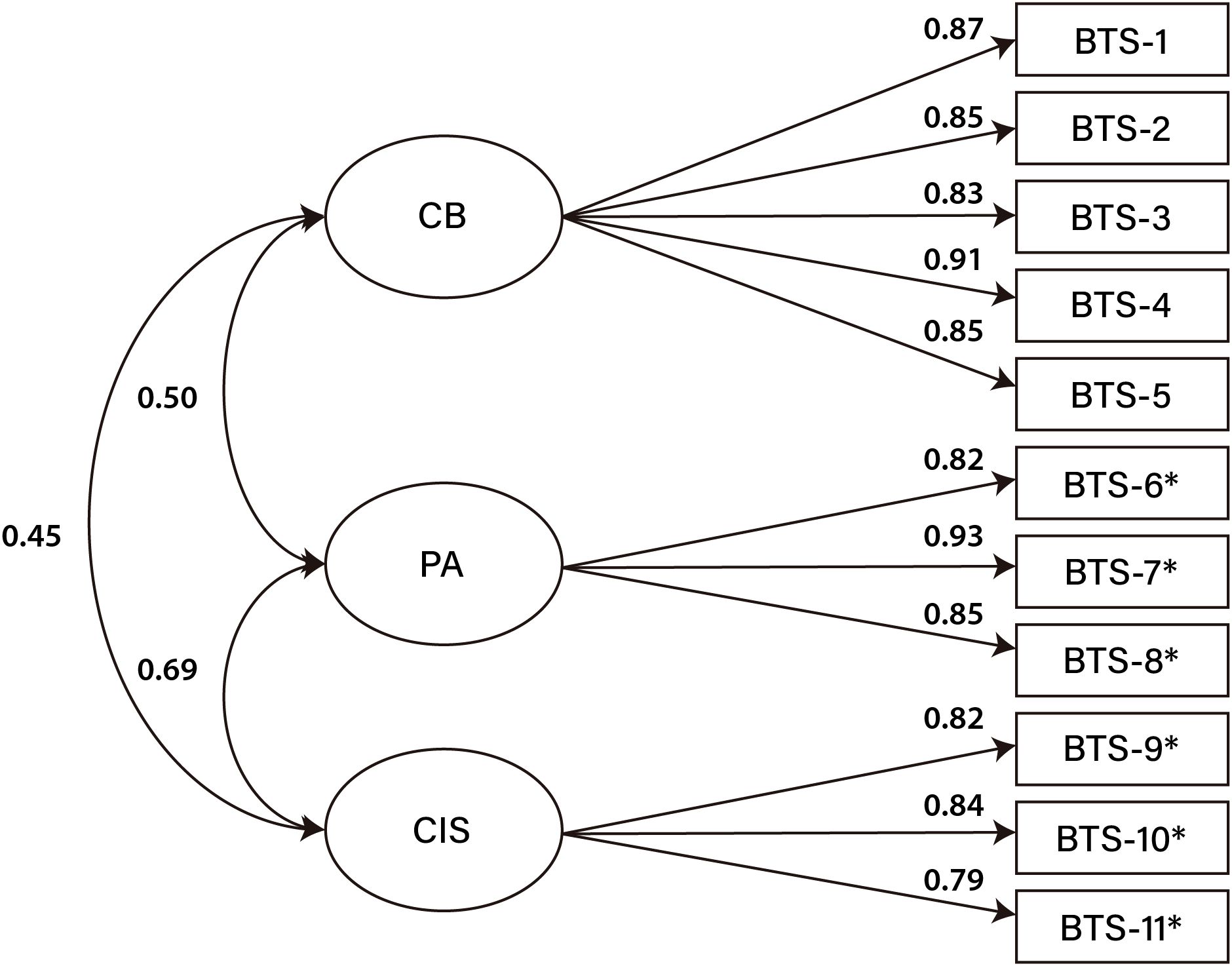
Figure 1. 3-factor model of the BTS (N = 775). Straight arrows, standardized regression weights, curved arrows, correlations between factors. CB, Comfort with One’s Body; PA, Physical Attractiveness; CIS, Comfort with Internal Sensations. *Reverse coded items.
Based on the relatively high part-whole corrected item-total correlations (Table 1) and inter-factor correlations (Figure 1), we additionally explored two alternative models: a unidimensional model and second-order factor model. The unidimensional model showed substantially poorer fit, whereas the second-order factor model demonstrated an identical level of model fit to the 3-factor model (see Supplementary Material Table 1). However, since the original scale (16) adopted a 3-factor model, the second-order factor model did not show a better fit than the 3-factor model, and each subscale is theoretically and practically meaningful, we retained the original 3-factor model as the primary structure for this study.
3.3 Invariance Testing
3.3.1 Measurement invariance across age groups
First, the configural invariance model was tested across age groups. Specifying the same factor structure simultaneously across age groups demonstrated an overall good fit, supporting factor structure equivalence [x2 (164) = 328.056, p <.001; CFI = 0.975; TLI = 0.966; RMSEA = 0.036; SRMR = 0.032; AIC = 616.056]. Second, the equivalence of factor loadings was tested across age groups. The analysis confirmed equivalent factor loadings, as evidenced by ΔCFI = - 0.001 and ΔRMSEA = - 0.002 [x2 (188) = 355.676, p <.001; CFI = 0.974; TLI = 0.970; RMSEA = 0.034; SRMR = 0.033; AIC = 595.676]. Third, the equivalence of the intercepts was tested across age groups. Intercept equivalence was not supported (ΔCFI = -0.014; ΔRMSEA = 0.005), as ΔCFI exceeded the cutoff. This suggests that one or more parameters differed across age groups. When the intercepts of item 9 were freely estimated, partial scalar invariance could be demonstrated [x2 (218) = 448.188, p <.001; CFI = 0.965; TLI = 0.964; RMSEA = 0.037; SRMR=0.035, AIC = 628.188]. The estimates of intercepts of item 9 across age groups were 4.15 (young adults), 4.27 (middle-aged adults), 4.46 (older adults) and 4.65 (seniors). This suggests that item 9 may be interpreted differently across age groups. Fourth, the equivalence of the latent means was tested across age groups. The change in CFI and RMSEA (ΔCFI = 0.004; ΔRMSEA = - 0.002) supported latent mean equivalence.
3.3.2 Measurement invariance across gender
Gender invariance was tested following the same four-step procedure used for age groups (i.e., configural, metric, scalar, and latent mean invariance). All levels demonstrated acceptable fit indices and changes within the predefined thresholds (ΔCFI ≤ 0.01; ΔRMSEA ≤ 0.015), supporting full measurement invariance across gender. Detailed fit statistics are provided in the Supplementary Material Table 2.
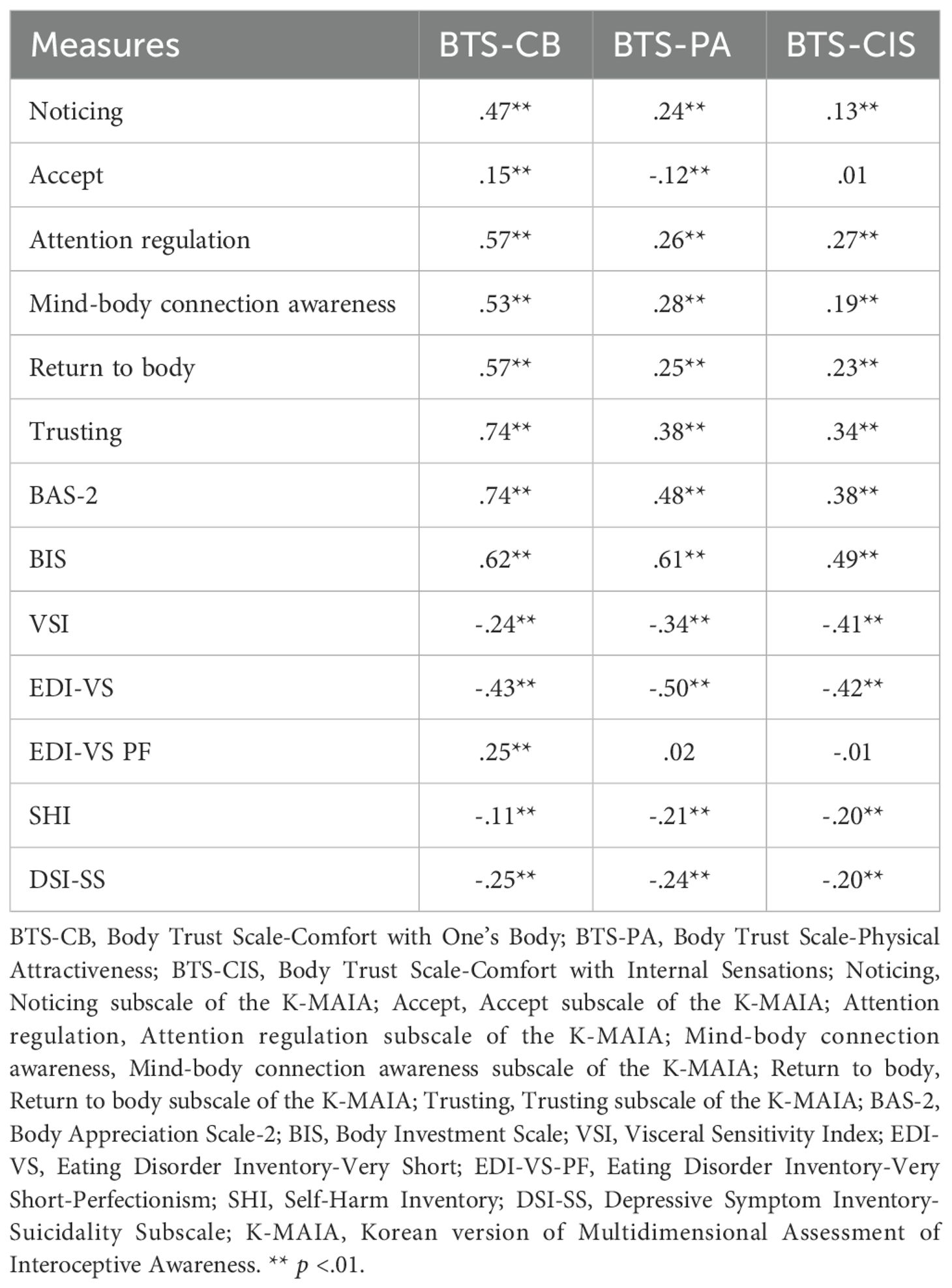
3.4 Correlations between the BTS and other measures
All subscales of the BTS were closely related to the Trusting subscale of the K-MAIA. The CB factor was strongly correlated with most K-MAIA subscales (e.g., Noticing, Attention regulation, Mind-body connection awareness, Return to body, and Trusting), with the correlation being highest for the Trusting subscale. Positive body image and body investment also demonstrated strong associations, particularly with the CB factor. The PA factor was closely related to body investment and showed the strongest negative correlation with eating pathology among the BTS subscales. The CIS factor exhibited the highest negative correlation with visceral sensitivity. Weak but significantly negative correlations were observed between all BTS factors and self-harm behaviors as well as suicidal ideation. Perfectionism was either not significant or weakly related to all BTS factors (see Table 2).
4 Discussion
The aim of this study was to validate the Korean version of the BTS and evaluate its psychometric properties in a Korean sample. The results showed that the items of the BTS exhibited strong internal consistency. As Grunewald et al. (16) suggested, the 3-factor model achieved satisfactory fit. Convergent and discriminant validity within the factor structure were also supported. This indicates that the three dimensions of body trust are present and function similarly within Korean culture. Although the 3-factor model was adopted as the main model in this study, the presence of a second-order factor—labeled ‘body trust’—was also confirmed. This finding suggests that, in addition to subscale scores, the total score of the BTS can also be meaningfully used.
To examine whether the factor structure of the BTS differs across age groups and gender, measurement invariance was tested in the current sample. First, age groups were examined. Full metric invariance was established, indicating that the factor loadings are equivalent across age groups. However, full scalar invariance was not achieved. Instead, partial scalar invariance was confirmed with the free estimation of item 9 (“Physical sensations in my body make me nervous/uncomfortable.”). Given that item 9 is reverse-coded, its intercepts decreased across age groups in the following order: young adults, middle-aged adults, older adults, and seniors. Since item 9 assesses emotional responses to bodily sensations, this finding may be consistent with a previous study (53) reporting a weaker connection between interoception and emotional reactivity in older individuals compared to younger individuals.
There are several possible explanations for this result. Older individuals tend to accept bodily sensation abnormalities as a natural part of the aging process, whereas younger individuals regard it as unusual and therefore experience more anxiety (54). Another possible explanation is that older individuals focus on emotional well-being and tend to minimize negative emotions, influenced by the recognition that their remaining time in life is finite (55). This interpretation is also supported by findings from a Korean study conducted with older adults (56). These results suggest the potential need for revising item 9. Future research may consider rewording this item or developing age-appropriate versions of the item.
Based on the partial scalar invariance model, the analysis of latent mean equivalence revealed that there were no significant mean differences in the BTS scores across age groups. This finding contrasts with a previous study (30) and indicates that in Korean culture, body trust levels do not significantly vary across age groups. Two hypotheses may explain this result. First, the discrepancy may stem from differences in measurement tools. The previous study assessed body trust using the Trusting subscale of the MAIA, which, as mentioned earlier, focuses on a narrow aspect of body trust. In contrast, this study employed the BTS, which includes CB, PA, and CIS to measure body trust. Therefore, to better understand these differences in findings, it is necessary to consider and control for the impact of measurement tool differences. Future research should re-examine age-related body trust levels in Western cultures using the BTS. Second, interoceptive accuracy (the ability to objectively detect internal sensations) and interoceptive sensibility (subjective belief in one’s ability to perceive and process internal sensations) are dissociated dimensions (7, 57). The relationship between these two dimensions may vary across cultures. In particular, these two dimensions may be negatively associated in non-Western cultures (57) due to collectivistic thinking and a tendency toward context-oriented information processing (26, 27). In other words, the tendency to prioritize communal and social harmony over individual internal states may influence this relationship (58). Although no studies have specifically addressed this issue in Korean culture, previous research allows for the following inference. As in Western cultures (30, 31), interoceptive accuracy may have declined with age in Korean culture. However, if the negative relationship between these two dimensions preserved interoceptive sensibility despite the decline in interoceptive accuracy, body trust levels may have remained stable. In future research, it would be meaningful to longitudinally track how body trust levels change throughout an individual’s developmental process while considering cultural influences. Another valuable avenue for research would be to explore how the relationships among different dimensions of interoception evolve over time in Korean culture.
Following this, measurement invariance across gender was tested. The results replicated the findings of Grunewald et al. (16), indicating that the factor structure of BTS functions equivalently for men and women in the Korean context as well.
Correlation analysis confirmed the convergent validity of the Korean version of the BTS. First, the results showed that the CB factor was strongly associated with most K-MAIA subscales: Noticing, Attention regulation, Mind-body connection awareness, Return to body, and Trusting. Positive body image and body investment were also closely related. The CB factor, in particular, showed a stronger association with the K-MAIA Trusting subscale compared to the other BTS factors. These findings are consistent with a previous study (16) indicating that the CB factor is particularly related to existing measures of body trust. Second, the PA factor was related to body investment and positive body image. Our expectations were based on previous findings by Grunewald et al. (16), which reported negative associations between body dissatisfaction and the PA factor, and by Mok (59), which demonstrated positive associations between appearance appreciation and body investment. These results are consistent with those expectations. Third, the CIS factor showed the most notable negative correlation with visceral sensitivity among the factors of BTS. This finding also aligns with a previous study (16), reaffirming that the CIS factor measures anxiety and hypersensitivity related to internal bodily sensations. Fourth, all three factors of the BTS showed weak but significant correlations with self-harm behaviors and suicidal ideation. This is consistent with previous studies (10, 16) that have suggested that body trust is related to self-harm and suicidal ideation. Regarding its relationship with eating pathology, all three BTS factors showed significant negative correlations with the EDI-VS scale. This is also consistent with previous studies (20, 21) that have reported a negative relationship between body trust and eating disorders. Among the BTS factors, the PA factor was the most closely associated with EDI-VS. These results indicate that higher perceived physical attractiveness is linked to lower levels of eating pathology. In summary, these findings support the convergent validity of the BTS with related variables.
For the discriminant validity of the BTS, a weak but significant correlation was found between Perfectionism and the CB factor. However, no significant correlations were observed with the other BTS factors. This result is aligned with previous studies (39) that found no significant relationship between interoceptive awareness and perfectionism, both of which are subscales of the EDI. Therefore, this finding supports the discriminant validity of the BTS. Taken together, the findings discussed above confirm that the BTS is a reliable and valid tool for measuring body trust.
4.1 Limitations
This study has several limitations to consider. First, although body trust has been identified as a relatively stable construct (16), this study was cross-sectional and did not investigate the temporal stability of the BTS. Future research should examine the test–retest reliability of the scale. Second, although body trust is associated with eating pathology, self-harm behaviors, and suicidal ideation, this study was conducted with a non-clinical population. Additionally, since this study was conducted with adults, its findings may not be applicable to adolescents. However, failure to adequately interpret and process interoceptive signals during adolescence, a period of significant physical and psychological changes, may increase the risk of developing psychopathology (5). Thus, it would be valuable to validate the BTS with clinical populations and adolescents. Third, because this study used an online research participant system, the sample, especially seniors, may be biased toward those more familiar with using the internet. Future research should include individuals with lower digital accessibility to ensure a more diverse and representative sample. Lastly, this study established the convergent validity of the BTS with related constructs. However, alexithymia is associated with atypical interoception (60, 61) and could serve as a useful construct for verifying the convergent validity of the BTS. Therefore, it would be meaningful to re-examine the convergent validity of the BTS by including alexithymia as well as other potentially related constructs.
5 Conclusion
Our study is the first to examine the reliability and validity of a Korean version of the BTS, a recently developed tool designed to comprehensively measure body trust. The large sample size and the balanced distribution of age and gender groups strengthen the validity of our findings. In conclusion, while further validation in clinical and adolescent population is warranted, the Korean version of the BTS appears to be a sound instrument with potential applicability in Korean adults. Furthermore, it may serve as a valuable tool for exploring associations between body trust and mental health factors, such as eating pathology and suicide risk (16).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Jeonbuk National University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YO: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. J-WS: Conceptualization, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. The research received funding from the Brain Korea 21 fourth project of the Korea Research Foundation (Jeonbuk National University, Psychology Department no. 4199990714213).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. Only for sentence correction purposes.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1631918/full#supplementary-material
References
1. Craig AD. Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiology. (2003) 13:500–5. doi: 10.1016/s0959-4388(03)00090-4
2. Khalsa SS, Adolphs R, Cameron OG, Critchley HD, Davenport PW, Feinstein JS, et al. Interoception and mental health: a roadmap. Biol Psychiatry: Cogn Neurosci Neuroimaging. (2018) 3:501–13. doi: 10.1016/j.bpsc.2017.12.004
3. Grunewald W, Fogelberg S, Ferguson W, Hines S, Fortenberry B, and Smith AR. Longitudinal relationships between specific domains of interoception and muscle dysmorphia symptoms. Eating Behaviors. (2023) 48:101686. doi: 10.1016/j.eatbeh.2022.101686
4. Mehling WE, Acree M, Stewart A, Silas J, and Jones A. The multidimensional assessment of interoceptive awareness, version 2 (MAIA-2). PloS One. (2018) 13:e0208034. doi: 10.1371/journal.pone.0208034
5. Murphy J, Brewer R, Catmur C, and Bird G. Interoception and psychopathology: A developmental neuroscience perspective. Dev Cogn Neurosci. (2017) 23:45–56. doi: 10.1016/j.dcn.2016.12.006
6. Quigley KS, Kanoski S, Grill WM, Barrett LF, and Tsakiris M. Functions of interoception: from energy regulation to experience of the self. Trends Neurosciences. (2021) 44:29–38. doi: 10.1016/j.tins.2020.09.008
7. Garfinkel SN, Tiley C, O’Keeffe S, Harrison NA, Seth AK, and Critchley HD. Discrepancies between dimensions of interoception in autism: implications for emotion and anxiety. Biol Psychol. (2016) 114:117–26. doi: 10.1016/j.biopsycho.2015.12.003
8. Paulus MP, Feinstein JS, and Khalsa SS. An active inference approach to interoceptive psychopathology. Annu Rev Clin Psychol. (2019) 15:97–122. doi: 10.1146/annurev-clinpsy-050718-095617
9. Gioia AN, Forrest LN, and Smith AR. Diminished body trust uniquely predicts suicidal ideation and nonsuicidal self-injury among people with recent self-injurious thoughts and behaviors. Suicide Life-Threatening Behavior. (2022) 52:1205–16. doi: 10.1111/sltb.12915
10. Smith AR, Duffy ME, and Joiner TE. Introduction to the special issue on interoception and suicidality. Behav Ther. (2021) 52:1031–4. doi: 10.1016/j.beth.2021.06.003
11. van Dyck Z, Schulz A, Blechert J, Herbert BM, Lutz APC, and Vogele C. Gastric interoception and gastric myoelectrical activity in bulimia nervosa and binge-eating disorder. Int J Eating Disord. (2021) 54:1106–15. doi: 10.1002/eat.23291
12. Martin E, Dourish CT, Rotshtein P, Spetter MS, and Higgs S. Interoception and disordered eating: A systematic review. Neurosci Biobehav Rev. (2019) 107:166–91. doi: 10.1016/j.neubiorev.2019.08.020
13. Perry TR, Wierenga CE, Kaye WH, and Brown TA. Interoceptive awareness and suicidal ideation in a clinical eating disorder sample: The role of body trust. Behav Ther. (2021) 52:1105–13. doi: 10.1016/j.beth.2020.12.001
14. Rogers ML, Hagan CR, and Joiner TE. Examination of interoception along the suicidality continuum. J Clin Psychol. (2018) 74:1004–16. doi: 10.1002/jclp.22564
15. Mehling WE, Price C, Daubenmier JJ, Acree M, Bartmess E, and Stewart A. The multidimensional assessment of interoceptive awareness (MAIA). PloS One. (2012) 7:e48230. doi: 10.1371/journal.pone.0048230
16. Grunewald W, Waitz-Kudla SN, Levinson CA, Brown TA, and Smith AR. Development and psychometric validation of the Body Trust Scale. Assessment. (2024) 31:1548–64. doi: 10.1177/10731911231225200
17. Gim WS, Sim KL, and Cho OK. Korean multidimensional assessment of interoceptive awareness (K-MAIA): Development and validation. Korean J Stress Res. (2016) 24:177–92. doi: 10.17547/kjsr.2016.24.3.177
18. van der Hoort B, Reingardt M, and Ehrsson HH. Body ownership promotes visual awareness. Elife. (2017) 6:e26022. doi: 10.7554/eLife.26022
19. Choi K, Hwang H, and Lee H. Mediating effect of body trust in the relationship between emotional neglect and emotion dysregulation. Korean J Health Psychol. (2024) 29:89–108. doi: 10.17315/kjhp.2024.29.1.005
20. Brown TA, Berner LA, Jones MD, Reilly EE, Cusack A, Anderson LK, et al. Psychometric evaluation and norms for the multidimensional assessment of interoceptive awareness (MAIA) in a clinical eating disorders sample. Eur Eating Disord Review. (2017) 25:411–6. doi: 10.1002/erv.2532
21. Sim KL, Jung AJ, and Gim WS. Follow-up study of the validation of Korean Multidimensional Assessment of Interoceptive Awareness(K-MAIA): Focused on eating behavior and somatic symptoms. Korean J Meditation. (2020) 10:1–22. doi: 10.23250/kjm.10.1.202002.001
22. Brown TA, Vanzhula IA, Reilly EE, Levinson CA, Berner LA, Krueger A, et al. Body mistrust bridges interoceptive awareness and eating disorder symptoms. J Abnormal Psychol. (2020) 129:445–56. doi: 10.1037/abn0000516
23. Duffy ME, Lieberman A, Siegfried N, Henretty JR, Bass G, Cox SA, et al. Body Trust, agitation, and suicidal ideation in a clinical eating disorder sample. Int J Eating Disord. (2020) 53:1746–50. doi: 10.1002/eat.23352
24. Tylka TL and Wood-Barcalow NL. The Body Appreciation Scale-2: item refinement and psychometric evaluation. Body image. (2015) 12:53–67. doi: 10.1016/j.bodyim.2014.09.006
25. Labus JS, Bolus R, Chang L, Wiklund I, Naesdal J, Mayer EA, et al. The Visceral Sensitivity Index: Development and validation of a gastrointestinal symptom-specific anxiety scale. Alimentary Pharmacol Ther. (2004) 20:89–97. doi: 10.1111/j.1365-2036.2004.02007.x
26. Ma-Kellams C. Cross-cultural differences in somatic awareness and interoceptive accuracy: a review of the literature and directions for future research. Front Psychol. (2014) 5:1379. doi: 10.3389/fpsyg.2014.01379
27. Tsai JL, Simeonova DI, and Watanabe JT. Somatic and social: Chinese Americans talk about emotion. Pers Soc Psychol Bulletin. (2004) 30:1226–38. doi: 10.1177/0146167204264014
28. Lee SJ, Lee M, Kim HB, and Huh HJ. The relationship between interoceptive awareness, emotion regulation and clinical symptoms severity of depression, anxiety and somatization. Psychiatry Invest. (2024) 21:255–64. doi: 10.30773/pi.2023.0221
29. Korean statistical information service. In: Causes of death statistics in 2023. Daejeon: Statistics Korea. Available online at: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B34E20&conn_path=I2.
30. Dobrushina OR, Dobrynina LA, Arina GA, Pechenkova EV, Kremneva EI, Gubanova MV, et al. Age-related changes of interoceptive brain networks: Implications for interoception and alexithymia. Emotion. (2024) 24:1536–49. doi: 10.1037/emo0001366
31. Ulus G and Aisenberg-Shafran D. Interoception in old age. Brain Sci. (2022) 12:1398. doi: 10.3390/brainsci12101398
32. Kline RB. Principles and practice of structural equation modeling. 2nd Edn. New York: New York: Guildford Publications (2004).
33. Myers ND, Ahn S, and Jin Y. Sample size and power estimates for a confirmatory factor analytic model in exercise and sport: A Monte Carlo approach. Res Q Exercise Sport. (2011) 82:412–23. doi: 10.1080/02701367.2011.10599773
34. Lee M. Factor structure and psychometric properties of a Korean translation of the Body Appreciation Scale-2. Body Image. (2022) 42:11–24. doi: 10.1016/j.bodyim.2022.05.004
35. Orbach I and Mikulincer M. The Body Investment Scale: Construction and validation of a body experience scale. psychol Assessment. (1998) 10:415–25. doi: 10.1037/1040-3590.10.4.415
36. Mok C. The role of body investment on the emotional cascade model of nonsuicidal self-injury. Seoul (KR: Seoul National University (2021). Master’s thesis.
37. Jang AL. The effects of cognitive behavior therapy for nursing college students with irritable bowel syndrome. Busan (KR: Pusan National University (2013). Doctoral dissertation.
38. Maiano C, Morin AJ, Monthuy-Blanc J, Garbarino JM, and Ninot G. Development and validity of a very short form of the Eating Disorder Inventory. Compr Psychiatry. (2016) 65:141–9. doi: 10.1016/j.comppsych.2015.11.004
39. Garner D, Olmstead M, and Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int J Eating Disord. (1983) 2:15–34. doi: 10.1002/1098-108X(198321)2:23.0.CO;2-6
40. Sansone RA, Wiederman MW, and Sansone LA. The Self-Harm Inventory (SHI): development of a scale for identifying self-destructive behaviors and borderline personality disorder. J Clin Psychol. (1998) 54:973–83. doi: 10.1002/(sici)1097-4679(199811)54:7<973::aid-jclp11>3.0.co;2-h
41. Kong SS. Impact of eating psychopathology, obsessive-compulsion and depression on self-harm behavior in patients with eating disorders. J Korean Acad Nursing. (2009) 39:459–68. doi: 10.4040/jkan.2009.39.4.459
42. Lee HL. Effect of reward sensitivity/punishment sensitivity on anxiety, depression, and self-harm behavior: The role of stress and controllable attribution style. Seoul (KR: The Catholic University of Korea (2013). Master’s thesis.
43. Han JH. The relationship between self-injurious behavior of adults and motivation of self-harm: The moderating effect of self-control. Seoul (KR: Ehwa Womans University (2018). Master’s thesis.
44. Metalsky GI and Joiner TE Jr. The hopelessness depression symptom questionnaire. Cogn Ther Res. (1997) 21:359–84. doi: 10.1023/A:1021882717784
45. Suh S, Ryu H, Chu C, Hom M, Rogers ML, and Joiner T. Validation of the korean depressive symptom inventory-suicidality subscale. Psychiatry Invest. (2017) 14:577–84. doi: 10.4306/pi.2017.14.5.577
46. Hu L and Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equation Modeling: A Multidiscip J. (1999) 6:1–55. doi: 10.1080/10705519909540118
47. Schermelleh-Engel K, Moosbrugger H, and Müller H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods psychol Res Online. (2003) 8:23–74.
48. Bentler PM. Comparative fit indexes in structural models. psychol Bulletin. (1990) 107:238–46. doi: 10.1037/0033-2909.107.2.238
49. Tucker LR and Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. (1973) 38:1–10. doi: 10.1007/BF02291170
51. Fornell C and Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J marketing Res. (1981) 18:39–50. doi: 10.1177/002224378101800104
52. Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equation Modeling: A Multidiscip J. (2007) 14:464–504. doi: 10.1080/10705510701301834
53. Mikkelsen MB, O’Toole MS, Lyby MS, Wallot S, and Mehlsen M. Emotional reactivity and interoceptive sensitivity: Exploring the role of age. Psychonomic Bull Review. (2019) 26:1440–8. doi: 10.3758/s13423-019-01603-y
54. Mahoney CT, Segal DL, and Coolidge FL. Anxiety sensitivity, experiential avoidance, and mindfulness among younger and older adults: Age differences in risk factors for anxiety symptoms. Int J Aging Hum Dev. (2015) 81:217–40. doi: 10.1177/0091415015621309
55. Carstensen LL. Evidence for a life-span theory of socioemotional selectivity. Curr Dir psychol Science. (1995) 4:151–6. doi: 10.1111/1467-8721.ep11512261
56. Kim MH and Min KH. Emotional experience and emotion regulation in old age. Korean J Psychology: General. (2004) 23:1–21.
57. Ma-Kellams C, Prentice F, Spooner R, and Murphy J. Demographic differences in interoception. In: Murphy J and Brewer R, editors. Interoception: A Comprehensive Guide, vol. . p . Springer, Cham (2024). p. 357–403.
58. Freedman A, Hu H, Liu I, Stewart AL, Adler S, and Mehling WE. Similarities and differences in interoceptive bodily awareness between US-american and Japanese cultures: A focus-group study in bicultural Japanese-americans. Culture Medicine Psychiatry. (2021) 45:234–67. doi: 10.1007/s11013-020-09684-4
59. Mok C. Preliminary validation of a Korean version of the Body Investment Scale. Korean J Cinical Psychol. (2024) 43:12–8. doi: 10.15842/kjcp.2024.43.1.016
60. Brewer R, Cook R, and Bird G. Alexithymia: a general deficit of interoception. R Soc Open Science. (2016) 3:150664. doi: 10.1098/rsos.150664
61. Gaggero G, Bizzego A, Dellantonio S, Pastore L, Lim M, and Esposito G. Clarifying the relationship between alexithymia and subjective interoception. PloS One. (2021) 16:e0261126. doi: 10.1371/journal.pone.0261126
Appendix. The Korean version of the BTS
Instructions; 다음은 귀하가 신체와 그 감각에 대해 가질 수 있는 다양한 태도, 감정 또는 행 동을 알아보기 위한 문항입니다. 아래 각 문항에 대해 얼마나 동의하시는지 해당하는 숫자에 표시해주십시오.
*9~11번 문항의 ‘신체 감각’ 이란, 심장박동, 포만감, 열감, 내장 감각 등 신체 내부에서 느낄 수 있는 감각을 의미합니다.
Keywords: body trust, interoception, BTS, validity, reliability
Citation: Oh Y and Seo J-W (2025) Body trust in Korean population: validation of the Korean version of the body trust scale. Front. Psychiatry 16:1631918. doi: 10.3389/fpsyt.2025.1631918
Received: 20 May 2025; Accepted: 28 July 2025;
Published: 21 August 2025.
Edited by:
Rakesh Pandey, Banaras Hindu University, IndiaReviewed by:
Tuğba Küçükkasap, Health Sciences University, Ankara, Turks and Caicos IslandsValentina Belalcazar Vivas, University of Pamplona, Colombia
Copyright © 2025 Oh and Seo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jang-Won Seo, andzZW9AamJudS5hYy5rcg==
 Yunyoung Oh
Yunyoung Oh Jang-Won Seo
Jang-Won Seo