- 1School of Psychology, Shenzhen University, Shenzhen, China
- 2The Shenzhen Humanities & Social Sciences Key Research Bases, Center for Mental Health, Shenzhen University, Shenzhen, China
- 3Institute of Analytical Psychology, City university of Macau, Macau, China
Introduction: In China’s collectivist healthcare context, the mechanisms linking social support to quality of life (QoL) in heart transplant recipients remain unclear. This study integrates Mishel’s uncertainty in illness theory and Confucian resilience frameworks to cross-sectionally examine dual pathways: direct enhancement of QoL through social support and indirect reduction of uncertainty in illness, moderated by culturally embedded psychological resilience.
Methods: A nationwide cross-sectional study included 428 Chinese heart transplant recipients. Social support (SSRS), uncertainty in illness (MUIS-A), resilience (CD-RISC), and QoL (SF-36) were assessed. Mediation (PROCESS Model 4) and moderated mediation (Model 14) were tested using 5,000 bootstrap resamples, controlling for age, gender, and transplant duration.
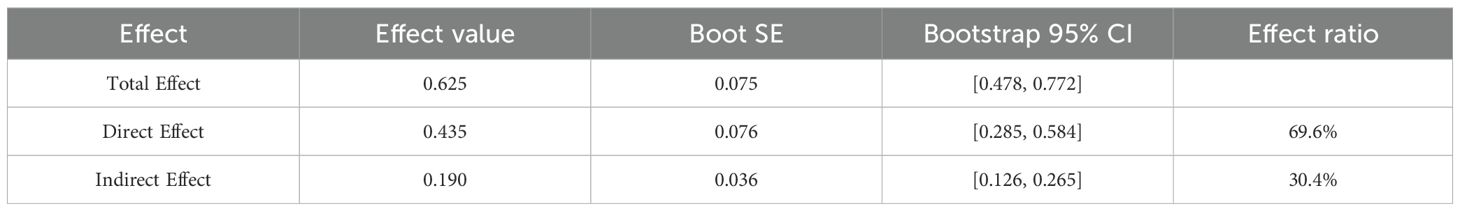
Results: Social support directly improved QoL (B = 0.625, p < 0.001, direct effect = 0.435, 95% CI [0.285, 0.584]) and indirectly reduced uncertainty in illness (indirect effect = 0.19, 95% CI [0.126, 0.265]). Psychological resilience moderated the uncertainty in illness-QoL link (B = 0.007, p < 0.001), with stronger negative effects in low-resilience individuals (B = -0.372 vs. high-resilience B = -0.111).
Conclusion: Based on this cross-sectional study, social support demonstrates significant associations with dual pathways: directly associated with improved QoL through relational support networks and indirectly linked to reduced uncertainty in illness via culturally mediated cognitive reframing. Culturally interventions integrating family-centered care and resilience training are recommended to improve long-term outcomes.
1 Introduction
1.1 Quality of life deficits in heart transplant recipients
Heart transplantation, while life-saving for end-stage cardiac patients, introduces profound psychosocial challenges that extend far beyond surgical recovery (1–4). Mishel’s Uncertainty in Illness Theory provides a critical lens for understanding these challenges, framing uncertainty as a multidimensional stressor arising from unpredictability of symptoms, ambiguous prognoses, and the lifelong complexity of post-transplant care (5). For heart transplant recipients, this uncertainty is amplified by the delicate balance of immunosuppression, graft acceptance risks, and existential anxieties about mortality (6, 7). Empirical studies consistently link uncertainty in illness to diminished quality of life (QoL) across chronic conditions, particularly in transplant populations where medical ambiguity persists despite clinical advancements (5, 8, 9).
Complementing this perspective, Connor-Davidson’s Resilience Framework shifts focus to individual adaptability, emphasizing the capacity to reframe adversity and maintain psychological equilibrium (10). Resilience has been associated with improved health outcomes in transplant recipients, yet its interplay with uncertainty remains underexplored (10, 11). While Mishel’s theory highlights environmental buffers like social support (12), resilience models prioritize intrapsychic processes (8, 10), creating a theoretical divide that obscures their synergistic potential. This study combines existing theories to explore how psychosocial resilience, such as social support and uncertainty in illness, influence quality of life in transplant populations.
1.2 Social support and quality of life
Empirical evidence establishes social support as a significant predictor of QoL in transplant populations (13), operating through two empirically validated dimensions: instrumental support (tangible assistance) and emotional support (affective reassurance). Previous studies demonstrates that perceived social support directly enhances physical recovery, emotional stability, and social reintegration, thereby improving overall QoL (8, 14). Instrumental support improves physical functioning in transplant recipients. This includes assistance with medication management (15). Instrumental support also encompasses help coordinating medical appointments (4). Concurrently, emotional support dimensions such as distress reduction interventions (16) and companionship provision (17) associate with improved psychological well-being indices.
In China’s collectivist cultural context, this support is operationalized through filial piety, where families assume caregiving roles as a moral obligation, providing both instrumental aid (e.g., managing complex medication regimens) and emotional reassurance (18, 19). Empirical studies in Chinese chronic illness populations highlight that strong family support is associated with significantly higher QoL scores compared to isolated individuals (20, 21). This contrasts with Western models, where professional healthcare systems and individualized coping strategies dominate (22, 23), underscoring cultural specificity in support mechanisms.
1.3 The mediating role of uncertainty in illness
Building on Mishel’s foundational work (5), uncertainty in illness emerges as a critical mediating mechanism linking social support to QoL in medically complex populations (8). Grounded in Mishel’s Uncertainty in Illness Theory, this construct is defined as the inability to determine the meaning of illness-related events, characterized by perceptions of ambiguity regarding symptoms, unpredictability of disease progression, complexity of treatment regimens, and lack of adequate information. Within the context of heart transplantation, patients face sustained uncertainty stemming from graft viability, immunosuppression management, risk of rejection, and long-term prognosis (1, 6). Empirical evidence across diverse chronic illness populations consistently demonstrates that elevated illness uncertainty correlates strongly with diminished quality of life outcomes (5, 9, 24). Research further suggests that social support may influence quality of life partly through its capacity to mitigate perceptions of illness-related uncertainty (8, 25).
Supportive interactions can provide informational clarity, enhance predictability, and reduce the perceived complexity of illness management, thereby potentially decreasing uncertainty levels (16, 26). For instance, investigations in hemodialysis and heart failure cohorts report inverse associations between perceived social support and illness uncertainty, with evidence suggesting uncertainty functions as an intermediary pathway linking social resources to well-being (15, 27).
However, the specific mediating role of uncertainty in illness within the relationship between social support and quality of life remains quantitatively underexamined in heart transplant populations (20, 28, 29). This gap is notable given the unique and persistent uncertainties inherent in post-transplant survivorship.
Consequently, this study quantitatively examines whether uncertainty in illness mediates the association between social support and quality of life in Chinese heart transplant recipients. Specifically, we investigate the extent to which social support influences quality of life indirectly by reducing perceptions of illness uncertainty. Verifying this mediating pathway is crucial for understanding the psychological mechanisms through which social resources operate and for identifying uncertainty reduction as a potential target for psychosocial interventions aimed at improving long-term adjustment in this population.
1.4 The moderating role of psychological resilience
The potential moderating role of psychological resilience in mitigating the adverse effects of uncertainty in illness on QoL warrants further investigation, particularly within specific clinical populations such as heart transplant recipients. Grounded in Connor and Davidson’s Resilience Framework (10), psychological resilience is conceptualized as the individual’s capacity to adapt positively to adversity, maintain psychological equilibrium, and effectively utilize coping resources. Emerging empirical evidence suggests resilience may function as a protective buffer. Studies in chronic illness populations indicate that individuals scoring higher on standardized resilience measures demonstrate greater tolerance for illness-related ambiguities and exhibit attenuated negative psychological responses to unpredictable health trajectories compared to those with lower resilience (30). Qualitative investigations with transplant recipients also report associations between resilience and adaptive cognitive appraisals of uncertainty (21, 31).
However, the specific moderating effect of resilience on the relationship between uncertainty in illness and quality of life remains quantitatively underexplored, especially within the context of heart transplantation. This gap is significant given the persistent and multifaceted uncertainties inherent in post-transplant management. Consequently, this study specifically examines whether psychological resilience attenuates the negative impact of uncertainty in illness on quality of life.
We hypothesize that higher levels of psychological resilience will weaken the strength of the negative association between uncertainty in illness and quality of life, meaning the detrimental effect of uncertainty will be less pronounced among individuals with greater resilience. This hypothesis aligns with the core proposition of resilience frameworks that individual differences in adaptive capacity significantly influence how stressors translate into health outcomes (10). Quantifying this moderating effect is crucial for identifying resilience as a potential intervention target to improve quality of life outcomes when uncertainty is unavoidable.
1.5 Confucian resilience in heart transplantation: family support, illness uncertainty, and quality of life
China’s collectivist societal structure, governed by Confucian relational ethics, fundamentally reconfigures psychosocial adaptation pathways for heart transplantation recipients (32, 33). Within this framework, familial obligation through filial piety operates as the primary support mechanism, where kin networks assume integrated caregiving roles—blending instrumental aid (e.g., medication supervision, appointment coordination) and emotional reassurance into a binding moral duty (19, 21). Concurrently, psychological resilience manifests as collective endurance, cultivated through intergenerational narratives that reframe health adversity as shared familial challenges rather than individual burdens (20, 34).
These cultural dynamics necessitate modifications to standard psychosocial models. First, social support reduces illness uncertainty through familial health brokering: relatives act as cultural translators who decode medical complexity into actionable knowledge using kinship-based decision hierarchies, thereby enhancing informational clarity (21, 26). Second, Confucian resilience moderates uncertainty’s impact by invoking familial duty framing—where health threats are reinterpreted as opportunities to fulfill generational obligations—thus attenuating distress through meaning-centered coping (31, 35).
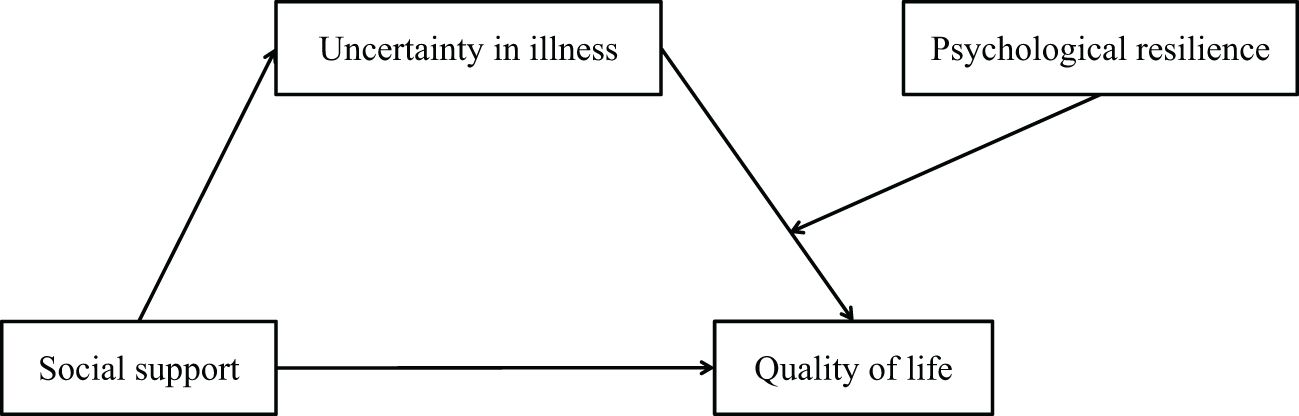
Consequently, we propose to investigate the hypotheses (section 1.3 & 1.4) in the context of Chinese heart transplant recipients. Empirically, this model diverges from Western paradigms where uncertainty management relies on patient autonomy and professional guidance (22, 23), highlighting the need for culture-specific intervention frameworks in China’s family-centric healthcare ecosystem. The hypothesized relationships among social support, uncertainty in illness, psychological resilience, and QoL in the context of Chinese heart transplant recipients are summarized in Figure 1.
Proposed hypotheses:
H1: Uncertainty in illness will mediate the association between social support and quality of life within the heart transplant recipients.
H2: Psychological resilience will moderate the relationship between uncertainty in illness and quality of life within heart transplant recipients.
2 Materials and methods
2.1 Participants
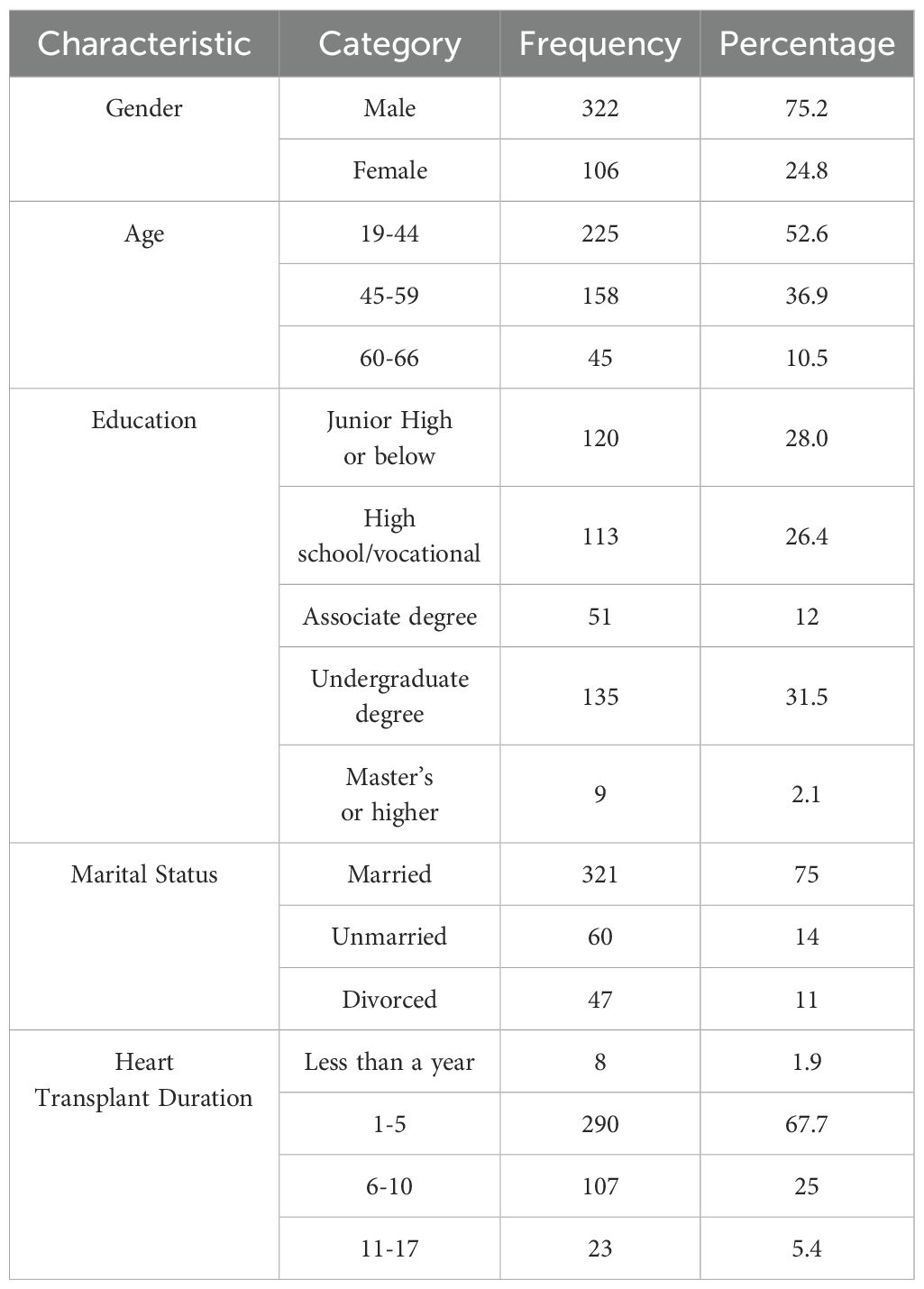
Initially 440 samples collected. After random responses and missing values were excluded, 428 valid samples were finally received with a validity rate of 97.3%. Descriptive statistics for demographic variables are presented in Table 1. Most participants were male (75.2%, n = 322), and the age distribution was as follows: 52.6% (n = 225) were categorized as young adults (19–44 years), 36.9% (n = 158) as middle-aged adults (45–59 years), and 10.5% (n = 45) as older adults (60–66 years). Regarding educational attainment, 28.0% (n = 120) had a junior high school education or below, 26.4% (n = 113) completed high school or vocational school, 12.0% (n = 51) held an associate degree, 31.5% (n = 135) had an undergraduate degree, and 2.1% (n = 9) held a master’s degree or higher. Most participants were married (75.0%, n = 321), while 14.0% (n = 60) were unmarried and 11.0% (n = 47) were divorced. For heart transplant duration, 67.7% (n = 290) of participants received their transplant 1–5 years prior to the study, followed by 25.0% (n = 107) at 6–10 years, 5.4% (n = 23) at 11–17 years, and 1.9% (n = 8) less than a year ago.
2.2 Measures
Quality of Life (QoL) was assessed using the Chinese version of the 36-item Short Form Health Survey (SF-36; 36). This instrument measures two primary domains: physical health (Physical Functioning, Role-Physical, Bodily Pain, General Health) and mental health (Vitality, Social Functioning, Role-Emotional, Mental Health). Raw scores were converted to a 0–100 scale following standard protocols, with higher scores indicating better QoL. The Cronbach’s α coefficient in this study was 0.916. Detailed item descriptions are provided in Supplementary section 1.1. Quality of Life.
Social Support was quantified using the Social Support Rating Scale (SSRS; 37), a 10-item tool widely applied in Chinese health research. It comprises three dimensions: objective support (tangible assistance), subjective support (perceived availability), and support utilization (help-seeking behaviors). Total scores range from 12 to 66, with higher values indicating stronger support networks. The Cronbach’s α coefficient for this measure was 0.92. Item-level psychometrics are reported in Supplementary section 1.2. Social Support.
Uncertainty in Illness was evaluated via the Chinese adaptation of the Mishel Uncertainty in Illness Scale for Adults (MUIS-A; 5, 38). This 32-item instrument (excluding item 15) measures four dimensions: Ambiguity, Complexity, Lack of Information, and Unpredictability. Responses were recorded on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree), with total scores ranging from 32 to 160. Higher scores reflect greater illness-related uncertainty. The Cronbach’s α coefficient in this study was 0.963. A complete item list and scoring details are archived in Supplementary section 1.3. Uncertainty in Illness.
Psychological Resilience was measured using the 25-item Connor-Davidson Resilience Scale (CD-RISC; 10), validated in Chinese populations (11). This scale comprises 25 items measuring resilience across three dimensions: Toughness, Strength, and Optimism. Responses were recorded on a 5-point Likert scale (0 = never to 4 = almost always), with total scores ranging from 0 to 100. Higher scores indicated greater resilience. The Cronbach’s α coefficient for this scale was 0.948. Subscale structures and sample items are available in Supplementary section 1.4. Psychological Resilience.
2.3 Procedures
The study was conducted across three high-volume cardiac transplant centers located in northern, central, and southern provinces of China. Data collection utilized a secure electronic questionnaire platform. Following institutional ethics approval from the Ethics Committee of Medical School, Shenzhen University (Approval No. PN-20250097), eligible participants were invited to complete the survey after providing digital informed consent via a certified authentication process.
Inclusion criteria comprised: (1) adults aged ≥ 18 years; (2) survival > 1-month post-transplant with successful hospital discharge; (3) intact cognitive function and communication capacity; (4) voluntary provision of informed consent. Exclusion criteria included: (1) cognitive impairment (assessed via a mental status examination score < 24); (2) severe comorbidities; (3) communication barriers (e.g., aphasia, hearing/visual impairments).
All responses were anonymized through unique participant codes, with personal identifiers permanently excluded. Real-time data encryption was implemented during transmission, and encrypted datasets were securely stored on password-protected servers. Physical copies of data were permanently destroyed post-analysis. Participants were explicitly informed of their right to withdraw at any stage, and confidentiality protocols were rigorously enforced throughout the study.
2.4 Statistical analyses
The data analysis was performed using SPSS 27.0 (39) following a three-stage analytical procedure. First, a common method bias test was conducted to assess potential measurement bias. Subsequently, descriptive statistics and Pearson correlation analyses were performed to examine the distribution characteristics and bivariate relationships among variables. Finally, the PROCESS macro (version 3.5) developed by Hayes (40) was employed to test mediation and moderated mediation effects. Specifically, Model 4 (simple mediation) and Model 14 (moderated mediation) were executed using the bias-corrected percentile Bootstrap method with 5,000 resamples to determine the significance of indirect effects. The bootstrapping approach we employed does not require normality assumptions for valid inference, as it generates bias-corrected confidence intervals that are robust to non-normality and other distributional issues (41, 42).
3 Results
3.1 Common method bias test
To assess common method bias, Harman’s single-factor test was performed through exploratory factor analysis (EFA) on the 106 items across four measurement scales. The results revealed 18 factors with eigenvalues exceeding 1.0 based on Kaiser’s criterion. Notably, the first unrotated factor accounted for 19.287% of the total variance explained, which is substantially below the critical threshold of 40% recommended by Podsakoff et al. (43) (43). These findings indicate no substantial common method bias in the current dataset, thereby supporting the validity of subsequent analytical procedures.
3.2 Descriptive statistics and correlation analyses
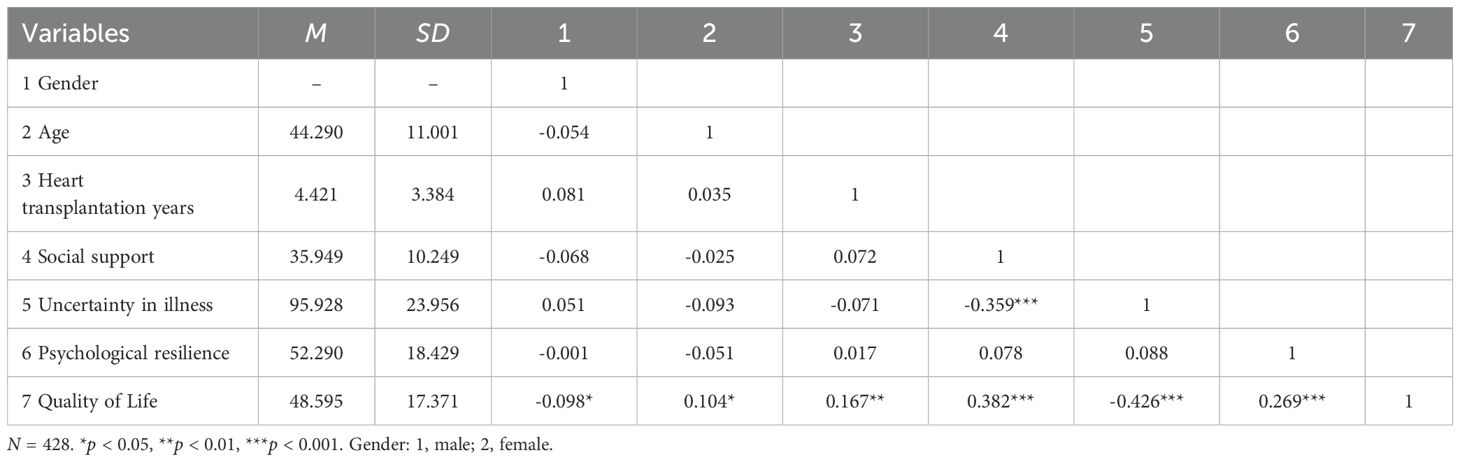
The descriptive statistics and bivariate correlations among key variables are presented in Table 2. Significant associations were observed between psychological constructs: Social support demonstrated a significant negative correlation with uncertainty in illness (r = -0.359, p < 0.001) and a positive correlation with quality of life (r = 0.382, p < 0.001). Furthermore, uncertainty in illness showed a strong inverse relationship with quality of life (r = -0.426, p < 0.001). Regarding demographic characteristics, three covariates – gender (coded 0 = male, 1 = female), age (in years), and time since heart transplantation (years post-operation) – exhibited statistically significant associations with QoL outcomes (all p-values < 0.05). These demographic variables were consequently included as covariates in subsequent multivariate analyses to control for potential confounding effects.
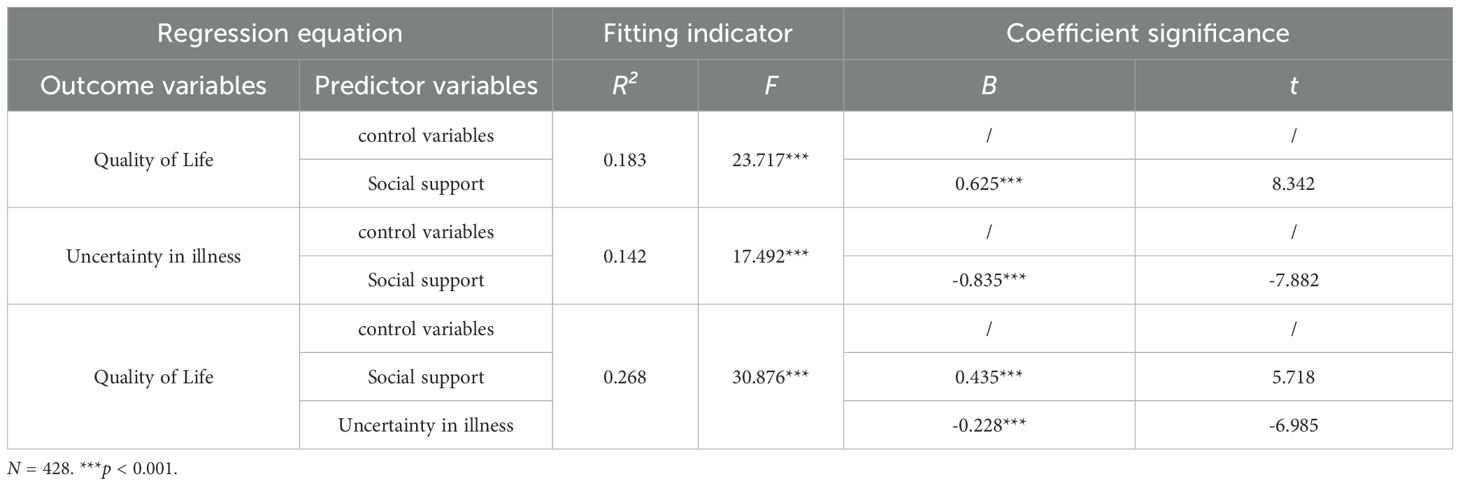
3.3 Mediating effect test
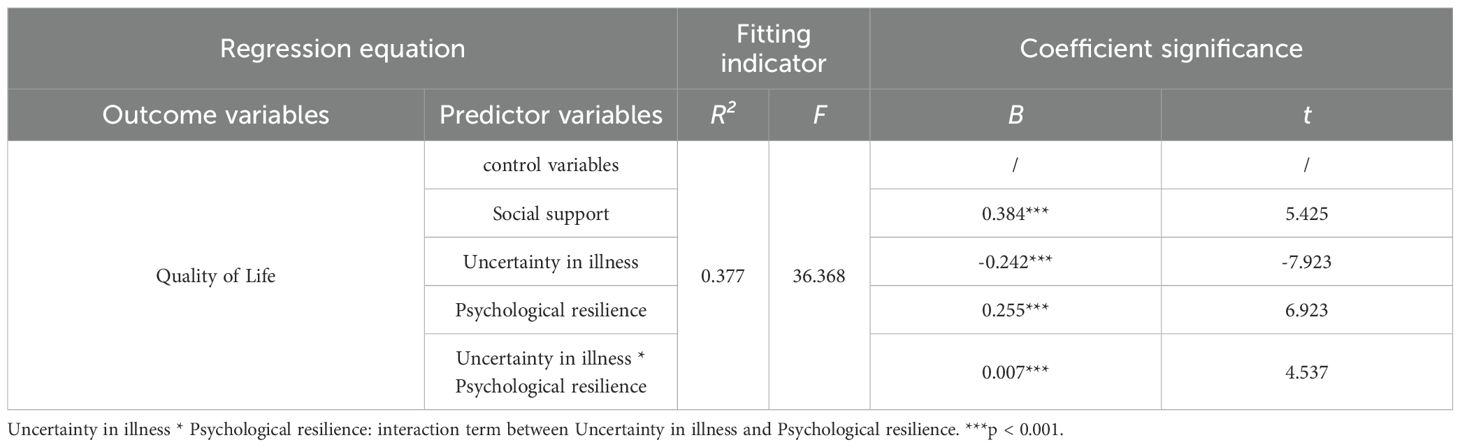
The mediation analysis was conducted using Model 4 from PROCESS macro (version 3.5) for SPSS (39, 40), with gender, age, and years of post-heart transplantation specified as demographic covariates. As shown in Tables 3, 4, social support demonstrated a significant positive predictive effect on quality of life (B = 0.625, t = 8.342, p < 0.001). When introducing uncertainty in illness as the mediator, while the direct effect of social support on quality of life remained statistically significant, its effect size showed substantial reduction (B = 0.435, t = 5.718, p < 0.001). Concurrently, uncertainty in illness exhibited a significant negative predictive effect on quality of life (B = -0.228, t = -6.985, p < 0.001), supporting Hypothesis H2. The analysis further confirmed that social support significantly predicted lower levels of uncertainty in illness (B = -0.835, t = -7.882, p < 0.001), thereby validating Hypothesis H1.
The bias-corrected bootstrap 95% confidence intervals for both the direct effect of social support and the indirect effect through uncertainty in illness excluded zero, as detailed in Table 4. This pattern confirms the presence of statistically significant partial mediation, consistent with Hypothesis H1.
Collectively, these findings substantiate that: (1) social support directly enhances quality of life, (2) uncertainty in illness negatively impacts quality of life, and (3) social support exerts indirect effects on quality of life through reducing uncertainty in illness. The complete mediation model is schematically represented in Figure 2.
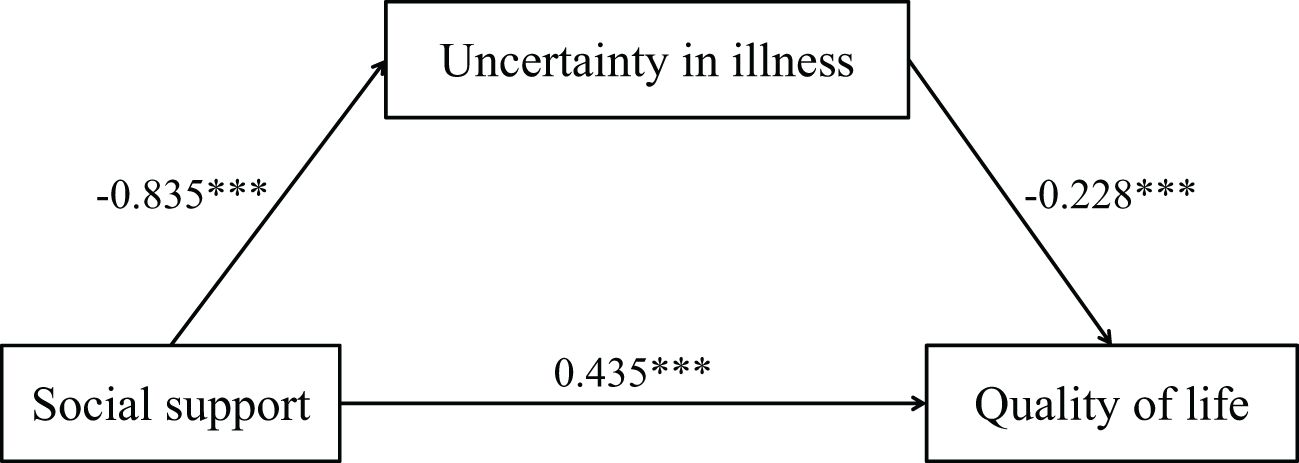
Figure 2. Illustration of the mediation effect of uncertainty in illness in the relationship between social support and quality of life. ***p<0.001.
3.4 Moderating effect test
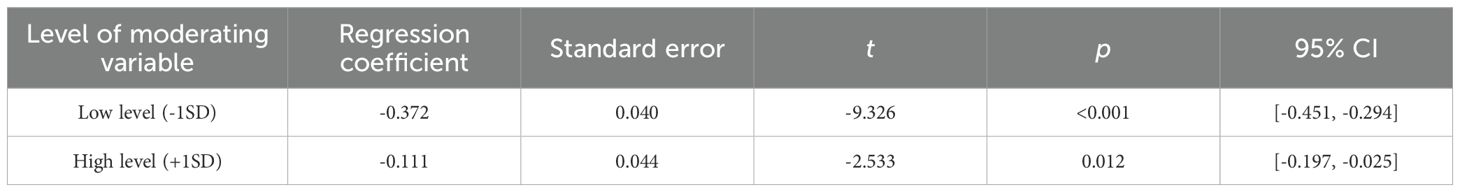
The moderated mediation analysis was performed using Model 14 PROCESS macro (version 3.5) in SPSS (39, 40), incorporating gender, age, and post-transplantation duration as covariates. All continuous predictors were mean centered prior to analysis to facilitate interaction interpretation. As presented in Tables 5, 6, the interaction term between Uncertainty in Illness and Psychological Resilience significantly predicted Quality of Life (B = 0.625, t = 8.342, p <.001), indicating a statistically significant moderating effect of psychological resilience on the uncertainty in illness-quality of life relationship, thereby confirming Hypothesis H2.
To elucidate the nature of this moderation, simple slope analysis was conducted at two conditional levels of the moderator: mean ±1 SD of Psychological Resilience (Figure 3). For individuals with low resilience levels (M -1 SD), uncertainty in illness demonstrated a strong negative association with quality of life (simple slope = -0.372, t = -9.326, p <0.001). Conversely, among high-resilience individuals (M +1 SD), this detrimental effect was substantially attenuated (simple slope = -0.111, t = -2.533, p < 0.05). The Johnson-Neyman technique further revealed that the conditional effect became nonsignificant (p > 0.05) when Psychological Resilience scores exceeded 1.8 SD above the mean (44, 45).
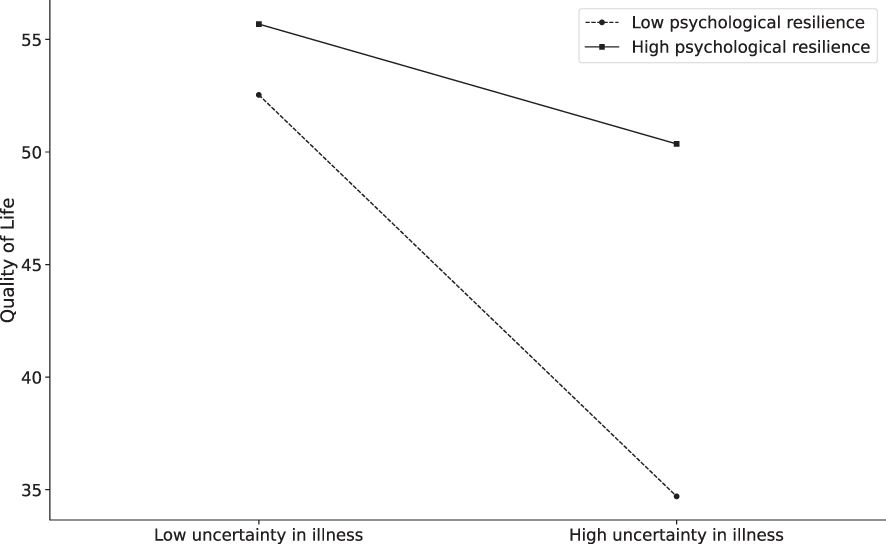
Figure 3. Psychological resilience moderates the relationship between Uncertainty in illness and Quality of life.
These findings collectively demonstrate that Psychological Resilience serves as a protective buffer, significantly mitigating the negative impact of uncertainty in illness on Quality of Life.
4 Discussion
This study identifies dual pathways linking social support to QoL in Chinese heart transplant recipients: a direct positive effect (B = 0.625, p < 0.001) and an indirect effect mediated through reduced illness uncertainty (indirect effect = 0.19, 95% CI [0.126, 0.265]). Critically, psychological resilience moderated the illness uncertainty-QoL relationship (interaction B = 0.007, p < 0.001). A quantifiable resilience threshold (≥ M + 1.8 SD) was identified, beyond which high resilience neutralized uncertainty’s negative impact on QoL (simple slope = -0.111 for high resilience, p = 0.012 vs. -0.372 for low resilience, p < 0.001).
These mechanisms operate within China’s collectivist context. Family systems reduce illness uncertainty through structured information mediation: relatives systematically translate clinical complexities using kinship-based decision protocols. This process enhances informational clarity, operationalizing social support’s uncertainty-reducing function observed in Chinese chronic illness populations (21, 46). Psychological resilience attenuates illness uncertainty’s impact through kinship-mediated coping processes rather than individual adaptive traits (47). This positions extended families as primary uncertainty regulators, with resilience operating as a socially contingent capacity distinct from Western autonomy-oriented coping models (10, 48).
4.1 The mediation effect of uncertainty in illness
Social support improves QoL by reducing uncertainty in illness. This mediating pathway represents a core psychosocial mechanism in transplant recovery. Our findings align with empirical studies of Chinese chronic illness populations demonstrating primary role of family systems in care provision (32, 46). This mediation process operates through observable behavioral patterns: kin networks integrate biomedical information using structured family decision-making processes (49). This translates health threats into collective responsibilities and reinforces treatment adherence through established norms of filial duty (21). Consequently, patients with strong family support exhibit significantly lower illness uncertainty when facing ambiguous prognoses (13), underscoring the effectiveness of this culturally embedded mechanism.
This family-centered pathway differs significantly from autonomy-focused Western models, where uncertainty management primarily occurs within individual-clinician partnerships (26). Our findings show a clear difference: multi-generational family involvement provides strong protection against medical uncertainty for patients. This protective effect is distinct and much less commonly observed in individualistic societies. Evidence supports this cultural contrast: studies show that when family support weakens, patients’ uncertainty levels rise significantly. In fact, this increase brings uncertainty up to levels typically seen in Western patient populations (50). Conversely, robust family networks offer substantially greater resilience against unpredictable health outcomes (51, 52). These empirically measured differences highlight the central role of families as active care coordinators who reshape the experience of illness (34), a function less emphasized in Western models prioritizing patient autonomy.
Clinically addressing illness uncertainty necessitates interventions that strategically engage families as cultural resources. Healthcare providers should train family members to communicate complex medical information using culturally resonant frameworks. These frameworks should be grounded in Confucian ethics (53, 54). This training involves two primary approaches. First, clinicians should guide families to reframe post-transplant complications using concepts like familial guardianship, thereby transforming biological threats into shared responsibilities (55). Second, treatment regimens should be interpreted through intergenerational commitment paradigms, explicitly linking clinical adherence to expressions of filial devotion (56). Collectively, this culturally adapted methodology reprocesses biomedical information via kinship-based cognition, converting illness uncertainty into actionable familial obligations (57).
4.2 The moderation effect of psychological resilience
Psychological resilience significantly moderated the illness uncertainty-QoL relationship (B = 0.007, p < 0.001). Simple slope analysis revealed a critical divergence: uncertainty strongly predicted reduced QoL in low-resilience recipients (B = -0.372, p < 0.001), but this effect attenuated markedly in high-resilience individuals (B = -0.111, p = 0.012). Crucially, resilience operated through culturally distinct pathways—specifically, recipients reframed health threats as opportunities to fulfill Confucian-based duties (e.g., enduring hardship for familial harmony) (47, 58). This collective coping mechanism fundamentally diverged from individual-focused resilience models (10).
The Johnson-Neyman technique quantified a significant threshold: uncertainty’s detrimental impact became non-significant (p > 0.05) when resilience exceeded 1.8 SD above the mean—indicating where collectivist cognitive processes effectively neutralize medical ambiguity. The result suggests possibility to implement intervention in clinical practices for heart transplantation recipients.
4.3 Limitations and future directions
While this study advances understanding of psychosocial pathways in Chinese heart transplant recipients, several limitations warrant attention. First, the cross-sectional design precludes causal inferences between variables. While the hypothesized mediation and moderation models align with theoretical frameworks, temporal dynamics (e.g., whether resilience develops after confronting uncertainty) remain unexamined. Future longitudinal studies tracking patients from pre-transplant evaluation to long-term recovery could elucidate how social support and resilience evolve across critical milestones (e.g., graft acceptance, relapse scares). Second, reliance on self-reported measures may introduce response bias, particularly for socially desirable constructs like resilience. For instance, participants might overreport familial harmony or underreport emotional distress due to cultural stigma. To enhance objectivity and mitigate this bias, future research should incorporate concrete triangulation strategies, such as clinician-rated assessments (e.g., structured psychiatric evaluations for anxiety/depression), objective behavioral metrics (e.g., immunosuppressant adherence monitored electronically), and biological stress markers (e.g., serial cortisol measurements). Third, the sample’s skewed demographics—75.2% male, predominantly younger adults—limit generalizability. Cultural norms emphasizing male authority in medical decisions (18) may explain this imbalance, but it also risks overlooking gender-specific challenges (e.g., caregiving burdens disproportionately affecting female recipients).
Future studies should employ stratified sampling to recruit underrepresented groups, including older adults (≥60 years) and women, and explore how gendered family roles modulate support effectiveness. Finally, while the study contextualizes resilience within Confucianism, it did not examine the critical influence of socioeconomic status (SES) and geographic origin (urban versus rural). These factors significantly impact both access to diverse forms of social support and the expression of cultural values. Regional heterogeneities in cultural practices (e.g., rural collectivism vs. urban individualism, ethnic minority traditions) combined with SES disparities were not examined. For example, rural families may rely more heavily on extended kinship networks for support, whereas higher-SES urban patients might prioritize professional counseling; similarly, economic constraints or urban/rural disparities in healthcare resources could profoundly affect stress levels and coping mechanisms. Future research should incorporate measures of SES and urbanicity to conduct comparative analyses, enabling the development of more nuanced and culturally adaptive interventions that resonate with localized values and resource availability.
4.4 Conclusion
This study identifies dual psychosocial pathways linking social support to QoL in Chinese heart transplant recipients: a direct path through enhanced familial cohesion and an indirect path through reduced illness uncertainty, with psychological resilience acting as a culturally significant moderator. Integrating Mishel’s Uncertainty in Illness Theory and the Connor-Davidson Resilience Scale within China’s collectivist context, we demonstrate how Confucian values, such as filial piety and collective endurance, shape adaptation processes, facilitating the management of uncertainty through family support. These findings address gaps in Western-centric psychosocial models by emphasizing cultural specificity, showing that resilience in this context functions not solely as individual trait but as a relational resource fostered within family narratives and communal obligations.
Clinically, these results highlight the need to develop family-integrated care protocols that combine culturally relevant resilience interventions (e.g., mindfulness integrated with family narratives) with structured family education to clarify post-transplant self-management. Policy initiatives should consider implementing routine psychosocial assessments to identify patients at higher risk due to low resilience or limited support networks, alongside exploring the potential for culturally adapted community-based peer support programs (e.g., tailored to rural kinship or urban professional settings). Integrating culturally informed, evidence-based psychosocial care within the Chinese transplant system provides a practical framework for improving long-term patient outcomes.
Data availability statement
The datasets analyzed during the current study contain sensitive information and are subject to ethical, legal, and privacy restrictions. Data may be made available by the corresponding author upon reasonable request with appropriate institutional review board (IRB) approval and data use agreements.
Ethics statement
Ethical approval was obtained from the Ethics Committee of Medical School, Shenzhen University (No. PN-20250097). Informed consent was obtained from all individual participants included in the study. Participants were informed of their right to withdraw at any stage, and the confidentiality of their data was strictly maintained throughout the research process.
Author contributions
CG: Investigation, Writing – original draft, Data curation, Formal Analysis, Writing – review & editing, Methodology, Conceptualization. SG: Formal Analysis, Data curation, Writing – review & editing. LZ: Writing – review & editing, Methodology. XB: Investigation, Data curation, Writing – review & editing. HS: Writing – review & editing, Supervision, Conceptualization. CJ: Writing – review & editing, Validation, Supervision.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We extend our deepest gratitude to all contributors who supported and participated in this research. We sincerely appreciate the participants for their time and dedication in completing the questionnaires.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1637110/full#supplementary-material
References
1. Gerhardt A, Weidner G, Grassmann M, and Spaderna H. Everyday physical activity in ambulatory heart transplant candidates: the role of expected health benefits, social support, and potential barriers. Int J Behav Med. (2014) 21:248–57. doi: 10.1007/s12529-013-9304-3
2. Keith F, Krantz DS, Chen R, Harris KM, Ware CM, Lee AK, et al. Anger, hostility, and hospitalizations in patients with heart failure. Health Psychol. (2017) 36:8295. doi: 10.1037/hea0000519
3. Peter-Marske KM. Associations of Social Relationships With Self-rated Health and Heart Failure. (PhD dissertation). The University of North Carolina at Chapel Hill (2024).
4. Brantmark A, Forsberg A, Lennerling A, Herlenius G, and Engström M. Beyond survival: unveiling psychological and social adaptation after visceral transplantation. J Clin Nurs. (2025). doi: 10.1111/jocn.17666
5. Mishel, M H. Reconceptualization of the uncertainty in illness theory. Image: J Nurs Scholarship. (1990) 22:256–62. doi: 10.1111/j.1547-5069.1990.tb00225.x
6. Asgari P, Jackson AC, and Bahramnezhad F. Adjustment to a new heart: Concept analysis using a hybrid model. Iranian J Nurs Midwifery Res. (2021) 26:89–965. doi: 10.4103/ijnmr.IJNMR_9_20
7. Brown J. The role of social support in coping with chronic illnesses. Res Consortium Arch. (2024) 2:38–45. Available online at: http://rc-archive.com/index.php/Journal/article/view/21.
8. Helgeson VS. Social support and quality of life. Qual Life Res. (2003) 12:25–31. doi: 10.1023/A:1023509117524
9. Zhang N, Tang X-Q, Lu K, Dong Q, Kong L-N, Jiang T-T, et al. Illness uncertainty, self-perceived burden and quality of life in patients with chronic myeloid leukaemia: a cross-sectional study. J Clin Nurs. (2022) 31:2935–42. doi: 10.1111/jocn.v31.19-20
10. Connor KM and Davidson JRT. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depression Anxiety. (2003) 18:76–825. doi: 10.1002/(ISSN)1520-6394
11. Yu X and Zhang J. Comparison of self-resilience scale and Connor-Davidson Resilience Scale. J psychol Sci. (2007) 05:1169–71. doi: 10.16719/j.cnki.1671-6981.2007.05.035
12. Mishel MH. Uncertainty in illness. Image: J Nurs Scholarship. (1988) 20:225–32. doi: 10.1111/j.1547-5069.1988.tb00082.x
13. Wang Y, Li F, Qiao W, Zhang J, and Dong N. Global challenges and development of heart transplantation: Wuhan Protocol development and clinical implementation. Chin Med J. (2025). doi: 10.1097/CM9.0000000000003715
14. Kekrebesi GA. Perceived Social Support and Emotional Regulation as Predictors of Health-Related Quality of Life among Patients with End-Stage Renal Disease. (PhD dissertation). University of Cape Coast (2021).
15. Alshraifeen A, Al-Rawashdeh S, Alnuaimi K, Alzoubi F, Tanash M, Ashour A, et al. Social support predicted quality of life in people receiving haemodialysis treatment: A cross-sectional survey. Nurs Open. (2020) 7:1517–15255. doi: 10.1002/nop2.v7.5
16. Ruiz-Rodríguez I, Hombrados-Mendieta I, Melguizo-Garín A, and Martos-Méndez MJ. The association of sources of support, types of support and satisfaction with support received on perceived stress and quality of life of cancer patients. Integr Cancer therapies. (2021) 20:1534735421994905. doi: 10.1177/1534735421994905
17. El Hadi SN, Zanotti R, and Danielis M. Lived experiences of persons with heart transplantation: A systematic literature review and meta-synthesis. Heart Lung. (2025) 69:174–84. doi: 10.1016/j.hrtlng.2024.10.013
19. Ma Z, Huang Y, Wu J, Dong W, and Qi L. What matters for knowledge sharing in collectivistic cultures? Empirical evidence from China. J Knowledge Manage. (2014) 18:1004–10195. doi: 10.1108/JKM-06-2014-0252
20. Yi M, Zhao B, Zhang X, and Wang Z. Exploration of subgroups and associated factors of the uncertainty in illness among older adults with chronic heart failure: A latent profile analysis. Geriatric Nurs. (2025) 61:470–8. doi: 10.1016/j.gerinurse.2024.12.025
21. Hu N, Yang Z, and Wang A. Early post-Transplant adaptation experience in young and middle-Aged people with kidney transplant in China: A qualitative study. Western J Nurs Res. (2024) 46:356–3655. doi: 10.1177/01939459241238683
22. Pankenier DW. Astrology and cosmology in early China: Conforming earth to heaven. Cambridge, England: Cambridge University Press (2013).
23. Haug SHK, DeMarinis V, Danbolt LJ, and Kvigne K. The illness reframing process in an ethnic-majority population of older people with incurable cancer: variations of cultural-and existential meaning-making adjustments. Ment Health Religion Culture. (2016) 19:150–63. doi: 10.1080/13674676.2015.1126705
24. Skojec TA, Davidson TM, and Kelechi TJ. The relationship between uncertainty in illness and psychological adjustment to chronic illness. J Health Psychol. (2024), 4(2025):622–37. doi: 10.1177/13591053241249861
25. Cohen S and Wills TA. Stress, social support, and the buffering hypothesis. psychol Bull. (1985) 98:3105. doi: 10.1037/0033-2909.98.2.310
26. Baik D, McIlvennan CK, Baker C, and Coats H. Caregiving experiences of older family caregivers of persons with heart failure: a mixed methods study. Geriatric Nurs. (2022) 48:51–7. doi: 10.1016/j.gerinurse.2022.08.015
27. An Y, Zhang Y, Wang L, Chen C, and Fan X. The relationship between uncertainty in illness and quality of life in patients with heart failure: Multiple mediating effects of perceived stress and coping strategies. J Cardiovasc Nurs. (2022) 37:257–2655. doi: 10.1097/JCN.0000000000000799
28. Li F, Wang Y, Sun Y, Zhang J, Li P, and Dong N. Heart transplantation in 47 children: single-center experience from China. Ann Trans Med. (2020) 8:4675. doi: 10.21037/atm.2020.03.99
29. Zheng X, Xue Y, Dong F, Shi L, Xiao S, Zhang J, et al. The association between health-promoting-lifestyles, and socioeconomic, family relationships, social support, health-related quality of life among older adults in China: a cross sectional study. Health Qual Life outcomes. (2022) 20:645. doi: 10.1186/s12955-022-01968-0
30. Zamanian H, Amini-Tehrani M, Jalali Z, Daryaafzoon M, Ramezani F, Malek N, et al. Stigma and quality of life in women with breast cancer: mediation and moderation model of social support, sense of coherence, and coping strategies. Front Psychol. (2022) 13:657992. doi: 10.3389/fpsyg.2022.657992
31. Meraz R, McGee J, Caldwell EP, Ke W, and Osteen K. The impact of resilience, health literacy, and social support on medication adherence and self-care among adults with heart failure. J Cardiovasc Nurs. (2023) 38:415–4245. doi: 10.1097/JCN.0000000000000948
32. Hu X-J, Dong N-G, Liu J-P, Li F, Sun Y-F, and Wang Y. Status on heart transplantation in China. Chin Med J. (2015) 128:3238–32425. doi: 10.4103/0366-6999.170238
33. Sun Y-f, Wang Z-w, Zhang J, Cai J, Shi F, and Dong N-g. Current status of and opinions on heart transplantation in China. Curr Med Sci. (2021) 41:841–6. doi: 10.1007/s11596-021-2444-9
34. Gao C and Shen H. Study of the images and contents in typical dreams of heart transplant recipients. Dreaming. (2021) 31:3205. doi: 10.1037/drm0000183
35. Xie Q and Wong DFK. Culturally sensitive conceptualization of resilience: A multidimensional model of Chinese resilience. Transcultural Psychiatry. (2021) 58:323–3345. doi: 10.1177/1363461520951306
36. Ware JE, Snow KK, Kosinski M, and Gandek B. SF-36 health survey. Manual and interpretation guide 2. (Boston, Masschusetts, US: Nimrod Press). (1993).
37. Xiao S. Theoretical foundation and research applications of the Social Support Rating Scale. J Clin Psychiatry. (1994) 2:98–100.
38. Shue S and Huang SL. Mishel's Uncertainty in Illness Scalem, Chinese version. J Nurs Res. (1996) 4:59–675.
40. Hayes SC, Hofmann SG, Stanton CE, Carpenter JK, Sanford BT, Curtiss JE, et al. The role of the individual in the coming era of process-based therapy. Behav Res Ther. (2019) 117:40–53. doi: 10.1016/j.brat.2018.10.005
41. Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, US: Guilford publications (2017).
42. Preacher KJ and Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. (2008) 40:879–8915. doi: 10.3758/BRM.40.3.879
43. Podsakoff PM, MacKenzie SB, Lee J-Y, and Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:8795. doi: 10.1037/0021-9010.88.5.879
44. Johnson PO and Fay LC. The Johnson-Neyman technique, its theory and application. Psychometrika. (1950) 15:349–3675. doi: 10.1007/BF02288864
45. D’Alonzo KT. The Johnson-Neyman procedure as an alternative to ANCOVA. Western J Nurs Res. (2004) 26:804–12. doi: 10.1177/0193945904266733
46. Zhang D, Zhang N, Chang H, Shi Y, Tao Z, Zhang X, et al. Mediating role of hope between social support and self-management among Chinese liver transplant recipients: a multi-center cross-sectional study. Clin Nurs Res. (2023) 32:776–7845. doi: 10.1177/10547738221078897
47. Ye ZJ. Resilience in chronic disease. Front Psychiatry. (2022) 13:846370. doi: 10.3389/fpsyt.2022.846370
48. Man J, Yan R, Yang K, Ouyang Y, Shu C, Sun J, et al. Cognitive behavioral therapy in China: practices and exploration. Int J Cogn Ther. (2024) 17:231–2505. doi: 10.1007/s41811-024-00203-6
49. Liu Q-Q, Yang X-J, Hu Y-T, Zhang C-Y, and Nie Y-G. How and when is family dysfunction associated with adolescent mobile phone addiction? Testing a moderated mediation model. Children Youth Serv Rev. (2020) 111:104827. doi: 10.1016/j.childyouth.2020.104827
50. Ng R and Indran N. Societal perceptions of caregivers linked to culture across 20 countries: Evidence from a 10-billion-word database. PloS One. (2021) 16:e02511615. doi: 10.1371/journal.pone.0251161
51. Bates CR, Nicholson LM, Rea EM, Hagy HA, and Bohnert AM. Life interrupted: Family routines buffer stress during the COVID-19 pandemic. J Child Family Stud. (2021) 30:2641–26515. doi: 10.1007/s10826-021-02063-6
52. Acoba EF. Social support and mental health: the mediating role of perceived stress. Front Psychol. (2024) 15:1330720. doi: 10.3389/fpsyg.2024.1330720
53. Stephens GC, Sarkar M, and Lazarus MD. Medical student experiences of uncertainty tolerance moderators: a longitudinal qualitative study. Front Med. (2022) 9:864141. doi: 10.3389/fmed.2022.864141
54. Bai P, Tang Y, Zhang W, and Zeng M. Does economic policy uncertainty matter for healthcare expenditure in China? A spatial econometric analysis. Front Public Health. (2021) 9:673778. doi: 10.3389/fpubh.2021.673778
55. Knight B, Keane N, Benea D, and Stone R. Values and the experience of family care-giving: cultural values or shared family values? Ageing Soc. (2024) 44:61–785. doi: 10.1017/S0144686X2200006X
56. Xiao C, Patrician PA, Montgomery AP, Wang Y, Jablonski R, and Markaki A. Filial piety and older adult caregiving among Chinese and Chinese-American families in the United States: a concept analysis. BMC Nurs. (2024) 23:1155. doi: 10.1186/s12912-024-01789-0
57. Yu Z, Sun D, and Sun J. Social support and fear of cancer recurrence among Chinese breast cancer survivors: the mediation role of illness uncertainty. Front Psychol. (2022) 13:864129. doi: 10.3389/fpsyg.2022.864129
Keywords: heart transplantation, social support, uncertainty in illness, psychological resilience, quality of life, moderated mediation model
Citation: Gao C, Gui S, Zhu L, Bian X, Shen H and Jiao C (2025) Social support and quality of life in Chinese heart transplant recipients: mediation through uncertainty in illness and moderation by psychological resilience. Front. Psychiatry 16:1637110. doi: 10.3389/fpsyt.2025.1637110
Received: 28 May 2025; Accepted: 30 June 2025;
Published: 22 July 2025.
Edited by:
Domenico De Berardis, ASL 4, ItalyReviewed by:
Anubhuti Dubey, Deen Dayal Upadhyay Gorakhpur University, IndiaVassilis Martiadis, Department of Mental Health, Italy
Copyright © 2025 Gao, Gui, Zhu, Bian, Shen and Jiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Heyong Shen, c2hlbmhleW9uZ0Bob3RtYWlsLmNvbQ==; Can Jiao, amlhb2NhbkBzenUuZWR1LmNu
 Chan Gao
Chan Gao Song Gui1,2
Song Gui1,2 Heyong Shen
Heyong Shen Can Jiao
Can Jiao