- 1Center for Psychiatry, Justus Liebig University Giessen, Giessen, Germany
- 2Department of Psychiatry and Neurosciences, Charité – Universitätsmedizin Berlin, Berlin, Germany
Introduction: Migration-related stressors (MRS), such as loss, cultural conflict, and language barriers, are linked to increased psychological distress. This study investigates the impact of MRS on de-pressive symptoms and somatization among Turkish-speaking first-generation migrants in Germany.
Method: In a cross-sectional study, 60 psychiatric outpatients completed standardized measures as-sessing MRS, depressive symptoms (BDI-II), and somatization (PHQ-15). Regression analy-ses controlled for age, gender, and socioeconomic status.
Results: Higher MRS significantly predicted both depressive symptoms and somatization. Somatic complaints were particularly associated with language difficulties, separation experiences, and intergenerational value conflicts.
Conclusion: Findings support the need to integrate cultural humility—defined as clinician self-awareness, openness, and contextual sensitivity—into evidence-based care. Symptom interpretation must consider patients’ migration histories and cultural frameworks. Culturally adapted, person-centered interventions may improve diagnostic accuracy and treatment outcomes for migrant populations.
Introduction
Germany remains one of the main destinations for migrants in Europe (1, 2). Currently, about one in four residents has a migration background, accounting for 26.0% of the population. Having a migration background is defined as being a person or having at least one parent who was not born with German citizenship. The largest migrant group in Germany originates from Turkey. Historically, between the 1960s and 1970s, approximately 750,000 to 900,000 Turkish guest workers arrived, and today about 2.8 million people of Turkish origin live in Germany (3). These individuals can be distinguished by migration circumstances and generational status, with each generation facing distinct challenges. Although, according to the Federal Commissioner for Integration, integration has improved in general, many institutions are still not adequately adapted to the realities of a diverse society (4). The exact number of first-generation Turkish migrants is difficult to determine, as many have naturalized and are no longer counted as foreigners in statistics.
With regard to mental health, migrants are at elevated risk for psychiatric disorders such as somatoform disorders, substance abuse, depression, and psychosis (5). Against this background, it becomes evident that the Turkish population in Germany is disproportionately affected by specific challenges in accessing mental health services. Turkish migrants in Germany encounter structural barriers - including language difficulties, lack of culturally sensitive services, and financial constraints - as well as non-structural barriers such as stigma, mistrust, and culturally specific expressions of psychological distress, which may lead to misdiagnosis. These factors collectively reduce help-seeking and worsen mental health outcomes among Turkish patients (6–8). Culturally adapted interventions, language-appropriate services, community outreach, and cultural mediators are therefore essential.
Migration processes and mental health
Migration can entail both protective and adverse effects on mental health. On the positive side, improved socioeconomic conditions and future prospects may enhance well-being (9). On the contrary, migration constitutes a critical life event that involves acculturative stress, often accompanied by physical and psychological problems (10, 11).
Although migration per se is not causally related to mental illness, numerous studies demonstrate a strong association between migration-related stressors (MRS) and psychiatric disorders, including dose-response effects: the greater the number of MRS, the higher the prevalence of mental disorders (9, 12). Stressors may occur before, during, and after migration, including separation from family, loss of familiar lifestyles, loneliness, discrimination, socioeconomic hardship, separation grief, communication difficulties or language barriers, unemployment, unmet expectations, and stigmatization.
A retrospective study of 268 immigrant patients in a psychiatric intensive care unit (13) found that 51.9% experienced acculturation stress, especially men, single individuals, unemployed persons, and those without residence permits. Acculturation stress was associated with psychotic disorders, first psychiatric episodes, and poorer outcomes at discharge. Similarly, Choy et al. (14) showed that marginalization had the most detrimental, and integration the most beneficial effects on mental health.
The nature of stressors differs between first- and second-generation migrants. The first generation faces challenges linked to migration motives, journey, and language acquisition, while the second generation more frequently struggles with identity-related issues, prejudice, and discrimination (15).
Migrants - particularly those who relocate by choice rather than through forced displacement - experience a distinct spectrum of stressors related to their migration. Pre-migration stressors in the context of voluntary migration often involve socioeconomic challenges such as limited educational or occupational opportunities, rather than persecution or war. For example, migrants may depart in search of improved career prospects or educational advancement, yet still face internal pressures such as high expectations or a sense of opportunity loss if those aspirations are unmet (16, 17). Post-migration stressors, emerging after arrival in the host country, frequently include education-occupation mismatch, discrimination, poor working conditions, and acculturative stress - with the latter sometimes described as a fatigue-inducing process marked by language difficulties, loneliness, and cultural disorientation (17).
Empirical studies suggest that while pre-migration pressures in voluntary migrants may derive from personal or socioeconomic motivations, the stressors encountered post-migration often have greater impact on mental health outcomes. Voluntary migrants are reported to experience roughly 50% less acculturative stress than refugees, yet still face substantial challenges such as over-qualification, underemployment, and barriers to social integration, all of which correlate strongly with depression and anxiety (16, 17).
Addressing post-migration stressors - e.g., through recognition of foreign qualifications, culturally sensitive workplace policies, and integration programs - represents a key target for prevention.
Language as a key factor
Language and communication are central determinants of integration and mental health. Insufficient language skills hinder healthcare access, impair diagnostic accuracy, and weaken therapeutic alliances. Educational attainment also plays a role: the first generation of Turkish migrants, recruited primarily as industrial workers in the 1960s and 1970s, often had limited educational opportunities, a disadvantage that affected subsequent generations. In particular for the first generation, language barriers were a significant obstacle to integration into the education system and the labour market (18, 19). In recent decades, the levels of education and qualifications among migrants have improved. Children and grandchildren of first-generation migrants are increasingly achieving higher educational qualifications. Many younger migrant families strongly emphasize education, and targeted support measures are helping to foster this development.
Limited host-country language proficiency is consistently associated with an increased prevalence and severity of psychiatric disorders, including psychotic, affective, anxiety, and post-traumatic stress disorders (20). In psychiatric care, low language proficiency correlates with poorer treatment outcomes and a greater likelihood of coercive interventions, such as involuntary admission, forced medication, and restraint (21). Studies show that better language skills - more common among women, legally residing migrants, and those from European countries - are linked to later illness onset and shorter treatment duration (22, 23). Systematic reviews confirm that language barriers reduce utilization of mental health services and contribute to underdiagnosis (24, 25). Addressing this modifiable stressor through structured language training and professional interpretation services should be a core component of culturally responsive psychiatric care.
Perceived discrimination is another key MRS (26). According to the 14th Integration Report, one in five immigrants and one in four descendants report personal experiences of discrimination (4). Discrimination in employment, housing, education, or public services contributes to psychological distress, and fear of discrimination further discourages the utilisation of healthcare, particularly for mental illness.
Migration and susceptibility to illness
The health burden of migration is particularly pronounced when disadvantages in multiple life domains accumulate (27). Many migrants live with low socioeconomic status, limited social networks, and exposure to migration-related stressors, which collectively increase vulnerability (28). Sociodemographic factors such as poverty, limited participation opportunities, and institutional discrimination should be considered alongside interpersonal experiences of prejudice (26).
Numerous studies confirm a higher prevalence of psychiatric disorders among migrants, including somatoform disorders, depression, substance abuse, and psychosis (5, 26, 28–30). Turkish migrants in Germany exhibit elevated vulnerability and lower utilisation of psychiatric services, often resulting in delayed treatment and longer duration (31). Contributing factors include fear of stigmatization, somatically oriented illness concepts, and lack of therapy options in Turkish.
Culturally influenced illness perceptions and treatment barriers
Cultural and religious beliefs can strongly shape illness concepts in Turkish migrants. In Islam, illness may be interpreted as fate, while supernatural attributions such as spirits (Cins) or the Nazar (evil eye) remain common (31–35). Folk medicine explanations are prevalent in cases of psychological distress, unclear symptoms, or when other treatments fail and may relieve personal guilt and legitimize illness roles within families and communities (33). Consequently, many first-generation migrants prefer traditional healers (e.g., Hoca) over psychiatric care.
During treatment by German doctors, migrants of Turkish origin may not fully understand the doctor’s recommendations and instructions, leading to inadequate treatment adherence and compliance. At the same time, they often present with culturally distinct symptoms, which can lead to misdiagnoses and complicated treatment courses. These perceptions of the illness, combined with language barriers, complicate medical treatment. Turkish patients often attribute illness to external factors and hold high expectations of healthcare providers, creating additional challenges. Addressing these culturally shaped perceptions is therefore crucial for effective treatment (31, 36).
Summary and study objective
Investigating migration-related stressors among Turkish migrants - particularly first- and second-generation - in Germany is of high relevance given their longstanding presence and distinct sociocultural dynamics. Research shows that first-generation migrants adopting marginalisation or separation acculturation patterns exhibit higher depressive symptoms, while integration correlates with lower burden (7). Separation and marginalization are also associated with reduced health-related quality of life, particularly among descendants, while integration has protective effects (37).
Epidemiological data highlight the substantial mental health burden: In a representative sample of Turkish migrants in Hamburg and Berlin, lifetime prevalence of any mental disorder was 78.8%, with mood disorders (41.9%), anxiety disorders (35.7%), and somatoform disorders (33.7%) being most common. Differences between first- and second-generation migrants were limited, except for higher bipolar disorder rates in the second generation (Dingoyan et al., 2017). In another cohort, first-generation migrants - especially of Turkish origin - showed a higher prevalence of depressive and anxiety symptoms and suicidal ideation compared to native Germans, while the second generation did not show significant differences (38).
Therefore, this study examines migration-related stressors and their relationship to depression and somatization among Turkish-speaking migrants in Germany. The aim is to clarify how such stressors influence the development and course of these disorders, and to derive implications for treatment. By focusing on this population, the study addresses a critical research gap and contributes to culturally sensitive intervention strategies and improved access to care.
Methods
Procedure
The study focused on patients of Turkish origin who underwent native language outpatient treatment at a University Hospital for Psychiatry and Psychotherapy.
The study was carried out in the outpatient clinic of a university hospital by a Turkish physician and board-certified specialist in psychiatry and psychotherapy (YE). She worked within a multidisciplinary team comprising a senior psychiatric consultant, additional medical specialists, resident physicians, psychologists and medical assistants, ensuring comprehensive clinical evaluation and care.
The study involved a single interview, randomly occurring during outpatient treatment after diagnosis. Data collected during outpatient treatment, such as essential documentation and patient records, were used whenever possible. Efforts were made to minimize the time burden on each patient. Visual scales and detailed explanations were provided for closed and written questions with predefined answer options to facilitate patient responses. The study population consisted of patients from the outpatient clinic in the Clinic for Psychiatry and Psychotherapy at the University Hospital in Giessen.
Eligible participants were individuals of Turkish origin who were receiving treatment in the psychiatric outpatient clinic, met ICD-10 diagnostic criteria for at least one depressive episode (F32.0–F32.2 or F33.0–F33.2), and provided written informed consent. Exclusion criteria included a clinical judgement of the treating physician that participation might interfere with ongoing treatment or adversely affect the participant’s well-being; inability to provide informed consent or refusal to participate; the presence of severe mental impairment, e.g., intellectual disability, dementia, psychotic disorder or delusional depression, acute intoxication, markedly reduced consciousness, or acute suicidality. The data collection phase occurred between January 2022 and April 2022. Patients who met the inclusion and exclusion criteria were informed about the study through personal conversations with the treating specialist. Those providing written consent were briefed verbally and in writing about the purpose, process, and content of the interview. Patients had the option to terminate the survey at any time without consequences. In the clinic, diagnoses are routinely reviewed, validated, and coded on a quarterly basis; prior to the interview, each diagnosis was reevaluated. All patients included were undergoing ongoing outpatient treatment in the clinic at the time of participation. The interview, which included half an hour for explanation and consent and an hour for questionnaire completion, lasted a total of one and a half hours. Following the interview, of the responses were checked for completeness, and the treating physician evaluated the patients based on their questionnaires. All questionnaires were numbered and stored in locked cabinets in the clinic’s outpatient department. The study was approved by the Ethics Committee of the Medical Faculty of the University of Giessen and was conducted in accordance with the Declaration of Helsinki.
Instruments
Questionnaire on sociodemographics and illness characteristics
Survey on medical history and psychosocial status, including questions on sociodemographics and illness characteristics. It includes inquiries about biography, sociodemographics, social networks, the patient’s illness characteristics, and treatment.
Questionnaire on Migration-Related Stressors
The Migration-Related Stressors (MRS) questionnaire was developed by Lujic (31) to assess migration-dependent stress factors. For this study, the questions were reevaluated to determine, through a list of 26 questions, whether the corresponding stress factor is present and the extent of the patient’s suffering.
Beck Depression Inventory
The Beck Depression Inventory (BDI) (39) measures the severity of depressive symptoms in individuals aged 13 and above in a clinical setting. Symptoms are described on affective, somatic, and cognitive levels, referring to the past week. The inventory consists of 21 items. We used the Turkish version from Hisli (40).
Screening for Somatoform Disorders
The Screening for Somatoform Disorders (SOMS) (41) is used for the classification, quantification, and description of somatoform disorders based on the criteria of Somatization Disorder according to DSM-IV (42) and ICD-10 (43) within the last 2 years. The Turkish version of SOMS is attributed to Erim et al. (44).
Migration-related stressors
Different types of MRS were assessed using a list of 25 questions, initially formulated by Lujic (31) to evaluate the treatment of Turkish migrants in Germany (see Table 1). Participants were asked whether each specific stressor had occurred (“yes” = 1) or not (“no” = 0) during their migration process.
Individual item scores from the MRS list were totaled to create a Migration Stressor Quantity (MSQ) index, where higher scores indicated a greater number of perceived stressors. Scores were calculated only when more than 75% of the relevant data were provided.
Statistical analysis
For the main analysis, hierarchical linear regression models were applied to assess the impact of the quantity of MRS on self-reported depressive symptoms and somatization. In the first step, sociodemographic variables (age, sex, and education level) were included as control variables, followed by the introduction of the quantity of MRS as the primary predictor in the second step. The BDI-II total score and SOMS scores were included as separate outcome variables.
All statistical analyses were conducted using IBM SPSS (Version 26). Values of p ≤ 0.05 were regarded as statistically significant, while values of p ≤ 0.001 were deemed highly significant. All reported p-values are based on two-tailed tests.
Results
Demographic-, clinical-, and migration-related sample characteristics
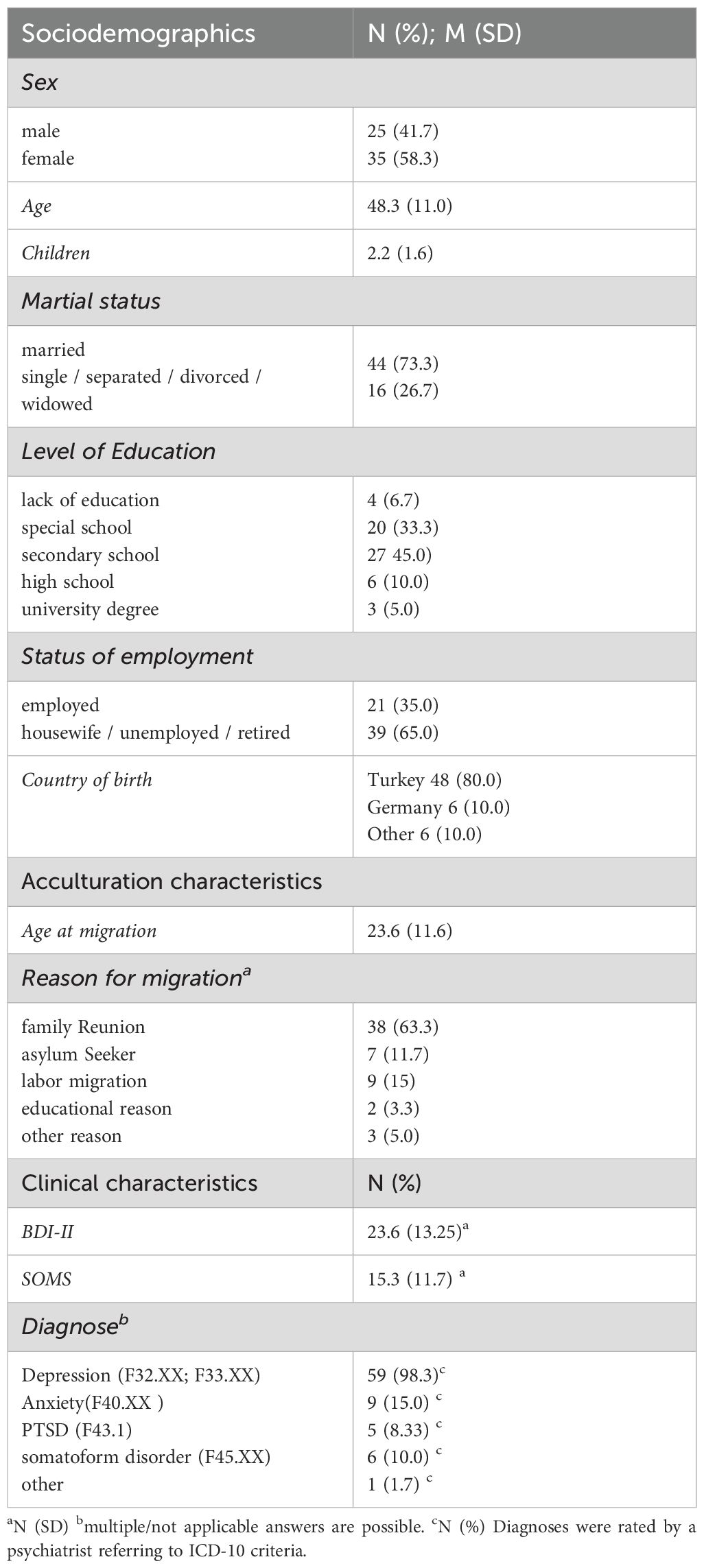
In total, 60 Turkish-origin patients who met the inclusion criteria (having secure residential status and having rated more than 75% of the MRS items) participated in the study, which included 35 women and 25 men. The mean age was 48.32 years. On average, participants had resided in the host country for 24.03 years (SD = 14.8). A notable 93.3% of the participants were first-generation migrants, while 6.7% were born in Germany. Additionally, 43.3% of individuals originated from urban regions, and 56.7% came from rural areas. The average age at the time of migration was 23.58 years. The primary reason for migration was cited as family reunification (63.3%), followed by political (11.7%) and economic (8.3%) reasons, job search (6.7%), and studying (3.3%). Moreover, 73.3% of the participants were married, with an average of 2.2 children. Participants mainly arrived in Germany during their youth, lacking professional qualifications from Turkey, and consequently engaged in unskilled occupations in Germany. They predominantly had two or more F-diagnoses. Regarding somatic comorbidities, 55% of the subjects had at least one somatic comorbidity, with arterial hypertension being the most common (35%), followed by diabetes mellitus (10%).
For further information, see Table 1.
Psychometric characteristics of the instruments utilized
The average intercorrelation (Cronbach’s α) of the total BDI-II items was α = .93, indicating a high internal consistency for the BDI-II. The SOMS questionnaire also demonstrated excellent internal consistency with Cronbach’s α = .918. MSR, with Cronbach’s α = .785, was also considered reliable.
BDI-II and SOMS
The mean BDI-II total score was 23.6 (SD = 13.25), indicating moderate to severe symptomatology among patients of Turkish origin.
Turkish-origin patients exhibited a strong tendency towards somatization in the screening for somatoform disorders (SOMS). The mean SOMS total score of 15.3 (SD = 11.7) indicates moderate to severe somatization symptomatology. They reported significantly more physical symptoms and symptoms of somatization disorder without an organic cause than the standard sample from the general population (Complaint Index according to DSM-IV and ICD-10 criteria).
Both measures (BDI-II and SOMS) were significantly correlated (r = .506, p <.001), indicating an overlap between depression and somatization in the sample (see Table 1).
Migration-related stressors
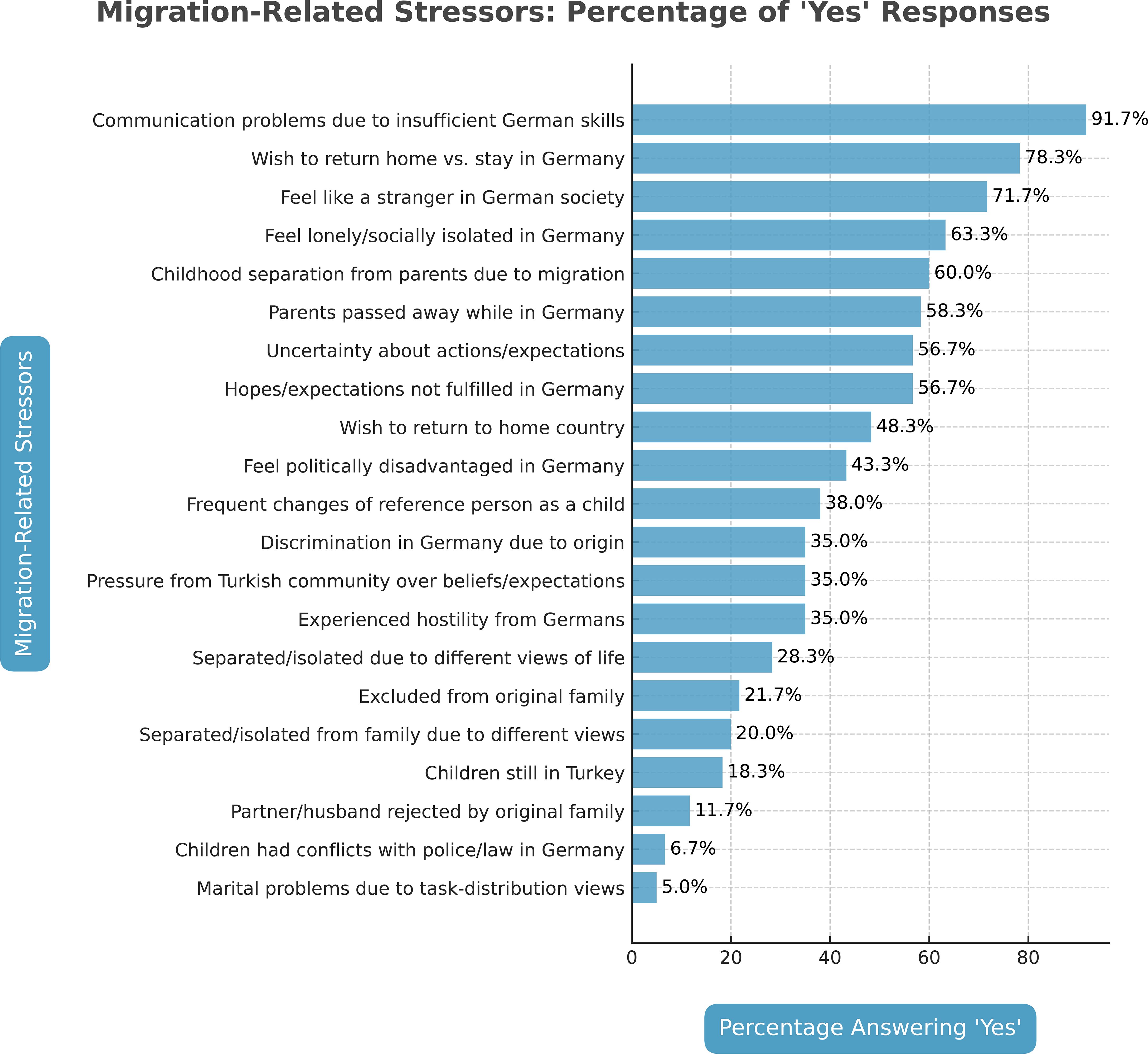
Communication problems were most frequently reported regarding migration-related stressors. However, missing family in Turkey, the desire to return, associated indecision, and difficulties adapting to German society were perceived as burdensome. Language issues constituted the greatest burden for 91.7%. More than half of the patients also mentioned prolonged separations from parents during childhood, the death of parents in their absence, loneliness, and feelings of isolation as stressors. Many Turkish-origin patients struggled with a lack of social competence, indicating that they could not assess what others expected of them. Consequently, uncertainties about expectations, unmet personal ambitions, and hopes were identified as stressors. Turkish-origin patients often described experiences of xenophobia and feeling pressured by peers in Turkish society. In contrast, marital problems arising from differing views on task distribution and issues involving children with law enforcement were less frequently reported. (In detail, see Figure 1).
MSQ as predictor and BDI-II and SOMS total scores as outcome variables
Hierarchical linear regression models revealed significant effects of migration stressor quantity (MSQ) as a predictor of the BDI-II and SOMS scores (see Table 2).
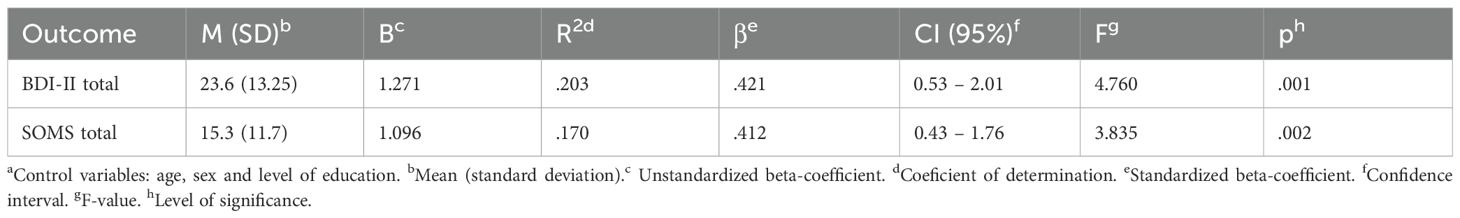
Table 2. Hierarchical regressionsa of the MRS-quantity on depressive (BDI-II) and somatization (SOMS) symptoms.
The MSQ predictor significantly affects the BDI-II total score (F (3) = 4.76, p = .001, η2 = .203), with a greater magnitude of experienced MSR associated with a higher burden of depressive symptoms.
Regarding somatization, the MSQ significantly predicted SOMS values (F (3)=3.835, p=.002, η2 = .170), indicating that greater experienced MSR is associated with a higher level of somatization.The sociodemographic factors of age, gender, and level of education, which were used as control variables, had no substantial effect on the results of the regression analyses (all p >.005).
Discussion
The present study systematically examined migration-related stressors (MRS) and their mental health impact in a sample of migrants treated in a psychiatric hospital setting. Several central findings stand out. First, a very high proportion of patients reported language-related difficulties, with 91.7% indicating that communication barriers significantly affected their ability to interact with healthcare professionals. In addition, more than 78% expressed a desire to return to their country of origin, 63% reported feelings of social isolation in Germany, 60% had been separated from parents due to migration, and 58% had experienced the death of a close family member. Participants also reported uncertainties regarding their future expectations, and more than half indicated that their migration-related expectations had not been fulfilled. These figures illustrate the cumulative burden of MRS and highlight the relevance of acculturative stress as a central determinant of psychological well-being in this population. In light of the citizenship law reforms in Germany enacted in June 2024 - facilitating shorter residency requirements and permitting mulitple citizenship - the relevance of MRS is expected to further increase (4). In our study, participants exhibited moderate to severe levels of both depression (BDI-II) and somatization (SOMS), with a significant correlation indicating substantial symptom overlap.
Second, we found a strong association between MRS and depressive symptomatology. Most notably, there was a dose-response relationship between the number of stressors and depressive symptom severity, suggesting that the accumulation of migration-related stressors is directly linked to an increased risk of depression. This finding is consistent with previous research, which has described a ‘risk accumulation’ model in migrant mental health, where the number and intensity of MRS, rather than a single factor, predict psychiatric outcomes (9, 12).
Third, our study underscores the role of somatization. Migrants with higher levels of MRS reported significantly more somatic symptoms, and we observed a positive correlation between somatization and the number of migration-related stressors. This is particularly relevant in the context of somatic hospitals, where somatization often leads to repeated medical consultations and potentially unnecessary diagnostic procedures. Our study confirmed, as previously established by Erim et al. (8), that somatic complaints among Turkish individuals often express underlying psychological problems. Migration-related stressors (MRS) can further amplify this tendency. In our sample of Turkish patients, MRS plays a central role in the development of psychological disorders, particularly in depressive illnesses and tendencies toward somatization. To support this, Bengi-Arslan et al. (6) found that somatic symptoms such as “tightness” were prevalent among Turkish immigrants and often indicative of underlying psychological distress. These findings highlight the need for comprehensive assessment and culturally sensitive approaches in the treatment of Turkish migrants. Therefore, it is essential to develop a contextualized bio-psycho-social model of illness that considers cultural specificities in treating patients with Turkish background. In addition to assessing individual symptoms, targeted inquiry into MRS and their integration into treatment planning should be prioritized. MRS can cause or exacerbate diseases, which is why a targeted approach to dealing with these stress factors and reducing the resulting burdens is crucial to improving the mental health of Turkish patients.
When compared to previous studies, our findings show both similarities and differences. The high prevalence of language barriers (91.7%) is in line with earlier research demonstrating that linguistic difficulties are among the most consistent predictors of poor mental health outcomes and reduced treatment satisfaction among migrants. A systematic review published by Pandey et al. (45) found that limited proficiency in the host country’s language significantly hinders immigrants’ access to healthcare services. Language barriers have consistently been identified as obstacles to seeking, accessing, and utilizing mental health services. Research in the United States indicates that immigrants from regions such as Asia, Latin America, and Africa use mental health services at lower rates compared to non-immigrants, despite having similar or greater needs. Structural barriers, including language difficulties, contribute to this underutilization (46). The multi-level barriers migrants face in accessing mental health services emphasize that language barriers not only impede service utilization but also exacerbate mental health issues due to increased stress and social isolation (47).
Likewise, the high frequency of social isolation (63%) and the expressed wish to return to the home country (78%) are consistent with evidence that disrupted social networks and ambiguous belonging are central contributors to acculturative stress. These findings align with broader evidence: among Sudanese voluntary migrants in the United Arab Emirates, homesickness was significantly linked to psychological distress, depressive and anxiety symptoms - especially among women, the unemployed, and unmarried individuals, whereas longer residence and higher age mitigated these effects (48). Furthermore, first-generation migrants in the U.S. report lower social support and poorer health, and, unlike non-migrants, do not reap health benefits from social networks. This highlights how social isolation can profoundly impact migrant well-being (49). Together, these results reinforce that migration is not only a life-changing decision but a deeply personal and emotional process that can challenge identity, belonging, and mental health.
The dose-response relationship between stressors and depression observed in our study has also been described in other migrant groups. Turkish-speaking migrants who reported greater difficulties adapting to German society, alongside experiences of discrimination and unmet expectations, were more likely to suffer from depressive disorders. Acculturation stress refers to the psychological impact of navigating between two cultures, balancing the preservation of one’s cultural identity with the requirements of adapting to a new cultural environment. This process can lead to feelings of alienation, cultural conflict, and identity confusion, which can subsequently contribute to mental health issues.
The findings are consistent with broader research on acculturation stress, which has shown that migrants facing significant barriers to integration - such as language difficulties, unemployment, and social exclusion - are at a higher risk of developing mental health problems (11, 50–52). Moreover, the study emphasizes the importance of addressing both external stressors (e.g., discrimination, unemployment) and internal conflicts (e.g., identity struggles, unmet expectations) that migrants face during acculturation.
At the same time, some caution is warranted in interpreting generational aspects. The vast majority of participants in our study (over 93%) belonged to the first generation of Turkish migrants, which limits the ability to draw conclusions about the experiences of the second generation. First-generation migrants generally exhibit a higher tendency toward somatization, often linked to cultural, linguistic, and systemic barriers in the host country. On the contrary, second-generation migrants typically benefit from better integration, greater proficiency in the host country language, and a more open attitude towards mental health issues; however, cultural influences and intergenerational conflicts may still affect psychological well-being (15). Due to the small number of second-generation participants in our sample, no subgroup analyses were conducted. Future research should specifically address this issue in more balanced samples.
The study findings have significant implications for the treatment and support of Turkish-speaking migrants in Germany. Given the strong correlation between migration-related stressors and mental health symptoms, it is essential to develop targeted interventions that address both the psychological and practical challenges faced by this population. Healthcare providers should be trained to recognize the cultural factors influencing somatization and to develop culturally sensitive approaches to mental health care. This may include integrating traditional beliefs and practices into therapeutic interventions. Language support is also a key intervention area. The study emphasizes the need for accessible healthcare services in the native language of migrants to ensure better communication between patients and providers. This could involve increasing the availability of Turkish-speaking healthcare professionals or providing interpreter services in healthcare settings. Addressing language barriers will improve mental health outcomes and increase trust and engagement with the healthcare system.
In addition, the emotional and social challenges of migration, such as family separation, loneliness, and discrimination, can have significant impacts on mental health. These effects can be mitigated through social support networks and community integration programs that foster connections among migrants with shared cultural backgrounds and promote social inclusion and a sense of belonging. Consistent with this, Kim et al. (53) found that social support significantly moderated the impact of acculturative stress on depression, highlighting the protective role of supportive networks in alleviating migration-related psychological stress.
In addition to migration-related stressors, it is equally important to consider resilience factors in the context of migration. The current body of research on this topic remains limited. A qualitative data analysis by Walther et al. (54) showed that participants described resilience either as a personal trait or as a lasting inner attitude. Furthermore, voluntary engagement, employment, and activism were experienced as promoting resilience. Five additional themes emerged as resilience-enhancing factors: social support; the perception of migration as an opportunity, both in general and specifically for personal development, the experience of parenthood, and being young. In addition, future orientation, hope, religiosity or spirituality, caring for others, and the creation of new opportunities were also found to support the development of resilience among migrants (27). Our findings suggest that migration-related stressors play a central role in the manifestation of both depressive symptoms and somatization among Turkish patients in psychiatric care. If these stressors are not systematically considered during diagnostic and therapeutic processes, there is a risk that treatment remains insufficient by focusing only on symptom relief without addressing underlying contributing factors. This may partly explain why standard treatment approaches often show limited effectiveness in migrant populations, as they fail to integrate the social, cultural, and migration-specific dimensions that shape patients’ symptomatology. Consequently, a more comprehensive clinical perspective that acknowledges migration-related stress is crucial for improving both diagnostic accuracy and treatment outcomes.
Limitations
Several limitations must be acknowledged. First, the relatively small sample size (60 participants) restricts the generalizability of the results. While the study offers a snapshot of the mental health challenges faced by Turkish-speaking migrants, a larger and more diverse sample would be necessary to validate these findings across different migrant groups. Additionally, the study’s cross-sectional design does not facilitate causal inferences. Longitudinal studies would be more effective in determining whether migration stressors directly lead to increased rates of depression and somatization over time. Finally, while the study mainly focuses on first-generation migrants, the experiences of second-generation migrants may vary, and future research should investigate intergenerational differences in mental health outcomes.
Conclusion
Taken together, our findings demonstrate the high prevalence of migration-related stressors, particularly language barriers, social isolation, and disrupted family structures, among migrants treated in a psychiatric hospital. Participants showed elevated levels of both depressive symptoms and somatization, with a strong dose–response relationship between the number of stressors and depression, as well as a significant association between migration-related stressors and somatization. These results underscore the clinical importance of considering migration-related stress in psychiatric assessment and treatment, in order to avoid insufficient care that overlooks key factors in the development of depression and somatization among Turkish patients.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Medical Faculty at the University of Giessen. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BH: Conceptualization, Project administration, Supervision, Writing – review & editing, Writing – original draft. EH: Validation, Writing – review & editing. TT: Validation, Writing – review & editing. YE: Writing – original draft, Investigation. MS: Methodology, Writing – original draft, Formal analysis, Visualization, Conceptualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Han P. Soziologie der Migration: Erklärungsmodelle, Fakten, politische Konsequenzen, Perspektiven. Stuttgart: Lucius & Lucius (2000).
2. Riecken A, Genkova P, and Sanabria AM eds. Migration, Akkulturation und Integration: Warum sollten wir uns mit Erfolg beschäftigen? In: Handbuch migration und erfolg. Springer, Wiesbaden. p. 3–30.
3. Sauer M and Brinkmann HU eds. Einführung: integration in deutschland. In: Einwanderungsgesellschaft deutschland. Springer, Wiesbaden. p. 1–22.
4. Directorate-General for Migration and Home Affairs. Integration progress and challenges and record naturalisation numbers. Germany: DG for Migration and Home Affairs (2024). Available online at: https://home-affairs.ec.europa.eu/news/Germany-integration-progress-and-challenges-and-record-naturalisation-numbers-2024-12-10_en.
5. Cindik ED. Migration, psychische Gesundheit und transkulturelle Psychiatrie. Heinrich Böll Foundation: Migration & Gesundheit Dossier (2009) p. 62–8.
6. Bengi-Arslan L, Verhulst FC, and Crijnen AAM. Prevalence and determinants of minor psychiatric disorders in Turkish immigrants living in The Netherlands. Soc Psychiatry Psychiatr Epidemiol. (2002) 37:118–24. doi: 10.1007/s001270200003
7. Morawa E and Erim Y. Acculturation and depressive symptoms among Turkish immigrants in Germany. Int J Environ Res Public Health. (2014) 11:9503–21. doi: 10.3390/ijerph110909503
8. Erim Y, Morawa E, Foto Ozdemir D, and Senf W. Prevalence, comorbidity and severity of psychosomatic disorders in outpatients with Turkish migration background. Psychother Psychosom Med Psychol. (2011) 61:472–80. doi: 10.1055/s-0031-1291274
9. Wolf S, Hahn E, Dettling M, Nguyen MH, Wingenfeld K, Stingl M, et al. Migration-related stressors and their effect on the severity level and symptom pattern of depression among Vietnamese in Germany. Depress Res Treat. (2017) 2017:8930432. doi: 10.1155/2017/8930432
10. Faltermaier T. Gesundheitspsychologie. In: Grundriss der psychologie. Kohlhammer, Stuttgart (2005).
11. Berry JW. Immigration, acculturation and adaptation. Appl Psychol. (1997) 46:5–68. doi: 10.1111/j.1464-0597.1997.tb01087.x
12. Wolf S, Hahn E, Wingenfeld K, Nguyen MH, von Poser A, Nguyen TH, et al. Mental health determinants among a psychiatric outpatient sample of Vietnamese migrants in Germany. Front Psychiatry. (2020) 11:580103. doi: 10.3389/fpsyt.2020.580103
13. Della Rocca B, Di Vincenzo M, Giallanella D, Gaggiano C, Martinelli F, Ricci F, et al. Acculturation stress and mental health outcomes in a sample of migrant inpatients: Findings from a naturalistic study. Int J Soc Psychiatry. (2025) 71:328–37. doi: 10.1177/00207640241291506
14. Choy B, Arunachalam K SG, Taylor M, and Lee A. Systematic review: Acculturation strategies and their impact on the mental health of migrant populations. Public Health Pract (Oxf). (2020) 2:100069. doi: 10.1016/j.puhip.2020.100069
15. Dingoyan D, Schulz H, Kluge U, Penka S, Vardar A, von Wolff A, et al. Lifetime prevalence of mental disorders among first and second generation individuals with Turkish migration backgrounds in Germany. BMC Psychiatry. (2017) 17:177. doi: 10.1186/s12888-017-1333-z
16. Foo SQ, Tam WW, Ho CS, Tran BX, Nguyen LH, McIntyre RS, et al. Prevalence of depression among migrants: a systematic review and meta-analysis. Int J Environ Res Public Health. (2018) 15:1986. doi: 10.3390/ijerph15091986
17. Herold R, Lieb M, Borho A, Voss A, Unverzagt S, Morarwa E, et al. Working conditions and mental health of migrants and refugees in Europe considering cultural origin – a systematic review. BMC Public Health. (2024) 24:662. doi: 10.1186/s12889-024-18096-7
18. Schührer S. Türkeistämmige Personen in Deutschland: Erkenntnisse aus der Repräsentativuntersuchung. In: Ausgewählte migrantengruppen in deutschland 2015” (RAM). Bundesamt für Migration und Flüchtlinge, Nürnberg (2018). Available online at: https://www.bamf.de/SharedDocs/Anlagen/DE/Forschung/WorkingPapers/wp81-tuerkeistaemmige-in-deutschland.pdf.
19. Sürig I and Wilmes M. Die Integration der zweiten Generation in Deutschland: Ergebnisse der TIES-Studie zur türkischen und jugoslawischen Einwanderung. IMIS-Beiträge. (2011) 39.
20. Montemitro C, D’Andrea G, Cesa F, Martinotti G, Pettorruso M, Di Giannantonio M, et al. Language proficiency and mental disorders among migrants: A systematic review. Eur Psychiatry. (2021) 64:e49. doi: 10.1192/j.eurpsy.2021.2224
21. Miteva D, Georgiadis F, McBroom L, Noboa V, Quednow BB, Seifritz E, et al. Impact of language proficiency on mental health service use, treatment and outcomes: “Lost in Translation. Compr Psychiatry. (2022) 114:152299. doi: 10.1016/j.comppsych.2022.152299
22. Carta MG, Bernal M, Hardoy MC, and Haro-Abad JM. Migration and mental health in Europe (the state of the mental health in Europe working group: Appendix 1). Clin Pract Epidemiol Ment Health. (2005) 1:13. doi: 10.1186/1745-0179-1-13
23. Riecken A, Wiedl KH, and Weig W. Die Bedeutung der Deutschkenntnisse für die Entwicklung und Behandlung von psychiatrischen Erkrankungen. Psychiatr Prax. (2001) 28:275–7. doi: 10.1055/s-2001-16878
24. Kirmayer LJ, Narasiah L, Munoz M, Rashid M, Ryder AG, Guzder J, et al. Common mental health problems in immigrants and refugees: General approach in primary care. CMAJ. (2011) 183:E959–67. doi: 10.1503/cmaj.090292
25. Krystallidou D, Temizöz Ö, Wang F, de Looper M, Di Maria E, Gattiglia N, et al. Communication in refugee and migrant mental healthcare: A systematic rapid review on the needs, barriers and strategies of seekers and providers of mental health services. Health Policy. (2024) 139:104949. doi: 10.1016/j.healthpol.2023.104949
26. Blume M, Bartig S, Wollgast L, Koschollek C, Kajikhina K, Bug M, et al. Determinants of mental health inequalities among people with selected citizenships in Germany. Int J Public Health. (2024) 69:1607267. doi: 10.3389/ijph.2024.1607267
27. Lindert J, Ehrenstein OS, Priebe S, Mielck A, and Brähler E. Depression and anxiety in labor migrants and refugees: A systematic review and meta-analysis. Soc Sci Med. (2009) 69:246–57. doi: 10.1016/j.socscimed.2009.05.003
28. Vonneilich N, Becher H, Bohn B, Brandes B, Castell S, Deckert A, et al. Associations of migration, socioeconomic position and social relations with depressive symptoms – Analyses of the German National Cohort baseline data. Int J Public Health. (2023) 68:1606097. doi: 10.3389/ijph.2023.1606097
29. Ünlü Ince B, Fassaert T, de Wit MAS, Cuijpers P, Smit J, Ruwaard J, et al. The relationship between acculturation strategies and depressive and anxiety disorders in Turkish migrants in the Netherlands. BMC Psychiatry. (2014) 14:252. doi: 10.1186/s12888-014-0252-5
30. van der Wurff FB, Beekman AT, Dijkshoorn H, Spijker JA, Smits CH, Stek ML, et al. Prevalence and risk factors for depression in elderly Turkish and Moroccan migrants in the Netherlands. J Affect Disord. (2004) 83:33–41. doi: 10.1016/j.jad.2004.04.009
31. Lujic C. Illness- and therapy-relevant characteristics of Turkish immigrants suffering from health disorders: Suggestions for improvement of care. (Germany: Inaugural dissertation, Justus Liebig University Giessen) (2008).
32. Ostermann B. Wer versteht mich? Der Krankheitsbegriff zwischen Volksmedizin und High Tech. In: Zur Benachteiligung von AusländerInnen in deutschen Arztpraxen. Verlag für Interkulturelle Kommunikation, Frankfurt am Main (1990).
33. Becker SA, Wunderer E, and Schultz-Gambard J. Muslimische Patienten: Ein Leitfaden zur interkulturellen Verständigung in Krankenhaus und Praxis. Germering/München: Zuckschwerdt (1998).
34. Assion HJ, Dana I, and Heinemann F. Volksmedizinische Praktiken bei psychiatrischen Patienten türkischer Herkunft in Deutschland. Fortschr Neurol Psychiatr. (1999) 67:12–20. doi: 10.1055/s-2007-993733
35. Zielke-Nadkarni A. Gesundheits- und krankheitskonzepte. In: Domenig D, editor. Professionelle Transkulturelle Pflege: Handbuch für Lehre und Praxis in Pflege und Geburtshilfe. Hans Huber, Bern (2001). p. 123–36.
36. Schäfer-Böker G. Krankheitskonzepte ausländischer familien. In: Buchkremer H and Emmerich M, editors. Ausländerkinder: Sonder- und sozialpädagogische Fragestellungen. EBV, Hamburg (1987). p. 88–100.
37. Brand T, Samkange-Zeeb F, Ellert U, Keil T, Krist L, Dragano N, et al. Acculturation and health-related quality of life: Results from the German National Cohort migrant feasibility study. Int J Public Health. (2017) 62:521–9. doi: 10.1007/s00038-017-0957-6
38. Beutel ME, Jünger C, Klein EM, Wild P, Lackner KJ, Blettner M, et al. Depression, anxiety and suicidal ideation among 1st and 2nd generation migrants – results from the Gutenberg Health Study. BMC Psychiatry. (2016) 16:288. doi: 10.1186/s12888-016-0995-2
39. Beck AT, Ward CH, Mendelson M, Mock J, and Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. (1961) 4:561–71. doi: 10.1001/archpsyc.1961.01710120031004
40. Hisli N. Beck Depresyon Envanterinin üniversite öğrencileri için geçerliği, güvenirliği. Psikoloji Dergisi. (1989) 7:3–13.
41. Rief W, Hiller W, and Heuser J. SOMS – Das Screening für Somatoforme Störungen: Manual zum Fragebogen. Bern: Huber (1997).
42. Sass H, Wittchen HU, and Zaudig M. Diagnostisches und statistisches Manual psychischer Störungen – DSM-IV. Göttingen: Hogrefe (1996). Deutsche Bearbeitung.
43. Dilling H, Mombour W, and Schmidt MH. Internationale klassifikation psychischer störungen: ICD-10. In: Kapitel V, editor. (F) – klinisch-diagnostische leitlinien, 10th ed. Hogrefe, Bern (2015).
44. Erim Y, Beckmann M, Tagay S, Aygün S, Gencoglu PG, and Senf W. Validierung der türkischen Version des Screenings für Somatoforme Störungen (SOMS). Diagnostica. (2012) 58:194–210. doi: 10.1026/0012-1924/a000075
45. Pandey M, Maina RG, Amoyaw J, Li Y, Kamrul R, Michaels CR, et al. Impacts of English language proficiency on healthcare access, use, and outcomes among immigrants: A qualitative study. BMC Health Serv Res. (2021) 21:741. doi: 10.1186/s12913-021-06750-4
46. Derr AS. Mental health service use among immigrants in the United States: A systematic review. Psychiatr Serv. (2016) 67:265–74. doi: 10.1176/appi.ps.201500004
47. Forray AI, Oltean O, Hanft-Robert S, Madzamba R, Liem A, Schouten B, et al. Uncovering multi-level mental healthcare barriers for migrants: A qualitative analysis across China, Germany, Netherlands, Romania, and South Africa. BMC Public Health. (2024) 24:1593. doi: 10.1186/s12889-024-19046-z
48. Hamid AARM. Psychological distress and homesickness among Sudanese migrants in the United Arab Emirates. Front Psychol. (2022) 12:710115. doi: 10.3389/fpsyg.2021.710115
49. Bilecen B and Vacca R. The isolation paradox: A comparative study of social support and health across migrant generations in the U.S. Soc Sci Med. (2021) 283:114204. doi: 10.1016/j.socscimed.2021.114204
50. Schwartz SJ, Unger JB, Zamboanga BL, and Szapocznik J. Rethinking the concept of acculturation: Implications for theory and research. Am Psychol. (2010) 65:237–51. doi: 10.1037/a0019330
51. Lueck K and Wilson M. Acculturative stress in Asian immigrants: The impact of social and linguistic factors. Int J Intercult Relat. (2010) 34:47–57. doi: 10.1016/j.ijintrel.2009.10.004
52. Bhugra D. Migration and mental health. Acta Psychiatr Scand. (2004) 109:243–58. doi: 10.1046/j.0001-690x.2003.00246.x
53. Kim Y, Lee H, and Lee M. Social support for acculturative stress, job stress, and perceived discrimination among migrant workers moderates COVID-19 pandemic depression. Int J Public Health. (2022) 67:1604643. doi: 10.3389/ijph.2022.1604643
Keywords: migration-related stressors, Turkish migrants, acculturation, cross-cultural psychiatry, depression, somatization
Citation: Hanewald B, Hahn E, Ta TTM, Elguen Y and Stingl M (2025) Depression and somatization in Turkish migrants in Germany: the role of migration-related stressors. Front. Psychiatry 16:1642491. doi: 10.3389/fpsyt.2025.1642491
Received: 06 June 2025; Accepted: 25 September 2025;
Published: 14 October 2025.
Edited by:
Eric Comte, Université de Genève, SwitzerlandReviewed by:
Bartolomei Javier, Universitary Hospital of Geneva, SwitzerlandBedia Tarsuslu, Ordu University, Türkiye
Copyright © 2025 Hanewald, Hahn, Ta, Elguen and Stingl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bernd Hanewald, YmVybmQuaGFuZXdhbGRAcHN5Y2hpYXQubWVkLnVuaS1naWVzc2VuLmRl
 Bernd Hanewald
Bernd Hanewald Eric Hahn
Eric Hahn Tam Thi Minh Ta
Tam Thi Minh Ta Yasemin Elguen1
Yasemin Elguen1 Markus Stingl
Markus Stingl