- 1Department of Clinical and Experimental Medicine, Section of Psychiatry, University of Pisa, Pisa, Italy
- 2Department of Biomedical and Dental Sciences and Morphofunctional Imaging, University of Messina, Messina, Italy
- 3Department of Psychiatry, University of Campania “Luigi Vanvitelli”, Naples, Italy
Background: Borderline Personality Disorder (BPD) frequently co-occurs with both eating disorders (EDs) and elevated autistic traits, particularly among women. Social camouflaging—a set of strategies used to mask neurodivergent behaviors—has been extensively studied in autism spectrum conditions but remains underexplored in BPD populations. Given emerging evidence linking camouflaging behaviors to disordered eating, this study aimed to investigate the relationship between social camouflaging and eating disorder symptomatology in women with BPD.
Methods: A total of 110 female participants (64 with BPD, 46 healthy controls) were assessed using the Camouflaging Autistic Traits Questionnaire (CAT-Q), the Eating Disorder Inventory-2 (EDI-2), and the Adult Autism Subthreshold Spectrum (AdAS Spectrum).
Results: Women with BPD scored significantly higher on all domains of the CAT-Q, AdAS Spectrum, and EDI-2. Significant correlations emerged between CAT-Q and EDI-2 scores. CAT-Q total score and CAT-Q compensation domain significantly predicted EDI-2 total score.
Conclusion: Social camouflaging is significantly elevated in women with BPD and is closely associated with disordered eating symptoms. Findings highlight camouflaging as a potential transdiagnostic mechanism linking autistic traits and ED symptomatology in BPD populations, with implications for diagnostic clarity and personalized treatment strategies.
1 Introduction
Borderline Personality Disorder (BPD) is a complex and multifaceted mental health condition characterized by pervasive instability in mood, self-image, interpersonal relationships, and impulse control (1). Individuals with BPD frequently struggle with emotional dysregulation, impulsivity and self-harming behaviors, identity disturbances, and profound fear of abandonment (1). BPD is estimated to affect between 0.7% and 2.7% of the general population, with markedly higher rates observed in clinical settings (up to 22% among psychiatric inpatients) (2). The disorder is often associated with profound functional impairments and elevated rates of comorbid psychiatric conditions (3). Although BPD is diagnosed more frequently in women, with a clinical gender ratio of roughly 3:1, this discrepancy may be influenced by gendered diagnostic practices and sociocultural biases in both symptom expression and referral patterns (1, 3). Recent evidences are suggesting how the core symptoms of BPD are often rooted in a history of trauma. Experiences such as abandonment, neglect, and various forms of abuse—particularly physical and sexual—are common among those affected and may contribute significantly to the disorder’s development and clinical course (4–6). Moreover, BPD often coexists with other psychiatric disorders, among which eating disorders are especially prevalent. Conditions such as anorexia nervosa (AN), bulimia nervosa (BN), and binge-eating disorder (BED) are not only commonly comorbid with BPD but also disproportionately affect women, underscoring the complex interplay of gender, trauma, and psychopathology in this population (7, 8).
Recent research has increasingly highlighted the significant overlap, especially in female populations, between BPD and features typically associated with Autism Spectrum Disorder (ASD), a neurodevelopmental disorder characterized by deficits in social communication and the presence of restricted interests and repetitive behaviors (1, 9–12). This overlap includes traits such as social communication difficulties, heightened emotional sensitivity, and rigid thinking patterns (9, 10). Indeed, individuals with either condition may exhibit intense yet unstable interpersonal relationships, difficulties in both verbal and non-verbal communication, a tendency to act impulsively rather than verbalize emotions, impairments in Theory of Mind, emotional dysregulation, and engagement in self-harming behaviors (13–17). However, despite these similarities, important distinctions remain between the two.
One phenomenon that may bridge these conditions is social camouflaging—a set of compensatory strategies employed by individuals, often women, to mask neurodivergent traits and conform to neurotypical social expectations. Indeed, autistic individuals who do not present with intellectual impairments often demonstrate a greater awareness of their social communication challenges (18). In particular, this feature seems to be particularly present among female patients: some authors even hypothesized that the higher tendency to adopt social camouflaging strategies may contribute to an underdiagnosis of ASD among females (8, 19–22). This heightened self-awareness may drive them to consciously modify their behavior in order to align with the social norms and expectations of neurotypical individuals (14, 16). Within this context, the concept of social camouflaging has emerged as a significant area of interest in both clinical practice and research (19, 20, 23–25). Social camouflaging refers to a set of adaptive strategies aimed at concealing social difficulties and presenting oneself in a socially acceptable manner by subjects in the autism spectrum. These strategies can involve suppressing behaviors perceived as atypical or deliberately performing actions that are considered more socially normative in an effort to appear socially competent (19). Such behaviors are often acquired through observation of peers or intentional learning from various media sources. Examples include maintaining eye contact, mimicking facial expressions and body language, or using rehearsed phrases and scripted dialogue during interactions (19, 20). Notably, camouflaging can become increasingly sophisticated over time, especially when initiated in early childhood. While some aspects of these strategies may develop unconsciously, prolonged and consistent use may eventually contribute to the creation of a socially constructed persona, often referred to as a “mask,” which the individual adopts in public or interpersonal contexts (24). However, while social camouflaging has been well-documented in ASD, studies in different samples, such as university students, seem to point out a continuous distribution of camouflaging from the general to the clinical population, following the continuous distribution of autistic traits (25). However, its presence and clinical significance in BPD remain underexplored, despite the presence of high autistic features in BPD subjects according to the scientific literature (13).
In addition, as reported above, BPD patients frequently exhibit comorbid symptoms of eating disorders, further complicating diagnostic clarity and treatment planning. In fact, a growing body of research has shown that individuals with BPD frequently engage in disordered eating behaviors, even in the absence of a formal eating disorder diagnosis (26). These behaviors commonly include binge eating, restrictive dieting, meal skipping, and self-induced vomiting. Vice versa, a recent systematic review identified BPD as the most prevalent comorbid personality disorder among individuals exhibiting pathological eating behaviors (27). On the other hand, numerous investigations have documented a significant overlap between autism spectrum and eating disorders, with elevated levels of autistic traits consistently observed in individuals with AN and BN. While it could be hypothesized that autistic traits may at least in part constitute a common ground for different psychopathological manifestations such as BPD and eating disorders, recent studies also highlighted a possible association between camouflaging behaviors and eating disorder symptoms in ASD subjects (28–34). Some scholars have also proposed that specific presentations of BPD and eating disorders—particularly among females—may represent an alternative manifestation of the autism spectrum, underscoring the importance of considering neurodevelopmental dimensions in these clinical profiles (8).
The present study aims to fill a critical gap in the literature by examining the presence of social camouflaging among women diagnosed with BPD and its psychopathological correlates, specifically focusing on eating disorder symptomatology.
2 Materials and methods
2.1 Study sample and procedures
The study included a sample of 64 in and out patients diagnosed with BPD, followed at the Psychiatric clinic of the Azienda Ospedaliero-Universitaria of Pisa, as well as 46 healthy controls (HCs) recruited from medical and paramedical staff on a voluntary basis. Diagnosis were made through clinical assessment by trained psychiatrists. Patients recruited had not received a diagnosis of autism in childhood. Participants were excluded if they had intellectual disabilities, poor cooperation skills, were under 18 years of age, had language or intellectual impairments that could hinder the completion of assessments, or presented with ongoing psychotic symptoms. The study adhered to the principles outlined in the Declaration of Helsinki, and all recruitment and evaluation procedures were approved by the Ethics Committee of the Azienda Ospedaliero-Universitaria of Pisa (protocol code: 23910_Dell’osso; date of approval: 20th April 2023). Informed consent was obtained from all participants after a detailed explanation of the study, with an opportunity to ask questions. No financial compensation was provided for participation.
All participants underwent evaluation using the Adult Autism Subthreshold Spectrum (AdAS Spectrum), the Eating Disorder Inventory—2 (EDI-2) and the Camouflaging Autistic Traits Questionnaire (CAT-Q).
All questionnaires were administered in a quiet outpatient clinical setting at the Department of Psychiatry, University of Pisa. Participants completed the instruments in paper-and-pencil format in a dedicated room free from external distractions. The assessments were carried out during a single session, lasting approximately 60–90 minutes. A trained clinical psychiatry resident was present to provide standardized instructions, ensure comprehension of the items, and supervise the completion process. Participants were encouraged to ask clarification questions if needed, but no guidance on item content or interpretation was provided. Breaks were allowed to prevent fatigue, particularly for BPD patients who might experience distress when completing long questionnaires.
2.2 Measures
2.2.1 The CAT-Q
The CAT-Q is a self-report instrument designed to evaluate camouflaging behaviors related to the autism spectrum in both clinical and non-clinical populations. It consists of 25 items, categorized into three domains: Assimilation, Masking, and Compensation, each assessed on a seven-point Likert scale. The Italian version of the questionnaire demonstrated excellent internal consistency, with a Cronbach’s alpha of 0.904. Moreover, it exhibited strong test-retest reliability and convergent validity when compared to other established autism assessment tools (35, 36).
2.2.2 The EDI-2
The EDI-2 is a self-report tool designed to assess eating disorder symptoms and associated psychological traits. It comprises 91 items across 11 domains: Drive for Thinness, Bulimia, Body Dissatisfaction, Ineffectiveness, Perfectionism, Interpersonal Distrust, Interoceptive Awareness, Maturity Fears, Asceticism, and Impulsivity. Responses are given on a 6-point Likert scale. This broad range of sub-scales allows for a comprehensive evaluation of both behavioral and psychological aspects of eating disorders (37).
2.2.3 The AdAS spectrum
The AdAS Spectrum is a 160-item self-report questionnaire designed to assess a wide range of autism-related symptoms in individuals without cognitive or language impairments. It covers seven domains: Childhood and adolescence, Verbal and Non-verbal communication, Empathy, a Rigidity and adherence to routine, Restricted interests and rumination, and Hyper- or Hyporeactivity to sensory stimuli. The validation study demonstrated strong internal consistency, excellent test-retest reliability, and convergent validity with other dimensional autism spectrum measures (38).
2.3 Statistical analysis
Cronbach’s Alpha were calculated for all psychometric questionnaires. Student t-test was used for comparing mean age. Mann-Whitney tests were used for comparing CAT-Q domains and total scores, as well as AdAS Spectrum and EDI-2 total scores among the two diagnostic groups.
Spearman’s correlation coefficients were then used to examine the relationships between CAT-Q and EDI-2 scores.
Afterwards, a linear regression analysis was performed using EDI-2 total score as dependent variable and CAT-Q total score and diagnostic group (BPD vs HC) as independent variables in order to investigate the eventual role of social camouflaging as a statistical predictor of greater symptoms of eating disorders. A second linear regression analysis was then performed with the same dependent variable and CAT-Q domain scores and diagnostic group as independent variables.
All statistical analyses were performed with SPSS version 26.0.
3 Results
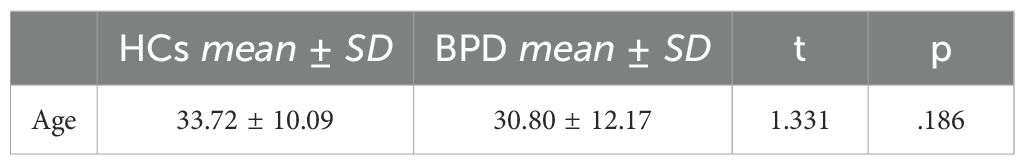
The total sample was made of 110 female subjects of which 64 with a clinical diagnosis of BPD (mean age: 30.8 ± 12.17 years) and 46 healthy controls (mean age: 33.72 ± 10.09). The groups did not significantly differ for age. All questionnaires reported excellent Cronbach’s alpha values in the sample (Cronbach’s alpha for AdAS Spectrum:.978; for CAT-Q:.963; for EDI-2:.957) (see Table 1).
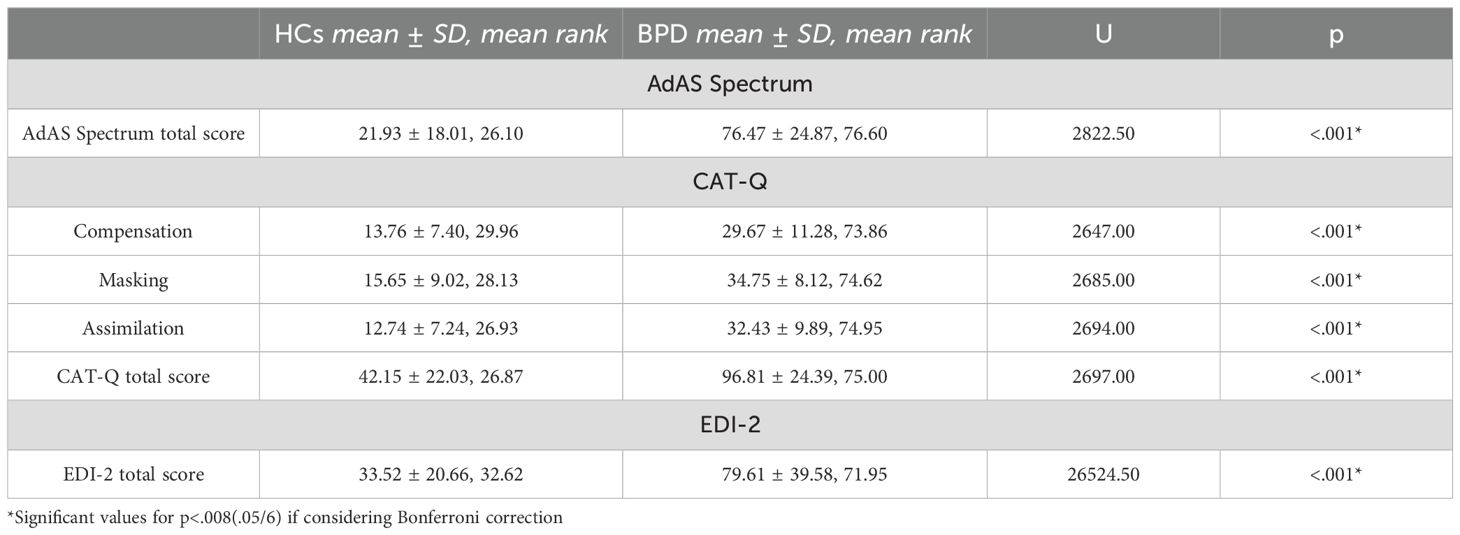
The results of the Mann-Whitney tests revealed that individuals with BPD scored significantly higher across all CAT-Q domains, as well as in the total CAT-Q score. Additionally, they reported significantly higher scores on the AdAS Spectrum and EDI-2 total scores (see Table 2).
The results of the correlation analysis showed a pattern of medium to strong correlations between EDI-2 and CAT-Q scores. Specifically, while CAT-Q and EDI-2 total scores were significantly and positively correlated, significant positive correlations were also found between almost all CAT-Q and EDI-2 domains, with the exception of EDI-2 Interpersonal distrust and Social insecurity domains, which were not significantly correlated with CAT-Q scores (see Table 3).
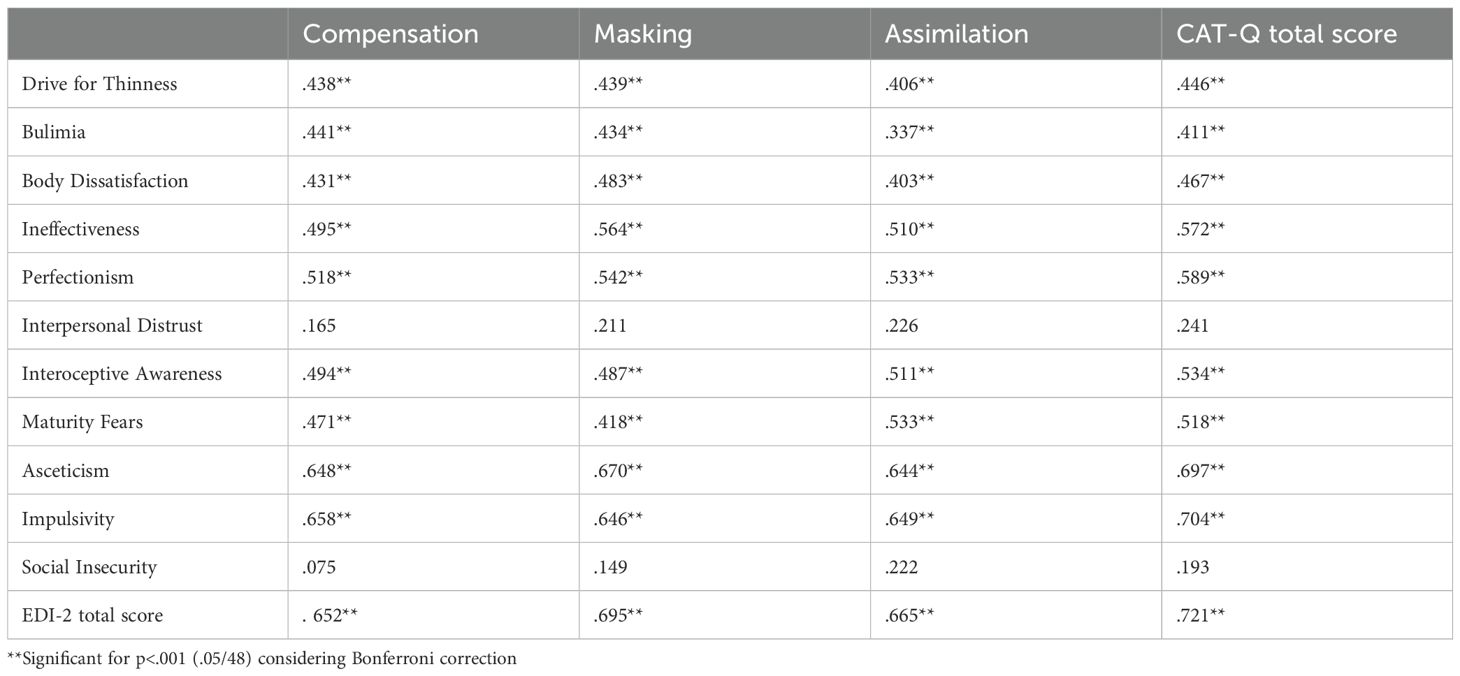
Table 3. Spearman’s correlations coefficients among AdAS Spectrum domains and total score and CAT-Q domains and total score in the total sample.
Results from the linear regression analysis performed using EDI-2 total score as dependent variable and CAT-Q total score and diagnostic group as independent variables showed that the CAT-Q total score, but not diagnostic group, was significant positive predictors of greater eating disorder symptoms (see Table 4).
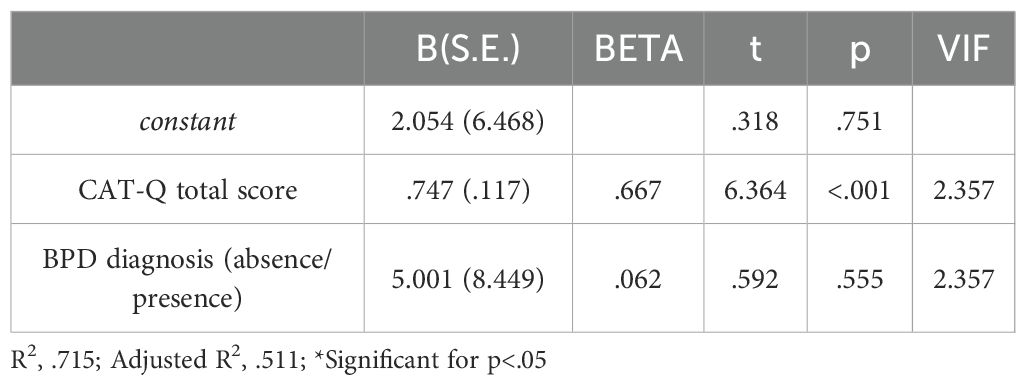
Table 4. Linear regression analysis with EDI-2 total score as dependent variable and CAT-Q total score and diagnostic group (BPD vs HC) as independent variables, carried in the whole sample.
Results from a further linear regression analysis performed using EDI-2 total score as dependent variable and CAT-Q domains and diagnostic group as independent variables showed that CAT-Q Compensation domain was a significant positive predictor of greater eating disorder symptoms (see Table 5).
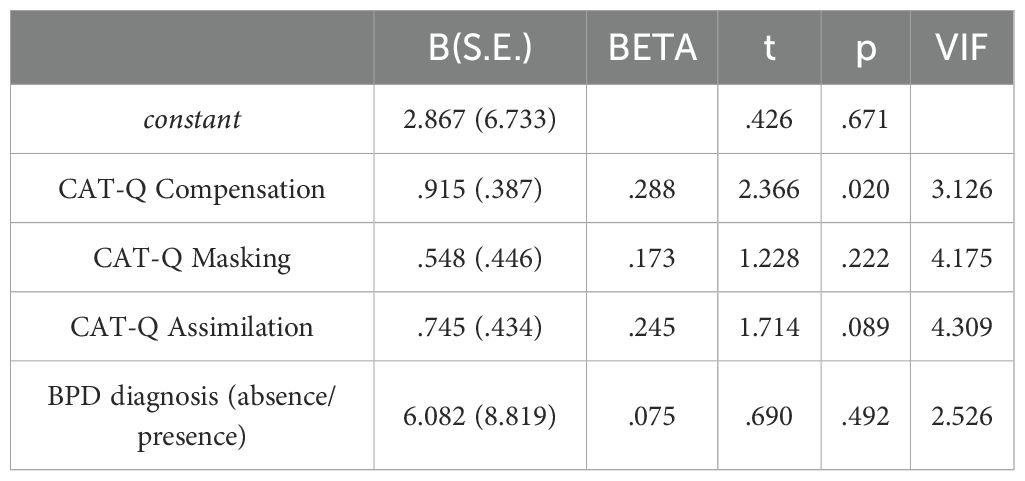
Table 5. Linear regression analysis with EDI-2 total score as dependent variable and CAT-Q domain scores and diagnostic group (BPD vs HC) as independent variables, carried in the whole sample.
4 Discussion
The main objective of our study was to investigate the presence and correlates of camouflaging behaviors in a sample of patients with BPD, specifically focusing on eating disorder symptoms. As expected, BPD subjects scored significantly higher in the AdAS Spectrum, EDI-2 and CAT-Q questionnaires. The strong link between BPD and eating disorders is well-recognized (39). Numerous studies have shown that individuals with BPD often engage in disordered eating behaviors, such as binge eating, dieting, meal skipping, and vomiting, regardless of whether they have a formal eating disorder diagnosis (26). Additionally, some researchers have highlighted a direct relationship between these two conditions, suggesting that shared transdiagnostic factors, such as socio-cultural influences, common underlying causes, and overlapping symptoms —like emotional regulation difficulties, interpersonal struggles, self-concept issues, and impulsivity— play a role in both disorders (40). Also, the evidence of higher autistic traits in BPD patients is consistent with the current literature highlighting not only a greater presence of autistic symptomatology in patients with BPD, but also a partial clinical overlap between these two conditions (9–12, 41). Indeed, recent data have reported how BPD patients have an increased odds ratio of having an ASD diagnosis and vice versa a significant prevalence of BPD – up to 15% – in autistic subjects, supporting the hypothesis that disorders such as BPD can mask the presence of ASD, especially in women, leading to a greater rate of misdiagnosis (8, 9, 41–43). In this regard, the concept of a “female autistic phenotype” has long been acknowledged, referring to a distinct manifestation of autism in women with respect to the traditional, male-centered models of ASD (44–46).
A key feature of this phenotype is the ability to “camouflage” social difficulties across different social situations (47). Studies consistently show that women with full-blown ASD or elevated autistic traits often exhibit higher social motivation and a greater ability to engage in typical social connections (47, 48), allowing them to develop masking strategies to conceal their neuroatypical traits and better integrate with neurotypical individuals. This documented ability to camouflage in women with high autistic traits supports our finding of a higher score BPD group in both AdAS Spectrum and CAT-Q questionnaires, aimed at investigating autistic-like camouflaging behaviors.
Moreover, EDI-2 total score was significantly correlated with all CAT-Q domains and its total score, with CAT-Q total score also being a positive predictor of higher symptoms of eating disorders, without a predictive role of the diagnostic group. These results align with previous studies indicating a link between eating disorders and camouflaging behaviors (34, 49). Specifically, research by Bradley et al. highlighted that social camouflaging, as assessed by the CAT-Q, can predict symptoms of eating disorders in population with autism spectrum (34). In particular, the study suggests that camouflaging may contribute to the development of eating disorder symptoms, serving as a coping mechanism for social pressures. An intriguing aspect of this is the pivotal role that identity plays in the onset and persistence of these disorders (1, 50). Moreover, a more recent research how in a sample of university students camouflaging behaviors seem to mediate the relationship between autistic traits and orthorexic symptoms (1). Some have argued that eating disorders may stem from identity struggles, which are also one of the core issues in BPD. In this context, an eating disorder may provide a sense of self or a community to belong to (50). In addition, it is also possible that female subjects in the autism spectrum may try to focus on socially accepted interests among girls, such as eating styles and body shape, as an attempt to mask their autism; however, they may pursue the interest with the inflexible and pervasive fashion typical of autism spectrum, enhancing the risk to develop an eating disorder (1). Our results are in line with these data, suggesting an association between camouflaging and eating disorders in different populations. These findings add to the broader body of research showing that camouflaging behaviors are strongly associated with poor mental health outcomes, including symptoms of eating disorders (20, 34, 51).
Interestingly, the EDI-2 domains of Ineffectiveness, Perfectionism, Interoceptive Awareness, Impulsivity and Ascetism were those for which the strongest correlations were reported with CAT-Q scores. Although to this date there is paucity of literature on the topic, it is plausible that Ineffectiveness, conceptualized as feelings of low self-esteem, heightened sensitivity to criticism, and a sense of inadequacy, may be linked to the use of camouflaging behaviors in order to conceal the perceived social difficulties. Moreover, using such behaviors could eventually make the subject feel as though they are living a “double” or “false” life, which may lead to a sense of inadequacy and mental or physical exhaustion. This is partly because they often view their social acceptance as dependent on their ability to mask their true selves, rather than being accepted for who they are (20, 51–54). As for ascetism, camouflaging can contribute to the development of ascetic traits when an individual feels compelled to suppress or sacrifice parts of themselves in order to conform to social norms or expectations. Since camouflaging involves hiding or downplaying one’s behaviors and emotions to fit in or avoid social judgment, constant engagement in this process may lead a person to view their emotional, social, or physical needs as something to be repressed or ignored. This can foster a form of asceticism, where the individual attempts to “purify” themselves by voluntarily sacrificing their well-being or needs to meet an external standard of perfection or social acceptability. Over time, the suppression of emotions deemed “inappropriate” may cause them to perceive their needs or desires as unnecessary or even negative. Consequently, they may begin to reject and suppress these needs, viewing self-sacrifice as a virtue that helps them gain greater control or better adapt socially (22, 24, 55).
Concerning perfectionism, it could be hypothesized that these subjects, due to their heightened sensitivity to criticism and judgment, impose unrealistic standards on themselves. As a result, they often adopt communication strategies to compensate for their perceived social shortcomings and present an image of themselves that they believe is better and more socially acceptable. However, the idealized and perfect image they strive to project is often unattainable and unsustainable, which can lead to physical and mental exhaustion over time (19, 21, 54, 55). Altered interoceptive awareness has been widely documented in BPD populations, where it has frequently been associated with alexithymia and trauma-related dissociative symptoms (56–60). This difficulty in understanding and processing bodily sensations may lead to the adoption camouflaging behaviors in order to fit in with others, without basing on self-perceived stimuli (60–63). This hypothesis is further supported by a recent study that highlighted how interoceptive deficits correlated with measures of camouflaging (63). Lastly, the link between impulsivity and camouflaging likely stems from the emotional toll and build up stress and frustration of continually using strategies to conceal social difficulties. Individuals who engage in camouflaging often become deeply focused on hiding their social struggles to fit in or meet societal expectations. This ongoing effort can lead to significant emotional strain over time (21, 22, 64). While the fear of emotional dysregulation may enhance the drive for adopting compensation strategy in order to regulate emotion and properly behave in social situations, when emotional regulation falters, this accumulated pressure may trigger intense emotional reactions or impulsive behaviors. This also aligns with previous research indicating that camouflaging can predict emotional dysregulation in autistic individuals, with emotional regulation difficulties potentially mediating the link between social camouflaging and symptoms of depression or anxiety (65, 66).
Significant correlations were also found between CAT-Q and EDI-2 Drive for thinness, Body dissatisfaction, Bulimia and Maturity Fears domains. Although there is no systematic data on this, it is conceivable that individuals who have a strong drive for thinness may use masking to hide their emotional distress, such as feelings of shame, anxiety, or insecurity about their bodies. In this vein, masking may also involve hiding real emotions related to food, body image, or self-esteem. Similarly, when individuals experience dissatisfaction with their bodies, they may become hyper-aware of how others perceive them, and the fear of being judged or criticized based on their appearance may trigger masking behaviors, in which they try to hide their real emotions or discomfort (67, 68). On the other hand, bulimia is in fact often associated with intense feelings of shame, guilt and embarrassment for eating behaviors, such as binge eating and purging behaviors (through vomiting, excessive exercise or use of laxatives), which are considered socially inappropriate and unacceptable (69). It is therefore possible that to avoid this potential judgment, individuals with bulimia adopt camouflaging behaviors, which could include lying about their eating habits. On the other hand, it is possible that the habit of camouflaging may also enhance in these patients the risk to develop bulimia symptoms by try to maladaptively employ compensative behaviors also in other contexts, such as after binge eating, thus masking and compensating for the episode of loss of control as they try to do with autism symptoms.
Intriguingly, our results did not shown a correlation between EDI-2 interpersonal distrust and social insecurity domains and the CAT-Q. It is possible that the use of camouflaging strategies, although requiring a great mental effort and identity struggles, would allow subjects to feel relatively more confident in social situations, thus reducing insecurity feelings with respect to those with similar psychopathological traits who do not adopt camouflaging strategies (22, 24, 55, 70).
Our findings also bear potential clinical implications. Although preliminary, they suggest that the assessment of social camouflaging in women with BPD may enrich clinical evaluation and treatment planning. In particular, the combined use of the CAT-Q, together with dimensional measures such as the AdAS Spectrum and the EDI-2, could represent a useful battery for identifying patients in whom camouflaging strategies contribute to diagnostic complexity and symptom severity. From a therapeutic perspective, greater clinical awareness of camouflaging may help clinicians to explore masking behaviors that exacerbate emotional dysregulation and maladaptive eating patterns. Psychoeducation about camouflaging, the integration of emotion regulation skills training (as in dialectical behavior therapy), and interventions aimed at enhancing interoceptive awareness may represent promising strategies to address these processes. Furthermore, recognizing camouflaging may reduce the risk of misdiagnosing autistic traits in BPD patients and favor more personalized treatment approaches. Nevertheless, these considerations remain exploratory, and further longitudinal and interventional studies are warranted to provide evidence-based clinical guidelines.
These findings should be considered in the context of several limitations. Firstly, the study’s cross-sectional design limits our ability to draw conclusions about cause-and-effect relationships or the temporal progression of the variables being examined. Additionally, the reliance on self-report psychometric questionnaires to assess participants may lead to either over- or under-estimation of symptoms, depending on individuals’ subjective perceptions. Moreover, the relatively small size of the sample and the choice of an all-female sample limits the generalizability of the findings, making it challenging to apply these findings to larger or more diverse populations. The relatively small sample size also prevented us from performing more in-depth within-group analyses and stratifying patients for autistic traits severity.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Azienda Ospedaliero-Universitaria of Pisa. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BC: Methodology, Conceptualization, Supervision, Writing – review & editing. BN: Investigation, Writing – original draft, Data curation, Writing – review & editing. FG: Investigation, Data curation, Writing – original draft. FP: Investigation, Data curation, Writing – original draft. CP: Writing – original draft, Data curation, Investigation. CB: Writing – original draft, Investigation, Data curation. GM: Writing – review & editing, Data curation, Formal Analysis, Methodology. SP: Conceptualization, Methodology, Supervision, Writing – review & editing. AB: Data curation, Writing – review & editing. MM: Writing – review & editing, Supervision, Methodology, Conceptualization. BD: Data curation, Writing – review & editing. AF: Writing – review & editing, Supervision, Conceptualization, Methodology. LD: Writing – review & editing, Supervision, Conceptualization, Methodology.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC, USA: American Psychiatric Press (2022). Text Revision.
2. Leichsenring F, Fonagy P, Heim N, Kernberg OF, Leweke F, Luyten P, et al. Borderline personality disorder: a comprehensive review of diagnosis and clinical presentation, etiology, treatment, and current controversies. World Psychiatry. (2024) 23:4. doi: 10.1002/WPS.21156
3. Bohus M, Stoffers-Winterling J, Sharp C, Krause-Utz A, Schmahl C, and Lieb K. Borderline personality disorder. Lancet. (2021) 398:1528–40. doi: 10.1016/S0140-6736(21)00476-1
4. Cattane N, Rossi R, Lanfredi M, and Cattaneo A. Borderline personality disorder and childhood trauma: exploring the affected biological systems and mechanisms. BMC Psychiatry. (2017) 17:221. doi: 10.1186/s12888-017-1383-2
5. Porter C, Palmier-Claus J, Branitsky A, Mansell W, Warwick H, and Varese F. Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr Scand. (2020) 141:6–20. doi: 10.1111/acps.13118
6. Yuan Y, Lee H, Eack SM, and Newhill CE. A systematic review of the association between early childhood trauma and borderline personality disorder. J Pers. Disord. (2023) 37:16–35. doi: 10.1521/pedi.2023.37.1.16
7. Barakat S, McLean SA, Bryant E, Le A, Marks P, National Eating Disorder Research Consortium, et al. Risk factors for eating disorders: findings from a rapid review. J Eat. Disord. (2023) 11:8. doi: 10.1186/s40337-022-00717-4
8. Carpita B, Nardi B, Pronestì C, Parri F, Giovannoni F, Cremone IM, et al. May female autism spectrum be masked by eating disorders, borderline personality disorder, or complex PTSD symptoms? A Case Series. Brain Sci. (2023) 14:37. doi: 10.3390/brainsci14010037
9. Tamilson B, Eccles JA, and Shaw SCK. The experiences of autistic adults who were previously diagnosed with borderline or emotionally unstable personality disorder: A phenomenological study. Autism. (2025) 29:504–17. doi: 10.1177/13623613241276073
10. Pires S, Felgueiras P, Borges S, and Jorge J. Autism spectrum disorder in females and borderline personality disorder: the diagnostic challenge. Cureus. (2023) 15:e40279. doi: 10.7759/cureus.40279
11. Cheney L, Dudas RB, Traynor JM, Beatson JA, Rao S, and Choi-Kain LW. Co-occurring autism spectrum and borderline personality disorder: an emerging clinical challenge seeking informed interventions. Harv Rev Psychiatry. (2023) 31:83–91. doi: 10.1097/HRP.0000000000000361
13. Rydén G, Rydén E, and Hetta J. Borderline personality disorder and autism spectrum disorder in females: A cross-sectional study. Clin Neuropsychiatry. (2008) 5:22–30.
14. Dell’Osso L, Cremone IM, Nardi B, Tognini V, Castellani L, Perrone P, et al. Comorbidity and overlaps between autism spectrum and borderline personality disorder: state of the art. Brain Sci. (2023) 13:862. doi: 10.3390/brainsci13060862
15. Salgado RM, Pedrosa R, and Bastos-Leite AJ. Dysfunction of empathy and related processes in borderline personality disorder: A systematic review. Harv. Rev Psychiatry. (2020) 28:238–54. doi: 10.1097/HRP.0000000000000260
16. Dell’Osso L, Massoni L, Battaglini S, De Felice C, Nardi B, Amatori G, et al. Emotional dysregulation as a part of the autism spectrum continuum: A literature review from late childhood to adulthood. Front Psychiatry. (2023) 14:1234518. doi: 10.3389/fpsyt.2023.1234518
17. Vegni N, D’Ardia C, and Torregiani G. Empathy, mentalization, and theory of mind in borderline personality disorder: possible overlap with autism spectrum disorders. Front Psychol. (2021) 12:626353. doi: 10.3389/fpsyg.2021.626353
18. Watts J. Engendering misunderstanding: autism and borderline personality disorder. Int J Psychiatry Clin Pract. (2023) 27:316–7. doi: 10.1080/13651501.2023.2187843
19. Bargiela S, Steward R, and Mandy W. The experiences of late-diagnosed women with autism spectrum conditions: an investigation of the female autism phenotype. J Autism Dev Disord. (2016) 46:3281–94. doi: 10.1007/s10803-016-2872-8
20. Vickerstaff S, Heriot S, Wong M, Lopes A, and Dossetor D. Intellectual ability, self-perceived social competence, and depressive symptomatology in children with high-functioning autistic spectrum disorders. J Autism Dev Disord. (2007) 37:1647–64. doi: 10.1007/s10803-006-0292-x
21. Dell’Osso L, Lorenzi P, and Carpita B. Camouflaging: psychopathological meanings and clinical relevance in autism spectrum conditions. CNS Spectr. (2021) 26:437–9. doi: 10.1017/S1092852920001467
22. Cremone IM, Carpita B, Nardi B, Casagrande D, Stagnari R, Amatori G, et al. Measuring social camouflaging in individuals with high functioning autism: A literature review. Brain Sci. (2023) 13:469. doi: 10.3390/brainsci13030469
23. Dell’Osso L, Cremone IM, Chiarantini I, Arone A, Massimetti G, Carmassi C, et al. Autistic traits and camouflaging behaviors: a cross-sectional investigation in a University student population. CNS Spectr. (2022) 27:740–6. doi: 10.1017/S1092852921000808
24. Cook J, Hull L, Crane L, and Mandy W. Camouflaging in autism: A systematic review. Clin Psychol Rev. (2021) 89:102080. doi: 10.1016/j.cpr.2021.102080
25. Lai MC, Lombardo MV, Ruigrok AN, Chakrabarti B, Auyeung B, Szatmari P, et al. Quantifying and exploring camouflaging in men and women with autism. Autism. (2017) 21:690–702. doi: 10.1177/1362361316671012
26. Marino MF and Zanarini MC. Relationship between EDNOS and its subtypes and borderline personality disorder. Int J Eat Disord. (2001) 29:349–53. doi: 10.1002/eat.1029
27. Sansone RA, Levitt JL, and Sansone LA. The prevalence of personality disorders among those with eating disorders. Eat. Disord. (2004) 13:7–21. doi: 10.1080/10640260590893593
28. Carpita B, Nardi B, Giovannoni F, Parri F, Cerofolini G, Bonelli C, et al. Assessing autistic traits, hikikomori tendencies, pathological videogaming, and eating disorders in university students: are pathological videogaming and eating disorders gender-specific manifestations of the autism spectrum? Brain Sci. (2024) 14:720. doi: 10.3390/brainsci14070720
29. Carpita B, Muti D, Cremone IM, Fagiolini A, and Dell’Osso L. Eating disorders and autism spectrum: links and risks. CNS Spectr. (2022) 27:272–80. doi: 10.1017/S1092852920002011
30. Christensen SS, Bentz M, Clemmensen L, Strandberg-Larsen K, and Olsen EM. Disordered eating behaviours and autistic traits-Are there any associations in nonclinical populations? A systematic review. Eur Eat. Disord Rev. (2019) 27:8–23. doi: 10.1002/erv.2627
31. Carpita B, Nardi B, Pronestì C, Cerofolini G, Filidei M, Bonelli C, et al. The mediating role of social camouflaging on the relationship between autistic traits and orthorexic symptoms. Brain Sci. (2025) 15:503. doi: 10.3390/brainsci15050503
32. Dell’Osso L, Nardi B, Giovannoni F, Bonelli C, Massimetti G, Cremone IM, et al. Orthorexic tendencies are associated with autistic traits in patients with borderline personality disorder. J Clin Med. (2025) 14:3891. doi: 10.3390/jcm14113891
33. Dell’Osso L, Lorenzi P, and Carpita B. Autistic traits and illness trajectories. Clin Pract Epidemiol. Ment Health. (2019) 15:94–8. doi: 10.2174/1745017901915010094
34. Bradley S, Moore F, Duffy F, Clark L, Suratwala T, Knightsmith P, et al. Camouflaging, not sensory processing or autistic identity, predicts eating disorder symptoms in autistic adults. Autism. (2024) 28:2858–68. doi: 10.1177/13623613241245749
35. Hull L, Mandy W, Lai MC, Baron-Cohen S, Allison C, Smith P, et al. Development and validation of the camouflaging autistic traits questionnaire (CAT-Q). J Autism Dev Disord. (2019) 49:819–33. doi: 10.1007/s10803-018-3792-6
36. Dell’Osso L, Cremone IM, Muti D, Massimetti G, Lorenzi P, Carmassi C, et al. Validation of the Italian version of the Camouflaging Autistic Traits Questionnaire (CAT-Q) in a University population. Compr Psychiatry. (2022) 114:152295. doi: 10.1016/j.comppsych.2022.152295
38. Dell’Osso L, Gesi C, Massimetti E, Cremone IM, Barbuti M, Maccariello G, et al. Adult Autism Subthreshold Spectrum (AdAS Spectrum): Validation of a questionnaire investigating subthreshold autism spectrum. Compr Psychiatry. (2017) 73:61–83. doi: 10.1016/j.comppsych.2016.11.001
39. Kawada T. Comorbidity of eating disorders and borderline personality disorder. Int J Eat Disord. (2023) 56:478–9. doi: 10.1002/eat.23865
40. Newton JR. Borderline personality disorder and eating disorders: a trans-diagnostic approach to unravelling diagnostic complexity. Australas Psychiatry. (2019) 27:556–8. doi: 10.1177/1039856219852297
41. Dell’Osso L, Cremone IM, Carpita B, Fagiolini A, Massimetti G, Bossini L, et al. Correlates of autistic traits among patients with borderline personality disorder. Compr Psychiatry. (2018) 83:7–11. doi: 10.1016/j.comppsych.2018.01.002
42. Shen CC, Hu LY, Tsai SJ, Yang AC, Chen PM, and Hu YH. Risk stratification for the early diagnosis of borderline personality disorder using psychiatric co-morbidities. Early Interv. Psychiatry. (2018) 12:605–12. doi: 10.1111/eip.12364
43. May T, Pilkington PD, Younan R, and Williams K. Overlap of autism spectrum disorder and borderline personality disorder: A systematic review and meta-analysis. Autism Res. (2021) 14:2688–710. doi: 10.1002/aur.2619
44. Hiller RM, Young RL, and Weber N. Sex differences in autism spectrum disorder based on DSM-5 criteria: evidence from clinician and teacher reporting. J Abnorm. Child Psychol. (2014) 42:1381–93. doi: 10.1007/s10802-014-9881-x
45. Lai M-C, Lombardo MV, Auyeung B, Chakrabarti B, and Baron-Cohen S. Sex/gender differences and autism: Setting the scene for future research. J Am Acad Child Adolesc. Psychiatry. (2015) 54:11–24. doi: 10.1016/j.jaac.2014.10.003
46. Mandy W, Chilvers R, Chowdhury U, Salter G, Seigal A, and Skuse D. Sex differences in autism spectrum disorder: Evidence from a large sample of children and adolescents. J Autism Dev Disord. (2012) 42:1304–13. doi: 10.1007/s10803-011-1356-0
47. Head AM, McGillivray JA, and Stokes MA. Gender differences in emotionality and sociability in children with autism spectrum disorders. Mol Autism. (2014) 5:19. doi: 10.1186/2040-2392-5-19
48. Sedgewick F, Hill V, Yates R, Pickering L, and Pellicano E. Gender differences in the social motivation and friendship experiences of autistic and non-autistic adolescents. J Autism Dev Disord. (2016) 46:1297–306. doi: 10.1007/s10803-015-2669-1
49. Brede J, Babb C, Jones C, Elliott M, Zanker C, Tchanturia K, et al. ‘For me, the anorexia is just a symptom, and the cause is the autism’: Investigating restrictive eating disorders in autistic women. J Autism Dev Disord. (2020) 50:4280–96. doi: 10.1007/s10803-020-04479-3
50. Dandil Y, Baillie C, and Tchanturia K. Cognitive remediation therapy as a feasible treatment for a young person with anorexia nervosa and autism spectrum disorder comorbidity: A case study. Clin Case Stud. (2019) 19:115–32. doi: 10.1177/1534650119890425
51. Beck JS, Lundwall RA, Gabrielsen T, Cox JC, and South M. Looking good but feeling bad: ‘camouflaging’ behaviors and mental health in women with autistic traits. Autism. (2020) 24:809–21. doi: 10.1177/1362361320912147
52. Tierney S, Burns J, and Kilbey E. Social coping strategies of girls on the autistic spectrum. Res Autism Spectr. Disord. (2016) 23:73–83. doi: 10.1016/j.rasd.2015.11.013
53. Cage E, Di Monaco J, and Newell V. Experiences of autism acceptance and mental health in autistic adults. J Autism Dev Disord. (2018) 48:473–84. doi: 10.1007/s10803-017-3342-7
54. Hull L and Mandy W. Protective effect or missed diagnosis? Females with autism spectrum disorder. Future Neurology. (2017) 12:159–69. doi: 10.2217/fnl-2017-0006
55. Perry E, Mandy W, Hull L, and Cage E. Understanding camouflaging as a response to autism-related stigma: A social identity theory approach. J Autism Dev Disord. (2022) 52:800–10. doi: 10.1007/s10803-021-04987-w
56. Domes G, Grabe HJ, Czieschnek D, Heinrichs M, and Herpertz SC. Alexithymic traits and facial emotion recognition in borderline personality disorder. Psychother. Psychosom. (2011) 80:383. doi: 10.1159/000325828
57. New AS, Mah R, Ripoll LH, Perez-Rodriguez MM, Lazarus S, Zipursky E, et al. Empathy and alexithymia in borderline personality disorder: clinical and laboratory measures. J Personal. Disord. (2012) 26:660–75. doi: 10.1521/pedi.2012.26.5.660
58. Korzekwa MI, Dell PF, and Pain C. Dissociation and borderline personality disorder: an update for clinicians. Curr Psychiatry Rep. (2009) 11:82–8. doi: 10.1007/s11920-009-0013-1
59. Popkirov S, Flasbeck V, Schlegel U, Juckel G, and Brüne M. Childhood trauma and dissociative symptoms predict frontal EEG asymmetry in borderline personality disorder. J Trauma Dissociation. (2019) 20:32–47. doi: 10.1080/15299732.2018.1451808
60. Löffler A, Foell J, and Bekrater-Bodmann R. Interoception and its interaction with self, other, and emotion processing: implications for the understanding of psychosocial deficits in borderline personality disorder. Curr Psychiatr Rep. (2018) 20:28. doi: 10.1007/s11920-018-0890-2
61. Brewer R, Cook R, and Bird G. Alexithymia: A general deficit of interoception. R Soc Open Sci. (2016) 3:150664. doi: 10.1098/rsos.150664
62. Hatfield TR, Brown RF, Giummarra MJ, and Lenggenhager B. Autism spectrum disorder and interoception: Abnormalities in global integration? Autism. (2019) 23:212–22. doi: 10.1177/1362361317738392
63. Califano M, Pruccoli J, Martucci M, Visconti C, Barasciutti E, Sogos C, et al. Autism spectrum disorder traits predict interoceptive deficits and eating disorder symptomatology in children and adolescents with anorexia nervosa-A cross-sectional analysis: italian preliminary data. Pediatr Rep. (2024) 16:1077–88. doi: 10.3390/pediatric16040092
64. Hull L, Petrides KV, Allison C, Smith P, Baron-Cohen S, Lai MC, et al. Putting on my best normal”: social camouflaging in adults with autism spectrum conditions. J Autism Dev Disord. (2017) 47:2519–34. doi: 10.1007/s10803-017-3166-5
65. Bemmouna D, Lagzouli A, and Weiner L. The biosocial correlates and predictors of emotion dysregulation in autistic adults compared to borderline personality disorder and nonclinical controls. Mol Autism. (2023) 14:47. doi: 10.1186/s13229-023-00580-3
66. McQuaid GA, Sadowski LY, Lee NR, and Wallace GL. An examination of perceived stress and emotion regulation challenges as mediators of associations between camouflaging and internalizing symptomatology. Autism Adulthood. (2024) 6:345–61. doi: 10.1089/aut.2022.0121
67. Papalini S, Beckers T, Claes L, and Vervliet B. The drive for thinness: Towards a mechanistic understanding of avoidance behaviors in a non-clinical population. Behav Res Ther. (2021) 142:103868. doi: 10.1016/j.brat.2021.103868
68. Trautmann J, Worthy SL, and Lokken KL. Body dissatisfaction, bulimic symptoms, and clothing practices among college women. J Psychol. (2007) 141:485–98. doi: 10.3200/JRLP.141.5.485-498
69. Blythin SPM, Nicholson HL, Macintyre VG, Dickson JM, Fox JRE, and Taylor PJ. Experiences of shame and guilt in anorexia and bulimia nervosa: A systematic review. Psychol Psychother. (2020) 93:134–59. doi: 10.1111/papt.12198
Keywords: camouflaging, eating disorders, Borderline Personality Disorder, autistic traits, disordered eating
Citation: Carpita B, Nardi B, Giovannoni F, Parri F, Pronestì C, Bonelli C, Massimetti G, Pini S, Bruno A, Muscatello MRA, Della Rocca B, Fiorillo A and Dell’Osso L (2025) Social camouflaging predicts eating disorder symptomatology among female patients with Borderline Personality Disorder. Front. Psychiatry 16:1646586. doi: 10.3389/fpsyt.2025.1646586
Received: 13 June 2025; Accepted: 15 September 2025;
Published: 10 October 2025.
Edited by:
Costanza Colombi, Stella Maris Foundation (IRCCS), ItalyReviewed by:
Joanna Monika Kossewska, Pedagogical University of Kraków, PolandAntoine Frigaux, EA4432 Laboratoire de Psychologie de l’Interaction et des Relations Intersubjectives (INTERPSY), France
Copyright © 2025 Carpita, Nardi, Giovannoni, Parri, Pronestì, Bonelli, Massimetti, Pini, Bruno, Muscatello, Della Rocca, Fiorillo and Dell’Osso. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benedetta Nardi, YmVuZWRldHRhLm5hcmRpQGxpdmUuaXQ=
 Barbara Carpita
Barbara Carpita Benedetta Nardi
Benedetta Nardi Federico Giovannoni1
Federico Giovannoni1 Francesca Parri
Francesca Parri Cristiana Pronestì
Cristiana Pronestì Chiara Bonelli
Chiara Bonelli Stefano Pini
Stefano Pini Antonio Bruno
Antonio Bruno Andrea Fiorillo
Andrea Fiorillo