Abstract
Introduction:
Studies have suggested a link between dietary behavior and adolescent depressive symptoms, but longitudinal data are scarce. This study examines the longitudinal association of breakfast and midnight snacks consumption with depressive symptoms among multi-ethnic adolescents in China.
Methods:
From October 2022 to October 2024, 1,693 middle school students (52.3% females) from Yunnan Province participated in five follow-up surveys (T1-T5) conducted every six months. Breakfast and midnight snacks consumption were assessed using questionnaires, and depressive symptoms were measured using Children’s Depression Inventory. The latent growth curve model was analyzed using Mplus software to assess the potential growth trajectories of breakfast days, midnight snacks days, and depressive symptom scores across five time points. The generalized estimation equation model was applied to examine the association between the number of breakfast and midnight snacks days and depressive symptom scores. Two models were established: Model 1 was unadjusted, without controlling any variables; Model 2 was adjusted for demographic variables and other potential confounders influencing depressive symptoms. A restricted cubic spline analysis was used to examine the relationship between the number of breakfast days per week, midnight snacks days per week, and depressive symptoms.
Results:
The prevalence of depressive symptoms increased from 26.3% at T1 to 37.3% at T5 (P < 0.01). After adjusting for confounders, breakfast frequency (β = -0.71, 95%CI: -0.87-0.56) and midnight snacks frequency in males (β = 0.39, 95%CI: 0.24 - 0.55) and females (β = -0.77, 95%CI: -0.92 - -0.63; β = 0.17, 95%CI: 0.02 - 0.32) were associated with depressive symptoms (all P < 0.05). Males eating breakfast and midnight snacks fewer than three days and more than four days, respectively, per week, and females eating breakfast and midnight snacks fewer than four days and more than two day, respectively, per week, had an increased risk of depressive symptoms.
Discussion:
Skipping breakfast and eating midnight snacks are related to depressive symptoms in multi-ethnic Chinese adolescents. Addressing unhealthy eating behaviors is critical for preventing and mitigating adolescent depressive symptoms.
Introduction
Adolescent depression is a significant public health concern. This developmental stage is marked by rapid social, emotional, and cognitive changes, as well as major life transitions (1). Adolescence is also the peak period for depression onset (2) and represents a substantial disease burden in this age group (3, 4). Furthermore, depression is a key risk factor for self-harm and suicidal behaviors among adolescents (5, 6). Globally, the incidence and prevalence of depressive symptoms in adolescents are increasing (7–9). A representative study in Germany reported a prevalence of 18.4%, with both the severity and frequency of depressive symptoms being higher in females than in males. Additionally, depressive symptoms were found to increase with age (10). The prevalence of depressive symptoms among adolescents in the United exceeds 30% (11). Numerous studies have examined the prevalence of depressive symptoms among adolescents in developing countries. In Malaysia and India, reported prevalence rates range from 26.2% to 52.3%. In Bangladesh, 25.0% of adolescents experience depressive symptoms, with a higher prevalence in females (30.0%) compared to males (19.0%) (12). In China, the prevalence of depressive symptoms among adolescents is close to 40% (13). However, data on the prevalence of depressive symptoms among multi-ethnic adolescents in western China remain limited. Existing research suggests that depressive symptoms are influenced by multiple factors, including academic pressure, family stress, physical activity, screen time, and physical literacy (14–18). Recently, the relationship between dietary behaviors and depressive symptoms in adolescents has gained increasing attention.
Emerging evidence suggests that healthy dietary patterns, such as adherence to the Mediterranean diet, are negatively associated with depressive symptoms (19). In contrast, unhealthy dietary behaviors— including frequent snacking, skipping breakfast, consuming sugar-sweetened beverages, and eating ultra-processed foods —are positively linked to depressive symptoms in adolescents (20–23). Previous research has primarily examined the relationship between breakfast consumption and adolescent mental health (24, 25). Systematic reviews and meta-analyses indicate that skipping breakfast is positively associated with an increased risk of depressive symptoms in adolescents (25). In contrast, regular breakfast consumption (≥6 days per week) among Japanese adolescents is negatively associated with depressive symptoms (26, 27). Studies conducted in Spain, Turkey, and Bangladesh have identified skipping breakfast as a predictor of depressive symptoms. Adolescents who skip breakfast or consume it fewer than five days per week have a significantly higher incidence of depressive symptoms compared to those who eat breakfast regularly (12, 28, 29). However, few cross-sectional studies in China have examined the relationship between breakfast consumption and depressive symptoms in adolescents (30). Among Chinese adolescents aged 12–17 years, inconsistent breakfast consumption is a significant risk factor for mental health problems, with a more pronounced effect in females (31). Compared to those who consume breakfast ≥6 per week, the risk of depressive symptoms is higher in adolescents who eat breakfast 2–5 days per week (OR = 1.76) and those who do so ≤1 day per week (OR = 3.78) (32). Additionally, a study in eastern China among adolescents aged 11–19 years found that skipping breakfast (OR = 2.56) was independently associated with depressive symptoms (33).
Few studies have examined midnight snacks consumption among adolescents (34). Midnight snacks, also referred to as nighttime eating, typically involves consuming food between 9:00 PM and 04:00 AM, in addition to the three main daily meals. This behavior includes a variety of foods, such as snacks, vegetables, desserts, and other small meals. Previous research suggests that midnight snacks are common among adolescents, with reported prevalence rates of 9.0% in Canada (35), 16.6% in Bangladesh (36), and 29.7% in Palestine (37). Notably, the prevalence of midnight snacks among Chinese adolescents is significantly higher (72.5%) (38). Previous studies suggest associations between adolescent dietary disorders, intuitive eating, nighttime eating syndrome, and mental health (39–41). However, research on the relationship between midnight snacks and depressive symptoms in adolescents remains unlimited. In Palestinian adolescents, nighttime eating was linked to mental health issues, including depressive symptoms (OR = 4.18) (37). Additionally, a cross-sectional study of adolescents aged 12–13 years found that nighttime eating was associated with severe depressive symptoms (OR = 1.04) (35). A cross-sectional study in Turkey found that adolescents who frequently consumed midnight snacks reported higher levels of depressive symptoms (42). Similarly, studies in the United States and Switzerland indicated that depressive symptoms were more prevalent among adolescents diagnosed with night-eating syndrome (43, 44). Additionally, among Chinese children and adolescents in grades 1-9, those who ate before bedtime had a 1.28 times higher risk of depressive symptoms compared to those who did not (45).
While some studies have examined the relationship between breakfast and midnight snacks behaviors and adolescent depressive symptoms, research on multi-ethnic adolescents in China remains scarce. Yunnan Province, located in southwest China, is a major multi-ethnic region. Due to the influence of diverse food cultures and economic situations, adolescents in this area may be more likely to skip breakfast and consume midnight snacks. This study hypothesizes a longitudinal association between skipping breakfast, midnight snacks, and depressive symptoms among multi-ethnic adolescents in China. To test this hypothesis, we conducted a follow-up survey in Yunnan Province.
Materials and methods
Participants
A longitudinal questionnaire survey was conducted among 1,693 middle school students from four schools in three regions of Yunnan Province, China. The baseline survey (T1) took place in October 2022, followed by an assessment every six months. The subsequent follow-up surveys were conducted in June 2023 (T2), October 2023 (T3), June 2024 (T4), and October 2024 (T5). The attrition rates for each follow-up were 15.6%, 2.7%, 1.7%, and 3.7%, respectively. Ultimately, 1,693 participants were included in the final analysis. A flowchart depicting the inclusion of study participants is presented in Figure 1. The average age the participants was (12.5 ± 0.5) years, with the minimum age being 12 years and the maximum 15 years. The final sample consisted of 808 males (47.7%), and 885 females (52.3%). The participants comprised 629 Han (37.2%), 628 Yi (37.1%), 66 Hani (3.9%), 143 Lahu (8.4%), 78 Dai (4.6%), and 149 individuals from other ethnic groups (8.8%). Among them, 1,278 (75.5%) resided in rural areas, while 415 (24.5%) were from urban areas. In terms of family structure, 1,391 participants (82.2%) came from two-parent families, 166 (9.8%) from single-parent families, 110 (6.5%) from blended families, and 26 (1.5%) from other family types. Additionally, 321 participants (19.0%) were only children. Regarding socioeconomic status, participants self-reported as follows: 49 (2.9%) as “worse,” 180 (10.6%) as “poor,” 1,132 (66.9%) as “medium,” 246 (14.5%) as “good,” and 86 (5.1%) as “better.” Table 1 displays the distribution of demographic variables in relation to the prevalence of depressive symptoms. The study was in accordance with the requirement of the World Medical Association Declaration of Helsinki and granted with consent from the students, schools, and parents. The questionnaire survey was conducted anonymously, with voluntary participation from all teenage respondents. Participants retained the right to withdraw from the follow-up survey at any time. All collected data were treated with strict confidentiality and used exclusively for data analysis in this study, with no other applications. The study was approved by the Medical Ethics Committee of the School of Medicine, Kunming University (Approval Number: 20210222).
Figure 1
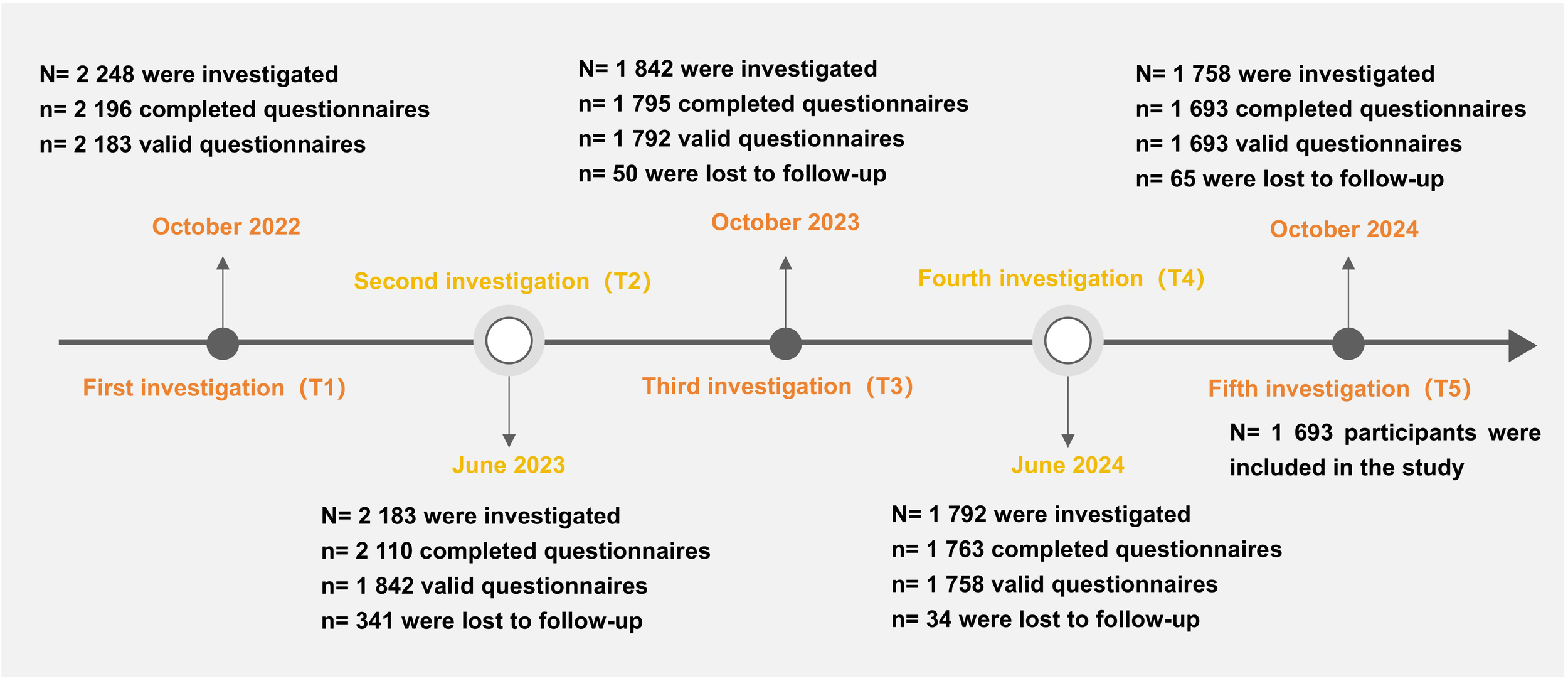
Flow chart of participants.
Table 1
| Variables | Category | T1 | T2 | T3 | T4 | T5 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Depressive symptomS | Normal | χ2 | P | Depressive symptomS | Normal | χ2 | P | Depressive symptomS | Normal | χ2 | P | Depressive symptomS | Normal | χ2 | P | Depressive symptomS | Normal | χ2 | P | |||
| Sex | Male | 175 | 633 | 17.07 | <0.01 | 203 | 605 | 27.47 | <0.01 | 232 | 576 | 19.41 | <0.01 | 260 | 548 | 9.66 | 0.002 | 255 | 553 | 21.57 | <0.01 | |
| Female | 270 | 615 | 327 | 558 | 344 | 541 | 349 | 536 | 376 | 509 | ||||||||||||
| Residence | Rural | 357 | 921 | 7.32 | 0.007 | 417 | 861 | 4.25 | 0.039 | 449 | 829 | 2.87 | 0.091 | 465 | 813 | 0.39 | 0.534 | 479 | 799 | 0.10 | 0.755 | |
| Urban | 88 | 327 | 113 | 302 | 127 | 288 | 144 | 271 | 152 | 263 | ||||||||||||
| Age(year) | 12 | 243 | 716 | 1.24 | 0.539 | 311 | 648 | 1.34 | 0.511 | 328 | 631 | 0.07 | 0.965 | 357 | 602 | 1.55 | 0.460 | 374 | 585 | 2.92 | 0.232 | |
| 13 | 195 | 517 | 212 | 500 | 241 | 471 | 244 | 468 | 250 | 462 | ||||||||||||
| 14-15 | 7 | 15 | 7 | 15 | 7 | 15 | 8 | 14 | 7 | 15 | ||||||||||||
| Ethnicity | Han | 145 | 484 | 44.77 | <0.01 | 198 | 431 | 2.45 | 0.785 | 200 | 429 | 9.36 | 0.096 | 219 | 410 | 2.05 | 0.842 | 231 | 398 | 2.35 | 0.799 | |
| Hani | 28 | 38 | 26 | 40 | 32 | 34 | 25 | 41 | 29 | 37 | ||||||||||||
| Yi | 142 | 486 | 191 | 437 | 217 | 411 | 226 | 402 | 230 | 398 | ||||||||||||
| Lahu | 63 | 80 | 44 | 99 | 45 | 98 | 49 | 94 | 52 | 91 | ||||||||||||
| Dai | 29 | 49 | 23 | 55 | 25 | 53 | 30 | 48 | 33 | 45 | ||||||||||||
| Other | 38 | 111 | 48 | 101 | 57 | 92 | 60 | 89 | 56 | 93 | ||||||||||||
| The number of close friends | 0 | 15 | 18 | 77.40 | <0.01 | 12 | 21 | 13.40 | 0.009 | 14 | 19 | 9.04 | 0.060 | 15 | 18 | 9.97 | 0.041 | 15 | 18 | 8.10 | 0.088 | |
| 1-2 | 89 | 85 | 74 | 100 | 75 | 99 | 69 | 105 | 78 | 96 | ||||||||||||
| 3-4 | 84 | 209 | 95 | 198 | 101 | 192 | 115 | 178 | 117 | 176 | ||||||||||||
| 5-6 | 60 | 248 | 94 | 214 | 102 | 206 | 122 | 186 | 108 | 200 | ||||||||||||
| ≥7 | 197 | 688 | 255 | 630 | 284 | 601 | 288 | 597 | 313 | 572 | ||||||||||||
| The only child in the family | Yes | 80 | 241 | 0.38 | 0.538 | 97 | 224 | 0.22 | 0.641 | 106 | 215 | 0.18 | 0.674 | 113 | 208 | 0.10 | 0.750 | 115 | 206 | 0.35 | 0.552 | |
| No | 365 | 1007 | 433 | 939 | 470 | 902 | 496 | 876 | 516 | 856 | ||||||||||||
| Family type | Two-parent family | 351 | 1040 | 5.39 | 0.146 | 430 | 961 | 0.99 | 0.804 | 467 | 924 | 0.92 | 0.822 | 494 | 897 | 3.98 | 0.264 | 517 | 874 | 1.35 | 0.717 | |
| One-parent family | 48 | 118 | 55 | 111 | 61 | 105 | 59 | 107 | 64 | 102 | ||||||||||||
| Combined family | 37 | 73 | 35 | 75 | 38 | 72 | 42 | 68 | 38 | 72 | ||||||||||||
| Other | 9 | 17 | 10 | 16 | 10 | 16 | 14 | 12 | 12 | 14 | ||||||||||||
| Self-perceived socioeconomic status | Worse | 18 | 31 | 48.24 | <0.01 | 19 | 30 | 20.93 | <0.01 | 28 | 21 | 33.40 | <0.01 | 23 | 26 | 6.83 | 0.145 | 27 | 22 | 17.20 | 0.002 | |
| Poor | 82 | 98 | 78 | 102 | 84 | 96 | 73 | 107 | 81 | 99 | ||||||||||||
| Medium | 283 | 849 | 351 | 781 | 376 | 756 | 400 | 732 | 416 | 716 | ||||||||||||
| Good | 47 | 199 | 64 | 182 | 67 | 179 | 89 | 157 | 85 | 161 | ||||||||||||
| Better | 15 | 71 | 18 | 68 | 21 | 65 | 24 | 62 | 22 | 64 | ||||||||||||
| Father's education level | Illiteracy | 55 | 95 | 11.92 | 0.018 | 50 | 100 | 1.68 | 0.794 | 52 | 98 | 1.68 | 0.794 | 60 | 90 | 5.91 | 0.206 | 54 | 96 | 2.00 | 0.736 | |
| Elementary school | 116 | 299 | 135 | 280 | 148 | 267 | 153 | 262 | 160 | 255 | ||||||||||||
| Secondary school | 196 | 593 | 237 | 552 | 268 | 521 | 276 | 513 | 292 | 497 | ||||||||||||
| High school | 51 | 179 | 76 | 154 | 76 | 154 | 90 | 140 | 90 | 140 | ||||||||||||
| University | 27 | 82 | 32 | 77 | 32 | 77 | 30 | 79 | 35 | 74 | ||||||||||||
| Mother's education level | Illiteracy | 63 | 131 | 7.04 | 0.134 | 61 | 133 | 2.10 | 0.717 | 73 | 121 | 3.16 | 0.531 | 73 | 121 | 2.14 | 0.711 | 73 | 121 | 2.17 | 0.704 | |
| Elementary school | 123 | 310 | 147 | 286 | 154 | 279 | 164 | 269 | 151 | 282 | ||||||||||||
| Secondary school | 190 | 594 | 236 | 548 | 262 | 522 | 275 | 509 | 305 | 479 | ||||||||||||
| High school | 43 | 131 | 52 | 122 | 52 | 122 | 63 | 111 | 62 | 112 | ||||||||||||
| University | 26 | 82 | 34 | 74 | 35 | 73 | 34 | 74 | 40 | 68 | ||||||||||||
| Father's occupation | Civil servant | 237 | 628 | 4.41 | 0.491 | 262 | 603 | 10.39 | 0.065 | 305 | 560 | 5.30 | 0.381 | 300 | 565 | 14.43 | 0.013 | 322 | 543 | 7.98 | 0.157 | |
| Worker | 29 | 85 | 33 | 81 | 31 | 83 | 39 | 75 | 37 | 77 | ||||||||||||
| Staff | 87 | 253 | 117 | 223 | 117 | 223 | 142 | 198 | 139 | 201 | ||||||||||||
| Merchant | 29 | 119 | 38 | 110 | 45 | 103 | 39 | 109 | 43 | 105 | ||||||||||||
| Farmer | 16 | 40 | 26 | 30 | 23 | 33 | 26 | 30 | 23 | 33 | ||||||||||||
| Other | 47 | 123 | 54 | 116 | 55 | 115 | 63 | 107 | 67 | 103 | ||||||||||||
| Mother's occupation | Civil servant | 270 | 701 | 3.77 | 0.583 | 299 | 672 | 6.13 | 0.293 | 344 | 627 | 4.47 | 0.484 | 347 | 624 | 4.22 | 0.518 | 366 | 605 | 2.94 | 0.709 | |
| Worker | 25 | 83 | 27 | 81 | 31 | 77 | 32 | 76 | 37 | 71 | ||||||||||||
| Staff | 42 | 137 | 62 | 117 | 62 | 117 | 68 | 111 | 68 | 111 | ||||||||||||
| Merchant | 42 | 128 | 48 | 122 | 49 | 121 | 57 | 113 | 55 | 115 | ||||||||||||
| Farmer | 15 | 57 | 24 | 48 | 23 | 49 | 28 | 44 | 28 | 44 | ||||||||||||
| Other | 51 | 142 | 70 | 123 | 67 | 126 | 77 | 116 | 77 | 116 | ||||||||||||
The distribution of the positive rate of depressive symptoms in adolescents.
Methods
Survey methods
A cross-sectional questionnaire survey was conducted among middle school students across 11 counties in Yunnan Province using random cluster sampling. The details of this methodology have been described in our previously published work (46). Based on the cross-sectional survey, four middle schools with high multi-ethnic representation and strong participant compliance were selected for the longitudinal follow-up study. All seventh-grade (Grade 7) students from the selected schools participated in the survey. The adolescents completed a self-administered questionnaire in a classroom setting. The survey collected data on demographic characteristics (e.g., gender, age, ethnicity, only child status, family residence, self-rated family economic status, family structure, number of close friends, parental education levels, and parental occupations). Additionally, it assessed dietary behaviors (breakfast and midnight snacks), depressive symptoms, and potential confounding factors influencing adolescents’ depression, including family changes, hospitalization history, screen time, smoking, alcohol consumption, physical activity, family history of depression, self-rated academic pressure impact of the COVID-19 pandemic. Trained surveyors administered the survey in person, addressing participants’ questions face-to-face. Adolescents completed the questionnaire independently without discussing responses with peers. The process took approximately 15–20 minutes. Surveyors reviewed the completed questionnaires upon collection, promptly addressing any missing responses.
Evaluation of depressive symptoms
Depressive symptoms were assessed using the Chinese version of the Children’s Depression Inventory (CDI), a widely used self-report scale for measuring depression in children and adolescents (47, 48). The CDI evaluates depressive mood and behavior in individuals aged 7–17 years, based on self-reported experiences over the past two weeks. The inventory consists of 27 items across five dimensions: anhedonia, negative mood, negative self-esteem, ineffectiveness, and interpersonal problems. Each item is rated on a 3-point scale (“occasionally,” “often” and “always”), with scores ranging from 0 to 2 per item, resulting in a total possible score of 0-54. Higher scores indicate more severe depressive symptoms. A total CDI score ≥19 was considered indicative of depressive symptoms, while a score < 19 was classified as negative. Studies on Chinese children and adolescents (aged 7–17 years) have demonstrated that the CDI has good reliability and validity, with a Cronbach’s α of 0.84 (49). Research on Chinese middle school students further supports the CDI’s high reliability and validity, confirming its suitability for assessing depressive symptoms in this population (Cronbach’s α coefficient of 0.853) (50). Cronbach’s α coefficients at T1 –T5 were 0.861, 0.892, 0.900, 0.893 and 0.904, respectively, indicating strong internal consistency.
Breakfast behavior and midnight snacks behavior evaluation
Adolescent dietary behaviors were assessed using a dietary frequency questionnaire developed by the research group, which has been repeatedly validated for good reliability and validity (46, 51). Firstly, a pilot test was conducted in 131 middle school students before the field survey to assess participant understanding of the questionnaire. The pilot test results showed that middle school students were able to fully understand the content of the questionnaire, and the average time taken to complete the questionnaire was 16 minutes. Secondly, in each follow-up survey, we evaluated the reliability and validity of the dietary frequency questionnaire, the Cronbach’s α coefficients at T1 –T5 were 0.921, 0.936, 0.942, 0.945, and 0.940, respectively.
Midnight snacks behavior refers to the behavior of consumption of food between 21:00 and 04:00, in addition to the three main meals of the day. This includes various snacks, desserts, and other food items. Breakfast behavior refers to the consumption of the first meal of the day, typically between 06:00 and 08:00. This study the breakfast and midnight snacks behaviors of multi-ethnic adolescents. Participants were asked the following questions (1): “How many days did you eat breakfast in the past week?” Response options included (1) 0 days (2), 1–2 days (3), 3–4 days (4), 5–6 days (5), 7 days (2). “How many days did you consume midnight snacks (including snacks) before going to bed in the past week?” The response options included (1) 0 days (2), 1–2 days (3), 3–4 days (4), 5–6 days (5), 7 days. Adolescents selected the number of days they consumed breakfast and midnight snacks based on their actual eating habits.
Statistical analysis
Data were entered into a database using EpiData 3.0. After data verification, statistical analyses were conducted using SPSS (version 23.0; SPSS Inc., Chicago, IL, USA), R (version 4.3.1), and Mplus (version 7.4). Descriptive statistics, χ2 tests, and generalized estimation equation (GEE) models were performed in SPSS. Restricted cubic spline analysis was conducted using R software. The latent growth curve model (LGCM) was analyzed using Mplus software to assess the potential growth trajectories of breakfast days, midnight snacks days, and depressive symptom scores across five time points. Intercept and slope factors were included as observation indices. A χ2 test was used to compare differences in the detection rates of depressive symptoms among college students with different demographic characteristics over time. The generalized estimation equation (GEE) model was applied to examine the association between the number of breakfast and midnight snacks days and depressive symptom scores. In the model, breakfast days and the number of midnight snacks per week were treated as independent variables, while depressive symptom scores were the dependent variable. Both independent and dependent variables were continuous variables. Two models were established: Model 1, which was unadjusted, without controlling any variables; Model 2, which was adjusted for demographic variables and other potential confounders influencing depressive symptoms, followed by an association analysis. The identification of confounding factors mainly stems from the variables reported in the literature that have evidence suggesting they may affect adolescent depression symptoms. The adjustment method is to include both the confounding variables and the analysis variables (the days of eating breakfast per week and the days of eating midnight snacks per week) in the model as independent variables. A restricted cubic spline analysis was used to examine the relationship between the number of breakfast days per week, midnight snacks days per week, and depressive symptoms. The statistical significance level was set at α = 0.05.
Results
The growth trajectories of breakfast and midnight snacks consumption and depressive symptoms among adolescents
The prevalence rates of depressive symptoms from T1 to T5 were 26.3%, 31.3%, 34.0%, 36.0%, and 37.3%, respectively. The reported frequencies of breakfast consumption on day 0, day 1–2, day 3–4, day 5–6, and day 7 in the past week were as follows: T1 (5.0%, 9.2%, 13.3%, 21.5%, and 51.1%, respectively), T2 (6.1%, 13.1%, 14.6%, 21.7%, and 44.5%, respectively), T3 (1.4%, 7.6%, 14.2%, 30.5%, and 46.3%, respectively), T4 (2.2%, 7.0%, 15.2%, 26.8%, and 48.7%, respectively), and T5 (4.7%, 9.2%, 14.7%, 24.6%, and 46.8%, respectively). The reported frequencies of eating a midnight snacks on day 0, day 1–2, day 3–4, day 5–6, and day 7 in the past week were as follows: T1 (28.7%, 36.3%, 18.7%, 7.6%, and 8.7%, respectively), T2 (22.9%, 40.6%, 20.3%, 7.6%, and 8.6%, respectively), T3 (19.7%, 43.4%, 20.5%, 8.5%, and 7.9%, respectively), T4 (16.6%, 41.0%, 22.1%, 10.7%, and 9.6%, respectively), and T5 (21.3%, 39.8%, 20.1%, 8.3%, and 10.5%, respectively).Table 2 shows the fitting results of the latent growth curve model. The fitting index Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), Sample-Size Adjusted BIC, Chi-Square Test of Model Fit (P-Value), Root Mean Square Error Of Approximation (RMSEA), Comparative Fit Index (CFI), Tucker-Lewis index (TLI), and Standardized Root Mean Square Residual (SRMR) of the days of eating midnight snacks per week were 25170.64, 25279.32, 25215.78, 92.19 (<0.01), 0.07, 0.96, 0.96, and 0.05, respectively. These indices of the days of eating breakfast per week were 25016.14, 25124.82, 25061.28, 210.95 (<0.01), 0.11, 0.87, 0.87, and 0.09, respectively. These indices of depressive symptoms were 55776.48, 55885.17, 55821.63, 362.53 (<0.01), 0.14, 0.93, 0.93, and 0.12, respectively. Figure 2 illustrates the potential growth trajectories of adolescents’ breakfast consumption, midnight snacks consumption, and depressive symptom scores over the past week. The variance estimates for the intercept and slope factors of breakfast consumption and depressive symptom scores were statistically significant for both males and females (all P < 0.01), indicating differences in initial levels and growth rates of breakfast consumption and depressive symptoms among adolescents.
Table 2
| Variable | Sex | Growth factor | Estimate | SE | Est/SE | P-Value |
|---|---|---|---|---|---|---|
| The days of eating midnight snack per week | Male | Intercept factor | 0.51 | 0.06 | 8.21 | <0.01 |
| Slope factor | 0.01 | 0.01 | 1.18 | 0.237 | ||
| Female | Intercept factor | 0.45 | 0.05 | 9.07 | <0.01 | |
| Slope factor | 0.04 | 0.01 | 5.97 | <0.01 | ||
| The days of eating breakfast per week | Male | Intercept factor | 0.45 | 0.06 | 7.63 | <0.01 |
| Slope factor | 0.03 | 0.01 | 4.37 | <0.01 | ||
| Female | Intercept factor | 0.37 | 0.05 | 6.86 | <0.01 | |
| Slope factor | 0.03 | 0.01 | 4.05 | <0.01 | ||
| Depressive symptoms | Male | Intercept factor | 30.39 | 2.51 | 12.13 | <0.01 |
| Slope factor | 1.73 | 0.25 | 7.10 | <0.01 | ||
| Female | Intercept factor | 40.29 | 3.03 | 13.31 | <0.01 | |
| Slope factor | 2.35 | 0.26 | 9.120 | <0.01 |
The latent growth curve of depressive symptoms, the days of eating midnight snack and breakfast per week.
Figure 2
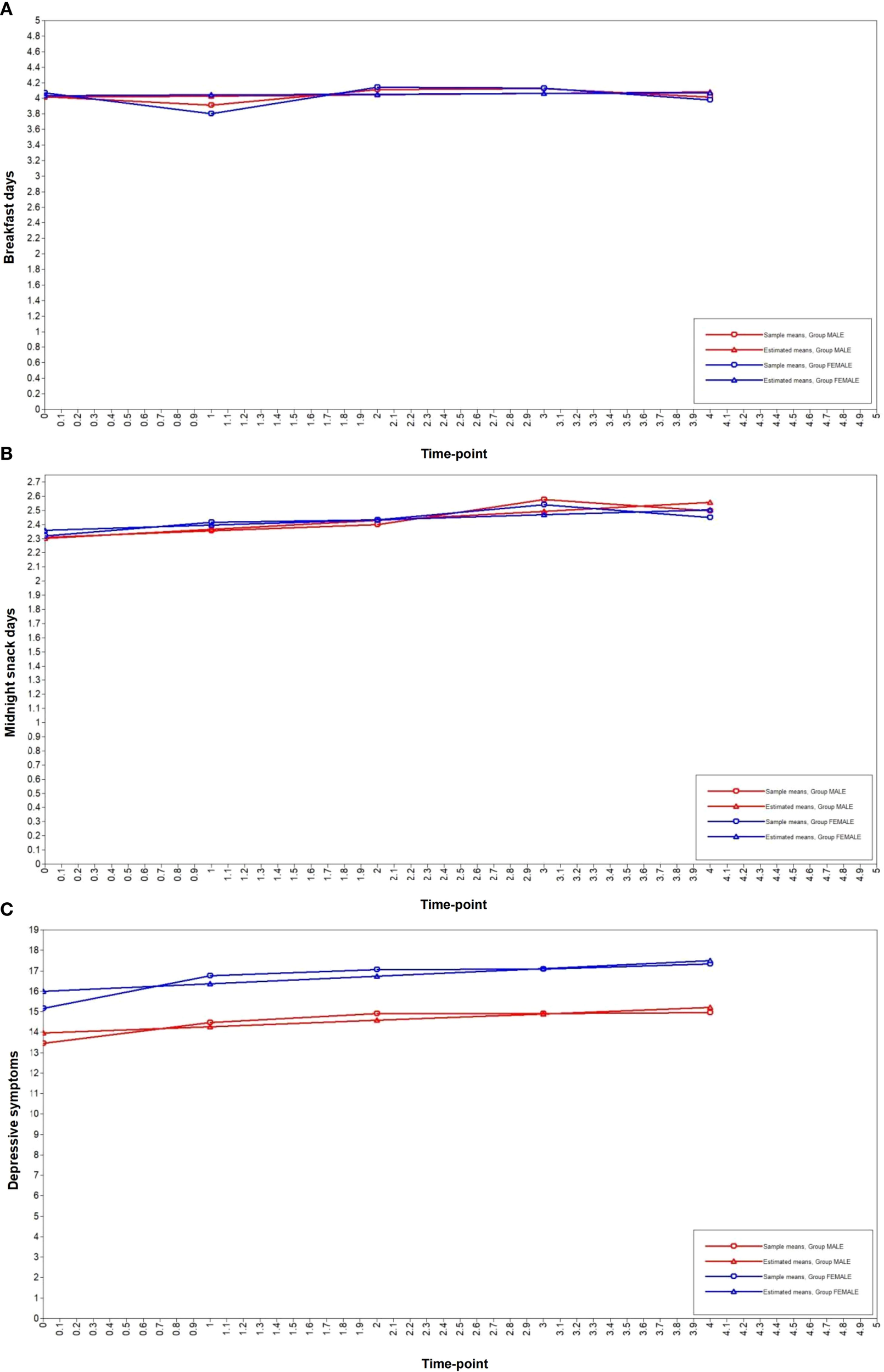
The latent growth curve of depressive symptoms, the days of eating midnight snack and breakfast per week. (A) breakfast days, (B) midnight snack days, (C) depressive symptoms.
The variance estimates for the intercept factor and slope factors of the potential growth trajectory of midnight snacks days in the previous week were statistically significant for females (all P < 0.01). However, for males, the variance estimates for the intercept factor of the potential growth trajectory of male slope factors were not statistically significant (P > 0.05). There were differences in the initial level and growth rate of the number of midnight snacks days for females in the last week, whereas there were differences only in the initial level of the number of midnight snacks days for males in the last week, and there was no difference in the growth rate.
Distribution of depressive symptoms among adolescents
Table 1 presents the prevalence of depressive symptoms among adolescents with different demographic characteristics. Significant differences were observed between boys and girls at all five time points (T1: χ2 = 17.07, T2: χ2 = 27.47, T3: χ2 = 19.41, T4: χ2 = 9.66, T5: χ2 = 21.57; all P < 0.01). In addition, the prevalence of depressive symptoms varied significantly at certain time points based on family residence, ethnicity, number of close friends, self-rated family economic status, father’s education level, and father’s occupation (P < 0.05). However, no significant differences in the prevalence of depressive symptoms were observed across other demographic variables (P > 0.05).
The association between adolescents’ breakfast behavior and midnight snacks behavior and depressive symptoms
Table 3 presents the results of the generalized linear model analysis of the association between the number of breakfast and midnight snacks days and depressive symptom scores in adolescents in the past week. After adjusting for confounding variables, the number of breakfast days was negatively associated with depressive scores across all groups: adolescents overall (β = -0.76, 95%CI: -0.87 to -0.65, P < 0.01), males (β = -0.71, 95%CI: -0.87 to -0.56, P < 0.01) and females (β = -0.77, 95%CI: -0.92 to -0.63, P < 0.01). In addition, the number of midnight snacks days was positively associated with depressive symptoms across all groups: adolescents overall (β = 0.29, 95%CI: 0.18 to 0.40, P < 0.01), males (β = 0.39, 95%CI: 0.24 to 0.55, P < 0.01), and females (β = 0.17, 95%CI: 0.02 to 0.32, P = 0.027). Figure 3 shows the results of the restricted cubic spline analysis of the association between the number of breakfast and midnight snacks days per week and depressive symptom scores. Overall, breakfast and midnight snacks behaviors were related to adolescent depressive symptoms. Males’ breakfast behavior was more sensitive to depressive symptoms, whereas females’ midnight snacks behavior was more sensitive to depressive symptoms. Adolescents who ate breakfast fewer than four days in the past week and consumed midnight snacks more than two day per week exhibited an increased risk of depressive symptoms. Among males, eating breakfast fewer than three days per week and eating midnight snacks more than four days per week increased the risk of depressive symptoms. Among females, eating breakfast fewer than four days per week and eating midnight snacks more than two day per week was associated with an increased risk of depressive symptoms.
Table 3
| Model | Adolescents | Variables | β (95% CI) | SE | Wald χ2 | P |
|---|---|---|---|---|---|---|
| Model 1 | All participants | The days of eating breakfast per week | -0.98(-1.09−-0.87) | 0.06 | 288.10 | <0.01 |
| The days of eating midnight snack per week | 0.51(0.39−0.62) | 0.06 | 77.28 | <0.01 | ||
| Male | The days of eating breakfast per week | -0.95(-1.11−-0.79) | 0.08 | 131.15 | <0.01 | |
| The days of eating midnight snack per week | 0.60(0.44−0.76) | 0.08 | 54.71 | <0.01 | ||
| Female | The days of eating breakfast per week | -1.00(-1.16−-0.84) | 0.08 | 156.13 | <0.01 | |
| The days of eating midnight snack per week | 0.40 (0.24−0.56) | 0.08 | 23.86 | <0.01 | ||
| Model 2 | All participants | The days of eating breakfast per week | -0.76(-0.87−-0.65) | 0.06 | 185.87 | <0.01 |
| The days of eating midnight snack per week | 0.29(0.18−0.40) | 0.06 | 26.59 | <0.01 | ||
| Male | The days of eating breakfast per week | -0.71(-0.87−-0.56) | 0.08 | 80.32 | <0.01 | |
| The days of eating midnight snack per week | 0.39(0.24−0.55) | 0.08 | 24.21 | <0.01 | ||
| Female | The days of eating breakfast per week | -0.77(-0.92−-0.63) | 0.07 | 107.73 | <0.01 | |
| The days of eating midnight snack per week | 0.17(0.02−0.32) | 0.08 | 4.89 | 0.027 |
Longitudinal association of breakfast and midnight snack with depressive symptoms in Yunnan multi-ethnic adolescents.
Model 1 unadjusted for variables. Model 2 adjusted for age, ethnicity, residence, the only child in the family, family type, parental educational level, parental occupation, family changes, hospital experience, the impact of COVID-19, family history of depression, self-perceived socioeconomic status, self-perceived academic stress, video time, physical activity, smoking, alcohol consumption, the number of close friends, consumption of takeaway fast food and sugar-sweetened beverage.
Figure 3
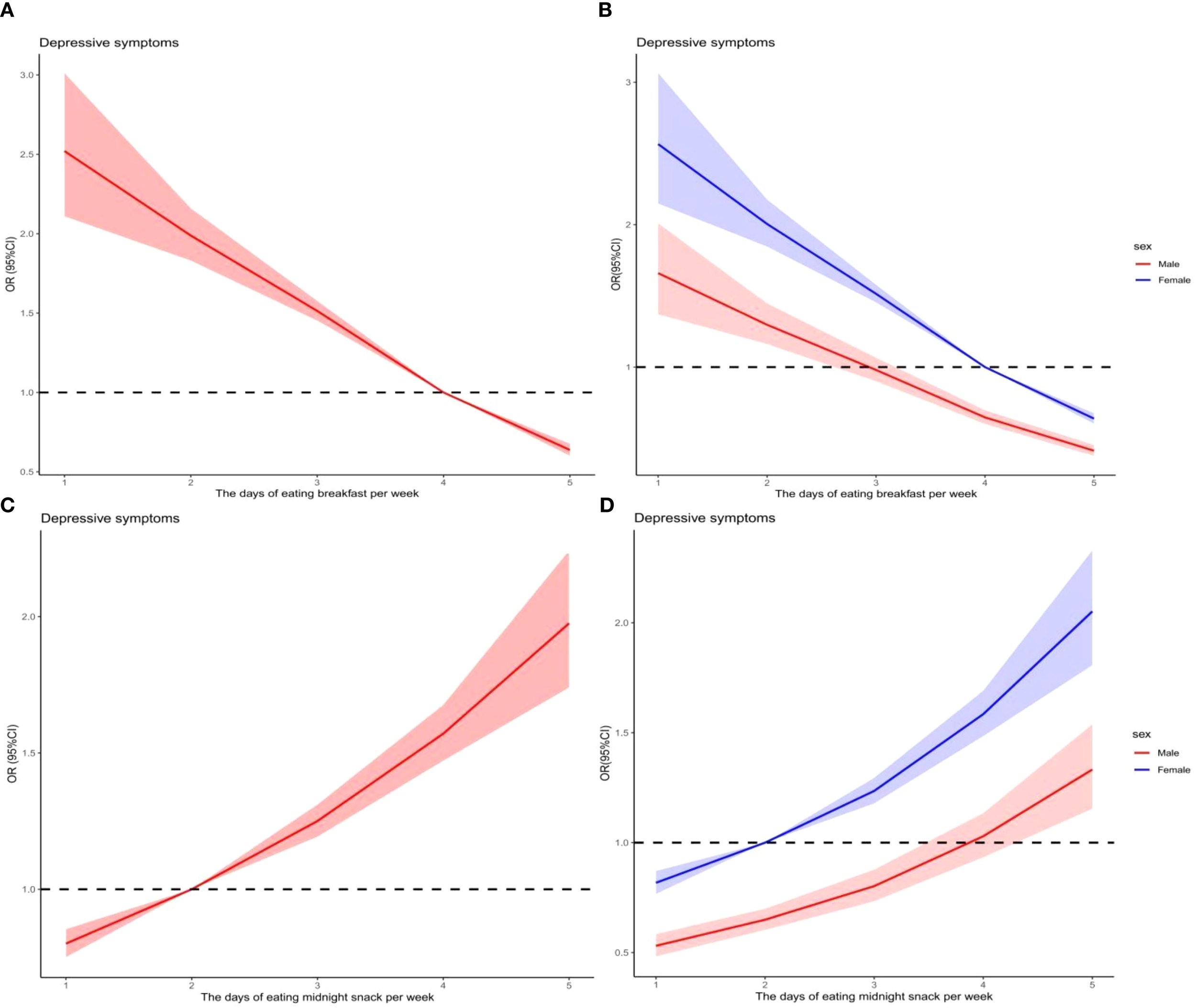
Association of breakfast and midnight snack with depressive symptoms in Yunnan multi-ethnic adolescents.
Discussion
This follow-up study revealed that the prevalence of depressive symptoms among multi-ethnic adolescents in China ranged from 26.3%-37.3%, showing a significant increasing trend. The prevalence found in this study aligns closely with that of adolescents in Eastern (36.2%) (13), as well as Bangladesh (36.6%) (52). However, the prevalence of depressive symptoms among adolescents in this study was higher than that in Northeast China (28.2%) (24) and lower than in India (52.3%) (53). Moreover, the latent growth trajectory analysis indicated that depressive symptom scores among multi-ethnic adolescents in China increased over the follow-up period. These findings are consistent with other studies, which have reported a significant increase in depression prevalence among Chinese adolescents from 2021 to 2023 (54). The results highlight that depressive symptoms among multi-ethnic adolescents in China are at a high level. While Eastern and Central China have seen societal, school, and family attention toward adolescent depression, ethnic adolescents in Western China have not received sufficient attention. Therefore, school-based health promotion programs targeting depression among multi-ethnic adolescents in China should be prioritized on the national agenda.
The reported rate of not eating breakfast for ≥1 d in the past week among Chinese multi-ethnic adolescents was 48.9%-55.5%, which is comparable to the rate in Turkish adolescents (54.1%) (29), higher than that of South Korean adolescents (29.2%) (55), and lower than that of Brazilian adolescents (87%) (56). We indicate that the number of days per week that males and females ate breakfast was negatively correlated with the risk of developing depressive symptoms. Specifically, the risk of depressive symptoms increased when males ate breakfast less than three days per week, and females ate breakfast less than four days per week. These results align with previous studies. For instance, a cross-sectional study found that Turkish adolescents who ate breakfast ≤5 days per week were at a higher risk for depressive and anxiety symptoms, and low breakfast quality was also linked to these mental health issues (29). Studies have shown that skipping breakfast is associated with higher levels of depressive symptoms. Spanish individuals who did not eat breakfast exhibited more depressive symptoms than those who did (28). Among Japanese adolescents, regular breakfast consumption (≥6 days per week) was negatively correlated with depressive symptoms (26, 27). A Chinese study found a similar pattern, with a stronger association observed in younger adolescents (11–15) compared to older ones (16–19) (33). Additionally, research on children in grades 1–9 in Shanghai, China, indicated that adolescents who skipped breakfast had a 2.70 times higher risk of depressive symptoms than those who ate breakfast regularly (45). Few longitudinal studies have examined this relationship. However, a one-year prospective cohort study in China found that compared to adolescents who ate breakfast ≥6 days per week, those who ate breakfast only 2–5 days per week had a significantly higher risk of depressive symptoms (OR = 2.045), with an even greater risk for those eating breakfast ≤1 day per week (OR = 2.722) (32). Similarly, a large-sample prospective study in the United States confirmed a positive association between breakfast and depressive symptoms (57). Moreover, skipping breakfast has been linked to an increased risk of suicidal ideation, planning, and attempts among adolescents in the United States and South Korea (58, 59). Given these findings, promoting consistent breakfast consumption among adolescents is crucial for mental health.
This study found that 71.3%-83.4% of multi-ethnic Chinese adolescents consumed midnight snacks at least once in the past week, a significantly higher rate than that of Bangladeshi (16.6%) (36) and Palestinian (29.7%) adolescents (37). Additionally, our findings indicate a positive correlation between the frequency of midnight snacks consumption and the risk of depressive symptoms in both males and females. The risk of depressive symptoms increased when males consumed midnight snacks more than four days per week and females more than two day per week. This finding aligns with previous research indicating that midnight snacks are associated with a higher risk of depressive symptoms in adolescents (41, 43). Similarly, children and adolescents in grades 1–9 in Shanghai, China who ate before bedtime showed a significantly elevated risk of depressive symptoms (45). Turkish adolescents aged 13–18 who ate after 10 PM were also more likely to experience depressive symptoms (42). Similarly, a longitudinal study in Montreal that followed Canadian adolescents from ages 12 to 17 found that nighttime eating was longitudinally associated with an increased risk of depressive symptoms (OR = 1.75) (35).
Our research data indicate the gender-specific thresholds for skipping breakfast and eating midnight snacks increase the risk of depressive symptoms, the possible explanations include Physiological and social-cultural factors. Meta-analysis shows that the gender difference for diagnoses of depression emerged earlier than previously thought, peaked in adolescence, but then declined and remained stable in adulthood (60). The Social Signal Transduction Theory posits that adolescent females are more sensitive to experiences of social-environmental adversity. Moreover, fluctuations in hormone levels can regulate the sensitivity of females to stress, as well as the structure and function of the brain, and their reactivity, which leads to a higher likelihood of depressive symptoms in adolescent females (61).
In this study, skipping breakfast and eating midnight snacks among multi-ethnic Chinese adolescents were longitudinally associated with depressive symptoms. Several mechanisms may explain this relationship. First, both behaviors negatively impact physical health, which serves as the foundation for mental well-being. Breakfast is a crucial meal of the day, providing essential energy and nutrients that contribute significantly to daily dietary intake. Breakfast typically includes grains, dairy products such as cheese or milk, and eggs. Whole grains are rich in several macronutrients, including magnesium (62); dairy products are excellent sources of Calcium, magnesium and vitamins (such as B2, B12, A), amino acids (such as proline, tyrosine, serine, lysine, valine, and leucine) (63); and eggs provide a high amount of choline (64). These nutrients may contribute positively to mental health. Consistently skipping breakfast can result in nutrient deficiencies, while frequent midnight snacks places excessive strain on the gastrointestinal tract, potentially leading to indigestion. Additionally, frequent midnight snacks can contribute to obesity, increasing the likelihood of adolescents entering a sub-health state. Research indicates that sub-health serves as a mediating factor in the relationship between dietary behaviors and depressive symptoms (65). Second, both skipping breakfast and eating midnight snacks can negatively impact sleep quality and even contribute to insomnia (33, 66). Previous studies have suggested that night eating symptoms have a direct effect on the chronotype differences and insomnia and an indirect effect on disordered eating attitudes, by increasing insomnia scores (67). Midnight snacks keeps the stomach full, disrupts sleep, and is a significant predictor of depressive symptoms (68). Third, irregular eating habits, such as skipping breakfast and frequently eating midnight snacks, can disrupt the biological clock and lead to endocrine imbalances, which may further contribute to depressive symptoms (69). Fourth, most midnight snacks consumed by adolescents are ultra-processed foods that are easy to access and are significant predictors of depressive symptoms (70). Nighttime eating is also linked to food addiction (71). These foods—such as sugar-sweetened beverages, processed meat, sweets, and snacks—are frequently consumed, further increasing the risk of depressive symptoms in adolescents (23).
The data collected in this study were during the COVID-19 pandemic. Therefore, the depressive symptoms of adolescents might have been affected by COVID-19. A nationwide, multicenter, cross-sectional study in China revealed that the COVID-19 pandemic has exacerbated anxiety, depression, and sleep problems among people (72). Moreover, social isolation and reduced outdoor activities have emerged as significant risk factors for anxiety, depression, and insomnia (73). However, we have taken into account the impact of the COVID-19 pandemic on the participants’ depressive symptoms, and in the multivariate analysis model, we have adjusted for the COVID-19 pandemic.
Adolescent depression is a pressing global public health concern (74). It not only impacts adolescents’ well-being but also affects their long-term health and that of future generations (60). From a life-cycle perspective, as well as in terms of treatment effectiveness and health economics, preventing adolescent depression is crucial (1). The link between adolescent dietary behaviors and depressive symptoms has garnered increasing attention (75). Research suggests that dietary interventions can effectively prevent depression or serve as an alternative or adjunct therapy (76). Therefore, the habits of skipping breakfast and eating midnight snacks among multi-ethnic adolescents in China require attention. Effective health education and behavioral interventions should be implemented to correct these unhealthy eating patterns. Adolescents should be encouraged to eat a balanced breakfast regularly, maintain consistent meal timing, and develop healthy dietary habits to support mental well-being.
Emerging evidence suggests a bidirectional relationship between dietary behaviors and depressive symptoms among adolescents. Specifically, depressive symptoms may adversely influence eating behaviors, leading to poorer nutritional choices (77). Empirical research supports this association, demonstrating a significant link between depression and uncontrolled eating behaviors (β = 0.61) (78). Consistent with these findings, a Brazilian study involving college students revealed that elevated depressive symptom scores were correlated with increased consumption of hyperpalatable foods, indicating a preference for energy-dense, nutrient-poor diets (79). Further corroborating this trend, an Indian longitudinal study observed that adolescents with depressive symptoms exhibited a higher propensity for unhealthy dietary practices, subsequently elevating their risk of weight gain (80). We will further explore the association of depressive symptoms with breakfast and midnight snacks in China multi-ethnic adolescents.
This study has several strengths. First, it explored the longitudinal relationship between breakfast and midnight snacks behaviors and depressive symptoms among multi-ethnic adolescents in China, reducing the risk of spurious correlations often found in cross-sectional studies. Our research findings hold practical value for developing intervention strategies aimed at modifying unhealthy dietary behaviors among multi-ethnic adolescents in Yunnan Province, fostering healthy eating habits, and promoting psychological well-being. Second, this is the first study to examine the breakfast and midnight snacks habits of multi-ethnic adolescents in Yunnan, China, and their impact on depressive symptoms, addressing a gap in existing research on this population.
This study has some limitations. First, self-reported questionnaires used to assess dietary behaviors and depressive symptoms may introduce recall bias or social desirability bias, particularly among adolescents. throughout the study, we implemented several strategies to mitigate such biases. Second, the study focuses only on the frequency of breakfast and midnight snacks consumption while ignoring critical factors like the nutritional content of breakfast and the type of midnight snacks, limiting the interpretation of whether associations stem from quantity or quality, which may limit the precision of the analysis. Third, although the study adjusted for confounders such as demographics and lifestyle factors, it omitted other relevant variables (e.g., family dietary habits, peer influence, specific nutrient deficiencies), which may leave residual confounding. Fourth, this study has a limited sample size and was conducted only in specific regions of Yunnan Province, which may not fully represent all Yunnan. Consequently, the generalizability and application of the findings are constrained.
Conclusion
In conclusion, our longitudinal data indicate that skipping breakfast and eating midnight snacks are significant predictors of depressive symptoms among multi-ethnic adolescents in China. These findings underscore the importance of implementing school-based health education and behavioral interventions. By guiding students to adopt healthy dietary habits—such as eating breakfast regularly and avoiding midnight snacks—depressive symptoms can be prevented and improved, ultimately promoting better health among multi-ethnic adolescents in China.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was approved by the Ethics Committee of School of Medicine, Kunming University (approval number: 20210222). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
HX: Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft. GZ: Data curation, Writing – review & editing. ZL: Investigation, Writing – review & editing. XX: Investigation, Writing – review & editing. DH: Investigation, Writing – review & editing. JY: Investigation, Writing – review & editing. JJ: Data curation, Writing – review & editing. XZ: Data curation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was supported by the National Natural Science Foundation of China (82160622), the Young Talents Special Project of “Xingdian Talent Support Plan” in Yunnan Province (XDYC-QNRC-2022-0289) and Yunnan Fundamental Research Projects (202501AT070481).
Acknowledgments
We would like to thank the participants of the behavior and sub-health study in Yunnan adolescents (BSSYA).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
ThaparAEyreOPatelVBrentD. Depression in young people. Lancet. (2022) 400:617–31. doi: 10.1016/S0140-6736(22)01012-1
2
NotaMHCNicolasSO'LearyOFNolanYM. Outrunning a bad diet: Interactions between exercise and a Western-style diet for adolescent mental health, metabolism and microbes. Neurosci Biobehav Rev. (2023) 149:105147. doi: 10.1016/j.neubiorev.2023.105147
3
ErayŞTekcanDBaranY. More anxious or more shy? Examining the social anxiety levels of adolescents with primary enuresis nocturna: a controlled study. J Pediatr Urol. (2019) 15:341–3. doi: 10.1016/j.jpurol.2019.04.002
4
MalhiGSMannJJ. Depression. Lancet. (2018) 392:2299–312. doi: 10.1016/S0140-6736(18)31948-2
5
SeniorMPierceMTaxiarchiVPGargSEdgeDNewlove-DelgadoTet al. 5-year mental health outcomes for children and adolescents presenting with psychiatric symptoms to general practitioners in England: a retrospective cohort study. Lancet Psychiatry. (2024) 11:274–84. doi: 10.1016/S2215-0366(24)00038-5
6
ReangsingCPunsuwunSSchneiderJK. Effects of mindfulness interventions on depressive symptoms in adolescents: A meta-analysis. Int J Nurs Stud. (2021) 115:103848. doi: 10.1016/j.ijnurstu.2020.103848
7
LiuJLiuYMaWTongYZhengJ. Temporal and spatial trend analysis of all-cause depression burden based on Global Burden of Disease (GBD) 2019 study. Sci Rep. (2024) 14:12346. doi: 10.1038/s41598-024-62381-9
8
ShoreySNgEDWongCHJ. Global prevalence of depression and elevated depressive symptoms among adolescents: A systematic review and meta-analysis. Br J Clin Psychol. (2022) 61:287–305. doi: 10.1111/bjc.12333
9
XiangAHMartinezMPChowTCarterSANegriffSVelasquezBet al. Depression and anxiety among US children and young adults. JAMA Netw Open. (2024) 7:e2436906. doi: 10.1001/jamanetworkopen.2024.36906
10
KonigLSchroderRHamerTSuhrR. Depression and health literacy among adolescents and adults in Germany: findings from two representative samples. Front Psychol. (2024) 15:1494333. doi: 10.3389/fpsyg.2024.1494333
11
RandhawaSSMarcenesWStansfeldSABernabeE. Depressive symptoms and traumatic dental injuries among adolescents. Dent Traumatol. (2020) 36:192–7. doi: 10.1111/edt.12524
12
KhanAAhmedRBurtonNW. Prevalence and correlates of depressive symptoms in secondary school children in Dhaka city, Bangladesh. Ethn Health. (2020) 25:34–46. doi: 10.1080/13557858.2017.1398313
13
YangRTanSAbdukerimaGLuTChenCSongLet al. Combined effect of the smartphone addiction and physical activity on the depressive symptoms in secondary school students: a cross sectional study in Shanghai, China. Front Psychiatry. (2024) 15:1473752. doi: 10.3389/fpsyt.2024.1473752
14
SteareTLewisGLangeKLewisG. The association between academic achievement goals and adolescent depressive symptoms: a prospective cohort study in Australia. Lancet Child Adolesc Health. (2024) 8:413–21. doi: 10.1016/S2352-4642(24)00051-8
15
ReckAJKoganSM. Family stress and rural african-american adolescents’ Depressive symptoms. J Adolesc Health. (2021) 69:1006–12. doi: 10.1016/j.jadohealth.2021.05.005
16
CohenALangJJPrinceSAColleyRCTremblayMSChaputJet al. Are adolescents who do physical activity with their parents more active and mentally healthier? Health Rep. (2025) 36:19–33. doi: 10.25318/82-003-x202500100002-eng
17
Pastor-CisnerosRLopez-GilJFCarlJAdsuarJCMendoza-MunozM. Exploring the associations of perceived physical literacy with depression, anxiety, and stress among Spanish adolescents. Complement Ther Clin Pract. (2025) 59:101948. doi: 10.1016/j.ctcp.2025.101948
18
VelazquezBPetrescoSPereiraRBuchweitzCManfroPHCayeAet al. Physical activity and depressive symptoms among adolescents in a school-based sample. Braz J Psychiatry. (2022) 44:313–6. doi: 10.1590/1516-4446-2021-2235
19
Jimenez-LopezEMesasAEVisier-AlfonsoMEPascual-MorenaCMartinez-VizcainoVHerrera-GutierrezEet al. Adherence to the Mediterranean diet and depressive, anxiety, and stress symptoms in Spanish adolescents: results from the EHDLA study. Eur Child Adolesc Psychiatry. (2024) 33:2637–46. doi: 10.1007/s00787-023-02351-0
20
Faisal-CuryALeiteMAEscuderMMLLevyRBPeresMFT. The relationship between ultra-processed food consumption and internalising symptoms among adolescents from Sao Paulo city, Southeast Brazil. Public Health Nutr. (2022) 25:2498–506. doi: 10.1017/S1368980021004195
21
ChopraCMandalikaSKingerN. Does diet play a role in the prevention and management of depression among adolescents? A narrative review. Nutr Health. (2021) 27:243–63. doi: 10.1177/0260106020980532
22
KhannaPChattuVKAeriBT. Nutritional aspects of depression in adolescents - A systematic review. Int J Prev Med. (2019) 10:42. doi: 10.4103/ijpvm.IJPVM_400_18
23
MalmirHMahdaviFSEjtahedHKazemianEChaharrahiAMohammadian KhonsariNet al. Junk food consumption and psychological distress in children and adolescents: A systematic review and meta-analysis. Nutr Neurosci. (2023) 26:807–27. doi: 10.1080/1028415X.2022.2094856
24
CaoRGaoTRenHHuYQinZLiangLet al. Unique and cumulative effects of lifestyle-related behaviors on depressive symptoms among Chinese adolescents. Int J Soc Psychiatry. (2022) 68:354–64. doi: 10.1177/0020764021996739
25
ZahediHDjalaliniaSSadeghiOZare GariziFAsayeshHPayabMet al. Breakfast consumption and mental health: a systematic review and meta-analysis of observational studies. Nutr Neurosci. (2022) 25:1250–64. doi: 10.1080/1028415X.2020.1853411
26
YamaguchiSKawasakiYOuraAKimuraSHoriiMWatanabeSet al. Differential associations of sports participation with self-rated health and depressive symptoms among Japanese adolescents. Cureus. (2023) 15:e43776. doi: 10.7759/cureus.43776
27
TanakaMHashimotoK. Impact of consuming green and yellow vegetables on the depressive symptoms of junior and senior high school students in Japan. PloS One. (2019) 14:e211323. doi: 10.1371/journal.pone.0211323
28
Ferrer-CascalesRSanchez-SanSegundoMRuiz-RobledilloNAlbaladejo-BlazquezNLaguna-PerezAZaragoza-MartiAet al. Eat or skip breakfast? The important role of breakfast quality for health-related quality of life, stress and depression in spanish adolescents. Int J Environ Res Public Health. (2018) 15:1781. doi: 10.3390/ijerph15081781
29
GurbuzMBayramHMKabayelNTurkerZSSahinSIcerSet al. Association between breakfast consumption, breakfast quality, mental health and quality of life in Turkish adolescents: A high school-based cross-sectional study. Nutr Bull. (2024) 49:157–67. doi: 10.1111/nbu.12668
30
YaoLLiangKHuangLXiaoJZhouKChenSet al. Longitudinal associations between healthy eating habits, resilience, insomnia, and internet addiction in chinese college students: A cross-lagged panel analysis. Nutrients. (2024) 16:2470. doi: 10.3390/nu16152470
31
LiangKChenSChiX. Care their diet and mind: association between eating habits and mental health in chinese left-behind children. Nutrients. (2022) 14:524. doi: 10.3390/nu14030524
32
RenZCaoJChengPShiDCaoBYangGet al. Association between breakfast consumption and depressive symptoms among chinese college students: A cross-sectional and prospective cohort study. Int J Environ Res Public Health. (2020) 17:1571. doi: 10.3390/ijerph17051571
33
LiSLiXWangJJiangDZhangYLouWet al. Associations between insufficient sleep, skipping breakfast and depressive symptoms in children and adolescents: A school-based cross-sectional study in China. Prev Med. (2024) 184:107978. doi: 10.1016/j.ypmed.2024.107978
34
HeJHuangFYanJWuWCaiZFanXet al. Prevalence, demographic correlates, and association with psychological distress of night eating syndrome among Chinese college students. Psychol Health Med. (2018) 23:578–84. doi: 10.1080/13548506.2017.1400669
35
GuentchevaIDugasENHanusaikNDrapeauVSylvestreMO'LoughlinJet al. Depression symptoms and night eating in young adulthood. Eat Weight Disord. (2020) 25:1593–600. doi: 10.1007/s40519-019-00796-4
36
SahrinSBannaMHAHamiduzzamanMGbordzoeNIDisuTRAkterSet al. Night eating syndrome among university students in Bangladesh: investigation of prevalence and associated factors. Brain Behav. (2024) 14:e70118. doi: 10.1002/brb3.70118
37
HamdanMBadrasawiMZidanSThawabtehRMohtasebRArqoubKAet al. Night eating syndrome is associated with mental health issues among palestinian undergraduate students-cross sectional study. J Eat Disord. (2023) 11:1. doi: 10.1186/s40337-022-00727-2
38
LiXAoYHuangGZhangXWangLLiYet al. Association between eating at night and skipping breakfast with anxiety symptoms among freshman in colleges in Yunnan Province. Chin J Sch Health. (2023) 44:274–7. doi: 10.16835/j.cnki.1000-9817.2023.02.026
39
Sinclair-McbrideKColeDA. Prospective relations between overeating, loss of control eating, binge eating, and depressive symptoms in a school-based sample of adolescents. J Abnorm Child Psychol. (2017) 45:693–703. doi: 10.1007/s10802-016-0186-0
40
HazzardVMTelkeSESimoneMAndersonLMLarsonNINeumark-SztainerDet al. Intuitive eating longitudinally predicts better psychological health and lower use of disordered eating behaviors: findings from EAT 2010-2018. Eat Weight Disord. (2021) 26:287–94. doi: 10.1007/s40519-020-00852-4
41
LepleyTSchwagerZKhalidZ. Identification and management of night eating syndrome in the adolescent and young adult population. Prim Care Companion CNS Disord. (2022) 24:21r03062. doi: 10.4088/PCC.21r03062
42
TuncaySSarmanA. Late-night eating and inactivity: Links to depression and suicide risk in adolescents living in Turkey. J Child Adolesc Psychiatr Nurs. (2024) 37:e12474. doi: 10.1111/jcap.12474
43
RunfolaCDAllisonKCHardyKKLockJPeeblesR. Prevalence and clinical significance of night eating syndrome in university students. J Adolesc Health. (2014) 55:41–8. doi: 10.1016/j.jadohealth.2013.11.012
44
FischerSMeyerAHHermannETuchAMunschS. Night eating syndrome in young adults: delineation from other eating disorders and clinical significance. Psychiatry Res. (2012) 200:494–501. doi: 10.1016/j.psychres.2012.07.028
45
LiHLuZZhangEZhangJCuiSTakahashiMet al. Meal timing and depression among chinese children and adolescents: cross-sectional study. JMIR Public Health Surveill. (2024) 10:e54275. doi: 10.2196/54275
46
XuHZhangMYangCFuYYangJYangWet al. Fast food and anxiety symptoms of Chinese multi-ethnic adolescents: The moderating role of regulatory emotional self-efficacy. J Affect Disord. (2025) 374:160–70. doi: 10.1016/j.jad.2025.01.036
47
SammAVarnikAToodingLSisaskMKolvesKvon KnorringAet al. Children’s Depression Inventory in Estonia. Single items and factor structure by age and gender. Eur Child Adolesc Psychiatry. (2008) 17:162–70. doi: 10.1007/s00787-007-0650-z
48
GomezRVanceAGomezA. Children’s Depression Inventory: invariance across children and adolescents with and without depressive disorders. Psychol Assess. (2012) 24:1–10. doi: 10.1037/a0024966
49
WangLFengZYangGYangYWangKDaiQet al. Depressive symptoms among children and adolescents in western China: An epidemiological survey of prevalence and correlates. Psychiatry Res. (2016) 246:267–74. doi: 10.1016/j.psychres.2016.09.050
50
HongXLiJLiangYWangZXuF. Reliability and validity of the Chinese version of Children’ s Depression Inventory. Chin J Sch Health. (2012) 33:1182–5. doi: 10.16835/j.cnki.1000-9817.2012.10.011
51
XuHWangJYangJYangWZhangMFuYet al. Association between latent classes of dietary patterns and depressive symptoms among first-grade students from multi-ethnic middle schools in Yunnan Province. Chin J Sch Health. (2024) 45:168–72. doi: 10.16835/j.cnki.1000-9817.2024049
52
AnjumAHossainSSikderTUddinMERahimDA. Investigating the prevalence of and factors associated with depressive symptoms among urban and semi-urban school adolescents in Bangladesh: a pilot study. Int Health. (2022) 14:354–62. doi: 10.1093/inthealth/ihz092
53
GuptaSDasSDasMBanerjeeSNeogiRMukherjeeSet al. Prevalence and correlates of depression, anxiety, and stress among high school students in a block of Hooghly district, West Bengal: Across-sectional study. J Educ Health Promot. (2023) 12:345. doi: 10.4103/jehp.jehp_1769_22
54
DuXWuHYalikunSLiJJiaJDuanTet al. Trajectories of Chinese adolescent depression before and after COVID-19: A cross-temporal meta-analysis with segmented regression. J Affect Disord. (2024) 373:333–44. doi: 10.1016/j.jad.2024.12.094
55
LeeJYBanDKimHKimSYKimJMShinISet al. Sociodemographic and clinical factors associated with breakfast skipping among high school students. Nutr Diet. (2021) 78:442–8. doi: 10.1111/1747-0080.12642
56
GarcezMRde CastroMACésarCLGGoldbaumMFisbergRM. A chrononutrition perspective of diet quality and eating behaviors of Brazilian adolescents in associated with sleep duration. Chronobiol Int. (2021) 38:387–99. doi: 10.1080/07420528.2020.1851704
57
GongWFongDYWangMLamTChungTWHoSet al. Skipping breakfast and eating breakfast away from home were prospectively associated with emotional and behavioral problems in 115, 217 chinese adolescents. J Epidemiol. (2022) 32:551–8. doi: 10.2188/jea.JE20210081
58
LiuBPFangHJJiaCX. The serial mediation of the association between breakfast skipping and suicidality by weight status and depressive symptoms: findings from the national youth risk behavior surveys of the United States. Nutrients. (2022) 14:956. doi: 10.3390/nu14050956
59
ParkHLeeK. Association between breakfast consumption and suicidal attempts in adolescents. Psychol Res Behav Manag. (2022) 15:2529–41. doi: 10.2147/PRBM.S380192
60
SalkRHHydeJSAbramsonLY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol Bull. (2017) 143:783–822. doi: 10.1037/bul0000102
61
SlavichGMSacherJ. Stress, sex hormones, inflammation, and major depressive disorder: Extending Social Signal Transduction Theory of Depression to account for sex differences in mood disorders. Psychopharmacol (Berl). (2019) 236:3063–79. doi: 10.1007/s00213-019-05326-9
62
Anjom-ShoaeJSadeghiOHassanzadeh KeshteliAAfsharHEsmaillzadehAAdibiPet al. The association between dietary intake of magnesium and psychiatric disorders among Iranian adults: a cross-sectional study. Br J Nutr. (2018) 120:693–702. doi: 10.1017/S0007114518001782
63
Gorska-WarsewiczHRejmanKLaskowskiWCzeczotkoM. Milk and dairy products and their nutritional contribution to the average polish diet. Nutrients. (2019) 11:1771. doi: 10.3390/nu11081771
64
RileyCARenshawPF. Brain choline in major depression: a review of the literature. Psychiatry ResNeuroimaging. (2018) 271:142–53. doi: 10.1016/j.pscychresns.2017.11.009
65
XuHYangZLiuDYuCZhaoYYangJet al. Mediating effect of physical sub-health in the association of sugar-sweetened beverages consumption with depressive symptoms in Chinese college students: A structural equation model. J Affect Disord. (2023) 342:157–65. doi: 10.1016/j.jad.2023.09.020
66
BeigrezaeiSMazidiMDaviesIGSalehi-AbargoueiAGhayour-MobarhanMKhayyatzadehSSet al. The association between dietary behaviors and insomnia among adolescent girls in Iran. Sleep Health. (2022) 8:195–9. doi: 10.1016/j.sleh.2021.12.002
67
KandegerAEgilmezUSayinAASelviY. The relationship between night eating symptoms and disordered eating attitudes via insomnia and chronotype differences. Psychiatry Res. (2018) 268:354–7. doi: 10.1016/j.psychres.2018.08.003
68
ChenSJQueJChanNYShiLLiSXChanJWYet al. Effectiveness of app-based cognitive behavioral therapy for insomnia on preventing major depressive disorder in youth with insomnia and subclinical depression: A randomized clinical trial. PloS Med. (2025) 22:e1004510. doi: 10.1371/journal.pmed.1004510
69
QuYLiTXieYTaoSYangYZouLet al. Association of chronotype, social jetlag, sleep duration and depressive symptoms in Chinese college students. J Affect Disord. (2023) 320:735–41. doi: 10.1016/j.jad.2022.10.014
70
Reales-MorenoMToniniPEscorihuelaRMSolanasMFernández-BarrésSRomagueraDet al. Ultra-processed foods and drinks consumption is associated with psychosocial functioning in adolescents. Nutrients. (2022) 14:4831. doi: 10.3390/nu14224831
71
NolanLJGeliebterA. Food addiction” is associated with night eating severity. Appetite. (2016) 98:89–94. doi: 10.1016/j.appet.2015.12.025
72
WangSZhangYDingWMengYHuHLiuZet al. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: A nationwide multicenter cross-sectional study. Eur Psychiatry. (2020) 63:e77. doi: 10.1192/j.eurpsy.2020.78
73
WangSZhangYGuanYDingWMengYHuHet al. A nationwide evaluation of the prevalence of and risk factors associated with anxiety, depression and insomnia symptoms during the return-to-work period of coronavirus disease 2019 in China. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:2275–86. doi: 10.1007/s00127-021-02046-4
74
DienerMJGottdienerWHKeefeJRLevyKNMidgleyN. Treatment of depression in children and adolescents. Lancet Psychiatry. (2021) 8:97. doi: 10.1016/S2215-0366(20)30518-6
75
MeaselleJRSticeEHogansenJM. Developmental trajectories of co-occurring depressive, eating, antisocial, and substance abuse problems in female adolescents. J Abnorm Psychol. (2006) 115:524–38. doi: 10.1037/0021-843X.115.3.524
76
BearTLKDalzielJECoadJRoyNCButtsCAGopalPKet al. The role of the gut microbiota in dietary interventions for depression and anxiety. Adv Nutr. (2020) 11:890–907. doi: 10.1093/advances/nmaa016
77
RodgersRFPaxtonSJChabrolH. Depression as a moderator of sociocultural influences on eating disorder symptoms in adolescent females and males. J Youth Adolesc. (2010) 39:393–402. doi: 10.1007/s10964-009-9431-y
78
MutwalliHHerleMKanCKeelerJLStevesCTreasureJet al. Lifetime history of depression and eating behaviours: a co-twin control study of the TwinsUK registry. J Affect Disord. (2025) 382:264–73. doi: 10.1016/j.jad.2025.04.111
79
Verly-MiguelMLopesCDSFreitasJVGarciaMCMarquesMCParavidinoVBet al. Depression, anxiety and change in eating habits during the COVID-19 pandemic in Brazilian university students. PloS One. (2025) 20:e0326856. doi: 10.1371/journal.pone.0326856
80
MoitraPMadanJShaikhNI. Eating habits and sleep patterns of adolescents with depression symptoms in Mumbai, India. Matern Child Nutr. (2020) 16:e12998. doi: 10.1111/mcn.12998
Summary
Keywords
adolescent, depressive symptoms, breakfast, midnight snacks, longitudinal study
Citation
Xu H, Zhang G, Liu Z, Xue X, Hu D, Yang J, Jia J and Zhang X (2025) Longitudinal association of breakfast and midnight snacks with depressive symptoms in China multi-ethnic adolescents. Front. Psychiatry 16:1651630. doi: 10.3389/fpsyt.2025.1651630
Received
22 June 2025
Accepted
09 September 2025
Published
09 October 2025
Volume
16 - 2025
Edited by
Tomoya Hirota, University of California, San Francisco, United States
Reviewed by
Chen Hong, First Affiliated Hospital of Wenzhou Medical University, China
Shu Wang, Capital Medical University, China
Updates
Copyright
© 2025 Xu, Zhang, Liu, Xue, Hu, Yang, Jia and Zhang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Honglv Xu, x___hl@126.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.