Abstract
Introduction:
Children of parents with mental illness face heightened risks of adverse health, social, and educational outcomes. Yet, families affected by parental mental illness are often overlooked in mental health and social care systems. Identifying parents in psychiatric care enables targeted interventions to mitigate intergenerational risks. This study aims to estimate the prevalence and describe the sociodemographic characteristics of patients in psychiatric hospital services in Denmark who are parents, with particular focus on those living with minor children, to inform future preventive support strategies.
Methods:
Using Danish nationwide register data from 2020-2022, we identified individuals with at least one adult psychiatric hospital contact. Parenthood was determined through linkage to the Civil Registration System, including children aged 0–29 years. Diagnoses, socioeconomic status, and living arrangements were described, and associations between parental characteristics and co-residence with a minor child were described using crude relative risks.
Results:
Among 164,223 patients in psychiatric hospital services, 24% had at least one minor child (aged 0–17 years), and 8% had only adult children (aged 18–29 years). The most common diagnoses among parents with minor children were neurotic and stress-related disorders (31%) and affective disorders (25%). Geographic and diagnostic variation in the prevalence of parents was observed, and parent patients generally had higher socioeconomic status than non-parent patients. Among parent patients, those with a partner, higher education, and labor market affiliation were more likely to live with their child.
Conclusions:
One in four Danish psychiatric hospital patients have minor children, highlighting the need for systematic identification and tailored services. The findings underscore the importance of integrating family-focused approaches within psychiatric care to reduce the long-term burden on children and break cycles of mental illness.
1 Introduction
Children of parents with mental illness face a wide range of adverse health and social risks. These include poorer mental health and early onset of mental disorders (1–4), poorer physical health (5, 6), negative social outcomes such as lower graduation rates (7) and higher likelihood of conviction for crime (8). Further, parental mental illness may impact family dynamics and access to social resources leading to fewer protective or buffering factors than in families without parental mental illness (9).
In Denmark, research has shown that approximately two in five children aged 0–16 years have parents with a mental health condition, and 13% have parents who received treatment in adult psychiatric hospital service (10). Despite this high prevalence, these children are often overlooked in both mental health care systems and in social systems in the surrounding society. While some parents with mental illness experience periods of remission or recovery and thus can provide a stable and supportive home environment, many still face challenges that can affect their ability to care for their children, particularly during episodes of symptoms and active illness. Identifying families in need of support provides a window of opportunity for early intervention with tremendous preventive potential for these children.
Psychiatric hospitals (i.e., both wards and outpatient clinics) present a key opportunity for the detection of children in need of support while their parents are in treatment. A systematic, top-management prioritized approach is essential for effective identification and subsequent support. Moreover, it is acknowledged that the social environment is critical to patient recovery and thus knowing more about the importance of parenting for the patient, and the impact of family dynamics for parents as patients in psychiatry is of most importance. Few studies have investigated the effect of involving the family in the treatment of psychiatric disorders. However, Reupert et al. found that the role of being a parent is an important motivation for the recovery of parents in psychiatric care, that is often overlooked in clinical measures (11).
Still, data on the prevalence of parents among patients in psychiatric hospital services is lacking but needed to inform clinicians, service providers, and decision-makers. Accurate estimates support the development of targeted interventions, improve clinical identification and guide resource allocation. However, many countries lack comprehensive data, limiting researchers’ ability to provide evidence-based recommendations. Addressing this gap by analyzing prevalence rates and associated risk and resilience factors is crucial for strengthening mental health services and ensuring appropriate support for affected families (12).
One way to describe the prevalence of parental mental illness is a population-level “top-down” approach, where the prevalence of children living with parents who have a mental illness is estimated (12). Population-based cohort studies using this approach have reported that 12.8% of children in Denmark (10) and 11% in Sweden (13) live with a parent receiving hospital-based psychiatric care. However, such population-level prevalence is not useful in clinical everyday life. Another approach to estimating prevalence is the “bottom-up” approach that determines the number of patients in the psychiatric settings who are parents (12). This method provides a prevalence that is helpful in a clinical context.
While studies from Australia, Norway, and Sweden provide some prevalence data, research on this issue in Denmark remains limited. In Australia, a study across New South Wales reported that 25-28% of current patients in psychiatric hospital services were parents, based on annual one-day census data from 2008-2011 (14). A large Australian study spanning 2003–2011 showed that approximately 20% of patients in psychiatric hospital services were parents (15), and a Czech study reported a prevalence of 35% of patients with severe mental illness were parents, including those with adult offspring (16). A Swedish study from 2001 reported that 36% of adult patients in psychiatric hospital services had children under 18 years of age (17), while a Norwegian study from 2013 found a 36% prevalence among psychiatric outpatients (18).
However, audit-based studies such as these (14, 17, 18) are often restricted to specific regions and modest sample sizes, limiting their generalizability. Additionally, patients with mental illness may avoid disclosing their parenting status in mental health services due to fear of child protection involvement (18), while also concealing their mental health challenges in social services to avoid stigmatization. This dual concern can lead to under-identification and inadequate support. Further, data collection is resource-intensive, which may contribute to incomplete and unrepresentative findings.
The provision of preventive family interventions including psychoeducation with parents within adult mental health settings has demonstrated positive outcomes for children (19–21) as well as improving family psychosocial functioning (21). Thus, effective interventions do exist, but prior identification is needed to be able to intervene. A review highlights the importance of early detection and preventive interventions in clinical settings. It recommends that mental health professionals place greater emphasis on prevention and early identification in daily practice to reduce the burden on children as relatives, and over time, to lower the incidence of mental illness or change expected trajectories to less debilitating outcomes (22). Unlike Norway and Sweden, where laws are made to ensure focus on children as relatives, Denmark lacks regulations mandating the identification of children whose parents suffer from a mental illness. While the Danish Child’s Law requires all public professionals, including mental health staff, to report any concerns regarding children’s welfare (23), interventions and guidelines for how to serve this vulnerable group are inconsistent across and within Danish regions (24). Despite recommendations from the Danish Health Authority to prioritize children of parents with a mental illness (25), a systematic, nationwide effort has yet to be implemented.
To address the knowledge gap, this study aims to estimate the prevalence of parenthood among patients treated in Danish psychiatric hospitals. Specifically, we focus on patients with minor children and describe their sociodemographic characteristics, including partnership status, education, with particular attention to those living with their children. Additionally, we explore geographic variation in the prevalence of parenthood across regions and municipalities to inform future, locally tailored, preventive and family-focused support strategies.
2 Materials and methods
2.1 Study design and settings
This study utilized the Danish nationwide registers. Denmark’s tax-funded healthcare system provides free access to healthcare, including mental health services, with a few private outpatient clinics also in operation (26). The healthcare administration is managed by five regions, each with varying population sizes. The psychiatry specialty is organized separately from other medical specialties. Responsibility for social care and related interventions falls to the 98 municipalities.
The regional mental health services are structured into two main sectors: the primary healthcare sector, which include general practitioners (GPs) and practicing psychiatrists, and the secondary healthcare sector, which encompasses psychiatric hospitals and related outpatient services. It is estimated that GPs manage 80–90% of minor psychiatric disorders, such as mild to moderate depression and non-comorbid anxiety conditions. GPs also serve as ‘gatekeepers’, referring patients to either practicing psychiatrists or to treatment within the hospital sector, and they perform medical controls (26). The secondary sector provides a range of services, including inpatient and outpatient facilities, as well as community psychiatry, with variations between regions likely influenced by demographic differences, prioritization, and funding.
Addiction services such as treatment of alcohol or drug addiction are organized and provided by the municipalities. We were not able to include information on parents in treatment for addiction.
2.2 Data sources
From the Danish Civil Registration System (27) information on the individuals’ children, age, sex, geography, and cohabitation were obtained.
Information from the psychiatric hospital services were provided from the National Patient Register (28) and included information on inpatient and outpatient contacts and diagnoses that used the International Classification of Diseases, Tenth Revision (ICD-10) codes.
The parents’ highest level of completed education was extracted from the Population Education Registry (29), and The Income Statistics Register provided information on socioeconomic classification (30).
Data linkages were achieved via the personal identity number that is assigned to all Danish residents at birth or when individuals become residents. The register keepers at Statistics Denmark carried out the data collection and register linkage. All the data were deidentified before the researchers received access.
2.3 Study population
We included all individuals who had contact with adult psychiatric hospitals and related outpatient services between January 1st, 2020, and December 31st, 2022. Their children were identified if they were aged 0–29 years in the study period. Individuals with contact to the geriatric psychiatry or child- and adolescent psychiatry were excluded from the study.
2.4 Variables
All variables were measured in the calendar year of the patient’s first contact with psychiatric hospital services during the study period (2020–2022), except ‘living with child’, geographical region and municipality that was based on residence of the patient in the beginning of the study period.
Based on the primary ICD-10 diagnosis from the patient record, the diagnoses were grouped according to the main DF-category, see Box 1.
Box 1 ICD-10 diagnostic categories used in the study.
| ICD-10 code | ICD-10 diagnosis |
| DF00-DF09 | Organic, including symptomatic, mental disorders |
| DF10-DF19 | Mental and behavioral disorders due to psychoactive substance use |
| DF20-DF29 | Schizophrenia, schizotypal and delusional disorders |
| DF30-DF39 | Mood [affective] disorders |
| DF40-DF48 | Neurotic, stress-related and somatoform disorders |
| DF50-DF59 | Behavioral syndromes associated with physiological disturbances and physical factors |
| DF60-DF69 | Disorders of adult personality and behavior |
| DF70-DF79 | Intellectual disability |
| DF80-DF89 | Disorders of psychological development |
| DF90-DF98 | Behavioral and emotional disorders with onset usually occurring in childhood and adolescence |
| DF99 | Unspecified mental disorder |
| DZ00-DZ99 | Factors influencing health status and contact with health services |
In cases of patients with more than one primary diagnosis during the three years, the earliest diagnosis in the ICD-hierarchy, was included. Patients were categorized as outpatients if they had solely outpatient contacts during the study period. If they had at least one inpatient contact, they were categorized as inpatients.
The variable ‘lives with child’ describes whether the patient shared the same address as the child. For patients with both minor and adult children, cohabitation status was determined based solely on living with af minor child. These patients were classified as having minor children. If the child partly resides with but does not have the same address as the parent who is a patient, it is categorized as not living with child.
Educational status was based on the levels of the International Standard Classification of Education (ISCED 2011) (31) and grouped into three categories according to the parent’s highest educational attainment. These were level 0–2 if they had 10 years of mandatory education or below, level 3–4 for 10–14 years of education, such as high school, and level 5–8 for more than 14 years of education, such as a bachelor’s degree. Socioeconomic position was dichotomized into “affiliated” and “not affiliated” with labor marked or education. Individuals were classified as affiliated if they were employed, enrolled in education, or receiving temporary benefits such as unemployment or sickness benefits. Individuals receiving disability pension, cash benefits, or other forms of long-term public support were classified as not affiliated (30).
2.5 Data analyses
We calculated the prevalence of patients in adult psychiatric hospital services who had at least one child aged 0–29 years, and presented descriptive sociodemographic characteristics stratified by parental status. Separate prevalence estimates were provided for patients with minor children (aged 0–17 years) and patients with only adult children (aged 18–29 years). Patients with both minor and adult children were classified under the minor children group.
To describe the association between parental characteristics and co-residence with minor children, we estimated relative risks (RRs) and 95% confidence intervals. This analysis was restricted to patients identified as parents of at least one minor child, comparing those who were living with their child to those who were not. RRs were calculated as simple ratios of proportions within each characteristic group (e.g., females vs. males). We did not adjust for covariates in these analyses since the aim of the study solely was descriptive.
3 Results
We identified 164,223 individuals in total with at least one contact with the adult psychiatric hospitals and related outpatient services between 2020-2022 (Table 1). Of these, 24% had at least one child aged 0–17 years (minor children) and 8% had only child(ren) aged 18–29 years. In the following, we focus on the group of patients with minor children.
Table 1
| Overall population | Patients with at least minor child | Patients with solely child(ren) aged 18-29 years | Patients with no children | |
|---|---|---|---|---|
| N=164,223 | N=39,153 | N=13,859 | N=111,211 | |
| Prevalence of parenthood | 24% | 8% | ||
| Age | ||||
| Mean (SD) | 39.9 (17.3) | 39.1 (8.48) | 54.2 (6.18) | 38.4 (19.6) |
| Median [Min, Max] | 35.5 [18.0, 105] | 38.7 [18.0, 79.8] | 54.2 [34.7, 88.5] | 29.7 [18.0, 105] |
| Sex | ||||
| Male | 73087 (44.5%) | 15790 (40.3%) | 5597 (40.4%) | 51700 (46.5%) |
| Female | 91136 (55.5%) | 23363 (59.7%) | 8262 (59.6%) | 59511 (53.5%) |
| Type of contact | ||||
| Outpatient | 72723 (44.3%) | 17544 (44.8%) | 5347 (38.6%) | 49832 (44.8%) |
| Inpatient | 91500 (55.7%) | 21609 (55.2%) | 8512 (61.4%) | 61379 (55.2%) |
| Diagnosis | ||||
| DF00–09 Organic, including symptomatic, mental disorders |
7305 (4.4%) | 339 (0.9%) | 495 (3.6%) | 6471 (5.8%) |
| DF10–19 Mental and behavioral disorders due to psychoactive substance use |
13075 (8.0%) | 2777 (7.1%) | 1659 (12.0%) | 8639 (7.8%) |
| DF20–29 Schizophrenia, schizotypal and delusional disorders |
28630 (17.4%) | 3622 (9.3%) | 1742 (12.6%) | 23266 (20.9%) |
| DF30–39 Mood [affective] disorders | 36149 (22.0%) | 9648 (24.6%) | 4124 (29.8%) | 22377 (20.1%) |
| DF40–48 Neurotic, stress-related and somatoform disorders |
36140 (22.0%) | 12301 (31.4%) | 3517 (25.4%) | 20322 (18.3%) |
| DF50–59 Behavioral syndromes associated with physiological disturbances and physical factors |
4187 (2.5%) | 936 (2.4%) | 240 (1.7%) | 3011 (2.7%) |
| DF60–69 Disorders of adult personality and behavior | 9917 (6.0%) | 3109 (7.9%) | 503 (3.6%) | 6305 (5.7%) |
| DF70–79 Intellectual disability | 2779 (1.7%) | 77 (0.2%) | 11 (0.1%) | 2691 (2.4%) |
| DF80–89 Disorders of psychological development | 2881 (1.8%) | 258 (0.7%) | 35 (0.3%) | 2588 (2.3%) |
| DF90–98 Behavioral and emotional disorders with onset usually occurring in childhood and adolescence |
6250 (3.8%) | 1928 (4.9%) | 185 (1.3%) | 4137 (3.7%) |
| DF99 Unspecified mental disorder | 1107 (0.7%) | 259 (0.7%) | 60 (0.4%) | 788 (0.7%) |
| DZ00–99 Factors influencing health status and contact with health services |
15803 (9.6%) | 3899 (10.0%) | 1288 (9.3%) | 10616 (9.5%) |
| Living with the child | ||||
| No | 139408 (84.9%) | 16510 (42.2%) | 11687 (84.3%) | 111211 (100%) |
| Yes | 24815 (15.1%) | 22643 (57.8%) | 2172 (15.7%) | 0 (0%) |
| Region | ||||
| North | 13934 (8.5%) | 3355 (8.6%) | 1144 (8.3%) | 9435 (8.5%) |
| Central | 33256 (20.3%) | 7647 (19.5%) | 2563 (18.5%) | 23046 (20.7%) |
| Southern | 40797 (24.8%) | 10973 (28.0%) | 3824 (27.6%) | 26000 (23.4%) |
| Capital | 53724 (32.7%) | 11855 (30.3%) | 4229 (30.5%) | 37640 (33.8%) |
| Zealand | 22512 (13.7%) | 5323 (13.6%) | 2099 (15.1%) | 15090 (13.6%) |
| Educational status | ||||
| <10 years (ISCED 0-2) | 68695 (41.8%) | 13173 (33.6%) | 4414 (31.8%) | 51108 (46.0%) |
| 10–14 years (ISCED 3-4) | 58371 (35.5%) | 13968 (35.7%) | 5700 (41.1%) | 38703 (34.8%) |
| >14 years (ISCED 5-8) | 32295 (19.7%) | 11080 (28.3%) | 3297 (23.8%) | 17918 (16.1%) |
| Missing | 4862 (3.0%) | 932 (2.4%) | 448 (3.2%) | 3482 (3.1%) |
| Number of unique children | ||||
| n | 106458 | 82597 | 23861 | 0 |
| Socioeconomic position | ||||
| Affiliated to labor marked or education | 84216 (51.3%) | 21653 (55.3%) | 6305 (45.5%) | 56258 (50.6%) |
| No affiliation to labor marked or education | 57585 (35.1%) | 12099 (30.9%) | 6369 (46.0%) | 39117 (35.2%) |
| Missing | 22422 (13.7%) | 5401 (13.8%) | 1185 (8.6%) | 15836 (14.2%) |
| Living with partner | ||||
| No | 101003 (61.5%) | 16899 (43.2%) | 7848 (56.6%) | 76256 (68.6%) |
| Yes | 58154 (35.4%) | 21533 (55.0%) | 5749 (41.5%) | 30872 (27.8%) |
| Missing | 5066 (3.1%) | 721 (1.8%) | 262 (1.9%) | 4083 (3.7%) |
Baseline characteristics.
3.1 Characteristics of patients with minor children
Among the 39,153 identified patients with children, a total of 82,597 minor children (unique individuals) were found (Table 1). Among these patients, three out of five (59%) lived with at least one child. The majority of patients with children were female (60%), while 40% were male, a distribution comparable to that of patients without children under 30 years of age (54% female and 47% male) (Table 1). The meadian age of patients with minor children was 38.7 years (min-max 18.0-79.8), compared with 29.7 years (min-max 18.0-105) among patients without children.
The most common diagnoses among patients with minor children were DF40–48 nervous and stress-related conditions (31%) followed by DF30–39 affective disorders (25%). A diagnosis within the schizophrenia spectrum (DF20-29) was present in 9% of patients with minor children compared with 21% of the patients without children.
One third of patients with children received public welfare (31%), compared with 36% of patients without children. More patients with children (55%) lived with a partner than patients without children (28%). A greater proportion of patients with children had completed more than 14 years of education (28%) compared with patients without children (16%).
Figure 1 shows the prevalence of parenthood among patients across diagnostic categories including the share of at least one inpatient contact versus solely outpatient contacts. The prevalence of parenthood to minor children varied between diagnoses, ranging from 3% among patients with DF7 intellectual disability as the main diagnosis, to 13% in patients with DF2 schizophrenia spectrum disorders, 27% in patients with DF3 affective disorders, and 31% in patients with DF90–98 behavioral and emotional disorders and DF6 personality disorders, and 34% in patients with DF4 neurotic and stress-related disorders.
Figure 1
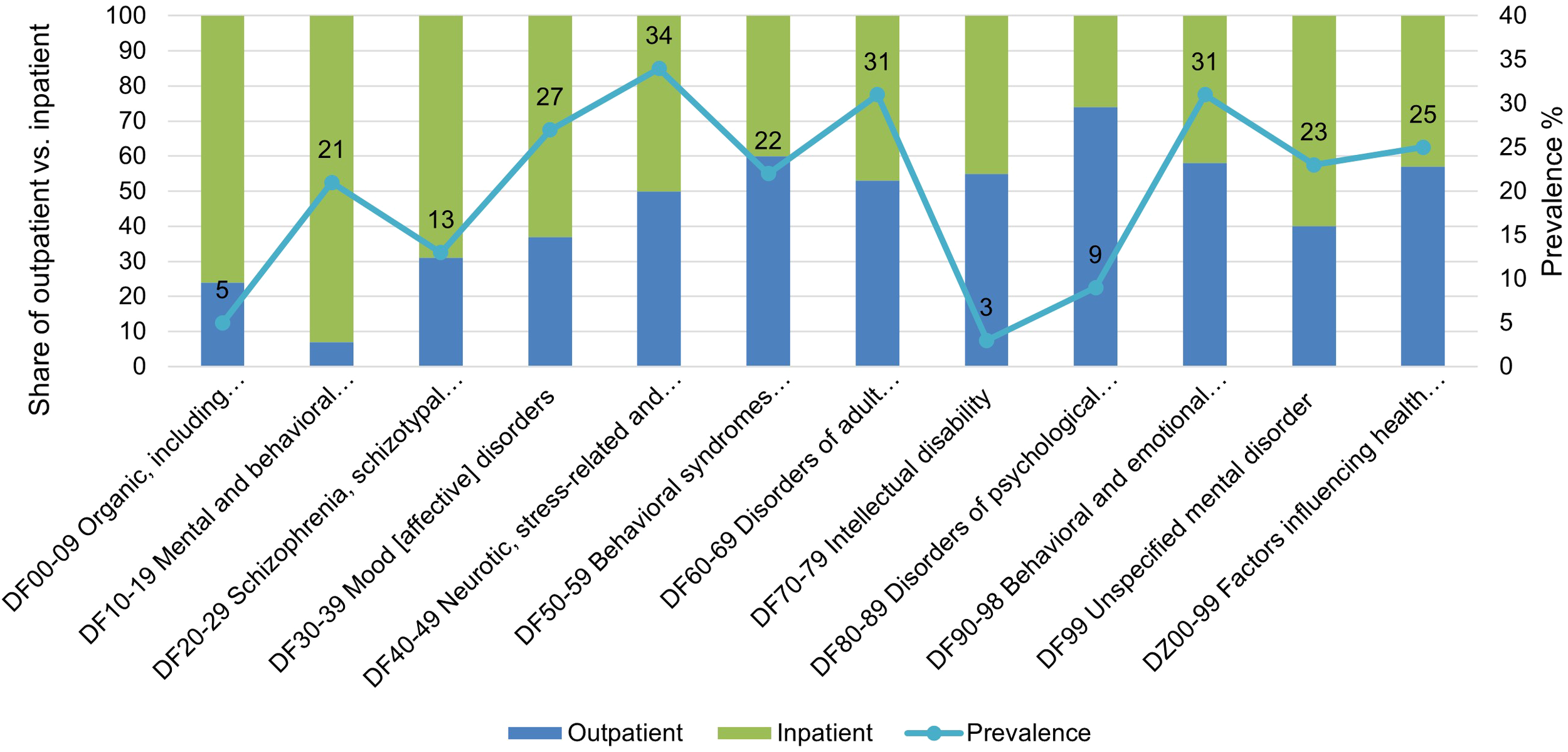
Prevalence of parent patients with minor children.
Figure 2 summarizes the characteristics of patients who are parents to minor children. Among these patients, females were more likely to live with their child compared with males [RR 1.63 (95% CI 1.63-1.73)]. The parent patients living with a partner were twice as likely to live with their child compared to parent patients not living with a partner (RR 2.02 (95% CI 2.02-2.14). Compared to those with affective disorders (DF3), parent patients diagnosed with DF4, DF5, and DF6 had similar likelihood of living with their child. In contrast, those with DF0, DF1, DF2, DF7, DF9, or DZ were significantly less likely to live with their child (RR range: 0.35-0.89).
Figure 2
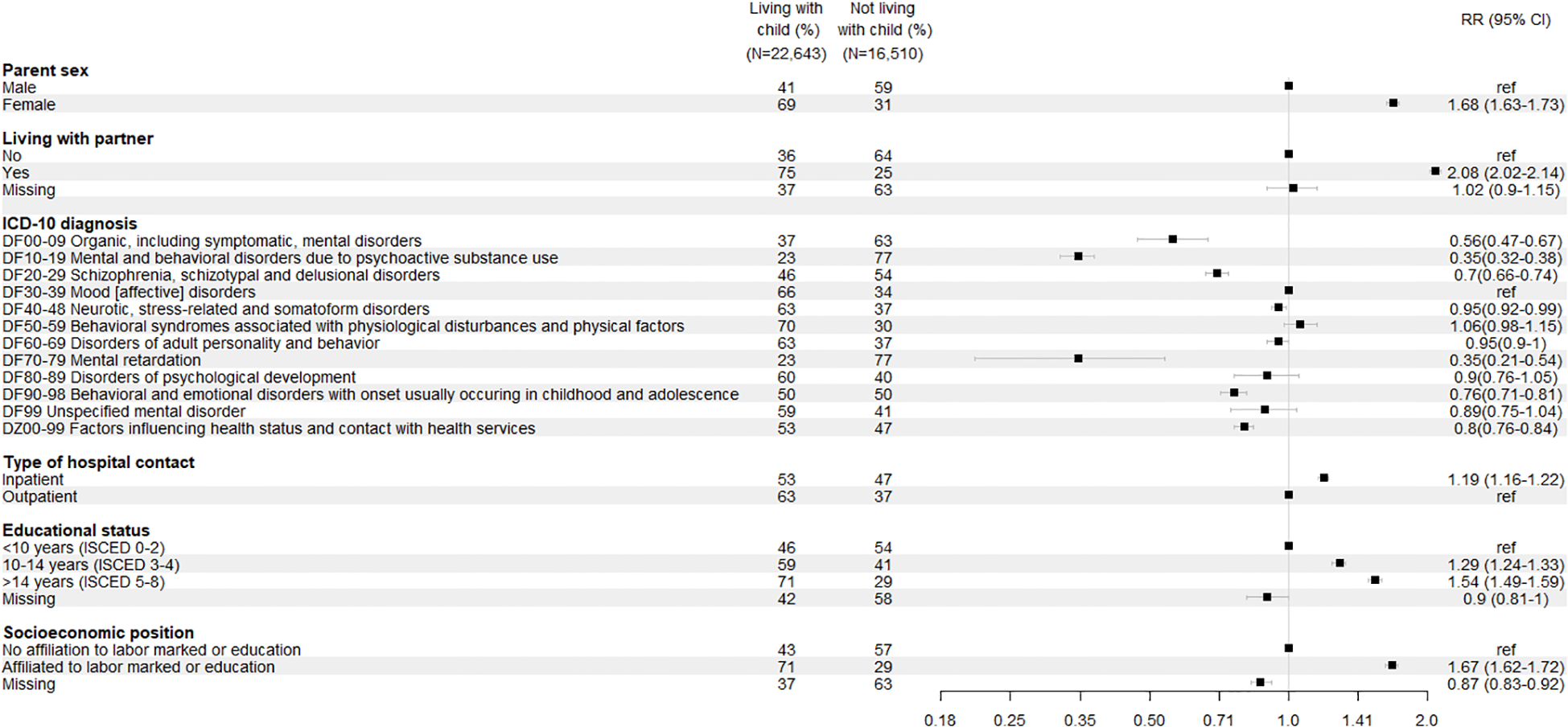
Characteristics of parent patients with minor children.
A similar pattern was observed regarding educational attainment and self-sufficiency. Parent patients with a long education (ISCED 5-8) or being affiliated to labor market or education were one and a half times more likely to live with their child compared to those with a shorter education (ISCED 0-2) or with no affiliation to the labor market or education.
Approximately half (55%) of the patients who are also parents had been admitted to inpatient psychiatric care during the study period, while the other (45%) half had only outpatient psychiatric contacts (Table 1). Parent patients with inpatients contacts were 19% more likely to live with their child compared to those with solely outpatient contacts [RR 1.19 (95% CI 1.16-1.22)].
Figure 3 illustrates the geographical variation in the prevalence of parenthood among patients in psychiatric hospital services, ranging from below 20% to above 30% across municipalities and within larger cities. Also, variation between the different psychiatric departments ranging from zero to 100%, Supplementary Figure S1.
Figure 3
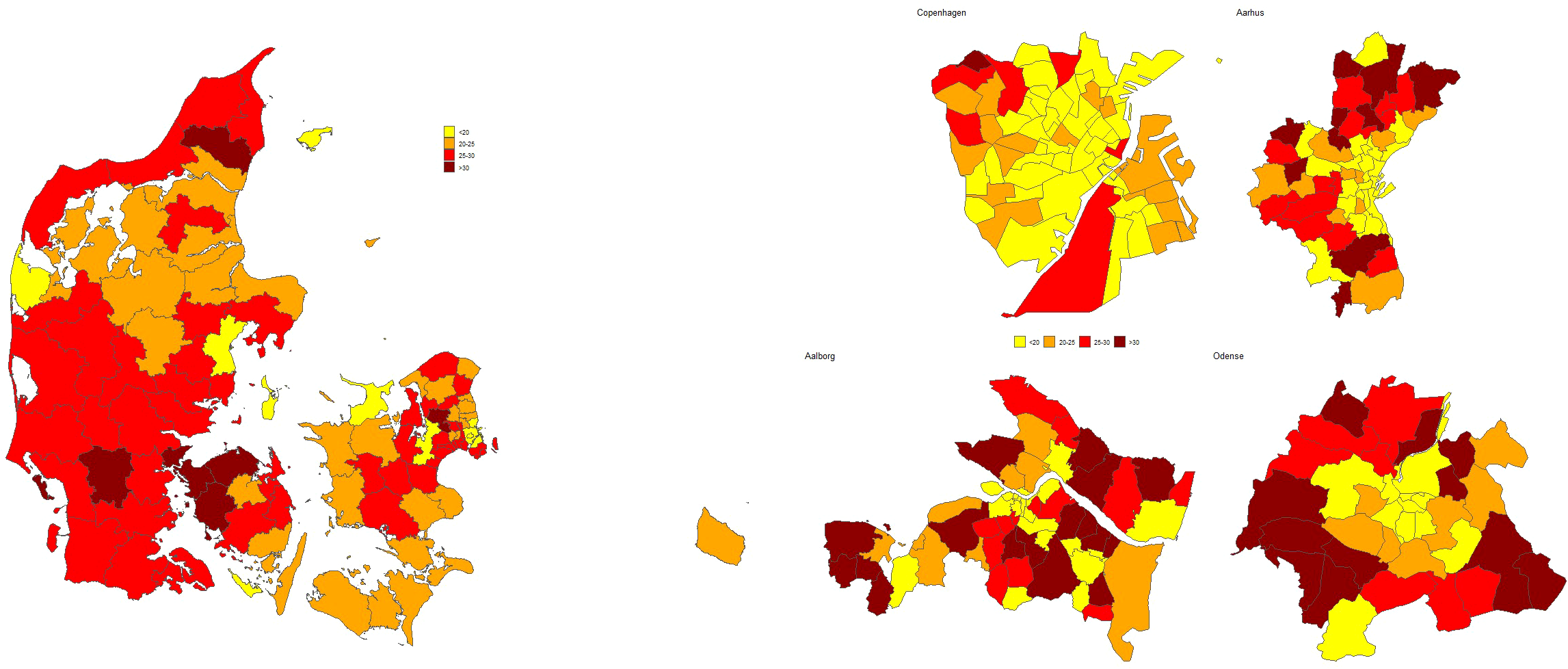
Geographical variation of prevalence of parent patients with minor children.
4 Discussion
This Danish nationwide study identified that 24.2% of the patients being treated in psychiatric hospitals in Denmark between 2020–2022 had minor children, corresponding to 82,597 unique children below age 18. These findings align with prior research, including Ruud et al. who reported a prevalence of 36% among outpatients (18), and Maybery et al, who found a prevalence of 20.4% in a whole-of-service study (15). Additionally, a recent Czech study reported that 34.6% of inpatients with severe mental illness were parents (16), which is comparable to our findings, considering that two-thirds of the offspring in that study were adults (16). Our study found that 8.5% of patients were parents to solely children aged 18–29 years, leading to an overall prevalence of 32.7% for patients with children aged 0–29 years.
The most common diagnoses among parent patients to minor children were DF40-48 (neurotic, stress-related, and somatoform disorders) (31%) and DF30-39 (affective disorders) (25%), whereas DF2 schizophrenia and other psychotic disorders were seen in only 9% of the parent patients. This contrasts with findings from Howe et al., who reported that 21.5-35.2% of the parents had psychotic disorders (14), and Ruud et al., who reported a prevalence of 13% for schizophrenia and related disorders (18). The variation in diagnostic distribution may stem from differences in psychiatric service structure, treatment approaches, and hospitalization thresholds across countries. Our study’s inclusion of both inpatient and outpatient populations further distinguishes our findings from those in previous research, which often focused on a narrower patient group.
A novel contribution of this study is the identification of substantial geographic variation in the prevalence of parenthood among patient within psychiatric hospital services across Denmark ranging from below 20% to above 30% in different municipalities. This geographic disparity has not previously been studied using a comprehensive nationwide approach but is consistent with earlier research on the prevalence of children with parents with mental disorders in Denmark (10).
In general, parent patients had a higher socioeconomic position (longer educational attainment and self-sufficient/not receiving public benefits) than patients without children. Socioeconomic advantage also characterized the parent patients living with their children compared with parent patients not living with their children. However, it is important to keep in mind that children of parents with mental illness have markedly higher risks of broad socioeconomic adversity than other children (13).
Furthermore, the observed differences in diagnoses and sociodemographic characteristics between patients with and without minor children likely reflect, at least in part, a selection effect. Individuals with greater social and functional stability—such as those in partnerships or with higher education—may be more likely to become parent in the first place. Conversely, patients with conditions such as schizophrenia, intellectual disability, or organic mental disorders may be less likely to have children due to both biological and social factors. This has been demonstrated in prior research showing markedly lower fertility rates among individuals with a range of mental disorders (32). This selective parenthood must be considered when interpreting our findings, as some differences may stem from this initial selection rather from the impacts of parenthood itself.
The relative risks presented in this are based on unadjusted comparisons. Our primary aim was descriptive, focusing on mapping the prevalence and characteristics of parents in psychiatric hospital services. The unadjusted estimates should therefore be interpreted as indicative patterns within the population rather than causal effects.
4.1 Strengths
This study has several strengths. By using the national Danish registers, which are considered valid regarding accuracy and completeness (33), we were able to include all patients with at least one contact with the public psychiatric hospitals in Denmark in 2020-2022. To our knowledge, this is the first nationwide study to systematically assess parenthood among patients in psychiatric hospital services in Denmark. Additionally, the study included both inpatient and outpatient populations, capturing a more complete picture, inclusive diagnoses, and sociodemographic characteristics, of parental prevalence being treated in psychiatric hospitals, which are absent or underreported in other studies (16–18).
4.2 Limitations
Despite these strengths, some limitations must be acknowledged. The study only identified parenthood among patients who sought mental health care within the hospital system, thereby excluding parents with mental illness who did not receive hospital-based treatment during the study period, but who may have received treatment from, for example, private practitioning psychiatrists. Additionally, we were unable to include data on parents receiving addiction treatment through municipal services.
In this study, patients with more than one diagnosis were assigned a primary diagnosis based on the highest-ranked diagnosis according to the ICD-10 hierarchy. While this approach is commonly used in register-based studies to ensure consistency and comparability across large populations, it may not fully reflect the complexity of clinical presentations or comorbidities. In some cases, a less severe but more functionally impairing disorder may be more relevant to a patient’s parental role. As such, this method could potentially underrepresent the prevalence of parenthood within diagnostic categories associated with milder disorders, and should be interpreted with this limitation in mind.
Additionally, variable such as co-residence with children and socioeconomic position were measured at the time of the patient’s first contact with psychiatric hospital services during the study period. These characteristics may change over time, an in particular, the onset or progression of severe mental illness may lead to disruptions in family structure and employment status. As such, our findings should be interpreted in the light of the fact that these variables reflect the situation at first contact and may not represent long-term or post-diagnosis trajectories.
4.3 Implications
The high prevalence of patients in the psychiatric hospital system who are also parents calls for attention from both policy makers and health professionals. Given the well-documented adverse consequences of parental mental illness on children (1–7), it is critical to implement structured screening and support strategies within psychiatric services. A recent Danish report highlights that overcoming identified barriers requires structured action-oriented guidelines, sustained leadership attention, and practical tolls such as reminders and visual patient information (34). The significant variation in prevalence across diagnostic groups and geographic regions suggests that tailored, location-specific interventions may be necessary to effectively reach and support these families.
Ensuring that children of patients within psychiatric hospital services receive adequate support requires clear guidelines and policies. While countries such as Norway and Sweden have legal frameworks mandating the identification of children of patients being treated in psychiatric hospitals, Denmark lacks a similar systematic approach. The Danish Child’s Law obligates professionals to report concerns regarding children’s well-being, but specific guidelines for proactively identifying and supporting these children remain inconsistent. This study underscores the need for a national strategy to bridge this gap and provide comprehensive, evidence-based interventions for patients in psychiatric hospital services who are parents, as well as their children.
Further, our findings highlight the influence of social determinants on mental health, reinforcing evidence that structural factors shape the life circumstances of patients with mental disorders. Addressing these social determinants through mental health policies could help break intergenerational cycles of disadvantage and improve outcomes for both patients and their children (9).
5 Conclusions
Approximately one in four Danish patients being treated in psychiatric hospitals have minor children. This prevalence varied by diagnosis and geography, underscoring the importance of systematic identification and evidence-based, tailored intervention strategies for these families. Addressing the needs of these families through targeted policies and resource allocation is critical to mitigate the intergenerational impacts of parental mental illness and improve outcomes for both parents and children.
Statements
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The data that support the findings of this study is available from the Statistics Denmark, but restrictions apply to the availability of these data, which were used under licence for the current study, and so are not publicly available. Questions or requests concerning these data are directed to the corresponding author Signe Heuckendorff. Requests to access these datasets should be directed to Signe Heuckendorff, s.heuckendorff@rn.dk.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
SH: Formal analysis, Writing – original draft, Conceptualization, Funding acquisition, Project administration, Methodology, Investigation, Writing – review & editing. RB: Formal analysis, Methodology, Investigation, Writing – review & editing, Data curation, Writing – original draft. JB-W: Writing – original draft, Funding acquisition, Conceptualization, Writing – review & editing. AT: Writing – original draft, Writing – review & editing. AR: Writing – review & editing, Writing – original draft. AM: Writing – original draft, Writing – review & editing. KF: Methodology, Writing – review & editing, Writing – original draft.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. TrygFonden (grant number N/A).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1654760/full#supplementary-material
Supplementary Figure 1Variation of prevalence of parent patients in different psychiatric departments.
References
1
Paananen R Tuulio-Henriksson A Merikukka M Gissler M . Intergenerational transmission of psychiatric disorders: the 1987 Finnish Birth Cohort study. Eur Child Adolesc Psychiatry. (2021) 30:381–9. doi: 10.1007/s00787-020-01524-5
2
Ellersgaard D Jessica Plessen K Richardt Jepsen J Soeborg Spang K Hemager N Klee Burton B et al . Psychopathology in 7-year-old children with familial high risk of developing schizophrenia spectrum psychosis or bipolar disorder – The Danish High Risk and Resilience Study - VIA 7, a population-based cohort study. World Psychiatry. (2018) 17:210–9. doi: 10.1002/wps.20527
3
Gregersen M Søndergaard A Brandt JM Ellersgaard D Rohd SB Hjorthøj C et al . Mental disorders in preadolescent children at familial high-risk of schizophrenia or bipolar disorder – a four-year follow-up study. J Child Psychol Psychiatry. (2022) 63:1046–56. doi: 10.1111/jcpp.13548
4
Uher R Pavlova B Radua J Provenzani U Najafi S Fortea L et al . Transdiagnostic risk of mental disorders in offspring of affected parents: a meta-analysis of family high-risk and registry studies. World Psychiatry. (2023) 22:433–48. doi: 10.1002/wps.21147
5
Heuckendorff S . Health outcomes in children of parents with mental health conditions: Morbidity and use of healthcare services in early childhood. Aalborg University (2021). Aalborg Ø, Denmark: Aalborg University Press. Available online at: https://vbn.aau.dk/en/publications/health-outcomes-in-children-of-parents-with-mental-health-conditi. (Accessed January 21, 2022)
6
Renneberg CK Brund RBK Heuckendorff S Bech BH Fonager K . Children of parents with different severities of mental health conditions have higher risk of somatic morbidity: a Danish nationwide register-based cohort study. BMC Public Health. (2023) 23:810. doi: 10.1186/s12889-023-15714-8
7
Ranning A Laursen T Agerbo E Thorup A Hjorthøj C Jepsen JRM et al . School performance from primary education in the adolescent offspring of parents with schizophrenia and bipolar disorder– a national, register-based study. Psychol Med. (2018) 48:1993–2000. doi: 10.1017/S0033291717003518
8
Rasmussen I Kruse M . Samfundsøkonomiske konsekvenser af at vaere barn af foraeldre med mentale helbredsproblemer. Odense: University of Southern Denmark. (2022). Available online at: https://www.sdu.dk/da/om-sdu/fakulteterne/sundhedsvidenskab/nyheder/foraeldres-mentale-problemer. (Accessed August 13, 2024)
9
Kirkbride JB Anglin DM Colman I Dykxhoorn J Jones PB Patalay P et al . The social determinants of mental health and disorder: evidence, prevention and recommendations. World Psychiatry. (2024) 23:58–90. doi: 10.1002/wps.21160
10
Christesen AMS Knudsen CK Fonager K Johansen MN Heuckendorff S . Prevalence of parental mental health conditions among children aged 0–16 years in Denmark: A nationwide register-based cross-sectional study. Scand J Public Health. (2022) 50:1124–32. doi: 10.1177/14034948211045462
11
Reupert A Maybery D Cox M Scott Stokes E . Place of family in recovery models for those with a mental illness. Int J Ment Health Nurs. (2015) 24:495–506. doi: 10.1111/inm.2015.24.issue-6
12
Maybery D Nicholson J Rupert A . Parental mental illness: Estimating prevalence to inform policy and practice. In: Parental Psychiatric Disorder: Distressed Parents and their Families, 3rd ed. Cambridge, United Kingdom: Cambridge University Press (2015). p. 20–8.
13
Pierce M Abel KM Muwonge J Wicks S Nevriana A Hope H et al . Prevalence of parental mental illness and association with socioeconomic adversity among children in Sweden between 2006 and 2016: a population-based cohort study. Lancet Public Health. (2020) 5:e583–91. doi: 10.1016/S2468-2667(20)30202-4
14
Howe D Batchelor S Bochynska K . Prevalence of parents within an adult mental health service: Census results 2008–2011. Australas Psychiatry. (2012) 20:413–8. doi: 10.1177/1039856212459583
15
Maybery DJ Reupert AE Patrick K Goodyear M Crase L . Prevalence of parental mental illness in Australian families. Psychiatr Bull. (2009) 33:22–6. doi: 10.1192/pb.bp.107.018861
16
Havelková A Havelka D Koros Bartošová K . Prevalence of parenthood among hospitalized adult patients with severe mental illness: a quantitative data analysis. Front Psychiatry. (2024) 15:1386842/full. doi: 10.3389/fpsyt.2024.1386842/full
17
Östman M Eidevall L . Illuminating patients with children up to 18 years of age – A 1-day-inventory study in a psychiatric service. Nord J Psychiatry. (2005) 59:388–92. doi: 10.1080/08039480500330164
18
Ruud T Maybery D Reupert A Weimand B Foster K Grant A et al . Adult mental health outpatients who have minor children: prevalence of parents, referrals of their children, and patient characteristics. Front Psychiatry. (2019) 10:163/full. doi: 10.3389/fpsyt.2019.00163/full
19
Lannes A Bui E Arnaud C Raynaud JP Revet A . Preventive interventions in offspring of parents with mental illness: a systematic review and meta-analysis of randomized controlled trials. Psychol Med. (2021) 51:2321–36. doi: 10.1017/S0033291721003366
20
Siegenthaler E Munder T Egger M . Effect of preventive interventions in mentally ill parents on the mental health of the offspring: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. (2012) 51:8–17.e8. doi: 10.1016/j.jaac.2011.10.018
21
Furlong M McGuinness C Mulligan CM McGarr SL McGilloway S . Family Talk versus usual services in improving child and family psychosocial functioning in families with parental mental illness: a randomised controlled trial and cost analysis. Front Psychiatry. (2024) 15. doi: 10.3389/fpsyt.2024.1287378
22
Arango C Díaz-Caneja CM McGorry PD Rapoport J Sommer IE Vorstman JA et al . Preventive strategies for mental health. Lancet Psychiatry. (2018) 5:591–604. doi: 10.1016/S2215-0366(18)30057-9
23
Retsinformation . Bekendtgørelse af barnets lov - Kapitel 16 Underretning. (2024) Copenhagen: Ministry of Social Affairs and Housing.
24
Psykiatrifonden Børns Vilkår Ole Kirk’s Fond . Opsporing af pårørende børn til patienter i voksenpsykiatrien (2023). Available online at: https://bornsvilkar.dk/wp-content/uploads/2023/10/Spoerg-Mere_okt2023_WEB.pdf. (Accessed August 26, 2024)
25
Sundhedsstyrelsen . Bedre mental sundhed og en styrket indsats til mennesker med psykiske lidelser: Fagligt oplæg til en 10-årsplan [Strengthening mental health care - Recommendations for a 10-year action plan in Denmark]. Copenhagen: Sundhedsstyrelsen (2022). Available online at: https://www.sst.dk/da/udgivelser/2022/Fagligt-oplaeg-til-en-10-aarsplan. (Accessed September 12, 2024)
26
Bauer J Okkels N Munk-Jørgensen P . State of psychiatry in Denmark. Int Rev Psychiatry. (2012) 24:295–300. doi: 10.3109/09540261.2012.692321
27
Pedersen CB . The Danish civil registration system. Scand J Public Health. (2011) 39:22–5. doi: 10.1177/1403494810387965
28
Schmidt M Schmidt SAJ Sandegaard JL Ehrenstein V Pedersen L Sørensen HT . The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. (2015) 7:449. doi: 10.2147/CLEP.S91125
29
Jensen VM Rasmussen AW . Danish education registers. Scand J Public Health. (2011) 39:91–4. doi: 10.1177/1403494810394715
30
Baadsgaard M Quitzau J . Danish registers on personal income and transfer payments. Scand J Public Health. (2011) 39:103–5. doi: 10.1177/1403494811405098
31
United Nation Educational Scientific an Cultural Organisation (UNESCO) . International Standard Classification of Education . Available online at: http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf. (Accessed August 26, 2024)
32
Power RA Kyaga S Uher R MacCabe JH Långström N Landen M et al . Fecundity of patients with schizophrenia, autism, bipolar disorder, depression, anorexia nervosa, or substance abuse vs their unaffected siblings. JAMA Psychiatry. (2013) 70:22. doi: 10.1001/jamapsychiatry.2013.268
33
Schmidt M Pedersen L Sørensen HT . The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. (2014) 29:541–9. doi: 10.1007/s10654-014-9930-3
34
Danish Mental Health Foundation WElearn Center for Family-based Interventions Mental Health Services CR of D . Catch the Children – How Do Children and Adolescents Receive the Necessary Support When Their Mother or Father Has a Mental Illness (2024). Available online at: https://psykiatrifonden.dk/files/media/document/Grib_boernene_rapport_psykiatrifonden_2024.pdf. (Accessed November 6, 2024)
Summary
Keywords
parental mental illness, childhood adversity, mental health services, family interventions, prevalence, health policy
Citation
Heuckendorff S, Brund RBK, Buhl-Wiggers J, Thorup AAE, Ranning A, Müller AD and Fonager K (2025) Prevalence and sociodemographic characteristics of parents among patients treated in adult psychiatric hospitals – a register-based nationwide study. Front. Psychiatry 16:1654760. doi: 10.3389/fpsyt.2025.1654760
Received
26 June 2025
Accepted
18 August 2025
Published
03 September 2025
Volume
16 - 2025
Edited by
Ottar Ness, Norwegian University of Science and Technology, Norway
Reviewed by
Firas Mousatat, Sainte-Anne Hospital Center, France
Yishan Liu, Lund University, Sweden
Updates
Copyright
© 2025 Heuckendorff, Brund, Buhl-Wiggers, Thorup, Ranning, Müller and Fonager.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Signe Heuckendorff, s.heuckendorff@rn.dk
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.