- 1Department of Psychiatry, The Fourth Affiliated Hospital of Anhui Medical University, Hefei, Anhui, China
- 2Department of Psychiatry, School of Mental Health and Psychological Sciences, Anhui Medical University, Hefei, Anhui, China
Background: Suicidal ideation (SI) is common in adolescents with major depressive disorder (MDD). SI not only poses a serious threat to the patient’s life safety, but also significantly hinders the process of psychological recovery and the restoration of social functioning. However, there is still a relative lack of longitudinal studies on the factors influencing SI in adolescents with MDD. Therefore, this study aimed to explore the longitudinal trajectory of SI in adolescents with MDD and to identify the relevant influencing factors.
Methods: This study included 122 adolescents with MDD. At baseline and one-year follow-up, patients were assessed for SI. Based on the assessment results, patients were divided into SI group and non-SI group. In addition, the standardized questions and the Center for Epidemiological Studies Depression scale (CES-D), the Childhood Trauma Questionnaire (CTQ), and the Toronto Alexithymia Scale (TAS-20) were used to evaluate non-suicidal self-injury (NSSI), depressive symptoms, childhood maltreatment (CM), and alexithymia. Logistic stepwise regression analyses were employed to identify factors independently associated with SI in adolescents with MDD.
Results: In adolescents with MDD, the prevalence of SI was 68.0%. At the follow-up period, the prevalence of persistent suicidal ideation (PSI) was 19.7%, and the prevalence of new-onset SI was 20.5%. Regression analyses showed that single-child family (OR = 3.969, 95%CI: 1.227 - 12.839, P = 0.021), TAS-20 score (OR = 1.091, 95%CI: 1.006 - 1.184, P = 0.035), and difficulties identifying feelings (OR = 1.134, 95%CI: 1.000 - 1.287, P = 0.050) were risk factors for PSI. NSSI (OR = 4.552, 95%CI: 1.488 - 13.921, P = 0.008) and positive affect (OR = 1.424, 95%CI: 1.125-1.804, P = 0.003) were risk factors for new-onset SI.
Conclusion: Adolescents with MDD have a high risk of PSI, and new-onset SI should not be ignored. Factors such as single-child family, alexithymia, NSSI, and reduction of positive affect significantly affect the occurrence and persistence of SI. Therefore, early intervention targeting these factors is important to reduce the risk of adolescent suicide and improve mental health outcomes.
1 Introduction
Major depressive disorder (MDD) is a mental illness characterized by significant and persistent low mood, which is particularly common in adolescents (1). A study indicated that the point-in-time prevalence and lifetime prevalence of MDD in global adolescents were 8.0% and 19.0%, respectively (2). MDD not only had a serious impact on the physical and mental health of adolescents, but also significantly increased their risk of suicide (3). Suicidal ideation (SI) is a common psychological phenomenon in adolescents with MDD. It refers to the psychological state in which an individual has the idea of ending their life but has not yet taken any actual action. A cross-sectional study showed that the prevalence of SI in adolescents with MDD was as high as 75.7% (4). This indicates that the prevalence and severity of SI in this group cannot be ignored. However, although cross-sectional studies reveal a high incidence trend of SI, it is difficult to elucidate its longitudinal progression. Therefore, in recent years, scholars both domestically and internationally increasingly focused on the persistent characteristics of SI. They referred to the phenomenon where individuals reported SI at baseline assessment and again at follow-up as persistent suicidal ideation (PSI) (5, 6). A study showed that PSI was a more effective predictor of suicide attempt than single-point-in-time reports of SI (7). A recent data further showed that the probability of a suicide attempt for individuals with PSI was 13.8%, compared to 1.8% among individuals who reported only a single episode of SI (8). In addition, adolescents with PSI were at significantly higher risk of attempting suicide in adulthood (9). Therefore, SI, particularly PSI, serves as an important predictor of future suicide risk in adolescents.
Currently, interventions for SI in patients with MDD were still largely focused on the acute management phase after the onset of symptoms. Although treatments such as modified electroconvulsive therapy (10), subnarcotic doses of esketamine (11, 12), and circadian rhythm modulation (13)could indirectly ameliorate SI through the rapid alleviation of depressive symptoms, particularly in patients with treatment-resistant depression (14), their efficacy for use in preventing the onset of SI in the adolescent population had not been systematically evaluated. Therefore, investigating the potential influencing factors of SI in adolescents with MDD was crucial for early identification, prevention and optimized treatment in this population.
The emergence of SI is a complex psychological process, which involves the interaction of multiple factors, including psychological factors, socio-environmental factors, and deficits in individual coping capacity. Among these factors, the severity of depressive symptoms was found to be the most important predictor of SI, and the two are significantly correlated (15). A longitudinal study further revealed that improvements in depressive symptoms often preceded reduction in SI, suggesting that depressive symptoms may be an important driver of SI (16). It was worth noting that a low level of positive affect might be an independent and important mechanism, especially prominent in SI and behavior among adolescents (17). For example, the absence of positive affect was found to be an independent risk factor for SI, which may be related to an individual’s psychological resilience and emotional regulation ability (18). Further research indicated that the absence of positive affect could more specifically predict the risk of suicide than negative emotions, which was particularly important for the assessment of suicide risk among adolescents (19).
On the other hand, research has shown that childhood maltreatment (CM) was significant risk factors for SI, with emotional abuse having an independent predictive effect on SI (20). CM not only directly increases the risk of SI but also indirectly promotes its development by exacerbating emotional regulation difficulties and depressive symptoms (21). Similarly, alexithymia, as a psychological trait, had a significant positive correlation with SI (22, 23). Specifically, a 12-month prospective follow-up study found that, after controlling for baseline depression levels, changes in alexithymia characteristics were independently associated with the occurrence or reduction of SI (24). Furthermore, an exploratory study based on daily clinical practice indicated that alexithymia is one of the important predictors of SI during the first episode of depressive disorder (25). Further analyses indicates that specific sub-dimensions of alexithymia, such as difficulty in identifying feelings, are more significantly associated with SI. For instance, a cross-sectional study found that patients with SI scored significantly higher on the subscale of difficulty in identifying feelings, suggesting that difficulty in recognizing one’s own emotions may directly increase the risk of suicide (26).
In addition, non-suicidal self-injury (NSSI) is considered one of the important risk factors for SI. It reflects the impulsivity and self-harm tendencies of individuals in response to negative affect (27). A prospective longitudinal study among German adolescents showed that individuals with NSSI behaviors at baseline had a significantly higher risk of developing SI or engaging in suicide attempt two years later, with a two-fold increase (28). Therefore, early and accurate identification and effective intervention of these underlying factors are crucial for preventing suicide. It also provides a key entry point for exploring the persistence of SI.
However, most current studies on SI in adolescents with MDD use cross-sectional designs, which make it difficult to reveal the dynamic process of SI. The aim of this study is to systematically evaluate the dynamic changes of SI in adolescents with MDD through a longitudinal study method, and to explore in depth the influencing factors related to persistent and new-onset SI, thereby providing new longitudinal evidence for the mechanism interpretation of SI and the development of intervention programs.
2 Methods
2.1 Study design and participants
This study employed a prospective research design. From January 2021 to December 2023, we conducted a questionnaire survey in adolescents with MDD who visited the Fourth Affiliated Hospital of Anhui Medical University. The survey was administered at both the baseline assessment and the one-year follow-up. Inclusion criteria were as follows: (1) age between 12 and 18 years; (2) fulfillment of the diagnostic criteria for MDD according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5); (3) no prior treatment or receipt of only conventional antidepressant medication (e.g., SSRIs, SNRIs) before enrollment, with no other interventions, such as electroconvulsive therapy; and (4) ability to understand and complete the entire study process. Exclusion criteria included: (1) current or previous diagnosis of other mental disorders (e.g., schizophrenia, bipolar disorder); (2) comorbid serious infections, autoimmune diseases, or other severe physical illnesses; (3) change in diagnosis after reassessment according to DSM-5 criteria during the follow-up period; and (4) inability to complete the assessment or cooperate with follow-up visits.
To ensure the accuracy of the measurement results, all data collection and scale assessment work were completed by two clinicians who had undergone strict consistency training. Before the subjects underwent each assessment, the assessors gave them detailed explanations to ensure that the subjects could fully understand the meaning of the questions. This study was reviewed and approved by the Ethics Committee of the Fourth Affiliated Hospital of Anhui Medical University (Approval Number: 202009-KYXM-04). Prior to the commencement of the study, detailed information regarding the study procedures was provided to all participants and their legal guardians, who were required to sign written informed consent forms.
2.2 Measuring instruments
2.2.1 Socio-demographic characteristics
A self-designed questionnaire was used to collect socio-demographic information from all enrolled patients, including gender, age, body mass index (BMI), age at onset, duration of illness, single-child family, NSSI and antidepressant use. NSSI was evaluated according to the criteria in DSM-5 (29).
2.2.2 SI
The Beck Suicidal Ideation Scale (BSI) was used to assess the SI of patients in the recent week (30). BSI comprises 19 items and employs a 3-point scoring system. The study used the first five items of this scale to screen patients for SI. If both items 4 and 5 were scored as 0, then SI was considered to be absent; otherwise, SI was considered to be present (31, 32).
2.2.3 Depressive symptoms
In this study, the Center for Epidemiological Studies Depression Scale (CES-D) was employed to assess the depressive symptoms of patients over the past week (33). CES-D is a self-assessment questionnaire comprising 20 items. Each item is rated on a 4-point scale, ranging from “0 = None” to “3 = Almost every day”. The scale is divided into four factors: depressed affect, positive affect, somatic complaints, and interpersonal difficulties (34). The total score ranges from 0 to 60 points, with higher scores indicating more severe depressive symptoms. CES-D demonstrated good reliability and validity among Chinese adolescents (35).
2.2.4 Childhood trauma
In this study, the Childhood Trauma Questionnaire (CTQ) was employed to assess the trauma experienced by the research subjects during their childhood (36). The questionnaire comprises 28 items, each rated on a 5-point scale ranging from “1 = never” to “5 = always”. It covers five dimensions: emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect. The total score of CTQ ranges from 25 to 125 points, with higher scores indicating more severe trauma. The Chinese version of the CTQ has shown good reliability and validity with adolescents in previous studies (37).
2.2.5 Alexithymia
In this study, the Toronto Alexithymia Scale (TAS-20) was employed to assess individuals’ difficulties in recognizing and expressing emotions (38). This questionnaire contains 20 items. Each item is scored on a 5-point scale, ranging from “1 = completely disagree” to “5 = completely agree”, and is divided into three subscales: difficulty identifying feelings, difficulty describing feelings, and externally oriented thinking. The total score range of TAS-20 is 20 to 100 points. The higher the score, the more severe the alexithymia.
2.3 Statistical analysis
All statistical descriptions and analyses were conducted using SPSS 23.0. Continuous variables were presented as mean ± standard deviation (SD) or median (quartiles) [M (P25, P75)]. For data that conformed to the normal distribution, the independent samples t-test was used for intergroup comparisons. If the data did not conform to the normal distribution, the Mann-Whitney U test was employed. Categorical variables were expressed as frequency (%), and the chi-square test was used for comparisons between the two groups. The independent variables included socio-demographic and clinical variables that varied between groups, while the dependent variable was SI. Logistic stepwise regression analyses was performed using the “Forward: LR” method to identify the factors independently associated with SI in adolescents with MDD, and to calculate the corresponding odds ratios (OR) and 95% confidence intervals (CI). Model 1 included socio-demographic variables with intergroup differences and total scale scores with intergroup differences. Model 2 included socio-demographic variables with intergroup differences and subscale scores with intergroup differences. All statistical tests were two-tailed, and a P-value of ≤ 0.05 was considered statistically significant.
3 Results
3.1 Comparison of clinical characteristics between the SI group and the non-SI group in adolescents with MDD
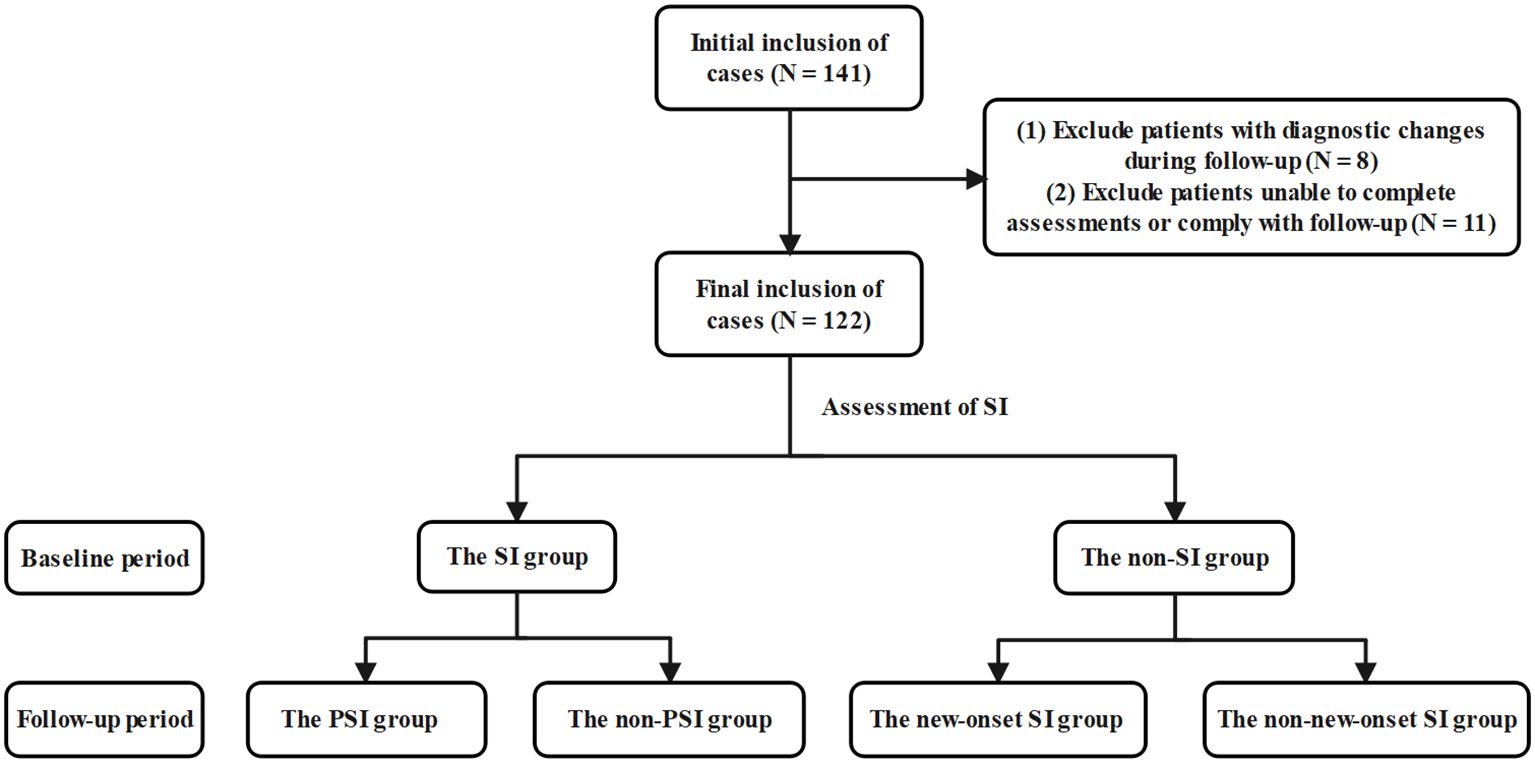
This study included a total of 122 adolescents with MDD (Figure 1), among whom 87 were female (71.3%), with a mean age of 15.61 ± 1.57 years. Regarding SI, a total of 83 patients (68.0%) reported having SI, 24 patients (19.7%) exhibited PSI, and 25 patients (20.5%) experienced new-onset SI.
At the baseline period, the SI group exhibited significantly higher total scores on CTQ, CES-D, and TAS-20 compared with the non-SI group (all P < 0.05). Among them, the SI group had significantly higher scores than the non-SI group on the CTQ scale for emotional abuse (P < 0.001) and emotional neglect (P = 0.009), on the CES-D scale for depressed affect (P = 0.019) and interpersonal difficulties (P = 0.020), and on the TAS-20 scale for difficulty identifying feelings (P = 0.050) and externally oriented thinking (P = 0.021) (Table 1). In summary, the above differences indicated that adolescents with MDD accompanied by SI exhibited more severe experiences of childhood trauma, heightened depressive symptoms, and increased levels of alexithymia.
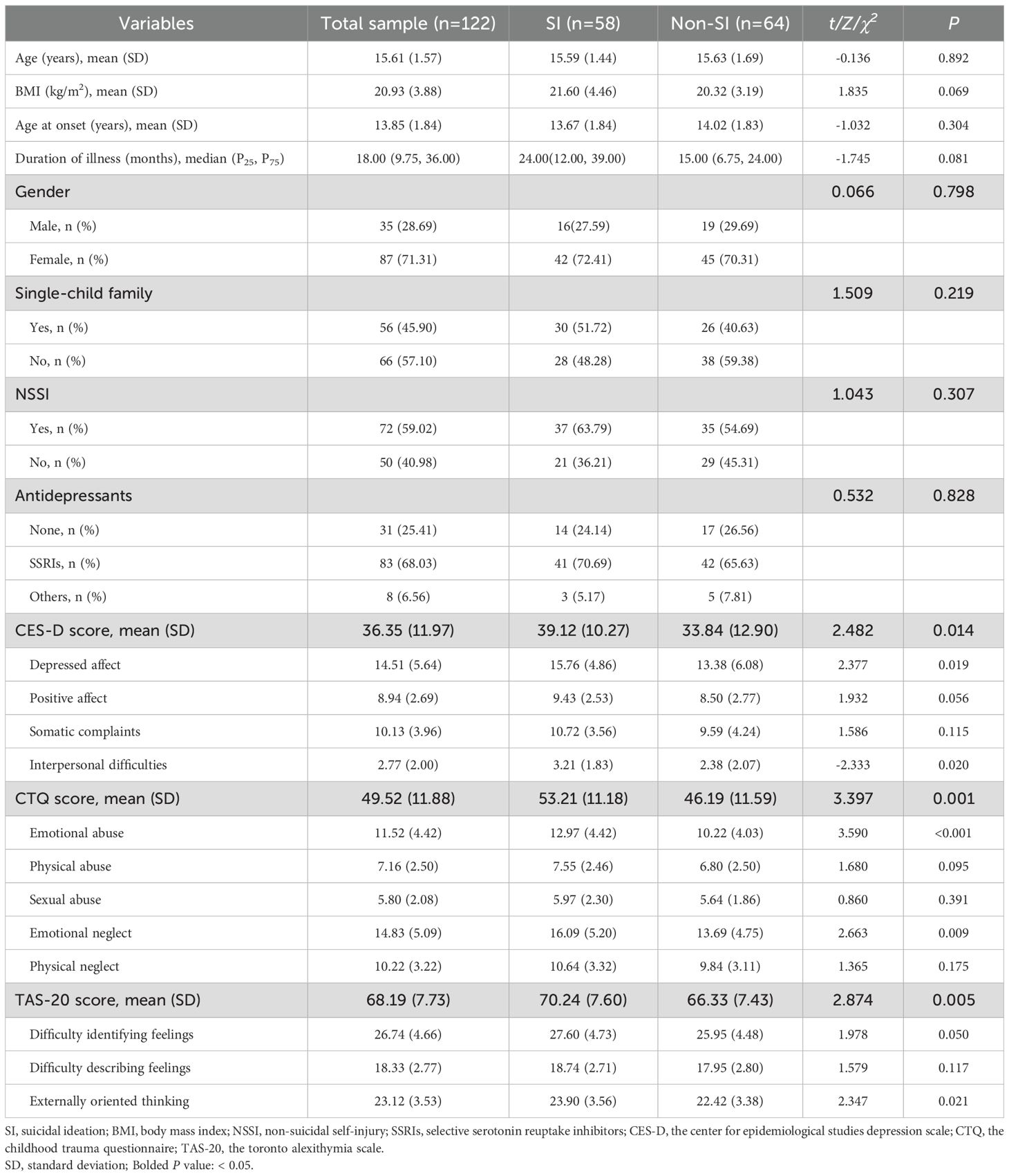
Table 1. Comparison of socio-demographic and clinical characteristics between the SI group and the non-SI group in adolescents with MDD.
At the one-year follow-up period, the proportion of single-child family, the proportion of NSSI, the total score of TAS-20, the score of interpersonal difficulties and the score of difficulty identifying feelings in the PSI group were significantly higher than those in the non-PSI group (all P < 0.05). In addition, the proportion of NSSI, the total score of CES-D, the score of depressed affect and the score of positive affect in the new-onset SI group were significantly higher than those in the non- new-onset SI group (all P < 0.05) (Tables 2, 3). In conclusion, adolescents with PSI exhibited significantly higher rates of single-child family, NSSI and alexithymia, while those with new-onset SI showed a significant increase in NSSI risk and depressive symptoms.
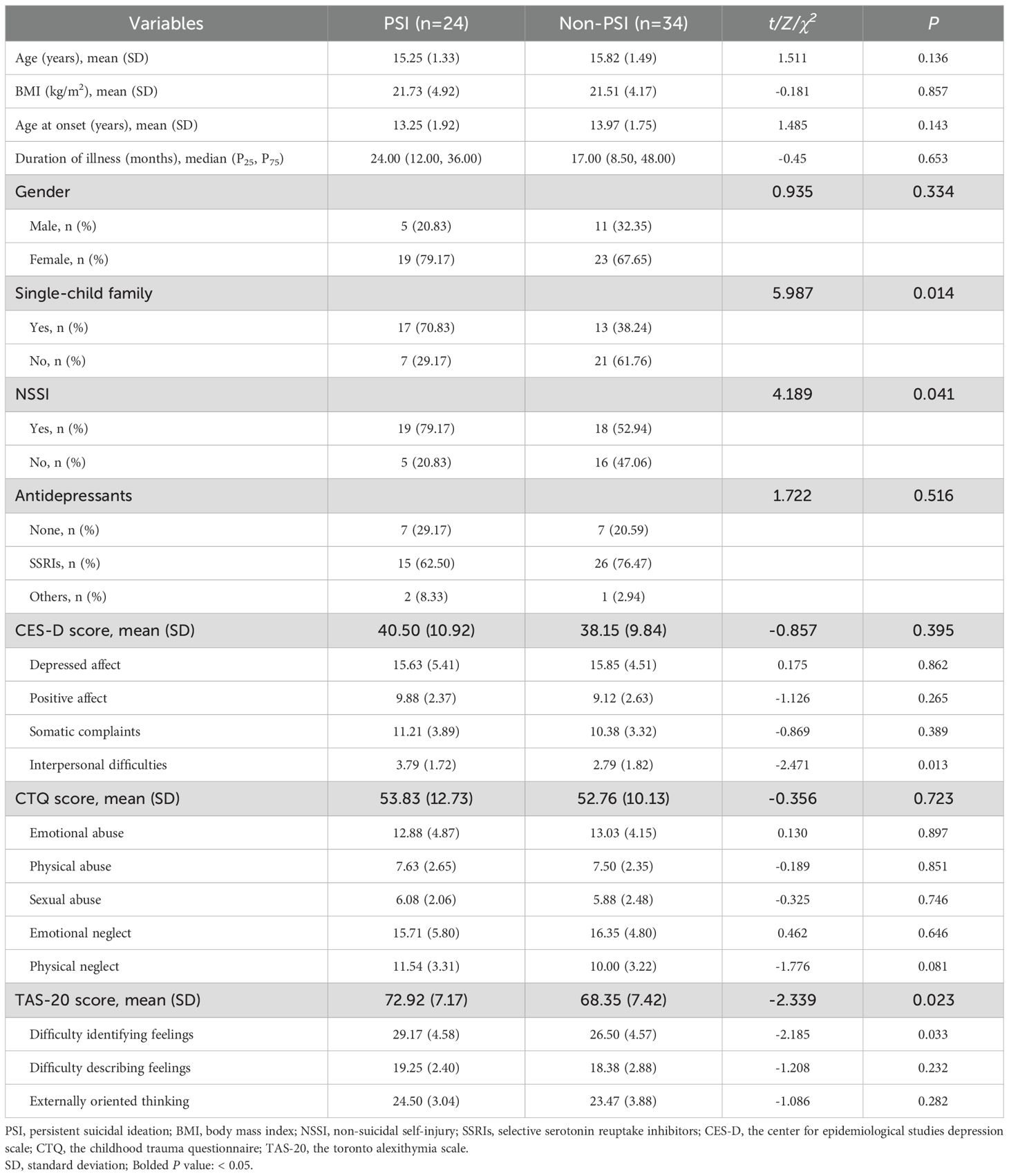
Table 2. Comparison of socio-demographic and clinical characteristics between the PSI group and the non-PSI group in adolescents with MDD.
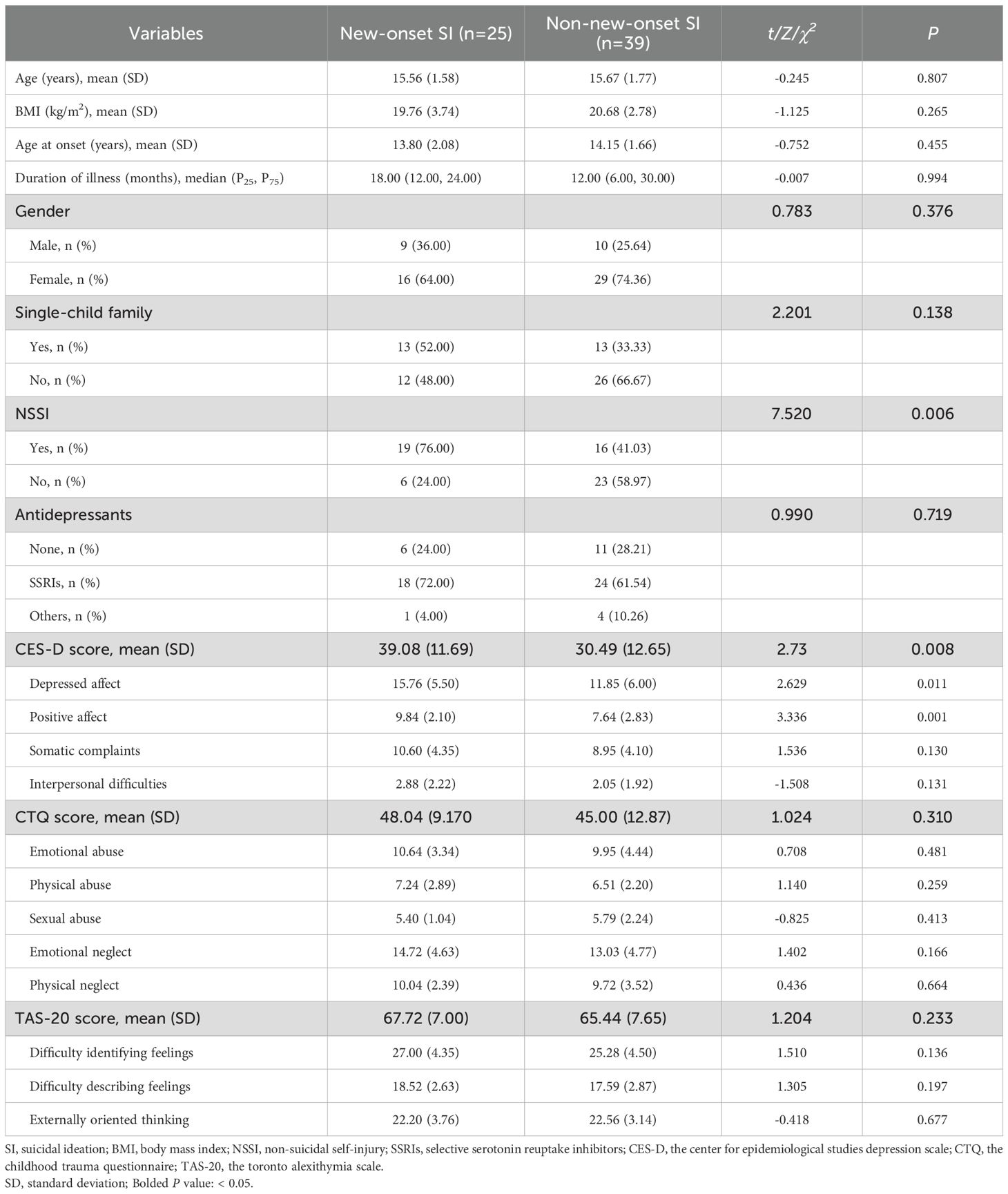
Table 3. Comparison of socio-demographic and clinical characteristics between the new-onset SI group and the non-new-onset SI group in adolescents with MDD.
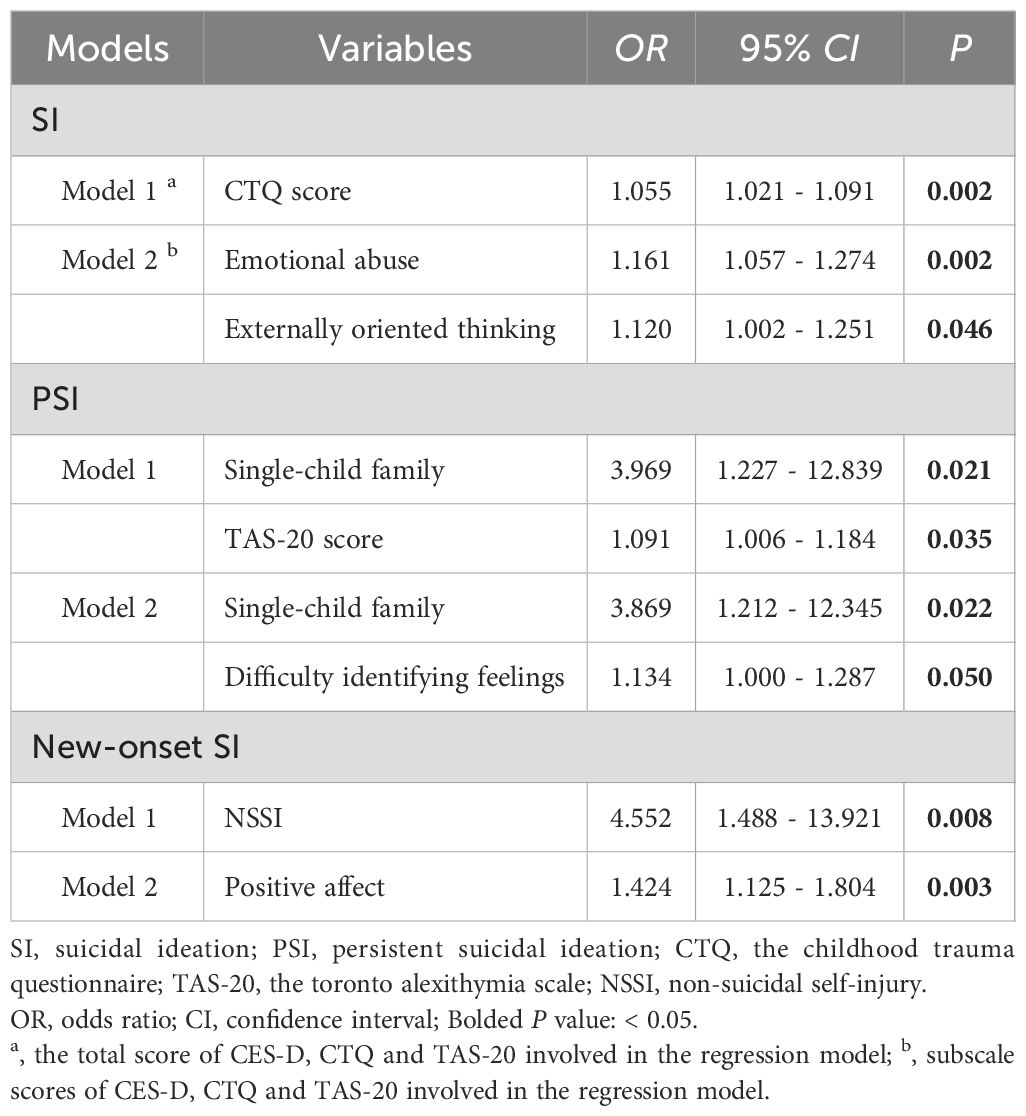
3.2 Multivariate logistic stepwise regression analysis of SI in adolescents with MDD
At the baseline period, Model 1 indicated that CTQ score (OR = 1.055, 95%CI: 1.021 - 1.091, P = 0.002) was a risk factor for SI in adolescents with MDD. In Model 2, the score of emotional abuse (OR = 1.161, 95%CI: 1.057 - 1.274, P = 0.002) and the score of externally oriented thinking (OR = 1.120, 95%CI: 1.002 - 1.251, P = 0.046) were identified as risk factors for SI.
At the follow-up period of the baseline SI group, Model 1 showed that single-child family (OR = 3.969, 95%CI: 1.227 - 12.839, P = 0.021) and TAS-20 score (OR = 1.091, 95%CI: 1.006 - 1.184, P = 0.035) were risk factors for PSI in adolescents with MDD. In Model 2, single-child family (OR = 3.869, 95%CI: 1.212 - 12.345, P = 0.022) and the score of difficulty identifying feelings (OR = 1.134, 95%CI: 1.000 - 1.287, P = 0.050) were risk factors for PSI.
At the follow-up period of the baseline non-SI group, Model 1 showed that NSSI (OR = 4.552, 95%CI: 1.488 - 13.921, P = 0.008) was a risk factor for new-onset SI in adolescents with MDD. In Model 2, the score of positive affect (OR = 1.424, 95%CI: 1.125-1.804, P = 0.003) was a risk factor for new-onset SI (Table 4). In addition, multicollinearity among the variables in this study was also assessed by calculating the variance inflation factor (VIF). All VIF values were less than 5.0, indicating that the multicollinearity was within acceptable limits.
In summary, at the baseline period, the CTQ score and its emotional abuse subscale, along with externally oriented thinking on the TAS-20, independently predicted the presence of suicidal ideation. At the follow-up period, the main drivers of PSI included single-child family and TAS-20 score, among which the dimension of difficulty identifying feelings was particularly significant. NSSI behavior and the absence of positive affect were the main predictors of new-onset SI.
4 Discussion
Given the strong predictability of SI for suicidal behavior, an in-depth study of its longitudinal developmental process and associated influencing factors is of great significance for reducing suicide risk. This study demonstrated that the prevalence of PSI in adolescents with MDD was 19.7%, and the prevalence of new-onset SI was 20.5%. The prevalence of PSI in this study was significantly higher than that reported in the general adolescent population in China. A previous study on Chinese teenagers reported that in the general student population, the prevalence of individuals with PSI was only 1.8%, and approximately two-fifths of these individuals indicated that they had further suicidal plans and attempts (5). Furthermore, in a study encompassing 17 countries, 60% of individuals experienced the transition from SI to a first suicide attempt within the first year following the onset of SI (39). These findings suggest that clinicians need to identify high-risk groups at an early stage and intervene in a timely manner to enhance the effectiveness of preventive measures.
At the baseline period, this study found that the total score of the CES-D, CTQ, and TAS-20 were significantly higher in the SI group than in the non-SI group, consistent with previous studies. Firstly, an increasing number of studies have confirmed a direct positive correlation between the severity of depressive symptoms and SI. A study on SI in Chinese adolescents with MDD indicated that the severity of depression could serve as a significant predictor of SI in this population (4). A follow-up study further demonstrated that changes in depressive symptoms could predict subsequent changes in SI, thereby supporting the temporal impact of the severity of depressive symptoms on SI (16). Secondly, CM is an important predictor of SI. A meta-analysis demonstrated that CM can increase an individual’s risk of SI by 2.3 times, and the earlier the CM occurs, the higher the risk (40). On this basis, the study found that emotional abuse significantly influences SI in Chinese adolescents through a cascade of stress-related mediators (41). Similarly, a study on CM and SI indicated that emotional abuse influenced SI via separation-related mediators, emotional neglect influenced SI via despair-related mediators, and sexual abuse had a direct impact on SI (42). These findings suggest the necessity of focusing on the potential risks associated with different types of CM and implementing targeted interventions within suicide prevention efforts. Finally, a cross-sectional study indicated that alexithymia was a significant predictor of SI in patients with MDD, and this association remains significant even after controlling for depressive symptoms (43). Further research found that adolescents with MDD who exhibited pronounced extroverted thinking were more likely to engage in negative behaviors due to their inability to effectively manage negative emotions (44). Therefore, improving depressive symptoms, optimizing the family environment, and enhancing emotional regulation skills may help adolescents with MDD to improve their mental health status, reduce the occurrence of SI and behavior, and thereby promote the recovery of social functioning.
At the follow-up period, single-child family, the total score of TAS-20, and the score of difficulty identifying feelings were all identified as risk factors for PSI in adolescents with MDD, suggesting a possible synergy between family environment and emotional regulation deficits. Previous studies showed that single-child family was one of the key risk factors for SI in adolescents. A study found through logistic regression analyses that the background of single-child family increased the risk of SI in adolescents by more than four times (45). This might be related to certain unique psychological experiences encountered by children in single-child family during their developmental trajectory. For instance, children from single-child family often experienced a higher degree of loneliness, and chronic feelings of loneliness were closely associated with SI (46). These results suggest that the uniqueness of children from single-child family in terms of family support, psychological stress, and emotional regulation may be an important factor for the persistence of SI. Alexithymia, a stable personality trait characterized by difficulty in recognizing and describing one’s own emotions, is closely associated with difficulties in emotion regulation (47). A study on SI proposed that individuals with a lack of emotional awareness, inadequate coping and regulation strategies, and an inability to accept their emotions were more likely to report PSI (48). This discovery was in accordance with a study on the biosocial theory, which posited that difficulty in emotion regulation was a key factor in maintaining suicidal tendencies (49). Specifically, a meta-analysis revealed a significant association between SI and alexithymia, particularly difficulty identifying feelings (50). Furthermore, a domestic study also found that difficulty in emotion recognition was not only an independent risk factor for SI, but also indirectly affected the generation and persistence of SI by intensifying perceived stress and depressive symptoms (26). Therefore, in patients with MDD, the disorder of emotion recognition and expression can lead to the long-term accumulation of negative emotions, thereby intensifying the persistence of SI. However, although the effect size of the TAS-20 score reached statistical significance, its corresponding OR close to 1, indicating that its clinical significance requires further validation. Future studies should employ multicenter, large-sample designs to reassess its effect size in order to clarify its actual clinical utility.
In addition, this study found that NSSI and CES-D (positive affect) score could be used as risk factors for predicting new-onset SI, which was basically consistent with previous studies. There is a significant association between NSSI and SI, which has a longitudinal predictive effect. Specifically, a longitudinal study of adolescents showed that NSSI at baseline significantly predicted subsequent SI, which in turn reinforced NSSI behavior, forming a bidirectional cycle (51). Moreover, the severity and persistence of NSSI had a stratified effect on suicide risk. Individuals with a high frequency or persistence of NSSI exhibited more severe SI and behavior, whereas a decrease in the frequency of NSSI was accompanied by a parallel decrease in SI (52, 53). This association may have stemmed from the negative self-perception of individuals with NSSI, such as low self-esteem, low self-efficacy, and excessive self-criticism (54, 55). These traits were not only closely related to NSSI, but may also have further strengthened SI, thereby forming a vicious cycle. A study further indicated that NSSI might be a maladaptive coping strategy. In the short term, it reduced SI, but in the long term, it increased the risk of suicide (56). Therefore, NSSI is not only a risk marker for SI, but may also influence long-term changes in suicide risk through complex mechanisms. In the CES-D, the reduction of positive affect is a core dimension of depressive symptoms. This subscale is reverse-scored, and the higher scores are associated with fewer positive affect experienced by individuals and more severe depressive symptoms. Previous studies indicated that the reduction of positive affect might serve as one of the important mechanisms underlying the development of SI and behavior among adolescents. A prospective study found that lower levels of positive affect still significantly predicted the risk of suicide-related events in adolescents at 6 months, after controlling for levels of depression, world-aversion, and other potential confounders (57). A study demonstrated that a lower level of positive affect in an individual’s daily life was a significant risk factor for SI the following day (58). Furthermore, a randomized controlled trial indicated that the reduction of positive affect may increase the risk of SI among teenagers by enhancing their feelings of depression and despair (17). In conclusion, NSSI and the reduction of positive affect both reflect that individuals lack effective coping strategies when facing negative emotions and life stress, thereby increasing the risk of SI in the future.
This study systematically elucidated the key predictors of persistent or new-onset SI in adolescents with MDD, and provided an empirical basis for the development of evidence-based screening indicators and early intervention programs. Based on these findings, it is recommended to introduce a brief and effective screening tool in routine clinical assessments and early identification system in school/community, focusing on alexithymia, single-child family, NSSI behaviors and changes in positive affect. Early interventions should be implemented for high-risk individuals identified through screening to enhance their emotional regulation, reduce the incidence of NSSI behaviors and enhance experiences of positive affect. Meanwhile, families, schools, and society should collaborate to establish a multi-layered support system and optimize psychological intervention measures, thereby effectively reducing the risks of the emergence and persistence of SI and jointly safeguarding the mental health of adolescents.
This study also had certain limitations: (1) This study was exploratory in nature, with a relatively small sample size and limited statistical power. Furthermore, the study population was entirely recruited from Anhui Province, which may limit the generalizability of the findings. Therefore, future multicenter, large-sample prospective clinical studies are needed to further investigate this issue, thereby enhancing the statistical power and reliability of the findings. (2) In this study, SI was assessed only at baseline and one-year follow-up. Future studies will add additional assessment time points to more accurately capture the trajectory of SI, thereby improving the accuracy and reliability of the study data. (3) This study did not adequately consider all of the potential confounders that may influence SI in adolescents, such as biological, genetic, and environmental factors. Future studies will address these limitations by including a wider range of variables in their analyses.
In conclusion, this study found that PSI in adolescents with MDD was closely associated with single-child family and alexithymia, whereas new-onset SI was influenced by NSSI and reduced positive affect. These factors may further promote the occurrence and persistence of SI by exacerbating difficulties in emotion regulation, negative self-perception, and depressive symptoms.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Chaohu Hospital of Anhui Medical University, under reference number 202009-KYXM-04. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
YZ: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Visualization, Writing – original draft, Writing – review & editing. LL: Data curation, Formal Analysis, Investigation, Methodology, Writing – review & editing. HF: Data curation, Formal Analysis, Investigation, Methodology, Writing – review & editing. XZ: Data curation, Formal Analysis, Investigation, Methodology, Writing – review & editing. LX: Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Supervision, Writing – review & editing. HL: Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was supported by the National Natural Science Foundation of China (No. 82401798), the Research Fund Project of Anhui Translational Research Institute (No. 2022zhyx-B01) and the Scientific Research Project of Anhui Higher Education Institutions (No. 2024AH050681).
Acknowledgments
We sincerely thank all the study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Li F, Cui Y, Li Y, Guo L, Ke X, Liu J, et al. Prevalence of mental disorders in school children and adolescents in China: diagnostic data from detailed clinical assessments of 17,524 individuals. J Child Psychol Psychiatry. (2022) 63:34–46. doi: 10.1111/jcpp.13445
2. Shorey S, Ng ED, and Wong CHJ. Global prevalence of depression and elevated depressive symptoms among adolescents: A systematic review and meta-analysis. Br J Clin Psychol. (2022) 61:287–305. doi: 10.1111/bjc.12333
3. Roseman M, Kloda LA, Saadat N, Riehm KE, Ickowicz A, Baltzer F, et al. Accuracy of depression screening tools to detect major depression in children and adolescents: A systematic review. Can J Psychiatry. (2016) 61:746–57. doi: 10.1177/0706743716651833
4. Xu H, Chen ZH, Ji JJ, Qian HY, She J, Hou CT, et al. Behavioral and psychosocial factors associated with suicidal ideation in adolescents with depression: An ecological model of health behavior. J Psychiatr Res. (2025) 181:411–6. doi: 10.1016/j.jpsychires.2024.12.014
5. Guo Y, Zhang J, Cui Y, Cui Y, Huang X, Guo Y, et al. Psychosocial predictors of persistent suicidal ideation among Chinese adolescents: A longitudinal study. J Affect Disord. (2023) 334:137–44. doi: 10.1016/j.jad.2023.04.090
6. Mulholland H, Whittington R, Lane S, Haines-Delmont A, Nathan R, Saini P, et al. Longitudinal investigation of the presence of different trajectories and associated health and socio-economic determinants, for participants who report suicidal ideation within a community-based public health survey. BMJ Open. (2023) 13:e063699. doi: 10.1136/bmjopen-2022-063699
7. Oquendo MA, Currier D, and Mann JJ. Prospective studies of suicidal behavior in major depressive and bipolar disorders: what is the evidence for predictive risk factors? Acta Psychiatr Scand. (2006) 114:151–8. doi: 10.1111/j.1600-0447.2006.00829.x
8. Kjm OH, Poulton R, and Linscott RJ. Psychotic experiences and schizotypy in early adolescence predict subsequent suicidal ideation trajectories and suicide attempt outcomes from age 18 to 38 years. Schizophr Bull. (2021) 47:456–64. doi: 10.1093/schbul/sbaa151
9. Czyz EK and King CA. Longitudinal trajectories of suicidal ideation and subsequent suicide attempts among adolescent inpatients. J Clin Child Adolesc Psychol. (2015) 44:181–93. doi: 10.1080/15374416.2013.836454
10. APA. Practice guideline for the treatment of patients with major depressive disorder. 3rd edition. American Psychiatric Association (2000).
11. Maina G, Adami M, Ascione G, Bondi E, De Berardis D, Delmonte D, et al. Nationwide consensus on the clinical management of treatment-resistant depression in Italy: a Delphi panel. Ann Gen Psychiatry. (2023) 22:48. doi: 10.1186/s12991-023-00478-7
12. Sarasso P, Billeci M, Ronga I, Raffone F, Martiadis V, and Di Petta G. Disembodiment and affective resonances in esketamine treatment of depersonalized depression subtype: two case studies. Psychopathology. (2024) 57:480–91. doi: 10.1159/000539714
13. Monteleone P, Martiadis V, and Maj M. Circadian rhythms and treatment implications in depression. Prog Neuropsychopharmacol Biol Psychiatry. (2011) 35:1569–74. doi: 10.1016/j.pnpbp.2010.07.028
14. Fiorillo A, Demyttenaere K, Martiadis V, and Martinotti G. Editorial: Treatment resistant depression (TRD): epidemiology, clinic, burden and treatment. Front Psychiatry. (2025) 16:1588902. doi: 10.3389/fpsyt.2025.1588902
15. Millgram Y, Goldenberg A, and Nock MK. Suicidal thoughts are associated with reduced source attribution of emotion. J Psychopathol Clin Sci. (2025) 134:18–30. doi: 10.1037/abn0000939
16. Shaygan M, Hosseini FA, and Negad SS. Temporal relationships between changes in depression and suicidal ideation: A mediation analysis in a randomized double-blinded clinical trial. Psychol Psychother. (2023) 96:364–82. doi: 10.1111/papt.12444
17. Yen S, Suazo N, Doerr J, Macrynikola N, Villarreal LS, Sodano S, et al. Skills to Enhance Positivity in adolescents at risk for suicide: Protocol for a randomized controlled trial. PLoS One. (2023) 18:e0287285. doi: 10.1371/journal.pone.0287285
18. Darquennes G, Wacquier B, Loas G, and Hein M. Suicidal ideations in major depressed subjects: role of the temporal dynamics of anhedonia. Brain Sci. (2023) 13:1065. doi: 10.3390/brainsci13071065
19. Metts AV, Echiverri-Cohen AM, Yarrington JS, Zinbarg RE, Mineka S, and Craske MG. Longitudinal associations among dimensional symptoms of depression and anxiety and first onset suicidal ideation in adolescents. Suicide Life Threat Behav. (2023) 53:457–69. doi: 10.1111/sltb.12956
20. Ihme H, Olié E, Courtet P, El-Hage W, Zendjidjian X, Mazzola-Pomietto P, et al. Childhood trauma increases vulnerability to attempt suicide in adulthood through avoidant attachment. Compr Psychiatry. (2022) 117:152333. doi: 10.1016/j.comppsych.2022.152333
21. Laghaei M, Mehrabizadeh Honarmand M, Jobson L, Abdollahpour Ranjbar H, and Habibi Asgarabad M. Pathways from childhood trauma to suicidal ideation: mediating through difficulties in emotion regulation and depressive symptoms. BMC Psychiatry. (2023) 23:295. doi: 10.1186/s12888-023-04699-8
22. Izci F, Zincir S, Zincir SB, Bilici R, Gica S, Koc MSI, et al. Suicide attempt, suicidal ideation and hopelessness levels in major depressive patients with and without alexithymia. Düünen Adam J Psychiatry Neurological ences. (2015) 28. doi: 10.5350/DAJPN2015280103
23. De Berardis D, Serroni N, Campanella D, Carano A, Gambi F, Valchera A, et al. Alexithymia and its relationships with C-reactive protein and serum lipid levels among drug naïve adult outpatients with major depression. Prog Neuropsychopharmacol Biol Psychiatry. (2008) 32:1982–6. doi: 10.1016/j.pnpbp.2008.09.022
24. Hintikka J, Honkalampi K, Koivumaa-Honkanen H, Antikainen R, Tanskanen A, Haatainen K, et al. Alexithymia and suicidal ideation: a 12-month follow-up study in a general population. Compr Psychiatry. (2004) 45:340–5. doi: 10.1016/j.comppsych.2004.06.008
25. De Berardis D, Fornaro M, Valchera A, Rapini G, Di Natale S, De Lauretis I, et al. Alexithymia, resilience, somatic sensations and their relationships with suicide ideation in drug naïve patients with first-episode major depression: An exploratory study in the “real world” everyday clinical practice. Early Interv Psychiatry. (2020) 14:336–42. doi: 10.1111/eip.12863
26. Li D, Gao Y, Li S, Zhou C, Wang Y, Li M, et al. Perceived stress and severity of depression mediate the association between alexithymia and suicidal ideation in patients with major depressive disorder. Heliyon. (2023) 9:e21986. doi: 10.1016/j.heliyon.2023.e21986
27. Zhou L, Qiao C, Huang J, Lin J, Zhang H, Xie J, et al. The impact of recent life events, internalizing symptoms, and emotion regulation on the severity of non-suicidal self-injury in adolescents: A mediation analysis. Neuropsychiatr Dis Treat. (2024) 20:415–28. doi: 10.2147/ndt.S444729
28. Brausch AM, Kalgren T, and Littlefield A. Onset and offset of nonsuicidal self-injury prospectively associates with emotion regulation and suicide ideation in adolescents. J Affect Disord. (2025) 373:412–9. doi: 10.1016/j.jad.2025.01.004
29. Association A P. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed Vol. 25. Codas: American Psychiatric Association (2013). p. 191.
30. Jeon ME, Goncearenco I, Rogers ML, Campione MT, Lamis DA, Kaslow NJ, et al. Psychometric properties of the beck scale for suicidal ideation in a diverse sample. Assessment. (2025), 10731911251330498. doi: 10.1177/10731911251330498
31. Beck AT, Kovacs M, and Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. (1979) 47:343–52. doi: 10.1037//0022-006x.47.2.343
32. Hu S, Mo D, Guo P, Zheng H, Jiang X, and Zhong H. Correlation between suicidal ideation and emotional memory in adolescents with depressive disorder. Sci Rep. (2022) 12:5470. doi: 10.1038/s41598-022-09459-4
33. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl psychol Measurement. (1977) 1:385–401. doi: 10.1177/014662167700100306
34. Blodgett JM, Lachance CC, Stubbs B, Co M, Wu YT, Prina M, et al. A systematic review of the latent structure of the Center for Epidemiologic Studies Depression Scale (CES-D) amongst adolescents. BMC Psychiatry. (2021) 21:197. doi: 10.1186/s12888-021-03206-1
35. Yang W, Xiong G, Garrido LE, Zhang JX, Wang MC, and Wang C. Factor structure and criterion validity across the full scale and ten short forms of the CES-D among Chinese adolescents. Psychol Assess. (2018) 30:1186–98. doi: 10.1037/pas0000559
36. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/s0145-2134(02)00541-0
37. Peng C, Cheng J, Rong F, Wang Y, and Yu Y. Psychometric properties and normative data of the childhood trauma questionnaire-short form in Chinese adolescents. Front Psychol. (2023) 14:1130683. doi: 10.3389/fpsyg.2023.1130683
38. Bagby RM, Parker JD, and Taylor GJ. The twenty-item Toronto Alexithymia Scale–I. Item selection and cross-validation of the factor structure. J Psychosom Res. (1994) 38:23–32. doi: 10.1016/0022-3999(94)90005-1
39. Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. (2008) 192:98–105. doi: 10.1192/bjp.bp.107.040113
40. Angelakis I, Austin JL, and Gooding P. Association of childhood maltreatment with suicide behaviors among young people: A systematic review and meta-analysis. JAMA Netw Open. (2020) 3:e2012563. doi: 10.1001/jamanetworkopen.2020.12563
41. Fan Q, Liu Q, Liu C, and Wang Z. Childhood trauma and suicidal ideation among Chinese adolescents: The mediating effects of character strengths and perceived stress. J Psychiatr Ment Health Nurs. (2023) 30:526–36. doi: 10.1111/jpm.12892
42. Berardelli I, Sarubbi S, Rogante E, Erbuto D, Giuliani C, Lamis DA, et al. Association between childhood maltreatment and suicidal ideation: A path analysis study. J Clin Med. (2022) 11:2179. doi: 10.3390/jcm11082179
43. Mohamed BES and Ahmed M. Emotional intelligence, alexithymia and suicidal ideation among depressive patients. Arch Psychiatr Nurs. (2022) 37:33–8. doi: 10.1016/j.apnu.2021.12.002
44. Li X, Wang X, Sun L, Hu Y, Xia L, Wang S, et al. Associations between childhood maltreatment and suicidal ideation in depressed adolescents: The mediating effect of alexithymia and insomnia. Child Abuse Negl. (2023) 135:105990. doi: 10.1016/j.chiabu.2022.105990
45. Li C, Wei Z, Wang Y, and Sun L. Associations between suicidal ideation and relatives’ Physical and mental health among community residents: differences between family members and lineal consanguinity. Int J Environ Res Public Health. (2022) 19:15997. doi: 10.3390/ijerph192315997
46. Mcclelland H, Evans JJ, Nowland R, Ferguson E, and O'connor RC. Loneliness as a predictor of suicidal ideation and behaviour: a systematic review and meta-analysis of prospective studies. J Affect Disord. (2020) 274:880–96. doi: 10.1016/j.jad.2020.05.004
47. Pandey R, Saxena P, and Dubey A. Emotion regulation difficulties in alexithymia and mental health. (2011) 7. doi: 10.5964/ejop.v7i4.155
48. Wolff JC, Davis S, Liu RT, Cha CB, Cheek SM, Nestor BA, et al. Trajectories of suicidal ideation among adolescents following psychiatric hospitalization. J Abnorm Child Psychol. (2018) 46:355–63. doi: 10.1007/s10802-017-0293-6
49. Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. Guilford Press. (1993) 6:225–31.
50. Hemming L, Taylor P, Haddock G, Shaw J, and Pratt D. A systematic review and meta-analysis of the association between alexithymia and suicide ideation and behaviour. J Affect Disord. (2019) 254:34–48. doi: 10.1016/j.jad.2019.05.013
51. Xu Z, Li N, Kong Y, Lin L, Liu Y, Zhang H, et al. Nonsuicidal self-injury as the gateway and consequence of suicidal ideation among adolescents: a cross-lagged regression analysis. Front Psychiatry. (2024) 15:1434191. doi: 10.3389/fpsyt.2024.1434191
52. Muehlenkamp JJ, Brausch AM, and Littlefield A. Concurrent changes in nonsuicidal self-injury and suicide thoughts and behaviors. Psychol Med. (2023) 53:4898–903. doi: 10.1017/s0033291722001763
53. Masi G, Pisano S, Sesso G, Mazzullo C, Berloffa S, Fantozzi P, et al. Persistent non-suicidal self-injury and suicidality in referred adolescents: A longitudinal study exploring the role of cyclothymic temperament. Brain Sci. (2023) 13:755. doi: 10.3390/brainsci13050755
54. Kiekens G, Hasking P, Nock MK, Boyes M, Kirtley O, Bruffaerts R, et al. Fluctuations in affective states and self-efficacy to resist non-suicidal self-injury as real-time predictors of non-suicidal self-injurious thoughts and behaviors. Front Psychiatry. (2020) 11:214. doi: 10.3389/fpsyt.2020.00214
55. Sorgi-Wilson KM, Cheung JC, Ciesinski NK, and Mccloskey MS. Cognition and non-suicidal self-injury: exploring relationships with psychological functions. Arch Suicide Res. (2023) 27:1002–18. doi: 10.1080/13811118.2022.2106919
56. Herzog S, Choo TH, Galfalvy H, Mann JJ, and Stanley BH. Effect of non-suicidal self-injury on suicidal ideation: real-time monitoring study. Br J Psychiatry. (2022) 221:485–7. doi: 10.1192/bjp.2021.225
57. Yen S, Weinstock LM, Andover MS, Sheets ES, Selby EA, Spirito A, et al. Prospective predictors of adolescent suicidality: 6-month post-hospitalization follow-up. Psychol Med. (2013) 43:983–93. doi: 10.1017/s0033291712001912
58. Wallace GT, Brick LA, Provost EM, Peters JR, Miller IW, Schatten HT, et al. Daily levels and dynamic metrics of affective-cognitive constructs associate with suicidal thoughts and behaviours in adults after psychiatric hospitalization. Clin Psychol Psychother. (2024) 31:e2982. doi: 10.1002/cpp.2982
Keywords: suicidal ideation, major depressive disorder, adolescents, predictive factors, longitudinal study
Citation: Zhang Y, Liu L, Fan H, Zhang X, Xia L and Liu H (2025) Clinical correlates of new-onset and persistent suicidal ideation in adolescents with major depressive disorder. Front. Psychiatry 16:1655037. doi: 10.3389/fpsyt.2025.1655037
Received: 27 June 2025; Accepted: 25 August 2025;
Published: 10 September 2025.
Edited by:
Vassilis Martiadis, Asl Napoli 1 Centro, ItalyReviewed by:
Alessandro Cuomo, University of Siena, ItalyFabiola Raffone, Asl Napoli 1 Centro, Italy
Copyright © 2025 Zhang, Liu, Fan, Zhang, Xia and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huanzhong Liu, aHVhbnpob25nbGl1QGFobXUuZWR1LmNu; Lei Xia, eGlhbGVpQGFobXUuZWR1LmNu
†These authors have contributed equally to this work
 Yun Zhang
Yun Zhang Lewei Liu
Lewei Liu Haojie Fan
Haojie Fan Xi Zhang
Xi Zhang Lei Xia
Lei Xia Huanzhong Liu
Huanzhong Liu