Abstract
Objective:
To validate the psychometric properties of the Swanson, Nolan, and Pelham Rating Scale (SNAP-IV) in amblyopic children at high AD/HD risk and establish its clinical utility for comorbid AD/HD screening.
Methods:
This cross-sectional study utilized baseline data from the China Amblyopia Behavioral Cohort (CABC), which comprises 465 amblyopic children (aged 4–17 years). The reliability of the SNAP-IV was comprehensively assessed using Cronbach’s alpha and the split-half coefficient. The validity of the SNAP-IV was evaluated using criterion validity with the Conners’ parent rating scale (CPRS) and construct validity via confirmatory factor analysis (CFA). The measurement invariance of the SNAP-IV across gender and age groups was also investigated.
Results:
The SNAP-IV demonstrated exceptional internal consistency (Cronbach’s α = 0.965 [95% CI: 0.958–0.972], split-half coefficient = 0.891) and strong criterion validity with the CPRS domains, particularly with respect to the oppositional factor of the SNAP-IV scale, which showed the highest correlation with the conduct problem factor of the Conners’ Parent Rating Scale (CPRS) (rs = 0.837, 95% CI: 0.807–0.863, p<0.001, large effect). The findings indicated a substantial correlation between inattention and learning problems (rs = 0.808, 95% CI: 0.767–0.834, p<0.001, large effect) and conduct problems (rs = 0.719, 95% CI: 0.675–0.765, p<0.001, large effect). Confirmatory factor analysis confirmed a three-factor structure (inattention, hyperactivity/impulsivity, oppositional) with robust fit indices (χ²/(291) = 1033.4, χ²/df = 3.551, RMSEA=0.074, CFI=0.92, IFI=0.92), with full measurement invariance confirmed across gender and age groups.
Conclusions:
This study constitutes the first systematic validation of the SNAP-IV in amblyopic children, thereby establishing its robustness for AD/HD screening in visually impaired populations. The scale’s standardized application has the potential to enhance the screening of early AD/HD-amblyopia comorbidity and the development of multidisciplinary intervention strategies for integrating visual and behavioral rehabilitation.
Introduction
Attention Deficit/Hyper Activity (AD/HD), a neurodevelopmental disorder characterized by inattention, hyperactivity, and impulsivity (1), has a global prevalence of approximately 4.8% in children (2), and an estimated prevalence of 9.8% in the United States (3, 4). Its persistence into adulthood (2) and profound impacts on cognitive, behavioral, and psychosocial functioning (5, 6) underscore the urgency of early identification and intervention. Emerging evidence reveals a notable comorbidity between amblyopia and AD/HD. The prevalence of amblyopia among children has been documented to be approximately 2.0% in South Korea (7),1.09% (95% CI: 0.86–1.35%) in central–southern China (8), and 0.99% in Taiwan, China (9). With respect to comorbidity risk, children diagnosed with amblyopia present a 68.7% increased risk of developing AD/HD (OR=1.687, 95% CI: 1.444–1.970) in the Republic of Korea (7), and a 1.81-fold elevated risk in Taiwan, China (HR=1.81, 95% CI: 1.59–2.06) (10). However, AD/HD patients present an 89% higher prevalence of amblyopia (OR=1.89, 95% CI: 1.76–2.05) (11). Given that amblyopia, a visual developmental disorder affecting 1.44% of preschoolers globally (12), shares pathophysiological mechanisms with AD/HD—such as striatal and subcortical neuronal dysfunction affecting executive attention and multisensory integration (13–16)—the co-occurrence of these disorders creates substantial clinical and economic burdens (17–19).
Despite these intersections, contemporary behavioral evaluations for AD/HD (e.g., the Conners’ Parent Rating Scale [CPRS] (20) and the Child Behavior Checklist [CBCL] (21)) lack specificity for populations affected by amblyopia (22). Furthermore, three significant limitations pertaining to the current validation of the SNAP-IV exist: (1) Methodological constraints: Previous studies have systematically excluded cohorts with visual impairments, notwithstanding the evidence that visual deficits can significantly modify behavioral phenotypes (e.g., irritability induced by visual fatigue) (23); (2) Cultural–theoretical deficiencies: The adaptation of the SNAP-IV for Chinese populations (24) remains unvalidated within sensory-impaired groups, prompting concerns regarding its generalizability; and (3) Clinical diagnostic complications: the attention dysfunction associated with amblyopia frequently overlaps with symptoms of visual impairment, resulting in diagnostic misattribution (17). These limitations pose a threat to timely identification and effective intervention strategies for AD/HD linked to amblyopia.
To address these gaps, this study conducted a systematic psychometric evaluation of the Chinese SNAP-IV in 465 amblyopic children (aged 4–17 years) from the China Amblyopia Behavioral Cohort (CABC). Utilizing a multidimensional validation framework, the present study examines internal consistency (Cronbach’s α), structural validity via confirmatory factor analysis (CFA), and measurement invariance across gender and age groups.
By establishing the reliability and validity of the SNAP-IV in this understudied population, our study aims to 1) provide evidence-based guidelines for integrating the SNAP-IV into amblyopia-associated AD/HD screening protocols, 2) increase diagnostic precision by clarifying behavioral manifestations related to visual impairment, and 3) reduce healthcare costs through early identification and multidisciplinary interventions. The present research addresses a critical methodological void (24–28) and offers a translational solution to improve behavioral health outcomes in visually impaired children.
Methods
Participants
This study recruited 465 amblyopic children aged 4–17 years from the China Amblyopia Behavioral Cohort (CABC), a multicenter initiative conducted between April 2024 and May 2026 across Guangxi, Guangdong, and Sichuan Provinces. The sample size was determined via an empirical approach (29), calculating 5–10 times the number of items in the SNAP-IV scale (26 items), yielding a minimum target of 130–260 participants.
The inclusion criteria for the study participants were as follows: The subject met the diagnostic criteria for amblyopia of the Chinese Medical Association Ophthalmology Branch (30), including anisometropic amblyopia (binocular spherical anisometropia ≥ 1.5D or cylindrical anisometropia ≥ 1.0D), ametropia amblyopia (binocular equivalent spherical anisometropia < 0.75D), and strabismic amblyopia; In addition, the subject had no other eye diseases or related systemic diseases; and no history of eye surgery. The exclusion criteria were as follows: The subject was found to be (1) unable to cooperate with the examination and (2) had other diseases that may affect the development of the central nervous system.
The severity classification criteria for amblyopia were as follows: (1) mild-to-moderate amblyopia, with best-corrected visual acuity (BCVA) lower than the age-specific normal value but ≤ 0.6 logMAR; and (2) severe amblyopia, with BCVA > 0.6 logMAR.
This study received ethical approval from the Ethics Committee of the Guangxi Zhuang Autonomous Region People’s Hospital (Approval No. KY-KJT-2023-285) and complied with the principles of the Declaration of Helsinki. Written informed consent was obtained from all participants and their guardians.
Measures
Demographic data
The demographic data of the participants was collected via questionnaires, encompassing age, gender, parental education level, maternal smoking/alcohol history, family history of amblyopia, family history of myopia, and birth weight of amblyopic children, were collected through questionnaires.
Clinical data
The clinical data of the patients were collected through a comprehensive eye examination, including an assessment of visual acuity, a fundus examination, and an ocular alignment evaluation. At the initial visit, retinoscopy was performed using 1% atropine sulfate-induced ciliary muscle paralysis, and BCVA was converted to the logarithm of the minimum angle of resolution (LogMAR).
Behavioral questionnaires
The questionnaires were conducted through via the Questionnaire Star platform, with parents completing them under the guidance of professionals. The researchers then proceeded to review and process the collected questionnaires, identifying and addressing missing or anomalous values and removing invalid responses.
The SNAP-IV Rating Scale is comprised of 26 items (31, 32), which constitute three factors: inattention (9 items), hyperactivity/impulsivity (9 items), and oppositional (8 items). The 4-point Likert scale ranges from 0 (none) to 3 (extremely severe) (24) and is suitable for children aged 6–18 years. Although the SNAP-IV/CPRS are normed for children ages 6–18 years, prior adaptations have demonstrated adequate validity and reliability in younger children (aged 4–5 years) via parental reports (28, 33).
The conners parent rating scale (CPRS) used in the study is the 48-item version (34). The CPRS includes five subscales: conduct problem, learning problem, psychosomatic, hyperactivity/impulsivity, and anxiety. The scale utilized is a parallel 4-point rating scale, ranging from 0 to 3. This CPRS version was selected as the criterion measure for validating the SNAP-IV, primarily because of its extensive validation and establishment of normative data in Chinese populations, ensuring cultural appropriateness. The 48-item CPRS is a well-validated and optimal benchmark specifically for establishing criterion validity in this initial study, given its strong conceptual overlap with the SNAP-IV and proven utility in comparable Chinese research.
Statistical analyzes
The data were analyzed via IBM SPSS Statistics 28.0 and AMOS 26.0. Normality was assessed via the Shapiro–Wilk test. Descriptive statistics (mean ± SDs) were used for normally distributed data; medians and interquartile ranges (IQR) were used for skewed data. Categorical variables are reported as frequencies/percentages (n, %). All the statistical tests were two-tailed, and a p-value < 0.05 was considered statistically significant. For comparisons involving multiple groups, Bonferroni-adjusted post hoc tests were applied to control for Type I error. To comprehensively convey the magnitude and precision of the findings, 95% confidence intervals (CIs) and specific effect sizes were reported for all key results. The specific effect size metrics used for each type of statistical test were listed as follow and were interpreted according to conventional thresholds.
Group comparisons
For demographic and clinical characteristics, Cramer’s V (phi (φ) coefficients or V) were used for chi-square tests, with interpretations as small (0.1), medium (0.3), or large (0.5); for non-normally distributed continuous variables, the effect size rank-biserial correlation (rrβ) was calculated alongside Mann-Whitney U tests, interpreted similarly to Cohen’s guidelines (small: 0.1, medium: 0.3, large: 0.5); and for parametric tests, Cohen’s d or η² were reported as appropriate.
Item analysis
Spearman’s rank correlation coefficients (rs) were calculated between items and factors, with the correlation coefficient (rs) itself interpreted as the effect size, reported with 95% confidence intervals (CI), where r values indicate effect size (small: 0.1-0.3, medium: 0.3-0.5, large: >0.5). Acceptable item–factor correlations were defined as those that were ≥ 0.40 (marginally acceptable) (35).
Reliability assessment
Cronbach’s α coefficient and split-half coefficients were used to evaluate the internal consistency of the scale and its factors. Which served as the primary reliability indices. A Cronbach’s α coefficient ≥ 0.70 was considered acceptable (36).
Validity evaluation
Criterion-related validity was analyzed via Spearman’s correlation analysis to examine the correlation between the SNAP-IV rating scale and each factor of the CPRS dimensions. The correlation coefficient (rs) and 95%CI was interpreted as the effect size. Structural validity was assessed via confirmatory factor analysis (CFA). The commonly used fit evaluation indicators are as follows: 1) χ²/df < 5.0 is an acceptable model; 2) Comparative Fit Index (CFI) and Incremental Fit Index (IFI) > 0.90 are acceptable standards; 3) Root Mean Square Error of Approximation (RMSEA) and Root Mean Square Residual (RMR) < 0.08 are acceptable standards. These fit indices serve as effect size measures for model adequacy. Convergent validity was supported by standardized factor loadings (λ) values > 0.50, composite reliability (CR) > 0.70 and average variance extracted (AVE) > 0.50 are ideal values (36–38). Discriminant validity was assessed using the Fornell-Larcker criterion by comparing the square root of the AVE for each factor with the inter-factor correlations. Additionally, the Maximum Shared Variance (MSV) and the Average Shared Variance (ASV) were calculated. Strong discriminant validity is indicated when the AVE for each construct is greater than its MSV, and simultaneously greater than its ASV.
Measurement invariance
Multigroup CFA was used to evaluate measurement invariance across gender and age. Invariance was tested by sequentially constraining the factor loadings (metric), intercepts (scalar), and residuals (strict) to be equal across groups. Invariance was supported if the change in fit indices between nested models met the following criteria: ΔCFI was < 0.01 and ΔRMSEA < 0.015 (39). These difference indices are the critical effect sizes for evaluating measurement invariance.
Results
Demographics and clinical characteristics of amblyopic children
A total of 465 amblyopic children (99.1% valid questionnaires) participated in this study, and their demographics and clinical features are summarized in Table 1. The sample had a mean age of 6.28 ± 1.87 years, with 67.96% of subjects being aged ≤ 6 years and 51.0% being boys. Amblyopia severity was predominantly mild-to-moderate (94.6%), with refractive amblyopia being the most prevalent subtype (63.6%). Stratified analyses (Supplementary Table S1) revealed no significant gender- or age-related differences in amblyopia severity (all p > 0.05, φ = 0.005–0.041, indicating negligible effects). However, severe amblyopia was associated with poorer BCVA in the worse eye (U=0, p<0.001, rrβ = 0.398, medium effect) and was more prevalent in the anisometropic and strabismic subtypes (χ² = 17.2, p<0.001, Cramér’s V=0.192, small effect). Maternal smoking/alcohol history was low (< 5%), and 58.4% of the caregivers had a college-level education or higher. These results indicate that the sample was representative of typical clinical amblyopia populations.
Table 1
| Characteristics | Total (N=465) |
|---|---|
| Gender (n (%)) | |
| Boy | 237 (51.0) |
| Girl | 228 (49.0) |
| Age (years) (n (%)) | |
| ≤6 | 316 (67.96) |
| >6 | 149 (32.04) |
| Family history of amblyopia (n (%)) | |
| Yes | 30 (6.5) |
| No | 435 (93.5) |
| Family history of myopia (n (%)) | |
| Yes | 87 (18.7) |
| No | 378 (81.3) |
| Parental education (n (%)) | |
| Middle school | 103 (22.2) |
| High school | 90 (19.4) |
| College or above | 272 (58.4) |
| Mother’s smoking history (n (%)) | |
| Yes | 9 (1.94) |
| No | 456 (98.06) |
| Mother’s history of alcohol consumption (n (%)) | |
| Yes | 38 (8.17) |
| No | 427 (91.83) |
| Child’s birth weight (n (%)) | |
| ≤2500 g | 69 (14.8) |
| 2500~4000 g | 376 (80.9) |
| ≥4000 g | 20 (4.3) |
| Types of amblyopia (n (%)) | |
| Ametropic amblyopia | 296 (63.6) |
| Anisometropic amblyopia | 144 (31.0) |
| Strabismic amblyopia | 25 (5.4) |
| Severity of amblyopia (n (%)) | |
| Mild to moderate | 440 (94.6) |
| Severe | 25 (5.4) |
| BCVA (Median (P25, P75)) | |
| Better eye | 0.2 (0.1,0.3) |
| Worse eye | 0.3 (0.2,0.4) |
| Subscales (Median (P25, P75)) | |
| Inattention | 0.67 (0.22,1.0) |
| Hyperactivity/Impulsivity | 0.67 (0.22,1.0) |
| Oppositional | 0.625 (0.125,1.0) |
Demographic and clinical characteristics.
Item analysis and factor correlations of the SNAP-IV
As shown in Table 2, all the factors were significantly positively correlated after Bonferroni correction (p < 0.001), with correlations ranging from moderate to strong (rs = 0.724–0.923, large effect). The factor–total correlations (rs = 0.887–0.923, large effect) were consistently greater than the correlations between factors (rs = 0.724–0.768, large effect), supporting strong internal consistency. The strongest link was observed between inattention and hyperactivity/impulsivity (rs = 0.768, 95% CI: 0.715–0.795, large effect), followed by moderate associations between inattention and oppositional behavior (rs = 0.724, 95% CI: 0.677–0.766, large effect) and between hyperactivity/impulsivity and oppositional behavior (rs = 0.739, 95% CI: 0.693–0.779, large effect). These results confirm the internal homogeneity of each factor and highlight meaningful relationships among core behavioral constructs.
Table 2
| Subscales | Inattention | Hyperactivity/Impulsivity | Oppositional |
|---|---|---|---|
| Inattention | 1.00 | ||
| Hyperactivity/Impulsivity | 0.768 (0.715,0.795) *** | 1.00 | |
| Oppositional | 0.724 (0.677,0.766) *** | 0.739 (0.693,0.779) *** | 1.00 |
| Total | 0.903 (0.885,0.919) *** | 0.923 (0.908,0.936) *** | 0.887 (0.865,0.905) *** |
Spearman correlations of the interfactor and factor-total scores.
Values are Spearman’s correlation coefficients (rs) with 95% confidence intervals (95% CI) in parentheses.
*p < 0.05; **p < 0.01; ***p < 0.001.
Internal consistency and reliability of the SNAP-IV
As demonstrated in Table 3, the reliability results for the SNAP-IV scale are presented. Cronbach’s α and split-half coefficients are retained as reliability metrics, which inherently reflect effect size-like properties for internal consistency. The Cronbach’s α for the total scale is 0.965 (95% CI: 0.958–0.972), and the Cronbach’s α values of each factor are greater than 0.90. The split-half reliability for the total scale is 0.891, and the individual factor coefficients range from 0.844–0.904. These metrics exceed the conventional psychometric thresholds (α ≥ 0.70), confirming that the SNAP-IV yields stable and reproducible scores in amblyopic children.
Table 3
| Subscales | Cronbach’s α | Split-Half reliability |
|---|---|---|
| Total | 0.965 | 0.891 |
| Inattention | 0.929 | 0.904 |
| Hyperactivity/Impulsivity | 0.925 | 0.844 |
| Oppositional | 0.928 | 0.900 |
Reliability of the SNAP-IV.
p<0.05*, p<0.01**, and p<0.001***.
Criterion-related validity with the CPRS
The correlations with the CPRS revealed strong convergent validity (Table 4). Overall, the oppositional of the SNAP-IV exhibited the strongest associations, particularly with the conduct problem of the CPRS (rs = 0.837, 95% CI: 0.807–0.863, p<0.001, large effect), indicating a close alignment between behavioral measures of oppositionality across the two instruments. Inattention was strongly correlated with both learning problems (rs = 0.808, 95% CI: 0.767–0.834, p<0.001, large effect) and conduct problems (rs = 0.719, 95% CI: 0.675–0.765, p<0.001, large effect), In contrast, correlations between the SNAP-IV subscales and the psychosomatic and anxiety factors of the CPRS were moderate (rs = 0.346–0.478, p < 0.001, medium effects), indicating that these dimensions are less directly related to core ADHD symptom domains but still significantly overlap. Collectively, these results provide robust evidence that the SNAP-IV captures behavioral dimensions that are meaningfully associated with established CPRS constructs.
Table 4
| Subscales | Inattention | Hyperactivity/Impulsivity | Oppositional |
|---|---|---|---|
| Conduct problem | 0.719 (0.675,0.765) *** | 0.710 (0.660,0.753) *** | 0.837 (0.807,0.863) *** |
| Learning problem | 0.808 (0.767,0.834) *** | 0.676 (0.622,0.724) *** | 0.677 (0.623,0.724) *** |
| Psychosomatic | 0.475 (0.389,0.536) *** | 0.423 (0.343,0.497) *** | 0.478 (0.403,0.547) *** |
| Impulsivity/Hyperactivity | 0.627 (0.567,0.681) *** | 0.673 (0.618,0.721) *** | 0.696 (0.644,0.741) *** |
| Anxiety | 0.450 (0.371,0.520) *** | 0.346 (0.261,0.426) *** | 0.456(0.378,0.527) *** |
Spearman correlations of the SNAP-IV and the CPRS.
Values are Spearman’s correlation coefficients (rs) with 95% confidence intervals (95% CI) in parentheses.
*p < 0.05; **p < 0.01; ***p < 0.001.
Confirmatory factor analysis
The initial three-factor model demonstrated suboptimal fit (χ²/(296) = 1225.6, χ²/df = 4.141, p < 0.05, RMSEA=0.082, CFI=0.90, IFI=0.90). Model refinement resulted in indices that met to acceptable levels (χ²/(291) = 1033.4, χ²/df = 3.551, p<0.05, RMSEA=0.074, CFI=0.92, IFI=0.92; Figure 1). The improved fit supports the scale’s structural validity in amblyopic populations.
Figure 1
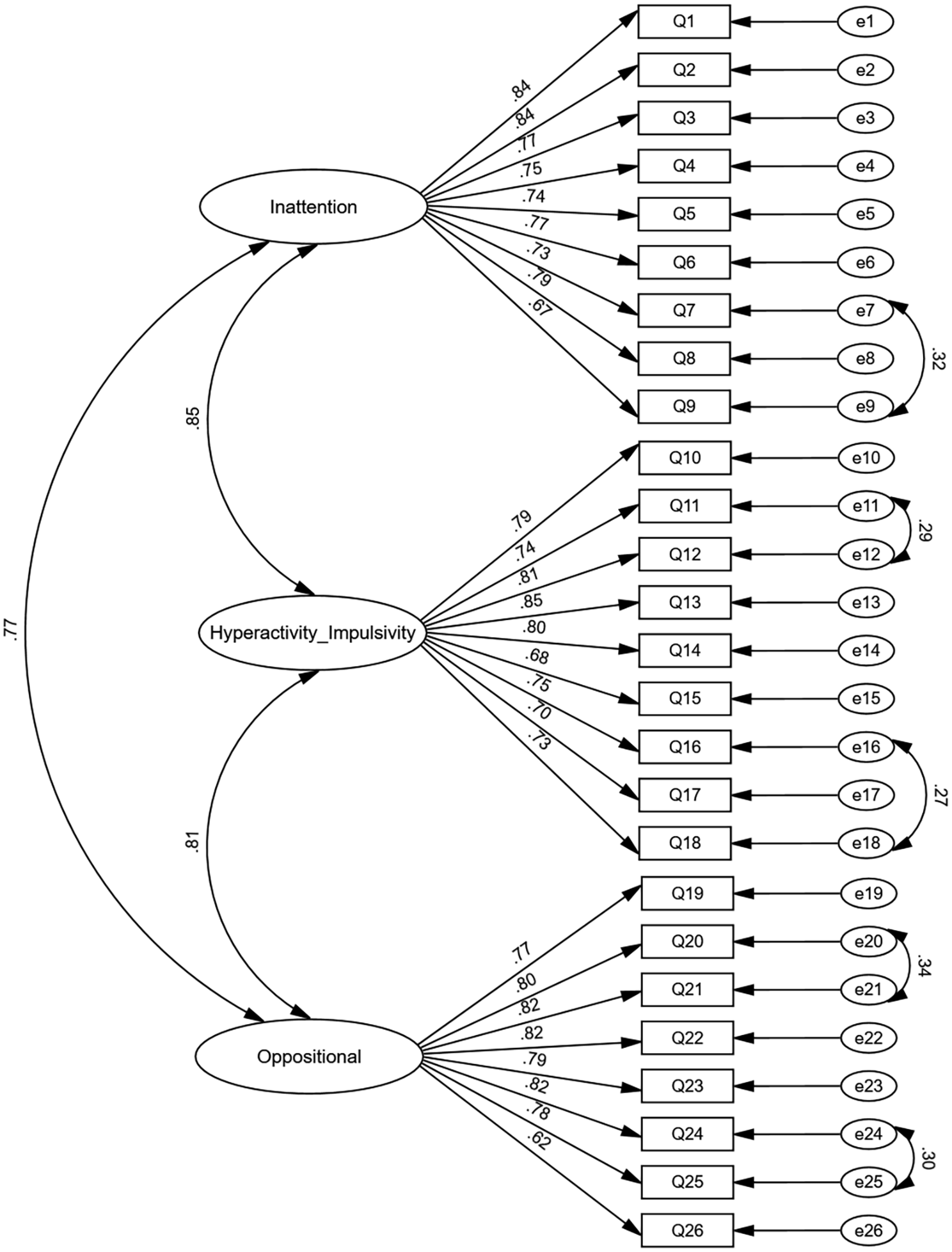
Standardized path coefficients of the SNAP-IV.
Convergent and discriminant validity
The results of the convergent validity study are presented in Table 5. Standardized factor loadings exceeded 0.5 (λ = 0.619–0.847, indicating large effects), with composite reliability (CR=0.924–0.928) and average variance explained (AVE=0.50–0.57) both meeting psychometric standards. The discriminant validity results in Table 6 show that the correlation coefficients between the factors range from 0.767 to 0.851, with some exceeding the square root of their respective AVEs. The correlation coefficient between inattention and hyperactivity/impulsivity (r =0.851) is greater than the square root value of the AVE (0.769), and the correlation coefficient between hyperactivity/impulsivity and the oppositional factor (r =0.811) is greater than the square root value of the AVE (0.762), indicating that some factors are not independent enough and that the discriminant validity needs to be improved. Furthermore, we now include maximum shared variance (MSV=0.724) and average shared variance (ASV=0.657) as supplemental effect size metrics, confirming moderate-to-high shared variance but acceptable discriminant validity per Fornell-Larcker criterion. These indices collectively suggest that while the factors are robust, discriminant validity between them requires improvement.
Table 5
| Item | Estimate | S.E. | p | AVE | CR | ||
|---|---|---|---|---|---|---|---|
| Q1 | <––– | Inattention | 0.837 | 0.591 | 0.928 | ||
| Q2 | <––– | Inattention | 0.841 | 0.044 | *** | ||
| Q3 | <––– | Inattention | 0.772 | 0.046 | *** | ||
| Q4 | <––– | Inattention | 0.754 | 0.041 | *** | ||
| Q5 | <––– | Inattention | 0.740 | 0.042 | *** | ||
| Q6 | <––– | Inattention | 0.771 | 0.044 | *** | ||
| Q7 | <––– | Inattention | 0.731 | 0.048 | *** | ||
| Q8 | <––– | Inattention | 0.790 | 0.049 | *** | ||
| Q9 | <––– | Inattention | 0.667 | 0.045 | *** | ||
| Q10 | <––– | Hyperactivity/Impulsivity | 0.794 | 0.581 | 0.925 | ||
| Q11 | <––– | Hyperactivity/Impulsivity | 0.742 | 0.043 | *** | ||
| Q12 | <––– | Hyperactivity/Impulsivity | 0.809 | 0.052 | *** | ||
| Q13 | <––– | Hyperactivity/Impulsivity | 0.847 | 0.047 | *** | ||
| Q14 | <––– | Hyperactivity/Impulsivity | 0.800 | 0.057 | *** | ||
| Q15 | <––– | Hyperactivity/Impulsivity | 0.681 | 0.058 | *** | ||
| Q16 | <––– | Hyperactivity/Impulsivity | 0.748 | 0.050 | *** | ||
| Q17 | <––– | Hyperactivity/Impulsivity | 0.698 | 0.040 | *** | ||
| Q18 | <––– | Hyperactivity/Impulsivity | 0.725 | 0.047 | *** | ||
| Q19 | <––– | Oppositional | 0.772 | 0.605 | 0.924 | ||
| Q20 | <––– | Oppositional | 0.804 | 0.055 | *** | ||
| Q21 | <––– | Oppositional | 0.820 | 0.052 | *** | ||
| Q22 | <––– | Oppositional | 0.793 | 0.052 | *** | ||
| Q23 | <––– | Oppositional | 0.793 | 0.051 | *** | ||
| Q24 | <––– | Oppositional | 0.822 | 0.054 | *** | ||
| Q25 | <––– | Oppositional | 0.782 | 0.050 | *** | ||
| Q26 | <––– | Oppositional | 0.619 | 0.040 | *** | ||
Standardized regression coefficients of the SNAP-IV.
p<0.05*, p<0.01**, and p<0.001***.
Table 6
| Variables | Inattention | Hyperactivity/Impulsivity | Oppositional |
|---|---|---|---|
| Inattention | 0.591 | ||
| Hyperactivity/Impulsivity | 0.851*** | 0.581 | |
| Oppositional | 0.767*** | 0.811*** | 0.605 |
| Square root of AVE | 0.769 | 0.762 | 0.778 |
| MSV (Maximum Shared Variance) | 0.724 | 0.724 | 0.724 |
| ASV (Average Shared Variance) | 0.657 | 0.657 | 0.657 |
Discriminant validity of the SNAP-IV.
Square root of AVE is compared with inter-factor correlations for discriminant validity. MSV and ASV are included as supplementary indicators of discriminant validity; p<0.05*, p<0.01**, and p<0.001***.
Measurement invariance
Measurement invariance for gender and age groups was evaluated via the three-factor model, with the results summarized in Table 7. ΔCFI and ΔRMSEA are reported as effect sizes for model differences (e.g., for gender scalar invariance: ΔCFI=-0.002, small effect; ΔRMSEA=-0.001, negligible effect). Both groups showed an acceptable fit in the configural model (RMSEA=0.063, CFI=0.885, RMR=0.028 for gender; RMSEA=0.063, CFI=0.886, RMR=0.331 for age). The fit of the metric, scalar, and strict factor models was similar to that of the configural model (ΔRMSEA < 0.015, ΔCFI < 0.01), thereby supporting measurement invariance across gender and age groups.
Table 7
| Model (gender) | χ2 | df | Δχ2 | Δdf | p | CFI | RMSEA | RMR | ΔCFI | ΔRMSEA |
|---|---|---|---|---|---|---|---|---|---|---|
| Model1 (configural invariance) | 1669.454 | 592 | 0.885 | 0.063 | 0.028 | |||||
| Model2 (metric invariance) | 1690.035 | 615 | 20.581 | 23 | 0.607 | 0.885 | 0.061 | 0.031 | 0 | -0.002 |
| Model3 (scalar invariance) | 1713.67 | 621 | 44.216 | 29 | 0.035 | 0.883 | 0.062 | 0.043 | -0.002 | -0.001 |
| Model4 (strict invariance) | 1770.387 | 647 | 100.933 | 55 | 0.000 | 0.88 | 0.061 | 0.044 | -0.005 | -0.002 |
| Model (age) | ||||||||||
| Model1 (configural invariance) | 1664.644 | 592 | 0.886 | 0.063 | 0.031 | |||||
| Model2 (metric invariance) | 1691.426 | 615 | 26.782 | 23 | 0.265 | 0.886 | 0.061 | 0.037 | 0 | -0.002 |
| Model3 (scalar invariance) | 1697.805 | 621 | 33.161 | 29 | 0.271 | 0.886 | 0.061 | 0.055 | 0 | -0.002 |
| Model4 (strict invariance) | 1780.282 | 647 | 115.638 | 55 | 0.000 | 0.88 | 0.062 | 0.056 | -0.006 | -0.001 |
Multigroup CFA fit indices for the SNAP-IV across gender and age.
p<0.05*, p<0.01**, and p<0.001***.
Discussions
Key findings and psychometric robustness
This study represents the first systematic psychometric evaluation of the SNAP-IV rating scale in amblyopic children at high AD/HD risk, demonstrating exceptional reliability and validity. The scale exhibited outstanding internal consistency, surpassing previous cross-cultural adaptations in Brazil (α > 0.91) and China (α =0.88–0.90) (24, 28). These findings serve to reinforce the stability of the SNAP-IV in capturing homogenous behavioral constructs across diverse populations. The findings of the factorial analysis provided further support for the construct validity of the scale, with strong correlations between factors, indicating that all items reliably discriminate their respective dimensions (40, 41).
Importantly, the observed effect sizes across the main psychometric indices ranged from medium to large, highlighting that the associations observed are not only statistically significant but also of practical and clinical importance. Convergent validity with the CPRS was robust, particularly with respect to the oppositional factor of the SNAP-IV scale, which showed a large effect size correlation with the conduct problem factor of the CPRS (rs = 0.837, p <0.001), which is consistent with evidence that children with unilateral visual impairment frequently present with heightened behavioral difficulties, including externalizing symptoms (23). Notably, large correlations between inattention and behavior problems (with learning problems and conduct problems, all p <0.001) underscore that attentional deficits exert a substantial behavioral impact in visually impaired children. Such magnitudes suggest that these relationships reflect meaningful behavioral mechanisms rather than trivial statistical findings. The large effect sizes observed support the hypothesis that attentional resource allocation deficits secondary to visual impairment, manifesting as cascading behavioral sequelae (42), thereby supporting theories of symptom overlap in neurodevelopmental disorders (43, 44). Together, these results demonstrate both statistical robustness and real-world relevance, underscoring the need for integrated interventions that addressing both visual symptoms and behavioral comorbidities in children with amblyopia.
Factor structure and measurement invariance
The three-factor model of the SNAP-IV (inattention, hyperactivity/impulsivity, oppositional) is illustrated in Figure 1. This model demonstrated strong cross-cultural adaptability with acceptable fit indices (p < 0.05) (28, 41, 45). However, initial model misfit (RMSEA=0.082) highlighted insufficient factor independence, a finding that is probably attributable to the clinical co-occurrence of AD/HD symptoms (44) and nonspecific behavioral responses to visual dysfunction (46). As depicted in Figure 1, the standardized path coefficients ranged from 0.62 to 0.85, corresponding to large effect sizes, which affirm both the statistical robustness and the practical interpretability of the model. These magnitudes indicate that items have substantial loading strength on their latent constructs, advancing SNAP-IV understanding by confirming its factor structure in amblyopic children-a previously untested domain-and supporting its use for nuanced ADHD subtyping in visual impairment contexts. A high proportion of individuals ≤6 years of age (67.96%) may attenuate age norms, but invariance tests confirmed their applicability. Similarly, the measurement invariance across gender groups further corroborated the scale’s applicability across demographic subgroups.
However, configural and metric invariance were maintained (Δχ² = 26.782, Δdf = 23, p =0.265), and the small-to-medium effect size differences observed at the intercept level (ΔRMSEA = 0.001, ΔCFI = 0.006), which may reflect variations in behavioral expression due to age and environmental factors. This aligns with developmental trends showing declining hyperactivity with increasing age (20, 24). These effects are modest yet informative, emphasizing the need for age-adjusted thresholds in clinical practice. Furthermore, small effect size differences were detected across gender in scalar and strict invariance models (both p<0.05, ΔRMSEA < 0.005, ΔCFI < 0.002), with behavioral patterns consistent with clinical features of AD/HD (47). The minimal magnitude of these differences suggests they represent true behavioral variation rather than measurement bias. The small magnitude of these differences indicates they reflect genuine behavioral variation rather than measurement bias. Cross-cultural evidence suggests that these gender differences cannot be attributed to reporter bias or differences in assessment tools (48). These insights underscore the necessity of gender-sensitive assessment protocols in pediatric populations.
Clinical and theoretical implications
The SNAP-IV scale has demonstrated strong reliability and validity across various cultural adaptations (28, 49, 50), underscoring its clinical value in assessing behavioral issues in amblyopic children. The validated reliability and validity of the SNAP-IV in this understudied population provide a critical tool for the early identification of AD/HD comorbidities in amblyopic children. Given that a high percentage of amblyopic children develop AD/HD-related behaviors (51) and that visual treatment windows is typically limited to age 7 (52), this scale offers timely clinical utility. Our findings align with transactional developmental theory (42, 53), suggesting that visual impairment disrupts attentional processes, which in turn exacerbate behavioral outcomes. The overlap between attentional difficulties and visual impairment may further complicate diagnostic processes, underscoring the need for precise, population-specific assessment protocols. This mechanistic framework justifies multidisciplinary interventions targeting both sensory and behavioral domains in children with amblyopia. From the perspective of multidisciplinary management of amblyopia, the results of this study provide a practical tool for the comprehensive assessment and intervention of children with amblyopia, ultimately leading to better long-term outcomes for these children.
Limitations and future directions
While groundbreaking, this study has several limitations. First, parent-reported data introduced potential reporter bias, as both the SNAP-IV and the CPRS were completed by caregivers (54). Second, the absence of a clinical AD/HD diagnosis group precluded sensitivity/specificity analysis. Third, the cross-sectional design provided limited insights into the temporal stability of the scale. Fourth, both the authors and the participants in this study belong to the same ethnic and cultural group, potentially influencing the results through in-group familiarity with subtle behavioral norms (42). Caution is warranted when generalizing findings to other populations. Last but still important, while the SNAP-IV/CPRS lack age/gender norms (unlike Conners-4), they were chosen for validated Chinese adaptations in pediatric cohorts and brevity for clinical feasibility. Future research should incorporate teacher and self-reports to triangulate data, longitudinal tracking to assess developmental trajectories (55, 56), and validation against gold-standard diagnostic interviews (e.g., Conners-4) (57). Additionally, optimizing items for age-specific expression (e.g., preschool vs. school-age) and incorporating neurocognitive measures (e.g., eye-tracking, fMRI) could enhance discriminative validity (58).
Conclusions
This study establishes the SNAP-IV as a reliable and valid instrument for assessing AD/HD-related behaviors in amblyopic children, filling a critical gap in developmental psychology research. While measurement invariance was largely preserved, age- and gender-related variations necessitate refined calibration for clinical use. Future advancements should prioritize longitudinal validation and multidisciplinary integration to address the complex interplay between visual impairment and behavioral comorbidities, ultimately improving long-term developmental outcomes for these vulnerable children.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the ethics committee of People’s Hospital of Guangxi Zhuang Autonomous Region (Approval No: KY-KJT-2023-285). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
LP: Data curation, Investigation, Writing – original draft. MR: Data curation, Formal analysis, Writing – original draft. YH: Data curation, Investigation, Writing – original draft. WL: Investigation, Validation, Writing – original draft. LL: Data curation, Investigation, Writing – original draft. YL: Data curation, Investigation, Writing – original draft. EL: Data curation, Investigation, Writing – original draft. MK: Investigation, Validation, Writing – original draft. QC: Data curation, Investigation, Validation, Writing – original draft. YaL: Data curation, Investigation, Writing – original draft. HL: Formal analysis, Writing – original draft. SH: Formal analysis, Writing – original draft. JZ: Conceptualization, Funding acquisition, Methodology, Writing – review & editing. FH: Methodology, Writing – review & editing. XX: Conceptualization, Funding acquisition, Methodology, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was supported by the Guangxi Key Research and Development Program (No. Guike AB23026047), Guangxi Natural Science Foundation (2024GXNSFAA010262), Guangdong Basic and Applied Basic Research Foundation (2021A1515011822), Guangxi Medical and Health Appropriate Technology Research and Development Project (2023003), and Guangxi Clinical Ophthalmic Research Center (No. Guike AD19245193). All funding parties did not have any role in the study design, conduct of this research, data analysis, or decisions in preparation or publishing of the manuscript.
Acknowledgments
The authors wish to express their sincere gratitude to Professor Jian Song for his professional native English editing, which has significantly improved the readability and quality of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1655548/full#supplementary-material
References
1
Thapar A Cooper M . Attention deficit hyperactivity disorder. Lancet (London England). (2016) 387:1240–50. doi: 10.1016/s0140-6736(15)00238-x
2
Popit S Serod K Locatelli I Stuhec M . Prevalence of attention-deficit hyperactivity disorder (ADHD): systematic review and meta-analysis. Eur Psychiatry. (2024) 67:e68. doi: 10.1192/j.eurpsy.2024.1786
3
Bozinovic K McLamb F O’Connell K Olander N Feng Z Haagensen S et al . U.S. National, regional, and state-specific socioeconomic factors correlate with child and adolescent ADHD diagnoses pre-Covid-19 pandemic. Sci Rep. (2021) 11:22008. doi: 10.1038/s41598-021-01233-2
4
Peterson BS Trampush J Maglione M Bolshakova M Rozelle M Miles J et al . Treatments for ADHD in children and adolescents: A systematic review. Pediatrics. (2024) 153:e2024065787. doi: 10.1542/peds.2024-065787
5
Posner J Polanczyk GV Sonuga-Barke E . Attention-deficit hyperactivity disorder. Lancet (London England). (2020) 395:450–62. doi: 10.1016/s0140-6736(19)33004-1
6
Mohr-Jensen C Steinhausen HC . A meta-analysis and systematic review of the risks associated with childhood attention-deficit hyperactivity disorder on long-term outcome of arrests, convictions, and incarcerations. Clin Psychol Rev. (2016) 48:32–42. doi: 10.1016/j.cpr.2016.05.002
7
Kim M Lee S Lee JE Kim JH Ha EK Han M et al . A nationwide cohort study on the risk of ADHD in children with amblyopia mediated by fine motor skill impairment in East Asia. Sci Rep. (2022) 12:6932. doi: 10.1038/s41598-022-10845-1
8
Li YP Zhou MW Forster SH Chen SY Qi X Zhang HM et al . Prevalence of amblyopia among preschool children in central south China. Int J Ophthalmol. (2019) 12:820–5. doi: 10.18240/ijo.2019.05.19
9
Hu B Liu Z Zhao J Zeng L Hao G Shui D et al . The global prevalence of amblyopia in children: A systematic review and meta-analysis. Front Pediatr. (2022) 10:819998. doi: 10.3389/fped.2022.819998
10
Su CC Tsai CY Tsai TH Tsai IJ . Incidence and risk of attention-deficit hyperactivity disorder in children with amblyopia: A nationwide cohort study. Clin Exp Ophthalmol. (2019) 47:259–64. doi: 10.1111/ceo.13465
11
Ho JD Sheu JJ Kao YW Shia BC Lin HC . Associations between attention-deficit/hyperactivity disorder and ocular abnormalities in children: A population-based study. Ophthalmic Epidemiol. (2020) 27:194–9. doi: 10.1080/09286586.2019.1704795
12
Fu Z Hong H Su Z Lou B Pan CW Liu H . Global prevalence of amblyopia and disease burden projections through 2040: A systematic review and meta-analysis. Br J Ophthalmol. (2020) 104:1164–70. doi: 10.1136/bjophthalmol-2019-314759
13
Hubel DH Wiesel TN LeVay S . Plasticity of ocular dominance columns in monkey striate cortex. Philos Trans R Soc London Ser B Biol Sci. (1977) 278:377–409. doi: 10.1098/rstb.1977.0050
14
Mortazavi M Aigner KM Antono JE Gambacorta C Nahum M Levi DM et al . Neural correlates of visual spatial selective attention are altered at early and late processing stages in human amblyopia. Eur J Neurosci. (2021) 53:1086–106. doi: 10.1111/ejn.15024
15
Niechwiej-Szwedo E Colpa L Wong AMF . Visuomotor behaviour in amblyopia: deficits and compensatory adaptations. Neural plasticity. (2019) 2019:6817839. doi: 10.1155/2019/6817839
16
Wong AM . New concepts concerning the neural mechanisms of amblyopia and their clinical implications. Can J Ophthalmol J canadien d’ophtalmologie. (2012) 47:399–409. doi: 10.1016/j.jcjo.2012.05.002
17
Randhawa S Griffiths N O’Brien P Panter C Boparai K Harrad R et al . Qualitative exploration of the visual function impairments and health-related quality of life impacts of amblyopia in adult and pediatric populations. Ophthalmol Ther. (2023) 12:2505–28. doi: 10.1007/s40123-023-00751-8
18
Gupte-Singh K Singh RR Lawson KA . Economic burden of attention-deficit/hyperactivity disorder among pediatric patients in the United States. Value Health. (2017) 20:602–9. doi: 10.1016/j.jval.2017.01.007
19
Malvankar-Mehta MS Wilson R Leci E Hatch K Sharan S . Cost and quality of life of overlooked eye care needs of children. Risk Manage healthcare Policy. (2018) 11:25–33. doi: 10.2147/rmhp.s141659
20
Conners CK Sitarenios G Parker JD Epstein JN . The revised conners’ Parent rating scale (Cprs-R): factor structure, reliability, and criterion validity. J Abnormal Child Psychol. (1998) 26:257–68. doi: 10.1023/a:1022602400621
21
Neo WS Suzuki T Kelleher BL . Structural validity of the child behavior checklist (Cbcl) for preschoolers with neurogenetic syndromes. Res Dev Disabil. (2021) 109:103834. doi: 10.1016/j.ridd.2020.103834
22
Sibley MH . Empirically-informed guidelines for first-time adult Adhd diagnosis. J Clin Exp Neuropsychol. (2021) 43:340–51. doi: 10.1080/13803395.2021.1923665
23
Celano M Cotsonis GA Hartmann EE Drews-Botsch C . Behaviors of children with unilateral vision impairment in the infant Aphakia treatment study. J AAPOS. (2016) 20:320–5. doi: 10.1016/j.jaapos.2016.04.008
24
Gau SS Shang CY Liu SK Lin CH Swanson JM Liu YC et al . Psychometric properties of the Chinese version of the Swanson, Nolan, and Pelham, version iv scale - parent form. Int J Methods Psychiatr Res. (2008) 17:35–44. doi: 10.1002/mpr.237
25
Faganello IB Zomerfeld MD de Oliveira RE da Paixão TC Gemelli H de Carvalho MD et al . Application of snap-iv scale on children with academic underachievement. SBN Conf. (2023) A064. doi: 10.1055/s-0043-1774483
26
Tamm L Denton CA Epstein JN Schatschneider C Taylor H Arnold LE et al . Comparing treatments for children with ADHD and word reading difficulties: A randomized clinical trial. J consulting Clin Psychol. (2017) 85:434–46. doi: 10.1037/ccp0000170
27
Lundervold AJ Sørensen L Posserud MB Hysing M . Low persistence of inattention symptoms from childhood to adolescence: A population-based study. J attention Disord. (2023) 27:1532–9. doi: 10.1177/10870547231187147
28
Costa DS de Paula JJ Malloy-Diniz LF Romano-Silva MA Miranda DM . Parent snap-iv rating of attention-deficit/hyperactivity disorder: accuracy in a clinical sample of ADHD, validity, and reliability in a Brazilian sample. Jornal pediatria. (2019) 95:736–43. doi: 10.1016/j.jped.2018.06.014
29
de Vet HCW Terwee CB Mokkink LB Knol DL . Measurement in Medicine: A Practical Guide. Cambridge: Cambridge University Press (2011).
30
Strabismus; CAfPOa Association POaSGoCO . Expert consensus on prevention and treatment of amblyopia in children. [Zhonghua yan ke za zhi] Chin J Ophthalmol. (2021) 57:336–40. doi: 10.3760/cma.j.cn112142-20210109-00014
31
Child ADHD snap iv. Available online at: https://greenspacehealth.com/en-ca/child-adhd-snap-iv-26/ (Accessed April 18, 2025).
32
Bussing R Fernandez M Harwood M Wei H Garvan CW Eyberg SM et al . Parent and teacher snap-iv ratings of attention deficit hyperactivity disorder symptoms: psychometric properties and normative ratings from a school district sample. Assessment. (2008) 15:317–28. doi: 10.1177/1073191107313888
33
Lúcio PS Eid M Cogo-Moreira H Puglisi ML Polanczyk GV . Investigating the measurement invariance and method-trait effects of parent and teacher snap-iv ratings of preschool children. Child Psychiatry Hum Dev. (2022) 53:489–501. doi: 10.1007/s10578-021-01145-2
34
Goyette CH Conners CK Ulrich RF . Normative data on revised conners parent and teacher rating scales. J Abnormal Child Psychol. (1978) 6:221–36. doi: 10.1007/bf00919127
35
Cella D Lenderking WR Chongpinitchai P Bushmakin AG Dina O Wang L et al . Functional assessment of chronic illness therapy-fatigue is a reliable and valid measure in patients with active ankylosing spondylitis. J patient-reported outcomes. (2022) 6:100. doi: 10.1186/s41687-022-00508-0
36
Strömbeck J Heyne D Ferrer-Wreder L Alanko K . Reliability and validity of the Swedish version of the inventory of school attendance problems (Isap). Eur Child Adolesc Psychiatry. (2024) 34:2069–82. doi: 10.1007/s00787-024-02618-0
37
Yang R Zhou H Liu J Wang Y Zhang Y Wang Y et al . Psychometric properties of the caregiver strain questionnaire among Chinese parents of children with ADHD or ASD. Gen Psychiatry. (2021) 34:e100246. doi: 10.1136/gpsych-2020-100246
38
Fornell C Larcker DF . Structural equation models with unobservable variables and measurement error: algebra and statistics. J Marketing Res. (1981) 18:382–8. doi: 10.1177/002224378101800313
39
Riglin L Dennison C Martin J Tseliou F Armitage JM Shakeshaft A et al . Emotional Problems across Development: Examining Measurement Invariance across Childhood, Adolescence and Early Adulthood. Eur Child Adolesc Psychiatry. (2024) 33:4237–45. doi: 10.1007/s00787-024-02461-3
40
Zieff MR Hoogenhout M Eastman E Christ BU Galvin A de Menil V et al . Validity of the snap-iv for ADHD assessment in South African children with neurodevelopmental disorders. J Autism Dev Disord. (2023) 53:2851–62. doi: 10.1007/s10803-022-05530-1
41
Abhayaratna HC Ariyasinghe DI Ginige P Chandradasa M Hansika KS Fernando A et al . Psychometric properties of the sinhala version of the swanson, nolan, and pelham rating scale (Snap-iv) parent form in healthy children and children with ADHD. Asian J Psychiatry. (2023) 83:103542. doi: 10.1016/j.ajp.2023.103542
42
Verghese P McKee SP Levi DM . Attention deficits in amblyopia. Curr Opin Psychol. (2019) 29:199–204. doi: 10.1016/j.copsyc.2019.03.011
43
Frick PJ Nigg JT . Current issues in the diagnosis of attention deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder. Annu Rev Clin Psychol. (2012) 8:77–107. doi: 10.1146/annurev-clinpsy-032511-143150
44
Willcutt EG Nigg JT Pennington BF Solanto MV Rohde LA Tannock R et al . Validity of dsm-iv attention deficit/hyperactivity disorder symptom dimensions and subtypes. J Abnormal Psychol. (2012) 121:991–1010. doi: 10.1037/a0027347
45
Nazeer N Rohanachandra Y Prathapan S . Prevalence of ADHD in primary school children, in Colombo district, Sri Lanka. J attention Disord. (2022) 26:1130–8. doi: 10.1177/10870547211058704
46
Black AA Wood JM Hoang S Thomas E Webber AL . Impact of amblyopia on visual attention and visual search in children. Invest Ophthalmol Visual Sci. (2021) 62:15. doi: 10.1167/iovs.62.4.15
47
Lambek R Trillingsgaard A Kadesjö B Damm D Thomsen PH . Gender differences on the five to fifteen questionnaire in a non-referred sample with inattention and hyperactivity-impulsivity and a clinic-referred sample with hyperkinetic disorder. Scandinavian J Psychol. (2010) 51:540–7. doi: 10.1111/j.1467-9450.2010.00825.x
48
Crijnen AA Achenbach TM Verhulst FC . Problems reported by parents of children in multiple cultures: the child behavior checklist syndrome constructs. Am J Psychiatry. (1999) 156:569–74. doi: 10.1176/ajp.156.4.569
49
Inoue Y Ito K Kita Y Inagaki M Kaga M Swanson JM . Psychometric properties of Japanese version of the Swanson, Nolan, and Pelham, version-iv scale-teacher form: A study of school children in community samples. Brain Dev. (2014) 36:700–6. doi: 10.1016/j.braindev.2013.09.003
50
Jusoh M Dzulkarnain AAA Rahmat S Musa R Che Azemin MZ . Cross-cultural translation and validation of the Malay version of the Swanson, Nolan, and Pelham parent rating scale of attention deficit hyperactivity disorders symptoms among Malaysian probands: A preliminary study. Asia-Pacific Psychiatry. (2021) 13:e12414. doi: 10.1111/appy.12414
51
Webber AL . The functional impact of amblyopia. Clin Exp optometry. (2018) 101:443–50. doi: 10.1111/cxo.12663
52
Sengpiel F . Plasticity of the visual cortex and treatment of amblyopia. Curr biology: CB. (2014) 24:R936–r40. doi: 10.1016/j.cub.2014.05.063
53
Sameroff AJ Mackenzie MJ . Research strategies for capturing transactional models of development: the limits of the possible. Dev Psychopathol. (2003) 15:613–40. doi: 10.1017/s0954579403000312
54
Weden MM Brownell PB Rendall MS Lau C Fernandes M Nazarov Z . Parent-reported height and weight as sources of bias in survey estimates of childhood obesity. Am J Epidemiol. (2013) 178:461–73. doi: 10.1093/aje/kws477
55
Bosch R Pagerols M Rivas C Sixto L Bricollé L Español-Martín G et al . Neurodevelopmental disorders among Spanish school-age children: prevalence and sociodemographic correlates. psychol Med. (2022) 52:3062–72. doi: 10.1017/s0033291720005115
56
Canals J Morales-Hidalgo P Jané MC Domènech E . ADHD prevalence in Spanish preschoolers: comorbidity, socio-demographic factors, and functional consequences. J attention Disord. (2018) 22:143–53. doi: 10.1177/1087054716638511
57
Peterson BS Trampush J Brown M Maglione M Bolshakova M Rozelle M et al . Tools for the diagnosis of ADHD in children and adolescents: A systematic review. Pediatrics. (2024) 153:e2024065854. doi: 10.1542/peds.2024-065854
58
Joly O Frankó E . Neuroimaging of amblyopia and binocular vision: A review. Front Integr Neurosci. (2014) 8:62. doi: 10.3389/fnint.2014.00062
Summary
Keywords
SNAP-IV, validation, reliability, amblyopia, AD/HD, children
Citation
Pan L, Ru M, Huang Y, Luo W, Li L, Luo Y, Lin E, Kong M, Chen Q, Luo Y, Liu H, Huang S, Zeng J, Han F and Xiao X (2025) Psychometric validation of the SNAP-IV rating scale in amblyopic children at high AD/HD risk: structural validity and measurement invariance. Front. Psychiatry 16:1655548. doi: 10.3389/fpsyt.2025.1655548
Received
28 June 2025
Accepted
09 October 2025
Published
28 October 2025
Volume
16 - 2025
Edited by
Eduardo Fernández-Jiménez, European University of Madrid, Spain
Reviewed by
Lorenz S. Neuwirth, State University of New York at Old Westbury, United States
Jane Wotherspoon, Queensland University of Technology, Australia
Updates
Copyright
© 2025 Pan, Ru, Huang, Luo, Li, Luo, Lin, Kong, Chen, Luo, Liu, Huang, Zeng, Han and Xiao.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Xiao, xiaoxi3891@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.