- 1Department of Radiology, Affiliated Hospital of North Sichuan Medical College, Nanchong, China
- 2Department of Radiology, Nanchong Hospital of Traditional Chinese Medicine, Nanchong, China
Background: Magnetic resonance imaging (MRI) exams often induce higher levels of patient anxiety compared to other routine examinations due to factors such as enclosed spaces, prolonged immobility, and noise interference. This anxiety may interfere with cognitive function and reduce patients’ willingness to adhere to medical instructions. However, previous research has seldom investigated the impact of MRI anxiety on patients’ treatment adherence.
Method: To address this gap, the current study employs a convenience sampling method to select 495 patients who underwent MRI examinations at a tertiary hospital in Sichuan Province between April and June 2025. We utilize the MRI Anxiety Scale, Loss Aversion Scale, Information Avoidance Scale, and Treatment Adherence Scale to conduct our investigation. Based on the Information asymmetry theory, this study constructs a structural equation model to analyze the relationship between MRI anxiety and treatment adherence, as well as the underlying mechanisms.
Result: The results show that MRI anxiety is significantly negatively correlated with treatment adherence and significantly positively correlated with both loss aversion and information avoidance. Loss aversion and information avoidance partially mediate the association between MRI anxiety and treatment adherence. The findings suggest that higher levels of MRI anxiety are associated with lower treatment adherence, with loss aversion and information avoidance behaviors potentially contributing to this relationship.
Conclusion: Therefore, clinical practice should include targeted interventions addressing loss aversion and information avoidance, such as optimizing risk communication strategies and providing structured informational support, to alleviate anxiety and improve treatment adherence, thereby providing a theoretical foundation and practical pathway to enhance MRI examination outcomes.
1 Introduction
Magnetic Resonance Imaging (MRI) is an imaging technique that reconstructs signals generated by the resonance of atomic nuclei in a magnetic field to produce images of the body’s internal structures and abnormalities (1, 2). In recent years, the psychological anxiety induced by MRI examinations, characterized by enclosed environments, loud noises, and prolonged examination times, has garnered significant attention from scholars (3, 4). For example, Oktay et al. (5) found that audiovisual interventions can effectively reduce MRI anxiety and improve image quality. Previous studies have focused on interventions to alleviate MRI anxiety to reduce patients’ psychological discomfort and pain and enhance image quality (6–8). However, despite these contributions, the impact of MRI anxiety on patients’ adherence to treatment has not received adequate attention. This oversight is unfortunate, as this influence may extend throughout the examination and subsequent treatment phases. Specifically, pre-examination anxiety may intensify patients’ perceived threat of the MRI environment, leading to behavioral avoidance such as hesitation, repeated reassurance-seeking, or requests to postpone the examination. These behaviors represent an attempt to regain a sense of control under uncertainty, yet paradoxically amplify cognitive and emotional distress, increasing the likelihood of examination refusal or incomplete cooperation (9). Some patients may even experience physical reactions due to anxiety, making it difficult to complete the examination, leading to interruptions or delays (10). During the examination, anxiety can distract patients’ attention, making it harder for them to remain still or follow instructions, potentially affecting image quality and necessitating repeated scans, which further increases patients’ psychological and financial burdens (11). Post-examination anxiety may manifest as excessive concern about the results, leading patients to repeatedly search for information online or through non-professional channels, entering a vicious cycle of information overload, misinterpretation, and escalating anxiety. In extreme cases, fear of being diagnosed with a severe condition may cause patients to avoid receiving reports or evade communication with physicians about the results. Particularly in the management of chronic diseases, cancer treatment, and neurological disorders, where the frequency and importance of MRI examinations are increasing (12), investigating the relationship between MRI anxiety and treatment adherence becomes even more critical.
Treatment adherence refers to the extent to which patients follow medical instructions for treatment and management (13, 14). Poor adherence can lead to adverse consequences, such as disease progression, increased cardiovascular risk, worsening health conditions, and hindered social integration (15, 16). Numerous studies have proposed targeted interventions from various perspectives, including psychological education, pharmacological interventions, mobile health applications, telemedicine, wearable devices (17, 18). For example, Butler et al. (19) found that using digital health technologies can effectively enhance patients’ treatment adherence. However, the impact of anxiety caused by medical devices and examinations on treatment adherence, particularly in the context of MRI, has not been adequately explored. In the MRI context, treatment adherence encompasses not only whether patients can successfully complete the MRI examination but also their subsequent adherence to treatment and follow-up based on the examination results. Patients’ anxiety may lead to refusal to cooperate with the examination, potentially resulting in unclear or distorted images that affect diagnostic accuracy (9). Additionally, for minor, early-stage, or special types of lesions, accurate detection of their size and location through MRI requires high patient adherence (20, 21). Despite the close relationship between MRI anxiety and treatment adherence, previous research has rarely analyzed or discussed this connection. Therefore, this study attempts to address the following questions: (1) Does MRI anxiety have a negative impact on patients’ treatment adherence? (2) What internal mechanisms mediate the relationship between MRI anxiety and treatment adherence?
Loss aversion theory provides a crucial framework for understanding MRI anxiety and its behavioral consequences. Loss aversion refers to the phenomenon where individuals are more sensitive to losses than to gains of the same magnitude (22, 23). This psychological tendency is particularly pronounced in medical decision-making, especially in situations involving invasive procedures or treatments. In other words, in medical contexts, patients tend to focus more on potential negative outcomes than on potential benefits (24), a tendency that significantly impacts decision quality and treatment adherence. For example, Reitich-Stolero et al. (25) noted that loss aversion in medical decision-making often stems from individuals’ heightened sensitivity to unknown risks and short-term discomfort. Therefore, in the context of imaging examinations, patients often overemphasize the discomfort or potential risks associated with the procedure, leading to excessive anxiety or irrational refusal of necessary examinations (26). In essence, MRI anxiety can be viewed as a fear of potential “losses,” such as losses in health, safety, or control. When patients undergo MRI examinations, they may associate the process with the potential revelation of unfavorable diagnoses, leading to negative expectations about their future health. This heightened sensitivity to loss directly influences patients’ psychological states and behavioral choices, thereby affecting their adherence to treatment protocols.
Information avoidance is the tendency for individuals to actively avoid exposure to information related to potential threats or negative outcomes (27, 28). While information avoidance may alleviate short-term anxiety, its long-term effects can negatively impact health behaviors (29). Recent research in the field of psychological health has revealed the complex role of information avoidance in health-related decision-making (30, 31). Studies have shown that information avoidance is significantly positively correlated with psychological distress and can indirectly lower individuals’ sense of control over health threats by delaying information processing and weakening problem-solving abilities, thereby influencing health behavior choices and execution (32–34). In the context of MRI examinations, the uncertainty of the examination process and the potential for painful or uncomfortable experiences, coupled with the possibility of revealing health issues, make patients more prone to information avoidance, thereby inducing anxiety. According to Emotion Regulation Theory, individuals consciously or unconsciously modify the onset, intensity, and expression of their emotions to maintain psychological equilibrium (35, 36). In the MRI context, anxiety activates regulatory mechanisms such as avoidance, enabling individuals to temporarily reduce emotional discomfort by minimizing exposure to threatening information. However, this behavior can lead to misunderstandings or underestimation of examination results, diminishing patients’ trust in diagnostic findings and their acceptance of treatment recommendations (37). Furthermore, information avoidance may exacerbate MRI anxiety, thereby negatively impacting subsequent treatment adherence. Additionally, information avoidance may weaken patients’ sense of control over their condition (38), indirectly influencing their cognitive evaluation of and behavioral willingness to adhere to treatment recommendations.
According to information asymmetry theory, asymmetric distribution of information in decision-making processes leads to systematic biases in choice, often stemming from misjudgments of risk and selective use of information (39, 40). In the context of MRI examinations, information asymmetry primarily manifests in patients’ uncertainty about the examination process, result interpretation, and subsequent treatment options. Based on this, patients’ uncertainty about the MRI process and its outcomes can activate loss aversion psychology, influencing their information processing patterns and making them overly sensitive to potential negative outcomes (41). This heightened sensitivity generates strong psychological discomfort, prompting patients to adopt information avoidance strategies (42), such as selectively avoiding information related to the examination or refraining from deeper understanding of examination details, to temporarily alleviate anxiety. However, information avoidance is not merely a passive behavior but rather an active process of selectively filtering information sources or avoiding in-depth exploration of examination details. While this behavior may reduce short-term anxiety, it can lead to long-term distortions in patients’ understanding of the examination’s purpose, process, and outcomes, thereby influencing their cognitive evaluation of and behavioral willingness to adhere to treatment recommendations.
Based on the above analysis, this study proposes the following hypotheses:
H1: MRI anxiety is negatively associated with patients’ treatment adherence.
H2: Loss aversion significantly mediates the association between MRI anxiety and treatment adherence.
H3: Information avoidance significantly mediates the association between MRI anxiety and treatment adherence.
H4: Loss aversion and information avoidance exhibit a significant chain mediation in the association between MRI anxiety and treatment adherence.
2 Methods
2.1 Participants
To validate the four hypotheses proposed, this study employed a convenience sampling method to collect data in the Radiology Department of a tertiary Grade A hospital in Sichuan Province. Participants were selected based on their availability and willingness to participate during their scheduled MRI examinations, as this approach was feasible given the clinical setting and time constraints (43). This non-probability sampling method was chosen to ensure adequate sample size and diversity within the study period (April to June 2025), though it may limit the generalizability of findings to broader populations. Prior to data collection, all measurement scales were developed into both electronic and paper questionnaires. These were distributed to professional clinical doctors and the Chief of the Radiology Department for evaluation and revision. Subsequently, the research team communicated the purpose, risks, and benefits of the study to the Chief of the Radiology Department. Upon obtaining consent, data collection commenced.
Sample size calculation. The minimum sample size was calculated using G*power 3.1 software (44). This study selected an F-test with a significance level (α) of 0.05, a desired power (1-β) of 0.8, and an effect size (f²) of 0.15. The results indicated that a minimum of 119 participants was required.
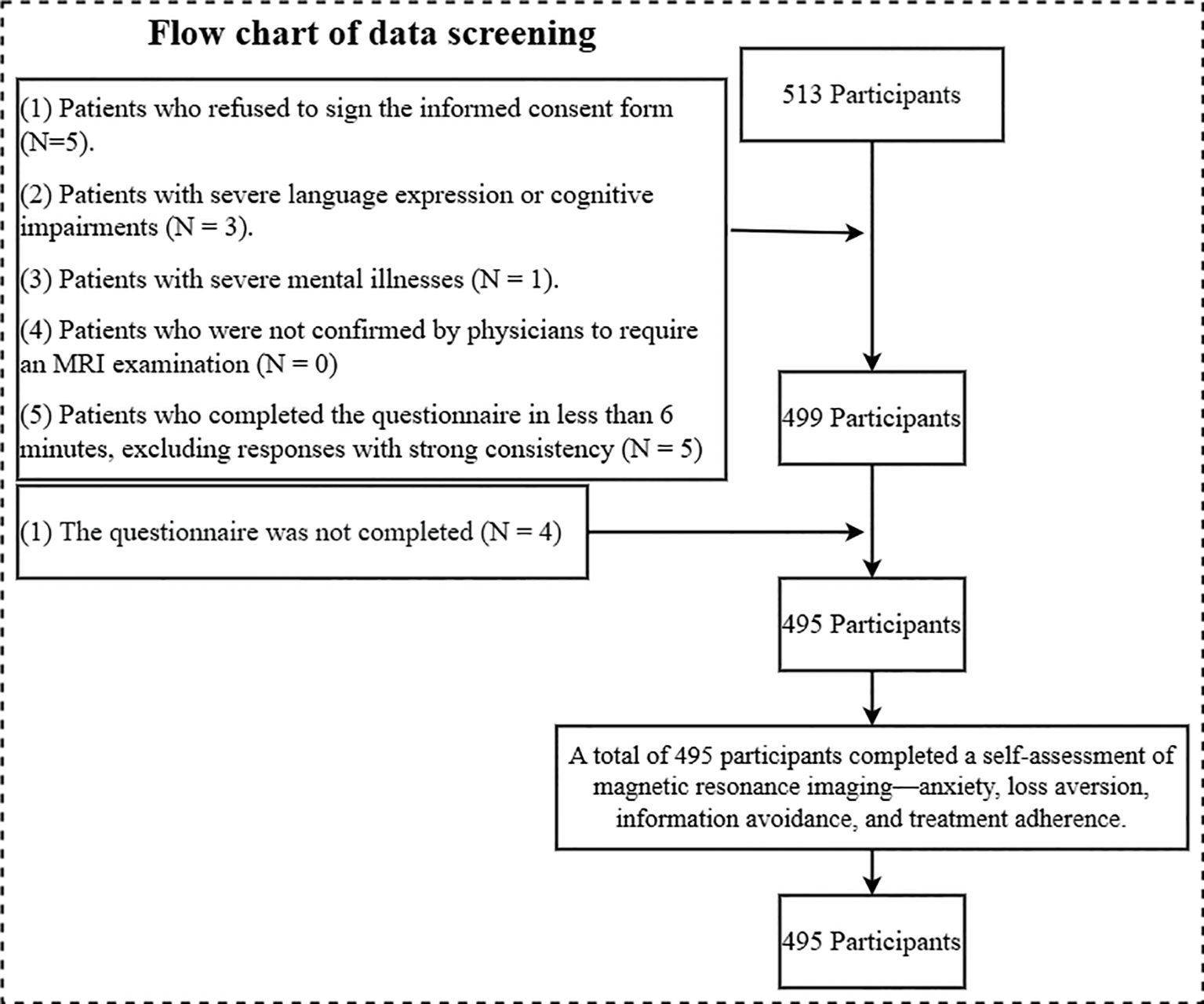
Data collection process: Patients who could use mobile electronic devices completed the electronic questionnaire, while those who could not use the paper-based version. During this process, each patient was informed about the risks, benefits, and procedures of the study to ensure their right to informed consent. After obtaining the patients’ signed consent forms, they proceeded to complete the questionnaires. Based on this process, a total of 513 patients were recruited for this survey, meeting the minimum sample size requirement.
Exclusion criteria: (1) patients who refused to sign the informed consent; (2) patients with severe language, cognitive or psychiatric impairment, unable to understand study instructions or independently complete questionnaires; (3) patients with severe mental disorders such as schizophrenia or severe bipolar disorder confirmed by psychiatric history or clinical evaluation; (4) patients who need MRI examination without physician confirmation; and (5) Patients who completed the questionnaire within 6 minutes were excluded from the responses with strong consistency. Severe impairment was defined as significant impairment in communication or cognitive function, such as the inability to respond coherently in patients with advanced dementia or severe aphasia (45, 46). Using Mini-Mental State Examination (MMSE), the patient’s score was less than 10 (47, 48). During the preexamination consultation, a brief cognitive screening using the MMSE was performed by a radiologist, supplemented by a review of medical records, for assessment. Patients with MMSE scores of 19-23 (indicating mild cognitive impairment) (49, 50) were included if they could provide informed consent and complete the questionnaire without assistance, as this enhances representativeness of the target population undergoing MRI. Patients with MMSE scores ≥24 were considered cognitively normal (51, 52). Given the potential variability in response accuracy due to mild cognitive or communication impairments, we excluded patients with communication difficulties from the study. Patients with moderate cognitive impairment (MMSE score of 11 to 18) were assigned a value of 1, those with mild cognitive impairment (MMSE score of 19 to 23) were assigned a value of 2, and those with normal cognitive function (MMSE score of 24 to 30) were assigned a value of 3; this category of patients was applied to subsequent analyses.
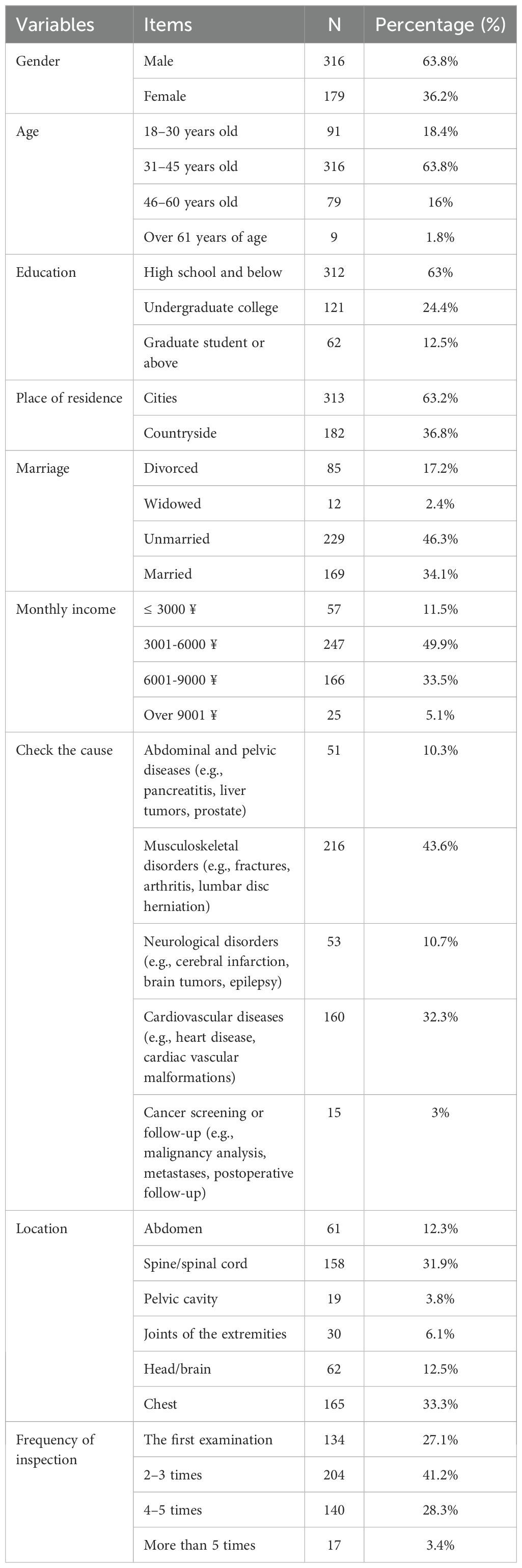
Based on the above exclusion criteria, 18 participants were excluded during the data cleaning phase, with the specific exclusion process and numbers detailed in Figure 1. The final sample size was 495, with an effective response rate of 96.49%. Among these, there were 316 male patients and 179 female patients. Detailed demographic information is presented in Table 1.
2.2 Research tools
2.2.1 Magnetic resonance imaging - anxiety scale
The Magnetic Resonance Imaging Anxiety Scale, developed by Ahlander et al. (53), consists of 15 measurement items designed to assess patients’ anxiety related to magnetic resonance imaging. Each item uses a 5-point Likert scale, ranging from 1 (“strongly disagree”) to 5 (“strongly agree”). Higher scores indicate greater anxiety levels regarding MRI. This scale has been widely applied to Chinese patient populations, demonstrating good cultural adaptability (54). In this study, the Cronbach’s α value for this scale was 0.904. Confirmatory factor analysis indicated good structural validity (CMIN/DF = 3.304, GFI = 0.917, AGFI = 0.890, RMSEA = 0.068, CFI = 0.924, TLI = 0.912).
2.2.2 Loss aversion scale
The Loss Aversion Scale was adapted from Lam and Lin (55), originally developed to assess loss aversion in the context of cancer fear and screening behaviors. In the original scale, items focused on “cancer” as the potential loss domain; for this study, “cancer” was replaced with “potential negative outcomes from the MRI examination” to align with the MRI-specific context, capturing patients’ sensitivity to perceived losses such as health deterioration, loss of control, or disruption to daily life revealed by MRI results. This adaptation maintains the scale’s focus on how individuals weigh potential losses more heavily than equivalent gains, manifesting as reluctance to engage with threatening scenarios to preserve current psychological gains (e.g., hope or normalcy).
The scale consists of 4 items, each rated on a 5-point Likert scale ranging from 1 (“strongly disagree”) to 5 (“strongly agree”), with higher scores indicating greater loss aversion. The adapted items are: (1) I would rather not think about potential negative outcomes from the MRI examination because not knowing helps me maintain hope; (2) I would rather not think about potential negative outcomes from the MRI examination and enjoy the life that I have; (3) Being constantly reminded of potential negative outcomes from the MRI examination makes me nervous about my own health condition; (4) Being diagnosed with a condition based on the MRI examination means I would have to stop all activities to seek treatment.
These items relate to the construct of loss aversion, as defined in the introduction (individuals are more sensitive to losses than to gains of the same magnitude) (22, 23), by operationalizing it in health decision-making contexts. Rooted in prospect theory Kai-Ineman and Tversky (56), loss aversion leads to status quo bias, where individuals avoid actions or thoughts that risk losses (e.g., confronting bad MRI results, which could “lose” hope or lifestyle) despite potential gains (e.g., early intervention). Unlike traditional behavioral paradigms using gambles (e.g., preferring no change over a 50% chance of gain/loss to reveal aversion), this self-report scale captures cognitive manifestations in real-world health scenarios, where loss aversion influences avoidance of diagnostic processes to prevent perceived asymmetrical losses. This adaptation is theoretically justified in health psychology, as loss aversion in medical contexts often amplifies fear of negative outcomes, reducing adherence (Tamar 25).
Importantly, while some items involve “not thinking about” threats, which may superficially resemble information avoidance (active dodging of info to reduce distress), the constructs are distinct: loss aversion reflects an emotional bias in valuing losses over gains, leading to broader decision biases, whereas information avoidance is a specific cognitive strategy. The scale’s mediation role in the SEM (distinct from information avoidance paths) empirically supports this separation.
In this study, the Cronbach’s α value for the adapted Loss Aversion Scale was 0.760, indicating acceptable internal consistency. Confirmatory factor analysis supported good structural validity (CMIN/DF = 2.193, GFI = 0.996, AGFI = 0.979, RMSEA = 0.049, CFI = 0.995, TLI = 0.985), confirming the scale’s suitability for assessing loss aversion in the MRI context.
2.2.3 Information avoidance scale
The Information Avoidance Scale was developed and validated by Howell and Shepperd (57). The scale consists of 8 measurement items specifically designed to assess information avoidance related to MRI examinations. This scale has been widely applied to Chinese patient populations, for example, in Gu et al. (58), where it was used to analyze health information avoidance among patients undergoing mindfulness interventions. Thus, it demonstrated good cultural adaptability and was deemed appropriate for assessing information avoidance in MRI contexts. In this study, blanks were filled with “the results of the MRI examination” to focus on MRI-specific avoidance, without referencing participants’ exact diseases (e.g., cancer, brain damage) for generalizability across diverse conditions (Table 1). Example items: (1) “I would rather not know the results of the MRI examination”; (2) “I would avoid learning the results of the MRI examination”; (3) “Even if it will upset me, I want to know the results of the MRI examination” (reverse coded); (4) “When it comes to the results of the MRI examination, sometimes ignorance is bliss”; (5) “I want to know the results of the MRI examination” (reverse coded); (6) “I can think of situations in which I would rather not know the results of the MRI examination”; (7) “It is important to know the results of the MRI examination” (reverse coded); (8) “I want to know the results of the MRI examination immediately” (reverse coded). Each item uses a 5-point Likert scale (1 = “strongly disagree,” 5 = “strongly agree”). Higher scores indicate a stronger tendency to avoid information. In this study, the Cronbach’s α value for this scale was 0.870. Confirmatory factor analysis indicated good structural validity (CMIN/DF = 1.772, GFI = 0.983, AGFI = 0.970, RMSEA = 0.040, CFI = 0.989, TLI = 0.985).
2.2.4 Treatment adherence scale
The Treatment Adherence Scale was adapted from the Chinese version of the Morisky Medication Adherence Scale-8, as validated by Zhao et al. (59) for assessing warfarin adherence in Chinese patients. The MMAS-8 is originally based on Morisky et al. (60), a foundational tool for measuring self-reported adherence, with strong psychometric properties (original internal consistency α = 0.83, predictive validity for clinical outcomes). Although Morisky et al. (61), which further validated the scale, was retracted in 2023 due to intellectual property disputes, the core MMAS-8 items remain widely used and psychometrically sound in adapted forms, as in Wang et al. (62). In this study, the scale was modified to evaluate patients’ adherence to MRI-related treatment instructions, including cooperation during the examination and follow-up based on results, rather than medication-specific adherence. Each item uses a 5-point Likert scale (1 = “strongly disagree,” 5 = “strongly agree”). Higher scores indicate greater treatment adherence. The adapted items are as follows: (1) Do you sometimes forget to follow the MRI-related treatment instructions?; (2) Thinking over the past 2 weeks, were there any days when you forgot to follow the MRI-related treatment instructions?; (3) Have you ever cut back or stopped following the MRI-related treatment instructions because you felt worse when you followed them?; (4) When you travel or leave home, do you sometimes forget to follow the MRI-related treatment instructions?; (5) Didn’t you follow the MRI-related treatment instructions yesterday?; (6) When you feel better, do you sometimes stop following the MRI-related treatment instructions?; (7) Do you ever feel hassled about sticking to the MRI-related treatment regimen?; (8) How often do you have difficulty remembering to follow the MRI-related treatment instructions?.
In this study, the Cronbach’s α value was 0.847, indicating high reliability. Confirmatory factor analysis demonstrated good structural validity (CMIN/DF = 1.906, GFI = 0.985, AGFI = 0.971, RMSEA = 0.043, CFI = 0.988, TLI = 0.983). This adaptation ensures relevance to the MRI context while maintaining the scale’s established validity.
3 Result
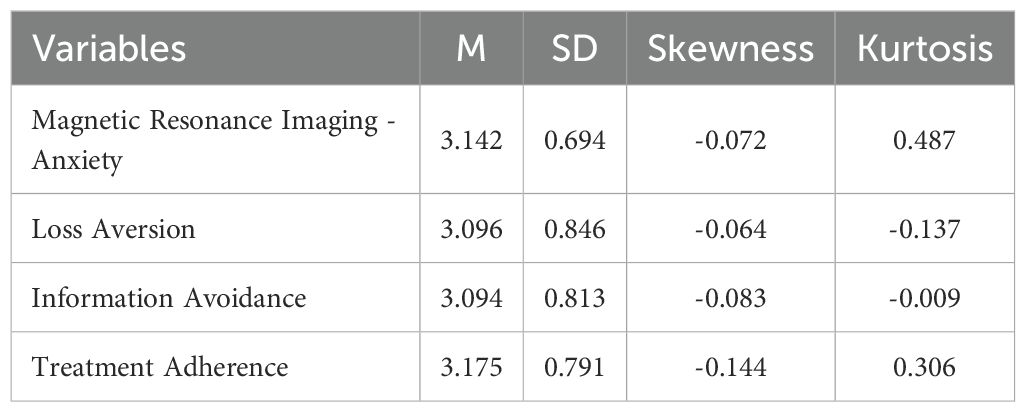
3.1 Normality test
Following Kline (63) study, we considered that when the absolute skewness of the data samples is less than 3 and the kurtosis is less than 8, the data are approximately normally distributed. In this study, descriptive analysis was used to test the skewness and kurtosis of each variable. The data results showed that both the skewness and kurtosis of all variables met the requirements, as shown in Table 2. Therefore, the data samples in this study conformed to a normal distribution.
3.2 Common method bias test
Common method bias arises due to single-source bias, same-context measurement bias, or similarity in measurement formats, leading to artificial covariance between predictor and criterion variables (64). To mitigate this, we informed the participants that their data would be strictly confidential and anonymous at the data collection stage to reduce social desirability bias and subsequently minimize common method bias (65).
Additionally, we conducted Harman’s single-factor test by including all measurement items in an exploratory factor analysis. The results indicated that the study extracted 4 factors with eigenvalues greater than 1, and the variance explained by the first factor was below the critical threshold of 50%. Therefore, no common method bias was found in this study.
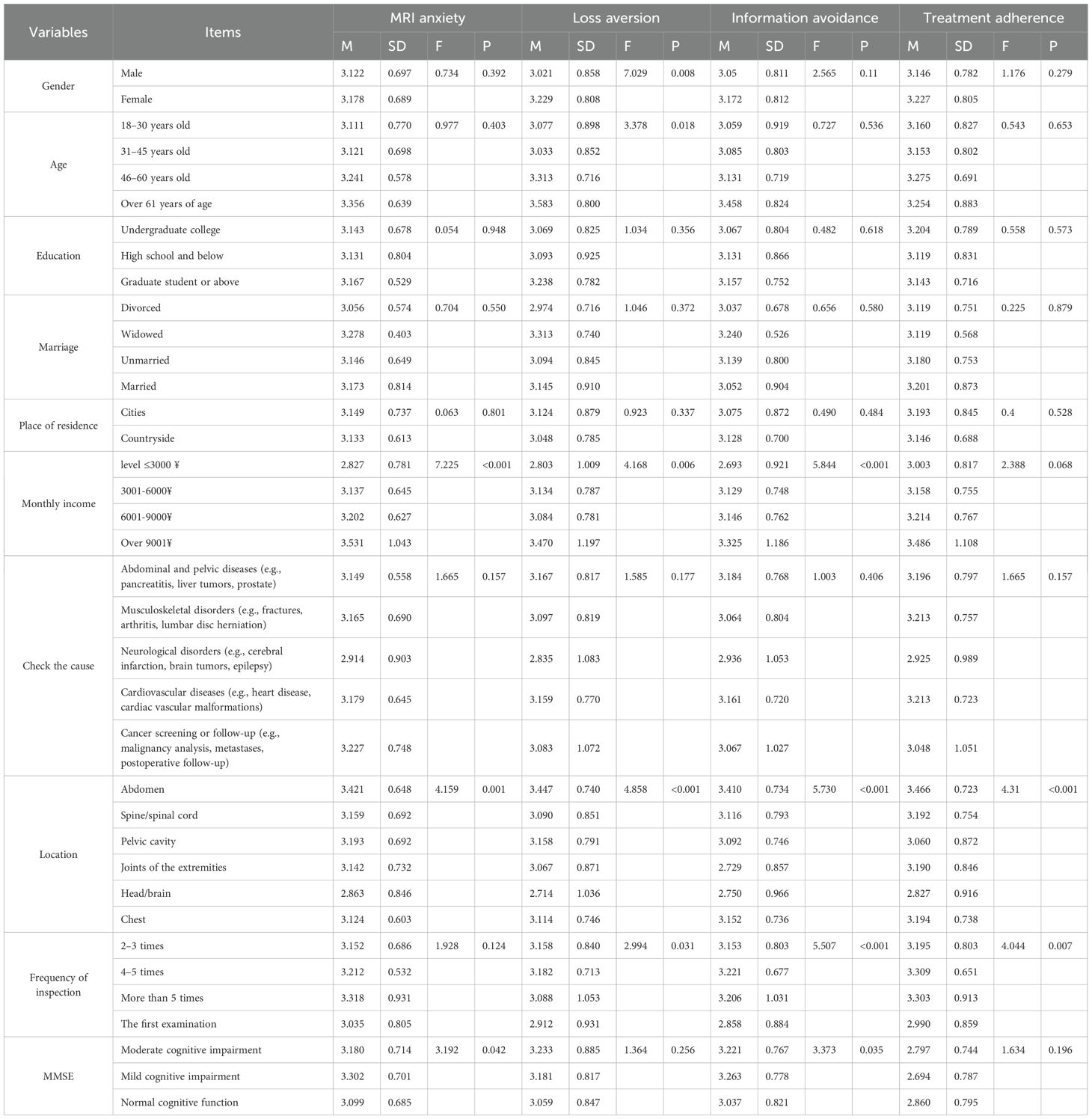
3.3 One-way ANOVA of demographic information and core variables
Referring to the study of Gui et al. (66), in order to further enhance the accuracy of the experimental results, this study used all the demographic information of the patients as independent variables and the core variables as dependent variables, using one-way ANOVA. The results showed that the gender of patients had a significant effect on loss aversion. The age of the patient had a significant effect on loss aversion. Differences in education, marriage, and place of residence of the patients did not significantly affect the core variables. The patient’s income level had a significant effect on MRI anxiety, loss aversion, and information avoidance. There was no significant difference in any of the core variables by patient reason for testing. Patient examination site showed significant differences for all core variables. Loss aversion, information avoidance, and treatment adherence were significantly affected by the number of examinations performed by patients. The type of cognitive function of patients has a significant impact on MRI anxiety and information avoidance. The specific one-way ANOVA results are shown in Table 3.
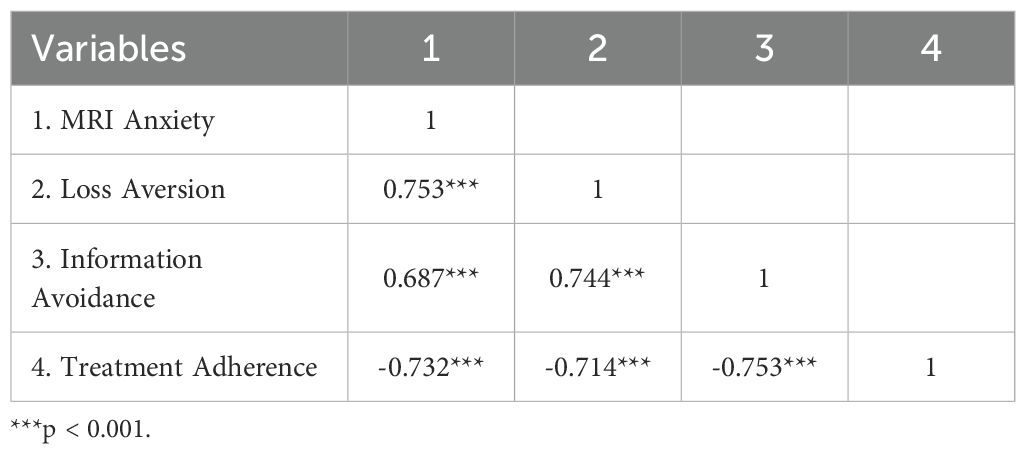
3.4 Correlation analysis
We conducted a correlation analysis of MRI anxiety, loss aversion, information avoidance, and treatment adherence, as shown in Table 4. The results showed: MRI anxiety was significantly negatively correlated with treatment adherence (r = -0.732, P < 0.001); MRI anxiety was significantly positively correlated with loss aversion (r = 0.753, P < 0.001); MRI anxiety was significantly positively correlated with information avoidance (r = 0.687, P < 0.001); loss aversion was significantly positively correlated with information avoidance (r = 0.744, P < 0.001); loss aversion was significantly negatively correlated with treatment adherence (r = -0.714, P < 0.001); and information avoidance was significantly negatively correlated with treatment adherence (r = -0.753, P < 0.001). These results provided the conditions for further mediation testing.
Based on SPSS guidance from Field (67) and American Psychological (68), the number of comparisons in this study (K = n (n-1)/2) with an initial alpha level of 0.05 and Bonferroni corrected alpha level (α_bonF = α/k). Correlation comparison results: P-value ≤ α_bonF, after Bonferroni correction, the correlation was statistically significant at the α=0.05 level; However, the p-value was greater than α_bonF, and the correlation was no longer statistically significant at the α=0.05 level after Bonferroni correction.
The results show that the number of comparisons (K) is 6, and the value of α_bonf is 0.0083. The P values of the correlation coefficients according to Table 4 are all less than α_bonF. After this adjustment, all reported associations remained statistically significant, as the unadjusted p values were all < 0.001, well below the adjusted threshold. This conservative adjustment confirmed the robustness of the association between MRI anxiety, loss aversion, information avoidance, and treatment adherence.
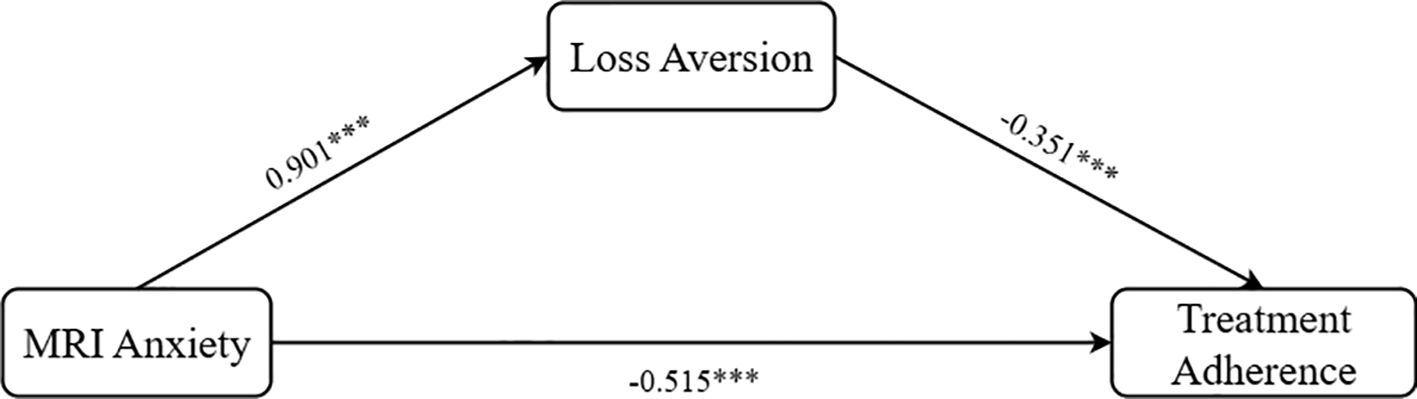
3.5 Mediation analysis of loss aversion
After controlling for factors such as gender, age, monthly income, frequency of inspection, check the cause and types of cognitive functions (MMSE score), we used loss aversion as the mediator, MRI anxiety as the independent variable, and treatment adherence as the dependent variable. The Process Model 4 was employed to test the mediating effect of loss aversion (Bootstrap sample: 5000; Igartua and Hayes (69)), validating Hypothesis H2. The results demonstrated: MRI anxiety was significantly positively associated with loss aversion (β = 0.901, P < 0.001, 95% CI = [0.838, 0.982]); MRI anxiety was significantly negatively associated with treatment adherence (β = -0.515, P < 0.001, 95% CI = [-0.614, -0.415]); and loss aversion was significantly negatively associated with treatment adherence (β = -0.351, P < 0.001, 95% CI = [-0.432, -0.269]). Overall, loss aversion exhibited a significant partial mediating effect between MRI anxiety and treatment adherence (β = -0.319, SE = 0.049, 95% CI = [-0.416, -0.221]), as shown in Figure 2, thereby validating Hypothesis H2.
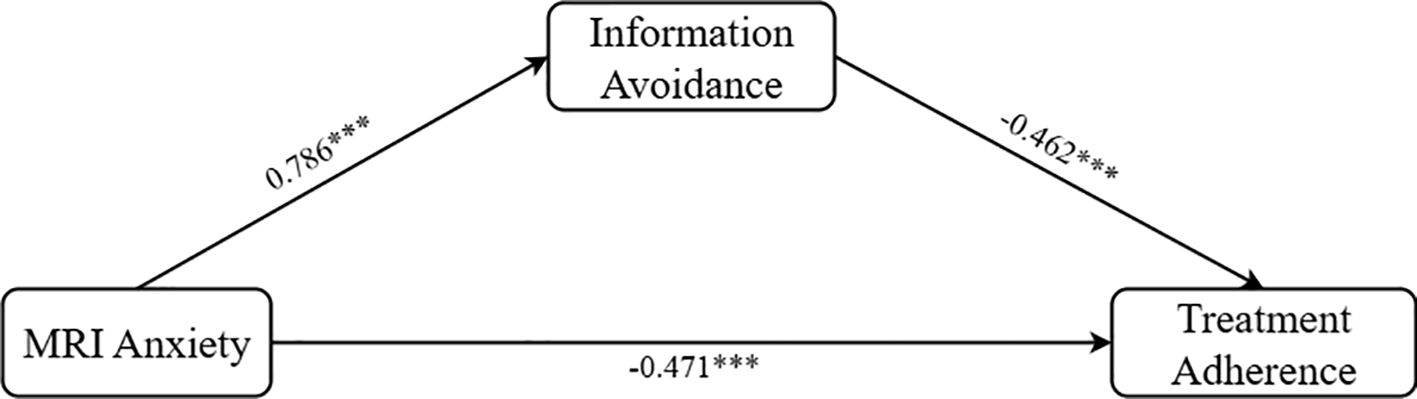
3.6 Mediation analysis of information avoidance
Subsequently, we retained the same control variables and used information avoidance as the mediator. The Process Model 4 was again applied to test the mediating effect (Bootstrap sample: 5000; Igartua and Hayes (69)), this time verifying Hypothesis H3. The results indicated: MRI anxiety had a significant associated on information avoidance (β = 0.786, P < 0.001, 95% CI = [0.709, 0.863]); MRI anxiety had a significant associated on treatment adherence (β = -0.471, P < 0.001, 95% CI = [-0.554, -0.388]); and information avoidance had a significant associated on treatment adherence (β = -0.462, P < 0.001, 95% CI = [-0.533, -0.391]). Overall, information avoidance displayed a significant partial mediating effect between MRI anxiety and treatment adherence (β = -0.363, SE = 0.046, 95% CI = [-0.457, -0.276]), as shown in Figure 3, thus validating Hypothesis H3.
3.7 Chain mediation analysis of loss aversion and information avoidance
Finally, we treated both loss aversion and information avoidance as mediators, retained the same control variables, and utilized Process Model 6 to test their chain mediating effects (Bootstrap sample: 5000; Igartua and Hayes (69)). The results revealed: loss aversion had a significant associated on information avoidance (β = 0.495, P < 0.001, 95% CI = [0.411, 0.579]); loss aversion exhibited a significant partial mediating effect between MRI anxiety and treatment adherence (β = -0.142, SE = 0.047, 95% CI = [-0.233, -0.049]); and information avoidance also showed a significant partial mediating effect between MRI anxiety and treatment adherence (β = -0.132, SE = 0.032, 95% CI = [-0.203, -0.079]). Overall, loss aversion and information avoidance demonstrated a significant chain mediating effect in the relationship between MRI anxiety and treatment adherence (β = -0.178, SE = 0.030, 95% CI = [-0.241, -0.123]). The path coefficients are illustrated in Figure 4, thereby validating Hypothesis H4.
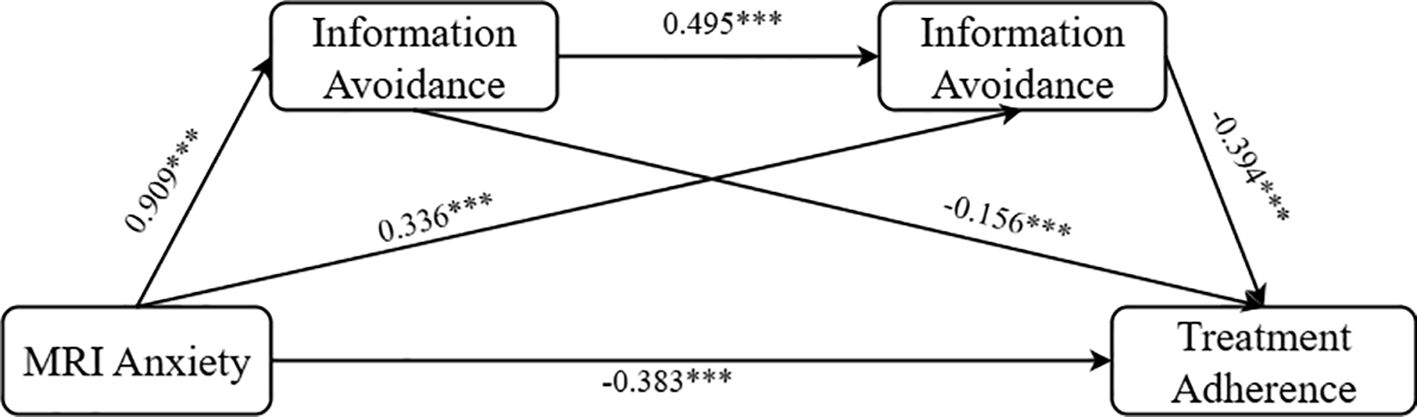
Figure 4. Graphs of chain mediation path coefficients for loss aversion and information avoidance. ***p < 0.001.
4 Discussion
4.1 The negative impact of MRI anxiety on treatment adherence
This study confirmed that MRI anxiety is negatively associated with patients’ treatment adherence. Specifically, MRI, as a non-invasive diagnostic tool, is associated with heightened emotions and cognition, which may correlate with increased anxiety and stress during the examination process (70), potentially relating to lower treatment adherence. This finding demonstrates that MRI anxiety is not only a subjective experience but also an objectively significant psychological phenomenon with clinical relevance. It expands our understanding of the sources of anxiety in healthcare settings. Traditional views have posited that medical anxiety primarily stems from the pain or side effects associated with treatment (71, 72). However, this study reveals that diagnostic tools themselves can become important psychological factors influencing treatment outcomes. Furthermore, certain objective factors within the healthcare environment may influence health behaviors by eliciting emotional responses. Therefore, a deeper understanding and intervention of MRI anxiety could enhance patients’ treatment adherence, ultimately improving overall therapeutic effects.
4.2 The mediating role of loss aversion
This study identified a mediating role of loss aversion between MRI anxiety and treatment adherence. These findings suggest that loss aversion, as a core psychological mechanism, amplifies patients’ perceived risks associated with MRI examinations, thereby intensifying their anxiety and subsequently reducing treatment adherence. This extends the application of loss aversion theory beyond its traditional focus on economic decision-making to the realm of emotional regulation in healthcare contexts. Furthermore, this discovery provides new empirical support for the health belief model, emphasizing that individuals’ perceptions of health threats and beliefs about treatment efficacy are critical factors influencing health behaviors (73). By elucidating the mediating pathway of loss aversion, this study reveals the psychological mechanisms underlying patients’ risk assessment processes during MRI examinations. This also opens new research directions inpatient psychological interventions, demonstrating that core concepts from economic decision-making theory hold significant explanatory power in medical psychology.
4.3 The mediating role of information avoidance
This study revealed the mediating role of information avoidance in the relationship between MRI anxiety and treatment adherence, providing a key cognitive mechanism to explain the behavioral withdrawal of high-anxiety patients. When faced with MRI examinations, patients tend to avoid relevant information, and this information processing strategy exacerbates their fear of the procedure, ultimately reducing treatment adherence. Based on the cognitive-emotional stress model (74), chronic stressors such as MRI anxiety can deplete limited cognitive resources, prompting individuals to adopt information avoidance strategies to alleviate cognitive overload and emotional discomfort. While this active cognitive avoidance may provide short-term emotional relief, it hinders comprehensive evaluation of risks and benefits and the development of coping strategies, ultimately weakening adherence. Thus, this study proposes a new pathway of fear-induced cognitive resource depletion and information avoidance leading to behavioral inhibition. This enhances the explanatory dimension of self-regulation theory in the context of health threat responses, highlighting the adaptive strategies individuals employ to maintain psychological stability under high emotional load.
This study revealed the mediating role of information avoidance in the relationship between MRI anxiety and treatment adherence, explaining behavioral withdrawal in anxious patients. Patients avoid MRI-related information (e.g., “I would rather not know the results of the MRI examination”), exacerbating fear and reducing adherence. This differs from loss aversion (e.g., “I would rather not think about MRI results because not knowing helps me maintain hope”), which emphasizes loss sensitivity. Per the cognitive-emotional stress model (74), MRI anxiety depletes resources, prompting avoidance for relief, but hindering risk evaluation. SEM results show distinct mediations (information avoidance: β = -0.142, p < 0.001; loss aversion: β = -0.159, p < 0.001; chain: β = -0.183, p < 0.001), confirming complementary roles: information avoidance as cognitive filtering, loss aversion as emotional bias. This enriches self-regulation theory in health threats.
4.4 Demographic information
The significant gender disparity in loss aversion highlights critical psychosocial dimensions of MRI anxiety. Females exhibited heightened sensitivity to potential health-related losses, aligning with broader literature on gender-specific risk perception in medical contexts. This may stem from sociocultural factors where women often assume primary health decision-making roles, amplifying anticipatory anxiety about diagnostic outcomes. Importantly, while gender influenced loss aversion, it did not significantly affect MRI anxiety itself, suggesting loss aversion operates as a distinct cognitive mediator rather than a direct correlate of baseline anxiety. These findings necessitate gender-tailored interventions, such as cognitive reframing techniques focused on loss-gain balance for female patients during pre-MRI counseling.
Age stratification revealed escalating loss aversion in older cohorts, reflecting cumulative health vulnerability. Older adults’ intensified focus on potential losses likely interfaces with comorbid health burdens and mortality salience, exacerbating MRI-related threat appraisal. Conversely, the absence of age effects on MRI anxiety or treatment adherence implies that while aging amplifies loss sensitivity, this manifests selectively rather than globally across psychological domains. Clinically, this underscores the need for age-specific communication strategies that address long-term health preservation benefits to counterbalance loss-focused cognitions in elderly populations.
Monthly income exerted a robust influence on MRI anxiety, loss aversion, and information avoidance. Paradoxically, both extremes of income exhibited elevated distress. Low-income groups face tangible stressors (e.g., out-of-pocket costs), while high-income patients may experience “hyper-vigilance” from heightened health literacy. This economic duality necessitates tiered interventions: financial counseling and sliding-scale fees for resource-constrained patients, and value-based framing emphasizing diagnostic efficacy for affluent subgroups to mitigate catastrophic thinking.
Examination location generated striking variations: abdominal MRI patients reported maximal anxiety, loss aversion, and information avoidance, whereas head/brain scans elicited the lowest scores. This anatomical gradient likely reflects visceral salience (e.g., abdominal organs symbolizing core vitality) and procedural discomfort (e.g., breath-holding requirements). The inverse pattern for treatment adherence further confirms that region-specific threats directly compromise compliance. These data argue for location-adjusted preparatory protocols, such as enhanced sensory mapping for abdominal scans to reduce unpredictability-driven avoidance.
First-time MRI recipients showed marked loss aversion and information avoidance. Surprisingly, MRI anxiety itself remained stable across exposure frequency, indicating that while procedural familiarity reduces cognitive avoidance mechanisms, visceral anxiety persists. This dissociation suggests that experiential interventions (e.g., virtual reality MRI simulators) should target informational coping rather than expecting anxiety extinction. The rise in treatment adherence with repeated scans further validates exposure-based desensitization for adherence optimization.
The absence of marital status effects contradicts theories linking social support to medical coping. Similarly, diagnostic indications (e.g., cancer vs. musculoskeletal) showed no psychological differentiation, suggesting MRI’s procedural characteristics dominate over condition-specific meanings. This reinforces MRI anxiety as a process-centric phenomenon requiring sensory-focused interventions rather than condition-specific counseling.
4.5 Practical implications
Based on the core finding that MRI anxiety significantly reduces patients’ treatment adherence, clinical practice urgently requires systemic innovations in screening and early intervention strategies. Traditional nursing protocols often underestimate or overlook the standardized assessment of pre-MRI anxiety, resulting in the failure to identify high-risk patients in a timely manner. This study confirms the direct negative effect of anxiety on adherence, strongly supporting the integration of efficient, standardized anxiety screening tools during the initial appointment or pre-screening phase. These tools should facilitate a tiered intervention approach based on the level of anxiety. For example, mild anxiety can be alleviated through enhanced informational support, while moderate-to-severe anxiety may require multidisciplinary collaboration, including cognitive behavioral therapy and, if necessary, the cautious use of short-term anxiolytic medications. Most importantly, these interventions should be implemented through optimized patient education and communication strategies, such as providing detailed examination information and emotional support to help patients manage their anxiety rationally. Such interventions not only improve treatment adherence but also enhance overall medical outcomes. By implementing these measures, healthcare teams can better assist patients in overcoming MRI anxiety, ensuring their active participation in treatment and achieving optimal therapeutic effects.
The critical mediating role of loss aversion in the relationship between MRI anxiety and treatment adherence provides new perspectives for designing precise interventions based on behavioral economics principles. Patients often amplify their fear by focusing excessively on potential losses, leading to avoidance of necessary examinations. This suggests that healthcare professionals should address patients’ loss sensitivity during communication. This can be achieved by emphasizing the efficiency and accuracy of the examination, reducing unnecessary focus on potential losses, and helping patients understand the necessity of the procedure from a positive perspective. Such psychological intervention strategies can reduce Patients’ loss aversion, lower MRI anxiety, increase treatment adherence, and ultimately improve therapeutic outcomes. This also implies that clinical staff should use structured decision aids to visually present the long-term benefits of timely examinations compared to the catastrophic consequences of delays. Training for healthcare professionals should focus on identifying and addressing loss-averse psychology, guiding patients to cognitive restructuring, and redefining MRI as an active, defensive investment in health.
The mediating role of information avoidance in the relationship between MRI anxiety and treatment adherence underscores the need for healthcare teams to adopt more transparent and moderate approaches to information disclosure. This not only helps patients acquire necessary knowledge but also reduces unnecessary concerns and anxiety. By optimizing information transmission strategies, such as using visual aids and simple, clear language, healthcare teams can effectively reduce patients’ information avoidance behaviors, alleviate MRI anxiety, and ultimately improve treatment adherence and overall therapeutic outcomes. This patient-centered approach to information disclosure fosters positive doctor-patient relationships, promoting the success of treatment.
4.6 Limitations and future research directions
Although this study provides valuable insights into the impact of MRI anxiety on treatment adherence and its underlying mechanisms, several limitations must be acknowledged. First, the use of convenience sampling, a non-probability method, may limit the representativeness of the sample (75). Participants were selected based on their availability in the Radiology Department of a tertiary hospital in Sichuan Province, without randomization, which may introduce selection bias and restrict the generalizability of findings to other regions, cultural backgrounds, or healthcare settings. The term “randomized convenience sampling” was avoided in this study to clarify that no probabilistic selection was employed, ensuring alignment with statistical terminology. Despite the robust sample size of 495 participants, which exceeded the minimum requirement calculated via G*Power (n = 119), the single-center design further constrains external validity. Factors such as medical resources in different regions, patient education level and cultural concepts may affect the relationship between MRI anxiety and treatment compliance. Therefore, future research can use multi-center, large-sample random sampling to carry out research in a wider range of regions and populations to enhance the universality of the conclusions.
Second, this study only performed a one-time data collection at the time of the MRI examination and lacked longitudinal follow-up of the patients before and after the examination. Treatment compliance is a dynamic process. Patients’ anxiety level and expectations before the examination may affect their treatment decisions and compliance behavior after the examination, and one-time measurement is difficult to capture this dynamic change. Future studies can design longitudinal research protocols to collect patients’ data at multiple time points before, during and after the examination, and deeply analyze the specific mechanism of MRI anxiety on treatment compliance at different stages, so as to provide a basis for clinical development of more targeted and staged interventions.
Third, the exclusive use of self-reported scales introduces potential measurement biases, such as social desirability bias, where patients may select responses aligned with perceived social norms, thus affecting data authenticity. Additionally, discrepancies may exist between self-reported anxiety levels and actual behaviors, as some patients reporting high anxiety may not exhibit reduced adherence in practice. To address this limitation, future research should triangulate self-reported data with objective behavioral and physiological measures to enhance validity. For instance, behavioral data, such as rates of missed MRI appointments, premature scan terminations, or non-compliance with radiographer instructions, can be extracted from medical records or radiology department logs to objectively assess treatment adherence (16). Similarly, physiological indicators, such as heart rate variability (HRV) or cortisol levels, can provide objective measures of anxiety during MRI examinations. HRV, in particular, is a non-invasive marker of autonomic nervous system activity and has been used to assess stress responses in medical imaging contexts (76). Wearable devices could be integrated into clinical settings to monitor HRV in real-time during MRI scans, offering a robust complement to self-reported anxiety measures. Combining these objective measures with self-reported data would provide a more comprehensive understanding of the interplay between MRI anxiety, loss aversion, information avoidance, and treatment adherence, mitigating the limitations of subjective reporting. Moreover, incorporating objective measures aligns with the cognitive-emotional stress model, which posits that chronic stressors deplete cognitive resources, influencing behavioral outcomes (74).
The study included participants with minor language, cognitive, or psychiatric impairments while ensuring that they were able to provide informed consent and complete the questionnaire, which may have led to variability in response. Although clinical assessment and standardized tools such as the MMSE rule out severe impairment, the presence of mild impairment may affect the accuracy of self-reported data, especially for scales assessing complex psychological constructs such as loss aversion and information avoidance. This variability may affect the reliability of responses, as patients with minor impairments may interpret or respond differently to questionnaire items. Future studies should adopt stricter inclusion criteria or employ standardized assessment tools to quantify the degree of impairment and ensure a homogeneous study population.
At the same time, although the model constructed in this study revealed the mediating role of loss aversion and information avoidance in the relationship between MRI anxiety and treatment adherence, the exploration of other potential influencing factors is limited. For example, factors such as the patient’s personality characteristics (e.g., neuroticism, extraversion, etc.), social support system, previous medical experience, and degree of trust in the health care system may also play an important role. Future research can further expand the model to include more potential moderating variables and mediating variables, and further explore the complex mechanism of MRI anxiety affecting treatment adherence, so as to provide more comprehensive theoretical support for optimizing clinical intervention strategies.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Academic Ethics Committee of North Sichuan Medical College. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LL: Writing – review & editing, Writing – original draft, Validation, Methodology, Conceptualization, Investigation. XY: Investigation, Methodology, Writing – review & editing, Conceptualization, Formal analysis, Writing – original draft. NL: Formal analysis, Writing – review & editing, Writing – original draft, Conceptualization, Investigation, Supervision, Resources. LT: Conceptualization, Investigation, Writing – original draft, Validation, Writing – review & editing, Methodology. XH: Software, Investigation, Writing – original draft, Project administration, Writing – review & editing, Data curation. XHH: Supervision, Writing – original draft, Methodology, Investigation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was funded by Sichuan Science and Technology Program (No.:2024ZYD0272), the youth innovation project of Sichuan Medical Association (No.:Q2024001) and the Bureau of Science & Technology and Intellectual Property Nanchong City (No.: 23YYJCYJ0131).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Grover V P B, Tognarelli J M, Crossey M M E, et al. Magnetic resonance imaging: principles and techniques: lessons for clinicians. J Clin Exp Hepatol. (2015) 5(3):246–55.
2. Huk W J and Gademann G. Magnetic resonance imaging (MRI): method and early clinical experiences in diseases of the central nervous system. Neurosurg Rev. (1984) 7(4):259–80.
3. Kurudirek F, Demir Barbak Z, Demir İmamoğlu Z, Çiftci K, and Delice O. The effect of music on fear and anxiety of children during tomography: A randomized controlled double-blind study. Int J Nurs Pract. (2025) 31:e70029. doi: 10.1111/ijn.70029
4. Zhou SP, Wan XC, Wang XD, Zhang XM, Yu YH, and Wang WJ. Investigation and analysis of magnetic resonance imaging experience and psychological status of patients. BMC Psychol. (2024) 12:115. doi: 10.1186/s40359-024-01570-7
5. Oktay S, Söğütlüler T, Avcil S, Akçanal Şeker C, Öner H, Öztürk H, et al. Using audiovisual intervention to reduce anxiety and improve image quality in pediatric magnetic resonance imaging. Pediatr Radiol. (2025) 2025:1–9. doi: 10.1007/s00247-025-06276-5
6. Hamd ZY, Alorainy AI, Alrujaee LA, Alshdayed MY, Wdaani AM, Alsubaie AS, et al. How different preparation techniques affect MRI-induced anxiety of MRI patients: A preliminary study. Brain Sci. (2023) 13(4):416. doi: 10.3390/brainsci13030416
7. Stanley E, Cradock A, Bisset J, McEntee C, and O’Connell MJ. Impact of sensory design interventions on image quality, patient anxiety and overall patient experience at MRI. Br J Radiol. (2016) 89:20160389. doi: 10.1259/bjr.20160389
8. Zhou Y, Cao Y, Xu S, Li S, Liang Y, Zhang W, et al. Randomized controlled trial on the effects of mindfulness-based respiratory decompression therapy in claustrophobic patients undergoing MRI inspection. Front Med (Lausanne). (2023) 10:1253824. doi: 10.3389/fmed.2023.1253824
9. Carlsson S and Carlsson E. ‘The situation and the uncertainty about the coming result scared me but interaction with the radiographers helped me through’: a qualitative study on patients’ experiences of magnetic resonance imaging examinations. J Clin Nurs. (2013) 22:3225–34. doi: 10.1111/jocn.12416
10. Klumpers F, Kroes MC, Heitland I, Everaerd D, Akkermans SE, Oosting RS, et al. Dorsomedial prefrontal cortex mediates the impact of serotonin transporter linked polymorphic region genotype on anticipatory threat reactions. Biol Psychiatry. (2015) 78:582–9. doi: 10.1016/j.biopsych.2014.07.034
11. Tekinhatun M, Alver KH, Akbudak İ, Turmak M, Çavdar E, and Deniz MA. Influence of visual objects and music on anxiety levels and imaging process in patients undergoing coronary CT angiography. Eur Radiol. (2025) 2025:1–13. doi: 10.1007/s00330-025-11614-0
12. Hussain S, Mubeen I, Ullah N, Shah S, Khan BA, Zahoor M, et al. Modern diagnostic imaging technique applications and risk factors in the medical field: A review. BioMed Res Int. (2022) 2022:5164970. doi: 10.1155/2022/5164970
13. DiMatteo MR, Giordani PJ, Lepper HS, and Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. (2002) 40:794–811. doi: 10.1097/00005650-200209000-00009
14. van Dulmen S, Sluijs E, van Dijk L, de Ridder D, Heerdink R, and Bensing J. Patient adherence to medical treatment: a review of reviews. BMC Health Serv Res. (2007) 7:55. doi: 10.1186/1472-6963-7-55
15. Goldstein CM, Gathright EC, and Garcia S. Relationship between depression and medication adherence in cardiovascular disease: the perfect challenge for the integrated care team. Patient Prefer Adherence. (2017) 11:547–59. doi: 10.2147/ppa.S127277
16. Kvarnström K, Westerholm A, Airaksinen M, and Liira H. Factors contributing to medication adherence in patients with a chronic condition: a scoping review of qualitative research. Pharmaceutics. (2021) 13:1100. doi: 10.3390/pharmaceutics13071100
17. Kamei T, Kanamori T, Yamamoto Y, and Edirippulige S. The use of wearable devices in chronic disease management to enhance adherence and improve telehealth outcomes: A systematic review and meta-analysis. J Telemed Telecare. (2022) 28:342–59. doi: 10.1177/1357633x20937573
18. Vitija A, Amirthalingam A, and Soltani A. The impact of digital interventions on medication adherence in paediatric populations with attention deficit hyperactivity disorder, depression, and/or anxiety: A rapid systematic review and meta-analysis. Res Soc Adm Pharm. (2022) 18:4017–27. doi: 10.1016/j.sapharm.2022.07.042
19. Butler S, Sculley D, Santos D, Girones X, Singh-Grewal D, and Coda A. Using digital health technologies to monitor pain, medication adherence and physical activity in young people with juvenile idiopathic arthritis: A feasibility study. Healthc (Basel). (2024) 12(3):392. doi: 10.3390/healthcare12030392
20. Thompson SM, Gorny KR, Koepsel EMK, Welch BT, Mynderse L, Lu A, et al. Body interventional MRI for diagnostic and interventional radiologists: current practice and future prospects. Radiographics. (2021) 41:1785–801. doi: 10.1148/rg.2021210040
21. Tsoumakidou G, Saltiel S, Villard N, Duran R, Meuwly JY, and Denys A. Image-guided marking techniques in interventional radiology: A review of current evidence. Diagn Interv Imaging. (2021) 102:699–707. doi: 10.1016/j.diii.2021.07.002
22. Erev I, Ert E, and Yechiam E. Loss aversion, diminishing sensitivity, and the effect of experience on repeated decisions. J Behav Decision Making. (2008) 21:575–97. doi: 10.1002/bdm.602
23. Gal D and Rucker DD. The loss of loss aversion: Will it loom larger than its gain? J Consumer Psychol. (2018) 28:497–516. doi: 10.1002/jcpy.1047
24. Campbell R, Ju A, King MT, and Rutherford C. Perceived benefits and limitations of using patient-reported outcome measures in clinical practice with individual patients: a systematic review of qualitative studies. Qual Life Res. (2022) 31:1597–620. doi: 10.1007/s11136-021-03003-z
25. Reitich-Stolero T, Halperin D, Morris G, Goldstein L, Bergman L, Fahoum F, et al. Aversive generalization in human amygdala neurons. Curr Biol. (2025) 35:1137–1144.e1133. doi: 10.1016/j.cub.2025.01.013
26. Marx R. Reassurance for patients-essential not optional. J Eval Clin Pract. (2025) 31:e14287. doi: 10.1111/jep.14287
27. Golman R, Hagmann D, and Loewenstein G. Information avoidance. J Econ Literature. (2017) 55:96–135. doi: 10.1257/jel.20151245
28. Sweeny K, Melnyk D, Miller W, and Shepperd JA. Information avoidance: Who, what, when, and why. Rev Gen Psychol. (2010) 14:340–53. doi: 10.1037/a0021288
29. Howell JL and Shepperd JA. Reducing health-information avoidance through contemplation. Psychol Sci. (2013) 24:1696–703. doi: 10.1177/0956797613478616
30. Chen M, Huang X, Wu Y, Song S, and Qi X. A model for predicting factors affecting health information avoidance on WeChat. Digit Health. (2025) 11:20552076251314277. doi: 10.1177/20552076251314277
31. Soroya SH, Farooq A, Mahmood K, Isoaho J, and Zara SE. From information seeking to information avoidance: Understanding the health information behavior during a global health crisis. Inf Process Manag. (2021) 58:102440. doi: 10.1016/j.ipm.2020.102440
32. Siebenhaar KU, Köther AK, and Alpers GW. Dealing with the COVID-19 infodemic: distress by information, information avoidance, and compliance with preventive measures. Front Psychol. (2020) 11:567905. doi: 10.3389/fpsyg.2020.567905
33. Yu Y and Sherman KA. Communication avoidance, coping and psychological distress of women with breast cancer. J Behav Med. (2015) 38:565–77. doi: 10.1007/s10865-015-9636-3
34. Zhu R, Zhao H, Yun Y, Zhao Y, Wang W, Wang L, et al. Research on health information avoidance behavior and influencing factors of cancer patients-an empirical analysis based on structural equation modeling. BMC Public Health. (2024) 24:3617. doi: 10.1186/s12889-024-21113-4
35. Grandey AA. Emotion regulation in the workplace: a new way to conceptualize emotional labor. J Occup Health Psychol. (2000) 5:95–110. doi: 10.1037//1076-8998.5.1.95
36. Roth G, Vansteenkiste M, and Ryan RM. Integrative emotion regulation: Process and development from a self-determination theory perspective. Dev Psychopathol. (2019) 31:945–56. doi: 10.1017/s0954579419000403
37. Case DO, Andrews JE, Johnson JD, and Allard SL. Avoiding versus seeking: the relationship of information seeking to avoidance, blunting, coping, dissonance, and related concepts. J Med Libr Assoc. (2005) 93:353–62.
38. Sun H, Li J, Cheng Y, Pan X, Shen L, and Hua W. Developing a framework for understanding health information behavior change from avoidance to acquisition: a grounded theory exploration. BMC Public Health. (2022) 22:1115. doi: 10.1186/s12889-022-13522-0
39. Bergh DD, Ketchen DJ Jr., Orlandi I, Heugens PP, and Boyd BK. Information asymmetry in management research: Past accomplishments and future opportunities. J Manage. (2019) 45:122–58. doi: 10.1177/0149206318798026
40. Mavlanova T, Benbunan-Fich R, and Koufaris M. Signaling theory and information asymmetry in online commerce. Inf Manage. (2012) 49:240–7. doi: 10.1016/j.im.2012.05.004
41. Ding Q, Gu Y, Zhang G, Li X, Zhao Q, Gu D, et al. What causes health information avoidance behavior under normalized COVID-19 pandemic? A research from fuzzy set qualitative comparative analysis. Healthc (Basel). (2022) 10(8):1381. doi: 10.3390/healthcare10081381
42. Zhang J, Hu X, Wu D, and Yan H. Exploring the influence mechanism of Chinese young researchers’ academic information avoidance behavior. J Acad Librarianship. (2023) 49:102649. doi: 10.1016/j.acalib.2022.102649
43. Boyacı H and Söyük S. Healthcare workers’ readiness for artificial intelligence and organizational change: a quantitative study in a university hospital. BMC Health Serv Res. (2025) 25:813. doi: 10.1186/s12913-025-12846-y
44. Wang L and Yang D. How recycling and transformation information influences tourists’ purchase intentions towards green food products. CyTA J Food. (2025) 23:2528540. doi: 10.1080/19476337.2025.2528540
45. Bayles K, McCullough K, and Tomoeda CK. Cognitive-communication disorders of MCI and dementia: Definition, assessment, and clinical management. United States: Plural Publishing (2018).
46. Mueller KD, Hermann B, Mecollari J, and Turkstra LS. Connected speech and language in mild cognitive impairment and Alzheimer’s disease: A review of picture description tasks. J Clin Exp Neuropsychol. (2018) 40:917–39. doi: 10.1080/13803395.2018.1446513
47. Salis F, Costaggiu D, and Mandas A. Mini-mental state examination: optimal cut-off levels for mild and severe cognitive impairment. Geriatrics. (2023) 8:12. doi: 10.3390/geriatrics8010012
48. Tombaugh TN and McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc. (1992) 40:922–35. doi: 10.1111/j.1532-5415.1992.tb01992.x
49. Mitchell AJ. A meta-analysis of the accuracy of the mini-mental state examination in the detection of dementia and mild cognitive impairment. J Psychiatr Res. (2009) 43:411–31. doi: 10.1016/j.jpsychires.2008.04.014
50. Tang-Wai DF, Knopman DS, Geda YE, Edland SD, Smith GE, Ivnik RJ, et al. Comparison of the short test of mental status and the mini-mental state examination in mild cognitive impairment. Arch Neurol. (2003) 60:1777–81. doi: 10.1001/archneur.60.12.1777
51. Friedman TW, Yelland GW, and Robinson SR. Subtle cognitive impairment in elders with Mini-Mental State Examination scores within the ‘normal’ range. Int J Geriatr Psychiatry. (2012) 27:463–71. doi: 10.1002/gps.2736
52. Mamikonyan E, Moberg PJ, Siderowf A, Duda JE, Have TT, Hurtig HI, et al. Mild cognitive impairment is common in Parkinson’s disease patients with normal Mini-Mental State Examination (MMSE) scores. Parkinsonism Relat Disord. (2009) 15:226–31. doi: 10.1016/j.parkreldis.2008.05.006
53. Ahlander BM, Årestedt K, Engvall J, Maret E, and Ericsson E. Development and validation of a questionnaire evaluating patient anxiety during Magnetic Resonance Imaging: the Magnetic Resonance Imaging-Anxiety Questionnaire (MRI-AQ). J Adv Nurs. (2016) 72:1368–80. doi: 10.1111/jan.12917
54. Zhang XX, Zhang XH, and Dong YC. Effects of psychological nursing in Parkinson’s related depression patients undergoing functional magnetic resonance imaging: A randomized controlled trial. World J Clin cases. (2024) 12:3086–93. doi: 10.12998/wjcc.v12.i17.3086
55. Lam JY and Lin SH. Unravelling moderated mediating effects of loss aversion, information avoidance and self-efficacy on cancer fear and cancer screening. Health Info Libr J. (2024). doi: 10.1111/hir.12536
56. Kai-Ineman D and Tversky A. Prospect theory: An analysis of decision under risk. Econometrica. (1979) 47:363–91. doi: 10.1037/pas0000315
57. Howell JL and Shepperd JA. Establishing an information avoidance scale. Psychol Assess. (2016) 28:1695–708. doi: 10.1037/pas0000315
58. Gu C, Qian L, and Zhuo X. Mindfulness intervention for health information avoidance in older adults: mixed methods study. JMIR Public Health Surveill. (2025) 11:e69554. doi: 10.2196/69554
59. Zhao S, Zhao H, Wang X, Gao C, Qin Y, Cai H, et al. Factors influencing medication knowledge and beliefs on warfarin adherence among patients with atrial fibrillation in China. Patient Prefer Adherence. (2017), 213–20. doi: 10.2147/ppa.S120962
60. Morisky DE, Green LW, and Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. (1986) 24:67–74. doi: 10.1097/00005650-198601000-00007
61. Morisky DE, Ang A, Krousel-Wood M, and Ward HJ. Retracted: predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. (2008) 10:348–54. doi: 10.1111/j.1751-7176.2008.07572.x
62. Wang W, Luan W, Zhang Z, and Mei Y. Association between medication literacy and medication adherence and the mediating effect of self-efficacy in older people with multimorbidity. BMC Geriatr. (2023) 23:378. doi: 10.1186/s12877-023-04072-0
63. Kline RB. Software review: Software programs for structural equation modeling: Amos, EQS, and LISREL. J Psychoeducational Assess. (1998) 16:343–64. doi: 10.1177/073428299801600407
64. Podsakoff PM, MacKenzie SB, Lee J-Y, and Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879. doi: 10.1037/0021-9010.88.5.879
65. Bergen N and Labonté R. Everything is perfect, and we have no problems”: detecting and limiting social desirability bias in qualitative research. Qual Health Res. (2020) 30:783–92. doi: 10.1177/1049732319889354
66. Gui G, Yang D, Liu Y, Yao Y, Xie X, Liu R, et al. How family support alleviates death anxiety in breast cancer patients: the mediating role of meaning in life. Front Public Health. (2025) 13:1567485. doi: 10.3389/fpubh.2025.1567485
67. Field A. Discovering statistics using IBM SPSS statistics. United States: Sage publications limited (2024).
68. American Psychological A. Publication manual of the American psychological association 2020. American psychological association (2020).
69. Igartua JJ and Hayes AF. Mediation, moderation, and conditional process analysis: concepts, computations, and some common confusions. Span J Psychol. (2021) 24:e49. doi: 10.1017/sjp.2021.46
70. Madl J, Janka R, Bay S, and Rohleder N. MRI as a stressor: the psychological and physiological response of patients to MRI, influencing factors, and consequences. J Am Coll Radiol. (2022) 19:423–32. doi: 10.1016/j.jacr.2021.11.020
71. McWilliams LA, Goodwin RD, and Cox BJ. Depression and anxiety associated with three pain conditions: results from a nationally representative sample. Pain. (2004) 111:77–83. doi: 10.1016/j.pain.2004.06.002
72. Meuret AE, Tunnell N, and Roque A. Anxiety disorders and medical comorbidity: treatment implications. Adv Exp Med Biol. (2020) 1191:237–61. doi: 10.1007/978-981-32-9705-0_15
73. Carpenter CJ. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. (2010) 25:661–9. doi: 10.1080/10410236.2010.521906
74. Pinderhughes EE, Dodge KA, Bates JE, Pettit GS, and Zelli A. Discipline responses: influences of parents’ socioeconomic status, ethnicity, beliefs about parenting, stress, and cognitive-emotional processes. J Family Psychol. (2000) 14:380. doi: 10.1037/0893-3200.14.3.380
75. Stratton SJ. Population sampling: Probability and non-probability techniques. Prehospital Disaster Med. (2023) 38:147–8. doi: 10.1017/S1049023X23000304
Keywords: magnetic resonance imaging, anxiety, treatment adherence, loss aversion, information avoidance
Citation: Lei L, Yang X, Liu N, Tang L, He X and Huang X (2025) The impact of magnetic resonance imaging anxiety on treatment adherence. Front. Psychiatry 16:1658226. doi: 10.3389/fpsyt.2025.1658226
Received: 02 July 2025; Accepted: 21 October 2025;
Published: 03 November 2025.
Edited by:
Gabriella Martino, University of Messina, ItalyReviewed by:
Maya Visser, University of Jaume I, SpainChang Hu, Jiangxi Normal University, China
Eason Yao, Qingdao University, China
Copyright © 2025 Lei, Yang, Liu, Tang, He and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaohua Huang, MTUwODI3OTc1NTNAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Lixing Lei
Lixing Lei Xiongxiong Yang2†
Xiongxiong Yang2† Nian Liu
Nian Liu Lingling Tang
Lingling Tang Xiaohua Huang
Xiaohua Huang