- 1Cambridge Institute for Music Therapy Research, Anglia Ruskin University, Cambridge, United Kingdom
- 2Centre for Health, Performance, and Wellbeing, Anglia Ruskin University, Cambridge, United Kingdom
- 3Department of Psychiatry, University of Cambridge, Cambridge, United Kingdom
- 4Department of Paediatrics, Cambridge University Hospitals National Health Service (NHS) Foundation Trust, Cambridge, United Kingdom
Introduction: Eating disorders (EDs) are potentially life-threatening conditions characterized by persistent eating- and body-related disturbances that negatively impact nutritional intake, psychological well-being, and physical health. While psychological therapies remain the primary treatment for patients with EDs, music-based interventions (MBIs) show significant promise for addressing symptoms in clinical practice. However, little is known about the methods employed in these interventions or their effectiveness in addressing or improving ED outcomes.
Methods: Following PRISMA-ScR guidelines, we conducted a scoping review of the literature. Eight electronic databases were systematically queried from inception to May 2025 for studies evaluating MBIs in patients engaged in ED treatment. Data regarding study design, sample characteristics, intervention components, and primary outcomes were extracted and analysed utilising either reflexive thematic analysis or descriptive statistics. The quality of intervention reporting was additionally examined utilising the established MBI reporting guidelines.
Results: Of the 114 articles screened, 21 met inclusion criteria. The final sample comprised 10 case studies, 6 qualitative studies, 4 quantitative studies, and 1 mixed methods study, with all but one conducted in high-income countries. Settings included inpatient (n = 12), outpatient (n = 7), and combined (n = 2) ED programs. Most MBIs involved music therapy (n = 18), while others incorporated vibroacoustic therapy (n = 1), background music during mealtimes (n = 1), and group singing (n = 1). Delivery formats encompassed individual (n = 14), group (n = 5), and hybrid (n = 1) sessions, or were not indicated. Qualitative synthesis identified seven themes reflecting symptom management, self-development, and treatment engagement. Quantitative studies reported improvements in anxiety, mood, ED symptoms and increased food eaten and weight gain. However, robust conclusions were limited by small sample sizes, a lack of control group, non-randomisation, or another intervention being implemented with the MBI. Overall, reporting of MBI components was inconsistent, with a mean completeness of 45–100%.
Discussion: To our knowledge, this is the largest scoping review to map the breadth and depth of studies assessing MBIs in ED treatment. Preliminary evidence supports positive psychological and behavioural outcomes for patients with EDs. However, conclusions are limited by lack of methodological rigor, variable outcome measures, and inconsistent reporting of intervention components or theoretical framework. The complex and multifaceted nature of EDs and high rates of comorbidities and trauma histories further complicates interpretations. To advance research and clinical application of MBIs in ED care, standardized approaches to intervention design and reporting are needed, as well as randomised controlled studies clearly testing MBIs against other interventions.
Introduction
Individuals diagnosed with eating disorders (EDs) present with a variety of eating-related behaviours that negatively impact nutritional intake, affect psychological and psychosocial wellbeing, and result in somatic complications (1, 2). ED diagnoses (including anorexia nervosa, bulimia nervosa, binge eating disorder and other specified feeding or eating disorders) have an onset at the developmentally vulnerable period of adolescence (ages 15–25 years), with a peak age onset of 15.5 years and an average duration of six years (3, 4). Further, mortality rates for individuals with EDs are higher than the general population: a six times higher mortality rate for those with anorexia nervosa (AN), and a doubled mortality rate for those with other EDs (5).
Research indicates significant increases in EDs over the past two decades (6–8). An estimated 55.5 million people globally were living with an ED in 2019 (9). In 2020, during the COVID-19 pandemic, there was a reported 15% increase in the incidence of EDs (10, 11). Overall, the data indicate a worsening burden of the illness (7) and an increase in the associated treatment and economic costs due to an increasing prevalence of EDs (12).
The complex profile of ED patients is exacerbated by multiple comorbidities, with an estimated 56%-95% presenting with an additional psychiatric disorder, depending on the type of ED (13–15). The most prevalent comorbidities are substance use disorders (SUD), ranging from 20% to 51% (16), followed by post-traumatic stress disorder (PTSD) at 25% (17). Further, 33% of individuals with EDs have experienced sexual trauma and 21% physical assault (18, 19). Perfectionism, and impaired affect regulation and cognitive processing are common features in EDs which complicate treatment (20, 21). Additionally, there are a myriad of medical complications associated with EDs because of malnutrition, purging, laxative abuse, excessive exercise, and weight loss (22, 23). Thus, ED behaviours can impact every system of the body, resulting in gastrointestinal, dermatologic, endocrine, neurological, haematological, pulmonary, and cardiac issues and abnormalities (24–29).
ED treatment programs apply psychological therapies, which address different presenting issues common to individuals with EDs (30). Therapies include cognitive behavioural therapy (CBT), dialectical behaviour therapy (DBT), family-based therapy (FBT), and interpersonal therapy (IPT) (31). The focus of CBT is on addressing thoughts and feelings as these relate to and impact ED behaviours (31). DBT addresses issues related to affect regulation and how this impacts ED behaviours (32, 33). FBT focuses on engaging families as a resource to help make changes to reduce and eliminate ED behaviours (34). IPT aims at addressing interpersonal issues and how disordered eating and ED behaviours impact relationships (35). However, estimates indicate that ED treatment is effective for about 50% of individuals (36), suggesting that ED treatment needs further development to more adequately address the complex matrix of ED behaviours (37, 38).
Music-based interventions in eating disorder treatment
Music-based interventions (MBIs) include a broad range of practices that utilise music to support health and wellbeing. These can integrate the use of music in various ways, including listening to, singing, playing, composing, and improvising music (39). MBIs can be distinguished by the way one engages with the music (for example, listening to songs and discussing them, listening to instrumental music for relaxation, actively playing instruments or singing songs, improvising instrumentally or vocally, composing a song or instrumental music) and by who facilitates the MBI. MBIs may be facilitated by qualified music therapists (music therapy) or other healthcare professionals (non-music therapists) as well as musical experiences led by community musicians or the use of self-selected music implemented by the client themselves (39). The accessible nature and myriad ways of engaging with music allows for the use of MBIs in various contexts and for a range of client needs, across therapeutic and community-based settings (27). While music therapy is encompassed in this broad category, it is a specialist-delivered intervention differentiated by formal training and qualification. Music therapists are allied health professionals trained in a wide range of music therapy theories, approaches and methods to address therapeutic goals across clinical populations. Music therapists use both active and receptive methods, adapting sessions reflexively to meet emerging and changing needs of the individual or group throughout the therapeutic process (40–42). MBIs therefore can encompass a continuum of music use for wellbeing, from personal use to specialist music therapy sessions (43).
There has been a recent increase in reviews evaluating the use and potential outcomes of music in people with or at risk of EDs (44–47). Testa et al. completed a systematic review that included 16 studies examining the effects of music in people with EDs or at risk of EDs. Studies were limited to experimental or observational designs which reported measurable outcomes, and thus only one qualitative study was included (44). Results indicated that listening to music improved nutritional intake, group singing reduced anxiety after meals, while songwriting assisted in processing various therapeutic issues. A recent systematic review of controlled studies utilizing music therapy in ED treatment found no randomised studies and only two relevant publications from one treatment-as-usual (TAU) controlled study (45). Pre-post results (quantitative and qualitative) indicated a decrease in post-meal stress and anxiety following 1-hour music therapy group sessions twice per week, which was greater for the music therapy intervention than TAU (48, 49). The group sessions integrated various music therapy methods such as singing, listening to music, and songwriting. Chang et al. conducted a narrative systematic review that evaluated therapeutic outcomes in individuals with EDs, where music was a component of the intervention (46). Results from 16 quantitative, qualitative and mixed methods studies indicated that the intervention improved mood regulation, helped manage distress associated with mealtimes, and improved emotional wellbeing. The authors indicate generalisability of the results is limited due to small sample sizes (16 studies ranged from 3 to 20 participants) and the lack of detailed information about the MBIs. While in a recent systematic review exploring the extent to which music therapy and systemic or family-based therapy is integrated into ED treatment, the examination of 26 studies revealed common parallels across where both facilitated embodiment and interconnectedness, served as a gateway of deeper engagement with self and illness, fostered and self-expression, and supported emotion regulation (47).
Each of these systematic reviews have captured a corpus of the literature, helping to explicate the use of music in the context of EDs or subclinical disorder. However, there has been a lack of singular focus on studies where music is a key component to the intervention, which is instrumental to a clearer understanding of the impact of MBIs. For example, all the above reviews except one (45) included studies where background music was played in a video, but music was not a focus of the intervention. Further, systematic reviews can limit the type of research literature included, resulting in rich therapeutic descriptions from clinical case studies being excluded. A recent study revealed widespread adaptation of music therapy methods to meet the needs of patients in ED treatment (50). Case studies illustrating these varied and nuanced ways of delivering and engaging with MBIs would further inform literature reviews and support clinicians employing MBIs in building an evidence-based practice.
Therefore, the aim of this scoping review was to encompass studies where music comprised an essential component of the intervention in a therapeutic ED setting, including case studies to contextualise and more comprehensively understand the use of MBIs in the context of ED treatment. A challenge in reviewing and evaluating MBIs in research is that there is often a lack of clarity in the literature due to inconsistent terminology and quality of reporting (51, 52). As a result, MBI reporting guidelines were introduced in an effort to improve the transparency and specificity of MBIs as well as to evaluate the quality of the research and ensure that it can be replicated (51). The present scoping review therefore also expands on prior systematic reviews by examining the clarity of reporting based on these MBI reporting guidelines.
Methods
A scoping review of the literature was conducted, using a systematic and iterative approach to evidence synthesis. This adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines (53) and was pre-registered with the Open Science Framework (https://osf.io/4xv9f).
Search strategy
Eight electronic databases were queried for relevant articles from inception to May 2025, including MEDLINE (National Library of Medicine), Embase (Elsevier), Scopus (Elsevier), APA PsycArticles (American Psychological Association), APA PsycINFO (American Psychological Association), Psychology and Behavioural Sciences Collection (EBSCO), Web of Science (Clarivate), and Cochrane Library (The Cochrane Collaboration). The following search terms were applied: (music therapy OR music-based intervention OR guided imagery and music OR songwriting OR song composition OR drumming OR music listening OR music improvisation OR song discussion OR active music making) AND (eating disorders OR anorexia nervosa OR bulimia nervosa OR binge eating disorder OR pica OR rumination disorder OR avoidant restrictive food intake disorder OR unspecified feeding OR eating disorder). There were no restrictions on publication date or status; however, articles were filtered by subject (humans only), study type (peer-reviewed), and language (English). In addition to database searches, reference lists and relevant conference abstracts were hand-searched to identify supplementary eligible studies.
Study selection
The following inclusion criteria were applied to evaluate eligibility in the qualitative synthesis: (1) patients of any age and sex with a primary ED diagnosis; (2) MBIs (i.e. any intervention utilising music as a core component, including music therapy and other non-music therapist delivered music experiences used in the treatment or management of EDs across any clinical or community setting; (3) qualitative, quantitative, and mixed methods studies, whether prospective or retrospective, including case reports; and (4) peer-reviewed articles and published in the English language. To ensure breadth and relevance, inclusion was not limited by study design, publication status, or geographical location. Primary outcomes of interest encompassed physical and mental health following the implementation of MBIs. We included all study designs, excluding review articles, book chapters, nonhuman studies, conference abstracts, and articles in a language other than English. Studies were excluded if ED was not the primary diagnosis, if the MBI was not a key component of the intervention, or the paper was not available in English. Screening of the articles was independently performed by four reviewers (AH, AR, JB, JG). Any disagreements were resolved during discussions between the reviewers.
Data charting
Data from eligible studies were charted by five independent reviewers (AH, AR, JB, JG, TM), including two (JG, TM) with no prior content knowledge of the topic. This approach allowed for both subject-matter expertise and naïve interpretation, helping to minimize potential bias while enhancing objectivity and transparency. Using a standardised charting form created in Microsoft Excel, the following variables were extracted: author, publication year, country, study design, and outcome measures; sample size, participant age, and ED diagnosis; intervention type, duration, and setting; and primary outcomes and any other pertinent findings. Details were recorded when studies indicated the facilitator’s theoretical approach and methods or techniques used. A sixth reviewer (SASN) examined all extracted data to ensure alignment with inclusion criteria and internal consistency. Discrepancies were resolved through team consensus. The charting form was updated iteratively to accommodate emerging themes and variations in data reporting across studies.
Evidence synthesis
Qualitative and quantitative studies were summarised in a narrative format. Qualitative data were then analysed thematically. Additionally, evaluation of MBI reporting for each study was also conducted following established MBI reporting guidelines (51, 54).
Qualitative data analysis
Qualitative data was integral to 17 of the studies and was initially reviewed by one research team member (AH) to begin the reflexive thematic analysis. This process entailed reviewing and coding the data following the six-step process (55, 56). Emergent themes were identified based on integrating the outcome data from these studies. This iterative process included grouping themes into categories of similar orientation. The next step involved examining these categories to identify points of connection and patterns. This led to developing subordinate themes which were then reviewed by all members of the research team and integrated into a comprehensive framework. When discrepancies emerged, the reviewers returned to the data to inform their discussion and understanding of the themes. This iterative process continued until reviewers (AH, SN) reached a mutually agreeable decision. Following this, other research team members were asked to complete a final review of the themes to ensure full team consensus.
Results
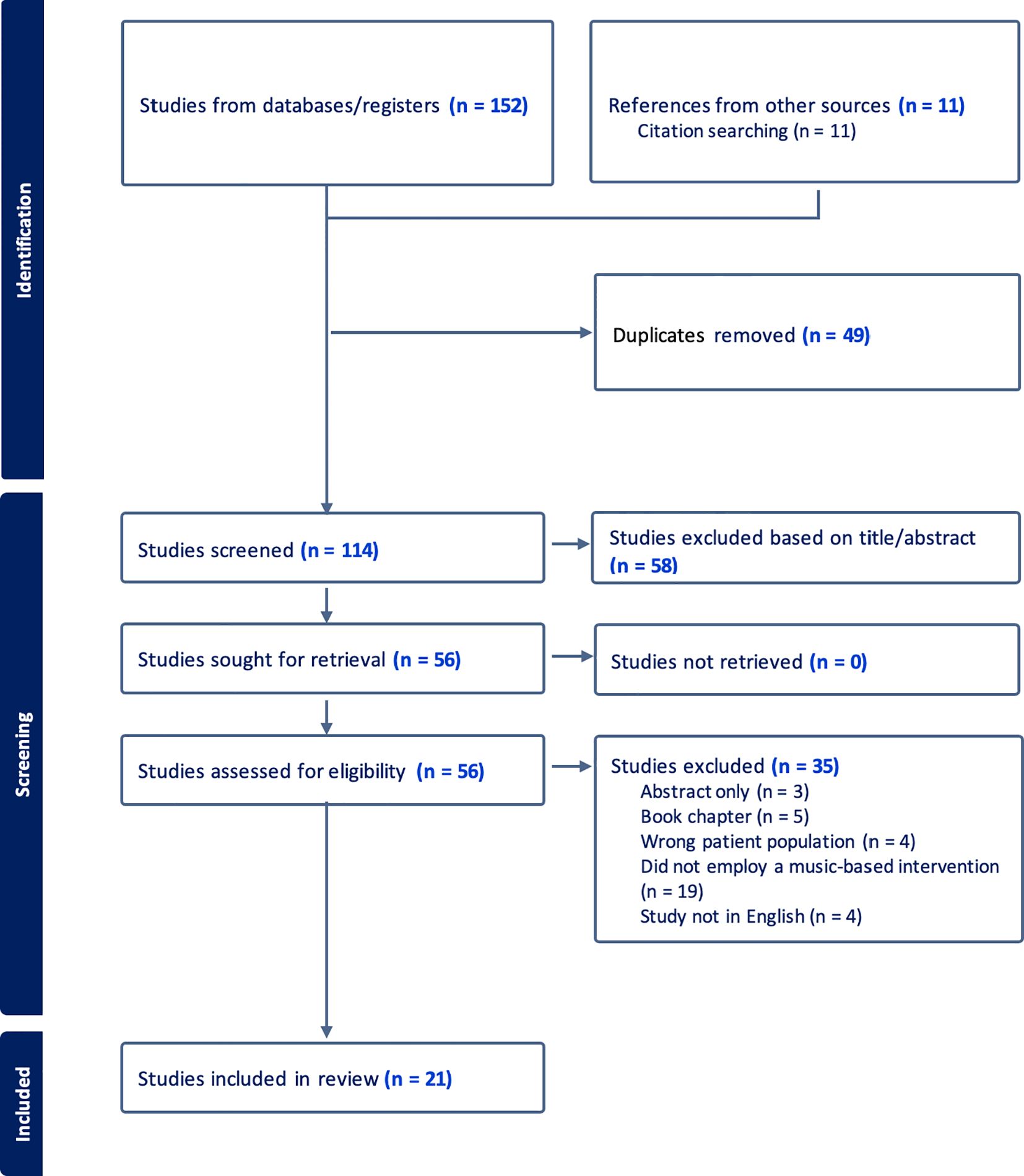
The literature search identified 163 relevant citations. After removing duplicates and conducting title and abstract screening, 56 articles remained for further evaluation. Full texts of all potentially eligible papers underwent a thorough review, resulting in the exclusion of 35 articles. After careful consideration, 21 articles met all the criteria and were included in the scoping review. The PRISMA flow diagram illustrating the study selection process can be seen in Figure 1.
Study characteristics
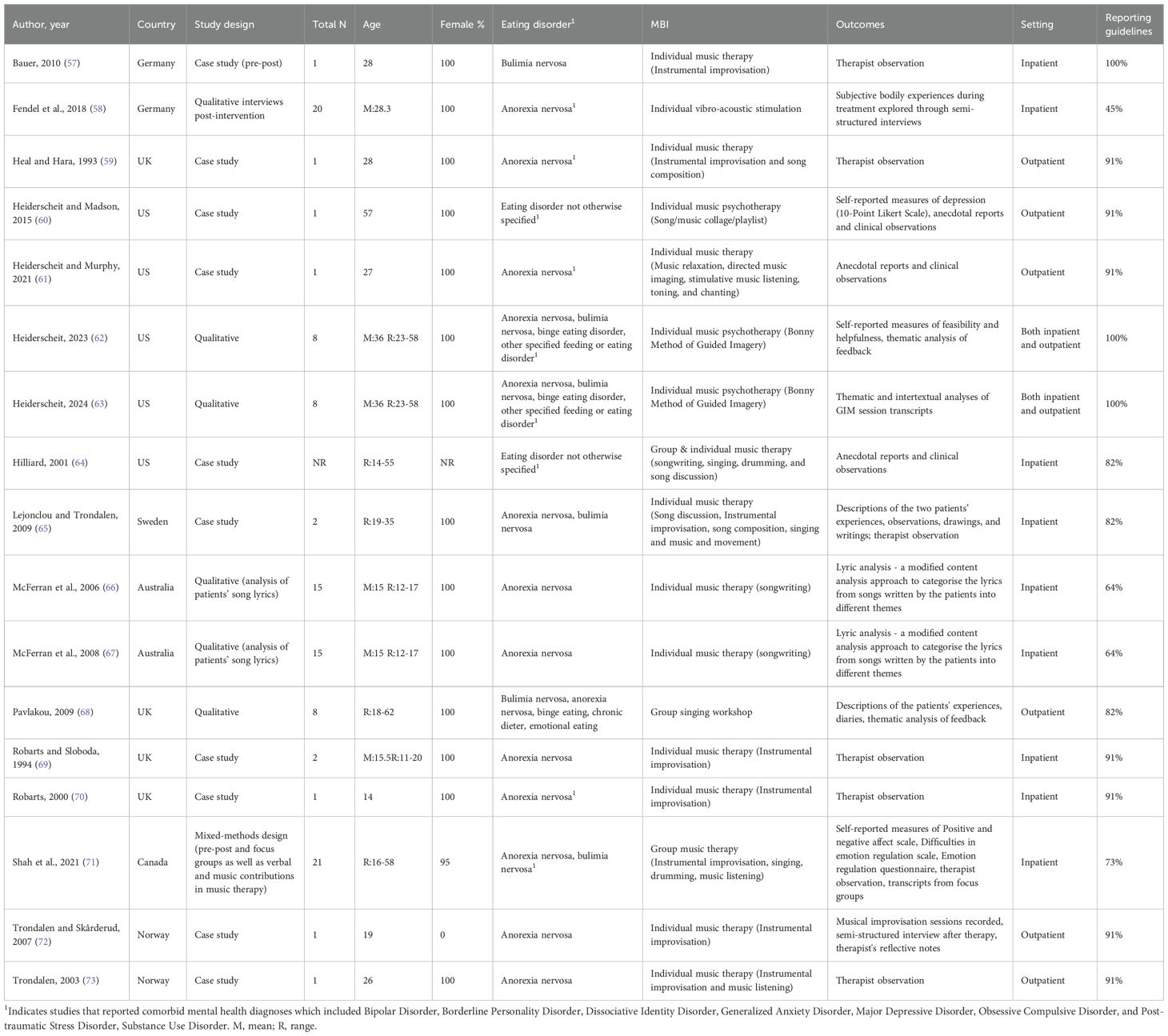
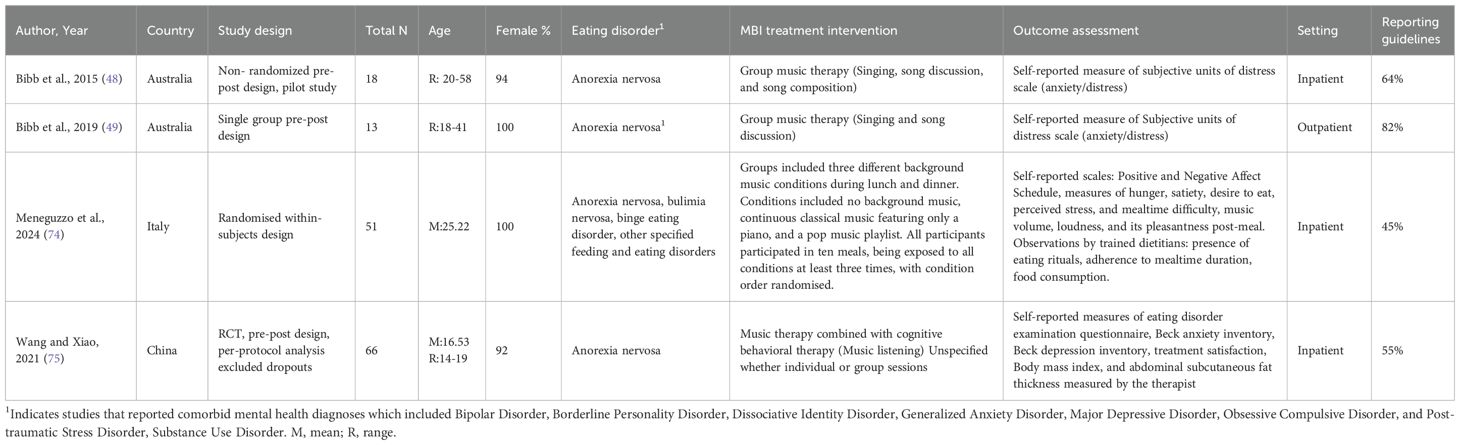
Study characteristics and participant demographics are reported in Table 1 (qualitative studies) and Table 2 (quantitative studies) including country of publication, study design, sample size, participants’ age, gender, participant diagnostic information, type of music intervention, source of outcome assessment used, setting, and assessment based on reporting guidelines. This included identifying how many of the 11 recommended and relevant components from the 7 criteria were included in the MBI reporting of the study (50, 53). The component of treatment fidelity was not included in evaluating case reports as it is not relevant to this type of research.
The majority of included studies were carried out in Europe (n=10) followed by North America (n=6), Australia (n=4), Asia (n=1), for studies with available data. Overall, 254 participants (range:1-66) were included from ages 11 to 62 for studies with available data. The research methods used were primarily qualitative (n=16), with the remainder quantitative (n=4) or mixed methods (n=1). Most studies reported on anorexia nervosa (n=19), followed by bulimia nervosa (n=7), binge eating disorder (n=4), other specified feeding or eating disorder (n=4), emotional eating (n=1), chronic dieter (n=1), and eating disorder not otherwise specified (n=4). Evaluation of reporting guidelines differed across studies, with a range of 45-100% and a mean of 76%, equivalent to reporting on nearly 8 of the 11 components.
MBIs were identified when details regarding the music experience were provided. MBIs are reported as music therapy when facilitated by a qualified music therapist and other MBIs (non-music therapist delivered) are reported by the type of intervention only. Within the included studies, the majority investigated music therapy (n=18). Music therapy sessions included individual (n=12), group (n=4), and both individual and group sessions (n=1). One study did not specify whether the sessions were in a group or individual format. Music therapy sessions utilized receptive music experiences (n=10) (song discussion, music listening for relaxation, or music directed imaging), instrumental improvisation (n=8), songwriting or song/music collage (n=7), singing or chanting/toning (n=5), drumming (n=2) or movement to music (n=1). One music therapy intervention combined music listening with cognitive behavioural therapy. MBIs led by non-music therapists (n=3), two qualitative and one quantitative) included vibroacoustic stimulation, a singing workshop, and music listening during mealtimes. Details of the music therapy theoretical approaches, when indicated, are further outlined in subsequent sections.
Qualitative results
Qualitative studies included a total of 106 participants, which were comprised predominantly of case reports/studies (n=10), and qualitative designs (n=6), followed by mixed methods pre-post design (n=1). Nine were conducted in an inpatient setting, six in outpatient settings, and two studies across both inpatient and outpatient settings. Gender of study participants was between 95-100% female; one case report did not report gender. Nine of the studies reported comorbid mental health diagnoses that included bipolar disorder, dissociative identity disorder, generalized anxiety disorder, major depressive disorder, obsessive compulsive disorder, post-traumatic stress disorder, and substance use disorder. Study outcomes were based on therapist observations (n=9), self-report (n=3), analysis of content from sessions (song lyrics, musical improvisation, imagery) (n=5), and semi-structured interviews (n=2). Evaluation of the reporting of the qualitative studies represents a range of 45-100% with a mean of 84%, reflecting reporting of approximately 9 of the 11 components.
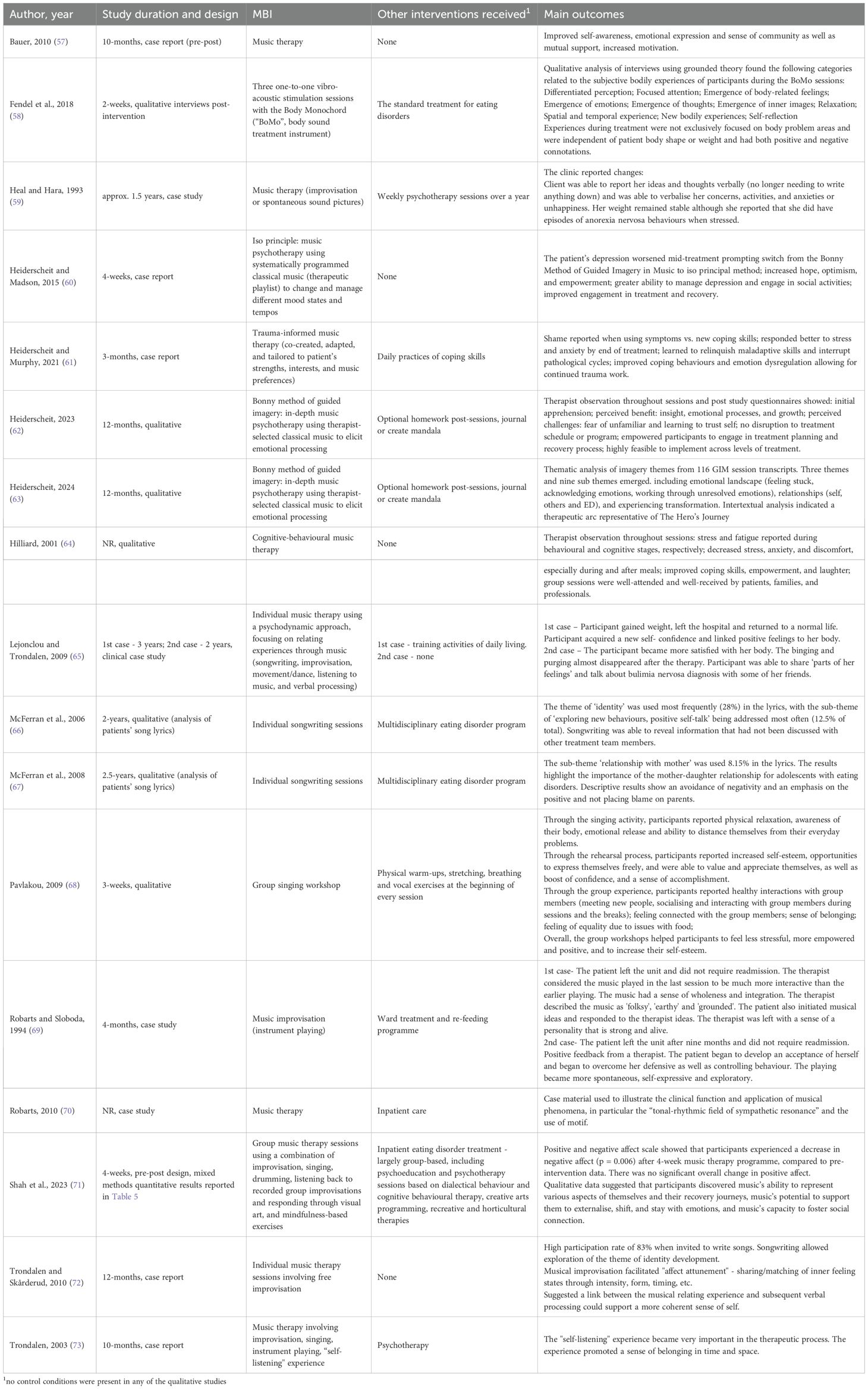
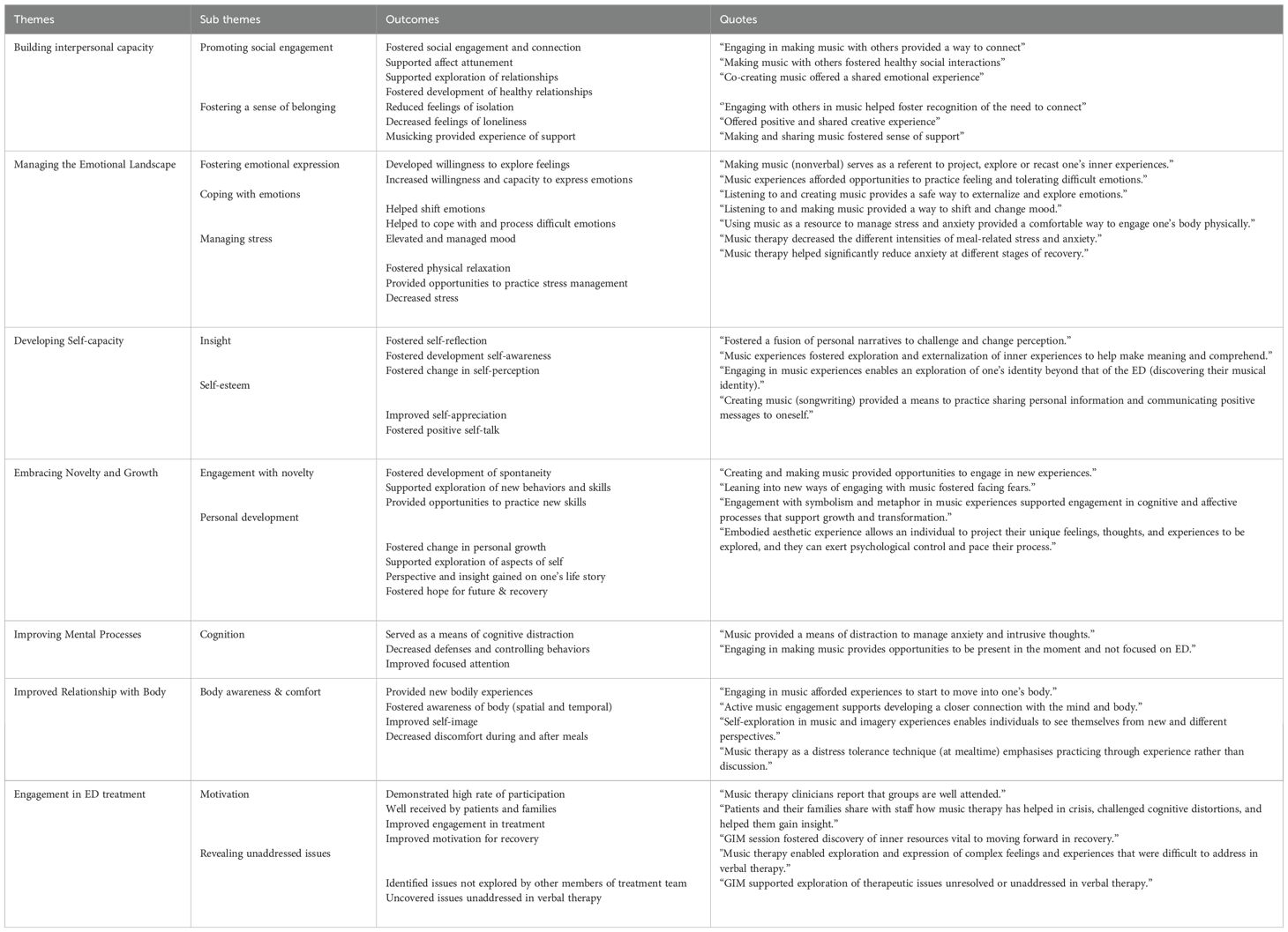
Table 3 highlights study duration within the context of design, detailing information on the MBI, theoretical approaches, and any other intervention components. Finally, the main results from the studies are indicated. We note that length of intervention varied widely across these studies, from two weeks to 2.5 years. Main results were further explored through the thematic analysis. This analysis resulted in seven emergent outcome themes being identified including: building interpersonal capacity, managing the emotional landscape, developing capacity in self, embracing novelty and growth, mental processes, experience and relationship with body, and fostering engagement in ED treatment. Table 4 presents the 7 themes with the 13 emergent subthemes, along with related outcomes and quotes. Quotes from the studies included in the analysis provide examples of content that informed the themes. We note that negative outcomes were only reported in one study and consisted of experiencing the body more consciously and a negative evaluation of new experiences.
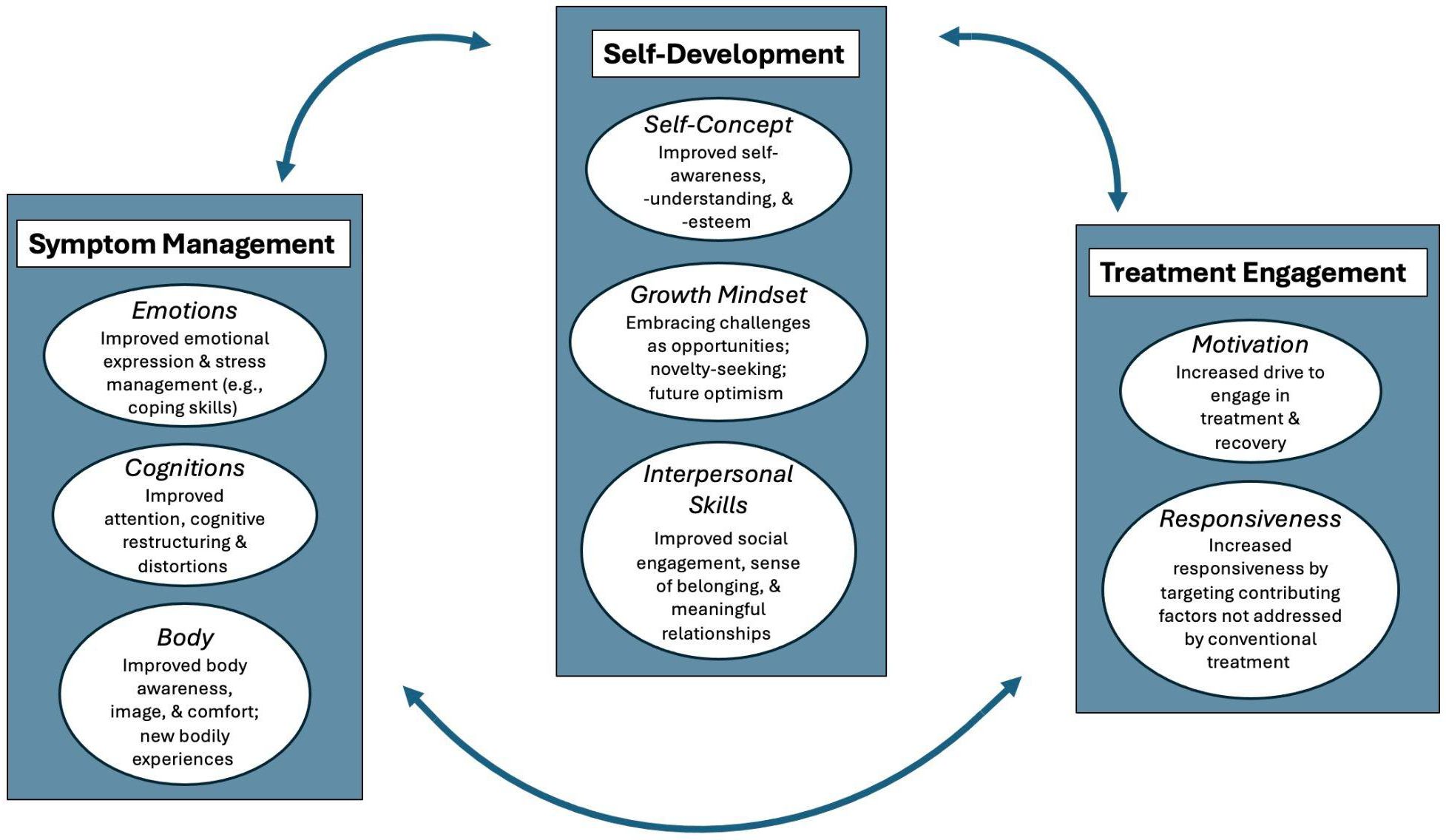
Organization of these themes reflects various stages of the treatment and recovery process. Figure 2 illustrates how these themes follow differing levels of treatment, beginning with symptom management that focuses on fostering emotional expression, stress management and developing coping skills which leads to improved attention and cognitive restructuring, leading to improved body awareness and body image. This therapeutic work supports transitioning to self-development that highlights improved self-awareness and self-esteem, developing a growth mindset through engaging in new and novel experiences, and supporting the development of interpersonal skills through social engagement. The therapeutic work in these areas fosters engagement in treatment through increased motivation and responsiveness by addressing contributing or underlying issues that have not been addressed by conventional treatment. Figure 2 illustrates that these processes are not linear but rather circuitous, meaning an individual may move back and forth through these at different levels of ED treatment.
Quantitative results
Overview of quantitative study characteristics (SN) included only five studies which met inclusion criteria (see Table 2, with one study included in Tables 1, 3 and 5 as a mixed methods study (71)). Three studies focused on patients with anorexia and two studies also included other EDs. Comorbid mental health diagnoses were reported in two studies. Subjects were 92-100% female (seven males out 169 total participants across studies), all but one study was conducted in adults, and all studies used a pre-post design. Table 5 outlines the results of the quantitative studies, explicating study duration, design, music intervention and main outcomes. A Canadian study of group music therapy (MT, e.g. improvising and drumming) showed a significant decrease in negative affect and emotional suppression following MT; however, the MT also included mindfulness and was accompanied by treatment as usual (TAU) such as CBT and DBT (71). With this multifaceted intervention and no control group, one cannot discern whether the MT or other intervention components were instrumental in driving this observed improvement. Two Australian studies involved interventions comprised solely of group MT (e.g. singing and discussing songs), based on a humanistic therapeutic approach (48, 49). While neither study had random assignment, both interventions showed a significant decline in anxiety and distress immediately post intervention and one study showed a steeper decline in the intervention versus inpatient TAU control (48). A crossover study (where participants receive all conditions and so are their own control) of an MBI in Italian inpatients showed that compared with no music being played at supervised mealtimes, when patients listened to either classical or pop music during mealtimes, they consumed more food and had greater positive emotions following the meal (74). However, there was no waiting period between the interventions to ensure the effects of the first treatment wore off before delivering the next treatment (75).
Finally, a Chinese study on adolescents involved a receptive (music listening) MT intervention plus CBT and TAU compared with inpatient TAU only as the control group (76). While these groups were randomly assigned, the study conducted per-protocol analyses without dropouts, and there was a significantly greater dropout in the control vs intervention group (22.5% vs 5.4%). The study reported a greater increase in post-treatment weight, BMI, and abdominal subcutaneous fat in the MT + CBT arm compared with the control group. However, it is impossible to determine whether this was due to MT, CBT, or both. MBI reporting of the quantitative studies ranged from 55-82% with a mean of 67%, reflecting reporting on about 7 of the 11 components. While no negative outcomes were reported in any of the quantitative studies, null findings were reported in two of the studies (e.g. positive affect and impulse control (71); negative affect, stress, satiety (74)). In sum, coupled with small sample sizes, none of the quantitative studies implemented best practice of randomly assigning individuals to clear MBI and control groups, precluding firm conclusions about the efficacy of MBIs in people with EDs.
Discussion
This scoping review examined a broad body of evidence allowing for a general synthesis of outcomes following MBIs for individuals in ED treatment. It included 20 studies that investigated MBIs for individuals engaged in ED treatment. This resulted in 16 studies that examined purely qualitative data (including case reports), four that assessed quantitative outcomes and one mixed methods study. Due to the specialized nature of ED treatment and the limited body of literature related to MBIs in ED treatment, this scoping review was conducted to capture and review a broader scope of research literature focused on MBIs as a primary intervention for ED, which differs from previous reviews (44–47). This helped to capture research with diverse methodologies as it included clinical case reports that are reflective of clinical practice and the therapeutic process. As a result, it helps contextualize and provide a more comprehensive understanding of the use of MBIs in research and in practice of music therapy in ED treatment (64, 78).
The nature of a scoping review is not to provide an overall assessment of quality of the literature, as this rigor can lead to missing or excluding relevant research (79). Capturing a diverse body of literature can provide deep and rich data to examine thorough descriptions of the therapeutic process (80). This scoping review examined studies published in English which precluded non-English language studies and as a result limits generalisability in some cultures (81, 82). Furthermore, our review only found one study which was not from a high-income Western country, and there were very few males studied, pointing to the importance of focused work in these groups. Given the majority of the literature reviewed included case studies, feasibility and pilot studies with small sample sizes and no control groups includes a risk of selection or information bias which limits the generalisability of the results (83). Further, it is worth noting that synthesizing the findings was challenging as therapeutic work within case reports is tailored and unique to each individual and at times a lack of clear and detailed information is provided when reporting the MBI. As a result, the findings are less directly relevant to clinical or treatment guidelines but can help to identify clinical considerations for treatment and inform recommendations for future research (50). Further, negative outcomes were only reported in one study and were specific to the use of the body monochord (BoMo) during inpatient ED treatment which resulted in experiencing the body more consciously and a negative evaluation of new experiences. Further, it is not clear what experience or training the therapist had with the BoMo as the therapist was not a qualified music therapist (59). These findings may indicate the need to identify at what point in the treatment trajectory is most appropriate for this type of body based therapeutic work. The limited reporting of negative outcomes across studies may indicate bias and a need for more transparent reporting. However, negative outcomes may be mitigated by music therapists’ reported awareness and training regarding avoiding harm in ED therapeutic settings (50, 84, 85).
Music-based interventions utilised in eating disorder treatment
The studies implemented a wide array of MBIs, including music listening (listening to classical or popular music and song discussion, music-based relaxation, music-directed imaging, movement to music, and vibroacoustic stimulation), song writing, instrumental and vocal improvisation and active music making experiences (singing, group singing and drumming), while several studies integrated multiple types of MBIs. Although not reported in many of the included studies, theoretical approaches reported within the music therapy interventions included psychotherapeutic, cognitive-behavioural and trauma-informed music therapy. The large number of interventions utilised illustrates the diversity and depth of MBI options available to meet the emerging and changing needs of a patient at various levels of care and across the treatment process (63). These findings are consistent with a recent mixed methods study that surveyed and interviewed music therapists working with patients in ED treatment, which indicated clinicians utilize a wide array of methods in their regular clinical practice to address diverse therapeutic needs across levels of treatment and adapt these to meet the needs of individual patients and groups (50). This aligns with the focus on personalized ED care with tailored interventions based on individual psychological, biological, environmental, and genetic profiles (86).
While it is evident that the current body of research does not fully represent the diversity of interventions utilized by qualified music therapists and non-music therapists in the context of clinical practice in ED treatment, the inclusion of case reports (half of the studies in our review) gives breadth and depth of understanding and further highlights other methods including song discussion, music listening, group drumming, guided imagery and music, and music and movement. Additionally, it is worth noting that all but two of the studies in the scoping review (18/20) integrated music therapy facilitated by a qualified music therapist, highlighting a need for professional training required to implement MBIs within the treatment of these complex disorders.
Overall, the qualitative studies provided detailed information when reporting the MBI, meeting an average of 84% of MBI reporting guidelines (51, 53), compared to the quantitative studies that reported an average of 67% of the guidelines (note six qualitative studies were published before the MBI guidelines and all quantitative studies were published four or more years after publication of the MBI guidelines). Given that 10 of the 17 qualitative studies include case reports which typically provide rich and thorough descriptions of the therapeutic process, this difference in reporting is not surprising. Information consistently missing from the quantitative studies included details regarding the music intervention and materials utilized in the sessions. Clear and detailed reporting of MBIs is key to transparent reporting of the intervention and for replicating a study. Nonetheless, studies within this review demonstrate an improvement in the overall quality of reporting compared to a previous evaluation of music intervention studies, where reporting was poor (52). This may be due to the fact that more of the present studies were, which typically include detailed information about the music-intervention within the therapeutic process.
Music-based interventions methods of delivery
In a majority of the studies in this review the MBIs were facilitated by a qualified music therapist. The other three studies included group singing workshops led by music teachers (68), vibroacoustic stimulation led by a therapist (no specific therapeutic training specified) (58) and music listening during mealtime delivered by dieticians and nurses (75). In the three studies facilitated by non-music therapists, participants reported numerous positive outcomes, with some negative outcomes related to the vibroacoustic body music. These studies illustrate how researchers are flexibly utilizing different ways of engaging with music to address the needs of patients in ED treatment. The reporting of the MBI in these three studies varied significantly, from 5 of the 11 aspects of the intervention (58) to 9 of the 11 (68). Ensuring that all MBI research adheres to the MBI quality reporting guidelines (51, 54) is instrumental, so the intervention is described in detail and there is clarity, and transparency in research methodology. The complex nature of music stimuli requires detailed and careful description to ensure a study can be replicated and necessitates music-based knowledge and expertise to describe it effectively. Since MBIs include music experiences that may be facilitated by music therapists, administered by staff, community musicians, other providers, or self-administered by the patient/patient, clarity in intervention descriptions is vital (50, 54). Dedication and advocacy to improve the quality of reporting of MBIs will help improve the rigor and reproducibility of these interventions (51, 52, 54, 85).
It is evident from our review that group and individual sessions offer unique affordances and may help to address different therapeutic needs. Across our reviewed studies (excluding case studies, which by necessity were individual MBIs), individual and group MBIs were used comparably (n=5 and n=4, respectively), with one study not reporting which method was used. Group based music interventions provide opportunities that capitalise on meeting new people, fostering a social connection (71), engaging in healthy social interactions, and feeling a sense of belonging (68), as well as feeling motivated to engage in treatment (64).
Group sessions can be economical and providing opportunities for social engagement in a shared or collaborative experience is particularly important if an individual feels isolated due to their ED (76). There is also a means of support that can be embedded or experienced in group MBIs that is valuable when engaging in a new or novel experience such as improvisation or songwriting (66, 73). Conversely, individual sessions can provide therapeutic space needed to address complex or deeply personal issues, which may include ED symptoms (restricting or purging) or trauma that are not appropriate for group based work (61, 86, 87). A trauma-informed approach to MBI practice is recommended to inform clinical decision-making and avoid causing harm (42, 50, 61). From synthesising information regarding patient presentation across the studies, we are encouraged that choice of group versus individual MBIs appear to have been selected to best meet patient needs.
Addressing multiple and diverse issues in eating disorder treatment
EDs are complex in nature due to the multiple underlying factors that contribute to their development, the symptoms that negatively impact physical health and psychological wellbeing, a myriad of comorbid diagnoses, and a high incidence of trauma (15, 86, 87). While only half of the studies in our scoping review reported on comorbid mental health conditions, seven comorbid conditions (including trauma-related conditions) were reported across these studies. This indicates that many MBI studies include complex cases but also highlights that presence (or absence) of comorbid conditions needs more consistent reporting in future studies. This complex clinical matrix necessitates treatment across various levels of care that addresses the diverse and underlying issues needed to support an individual’s ED treatment process (36, 37, 62). The studies in this scoping review included individuals engaged in various levels of treatment including inpatient, residential, and outpatient. This is consistent with survey data indicating the clinical settings in which music therapists work with patients with EDs (50). While ED treatment may occur at specialty ED treatment programs, music therapists also provide services to patients in private practice, mental health units, medical units, long term psychiatric settings, and community mental health settings (46, 50). Providing treatment across various levels of care indicates that music therapy and MBIs are utilized to address a variety of therapeutic needs.
The present review’s qualitative and quantitative results indicate MBIs focus on a wide array of therapeutic issues and needs. The qualitative themes emerging from these interventions operate across various levels of ED treatment and recovery - that of symptom management, self-development, and treatment engagement as indicated by our model in Figure 1. The organization of these themes aligns with various levels of therapeutic work consistent with previous literature that highlights, “the flexibility of music as a therapeutic agent allows the therapist to individualize the process and meet a wide array of needs simultaneously, especially when feelings and emotions may be fragmented, elusive and inaccessible to language” (77) (p.128). Addressing core emotional processes is key, as impaired affective processes are often implicated in the maintenance of disordered eating behaviours (87). Recent research including a comprehensive synthesis of 30 years of clinical and empirical evidence underscores the importance of affective temperament, emotion regulation, and personality vulnerabilities related to symptom management (emotions, cognition, and body image) as a prerequisite to self-development (89–92). Thus, our model begins with symptom management by fostering emotional expression and learning coping skills to manage stress. This supports changes in cognition such as improved attention, and cognitive restructuring, which helps to decrease distortions. This supports shifting the relationship with one’s body by improved body awareness and image and increasing the level of comfort in one’s body through experiencing new ways of engaging the body.
In our model, symptom management then supports engaging in the next level of self-development which includes improved self-awareness, understanding, and self-esteem, which is substantiated by research indicating that addressing these emotional underpinning of the ED enhances treatment outcomes (88). Prior MBI literature highlights how songwriting links self-expression to the development of autonomy and exploring or developing one’s identity (66, 69). Building this self-capacity is key to a growth mindset which is necessary to support embracing challenges by facing fears and engaging in new experiences, which can foster hope and optimism (62, 63). These experiences are instrumental in having the capacity to develop interpersonal skills through increased social engagement, which helps to foster a sense of belonging and engagement in meaningful relationships (61, 65). This work can then lead to increased motivation to engage in treatment, fostering responsiveness to address and target contributing issues that have not been addressed in conventional ED treatment (44, 46, 62). However, we note that our model follows an iterative feedback loop, with treatment engagement facilitating further symptom management and self-development, which promotes continued healing and recovery. We further acknowledge that effective initial symptom management must be catalysed by an initial willingness to engage in treatment.
The capacity of MBIs to address diverse therapeutic needs across various levels of treatment is also highlighted in Dvorak’s survey of music therapists working in ED treatment (50). These therapists reported addressing 90 different treatment areas, with the five most common including self-expression, development of coping skills, managing mood and depression, and identifying and expressing feelings. While these only encompass the first component of the “symptom management” level in our model, cognition and body image/awareness (other components of the “symptom management” level) were treatment areas identified by more than half of therapists in that study. Further, self-esteem and self-awareness (operating on the “self-development” level of our model) were identified by therapists as comparably frequent treatment areas to identifying and expressing feelings (50). However, interpersonal/social aspects and optimism (other components of the “self-development” level) were less frequently cited as treatment areas by therapists in the study, and growth mindset components of embracing challenge and novelty-seeking were not included as a response in this survey. This highlights the importance of qualitative research which can bring out important factors which have been previously unidentified. Our review reveals growth mindset as a potentially important outcome which should be assessed in future MBIs for people with EDs. Indeed, previous research has explicated the unique capacity of creative and aesthetic experiences to afford opportunities to externalize and explore their thoughts and feelings in new and different ways, which helps an individual to develop new understandings and attach new meaning to them (63, 93, 94). This is further evidenced by quotes from Table 4 which indicate that making music (nonverbal) serves as a referent to project, explore or recast one’s inner experiences (65) and that this process of externalizing inner experiences helps to make meaning and comprehend their experiences (62). Engagement in a supported creative aesthetic therapeutic experience can help individuals in ED treatment access affective, cognitive and perceptual brain functions which are key to their treatment and recovery process (92) and are instrumental in developing insight, fostering growth, and a sense of mastery and self-efficacy (62, 63, 66, 72, 73).
Implications of this study and recommendations for future research
Although findings generally support positive outcomes for individuals ED treatment following a MBI, our conclusions are impeded by the heterogeneity of interventions and outcomes, and inadequately controlled methods to ascertain effectiveness. Synthesizing this body of literature is also impacted by the complex nature of EDs, including the physical and psychological aspects of the disorder, as well multiple comorbid diagnoses and trauma history. While some research methodologies may not be able to robustly capture the nuanced and complex phenomenon of MBIs, ensuring clear and transparent reporting is necessary to provide a clear understanding of the therapeutic intervention. Further, these shortcomings will be addressed with more rigorous quantitative studies which capture the range of patients treated in practice and appropriately assess treatment effects. To that end, there is a particular need for well-powered randomised controlled trials with distinct and clearly defined comparison groups, implementing intention-to-treat analyses and assessment of and controlling for diverse clinical and background factors (96). This will necessitate researchers addressing the challenges and barriers in conducting RCTs with MBIs in ED treatment, particularly balancing the personalisation of therapy with the required standardisation (97).
Future reviews should aim to understand and explicate the efficacy, benefits, and risks of MBIs in ED treatment, and the role of MBIs in addressing the complex and myriad needs of individuals in the treatment process. Given the established link between emotional rigidity, emotion regulation, and ED symptoms, there is need for specific exploration of MBIs that support the development of temperament-linked coping styles (50, 78, 89). Further, all future studies should provide detailed information on case presentation (including comorbidities), comprehensive descriptions of the MBIs utilized, as well as the experience, qualifications, and theoretical orientation of the professionals facilitating the MBI. Future reviews should assess each study’s adherence to MBI quality reporting guidelines (51, 54). Due to the unique nature, variety, and complexity of MBIs, adhering to these reporting guidelines to explicate the different components of the intervention is crucial in supporting replicability and identifying key and active elements in the intervention (44, 51, 52, 54).
Conclusion
The high economic cost and incidence of EDs indicates a need for innovative and effective treatment approaches (97, 98). While there is a small corpus of literature to date on MBIs for EDs, there is clear evidence that MBIs have the capacity to address a wide array of therapeutic needs for individuals across the various levels of ED treatment. The present review shows across a range of case reports and research studies that MBIs can be tailored to individual or group therapy to meet emerging and changing needs over the course of ED treatment. The unique potential of music therapy to not only address a myriad of issues but also uncover issues that have not been addressed in verbal therapy suggests that ED treatment programs would benefit from integrating this type of creative modality alongside psychological therapies. Further rigorous quantitative studies, especially randomised controlled trials evaluating and comparing MBI enhanced therapy to more traditional approaches are required to evidence support of more widespread usage of MBI for people living with ED. This type of evidence is necessary to inform clinical treatment guidelines (i.e. NICE guidelines), help to promote government support for funding, and foster widespread usage of these modalities (95).
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
AH: Conceptualization, Resources, Writing – review & editing, Visualization, Supervision, Data curation, Writing – original draft, Project administration, Formal analysis, Validation, Methodology. SN: Conceptualization, Writing – original draft, Formal analysis, Resources, Methodology, Writing – review & editing, Data curation, Visualization, Supervision, Validation. AR: Conceptualization, Writing – review & editing, Methodology, Formal analysis, Data curation. JG: Data curation, Writing – original draft, Formal analysis, Conceptualization, Writing – review & editing, Methodology. JB: Writing – original draft, Writing – review & editing, Formal analysis, Data curation, Methodology, Conceptualization. TM: Formal analysis, Writing – review & editing, Data curation.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. SN was supported by the Wellcome Trust Early-Career Award (226392/Z/22/Z). AR was supported by the Reginald John Smith Studentship; the King’s College Studentship; the Cambridge Commonwealth, European, and International Trust. All research in the Department of Psychiatry at the University of Cambridge is supported by the NIHR Cambridge Biomedical Research Centre (NIHR203312) and the NIHR Applied Research Collaboration East of England. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. The funders had no involvement in the collection, analysis, or interpretation of data, writing of the report, or the decision to submit the article for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th. (2013). doi: 10.1176/appi.books.9780890425596.
2. Schaumberg K, Welch E, Breithaupt L, Hubel C, Baker J, Munn-Chernoff M, et al. The science behind the Academy for Eating Disorders’ Nine Truths About Eating Disorders. Eur Eating Disord Rev. (2017) 25:432–50. doi: 10.1002/erv.2553
3. Schmidt U, Adan R, Bohm I, Campbell I, Dingemans A, Ehrlich S, et al. Eating Disorders: The big issue. Lancet Psychiatry. (2016) 3:P313–315. doi: 10.1016/S2215-0366(16)00081-X
4. Solmi M, Radua J, Olivola M, Croce E, Soardo L, de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. (2022) 27:281–95. doi: 10.1038/s41380-021-01161-7
5. World Health Organization (WHO). Global health estimates: Leading causes of DALYs (2024). Available online at: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/global-health-estimages-leading-causes-of-dalys (Accessed April 2, 2024).
6. Erskine H, Whiteford H, and Pike K. The global burden of eating disorders. Curr Opin Psychiatry. (2016) 29:346–53. doi: 10.1097/YCO.0000000000000276
7. Hay P, Aouad P, Marks P, Maloney D, National Eating Disorder Research Consortium, Touyz S, et al. Epidemiology of eating disorders: Population, prevalence, disease burden and quality of life informing public policy in Australia-a rapid review. J Eating Disord. (2023) 11. doi: 10.1186/s40337-023-007387
8. Zahra S, Safdar M, Khalid M, Khalid W, and Ranjha M. Trends in the burden of eating disorders in Pakistan over the past three decades: A joint point regression analysis. Ann Indian Psychiatry. (2023) 7:140–51. doi: 10.4103/aip.aip_8_22
9. Santomauro D, Melen S, Mitchison D, Vos T, Whitford H, and Ferrari A. The hidden burden of eating disorders: an extension of estimates from the global burden of disease study 2019. Lancet. (2021) 8:320–8. doi: 10.1016/S2215-0366(21)00040-7
10. Martin-Wagar C, Boswell R, Bennett B, Perelman H, and Forrest L. Psychological and eating disorder symptoms as predictors of starting eating disorder treatment. Int J Eating Disord. (2021) 54:1500–8. doi: 10.1002/eat.23538
11. Zipfel S, Schmidt U, and Giel K. The hidden burden of eating disorders during the COVID-19 pandemic. Lancet Psychiatry. (2022) 9:9–11. doi: 10.1016/S2215-0366(21)00435-1
12. Tannous W, Hay P, Girosi F, Heriseanu A, Ahmend M, and Touyz S. The economic cost of bulimia nervosa and binge eating disorder: A population-based study. psychol Med. (2022) 52:3924–38. doi: 10.1017/S0033291721000775
13. Berry L, Rock B, Houskamp B, Brueggeman L, Houskamp B, and Tucker L. Care coordination for patients with complex health profiles in inpatient and outpatient settings. Mayo Clin Proc. (2013) 88:184–94. doi: 10.1016/j.mayocp.2012.10.016
14. Halmi K. Psychological comorbidities of eating disorders. In: Agras W and Robinson A, editors. The Oxford Handbook of Eating Disorders, 2nd. New York, NY: Oxford University Press (2018). p. 229–43.
15. Juli R, Juli M, Juli G, and Juli L. Eating disorders and psychiatric comorbidity. Psychiatr Danubina. (2023) 35:217–20.
16. Bulik C, Klump K, Thompson L, Kaplan A, Devlin B, Fichter M, et al. Alcohol abuse disorder comorbidity in eating disorders: A multi-center study. J Clin Psychiatry. (2004), 7: 65, 1000–1006. doi: 10.4088/jcp.v65n0718
17. Tagay S, Schlottbohm E, Reyes-Rodriguez M, Repic N, and Senf W. Eating disorders, trauma, PTSD, and psychological resources. J Treat Prev. (2014) 22:33–49. doi: 10.1080/10640266.2014.857517
18. Hudson J, Hiripi E, Pope H, and Kessler R. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. (2007) 61:348–58. doi: 10.1016/j.biopsych.2006.03.040
19. Dyer K and Corrigan J. Psychological treatments for complex PTSD: A commentary on the clinical and empirical impasse dividing unimodal and phase-oriented therapy positions. psychol Trauma: Theory Res Practice Policy. (2021) 8 pp. 869–76. doi: 10.1037/tra0001080
20. Abbate-Daga G, Buzzichelli S, Marzola E, Amianto F, and Fassino S. Clinical investigation of set-sifting sub-types in anorexia nervosa. Psychiatry Res. (2014) 219:592–7. doi: 10.1016/j.psychres.2014.06.024
21. Zander M and Young K. Individual differences in negative affect and weekly variability in binge eating frequency. Int J Eating Disord. (2014) 47:296–301. doi: 10.1002/eat.22222
22. Gibson D, Workman C, and Mehler P. Medical complications of anorexia nervosa and bulimia nervosa. Psychiatr Clinics North America. (2019) 42:263–74. doi: 10.1016/j.psc.2019.01.009
23. Hambleton A, Pepin G, Le A, Maloney D, Touyz S, and Maguire S. Psychiatric and medical comorbidities of eating disorders: findings from a rapid review of the literature. J Eating Disord. (2022) 10:132. doi: 10.1186/s40337-022-00654-2
24. Biffl W, Narayanan V, Gaudiani J, and Mehler P. The management of pneumothorax in patients with anorexia nervosa. Patient Saf Survey. (2010) 4:1–4. doi: 10.1186/1754-9493-4-1
25. Faje A, Fazeli P, Miller K, Katzman D, Ebrahimi S, Lee H, et al. Fracture risk and areal bone mineral density in adolescent females with anorexia nervosa. Int J Eating Disord. (2014) 49:249–59. doi: 10.1002/eat.22248
26. Kaplan A S and Noble S. Medical complications of eating disorders. In: Wonderlich S, Mitchell J, and de Zwaan M, editors. Annual Review of Eating Disorders: Part 1, 1st. Philadelphia, PA: CRC Press (2007) Ch.8.
27. Lamzabi I, Syed S, Reddy V, Jain R, Harbhanjanka A, and Arunkumar P. Myocardial changes in a patient with anorexia nervosa: A case report and review of literature. Am J Clin Pathol. (2015) 143:734–7. doi: 10.1309/AJCP4PLFF1TTKENT
28. Mascolo M, Dee E, Townsend R, Brinton J, and Mehler P. Severe gastric dilation due to superior mesenteric artery syndrome in anorexia nervosa. Int J Eating Disord. (2015) 48:532–4. doi: 10.1002/eat.22385
29. Westmoreland P, Krantz M, and Mehler P. Medical complications of anorexia nervosa and bulimia. Am J Med. (2016) 129:30–7. doi: 10.1016/j.amjmed.2015.06.031
30. Agras W and Robinson A. The Oxford handbook of eating disorders. 2nd. New York, NY: Oxford University Press (2018).
31. Wilson G. Cognitive-behavioral therapy for eating disorders. In: Agras W and Robinson A, editors. Oxford Handbook of Eating Disorders, 2nd. New York, NY: Oxford University Press (2018). p. 271–86.
33. Chen E, Yiu A, and Safer D. Dialectical behavior therapy and emotion-focused therapies for eating disorders. In: Agras W and Robinson A, editors. The Oxford handbook of eating disorders, 2nd. New York, NY: Oxford University Press (2018). p. 334–50.
34. Le Grange D and Rienecke R. Family therapy for eating disorders. In: Agras W and Robinson A, editors. The Oxford handbook of eating disorders, 2nd. New York, NY: Oxford University Press (2018). p. 319–33.
35. Burke N, Karam A, Tanofsky-Kraff M, and Wilfley D. Interpersonal psychotherapy for the treatment of eating disorders. In: Agras W and Robinson A, editors. The Oxford handbook of eating disorders, 2nd. New York, NY: Oxford University Press (2018). p. 287–318.
36. Levinson C, Hunt R, Keshishian A, Brown M, Vanzhula I, Christian C, et al. Using individual networks to identify treatment targets for eating disorder treatment: A proof-of-concept study and initial data. J Eating Disord. (2021) 9:147. doi: 10.1186/s40337-021-00504-7
37. D’Abundo M and Chally P. Struggling with recovery: Participants’ perspectives on battling an eating disorder. Qual Health Res. (2004) 14:1094–106. doi: 10.1177/1049732304267753
38. Simic M, Stewart C, Konstantellou A, Hodsoll J, Eisler I, and Baudinet J. From efficacy to effectiveness: Child and adolescent eating disorder treatments in the real-world (part 1): Treatment and outcomes. J Eating Disord. (2022) 10:1–16. doi: 10.1186/s40337-002-00553-6
39. Heiderscheit A. Distinguishing type of music-based interventions in clinical research and improving the quality of reporting. J Anatolian Med. (2022) 1:3–10. doi: 10.5505/anadolutd.2022.24633
41. Heiderscheit A and Jackson N. Introduction to music therapy practice. Dallas, Texas: Barcelona Publishers (2018).
42. Heiderscheit A and Jackson N. Clinical decision-making in music therapy: Case studies. Dallas, Texas: Barcelona Publishers (2023).
43. Short A and MacRitchie J. Who does what and why? Exploring the Music, Health and Wellbeing Continuum: a Role-Agent model: Exploring the Music, Health and Wellbeing Continuum. Music Med. (2023) 15, 125–35. doi: 10.47513/mmd.v15i3.930
44. Testa F, Arunachalam S, Heiderscheit A, and Himmerich H. A systematic review of scientific studies on the effects of music in people with or at risk for eating disorders. Psychiatr Danubina. (2020) 32:334–45. doi: 10.24869/psyd.2020.334
45. Coutinho E, Criekinge T, Hanford G, Nathan R, and Ruaraidh Hill M. Music therapy interventions for eating disorders: Lack of robust evidence and recommendations for future research. Br J Music Ther. (2022) 36:84–93. doi: 10.1177/1359457522111019
46. Chang E, Brooker J, Hiscock R, and O’Callaghan C. Music-based intervention impacts for people with eating disorders: A narrative synthesis systematic review. J Music Ther. (2023) 60:202–31. doi: 10.1093/jmt/thac018
47. Seppendorf S, Hoorman J, Schloeßer N, and Jaschke AC. Music therapy in eating disorder treatment and its synergy with systemic and family-based therapy approaches: A systematic review. Br J Music Ther. (2024) 38:27–41. doi: 10.1177/13594575241239286
48. Bibb J, Castle D, and Newton R. The role of music therapy in reducing post meal related anxiety for patients with anorexia nervosa. J Eating Disord. (2015) 3:1–6. doi: 10.1186/s40337-015-0088-5
49. Bibb J, Castle D, and Skewes McFerran K. Reducing anxiety through music therapy at an outpatient eating disorder recovery service. J Creativity Ment Health. (2019) 14:306–14. doi: 10.1080/15401383.2019.1595804
50. Dvorak A. Explanatory sequential descriptive analysis of music therapists’ clinical practice for individuals with eating disorders. The Arts in Psychotherapy. (2023) 85:1–18. doi: 10.1016/j.aip.2023.102067
51. Robb S, Burns D, and Carpenter J. Reporting guidelines for music-based interventions. J Health Psychol. (2011) 16:342–52. doi: 10.1177/1359105310374781
52. Robb S, Hanson-Abromeit D, May L, Hernandez Ruiz E, Allison M, Beloat A, et al. Reporting quality of music intervention research in healthcare: A systematic review. Complementary Therapies Med. (2018) 38:24–41. doi: 10.1016/j.ctim.2018.02.008
53. Tricco A, Lillie E, Zarin W, O’Brien K, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMAScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
54. Robb S, Springs S, Edwards E, Golden T, Johnson J, Burns D, et al. Reporting guidelines for music-based interventions: An update and validation study. Front Psychol. (2025) 16:1551920. doi: 10.3389/fpsyg.2025.1551920
55. Braun V and Clarke V. Toward good practice in thematic analysis: avoiding common problems and be(com)ing a knowing researcher. Int J Transgender Health. (2023) 24:1–6. doi: 10.1080/26895269.2022.2129597
56. Braun V and Clarke V. Thematic analysis: a practical guide. Thousand Oaks, California: Sage (2023).
57. Bauer S. Music therapy and eating disorders-A single case study about the sound of human needs. In: Voices: a world forum for music therapy (2010) 10. doi: 10.15845/voices.v10i2.258
58. Fendel U, Sandler H, Papachristou C, Voigt B, Rose M, and Klapp B. Bodily experiences of patients diagnosed with anorexia nervosa during treatment with the body monochord—A modified grounded theory approach. Arts Psychother. (2018) 59:7–16. doi: 10.1016/j.aip.2018.03.003
59. Heal M and O’Hara J. The music therapy of an anorectic mentally handicapped adult. Br J Med Psychol. (1993) 66:33–41. doi: 10.1111/j.2044-8341.1993.tb01724.x
60. Heiderscheit A and Madson A. Use of the iso principle as a central method in mood management: A music psychotherapy clinical case study. Music Ther Perspect. (2015) 33:45–52. doi: 10.1093/mtp/miu042
61. Heiderscheit A and Murphy K. Trauma-informed care in music therapy: Principles, guidelines, and a clinical case illustration. Music Ther Perspect. (2021) 39:142–51. doi: 10.1093/mtp/miu042
62. Heiderscheit A. Feasibility of the Bonny Method of Guided Imagery and Music in eating disorder treatment: Clients’ perceived benefits and challenges. Arts Psychother. (2023) 86:102086. doi: 10.1016/j.aip.2023.102086
63. Heiderscheit A. Thematic and intertextual analysis from a feasibility study of the Bonny Method of Guided Imagery and Music with clients in eating disorder treatment. Front Psychol. (2024) 15:1456033. doi: 10.3389/fpsyg.2024.1456033
64. Hilliard R. The use of cognitive-behavioral music therapy in the treatment of women with eating disorders. Music Ther Perspect. (2001) 19:109–13. doi: 10.1093/mtp/19.2.109
65. Lejonclou A and Trondalen G. I’ve started to move into my own body”: Music therapy with women suffering from eating disorders. Nordic J Music Ther. (2009) 18:79–92. doi: 10.1080/08098130802610924
66. McFerran K, Baker F, Patton G, and Sawyer S. A retrospective lyrical analysis of songs written by adolescents with anorexia nervosa. Eur Eating Disord Rev: Prof J Eating Disord Assoc. (2006) 14:397–403. doi: 10.1002/erv.746
67. McFerran K, Baker F, Kildea C, Patton G, and Sawyer S. Avoiding conflict: what do adolescents with disordered eating say about their mothers in music therapy? Br J Music Ther. (2008) 22:16–23. doi: 10.1177/135945750802200
68. Pavlakou M. Benefits of group singing for people with eating disorders: Preliminary findings from a non-clinical study. Approaches: Interdiscip J Music Ther. (2009) 1, 30–48. doi: 10.56883/aijmt.2023.87
69. Robarts J and Sloboda A. Perspectives on music therapy with people suffering from anorexia nervosa. J Br Music Ther. (1994) pp.7–14. doi: 10.1177/135945759400800104
70. Robarts J Z. Music therapy and adolescents with anorexia nervosa. Nordic J Music Ther. (2000) 9:3–12. doi: 10.1080/08098130009477981
71. Shah P, Mitchell E, Remers S, Van Blyderveen S, and Ahonen H. The impact of group music therapy for individuals with eating disorders. Approaches: Interdiscip J Music Ther. (2023) 15, 36–57. doi: 10.56883/aijmt.2023.87
72. Trondalen G and Skårderud F. Playing with Affects:… and the importance of “affect attunement. Nordic J Music Ther. (2007) 16:100–11. doi: 10.1080/08098130709478180
73. Trondalen G. Self-listening in music therapy with a young woman suffering from anorexia nervosa. Nordic J Music Ther. (2003) 12:3–17. doi: 10.1080/08098130309478069
74. Meneguzzo P, Baron E, Marchesin S, Andretta AM, Nalesso L, Stella S, et al. Tuning in to recovery: influence of music on emotional well-being during mealtime in inpatient facilities for eating disorders. J Eating Disord. (2024) 12:7. doi: 10.1186/s40337-024-00970-9
75. Sibbald B and Roberts C. Understanding controlled trials Crossover trials. BMJ. (1998) 316:1719. doi: 10.1136/bmj.316.7146.1719
76. Wang C and Xiao R. Music and art therapy combined with cognitive behavioral therapy to treat adolescent anorexia patients. Am J Trans Res. (2021) 13:6534.
77. Heiderscheit A. Creative arts therapies with clients with eating disorders. Philadelphia, Pennsylvania: Jessica Kingsley Publishers (2016).
78. Peters M, Godfrey C, Khalil H, McInerney P, Parker D, and Baldini Soares C. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. (2015) 13:141–6. doi: 10.1097/XEB.0000000000000050
79. Kerwin-Boudreau S and Butler-Kisber L. Deepening understanding in qualitative inquiry. Qual Rep. (2016) 21:956–71. doi: 10.46743/2160-3715/2016.2623
80. Fewell L K, Levinson C A, and Stark L. Depression, worry, and psychosocial functioning predict eating disorder treatment outcomes in a residential and partial hospitalization setting. Eating Weight Disorders-Studies Anorexia Bulimia Obes. (2017) 22:291–301. doi: 10.1007/s40519-016-0357-6
81. Murakami B. The music therapy and harm model (MTHM). Conceptualizing harm within music therapy practice. ECOS. (2021) 6:e003. doi: 10.24215/27186199e003
82. Fetahi E, Søgaard AS, and Sjögren M. Estimating the effect of motivational interventions in patients with eating disorders: A systematic review and meta-analysis. J Pers Med. (2022) 12:577. doi: 10.3390/jpm12040577
83. Himmerich H and Heiderscheit A. The challenges and opportunities related to the therapeutic use of music in psychiatry. Expert Rev Neurother. (2024) 24:615–81. doi: 10.1080/14737175.2024.2359429
84. Bryant E, Marks P, Griffiths K, Boulet S, Pehlivan M, Sarakat S, et al. Treating the individual: Moving towards personalised eating disorder care. J Eating Disord. (2025) 13, 1–15. doi: 10.1186/s40337-025-01246-6
85. Ely A and Kaye W. Appetite regulation in anorexia nervosa and bulimia nervosa. In: Agras W and Robinson A, editors. The Oxford handbook of eating disorders, 2nd. Oxford University Press, New York (2018). p. 47–79.
86. Malchiodi C. Trauma and expressive arts therapies: Brain, body, & Imagination in the healing process. 2018. New York, New York: Guilford Press (2020).
88. Raffone F, Atripaldi D, Barone E, Marone L, Carfagno M, Mancini F, et al. Exploring the role of guilt in eating disorders: A pilot study. Clinics Practice. (2025) 15:56. doi: 10.3390/clinpract15030056
89. Favaretto E, Bedani F, Brancati G, De Berardis D, Giovannini S, Scarcella L, et al. Synthesising 30 years of clinical experience and scientific insight on affective temperaments in psychiatric disorders: State of the art. J Affect Disord. (2024) 362:406–15. doi: 10.1016/j.jad.2024.07.011
90. Keel P. Epidemiology and course of eating disorders. In: Agras W and Robinson A, editors. The Oxford handbook of eating disorders, 2nd. Oxford University Press, New York (2018). p. 34–46.
91. Heiderscheit A. Discovery and recovery through music: An overview of music therapy in eating disorder treatment. In: Brooke S, editor. The creative arts therapies and eating disorders (2008). p. 122–41. Springfield, Illinois: Charles C. Thomas Publisher Ltd.
92. Henderson C and Fox J. Emotional development in eating disorders: A qualitative metasynthesis. Clin Psychol Psychother. (2019) 26:501–14. doi: 10.1002/cpp.2365
93. Karoll C. Mindfulness and eating disorders. [Internet] Psychol Today. (2023). Available online at: https://www.psychologytoday.com/gb/blog/eating-disorder-recovery/202311/mindfulness-and-eating-disorders.
94. Vaisvaser S, King J, Orkibi H, and Aleem H. Neurodynamics of relational aesthetic engagement in creative arts therapies. Rev Gen Psychol. (2024) 28:203–18. doi: 10.1177/1089268024126084
95. National Institute for Health and Care Excellence. Eating disorders: Recognition and treatment (2017). Available online at: https://www.nice.org.uk/guidance/ng69 (accessed September 4, 2025).
96. Djurisic S, Rath A, Gaber S, Garattini S, Bertele V, Ngwabyt S, et al. Barriers to the conduct of randomised clinical trials within all disease areas. Trials. (2017) 18:360. doi: 10.1186/s13063-017-2099-9
97. Gao C, Telford N, Filia K, Menssink J, Albrecht S, McGorry P, et al. Capturing the clinical complexity in young people presenting to primary mental health services: a data-driven approach. Epidemiol Psychiatr Sci. (2024) 33:e39, 1–10. doi: 10.1017/S2045796024000386
Keywords: music therapy, music-based interventions, eating disorders, scoping review, eating disorder treatment
Citation: Heiderscheit A, Gawronska J, Bloska J, Ragnhildstveit A, Milton T and Neufeld SAS (2025) Music-based interventions in the treatment of eating disorders: a scoping review. Front. Psychiatry 16:1660696. doi: 10.3389/fpsyt.2025.1660696
Received: 06 July 2025; Accepted: 26 August 2025;
Published: 24 September 2025.
Edited by:
Domenico De Berardis, ASL 4, ItalyReviewed by:
Paolo Meneguzzo, University of Padua, ItalyVassilis Martiadis, Department of Mental Health, Italy
Copyright © 2025 Heiderscheit, Gawronska, Bloska, Ragnhildstveit, Milton and Neufeld. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Annie Heiderscheit, YW5uaWUuaGVpZGVyc2NoZWl0QGFydS5hYy51aw==
†ORCID: Annie Heiderscheit, orcid.org/0000-0002-8311-7188
Julia Gawronska, orcid.org/0009-0008-1766-9719
Jodie Bloska, orcid.org/0000-0001-9647-1437
Anya Ragnhildstveit, orcid.org/0000-0002-5796-3428
Thandi Milton, orcid.org/0000-0003-2444-1217
Sharon A. S. Neufeld, orcid.org/0000-0001-5470-3770
 Annie Heiderscheit
Annie Heiderscheit Julia Gawronska2†
Julia Gawronska2† Jodie Bloska
Jodie Bloska Anya Ragnhildstveit
Anya Ragnhildstveit Thandi Milton
Thandi Milton Sharon A. S. Neufeld
Sharon A. S. Neufeld