- 1Department of Biomedical and Dental Sciences and Morphofunctional Imaging, University of Messina, Messina, Italy
- 2Department of Clinical and Experimental Medicine, University of Messina, Messina, Italy
- 3Pediatric Unit of Ospedali Riuniti Presidium, Grande Ospedale Metropolitano Bianchi Melacrino Morelli, Reggio Calabria, Italy
- 4Department of Experimental Psychology, University of Oxford, Oxford, United Kingdom
- 5Department of Human and Pediatric Pathology ‘Gaetano Barresi’, University of Messina, Messina, Italy
Introduction: Type 1 Diabetes Mellitus (T1DM) represents a serious condition with high prevalence and increasing incidence. Phenomena such as alexithymia, intolerance to uncertainty and psychopathology are recognized as generally affecting individuals' health status and contributing to the worsening of T1DM. The present study aimed to study the relationships between these variables and differences relative to age and gender of T1DM patients.
Methods: A sample of 150 participants aged between 11 and 18 years old with T1DM was recruited. All participants completed the diagnostic protocol, consisting of a sociodemographic questionnaire, Toronto Alexithymia Scale, Intolerance to Uncertainty Scale and Self Administrated Psychiatric Scales for Children and Adolescents (different psychopathological domains). Descriptive, correlational, regression and differential analyses were conducted.
Results: Alexithymia and intolerance to uncertainty predicted psychopathology and significant differences were found among age and gender groups.
Discussion: Despite this, more studies are necessary to improve knowledge in the field of psychological functioning in T1DM. Further research to deepen understanding of how alexithymia and intolerance of uncertainty influence psychological functioning in T1DM are indicated.
1 Introduction
Type 1 Diabetes Mellitus (T1DM) represents a serious chronic condition affecting one in three hundred individuals worldwide, with a growing incidence (1, 2). Recent research demonstrated the need for multifactorial approach to managing the different etiological factors affecting participants’ quality of life (3–9).
Psychological factors have been recognized to play a fundamental role in the management of chronic conditions (10–17). With particular reference to T1DM, psychological phenomena have gained attention in the last twenty years, with evidence indicating they impact the onset, maintenance and worsening of the disease (7, 18–24, 186, 187). Thus, it is clear that continuous negligence of these factors can constitute a serious risk factor, affecting the physical and psychological health of patients. Several studies have considered the role of relevant variables such as age, gender and education. Despite these sociodemographic variables remain fundamental for research (25–30), including psychological variables in the study of T1DM dynamics represents important progression. For instance, recent studies demonstrate that the need of screening for risk factors linked to T1DM is fundamental (31). In fact, particular circumstances linked to gender, age, duration of the disease and psychopathological conditions have been identified as a significant risk factors (32). It follows that the quality of life of these patients can be negatively influenced (33). In detail, a systematic review published by Lindner and colleagues (34) demonstrates how the socio-economic status and the aforementioned sociodemographic variables represent target data to be considered in the clinic with subjects suffering from T1DM. The results are particularly serious with reference to the possibilities of presenting adverse outcomes such as ketoacidosis and other forms of significant alteration. With particular reference to individual variables, age has been identified as a significant predictor of disease progression (25, 26) included among the early-life factors (35). According to Tatti and Pavandeep, gender is an undervalued variable for subjects with T1DM (36). Other studies highlighted the importance of considering this variables in order to produce a complete overview of the factors including the progress of the pathology (37, 38), illness duration and related possible complications (39). In line with these data, Morone (40) suggests the need to grasp these data and compare them with psychological variables in order to produce interventions aimed at risk reduction. Furthermore, in accordance with the review by Turin and Drobnič Radobuljac (41), etiology and management of the T1DM would be strongly influenced by the phenomena taken into consideration in this contribution, therefore of both a sociodemographic and psychological nature.
In this regard, recent research consistently demonstrates an elevated risk of psychological difficulties among individuals with T1DM, with heightened prevalence rates of anxiety, depression, eating disorders, and other psychiatric conditions (6, 42–56). Such psychopathology has been shown to adversely affect patients’ life trajectories and adherence to treatment regimens. In adolescence, a critical developmental period, Dalsgaard and colleagues (57) reported that the incidence of psychological issues reached 16%, highlighting the need for focused investigation in this age group. To inform effective interventions and reduce prevalence rates, further empirical studies are required to delineate the scope of these adversities within the T1DM population. Specifically, it is essential to identify and characterize the most prominent psychopathological presentations through rigorous research designs, thereby providing a sound evidence base for intervention development.
Although, to the best of our knowledge, much of the existing literature has concentrated on Type 2 Diabetes Mellitus (T2DM), psychopathological research on T1DM remains relatively underdeveloped. While a number of important studies have explored emerging psychological issues in individuals with T1DM, there remains a paucity of research examining the psychological mechanisms that contribute to the onset, maintenance, and exacerbation of the illness. Notably, psychopathology has been repeatedly identified as a key factor undermining self-management and adherence to medical treatments in individuals with T1DM (21, 41, 58–61). For example, Bădescu and colleagues (62) highlighted that depression could be up to three-times higher in participants suffering from T1DM and double for patients suffering from T2DM, in line with other studies evidencing its presence and common links and neurobiological dynamics (63–65). The association between anxiety and depression has been clearly detected and considered as negatively influencing disease management, glycemic control and adherence to treatments (66–68).
Eating disorders have been found to be present and lead to higher risk of complications directly related to poor glycemic control and due consequences (51, 69–76). The importance of maintaining consistent glycemic regulation and regular glucose monitoring is well established in the literature, particularly given the serious health consequences associated with poor metabolic management (77–80).
The role of obsession, defined as intrusive, unwanted thoughts, urges, or images that cause significant anxiety, has gained less attention in the field of T1DM than other psychopathological fields. While depression and anxiety have been widely studied over the past decades, obsessive-compulsive disorders (OCD) and related features remain relatively neglected. Although some studies have addressed obsessive-compulsive behaviors indirectly, only recently has research begun to engage more directly with this area (48, 81–83). Nonetheless, there remains a marked paucity of studies specifically addressing obsessive phenomena in individuals with T1DM. In contrast, emerging evidence has begun to document obsessive-compulsive features in relation to (84–86), yet equivalent investigations in T1DM populations are notably lacking. There is a clear need for greater empirical and clinical focus on the relevance of obsessive-compulsive symptoms in T1DM, particularly given their potential implications for psychological wellbeing and illness management.
The field of somatization represents a particularly relevant area of inquiry in the context of chronic illness. As observed in other medical conditions (87, 88), psychosomatic phenomena are often closely linked to underlying psychological processes. In the case of T1DM, emerging evidence suggests that psychological functioning plays a significant role in the onset, progression, and potential exacerbation of the disease (89–93). However, further investigation is needed to better understand the specific psychological mechanisms that contribute to the development of these factors. For instance, some recent studies highlighted this need with specific reference to some major concerns. According to Alazmi and colleagues’ systematic review (7), patients reported greater scores for depression, fear oh hypoglycemia and stress. Data is confirmed by other significant reviews and meta-analyses addressing stress, suicide risk, and somatization (49, 94–96).
One of the most important phenomena related to psychosomatics and psychopathology is alexithymia. Alexithymia can be defined as the difficulty to recognize, identify and describe affective phenomena such as emotions, feelings and mood (97–103). Alexithymia has been widely conceptualized and measured by a three factors model by Bagby et al. (1994), constituting difficulty identifying feelings, difficulty describing feelings and externally oriented thinking (15, 104–107).
The role of alexithymia in the context of chronic health conditions has been increasingly recognized and continues to attract scholarly attention (108–110). Within the diabetes literature, however, research has predominantly focused on T2DM (111, 112), with significantly less attention directed towards T1DM. This relative neglect has resulted in a limited understanding of the potential associations between alexithymia and psychological functioning in individuals with T1DM. Investigating the interplay between alexithymia and other psychological variables in this population thus represents a meaningful and timely area of inquiry. A study by Housiaux and colleagues (113) directly linked alexithymia to deteriorating glycemic control, while other research has demonstrated its adverse impact on disease management (114), glycemic control (115) and its potential role in predicting diabetes-related complications (116). Despite these findings, only a small number of studies have specifically explored the relationship between alexithymia and psychopathology within T1DM populations (23, 117–119), underscoring the need for further focused investigation.
A particularly robust association has been identified between alexithymia and intolerance of uncertainty (120–123). However, this relationship remains underexplored in the contexts of T1DM (23, 118) and longitudinal studies involving pathological groups and healthy controls (124). Intolerance of uncertainty is typically conceptualized as a dispositional psychological trait characterized by negative beliefs about uncertainty and its implications, often associated with heightened risk for a wide range of disruptions in several domains, such as clinical worry, emotional and behavioural responses (125–129). IU typically includes two main factors, respectively prospective and inhibitory anxiety. The psychopathological significance of this construct has garnered increasing interest across both clinical and non-clinical populations (120, 122, 130–134). In particular, Larking and colleagues (122) identified a significant link between alexithymia, intolerance of uncertainty, and somatization, while Abbate-Daga et al. (123) highlighted their combined relevance in the context of eating disorders. Similarly, Ozsivadjian and colleagues, as well as Brown and colleagues, demonstrated the importance of these constructs in internalizing and externalizing phenomena in individuals with neurodevelopmental disorders (120, 135).
Brown and colleagues (135) further substantiated these links through a systematic review and meta-analysis, showing that the interaction between alexithymia and intolerance of uncertainty may meaningfully impact health outcomes. Despite these findings, there is a notable absence of systematic reviews or meta-analyses specifically addressing this relationship within adolescent and emerging adult populations. Given the relevance of these constructs in various clinical domains, they have been incorporated into predictive models of general psychopathology (98, 136–140). These models have demonstrated significant explanatory power and continue to generate interest for future research, particularly in understanding the psychological mechanisms that influence chronic illness outcomes.
However, there remains a clear lack of research directly examining the interrelationships among alexithymia, intolerance of uncertainty, and psychopathological features in individuals with Type 1 Diabetes Mellitus (T1DM). The present study seeks to address this gap by investigating the associations, differences, and potential dependencies among these psychological constructs within a T1DM population.
1.1 Study hypotheses
Based on the emerged state of the art, we hypothesize that:
Hypothesis 1: There are significant correlations among sociodemographic variables, alexithymia, intolerance to uncertainty and psychopathological factors.
Hypothesis 2: Alexithymia and intolerance to uncertainty predict psychopathological factors.
Hypothesis 3: There are significant differences between age groups with reference to alexithymia, intolerance to uncertainty and psychopathological factors.
Hypothesis 4: There are significant differences between gender groups considering alexithymia, intolerance to uncertainty and psychopathological factors.
2 Materials and methods
2.1 Participants
Cross-sectional clinical research involving 150 participants aged between 11 and 18 years old (Mean: 14.09; SD: 2.37; 65.3% female) diagnosed with T1DM. All patients were recruited at the Pediatric Unit of the Ospedali Riuniti of Reggio Calabria (Italy; Director Dr. Domenico Minasi) routinely. The study was conducted from November 2023 to December 2024. All patients were under pharmacological treatment for T1DM and were diagnosed by an expert MD. The inclusion criteria were diagnosis of T1DM and evidence of appropriate medical treatment. The exclusion criteria were absence of comorbidity with other physical illnesses, absence of previously diagnosed psychopathological diseases, use of alcohol, drugs, or medications influencing cognitive functioning. All patients, including parents/tutors for minors, were informed about the anonymous nature of data. All patients fully completed the protocol. Each included subject and parents/tutors received and signed the written informed consent. Only 0.66% of subjects invited to participate in the study or their parents/tutors refused. No selection of subjects or subsampling based on further criteria was performed. The sample consists of data referring to all patients who were effectively involved in the study. This recruitment represents original psychological assessment performed in the clinical reality of reference.
2.2 Instruments
The present study was conducted using a protocol comprising a clinical interview, sociodemographic questionnaire and a set of validated psychometric instruments. Sociodemographic variables collected included participants’ age, gender, age at diagnosis, duration of illness, and educational attainment (measured in years of formal education).
2.2.1 Self-administrated psychiatric scales for children and adolescents
Self-Administrated Psychiatric Scales for Children and Adolescents (SAFA) (141, 142) is a self-report clinical instrument validated in 2001 and developed by Cianchetti and Sannio Fratello (141). The instrument allows clinicians to build a complete report through principal scales and related subscales. The scales items are based on a 3-point Likert-type scale ranging from “not at all” to “entirely”. Each scale is composed of sub-scales related to psychopathological dynamics strictly linked to the main domain. Subscales of anxiety are for generalized, social, separation and school anxiety. Depression scale includes depressed mood, anhedonia, irritable mood, low self-esteem, insecurity, guilt and desperation. Obsessive-compulsive symptoms scale includes obsessive thoughts, compulsions/rituals, contamination, control and indecision. Psychogenic eating disorders scale includes bulimic behavior, anorexic behavior, body image and psychological aspects related to eating disorders. Somatic and hypochondria symptoms scale includes somatic and hypochondria symptoms.
The original validation provided for the following Cronbach’s alphas: Anxiety=0.887 for the nonclinical sample and 0.956 for the clinical sample (test–retest Pearson r:.913); Depression=0.909 for the nonclinical sample and 0.943 for the clinical sample (test–retest Pearson r:.881, highly significant); Obsession=0.916 for the nonclinical sample and 0.895 for the clinical sample (test–retest Pearson r: 0.820); Psychogenic eating disorders=0.814 for the nonclinical sample (test–retest Pearson r: 0.740, highly significant); Somatic symptoms and hypochondria = 0.876 for the nonclinical sample and 0.797 for the clinical sample (test-retest Pearson r: 0.567, highly significant).
2.2.2 Toronto Alexithymia Scale (TAS-20)
TAS-20 (143) is a 20 items self-report scale based on a 5-point Likert-type scale ranging from “strongly disagree” to “strongly agree”. The scale is composed of three main factors - difficulty identifying feelings, difficulty describing feelings and externally oriented thinking. The instrument allows clinicians to assess alexithymia and related phenomena (see factors) through a valid and reliable widely recognized instrument. Thus, the use of TAS-20 in adolescent populations has been proved as effective (144–146). The validation of the original version of the scale produced the following Cronbach’s alpha indexes: 0.81 for the full scale; 0.78 for difficulty identifying feelings (DIF); 0.75 for difficulty describing feelings (DDF); 0.66 for externally oriented thinking (EOT). The Italian adaptation (147) of the scale provided for: 0.82 for the full scale, 0.79 for the first factor, 0.68 for the third factor and 0.54 for the last factor.
2.2.3 Intolerance to Uncertainty Scale (IUS-12)
IUS-12 (148) is a self-report instrument assessing intolerance to uncertainty through 12 items based on a 5-point Likert scale ranging from “not at all characteristic of me” to “entirely characteristic of me”. The scale is composed of two main factors, respectively prospective and inhibitory anxiety. Its value has been demonstrated in different contests and samples, including adolescents (149–151). The original validation study demonstrated a good reliability (Cronbach’s alphas): 0.91 for the whole scale, 0.85 for both factors. The Italian validation (152) of the scale demonstrated good reliability for both full scale (0.80) and related factors (0.68 for prospective anxiety and 0.79 for inhibitory anxiety).
2.3 Ethics
The present study and all the related procedures were consistent with the Declaration of Helsinki (1964) and its amendments. The study was approved by the Ethical Committee “Comitato Etico Regionale Sezione Area Sud, Grande Ospedale Metropolitano Bianchi-Melacrino-Morelli” (Reggio Calabria), approval number: 19-2022 (27th April 2022).
2.4 Statistical analysis
For the statistical analyses categorial variables were expressed as number and percentage and numerical data through means and standard deviation. The Kolmogorov-Smirnov test was used to assess the normality of the distribution. After detecting the non-normality of some of the distributions, a non-parametric approach was chosen. Correlation analyses were performed using the Spearman Rho test. Generalized linear regressions were conducted to examine the relationship between clinical variables from a set of predictors (alexithymia and intolerance to uncertainty). Avoiding confounding effects, total score predictors analyses were performed separately from related factors. Statistical differences were studied using the Mann-Whitney test. A significance level of.05 was used for all analyses. A correction for multiple comparisons has not been applied as analyses were exploratory at this stage. Statistical analyses were performed using SPSS.25 for Windows package.
3 Results
The sequence of tables covers descriptive statistics, correlations, regressions and differential analyses.
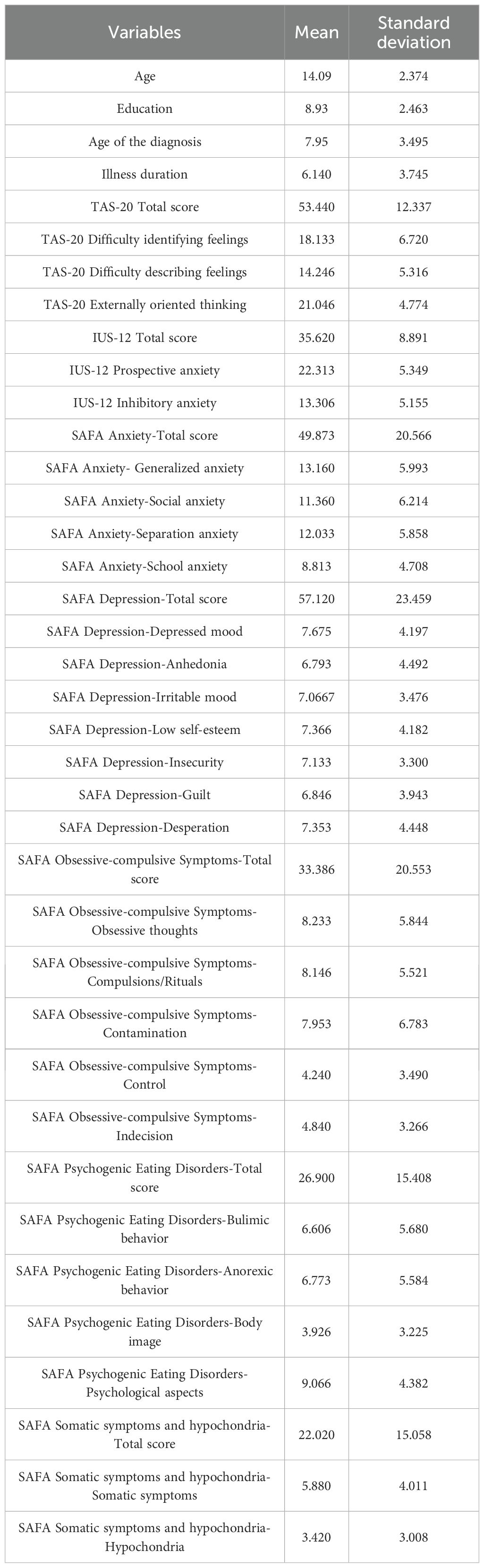
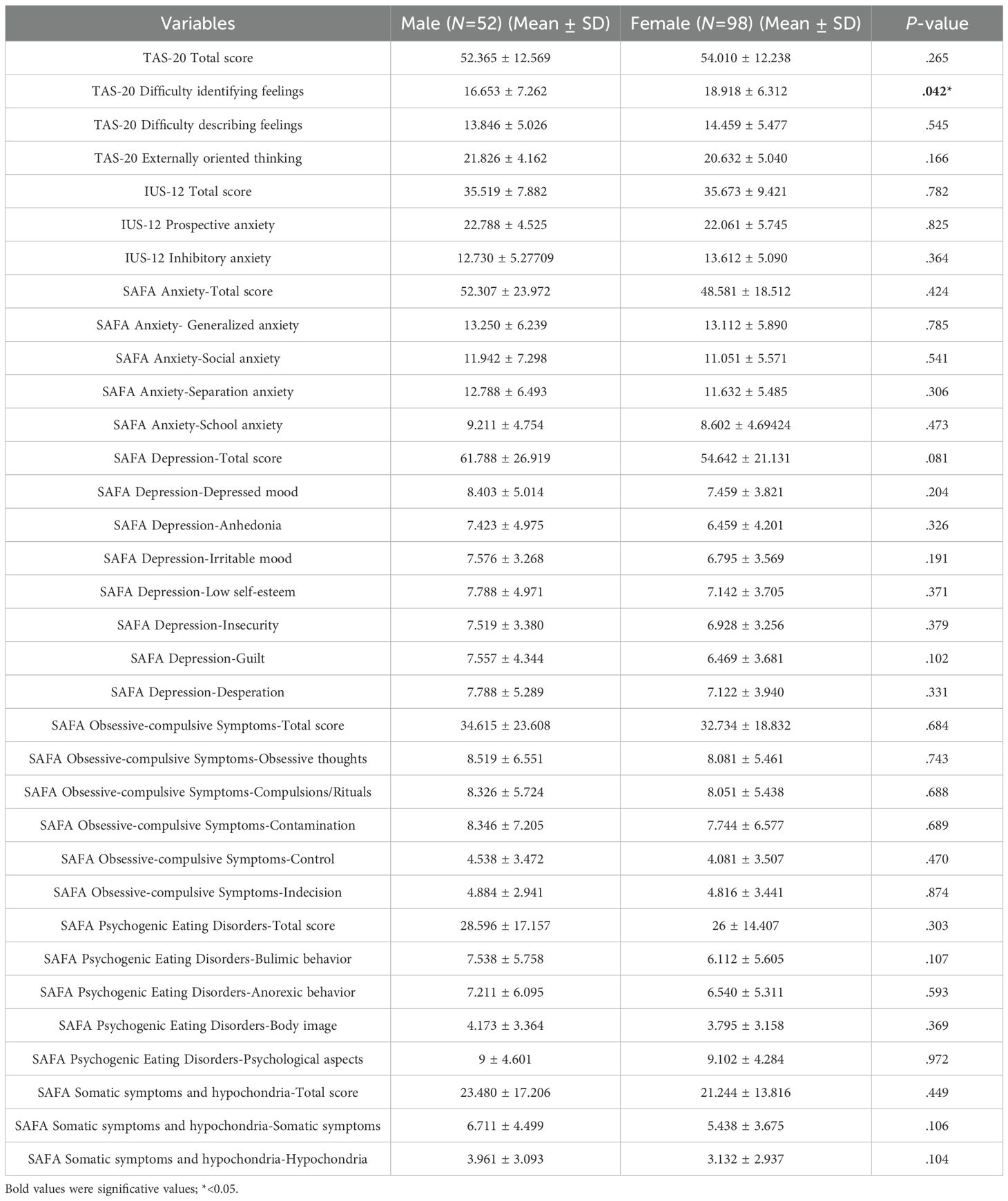
Table 1 includes the descriptive statistics expressed through mean and standard deviation for all study variables.
Hypothesis 1
Table 2 presents correlational analyses that included sociodemographic data and TAS-20 and IUS-12 scores. The first significant and negative correlation was age and externally oriented thinking. Thus, a significant and positive correlation was found with prospective anxiety. Considering education, the first significant and negative relationship regarded alexithymia (total score). A second significant and positive correlation involved externally oriented thinking. Age of the diagnosis produced two significant and positive relationships, involving alexithymia and difficulty describing feelings. Significant and negative correlations emerged among illness duration, alexithymia total score, difficulty identifying feelings and difficulty describing feelings. In line with this data, increasing age corresponded to decreased externally oriented thinking, representing a result consistent with maturation processes and the role of externally oriented thinking in subjects’ development. This tendency corresponded also to increasing education and related development of rational thinking. Alexithymia variables such as difficulty describing and difficulty identifying also assumed negative directions referring to illness duration and a positive direction with age of the diagnosis. The increasing age of diagnosis was linked to higher levels in difficulty describing feelings, while the relationship with illness duration was positive. The positive relationship between age of the diagnosis and alexithymia would represent a clear implication for possible interventions, while illness duration appeared to suggest the role of developmental processes influencing affective functioning of subjects.
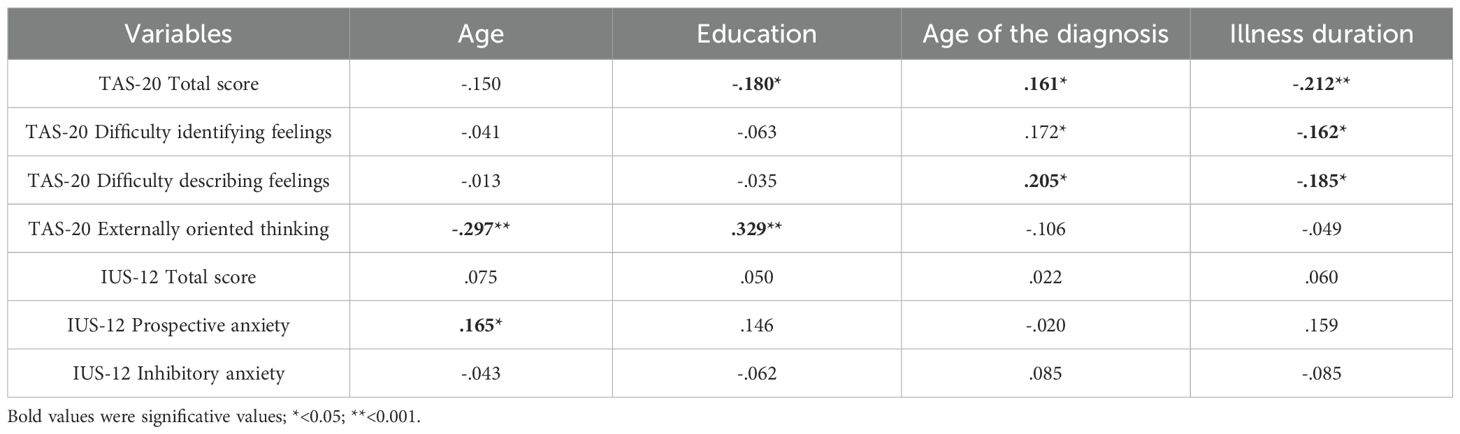
Table 2. Correlation analyses among sociodemographic variables, alexithymia and intolerance to uncertainty.
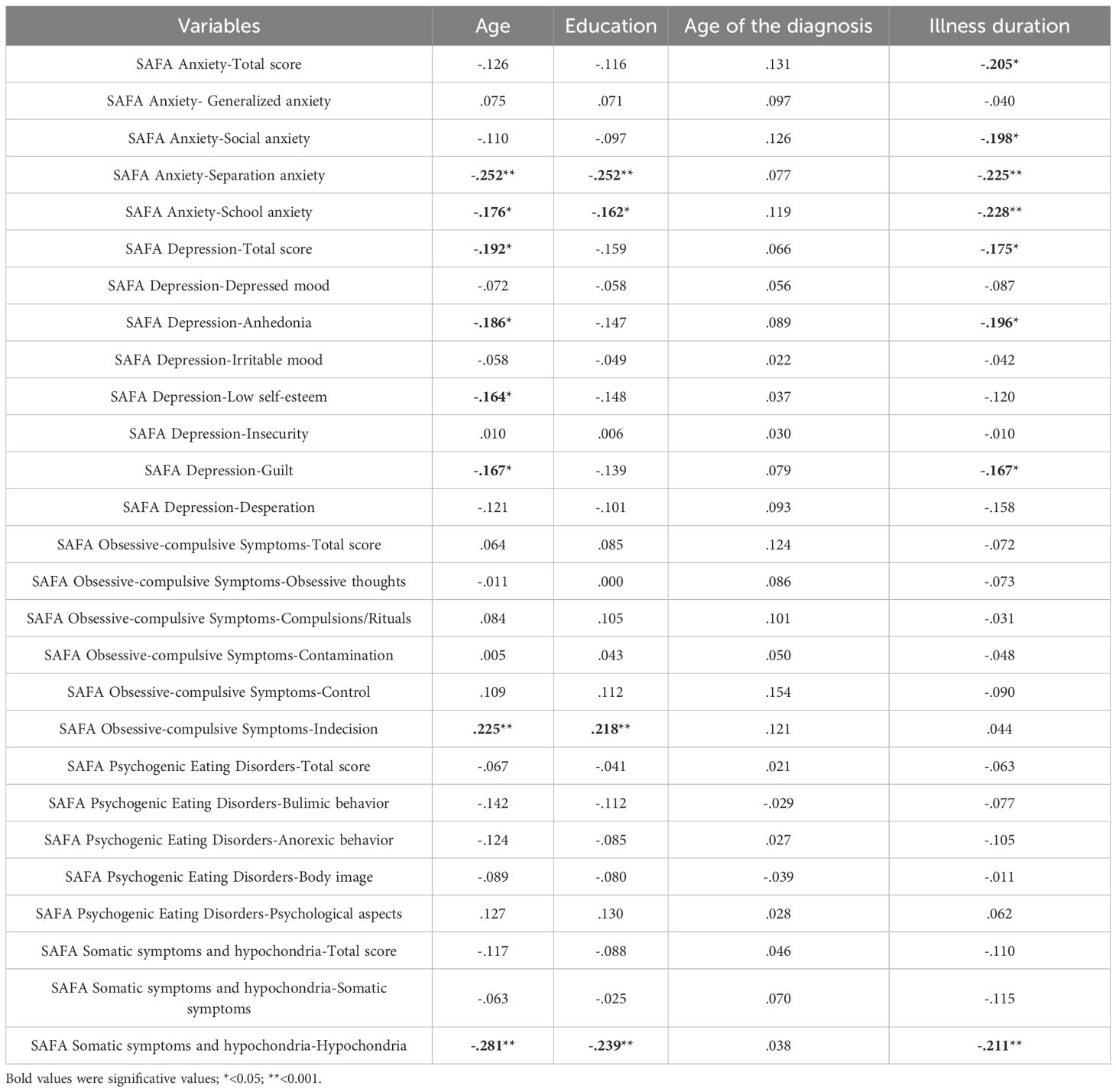
Table 3 presents the correlational analyses performed between sociodemographic data and all clinical variables (SAFA scales). The first sociodemographic variable was age, presenting several significant correlations. Significant and negative correlations emerged with separation anxiety, school anxiety, depression (total scale score), anhedonia, low self-esteem guilt and hypochondria. A positive correlation emerged with reference to age and indecision (obsessive-compulsive scale). Considering education, significant and negative correlations emerged with separation anxiety, school anxiety and hypochondria, while a positive correlation regarded indecision. Illness duration presented several significant and negative correlations. The emerged significant results referred to anxiety (total score), social anxiety, separation anxiety, school anxiety, depression (total score), anhedonia, guilt and hypochondria. No significant relations emerged between age of the diagnosis and clinical variables. With reference to clinical implications related to emerging significant data, age assumed several negative directions towards psychopathological factors. Supporting these results, education represents a key variable for subject’s health status. The significant and negative correlations that emerged between psychopathological variables and illness duration suggest that maturation processes play a crucial role for the subjects.
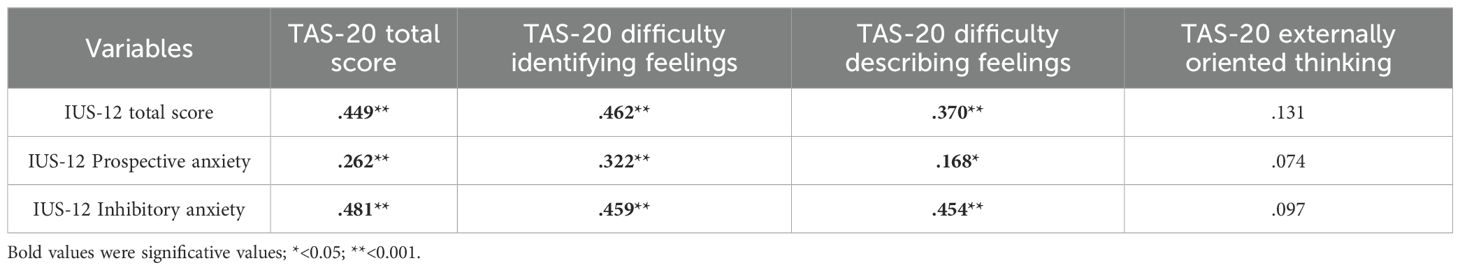
Table 4 shows the correlation analyses between TAS-20 and IUS-12 variables. All emerged significant results were positive, including alexithymia total score, difficulty identifying feelings, difficulty describing feelings and all IUS-12 variables (total score, prospective and inhibitory anxiety. No significant correlations emerged with externally oriented thinking. The high number of significant and positive correlations emerged between alexithymia and intolerance to uncertainty represent an added value. The link regarding alexithymia and intolerance to uncertainty emerged as relevant and positive.
Hypothesis 2
Table 5 reflects the generalized regression analyses between a set of predictors such as alexithymia and intolerance to uncertainty total scores and clinical variables (SAFA scales). The first significant and positive dependence emerged between intolerance to uncertainty and generalized anxiety. The second regarded intolerance to uncertainty and indecision, demonstrating the opposite direction of the phenomena. In line with this last relation, a significant and negative dependency emerged between intolerance to uncertainty and bulimic behavior, as well as for hypochondria. No significant relations emerged due to alexithymia predictor. The emerged significant dependencies highlight the predictive role of intolerance of uncertainty for anxiety, obsessive phenomena, eating and somatization symptoms.
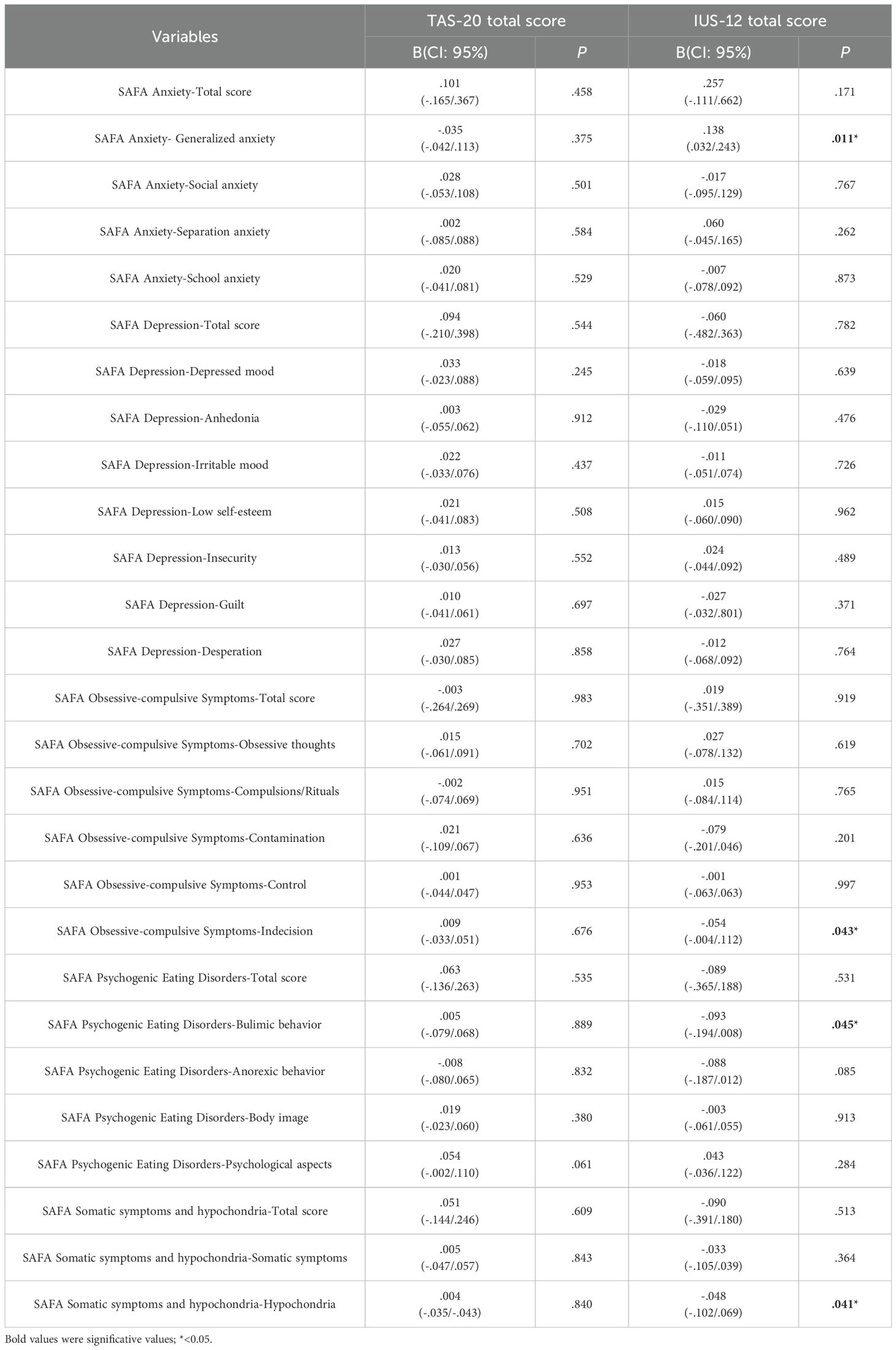
Table 5. Generalized regression analysis among alexithymia and intolerance to uncertainty (predictors) and psychopathology.
Table 6 reports the generalized regression analyses between alexithymia and intolerance to uncertainty factors (predictors) and clinical variables. Externally oriented thinking predicted higher levels of depression, anhedonia, irritable mood, low self-esteem, obsessive thoughts and body image issues. Prospective anxiety predicted higher levels of generalized anxiety and psychological aspects related to eating disorders. No significant dependencies emerged with reference to the predictors difficulty identifying, describing feelings and inhibitory anxiety. The predictive role of alexithymia on psychopathological phenomena appears crucial. Confirming the previous analyses, prospective anxiety predicted some relevant pathological domains.
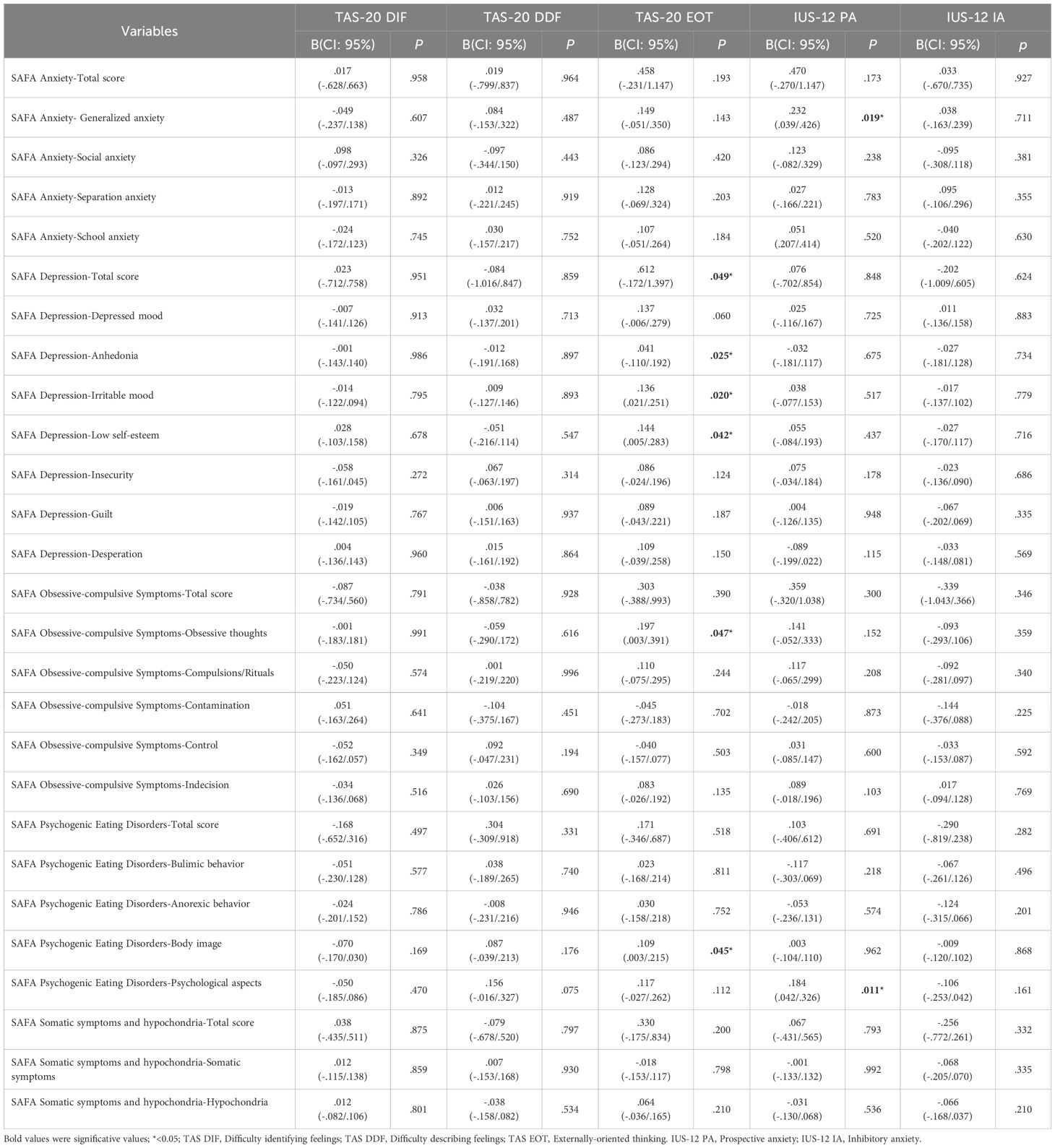
Table 6. Generalized regression analysis among alexithymia and intolerance to uncertainty (predictors) and psychopathology.
Hypothesis 3
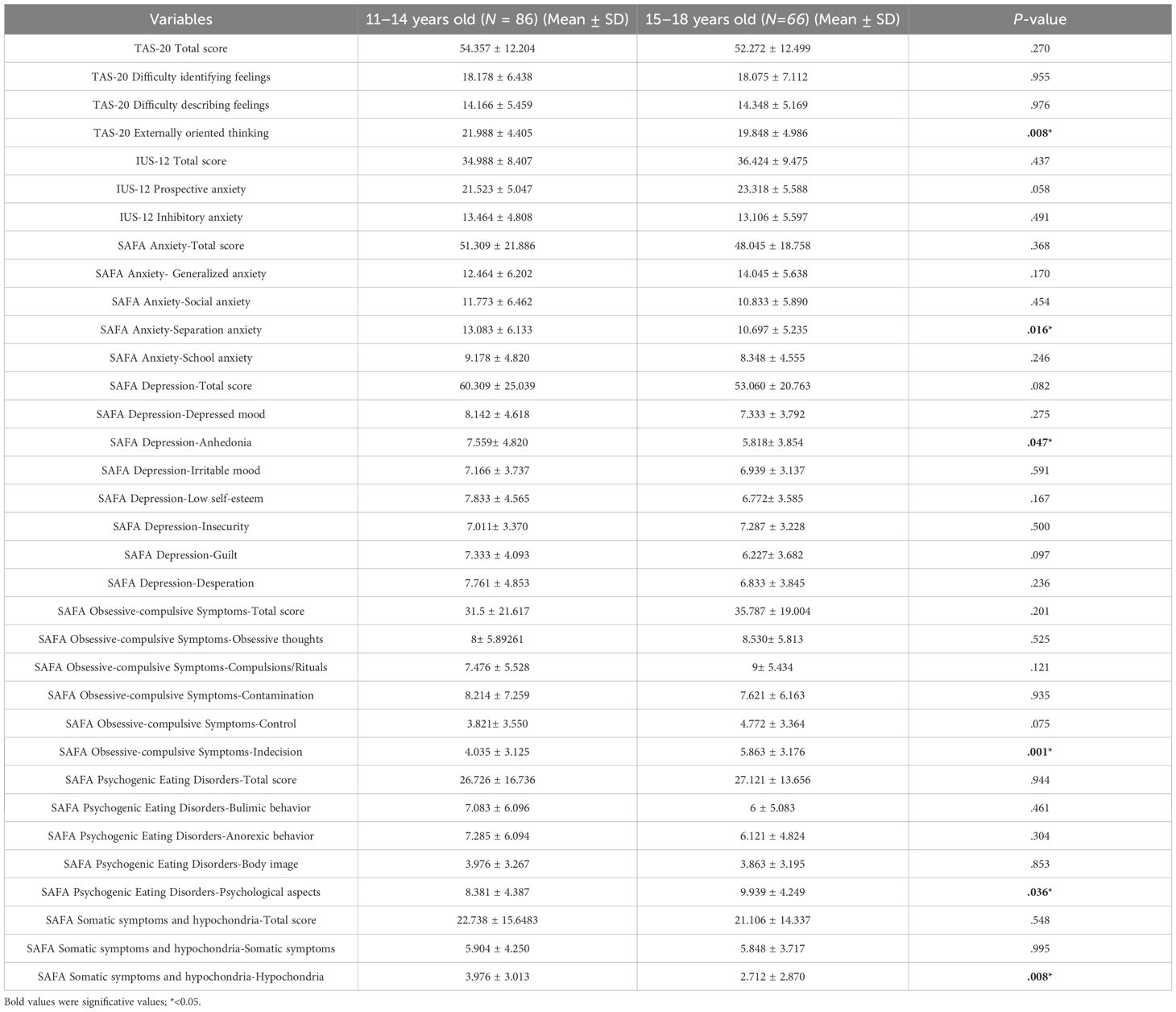
Table 7 includes the differential analyses performed with reference to two age groups (11–14 and 15-18). The first significant difference was found considering externally oriented thinking with higher scores in younger participants. The second significant difference regarded separation anxiety, in line with the previous one. Higher scores of anhedonia were found in younger participants. Indecision appeared significantly higher in older participants, as well as psychological aspects related to eating disorders. Hypochondria appeared significantly higher in younger participants. Results lead to clinical implications. Externally oriented thinking refers more to younger participants, as well as separation anxiety. In these terms, increasing age corresponds to diminishing rate of the considered phenomena. Hypochondria and anhedonia represent significant phenomena related to somatization and depressive symptomatology.
Hypothesis 4
Table 8 reports differential analyses between male and female groups. The only significant difference emerged in relation to difficulty identifying feelings, with higher scores in female participants. No other significant differences were found between male and female groups.
4 Discussion
The present study investigated the relationships among sociodemographic variables, alexithymia, intolerance of uncertainty, and psychopathological factors in a sample of young individuals with T1DM. Guided by four hypotheses, the study first examined whether significant correlations existed among these variables (Hypothesis 1). It then explored the predictive value of alexithymia and intolerance of uncertainty on psychopathological features (Hypothesis 2). To further assess group-level differences, the study conducted comparative analyses to evaluate whether age groups differed significantly in levels of alexithymia, intolerance of uncertainty, and psychopathological symptoms (Hypothesis 3), and whether similar differences emerged across gender groups (Hypothesis 4). Through this multi-level analytic approach, the study aimed to clarify the interplay of psychological and demographic factors in the mental health profiles of individuals with T1DM.
The first hypothesis addressed potential correlations among sociodemographic variables, alexithymia, intolerance of uncertainty and psychopathological factors. In relation to alexithymia, both educational attainment and illness duration were negatively associated with total alexithymia scores, suggesting that higher levels of education and longer illness duration may be linked to lower levels of alexithymic traits. These findings are consistent with prior literature (153–156). Specifically, illness duration was inversely related to total alexithymia scores, as well as to the subscales assessing difficulty identifying feelings and difficulty describing feelings. While several studies have explored the association between alexithymia and physical illness, there remains a lack of clear evidence specifically examining its relationship with illness duration.
Externally oriented thinking demonstrated a positive correlation with education and a negative correlation with age, a pattern aligned with previous research on developmental changes in emotional processing (157, 158), while age was positively associated with prospective anxiety on the Intolerance of Uncertainty Scale (IUS-12), suggesting a possible decline in psychological flexibility and overall mental health with age, as supported by studies such as Okayama and colleagues (159) and others (149, 160).
Conversely, increasing age was linked to lower levels of separation anxiety, school-related anxiety, depression, anhedonia, low self-esteem, guilt and hypochondriasis. These findings are consistent with evidence indicating a general reduction in anxiety and depressive symptoms across adolescence, likely due to neurobiological maturation (161–163). However, as previously noted, the presence of a chronic condition such as T1DM constitutes a significant risk factor for psychopathological expression (164). Therefore, timely psychological intervention should be considered a crucial component of care following the identification of psychological distress.
Higher levels of education were associated with lower levels of separation anxiety, school-related anxiety, and hypochondriasis. Additionally, indecisiveness showed a significant positive association with both age and education. While the protective role of education in mitigating risk for psychopathology is well established in the general population (165–168), limited empirical evidence exists regarding its specific impact in individuals with T1DM. These findings suggest that educational attainment may serve as a potential buffer against certain psychological issues in this clinical group, although considering the exploratory nature of the study, further research is needed to clarify the mechanisms underlying this relationship.
A particularly noteworthy finding was the set of significant negative correlations between illness duration and a range of psychopathological variables. Specifically, longer illness duration was significantly associated with lower levels of general anxiety, social anxiety, separation anxiety, school-related anxiety, depression, anhedonia, guilt, and hypochondriasis. These results may reflect a possible psychological adjustment process to living with a chronic illness over time, a phenomenon supported by previous research (169–171). However, it is important to note that such adaptive processes do not negate the need for appropriate psychological support. Even when indicators of distress decrease with time, structured psychological interventions remain essential to promote long-term well-being and adaptive functioning in individuals with T1DM.
The association between alexithymia and intolerance of uncertainty was clearly supported by the present findings, with all significant correlations being positive. These results are consistent with recent theoretical developments and empirical trends, further reinforcing the relevance of these constructs in health psychology. The interplay between alexithymia and intolerance of uncertainty is particularly noteworthy given their established influence on health-related outcomes. However, as previously noted, these constructs have rarely been examined in tandem within the context of T1DM. While existing literature has explored alexithymia and intolerance of uncertainty, primarily in isolation, in relation to T2DM, only a limited number of studies have included T1DM populations (113–115, 119, 124, 172, 173). This gap is especially evident with respect to intolerance of uncertainty, which remains under-investigated in T1DM and other chronic health conditions.
The second hypothesis focused on the predictive role of alexithymia and intolerance of uncertainty in relation to psychopathological factors. The link between anxiety and intolerance of uncertainty is well established (174, 175), and a recent review by Sternheim and colleagues (176) further underscored intolerance of uncertainty as a risk factor for the development of eating disorders. Although comprehensive reviews by Kesby and colleagues (177) and Brown and colleagues (135) have examined this relationship in broader contexts, studies explicitly addressing these associations in T1DM are still lacking. Of particular relevance, Brown and colleagues (135) reported a connection between intolerance of uncertainty and bulimia, highlighting associations with harm avoidance and depressive symptoms. These findings point to the potential clinical utility of targeting intolerance of uncertainty in psychological interventions, including for populations with chronic conditions such as T1DM.
Emotional regulation, alexithymia’s feeling identification and description have been found associated with orthorexic tendencies (178), diabetes management and glycemic control issues and presence of eating disorders in participants suffering from T1DM (23, 114, 118, 179). Accordingly, the present findings align with existing literature, reinforcing the relevance of alexithymic traits in the psychological and clinical profiles of individuals with T1DM. Furthermore, consistent with the hypothesized predictive role of intolerance of uncertainty, prospective anxiety was found to possibly predict elevated levels of generalized anxiety and hypochondriasis. These results support and extend previous findings, further emphasizing the importance of targeting intolerance of uncertainty and alexithymic traits in interventions aimed at improving mental health and self-management outcomes in this population.
The third hypothesis explored potential age-related differences in alexithymia and associated psychopathological variables. A significant difference was found in externally oriented thinking, with younger participants exhibiting higher levels of this cognitive style. Additionally, younger individuals reported greater levels of separation anxiety, anhedonia, and hypochondriasis. In contrast, older participants demonstrated higher levels of indecision and psychological difficulties related to eating disorders.
Although previous research has reported comparable levels of alexithymia across paediatric and adult populations with T1DM (155), and few studies have specifically examined age-related variations in emotional recognition (180, 181), the present findings underscore the developmental sensitivity of externally oriented thinking. This result is consistent with a recent meta-analysis highlighting the developmental dependence of externally oriented thinking, particularly during adolescence and early adulthood (182). Regarding hypochondriasis, earlier studies have typically reported no significant age-related differences (183), with only limited evidence pointing to developmental trends in somatization and health anxiety (184). However, it is important to note that most of this literature is based on general or psychiatric populations rather than individuals with chronic medical conditions such as T1DM. The present study contributes novel insights by identifying age-specific psychological patterns within this clinical group, underscoring the importance of developmental considerations in both research and intervention design.
The final hypothesis examined gender differences in alexithymia, intolerance of uncertainty, and psychopathological variables. The only statistically significant difference emerged in the domain of alexithymia, specifically in difficulty identifying feelings, with female participants reporting higher levels. This finding is consistent with a recent meta-analysis by Mendia and colleagues (182), which highlighted gender-related differences in alexithymia—particularly during adolescence—with females more likely to report greater difficulty identifying emotions. These gender differences appeared to diminish in young adulthood, underscoring the developmental variability of emotional processing. Thus, this interesting result should be considered in the light of the influence provided by socialization effects and response biases. Even in this case, more studies are needed. Furthermore, consistent with the age-related analyses, younger participants also reported higher scores on the difficulty identifying feelings subscale, suggesting a broader trend linked to developmental stage.
Overall, the four hypotheses facilitated the identification of key psychological characteristics and group-level differences within individuals living with T1DM, contributing to a deeper understanding of an underexplored area. Despite the emergence of several significant and clinically relevant findings, the cross-sectional design of the present study limits the ability to draw causal inferences. Single hospital unit, absence of a control group and recruitment performed through routine visits represent another limit for the study. Nevertheless, these limitations highlight the need for longitudinal and experimental research to further investigate the developmental trajectories and psychological mechanisms implicated in T1DM. Building on the current results, future studies should aim to develop targeted interventions to mitigate psychopathological symptoms and related emotional difficulties in this population (185). Moreover, it is of fundamental importance that these interventions are realistic and sustainable for regular implementation by clinicians.
5 Conclusions
The findings of this study underscore the importance of alexithymia, intolerance of uncertainty and psychopathological factors in the context of chronic illness, with a specific focus on T1DM. By examining these variables in a sample of young individuals, the study sought to illuminate their interrelationships and identify developmental and gender-based differences. Consistent patterns emerged indicating the relevance of alexithymia and intolerance of uncertainty in the psychological profile of T1DM patients, with significant associations also observed with psychopathological symptoms. Thus, intolerance to uncertainty predicted anxiety and obsessive phenomena, while alexithymia showed fewer predictive associations. The significant associations observed offer valuable insights for the development of targeted, evidence-based psychological interventions. Given the potential health risks associated with unaddressed psychological distress in T1DM, the continued neglect of these factors in clinical practice and research cannot be justified. Closing this gap is critical to advancing both the scientific understanding and holistic care of individuals with T1DM.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethical Committee “Comitato Etico Regionale Sezione Area Sud, Grande Ospedale Metropolitano Bianchi-Melacrino-Morelli” (Reggio Calabria), approval number: 19-2022 (27th April 2022). The studies were conducted in accordance with the local legislation and institutional requirements. The study and all the related procedures were consistent with the Declaration of Helsinki (1964) and its amendments. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
EM: Conceptualization, Project administration, Writing – review & editing, Investigation, Formal analysis, Writing – original draft, Supervision, Data curation, Methodology. GM: Supervision, Project administration, Conceptualization, Writing – review & editing, Methodology, Data curation, Investigation, Writing – original draft, Formal analysis. RT: Conceptualization, Investigation, Writing – review & editing, Writing – original draft, Data curation. LM: Formal Analysis, Data curation, Writing – review & editing, Writing – original draft, Investigation. SH: Writing – original draft, Writing – review & editing. AA: Formal analysis, Writing – review & editing, Data curation, Writing – original draft. ML: Writing – review & editing, Writing – original draft. DM: Writing – review & editing, Writing – original draft, Conceptualization, Supervision.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Quattrin T, Mastrandrea LD, and Walker LSK. Type 1 diabetes. Lancet. (2023) 401:2149–62. doi: 10.1016/S0140-6736(23)00223-4
2. Patterson CC, Karuranga S, Salpea P, Saeedi P, Dahlquist G, Soltesz G, et al. Worldwide estimates of incidence, prevalence and mortality of type 1 diabetes in children and adolescents: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. (2019) 157:107842. doi: 10.1016/j.diabres.2019.107842
3. Giwa AM, Ahmed R, Omidian Z, Majety N, Karakus KE, Omer SM, et al. Current understandings of the pathogenesis of type 1 diabetes: Genetics to environment. World J Diabetes. (2020) 11:13–25. doi: 10.4239/wjd.v11.i1.13
4. Powers AC. Type 1 diabetes mellitus: much progress, many opportunities. J Clin Invest. (2021) 131:1–10. doi: 10.1172/JCI142242
5. Guerra JVS, Dias MMG, Brilhante A, Terra MF, Garcia-Arevalo M, and Figueira ACM. Multifactorial basis and therapeutic strategies in metabolism-related diseases. Nutrients. (2021) 13:2830. doi: 10.3390/nu13082830
6. van Duinkerken E, Snoek FJ, and de Wit M. The cognitive and psychological effects of living with type 1 diabetes: a narrative review. Diabetes Med. (2020) 37:555–63. doi: 10.1111/dme.14216
7. Alazmi A, Bashiru MB, Viktor S, and Erjavec M. Psychological variables and lifestyle in children with type1 diabetes and their parents: A systematic review. Clin Child Psychol Psychiatry. (2024) 29:1174–94. doi: 10.1177/13591045231177115
8. Bauer W, Gyenesei A, and Kretowski A. The multifactorial progression from the islet autoimmunity to type 1 diabetes in children. Int J Mol Sci. (2021) 22:7493. doi: 10.3390/ijms22147493
9. Giorgianni CM, Martino G, Brunetto S, Buta F, Lund-Jacobsen T, Tonacci A, et al. Allergic sensitization and psychosomatic involvement in outdoor and indoor workers: A preliminary and explorative survey of motorway toll collectors and office employees. Healthcare (Basel Switzerland). (2024) 12:1429. doi: 10.3390/healthcare12141429
10. Caputo A, Vicario CM, Cazzato V, and Martino G. Psychological factors as determinants of medical conditions. Front Psychol. (2022) 10. doi: 10.3389/fpsyg.2022.865235
11. Ricciardi L, Spatari G, Vicario CM, Liotta M, Cazzato V, Gangemi S, et al. Clinical Psychology and Clinical Immunology: is there a link between Alexithymia and severe Asthma? Mediterr J Clin Psychol. (2023) 11:1–18. doi: 10.13129/2282-1619/mjcp-3704
12. Martino G, Caputo A, Vicario CM, Feldt-Rasmussen U, Watt T, Vita R, et al. Interrelations between mental health, generic and thyroid-related quality of life in patients with Hashimoto’s thyroiditis receiving levothyroxine replacement. Mediterr J Clin Psychol. (2021) 9:1–22. doi: 10.13129/2282-1619/mjcp-3072
13. Jiakponna EC, Agbomola JO, Ipede O, Karakitie L, Ogunsia A, Adebayo KT, et al. Psychosocial factors in chronic disease management: Implications for health psychology. Int J Sci Res Archive. (2024) 12:117–28. doi: 10.30574/ijsra.2024.12.2.1219
14. Conversano C and Di Giuseppe M. Psychological factors as determinants of chronic conditions: clinical and psychodynamic advances. Front Psychol. (2021) 12:635708. doi: 10.3389/fpsyg.2021.635708
15. Di Giuseppe M and Conversano C. Psychological components of chronic diseases: the link between defense mechanisms and alexithymia. Mediterr J Clin Psychol. (2022) 10:1–11. doi: 10.13129/2282-1619/mjcp-3602
16. McCracken LM, Yu L, and Vowles KE. New generation psychological treatments in chronic pain. BMJ. (2022) 376:e057212. doi: 10.1136/bmj-2021-057212
17. Silvestro O, Vicario CM, Costa L, Sparacino G, Lund-Jacobsen T, Spatola CAM, et al. Defense mechanisms and inflammatory bowel diseases: a narrative review. Res Psychother. (2025) 28:60–8. doi: 10.4081/ripppo.2025.854
18. Bhat NA, Muliyala KP, and Kumar S. Psychological aspects of diabetes. Diabetes. (2020) 8:90–8. doi: 10.33590/emjdiabet/20-00174
19. Ingrosso DMF, Primavera M, Samvelyan S, Tagi VM, and Chiarelli F. Stress and diabetes mellitus: pathogenetic mechanisms and clinical outcome. Horm Res Paediatr. (2023) 96:34–43. doi: 10.1159/000522431
20. Schmidt CB, van Loon BJP, Vergouwen ACM, Snoek FJ, and Honig A. Systematic review and meta-analysis of psychological interventions in people with diabetes and elevated diabetes-distress. Diabetes Med. (2018) 35:1157–72. doi: 10.1111/dme.13709
21. Kalra S, Jena BN, and Yeravdekar R. Emotional and psychological needs of people with diabetes. Indian J Endocrinol Metab. (2018) 22:696–704. doi: 10.4103/ijem.IJEM_579_17
22. Marchini F, Langher V, Napoli A, Balonan JT, Fedele F, Martino G, et al. Unconscious loss processing in diabetes: associations with medication adherence and quality of care. Psychoanalytic Psychotherapy. (2021) 35:5–23. doi: 10.1080/02668734.2021.1922492
23. Merlo EM, Tutino R, Myles LAM, Alibrandi A, Lia MC, and Minasi D. Type 1 diabetes mellitus, psychopathology, uncertainty and alexithymia: A clinical and differential exploratory study. Healthcare (Basel). (2024) 12:257. doi: 10.3390/healthcare12020257
24. Ademoyegun AB, Afolabi OE, Aghedo IA, Adelowokan OI, Mbada CE, and Awotidebe TO. The mediating role of sedentary behaviour in the relationship between social support and depression among individuals with diabetes. Mediterr J Clin Psychol. (2022) 10:1–26. doi: 10.13129/2282-1619/mjcp-3420
25. Leete P, Mallone R, Richardson SJ, Sosenko JM, Redondo MJ, and Evans-Molina C. The effect of age on the progression and severity of type 1 diabetes: potential effects on disease mechanisms. Curr Diabetes Rep. (2018) 18:115. doi: 10.1007/s11892-018-1083-4
26. So M, O’Rourke C, Ylescupidez A, Bahnson HT, Steck AK, Wentworth JM, et al. Characterising the age-dependent effects of risk factors on type 1 diabetes progression. Diabetologia. (2022) 65:684–94. doi: 10.1007/s00125-021-05647-5
27. Szadkowska A, Madej A, Ziolkowska K, Szymanska M, Jeziorny K, Mianowska B, et al. Gender and Age - Dependent effect of type 1 diabetes on obesity and altered body composition in young adults. Ann Agric Environ Med. (2015) 22:124–8. doi: 10.5604/12321966.1141381
28. Alonso Martín DE, Roldán Martín MB, Álvarez Gómez MÁ, Yelmo Valverde R, Martín-Frías M, Alonso Blanco M, et al. Impact of diabetes education on type 1 diabetes mellitus control in children. Endocrinología y Nutrición (English Edition). (2016) 63:536–42. doi: 10.1016/j.endoen.2016.08.012
29. Milton B, Holland P, and Whitehead M. The social and economic consequences of childhood-onset Type 1 diabetes mellitus across the lifecourse: a systematic review. Diabetes Med. (2006) 23:821–9. doi: 10.1111/j.1464-5491.2006.01796.x
30. Nieuwesteeg A, Pouwer F, van der Kamp R, van Bakel H, Aanstoot HJ, and Hartman E. Quality of life of children with type 1 diabetes: a systematic review. Curr Diabetes Rev. (2012) 8:434–43. doi: 10.2174/157339912803529850
31. Allali N, Petrie J, Grandhomme A, Vataire A, Miry B, and Bahloul A. EPH160 A targeted literature review to assess the impact of environmental and socio-demographic factors on the onset of type 1 diabetes. Value Health. (2024) 27:S251. doi: 10.1016/j.jval.2024.10.1288
32. Butalia S, Johnson J, Ghali W, and Rabi D. Clinical and socio-demographic factors associated with diabetic ketoacidosis hospitalization in adults with Type 1 diabetes. Diabetic Med. (2013) 30:567–73. doi: 10.1111/dme.12127
33. Murillo M, Bel J, Pérez J, Corripio R, Carreras G, Herrero X, et al. Health-related quality of life (HRQOL) and its associated factors in children with Type 1 Diabetes Mellitus (T1DM). BMC pediatrics. (2017) 17:16. doi: 10.1186/s12887-017-0788-x
34. Lindner LM, Rathmann W, and Rosenbauer J. Inequalities in glycaemic control, hypoglycaemia and diabetic ketoacidosis according to socio-economic status and area-level deprivation in type 1 diabetes mellitus: a systematic review. Diabetic Med. (2018) 35:12–32. doi: 10.1111/dme.13519
35. Craig ME, Kim KW, Isaacs SR, Penno MA, Hamilton-Williams EE, Couper JJ, et al. Early-life factors contributing to type 1 diabetes. Diabetologia. (2019) 62:1823–34. doi: 10.1007/s00125-019-4942-x
36. Tatti P and Pavandeep S. Gender difference in type 1 diabetes: An underevaluated dimension of the disease. Diabetology. (2022) 3:364–8. doi: 10.3390/diabetology3020027
37. Wandell PE and Carlsson AC. Time trends and gender differences in incidence and prevalence of type 1 diabetes in Sweden. Curr Diabetes Rev. (2013) 9:342–9. doi: 10.2174/15733998113099990064
38. Ciarambino T, Crispino P, Leto G, Mastrolorenzo E, Para O, and Giordano M. Influence of gender in diabetes mellitus and its complication. Int J Mol Sci. (2022) 23:8850. doi: 10.3390/ijms23168850
39. Bjerg L, Gudbjörnsdottir S, Franzén S, Carstensen B, Witte DR, Jørgensen ME, et al. Duration of diabetes-related complications and mortality in type 1 diabetes: a national cohort study. Int J Epidemiol. (2021) 50:1250–9. doi: 10.1093/ije/dyaa290
40. Morone J. Systematic review of sociodemographic representation and cultural responsiveness in psychosocial and behavioral interventions with adolescents with type 1 diabetes. J Diabetes. (2019) 11:582–92. doi: 10.1111/1753-0407.12889
41. Turin A and Radobuljac MD. Psychosocial factors affecting the etiology and management of type 1 diabetes mellitus: A narrative review. World J diabetes. (2021) 12:1518. doi: 10.4239/wjd.v12.i9.1518
42. Pursey KM, Hart M, Jenkins L, McEvoy M, and Smart CE. Screening and identification of disordered eating in people with type 1 diabetes: A systematic review. J Diabetes Complications. (2020) 34:107522. doi: 10.1016/j.jdiacomp.2020.107522
43. Chen Z, Wang J, Carru C, Coradduzza D, and Li Z. The prevalence of depression among parents of children/adolescents with type 1 diabetes: A systematic review and meta-analysis. Front Endocrinol (Lausanne). (2023) 14:1095729. doi: 10.3389/fendo.2023.1095729
44. Farooqi A, Gillies C, Sathanapally H, Abner S, Seidu S, Davies MJ, et al. A systematic review and meta-analysis to compare the prevalence of depression between people with and without Type 1 and Type 2 diabetes. Prim Care Diabetes. (2022) 16:1–10. doi: 10.1016/j.pcd.2021.11.001
45. Yahya AS, Khawaja S, and Naguib M. ‘Diabulimia’: current insights into type 1 diabetes and bulimia nervosa. Prog Neurol Psychiatry. (2023) 27:44–9. doi: 10.1002/pnp.782
46. Kiriella DA, Islam S, Oridota O, Sohler N, Dessenne C, de Beaufort C, et al. Unraveling the concepts of distress, burnout, and depression in type 1 diabetes: A scoping review. EClinicalMedicine. (2021) 40:101118. doi: 10.1016/j.eclinm.2021.101118
47. Akbarizadeh M, Naderi Far M, and Ghaljaei F. Prevalence of depression and anxiety among children with type 1 and type 2 diabetes: a systematic review and meta-analysis. World J Pediatr. (2022) 18:16–26. doi: 10.1007/s12519-021-00485-2
48. Benton M, Cleal B, Prina M, Baykoca J, Willaing I, Price H, et al. Prevalence of mental disorders in people living with type 1 diabetes: A systematic literature review and meta-analysis. Gen Hosp Psychiatry. (2023) 80:1–16. doi: 10.1016/j.genhosppsych.2022.11.004
49. Martinez K, Frazer SF, Dempster M, Hamill A, Fleming H, and McCorry NK. Psychological factors associated with diabetes self-management among adolescents with Type 1 diabetes: A systematic review. J Health Psychol. (2018) 23:1749–65. doi: 10.1177/1359105316669580
50. Marucci S, De Iaco G, Lisco G, Mariano F, Giagulli VA, Guastamacchia E, et al. Eating disorders and type 1 diabetes: A perspective. Endocr Metab Immune Disord Drug Targets. (2022) 22:1245–51. doi: 10.2174/1871530321666211109152353
51. Winston AP. Eating disorders and diabetes. Curr Diabetes Rep. (2020) 20:32. doi: 10.1007/s11892-020-01320-0
52. Bonfanti RC, Melchiori F, Teti A, Albano G, Raffard S, Rodgers R, et al. The association between social comparison in social media, body image concerns and eating disorder symptoms: A systematic review and meta-analysis. Body Image. (2025) 52:101841. doi: 10.1016/j.bodyim.2024.101841
53. Markey CH, Strodl E, Aime A, McCabe M, Rodgers R, Sicilia A, et al. A survey of eating styles in eight countries: Examining restrained, emotional, intuitive eating and their correlates. Br J Health Psychol. (2023) 28:136–55. doi: 10.1111/bjhp.12616
54. de la Portilla Maya SR, de la Portilla Maya DA, Londoño DMM, and Martínez DAL. Association between obesity, executive functions, and affective states: an analysis of patients from an endocrinology clinic. Mediterr J Clin Psychol. (2025) 13:1–24. doi: 10.13129/2282-1619/mjcp-4709
55. Lucifora C, Martino G, Grasso G, Mucciardi M, Magnano P, Massimino S, et al. Does fasting make us all equal? Evidence on the influence of appetite on implicit sexual prejudice. Mediterr J Clin Psychol. (2025) 13:1–22. doi: 10.13129/2282-1619/mjcp-4667
56. Batt E and Asif-Malik A. A narrative review of the current literature into the impacts of fasting on levels of impulsivity and psychological stress. Mediterr J Clin Psychol. (2025) 13:1–15. doi: 10.13129/2282-1619/mjcp-4408
57. Dalsgaard S, Thorsteinsson E, Trabjerg BB, Schullehner J, Plana-Ripoll O, Brikell I, et al. Incidence rates and cumulative incidences of the full spectrum of diagnosed mental disorders in childhood and adolescence. JAMA Psychiatry. (2020) 77:155–64. doi: 10.1001/jamapsychiatry.2019.3523
58. Bombaci B, Torre A, Longo A, Pecoraro M, Papa M, Sorrenti L, et al. Psychological and clinical challenges in the management of type 1 diabetes during adolescence: A narrative review. Children (Basel). (2024) 11:1085. doi: 10.3390/children11091085
59. Malachowska M, Goslawska Z, Rusak E, and Jarosz-Chobot P. The role and need for psychological support in the treatment of adolescents and young people suffering from type 1 diabetes. Front Psychol. (2022) 13:945042. doi: 10.3389/fpsyg.2022.945042
60. Settineri S, Frisone F, Merlo EM, Geraci D, and Martino G. Compliance, adherence, concordance, empowerment, and self-management: five words to manifest a relational maladjustment in diabetes. J Multidiscip Healthc. (2019) 12:299–314. doi: 10.2147/JMDH.S193752
61. Winkley K, Upsher R, Stahl D, Pollard D, Kasera A, Brennan A, et al. Psychological interventions to improve self-management of type 1 and type 2 diabetes: a systematic review. Health Technol Assess. (2020) 24:1–232. doi: 10.3310/hta24280
62. Badescu SV, Tataru C, Kobylinska L, Georgescu EL, Zahiu DM, Zagrean AM, et al. The association between Diabetes mellitus and Depression. J Med Life. (2016) 9:120–5.
63. Korczak DJ, Pereira S, Koulajian K, Matejcek A, and Giacca A. Type 1 diabetes mellitus and major depressive disorder: evidence for a biological link. Diabetologia. (2011) 54:2483–93. doi: 10.1007/s00125-011-2240-3
64. Wang K, Li F, Cui Y, Cui C, Cao Z, Xu K, et al. The association between depression and type 1 diabetes mellitus: inflammatory cytokines as ferrymen in between? Mediators Inflammation. (2019) 2019:2987901. doi: 10.1155/2019/2987901
65. Hassan K, Loar R, Anderson BJ, and Heptulla RA. The role of socioeconomic status, depression, quality of life, and glycemic control in type 1 diabetes mellitus. J Pediatr. (2006) 149:526–31. doi: 10.1016/j.jpeds.2006.05.039
66. Subasinghe S. A review of the prevalence and associations of depression and anxiety in type 1 diabetes mellitus. Diabetes Metab Disord. (2015) 2:1–11. doi: 10.24966/dmd-201x/100007
67. Johnson B, Eiser C, Young V, Brierley S, and Heller S. Prevalence of depression among young people with Type 1 diabetes: a systematic review. Diabetes Med. (2013) 30:199–208. doi: 10.1111/j.1464-5491.2012.03721.x
68. Lustman PJ, Clouse RE, Ciechanowski PS, Hirsch IB, and Freedland KE. Depression-related hyperglycemia in type 1 diabetes: a mediational approach. Psychosom Med. (2005) 67:195–9. doi: 10.1097/01.psy.0000155670.88919.ad
69. Turner H and Peveler R. Eating disorders and type 1 diabetes mellitus. Psychiatry. (2005) 4:30–3. doi: 10.1383/psyt.4.4.30.63442
70. Mannucci E, Rotella F, Ricca V, Moretti S, Placidi GF, and Rotella CM. Eating disorders in patients with type 1 diabetes: a meta-analysis. J Endocrinol Invest. (2005) 28:417–9. doi: 10.1007/BF03347221
71. Goebel-Fabbri AE. Disturbed eating behaviors and eating disorders in type 1 diabetes: clinical significance and treatment recommendations. Curr Diabetes Rep. (2009) 9:133–9. doi: 10.1007/s11892-009-0023-8
72. Pinhas-Hamiel O, Hamiel U, and Levy-Shraga Y. Eating disorders in adolescents with type 1 diabetes: Challenges in diagnosis and treatment. World J Diabetes. (2015) 6:517–26. doi: 10.4239/wjd.v6.i3.517
73. Barakat S, McLean SA, Bryant E, Le A, and Marks P. National Eating Disorder Research C, et al. Risk factors eating disorders: findings Rapid review J Eat Disord. (2023) 11:8. doi: 10.1186/s40337-022-00717-4
74. Hornberger LL, Lane MA, and Committee On A. Identification and management of eating disorders in children and adolescents. Pediatrics. (2021) 147:1–23. doi: 10.1542/peds.2020-040279
75. Capucho AM and Conde SV. Impact of sugars on hypothalamic satiety pathways and its contribution to dysmetabolic states. Diabetology. (2022) 4:1–10. doi: 10.3390/diabetology4010001
76. Fuller-Tyszkiewicz M, Rodgers RF, Maiano C, Mellor D, Sicilia A, Markey CH, et al. Testing of a model for risk factors for eating disorders and higher weight among emerging adults: Baseline evaluation. Body Image. (2022) 40:322–39. doi: 10.1016/j.bodyim.2022.01.007
77. Teo E, Hassan N, Tam W, and Koh S. Effectiveness of continuous glucose monitoring in maintaining glycaemic control among people with type 1 diabetes mellitus: a systematic review of randomised controlled trials and meta-analysis. Diabetologia. (2022) 65:604–19. doi: 10.1007/s00125-021-05648-4
78. Elbalshy M, Haszard J, Smith H, Kuroko S, Galland B, Oliver N, et al. Effect of divergent continuous glucose monitoring technologies on glycaemic control in type 1 diabetes mellitus: A systematic review and meta-analysis of randomised controlled trials. Diabetes Med. (2022) 39:e14854. doi: 10.1111/dme.14854
79. Lin R, Brown F, James S, Jones J, and Ekinci E. Continuous glucose monitoring: A review of the evidence in type 1 and 2 diabetes mellitus. Diabetes Med. (2021) 38:e14528. doi: 10.1111/dme.14528
80. Bitew ZW, Alemu A, Jember DA, Tadesse E, Getaneh FB, Sied A, et al. Prevalence of glycemic control and factors associated with poor glycemic control: A systematic review and meta-analysis. Inquiry. (2023) 60:469580231155716. doi: 10.1177/00469580231155716
81. Grassi G, Figee M, Pozza A, and Dell’Osso B. Obsessive-compulsive disorder, insulin signaling and diabetes - A novel form of physical health comorbidity: The sweet compulsive brain. Compr Psychiatry. (2022) 117:152329. doi: 10.1016/j.comppsych.2022.152329
82. Sivertsen B, Petrie KJ, Wilhelmsen-Langeland A, and Hysing M. Mental health in adolescents with Type 1 diabetes: results from a large population-based study. BMC Endocr Disord. (2014) 14:83. doi: 10.1186/1472-6823-14-83
83. Grammatikopoulou MG, Gkiouras K, Polychronidou G, Kaparounaki C, Gkouskou KK, Magkos F, et al. Obsessed with healthy eating: A systematic review of observational studies assessing orthorexia nervosa in patients with diabetes mellitus. Nutrients. (2021) 13:3823. doi: 10.3390/nu13113823
84. Mustač F, Matovinović M, Galijašević T, Škarić M, Podolski E, Perko T, et al. A review of the literature relationship between psychological eating patterns and the risk of type 2 diabetes mellitus and metabolic syndrome. Diabetology. (2024) 5:365–74. doi: 10.3390/diabetology5040028
85. Kristo AS, İzler K, Grosskopf L, Kerns JJ, and Sikalidis AK. Emotional eating is associated with T2DM in an urban turkish population: A pilot study utilizing social media. Diabetology. (2024) 5:286–99. doi: 10.3390/diabetology5030022
86. Randväli M, Toomsoo T, and Šteinmiller J. The main risk factors in type 2 diabetes for cognitive dysfunction, depression, and psychosocial problems: A systematic review. Diabetology. (2024) 5:40–59. doi: 10.3390/diabetology5010004
87. Leue C, van Schijndel MA, Keszthelyi D, van Koeveringe G, Ponds RW, Kathol RG, et al. The multi-disciplinary arena of psychosomatic medicine – Time for a transitional network approach. Eur J Psychiatry. (2020) 34:63–73. doi: 10.1016/j.ejpsy.2020.02.003
88. Fava GA. Patients as health producers: the psychosomatic foundation of lifestyle medicine. Psychother Psychosom. (2023) 92:81–6. doi: 10.1159/000529953
89. Wasserman LI and Trifonova EA. Diabetes mellitus as a model of psychosomatic and somatopsychic interrelationships. Span J Psychol. (2006) 9:75–85. doi: 10.1017/s1138741600005990
90. Kose S and Murat M. Psychological symptoms in children with type-1 diabetes. Int J Caring Sci. (2020) 13:288.
91. Petrak F, Hardt J, Wittchen HU, Kulzer B, Hirsch A, Hentzelt F, et al. Prevalence of psychiatric disorders in an onset cohort of adults with type 1 diabetes. Diabetes Metab Res Rev. (2003) 19:216–22. doi: 10.1002/dmrr.374
92. Costa-Cordella S, Luyten P, Cohen D, Mena F, and Fonagy P. Mentalizing in mothers and children with type 1 diabetes. Dev Psychopathol. (2021) 33:216–25. doi: 10.1017/S0954579419001706
93. Merlo EM, Myles LAM, and Martino G. Letter to the Editor: On the critical nature of psychosomatics in clinical practice. Clin Psychol Europe. (2025) 7:1–3. doi: 10.32872/cpe.16309
94. Pompili M, Forte A, Lester D, Erbuto D, Rovedi F, Innamorati M, et al. Suicide risk in type 1 diabetes mellitus: A systematic review. J Psychosom Res. (2014) 76:352–60. doi: 10.1016/j.jpsychores.2014.02.009
95. Chida Y and Hamer M. An association of adverse psychosocial factors with diabetes mellitus: a meta-analytic review of longitudinal cohort studies. Diabetologia. (2008) 51:2168–78. doi: 10.1007/s00125-008-1154-1
96. Sharif K, Watad A, Coplan L, Amital H, Shoenfeld Y, and Afek A. Psychological stress and type 1 diabetes mellitus: what is the link? Expert Rev Clin Immunol. (2018) 14:1081–8. doi: 10.1080/1744666X.2018.1538787
97. Preece DA and Gross JJ. Conceptualizing alexithymia. Pers Individ Differences. (2023) 215:112375. doi: 10.1016/j.paid.2023.112375
98. Preece DA, Becerra R, Robinson K, Allan A, Boyes M, Chen W, et al. What is alexithymia? Using factor analysis to establish its latent structure and relationship with fantasizing and emotional reactivity. J Pers. (2020) 88:1162–76. doi: 10.1111/jopy.12563
99. Lesser IM. A review of the alexithymia concept. Psychosom Med. (1981) 43:531–43. doi: 10.1097/00006842-198112000-00009
100. Timoney LR, Holder MD, Timoney LR, and Holder MD. Definition of alexithymia. Dordrecht: Springer (2013). pp. 1–6.
101. Taylor GJ. Alexithymia: 25 years of theory and research. Hove & New York: Brunner-Routledge (2004). pp. 137–53.
102. Bagby RM, Quilty LC, Taylor GJ, Grabe HJ, Luminet O, Verissimo R, et al. Are there subtypes of alexithymia? Pers Individ Dif. (2009) 47:413–8. doi: 10.1016/j.paid.2009.04.012
103. Gangemi S, Ricciardi L, Caputo A, Giorgianni C, Furci F, Spatari G, et al. Alexithymia in an unconventional sample of Forestry Officers: a clinical psychological study with surprising results. Mediterr J Clin Psychol. (2021) 9:1–18. doi: 10.13129/2282-1619/mjcp-3245
104. Taylor GJ and Bagby RM. New trends in alexithymia research. Psychother Psychosom. (2004) 73:68–77. doi: 10.1159/000075537
105. Taylor GJ. Recent developments in alexithymia theory and research. Can J Psychiatry. (2000) 45:134–42. doi: 10.1177/070674370004500203
106. Nouemssi JPM, Dumet N, and Djemo JBF. Operative thinking, alexithymia, feeling and expression of the theme of persecution. Mediterr J Clin Psychol. (2021) 9:1–35. doi: 10.6092/2282-1619/mjcp-2920
107. Kiskimska ND and Martínez-Sánchez F. Spanish adaptation of the Perth Alexithymia Questionnaire: psychometric properties. Mediterr J Clin Psychol. (2023) 11:1–21. doi: 10.13129/2282-1619/mjcp-3717
108. Baiardini I, Abba S, Ballauri M, Vuillermoz G, and Braido F. Alexithymia and chronic diseases: the state of the art. G Ital Med Lav Ergon. (2011) 33(1 Suppl A):A47–52.
109. Martino G, Caputo A, Schwarz P, Bellone F, Fries W, Quattropani MC, et al. Alexithymia and inflammatory bowel disease: A systematic review. Front Psychol. (2020) 11:1763. doi: 10.3389/fpsyg.2020.01763
110. Silvestro O, Ricciardi L, Catalano A, Vicario CM, Tomaiuolo F, Pioggia G, et al. Alexithymia and asthma: a systematic review. Front Psychol. (2023) 14:1221648. doi: 10.3389/fpsyg.2023.1221648
111. Mustač F, Galijašević T, Podolski E, Belančić A, Matovinović M, and Marčinko D. Recent advances in psychotherapeutic treatment and understanding of alexithymia in patients with obesity and diabetes mellitus type 2. Diabetology. (2023) 4:481–9. doi: 10.3390/diabetology4040041
112. Puşcaşu A, Bolocan A, Păduraru DN, Salmen T, Bica C, and Andronic O. The implications of chronic psychological stress in the development of diabetes mellitus type 2. Mediterr J Clin Psychol. (2022) 10:1–14. doi: 10.13129/2282-1619/mjcp-3544
113. Housiaux M, Luminet O, Van Broeck N, and Dorchy H. Alexithymia is associated with glycaemic control of children with type 1 diabetes. Diabetes Metab. (2010) 36:455–62. doi: 10.1016/j.diabet.2010.06.004
114. Shayeghian Z, Moeineslam M, Hajati E, Karimi M, Amirshekari G, and Amiri P. The relation of alexithymia and attachment with type 1 diabetes management in adolescents: a gender-specific analysis. BMC Psychol. (2020) 8:30. doi: 10.1186/s40359-020-00396-3
115. Luminet O, de Timary P, Buysschaert M, and Luts A. The role of alexithymia factors in glucose control of persons with type 1 diabetes: a pilot study. Diabetes Metab. (2006) 32:417–24. doi: 10.1016/s1262-3636(07)70299-9
116. Lorenzo P and Simona P. Alexithymia in adults with brittle type 1 diabetes. Acta Bio Medica: Atenei Parmensis. (2019) 90:279. doi: 10.23750/abm.v90i2.6818
117. Pechnikova L, Manuylova Y, Ryzhov A, Zhuykova E, Sokolova E, and Tkhostov A. Predictors of compliance in adolescents with type 1 diabetes mellitus. Eur Psychiatry. (2021) 64:S251–S. doi: 10.1192/j.eurpsy.2021.673
118. Merlo EM, Tutino R, Myles LAM, Lia MC, and Minasi D. Alexithymia, intolerance to uncertainty and mental health difficulties in adolescents with Type 1 diabetes mellitus. Ital J Pediatr. (2024) 50:99. doi: 10.1186/s13052-024-01647-4
119. Mnif L, Damak R, Mnif F, Ouanes S, Abid M, Jaoua A, et al. Alexithymia impact on type 1 and type 2 diabetes: a case-control study. In: Annales d’endocrinologie. Amsterdam: Elsevier (2014).
120. Ozsivadjian A, Hollocks MJ, Magiati I, Happe F, Baird G, and Absoud M. Is cognitive inflexibility a missing link? The role of cognitive inflexibility, alexithymia and intolerance of uncertainty in externalising and internalising behaviours in young people with autism spectrum disorder. J Child Psychol Psychiatry. (2021) 62:715–24. doi: 10.1111/jcpp.13295
121. Moore HL, Brice S, Powell L, Ingham B, Freeston M, Parr JR, et al. The mediating effects of alexithymia, intolerance of uncertainty, and anxiety on the relationship between sensory processing differences and restricted and repetitive behaviours in autistic adults. J Autism Dev Disord. (2022) 52:4384–96. doi: 10.1007/s10803-021-05312-1
122. Larkin F, Ralston B, Dinsdale SJ, Kimura S, and Hayiou-Thomas ME. Alexithymia and intolerance of uncertainty predict somatic symptoms in autistic and non-autistic adults. Autism. (2023) 27:602–15. doi: 10.1177/13623613221109717
123. Abbate-Daga G, Quaranta M, Marzola E, Amianto F, and Fassino S. The relationship between alexithymia and intolerance of uncertainty in anorexia nervosa. Psychopathology. (2015) 48:202–8. doi: 10.1159/000381587
124. Gibson B, Rosser BA, Schneider J, and Forshaw MJ. The role of uncertainty intolerance in adjusting to long-term physical health conditions: A systematic review. PloS One. (2023) 18:e0286198. doi: 10.1371/journal.pone.0286198
125. Koerner N and Dugas MJ. A cognitive model of generalized anxiety disorder: The role of intolerance of uncertainty. Worry its psychol disorders: Theory Assess Treat. (2006), 201–16. doi: 10.1002/9780470713143.ch12
126. Koerner N and Dugas MJ. An investigation of appraisals in individuals vulnerable to excessive worry: the role of intolerance of uncertainty. Cogn Ther Res. (2007) 32:619–38. doi: 10.1007/s10608-007-9125-2
127. Birrell J, Meares K, Wilkinson A, and Freeston M. Toward a definition of intolerance of uncertainty: a review of factor analytical studies of the Intolerance of Uncertainty Scale. Clin Psychol Rev. (2011) 31:1198–208. doi: 10.1016/j.cpr.2011.07.009
128. Morriss J, Abend R, Zika O, Bradford DE, and Mertens G. Neural and psychophysiological markers of intolerance of uncertainty. Elsevier;. (2023) p:94–9. doi: 10.1016/j.ijpsycho.2023.01.003
129. Tanovic E, Gee DG, and Joormann J. Intolerance of uncertainty: Neural and psychophysiological correlates of the perception of uncertainty as threatening. Clin Psychol Rev. (2018) 60:87–99. doi: 10.1016/j.cpr.2018.01.001
130. Oshrieh V, Besharat MA, and Gholamali Lavasani M. Predicting illness anxiety symptoms based on worry, alexithymia, intolerance of uncertainty and cognitive emotion regulation strategies. J psychol Science. (2024) 23:2311–26. doi: 10.52547/JPS.23.142.2311
131. Becerra R, Gainey K, Murray K, and Preece DA. Intolerance of uncertainty and anxiety: The role of beliefs about emotions. J Affect Disord. (2023) 324:349–53. doi: 10.1016/j.jad.2022.12.064
132. Sharratt L and Ridout N. Direct and indirect effects of childhood adversity on psychopathology: Investigating parallel mediation via self-concept clarity, self-esteem and intolerance of uncertainty. Br J Clin Psychol. (2025) 64:539–52. doi: 10.1111/bjc.12523
133. Feng B, Zeng L, Hu Z, Fan X, Ai X, Huang F, et al. Global precedence effect in fear generalization and the role of trait anxiety and intolerance of uncertainty. Behav Res Ther. (2025) 184:104669. doi: 10.1016/j.brat.2024.104669
134. Ye H, Liu Y, Cai Z, Jiang N, He S, Yu W, et al. The asymmetric moderating role of intolerance of uncertainty in the longitudinal reciprocal associations between sleep disturbance and internalizing symptoms: A two-wave study among 54,240 adolescents. Int J Ment Health Addict. (2024), 1–20. doi: 10.1007/s11469-024-01420-y
135. Brown M, Robinson L, Campione GC, Wuensch K, Hildebrandt T, and Micali N. Intolerance of uncertainty in eating disorders: A systematic review and meta-analysis. Eur Eat Disord Rev. (2017) 25:329–43. doi: 10.1002/erv.2523
136. Gu Y, Gu S, Lei Y, and Li H. From uncertainty to anxiety: how uncertainty fuels anxiety in a process mediated by intolerance of uncertainty. Neural Plast. (2020) 2020:8866386. doi: 10.1155/2020/8866386
137. Shapiro MO, Short NA, Morabito D, and Schmidt NB. Prospective associations between intolerance of uncertainty and psychopathology. Pers Individ Differences. (2020) 166:110210. doi: 10.1016/j.paid.2020.110210
138. Geok ET, Lee KYC, and Sundermann O. An experimental investigation of intolerance of uncertainty and its impact on sub-clinical psychopathology. J Behav Ther Exp Psychiatry. (2022) 75:101718. doi: 10.1016/j.jbtep.2021.101718
139. Zemestani M, Heshmati R, Comer JS, and Kendall PC. Intolerance of uncertainty as a transdiagnostic vulnerability to anxiety disorders in youth. Curr Psychol. (2023) 42:26966–78. doi: 10.1007/s12144-022-03645-3
140. Kick L, Schleicher D, Ecker A, Kandsperger S, Brunner R, and Jarvers I. Alexithymia as a mediator between adverse childhood events and the development of psychopathology: a meta-analysis. Front Psychiatry. (2024) 15:1412229. doi: 10.3389/fpsyt.2024.1412229
141. Cianchetti C and Sannio Fascello G. . Scale psichiatriche di autosomministrazione per fanciulli e adolescenti (SAFA). Firenze: Organizzazioni Speciali (2001).
142. Franzoni E, Monti M, Pellicciari A, Muratore C, Verrotti A, Garone C, et al. SAFA: A new measure to evaluate psychiatric symptoms detected in a sample of children and adolescents affected by eating disorders. Correlations Risk factors Neuropsychiatr Dis Treat. (2009) 5:207–14. doi: 10.2147/ndt.s4874
143. Bagby RM, Parker JD, and Taylor GJ. The twenty-item Toronto Alexithymia Scale–I. Item selection and cross-validation of the factor structure. J Psychosom Res. (1994) 38:23–32. doi: 10.1016/0022-3999(94)90005-1
144. Craparo G, Faraci P, and Gori A. Psychometric properties of the 20-item toronto alexithymia scale in a group of italian younger adolescents. Psychiatry Investig. (2015) 12:500–7. doi: 10.4306/pi.2015.12.4.500
145. Ballarotto G, Muzi S, Renzi A, Cimino S, Dentale F, Di Trani M, et al. Psychometric properties of the toronto alexithymia scale in italian adolescents. Mediterr J Clin Psychol. (2025) 13:1–22. doi: 10.13129/2282-1619/mjcp-4813
146. Parker JD, Eastabrook JM, Keefer KV, and Wood LM. Can alexithymia be assessed in adolescents? Psychometric properties of the 20-item Toronto Alexithymia Scale in younger, middle, and older adolescents. psychol assessment. (2010) 22:798. doi: 10.1037/a0020256
147. Bressi C, Taylor G, Parker J, Bressi S, Brambilla V, Aguglia E, et al. Cross validation of the factor structure of the 20-item Toronto Alexithymia Scale: an Italian multicenter study. J Psychosom Res. (1996) 41:551–9. doi: 10.1016/s0022-3999(96)00228-0
148. Carleton RN, Norton MA, and Asmundson GJ. Fearing the unknown: a short version of the Intolerance of Uncertainty Scale. J Anxiety Disord. (2007) 21:105–17. doi: 10.1016/j.janxdis.2006.03.014
149. Boelen PA, Vrinssen I, and van Tulder F. Intolerance of uncertainty in adolescents: correlations with worry, social anxiety, and depression. J Nerv Ment Dis. (2010) 198:194–200. doi: 10.1097/NMD.0b013e3181d143de
150. Dekkers LM, Jansen BR, Salemink E, and Huizenga HM. Intolerance of Uncertainty Scale: Measurement invariance among adolescent boys and girls and relationships with anxiety and risk taking. J Behav Ther Exp Psychiatry. (2017) 55:57–65. doi: 10.1016/j.jbtep.2016.11.009
151. Bottesi G, Iannattone S, Carraro E, and Lauriola M. The assessment of Intolerance of uncertainty in youth: An examination of the Intolerance of Uncertainty Scale-Revised in Italian nonclinical boys and girls. Res Child Adolesc Psychopathology. (2023) 51:209–22. doi: 10.1016/j.jbtep.2016.11.009
152. Lauriola M, Mosca O, and Carleton RN. Hierarchical factor structure of the Intolerance of Uncertainty Scale short form (IUS-12) in the Italian version. TPM-Testing Psychometrics Method Appl Psychol. (2017) 23:1–18. doi: 10.1037/t57434-000
153. Iuso S, Severo M, Ventriglio A, Bellomo A, Limone P, and Petito A. Psychoeducation reduces alexithymia and modulates anger expression in a school setting. Children (Basel). (2022) 9:1418. doi: 10.3390/children9091418
154. Lane RD, Sechrest L, and Riedel R. Sociodemographic correlates of alexithymia. Compr Psychiatry. (1998) 39:377–85. doi: 10.1016/s0010-440x(98)90051-7
155. Joukamaa M, Taanila A, Miettunen J, Karvonen JT, Koskinen M, and Veijola J. Epidemiology of alexithymia among adolescents. J Psychosom Res. (2007) 63:373–6. doi: 10.1016/j.jpsychores.2007.01.018
156. Pasini A, Delle Chiaie R, Seripa S, and Ciani N. Alexithymia as related to sex, age, and educational level: results of the Toronto Alexithymia Scale in 417 normal subjects. Compr Psychiatry. (1992) 33:42–6. doi: 10.1016/0010-440x(92)90078-5
157. Schooler JW, Smallwood J, Christoff K, Handy TC, Reichle ED, and Sayette MA. Meta-awareness, perceptual decoupling and the wandering mind. Trends Cognit Sci. (2011) 15:319–26. doi: 10.1016/j.tics.2011.05.006
158. Irish M, Goldberg ZL, Alaeddin S, O’Callaghan C, and Andrews-Hanna JR. Age-related changes in the temporal focus and self-referential content of spontaneous cognition during periods of low cognitive demand. Psychol Res. (2019) 83:747–60. doi: 10.1007/s00426-018-1102-8
159. Okayama S, Minihan S, Andrews JL, Daniels S, Grunewald K, Richards M, et al. Intolerance of uncertainty and psychological flexibility as predictors of mental health from adolescence to old age. Soc Psychiatry Psychiatr Epidemiol. (2024) 59:2361–8. doi: 10.1007/s00127-024-02724-z
160. Osmanagaoglu N, Creswell C, and Dodd HF. Intolerance of Uncertainty, anxiety, and worry in children and adolescents: A meta-analysis. J Affect Disord. (2018) 225:80–90. doi: 10.1016/j.jad.2017.07.035
161. Xie S, Zhang X, Cheng W, and Yang Z. Adolescent anxiety disorders and the developing brain: comparing neuroimaging findings in adolescents and adults. Gen Psychiatr. (2021) 34:e100411. doi: 10.1136/gpsych-2020-100411
162. Albaugh MD, Nguyen TV, Ducharme S, Collins DL, Botteron KN, D’Alberto N, et al. Age-related volumetric change of limbic structures and subclinical anxious/depressed symptomatology in typically developing children and adolescents. Biol Psychol. (2017) 124:133–40. doi: 10.1016/j.biopsycho.2017.02.002
163. Sergi A, Messina A, Saija R, Martino G, Caccamo MT, Kuo M-F, et al. Time-irreversible quantum-classical dynamics of molecular models in the brain. Symmetry. (2025) 17:285. doi: 10.3390/sym17020285
164. Beynon AM, Hebert JJ, Hodgetts CJ, Boulos LM, and Walker BF. Chronic physical illnesses, mental health disorders, and psychological features as potential risk factors for back pain from childhood to young adulthood: a systematic review with meta-analysis. Eur Spine J. (2020) 29:480–96. doi: 10.1007/s00586-019-06278-6
165. Hoover S and Bostic J. Schools as a vital component of the child and adolescent mental health system. Psychiatr Serv. (2021) 72:37–48. doi: 10.1176/appi.ps.201900575
166. Pulimeno M, Piscitelli P, Colazzo S, Colao A, and Miani A. School as ideal setting to promote health and wellbeing among young people. Health Promot Perspect. (2020) 10:316–24. doi: 10.34172/hpp.2020.50
167. Arango C, Dragioti E, Solmi M, Cortese S, Domschke K, Murray RM, et al. Risk and protective factors for mental disorders beyond genetics: an evidence-based atlas. World Psychiatry. (2021) 20:417–36. doi: 10.1002/wps.20894
168. Hiirola A, Pirkola S, Karukivi M, Markkula N, Bagby RM, Joukamaa M, et al. An evaluation of the absolute and relative stability of alexithymia over 11years in a Finnish general population. J Psychosom Res. (2017) 95:81–7. doi: 10.1016/j.jpsychores.2017.02.007
169. de Ridder D, Geenen R, Kuijer R, and van Middendorp H. Psychological adjustment to chronic disease. Lancet. (2008) 372:246–55. doi: 10.1016/S0140-6736(08)61078-8
170. Dekker J and de Groot V. Psychological adjustment to chronic disease and rehabilitation - an exploration. Disabil Rehabil. (2018) 40:116–20. doi: 10.1080/09638288.2016.1247469
171. Livneh H. Psychosocial adaptation to chronic illness and disability: An updated and expanded conceptual framework. Rehabil Couns Bulletin. (2022) 65:171–84. doi: 10.1177/00343552211034819
172. Chatzi L, Bitsios P, Solidaki E, Christou I, Kyrlaki E, Sfakianaki M, et al. Type 1 diabetes is associated with alexithymia in nondepressed, non-mentally ill diabetic patients: a case-control study. J Psychosom Res. (2009) 67:307–13. doi: 10.1016/j.jpsychores.2009.04.011
173. Strout TD, Hillen M, Gutheil C, Anderson E, Hutchinson R, Ward H, et al. Tolerance of uncertainty: A systematic review of health and healthcare-related outcomes. Patient Educ Couns. (2018) 101:1518–37. doi: 10.1016/j.pec.2018.03.030
174. Ren L, Wei Z, Li Y, Cui LB, Wang Y, Wu L, et al. The relations between different components of intolerance of uncertainty and symptoms of generalized anxiety disorder: a network analysis. BMC Psychiatry. (2021) 21:448. doi: 10.1186/s12888-021-03455-0
175. Wilson EJ, Abbott MJ, and Norton AR. The impact of psychological treatment on intolerance of uncertainty in generalized anxiety disorder: A systematic review and meta-analysis. J Anxiety Disord. (2023) 97:102729. doi: 10.1016/j.janxdis.2023.102729
176. Sternheim L, Bijsterbosch J, Boelen PA, and Frank G. Intolerance of Uncertainty in Eating Disorders: a scoping review. Center Open Science. (2023). doi: 10.17605/OSF.IO/JCDRQ
177. Kesby A, Maguire S, Brownlow R, and Grisham JR. Intolerance of Uncertainty in eating disorders: An update on the field. Clin Psychol Rev. (2017) 56:94–105. doi: 10.1016/j.cpr.2017.07.002
178. Muir X, Preece DA, and Becerra R. Alexithymia and eating disorder symptoms: the mediating role of emotion regulation. Aust Psychol. (2023) 59:121–31. doi: 10.1080/00050067.2023.2236280
179. Celik S, Taskin Yilmaz F, Yurtsever Celik S, Anataca G, and Bulbul E. Alexithymia in diabetes patients: its relationship with perceived social support and glycaemic control. J Clin Nurs. (2022) 31:2612–20. doi: 10.1111/jocn.16088
180. Malykhin N, Pietrasik W, Aghamohammadi-Sereshki A, Ngan Hoang K, Fujiwara E, and Olsen F. Emotional recognition across the adult lifespan: Effects of age, sex, cognitive empathy, alexithymia traits, and amygdala subnuclei volumes. J Neurosci Res. (2023) 101:367–83. doi: 10.1002/jnr.25152
181. Gómez Tabares AS, Carmona Marín JP, Muñoz Vanegas A, Mogollón Gallego EM, Catalina Muñoz A, Núñez C, et al. The impact of emotional intelligence and coping strategies on suicide risk in adolescents. Mediterr J Clin Psychol. (2025) 13:1–27. doi: 10.13129/2282-1619/mjcp-4930
182. Mendia J, Zumeta LN, Cusi O, Pascual A, Alonso-Arbiol I, Díaz V, et al. Gender differences in alexithymia: Insights from an Updated Meta-Analysis. Pers Individ Differences. (2024) 227:112710. doi: 10.1016/j.paid.2024.112710
183. Barsky AJ, Frank CB, Cleary PD, Wyshak G, and Klerman GL. The relation between hypochondriasis and age. Am J Psychiatry. (1991) 148:923–8. doi: 10.1176/ajp.148.7.923
184. Creed F and Barsky A. A systematic review of the epidemiology of somatisation disorder and hypochondriasis. J Psychosom Res. (2004) 56:391–408. doi: 10.1016/S0022-3999(03)00622-6
185. Merlo EM and Myles LAM. Navigating the multidisciplinary landscape of clinical psychology. Mediterr J Clin Psychol. (2024) 12:1–9. doi: 10.13129/2282-1619/mjcp-4275
186. Galletti B, Freni F, Meduri A, Oliverio GW, Signorino GA, Perroni P, et al. Rhino-Orbito-Cerebral Mucormycosis in Diabetic Disease Mucormycosis in Diabetic Disease. J Craniofac Surg. (2020) 31:e321–e4. doi: 10.1097/scs.0000000000006191
Keywords: alexithymia, anxiety, clinical psychology, depression, diabetes, intolerance to uncertainty, psychopathology, type 1 diabetes mellitus
Citation: Merlo EM, Martino G, Tutino R, Myles LAM, Hill S, Alibrandi A, Lia MC and Minasi D (2025) Psychological functioning of patients with type I diabetes: the relevant role of alexithymia and intolerance to uncertainty. Front. Psychiatry 16:1667103. doi: 10.3389/fpsyt.2025.1667103
Received: 16 July 2025; Accepted: 11 September 2025;
Published: 01 October 2025.
Edited by:
Daniela Marchetti, University of Studies G. d’Annunzio Chieti and Pescara, ItalyReviewed by:
Jayne Morriss, University of Southampton, United KingdomPaolo Meneguzzo, University of Padua, Italy
Copyright © 2025 Merlo, Martino, Tutino, Myles, Hill, Alibrandi, Lia and Minasi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emanuele Maria Merlo, ZW1lcmxvQHVuaW1lLml0
†These authors have contributed equally to this work and share first authorship
 Emanuele Maria Merlo
Emanuele Maria Merlo Gabriella Martino
Gabriella Martino Rita Tutino3
Rita Tutino3 Liam Alexander MacKenzie Myles
Liam Alexander MacKenzie Myles Sean Hill
Sean Hill Angela Alibrandi
Angela Alibrandi