- 1Department of Psychology, University of Zurich, Zurich, Switzerland
- 2Digital Society Initiative, University of Zurich, Zurich, Switzerland
Main text
An increasing number of randomized controlled trials (RCTs) demonstrate the efficacy of psychotherapy delivered by artificial intelligence (AI)-based chatbots (reviewed in (1–3)). For instance, a recent first-of-its-kind RCT of a generative AI chatbot found a large effect size for depression reduction at 8 weeks (Cohen’s d ≈ 0.8) (4). Picked up by industry stakeholders, media outlets, and even some researchers, this has led to the claims that AI psychotherapy might already be comparable to human psychotherapy. Anticipating more studies showing similar results, a crucial question emerges: Do comparable effect sizes imply equivalence between AI chatbot therapy and human psychotherapy, such that they can be considered interchangeable treatment options?
This perspective argues that while symptom-level outcome comparability is an important milestone, it alone does not establish equivalence. True equivalence requires meeting a broader and more nuanced set of empirical and theoretical criteria that capture the complexity of psychotherapy as a clinical practice. Currently, these criteria are largely absent from the literature, with only a few papers so far formally discussing the comparability of chatbot- and human-based therapies (see, e.g (5, 6)). In the attempt to contribute to this discussion, we propose an exploratory set of criteria to guide rigorous evaluation and inform clinical, ethical, and policy decisions.
For example, one long-standing limitation of Digital Mental Health (DMH) interventions is the high attrition rates (7–9). RCTs often show efficacy in controlled settings with motivated participants, whereas real-world environments are more varied and less structured. Traditional psychotherapy benefits from a unique form of human accountability that sustains engagement despite fluctuations in motivation or external stressors. The absence of at least minimal human-to-human contact in chatbot-based interventions may limit sustained use and thereby reduce long-term effectiveness (7). Claims of comparability must therefore be supported by studies demonstrating sustainable real-world adherence and engagement.
In addition, the implementation of DMH tools within established healthcare systems remains a significant challenge (8). Interventions tested in isolation (e.g (4)) may fail when integrated into real-world workflows. For chatbot-based therapy to be considered comparable, it must demonstrate not only stand-alone efficacy but also effective incorporation into healthcare settings, including primary care, mental health clinics, and stepped-care models (9). Previous DMH tools, despite showing efficacy, often failed in practice due to misalignment with patient needs or clinician workflows (e.g., see (9, 10)). Therefore, feasibility studies are essential to assess whether chatbot therapy is viable and compatible with daily clinical workflows.
The APA’s recent ethical guidance for AI in psychological services contributes to solving this issue by emphasizing that AI tools must be designed with user-centered features, such as culturally responsive interfaces and personalized feedback, to enhance engagement in diverse real-world populations (11). It also emphasizes the human-in-the-loop approach that might help to mitigate engagement concerns. For example, studies show that at least minimal involvement of a human in the digital intervention (e.g., in the form of coaching) might help retain people (10).
Furthermore, current RCTs evaluating chatbot interventions primarily report short-term outcomes, often limited to 6–8 weeks (e.g (4, 12, 13)). In contrast, psychotherapy research emphasizes long-term change, including relapse prevention and maintenance of gains. Without longitudinal follow-up data, ideally extending at least 6–12 months, claims about the therapeutic potential of chatbots remain provisional. Future studies should assess time to relapse, symptom recurrence, and long-term functioning to determine if chatbot therapy fosters enduring change.
Another important issue is that therapeutic change often arises from the quality and dynamics of the therapeutic relationship (14). While chatbot interactions can simulate empathy and responsiveness, it is unclear whether they can replicate deeper interpersonal processes, such as the formation and resolution of alliance ruptures. Decades of psychotherapy research show that effective therapy is not only about empathy and affirmation but about navigating tension, misalignment, negative emotions toward the therapist, and repair, all of which contribute to psychological growth (15, 16). It remains an open question whether AI systems can support these fundamentally human relational processes. This is especially relevant in treating personality disorders or relational trauma, where change depends on corrective relational experiences (17, 18).
As an expansion of the point made above, it is well-known that human psychotherapy can lead to deep psychological transformations beyond mere symptom reduction (19). While symptom reduction is a valuable metric for RCTs, it does not fully capture lasting and meaningful psychological transformation. Shedler (20) lists criteria for mental health beyond symptom reduction, including, for example, (a) being able to form close and lasting friendships characterized by mutual support and sharing of experiences, (b) coming to terms with painful experiences from the past and finding meaning in and grown from such experiences, and (c) being capable of sustaining a meaningful love relationship characterized by genuine intimacy and caring. It is unclear whether chatbot therapy can facilitate such a transformation beyond mere symptom reduction. Note that although these outcomes are not achieved in every case with human therapy, it has at least demonstrated the potential to produce them.
An additional challenge is that most studies of chatbot interventions focus on mild-to-moderate depression and anxiety (1–4). These samples often exclude individuals with severe, comorbid, or high-risk conditions. Human psychotherapists are trained, and healthcare systems are prepared to navigate diagnostic ambiguity, emotional complexity, and clinical risk. In contrast, chatbot systems lack grounding in contextual understanding and may respond inappropriately to delusional thinking, self-harm ideation, or trauma disclosures (e.g., affirm and reassure these tendencies due to inherent sychophancy). To be deemed comparable in a general sense, chatbot therapy must either demonstrate efficacy across a broader spectrum of psychopathology or be explicitly positioned as symptom-managing tools for circumscribed conditions (e.g., mild depressive symptoms).
Relevant to this issue is the entry point into care. People access therapy under very different circumstances. Some enter treatment during an acute crisis (e.g., suicidality, abrupt relational changes), where risk management is essential. Others begin therapy when they are relatively stable but motivated for deep, long-term change. A third group may only seek psychoeducation, information, or short-term skills training. Human psychotherapy is designed to flexibly accommodate this diversity of goals, whereas chatbot therapy may only be suited for a narrower range (e.g., psychoeducation or structured short-term interventions). Therefore, claims of comparability must be carefully considered in the context: for whom and for what aims chatbot interventions are intended. Equivalence cannot be assumed across all entry points and therapeutic goals. Rather, chatbot-based therapy should be explicitly positioned within a limited scope of use cases and evaluated accordingly.
Finally, despite constant technological developments, ethical and risk concerns still remain a big challenge for chatbot-based mental health interventions (21). Unlike human therapists, who undergo licensing processes that ensure extensive training, supervision, and accountability, chatbots cannot be considered licensed practitioners. While they may be trained on therapy manuals and overseen by clinicians or engineers, this is not equivalent to professional preparation or responsibility. Moreover, ethical risks extend beyond licensing. Chatbots may fail to adequately detect crisis situations (e.g., suicidality or psychotic episodes), may inadvertently reinforce harmful cognitions, or may not provide appropriate escalation pathways to human care. Issues of data privacy, bias and cultural adjustments, and informed consent further complicate deployment.
In addition to the conceptual and clinical concerns outlined above, in what follows, we address methodological and design considerations that must be met in future RCTs for claims of comparability between AI-based and human-delivered psychotherapy to be valid.
First, true comparability requires head-to-head studies between chatbot and human-delivered psychotherapy using robust methodologies. Ideally, they should use non-inferiority designs, strong randomization, and control for expectancy/placebo effects.
Second, in the recent study by Heinz et al. (4)—a state-of-the-art RCT that dictates the chatbot therapy narrative—no blinding procedures were implemented. This omission presents a significant methodological limitation, particularly given the advanced language capabilities of current AI chatbots, which may lead participants to form heightened expectations. To strengthen causal inference, future studies should incorporate carefully designed control conditions. A control chatbot could mimic conversation but omit therapeutic mechanisms, acting as a neutral digital companion. Without this level of experimental control, reported effect sizes may overestimate the true therapeutic impact of AI interventions.
Third, current trials often recruit participants through mainstream social media (4), digital platforms, or mental health apps, resulting in samples that do not reflect typical psychotherapy populations. A recent systematic review suggests that online samples significantly differ from traditional populations that use psychotherapy services in terms of demographics, severity, and treatment history (22). Current chatbot RCTs primarily recruit individuals who are already motivated and willing to engage, often in a non-crisis state. This limits generalizability, as many real-world patients initiate therapy in crisis or with ambivalent readiness to change. For conclusions to generalize, studies should recruit from naturalistic clinical settings and ensure representativeness across age, socioeconomic status, cultural background, and clinical presentation.
In conclusion, the criteria proposed here offer a preliminary framework for evaluating whether an AI chatbot-delivered psychotherapy can be considered comparable to human psychotherapy (see also Table 1 for summarization). At present, claims of equivalence and even comparability are premature and risk misleading both policymakers and the public. In the absence of rigorous theoretical grounding and empirical validation, there is a danger of overstating the readiness of chatbot-based interventions as substitutes for human care. We argue that unless clearly defined criteria are met, chatbot psychotherapy should not be marketed or presented as legitimate psychotherapy, nor as equivalent or comparable to human-delivered care. We hope to inspire further research and debate on the appropriate criteria for establishing therapeutic comparability in mental health care, and to encourage researchers to propose additional or alternative criteria to help the field progress.
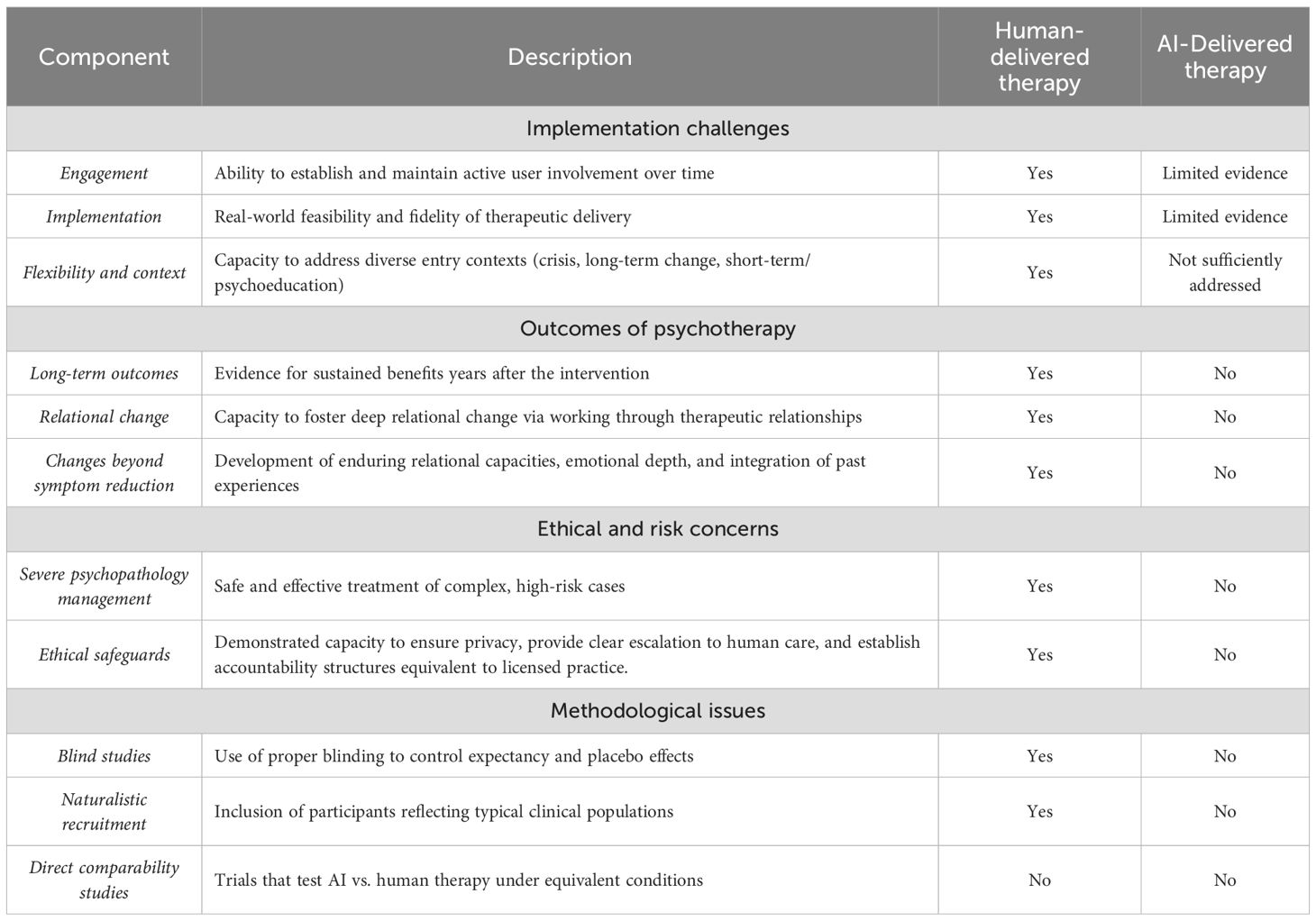
Table 1. Critical gaps in current chatbot interventions that must be addressed before claims of equivalence can be substantiated.
Author contributions
NK: Conceptualization, Writing – review & editing, Writing – original draft.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. NK was supported by the UZH Digital Society Initiative Excellence Fellowship. Open Access costs were funded by the University Library of Zurich.
Acknowledgments
I’m grateful to Jaan Aru, Johannes C. Eichstaedt, Betsy Stade, and Markus Wolf for fruitful discussions.
Conflict of interest
The author declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author declares that Gen AI was used in the creation of this manuscript. Generative AI was used to proofread and improve the manuscript’s clarity. All intellectual aspects of this work were conceived entirely by the author and discussed and presented publicly before any involvement of generative AI. The author(s) declare that Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. He Y, Yang L, Qian C, Li T, Su Z, Zhang Q, et al. Conversational agent interventions for mental health problems: systematic review and meta-analysis of randomized controlled trials. J Med Internet Res. (2023) 25:e43862. doi: 10.2196/43862
2. Li H, Zhang R, Lee YC, Kraut RE, and Mohr DC. Systematic review and meta-analysis of AI-based conversational agents for promoting mental health and well-being. NPJ Digit Med. (2023) 6:236. doi: 10.1038/s41746-023-00979-5
3. Zhong W, Luo J, and Zhang H. The therapeutic effectiveness of artificial intelligence-based chatbots in alleviation of depressive and anxiety symptoms in short-course treatments: A systematic review and meta-analysis. J Affect Disord. (2024) 356:459–69. doi: 10.1016/j.jad.2024.04.057
4. Heinz MV, Mackin DM, Trudeau BM, Bhattacharya S, Wang Y, Banta HA, et al. Randomized trial of a generative AI chatbot for mental health treatment. NEJM AI. (2025) 2:AIoa2400802. doi: 10.1056/AIoa2400802
5. Scholich T, Barr M, Stirman SW, and Raj S. A comparison of responses from human therapists and large language model–based chatbots to assess therapeutic communication: mixed methods study. JMIR Ment Health. (2025) 12:e69709. doi: 10.2196/69709
6. Molden H. AI, automation and psychotherapy–A proposed model for losses and gains in the automated therapeutic encounter. Eur J Psychother Counselling. (2024) 26:48–66. doi: 10.1080/13642537.2024.2318628
8. Mohr DC, Weingardt KR, Reddy M, and Schueller SM. Three problems with current digital mental health research … and three things we can do about them. Psychiatr Serv. (2017) 68:427–9. doi: 10.1176/appi.ps.201600541
9. Jabir AI, Lin X, Martinengo L, Sharp G, Theng YL, and Tudor Car L. Attrition in conversational agent–delivered mental health interventions: systematic review and meta-analysis. J Med Internet Res. (2024) 26:e48168. doi: 10.2196/48168
10. Mohr DC, Riper H, and Schueller SM. A solution-focused research approach to achieve an implementable revolution in digital mental health. JAMA Psychiatry. (2018) 75:113–4. doi: 10.1001/jamapsychiatry.2017.3838
11. American Psychological Association. Ethical guidance for AI in the professional practice of health service psychology (2025). Available online at: https://www.apa.org/topics/artificial-intelligence-machine-learning/ethical-guidance-professional-practice.pdf. (Accessed July 27, 2025)
12. Fitzpatrick KK, Darcy A, and Vierhile M. Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (Woebot): a randomized controlled trial. JMIR Ment Health. (2017) 4:e7785. doi: 10.2196/mental.7785
13. Mehta A, Niles AN, Vargas JH, Marafon T, Couto DD, and Gross JJ. Acceptability and effectiveness of artificial intelligence therapy for anxiety and depression (Youper): longitudinal observational study. J Med Internet Res. (2021) 23:e26771. doi: 10.2196/26771
14. Wampold BE and Imel ZE. The great psychotherapy debate: The evidence for what makes psychotherapy work. Milton Park in Abingdon, Oxfordshire, England, UK: Routledge (2015).
15. Safran JD, Muran JC, and Eubanks-Carter C. Repairing alliance ruptures. Psychotherapy. (2011) 48:80. doi: 10.1037/a0022140
16. Eubanks CF, Muran JC, and Safran JD. Alliance rupture repair: A meta-analysis. Psychotherapy. (2018) 55:508. doi: 10.1037/pst0000185
17. McMain SF, Boritz TZ, and Leybman MJ. Common strategies for cultivating a positive therapy relationship in the treatment of borderline personality disorder. J Psychother Integr. (2015) 25:20. doi: 10.1037/a0038768
18. Bender DS. The therapeutic alliance in the treatment of personality disorders. J Psychiatr Pract. (2005) 11:73–87. doi: 10.1097/00131746-200503000-00002
19. Campbell LF, Norcross JC, Vasquez MJ, and Kaslow NJ. Recognition of psychotherapy effectiveness: the APA resolution. Psychother (Chicago Ill.). (2013) 50:98–101. doi: 10.1037/a0031817
20. Shedler J. The efficacy of psychodynamic psychotherapy. Am Psychol. (2010) 65:98–109. doi: 10.1037/a0018378
21. Sedlakova J and Trachsel M. Conversational artificial intelligence in psychotherapy: a new therapeutic tool or agent? Am J Bioethics. (2023) 23:4–13. doi: 10.1080/15265161.2022.2048739
Keywords: psychotherapy, chatbot, AI, RCT, ChatGPT
Citation: Kabrel N (2025) When can AI psychotherapy be considered comparable to human psychotherapy? Exploring the criteria. Front. Psychiatry 16:1674104. doi: 10.3389/fpsyt.2025.1674104
Received: 27 July 2025; Accepted: 10 September 2025;
Published: 24 September 2025.
Edited by:
Heleen Riper, VU Amsterdam, NetherlandsReviewed by:
Helen Molden, Psychological, United KingdomCopyright © 2025 Kabrel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nick Kabrel, bmljay5rYWJyZWxAZ21haWwuY29t
 Nick Kabrel
Nick Kabrel