- 1Faculty of Health, Southern Cross University, Coffs Harbour, NSW, Australia
- 2Faculty of Health, Southern Cross University, Lismore, NSW, Australia
- 3School of Nursing and Midwifery, University of Southern Queensland, Toowoomba, QLD, Australia
Objectives: De-escalation is widely endorsed as an intentional strategy to replace and reduce restrictive practices in acute mental health units. However, high-quality evidence for its effective implementation remains limited. In response, a pragmatic, complexity-informed evaluation was undertaken to generate empirical support for the impact of an intervention, Safe Steps for De-escalation, on restrictive practices. The intervention centres on a four-step framework for therapeutic responding, with implementation supported by co-designed training and restrictive practice reviews.
Methods: A mixed concurrent control study was conducted in three adult inpatient units in New South Wales, Australia, from March 2023 to April 2025. A priori weighted linear, linear mixed-effects, and generalised linear mixed-effects models were fitted between and within groups, to assess the impact of the intervention on restrictive practice events, including seclusion, physical restraint, as-needed intramuscular psychotropics, event duration, and physical injury. A priori hierarchical cluster analysis and between-cluster comparison were used to examine the most active de-escalation response components and any associated concurrent supplementary strategies contributing to the overall impact.
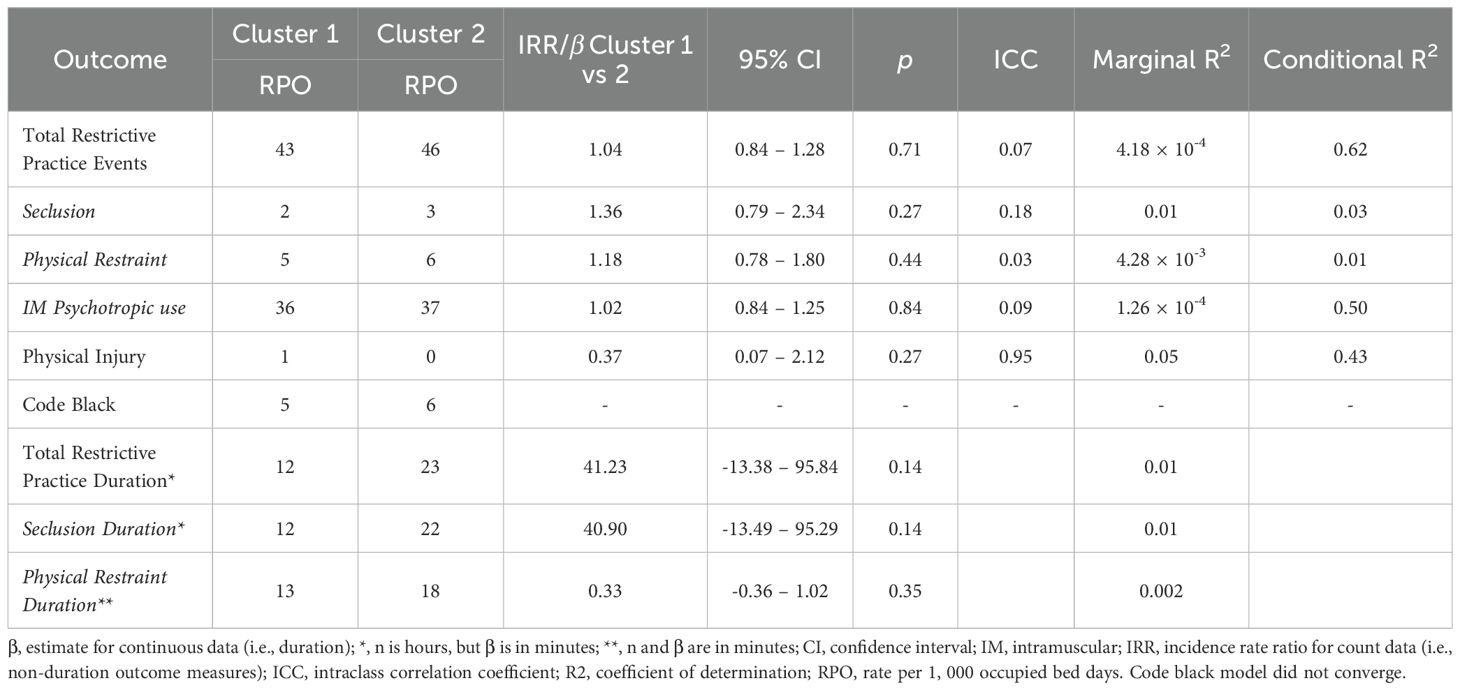
Results: Compared to three control sites, implementation sites had a lower total restrictive practice event rate (incidence rate ratio [IRR] = 0.65, 95% CI [0.60, 0.69], p <.001) over a twelve-month intervention period. At a granular level, implementation sites had lower IRRs for seclusion and as-needed intramuscular psychotropics than controls; however, within-group rates fluctuated over the year. Two clusters of de-escalation responses and additional supplementary strategies (including stimulus reduction, music, and one-on-one staff time) were noted. The differential associations between clusters and the outcomes were insignificant.
Conclusion: Despite mixed results, the evaluation offers support that structured therapeutic responding helps minimise restrictive practices, without evidence suggesting a substitution of one form of coercion for another.
Introduction
De-escalation is the purposeful use of verbal, non-verbal, and relational strategies to interrupt emotional activation, address troubling behaviours, defuse potential interpersonal conflict, and eventually restore some sense of safety for all parties (1, 2). In public acute mental health units, it occurs in an inherently coercive context, where hospitalisation is increasingly involuntary (3, 4). Nurses are the first to respond to an escalation event among other professionals in a unit (5), although they are often working with limited specialist mental health training (6, 7), are instrumental in ensuring the continuity of service delivery (8), and are deploying primarily pharmacological treatments (9). In addition, nurses enforce legally sanctioned measures that restrict individuals’ civil liberties or contradict their expressed preferences (10). Seclusion, physical restraint, and forced medication typify these rights-limiting measures (11), widely recognised as carrying moral and relational costs for nurses (12). Globally, in response to these challenges, governments and broader care communities have called for reducing restrictive practices by promoting the development of relational capabilities and less coercive responses to escalation (13–16). However, training remains variable and under-resourced, with further evidence needed to strengthen sustained integration (17). Some training also continue to focus on ‘breakaway’ and restraint techniques (18), with comparatively less emphasis on relational approaches to de-escalation.
There are gaps in scientific knowledge bases that inform the development and implementation of de-escalation and other non-pharmacological interventions to reduce restrictive practices. Evidence syntheses are accessible on, for instance, staff training (19), restrictive practice review (20), and multi-component interventions, such as the Safewards (21). The intended impact of these interventions on restrictive practices has generally been favourable, although the strength of their associations is often limited or unassessed. Specifically, for Safewards, reporting of implementation fidelity has been inconsistent, with low or highly variable uptake of core components across intervention sites (22). On the other hand, sensory room and equipment (20) and risk assessment (21) have been linked to a mixed impact on reducing restrictive practices. Trauma-informed solutions, while promoted for recognising trauma and preventing re-traumatisation, have been critiqued by people with experience of using mental health services as often indistinguishable in practice, with symbolic commitments undermined by enduring power imbalances in coercive systems (23). Many of these interventions were developed and evaluated without considering: a) a broader range of disaggregated nurse-sensitive outcomes beyond Safewards’ ‘conflict’ and ‘containment’ measures (24), b) research bias-reducing measures, such as statistical controls for confounding (25), c) extended follow-up durations approaching one year (26), d) theories, models, and frameworks in implementation and evaluation (27), and e) the wisdom, understandings, and preferences of disempowered groups of people (e.g., Indigenous people) and people with experience of using mental health services (28) and of coercion (29). Moreover, no attempt has been made to identify which specific de-escalation components, such as active listening and limit-setting, contributed most to the intervention’s overall impact on restrictive practice use (30). Initiatives are also needed to improve the content, scope, adaptation, implementation, evaluation quality, and impact of de-escalation training interventions (31).
Early implementation and support for the Safe Steps
In an adult mental health inpatient unit in regional New South Wales (NSW), Australia, a four-step approach to de-escalation, with tiered levels of complexity, was developed by a clinician in response to persistently high rates of physical restraint and seclusion, as well as the lack of clear, consistent guidance available to nurses on de-escalation (32). This approach was intended to bring order to how nurses hold space for the person in distress to explore their situation, feel listened to, discuss next steps collaboratively, and make sense of what actions may support exercising the following steps when the conversation is over. An earlier cluster analysis and between-cluster comparison, using a separate dataset, for discerning the most active co-occurring relational capabilities employed by nurses in the acute inpatient unit provides support for the structure and progression of the four-step approach (33). The steps were anchored in values of emotional intelligence, trauma-informed care, and personal recovery, which were emphasised in training on the approach. A separate feature analysis offers evidence for the importance of additional values, including cultivating situational and contextual awareness in early signs work and promoting autonomy-preserving de-escalation in inherently restrictive environments (34). These values were made explicit in tailoring practice through feedback loops in restrictive practice reviews. A separate weighted before-and-after analysis indicated that these restrictive practice reviews, conducted by a nurse unit manager with nurses as review participants and nurses’ practice of relational capabilities as a core review content, were associated with a significant reduction in seclusion in the acute inpatient unit (35). Taken together, the (i) four-step approach to therapeutic responding, implemented with the support of a (ii) phased training on the approach and the underlying values, and (iii) regular restrictive practice review meetings, comprise the Safe Steps for De-escalation, or simply the Safe Steps.
Given the observed reduction in seclusion, the initial proponents and evaluators of the Safe Steps considered this finding as preliminary evidence and expanded the evaluation to include a broader set of restrictive practice outcomes. The Safe Steps components were subsequently refined for implementation in a full-scale intervention evaluation. The hypothesised causal pathway from the Safe Steps implementation to reduced restrictive practice use, estimated using inverse probability weighting under standard causal inference assumptions, was considered to happen through changes in nurses’ relational capabilities, targeted to increase emphasis on developing and maintaining therapeutic relationships and self-management of people receiving care.
Materials and methods
Study design and participants
This paper reports findings from a larger study, employing a mixed concurrent control design, aimed at evaluating and implementing the Safe Steps. This paper addresses the study’s first objective, which sought to establish the intervention’s impact on total restrictive practice events (defined as the sum of events of seclusion, physical restraint, and as-needed intramuscular [IM] psychotropics), total restrictive practice durations (i.e., the sum of seclusion and physical restraint durations), and physical injury events (defined as the sum of bodily injury events incurred by unit staff, visitors, and people receiving care; this outcome does not include those that result from self-harm). The hypothesis tested was that the implementation units would show lower and more significant reductions in incidence rate ratios (IRRs) of total restrictive practice events, in model-derived estimates of total restrictive practice durations, and in IRRs of physical injuries, compared to control groups and within-group baseline. As an ancillary undertaking, the change mechanisms of the Safe Steps were explored through cluster analysis and by reviewing responses from the larger study’s qualitative assessment of process (experience and perspective of nurses and people receiving care through focus groups and interviews, respectively; to be published later).
The evaluation was informed by a researcher-designed implementation and evaluation framework, based on pragmatism (36) and complexity intervention research guidance (37). This framework posits that change is unique for every mental health service, grows through feedback, emerges unexpectedly, depends on shared relationships between agents of change, and needs to respect people’s choices. An overview of evidence syntheses has been a scaffold to this frame, indicating that the success of solutions in the field is hugely influenced by the contexts in which they were implemented (38). As used in health services research, complexity theory is a perspective that gives primacy to the relationships between agents of change in a service as influential in the successful delivery and evaluation of any service change (39). To support the assessment of selective reporting bias, the intervention, the proposed change mechanisms, the researcher-made implementation and evaluation framework, and the protocol for the larger study are described elsewhere (40).
Implementation was at the unit level in three sites in two NSW local health districts (LHD), with three control sites. An LHD is a regional health authority responsible for delivering public health services within a defined geographic area (41). Outcome comparisons were made between and within these six declared acute adult mental health inpatient units in public hospitals. Clinical input, each site’s readiness, and local governance processes determined the selection of implementation and control sites. The implementation sites had a combined bed capacity of 75, which included ten for high observation. The control sites had a total of 84 beds but had no high observation areas; one site lacked a seclusion room entirely. Each unit operates 24 hours a day, 7 days a week, and varies in care models, restrictive practice rates, peer worker integration, and restrictive practice review processes. These units have the legal authority to admit and treat people involuntarily, and are situated in NSW where 46% of public hospital acute mental health service hospitalisations for 2022 to 2023 were involuntary (4). Given the pragmatic, complexity-informed design of the current evaluation, which was intended to balance practicality and robustness in methodologies, inverse probability weighting was applied. This advanced statistical technique supports re-balancing the observed groups on measured characteristics to approximate the balance that randomisation would otherwise achieve (42).
At the time of the implementation, no other restrictive practice-reduction initiatives were being evaluated or trialled within the participating sites. Site implementation leads were proactive in informing the research team of any initiatives that might otherwise have conflated with the current evaluation. There were proposed initiatives identified towards the end of the Safe Steps evaluation, but implementation was postponed to avoid overlap. Furthermore, there was no standardised or structured approach regarded as a ‘go-to’ model for de-escalation across sites. In contrast, the Safe Steps was intended to bolster the uptake of relational approaches to de-escalation, strengthen reflective practice, and introduce proper documentation of relational capabilities. Foremost, it was designed to provide structured education on both theory and real-world examples of relational de-escalation.
The evaluation was undertaken across four time points per site over 12 months to support the emergence of short-, medium-, and long-term changes associated with the phased training on the Safe Steps. This observation period was informed by a priori Monte Carlo simulations, using the simr package version 1.0.8 (43) and the dataset from the initial implementation of the restrictive practice review meetings. It was estimated that, with a = 0.05 and a 20% attrition buffer, 3.60 to 12 months of data collection would be required to detect outcome-specific reductions in seclusion, physical restraint, and Code Black—a hospital emergency code called to summon the presence and support of security personnel in response to personal safety threats (44), with 85% to 99% power based on Poisson mixed-effects models. Effect size assumptions for the simulations aligned with findings from the NSW Safewards evaluation (45), which was judged as high in methodological quality (21) and shares a similar geographical context.
Ethical approvals for the implementation and evaluation were obtained from Human Research Ethics Committees in an LHD (2023/PID00297 - 2023/ETH00272) and a university (2023/069) in NSW, Australia. The implementation and evaluation were undertaken with oversight from a project steering committee.
Procedures
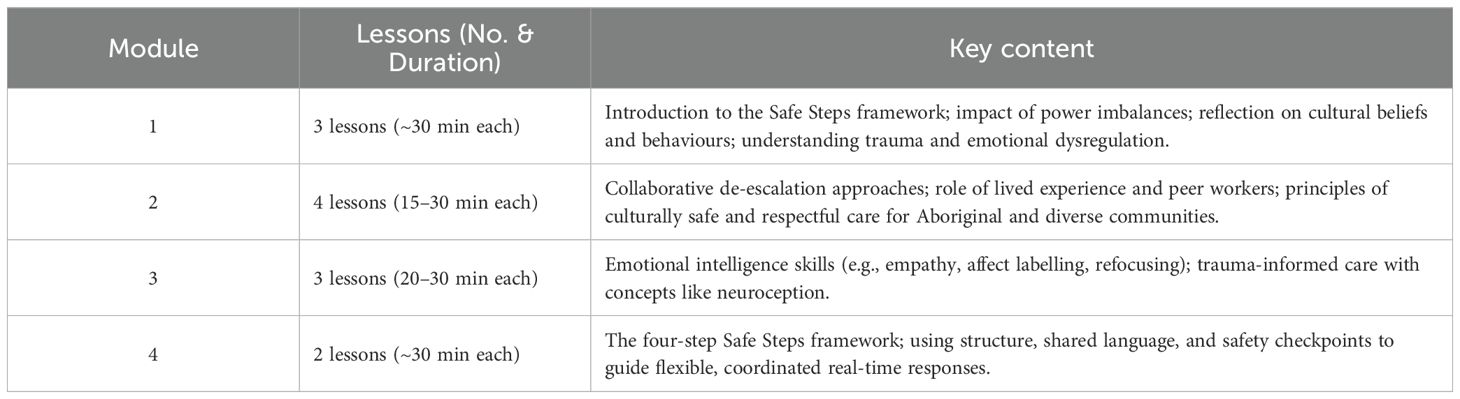
An opt-in approach was followed in the one-year, multi-part implementation, with each participating site deciding its own start date based on readiness and the value of autonomy and self-organisation. Implementation began on the 1st of March 2024 at the first site and concluded on the 15th of April 2025, following the completion of the one-year follow-up at the third site. The baseline period covered the year preceding each site’s implementation start date. After site-specific administrative preparations and train-the-trainer sessions, implementing the Safe Steps into routine practice commenced with in-person training on the four-step approach and complementary online multimedia modules delivered to all participating nursing staff. The online modules, with theoretical texts and diagrams, podcasts-like audios, and short video clips, were co-developed with peer workers, Aboriginal Elders and health leads, and interdisciplinary stakeholders (see Table 1 for the key contents).
A suite of implementation strategies was employed to embed the values emphasised in the Safe Steps into daily working practice, promote the uptake of the steps, and minimise the bias arising from deviation from the intended intervention. Implementation was supported by nurse educators and reinforced through applications of paper posters, pull-up banners, email signature banners, pocket cards on the four-step approach, coffee vouchers, and weekly routine site visits and meetings. All nursing staff were trained to promptly record contemporaneous event-level data through a de-escalation log to minimise recall bias. De-escalation log collection began on the first day of the implementation. Implementation fidelity was tracked once per time point per site, using an adapted observational checklist.
Restrictive practice review meetings were offered to, and received by, nurse participants from the third month of the implementation year, to allow for sufficient log data collection. The reviews were undertaken monthly during the units’ one-hour in-service sessions. Nurse educators used presentation slides on aggregated de-escalation log data to support ongoing reflection, feedback, and learning, focusing on celebrating the nurse participants’ practice of relational capabilities. Word clouds on de-escalation triggers and plots on trends and patterns in log completion, restrictive practices, the Safe Steps, other de-escalation techniques, and co-de-escalation across levels of situational aggression were employed.
Outcomes
Outcomes measured were the rates of total restrictive practice events, the estimates of total restrictive practice durations, and the rates of physical injury events. These were prospectively gathered from routinely maintained administrative datasets, including the incident management system (ims+) for physical injury and Code Black events, electronic medication records (eMeds) for the IM psychotropic administrations, and local unit registers on seclusion and physical restraint events and durations. All seclusion and physical restraint events and durations undergo data checks and cross-referencing with ims+, as part of legally mandated reporting to the Australian National Seclusion and Restraint Database (46). Similarly, all incidents recorded through ims+ are reviewed and flagged for action by service management (47). At the same time, eMeds offers digital oversight associated with fewer medication errors, particularly in rural NSW (48). Routinely collected administrative data for the outcomes were intended to minimise performance and detection bias risks.
Seclusion and physical restraint events and durations were chosen as evaluation outcomes, as they are nationally mandated performance indicators in Australian public acute mental health services (46). Seclusion refers to the act of placing a person alone in a room from which they are unable to leave independently, whereas physical restraint involves staff using their hands or body to restrict a person’s movement (46). On the other hand, Code Black was excluded a priori from hypothesis testing, yet was analysed and reported to support information development (49). As-needed IM psychotropics, while not a formal service performance indicator, were included due to their restrictive nature, particularly given their parenteral route, rapid onset, sedative formulation, and the influence nurses may have on their administration in practice. Sometimes, as-needed IMs are given involuntarily, often in conjunction with physical restraint. Included drug classes in this evaluation were typical and atypical antipsychotics (i.e., droperidol, haloperidol, olanzapine, ziprasidone, zuclopenthixol acetate) and benzodiazepines (i.e., lorazepam and midazolam). The selection of these psychotropics as evaluation outcomes was informed by a review of the academic literature (50–52), clinical inputs, and the participating sites’ guidelines for the care and preliminary sedation requirements of people who present with acute behavioural disturbance. Administration of zuclopenthixol acetate requires psychiatrist approval and was included, given its sedative profile and potential to restrict autonomy (53). Furthermore, nurses also play a role in suggesting or withholding zuclopenthixol acetate use and monitoring its effects after administration (54).
Nurse-recorded de-escalation logs were collected to document incident details (including triggers of the de-escalation), de-escalation contexts (including a clinician-made 6-point situational aggression scale), and de-escalation practices (e.g., the Safe Steps, redirection, sensory modulation; see page 5 in Supplementary Materials for descriptions). These logs were the primary data source for exploring key co-occurring responses contributing to the Safe Steps’ impact, and for describing the administratively recorded sex and mental distress diagnoses of individuals receiving care, who were involved in the de-escalation events. Implementation fidelity was also tracked using an adapted checklist from the Safewards (55). Items 1 to 5 were about the core elements of the Safe Steps in practice, including i) regular reflective practice, ii) nurses’ use of emotional intelligence capabilities, iii) identification and response to early warning signs of emotional distress, troubling behaviours, interpersonal conflict, and potential restrictive practice use, iv) engagement with the structured de-escalation framework, and v) application of de-escalation techniques.
Data analysis
Outcome events and durations were aggregated at the day level to serve as the unit of analysis. Aggregation was intended to support the determination of missing data (55) and imputation for outcomes without a true reference value. No exclusion criteria were applied to the outcome events and durations, provided they occurred within the defined study period. Administrative and log data were anonymised before analysis. The primary analysis excluded the log-derived demographic information of people and nurses involved in de-escalation. To minimise measurement bias, the first author remained blinded to the identities of the people and nurses involved in restrictive practice use and de-escalation events. The authors also held no employment affiliation with any participating sites.
A range of a priori analyses was conducted across three comparison types: i) between-group differences across intervention and control sites before and during the Safe Steps implementation, ii) within-group changes at the implementation sites, and iii) exploratory outcome associations with de-escalation response clusters, determined through a cluster analysis. All quantitative analyses were undertaken using R version 4.2.3 (56) and RStudio version 2023.12.1 + 402 ‘Ocean Storm’ (57), while visuals were plotted through matplotlib version 3.9.3 (58, 59). within JupyterLite version 0.6.3 (60). Hypotheses were tested using incidence rate ratios (IRRs) and model-derived estimates (β) at p <.05. For descriptive reporting, frequencies of events and durations and rates per 1,000 occupied bed days were used. With the guidance on handling missing data for randomised clinical trials (61), missing log data were addressed via multiple imputation through the mice package (62) under both missing at random and missing not at random assumptions.
A priori generalised linear mixed models (GLMMs) were used for between- and within-group comparisons for count-based outcomes (i.e., restrictive practice events, physical injury and Code Black). In contrast, a priori linear models (LMs) were used for continuous outcomes (i.e., restrictive practice duration). Model family selection for GLMMs (i.e., Poisson, negative binomial, or zero-inflated) was informed primarily by outcome distribution characteristics, including tests for over-dispersion and the presence of excess zeros. In instances where residual normality or independence assumptions were violated in the LMs, linear mixed-effects models (LMMs) were applied. A range of a priori random effects was considered in model specification, which included the implementation unit, calendar day, month, year, and study day index. All models underwent diagnostics, including convergence checks and overall model fit indices. The coefficients of determination (R²) were calculated using the delta method (63). Parsimony and explanatory strength were considered in the final selection among competing models (see page 2 in the Supplementary Materials for the final model specifications).
A priori inverse probability weighting (IPW) was applied using the ipw package (64) to address potential baseline imbalance and confounding. A priori covariates in the IPW models included the average harm scores of daily event aggregates, the number of high observation beds, the presence of seclusion rooms, and confounds, i.e., physical restraint and presence of security personnel, summoned during Code Black activations, are interrelated (65). A harm score was used to quantify the average impact severity of the daily aggregate of events (47); its inclusion was informed by a feature analysis that indicated event immediacy as an algorithmically, statistically, and epistemologically important restrictive practice driver (34). The unit without the seclusion room was removed from the weighted comparisons for the seclusion outcome. Relevant guidelines were considered for employing and reporting IPW (42).
To identify the most active co-occurring patterns of nursing de-escalation practices associated with the Safe Steps’ overall impact, a priori hierarchical cluster analysis was conducted on de-escalation log data using Canberra distance, average linkage, silhouette plots, and the cophenetic correlation coefficient (CCC) for determining the optimal clustering solution. These methods are a collection of tools for determining how best to group daily practice event patterns into clusters. Each daily aggregate of events during the implementation year was assigned to one of the emerging clusters. Median values and interquartile ranges were then calculated to describe the emerging clusters. The clusters were then included as fixed effects in GLMM, LM, or LMM models to assess their differential associations with restrictive practice events and duration, physical injuries, and Code Black. Model diagnostics and assumption verifications have been applied to the mixed models. Consistent with the aforementioned guidance for missing data treatment and this evaluation’s published protocol, no sensitivity analyses in relation to multiple imputation of missing log data were undertaken to avoid disrupting the clustering structure underpinning the fixed effect for the mixed modelling subsequent to the cluster analysis.
A priori fidelity assessment was undertaken by counting the conduct of core Safe Steps components across implementation sites. As no established norms exist to define full or partial implementation, higher counts on items 1 to 5 of the adapted checklist were interpreted as indicative of more robust implementation. In comparison, lower counts suggested partial or minimal uptake. Fidelity scores were summarised descriptively.
Results
There was no attrition among participating acute mental health units. Following the services’ check and balance systems, no outcomes from administrative data were considered missing. After a year of implementation, most days had at least one de-escalation log (ndays/Ndays = 324/365; 89%). This response rate equates to 2,955 logs across three implementation sites. When disaggregated into four time points, the response rate was 80% (ndays = 73) at the first time point, 96% (ndays = 87) at the second, 92% (ndays = 84) at the third, and 87% (ndays = 80) at the fourth. Total missing log data (ndays = 41; 11%), excluding demographics, was imputed.
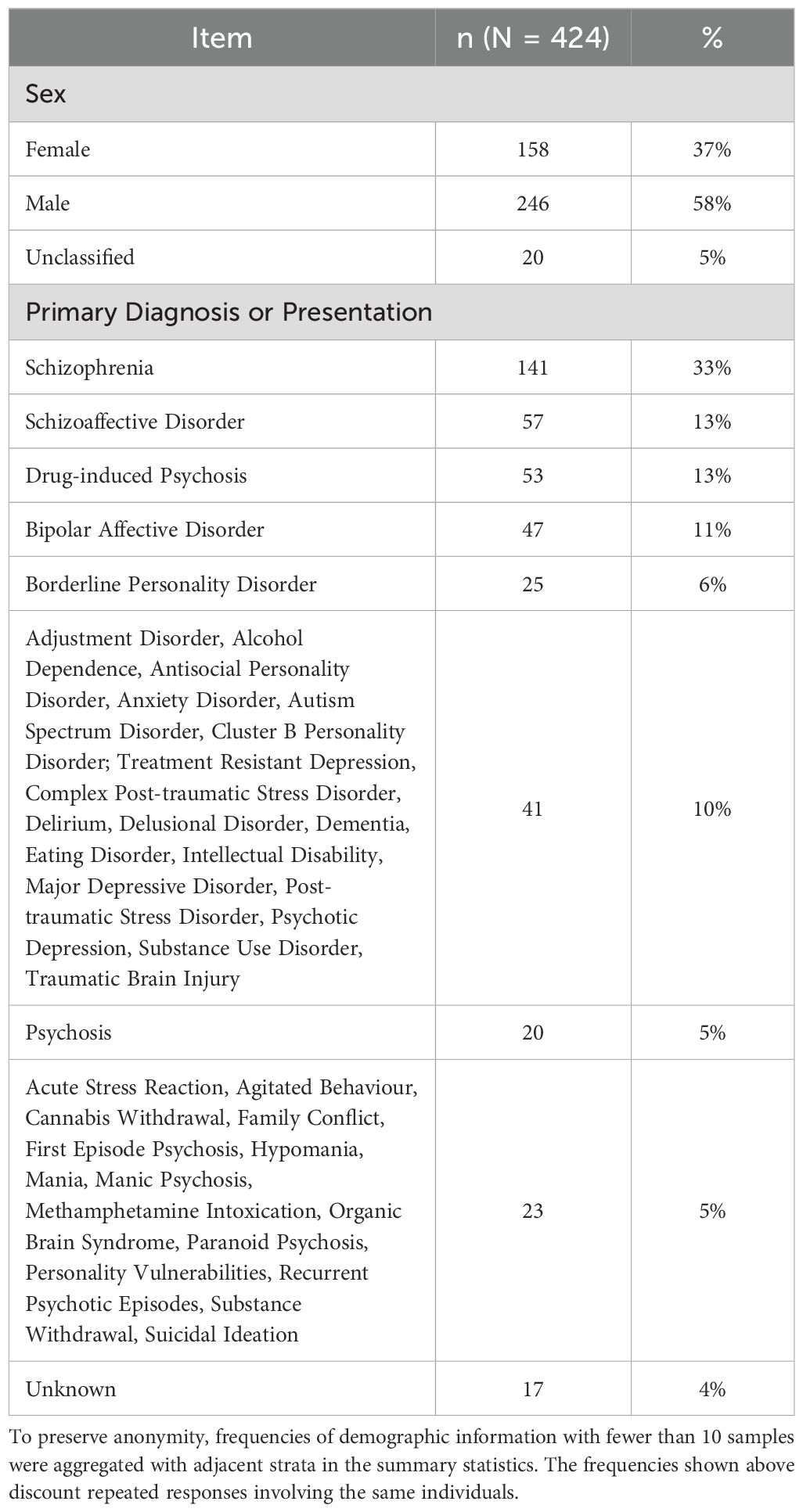
Of the recorded de-escalation events, 81% showed a decrease in situational aggression on a 6-point scale, with an average reduction of 1.20 points. The modal change was a 1-point reduction. Most events on the scale were reported as verbal aggression (level 3; 48%) and agitation (level 2; 30%), with 74% of events directed towards nurses. Discounting repeated responses involving the same individual, de-escalation mainly involved male individuals (58%). In comparison, schizophrenia (33%), schizoaffective disorder (13%), and drug-induced psychosis (13%) were the most common primary diagnoses recorded (see Table 2).
A good covariate balance was achieved on harm scores and the known confounds (i.e., physical restraint to Code Black, and vice versa). However, consistent imbalances were noted for the infrastructure-related covariates (i.e., the presence of a dedicated seclusion room and access to high-observation beds), which showed residual differences after weighting, specifically for between-group comparisons before and during the Safe Steps implementation. Sample sizes after adjustment remained sufficient to support outcome modelling. Love plots for the completed IPW are available on page 3 of the Supplementary Materials.
Between-group comparisons
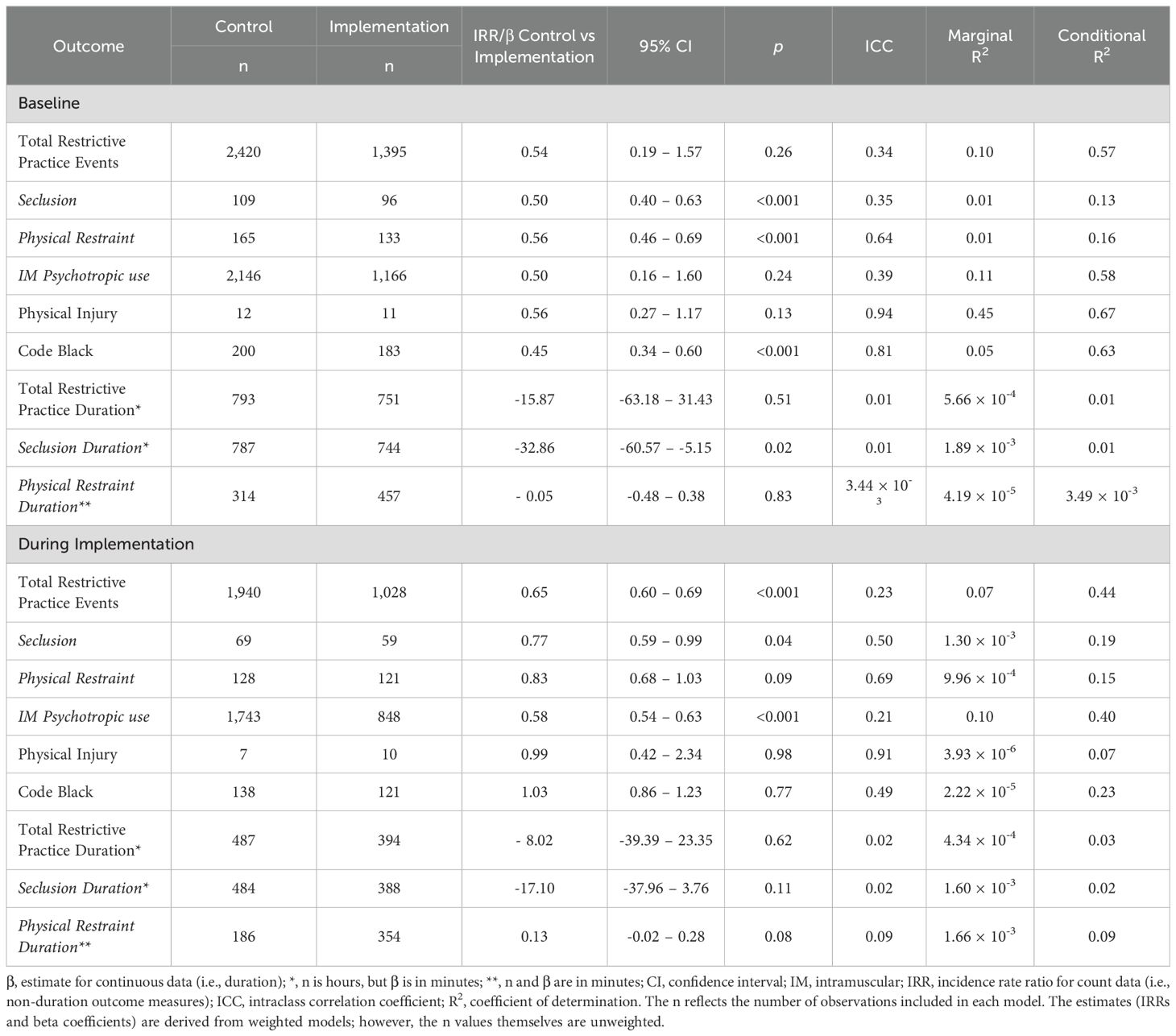
Table 3 shows the IRRs for the intervention effect on event rates and the β for the mean difference in event duration (in minutes) between implementation and control sites at one-year baseline and one-year implementation period. Compared to the control sites, the intervention sites showed during implementation significantly lower rates of seclusion (IRR = 0.77, 95% CI [0.59, 0.99], p = .04), as-needed IM psychotropics (IRR = 0.58, 95% CI [0.54, 0.63], p <.001), and total restrictive practice events (IRR = 0.65, 95% CI [0.60, 0.69], p <.001). There were no significant differences with the other outcome measures; however, most stayed directionally favourable for the implementation sites. Consequently, as the restrictive practice event rate at the implementation sites was significantly lower than the control sites, there is equivocal support for the between-group comparison subset of the hypothesis.
If the comparison was to be extended to the drug classes of as-needed IM psychotropics at a frequency level, the IM antipsychotics (discounting zuclopenthixol acetate) in the implementation sites (n = 307) were 61.2% lower than in the control sites (n = 791). In contrast, the use of IM benzodiazepines in the implementation sites (n = 366) was 59.1% lower than in the control sites (n = 895). When zuclopenthixol acetate was added to the IM antipsychotics, the implementation site recorded 482 administrations, which is 43.2% lower than in the control sites (n = 848).
Within-group comparisons
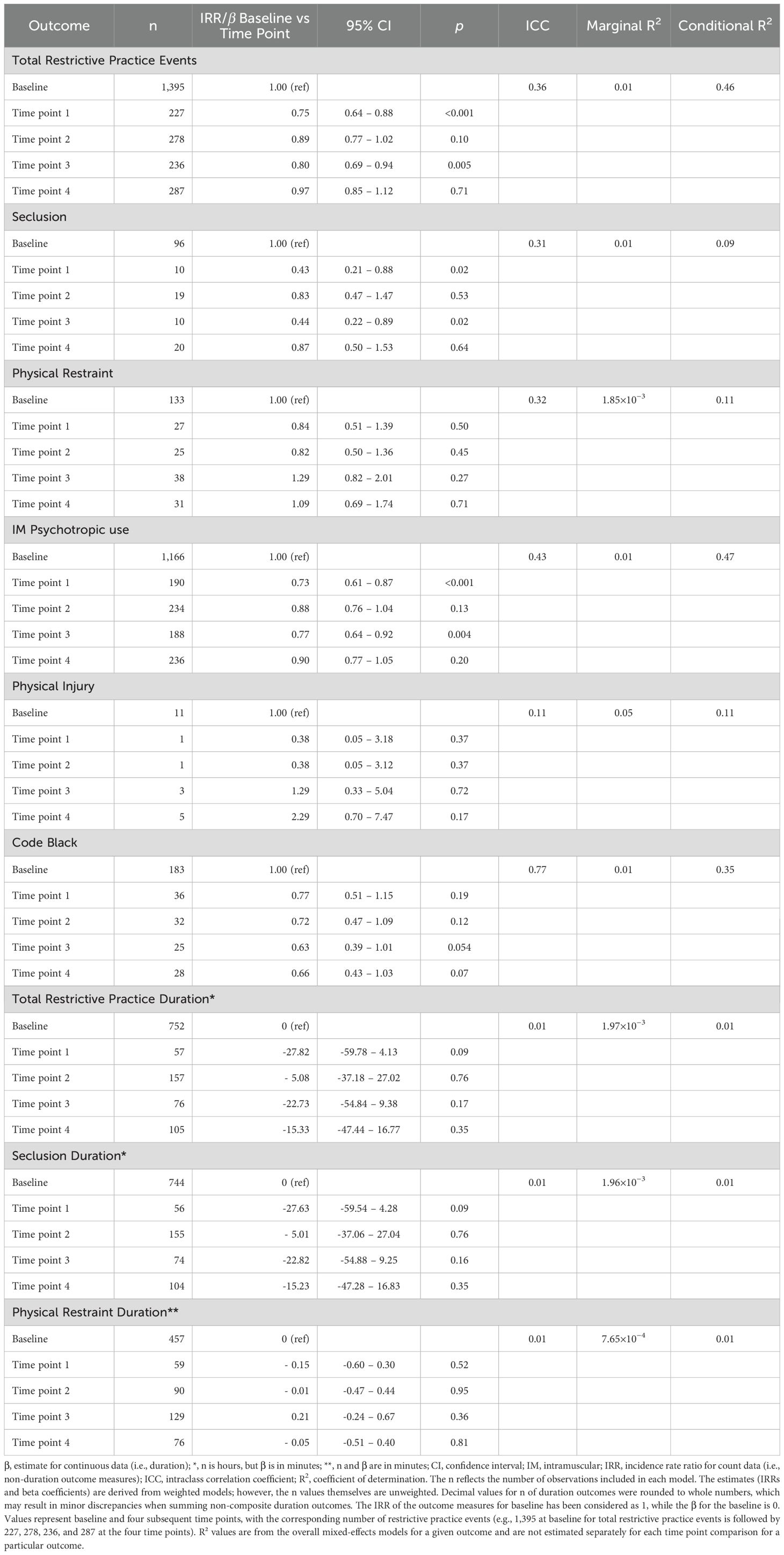
Out of the 36 within-group comparisons (see the number of IRRs and β in Table 4) conducted, six comparisons reached statistical significance. Compared to the one-year baseline, the implementation sites showed significant reductions in seclusion after time points 1 (IRR = 0.43, 95% CI [0.21, 0.88], p = .02) and 3 (IRR = 0.44, 95% CI [0.22, 0.89], p = .02). Significant reductions were also noted in as-needed IM psychotropics at time points 1 (IRR = 0.73, 95% CI [0.61, 0.87], p <.001) and 3 (IRR = 0.77, 95% CI [0.64, 0.92], p = .004), and in total restrictive practice events at time points 1 (IRR = 0.75, 95% CI [0.64, 0.88], p <.001) and 3 (IRR = 0.80, 95% CI [0.69, 0.94], p = .005). For the outcome measures with no significant changes, the directions of the effects were mostly downward. As no significant reductions in outcomes were observed at the fourth time point versus at baseline, the within-group comparison component of the hypothesis is not considered as supported.
Including zuclopenthixol acetate under IM antipsychotics, the total number of antipsychotic administrations across time points 1 to 4 was 482, representing a 28.5% reduction compared to the one-year baseline (n = 674). For IM benzodiazepines, administrations across time points 1 to 4 totalled 366, which is a 25.6% reduction from baseline (n = 492). Excluding zuclopenthixol acetate from the IM antipsychotic category, the implementation sites recorded 307 antipsychotic administrations across time points 1 to 4, being a 39.3% reduction compared to baseline (n = 506).
Cluster analysis and between-cluster comparisons
The silhouette plot showed that two clusters of co-occurring de-escalation practices provided the optimal solution (see page 4 of the Supplementary Materials), which is supported by a CCC of 0.79 that reflects a stable clustering. Consequently, each daily aggregate of log data was assigned a cluster. In 202 days (55%) of the implementation year, nurses responded to prompts of de-escalation through the Safe Steps and a range of co-occurring practices (Cluster 1), including distraction, redirection, change of environment, as-needed oral medication response to behavioural disturbances, and culturally sensitive care (see Figure 1). For the rest of the year, in addition to the co-occurring practices in Cluster 1, nurses also applied one-on-one staff time, reduced stimulus, and music, while using the Safe Steps variably (Cluster 2). Cluster 2 is higher by three total restrictive practice events per 1,000 occupied bed days than Cluster 1, and by 11 hours of total restrictive practice duration per 1,000 occupied bed days (see Table 5). However, the difference between Clusters 2 and 1 on all outcome measures is not statistically significant. At a frequency level, the Safe Steps was used most often at time point 2 of the implementation year, followed by time points 3, 4, and 1.
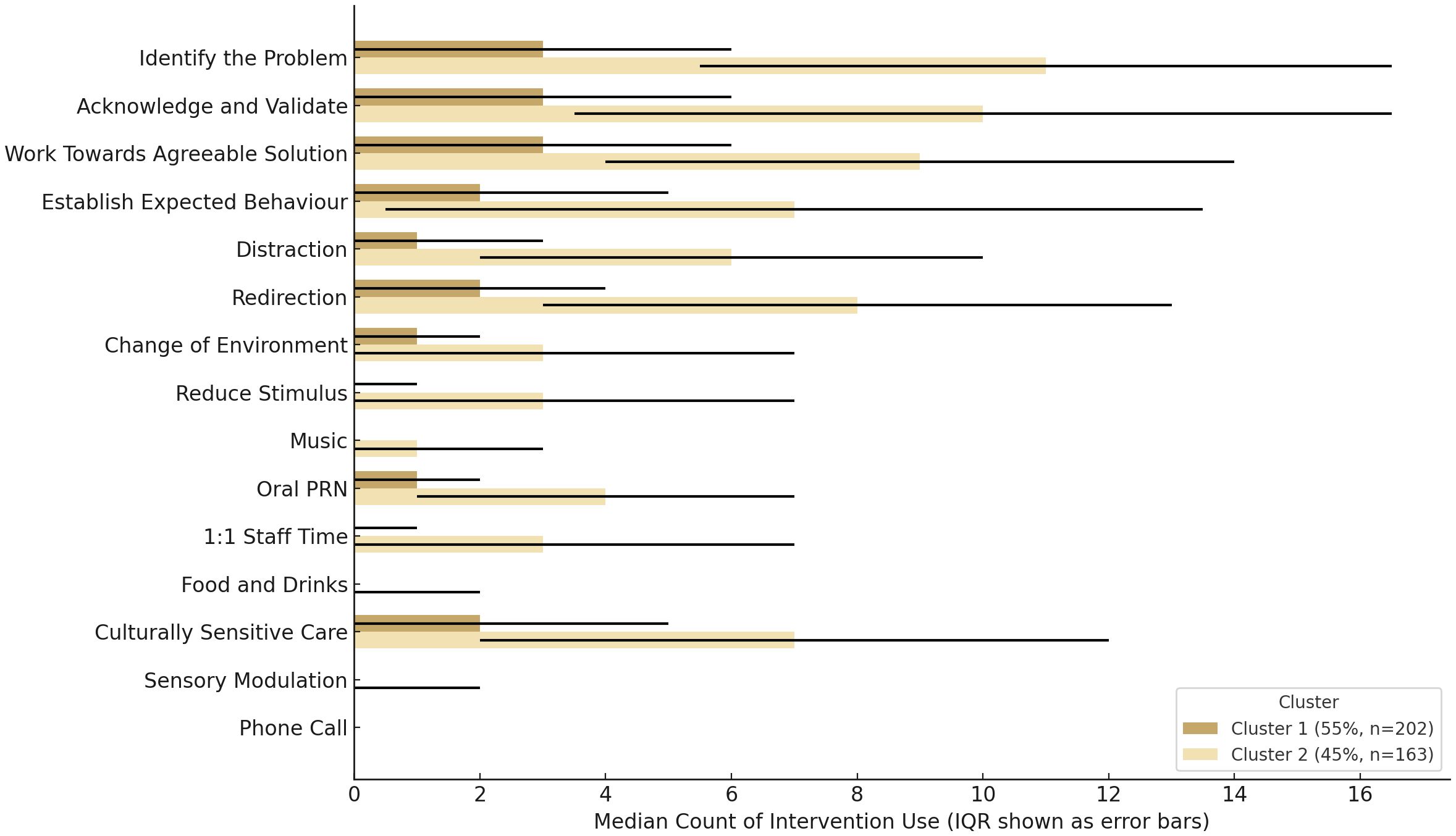
Figure 1. Median and interquartile ranges (IQR) of de-escalation practices across groups of co-occurring responses.
Fidelity checks
Assessment of fidelity to intended intervention was limited, as no checklists were completed during the first and second implementation time points, due to pending ethical approval for the modified checklist, which was obtained towards the end of the second time point. Checklists were then gathered for all three sites at the third and fourth time points, with multiple submissions at some sites (n = 4 for time point three; n = 8 for time point four). All gathered checklists indicated full implementation of the Safe Steps, with all items from 1 to 5 marked as completed.
Discussion
A year-long pragmatic implementation was undertaken across three acute mental health units in NSW, Australia, to assess the impact of the Safe Steps, a structured approach to therapeutic responding aimed at reducing the use of restrictive practices during events of emotional distress, troubling behaviours, and interpersonal conflict. This complex intervention research reflects multidisciplinary collaboration, sustained engagement from nurse participants, and the support of all participating inpatient units, with none withdrawing from the study. This collective effort helped determine the association between the Safe Steps implementation and lower total restrictive practice events, seclusion, and as-needed IM psychotropic use, compared to control sites, as well as other outcomes in which the implementation had no impact.
This evaluation fills several methodological gaps. A recent review on de-escalation training interventions found that much evaluative research was non-randomised, uncontrolled, and at serious risk of selective reporting bias (31). Many lacked preregistered protocols, statistical controls for confounding, blinded outcome analyses, a priori model-based power analyses, and detailed outcome reporting. Only one study examined forced medication, but no significant reduction was observed (66). Recent clustered randomised controlled trials (CRTs) have also narrowly focused on aggression, aggression severity, and physical restraint outcomes (67, 68). Similar concerns are evident in restrictive practice-reduction programmes beyond de-escalation (22, 25), with little attention given to discerning the most active intervention components (21, 69) and anchoring evaluations and implementations in frameworks (27, 70). In contrast, the current evaluation addressed these limitations.
During implementation, intervention sites had lower as-needed IM psychotropic use than controls, with no baseline between-group difference, suggesting the noted change may reflect an intervention-related effect. This finding contributed to the significantly lower total restrictive practice events during implementation, compared to controls. This finding aligns with earlier Safewards studies that included forced medication in the measure of total containment events (45, 55); nonetheless, it is unclear in these earlier studies as to which specific outcome drove the overall impact, making practical interpretations difficult. Beyond the de-escalation focus, hospital-wide interventions (i.e., open door policy and architectural modernisation of facilities) have shown comparable forced medication reductions (71, 72). However, they were without controls and multiple time points that help separate the intervention effect from natural outcome fluctuations. In contrast, this evaluation had four time points that helped identify significant within-group reductions in seclusion, IM use, and total restrictive practice event rates at months three and nine. Interestingly, these improvements contrasted the lack of change in seclusion and forced medication in a CRT for an evidence-based training (73), suggesting the potential positive difference that comes with inpatient-nurse relationship-building approaches like the Safe Steps.
There is a likely untracked increase in other potentially restrictive practices, particularly in as-needed oral medication use. This emergence is possible, given that clinical guidelines routinely recommend as-needed oral medication as an intermediate step between verbal de-escalation and IM sedation (74, 75). However, the cluster analysis findings, expert opinions, and a focus group insight suggest a more nuanced interpretation. Firstly, response clusters showed that, although as-needed oral medication had been used throughout the year, their median values were lower than those of the Safe Steps, suggesting their use may reflect more of an embedded stepped-care practice, rather than over-reliance. Secondly, unlike IM sedation, which is intrusive by virtue of its administration route, as-needed oral medication often involves a degree of choice (76), especially when voluntarily accepted. However, it can be challenging to recognise whether an agitated person’s acceptance of as-needed oral medication is truly voluntary (77), especially when a refusal may lead to an IM administration. Thirdly, a focus group account in the larger study reported that nurses prioritised relational engagement over IM use in containing escalated events. These findings suggest that the Safe Steps implementation did not influence substituting one restrictive practice for another, but may have promoted autonomy-preserving responses. Nevertheless, future studies may consider tracking as-needed oral medication alongside as-needed IM use to strengthen evaluations.
What might explain the positive findings? As seen in the emerged response clusters, the Safe Steps was used throughout the implementation year. This evidence suggests that nurses’ demonstrated relational capabilities could have restructured the unit’s social environment (78). Implementing the Safe Steps could have legitimised proactive relational engagement that reduced response ambiguity in escalated events. As reported in nurse focus groups nested in the larger study, another mechanism could be that repeated de-escalation log use may have improved nurses’ skills in recognising early warning signs of pending coercion. A Norwegian pilot study that included aggression risk assessment training to reduce coercion suggested a similar mechanism (79). Thirdly, as also found through nurse focus groups in the larger study, the four-step approach and the log may have functioned as cues and prompts (80) that reminded nurses of their uptake of relational capabilities. From the first author’s perspective, the Safe Steps likely operated through two mechanisms: instructional guidance through training and performance feedback and encouragement through review meetings (35). While there may have been a multi-part architecture for change behind the Safe Steps implementation, the possibility of reverse causation cannot be excluded. Implementation sites with lower baseline rates of restrictive practices may have been more predisposed to implementing the structured approach to de-escalation, which could have reinforced less coercive responses to escalations. This possibility intersects with the difficulty of detecting floor effects in count data where there are no true reference values. Sites already practicing less coercive de-escalation and have relatively low event rates may have shown limited capacity for further measurable reductions.
Implementing the Safe Steps did not impact restrictive practice durations between and within groups. This finding is similar to that of an earlier randomised control trial in fifty-four German psychiatric units on coercion and violence prevention guidelines (81). Physical injury in this evaluation was also too infrequent for meaningful comparison, and local policies typically influence Code Black activations. External factors during implementation, such as the state-wide industrial actions by nurses and psychiatrists coinciding with the third and fourth research time points and the sporadic organisational restructuring in participating sites, may have dampened change. These factors are difficult to control, similar to the infrastructure-related imbalances seen after applying IPW. Nonetheless, it was a pragmatic decision to control only for specific confounds and covariates, as closing too many potential back doors for a more robust causal pathway (82) could have shifted the evaluation’s focus from the original intention of assessing intervention effectiveness. In addition, adhering to the planned statistical analyses helps prevent potentially spurious results that may arise from questionable measurement practices (83).
The infrastructure-related difference and the relationship between bed profile and restrictive practice use are not straightforward issues. In Victoria, Australia, elevated restrictive practice rates have been attributed to higher thresholds for acute mental health service access (84), rather than bed profile. By contrast, the introduction of high observation units in Ireland coincided with a reduction in restrictive practices (85). There is also support for the link between physical design features (i.e., more private space, greater level of comfort, and greater visibility on the unit) and reduced risk of seclusion in psychiatric and forensic units within the Netherlands (86). In terms of intervention evaluations, it is uncommon for evidence syntheses to detail matching methods used in primary evaluation studies in the field (38), with some researchers noting that their control groups were ‘matched’ to service type (87), rather than bed profile. This service type matching is still valuable, although high-observation areas share features with secure services, where restrictive practices are more systematically embedded (88). Indeed, selecting controls for intervention evaluation is complex (89). However, if the relationship to be privileged is that high-observation areas are linked to higher restrictive practice use (34, 90), then it is notable that nurses in the implementation sites with high observation beds may have responded less coercively to a larger number of, and arguably more challenging, escalations there, suggesting the robustness of this evaluation’s between-group comparison findings.
The cluster analysis showed that Cluster 1, with no one-on-one staff time but consistent Safe Steps use, had lower restrictive practice rates per 1,000 bed days than Cluster 2, which included one-on-ones and more variable Safe Steps use. With the assumption that de-escalation is a form of brief psychotherapeutic intervention, these findings softly challenge the widely-held yet empirically under-explored view that uniform responding may be linked to increased aggression and consequent restrictive practice use (91) and that individual characteristics can moderate psychotherapy outcomes (92). This interpretation is supported by discharged patient interviews from the larger study, where therapeutic connections were said to form even in brief 5–10-minute interactions, when nurses offer genuine, relatable moments. Nurse focus groups from the larger study also revealed how understaffing could have led to random nurse assignments for one-on-one time, which may have been experienced as lacking in relational continuity or even coercive. On the other hand, there is a potential for social desirability bias in log completion, specifically concerning the uniform Safe Steps use in Cluster 1. This bias may be low, given the limited personal benefit from the task expressed by several nurse focus group participants from the larger study. Distortion in self-reports is more commonly observed in high-stakes contexts, such as compensation assessments, where impression management is driven by external incentives (93). Nonetheless, there is a notable absence of comparable tools for detecting ‘faking good’ in de-escalation logs that can support verifying such bias; thus, its presence remains open to question.
Limitations
There is a limitation in the fidelity checks. None were completed during the first and second time points. However, the de-escalation log completion rates remained high across all the implementation quarters, suggesting that the Safe Steps were actively deployed when fidelity was not checked. Also, excessive fidelity monitoring in reflective practice-based interventions may be counterproductive, as nurses may feel monitored for performance review, which can undermine the psychological safety needed for honest change. In contrast, many successful restrictive practice-reduction interventions were said to depend on giving staff the latitude to exercise their authentic voice (23, 94). This reasoning indicates that making intervention values explicit, rather than imposing compliance, could support staff to move from rewards passivity (where staff receive approval for compliance) towards empowerment, where approval to work towards the agreed values is unnecessary.
The Safe Steps evaluation has further limitations. No demographics were statistically modelled, although such modelling was not pre-specified in the evaluation’s protocol. Since the unit of analysis was at the daily aggregate level, and restrictive practices are often rare and zero-inflated, case-mix adjustment would be fragile without large, balanced subgroups (95), making this demographic modelling omission methodologically justified. Administratively recorded sex was in binary terms, which offers limited clinical relevance in a time of increasing recognition for gender diversity (96). Many administratively recorded mental distress diagnoses were not uniformly classified through standard codes, which limits reliable reporting. Nonetheless, summary data indicated that the sex and diagnostic profiles of individuals were broadly consistent with national patterns among people admitted involuntarily to Australian public acute mental health units (4), supporting the generalisability of the evaluation outcomes to similar service contexts. Nurses’ demographics were excluded to protect anonymity, as required in the obtained ethical approvals. High Australian mental health workforce turnover (97) also complicates longitudinal demographic tracking. Moreover, since mental health nursing is not a protected title in Australia (98), that is, anyone could use the ‘mental health nurse’ designation, regardless of actual educational qualifications or professional competence, a heterogeneous mix of nurse participants likely implemented the Safe Steps, which could reflect typical acute inpatient staffing.
Conclusion
The Safe Steps evaluation needs to be replicated. The intervention emerged bottom-up, with components co-designed with peer workers, Aboriginal Elders, cultural health leads, and cross-disciplinary professionals. There were a preregistered protocol, a priori model-based power analyses, and a sufficiently powered sample, representative of Australian acute mental units. Valid and reliable outcomes, verified through institutional reporting, were tracked over multiple time points, enabling detection of emergent outcomes. Independent cultural and clinical oversight was present. Blinded statistical analyses were undertaken. An implementation and evaluation framework was used, change mechanisms were proposed, nurses’ therapeutic responses were made visible, and a significantly lower as-needed IM psychotropics rate in implementation sites versus controls was found. This lower rate in as-needed IM psychotropic use may reflect a shift toward less coercive practices that reduce trauma and support autonomy, as such interventions are often experienced as disempowering and violent (99). Although IPW was applied and could be considered to have strengthened the plausibility of a causal interpretation, as discussed throughout, chance and some form of biases remain possible. Nonetheless, as the evaluation addresses key evidence gaps, independent replication is needed to strengthen confidence in its findings.
Data availability statement
The datasets presented in this article are not readily available, because of the conditions of the Human Research Ethics Committee approvals obtained. Requests to access the datasets should be directed to aHVtYW4uZXRoaWNzQHNjdS5lZHUuYXU=.
Ethics statement
This study involving humans was approved by a human research ethics committee (HREC) in an LHD within NSW, Australia (2023/PID00297 - 2023/ETH00272) in March 2023. In May 2023, further ethical approval was received from a university HREC through the minimisation of duplication of ethical review application (Approval Number: 2023/069). This study was conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin, because no identifiable data were collected or re-identifiable. Nurses’ completion of de-escalation logs was considered implied consent, with no nurse identifiers recorded. Approval was granted to report aggregate sex and diagnosis data for people involved in de-escalation. Identifiable details were collected only to support log completion, then removed by a project team member not involved in the analysis. A random study code replaced identifiers before data were shared with the first author, who remained blinded to participant identities.
Author contributions
ED: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – original draft. JY: Resources, Writing – review & editing. RL: Resources, Writing – review & editing. MH: Conceptualization, Funding acquisition, Methodology, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. Southern Cross University and the Translational Research Grant Scheme from the NSW Office for Health and Medical Research.
Acknowledgments
This evaluation is part of a research project with input from multiple research and implementation partners, including representatives from participating services in respective local health districts, the NSW Ministry of Health, the State mental health branch, the State’s lead organisation supporting safety and quality enhancements in health systems, the state-wide service that streamlines care pathways for culturally and linguistically diverse individuals, local Aboriginal Elders and cultural health leads, and individuals with lived experience of mental distress, mental health service use, and coercive engagement with mental health services. Their valuable contributions are gratefully acknowledged, as well as those from the participating nurses and acute mental health units. Special thanks are extended to Alison Taylor, Matthew Flowers, and Leo Waterhouse for their support of the project. Most importantly, the individuals whose recorded restrictive practice experiences underpin this evaluation are acknowledged. Their identities are unknown to the authors, although their data represent real needs that call for less coercive and more compassionate approaches to inpatient care.
Conflict of interest
Esario IV Daguman is supported by a PhD scholarship jointly funded by Southern Cross University and the Translational Research Grant Scheme of the NSW Office for Health and Medical Research. One funding body provided feedback during the initial protocol development to enhance the study’s scientific rigour. Neither organisation had any role in the original conceptualisation, study conduct, data gathering, data analysis, interpretation, reporting, or manuscript preparation. The views expressed are solely those of the authors and do not necessarily reflect those of the funding bodies, the authors’ affiliated organisations, or the research and implementation partners associated with the broader project in which this paper is embedded.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1676743/full#supplementary-material
References
1. Accinni T, Papadogiannis G, and Orso L. De-escalation techniques in various settings. In: Biondi M, Pasquini M, and Tarsitani L, editors. Empathy, normalization and de-escalation: Management of the agitated patient in emergency and critical situations. Springer International Publishing, Cham (2021). p. 65–91.
2. Lavelle M, Ferreira AL, Dixen S, and Berring LL. De-escalation in mental health care settings. In: Hallett N, Whittington R, Richter D, and Eneje E, editors. Coercion and violence in mental health settings: Causes, consequences, management. Springer Nature Switzerland, Cham (2024). p. 331–56.
3. Sheridan Rains L, Zenina T, Dias MC, Jones R, Jeffreys S, Branthonne-Foster S, et al. Variations in patterns of involuntary hospitalisation and in legal frameworks: An international comparative study. Lancet Psychiatry. (2019) 6:403–17. doi: 10.1016/s2215-0366(19)30090-2, PMID: 30954479
4. AIHW. Involuntary treatment - mental health - AIHW canberra, ACT, Australia (2024). Available online at: https://www.aihw.gov.au/mental-health/topic-areas/involuntary-treatment (Accessed July 30, 2025).
5. Stubbe DE. Psychiatric emergencies: Empowering connections to de-escalate aggression. FOCUS. (2023) 21:54–7. doi: 10.1176/appi.focus.20220079, PMID: 37205026
6. Hurley J, Lakeman R, Moxham L, Foster K, Hazelton M, and Happell B. Under prepared for practice: A qualitative study of mental health nurse undergraduate workforce preparation in Australia. Issues Ment Health Nurs. (2024) 45:1–7. doi: 10.1080/01612840.2024.2354385, PMID: 38901029
7. Warrender D, Connell C, Jones E, Monteux S, Colwell L, Laker C, et al. Mental health deserves better: Resisting the dilution of specialist pre-registration mental health nurse education in the United Kingdom. Int J Ment Health Nursing. (2024) 33:202–12. doi: 10.1111/inm.13236, PMID: 37788130
8. Lakeman R, Foster K, Hazelton M, Roper C, and Hurley J. Helpful encounters with mental health nurses in Australia: A survey of service users and their supporters. J Psychiatr Ment Health Nursing. (2022) 30:515–25. doi: 10.1111/jpm.12887, PMID: 36440476
9. Wong S and Müller A. Nurses’ use of pro re nata medication in adult acute mental healthcare settings: An integrative review. Int J Ment Health Nursing. (2023) 32:1243–58. doi: 10.1111/inm.13148, PMID: 37025073
10. Paradis-Gagné E, Pelosse D, Pariseau-Legault P, Brisebois L, and Cader M. Nurses’ Experiences of using coercion in forensic and non-forensic settings: A constant comparative analysis. J Psychiatr Ment Health Nurs. (2025) 32. doi: 10.1111/jpm.13159, PMID: 39991967
11. Belayneh Z, Chavulak J, Lee D-CA, Petrakis M, and Haines TP. Prevalence and variability of restrictive care practice use (physical restraint, seclusion and chemical restraint) in adult mental health inpatient settings: A systematic review and meta-analysis. J Clin Nursing. (2024) 33:1256–81. doi: 10.1111/jocn.17041, PMID: 38304928
12. Molloy L, Beckett P, Chidarikire S, Cutler N, Isobel S, Murphy G, et al. Mental health nurses’ Enforcement of involuntary care in inpatient settings: A meta-ethnography. Int J Ment Health Nursing. (2025) 34:e70044. doi: 10.1111/inm.70044, PMID: 40346428
13. NSW Government. Seclusion and restraint in NSW health settings policy manual. New South Wales, Australia: NSW Government (2020). Available online at: https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2020_004.pdf (Accessed July 30, 2025).
14. NICE. Quality statement 2: preventing and managing violent or aggressive behaviour | Violent and aggressive behaviours in people with mental health problems | Quality standards. In: NICE. National Institute for Health and Care Excellence, Niceorguk (2017). Available online at: https://www.nice.org.uk/guidance/qs154/chapter/quality-statement-2-preventing-and-managing-violent-or-aggressive-behaviour (Accessed July 30, 2025).
15. SAMHSA. National behavioral health crisis care guidance | SAMHSA publications and digital products. Samhsagov: Substance Abuse and Mental Health Services Administration (2025). Available online at: https://library.samhsa.gov/product/national-behavioral-health-crisis-care-guidance/pep24-01-037 (Accessed July 30, 2025).
16. Gill N, Drew N, Rodrigues M, Muhsen H, Morales Cano G, Savage M, et al. Bringing together the World Health Organization’s Quality Rights initiative and the World Psychiatric Association’s programme on implementing alternatives to coercion in mental healthcare: A common goal for action. BJPsych Open. (2024) 10:e23. doi: 10.1192/bjo.2023.622, PMID: 38179597
17. Schimmels J, Beeber L, Delaney KR, Hauenstein E, DeSanto Iennaco J, Sharp D, et al. Expanding the five urgent recommendations: Advancing workplace safety in healthcare settings. J Am Psychiatr Nurses Assoc. (2025) 0:10783903251348948. doi: 10.1177/10783903251348948, PMID: 40667703
18. Snipe J and Searby A. Elimination of restrictive interventions: Is it achievable under the current mental healthcare landscape? Int J Ment Health Nursing. (2023) 32:1178–1185. doi: 10.1111/inm.13180, PMID: 37278366
19. Barbui C, Purgato M, Abdulmalik J, Caldas-de-Almeida JM, Eaton J, Gureje O, et al. Efficacy of interventions to reduce coercive treatment in mental health services: Umbrella review of randomised evidence. Br J Psychiatry. (2020) 218:1–11. doi: 10.1192/bjp.2020.144, PMID: 32847633
20. Hammervold UE, Norvoll R, Aas RW, and Sagvaag H. Post-incident review after restraint in mental health care -a potential for knowledge development, recovery promotion and restraint prevention. A scoping review. BMC Health Serv Res. (2019) 19:235. doi: 10.1186/s12913-019-4060-y, PMID: 31014331
21. Finch K, Lawrence D, Williams MO, Thompson AR, and Hartwright C. A systematic review of the effectiveness of Safewards: Has enthusiasm exceeded evidence? Issues Ment Health Nurs. (2021) 43:1–18. doi: 10.1080/01612840.2021.1967533, PMID: 34534037
22. Ward-Stockham K, Kapp S, Jarden R, Gerdtz M, and Daniel C. Effect of Safewards on reducing conflict and containment and the experiences of staff and consumers: A mixed-methods systematic review. Int J Ment Health Nursing. (2022) 31:199–221. doi: 10.1111/inm.12950, PMID: 34773348
23. Saunders KRK, McGuinness E, Barnett P, Foye U, Sears J, Carlisle S, et al. A scoping review of trauma informed approaches in acute, crisis, emergency, and residential mental health care. BMC Psychiatry. (2023) 23:567. doi: 10.1186/s12888-023-05016-z, PMID: 37550650
24. Ngune I, Myers H, Cole A, Palamara P, Redknap R, Roche M, et al. Developing nurse-sensitive outcomes in acute inpatient mental health settings—A systematic review. J Clin Nurs. (2023) 32:6254–67. doi: 10.1111/jocn.16679, PMID: 36915223
25. Quinn M, Jutkowitz E, Primack J, Lenger K, Rudolph J, Trikalinos T, et al. Protocols to reduce seclusion in inpatient mental health units. Int J Ment Health Nursing. (2024) 33:600–15. doi: 10.1111/inm.13277, PMID: 38193620
26. Abraham J, Hirt J, Kamm F, and Möhler R. Interventions to reduce physical restraints in general hospital settings: A scoping review of components and characteristics. J Clin Nurs. (2020) 29:3183–200. doi: 10.1111/jocn.15381, PMID: 32558091
27. Lantta T, Duxbury J, Haines-Delmont A, Björkdahl A, Husum TL, Lickiewicz J, et al. Models, frameworks and theories in the implementation of programs targeted to reduce formal coercion in mental health settings: A systematic review. Front Psychiatry. (2023) 14:1158145. doi: 10.3389/fpsyt.2023.1158145, PMID: 37398581
28. Brierley-Jones L, Ramsey L, Canvin K, Kendal S, and Baker J. To what extent are patients involved in researching safety in acute mental healthcare? Res Involvement Engagement. (2022) 8:8. doi: 10.1186/s40900-022-00337-x, PMID: 35227330
29. Gooding P, McSherry B, and Roper C. Preventing and reducing “Coercion” in mental health services: An international scoping review of english-language studies. Acta Psychiatrica Scandinavica. (2020) 142:27–39. doi: 10.1111/acps.13152, PMID: 31953847
30. Leach B, Leach B, Gloinson E, Gloinson E, Sutherland A, Sutherland A, et al. Reviewing the evidence base for de-escalation training. Randorg. (2019). doi: 10.7249/RR3148
31. Price, Papastavrou Brooks C, Johnston I, McPherson P, Goodman H, Grundy A, et al. Development and evaluation of a de-escalation training intervention in adult acute and forensic units: The EDITION systematic review and feasibility trial. Health Technol Assess. (2024) 28:1–120. doi: 10.3310/fggw6874, PMID: 38343036
32. NSW Health MNCLHD. Mid north coast local health district safety and quality account (2020). Available online at: https://mnclhd.health.nsw.gov.au/wp-content/uploads/MNCLHDSafetyandQualityAccount2020Digital-VersionFINAL-1.pdf (Accessed July 30, 2025).
33. Daguman EI, Taylor A, Flowers M, Lakeman R, and Hutchinson M. Differentiating therapeutic responses that reduce restrictive practice use and situational aggression in an acute mental health unit. J Clin Nurs. (2025) 34:4698–4709. doi: 10.1111/jocn.17727, PMID: 40084814
34. Daguman EI, Taylor A, Flowers M, Lakeman R, and Hutchinson M. Drivers of seclusion and physical restraint in an acute mental health unit: A feature analysis. Issues Ment Health Nurs. (2025) 46:937–947. doi: 10.1080/01612840.2025.2538705, PMID: 40911824
35. Daguman EI, Taylor A, Flowers M, Lakeman R, and Hutchinson M. Outcomes of restrictive practice review meetings in an acute mental health unit: A retrospective before-and-after study. Int J Ment Health Nursing. (2025) 34. doi: 10.1111/inm.70059, PMID: 40346442
36. Dolan S, Nowell L, and McCaffrey G. Pragmatism as a philosophical foundation to integrate education, practice, research and policy across the nursing profession. J Advanced Nursing. (2022) 78:e118–e29. doi: 10.1111/jan.15373, PMID: 35854667
37. Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. BMJ. (2021) 374:n2061. doi: 10.1136/bmj.n2061, PMID: 34593508
38. Daguman EI, Hutchinson M, and Lakeman R. Uncovering complexities in reducing aggression, conflict and restrictive practices in acute mental healthcare settings: an overview of reviews. Int J Ment Health Nursing. (2024) 33:1666–86. doi: 10.1111/inm.13376, PMID: 38886873
39. Thompson DS, Fazio X, Kustra E, Patrick L, and Stanley D. Scoping review of complexity theory in health services research. BMC Health Serv Res. (2016) 16:87. doi: 10.1186/s12913-016-1343-4, PMID: 26968157
40. Daguman EI, Taylor A, Flowers M, Owen D, Wilson A, Lakeman R, et al. Evaluating the Safe Steps for De-escalation: A protocol for a mixed concurrent control study in acute mental health units. PloS One. (2025) 20:e0325558. doi: 10.1371/journal.pone.0325558, PMID: 40460134
41. NSW Government. Local health districts. New South Wales, Australia: NSW Government (2022). Available online at: https://www.nsw.gov.au/departments-and-agencies/nsw-health/local-health-districts (Accessed July 30, 2025).
42. Bettega F, Mendelson M, Leyrat C, and Bailly S. Use and reporting of inverse-probability-of-treatment weighting for multicategory treatments in medical research: a systematic review. J Clin Epidemiol. (2024) 2024. doi: 10.1016/j.jclinepi.2024.111338, PMID: 38556101
43. Green P, MacLeod C, and Alday P. Simr: Power analysis for generalised linear mixed models by simulation. In: R-packages (2023). Available online at: https://cran.r-project.org/web/packages/simr/index.html (Accessed July 30, 2025).
44. Muir-Cochrane E, Muller A, Fu Y, and Oster C. Role of security guards in Code Black events in medical and surgical settings: A retrospective chart audit. Nurs Health Sci. (2020) 22:758–68. doi: 10.1111/nhs.12725, PMID: 32314506
45. Dickens GL, Tabvuma T, and Frost SA. Safewards: Changes in conflict, containment, and violence prevention climate during implementation. Int J Ment Health Nursing. (2020) 29:1230–1240. doi: 10.1111/inm.12762, PMID: 32691495
46. AIHW. Seclusion and restraint - Mental health - AIHW. Canberra, Australian Capital Territory, Australia: Australian Institute of Health and Welfare (2024). Available online at: https://www.aihw.gov.au/mental-health/topic-areas/seclusion-and-restraint (Accessed July 30, 2025).
47. NSW Health. Incident management New South Wales, Australia (2020). Available online at: https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2020_047.pdf (Accessed July 30, 2025).
48. NSW Health. Digitally Improving quality, Safety and Effectiveness of Medication Management in NSW | Digital NSW. New South Wales, Australia: Nswgovau (2019). Available online at: https://www.digital.nsw.gov.au/article/digitally-improving-quality-safety-and-effectiveness-of-medication-management-nsw (Accessed July 30, 2025).
49. NMHPSC. Key performance indicators for Australian public mental health services. In: Commonwealth of Australia Canberra, Australian Capital Territory, Australia: National Mental Health Performance Subcommittee (2013). Available online at: https://www.aihw.gov.au/getmedia/f9bb1a07-a43b-458a-9b73-64ef19d8aedd/Key-Performance-Indicators-for-Australian-Public-Mental-Health-Services-Third-Edition.pdf.aspx (Accessed July 30, 2025).
50. Humble F and Berk M. Pharmacological management of aggression and violence. Hum Psychopharmacology: Clin Experimental. (2003) 18:423–36. doi: 10.1002/hup.504, PMID: 12923820
51. Vellar K, Khalid U, and Coleman M. Quality improvement through audit: Zuclopenthixol acetate prescribing, monitoring and patient outcomes in a regional health service. Australas Psychiatry. (2023) 31:27–33. doi: 10.1177/10398562231154311, PMID: 36772936
52. Jayakody K, Gibson RC, Kumar A, and Gunadasa S. Zuclopenthixol acetate for acute schizophrenia and similar serious mental illnesses. Cochrane Database Systematic Rev. (2012) 4). doi: 10.1002/14651858.CD000525.pub3, PMID: 22513898
53. Fitzgerald P. Long-acting antipsychotic medication, restraint and treatment in the management of acute psychosis. Aust New Z J Psychiatry. (1999) 33:660–6. doi: 10.1080/j.1440-1614.1999.00627.x, PMID: 10544989
54. Barnes CW, Alderton D, and Castle D. The development of clinical guidelines for the use of zuclopenthixol acetate. Australas Psychiatry. (2002) 10:54–8. doi: 10.1046/j.1440-1665.2002.00397.x
55. Bowers L, James K, Quirk A, Simpson A, Stewart D, and Hodsoll J. Reducing conflict and containment rates on acute psychiatric wards: The Safewards cluster randomised controlled trial. Int J Nurs Stud. (2015) 52:1412–22. doi: 10.1016/j.ijnurstu.2015.05.001, PMID: 26166187
56. R Core Team. R: A language and environment for statistical computing. 4.2.3 ed. Vienna, Austria: R Foundation for Statistical Computing (2023).
58. Hunter JD. Matplotlib: A 2D graphics environment. Computing Sci engineering. (2007) 9:90–5. doi: 10.1109/MCSE.2007.55
60. Project Jupyter. JupyterLite (2021). Available online at: https://jupyter.org/try-jupyter/lab/ (Accessed July 30, 2025).
61. Jakobsen JC, Gluud C, Wetterslev J, and Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials - A practical guide with flowcharts. BMC Med Res Methodology. (2017) 17:162. doi: 10.1186/s12874-017-0442-1, PMID: 29207961
62. van Buuren S and Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J Stat Software. (2011) 45:1–67. doi: 10.18637/jss.v045.i03
63. Nakagawa S, Johnson PCD, and Schielzeth H. The coefficient of determination R2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. J R Soc Interface. (2017) 14:20170213. doi: 10.1098/rsif.2017.0213, PMID: 28904005
64. van der Wal WM and Geskus RB. ipw: an R package for inverse probability weighting. J Stat Software. (2011) 43:1–23. doi: 10.18637/jss.v043.i13
65. Bowers L, van der Merwe M, Paterson B, and Stewart D. Manual restraint and shows of force: The City-128 study. Int J Ment Health Nursing. (2012) 21:30–40. doi: 10.1111/j.1447-0349.2011.00756.x, PMID: 21733054
66. Laker C, Gray R, and Flach C. Case study evaluating the impact of de-escalation and physical intervention training. J Psychiatr Ment Health Nursing. (2010) 17:222–8. doi: 10.1111/j.1365-2850.2009.01496.x, PMID: 20465771
67. Celofiga A, Kores Plesnicar B, Koprivsek J, Moskon M, Benkovic D, and Gregoric Kumperscak H. Effectiveness of de-escalation in reducing aggression and coercion in acute psychiatric units. A Cluster Randomized Study. Front Psychiatry. (2022) 13:856153. doi: 10.3389/fpsyt.2022.856153, PMID: 35463507
68. Ye J, Xia Z, Wang C, Liao Y, Xu Y, Zhang Y, et al. Effectiveness of CRSCE-based de-escalation training on reducing physical restraint in psychiatric hospitals: A cluster randomized controlled trial. Front Psychiatry. (2021) 12:576662. doi: 10.3389/fpsyt.2021.576662, PMID: 33679467
69. Gaynes BN, Brown CL, Lux LJ, Brownley KA, Van Dorn RA, Edlund MJ, et al. Preventing and de-escalating aggressive behavior among adult psychiatric patients: A systematic review of the evidence. Psychiatr Services. (2017) 68:819–31. doi: 10.1176/appi.ps.201600314, PMID: 28412887
70. Björkdahl A, Johansson U, Kjellin L, and Pelto-Piri V. Barriers and enablers to the implementation of Safewards and the alignment to the i-PARIHS framework – A qualitative systematic review. Int J Ment Health Nursing. (2024) 33:18–36. doi: 10.1111/inm.13222, PMID: 37705298
71. Rohe T, Dresler T, Stuhlinger M, Weber M, Strittmatter T, and Fallgatter AJ. Bauliche Modernisierungen in psychiatrischen Kliniken beeinflussen Zwangsmaßnahmen. Der Nervenarzt. (2017) 88:70–7. doi: 10.1007/s00115-015-0054-0, PMID: 26820456
72. Hochstrasser L, Fröhlich D, Schneeberger AR, Borgwardt S, Lang UE, Stieglitz RD, et al. Long-term reduction of seclusion and forced medication on a hospital-wide level: Implementation of an open-door policy over 6 years. Eur Psychiatry. (2018) 48:51–7. doi: 10.1016/j.eurpsy.2017.09.008, PMID: 29331599
73. Välimäki M, Lantta T, Anttila M, Vahlberg T, Normand S-L, and Yang M. An evidence-based educational intervention for reducing coercive measures in psychiatric hospitals: A randomized clinical trial. JAMA Network Open. (2022) 5:e2229076–e. doi: 10.1001/jamanetworkopen.2022.29076, PMID: 36040740
74. Patel MX, Sethi FN, Barnes TR, Dix R, Dratcu L, Fox B, et al. Joint BAP NAPICU evidence-based consensus guidelines for the clinical management of acute disturbance: De-escalation and rapid tranquillisation. J Psychopharmacology. (2018) 32:601–40. doi: 10.1177/0269881118776738, PMID: 29882463
75. NSW Government Agency for Clinical Innovation. Management of patients with acute severe behavioural disturbance in emergency departments. In: Agency for clinical innovation New South Wales, Australia: NSW Health (2015). Available online at: https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2015_007.pdf (Accessed July 30, 2025).
76. Curry A, Malas N, Mroczkowski M, Hong V, Nordstrom K, and Terrell C. Updates in the assessment and management of agitation. Focus. (2023) 21:35–45. doi: 10.1176/appi.focus.20220064, PMID: 37205032
77. Muir-Cochrane E. A wicked problem: Chemical restraint: Towards a definition. Int J Ment Health Nursing. (2020) 29:1272–4. doi: 10.1111/inm.12780, PMID: 32888233
78. Baker J, Berzins K, Canvin K, Benson I, Kellar I, Wright J, et al. Non-pharmacological interventions to reduce restrictive practices in adult mental health inpatient settings: The COMPARE systematic mapping review. Health Serv Delivery Res. (2021) 9:1–184. doi: 10.3310/hsdr09050, PMID: 33651527
79. Rognmo A and Bugge E. A pilot study of MAP – a program for handling of aggressive behaviour in psychiatric wards. An evaluation of mediating mechanisms. BMC Med Education. (2025) 25:630. doi: 10.1186/s12909-025-07083-0, PMID: 40301824
80. Abraham C and Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. (2008) 27:379–87. doi: 10.1037/0278-6133.27.3.379, PMID: 18624603
81. Steinert T, Baumgardt J, Bechdolf A, Bühling-Schindowski F, Cole C, Flammer E, et al. Implementation of guidelines on prevention of coercion and violence (PreVCo) in psychiatry: A multicentre randomised controlled trial. Lancet Regional Health – Europe. (2023) 35. doi: 10.1016/j.lanepe.2023.100770, PMID: 38058297
82. Huntington-Klein N. The effect: An introduction to research design and causality | The effect. New York: Chapman and Hall/CRC (2021). Available online at: https://theeffectbook.net/index.html (Accessed July 30, 2025).
83. Daguman EI and Taylor JE. An evaluation of the Opening Minds Scale for Health Care Providers. Stigma Health. (2025). doi: 10.1037/sah0000628
84. Fletcher J. Safewards in Victoria: A mixed methods, real-world evaluation of process, impacts, and outcomes. Melbourne, Victoria, Australia: The University of Melbourne (2021).
85. O’Donoghue J and Young M. Impact of a high observation ward on seclusion and restraint episodes. Irish J Psychol Med. (2024) 41:159–60. doi: 10.1017/ipm.2022.42, PMID: 36081189
86. van der Schaaf PS, Dusseldorp E, Keuning FM, Janssen WA, and Noorthoorn EO. Impact of the physical environment of psychiatric wards on the use of seclusion. Br J Psychiatry. (2013) 202:142–9. doi: 10.1192/bjp.bp.112.118422, PMID: 23307922
87. Fletcher J, Spittal M, Brophy L, Tibble H, Kinner S, Elsom S, et al. Outcomes of the Victorian Safewards trial in 13 wards: Impact on seclusion rates and fidelity measurement. Int J Ment Health Nursing. (2017) 26:461–71. doi: 10.1111/inm.12380, PMID: 28960739
88. Lawrence D, Davies JL, Mills S, and Watt A. Differences between restrictive practices applied to men and women in UK secure mental health services. J Forensic Psychiatry Psychol. (2025) 36:602–20. doi: 10.1080/14789949.2025.2507008
89. Hirsch S and Steinert T. Measures to avoid coercion in psychiatry and their efficacy. Deutsches Aerzteblatt Online. (2019) 116:336–343. doi: 10.3238/arztebl.2019.0336, PMID: 31288909
90. Oster C, Gerace A, Thomson D, and Muir-Cochrane E. Seclusion and restraint use in adult inpatient mental health care: An Australian perspective. Collegian. (2016) 23:183–90. doi: 10.1016/j.colegn.2015.03.006
91. Montreuil M, Thibeault C, McHarg L, and Carnevale FA. Children’s moral experiences of crisis management in a child mental health setting. Int J Ment Health Nursing. (2018) 27:1440–8. doi: 10.1111/inm.12444, PMID: 29446553
92. Furukawa TA, Karyotaki E, Suganuma A, Pompoli A, Ostinelli EG, Cipriani A, et al. Dismantling, personalising and optimising internet cognitive–behavioural therapy for depression: A study protocol for individual participant data component network meta-analysis. BMJ Open. (2018) 8:e026137. doi: 10.1136/bmjopen-2018-026137, PMID: 30798295
93. Yoxall J, Bahr M, and O’Neill T. Faking bad in workers compensation psychological assessments: elevation rates of negative distortion scales on the personality assessment inventory in an Australian sample. Psychiatry Psychol Law. (2017) 24:682–93. doi: 10.1080/13218719.2017.1291295, PMID: 31983982
94. Mullen A, Browne G, Hamilton B, Skinner S, and Happell B. Safewards: An integrative review of the literature within inpatient and forensic mental health units. Int J Ment Health Nursing. (2022) 31:1090–1108. doi: 10.1111/inm.13001, PMID: 35365947
95. King G and Zeng L. Logistic regression in rare events data. Political Analysis. (2001) 9:137–63. doi: 10.1093/oxfordjournals.pan.a004868
96. Gualtierotti R. Bridging the gap: Time to integrate sex and gender differences into research and clinical practice for improved health outcomes. Eur J Internal Med. (2025) 134:9–16. doi: 10.1016/j.ejim.2025.01.030, PMID: 39915168
97. Haywood D, Crocker KM, Gnatt I, Jenkins Z, Bhat R, Lalitha ARN, et al. What accounts for turnover intention in the Australian public mental health workforce? Int J Ment Health Nurs. (2024) 33:359–68. doi: 10.1111/inm.13233, PMID: 37795874
98. Lakeman R, Foster K, Happell B, Hazelton M, Moxham L, and Hurley J. Informing the development of a fit-for-purpose mental health nursing curriculum: A survey of mental health nurse academics in Australia. Int J Ment Health Nursing. (2024) 33:93–103. doi: 10.1111/inm.13226, PMID: 37705299
Keywords: de-escalation, psychiatric nursing, mental health services, coercion, psychiatric hospital, intervention evaluation
Citation: Daguman EIV, Yoxall J, Lakeman R and Hutchinson M (2025) Maximising relational capabilities and minimising restrictive practices in acute mental health units: the Safe Steps for De-escalation evaluation. Front. Psychiatry 16:1676743. doi: 10.3389/fpsyt.2025.1676743
Received: 31 July 2025; Accepted: 25 September 2025;
Published: 06 November 2025.
Edited by:
Tilman Steinert, ZfP Südwürttemberg, GermanyReviewed by:
Keith Reid, Tyne and Wear NHS Foundation Trust, United KingdomAndrew Watt, Cardiff Metropolitan University, United Kingdom
Copyright © 2025 Daguman, Yoxall, Lakeman and Hutchinson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Esario IV Daguman, ZS5kYWd1bWFuLjEwQHN0dWRlbnQuc2N1LmVkdS5hdQ==
 Esario IV Daguman
Esario IV Daguman Jacqui Yoxall2
Jacqui Yoxall2 Marie Hutchinson
Marie Hutchinson