- 1School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran
- 2Clinical Neurology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
- 3Student Research Committee, Bushehr University of Medical Sciences, Bushehr, Iran
- 4Department of Physical Therapy and Kinesiology, University of Massachusetts Lowell, Lowell, MA, United States
- 5Department of Neurology, Epilepsy Center Frankfurt Rhein-Main, University Medicine Frankfurt, Goethe University Frankfurt, Frankfurt, Germany
- 6Department of Psychology, University of Bath, Bath, United Kingdom
Background: Multiple sclerosis (MS) is a chronic disease of the central nervous system, most commonly affecting individuals in early adulthood. Uncertainty about future relapses and accumulating disability may lead to significant psychological distress, contributing to reduced quality of life.
Objective: This systematic scoping review aimed to synthesize current evidence on the prevalence, determinants, and consequences of fear of relapse and disease progression in people living with MS.
Method: The current systematic scoping review followed PRISMA-ScR guidelines. PubMed, Scopus, and Web of Science were searched from inception until October 6th. Original, English-language studies investigating fear of disease progression or relapse among people with multiple sclerosis were included, without restrictions on age, gender, disease stage, or study design. Data items were collected, and a quality assessment was conducted.
Results: Our search yielded 43 studies, of which 13 met the eligibility criteria. Nine studies utilized the fear of relapse scale and the remaining four used the fear of progression questionnaire. Fear of progression among MS patients ranged from minimal to severe, with concerns centered on losing independence, relying on external help, and potential medication side effects. In relapsing-remitting MS, fear was particularly associated with uncertainty about disease course, potential disability, and worsening fatigue. Increased fear of relapse and progression was strongly associated with higher levels of fatigue, depression, stress, health anxiety, and lower quality of life.
Conclusion: Fear of relapse and progression is common and significantly impacts the lives of people with MS. Future research should focus on evaluating and implementing tailored interventions — including psychological support, educational initiatives, and coping-based strategies — to help patients manage these fears.
1 Introduction
Multiple sclerosis (MS) is a chronic autoimmune disease of the central nervous system where immune cells attack the myelin sheath covering neurons (1). Globally, it is estimated that about 1.89 million people are living with MS, with more than 62,000 new cases diagnosed in 2021. The global prevalence is approximately 23.9 per 100,000 population, and this figure has shown a steady increase over the past three decades, reflecting both improved detection and a rising disease burden (2). MS typical onset is between 20–30 years of age and MS predominantly affects females compared to males [3:1 ratio] (3). Common symptoms include fatigue, visual disturbances, pain, and sensorimotor deficits (4). However, the disease course is highly variable. Some individuals experience long periods of remission with minimal symptoms, while others develop severe and progressive disability (5). The phenotype of the disease also varies between patients with the majority (85%) having the relapse remitting form (RRMS) followed by the primary progressive (PPMS) and the secondary progressive (SPMS) form (6). A relapse involves a flare-up of existing symptoms or the development of new ones during a phase of acute disease activity that lasts for over 24 hours that significantly alters a patients physical and/or mental health (7–9). Beyond its physical manifestations, MS has a profound psychological impact. Uncertainty about disease prognosis and the severity of future relapses often leads to significant fear of progression (10). This fear of progression (11) is related to distress, depression, generalized anxiety disorder, and reduced cognitive functioning (12) and adversely impacts quality of life (13, 14). Anxiety is common in people with MS, and fear is a central component of the anxious thoughts experienced by patients with chronic illnesses (15, 16). Due to the substantial contribution of fear of relapse and disease progression to the quality of life of people with MS, a systematical investigation of existing evidence offers critical insights into the prevalence, associated factors, and impacts of this fear in individuals with MS. However, despite growing recognition of its importance, recent studies remain fragmented, often focusing on anxiety or quality of life more broadly rather than specifically addressing fear of relapse and progression as a distinct construct. Moreover, there is no comprehensive synthesis of the literature that examines its prevalence, determinants, and consequences in one place.
While fear of disease progression has been explored extensively in other chronic illnesses such as cancer (17), it remains relatively underexamined in the context of MS.
To our knowledge, this is the first systematic review to address the burden of fear of relapse and disease progression in MS. Understanding how fear of disease relapse and progression affects quality of life can inform future tailored interventions for over 2.8 million people living with MS worldwide (18). This systematic scoping review summarizes the current literature on the prevalence, risk factors associated with fear of relapse/progression, and its impact on the lives of individuals with MS.
2 Materials and methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines (19).
2.1 Search strategy
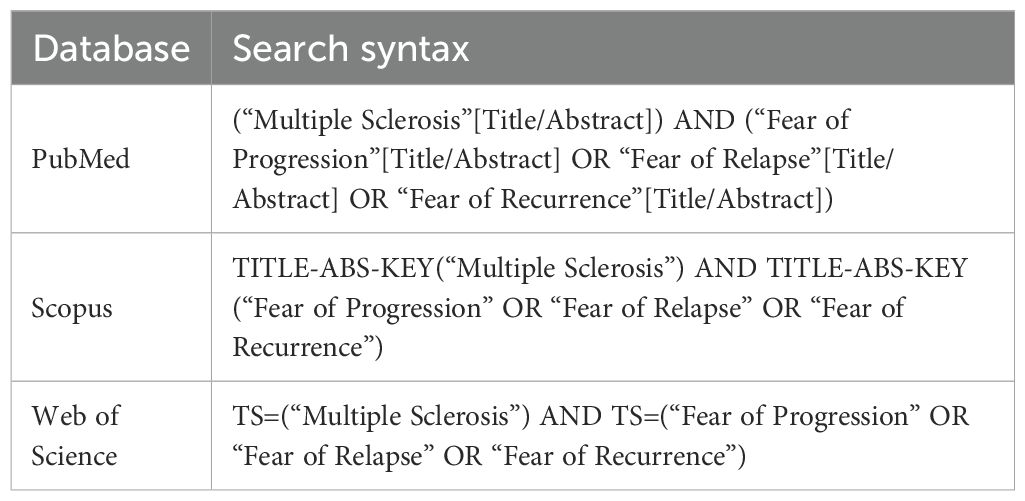
We conducted a systematic search across three major databases—PubMed, Web of Science, and Scopus from inception through October 6, 2024. The search strategy was designed to capture studies focusing on fear of progression or relapse among patients with MS. The keywords used to conduct this search were: (Multiple Sclerosis) AND (“Fear of Progression” OR “Fear of Relapse” OR “Fear of Recurrence”). The search syntax for each database is provided in Table 1.
All retrieved articles were imported into EndNote version 9 reference management software. Duplicates were identified and removed using the software’s automated deduplication feature, followed by manual verification to ensure accuracy.
2.2 Eligibility criteria
Any original paper investigating fear of progression or relapse among MS patients was considered eligible. Non-original, non-English and non-related papers were excluded from the review. The eligible studies were chosen following the PICO framework, which defines the population, independent variable, and outcome criteria (20).
o Population: People living with MS. No limitations regarding age, gender, disease severity, and the time of onset or diagnosis were considered.
o Intervention/Exposure: Fear of disease progression or relapse.
o Comparator: No limitations were considered regarding the presence of a control group.
o Outcome: Prevalence of fear and Quality of life, and any mental or physical health-related outcome measures.
Additionally, we examined risk factors for fear of relapse/progression among people living with multiple sclerosis and interventions that can mediate this fear.
2.3 Study selection
The lead (AM) and second author (TF), independently conducted an initial screening of the papers by reviewing the titles and abstracts, removed the duplicates, and identified relevant studies. Next, they (AM and TF) independently reviewed the full texts of the articles and assessed for eligibility based on the predefined inclusion and exclusion criteria. Collaborative discussion took place in case of a disagreement in inclusion of the studies until consensus was reached. If disagreements persisted, a third author (MFK) was consulted to provide a final decision.
2.4 Data extraction
The following data were extracted from each included article using Microsoft Excel (2022, version 16.62 for macOS/Windows): Senior author, publication date, country, design, scales of exposure, study subjects and their main characteristics (age, gender, type, severity of MS), main findings, and limitations. A data extraction form, designed by the lead author (AM), was utilized to ensure consistency and standardization. The form was explained to all authors for clarity prior to data collection. Two authors (AM, TF) independently extracted data from each study. To ensure accuracy, the independently extracted data were compared and discrepancies were collaboratively resolved through discussion.
2.5 Assessment of study quality
The risk of bias in the included studies was evaluated using the Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields by Kmet et al. (21). This tool offers distinct guidelines for assessing the quality of quantitative and qualitative studies. For this systematic review, only the quantitative assessment framework was applied, which consists of 14 specific criteria designed to evaluate the internal validity of studies by minimizing potential biases in their design, execution, and analysis.
Each criterion was rated based on predefined guidelines: “Yes” (score of 2), “Partial” (score of 1), “No” (score of 0), or “Not Applicable” (excluded from the calculation). These scores were then measured to produce a composite quality score for each study, ranging from 0 to 1.0, where scores above 0.75 are typically considered high quality (21, 22). All quality assessments were performed through a double-coding process to ensure reliability, with discrepancies resolved by consensus. Full guideline on the risk of bias method can be found https://ualberta.scholaris.ca/items/b8ff8755-6efb-4fb2-941a-def0d418fd07.
2.6 Analysis
Due to the heterogeneity of the methods, scales, and outcomes investigated in the included studies, a meta-analysis was not feasible. Thematic analysis was performed using Braun and Clarkes 6 phase thematic analysis method (23). This method involves systematically identifying, organizing, and interpreting patterns or themes within qualitative data. Two authors (AM, TF) generated the themes after familiarization with the data of the 13 studies included in this review.
The examined themes include: Scales utilized to assess fear of relapse/progression, Prevalence of fear of relapse/progression, Risk factors of fearing relapse/progression, Consequences of fear on patients’ lives, and Mediators of fear of relapse/progression.
3 Results
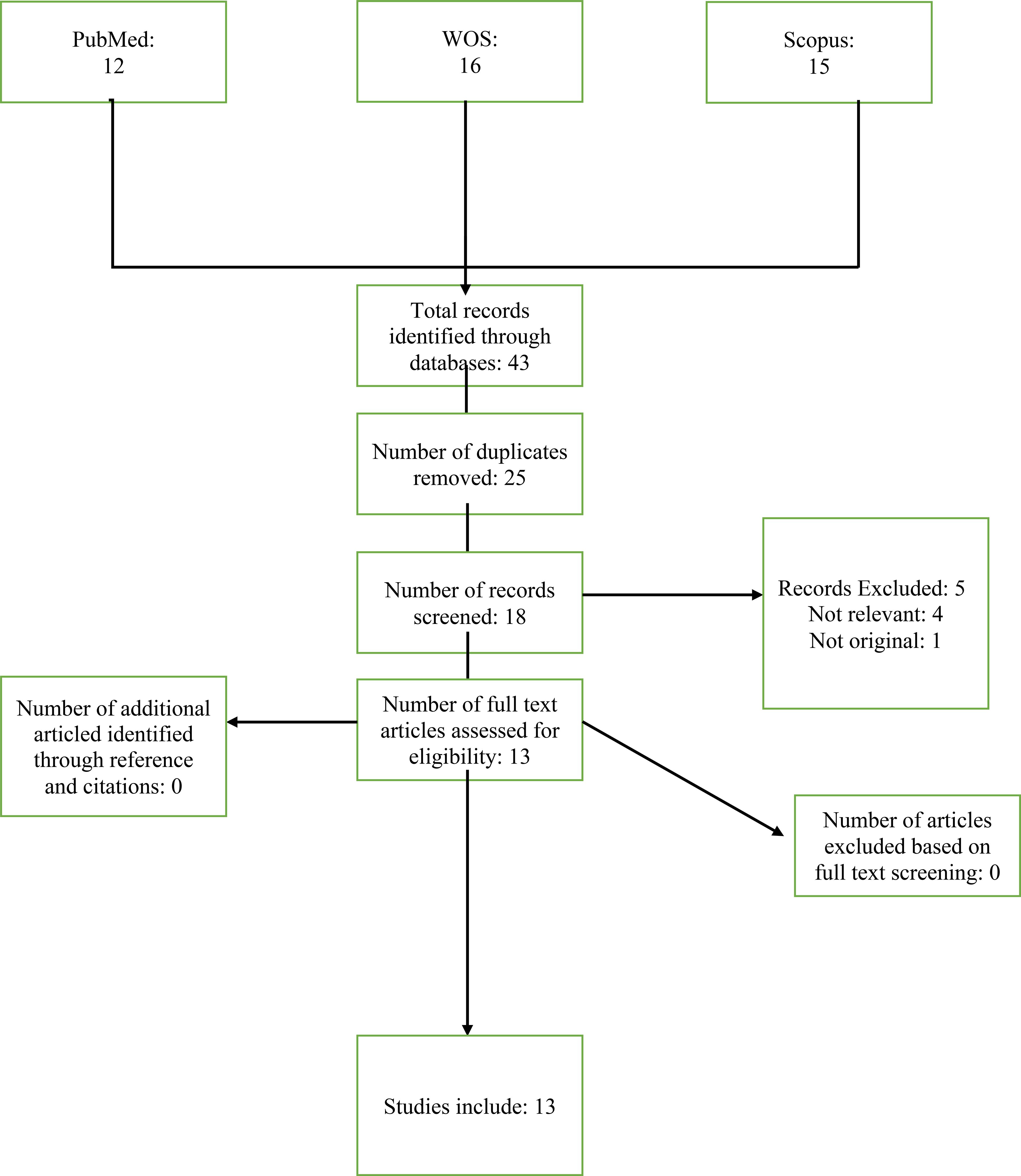
Our search strategy yielded 43 studies (Figure 1). After removing duplicates (n=25) and screening the titles, abstracts, and full-text articles, 13 studies met the eligibility criteria of this systematic scoping review (10, 14, 24–34). Full details of excluded studies, including titles, authors, and reasons for exclusion, are provided in the Supplementary Table 1.
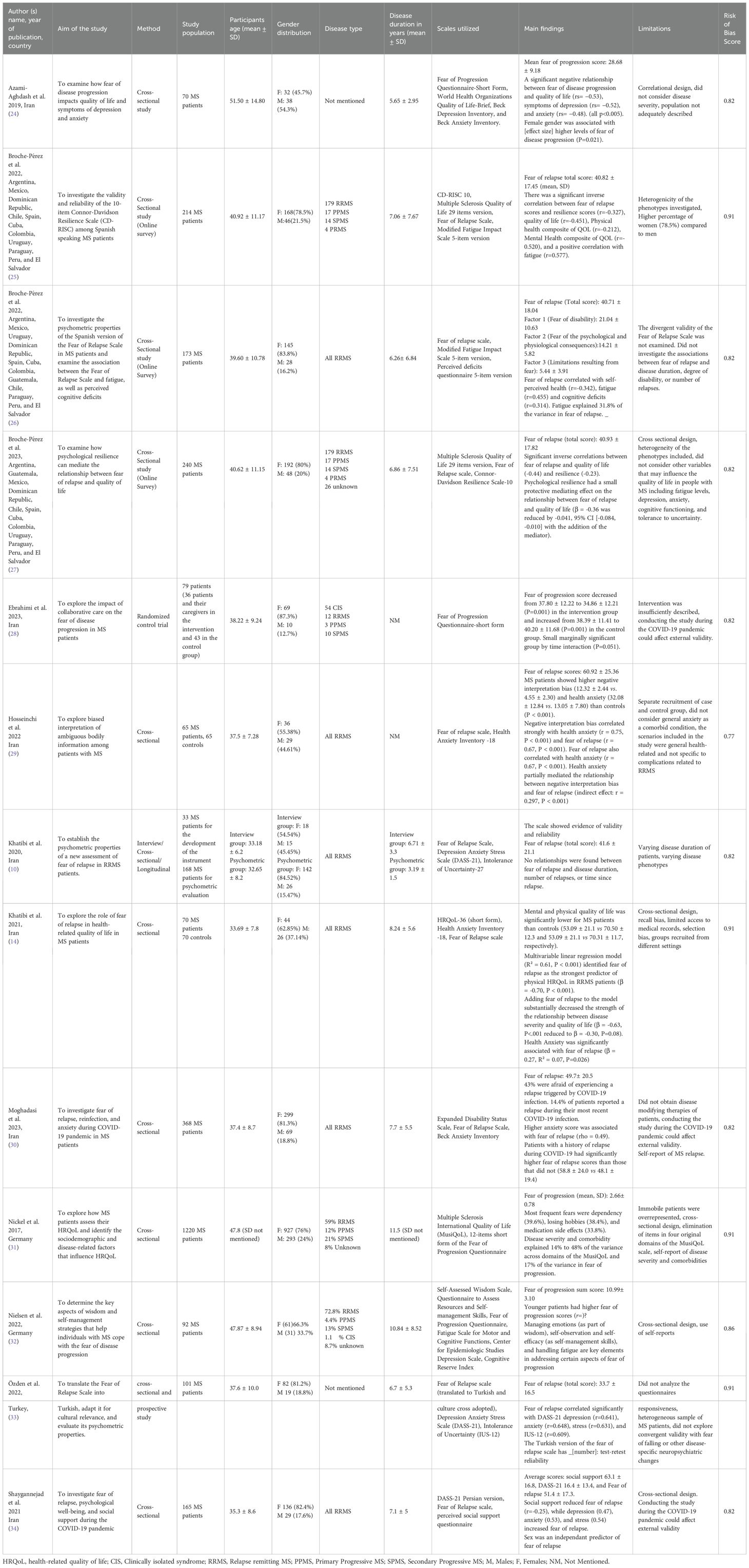
All included studies scored above the conservative threshold of 0.75, indicating high methodological quality with minimal risk of bias (Table 2).
3.1 Study features
Characteristics of the included studies are demonstrated in Table 2. Papers published between 2017 to 2023 and were conducted Argentina, Mexico, Dominican Republic, Chile, Spain, Cuba, Colombia, Uruguay, Paraguay, Peru, El Salvador, Iran, Turkey, and Germany. Of the 3058 individuals enrolled across all studies, 76.88% were women and 23.11% were men. Mean age of the participants in the studies ranged from 33.18 to 51.5 years old.
3.2 Scales utilized to assess fear of MS progression/relapse
The Fear of Relapse Scale developed by Khatibi et al. in 2020 (10) was employed by 9 out of the 13 studies included in this review (10, 14, 25–27, 29, 30, 33, 34). This scale has been validated in multiple languages, including English, Persian, Turkish, and Spanish (10, 26, 33). The Fear of Relapse Scale comprises 26 items categorized into three dimensions: Fear of disability following a relapse (13 items), Fear of the psychological and physical effects of a relapse (8 items), and Limitations due to fear (5 items). Each item is rated on a five-point Likert scale, ranging from 0 (never) to 4 (always). The scale has demonstrated strong psychometric properties, including a high internal consistency (Cronbach’s alpha = 0.92) and reliability (test-retest correlation = 0.74).
One study utilized the Fear of Progression Questionnaire, a 43-item self-report tool designed to assess fears related to disease progression across five subscales: affective reaction, partnership/family, occupation, loss of autonomy, and anxiety coping. Responses are rated on a five-point Likert scale (32). This scale is validated and widely used to study the impact of many different diseases, including MS, diabetes, and cancer and has shown high internal consistency (Cronbach’s alpha = 0.95) and high test-retest reliability over one week (rtt = 0.94) (11, 32, 35). The remaining three studies (24, 28, 31) utilized a shorter 12-item version of the Fear of Progression Questionnaire, which offers a more concise assessment of these same five dimensions. The scale’s reliability (Cronbach’s α > 0.7) and validity (coefficients ranging from 0.77 to 0.94) has been established. (28, 36).
3.3 Fear of progression
The four studies that examined fear of disease progression using the Fear of Progression Questionnaire (or its short form) revealed significant variability in levels of concern between individuals. One study that used the full form of the questionnaire reported that 18.4% of patients had low fear of progression, 61.9% moderate fear, and 19.6% dysfunctional levels of fear (32). The remaining three studies that utilized the short form of the Fear of Progression Questionnaire demonstrated that a significant proportion of patients expressed concerns about the progression of their disease (24, 28, 31). The most commonly reported fear was reliance on external help for daily activities, with nearly 40% of participants indicating they often or very often experienced this fear, followed by fear of inability to pursue hobbies and potential harm from medication (31).
3.4 Fear of relapse
The Fear of Relapse Scale, specifically designed for Relapsing-Remitting MS (RRMS) populations, consistently highlighted significant concerns among patients. The total mean fear of relapse scores ranged between 33.7 ± 16.5 (33) in Turkish-speaking patients to 60.92 ± 25.36 in studies conducted in Iran (29), with variability observed across geographic and linguistic groups. Turkish-speaking patients demonstrated the lowest scores (33.7 ± 16.5), reflecting generally mild to moderate levels of concern. Scores from Spanish-speaking countries ranged narrowly from 40.71± 18.04 to 40.93 ± 17.82 (25–27). Studies from Iran revealed a broader range of higher scores of 41.6± 21.1 (10), 49.7± 20.5 (30), 51.4± 17.3 (34), and 60.92± 25.36 (29), reflective of mild to very high levels of concern. Spanish-speaking MS patients reported a higher level of concern about psychological and physiological consequences (mean score per item: 1.78) compared to their concern about the risk of disability (mean score per item: 1.62) or limitations due to fear (mean score per item: 1.09) (26). Iranian MS patients (10) most feared worsening fatigue and the psychological impact of receiving grave news.
3.5 Risk factors of fear of relapse/progression
Two demographic factors were identified as significant contributors to fear of relapse or disease progression in patients with MS. Women were found to experience higher levels of fear of disease progression compared to men (24), with sex being identified as an independent predictor of this fear (34). Younger patients also reported higher fear of progression (32).
The relationship between disease characteristics and fear of relapse was less consistent. While no correlation was found between fear of relapse and disease duration, number of relapses, or time since the last relapse (10), weak associations suggested that fear of progression might increase slightly with comorbid conditions and decrease with longer disease duration (31).
Psychological factors played a significant role in predicting fear of relapse or progression. Fear of relapse was strongly associated with biased interpretations of ambiguous bodily information (29) (r = 0.75) and with perceived cognitive deficits (r=0.314), suggesting that negative cognitive biases might amplify fears about future relapses. Intolerance of uncertainty, which measures people’s reaction to uncertainties in life (37), was another factor that independently correlated with fear of relapse (10, 33) (r= 0.52, r=0.61, respectively). Fatigue also emerged as a critical factor influencing fear of relapse (r=0.455, β=0.318) (26). Higher fatigue levels were also associated with the “loss of autonomy” subscale in the fear of progression questionnaire (β=0.26) (32). The COVID-19 pandemic provided additional insight into how social/environmental factors might influence fear of relapse; patients who experienced a relapse during the pandemic reported significantly higher fear of future relapse compared to those who did not (58.8 ± 24.0 vs. 48.1 ± 19.4) (30). Greater social support was inversely correlated with this fear (r=-0.25) (34).
3.6 Fear of disease relapse/progression impacts health/wellness
Numerous studies have demonstrated that fear of disease progression and relapse is correlated with depression, anxiety, stress, and diminished psychological well-being (14, 24, 25, 29, 30, 33, 34) (See Table 2 for effect sizes). Increased fear adversely affected quality of life among people living with MS (β = -0.70, r= −0.53, r=-0.451, respectively) (14, 24, 25). Notably, in RRMS patients, fear of relapse emerged as the strongest predictor of quality of life, surpassing other factors such as age, education level, disease characteristics, and neurologists’ estimates of disease severity (14). Those with greater fear of relapse also perceived their health more poorly overall (r=-0.342). The three factors of the fear of relapse scale—fear of disability, psychological consequences, and limitations from fear—were all independently associated with poorer health self-perception (26).
3.7 Psychological factors influence fear of relapse and quality of life
Nielson and colleagues found that the following aspects of psychological resilience were determinants of fear of progression: emotional regulation (β= -0.26), self-observation (β=0.27, 0.26), and self-efficacy (β=-0.35) (32).Broche-Perez et al. showed that psychological resilience could also slightly reduce the adverse impact of fear of relapse on quality of life (including psychological resilience as a mediator reduced the β coefficient from -0.36 to -0.32) (27).
3.8 Interventions targeting fear of relapse/progression
Only one randomized controlled trial examined the impact of a 3-month nurse/physician collaborative care intervention on fear of progression in MS. The intervention encouraged patients to actively engage in managing their condition through seven 90–120 minute educational sessions, collaborative follow-up meetings (“in two collaborative care training sessions in the third and fourth weeks and two follow-up visits, with two weeks apart and the second training session in 90–120 minutes”), and periodic assessments. (38).
These sessions of collaborative care over nine weeks slightly decreased fear of progression scores from 37.80 ± 12.22 to 34.86 ± 12.21, whereas those who did not undergo collaborative care showed a small increase in fear (38.39 ± 11.4 to 40.20 ± 11.68). Between-group differences were small and not statistically significant (28).
4 Discussion
This systematic review synthesized current literature on the prevalence, impact, and associated factors of fear of relapse and disease progression among individuals living with MS. In each subsection below, we delve into the implications of these findings, compare them with existing literature, acknowledge the limitations of our review, and propose recommendations for clinical practice and future research.
4.1 Prevalence and impact of fear in MS
The studies consistently show that fear of relapse and disease progression is a frequent and substantial concern among people with MS. This aligns with findings in other chronic diseases—such as cancer, diabetes, and rheumatoid arthritis—where fear of disease progression is recognized as a common and distressing issue (39–41).
Our review found robust associations between fear of relapse/progression and several negative psychological outcomes, such as depression, anxiety, stress, fatigue, health anxiety (10, 14, 24–26, 29, 30, 32–34), and poor quality of life (14, 25, 26, 34). These findings suggest that fear of relapse/progression is not an isolated concern but part of a broader psychological profile, creating a vicious cycle in which psychological distress heightens fear, further worsening mental health and quality of life.
The high prevalence and significant impact of fear of relapse/progression necessitate proactive clinical interventions. Clinicians should routinely screen for fear using validated tools like the Fear of Relapse Scale or the Fear of Progression Questionnaire. Early identification allows for timely psychological support and tailored interventions. Screening is particularly important for women and younger individuals who experience greater fear of relapse/progression on average (24, 34). They particularly fear becoming dependent on others for daily activities (31) during a time in their lives where there is likely a greater societal expectation to be productive and to care for others. Previous studies investigating fear of recurrence in cancer have also demonstrated that younger individuals were more likely to be affected by this fear (17).
4.2 Clinical predictors and potential interventions
Clinical variables such as disease duration/severity, number of relapses, and time since the last relapse were not consistently associated with fear of relapse/progression (14). In contrast, social support, psychological resilience, and individual perceptions of one’s own health were much more influential (26, 27, 34). Interpreting ambiguous bodily stimuli as potential symptoms, experiencing more fatigue, and perceiving cognitive impairment significantly contributed to fear of relapse (29).
Exercise is a prime community-based intervention that addresses many factors linked to increased fear of progression; it concurrently reduces MS fatigue (42), enhances interoception (43), and may provide opportunities for social contact. Future in-clinic interventions educating patients about benign bodily sensations (29), guiding them towards reliable information sources, and cautioning against misinformation could also empower patients to interpret interoceptive signals more accurately and reduce unnecessary anxiety and fear. In support of this, a collaborative nursing/physician educational/monitoring intervention did produce a small positive impact (28). It is likely that integrating psychological services into MS care could provide further benefit through targeted stress management and resilience training. However, it is important to highlight that current evidence on interventions specifically targeting fear of relapse or progression remains extremely limited. To date, only one interventional study (28) has directly addressed this outcome.
Consistent with the broader literature emphasizing the importance of social networks for managing chronic illness (44), social support is associated with lower levels of fear of progression. Group- and community-based interventions may therefore be especially beneficial (34). Encouraging collaboration and interaction between newly diagnosed MS patients and those with well-controlled long-term disease could help alleviate the fear of relapse by providing reassurance and practical coping strategies. Such peer support initiatives have shown promise in previous studies (45, 46). Social workers, support groups, and/or recreational therapists can link patients to community programs and supportive resources.
The aim of any intervention targeting fear of relapse or progression should not be to eliminate the fear entirely, but to harness it as a motivator for self-care (47) while providing coping skills and resources to manage an uncertain disease course. Collaborative care models involving multidisciplinary teams—including neurologists, psychologists, social workers, exercise scientists, and patients with similar conditions—are likely needed to provide comprehensive support.
4.3 Limitations
The included studies were mostly conducted in Iran, Turkey, Germany, and Spanish-speaking countries, which limits the generalizability of findings to other regions with different cultural perceptions of illness and different health care systems. Two different assessment tools were used (Fear of Relapse Scale and Fear of Progression Questionnaire) with some differences in their focus and scope. Substantial heterogeneity in MS types (e.g., RRMS, PPMS, SPMS), disease durations, and severity levels further complicates synthesis of the evidence. Most studies employed cross-sectional designs, precluding causal inferences. While these studies provide valuable insights into associations between fear of relapse or disease progression and psychological or clinical outcomes, they do not allow for conclusions about causality or temporal sequence. As a result, it remains unclear whether fear contributes to increased anxiety, fatigue, and reduced quality of life, or whether these factors, in turn, exacerbate fear.
Another limitation was that our search was limited to PubMed, Scopus, and Web of Science, which may have led to the omission of relevant studies indexed in other databases such as EMBASE or Cochrane.
Finally, the potential for publication bias exists, as studies reporting significant findings are more likely to be published.
4.4 Future research directions
Future studies should aim to address these limitations. Conducting research in diverse geographic and cultural contexts will enhance the generalizability of findings. Cultural context likely plays a significant role in shaping how individuals perceive and respond to fear of relapse or disease progression, yet this aspect remains underexplored in the current literature. Most included studies were conducted in Iran, Turkey, Germany, and Spanish-speaking countries, each with distinct cultural beliefs, health system structures, social support norms, and attitudes toward chronic illness. For example, societies with strong family-oriented support systems may buffer some of the anxiety associated with disease progression, while cultures with high stigma around disability or chronic disease could amplify fear and psychological distress (48). Differences in health literacy, trust in healthcare providers, and access to reliable information may also influence how bodily changes are interpreted and whether they are perceived as threatening. Consequently, findings from these regions may not fully capture the experiences of individuals living with MS in other cultural contexts, such as North America. Future research should explicitly investigate how cultural values, beliefs, and healthcare contexts shape the experience of fear and develop culturally sensitive interventions tailored to diverse populations.
Longitudinal observational designs can track changes in fear throughout the disease course and establish directionality of associations between fear and clinical outcomes. Intervention studies are particularly needed. Randomized controlled trials evaluating the efficacy of psychological interventions—such as cognitive-behavioral therapy, resilience training, and social support enhancement—should add fear of progression/relapse as an outcome variable or mediator variable. To ensure health equity in regions with limited access to specialized care, research on digital health interventions, such as telemedicine counselling or online support groups, is especially high priority.
Qualitative studies exploring patients’ lived experiences would deepen understanding of the nuances of fear in MS and inform intervention development/implementation.
5 Conclusion
Fear of relapse and disease progression has been frequently reported among individuals with MS and may negatively influence psychological well-being, contributing to higher levels of anxiety, depression, stress, fatigue, and reduced quality of life. Available studies suggest that psychosocial and perceptual elements, including levels of social support, resilience, perceptions of health, and interpretation of bodily signals, may play a more prominent role in shaping this fear than clinical characteristics alone. However, the limited number of studies—particularly the scarcity of interventional research—makes it difficult to draw firm conclusions about its prevalence, predictors, or clinical consequences. These uncertainties highlight the need for routine assessment of fear in clinical practice for example using the Fear of Relapse Scale (specific to RRMS) or the Fear of progression questionnaire (applicable across chronic illnesses), and for future research to design and rigorously evaluate targeted interventions such as psychoeducation, resilience training and peer support.
Author contributions
AM: Conceptualization, Project administration, Methodology, Investigation, Writing – original draft, Writing – review & editing. TF: Writing – original draft, Writing – review & editing. LG: Writing – original draft, Writing – review & editing. MF: Writing – original draft, Writing – review & editing. SH: Writing – original draft, Writing – review & editing. AK: Writing – original draft, Writing – review & editing, Investigation.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1680781/full#supplementary-material
References
1. Woo MS, Engler JB, and Friese MA. The neuropathobiology of multiple sclerosis. Nat Rev Neurosci. (2024) 25:493–513. doi: 10.1038/s41583-024-00823-z
2. Khan G and Hashim MJ. Epidemiology of multiple sclerosis: global, regional, national and sub-national-level estimates and future projections. J Epidemiol Global Health. (2025) 15:21. doi: 10.1007/s44197-025-00353-6
3. McGinley MP, Goldschmidt CH, and Rae-Grant AD. Diagnosis and treatment of multiple sclerosis: a review. JAMA. (2021) 325:765–79. doi: 10.1001/jama.2020.26858
4. Fymat AL. Multiple sclerosis: II. Diagnosis and symptoms management. J Neurol Psychol Res. (2023) 4:1–21.
5. Klineova S and Lublin FD. Clinical course of multiple sclerosis. Cold Spring Harbor Perspect Med. (2018) 8:a028928. doi: 10.1101/cshperspect.a028928
6. Nazareth TA, Rava AR, Polyakov JL, Banfe EN, Waltrip Ii RW, Zerkowski KB, et al. Relapse prevalence, symptoms, and health care engagement: patient insights from the Multiple Sclerosis in America 2017 survey. Multiple sclerosis related Disord. (2018) 26:219–34. doi: 10.1016/j.msard.2018.09.002
7. Lublin FD, Häring DA, Ganjgahi H, Ocampo A, Hatami F, Čuklina J, et al. How patients with multiple sclerosis acquire disability. Brain. (2022) 145:3147–61. doi: 10.1093/brain/awac016
8. Berkovich RR. Acute multiple sclerosis relapse. CONTINUUM: Lifelong Learn Neurol. (2016) 22:799–814. doi: 10.1212/CON.0000000000000330
9. Mäurer M, Comi G, Freedman MS, Kappos L, Olsson TP, Wolinsky JS, et al. Multiple sclerosis relapses are associated with increased fatigue and reduced health-related quality of life–A post hoc analysis of the TEMSO and TOWER studies. Multiple sclerosis related Disord. (2016) 7:33–40. doi: 10.1016/j.msard.2016.02.012
10. Khatibi A, Moradi N, Rahbari N, Salehi T, and Dehghani M. Development and validation of fear of relapse scale for relapsing-remitting multiple sclerosis: understanding stressors in patients. Front Psychiatry. (2020) 11:226. doi: 10.3389/fpsyt.2020.00226
11. Herschbach P, Berg P, Dankert A, Duran G, Engst-Hastreiter U, Waadt S, et al. Fear of progression in chronic diseases: psychometric properties of the Fear of Progression Questionnaire. J psychosomatic Res. (2005) 58:505–11. doi: 10.1016/j.jpsychores.2005.02.007
12. Lebel S, Mutsaers B, Tomei C, Leclair CS, Jones G, Petricone-Westwood D, et al. Health anxiety and illness-related fears across diverse chronic illnesses: A systematic review on conceptualization, measurement, prevalence, course, and correlates. PLoS One. (2020) 15:e0234124. doi: 10.1371/journal.pone.0234124
13. Nielsen J, Saliger J, Montag C, Markett S, Nöhring C, and Karbe H. Facing the unknown: fear of progression could be a relevant psychological risk factor for depressive mood states among patients with multiple sclerosis. Psychother psychosomatics. (2018) 87:190–2. doi: 10.1159/000487329
14. Khatibi A, Weiland TJ, and Dehghani M. Fear of relapse in patients suffering from RRMS influence their quality of life. Multiple sclerosis related Disord. (2021) 54:103137. doi: 10.1016/j.msard.2021.103137
15. Butler E, Matcham F, and Chalder T. A systematic review of anxiety amongst people with Multiple Sclerosis. Multiple sclerosis related Disord. (2016) 10:145–68. doi: 10.1016/j.msard.2016.10.003
16. Crombez G, Vlaeyen JW, Heuts PH, and Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. (1999) 80:329–39. doi: 10.1016/S0304-3959(98)00229-2
17. Crist JV and Grunfeld EA. Factors reported to influence fear of recurrence in cancer patients: a systematic review. Psycho-Oncology. (2013) 22:978–86. doi: 10.1002/pon.3114
18. Portaccio E, Magyari M, Havrdova EK, Ruet A, Brochet B, Scalfari A, et al. Multiple sclerosis: emerging epidemiological trends and redefining the clinical course. Lancet Regional Health–Europe. (2024) 44. doi: 10.1016/j.lanepe.2024.100977
19. Tricco AC, Lillie E, Zarin W, O’brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Internal Med. (2018) 169:467–73. doi: 10.7326/M18-0850
20. Chandler J, Cumpston M, Li T, Page MJ, and Welch V. Cochrane handbook for systematic reviews of interventions. Hoboken: Wiley (2019).
21. Kmet L. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta, Canada: Alberta Heritage Foundation for Medical Research Edmonton (2004).
22. French-Lawyer J, Siano S, Ioerger M, Young V, and Turk MA. Health information seeking and people with disability: A systematic search and scoping review. Disability Health J. (2021) 14:100983. doi: 10.1016/j.dhjo.2020.100983
23. Braun V and Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
24. Azami-Aghdash S, Ghojazadeh M, Naghavi-Behzad M, Derakhshani N, Asl VP, and Samei B. A pilot study of fear of disease consequences and its relationship with quality of life, depression and anxiety in patients with multiple sclerosis. Int Arch Health Sci. (2019) 6:132–5. doi: 10.4103/iahs.iahs_9_19
25. Broche-Pérez Y, Jiménez-Morales RM, Monasterio-Ramos LO, and Bauer J. Validity and reliability of the 10-item Connor-Davidson Resilience Scale (CD-RISC-10) in a sample of Spanish-speaking patients with Multiple Sclerosis. Multiple Sclerosis Related Disord. (2022) 63:103914. doi: 10.1016/j.msard.2022.103914
26. Broche-Pérez Y, Jiménez-Morales RM, Monasterio-Ramos LO, Vázquez-Gómez LA, and Fernández-Fleites Z. Fear of Relapse Scale: Spanish version and psychometric characteristics in a sample of patients with Relapsing-Remitting multiple sclerosis. Neurología (English Edition). (2022) 39:749–55. doi: 10.1016/j.nrl.2022.06.005
27. Broche-Perez Y, Jimenez-Morales RM, Vázquez-Gómez LA, Bauer J, and Fernández-Fleites Z. Fear of relapse and quality of life in multiple sclerosis: The mediating role of psychological resilience. Multiple Sclerosis Related Disord. (2023) 79:105026. doi: 10.1016/j.msard.2023.105026
28. Ebrahimi M, Jaberi AA, and Bonabi TN. Effect of collaborative care on fear of disease progression in multiple sclerosis patients: A randomized controlled trial. J Nurs Midwifery Sci. (2023) 10. doi: 10.5812/jnms-141576
29. Hosseinchi P, Ghalibaf E, Dehghani A, and Khatibi A. Negative interpretation of ambiguous bodily information by patients with relapsing-remitting multiple sclerosis. Multiple sclerosis related Disord. (2022) 62:103808. doi: 10.1016/j.msard.2022.103808
30. Moghadasi AN, Vaheb S, Hamtaei-Ghashti S, Shaygannejad A, Askari M, Shaygannejad V, et al. Fear of re-infection, relapse, and anxiety during COVID-19 pandemic in patients with multiple sclerosis: A multi-center study. Curr J Neurol. (2023) 22:82. doi: 10.18502/cjn.v22i2.13332
31. Nickel S, Von Dem Knesebeck O, and Kofahl C. Self-assessments and determinants of HRQ oL in a German MS population. Acta neurologica scandinavica. (2018) 137:174–80. doi: 10.1111/ane.12854
32. Nielsen J, Saliger J, Folkerts A-K, Eschweiler M, Sayn-Reutelsterz C, Kalbe E, et al. The role of wisdom and self-management skills for coping with fear of progression among patients with multiple sclerosis with moderate disability: Results from a cross-sectional study. J Affect Disord Rep. (2022) 8:100311. doi: 10.1016/j.jadr.2022.100311
33. Özden F, Özkeskin M, and Yüceyar N. Cross-cultural adaptation, reliability and validity of the Turkish version of the Fear of Relapse Scale (FoR) in individuals with multiple sclerosis. Clin Neurol Neurosurg. (2022) 219:107338. doi: 10.1016/j.clineuro.2022.107338
34. Shaygannejad V, Mirmosayyeb O, Nehzat N, and Ghajarzadeh M. Fear of relapse, social support, and psychological well-being (depression, anxiety, and stress level) of patients with multiple sclerosis (MS) during the COVID-19 pandemic stage. Neurological Sci. (2021) 42:2615–8. doi: 10.1007/s10072-021-05253-8
35. Herschbach P, Dankert A, Duran-Atzinger G, Waadt S, Engst-Hastreiter U, Keller M, et al. Diagnostik von Progredienzangst–Entwicklung eines Fragebogens zur Erfassung von Progredienzangst bei Patienten mit Krebserkrankungen, Diabetes mellitus und entzündlich-rheumatischen Erkrankungen in der Rehabilitation. Munich: Institut für Psychosomatische Medizin, medizinische Psychologie und Psychotherapie der TU-München (2001).
36. Kwakkenbos L, Van Den Hoogen FH, Custers J, Prins J, Vonk MC, Van Lankveld WG, et al. Validity of the fear of progression questionnaire-short form in patients with systemic sclerosis. Arthritis Care Res. (2012) 64:930–4. doi: 10.1002/acr.21618
37. Freeston MH, Rhéaume J, Letarte H, Dugas MJ, and Ladouceur R. Why do people worry? Pers Individ Dif. (1994) 17:791–802. doi: 10.1016/0191-8869(94)90048-5
38. Mohammadi E, Abedi HA, Jalali F, Gofranipour F, and Kazemnejad A. Evaluation of ‘partnership care model’in the control of hypertension. Int J Nurs Pract. (2006) 12:153–9. doi: 10.1111/j.1440-172X.2006.00563.x
39. Clarke ST, Murphy BM, Rogerson M, Le Grande M, Hester R, and Jackson AC. Conceptualizing fear of progression in cardiac patients: Advancing our understanding of the psychological impact of cardiac illness. Heart Mind. (2024) 8:29–39. doi: 10.4103/hm.HM-D-23-00046
40. Dankert A, Duran G, Engst-Hastreiter U, Keller M, Waadt S, Henrich G, et al. Fear of progression in patients with cancer, diabetes mellitus and chronic arthritis. Die Rehabil. (2003) 42:155–63. doi: 10.1055/s-2003-40094
41. Herschbach P and Dinkel A. Fear of progression. Psycho-oncology. (2013) 197:11–29. doi: 10.1007/978-3-642-40187-9_2
42. Boda MR, Rees AE, Goldsworthy MR, Evangelou N, Sidhu SK, and Smith AE. Scoping review: The effects of diet, physical activity and sleep on motor and physical fatigue in people with multiple sclerosis. Neuroscience. (2025) 568:166–94. doi: 10.1016/j.neuroscience.2025.01.032
43. Mulder J, Boelens M, van der Velde LA, Brust M, and Kiefte-De Jong JC. The role of interoception in lifestyle factors: a systematic review. Neurosci Biobehav Rev. (2025) 106018. doi: 10.1016/j.neubiorev.2025.106018
44. De Vries J, Den Oudsten BL, Jacobs PM, and Roukema JA. How breast cancer survivors cope with fear of recurrence: a focus group study. Supportive Care Cancer. (2014) 22:705–12. doi: 10.1007/s00520-013-2025-y
45. Ng L, Amatya B, and Khan F. Outcomes of a peer support program in multiple sclerosis in an Australian community cohort: a prospective study. J Neurodegenerative Dis. (2013) 2013:429171. doi: 10.1155/2013/429171
46. Gerritzen EV, Lee AR, Mcdermott O, Coulson N, and Orrell M. Online peer support for people with multiple sclerosis: A narrative synthesis systematic review. Int J MS Care. (2022) 24:252–9. doi: 10.7224/1537-2073.2022-040
47. Koch L, Jansen L, Brenner H, and Arndt V. Fear of recurrence and disease progression in long-term (≥ 5 years) cancer survivors—a systematic review of quantitative studies. Psycho-oncology. (2013) 22:1–11. doi: 10.1002/pon.3022
Keywords: multiple sclerosis, fear of relapse, fear of progression, fear of disability, scoping review
Citation: Mallahzadeh A, Fereydoonnezhad T, Gauthier LV, Farjoud Kouhanjani M, Hosseinizadeh S and Khatibi A (2025) Fear of disease progression and relapse in multiple sclerosis: a systematic scoping review. Front. Psychiatry 16:1680781. doi: 10.3389/fpsyt.2025.1680781
Received: 06 August 2025; Accepted: 28 October 2025;
Published: 12 November 2025.
Edited by:
Ricardo Gusmão, University of Porto, PortugalReviewed by:
Mahlagha Dehghan, Kerman University of Medical Sciences, IranGiulia Marafioti, Bonino Pulejo Neurology Center (IRCCS), Italy
Copyright © 2025 Mallahzadeh, Fereydoonnezhad, Gauthier, Farjoud Kouhanjani, Hosseinizadeh and Khatibi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ali Khatibi, TWt0NDRAYmF0aC5hYy51aw==
 Arashk Mallahzadeh
Arashk Mallahzadeh Tahereh Fereydoonnezhad
Tahereh Fereydoonnezhad Lynne V. Gauthier
Lynne V. Gauthier Mohsen Farjoud Kouhanjani
Mohsen Farjoud Kouhanjani Shima Hosseinizadeh
Shima Hosseinizadeh Ali Khatibi
Ali Khatibi