- 1School of Public Health, Xuzhou Medical University, Xuzhou, China
- 2Office of the President, Xuzhou Medical University, Xuzhou, China
Background: Smartphones have become an essential part of daily life, but excessive use can lead to significant issues. This study assesses smartphone addiction among college students, examining its impact on dietary behaviors and health-promoting lifestyles. The aim is to provide a basis for targeted interventions.
Methods: A cross-sectional study was conducted among 1,002 students at Xuzhou Medical University in 2025 using a convenience sampling. Data were collected via questionnaires and analyzed using SPSS 21.0. The study used the Smartphone Addiction Scale-Short Version (SAS-SV), the Health-Promoting Lifestyle Profile (HPLP-II), and the Intuitive Eating Scale-2 (IES-2). Statistical methods included normality tests, descriptive statistics, and mediation analysis.
Results: Among the participants, medical students scored 34 (SAS), 74 (IES), and 134 (HPLP-II), while non-medical students scored 33.5 (SAS), 74 (IES), and 134 (HPLP-II). A negative correlation was observed between smartphone addiction and both intuitive eating (r = -0.174, p < 0.01) and health-promoting lifestyle (r = -0.074, p < 0.01). However, the effect sizes for these correlations are small, suggesting that, although statistically significant, the practical significance of these relationships may be limited. Intuitive eating mediated the relationship between smartphone addiction and health-promoting lifestyle (indirect effect = -0.1452, p < 0.001). Approximately 25.25% of participants reported feeling addicted to smartphones.
Conclusion: Smartphones have dual impacts on students’ eating behaviors and health. Excessive use is associated with disrupted eating patterns, while moderate use is associated with healthy behaviors that support well-being. It is crucial to educate students on balancing smartphone use with healthy habits is crucial. However, it is important to note that these findings, derived from a convenience sample at a single medical university, may not be fully generalizable to all college student populations. Future research with more diverse samples is needed to confirm these relationships.
1 Introduction
The rapid advancement of mobile internet technology has made smartphones essential part of modern life (1). However, this convenience has also led to smartphone addiction, which is becoming a significant global public health issue (2). Meta-analysis studies have indicated that the prevalence of smartphone addiction among global and Asian medical students was 26.99% (3) and 41.93% (4) respectively. The World Health Organization defines smartphone addiction as “an uncontrollable urge to use, with the behavior causing significant negative impacts on daily life, mental state, or physical health,” especially among adolescents and students.
Smartphone addiction exerts a significant influence on dietary behaviors. Excessive smartphone use can impede meal preparation and disrupt regular eating patterns, thereby fostering unhealthy habits such as reliance on fast food reliance and binge eating (5). Additionally, food marketing on social media platforms and concerns related to body image may distort individuals’ perceptions of diet and undermine intuitive eating practices. Emotional distress is frequently observed when access to smartphones is restricted (6). Behavioral addiction is characterized by factors including salience, tolerance, mood alterations, relapse, withdrawal, and conflict (7). Empirical studies have linked excessive smartphone use to increased anxiety and depression (8), cyberbullying (9), and poor dietary habits (9) among youth. These adverse outcomes can substantially affect dietary behaviors and health-related intentions, underscoring the necessity for balanced smartphone use. Therefore, acknowledging the importance of moderation is imperative.
Proactive health intention, defined as the intrinsic motivation to engage in health-promoting behaviors, encompasses commitment to a healthy lifestyle, active seeking of health information, and awareness of health risks. This construct is fundamental to effective health promotion (10). However, smartphone addiction may undermine proactive health intention by diminishing awareness of real-world health needs and reducing engagement in proactive behaviors such as exercise and dietary management (11). Empirical evidence suggests that individuals with exhibiting high levels of smartphone dependency demonstrate significantly lower in proactive health intention scores, particularly among adolescent populations (12).
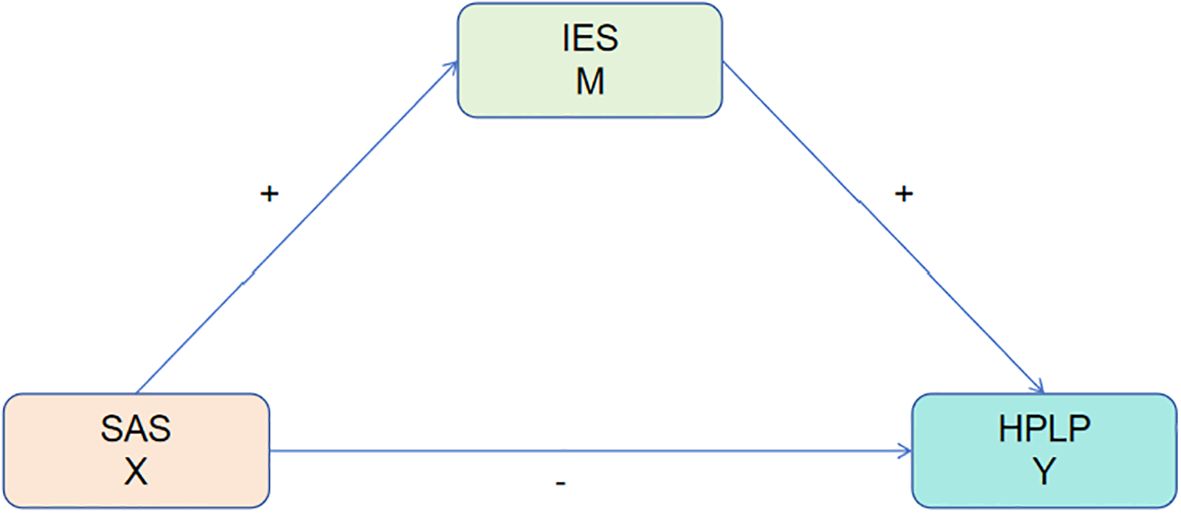
Current research predominantly examines the unidirectional relationships among smartphone addiction, dietary behaviors, and health intention, frequently neglecting their dynamic interactions (13). Disrupted dietary behaviors may exacerbate emotional smartphone use, whereas strong proactive health intention may attenuate the adverse effects of addiction on eating habits (14). A comprehensive understanding of these relationships is vital essential for the development of targeted interventions aimed at students. This study seeks to analyze the interrelations among smartphone addiction, dietary behaviors, and proactive health intention, with the objective of promoting healthy adolescent development. We hypothesize a negative correlation between smartphone addiction and both dietary behaviors and health intention, and we will assess its impact on medical and non-medical students (Figure 1).
Hypothesis 1 posits that smartphone addiction, dietary behaviors, and health-promoting lifestyles among college students are interrelated. Specifically, smartphone addiction is positively associated with dietary behaviors and negatively associated with health-promoting lifestyles, whereas dietary behaviors exhibit a positive correlation with health-promoting lifestyles.
Hypothesis 2 posits that dietary behaviors serve as a mediating factor in the relationship between smartphone addiction and health-promoting lifestyles among college students.
2 Study subjects and methods
2.1 Sample size calculation of study subjects
The sample size was determined using the formula for cross-sectional studies:
The P-value represents the prevalence of smartphone addiction among medical students in China was reported as 39.7% in a cross-sectional survey (15). Using a significance level (α) of 0.05, a corresponding Zα value of 1.96, and an allowable margin of error (δ) set at 5% in the present study, the minimum required sample size was calculated to be 368.
In February 2025, students from Xuzhou Medical University participated in this study. Of the 1,020 questionnaires distributed, 18 were excluded due to abnormal height and weight values or missing data, yielding 1,002 valid responses and a response rate of 98.24%.
2.2 Research methodology
A questionnaire survey was conducted to collect data on students’ personal information, mobile phone usage, dietary behaviors, and proactive health intentions.
2.2.1 Smartphone addiction scale - short version
The Smartphone Addiction Scale-Short Version (SAS-SV) is a self-reported instrument comprising 10 items designed to assess smartphone addiction (16). It employs a 6-point Likert scale to measure usage over the preceding six months, with higher scores reflecting greater dependency (16). The SAS-SV has been extensively utilized and validated across diverse cultural settings. In particular, the scale has demonstrated strong psychometric properties within the Chinese population (16), and conducted a translation and validation study among Chinese college students, confirming the unidimensional factor structure of the SAS-SV and reporting excellent internal consistency (Cronbach’s α = 0.89). These findings provide robust evidence supporting the scale’s validity and reliability in the cultural context relevant to the present study. Additionally, its applicability has been corroborated by another Chinese research (17). Consistent with Kwon et al. (18), this study adopted cut-off scores for smartphone addiction of ≥33 for female students and ≥31 for male students. In the current sample, the SAS-SV demonstrated a Cronbach’s alpha of 0.878, aligning with previous Chinese validation studies and indicating high reliability.
2.2.2 Health-promoting lifestyle profile
The Health-Promoting Lifestyle Profile II (HPLP-II) comprises 52 items distributed across six dimensions: Physical Activity (PA), Health Responsibility (HR), Stress Management (SM), Nutrition (NU), Interpersonal Relations (IR), and Spiritual Growth (SG) (19). Data collection involved a demographic questionnaire and the HPLP-II instrument, which evaluates health-promoting behaviors. The demographic questionnaire captured variables including age, gender, academic major, place of residence, economic status, weight, and height. This study employed the officially translated and validated Chinese version of the HPLP-II developed by Teng et al. (20). Their validation study, conducted among Taiwan adults, demonstrated satisfactory reliability and acceptable model fit indices, thereby supporting the instrument’s applicability within Chinese-speaking populations. Although originally developed in Taiwan, the shared written language and cultural similarities justify its use in Mainland China. Moreover, prior research has successfully implemented this version in mainland Chinese samples. In the current study, the HPLP-II exhibited a Cronbach’s alpha coefficient of 0.965, indicating excellent internal consistency and confirming its reliability for assessing health-promoting lifestyles among mainland Chinese university students.
2.2.3 Intuitive eating scale-2
The Intuitive Eating Scale-2 (IES-2), developed by Tylka and Babbott et al. (21), consists of four factors: Unconditional Permission to Eat (6 items), Eating for Physical Rather than Emotional Reasons (8 items), Eating in Response to Hunger and Satiety Cues (6 items), and Body-Food Choice Congruence (3 items), comprising a total of 23 items. Responses are measured on a 5-point Likert scale ranging from 1 (Strongly Disagree) to 5 (Strongly Agree), with higher scores reflecting greater levels of intuitive eating. The IES-2 has been validated within the Chinese cultural context. Specifically, Ji et al. (22) examined the psychometric properties of the IES-2 in a large sample of Chinese adults and confirmed its four-factor structure through psychometric network analysis. Their results support the cross-cultural validity and applicability of the IES-2 for assessing intuitive eating in China. In the present study, the Cronbach’s alpha for the IES-2 was 0.856, consistent with the good internal consistency reported by Ji et al., thereby further substantiating its reliability for the current study population.
2.3 Statistical analysis
Data were analyzed using SPSS version 21.0. The Shapiro-Wilk test was employed to assess normality; non-normally distributed data were presented as medians with interquartile ranges (M [P25, P75]). The Mann-Whitney U test was used to compare two groups, while the Kruskal-Wallis H test was applied for comparisons among multiple groups. Spearman’s correlation analysis was conducted to examine relationships among variables. Continuous variables were reported as medians (P25, P75), and categorical variables as frequencies and percentages. A significance level of α = 0.05 was adopted. The Bootstrap method (Model 4) was utilized to test the mediating effect of dietary behavior on the relationship between smartphone addiction and health-promoting lifestyle, with 5,000 resamples used to calculate the 95% confidence interval (CI). A path was considered significant if the 95% CI did not include zero, and p < 0.05 were deemed statistically significant.
3 Results
3.1 Common method bias
The Harman single-factor test revealed the presence of 15 factors with eigenvalues exceeding 1. The first factor accounted for 25.44% of the total variance, which is below the 40% threshold, suggesting that common method bias is not a significant concern in this study.
3.2 Study population characteristics
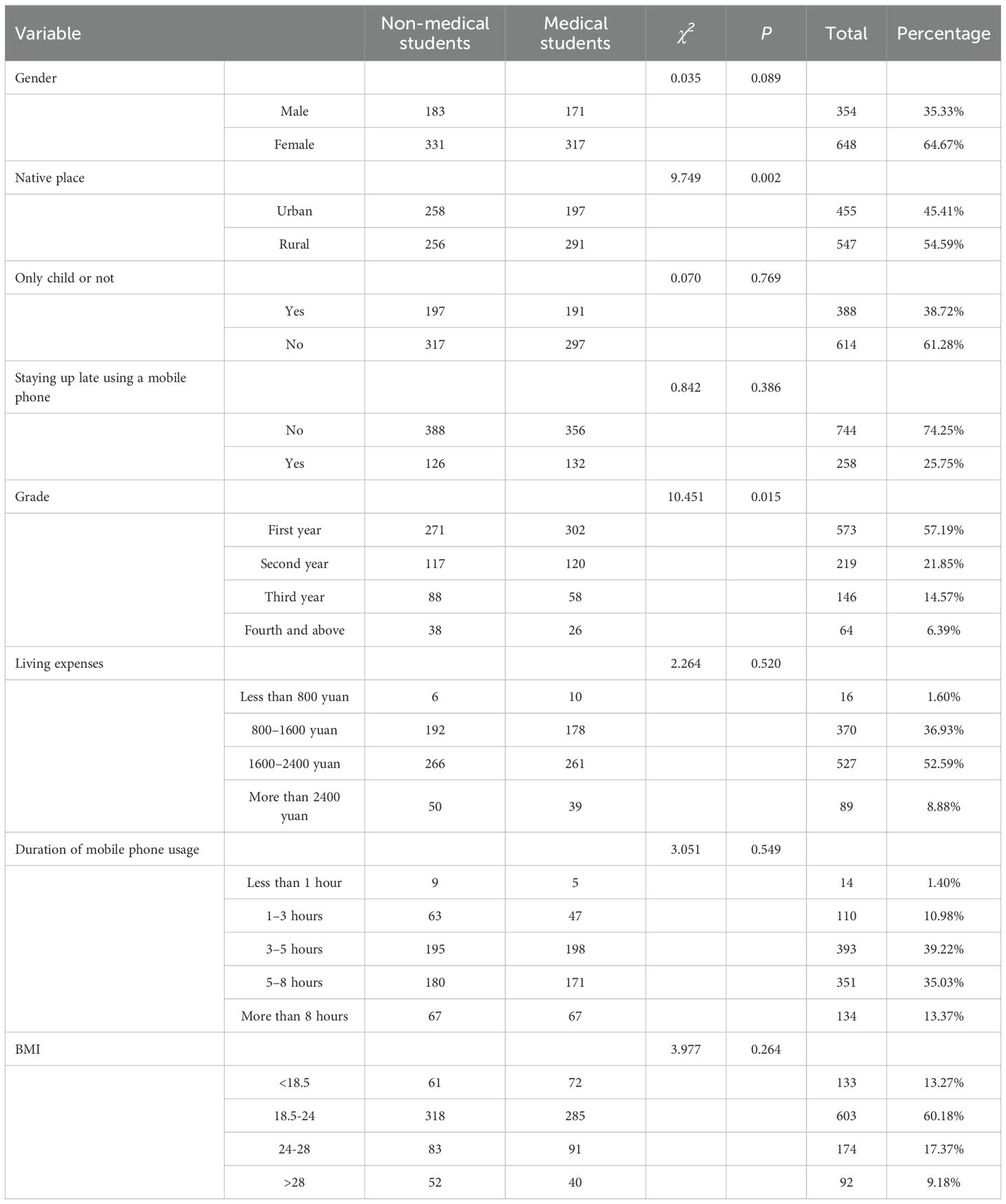
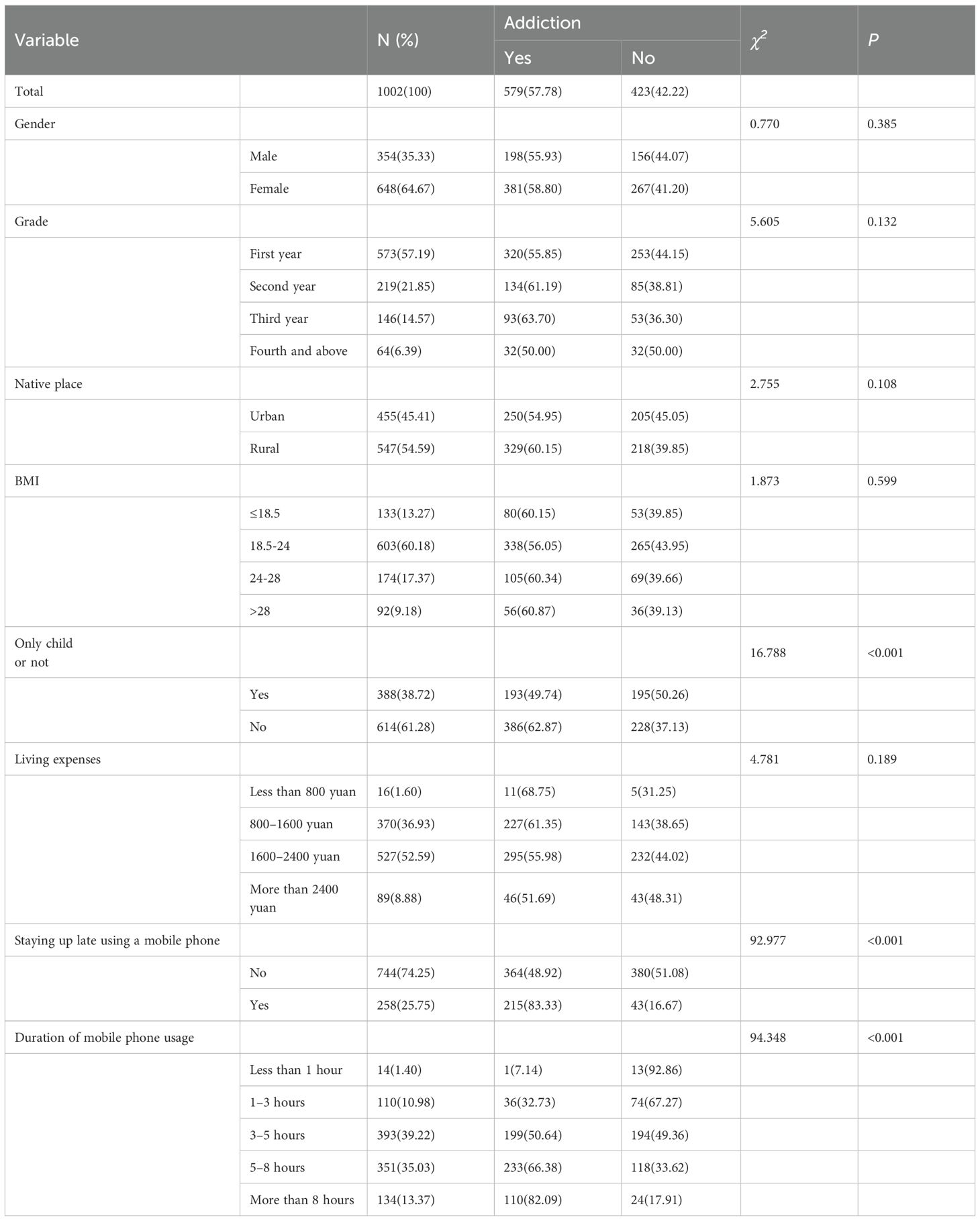
This study comprised 1,002 participants, who were categorized and analyzed as either non-medical or medical students (see Table 1). Among the participants, 198 males (55.93%) and 381 females (58.80%) were identified as exhibiting smartphone addiction (refer to Table 2). No significant differences were observed with respect to gender, living expenses, only-child status, mobile phone usage, or body mass index (BMI). However, a significant difference was detected in household registration status: 455 participants (45.41%) were urban residents, whereas 547 (54.59%) were rural residents (χ2 = 9.749, p = 0.002). First-year students constituted the majority at 57.19% (n = 573), followed by second-year students at 21.85% (n = 219). Additionally, a significant difference in the distribution of academic year was identified (χ2 = 10.451, p = 0.015), suggesting variations in student composition across disciplines.
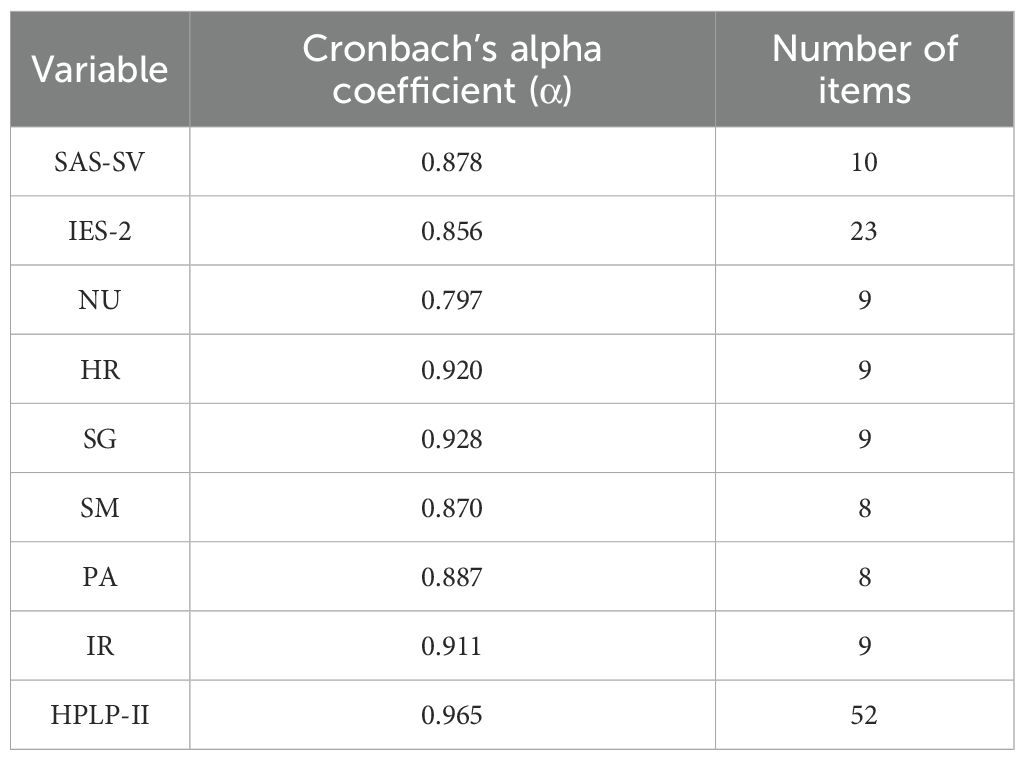
3.3 Reliability analysis
The reliability analysis results are presented in the Table 3. The reliability coefficients for the SAS-SV, IES-2, and HPLP-II scales, as well as their secondary dimensions, ranged from 0.7 to 1.0, indicating good internal consistency and high reliability.
3.4 Differences analysis
3.4.1 Analysis of differences in smartphone addiction scores
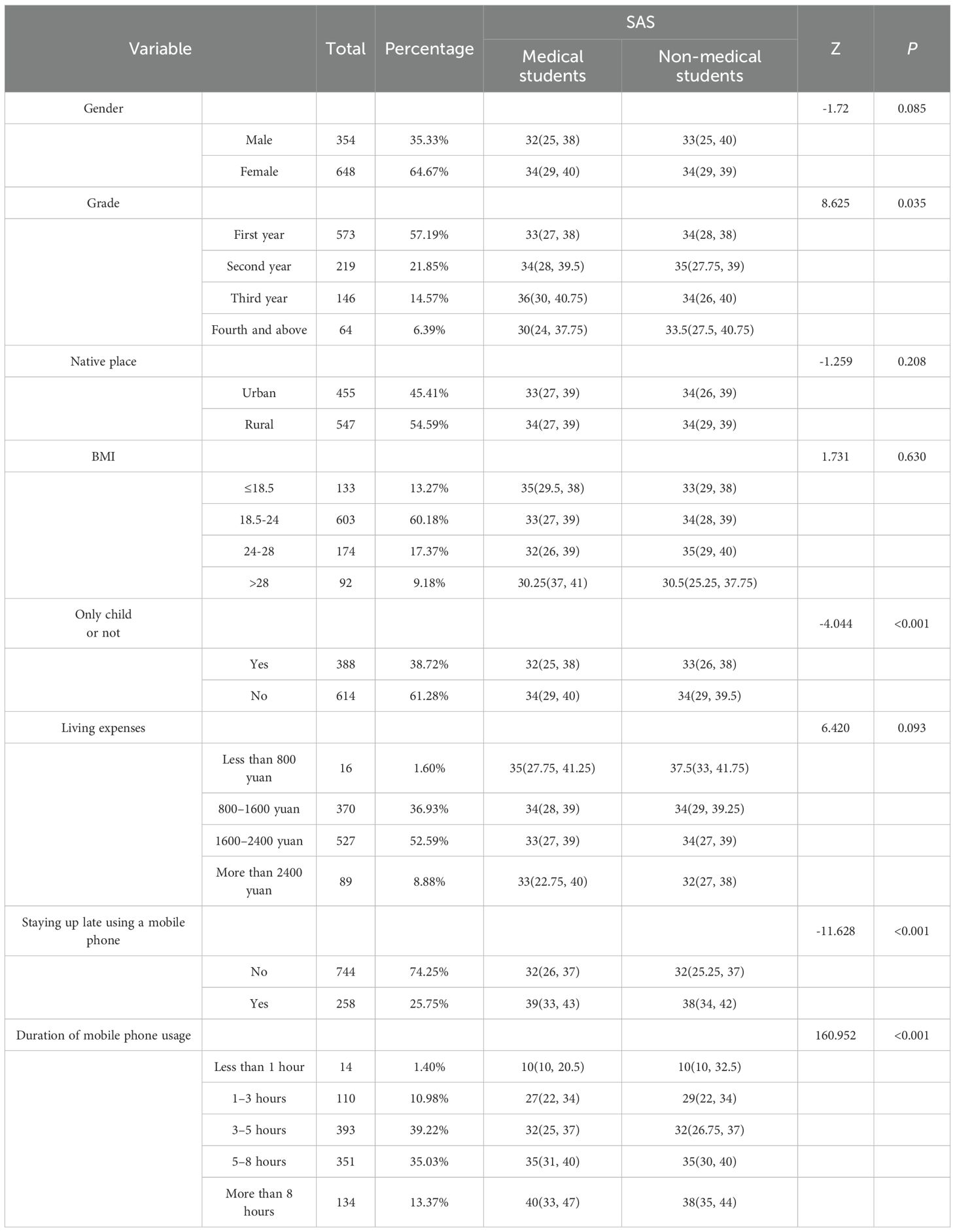
Given the non-normal distribution of the data, the median and interquartile range (M [P25, P75]) were employed for descriptive analysis (see Table 4). Comparative analysis of SAS-SV scores among university students indicated no significant differences between medical and non-medical students with respect to gender, living expenses, household registration, and BMI. Conversely, significant differences were observed based on academic year, late-night mobile phone use, and whether the student was an only-child status (p < 0.001). Students who engage in late-night mobile phone use exhibited higher addiction scores, suggesting a strong association between nocturnal usage and smartphone addiction. Furthermore, extended duration of mobile phone use was positively correlated with increased addiction scores (p < 0.001). Prolonged exposure to repetitive informational stimuli appears to impair self-control, with addictive behaviors becoming more pronounced after five hours of use.
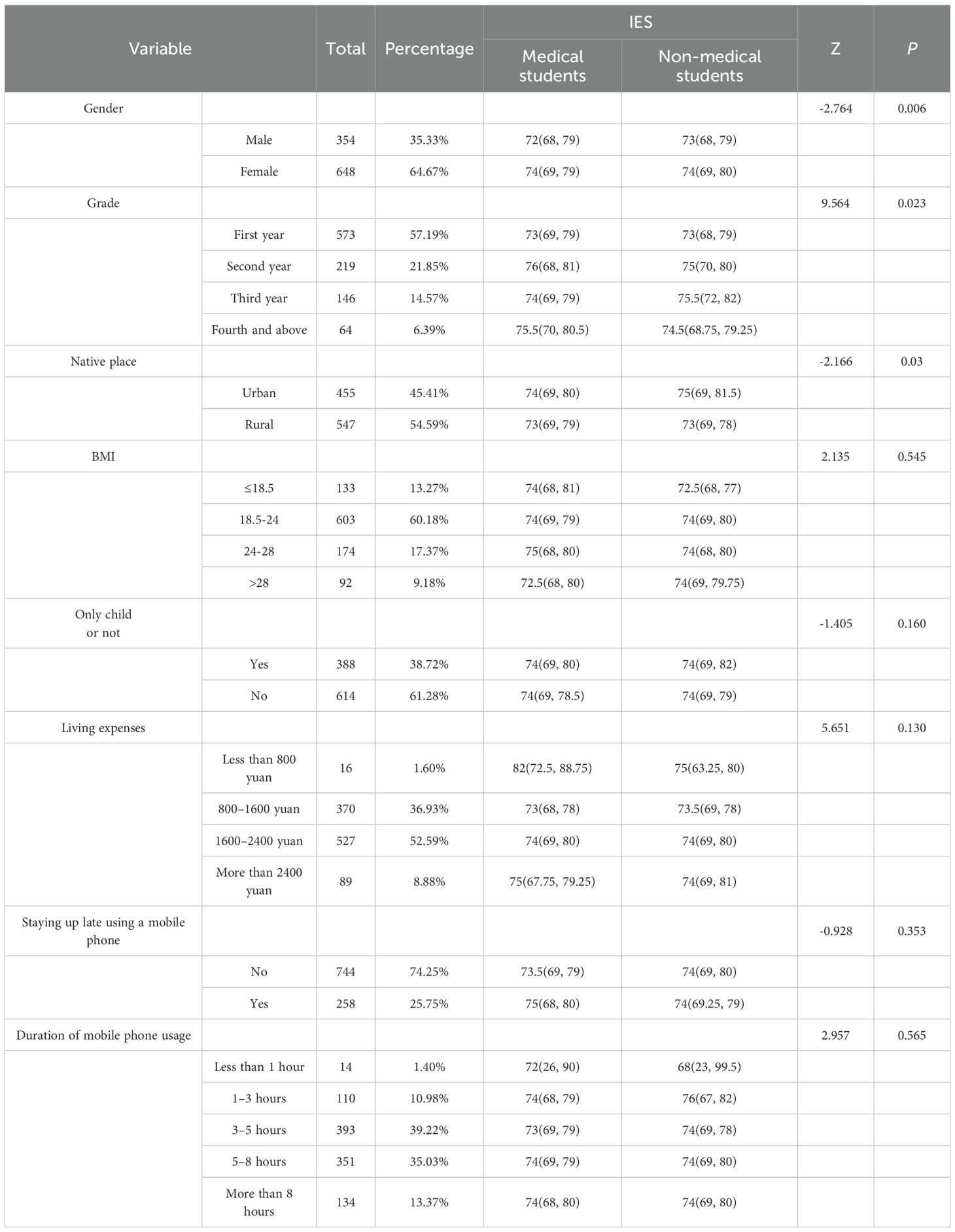
3.4.2 Analysis of differences in health-promoting lifestyle scores
Health-promoting lifestyle scores were presented as median (P25, P75) due to the non-normal distribution of the data (Table 5). Comparative analysis among university students indicated no significant differences between medical and non-medical students with respect to being an only child. However, significant differences were identified based on gender and academic year (p < 0.001). Scores generally decreased as students progressed through their academic years, which may be attributed to increased academic pressure, occupational stress, and social engagements. Additionally, significant differences in scores were observed across BMI categories (p = 0.048) and were associated with household registration status, living expenses, frequency of late-night mobile phone use, and duration of usage.
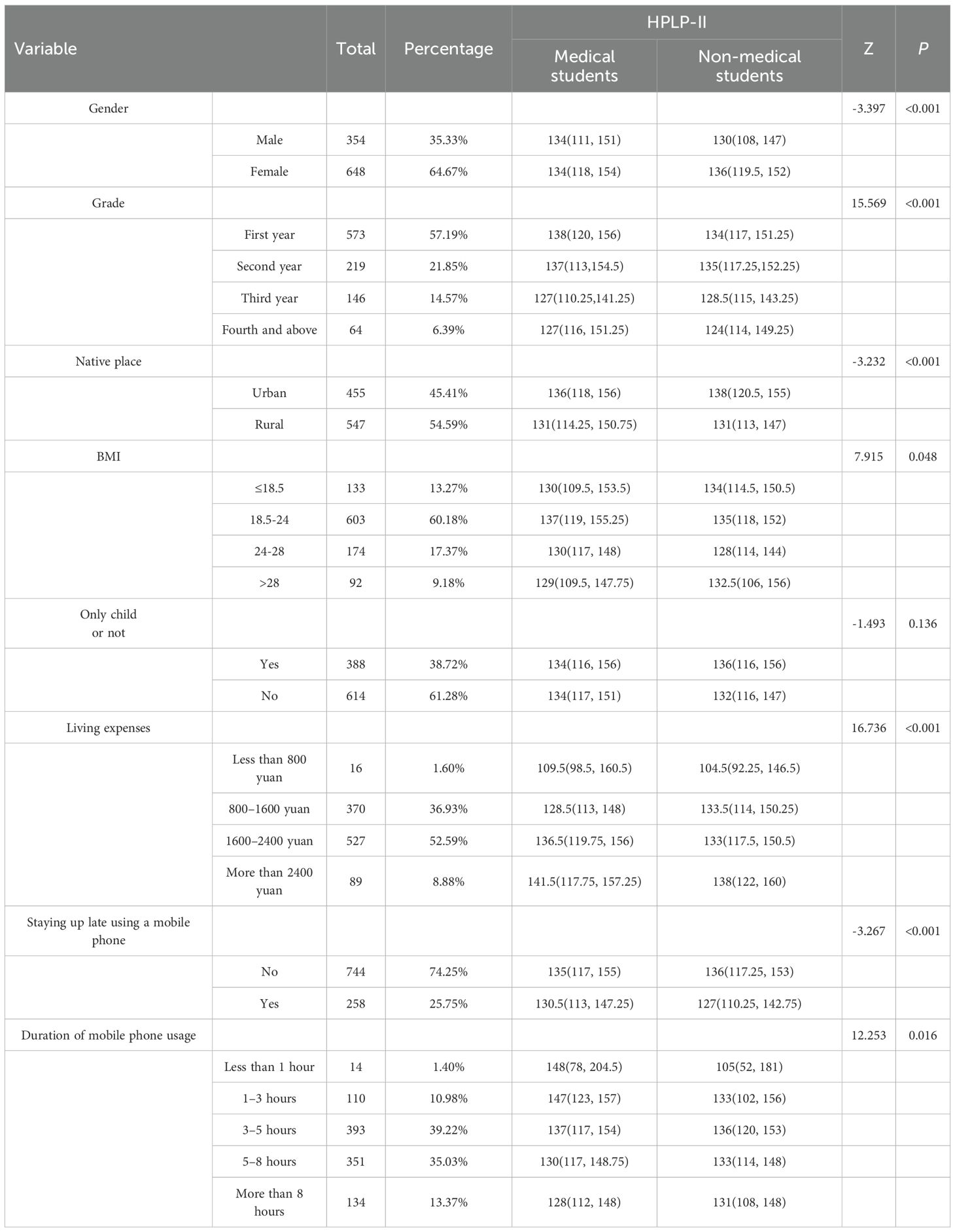
Table 5. Health-promoting lifestyle scores among university students with different characteristics.
3.4.3 Analysis of differences in dietary behavior scores
Given the non-normal distribution of the data, dietary behavior scores were presented as medians with interquartile ranges (M [P25, P75]). Analysis of the IES among university students revealed no significant differences between medical and non-medical students regarding mobile phone usage, late-night usage, only-child status, living expenses, and BMI. However, significant gender differences were observed (p = 0.006), suggesting that gender influences dietary behaviors. Additionally, dietary behavior scores varied significantly across academic years (p = 0.023), potentially reflecting fluctuations associated with changes in academic pressure and lifestyle pace. Furthermore, significant differences were identified between urban and rural students (p = 0.03), highlighting the influence of food culture (23). Consistent with these findings, Wang et al. (24) reported that Westernized dietary patterns are more prevalent in urban areas, whereas traditional plant-based diets remain predominant in rural regions. The results are summarized in Table 6.
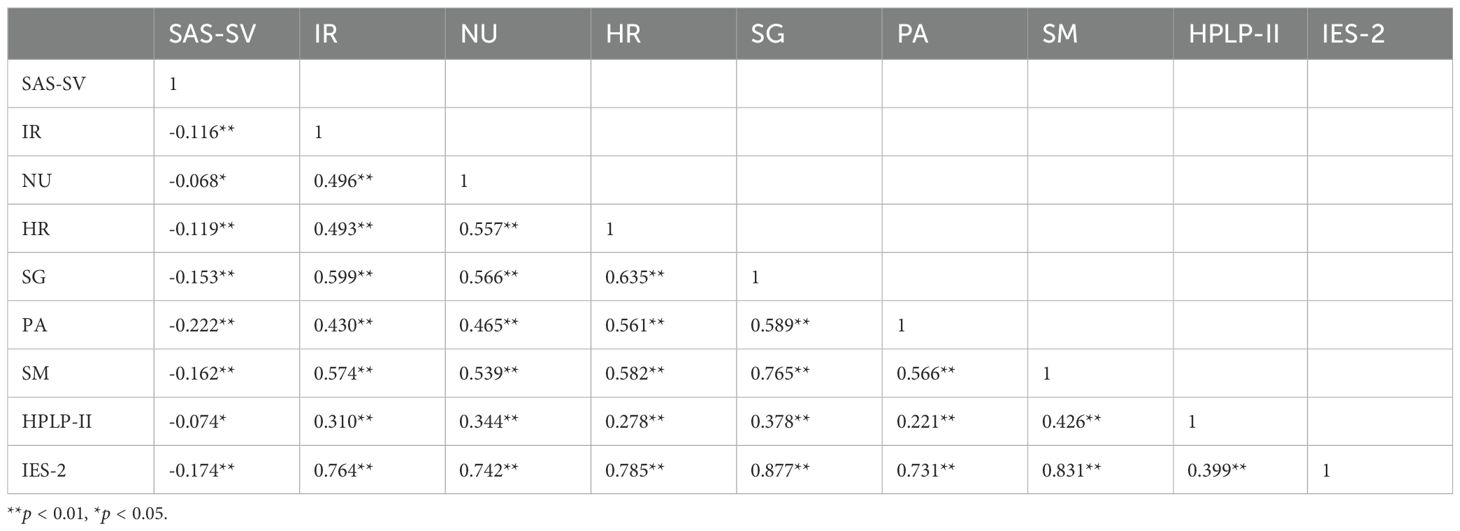
3.5 Correlation analysis
Smartphone addiction scores demonstrated statistically significant yet weak negative correlations with various dimensions of a health-promoting lifestyle. For instance, the correlation with the total HPLP-II score was r = -0.074 (p < 0.01). These findings suggest that although a relationship exists, the practical impact of smartphone addiction on overall health-promoting lifestyle is limited. A somewhat stronger, albeit still modest, negative correlation was identified with dietary behavior (r = -0.174, p < 0.01). In contrast, a moderate positive correlation was observed between health-promoting lifestyle dimensions and dietary behavior (r = 0.399, p < 0.01). The detailed results are presented in Table 7.
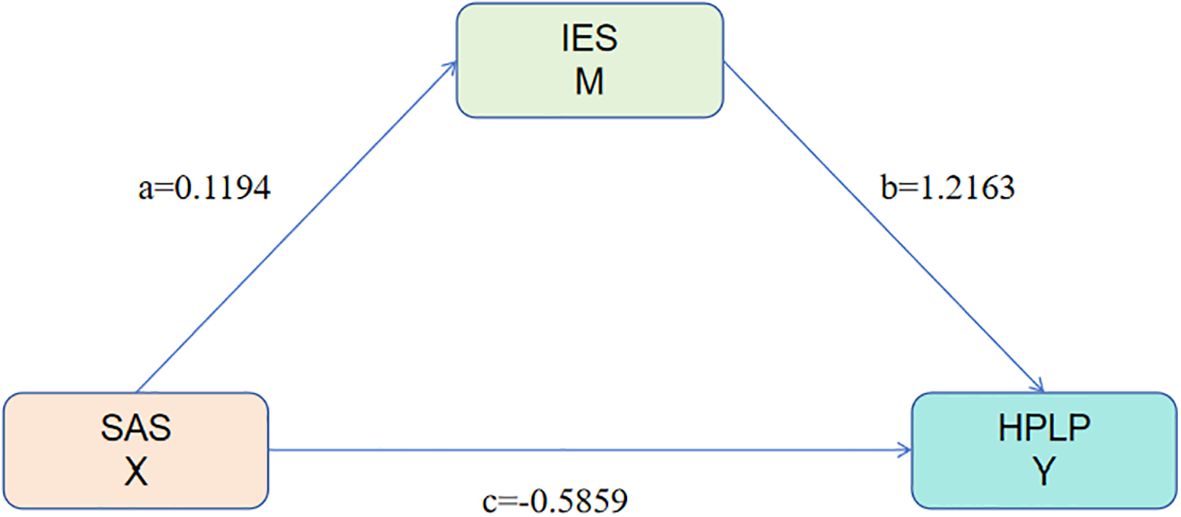
3.6 Mediation analysis
A mediation analysis was performed using SAS as the independent variable, IES as the mediator, and HPLP as the dependent variable (see Table 8). The findings indicated that smartphone addiction exerts a direct negative effect on health-promoting lifestyle, with a coefficient of -0.5859. The IES variable mediates 32.95% of this effect, demonstrating its significant role in the relationship between smartphone addiction and health-promoting lifestyle. Specifically, higher levels of smartphone addiction are associated with increased dietary behavior scores (a = 0.1194) and decreased health-promoting lifestyle scores (c = -0.5859). Moreover, healthier dietary behaviors are positively correlated with higher health-promoting lifestyle scores (b = 1.2163) (Figure 2). These results suggest that dietary behavior serves as a mediator in the relationship between smartphone addiction and health-promoting lifestyle, thereby supporting the study hypotheses.
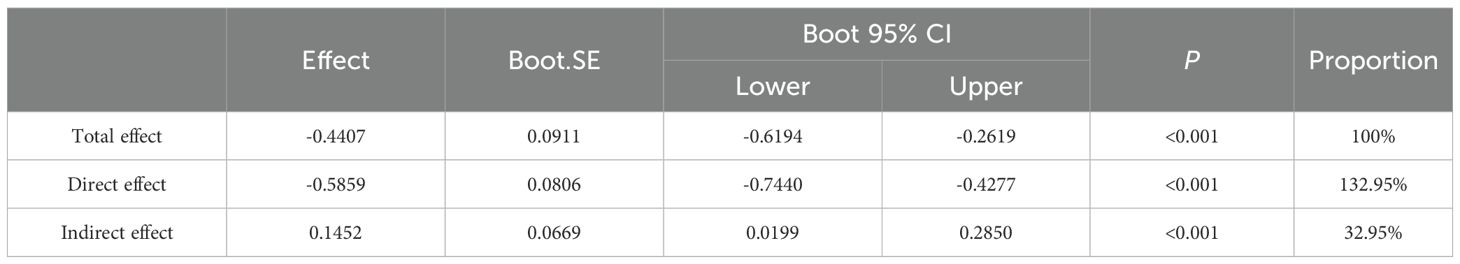
Table 8. Mediating effect of dietary behavior on the relationship between smartphone addiction and health-promoting lifestyle.
4 Discussion
This study investigated smartphone addiction and its association with intuitive eating and health-promoting lifestyles among university students. The primary objective was to assess addiction levels and their influence on dietary habits and health behaviors, thereby providing a foundation for targeted intervention strategies. The analysis revealed no significant differences in basic demographic characteristics -such as gender, living expenses, only-child status, mobile phone usage duration, and BMI - between non-medical and medical students. However, significant differences were observed in household registration and academic year. Given the non-normal distribution of scores across the three measurement scales, median values with interquartile ranges (M [P25, P75]) were employed for statistical analysis. No significant group differences in smartphone addiction were identified concerning gender, living expenses, household registration, or BMI; however, mobile phone usage duration differed significantly between groups. The findings suggest that interventions targeting nighttime phone use and average daily usage duration may contribute to reducing the risk of smartphone addiction among university students. Furthermore, while the within-group prevalence of smartphone addiction was similar between males (55.93%) and females (58.80%), the overall number of addicted participants was higher among females (381 out of 579 addicted individuals, 65.8%). This apparent gender skew is largely attributable to the imbalanced gender distribution in our sample, wherein female students constituted a majority (64.67%). Therefore, the higher absolute number of female addicted participants should not be interpreted as indicating a greater susceptibility to smartphone addiction among females. Instead, these findings suggest that smartphone addiction is prevalent across both genders, with no substantial difference in risk based on sex alone.
Health-promoting lifestyle scores did not differ significantly between medical and non-medical students when considering only-child status. However, significant variations were observed based on household registration, which may reflect the influence of urban versus rural living environments. Additionally, differences in scores across BMI categories suggest a potential association between BMI and engagement in health-promoting behaviors. Higher living expenses correlated with improved health-promoting lifestyle scores, implying greater access to health-enhancing resources. Furthermore, students who reported staying up late using mobile phones exhibited lower health-promoting lifestyle scores. A longer duration of mobile phone use was also linked to reduced scores, indicating that excessive mobile phone usage may detract from time allocated to health-promoting activities.
No significant differences were observed in intuitive eating behavior scores between non-medical and medical students with respect to mobile phone usage, late-night usage, only-child status, living expenses, and BMI. Correlation analysis revealed a negative association between smartphone addiction and a health-promoting lifestyle, suggesting that engagement in healthy behaviors may mitigate digital addiction. Participation in regular offline activities and effective health management strategies appear to reduce reliance on the virtual environment. Additionally, smartphone addiction was found to be negatively correlated with dietary behavior; individuals exhibiting healthier eating patterns demonstrated greater awareness of physiological cues and lower dependence on smartphones (25). Conversely, individuals with disordered eating behaviors may resort to smartphone use to compensate for psychological deficits. In our study, we observed significant differences in dietary behavior scores between urban and rural students (p = 0.03). Specifically, urban students had a median IES-2 score of 74 (IQR: 69, 80.5), while rural students had a median score of 73 (IQR: 69, 79). This suggests that urban students exhibited slightly higher levels of intuitive eating behaviors compared to their rural counterparts. Urban areas typically have greater access to a variety of food options, including a wider range of fresh produce, health food stores, and diverse dining options. This diversity may encourage healthier eating habits and a greater awareness of nutritional needs. Additionally, urban environments often have more resources for health education and promotion, which can influence dietary behaviors. In contrast, rural areas may have more limited access to fresh and diverse food options. The availability of convenience stores and fast-food outlets may be higher, leading to a greater reliance on processed and high-calorie foods. This can impact the overall quality of diet and intuitive eating practices. Most dimensions of a health-promoting lifestyle were positively correlated, underscoring their synergistic interrelations (26). Regular exercisers tended to place greater value on social connections, while those emphasizing health responsibility maintained better sleep hygiene (27). Furthermore, positive correlations between health-promoting lifestyle dimensions and dietary behavior highlight the integrative nature of health practices.
Path coefficient analysis demonstrates that smartphone addiction exerts a significant influence on dietary behavior, indicating that increased smartphone usage can modify eating patterns. Furthermore, this addiction is negatively correlated with a health-promoting lifestyle, highlighting the detrimental impact of digital dependence on healthy living. Healthy eating is linked to improved energy levels and fosters a sense of control over one’s health, thereby establishing a positive feedback loop that extends to exercise and sleep (28, 29). Additionally, dietary behavior mediates the relationship between smartphone addiction and a health-promoting lifestyle, as smartphone use is associated with distorted dietary cognition and behaviors that undermine healthy living.
An educational intervention targeting university students should emphasize literacy by teaching responsible smartphone use and addressing the effects of addiction on physical awareness and dietary habits. Mindfulness training (30) has been shown to enhance awareness of physiological signals (31). Nutrition education should incorporate principles of intuitive eating to assist students in resisting external food cues. Additionally, lifestyle education should focus on dietary behaviors and promote healthy habits, such as regular exercise and positive social interactions (32).
The campus environment exerts a significant influence on the behaviors of university students (33, 34). Higher education institutions should enhance mental health support by offering counseling services and resources for individuals affected by smartphone addiction. A collaborative framework encompassing family, school, and society is essential. Families are encouraged to promote healthy lifestyles, with parents reducing smartphone dependence and fostering regular eating habits and physical activity. Societal support also plays a critical role in encouraging healthy behaviors (35, 36). Future research should incorporate macro-level factors, such as family environment and social culture, to develop a comprehensive model of influences on students’ healthy lifestyles, thereby providing deeper insights and practical strategies for promoting well-being in contemporary society. Although the present study employed Chinese versions of scales previously validated in similar populations, future investigations should further examine the convergent and discriminant validity of these instruments specifically within the context of mainland Chinese university students to strengthen their psychometric robustness for this demographic. The findings of this study should be interpreted in light of its limitations. The use of a convenience sampling method from a single medical university restricts the generalizability of the results. Participants from Xuzhou Medical University may not be representative of the broader population of Chinese college students, who differ substantially in academic pressures, regional cultures, and socioeconomic backgrounds. Consequently, caution is advised when generalizing these findings to other student populations. Additionally, reliance on self-reported data introduces potential biases; participants may underreport undesirable behaviors, such as excessive smartphone use, due to social desirability bias, or may inaccurately recall dietary habits and lifestyle activities, resulting in recall bias.
5 Limitations
This study presents several limitations that warrant consideration. The primary limitation pertains to the sampling strategy employed. Specifically, the use of convenience sampling from a single institution, Xuzhou Medical University, considerably restricts the external validity and generalizability of the findings. The student population at a medical university may possess distinct characteristics, including increased academic demands and higher health literacy, relative to students from other disciplines or institutions. Therefore, the observed prevalence of smartphone addiction and its associations with lifestyle and dietary behaviors may not be representative of the broader population of Chinese college students. To enhance sample representativeness and strengthen the generalizability of future findings, subsequent research should utilize random sampling methods across multiple universities and diverse academic disciplines. Additionally, the cross-sectional design of the current study limits the ability to infer causal relationships, as confounding variables may influence the observed associations. Longitudinal research designs are recommended to monitor the temporal dynamics and interactions among smartphone addiction, dietary behaviors, and health-promoting lifestyles throughout different stages of university students’ development. Finally, reliance on convenience sampling and self-report questionnaires may introduce biases, such as reporting and recall biases, which could compromise the accuracy and interpretation of the results.
6 Conclusion
This study examined the impact of smartphone addiction on eating behaviors and healthy lifestyle practices among students in Xuzhou, China. The findings indicate that smartphone addiction is positively correlated with higher intuitive eating scores, suggesting that individuals with greater addiction levels exhibit increased awareness of hunger and satiety cues. Conversely, smartphone addiction is negatively associated with healthy lifestyle scores, as it diminishes time allocated to physical exercise, social interactions, and adherence to regular routines. Dietary behavior serves as a mediating factor, linking smartphone addiction to overall healthy lifestyle outcomes. Specifically, the influence of addiction on eating habits indirectly undermines broader health-promoting behaviors. Furthermore, negative emotional states stemming from smartphone addiction are related to unhealthy eating patterns, which subsequently adversely affect physical health, exercise motivation, and social confidence, thereby impeding the maintenance of a healthy lifestyle.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Ethics Committee of Xuzhou Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ZD: Conceptualization, Writing – original draft. QP: Writing – original draft, Data curation, Methodology. TF: Methodology, Data curation, Writing – original draft. LX: Methodology, Writing – review & editing. DY: Writing – review & editing, Conceptualization. ZS: Conceptualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was supported by the Project of Philosophy and Social Science Research in Colleges and Universities in Jiangsu Province (grant number: 2024SJYB0817). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1682921/full#supplementary-material
References
1. Andrade ALM, Scatena A, Martins GDG, Pinheiro B, Silva A, Enes CC, et al. Validation of smartphone addiction scale – Short version (SAS-SV) in Brazilian adolescents. Addict Behav. (2020) 110:106540–0. doi: 10.1016/j.addbeh.2020.106540
2. Bueno-Brito C, Pérez-Castro E, and Delgado-Delgado J. Smartphone addiction, anxiety, depression and stress in Mexican nursing students. Rev Cuid. (2024) 15:e3814. doi: 10.15649/cuidarte.3814
3. Meng SQ, Cheng JL, Li YY, Yang XQ, Zheng JW, Chang XW, et al. Global prevalence of digital addiction in general population: A systematic review and meta-analysis. Clin Psychol Rev. (2022) 92:102128. doi: 10.1016/j.cpr.2022.102128
4. Zhong Y, Ma H, Liang YF, Liao CJ, Zhang CC, and Jiang WJ. Prevalence of smartphone addiction among Asian medical students: A meta-analysis of multinational observational studies. Int J Soc Psychiatry. (2022) 68:1171–83. doi: 10.1177/00207640221089535
5. Fallahtafti S, Ghanbaripirkashani N, Alizadeh SS, and Rovoshi RS. Psychometric properties of the smartphone addiction scale – short version (SAS-SV) in a sample of Iranian adolescents. Int J Dev Sci. (2020) 14:19–26. doi: 10.3233/DEV-200002
6. Clavier T, Chevalier E, Demailly Z, Veber B, Messaadi IA, and Popoff B. Social media usage for medical education and smartphone addiction among medical students: national web-based survey. JMIR Med Educ. (2024) 10:e55149. doi: 10.2196/55149
7. Azami Gilan B, Janatolmakan M, Ashtarian H, Rezaei M, Khatony A, and Okosun IS. Health-promoting lifestyle and associated factors among medical sciences students in Kermanshah, Iran: A cross-sectional study. J Environ Public Health. (2021) 2021:1–6. doi: 10.1155/2021/6691593
8. Zhu W, Zhang Y, Lan Y, and Song X. Smartphone dependence and its influence on physical and mental health. Front Psychiatry. (2025) 16:1281841. doi: 10.3389/fpsyt.2025.1281841
9. Li Y, Tian E, Bakar ZBA, and Ashari ZBM. Gender differences in the relationship between bullying victimization and mobile phone addiction among adolescents: the mediating roles of depression and social anxiety. BMC Psychol. (2025) 13:847. doi: 10.1186/s40359-025-03202-0
10. Cao W, Chen C, Hua Y, Li Y, Xu Y, and Hua Q. Factor analysis of a health-promoting lifestyle profile (HPLP): Application to older adults in China's mainland. Arch Gerontol Geriatr. (2012) 55:632–8. doi: 10.1016/j.archger.2012.07.003
11. Karaca O, Yılmaz K, and Yurttaş AN. Reducing smartphone addiction through calisthenic exercises: A randomized controlled trial. Sport Sci Health. (2025) 21:2293–301. doi: 10.1007/S11332-025-01455-1. prepublish.
12. Roberto d, Nogueira NA, Lucilene F, Bonini CJAD, and Viren S. A psychometric investigation of Brazilian Portuguese versions of the Caregiver Eating Messages Scale and Intuitive Eating Scale-2. Eating Weight Disorders: EWD. (2020) 25:221–30. doi: 10.1007/s40519-018-0557-3
13. Ye Z, Zhang T, Peng Y, Rao W, and Jia P. Effects of physical activity on smartphone addiction in Chinese college students-chain mediation of self-control and stress perception. BMC Public Health. (2025) 25:1532–2. doi: 10.1186/S12889-025-22720-5
14. Türkkan T, Bülbül K, Yilmaz HÖ, and Meriç ÇS. The relationship between internet and smartphone addiction and body mass index: The mediating role of eating behaviors. Discov Public Health. (2025) 22:165–5. doi: 10.1186/S12982-025-00550-5
15. Liu H, Zhou Z, Zhu E, Huang L, and Zhang M. Smartphone addiction and its associated factors among freshmen medical students in China: a cross-sectional study. BMC Psychiatry. (2022) 22:308. doi: 10.1186/s12888-022-03957-5
16. Zhao H, Rafik-Galea S, Fitriana M, and Song TJ. Translation and psychometric evaluation of Smartphone Addiction Scale-Short Version (SAS-SV) among Chinese college students. PloS One. (2022) 17:e0278092. doi: 10.1371/journal.pone.0278092
17. Wu R, Guo L, Rong H, Shi J, Li W, Zhu M, et al. The role of problematic smartphone uses and psychological distress in the relationship between sleep quality and disordered eating behaviors among chinese college students. Front Psychiatry. (2021) 12:793506. doi: 10.3389/fpsyt.2021.793506
18. Kwon M, Kim DJ, Cho H, and Yang S. The smartphone addiction scale: development and validation of a short version for adolescents. PloS One. (2013) 8:e83558. doi: 10.1371/journal.pone.0083558
19. Beena D and Sagie DG. Validity and reliability evidence of Health-Promoting Lifestyle Profile (HPLP)-II among nursing students: A confirmatory factor analysis. Teach Learn Nurs. (2022) 17:364–70. doi: 10.1016/J.TELN.2022.05.009
20. Teng HL, Yen M, and Fetzer S. Health promotion lifestyle profile-II: Chinese version short form. J Adv Nurs. (2010) 66:1864–73. doi: 10.1111/j.1365-2648.2010.05353.x
21. Babbott KM, Tylka T, van der Werf B, Consedine NS, and Roberts M. Intuitive Eating Scale-2-EA: Psychometric properties and factor structure of the adapted IES-2 for early adolescents. Eat Behav. (2023) 51:101813. doi: 10.1016/j.eatbeh.2023.101813
22. Ji F, Sun H, Barnhart WR, Cui T, Cui S, Zhang J, et al. Psychometric network analysis of the Intuitive Eating Scale-2 in Chinese general adults. J Clin Psychol. (2024) 80:1098–114. doi: 10.1002/jclp.23657
23. Wang-Chen Y, Kellow NJ, and Choi TST. Exploring the determinants of food choice in chinese mainlanders and chinese immigrants: A systematic review. Nutrients. (2022) 14:346. doi: 10.3390/nu14020346
24. Wang C, Zheng Y, Zhang Y, Liu D, Guo L, Wang B, et al. Dietary patterns in association with hypertension: A community-based study in Eastern China. Front Nutr. (2022) 9:926390. doi: 10.3389/fnut.2022.926390
25. Quiñones JF, Cjuno J, García WCM, and Arias SS. Psychometric properties of the Smartphone Addiction Scale (SAS-SV) in adolescents in Peru. Humanit Soc Sci Commun. (2025) 12:978–8. doi: 10.1057/S41599-025-05285-X
26. Szakály Z, Gáthy AB, Kontor E, Balogh P, and Czine P. Analysis of heterogeneity in consumer attitudes based on the Intuitive Eating Scale-2. Int J Gastron Food Sci. (2024) 38:101039–9. doi: 10.1016/J.IJGFS.2024.101039
27. Karimian Z, Moradi M, and Zarifsanaiey N. Exploring the relationship between contextual factors and health-promoting lifestyle profile (HPLP) among medical students: A cross-sectional study. Health Sci Rep. (2024) 7:e2040–0. doi: 10.1002/HSR2.2040
28. Parsons LE, Wei M, Novak JR, Almeida G, Gast J, and Peak T. Exploring the intuitive eating scale-2 and dyadic associations between mental health and relational dynamics in a sample of married male sexual minority couples. Contemp Family Ther. (2024) 46:455–70. doi: 10.1007/S10591-023-09693-6
29. Bridget W, Amanda G, Katlyn E, and Joseph L. The relationship between social integration and physical activity, diet, and sleep among youths: cross-sectional survey study. JMIR Pediatr Parenting. (2022) 5:e40354–4. doi: 10.2196/40354
30. Liu F, Xi Y, Li N, and Wu M. Brief mindfulness training mitigates college students' Mobile phone addiction: the mediating effect of the sense of meaning in life. Psychol Res Behav Manage. (2024) 17:273–82. doi: 10.2147/PRBM.S439360
31. Flook L, Hirshberg MJ, Gustafson L, McGehee C, Knoeppel C, Tello LY, et al. Mindfulness training enhances students’ executive functioning and social emotional skills. Appl Dev Sci. (2025) 29:141–60. doi: 10.1080/10888691.2023.2297026
32. Matani N, Nazzal MS, Devanprabudoss J, and Aldiabat K. Healthy lifestyle behaviors among Omani undergraduates: a cross-sectional study. Int J Health Promot Educ. (2024) 62:507–16. doi: 10.1080/14635240.2021.2019602
33. Zhang S, Zhang N, Wang S, Hong J, Li F, Guo H, et al. Circadian rhythms and sleep quality among undergraduate students in China: The mediating role of health-promoting lifestyle behaviours. J Affect Disord. (2023) 333:225–32. doi: 10.1016/J.JAD.2023.04.077
34. Qiu Y, Zhao X, Liu J, Li Z, Wu M, Qiu L, et al. Understanding the relationship between smartphone distraction, social withdrawal, digital stress, and depression among college students: A cross-sectional study in Wuhan, China. Heliyon. (2024) 10:e35465. doi: 10.1016/j.heliyon.2024.e35465
35. Ifroh RH, Gai X, Rabiautsani MA, and Han X. The social support, healthy lifestyle, subjective well-being, and health-related quality of life among university students. J Educ Health Promot. (2024) 13:427. doi: 10.4103/JEHP.JEHP_1988_23
Keywords: smartphones, questionnaire, cross-sectional study, dietary behaviors, health-promoting lifestyle
Citation: Ding Z, Pei Q, Fang T, Xiao L, Yin D and Sun Z (2025) Assessment of smartphone addiction and its relationship with health-promoting lifestyle profile and intuitive eating behavior: a cross-sectional study. Front. Psychiatry 16:1682921. doi: 10.3389/fpsyt.2025.1682921
Received: 10 August 2025; Accepted: 22 September 2025;
Published: 03 October 2025.
Edited by:
Liana Fattore, CNR Neuroscience Institute (IN), ItalyReviewed by:
Ali Erdoğan, Akdeniz University Hospital, TürkiyeShivani Phugat, AIIMS, New Delhi, India
Copyright © 2025 Ding, Pei, Fang, Xiao, Yin and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dehui Yin, eWluZGgxNkB4emhtdS5lZHUuY24=; Zhiming Sun, MTA5NjE2MDI5QHFxLmNvbQ==
†These authors have contributed equally to this work
 Zhen Ding1,2†
Zhen Ding1,2† Lishun Xiao
Lishun Xiao Dehui Yin
Dehui Yin