- 1Department of Epidemiology, Columbia University Mailman School of Public Health, New York, NY, United States
- 2Center for Pharmacoepidemiology and Treatment Science, Rutgers University, New Brunswick, NJ, United States
- 3Department of Biostatistics and Epidemiology, Rutgers School of Public Health, Piscataway, NJ, United States
Aims/background: As cannabis use continues to increase in the United States, racialized stereotypes and structural barriers to care might lead to inequitable treatment uptake across racialized groups. A greater understanding of racial disparities in cannabis treatment uptake and perceived treatment need among people with cannabis use disorder (CUD) in community-based samples is needed.
Methods: Nationally representative data from the 2002–2019 National Survey on Drug Use and Health (N=1,005,421) included community-based people ages 12+ First, we assessed trends in CUD (i.e., meeting 2+ DSM-5 proxy CUD criteria) by racialized group. Among people with CUD (n=48,768), weighted logistic models regressed any CUD treatment, specialty CUD treatment, and perceived need for CUD treatment on racialized group and year, adjusting for age, gender, education, insurance, and criminal legal system exposure. We use interaction terms to examine group-specific trend differences.
Results: Overall, 2.64% of the US population ages 12+ had CUD, including 2.47% of white, 1.23% of AAPI (Asian American and Pacific Islander), 4.83% of AIAN (American Indian and Alaska Native), 3.70% of Black, and 2.71% of Hispanic people. CUD increased slightly across all groups (overall annual OR: 1.01, 95% CI =1.01,1.02), with AAPI, Hispanic and people with more than one race seeing steeper increases (ORs: 1.02-1.04). Treatment use and perceived need decreased consistently and there were no group differences in these trends across racialized groups with CUD (ORs: 0.93-0.97). Black people with CUD had 21% lower odds of any treatment than white people (aOR: 0.79, 95% CI=0.65, 0.95). All racialized groups (except AAPI people) had higher odds of perceived need than white people (aORs: 1.59–1.73).
Conclusion: Although all racialized groups had increasing CUD and decreasing CUD treatment use during the study period, the observed racialized disparities also persisted. For example, despite a higher prevalence of CUD among Black people compared to white people, Black people with CUD were less likely than their white counterparts to receive treatment and more likely to report perceived need. These disparities in CUD, treatment use, and perceived need underscore the need for CUD-related services overall and tailored services for racialized minorities, and especially Black people.
1 Introduction
The landscape of cannabis use in the United States has undergone a significant transformation in recent years, marked by legalization across many states (1), increasing availability, and shifting public attitudes (2). As a result of this expanded access and normalization (3–5), cannabis use has had an upward trend across populations in the US over the last couple decades (6, 7). Heavy cannabis use has been linked to adverse health outcomes, such as respiratory diseases (8) or increased risk of vehicle accidents (9) and can lead to cannabis use disorder (CUD), which is associated with cognitive impairments, psychiatric comorbidities, and functional disruptions across multiple domains of life (10–12). However, research on CUD trends for the same period is mixed. While some studies have shown that CUD has increased among some populations, such as veterans and those with chronic pain (13, 14), research looking at the US population overall and using the DSM-IV criteria shows no increases in CUD, despite some specific criteria trending upward (15).
At the same time, CUD treatment has been declining in recent years (16–18). Treatment for CUD can take various forms; evidence-based medical and specialty treatments for CUD include psychosocial approaches (particularly cognitive-behavioral therapy) proven to be the most effective (19). However, research shows that only a small proportion of adults with CUD receive any form of treatment, and even fewer access specialty care within the healthcare system (16). Individuals with CUD often report receiving support outside of formal medical settings, such as through community-based resources (e.g., churches) or peer support groups not specific to cannabis use, like Alcoholics Anonymous or Narcotics Anonymous (16, 20). In light of low treatment use, an important indicator to measure unmet need for treatment is perceived need for treatment, which has been shown to be a strong predictor of future treatment engagement (21, 22). While findings looking at the general population show that overall utilization of CUD treatment and perceived need has been declining in recent years (16–18), more information on racialized disparities in trends is needed.
Racialized minorities have historically experienced inequities in access to and engagement in substance use disorder treatment (23–25). Structural racism may differentially shape the treatment pathways available to different racialized groups—even when rates of treatment might look nominally similar. Structural barriers, such as discrimination within healthcare systems, culturally unresponsive care, stigma, and limited access to affordable, high-quality services (26, 27), may all contribute to lower rates of treatment uptake among racialized groups. Racialized stereotypes about drug use and who is “deserving” of care may further compound these barriers and shape individuals’ experiences of help-seeking (28–30). The criminal legal system also plays a critical role in shaping racialized disparities in substance use treatment, especially CUD treatment. Racist policies, over-policing of low-income racialized minority communities, and differential criminalization of non-White behaviors (31) have long disproportionately harmed Black and Hispanic populations, leading to large disparities in cannabis-related criminalization (31, 32). At the same time, the criminal legal system is the most common referral source for CUD treatment (33). As a result, Black individuals are overrepresented among those referred to CUD treatment by the courts (33), which may shape not only their access to care but the type and quality of care received because court-mandated treatment can function as both a form of correctional supervision and coerced health intervention. Accounting for exposure to the criminal legal system is necessary to fully understand racial disparities in CUD treatment access and engagement.
Although some research has examined racial differences in cannabis use and CUD prevalence (34), less is known about racial disparities in CUD treatment uptake and perceived need within community-based samples during the era of expanding cannabis legalization. This study aims to (1) describe trends over time in CUD using the DSM-5 proxy measure overall and across racialized groups, and (2) investigate trends in CUD treatment uptake and perceived treatment need overall and among different racialized groups in the United States utilizing nationally representative data from the 2002-2019. Using a proxy of the DSM-5 improves the measurement of CUD by replacing the separate DSM-IV categories of “abuse” and “dependence” with a single construct. The DSM-5 measures removed the potentially racially biased legal criterion and added other clinically relevant symptoms (15, 35, 36). By examining these trends, this research seeks to provide valuable insights into the evolving landscape of CUD and CUD treatment disparities across time and inform the development of more equitable and culturally responsive approaches to care. Throughout the manuscript, “racialized groups” is used instead of racial groups to emphasize the actively constructed nature of “race” and racial groups. “Racialized minorities” refers to the non-dominant racialized groups (i.e. non-White racialized groups). See Hochman (37) for more on this conceptual distinction.
2 Methods
2.1 Data and sample
Data sources: The National Survey on Drug Use and Health (NSDUH) is a nationally representative survey of non-institutionalized individuals aged 12 and above from all 50 states and DC. Topics covered include substance use, disorder, treatment, mental illness, and mental health care. We used public-use NSDUH datasets from 2002-2019, which contained about 56,000 records each year (N = 1,005,421). NSDUH underwent methodological changes that impacted the 2015 data collection and onwards. Variables from 2002–2014 and from 2015–2019 were harmonized where appropriate. We cannot include more recent data because of substantive methodological changes in NSDUH starting in 2021, and the COVID-19 data collection disruptions in 2020 (38–40).
Sample: For analyses describing trends in DSM-5 proxy CUD, our sample included all individuals in the NSDUH 2002-2019 (N = 1,005,421). For analyses assessing differences in CUD treatment uptake and perceived need, we restricted our sample to individuals who met past-year DSM-5 proxy CUD (N = 48,768), as described below.
2.2 Measures
2.2.1 Outcome measures
CUD DSM-5-proxy: Study participants were considered to have DSM-5 proxy CUD if they had two or more of the nine criteria collected in the NSDUH, as described in Compton et al., 15. This measure includes nine of the 11 DSM-5 criteria. DSM-5 CUD criterion 4 (“craving”) and criterion 11 (“withdrawal”) were not assessed in NSDUH before 2020 and were therefore not captured.
CUD treatment: Participants were considered as having any past-year CUD treatment if they answered that they had received treatment in any location for any illicit drug use in the past year, and if their last/current treatment episode was for cannabis, as done in previous research (16). Participants were considered as having past-year specialty CUD treatment if they answered that they had received treatment for any illicit drug use in the past year, if their last/current treatment episode was for cannabis, and if this treatment occurred at a specialty facility (i.e., inpatient or outpatient treatment at a hospital, rehabilitation facility, or mental health center).
Perceived need for CUD treatment: Perceived need for treatment was measured by asking participants who did not receive any treatment whether they thought they needed counseling or treatment, and participants who did receive treatment whether they thought they needed additional treatment, for their use of “marijuana or hashish” in the past 12 months.
2.2.2 Covariates
Race/Ethnicity: We categorized race/ethnicity into the following six mutually exclusive racialized groups: non-Hispanic white, non-Hispanic AAPI (Asian American/Pacific Islander/Native Hawaiian), non-Hispanic AIAN (American Indian and Alaska Native), non-Hispanic Black (Black/African American), Hispanic, and non-Hispanic more than one race.
Time: Year was treated as a continuous predictor starting at 0 (for year 2002). Although there was also a major redesign in 2015, previous research has shown that the redesign did not have an effect in the measurement of CUD treatment uptake and perceived treatment need (16).
Individual control variables: The following covariates known to be associated with the outcome (16) were included to improve the precision of our estimates and to facilitate comparisons across our main predictors of interest while holding other factors constant. These adjustments are not intended as a confounding control strategy, and the resulting estimates should not be interpreted causally. Participants were categorized as having lifetime CLS exposure if they answered that they had ever been arrested and/or booked. We adjusted for additional sociodemographic variables such as age (12-17, 18-21, 22-25, 26-34, 35+), education (high school or less, some college or college graduate), interviewer-recorded gender (male, female), and health insurance status (private insurance only, public insurance only, both private and public insurance, other, uninsured). NSDUH has been performing imputation using the predictive mean neighborhood (PMN) method since 1999 for several variables in the survey. NSDUH imputes responses for set groups of demographic and drug usage variables, described in the NSDUH 2019 Editing and Imputation Report (41). NSDUH implements this method in three steps: response propensity (determining probability of response) adjustment, prediction modeling (calculating predicted means), and hot-deck imputation (choosing a “donor” whose non-missing data will be used to fill in the missing values in the “recipient’s” data). Education and insurance status were the only variables in our analysis for which imputation procedures were performed. Among our sample of people meeting criteria for DSM-5 Proxy CUD (N = 48,768), N = 8 had imputed values for education, and N = 315 had imputed or logically assigned values for insurance status.
2.3 Analytical strategy
We first visually assessed trends in DSM-5 proxy CUD and CUD treatment over time overall and separately for racialized groups with plots fitted and smoothed using loess regression.
To assess trends in CUD over time we ran weighted, unadjusted logistic models regressing DSM-5 proxy CUD on the continuous year variable. To see if trends varied by racialized group we added an interaction term between race and continuous year.
To assess racial disparities in CUD treatment, we ran separate weighted logistic regressions modeling the odds of each outcome (i.e., any treatment, specialty treatment, and perceived treatment need) regressed on race and adjusting for age, education, gender, insurance status, CLS exposure, and continuous year.
All analyses used NSDUH’s complex sampling design and survey weights, which produces nationally representative estimates. All data analyses were performed in STATA version 19.5, and all loess plots were generated in R version 4.4.1 using the ggplot2 package version 3.5.1.
3 Results
3.1 Descriptive characteristics of sample
Table 1 explores weighted summary statistics of those meeting criteria for DSM-5 proxy CUD in NSDUH 2002-2019 (N = 48,768). Our weighted sample was 61.8% white, 2.4% AAPI, 1.0% AIAN, 16.7% Black, 15.4% Hispanic, and 2.8% more than one racialized group. The sample was 66.1% male, 27.6% were between the ages 18-21, 44.6% had up to a high school degree, 48.4% had private health insurance, and 43.0% had any lifetime CLS involvement.
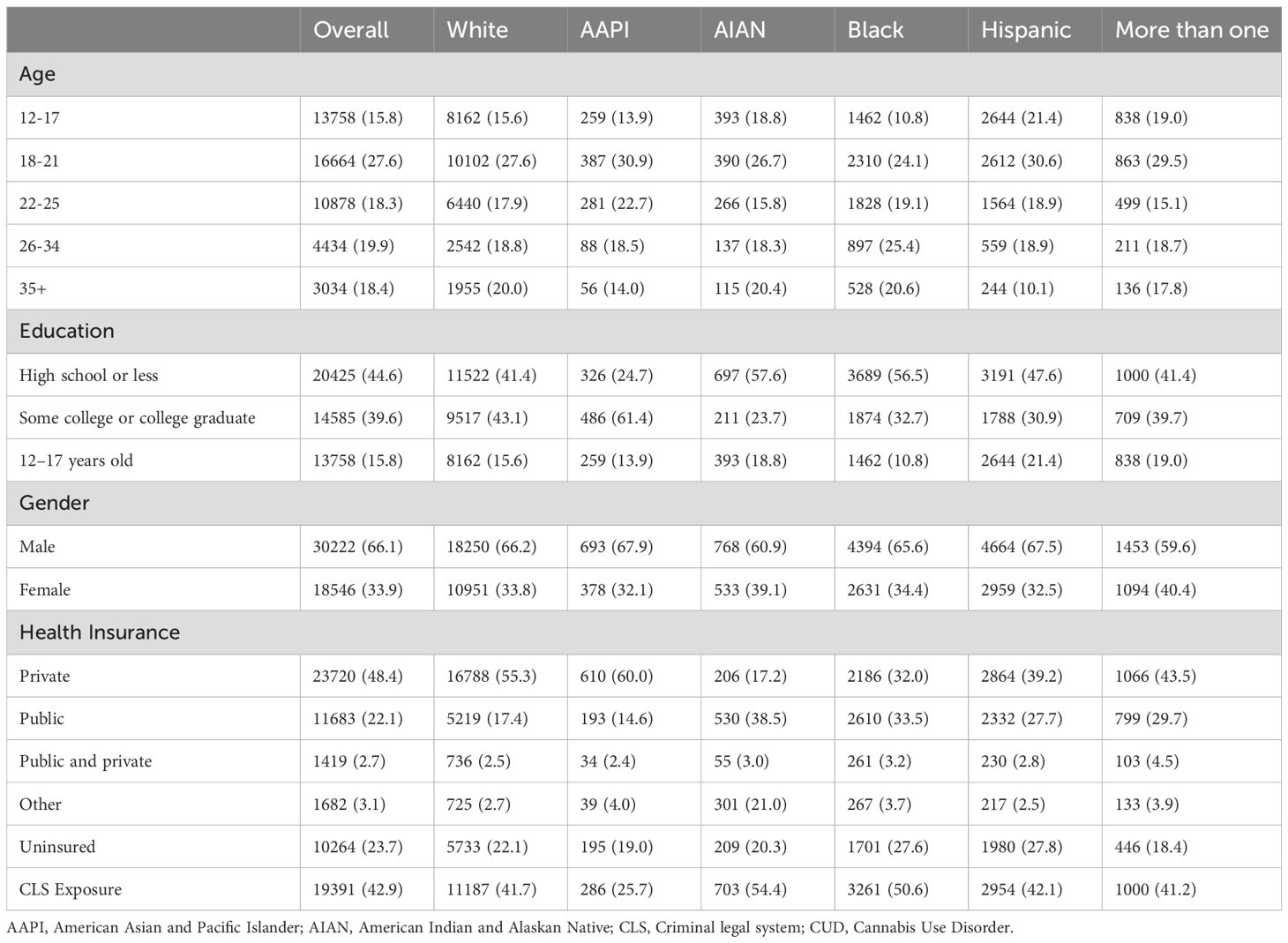
Table 1. Sample characteristics of people aged 12 and older meeting criteria for past-year DSM-5 proxy CUD, NSDUH 2002-2019 (N = 48,768).
3.2 Trends in DSM-5 Proxy CUD
Figure 1 shows weighted prevalences of DSM-5 proxy CUD overall and across racialized groups among the entire NSDUH 2002–2019 sample (N = 1,005,421). During the study period, 2.6% of the US population aged 12+ met the criteria for DSM-5 proxy CUD. By racialized group, 2.5% of white people, 1.2% of AAPI people, 4.8% of AIAN people, 3.7% of Black people, 2.7% of Hispanic people, and 5.0% of people categorized as more than one racialized group met criteria for DSM-5 proxy CUD.
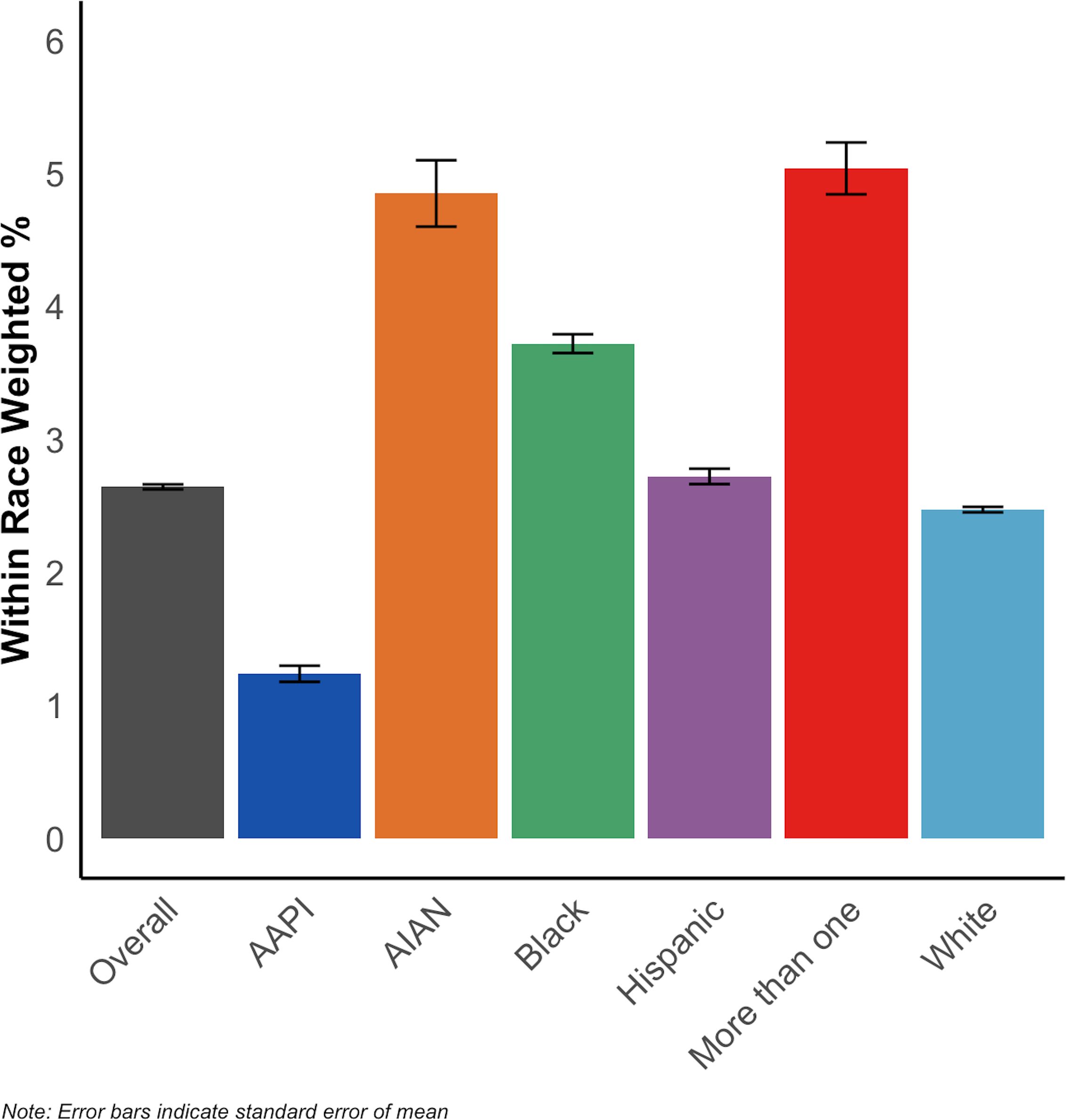
Figure 1. Prevalence of DSM-5 proxy CUD among people aged 12 and older, overall and by racialized group, NSDUH 2002-2019 (N = 1,005,421).
The overall prevalence of DSM-5 proxy CUD increased from 2.4% in 2002 to 3.2% in 2019 (N = 1,005,421). The odds of meeting criteria for DSM-5 proxy CUD among the US population increased by 1 percentage point per each one-year increase between 2002 and 2019 (annual OR = 1.01, 95% CI = 1.01, 1.02). Figure 2 shows the prevalence of DSM-5 proxy CUD increased across all racialized groups. Weighted logistic models regressing CUD on continuous year in Table 2 show the increase in odds of meeting criteria for DSM-5 proxy CUD per each 1 year increase were higher for AAPI people (interaction OR = 1.03, 95% CI = 1.01, 1.05), Hispanic people (interaction OR = 1.01, 95% CI = 1.00, 1.02), and people of more than one race (interaction OR = 1.02, 95% CI = 1.00, 1.04), compared to white people. There were no significant trend differences comparing Black and AIAN people to white people.
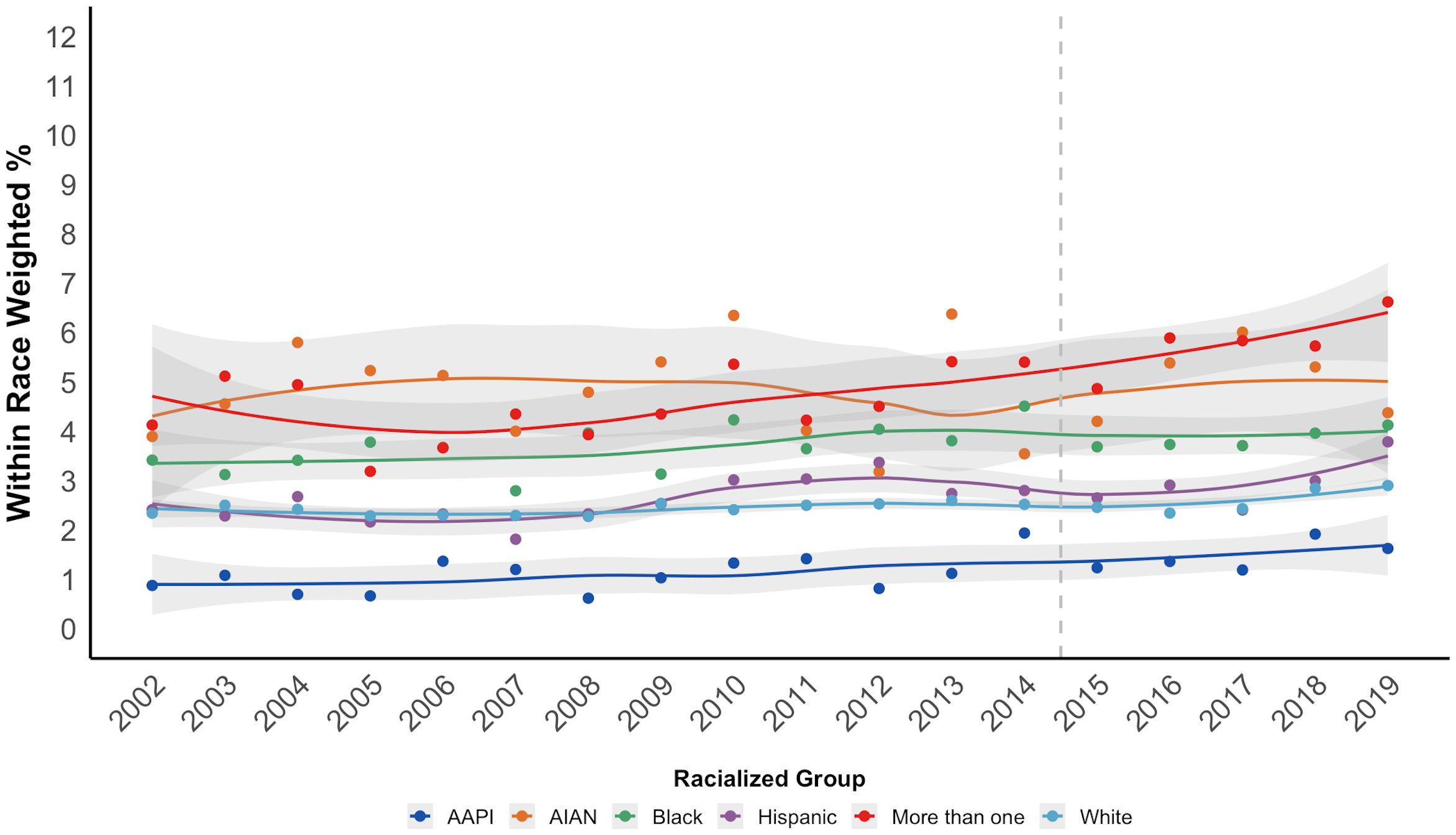
Figure 2. Time trends in prevalence of past-year DSM-5 proxy CUD among people aged 12 and older, by racialized group, NSDUH 2002-2019 (N = 1,005,421).
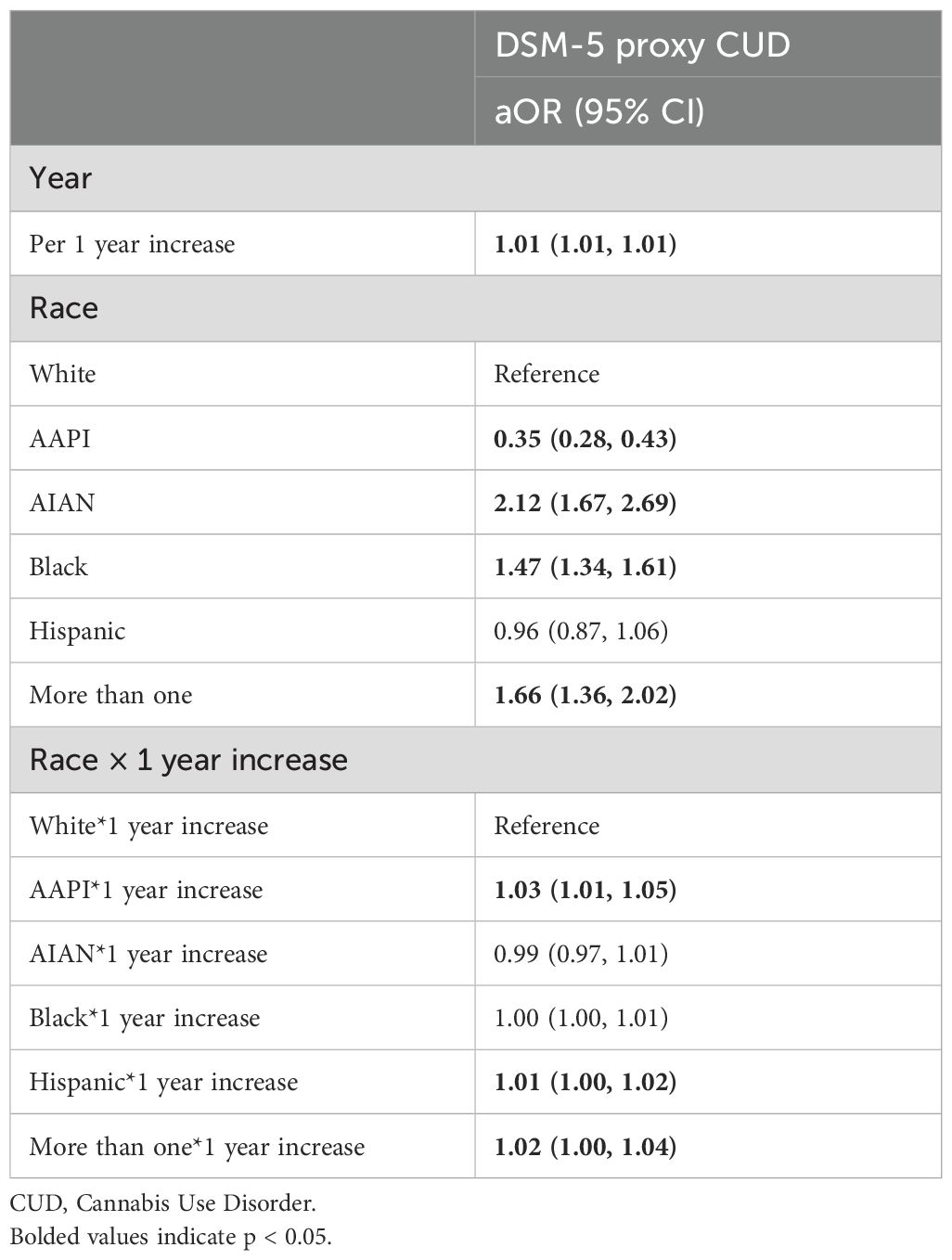
Table 2. Yearly trends in prevalence of DSM-5 proxy cannabis use disorder (CUD) among people aged 12 and older with interaction by racialized group, NSDUH 2002-2019 (N = 1,005,421).
3.3 Trends in CUD treatment uptake and unmet need
Figure 3 shows the prevalence of CUD treatment and perceived need by racialized groups among those with DSM-5 proxy CUD (N = 48,768). 5.8% of white people, 2.8% of AAPI people, 8.0% of AIAN people, 5.4% of Black people, 5.7% of Hispanic people, and 6.6% of people categorized as more than one race received any CUD treatment, while 2.6% of white people, 1.1% of AAPI people, 2.5% of AIAN people, 2.7% of Black people, 2.5% of Hispanic people, and 2.4% of people categorized as more than one race received specialty treatment. Finally, 1.7% of white people, 0.8% of AAPI people, 3.0% of AIAN people, 2.8% of Black people, 2.5% of Hispanic people, and 2.3% of people of more than one race reported unmet need for CUD treatment.
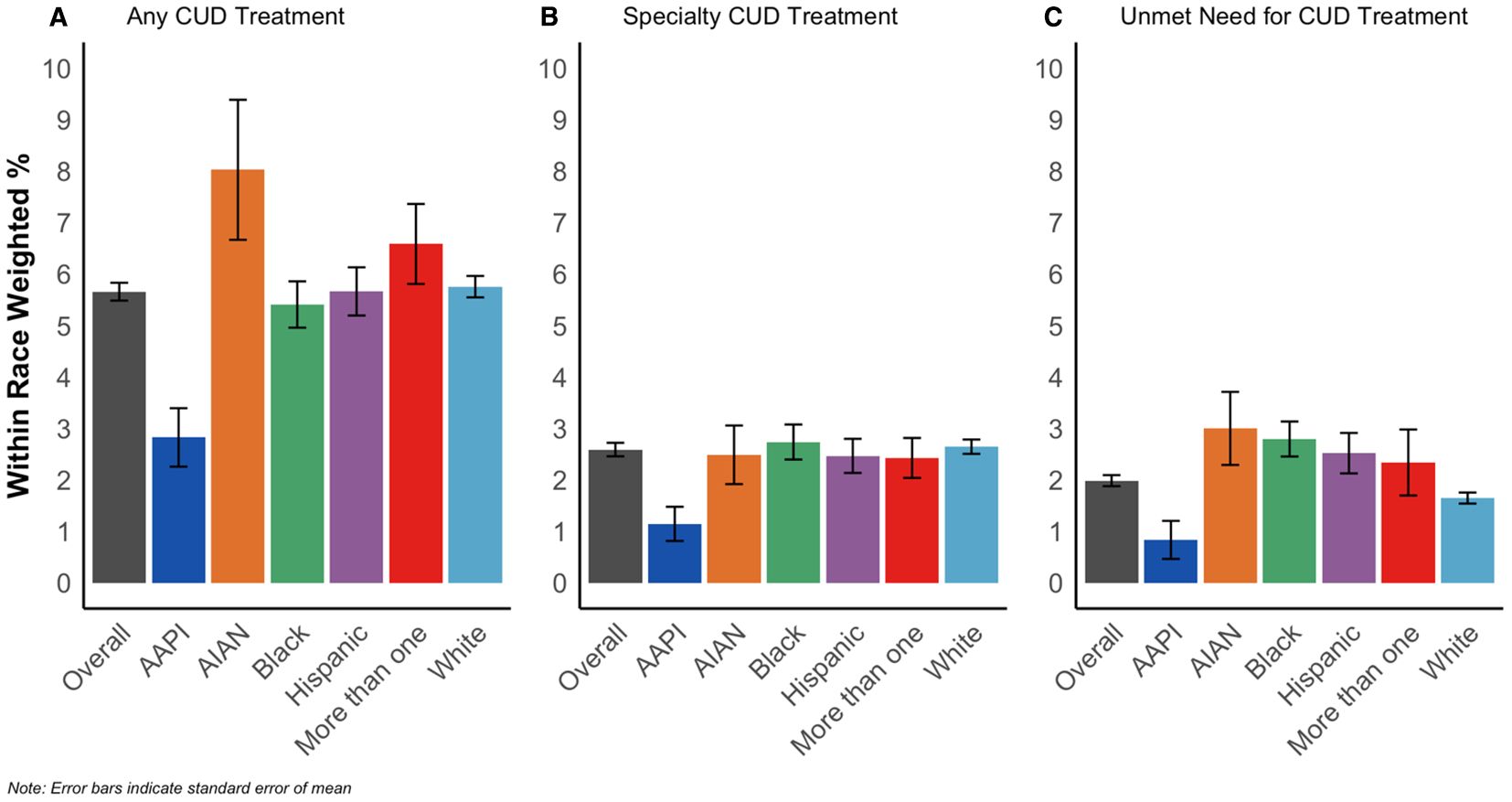
Figure 3. Prevalence of any CUD treatment (A), specialty CUD treatment (B), and unmet CUD treatment need (C) among people with DSM-5 proxy CUD, overall and by racialized group, NSDUH 2002-2019 (N = 48,768).
Figure 4 shows that all three CUD treatment outcomes show a downward trend across racialized groups. In Table 3 we report logistic model estimates confirming this downward trend. For every one-year increase, the odds of reporting CUD treatment decreased by 4% (OR: 0.96, 95% CI = 0.95, 0.98) for any treatment and by 3% for specialty treatment (aOR: 0.97, 95% CI = 0.95, 0.99). For perceived need, the odds decreased by 7% (aOR: 0.93, 95% CI = 0.90, 0.95) for every one-year increase. Testing interaction between continuous year and race found no significant differences in the downward treatment trend across racialized groups (Supplementary Table 1).
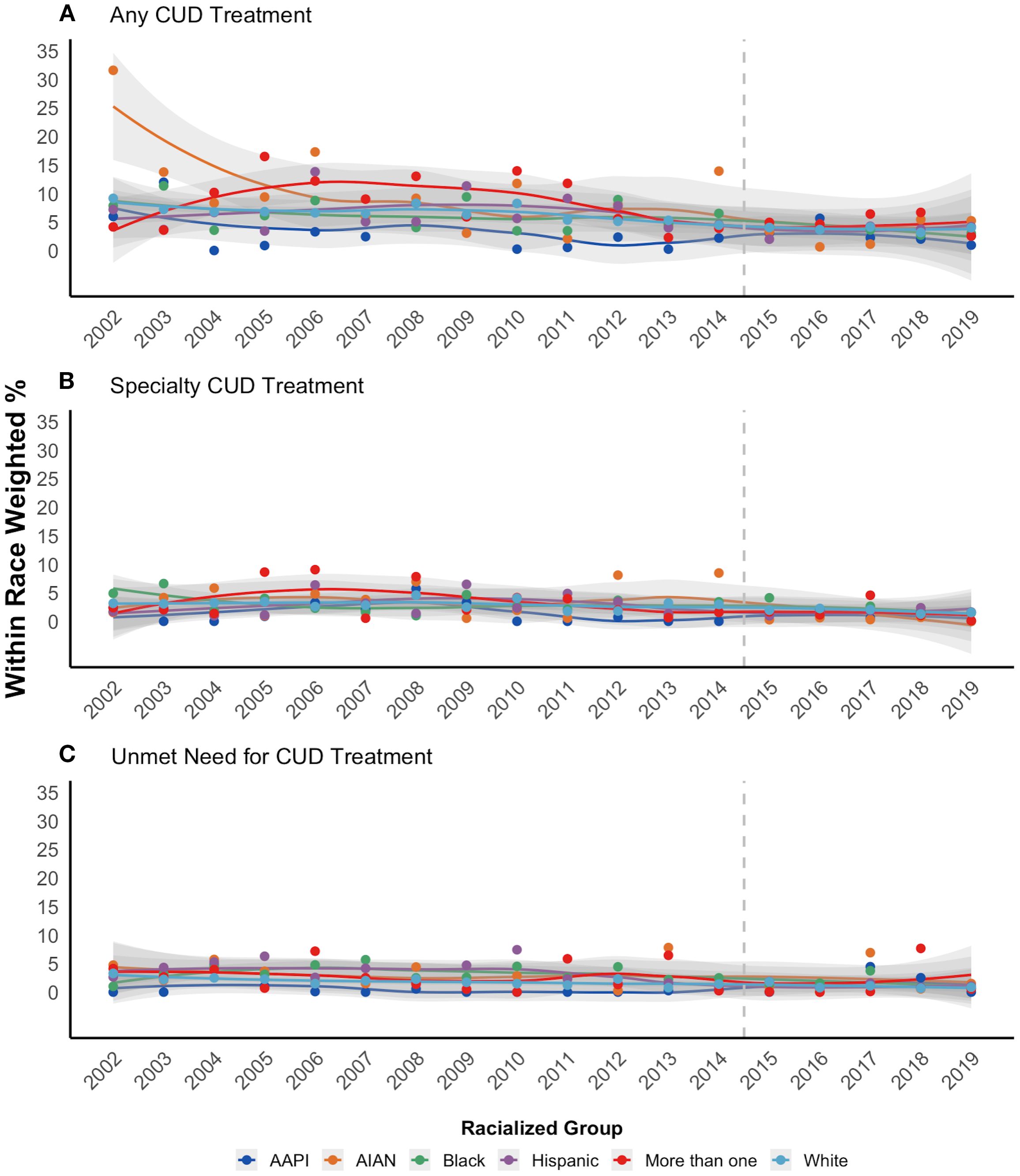
Figure 4. Time trends in prevalence of past-year CUD treatment (A), specialty CUD treatment (B), and unmet CUD treatment need (C) among people aged 12 and older who meet criteria for DSM-5 proxy CUD, by racialized group, NSDUH 2002-2019 (N = 48,768).
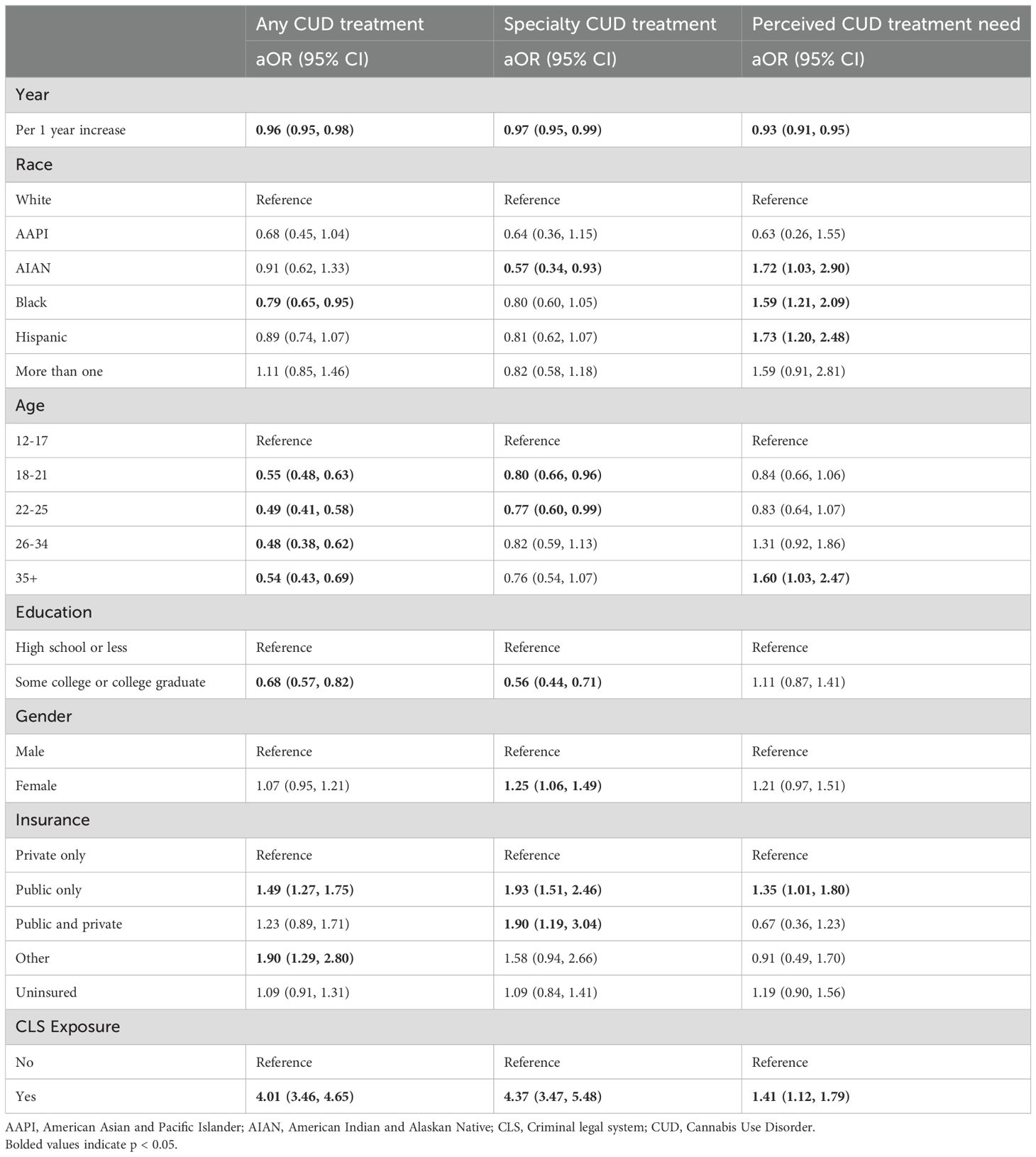
Table 3. Fully adjusted logistic regression models assessing relationship between treatment outcomes and race among people meeting criteria for DSM-5 Proxy CUD, NSDUH 2002-2019 (N = 48,768).
3.4 Racial differences in CUD treatment uptake and unmet need
Table 3 displays weighted logistic model results regressing our three outcomes on racialized group accounting for continuous year, age group, education, binary gender, health insurance status, and lifetime CLS exposure. The adjusted odds of any CUD treatment were significantly lower among Black people compared to white people (aOR = 0.79, 95% CI = 0.65, 0.95), but not for other racialized groups. AIAN people had significantly lower odds of specialty CUD treatment compared to white people (aOR = 0.57, 95% CI = 0.34, 0.93), but this relationship was not significant for other racialized groups. Black (aOR = 1.59, 95% CI = 1.21, 2.09), Hispanic (aOR = 1.73, 95% CI = 1.20, 2.49), and AIAN (aOR = 1.72, 95% CI = 1.03, 2.90) people all had higher odds of perceived treatment need compared to white participants. The odds of any CUD treatment (aOR = 4.01, 95% CI = 3.46, 4.65), specialty CUD treatment (aOR = 4.37, 95% CI = 3.47, 5.48), and perceived need for CUD treatment (aOR = 1.41, 95% CI = 1.12, 1.79) were all higher for those with lifetime CLS exposure compared to those without.
4 Discussion
This study assessed trends in CUD as well as CUD treatment use and perceived need for treatment in 2002–2019 by racial group in a nationally representative sample, describing racial disparities in treatment access and need as well as changes over time. DSM-5 proxy CUD prevalences increased across the population, signaling a growing treatment need in the US. In this same time period, both specialty and any CUD treatment uptake and perceived treatment need diminished over time for all racialized groups with past-year CUD. Decreases in CUD treatment were consistent across racialized groups, which indicates that these inequities have remained stagnant over time.
All racialized minorities with DSM-5 proxy CUD (with the exception of AAPI people) were more likely to report unmet perceived need for treatment when compared to white people with DSM-5 proxy CUD. Looking specifically at treatment, Black people with DSM-5 proxy CUD were less likely than white people to report receiving any CUD treatment, in spite of Black people having slightly higher rates of DSM-5 proxy CUD than white people among the general population. As for specialty treatment, AIAN people with DSM-5 proxy CUD were much less likely to receive specialty treatment than white people with DSM-5 proxy CUD. Decreases in treatment across groups are consistent with previous findings of CUD treatment decreases by age and among young adults (16, 18), and signal that CUD treatment gaps are growing across a range of demographic groups.
There are several reasons that could explain this overall diminishing trend in treatment while CUD increased. Increased access and shifts in public opinion in the last couple decades could have contributed to higher cannabis normalization (3–5), whereas people with CUD might be less likely to perceive a need for treatment and therefore seek out help. However, general barriers to access (such as insurance limiting access to treatment and brief interventions) could also be driving some of this diminishing trends. Changes in the legal status of cannabis across the country, particularly in states with cannabis dispensaries, might have also contributed to the overall observed reduction in treatment uptake (17). Since 2010 arrests for cannabis possession have been diminishing across the US (42), and research has observed that court-mandated treatment episodes in public hospitals have also experienced a downward trend during the same period (43). Another possibility is that the reduction in the prevalence of treatment uptake is a direct result of the increase in CUD prevalence among the general population: if increased access and normalization of CUD are contribution to increases in CUD prevalences but treatment system capacity has remained stagnant—because of structural constraints such as limited infrastructure, workforce shortages, or funding—this would create a supply-side bottleneck, producing an apparent decline in the proportion of people with CUD receiving treatment even if demand is rising.
Together, our findings indicate a general pattern of ongoing racialized access to CUD treatment. Racism and other racialized structural factors might explain this persistent gap. Access to medical services in the US is racialized (44). Black and Hispanic people are more likely to live in areas with fewer providers (27, 45, 46), and more likely to be overrepresented in low-paying jobs with less comprehensive health benefits. At the same time, racialized stigma toward cannabis use, as well as different groups’ perceptions of and lived experiences with the medical systems might impede CUD treatment among different racialized groups (26, 30, 32, 47). Importantly, access to treatment for CUD remains extremely low and the vast majority of people with a disorder do not access treatment.
Lastly, it is important to contextualize our understanding of racialized disparities in treatment uptake at the intersection of SUD treatment and the criminal legal system. Court-mandated treatment makes up the biggest share of referrals for CUD treatment episodes (33; TEDS-A, 2000-2023). Black and Hispanic people are over-represented in their CLS exposure, yet our analyses show that Black people with a CUD are less likely to receive treatment (although not specialty treatment) and more likely to report unmet treatment need. This indicates that, despite racialized structures that overly punish Black people’s consumption of cannabis, and a real reported need for treatment, the system is failing to meet this need.
4.1 Limitations and future research
The NSDUH does not directly measure our main outcomes of treatment need and uptake. Instead, following Askari et al., 16, we constructed composite measures of past-year CUD treatment based on multiple NSDUH variables. This may have resulted in people who received CUD treatment in the past year being misclassified as not having received CUD treatment if it was not their most recent or current treatment. The DSM-5 proxy measure excludes cravings and withdrawal symptoms, which might be underreporting the number of people with mild CUD (35, 48). Due to a structural redesign in the NSDUH, we could not include data after 2020. Because several covariates (e.g., education, insurance status, CLS exposure) are correlated with race and may shift over time, our models may be subject to collinearity, which could inflate standard errors and make it more difficult to isolate and interpret the independent and interactive effects of race and year. Finally, the NSDUH does not include institutionalized people, which makes our findings limited to non-institutionalized populations. Given the disproportionate rates of incarceration among Black and Hispanic populations, we might be underestimating some of the racialized gaps in CUD and CUD treatment among these groups.
Future research should try to understand how structural and cultural factors might explain why racialized minorities are more likely to report unmet treatment need and less likely to receive treatment for their CUD. Future research and clinical efforts should also address barriers to problem recognition, which could include increasing consistency in screening and brief interventions for cannabis (49). Growing social acceptability of cannabis and limited awareness of CUD symptoms, along with minimization of associated harms might prevent people from accessing treatment. More research is needed in understanding whether these barriers also vary across racialized groups. Finally, future research should investigate how changes in the criminalization of cannabis use and the downward trends in arrests and court-mandated CUD treatment (TEDS-A, 2000-2023) may be contributing to the observed downward trends in treatment uptake and need, as well as how CLS exposure, and specifically what types of exposure (e.g., arrest vs parole), fit in with the racial disparities in treatment presented in this study.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health/national-releases/. Data for 2002-2019 were used.
Ethics statement
The studies involving humans were approved by Columbia Institutional Review Board Protocol AAAU8700. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
MTR: Writing – original draft, Writing – review & editing, Conceptualization, Methodology, Investigation, Supervision. AV: Writing – original draft, Writing – review & editing, Visualization, Data curation, Formal analysis, Validation. EE: Writing – review & editing. PM: Conceptualization, Writing – review & editing, Methodology, Supervision.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. ELE is funded by the NIH/NIDA grant (T32DA031099; PIs: Hasin & Martins).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1689719/full#supplementary-material
Supplementary Table 1 | Fully adjusted logistic regression models assessing interaction between continuous year and race on prevalence of CUD treatment among people meeting criteria for DSM-5 Proxy CUD, NSDUH 2002-2019 (N = 48,768). AAPI, American Asian and Pacific Islander; AIAN, American Indian and Alaskan Native; CLS, Criminal legal system; CUD, Cannabis Use Disorder. Bolded values indicate p < 0.05.
References
1. State Medical Cannabis Laws. (2025). Available online at: https://www.ncsl.org/health/state-medical-cannabis-laws.
2. Levy NS, Mauro PM, Mauro CM, Segura LE, and Martins SS. Joint perceptions of the risk and availability of Cannabis in the United States 2002-2018. Drug Alcohol Depend. (2021) 226:108873. doi: 10.1016/j.drugalcdep.2021.108873
3. Lamy FR, Daniulaityte R, Sheth A, Nahhas RW, Martins SS, Boyer EW, et al. Those edibles hit hard”: Exploration of Twitter data on cannabis edibles in the U.S. Drug Alcohol Depend. (2016) 164:64–70. doi: 10.1016/j.drugalcdep.2016.04.029
4. Martins SS, Segura LE, Levy NS, Mauro PM, Mauro CM, Philbin MM, et al. Racial and ethnic differences in cannabis use following legalization in US states with medical cannabis laws. JAMA Network Open. (2021) 4:e2127002. doi: 10.1001/jamanetworkopen.2021.27002
5. Schuermeyer J, Salomonsen-Sautel S, Price RK, Balan S, Thurstone C, Min S-J, et al. Temporal trends in marijuana attitudes, availability and use in Colorado compared to non-medical marijuana states: 2003–11. Drug Alcohol Depend. (2014) 140:145–55. doi: 10.1016/j.drugalcdep.2014.04.016
6. Han BH, Yang KH, Cleland CM, and Palamar JJ. Trends in past-month cannabis use among older adults. JAMA Internal Med. (2025) 185:881–3. doi: 10.1001/jamainternmed.2025.1156
7. Hasin D and Walsh C. Trends over time in adult cannabis use: A review of recent findings. Curr Opin Psychol. (2021) 38:80–5. doi: 10.1016/j.copsyc.2021.03.005
8. Karila L, Roux P, Rolland B, Benyamina A, Reynaud M, Aubin H-J, et al. Acute and long-term effects of cannabis use: A review. Curr Pharm Design. (2014) 20:4112–8. doi: 10.2174/13816128113199990620
9. Asbridge M, Hayden JA, and Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: Systematic review of observational studies and meta-analysis. BMJ (Clinical Res Ed.). (2012) 344:e536. doi: 10.1136/bmj.e536
10. Broyd SJ, van Hell HH, Beale C, Yücel M, and Solowij N. Acute and chronic effects of cannabinoids on human cognition—A systematic review. Biol Psychiatry. (2016) 79:557–67. doi: 10.1016/j.biopsych.2015.12.002
11. Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, et al. Prevalence and correlates of DSM-5 cannabis use disorder 2012-2013: findings from the national epidemiologic survey on alcohol and related conditions–III. Am J Psychiatry. (2016) 173:588–99. doi: 10.1176/appi.ajp.2015.15070907
12. Volkow ND, Swanson JM, Evins AE, DeLisi LE, Meier MH, Gonzalez R, et al. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: A review. JAMA Psychiatry. (2016) 73:292. doi: 10.1001/jamapsychiatry.2015.3278
13. Hasin DS, Saxon AJ, Malte C, Olfson M, Keyes KM, Gradus JL, et al. Trends in cannabis use disorder diagnoses in the U.S. Veterans health administration 2005–2019. Am J Psychiatry. (2022) 179:748–57. doi: 10.1176/appi.ajp.22010034
14. Mannes ZL, Malte CA, Olfson M, Wall MM, Keyes KM, Martins SS, et al. Increasing risk of cannabis use disorder among U.S. veterans with chronic pain: 2005-2019. Pain. (2023) 164:2093–103. doi: 10.1097/j.pain.0000000000002920
15. Compton WM, Han B, Jones CM, and Blanco C. Cannabis use disorders among adults in the United States during a time of increasing use of cannabis. Drug Alcohol Depend. (2019) 204:107468. doi: 10.1016/j.drugalcdep.2019.05.008
16. Askari MS, Keyes KM, and Mauro PM. Cannabis use disorder treatment use and perceived treatment need in the United States: Time trends and age differences between 2002-2019. Drug Alcohol Depend. (2021) 229:109154. doi: 10.1016/j.drugalcdep.2021.109154
17. Mauro PM, Gutkind S, Askari MS, Hasin DS, Samples H, Mauro CM, et al. Associations between cannabis policies and state-level specialty cannabis use disorder treatment in the United States 2004–2019. Drug Alcohol Depend. (2024) 257:111113. doi: 10.1016/j.drugalcdep.2024.111113
18. Mennis J, Stahler GJ, and McKeon TP. Young adult cannabis use disorder treatment admissions declined as past month cannabis use increased in the U.S.: An analysis of states by year 2008–2017. Addictive Behav. (2021) 123:107049. doi: 10.1016/j.addbeh.2021.107049
19. Gates PJ, Sabioni P, Copeland J, Le Foll B, and Gowing L. Psychosocial interventions for cannabis use disorder. Cochrane Database Systematic Rev. (2016) 2016:CD005336. doi: 10.1002/14651858.CD005336.pub4
20. Mauro PM, Kaur N, Askari MS, and Keyes KM. Alcohol or drug self-help use among adults in the United States: age, period, and cohort effects between 2002 and 2018. Int J Ment Health Addict. (2024) 22:2667–81. doi: 10.1007/s11469-023-01012-2
21. Haughwout SP, Harford TC, Castle I-JP, and Grant BF. Treatment utilization among adolescent substance users: findings from the 2002 to 2013 national survey on drug use and health. Alcoholism: Clin Exp Res. (2016) 40:1717–27. doi: 10.1111/acer.13137
22. Mojtabai R and Crum RM. Perceived unmet need for alcohol and drug use treatments and future use of services: Results from a longitudinal study. Drug Alcohol Depend. (2013) 127:59–64. doi: 10.1016/j.drugalcdep.2012.06.012
23. Ben J, Cormack D, Harris R, and Paradies Y. Racism and health service utilisation: A systematic review and meta-analysis. PloS One. (2017) 12:e0189900. doi: 10.1371/journal.pone.0189900
24. Cook BL and Alegría M. Racial-ethnic disparities in substance abuse treatment: The role of criminal history and socioeconomic status. Psychiatr Serv (Washington D.C.). (2011) 62:1273–81. doi: 10.1176/ps.62.11.pss6211_1273
25. Matsuzaka S and Knapp M. Anti-racism and substance use treatment: Addiction does not discriminate, but do we? J Ethnicity Subst Abuse. (2020) 19:567–93. doi: 10.1080/15332640.2018.1548323
26. Earnshaw VA, Mousavi M, Qiu X, and Fox AB. Mental illness and substance use disorder stigma: mapping pathways between structures and individuals to accelerate research and intervention. Annu Rev Clin Psychol. (2025) 21:85–111. doi: 10.1146/annurev-clinpsy-081423-023228
27. Tadmon D and Bearman PS. Differential spatial-social accessibility to mental health care and suicide. Proc Natl Acad Sci. (2023) 120:e2301304120. doi: 10.1073/pnas.2301304120
28. Hansen H and Roberts SK. Two tiers of biomedicalization: METHADONE buprenorphine and the racial politics of addiction treatment. In: Netherland J, editor. Critical perspectives on addiction (2012). p. 79–102. doi: 10.1108/S1057-6290(2012)0000014008
29. Hatcher AE, Mendoza S, and Hansen H. At the expense of a life: race, class, and the meaning of buprenorphine in pharmaceuticalized “Care. Subst Use Misuse. (2018) 53:301–10. doi: 10.1080/10826084.2017.1385633
30. Walters SM, Kerr J, Cano M, Earnshaw V, and Link B. Intersectional stigma as a fundamental cause of health disparities: A case study of how drug use stigma intersecting with racism and xenophobia creates health inequities for Black and Hispanic persons who use drugs over time. Stigma Health. (2023) 8:325–43. doi: 10.1037/sah0000426
31. Najdowski CJ and Stevenson MC. A call to dismantle systemic racism in criminal legal systems. Law Hum Behav. (2022) 46:398–414. doi: 10.1037/lhb0000510
32. Hammarlund R, Crapanzano K, Luce L, Mulligan L, and Ward K. Review of the effects of self-stigma and perceived social stigma on the treatment-seeking decisions of individuals with drug- and alcohol-use disorders. Subst Abuse Rehabil. (2018) 9:115–36. doi: 10.2147/SAR.S183256
33. McElrath K, Taylor A, and Tran KK. Black-white disparities in criminal justice referrals to drug treatment: addressing treatment need or expanding the diagnostic net? Behav Sci (Basel Switzerland). (2016) 6:21. doi: 10.3390/bs6040021
34. Wu L-T, Zhu H, and Swartz MS. Trends in cannabis use disorders among racial/ethnic population groups in the United States. Drug Alcohol Depend. (2016) 165:181–90. doi: 10.1016/j.drugalcdep.2016.06.002
35. Compton WM, Einstein EB, and Han B. 12-month prevalence estimates of substance use disorders using DSM-5 versus DSM-IV criteria among U.S. Nonelderly adults with substance use. Am J Psychiatry. (2024) 181:1018–21. doi: 10.1176/appi.ajp.20231060
36. Fink DS, Shmulewitz D, Mannes ZL, Stohl M, Livne O, Wall M, et al. Construct validity of DSM-5 cannabis use disorder diagnosis and severity levels in adults with problematic substance use. J Psychiatr Res. (2022) 155:387–94. doi: 10.1016/j.jpsychires.2022.09.016
37. Hochman A. Racialization: A defense of the concept. Ethnic Racial Stud. (2019) 42:1245–62. doi: 10.1080/01419870.2018.1527937
38. 2015 NSDUH questionnaire redesign impact assessment, final report. CBHSQ Data. Available online at: https://www.samhsa.gov/data/report/2015-nsduh-questionnaire-redesign-impact-assessment-final-report.
39. 2021 national survey on drug use and health: methodological summary and definitions . Available online at: https://www.samhsa.gov/data/sites/default/files/reports/rpt39442/2021NSDUHMethodSummDefs100422/2021NSDUHMethodSummDefs100422.htm.
40. 2020 national survey on drug use and health: methodological summary and definitions. Available online at: https://www.samhsa.gov/data/sites/default/files/reports/rpt35330/2020NSDUHMethodSummDefs092421/2020NSDUHMethodsSummDefs092421.htm.
41. Substance Abuse and Mental Health Services Administration. 2019 NSDUH MRB editing and imputation report. U.S. Department of Health and Human Services (2020). Available online at: https://www.samhsa.gov/data/sites/default/files/reports/rpt34660/NSDUHmrbEditImputation2019.pdf.
42. Crime in the U.S. (2025). FBI. Available online at: https://ucr.fbi.gov/crime-in-the-u.s.
43. Treatment episode data set—Admissions (TEDS-A) series . Available online at: https://www.icpsr.umich.edu/web/ICPSR/series/56.
44. Lê Cook B, McGuire TG, Lock K, and Zaslavsky AM. Comparing methods of racial and ethnic disparities measurement across different settings of mental health care. Health Serv Res. (2010) 45:825–47. doi: 10.1111/j.1475-6773.2010.01100.x
45. Acevedo A, Panas L, Garnick D, Acevedo-Garcia D, Miles J, Ritter G, et al. Disparities in the treatment of substance use disorders: does where you live matter? J Behav Health Serv Res. (2018) 45:533. doi: 10.1007/s11414-018-9586-y
46. Eberth JM, Hung P, Benavidez GA, Probst JC, Zahnd WE, McNatt M-K, et al. The problem of the color line: spatial access to hospital services for minoritized racial and ethnic groups. Health Affairs. (2022) 41:237–46. doi: 10.1377/hlthaff.2021.01409
47. Adams C, Chatterjee A, Harder BM, and Mathias LH. Beyond unequal access: Acculturation, race, and resistance to pharmaceuticalization in the United States. SSM - Population Health. (2018) 4:350–7. doi: 10.1016/j.ssmph.2018.04.003
48. Hasin D and Stohl M. Higher prevalence estimates of substance use disorders with DSM-5 versus DSM-IV criteria among U.S. Nonelderly adults with substance use: the role of DSM-IV diagnostic orphans. Am J Psychiatry. (2024) 181:955–7. doi: 10.1176/appi.ajp.20240852
Keywords: cannabis use disorder, cannabis treatment, cannabis treatment need, racialized differences, cannabis trends
Citation: Triguero Roura M, Vora A, Eschliman EL and Mauro PM (2025) Trends in cannabis use disorder and treatment by race and ethnicity, 2002–2019. Front. Psychiatry 16:1689719. doi: 10.3389/fpsyt.2025.1689719
Received: 20 August 2025; Accepted: 19 September 2025;
Published: 05 November 2025.
Edited by:
Samantha Goldfarb, Florida State University, United StatesReviewed by:
Heather Barkholtz, University of Wisconsin-Madison, United StatesDongze Chen, Peking University Cancer Hospital & Institute, China
Copyright © 2025 Triguero Roura, Vora, Eschliman and Mauro. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mireia Triguero Roura, bXQzMTk3QGNvbHVtYmlhLmVkdQ==
†Present address: Pia M. Mauro, Center for Pharmacoepidemiology and Treatment Science, Rutgers Institute for Health, Health Care Policy and Aging Research, New Brunswick, NJ, United States
Department of Biostatistics and Epidemiology, Rutgers School of Public Health, Piscataway, NJ, United States
 Mireia Triguero Roura
Mireia Triguero Roura Aabha Vora
Aabha Vora Evan L. Eschliman
Evan L. Eschliman Pia M. Mauro1,2,3†
Pia M. Mauro1,2,3†