- 1The Second School of Clinical Medicine, Zhejiang Chinese Medical University, Hangzhou, Zhejiang, China
- 2Department of Gastroenterology, Hangzhou Third People’s Hospital, Hangzhou, Zhejiang, China
This case series reports three pregnant women with acute hepatitis B virus (AHB) infection, exploring their clinical outcomes and comorbid anxiety. All three patients presented with abnormal liver function and positive HBV markers. They received supportive therapy (liver-protective, enzyme-lowering agents, etc.), achieving HBsAg clearance and virological cure, with normal liver function during follow-up (one patient lost to follow-up). Despite favorable biomedical outcomes, all experienced significant anxiety over maternal-fetal health and disease progression. This study emphasizes that AHB in pregnancy, though usually self-limited, requires integrating psychosocial support into multidisciplinary management to address perinatal mental health, supporting WHO’s 2030 viral hepatitis elimination goal.
Introduction
Despite effective vaccines and antiviral drugs, hepatitis B virus (HBV) continues to pose a major global public health challenge. Aiming to eliminate viral hepatitis as a public health threat by 2030, the World Health Assembly endorsed the Global Health Sector Strategy (GHSS-VH) 2016–2021 in May 2016 (1). The strategy defines elimination as achieving a 65% reduction in mortality and a 90% reduction in incidence (1). Approximately 5-10% of patients with acute hepatitis B (AHB) progress to chronic infection, which may further develop into liver cirrhosis or even hepatocellular carcinoma; a small proportion of patients may also experience acute liver failure (2). Compared with immunocompetent adults, pregnant women are more likely to progress to chronic HBV infection following acute exposure due to pregnancy-associated immunological alterations. However, AHB during pregnancy is relatively uncommon in clinical reports. Studies revealed that maternal hepatitis B surface antigen (HBsAg) carriage was significantly associated with an increased risk of pregnancy-induced hypertension, gestational diabetes mellitus, meconium peritonitis, postpartum hemorrhage, intrahepatic cholestasis, fetal distress, cesarean delivery and macrosomia (3–6). Furthermore, HBV load during the second trimester was identified as an independent risk factor for preterm birth, with each log10 increase in viral load corresponding to an 18% elevation in risk. The risk of preterm delivery was 2.10 times higher in HBV DNA-positive carriers than in their DNA-negative counterparts (7).
Pregnancy is a period of heightened vulnerability to psychological distress, with anxiety disorders affecting approximately 20% of pregnant individuals (8). A meta-analysis found that one in five women in low- and middle-income countries experiences anxiety disorders during pregnancy and the postpartum period (9). Individuals with resolved HBV infection had an elevated risk of depression relative to uninfected individuals (8.5% vs. 10.6%) (10). In another survey, anxiety and depression were reported in 24.5% and 45.9% of individuals with HBV infection, respectively (11). However, little is known about the psychological burden in women with acute HBV infection, as most literature focuses on chronic HBV or non-infectious perinatal anxiety.
Therefore, pregnant women with acute HBV infection are at risk not only of hepatic decompensation but also of significant psychological distress. This report describes three cases of acute HBV infection concurrent with pregnancy. However, despite achieving virological cure, the patient still experienced significant psychological distress. This outcome underscores the imperative need to integrate psychosocial support into comprehensive hepatitis management strategies alongside biomedical care.
Case report
Case 1
Patient information
A 28-year-old woman was admitted with HBsAg positivity for 6 days and abnormal liver function tests for 1 day. She had undergone hospitalization in the gynecology department for a missed abortion 6 days earlier, during which hepatitis B serology revealed HBsAg >250.00 IU/mL, hepatitis B e antigen (HBeAg) 55.719 S/CO, hepatitis B core antibody (HBcAb) 3.42 S/CO, and IgM antibody against HBcAg (HBcAb-IgM) 0.07 S/CO. At that time, liver function and complete blood count (CBC) were normal. She subsequently underwent dilation and curettage, with pathology confirming degenerated villous tissue.
Her past medical history included a dental procedure two months prior. She denied blood transfusions, other surgeries, or known HBV infection. Obstetric history included gravida 3, para 1, with two induced abortions. Her last menstrual period was December 29, 2016. She denied unsafe sexual contact. Her husband and son were negative for hepatitis B markers, and there was no family history of HBV.
Clinical findings
On admission, she was asymptomatic, with the exception of mild scleral icterus.
Timeline
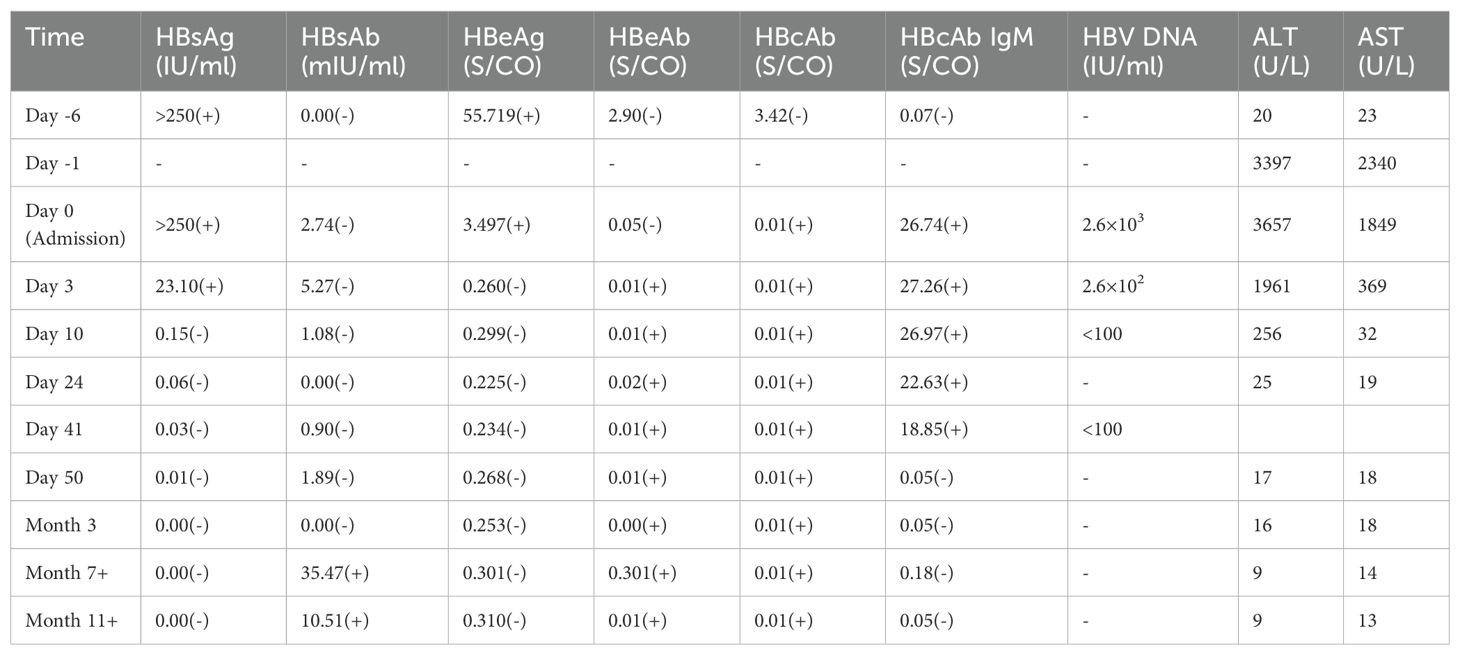
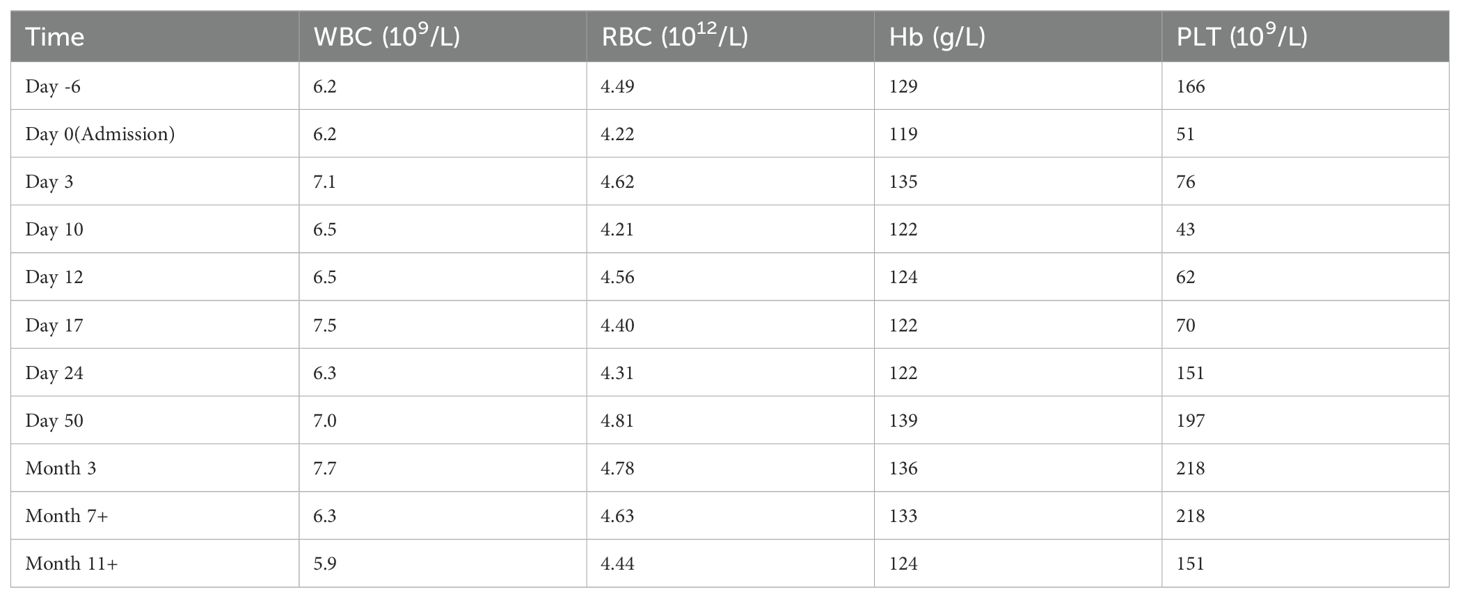
Day -6: Hospitalized for missed abortion, HBsAg >250 IU/mL detected. Day -2: Dilation and curettage performed. Day 0 (Admission): HBsAg >250 IU/mL, HBeAg 3.497 S/CO, HBcAb IgM 26.74 S/CO, HBV DNA 2.6×10³ IU/mL, ALT 3657 U/L, AST 1849 U/L, TBil 42.1 μmol/L, DBil 28.5 μmol/L, WBC 6.2×109/L, Hb 119 g/L, PLT 51×109/L. Week 2: HBsAg seroconverted to negative. Day 50: HBcAb IgM became undetectable. Month 7+: Anti-HBs appeared (Tables 1, 2).
Diagnostic assessment
Laboratory tests showed acute hepatocellular injury with elevated ALT/AST and positive HBV markers. Tests for hepatitis A, C, D, and E were negative, as were serologies for cytomegalovirus and Epstein-Barr virus. Autoantibodies (ANA, SLA/LP, anti-LKM) were negative. Abdominal ultrasound showed a hepatic cyst and chronic cholecystitis. Based on clinical, serological, and virological findings, a diagnosis of AHB was made.
Therapeutic intervention
She received supportive treatment with liver-protective and enzyme-lowering medications, including compound glycyrrhizin, reduced glutathione, and adenosylmethionine.
Follow-up and outcomes
Two weeks after admission, HBsAg became negative. HBcAb IgM became undetectable by day 50, and anti-HBs appeared more than seven months later. HBV DNA clearance was synchronized with HBsAg seroconversion. Liver function normalized and remained stable during one year of follow-up.
Patient perspective
During follow-up, the patient reported persistent depressed mood and difficulty concentrating on work, reflecting significant psychological distress despite favorable biomedical recovery.
Case 2
Patient information
A 23-year-old woman at 8 weeks of gestation presented with a two-week history of aversion to greasy food and one week of fatigue. Past medical history was unremarkable; she denied blood transfusions, surgical procedures, or hepatitis B infection. Obstetric history: gravida 0, last menstrual period April 12, 2018. She denied high-risk sexual behavior. Family history was negative for hepatitis B.
Clinical findings
On admission, physical examination was unremarkable.
Timeline
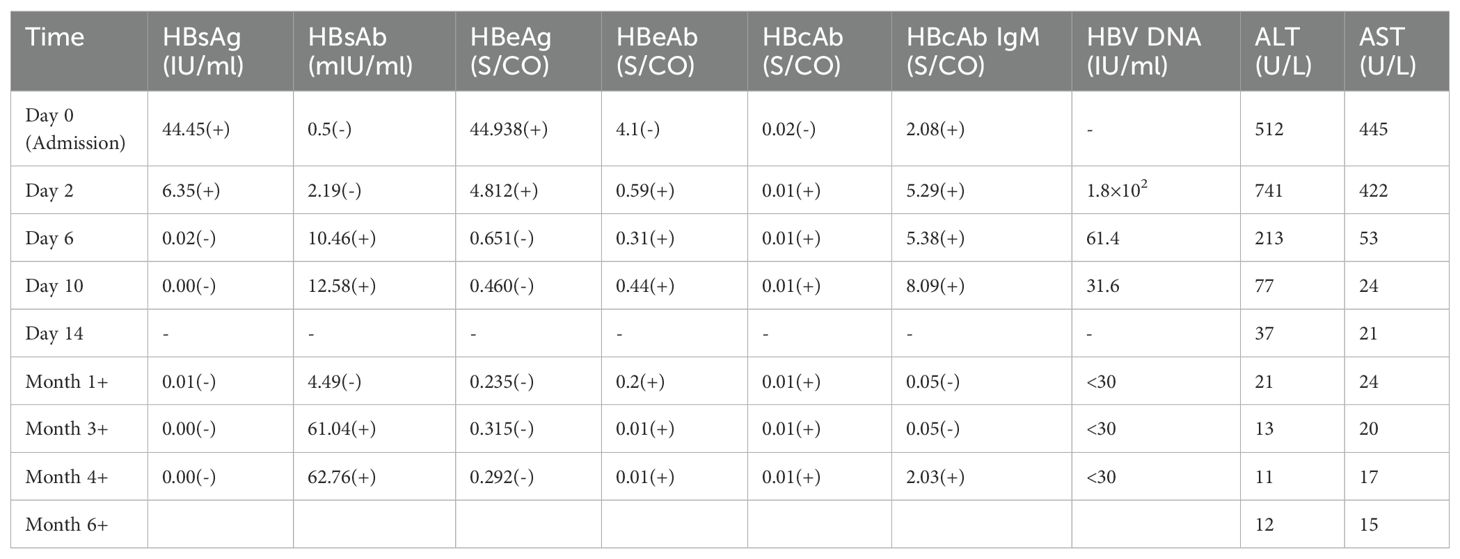
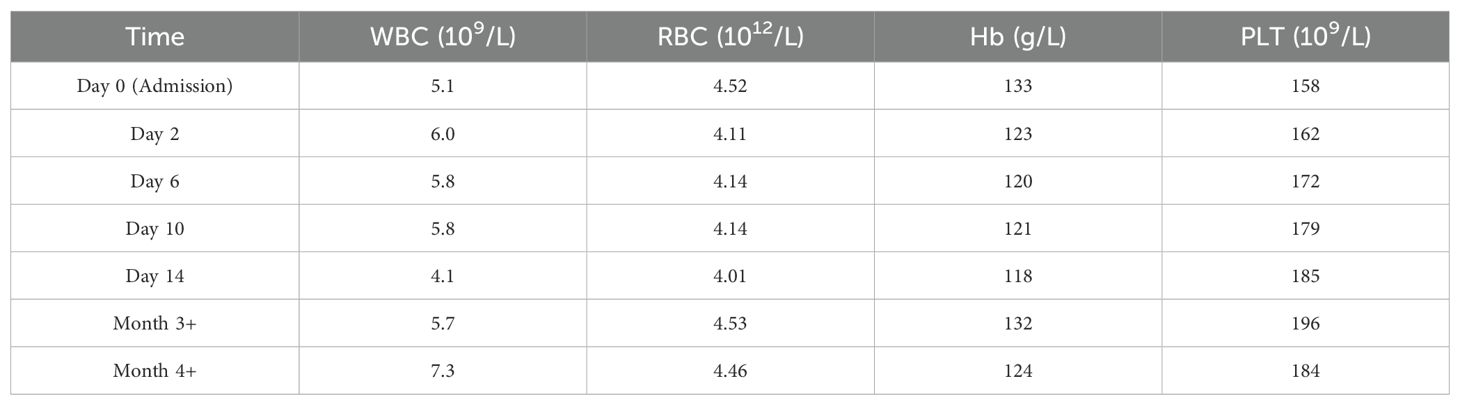
Day -14: Onset of aversion to greasy food. Day -7: Development of fatigue. Day 0 (Admission): HBsAg 44.45 IU/mL, HBeAg 44.938 S/CO, anti-HBc IgM 2.08 S/CO. ALT 512 U/L, AST 445 U/L, TBil 15 μmol/L. HBV DNA 1.8×10² IU/mL, Intrauterine early pregnancy confirmed by ultrasound. Hospital Day 6: HBsAg became negative, anti-HBs positive. Month 1: HBV DNA undetectable. Month 6: Liver function remained normal during follow-up (Tables 3, 4).
Diagnostic assessment
CBC was normal. Serologies for hepatitis A, C, D, and E, and non-hepatotropic viruses were negative. Autoantibody panels were negative. Abdominal ultrasound showed a hyperechoic hepatic nodule consistent with hemangioma. Serum β-hCG was 2057.4 IU/L; gynecological ultrasound confirmed intrauterine pregnancy. Diagnosis: AHB with early intrauterine pregnancy.
Therapeutic intervention
Supportive treatment was provided with liver-protective therapy (compound glycyrrhizin) without antiviral agents.
Follow-up and outcomes
HBsAg clearance occurred by hospital day 6, and HBV DNA became undetectable within one month. Liver function remained normal during six months of follow-up.
Patient perspective
Despite favorable clinical improvement, the patient persistently expressed marked anxiety regarding liver failure and potential fetal harm. Even after repeated reassurance by physicians, her anxiety remained high throughout hospitalization and follow-up.
Case 3
Patient information
A 25-year-old woman at 10 weeks of gestation presented with one week of dizziness and fatigue, accompanied by low-grade fever and a generalized pruritic rash for one day. Past medical history was unremarkable; she denied transfusions, surgery, or prior HBV infection. Obstetric history: gravida 0, last menstrual period March 20, 2018. She denied high-risk sexual behavior. Family history was negative for hepatitis B. Pre-pregnancy serological screening confirmed HBsAg negativity.
Clinical findings
On admission, she exhibited mild scleral icterus and scattered erythematous skin eruptions on the upper limbs.
Timeline
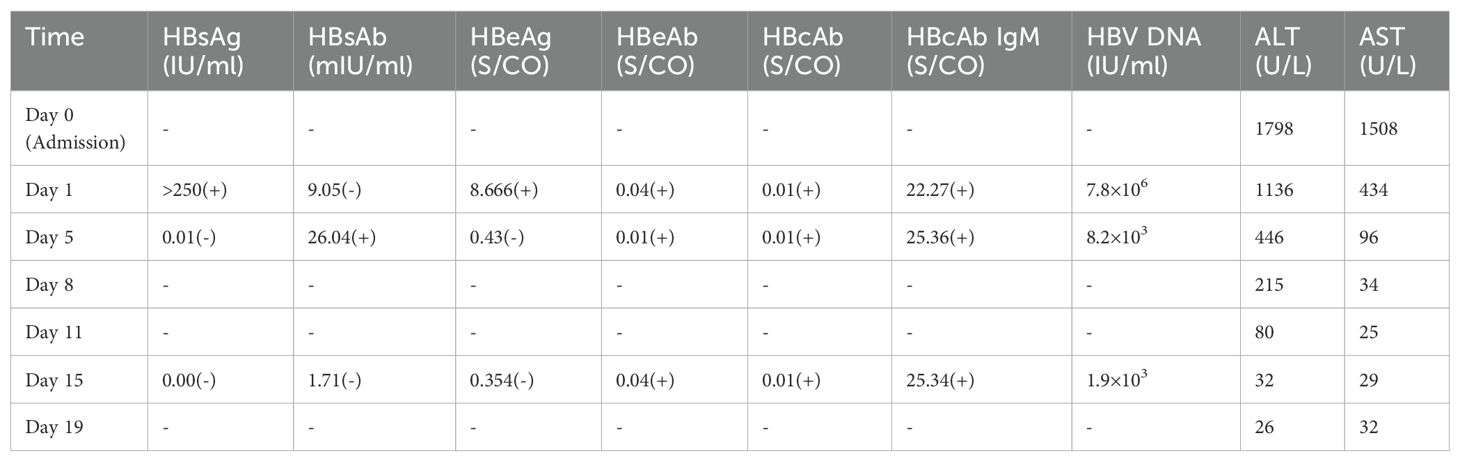
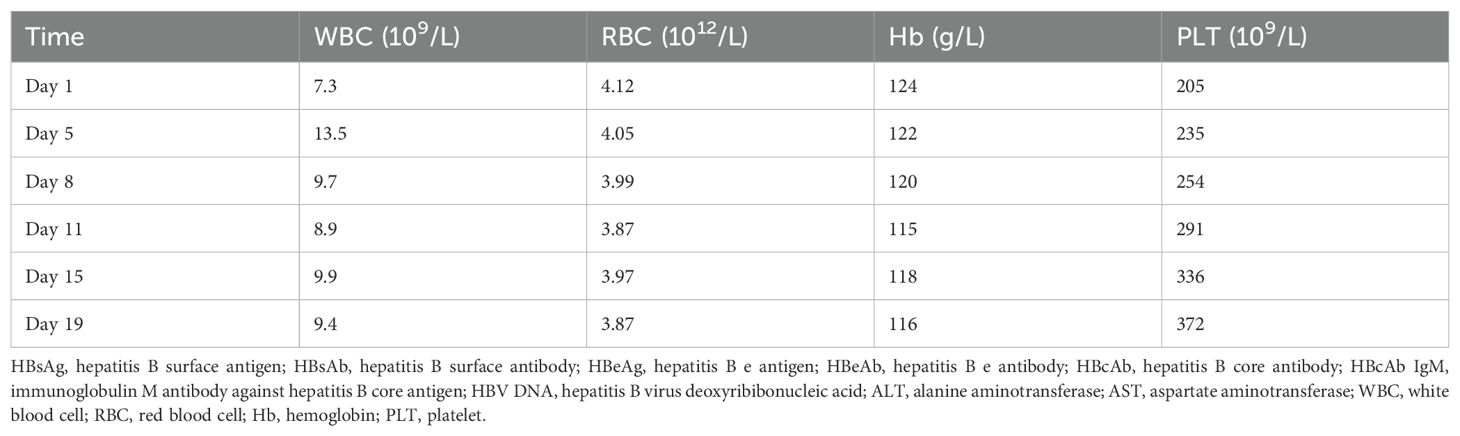
Day -7: Onset of dizziness and fatigue. Day -1: Development of low-grade fever and generalized rash. Day 0 (Admission): ALT 1798 U/L, AST 1508 U/L, TBil 51.8 μmol/L. Day 1: HBsAg >250 IU/mL, HBeAg 8.666 S/CO, anti-HBc IgM 22.27 S/CO. HBV DNA 7.8×106 IU/mL, ALT 1136 U/L, AST 434 U/L. Coagulation: mildly prolonged PT, no encephalopathy. CBC normal. Abdominal ultrasound: slight increase in hepatic echogenicity. Hospital Day 5: HBsAg negative, anti-HBs positive. Hospital Day 15: HBV DNA declined to 1.9×10³ IU/mL with marked biochemical improvement. Post-discharge: Patient did not return for further follow-up (Tables 5, 6).
Diagnostic assessment
Serologies for hepatitis A, C, D, and E viruses were negative. Non-hepatotropic viral panels were negative. Autoantibody screening revealed anti-mitochondrial antibody M2 positivity, raising the possibility of primary biliary cholangitis (PBC), though no follow-up evaluation was completed. Gynecological ultrasound confirmed a viable intrauterine pregnancy. Based on acute onset and serology, she was diagnosed with AHB with intrauterine pregnancy.
Therapeutic intervention
She received supportive therapy with liver-protective, enzyme-lowering, cholagogic, and antijaundice agents (compound glycyrrhizin, polyenylphosphatidylcholine, and adenosylmethionine).
Follow-up and outcomes
During hospitalization, the patient demonstrated rapid clinical and virological improvement. However, she did not return for post-discharge follow-up, limiting assessment of long-term outcomes or further evaluation of possible PBC.
Patient perspective
The patient reported profound anxiety about her prognosis and fetal health. She repeatedly sought reassurance from physicians regarding potential complications, vertical transmission risk, and long-term impacts, despite favorable virological and biochemical responses. Her persistent psychological distress underscored the significant mental health burden associated with perinatal HBV infection.
Discussion
AHB during pregnancy, though uncommon, is a clinically important condition that requires multidisciplinary management. This case series presents a unique perspective on the management and implications of AHB during pregnancy.
In most adults with intact immunity, AHB is a self-limited condition, with spontaneous viral clearance achieved in over 90% of cases through a robust T cell-mediated immune response (12). From an immunological perspective, the ability of AHB patients to clear infection is largely driven by vigorous CD8+ T cell activation. Markers such as CD69 and CD178 on CD8+ lymphocytes indicate enhanced cytotoxic and apoptotic activity, explaining why most AHB patients, unlike chronic carriers, succeed in eliminating HBV (13–15). However, pregnancy creates a unique immune environment where the mother’s cellular immune response is temporarily suppressed. This adaptation helps her body tolerate the developing fetus, which expresses foreign (paternal) antigens. Elevated levels of progesterone, estrogen, and human chorionic gonadotropin exert inhibitory effects on T cell function, resulting in weakened HBV-specific CD8+ responses compared with non-pregnant individuals (16). Consequently, pregnant women exposed to HBV may be at greater risk of progression to chronic infection. Furthermore, the clearance of HBsAg and seroconversion may be delayed in pregnant women with AHB compared to non-pregnant individuals with the same condition (17).
In the first patient analyzed, who was in the latent period following AHB infection, the dynamic changes of HBsAg viral markers during the AHB could be fully observed. HBcAb-IgM appeared 7 days later than HBsAg and HBeAg, persisted for 50 days, and HBsAg disappeared after 16 days. HBsAb appeared at 7 months, HBeAg disappeared on day 10 of the disease course, accompanied by the appearance of HBeAb positivity. The duration of HBV DNA was synchronized with HBsAg, disappearing at 16 days of the disease course. ALT and AST levels returned to normal within 1 month. During the disease course, this patient developed thrombocytopenia, with the lowest platelet count detected at 43×109/L. As the patient showed no significant bleeding, no intervention was taken, and close monitoring was maintained. The thrombocytopenia persisted for 24 days and subsequently resolved. It is speculated that the thrombocytopenia may be associated with the onset of HBV infection. In the second patient analyzed, who was positive for HBsAg on admission but seroconverted to negative on the sixth day of hospitalization. Given the relatively low HBV DNA level, it is considered that partial spontaneous viral clearance had already occurred prior to admission. Following HBsAg seroconversion, transitions in HBsAb and HBeAg were observed shortly afterward. HBV DNA became undetectable one month later than HBsAg, and HBcAb IgM disappeared within 1 month after admission. AST and ALT levels returned to normal by day 14. In the last patient analyzed, who’s HBsAg seroconverted to negative on the fifth day after admission. Unfortunately, due to poor compliance, we were unable to monitor the point at which HBV DNA levels fell below the detectable limit. Additionally, the patient tested positive for the anti-mitochondrial antibody M2 subtype, suggesting that the elevated bilirubin and abnormal liver enzymes may also be related to PBC. However, no further follow-up or treatment could be provided.
In these cases, the patient cleared the virus naturally without antiviral treatment, as shown by the rapid loss of HBsAg, illustrating the favorable outcome of AHB. Although our patients achieved rapid virological clearance, they experienced significant anxiety regarding their own and fetal health. In many societies, particularly in China where HBV is common, there is a strong social stigma against the virus. This stigma significantly increases anxiety for patients. Although acute HBV infection in early pregnancy does not increase the risk of birth defects or miscarriage, the virus can be passed to the newborn in about 10% of cases. On one hand, some experts advocate for a conservative approach without antiviral therapy, citing evidence that most patients experience a sharp decline in HBV DNA within one month and approximately 95% of adults achieve spontaneous recovery. Furthermore, long-term use of medication may lead to drug-resistant mutations. A study found that drug-resistant mutations were detected in 32.66% of hepatitis B patients (18). On the other hand, proponents of antiviral intervention argue that early treatment may enhance viral clearance, reduce HBsAg and HBV DNA levels, prevent chronic infection, and ultimately reduce the risk of hepatocellular carcinoma. Notably, several professional organizations recommend antiviral therapy at the 28th week of pregnancy if the maternal HBV DNA is >200,000IU/ml, as a conservative choice to minimize vertical HBV transmission (19, 20). For breastfed infants receiving birth-dose vaccine and immune globulin, the risk of HBV infection is minimal (21). But these uncertainties may overwhelm pregnant women.
As all three patients achieved HBsAg clearance, with two reaching virological cure, no adverse virological responses were observed. It is therefore important to consider potential outcomes in less favorable scenarios. Pregnant women have reduced immune clearance, and persistence of HBsAg beyond six months indicates progression to chronic hepatitis B, which increases maternal risks of fibrosis, cirrhosis, and hepatocellular carcinoma, as well as pregnancy complications such as gestational hypertension and diabetes. High maternal viral load, particularly >200,000 IU/mL in late pregnancy, also markedly increases the risk of mother-to-child transmission (22, 23). Without vaccination, 90% of newborns exposed to HBV will develop chronic infection, compared to 5-10% of adults exposed to HBV (24).
A comprehensive review on viral hepatitis in pregnancy noted that CHB is characterized by persistent viral replication. Maternal HBV DNA levels > 2×105 IU/mL are associated with a 10%-15% mother-to-child transmission (MTCT) risk despite standard immunoprophylaxis (25). In contrast, a hepatologist’s perspective on hepatitis B management in pregnancy stated that AHB in pregnancy has variable MTCT risks: first - trimester AHB carries a 10% transmission rate, while third - trimester infection raises this to 60% without intervention. However, rapid viral clearance can eliminate transmission risk (26). Management strategies also differ: AHB in pregnancy mainly requires supportive care, with antiviral intervention reserved for severe cases. On the other hand, CHB management focuses on long-term viral suppression to prevent postpartum flares and MTCT. A review on HBV diagnosis and treatment further emphasized that for CHB in pregnancy, antiviral therapy aims to suppress viral replication to reduce MTCT, while AHB treatment is more focused on addressing acute liver injury (27). Notably, while the review on viral hepatitis in pregnancy mentioned that CHB in pregnancy is linked to increased risks of gestational diabetes and antepartum hemorrhage, the impact of AHB on obstetric outcomes remains understudied. A study suggest no elevated maternal mortality in AHB during pregnancy but potential associations with preterm birth and low birth weight in cases of severe liver injury (26).
According to a 2023 global review, rates of anxiety during pregnancy have been gradually rising (28, 29). Antenatal anxiety and depression have been associated with preeclampsia, premature birth, low birth weight, neonatal infections, and impaired cognitive development in offspring (30, 31). Therefore, it is essential to incorporate psychosocial assessment into the comprehensive management of pregnant women infected with HBV. Although our cases highlight the psychological distress associated with acute HBV infection in pregnancy, systematic mental health protocols were not implemented during their clinical care. To address this, we propose a scalable framework for integrating mental health screening into HBV perinatal care. This includes: routine use of validated screening tools such as the Generalized Anxiety Disorder-7or the Edinburgh Postnatal Depression Scale; stratified management according to severity, with mild cases receiving enhanced counseling and reassurance, and moderate-to-severe cases referred for professional psychological support; establishing multidisciplinary collaboration among hepatologists, obstetricians, and mental health specialists; and incorporating mental health assessment into postpartum follow-up. Such an approach could help reduce anxiety, improve treatment adherence.
Limitations
This study has several limitations. First, its retrospective nature precluded the use of standardized psychometric instruments, so anxiety was assessed qualitatively, which may limit objectivity. Second, the sample size was very small and lacked a control group, making it difficult to determine whether the observed psychological distress was specific to acute HBV in pregnancy or a common perinatal phenomenon. Third, all patients showed favorable virological outcomes, which may introduce selection bias and limit generalizability to women with poorer responses or risk of chronicity. Finally, one patient was lost to follow-up, restricting assessment of long-term outcomes. These cases nevertheless provide valuable clinical insights and highlight the need for prospective studies with larger cohorts, control groups, validated psychometric tools, and extended follow-up.
In conclusion, AHB in pregnancy is usually self-limited with a good prognosis, but may cause psychological distress affecting reproductive decisions. A patient-centered approach is essential for better clinical and quality-of-life outcomes, bridging hepatology and mental health helps support these women.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Hangzhou Third People’s Hospital (Approval Number: 2025KA222). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
Author contributions
SW: Data curation, Writing – original draft. KH: Conceptualization, Supervision, Writing – review & editing. YW: Conceptualization, Formal Analysis, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health O. Global health sector strategy on viral hepatitis 2016-2021. In: Towards ending viral hepatitis, vol. 2016. World Health Organization, Geneva (2016). Contract No.: WHO/HIV/2016.06.
2. Esteban R. Is there a role for interferon in acute viral hepatitis? Gut. (1993) 34:S77–80. doi: 10.1136/gut.34.2_suppl.s77
3. Lao TT, Sahota DS, Cheng YK, Law LW, and Leung TY. Maternal hepatitis B surface antigen status and incidence of pre-eclampsia. J Viral hepatitis. (2013) 20:343–9. doi: 10.1111/jvh.12037
4. Nguyen G, Garcia RT, Nguyen N, Trinh H, Keeffe EB, and Nguyen MH. Clinical course of hepatitis B virus infection during pregnancy. Alimentary Pharmacol Ther. (2009) 29:755–64. doi: 10.1111/j.1365-2036.2009.03932.x
5. Potthoff A, Rifai K, Wedemeyer H, Deterding K, Manns M, and Strassburg C. Successful treatment of fulminant hepatitis B during pregnancy. Z fur Gastroenterologie. (2009) 47:667–70. doi: 10.1055/s-0028-1109148
6. Lao TT, Chan BC, Leung WC, Ho LF, and Tse KY. Maternal hepatitis B infection and gestational diabetes mellitus. J hepatol. (2007) 47:46–50. doi: 10.1016/j.jhep.2007.02.014
7. Wan Z, Zhou A, Zhu H, Lin X, Hu D, Peng S, et al. Maternal hepatitis B virus infection and pregnancy outcomes: A hospital-based case-control study in Wuhan, China. J Clin gastroenterol. (2018) 52:73–8. doi: 10.1097/MCG.0000000000000842
8. Sujan AC, Nance N, Quesenberry C, Ridout K, Bhalala M, and Avalos LA. Racial and ethnic differences in perinatal depression and anxiety. J Affect Disord. (2023) 334:297–301. doi: 10.1016/j.jad.2023.04.123
9. Roddy Mitchell A, Gordon H, Atkinson J, Lindquist A, Walker SP, Middleton A, et al. Prevalence of perinatal anxiety and related disorders in low- and middle-income countries: A systematic review and meta-analysis. JAMA network Open. (2023) 6:e2343711. doi: 10.1001/jamanetworkopen.2023.43711
10. Qin Z, Liu Y, Liu Y, Yang A, Zhang R, Zhang K, et al. Association between resolved hepatitis B virus infection and depression in American adults: a cross-sectional study. Sci Rep. (2025) 15:16141. doi: 10.1038/s41598-025-99864-2
11. Zi-mei -Z, Na -H, Zhen -X, Jing -L, De-zhen -C, and Xin-hua -L. Analysis of anxiety and depression and influencing factors of patients with chronic hepatitis B virus infection. Chin J Gen Pract. (2020) 18:1134. doi: 10.16766/j.cnki.issn.1674-4152.001448
12. Ganem D and Prince AM. Hepatitis B virus infection–natural history and clinical consequences. New Engl J Med. (2004) 350:1118–29. doi: 10.1056/NEJMra031087
13. He JS, Gong DE, and Ostergaard HL. Stored Fas ligand, a mediator of rapid CTL-mediated killing, has a lower threshold for response than degranulation or newly synthesized Fas ligand. J Immunol (Baltimore Md: 1950). (2010) 184:555–63. doi: 10.4049/jimmunol.0902465
14. Shivakumar P, Mourya R, and Bezerra JA. Perforin and granzymes work in synergy to mediate cholangiocyte injury in experimental biliary atresia. J hepatol. (2014) 60:370–6. doi: 10.1016/j.jhep.2013.09.021
15. Lambotin M, Raghuraman S, Stoll-Keller F, Baumert TF, and Barth H. A look behind closed doors: interaction of persistent viruses with dendritic cells. Nat Rev Microbiol. (2010) 8:350–60. doi: 10.1038/nrmicro2332
16. Mohite BJ, Rath S, Bal V, Kamat SA, Marathe SN, Zuckerman AJ, et al. Mechanisms of liver cell damage in acute hepatitis B. J Med virol. (1987) 22:199–210. doi: 10.1002/jmv.1890220302
17. Han YT, Sun C, Liu CX, Xie SS, Xiao D, Liu L, et al. Clinical features and outcome of acute hepatitis B in pregnancy. BMC Infect diseases. (2014) 14:368. doi: 10.1186/1471-2334-14-368
18. Yang JX, Liu BM, Li XG, Yan CH, Xu J, Sun XW, et al. Profile of HBV antiviral resistance mutations with distinct evolutionary pathways against nucleoside/nucleotide analogue treatment among Chinese chronic hepatitis B patients. Antiviral Ther. (2010) 15:1171–8. doi: 10.3851/IMP1677
19. Revill PA, Tu T, Netter HJ, Yuen LKW, Locarnini SA, and Littlejohn M. The evolution and clinical impact of hepatitis B virus genome diversity. Nat Rev Gastroenterol hepatol. (2020) 17:618–34. doi: 10.1038/s41575-020-0296-6
20. Terrault NA, Lok ASF, McMahon BJ, Chang KM, Hwang JP, Jonas MM, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatol (Baltimore Md). (2018) 67:1560–99. doi: 10.1002/hep.29800
21. Dionne-Odom J, Cozzi GD, Franco RA, Njei B, and Tita ATN. Treatment and prevention of viral hepatitis in pregnancy. Am J obstetrics gynecol. (2022) 226:335–46. doi: 10.1016/j.ajog.2021.09.002
22. Boucheron P, Lu Y, Yoshida K, Zhao T, Funk AL, Lunel-Fabiani F, et al. Accuracy of HBeAg to identify pregnant women at risk of transmitting hepatitis B virus to their neonates: a systematic review and meta-analysis. Lancet Infect diseases. (2021) 21:85–96. doi: 10.1016/S1473-3099(20)30593-4
23. Terrault NA, Levy MT, Cheung KW, and Jourdain G. Viral hepatitis and pregnancy. Nat Rev Gastroenterol hepatol. (2021) 18:117–30. doi: 10.1038/s41575-020-00361-w
24. Su WJ, Chen SF, Yang CH, Chuang PH, Chang HF, and Chang MH. The impact of universal infant hepatitis B immunization on reducing the hepatitis B carrier rate in pregnant women. J Infect diseases. (2019) 220:1118–26. doi: 10.1093/infdis/jiy706
25. Chilaka VN and Konje JC. Viral hepatitis in pregnancy. Eur J obstetrics gynecol Reprod Biol. (2021) 256:287–96. doi: 10.1016/j.ejogrb.2020.11.052
26. Wong GL, Wen WH, and Pan CQ. Hepatitis B-management of acute infection and active inflammation in pregnancy-a hepatologist’s perspective. Best Pract Res Clin obstetrics gynaecol. (2020) 68:54–65. doi: 10.1016/j.bpobgyn.2020.03.014
27. Guvenir M and Arikan A. Hepatitis B virus: from diagnosis to treatment. Polish J Microbiol. (2020) 69:391–9. doi: 10.33073/pjm-2020-044
28. Lebel C, MacKinnon A, Bagshawe M, Tomfohr-Madsen L, and Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. (2020) 277:5–13. doi: 10.1016/j.jad.2020.07.126
29. Berthelot N, Lemieux R, Garon-Bissonnette J, Drouin-Maziade C, Martel É, and Maziade M. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta obstetricia gynecologica Scandinavica. (2020) 99:848–55. doi: 10.1111/aogs.13925
30. Dadi AF, Miller ER, Bisetegn TA, and Mwanri L. Global burden of antenatal depression and its association with adverse birth outcomes: an umbrella review. BMC Public Health. (2020) 20:173. doi: 10.1186/s12889-020-8293-9
Keywords: acute hepatitis B, perinatal mental health, virological clearance, early gestation, case report
Citation: Wu S, Hu K and Wang Y (2025) Acute hepatitis B virus infection in pregnancy: a case report of three patients with comorbid anxiety and their clinical outcomes. Front. Psychiatry 16:1695165. doi: 10.3389/fpsyt.2025.1695165
Received: 29 August 2025; Accepted: 10 October 2025;
Published: 22 October 2025.
Edited by:
Haohao Yan, Central South University, ChinaReviewed by:
Rongqi Wang, Third Hospital of Hebei Medical University, ChinaJuan Yan, Hangzhou Seventh Peoples Hospital, China
Copyright © 2025 Wu, Hu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yufang Wang, d2FuZ3l1ZmFuZzIwMDdAMTI2LmNvbQ==
†ORCID: Yufang Wang, orcid.org/0000-0003-1597-3289
 Shenlu Wu
Shenlu Wu Kejie Hu2
Kejie Hu2