- 1School of Marxism, Liaoning University, Shenyang, China
- 2Department of Psychology, Renmin University of China, Beijing, China
- 3School of Nursing, Peking University, Beijing, China
- 4Xiangya School of Nursing, Central South University, Changsha, China
- 5School of Humanities and Social Sciences, Harbin Medical University, Harbin, China
- 6Department of Pharmacy, The Fifth Affiliated Hospital of Sun Yat-sat University, Zhuhai, China
- 7Xijing Hospital, Airforce Military Medical University, Xi'an, China
- 8School of Finance and Trade, Liaoning University, Shenyang, China
- 9Institute of Chinese Medical Sciences, University of Macau, Macao, Macao SAR, China
Background: Subthreshold depression is a risk factor for major depression. Psychotherapy is a kind of intervention for subthreshold depression. There have been many systematic reviews synthesized the evidence for its effectiveness toward subthreshold depression. However, there is currently no overview of these systematic reviews.
Objective: To undertake an overview of meta-analyses and systematic reviews to identify the efficacy of psychotherapy in subthreshold depression patients.
Methods: We will search several databases such as PubMed, Embase, the Cochrane Library, Web of Science, PsycINFO, CNKI, WanFang and VIP database, for systematic reviews and meta-analyses on psychotherapy in subthreshold depression patients. The search timeline will be from inception up to August 2022. Two researchers will screen related studies back-to-back. We will include studies that evaluate the efficacy of psychotherapy in subthreshold depression patients. We will evaluate the methodological quality, the reporting quality and the quality of evidence for outcomes by AMSTAR-2, the PRISMA 2020 checklist and the GRADE grading system. We will present the results of the overview in alignment with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. The anticipated start and completion dates for this overview are 1 August 2022 and 30 December 2022, respectively.
Results: From this study, we will evaluate the methodological quality and the level of evidence of the included systematic reviews and meta-analyses, and evaluate the efficacy of psychotherapy in patients with subthreshold depression.
Implications: We will ascertain the efficacy of psychotherapy in subthreshold depression patients, to provide evidence to guide the treatment of subthreshold depression in the future.
Registration number: Our research protocol has been registered with PROSPERO. The registration number of the protocol is CRD42021278871.
Introduction
Introduction of subthreshold depression
Subthreshold depression (SD) is a kind of less severe type of depression in which the individual does not meet the diagnostic threshold for major depressive disorder (MDD) in terms of frequency, severity, and/or duration of symptoms (1, 2). Currently, the most commonly used definition of SD in the scientific community, as described in Diagnostic and Statistical Manual 5th Edition (DSM-5), is two or more symptoms of depressive disorder occurring simultaneously, one of which is depressed mood, for most or all of a period of at least 2 weeks. The symptoms must cause functional impairment and have a negative impact on the individual's life and may never meet the criteria for major depressive disorder or dysthymia (3, 4).
Studies based on population have found that SD is widely prevalence all over the world. For example, Stubbs et al. (5) described a 12-month SD prevalence of 2.5% and (6) reported a rate of 4.2%, based on 237,952 individuals and a sample of 3,514 residents of Izmir, Turkey, respectively. Relevant studies have also explored the epidemiological status of SD in people of different ages. For example, many studies have found that the prevalence of SD increases significantly after age 12 and rises permanently in mid-adolescence (14–16 years) (7–10). In adults, a systematic review of 19 studies estimated the prevalence of SD ranged from 3 to 10% in clinical and from 1 to 17% in community settings, respectively (1). In older people, the prevalence of SD is usually at least 2–3 times higher than that of MDD (11). In addition, studies have found that SD is associated with other diseases. For instance, According to the previous studies, the prevalence of SD among people with diabetes reached 12% (12), higher than the prevalence of depression (13).
Although SD has less severe symptoms than MDD (14), it causes a wide range of adverse outcomes (15). It has been found to be a risk factor for developing MDD and other psychiatric disorders, because of persistent depressive symptoms (16–18). For example, Lee et al. found that people with SD were about twice as likely to develop depression than non-depressed people (19). In addition, it is often an ineffective state with considerable psychological distress (14) and is also associated with increased mortality (17, 20) and significant economic costs (21). It is therefore important to identify effective methods for treating SD (22).
Diagnosis and treatment of subthreshold depression
According to DSM-5, the diagnostic criteria for SD are “Depressed mood and at least one of the other eight symptoms of a Major Depressive episode, associated with clinically significant distress or deficit lasting at least 2 weeks, in individuals not meeting criteria for any other Depressive or Bipolar Disorder, and currently exhibiting no active or residual criteria for any Psychotic disorder, and does not meet the criteria of mixed anxiety or symptoms of depressive disorder.” In some studies, questionnaires were used to make a depression diagnosis. For example, Dirmaier et al. (23) categorized participants who scored between 5 and 8 on the Depression Screening Questionnaire (DSQ) as SD (23).
SD treatment aims to decrease or avoid the negative consequences associated with this depressive state and to act as a powerful tool for the prevention of MDD (24). There are multiple treatment strategies for SD, including pharmacotherapy, electroacupuncture, “Watchful waiting”, “Patient preferences”, and so on.
Pharmacotherapy for SD is mainly with antidepressants such as tricyclics, 5-hydroxytryptamine, reuptake inhibitors, etc. (25). The effectiveness of pharmacotherapy for SD is varied (26). Electroacupuncture has been extensively applied to the treatment of psychiatric disorders including depression (27), as it modulates the hypothalamic-pituitary-adrenal axis (28) and restores hippocampal CA1 synaptic plasticity by adjusting 5-hydroxytryptamine system receptor levels, thereby exerting antidepressant activity and improving depression-like behavior (29). “Watchful waiting” requires systematic monitoring, including assessment of symptoms, course, and impact, which may be appropriate for patients with good social support, no personal or family history of depressive disorder, and who refuse medication and/or psychotherapy even after explanation of risks and available treatment options (30). “Patient preferences” refers to educating patients about their disease and treatment options so that both physicians and patients can make shared decisions. A recent review has shown its benefits regarding adherence, treatment satisfaction, and outcomes (15). In addition to the therapies mentioned above, psychotherapy is becoming an increasingly important treatment option for SD. Currently psychotherapy is the intervention that has shown the strongest evidence of being the first-line treatment (31, 32). What's more, other studies suggest that, for comorbid SD, such as both depression and glycemic control, the preferred treatment would also be psychotherapy (33).
Psychotherapy
Psychotherapy is the establishment of a relationship with the patient through structured and purposeful contact and the use of a range of specific techniques to improve the patient's psychological state (34), which has contributed greatly to the treatment of SD.
According to different studies, psychotherapy is usually categorized as follows: psychodynamic therapies, cognitive and behavioral therapies (CBT), humanistic therapies, systemic therapies (35) and interpersonal psychotherapy (IPT) (36). Each category can also be divided into different types, such as cognitive and behavioral therapies, which contain web-based, bibliotherapy-based and telephone-based cognitive behavioral therapy, and so on (25).
Psychodynamic therapies includes many approaches influenced by Freud's psychoanalysis, such as transfer-focused psychotherapy (TFP) and mentalization-based therapy (37). CBT is a form of talking therapy that aims to recognize and challenge non-adaptive beliefs and behaviors and try to develop distinct ways of thinking and behaving to improve the patient's mental and physical outcomes. Humanistic therapies adopt person-centered perspective, focusing on individual experiences and different needs of each patient (35). Systemic therapies, such as family therapy, assume that the patient's problems are situationally rather than personally derived (38). IPT is a highly structured, time-limited intervening that focuses on current salient relationship and interpersonal experiences (39). According to the available literature, mainstream psychotherapy for SD include CBT and IPT (21, 40, 41).
Several instrumental scales can be used to assess the effect of psychotherapy on SD. Generally speaking, Hamilton Rating Scale for Depression (HRSD) (42), the Kessler Screening Scale for Psychological Distress (K-6), Beck Depression Inventory scale (BDI), the Patient Health Questionnaire-9 (PHQ-9) and Center for Epidemiologic Studies Depression Scale (CES-D) can often be used as efficacy outcomes for SD (25). Moreover, Children's Depression Inventory (CDI), Children's Depression Rating Scale (CDRS) or Children's Depression Rating Scale-Revised (CDRS-R) can be used to measure the intervention effect in children (34, 43). Sometimes anxiety can be used as a secondary outcome indicator because anxiety problems have a high-comorbidity with depression (44).
Psychotherapy has significant effects on SD. Psychotherapy was proven to be more effective than care-as-usual for SD patients in a meta-analysis of 700 patients, reducing depressive symptoms and preventing episodes of severe depression (21). The long-term effect of psychological intervention on SD is to improve their psychological wellbeing, as well as to improve their physical and social functions (33). However, the efficacy may also be related to the specific treatments adopted and the characteristics of the patients. For instance, a systemic review including eight studies on the efficacy of Internet-based cognitive behavioral treatments (ICBT) discovered that ICBT intervention had better short-term efficacy for SD patients compared to controls, but it is inconclusive for long-term effects (44). And another meta-analytic review focusing on children and adolescents found a positive acute effect of psychological treatment for adolescents with SD, but this effect has not been found in children under 12 years of age (40). Recently, He et al. (45) conducted a network meta-analysis to compare and rank the efficacy of nonpharmacological interventions in adults with SD, and the study found that psychotherapy, especially CBT, may be the most effective nonpharmacological intervention to treat SD in adults. However, more RCTs examining the efficacy of different nonpharmacological interventions are needed in the future (14, 40, 41).
Objective
Clinical and patient attention is increasingly focused on the treatment of SD by psychotherapy. There is a wide variety of psychotherapies available. With the popularization of systematic review methods, systematic reviews and meta-analyses of psychotherapies for SD are gradually increasing, but the quality are varied, so it is necessary to overview the systematic review. Meanwhile, there is no systemic overview to compare the therapeutic effects of different psychological interventions. Given the importance of psychotherapy in SD, and no overview has been conducted, this overview is expected to undertake a systematic overview to identify the efficacy of psychotherapy in SD patients and try to compare the efficacy of different kinds of psychotherapies.
Materials and methods
Study registration
We will follow the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for reporting our overview (46). Our research protocol has been registered with PROSPERO. The registration number of the protocol is CRD42021278871.
Search strategy and selection criteria
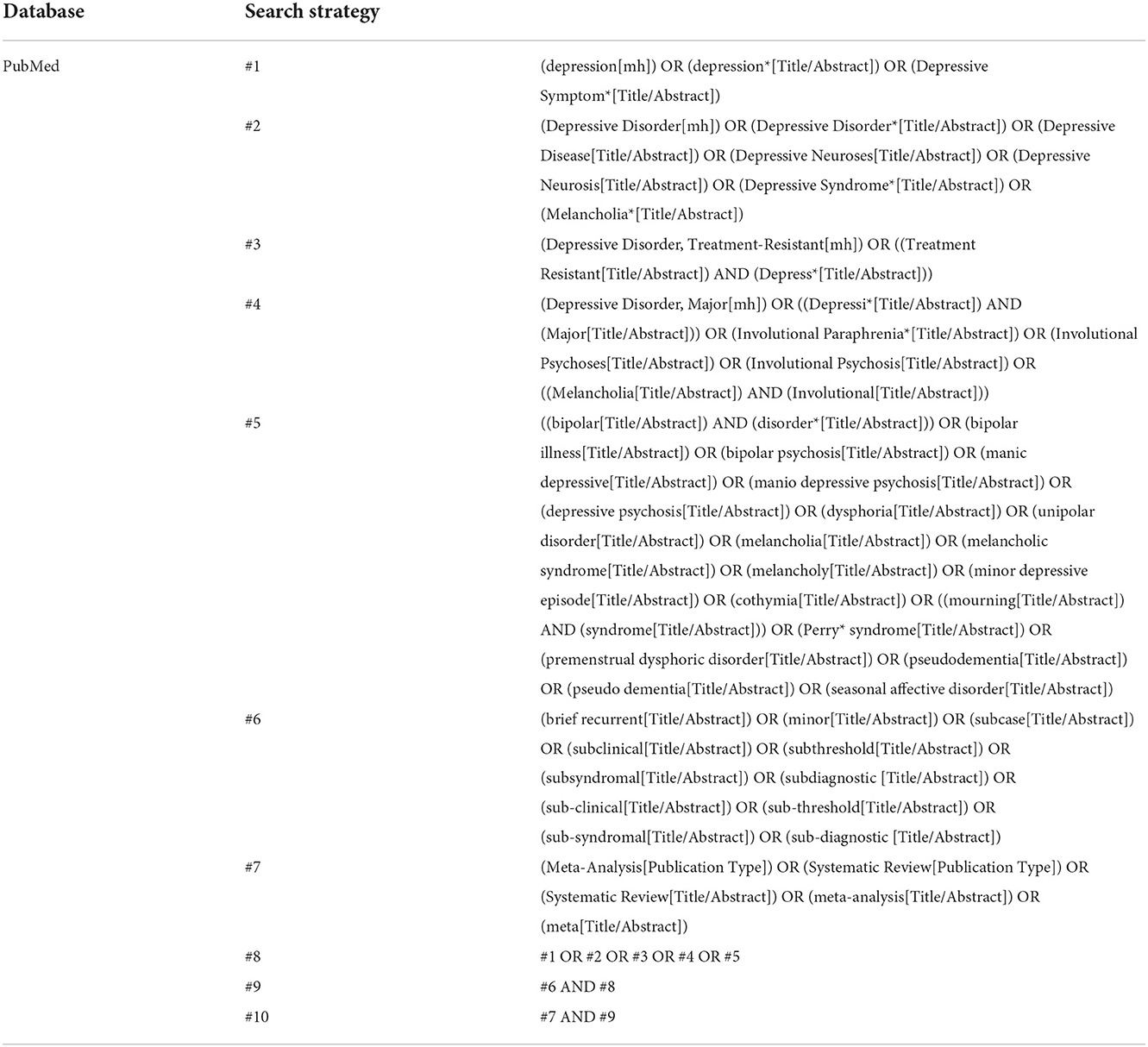
We will search databases including PubMed, Embase, the Cochrane Library, Web of Science, PsycINFO, CNKI, WanFang and VIP database. The search terms are related to SD, systematic reviews and meta-analyses. To avoid omitting relevant studies, the interventions/controls of the studies will not be restricted during the literature search phase. We will screen systematic reviews and meta-analyses of interventions/controls that meet the inclusion criteria of this study during the literature screening phase. The search timeline will be from inception up to August 2022. Studies in Chinese or English will be included in this overview. As an example, the Search strategy of Pubmed database is shown in Table 1. Search strategy of other databases can be seen in Supplementary Table 1.
Types of studies
Systematic reviews and meta-analyses of RCTs that examine the use of psychotherapy in SD patients will be included.
Types of participants
The participants had SD diagnosed according to any authoritative diagnostic criteria, no restrictions on age, sex, race, the source of cases, or onset time. Since SD is also found in minors, and there are also clinical studies and systematic reviews/meta-analyses on the treatment of SD in minors, in this overview, we will include relevant studies on the treatment of SD in minors.
Types of interventions
Systematic reviews and meta-analyses comparing one psychological intervention with another or either of the control conditions for patients with SD will be included. For psychotherapy, CBT, behavioral therapy (BT), cognitive therapy (CT), IPT, problem-solving therapy (PST), play therapy, supportive counseling, psychodynamic therapy (DYN) and family therapy will be included regardless of their treatment session and duration (34). In terms of control conditions, waiting-list control (WL), non-treatment control, treatment as usual (TAU) and (psychological or pill) placebo will be included.
Outcomes
The primary outcome of efficacy will be defined as mean overall change on continuous depression severity scales. Included systematic reviews or meta-analyses will be required to report at least one of the following indicators: Scores of HRSD, CDRS, CDRS-R, CES-D, BDI, the 9-item patient health questionnaire (PHQ-9), or the Kessler screening scale for psychological distress (K-6) (25).
The secondary indicators of this study are as follows. Quality of life/functioning improvement can be another indicator of psychotherapy. QoL/functioning an be captured by the mean overall change in functioning improvement scales or quality of life scales.
Suicide-related outcomes and anxiety can also be used as outcomes of psychological interventions. The former can be measured with the Suicidal Ideation Questionnaire-Junior High School version (47), and the latter can be measured with Hamilton Anxiety Scale Score (48).
Study screening process
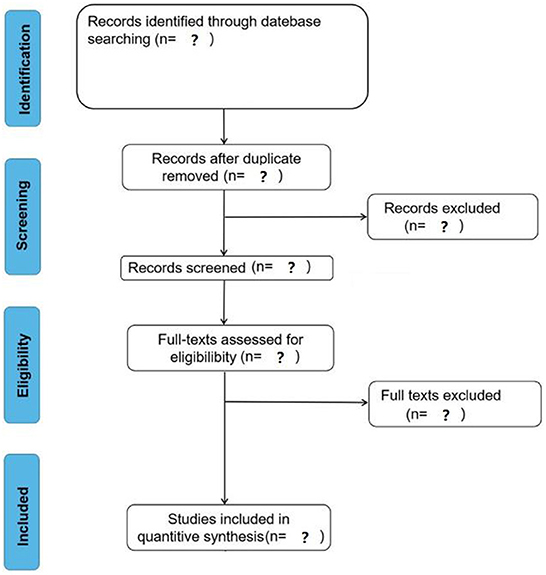
The screening process of the studies can be divided into four stages: deduplication, primary screening (screening studies based on titles and abstracts), secondary screening (screening studies based on full text), and cross-checking. After the studies are deduplication, two researchers will screen the eligible studies independently by reading the title, abstract and full text according to the inclusion and exclusion criteria. After the rescreening is completed, they will conduct a cross-check stage. If there is any disagreement, they will negotiate with the third researcher. The anticipated study screening process is shown in Figure 1.
Data screening and extraction
The basic data will be independently extracted by two researchers according to the pre-designed data extraction table, including first author, publication year, intervention/control measures, the efficacy outcomes, etc. If the included literature was incomplete, we would contact the original researcher to obtain the required study data.
Quality assessment
Two experienced investigators will conduct back-to-back quality evaluation of the included studies. If there is disagreement, another experienced investigator will be invited to join the discussion and finally reach an agreement.
A Measure Tool to Assess Systematic Reviews-2 (AMSTAR-2) (49) and the PRISMA 2020 checklist (46) will be used to evaluate the methodological quality of the included studies. As a recently developed methodological quality assessment tool for systematic reviews, AMSTAR-2 includes 16 items, which involve the whole process of systematic review topic selection, design, registration, data extraction, data statistical analysis and discussion. This tool classifies the methodological quality of systematic reviews into four levels: high, moderate, low, and very low. The PRISMA 2020 checklist includes a total of 27 items. When grading the included literature, 1 point is given for the item that is fully reported, 0.5 point for the partially reported item, and 0 point for the unreported item. The full score is 27 points. The literature with a score of < 15 points has relatively serious information defects, the literature with a score of ≥ 15 points and < 21 points has certain defects, and the report quality of the literature with a score of more than 21 points is relatively good.
The Grades of Recommendations Assessment, Development and Evaluation (GRADE) grading system of evidence will be used to assess the quality of evidence for outcomes (50, 51). The GRADE system, as a set of evidence rating system, includes five downgrading factors including study limitation, inconsistency, immediacy, imprecision and publication bias. It grades the quality of evidence into four levels: high, moderate, low, and very low.
Data synthesis
A qualitative analysis will be performed first. The characteristics of the original studies included in each systematic reviews and the results of the meta-analysis will be summarized and concluded.
Secondly, a network meta-analysis will be performed by R (Version 4.0.3) with suitable packages such as gemtc.
The mean change and standard deviation of the outcome measures from baseline to the endpoint will be used to calculate the effect size (ES) of different kinds of psychotherapy. The ES will be assessed with standardized mean difference (SMD) because several measures of SD are reported in the included studies, but few of them are common to all trials. The I2 test will be used to assess heterogeneity when more than one studies are pooled, and the level of heterogeneity will be rated as low ( ≤ 50%), or high (>50%) (52). We will use a random-effects model or a fixed-effects model, which will depends on the heterogeneity of the studies included.
To combine direct and indirect evidence of SD, an NMA model will be conducted to compare the effects of different kinds of psychotherapy. If there are multiple groups or control groups classified as the same modality in a study according to our classification of intervention or control, we will split the article and conducted statistical analysis (53). The effects of different kinds of psychotherapy on SD will be compared using a network meta-analysis within the frequentist framework. We will calculate whether there will be a significant difference in the inconsistency model. If not, the consistency model will be selected. We will assess the assumption of consistency locally using the node-splitting method (54, 55). The surface under the cumulative ranking curve (SUCRA) will be used to separately rank each intervention (56). The larger the SUCRA value is, the better the rank. We will assess the efficacy of the different control groups as additional proof of transitivity by computing prepost treatment changes in the continuous depression severity score for the waitlist group, no treatment group, usual care group and active control group (57). A p-value < 0.05 was considered statistically significant.
When we perform sensitivity analyses, we will exclude studies having a high risk of bias and calculate the ranking of different kinds of psychotherapy when we included only low-risk studies. Publication bias will be examined funnel plots.
Subgroup analyses
We will delivery the following subgroups analysis: (1) for the age of participants (e.g., Youth samples or Adult samples or Elderly samples); and (2) for the duration of psychotherapy (e.g., short-term treatment of six or fewer weeks or long-term treatment of more than 6 weeks); and (3) for the ample types of participants (e.g., Community-based samples or Primary care samples).
Ethics and dissemination
This overview will not require the approval of an Ethics Committee because it will use published studies. We will publish results in a peer-reviewed journal.
Discussion
Our overview will be a comprehensive synthesis of the existing systematic reviews and meta-analysis on the efficacy of psychotherapy in SD patients. To best of our knowledge, it will be the first overview in this filed.
In discussing our research, we plan to present the following sections: summary of key findings; comparison with other research and perspectives; implications for research and practice; interpretation of results; strengths and limitations; conclusions. We confirm that the results of this review will inform patients, physicians and clinical researchers about the reliability of the current evidence and the direction of future research.
Author contributions
PG and ZL: conceptualisation, supervision, and writing—review and editing. XuH and JLi: investigation. PG: project administration. XuH, JLiu, YY, JLi, JZ, XiH, and AR: original draft. All authors read and approved the final manuscript.
Funding
This study was funded by Supported by Research on Issues Related to the Integration of Ideological and Political Education in Universities, Middle and Primary Schools (L19ASZ004) and Research on the Modernisation of National Governance System and Governance Capability from the Perspective of Marxist Philosophy (LQN202037).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1017907/full#supplementary-material
References
1. Rodríguez MR, Nuevo R, Chatterji S, Ayuso-Mateos JL. Definitions and factors associated with subthreshold depressive conditions: a systematic review. BMC Psychiatr. (2012) 12:1–7. doi: 10.1186/1471-244X-12-181
2. National Collaborating Centre for Mental Health (UK). Depression: The Treatment and Management of Depression in Adults. Leicester: British Psychological Society (2010).
3. Alexopoulos GS. Depression in the elderly. Lancet. (2005) 365:1961–70. doi: 10.1016/S0140-6736(05)66665-2
4. Blazer DG. Depression in late life: review and commentary. J Gerontol Series Biol Sci Med Sci. (2003) 58:M249–65. doi: 10.1093/gerona/58.3.M249
5. Stubbs B, Vancampfort D, Veronese N, Thompson T, Fornaro M, Schofield P, et al. Depression and pain: primary data and meta-analysis among 237 952 people across 47 low-and middle-income countries. Psychol Med. (2017) 47:2906–17. doi: 10.1017/S0033291717001477
6. Topuzoglu A, Binbay T, Ulaş H, Elbi H, Tanik FA, Zagli N, Alptekin K. The epidemiology of major depressive disorder and subthreshold depression in Izmir, Turkey: Prevalence, socioeconomic differences, impairment and help-seeking. J Aff Disorders. (2015) 181:78–86. doi: 10.1016/j.jad.2015.04.017
7. Allgaier AK, Pietsch K, Frühe B, Prast E, Sigl-Glöckner J, Schulte-Körne G, et al. Depression in pediatric care: is the WHO-five well-being index a valid screening instrument for children and adolescents? Gen. Hospital Psychiatry. (2012) 34:234–41. doi: 10.1016/j.genhosppsych.2012.01.007
8. Cuijpers P, Boluijt P, Van Straten A. Screening of depression in adolescents through the Internet. Eur Child Adol Psychiatr. (2008) 17:32–8. doi: 10.1007/s00787-007-0631-2
9. Rohde P, Beevers CG, Stice E, O'Neil K. Major and minor depression in female adolescents: onset, course, symptom presentation, and demographic associations. J Clin Psychol. (2009) 65:1339–49. doi: 10.1002/jclp.20629
10. Sihvola E, Keski-Rahkonen A, Dick DM, Pulkkinen L, Rose RJ, Marttunen M, et al. Minor depression in adolescence: phenomenology and clinical correlates. J Aff Disorders. (2007) 97:211–8. doi: 10.1016/j.jad.2006.06.019
11. Meeks TW, Vahia IV, Lavretsky H, Kulkarni G, Jeste DV. A tune in “a minor” can “b major”: a review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. J Aff Disorders. (2011) 129:126–42. doi: 10.1016/j.jad.2010.09.015
12. Wang D, Shi L, Li L, Guo X, Li Y, Xu Y, et al. Subthreshold depression among diabetes patients in Beijing: cross-sectional associations among sociodemographic, clinical, and behavior factors. J Aff Dis. (2018) 237:80–6. doi: 10.1016/j.jad.2018.05.016
13. Albertorio-Diaz JR, Eberhardt MS, Oquendo M, Mesa-Frias M, He Y, Jonas B, et al. Depressive states among adults with diabetes: findings from the national health and nutrition examination survey, 2007–2012. Diab Res Clin Prac. (2017) 127:80–8. doi: 10.1016/j.diabres.2017.02.031
14. Cuijpers P, Smit F, Van Straten A. Psychological treatments of subthreshold depression: a meta-analytic review. Acta Psychiatr Scand. (2007) 115:434–41. doi: 10.1111/j.1600-0447.2007.00998.x
15. Biella MM, Borges MK, Strauss J, Mauer S, Martinelli JE, Aprahamian I, et al. Subthreshold depression needs a prime time in old age psychiatry? A narrative review of current evidence. Neuropsychiatr Dis Treatment. (2019) 15:2763. doi: 10.2147/NDT.S223640
16. Cuijpers P, Smit F. Subthreshold depression as a risk indicator for major depressive disorder: a systematic review of prospective studies. Acta Psychiatr Scand. (2004) 109:325–31. doi: 10.1111/j.1600-0447.2004.00301.x
17. Cuijpers P, Schoevers RA. Increased mortality in depressive disorders: a review. Curr Psychiatr Rep. (2004) 6:430–7. doi: 10.1007/s11920-004-0007-y
18. Johnson JG, Cohen P, Kasen S. Minor depression during adolescence and mental health outcomes during adulthood. Br J Psychiatr. (2009) 195:264–5. doi: 10.1192/bjp.bp.108.054239
19. Lee YY, Stockings EA, Harris MG, Doi SAR, Page IS, Davidson SK, et al. The risk of developing major depression among individuals with subthreshold depression: a systematic review and meta-analysis of longitudinal cohort studies. Psychol Med. (2019) 49:92–102. doi: 10.1017/S0033291718000557
20. Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Aff Dis. (2002) 72:227–36. doi: 10.1016/S0165-0327(01)00413-X
21. Cuijpers P, Smit F, Oostenbrink J, Graaf DE, Ten Have RM, Beekman A. Economic costs of minor depression: a population-based study. Acta Psychiatr Scand. (2007) 115:229–36. doi: 10.1111/j.1600-0447.2006.00851.x
22. Kroenke K. When and how to treat subthreshold depression. JAMA. (2017) 317:702–4. doi: 10.1001/jama.2017.0233
23. Dirmaier J, Watzke B, Koch U, Schulz H, Lehnert H, Pieper L, et al. Diabetes in primary care: prospective associations between depression, nonadherence and glycemic control. Psychother Psycho. (2010) 79:172–8. doi: 10.1159/000296135
24. Willemse GR, Smit F, Cuijpers P, Tiemens BG. Minimal-contact psychotherapy for sub-threshold depression in primary care: randomised trial. Br J Psychiatr. (2004) 185:416–21. doi: 10.1192/bjp.185.5.416
25. Jiang X, Luo Y, Chen Y, Yan J, Xia Y, Yao L, et al. Comparative efficacy of multiple therapies for the treatment of patients with subthreshold depression: a systematic review and network meta-analysis. Front Behav Neurosci. (2021) 15:755547. doi: 10.3389/fnbeh.2021.755547
26. Cameron IM, Reid IC, MacGillivray SA. Efficacy and tolerability of antidepressants for sub-threshold depression and for mild major depressive disorder. J Aff Dis. (2014) 166:48–58. doi: 10.1016/j.jad.2014.04.078
27. Woo JA, Nam YJ, Park YJ, Kwon YK. Review of recent clinical trials for depression in traditional Chinese medicine-based on randomized controlled trials and systematic reviews. J Physiol Pathol Med. (2015) 29:458–66. doi: 10.15188/kjopp.2015.12.29.6.458
28. Le JJ, Yi T, Qi L, Li J, Shao L, Dong JC, et al. Electroacupuncture regulate hypothalamic–pituitary–adrenal axis and enhance hippocampal serotonin system in a rat model of depression. Neurosci Lett. (2016) 615:66–71. doi: 10.1016/j.neulet.2016.01.004
29. Han X, Wu H, Yin P, Chen Z, Cao X, Duan Y, et al. Electroacupuncture restores hippocampal synaptic plasticity via modulation of 5-HT receptors in a rat model of depression. Brain Res Bullet. (2018) 139:256–62. doi: 10.1016/j.brainresbull.2018.03.004
30. Ten Have M, Penninx BWJH, Tuithof M, Van Dorsselaer SAFM, Kleinjan M, Spijker J, et al. Duration of major and minor depressive episodes and associated risk indicators in a psychiatric epidemiological cohort study of the general population. Acta Psychiatr Scand. (2017) 136:300–12. doi: 10.1111/acps.12753
31. Cuijpers P, Karyotaki E, Pot AM, Park M, Reynolds CF. Managing depression in older age: psychological interventions. Maturitas. (2014) 79:160–9. doi: 10.1016/j.maturitas.2014.05.027
32. Kirkham JG, Choi N, Seitz DP. Meta-analysis of problem solving therapy for the treatment of major depressive disorder in older adults. Int J Geriatr Psychiatr. (2016) 31:526–35. doi: 10.1002/gps.4358
33. Van der Feltz-Cornelis C, Allen SF, Holt RI, Roberts R, Nouwen A, Sartorius N. Treatment for comorbid depressive disorder or subthreshold depression in diabetes mellitus: Systematic review and meta-analysis. Brain Behav. (2021) 11:e01981. doi: 10.1002/brb3.1981
34. Qin B, Zhou X, Michael KD, Liu Y, Whittington C, Cohen D, et al. Psychotherapy for depression in children and adolescents: study protocol for a systematic review and network meta-analysis. BMJ Open. (2015) 5:e005918. doi: 10.1136/bmjopen-2014-005918
36. Markowitz JC, Svartberg M, Swartz HA. Is IPT time-limited psychodynamic psychotherapy? J. Psychother Prac Res. (1998) 7:185–95.
37. Bateman A, Fonagy P. Mentalization Based Treatment for Personality Disorders: A Practical Guide. Oxford: Oxford University Press (2016).
38. Juul S, Poulsen S, Lunn S, Sørensen P, Jakobsen JC, Simonsen S, et al. Short-term versus long-term psychotherapy for adult psychiatric disorders: a protocol for a systematic review with meta-analysis and trial sequential analysis. Syst Rev. (2019) 8:1–13. doi: 10.1186/s13643-019-1099-0
39. Driessen E, Cohen ZD, Weissman MM, Markowitz JC, Weitz ES, Hollon SD, et al. The efficacy of antidepressant medication and interpersonal psychotherapy for adult acute-phase depression: study protocol of a systematic review and meta-analysis of individual participant data. BJPsych Open. (2021) 7:2. doi: 10.1192/bjo.2021.4
40. Cuijpers P, Pineda BS, Ng MY, Weisz JR, Muñoz RF, Gentili C, et al. A meta-analytic review: psychological treatment of subthreshold depression in children and adolescents. J Am Acad Child Adol Psychiatr. (2021) 60:1072–84. doi: 10.1016/j.jaac.2020.11.024
41. Krishna M, Honagodu A, Rajendra R, Sundarachar R, Lane S, Lepping P, et al. A systematic review and meta-analysis of group psychotherapy for sub-clinical depression in older adults. Int J Geriatr Psychiatr. (2013) 28:881–8. doi: 10.1002/gps.3905
42. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatr. (1960) 23:56–62. doi: 10.1136/jnnp.23.1.56
44. Zhou T, Li X, Pei Y, Gao J, Kong J. Internet-based cognitive behavioral therapy for subthreshold depression: a systematic review and meta-analysis. BMC Psychiatr. (2016) 16:1–11. doi: 10.1186/s12888-016-1061-9
45. He R, Wei J, Huang K, Yang H, Chen Y, Liu Z, et al. Nonpharmacological interventions for subthreshold depression in adults: a systematic review and network meta-analysis. Psychiatry Res. (2022) 317:114897. doi: 10.1016/j.psychres.2022.114897
46. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. (2021) 10:1–11. doi: 10.1186/s13643-021-01626-4
47. Raynolds WM. Suicidal Ideation Questionnaire. Odessa, FL: Psychological Assessment Resources. (1987).
48. Slee A, Nazareth I, Bondaronek P, Liu Y, Cheng Z, Freemantle N, et al. Pharmacological treatments for generalised anxiety disorder: a systematic review and network meta-analysis. Lancet. (2019) 393:768–77. doi: 10.1016/S0140-6736(18)31793-8
49. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:21. doi: 10.1136/bmj.j4008
50. Norton ME, Kuller JA, Metz TD. Society for Maternal-Fetal Medicine special statement: grading of recommendations assessment, development, and evaluation (GRADE) update. Am J Obst Gynecol. (2021) 224:B24–8. doi: 10.1016/j.ajog.2020.12.1200
51. Edition F. Diagnostic and statistical manual of mental disorders. Am Psychiatric Assoc. (2013) 21:591–643.
52. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
53. Rücker G, Cates CJ, Schwarzer G. Methods for including information from multi-arm trials in pairwise meta-analysis. Res Synthesis Methods. (2017) 8:392–403. doi: 10.1002/jrsm.1259
54. Chaimani A, Salanti G. Visualizing assumptions and results in network meta-analysis: the network graphs package. Stata J. (2015) 15:905–50. doi: 10.1177/1536867X1501500402
55. Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. (2010) 29:932–44. doi: 10.1002/sim.3767
56. Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. (2011) 64:163–71. doi: 10.1016/j.jclinepi.2010.03.016
57. Mutz J, Vipulananthan V, Carter B, Hurlemann R, Fu C, Young AH, et al. Comparative efficacy and acceptability of non-surgical brain stimulation for the acute treatment of major depressive episodes in adults: systematic review and network meta-analysis. BMJ. (2019) 364:l1079. doi: 10.1136/bmj.l1079
Keywords: subthreshold depression, psychotherapy, meta-analyses, systematic reviews, protocol
Citation: Han X, Li J, Yang Y, Liu J, Zhang J, Han X, Reyila A, Liu Z and Ge P (2022) Efficacy of psychotherapy in subthreshold depression patients: A protocol for an overview of systematic reviews and meta-analyses. Front. Public Health 10:1017907. doi: 10.3389/fpubh.2022.1017907
Received: 12 August 2022; Accepted: 17 November 2022;
Published: 07 December 2022.
Edited by:
Haijiang Li, Shanghai Normal University, ChinaReviewed by:
Snehil Gupta, All India Institute of Medical Sciences Bhopal, IndiaJingsong Wu, Fujian University of Traditional Chinese Medicine, China
Copyright © 2022 Han, Li, Yang, Liu, Zhang, Han, Reyila, Liu and Ge. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhizhong Liu, lnuliu@163.com; Pu Ge, 17853140673@163.com
 Xu Han
Xu Han Jiaxin Li
Jiaxin Li Yajie Yang
Yajie Yang Jiaxin Liu
Jiaxin Liu Jinzi Zhang
Jinzi Zhang Xiao Han
Xiao Han Abudurousuli Reyila
Abudurousuli Reyila Zhizhong Liu
Zhizhong Liu Pu Ge
Pu Ge