- 1School of Education Science, Leshan Normal University, Leshan, Sichuan, China
- 2Arnold School of Public Health, University of South Carolina, Columbia, SC, United States
Previous research has documented that HIV-related stigma may be a significant trigger of mental health problems among people living with HIV (PLWH). However, less is known about how internalized HIV stigma is linked to depressive symptoms among PLWH during the COVID-19 pandemic. The current study sought to explore the network structure of internalized HIV stigma and depressive symptoms, along with bridge nodes, to elucidate how they co-exist. Participants were 1,197 Chinese PLWH (64.3% male, Mage = 41.52, SD = 9.20) who completed the measurements of internalized HIV stigma and depressive symptoms during the early phase of the COVID-19 outbreak (May 2020). Results revealed that “ashamed of having HIV” was identified as the most central nodes in the internalized HIV stigma network, whereas “mind wandered during tasks” ranked highest on centrality in the depressive symptoms network. Two bridge connections were exhibited within the combined internalized HIV stigma and depressive symptoms network model: “inferiority due to HIV” and “gloomy feelings” from internalized HIV stigma and depressive symptoms communities, respectively. This study is one of the first to examine the co-occurrence of internalized HIV stigma and depressive symptoms in the context of the COVID-19 pandemic using a network approach. These findings have potential clinical implications for mitigating depressive symptoms in populations facing socioeconomic disadvantage and vulnerability.
1 Introduction
The COVID-19 pandemic has underscored the intersection of public health crises and mental health challenges, particularly among disadvantaged and vulnerable populations such as people living with HIV (PLWH) (1). The added strain of the pandemic has exacerbated mental health problems, particularly depressive symptoms, among this group (2). Depressive symptoms, including persistent sadness, lack of interest in daily activities, cognitive difficulties, and physical malaise, are prevalent in PLWH due to the chronic nature of their condition (3–5). These symptoms may be exacerbated by the stressors and uncertainties of the COVID-19 pandemic, such as increased social isolation, fear of increased vulnerability to the virus, and disruptions in health care services (6, 7). A recent systematic review and meta-analysis study found that the pooled prevalence rate of (moderate-to-severe) depressive symptoms among PLWH during the COVID-19 was 16.9% [95% confidence interval (CI): 3.8–30.0%] (6). Winters and colleagues compared the prevalence of depression among PLWH in Shinyanga region, Tanzania before and during COVID-19 and found substantially higher prevalence of depression (prevalence differences: 38; CI: 34, 42) (8). Given the existing health complications and increased risk of mental health issues, understanding the interplay between predictive factors and depressive symptoms among PLWH during COVID-19 is of paramount importance to enable more tailored and effective interventions for this population.
Internalized HIV stigma has been found to be one of the most significant risk factors of depressive symptoms among PLWH (9, 10). This stigma involves the incorporation of negative societal attitudes about HIV, resulting in self-disparagement, feelings of rejection and guilt (11). The harmful self-perceptions that individuals hold may serve as a direct antecedent to depressive symptoms. This occurs as individuals cultivate a negative self-concept and engage in harmful self-evaluations (12). In support of Meyer’s minority stress theory, which emphasizes the consequential role of stigma in generating psychological distress, individuals who belong to disadvantaged minority groups, such as PLWH, exhibit greater susceptibility to both external and internal stressors (13). These stressors are inextricably intertwined with instances of stigma and discrimination, making PLWH more vulnerable to depressive symptoms than their non-HIV peers (13).
Simultaneously, the COVID-19 pandemic may exacerbate internalized HIV stigma in addition to depressive symptoms (14). The additional stigma associated with the pandemic may intersect with and reinforce existing HIV-related stigma, exacerbating depressive symptoms (2). Because of their interrelated nature, understanding the complex relationship between internalized HIV stigma and depressive symptoms in PLWH during the COVID-19 pandemic is critical. Internalized stigma may exacerbate depressive symptoms through feelings of isolation, self-blame, and anticipated rejection. Conversely, the presence of depressive symptoms may increase the experience of internalized stigma, as individuals may further blame themselves for their condition (15). Additionally, existing evidence suggests that several underlying problems experienced by PLWH during COVID-19 may exacerbate the incidence of internalized stigma and depressive symptoms. For example, a scoping review of 45 articles found that several factors were related to increased psychological distress during the pandemic, including substance use, social support, financial hardship, antiretroviral adherence, and economic vulnerability (16). A recent qualitative study revealed that medical mistrust among PLWH might be associated with HIV stigma during the COVID-19 pandemic (17). It is therefore important for HIV researchers to explore the potential relationship between internalized HIV stigma and depressive symptoms during the pandemic in this population.
Although numerous empirical studies have documented the strong association between internalized HIV stigma and depressive symptoms, there is still a research gap regarding the network analysis model between internalized HIV stigma and depressive symptoms among PLWH during the COVID-19 pandemic. In this study, we attempted to use a novel analytical method—psychometric network analysis—to explore the relationship between these two variables in the context of the COVID-19 pandemic.
In contrast to traditional approaches that treat internalized HIV stigma and depressive symptoms as latent variables that are independent of each other, network analysis offers an alternative methodology capable of visualizing and quantifying the complexity inherent in such a system of interrelated variables (18–21). It provides a detailed understanding of these complex interactions and sheds light on the interplay between internalized HIV stigma and depressive symptoms within a larger context of psychosocial factors (22, 23). Using network analysis, elements of internalized HIV stigma and depressive symptoms are conceptualized as “nodes,” while the relationships between these elements are referred to as “edges” (24). When these nodes coexist within a population, they are considered to be directly connected. These critical links that serve as conduits between internalized HIV stigma and depressive symptoms are referred to as “bridges” in the network model (25).
Applied to the context of PLWH, this methodology can highlight specific attributes of internalized HIV stigma or specific depressive symptoms that exert a significant influence within the network. This identification is important for intervention development, as strategies can be tailored to address these key nodes, potentially leading to a more profound system-wide impact. In addition, network analysis helps to demystify the potential pathways linking internalized HIV stigma and depressive symptoms. Understanding these pathways is useful in creating predictive models, allowing clinicians and researchers to anticipate the progression of these symptoms based on network models (26). Such insights could provide timely indications for intervention, potentially averting further psychological distress. Therefore, network analysis can serve as a valuable tool for understanding and addressing the intertwined relationship between internalized HIV stigma and depressive symptoms among PLWH. By providing a nuanced and targeted understanding of this relationship, it can inform more effective strategies to alleviate psychological distress during challenging public health crisis in the future.
1.1 The current study
In the present study, we utilized network analysis to construct three different models: a network for internalized HIV stigma, a network for depressive symptoms, and a combined network model that includes both internalized HIV stigma and depressive symptoms. The objective was to identify critical “bridging nodes” that is the fundamental elements providing connections between internalized HIV stigma and depressive symptoms. Because network analysis is fundamentally a method for revealing key relationships within and across groups of nodes, we did not hypothesize about the particular nodes or edges that might emerge as central in these network models.
2 Materials and methods
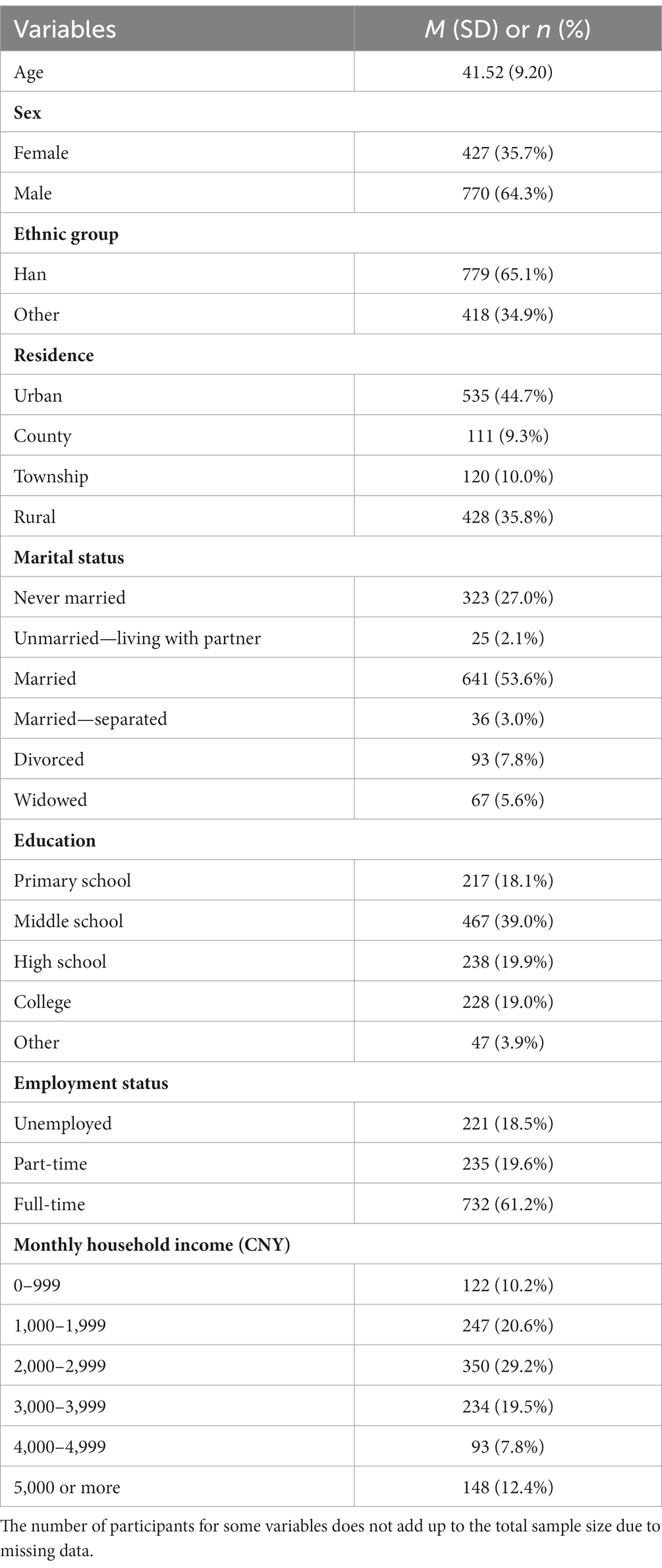
Data were drawn from a large cohort research project that attempted to explore the behavioral and mental health problems of PLWH in Guangxi, China (15, 27). The data were collected from May 2020 to October 2020. In collaboration with the Guangxi Center for Disease Control and Prevention (CDC), a strategic selection of study sites was made to conduct the research. We identified six hospitals and clinics in five cities based on their high numbers of HIV patients under care. This selection allowed us to focus on the sites with the largest HIV patient populations, thereby increasing the scope and relevance of our study. All participants were recruited from these local HIV clinics according to their medical records. This study was designed with precise inclusion criteria for participants: individuals who are aged between 18 and 60, diagnosed with HIV/AIDS, and have no plans to relocate from Guangxi for subsequent follow-up investigations lasting more than 12 months. Excluded from participation were those with language, mental, or physical impairments that might affect their ability to respond to assessment questions; those currently detained or institutionalized for drug use or involvement in commercial sex; or those intending to leave the province within the next year. In total, the study included 1,197 PLWH who successfully completed the survey. Sample demographics are shown in Table 1.
Ethical approval to conduct this study was granted by the Institutional Review Boards of University of South Carolina. The study procedures were fully disclosed to all participants, who were informed of the purpose of the study, the confidentiality of their responses, and their rights as participants. This information included their freedom to withdraw from the study at any time. After providing informed consent, participants were asked to complete a questionnaire administered by an interviewer. The interview-style questionnaires were administered by nurses trained by experts with more than 10 years of research experience with PLWH. In recognition of their contribution to the study, participants were offered an incentive of US$5.00 (equivalent to approximately 35 RMB, the Chinese currency).
2.1 Measures
2.1.1 Depressive symptoms
Depressive symptoms were assessed by a Chinese version of the Center of Epidemiological Studies Depression Scale (CESD-10) (28). The questionnaire contains 10 items, each rated on a four-point scale from 1 (rarely or none of the time) to 4 (all the time). Sample items include “I had trouble keeping my mind on what I was doing” and “My sleep was restless.” This questionnaire has shown good reliability and construct validity in Chinese samples (29, 30). A higher total score indicates a higher level of depressive symptoms. Cronbach’s alpha reliability for the CESD-10 in this study was 0.81.
2.1.2 Internalized HIV stigma
The assessment of internalized HIV stigma was conducted using an adapted Chinese version of eight items from the Negative Self Image Scale (31). Previous research with Chinese PLWH has demonstrated satisfactory validity and reliability for the Chinese version of this questionnaire (32, 33). Examples of the items include, “Having HIV makes me feel like I’m a bad person” and “I feel guilty because I have HIV.” This instruction consists of eight items, each rated on a four-point scale from 1 (strongly disagree) to 4 (strongly agree). A higher total score indicates a higher level of internalized HIV stigma. In the current study, the scale demonstrated excellent internal consistency, Cronbach’s alpha reliability was 0.94.
To ensure relevance to the COVID-19 context, we supplemented these with some COVID-19-specific instructions. This approach allowed us to capture the nuanced ways in which the pandemic has affected depressive symptoms and internalized stigma, despite the generic nature of these instruments.
2.2 Data analysis
Data management, univariate statistics, and network analyses were performed using SPSS 23.0 and R software version 4.2.2. Analyses of the distributions of internalized HIV stigma and depressive symptoms indicated that they did not deviate significantly from normality. Specifically, assessments of skewness and kurtosis-measures were used to describe the shape and distribution of the data-indicated nominal deviations. The absolute values for skewness ranged from 0.01 to 2.19, while those for kurtosis ranged from 0.05 to 5.66. These results suggest that the data for internalized HIV stigma and depressive symptoms were reasonably well distributed, allowing for the subsequent use of parametric statistical methods (34).
We implemented the graphical Least Absolute Shrinkage and Selection Operator (LASSO) method to establish regularized partial correlation networks (24). These networks were then visualized using the qgraph package (35). We assessed the centrality of each node within these networks by calculating the Expected Influence (EI), an effective centrality index. This step allowed us to identify the most influential nodes within each network model (36). In our approach, we created separate regularized partial correlation networks for internalized HIV stigma and depressive symptoms. We then merged these into a combined network model to examine their potential coexistence (20, 37). To understand the interplay between internalized HIV stigma and depressive symptoms within the combined network model, we used the networktools package. This tool facilitated the calculation of the Bridge Expected Influence (BEI), which allowed us to identify which nodes served as “bridges” between these two phenomena (38). Nodes with the highest BEI values were designated as bridge nodes in this model (38). To ensure the reliability of our network models, we used the bootnet package. We performed 1,000 case-dropping bootstraps to calculate the correlation stability coefficient (CS-coefficient), which measures the stability of each network model (39). Following previous researchers’ suggestions (24, 40), we used a CS-coefficient cutoff of 0.25 and set the default value for the bootstrapping procedure at r = 0.7.
3 Results
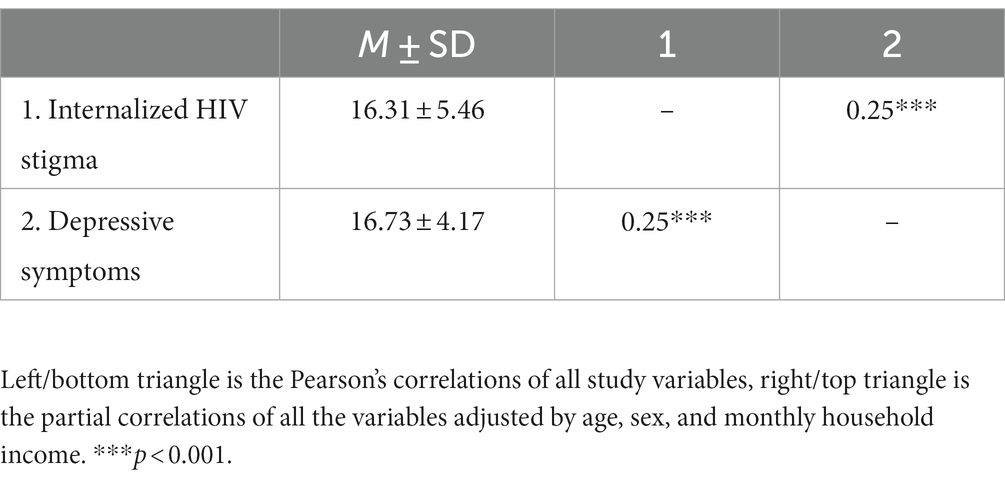
Descriptive statistics for this study, including means, standard deviations, and intercorrelations of the variables of interest, are detailed in Table 2. In addition, Table 3 describes the names of the nodes used in the network analysis for internalized HIV stigma and depressive symptoms, and presents univariate statistics for each node.
3.1 Internalized HIV stigma network model
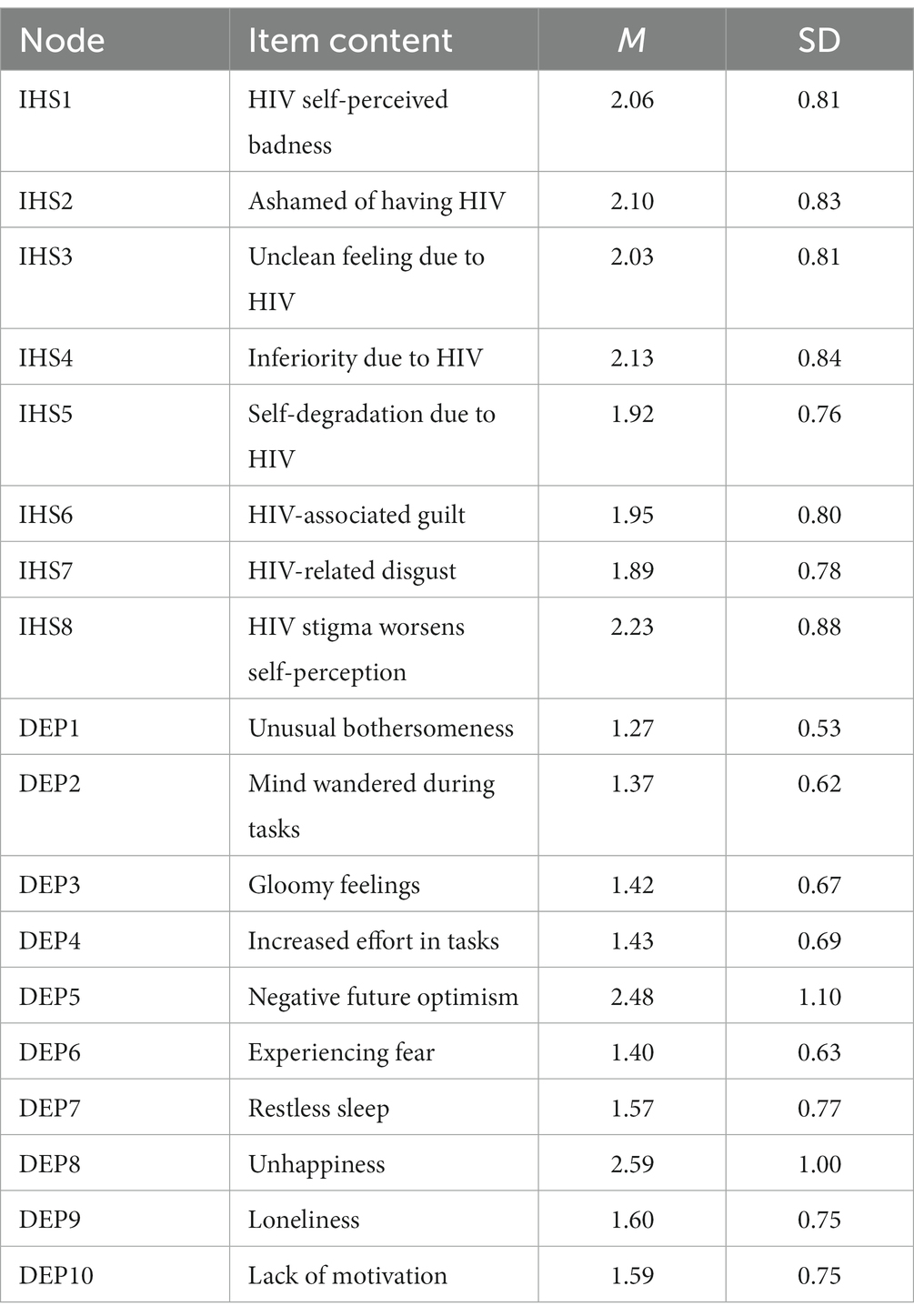
Figure 1 provides a visualization of the network structure of internalized HIV stigma, including the EI value for each node. The stability of the internalized HIV stigma network model is confirmed by acceptable CS-coefficients for edge weights [CS (cor = 0.7) = 0.75] and EI values [CS (cor = 0.7) = 0.74], according to the stability criteria (24). Within this model, the symptom “Ashamed of having HIV” (IHS2) emerged as the most influential node, followed by “Self-degradation due to HIV” (IHS5). The symptom with the least centrality was “HIV stigma worsens self-perception” (IHS8). The strongest edges were between “HIV self-perceived badness” (IHS1) and “Ashamed of having HIV” (IHS2), and between “HIV-associated guilt” (IHS6) and “HIV-related disgust” (IHS7). Supplementary Figure S1 shows the standardized estimates of node strength, betweenness, closeness, and expected influence, while Supplementary Figure S2 shows the bootstrapped confidence intervals (CIs) for the edge weights.
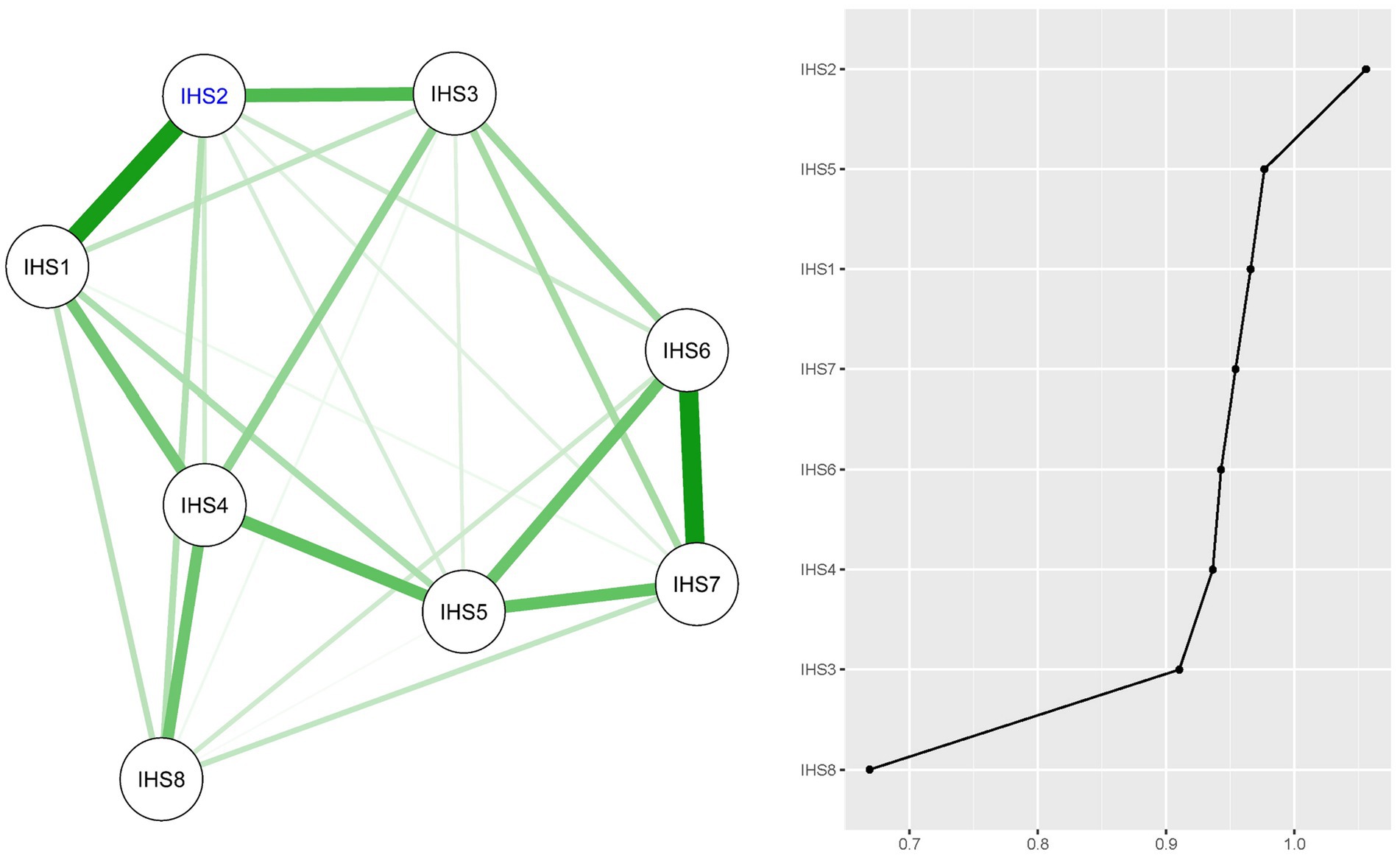
Figure 1. Regularized partial correlation network model for internalized HIV stigma (IHS) and expected influence (EI) values for each node. Node with largest EI value is represented by blue text (IHS2).
3.2 Depressive symptoms network model
The network model of depressive symptoms is shown in Figure 2, with edge weights [CS (cor = 0.7) = 0.75] and EI values [CS (cor = 0.7) = 0.75] confirming a stable network model of depressive symptoms. The symptom “Mind wandered during tasks” (DEP2) occupied the most central node in the network, while “Negative future optimism” (DEP5) held the position of the least central symptom. The strongest edge within the depressive symptoms network was found between “Negative future optimism” (DEP5) and “Unhappiness” (DEP8). Supplementary Figure S3 details the standardized estimates for node strength, betweenness, closeness, and expected influence, and Supplementary Figure S4 provides the bootstrapped confidence intervals (CIs) for the edge weights.
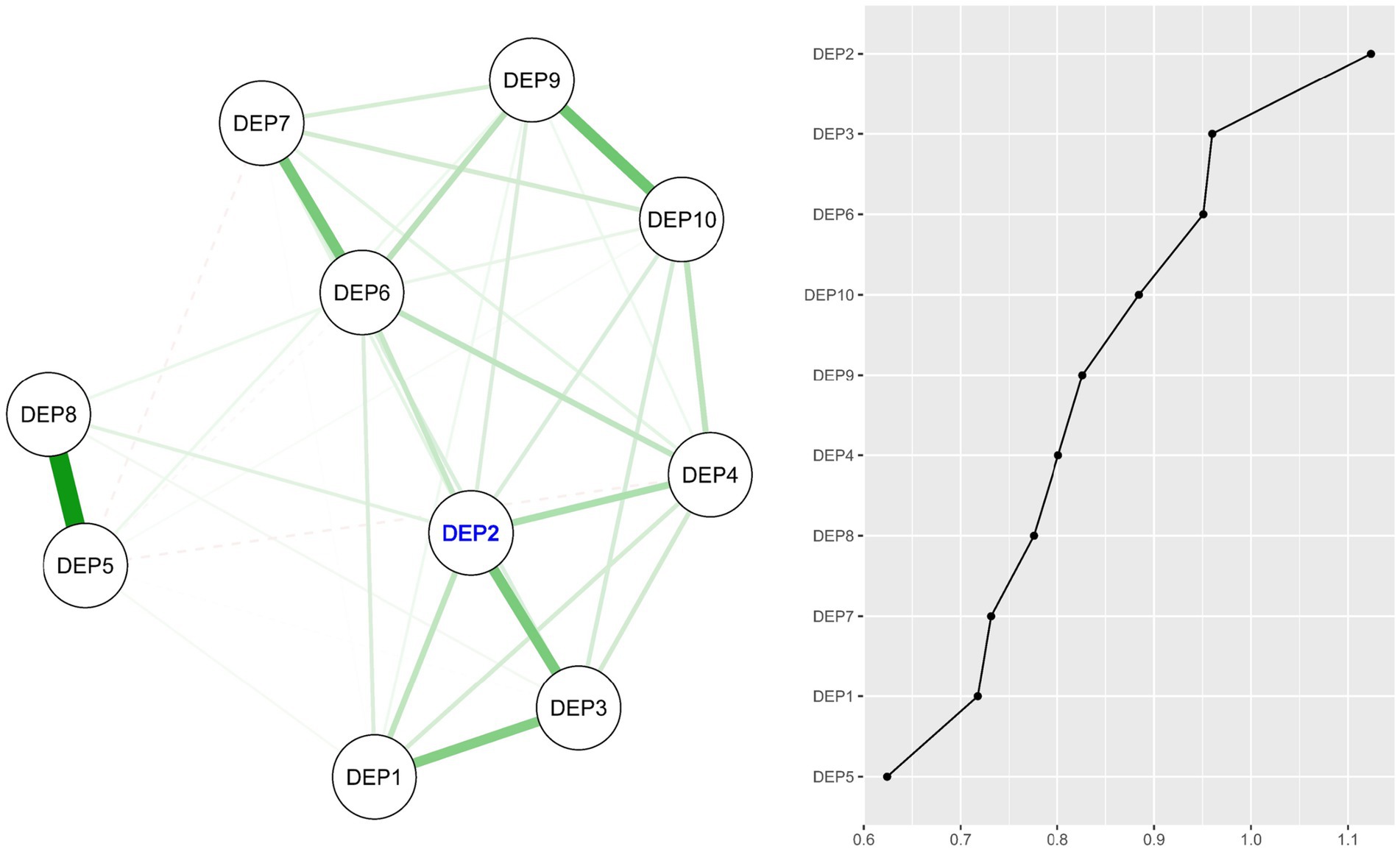
Figure 2. Regularized partial correlation network model for depressive symptoms (DEP) and expected influence (EI) values for each node. Node with largest EI value is represented by blue text (DEP2).
3.3 Combined internalized HIV stigma and depressive symptoms network model
Figure 3 presents the combined network model that connects internalized HIV stigma and depressive symptoms. The stability of the model is confirmed by CS-coefficient values for edge weights [CS (cor = 0.7) = 0.75] and for BEI values [CS (cor = 0.7) = 0.48]. Within this combined network model, the nodes “Inferiority due to HIV” (IHS4) from the internalized HIV stigma community and “Gloomy feelings” (DEP3) from the depressive symptoms cluster were highlighted as bridge nodes owing to their highest one-step BEI values. The metrics of node strength, betweenness, closeness, and expected influence are standardized and represented in Supplementary Figure S5. Furthermore, Supplementary Figure S6 illustrates the bootstrapped confidence intervals (CIs) corresponding to the edge weights.
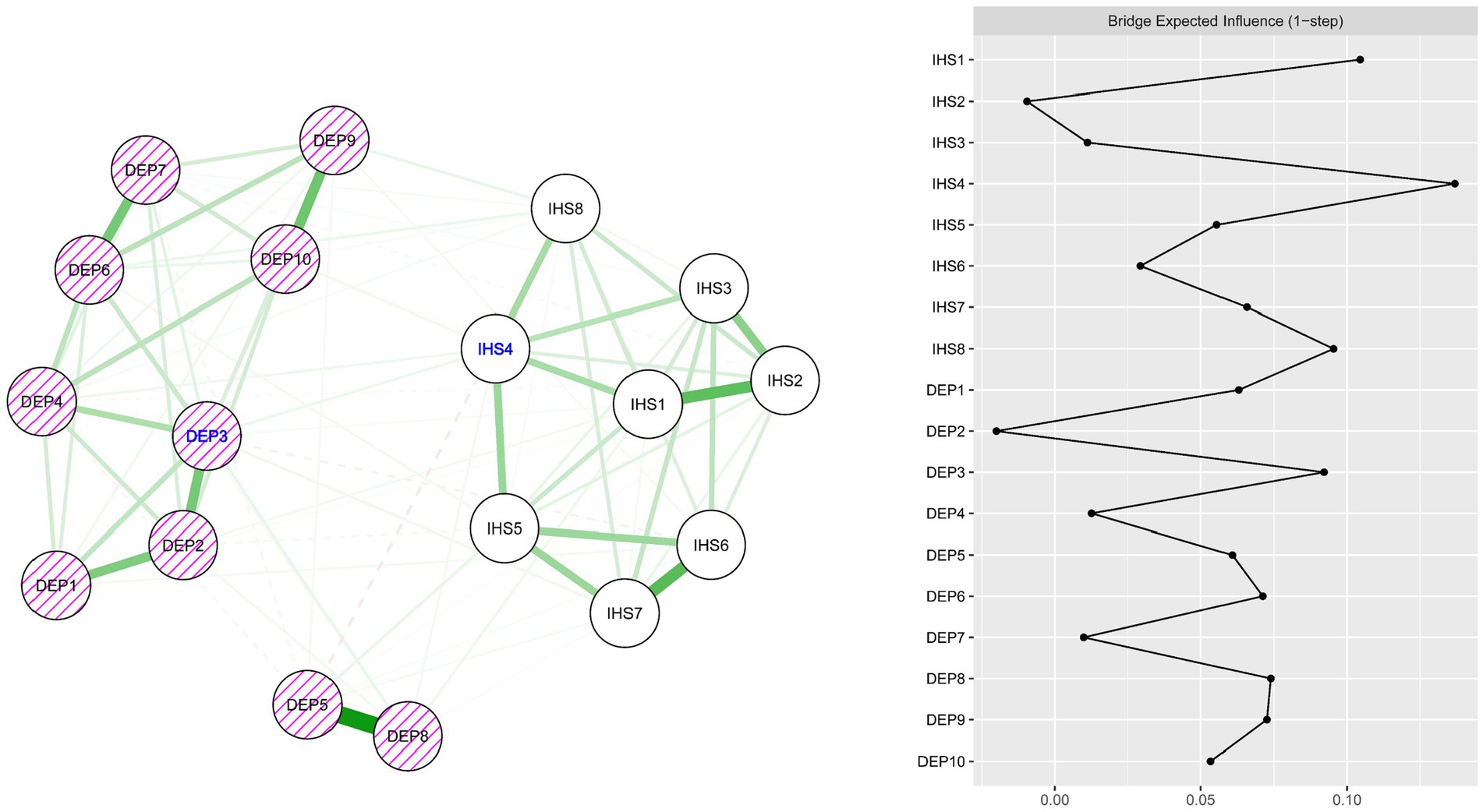
Figure 3. Combined regularized partial correlation network model for internalized HIV stigma (IHS) and depressive symptoms (DEP3) and bridge expected influence (BEI) values for each node. Bridge nodes with large BEI values are represented by blue text (IHS4 and DEP3).
4 Discussion
In this study, network analysis was utilized to explore the network structures of internalized HIV stigma, depressive symptoms, and their interactions in a large sample of 1,197 Chinese PLWH during the COVID-19 pandemic. This investigation is innovative because, to our understanding, it is the first to explore network models of internalized HIV stigma and depressive symptoms. It also examines the possible co-occurrence of internalized HIV stigma and depressive symptoms and identifies the bridge between these two psychological phenomena among the marginalized and vulnerable population.
Our study provides valuable insights into the network structure of internalized HIV stigma and depressive symptoms among PLWH during the COVID-19 pandemic. One of the key findings was that “ashamed of having HIV” emerged as the most central node within the internalized HIV stigma network, indicating its pivotal role in the interconnected system of stigma-related experiences. This suggests that shame associated with HIV diagnosis may significantly influence other stigma-related experiences and contribute to the overall burden of internalized stigma. Such a finding is consistent with previous research highlighting the detrimental effects of shame on individuals’ self-esteem and psychological well-being (41–44). The central role of shame in the internalized HIV stigma network underscores the need for interventions that specifically target and mitigate feelings of shame associated with an HIV diagnosis, especially when PLWH are facing public health crises. Our research recognizes that some components of internalized HIV stigma, such as the centrality of “ashamed of having HIV,” are not limited to the COVID-19 outbreak. Nonetheless, our investigation specifically sheds light on how the exceptional difficulties presented by the pandemic could have intensified and influenced these persistent factors of stigma and depression in individuals living with HIV. The COVID-19 pandemic has led to several challenges for PLWH, including amplified feelings of shame, guilt, and depressive symptoms due to increased social isolation, heightened health anxieties, and disruptions in healthcare services. Our network analysis, while based on established measures, contextualizes these phenomena within the specific challenges faced by PLWH during COVID-19, underscoring the pandemic’s impact on their mental health.
The centrality of “mind wandered during tasks” in the depressive symptoms network highlights the impact of cognitive dysfunction on PLWH’s daily functioning and mental health status. This finding aligns with previous research showing that cognitive difficulties are a common symptom of depression that can exacerbate other depressive symptoms and impede overall recovery (45–48). Cognitive difficulties can interfere with an individual’s ability to effectively engage in self-care behaviors, interpersonal interactions, and other activities critical to managing HIV and maintaining good mental health (49–51). Additionally, the process of mind wandering is often associated with a lack of focus, decreased productivity, and an overall diminished ability to engage in the present moment, all of which are common characteristics of depression (52–54). Frequent mind wandering may indicate a struggle to manage or control thoughts, which can lead to an increased experience of depressive symptoms (55, 56). Within the context of the COVID-19 pandemic, this finding suggests that pandemic-induced stressors, such as prolonged isolation and health anxiety, significantly worsen cognitive disruptions. Specifically, these factors have intensified PLWH’s difficulty in maintaining focus on daily tasks, a key aspect of depressive symptomatology.
Our network analysis also identified two critical bridge connections between the internalized HIV stigma and depressive symptoms communities—“inferiority due to HIV” and “gloomy feelings.” These bridge nodes suggest a reciprocal influence between these two psychological constructs, where feelings of inferiority due to HIV may lead to or exacerbate gloomy feelings, and vice versa. The bridge node “inferiority due to HIV” suggests that feelings of inferiority due to HIV status may act as a link between stigma and depressive symptoms. It may be that individuals who internalize societal stigma about HIV begin to perceive themselves as less than others because of their HIV status (57, 58). This sense of inferiority could subsequently trigger or exacerbate depressive symptoms. Inferiority could potentially lead to negative self-esteem and lack of self-worth, key aspects often associated with depressive states (59–64). On the other hand, “gloomy feelings” serving as a bridge node indicates that these symptoms are not only a consequence of internalized HIV stigma, but could also potentially feed back into the internalized HIV stigma cycle. Depression can lead to a negative cognitive bias, in which individuals interpret their experiences more negatively (65–67). Therefore, those with depressive symptoms may perceive their HIV status in a more negative light, thereby increasing the internalization of HIV stigma.
These bridge nodes highlight the possible bidirectional and complex relationship between internalized HIV stigma and depressive symptoms, suggesting a potentially cyclical and self-perpetuating system. The more an individual feels inferior because of their HIV status, the more susceptible they may become to depressive symptoms. In turn, these depressive symptoms could further increase feelings of stigma, creating a reinforcing loop. Recognizing the role of “inferiority due to HIV” and “gloomy feelings” as bridge nodes illuminates pathways through which HIV stigma and depressive symptoms may interact and influence each other. This insight underlines the importance of addressing both internalized HIV stigma and depressive symptoms in a holistic and integrated manner in mental health interventions, particularly in the context of the COVID-19 pandemic, which has exacerbated both of these challenges for PLWH.
4.1 In the context of COVID-19
Our study utilized network analysis to investigate the patterns of internalized HIV stigma and depressive symptoms among PLWH during the COVID-19 pandemic. The results revealed that “ashamed of having HIV” and “mind wandered during tasks” played central roles in the networks of internalized stigma and depressive symptoms, respectively. These findings underscore the significant influence of shame and cognitive dysfunction on the experiences of individuals living with HIV during the pandemic. Notably, the findings suggest that “inferiority due to HIV” and “gloomy feelings” play a critical role as bridge nodes, reflecting a potential bidirectional influence between internalized HIV stigma and depressive symptoms. The results suggest that the COVID-19 pandemic may have intensified these experiences, exacerbating the sense of inferiority and gloominess among people living with HIV. These findings highlight the intricate relationship between internalized HIV stigma and depressive symptoms during the pandemic, emphasizing the necessity for comprehensive and integrated mental health interventions. It is critical to address both internalized stigma and depressive symptoms, particularly given the supplementary stressors caused by COVID-19, including heightened social isolation and health anxieties.
4.2 Limitations and implications
Several limitations of this study must be acknowledged. First, the cross-sectional design of the study limits our ability to make causal inferences regarding the temporal characteristics and directional effects of associations between internalized HIV stigma items and depressive symptoms (18, 19). While our findings provide a preliminary empirical basis for future hypotheses, further longitudinal and experimental studies are needed to explore the temporal sequences and potential causal relationships between these psychological phenomena (20, 21). Second, the study relied on self-reported data, which may be susceptible to response bias. Future research would benefit from using multiple data collection methods, such as observer ratings, structured diagnostic interviews, and mixed methods, to minimize potential bias. Third, it should be noted that in the current study, we used the CESD-10 to assess participants’ depressive symptoms. Measurements with diagnostic function are recommended in future research exploring network analysis regarding depression in PLWH. Finally, the interpretation of which bridge symptoms are significant may be influenced by subjectivity, as bridge centrality does not necessarily indicate effect size (68). Therefore, additional research is needed to clarify the role and interpretation of bridge centrality in the context of internalized HIV stigma and depressive symptoms.
Despite the limitations, our research has significant implications for future strategies in public health and medical practice. In particular, this study highlights “inferiority due to HIV” and “gloomy feelings” as key bridging elements linking internalized HIV stigma and depressive symptoms among Chinese PLWH during the COVID-19 crisis. Expanding on these findings, understanding the central role of these bridge elements may provide a new focus for health professionals in addressing mental health concerns among PLWH. Therapeutic interventions should aim to address feelings of inferiority associated with HIV and manage depressive symptoms, such as cognitive behavioral therapy-based and mindfulness-based interventions (69–72). This approach can potentially break the cycle of stigma and depressive emotions, thereby improving mental health outcomes for this population (71–73). In a broader public health context, these findings highlight the need for stigma reduction initiatives. Programs aimed at improving societal attitudes toward HIV and providing mental health support to those affected could play an important role in reducing both internalized HIV stigma and related depressive symptoms (74). Increasing the availability and accessibility of mental health services for people living with HIV could help manage depressive symptoms more effectively (75). The health care community could use these findings to develop specific tools and resources to facilitate the management of feelings of inferiority and depressive symptoms among PLWH. This could include the development of psychosocial support groups, cognitive-behavioral interventions, or resilience-building programs tailored specifically for PLWH (74). Finally, our findings suggest that depression measurement in PLWH, particularly in the context of the COVID-19 pandemic, may benefit from the inclusion of items that capture the nuanced influence of HIV-related stigma on depressive symptoms and from a greater focus on symptom-specific measurement. These considerations could improve the accuracy and utility of depression measurement, thereby informing more effective interventions for this population. In addition, the implications of our study extend beyond the COVID-19 pandemic. The structures of internalized HIV stigma and depressive symptoms that we identified, along with their interactions, provide valuable insights for mental health interventions in any prolonged crisis or epidemic setting among PLWH. Understanding these intricate relationships aids in customizing strategies for alleviating depressive symptoms and internalized stigma, ultimately leading to improved mental health outcomes. This information is crucial for upcoming public health responses and mental health support structures, guaranteeing their suitability and efficiency during both pandemic and post-pandemic periods.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of University of South Carolina. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
GY: Conceptualization, Data curation, Formal analysis, Methodology, Software, Validation, Visualization, Writing – original draft. SQ: Data curation, Investigation, Project administration, Resources, Supervision, Writing – original draft. XL: Data curation, Funding acquisition, Project administration, Resources, Supervision, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The research was supported by National Institutes of Health (NIH)/National Institutes of Mental Health (NIMH) (Grant no. R01MH0112376).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1306414/full#supplementary-material
References
1. Chenneville, T, Gabbidon, K, Hanson, P, and Holyfield, C. The impact of COVID-19 on HIV treatment and research: a call to action. Int J Environ Res Public Health. (2020) 17:4548. doi: 10.3390/ijerph17124548
2. Sun, S, Hou, J, Chen, Y, Lu, Y, Brown, L, and Operario, D. Challenges to HIV care and psychological health during the COVID-19 pandemic among people living with HIV in China. AIDS Behav. (2020) 24:2764–5. doi: 10.1007/s10461-020-02903-4
3. Perumal, R, Shunmugam, L, Naidoo, K, Abdool Karim, SS, Wilkins, D, Garzino-Demo, A, et al. Long COVID: a review and proposed visualization of the complexity of long COVID. Front Immunol. (2023) 14:1117464. doi: 10.3389/fimmu.2023.1117464
4. Hoosain, NY. Developing predictive models for depression and risktaking behavior among people living with HIV and AIDS (PLWHA): A focus on the construction of the Self and Implicative Dilemmas. (2016).
5. De Francesco, D. Assessing Comorbidity Burden, Ageing and Cognitive Impairment of People Living with HIV. PhD Thesis. UCL (University College London). (2020)
6. Lee, KW, Ang, CS, Lim, SH, Siau, CS, Ong, LTD, Ching, SM, et al. Prevalence of mental health conditions among people living with HIV during the COVID-19 pandemic: A rapid systematic review and meta-analysis. HIV Med. (2022) 23:990–1001. doi: 10.1111/hiv.13299
7. Dyer, J, Wilson, K, Badia, J, Agot, K, Neary, J, Njuguna, I, et al. The psychosocial effects of the COVID-19 pandemic on youth living with HIV in Western Kenya. AIDS Behav. (2021) 25:68–72. doi: 10.1007/s10461-020-03005-x
8. Winters, S, Sabasaba, A, Fahey, CA, Packel, L, Katabaro, E, Ndungile, Y, et al. Increased prevalence of depression and anxiety among adults initiating antiretroviral therapy during the COVID-19 pandemic in Shinyanga region, Tanzania. AIDS Res Ther. (2023) 20:36. doi: 10.1186/s12981-023-00534-y
9. Turan, B, Rice, WS, Crockett, KB, Johnson, M, Neilands, TB, Ross, SN, et al. Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: the mediating role of depression. AIDS (London, England). (2019) 33:571–6. doi: 10.1097/QAD.0000000000002071
10. Earnshaw, VA, Smith, LR, Cunningham, CO, and Copenhaver, MM. Intersectionality of internalized HIV stigma and internalized substance use stigma: Implications for depressive symptoms. J Health Psychol. (2015) 20:1083–9. doi: 10.1177/1359105313507964
11. Earnshaw, VA, Smith, LR, Chaudoir, SR, Amico, KR, and Copenhaver, MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. (2013) 17:1785–95. doi: 10.1007/s10461-013-0437-9
12. Elder, J, Cheung, B, Davis, T, and Hughes, B. Mapping the self: A network approach for understanding psychological and neural representations of self-concept structure. J Pers Soc Psychol. (2023) 124:237–63. doi: 10.1037/pspa0000315
13. Meyer, IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. (2003) 129:674–97. doi: 10.1037/0033-2909.129.5.674
14. Jarolimova, J, Yan, J, Govere, S, Ngobese, N, Shazi, ZM, Khumalo, AR, et al. Medical mistrust and stigma associated with COVID-19 among people living with HIV in South Africa. AIDS Behav. (2021) 25:3967–77. doi: 10.1007/s10461-021-03307-8
15. Yuan, GF, Tam, CC, Yang, X, Qiao, S, Li, X, Shen, Z, et al. Associations between internalized and anticipated HIV stigma and depression symptoms among people living with HIV in China: A four-wave longitudinal model. AIDS Behav. (2023) 27:4052–61. doi: 10.1007/s10461-023-04119-8
16. Hong, C, Queiroz, A, and Hoskin, J. The impact of the COVID-19 pandemic on mental health, associated factors and coping strategies in people living with HIV: a scoping review. J Int AIDS Soc. (2023) 26:e26060. doi: 10.1002/jia2.26060
17. Hall, A, Joseph, O, Devlin, S, Kerman, J, Schmitt, J, Ridgway, JP, et al. “That same stigma…that same hatred and negativity:” a qualitative study to understand stigma and medical mistrust experienced by people living with HIV diagnosed with COVID-19. BMC Infect Dis. (2021) 21:1066. doi: 10.1186/s12879-021-06693-5
18. Lazarov, A, Suarez-Jimenez, B, Levi, O, Coppersmith, DDL, Lubin, G, Pine, DS, et al. Symptom structure of PTSD and co-morbid depressive symptoms – a network analysis of combat veteran patients. Psychol Med. (2020) 50:2154–70. doi: 10.1017/S0033291719002034
19. Fried, EI, and Cramer, AOJ. Moving Forward: Challenges and Directions for Psychopathological Network Theory and Methodology. Perspect Psychol Sci. (2017) 12:999–1020. doi: 10.1177/1745691617705892
20. Yuan, GF, Shi, W, Elhai, JD, Montag, C, Chang, K, Jackson, T, et al. Gaming to cope: Applying network analysis to understand the relationship between posttraumatic stress symptoms and internet gaming disorder symptoms among disaster-exposed Chinese young adults. Addict Behav. (2022) 124:107096. doi: 10.1016/j.addbeh.2021.107096
21. Yuan, G, Park, CL, Birkeland, SR, Yip, PSY, and Hall, BJ. A Network Analysis of the Associations Between Posttraumatic Stress Symptoms and Posttraumatic Growth Among Disaster-Exposed Chinese Young Adults. J Trauma Stress. (2021) 34:786–98. doi: 10.1002/jts.22673
22. Vasiliou, VS, Russell, H, Cockayne, S, de Holanda Coelho, GL, and Thompson, AR. A network analysis of psychological flexibility, coping, and stigma in dermatology patients. Front Med. (2023) 10:1075672. doi: 10.3389/fmed.2023.1075672
23. Mannarini, S, Taccini, F, and Rossi, AA. Stigma toward internalizing and externalizing disorders: How do adolescents perceive their peers? A network analysis approach. J Res Adolesc. (2023) 33:803–15. doi: 10.1111/jora.12839
24. Epskamp, S, and Fried, EI. A tutorial on regularized partial correlation networks. Psychol Methods. (2018) 23:617–34. doi: 10.1037/met0000167
25. Cramer, AO, Waldorp, LJ, Van Der Maas, HL, and Borsboom, D. Comorbidity: A network perspective. Behav Brain Sci. (2010) 33:137–50. doi: 10.1017/S0140525X09991567
26. Papini, S, Rubin, M, Telch, MJ, Smits, JAJ, and Hien, DA. Pretreatment Posttraumatic Stress Disorder Symptom Network Metrics Predict the Strength of the Association Between Node Change and Network Change During Treatment. J Trauma Stress. (2020) 33:64–71. doi: 10.1002/jts.22379
27. Yang, X, Li, X, Qiao, S, Shen, Z, and Zhou, Y. Socioeconomic disparity of immunologic outcome among people living with HIV in Guangxi, China. AIDS Care. (2021) 33:347–51. doi: 10.1080/09540121.2020.1738004
28. Andresen, EM, Malmgren, JA, Carter, WB, and Patrick, DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am J Prev Med. (1994) 10:77–84. doi: 10.1016/S0749-3797(18)30622-6
29. Jiang, L, Wang, Y, Zhang, Y, Li, R, Wu, H, Li, C, et al. The reliability and validity of the center for epidemiologic studies depression scale (CES-D) for Chinese university students. Front Psych. (2019) 10:315. doi: 10.3389/fpsyt.2019.00315
30. Yu, SC, Lin, YH, and Hsu, WH. Applying structural equation modeling to report psychometric properties of Chinese version 10-item CES-D depression scale. Qual Quant. (2013) 47:1511–8. doi: 10.1007/s11135-011-9604-0
31. Berger, BE, Ferrans, CE, and Lashley, FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Res Nurs Health. (2001) 24:518–29. doi: 10.1002/nur.10011
32. Mi, T, Lan, G, Yang, X, Li, X, Qiao, S, Shen, Z, et al. HIV-Related Stigma, Sexual Identity, and Depressive Symptoms Among MSM Living With HIV in China: A Moderated Mediation Modeling Analysis. Am J Mens Health. (2022) 16:15579883221087531. doi: 10.1177/15579883221087531
33. Yu, C, Huang, C, Lee, Y, and Cheng, S. Development of an 18-item abbreviated Chinese version of Berger’s HIV Stigma Scale. Int J Nurs Pract. (2019) 25:e12708. doi: 10.1111/ijn.12708
34. Griffin, MM. Steinbrecher TD. Large-scale datasets in special education research. Int Rev Res Dev Disabil. 45:155–83. doi: 10.1016/B978-0-12-407760-7.00004-9
35. Epskamp, S, Cramer, AO, Waldorp, LJ, Schmittmann, VD, and Borsboom, D. qgraph: Network visualizations of relationships in psychometric data. J Stat Softw. (2012) 48:1–18. doi: 10.18637/jss.v048.i04
36. Robinaugh, DJ, Millner, AJ, and McNally, RJ. Identifying highly influential nodes in the complicated grief network. J Abnorm Psychol. (2016) 125:747–57. doi: 10.1037/abn0000181
37. Peters, J, Bellet, BW, Jones, PJ, Wu, GW, Wang, L, and McNally, RJ. Posttraumatic stress or posttraumatic growth? Using network analysis to explore the relationships between coping styles and trauma outcomes. J Anxiety Disord. (2021) 78:102359. doi: 10.1016/j.janxdis.2021.102359
38. Jones, PJ, Ma, R, and McNally, RJ. Bridge centrality: A network approach to understanding comorbidity. Multivar Behav Res. (2021) 56:353–67. doi: 10.1080/00273171.2019.1614898
39. Epskamp, S, and Fried, EI. bootnet: Bootstrap Methods for Various Network Estimation Routines. (2021). Available at: https://CRAN.R-project.org/package=bootnet (Accessed January 19, 2023).
40. Epskamp, S, Borsboom, D, and Fried, EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav Res Methods. (2018) 50:195–212. doi: 10.3758/s13428-017-0862-1
41. Pradipto, YD, and Setiadi, BN. the role of internalized stigma and perceived discrimination regarding the self-esteem of people living with HIV/AIDS in Jakarta. ANIMA Indonesian Psychol J. (2018) 33:241–249. doi: 10.24123/aipj.v33i4.1797
42. Kurniawan, D, and Fitrio, D. Impact of HIV-related stigma: self-efficacy, self-esteem, and social isolation on ARV medication adherence among persons living with HIV in Turen, Malang. Pak J Med Health Sci. (2019) 13:1112–4.
43. Kalomo, EN. Associations between HIV-related stigma, self-esteem, social support, and depressive symptoms in Namibia. Aging Ment Health. (2018) 22:1570–6. doi: 10.1080/13607863.2017.1387763
44. Adimora, DE, Aye, EN, Akaneme, IN, Nwokenna, EN, and Akubuilo, FE. Stigmatization and discrimination as predictors of self-esteem of people living with HIV and AIDS in Nigeria. Afr Health Sci. (2019) 19:3160–71. doi: 10.4314/ahs.v19i4.39
45. Vanek, J, Prasko, J, Genzor, S, Ociskova, M, Kantor, K, Holubova, M, et al. Obstructive sleep apnea, depression and cognitive impairment. Sleep Med. (2020) 72:50–8. doi: 10.1016/j.sleep.2020.03.017
46. McIntyre, RS, Xiao, HX, Syeda, K, Vinberg, M, Carvalho, AF, Mansur, RB, et al. The prevalence, measurement, and treatment of the cognitive dimension/domain in major depressive disorder. CNS Drugs. (2015) 29:577–89. doi: 10.1007/s40263-015-0263-x
47. McIntyre, RS, Lee, Y, and Mansur, RB. Treating to target in major depressive disorder: response to remission to functional recovery. CNS Spectr. (2015) 20:17–31. doi: 10.1017/S1092852915000826
48. Cristancho, P, Lenze, EJ, Avidan, MS, and Rawson, KS. Trajectories of depressive symptoms after hip fracture. Psychol Med. (2016) 46:1413–25. doi: 10.1017/S0033291715002974
49. Zvolensky, MJ, Garey, L, Rogers, AH, Schmidt, NB, Vujanovic, AA, Storch, EA, et al. Psychological, addictive, and health behavior implications of the COVID-19 pandemic. Behav Res Ther. (2020) 134:103715. doi: 10.1016/j.brat.2020.103715
50. Waldron, EM, Burnett-Zeigler, I, Wee, V, Ng, YW, Koenig, LJ, Pederson, AB, et al. Mental health in women living with HIV: the unique and unmet needs. J Int Assoc Prov AIDS Care (JIAPAC). (2021) 20:232595822098566. doi: 10.1177/2325958220985665
51. Harkness, A, Rogers, BG, Puccinelli, M, Ivardic, I, Ironson, G, and Safren, SA. Engaging, retaining, and providing transdiagnostic integrated cognitive–behavioral therapy and motivational interviewing for underserved people with HIV. Psychotherapy. (2020) 57:15–22. doi: 10.1037/pst0000270
52. Seli, P, Beaty, RE, Marty-Dugas, J, and Smilek, D. Depression, anxiety, and stress and the distinction between intentional and unintentional mind wandering. Psychol Conscious Theory Res Pract. (2019) 6:163–70. doi: 10.1037/cns0000182
53. Greenberg, J, Datta, T, Shapero, BG, Sevinc, G, Mischoulon, D, and Lazar, SW. Compassionate hearts protect against wandering minds: Self-compassion moderates the effect of mind-wandering on depression. Spiritual Clin Pract. (2018) 5:155–69. doi: 10.1037/scp0000168
54. Figueiredo, T, Lima, G, Erthal, P, Martins, R, Corção, P, Leonel, M, et al. Mind-wandering, depression, anxiety and ADHD: Disentangling the relationship. Psychiatry Res. (2020) 285:112798. doi: 10.1016/j.psychres.2020.112798
55. Joormann, J, and Stanton, CH. Examining emotion regulation in depression: A review and future directions. Behav Res Ther. (2016) 86:35–49. doi: 10.1016/j.brat.2016.07.007
56. Bernstein, EE, Heeren, A, and McNally, RJ. Unpacking rumination and executive control: A network perspective. Clin Psychol Sci. (2017) 5:816–26. doi: 10.1177/2167702617702717
57. Earnshaw, VA, Bogart, LM, Dovidio, JF, and Williams, DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol. (2015) 1:60–74. doi: 10.1037/2376-6972.1.S.60
58. Berg, RC, and Ross, MW. The second closet: A qualitative study of HIV stigma among seropositive gay men in a southern US city. Int J Sex Health. (2014) 26:186–99. doi: 10.1080/19317611.2013.853720
59. Wei, L, Yan, H, Guo, M, Tian, J, Jiang, Q, Zhai, M, et al. Perceived HIV stigma, depressive symptoms, self-esteem, and suicidal ideation among people living with HIV/AIDS in China: A moderated mediation modeling analysis. J Racial Ethn Health Disparities. (2023) 10:671–9. doi: 10.1007/s40615-022-01255-0
60. Manhas, C. Self-esteem and quality of life of people living with HIV/AIDS. J Health Psychol. (2014) 19:1471–9. doi: 10.1177/1359105313493812
61. Eller, LS, Rivero-Mendez, M, Voss, J, Chen, WT, Chaiphibalsarisdi, P, Iipinge, S, et al. Depressive symptoms, self-esteem, HIV symptom management self-efficacy and self-compassion in people living with HIV. AIDS Care. (2014) 26:795–803. doi: 10.1080/09540121.2013.841842
62. Wong, MYC, Fung, HW, and Yuan, GF. The association between physical activity, self-compassion, and mental well-being after COVID-19: in the exercise and self-esteem model revised with self-compassion (EXSEM-SC) perspective. Healthcare. (2023) 11:233. doi: 10.3390/healthcare11020233
63. Singh, S, and Kaur, R. Problems of frustration, aggression and low self-esteem among adolescents. Int J Multidiscip Res Dev. (2015) 2:901–4.
64. Liu, C. Research on the influence of college students’ participation in sports activities on their sense of inferiority based on self-esteem and general self-efficacy. Front Psychol. (2022) 13:994209. doi: 10.3389/fpsyg.2022.994209
65. Platt, B, Waters, AM, Schulte-Koerne, G, Engelmann, L, and Salemink, E. A review of cognitive biases in youth depression: attention, interpretation and memory. Cognit Emot. (2017) 31:462–83. doi: 10.1080/02699931.2015.1127215
66. LeMoult, J, Kircanski, K, Prasad, G, and Gotlib, IH. Negative self-referential processing predicts the recurrence of major depressive episodes. Clin Psychol Sci. (2017) 5:174–81. doi: 10.1177/2167702616654898
67. LeMoult, J, and Gotlib, IH. Depression: A cognitive perspective. Clin Psychol Rev. (2019) 69:51–66. doi: 10.1016/j.cpr.2018.06.008
68. Christensen, AP, Garrido, LE, and Golino, H. What is bridge centrality? A comment on Jones, Ma, and McNally. (2019). Published online January 20, 2021. doi: 10.31234/osf.io/a8svr
69. Scott-Sheldon, LA, Balletto, BL, Donahue, ML, Feulner, MM, Cruess, DG, Salmoirago-Blotcher, E, et al. Mindfulness-based interventions for adults living with HIV/AIDS: a systematic review and meta-analysis. AIDS Behav. (2019) 23:60–75. doi: 10.1007/s10461-018-2236-9
70. Riley, KE, and Kalichman, S. Mindfulness-based stress reduction for people living with HIV/AIDS: preliminary review of intervention trial methodologies and findings. Health Psychol Rev. (2015) 9:224–43. doi: 10.1080/17437199.2014.895928
71. Shi, Y, Zhao, M, Chen, S, Wang, S, Li, H, Ying, J, et al. Effects of cognitive behavioral therapy on people living with HIV and depression: a systematic review and meta-analysis. Psychol Health Med. (2019) 24:578–94. doi: 10.1080/13548506.2018.1549739
72. Andersen, LS, Magidson, JF, O’Cleirigh, C, Remmert, JE, Kagee, A, Leaver, M, et al. A pilot study of a nurse-delivered cognitive behavioral therapy intervention (Ziphamandla) for adherence and depression in HIV in South Africa. J Health Psychol. (2018) 23:776–87. doi: 10.1177/1359105316643375
73. Mendez, NA, Mayo, D, and Safren, SA. Interventions addressing depression and HIV-related outcomes in people with HIV. Curr HIV/AIDS Rep. (2021) 18:377–90. doi: 10.1007/s11904-021-00559-w
74. Li, X, Qiao, S, Yang, X, Harrison, SE, Tam, CC, Shen, Z, et al. A Resilience-Based Intervention to Mitigate the Effect of HIV-Related Stigma: Protocol for a Stepped Wedge Cluster Randomized Trial. Frontiers. Public Health. (2022) 10:10. doi: 10.3389/fpubh.2022.857635
Keywords: internalized HIV stigma, depressive symptoms, PLWH, COVID-19, network analysis
Citation: Yuan GF, Qiao S and Li X (2024) Bridging internalized HIV stigma and depressive symptoms among people living with HIV in China during the COVID-19 pandemic: a network analysis. Front. Public Health. 11:1306414. doi: 10.3389/fpubh.2023.1306414
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Angga Wilandika, Universitas Aisyiyah Bandung, IndonesiaQi Wang, The University of Hong Kong, Hong Kong SAR, China
Copyright © 2024 Yuan, Qiao and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guangzhe F. Yuan, yb97316@umac.mo
 Guangzhe F. Yuan
Guangzhe F. Yuan Shan Qiao
Shan Qiao Xiaoming Li
Xiaoming Li