- 1Division of Health Systems Science, Department of Medicine, UMass Chan Medical School, Worcester, MA, United States
- 2Division of Pulmonary and Critical Care Medicine, Department of Medicine, UMass Chan Medical School, Worcester, MA, United States
- 3Tan Chingfen Graduate School of Nursing, UMass Chan Medical School, Worcester, MA, United States
- 4Boston Medical Center, Boston, MA, United States
- 5Section of Infectious Diseases, Department of Medicine, Boston University School of Medicine, Boston, MA, United States
- 6Boston University School of Public Health, Boston, MA, United States
Introduction: The COVID-19 pandemic has been characterized by disparities in disease burden and medical care provision. Whether these disparities extend to long COVID awareness and receipt of medical care is unknown. We aimed to characterize awareness of long COVID and receipt of medical care for long COVID symptoms among populations who experience disparities in the United States (US).
Methods: We conducted a cross-sectional survey among a national sample of US adults between January 26–February 5, 2023. We surveyed approximately 2,800 adults drawn from the Ipsos probability-based KnowledgePanel® who identify as White, Black, or Hispanic, with over-sampling of Black, Hispanic, and Spanish-proficient adults. Awareness of long COVID was assessed with the question, “Have you heard of long COVID? This is also referred to as post-COVID, Long-haul COVID, Post-acute COVID-19, or Chronic COVID.” Respondents reporting COVID-19 symptoms lasting longer than 1 month were classified as having long COVID and asked about receipt of medical care.
Results: Of the 2,828 respondents, the mean age was 50.4 years, 52.8% were female, 40.2% identified as Hispanic, 29.8% as Black, and 26.7% as White. 18% completed the survey in Spanish. Overall, 62.5% had heard of long COVID. On multivariate analysis, long COVID awareness was lower among respondents who identified as Black (OR 0.64; 95% CI 0.51, 0.81), Hispanic and completed the survey in English (OR 0.59; 95% CI 0.46, 0.76), and Hispanic and completed the survey in Spanish (OR 0.31, 95% C.I. 0.23, 0.41), compared to White respondents (overall p < 0.001). Long COVID awareness was also associated with educational attainment, higher income, having health insurance, prior history of COVID-19 infection, and COVID-19 vaccination. Among those reporting symptoms consistent with long COVID (n = 272), 26.8% received medical care. Older age, longer symptom duration and greater symptom impact were associated with receipt of medical care for long COVID symptoms. Of those who received care, most (77.8%) rated it as less than excellent on a 5-point scale.
Discussion: This survey reveals limited awareness of long COVID and marked disparities in awareness according to race, ethnicity, and language. Targeted public health campaigns are needed to raise awareness.
Introduction
During the initial phase of the COVID-19 pandemic, it became clear that some individuals who survived the acute phase of infection with SARS-CoV-2, the virus that causes COVID-19, do not experience a full recovery, but instead continue to experience symptoms weeks and months later. Long COVID, also known as post-acute sequelae of SARS-CoV-2 infection (PASC), is defined by the continuation, exacerbation, or new development of any one of a variety of wide-ranging, multisystem symptoms at least 4 weeks after initial COVID-19 infection and is not dependent on the severity of initial infection (1, 2). Commonly reported symptoms of long COVID include fatigue, respiratory and cardiac symptoms, neurological issues including brain fog, and joint pain (1–4). Lingering debilitating symptoms can impede a patient’s ability to work and negatively impact their quality of life (5, 6). In addition, some patients suffer from symptoms that are difficult to diagnose, resulting in delayed receipt of appropriate care (2). With the estimated prevalence of long COVID ranging from 6.9–40% of all people diagnosed with COVID, long COVID is a major public health concern (7–9).
The COVID-19 pandemic has been characterized by significant racial, ethnic, and socioeconomic disparities in the United States (US), with higher COVID-19 case rates, hospitalizations, and deaths among Black, Latino, and socioeconomically disadvantaged communities (10–15). Limited English proficiency has also emerged as a risk factor for COVID-19 infection, highlighting the limited reach of public health information among non-English speaking communities (16). In addition to disparities in disease burden, the COVID-19 pandemic has laid bare structural disparities in access to medical care, including COVID-19 diagnostics (17), vaccines (18), and treatment (19). The potential for these existing disparities in healthcare access to compound the frequent challenges that have been described among long COVID patients in accessing medical care (20, 21) is concerning. A few qualitative studies have documented the experience of long COVID among members of racial and ethnic minorities (22–24), but disparities in awareness of long COVID and utilization patterns of medical care for long COVID among a broader population have not been examined.
The goal of this study was to characterize awareness of long COVID and receipt of medical care for long COVID among populations at risk of healthcare disparities. We also describe the experience of those patients who received care for long COVID.
Methods
Study design
This is an observational, cross-sectional study, using a self-administered online survey.
Setting
We surveyed a sample of adults residing in the United States via the Ipsos KnowledgePanel®, an online panel representative of the entire US population. Ipsos recruits panel members using probability-based sampling methods; potential panel members are provided with internet access and hardware if needed. Both English and Spanish speakers are recruited to the KnowledgePanel®.
Participants
For the present survey, we recruited KnowledgePanel® members who identified as White, Black, and/or Hispanic. We oversampled Black, Hispanic, and Spanish-proficient Hispanic adults to enhance racial and ethnic diversity and ensure adequate representation of non-English speaking adults in the sub-sample of respondents with symptoms consistent with long COVID. In addition, we oversampled Spanish-proficient Hispanic adults to confirm the findings of a prior pilot survey that suggested there may be disparities in long COVID awareness among Spanish speakers. Ipsos sent email invitations to panel members, with reminder emails to non-responders three and 7 days after the initial invitation. The survey was available in English and Spanish. Participants received an incentive valued at ~$5 for their participation. We conducted the survey between January 26 and February 5, 2023.
Variables
The primary outcome was awareness of long COVID, assessed with the question, “Have you heard of long COVID? This is also referred to as post-COVID, Long-haul COVID, Post-acute COVID-19, or Chronic COVID.” A secondary outcome was report of symptoms consistent with long COVID, defined by the presence of COVID-19 symptoms lasting longer than 1 month, among respondents with a history of COVID-19 infection. An additional secondary outcome was receipt of medical care among respondents with symptoms consistent with long COVID.
Co-variates included sociodemographic items (e.g., race, ethnicity, education, insurance status), beliefs related to long COVID, history of COVID-19 infection, COVID-19 vaccination status, and long COVID symptom duration and impact (among respondents with symptoms consistent with long COVID). Respondents who did not receive medical care for symptoms of long COVID were asked why they did not pursue care or were not able to see a provider for their long COVID symptoms (open-ended response). Those who received medical care for their long COVID symptoms were asked to provide an overall rating of the care they received with response options: excellent; very good; good; fair; and poor. Respondents who rated their care as less than excellent were asked the open-ended question, “Please tell us how your care fell short, and what should be done differently in the future.” The full set of items included in the survey for the present study are provided in Supplementary file S1. The survey items were pre-tested in a small (n ~ 300) study with a local sample. Demographic information (e.g., age, education level, household income) was provided by members when they joined the panel.
We constructed five categories to reflect participants’ reported race, ethnicity, and language in a single variable: White, non-Hispanic; Black, non-Hispanic; Hispanic, survey completed in English; Hispanic, survey completed in Spanish; other or more than one race, non-Hispanic.
For the question “Have you had COVID-19,” we combined ‘Yes, had it once’ and ‘Yes, had it more than once’ into a single category. We dichotomized insurance status into ‘no insurance’ and ‘any insurance’. To examine care seeking related to long COVID, we categorized participants as having symptoms consistent with long COVID if they responded that they had COVID-19 at least once and they had experienced COVID-19 symptoms that lasted for at least 1 month. We further categorized participants who met these criteria as (a) having sought and received medical care or (b) having not received medical care at the time of the survey (not sought or sought care but not received). We combined the latter two groups (not sought care and sought care but not received) because our goal was to predict receipt of care and describe the experience of care among those who received it. The group who sought care but had not received it was small (n = 20).
Spanish language responses to the open-ended items (e.g., Why did not you pursue care for your long COVID symptoms?) were professionally translated into English for analysis.
Statistical methods
We used means, frequencies, and percentages to summarize participant characteristics. We computed chi-square statistics to examine the associations between participant characteristics and awareness of long COVID. To create a parsimonious model predicting long COVID awareness, we used a backward stepwise approach starting with standard demographic variables (race/ethnicity/language, age, gender, and education), and all additional variables that we hypothesized to be associated with long COVID awareness that also showed some evidence of possible association in the bivariate analyses (i.e., resulted in p < 0.20). The final model retained race/ethnicity/language, age, and gender independent of statistical significance. We used a similar approach to identify factors associated with receipt of medical care among respondents who reported symptoms consistent with long COVID. In addition to retaining standard demographics independent of statistical significance, this model also retained insurance status (no insurance vs. any insurance) given its relevance to receipt of care. For participants who received care, we computed descriptive statistics for their perceptions of care (taken seriously and satisfaction), whether they were diagnosed with long COVID and whether they were referred elsewhere for further care. Statistical analyses were performed with SAS version 9.4 (SAS Institute Inc., Cary, NC, United States) and SPSS version 28.0.1.0 (IBM SPSS Statistics, Armonk, NY, United States).
Qualitative analyses
We used conventional content analysis to separately analyze responses to each open-ended item (25). At least two authors reviewed a subset of the responses and generated an initial set of codes. Four authors (KF, KM, LG, HA) reviewed and discussed the initial coding scheme; modifications and clarifying distinctions were made based on that discussion. Two authors (LG, HA) then independently coded all responses in Excel. These two authors met to compare codes and to identify disagreements and questions. Questions and disagreements which were not readily resolved were brought to the senior authors (KF and/or KM, both experienced qualitative researchers) for further discussion and resolution. We summarized the themes identified in reasons given for not seeking and receiving care, and themes in responses describing how care fell short for those who received care but rated the care as less than excellent. Coding of responses to open-ended items was performed in Excel.
Results
Response rate and respondent characteristics
There were 2,840 completed surveys among the 5,097 KnowledgePanel® members invited to respond, for an overall completion rate of 55.7%. The analytic sample for this study consists of 2,828 respondents who either responded to the question assessing long COVID awareness (n = 2,827) and/or responded affirmatively to experiencing symptoms consistent with long COVID (n = 272). Of these, the mean age was 50.4 years (range 18–94), approximately half were female (n = 1,493; 52.8%), 40.2% identified as Hispanic, 29.8% as Black, and 26.7% as White. Nearly one-fifth (n = 508; 18.0%) completed the survey in Spanish. Additional demographic characteristics are provided in Table 1.
Long COVID awareness
Overall, 62.5% of respondents had heard of long COVID. Characteristics associated with having heard of long COVID on bivariate analysis are shown in Table 1. In multivariate analysis (Table 2), several factors were associated with increased odds of having heard of long COVID. For example, the odds of having heard of long COVID were more than twice as high in respondents with a master’s degree or higher (OR 2.21; 95% CI 1.49, 3.26) than in those without a high school diploma or GED, and those with an annual income of greater than $75,000 had a two-fold higher odds of having heard of long COVID (OR 2.08; 95% CI 1.38, 3.12) than those earning less than $10,000 annually. Additional factors associated with having heard of long COVID on multivariate analysis included having health insurance (OR 1.55; 95% CI 1.15, 2.08), a history of prior COVID-19 infection (OR 1.37; 95% C.I. 1.15, 1.64), and receipt of at least one dose of a COVID-19 vaccine (OR 1.34; 95% C.I. 1.06, 1.69). After multivariate adjustment, members of racial and ethnic minority groups remained significantly less likely to have heard of long COVID. Compared to White respondents, odds of having heard of long COVID were more than 25% lower among respondents who identify as Black (OR 0.64; 95% CI 0.51, 0.81), and odds of having heard of long COVID were 40% lower among those who identify as Hispanic and completed the survey in English (OR 0.59; 95% CI 0.46, 0.76). Respondents who identify as Hispanic and completed the survey in Spanish were least likely to have heard of long COVID (OR 0.31, 95% CI 0.23, 0.41) compared to White respondents who completed the survey in English.

Table 2. Associations between respondent characteristics and long COVID awareness, results from multivariable analysis.
Receipt and experience of medical care for long COVID
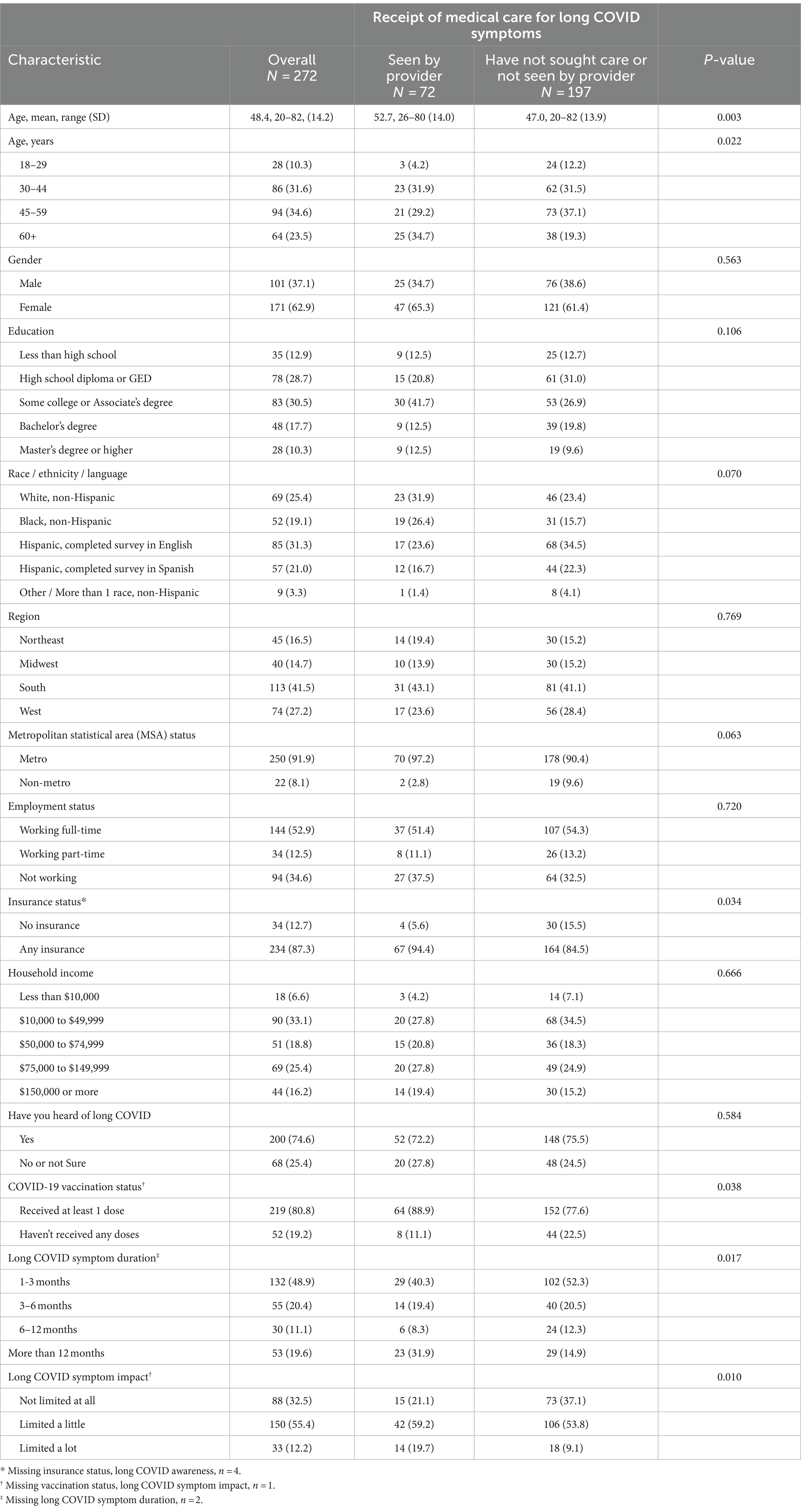
Of the 1,365 respondents who reported a history of COVID-19 infection, 272 (19.9%) reported symptoms consistent with long COVID (any symptom lasting longer than 1 month). Of those with symptoms consistent with long COVID, 25.4% (n = 68) had not heard of it. Nearly half (n = 132; 48.9%) reported a symptom duration of 1–3 months, and most were either not limited at all (n = 88; 32.5%) or limited a little (n = 150; 55.4%) by their long COVID symptoms (Table 3). Approximately one-quarter (n = 72; 26.8%) reported having been seen by a healthcare provider for their symptoms of long COVID. The most common reasons for not having been seen by a healthcare provider for symptoms of long COVID included that it did not occur to the respondent to seek care (n = 121), their symptoms were mild (n = 15), they expected their symptoms would get better with time (n = 15), they did not think anything could be done (n = 7), they could not afford an appointment (n = 7), there was a long wait for an appointment (n = 5), and they were too busy with competing health issues or had not prioritized seeking care (n = 5).
Factors associated with having seen a healthcare provider for symptoms of long COVID on bivariate analysis are shown in Table 3. In multivariate analysis, factors associated with having been seen by a healthcare provider for long COVID included older age (OR 1.03; 95% CI 1.01, 1.05), symptom duration longer than 12 months (OR 2.62; 95% CI 1.24, 5.57), and being limited “a lot” by long COVID symptoms (OR 3.44; 95% CI 1.28, 9.28) (Table 4).
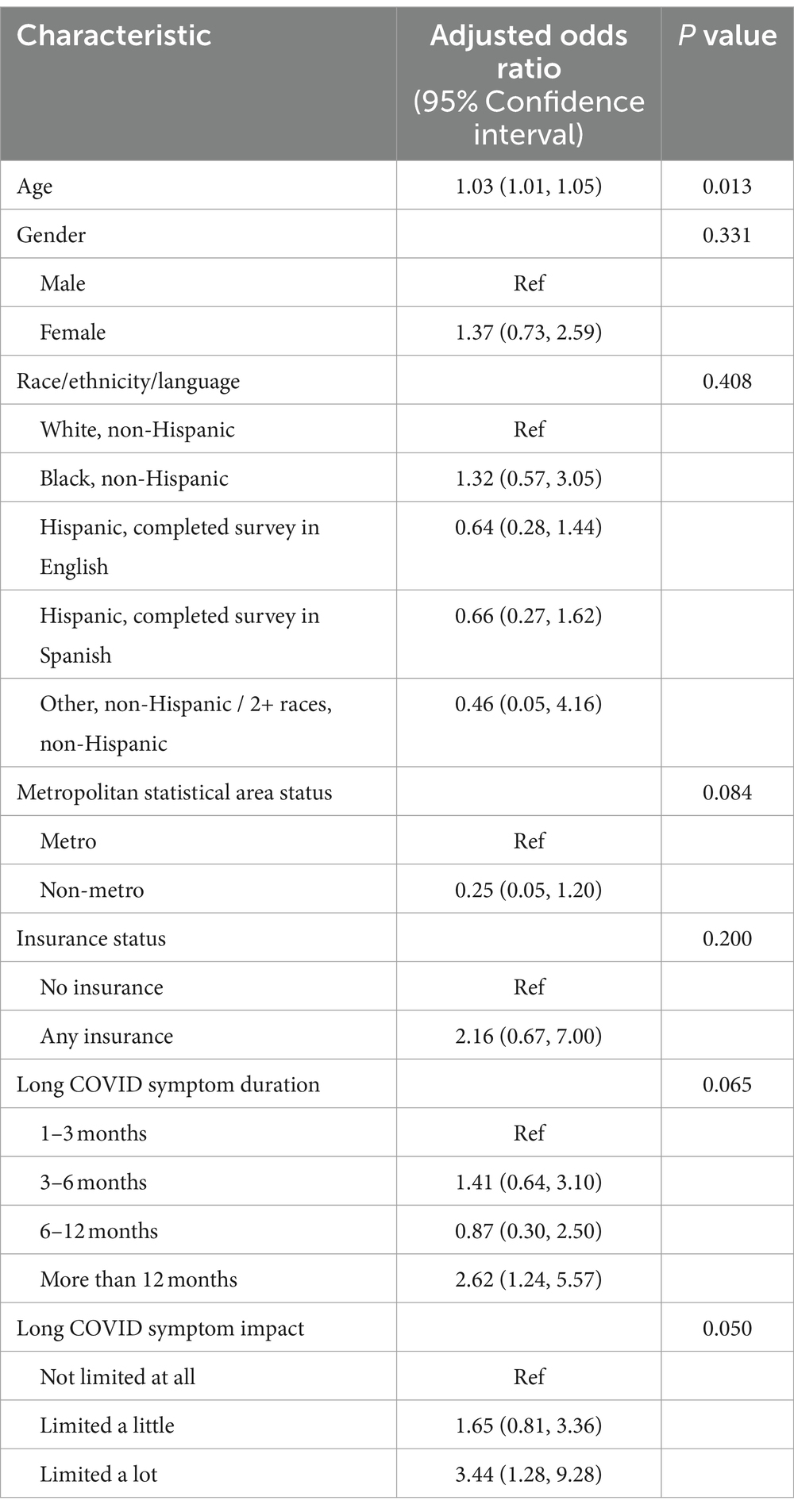
Table 4. Associations between respondent characteristics and receipt of medical care for long COVID symptoms, results from multivariable analysis.
Of the respondents with symptoms consistent with long COVID who had been seen by a healthcare provider for these symptoms (n = 72), approximately one-half (47.2%) reported being diagnosed with long COVID, and 14 (19.4%) were referred for additional medical care elsewhere. Most (56/72; 77.8%) rated the care they received as less than excellent. Of those who provided a reason why care fell short (n = 30), the most common reason (n = 19) was dissatisfaction with the lack of knowledge (“Her answer was ‘not a lot is known about long COVID.’ What do you do with that answer?”) and/or treatments (“I feel like I still have symptoms and there are no medications to heal it”) for long COVID. Other reasons included feeling like the provider did not listen, take them seriously, or was dismissive (“the cough is still there to this day and the physician ignored or never addressed my concerns”; n = 7), and wanting more testing or evaluation of their symptoms (n = 4). Most respondents (n = 61; 84.7%) somewhat or strongly agreed that the provider they saw for symptoms of long COVID took them seriously, but some (n = 11; 15.3%) disagreed.
Discussion
In this large survey that oversampled Black and Hispanic respondents, we found low rates of awareness of long COVID; nearly four in ten respondents had not heard of long COVID. Although there are no benchmarks for acceptable levels of public awareness, the limited awareness in this survey is striking given the magnitude of the COVID-19 pandemic overall and of long COVID specifically. As many as 35% of people with COVID-19 infection report having symptoms more than 60 days after infection (26), and the economic burden of long COVID is estimated to be a staggering $3.7 trillion (27), making it a major public health challenge. In the absence of currently approved treatments specific for long COVID, public awareness is critical to encouraging preventative behaviors, such as vaccination and treatment with oral antivirals which both appear to reduce the risk of developing long COVID or post-COVID conditions (PCC) (28–30). Indeed, in the present study, we found that long COVID awareness is positively associated with COVID-19 vaccination status supporting the idea that awareness of long COVID may be an important lever for motivating and promoting uptake of preventative behaviors.
In addition to low overall awareness, we also found marked disparities in awareness of long COVID according to race, ethnicity, and language, even after controlling for other social determinants of health such as education and income. Long COVID awareness was lowest among Hispanic respondents who completed the survey in Spanish. Although the present study was only conducted in English and Spanish, our findings suggest that long COVID awareness may also be low among other populations with limited English proficiency in the US. Low long COVID awareness in these populations may compound existing disparities in receipt of COVID-19 boosters (31–33) and oral antivirals (19). Concerted efforts to increase awareness of long COVID tailored for communities with limited English proficiency and members of racial and ethnic minority groups are needed.
Although long COVID awareness may be important for promoting preventative behaviors, it does not appear to drive healthcare utilization for long COVID. We did not find an association between long COVID awareness and receipt of medical care for long COVID symptoms. Our quantitative and qualitative results indicate that receipt of medical care for long COVID is primarily driven by both the duration and impact of symptoms suggesting that patients with protracted and/or severe symptoms seek care regardless of whether they are aware that their symptoms could be consistent with long COVID. At the same time, a quarter of patients with symptoms consistent with long COVID had not heard of it. Even if their symptoms may be less severe, medical care can still offer a diagnosis which for some patients can provide validation of their experience of symptoms (34), an additional potential benefit of increased public awareness.
Among the subset of respondents with symptoms consistent with long COVID who received care for these symptoms, only 22.2% rated their care for long COVID as excellent, indicating a need to improve the clinical care of patients with long COVID. A common reason for rating care as less than excellent was the perception that the provider had inadequate knowledge about long COVID. We also found a substantial minority of respondents who reported the provider was dismissive of their symptoms, consistent with other reports of patients with long COVID symptoms describing “medical gaslighting” (35). The proportion of respondents in the present study describing dismissive providers (15.8%) is lower than in a prior study (34%) conducted in 2021 (35). This difference may reflect improved provider knowledge and understanding about long COVID more recently or may simply be due to differences in populations sampled. The experiences of medical care by respondents with symptoms of long COVID in our study highlight the need for increased primary care provider education about long COVID, as has been called for in other reports (36–39).
The primary strength of this study is the large and diverse sample that allowed us to assess multiple aspects of long COVID from awareness to receipt of and experience of medical care for long COVID symptoms, including among non-primary English speakers. This study also has limitations. Because we oversampled specific populations to achieve diversity, the estimate of long COVID awareness is not nationally representative and does not include all racial groups. We relied on respondent’s self-report of history of COVID-19 infection which could result in misclassification. However, this is consistent with how patients with potential long COVID will come to medical attention. Although we used the CDC’s definition of long COVID, a universal challenge related to studying long COVID is the multiple definitions that rely on symptom report. Because our goal was not to describe the prevalence of long COVID, this limitation is not central to our findings. Further, our finding that 19.9% of respondents with a history of COVID-19 infection reported symptoms consistent with long COVID is in keeping with estimates from other US studies that have found symptoms lasting longer than 4 weeks among 10–30% of people with COVID-19 (36). Despite the large sample size, only a small proportion of respondents received care for long COVID symptoms limiting the conclusions we can draw about receipt of and experience of medical care for long COVID.
Conclusion
This large survey with oversampling of populations at risk of disparities in the US, documents limited overall awareness of long COVID and marked disparities in awareness among members of racial/ethnic minority groups and those with limited English proficiency. Reducing the risk of long COVID may be an important motivator for promoting uptake of preventative behaviors. Low public awareness of long COVID could reduce the impact of this as a lever for mitigating the major public health burden of long COVID. Public health efforts focused on building awareness of long COVID among members of racial/ethnic minority groups and those with limited English proficiency are needed.
Data availability statement
The datasets in this article will be made available upon reasonable request to the corresponding author and with an executed data use agreement in place. Requests to access the datasets should be directed to Kimberly.Fisher2@umassmed.edu.
Ethics statement
The studies involving humans were approved by the Boston University Medical Center Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/ next of kin because this study was deemed exempt by the reviewing IRB. As such, we provided participants with abbreviated consent language before they began study activities.
Author contributions
KF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft. KM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft. ME: Conceptualization, Methodology, Writing – original draft. LG: Data curation, Investigation, Writing – review & editing. HA: Data curation, Investigation, Writing – review & editing. YZ: Formal analysis, Writing – review & editing. SC: Formal analysis, Writing – review & editing. JM: Writing – review & editing, Conceptualization. BL: Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was funded by the NHLBI via a contract with Westat, grant number OT2HL158287 (Westat).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer RS declared a shared parent affiliation, with the authors JM and BL to the handling editor at the time of the review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1360341/full#supplementary-material
References
1. Pfaff, ER, Madlock-Brown, C, Baratta, JM, Bhatia, A, Davis, H, Girvin, A, et al. Coding long COVID: characterizing a new disease through an ICD-10 lens. BMC Med. (2023) 21:58. doi: 10.1186/s12916-023-02737-6
2. Centers for Disease Control and Prevention . Long COVID or post-COVID conditions. Available at: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (Accessed December 16, 2022).
3. Nalbandian, A, Sehgal, K, Gupta, A, Madhavan, MV, McGroder, C, Stevens, JS, et al. Post-acute COVID-19 syndrome. Nat Med. (2021) 27:601–15. doi: 10.1038/s41591-021-01283-z
4. Thaweethai, T, Jolley, SE, Karlson, EW, Levitan, EB, Levy, B, McComsey, GA, et al. Development of a definition of postacute sequelae of SARS-CoV-2 infection. JAMA. (2023) 329:1934–46. doi: 10.1001/jama.2023.8823
5. Malik, P, Patel, K, Pinto, C, Jaiswal, R, Tirupathi, R, Pillai, S, et al. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-a systematic review and meta-analysis. J Med Virol. (2022) 94:253–62. doi: 10.1002/jmv.27309
6. Davis, HE, McCorkell, L, Vogel, JM, and Topol, EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. (2023) 21:133–46. doi: 10.1038/s41579-022-00846-2
7. Ogungbe, O, Slone, S, Alharthi, A, Tomiwa, T, Kumbe, B, Bergman, A, et al. "living like an empty gas tank with a leak": mixed methods study on post-acute sequelae of COVID-19. PLoS One. (2022) 17:e0279684. doi: 10.1371/journal.pone.0279684
8. Bull-Otterson, L, Baca, S, Saydah, S, Boehmer, TK, Adjei, S, Gray, S, et al. Post–COVID conditions among adult COVID-19 survivors aged 18–64 and ≥65 years — United States, march 2020–November 2021. MMWR Morb Mortal Wkly Rep. (2022) 71:713–7. http://dx.doi.org/10.15585/mmwr.mm7121e1
9. Adjaye-Gbewonyo, D, Vahratian, A, Perrine, CG, and Bertolli, J. Long COVID in adults: United States, 2022. NCHS Data Brief. (2023) 480:1–8. doi: 10.15620/cdc:132417
10. Garg, S, Kim, L, Whitaker, M, O’Halloran, A, Cummings, C, Holstein, R, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 states, march 1–30, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:458–64. doi: 10.15585/mmwr.mm6915e3
11. Gold, JAW, Wong, KK, Szablewski, CM, Patel, PR, Rossow, J, da Silva, J, et al. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19 — Georgia, march 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:545–50. http://dx.doi.org/10.15585/mmwr.mm6918e1.
12. Vahidy, FS, Nicolas, JC, Meeks, JR, Khan, O, Pan, A, Jones, SL, et al. Racial and ethnic disparities in SARS-CoV-2 pandemic: analysis of a COVID-19 observational registry for a diverse US metropolitan population. BMJ Open. (2020) 10:e039849. doi: 10.1136/bmjopen-2020-039849
13. Yancy, CW . COVID-19 and African Americans. JAMA. (2020) 323:1891–2. doi: 10.1001/jama.2020.6548
14. Khazanchi, R, Beiter, ER, Gondi, S, Beckman, AL, Bilinski, A, and Ganguli, I. County-level association of social vulnerability with COVID-19 cases and deaths in the USA. J Gen Intern Med. (2020) 35:2784–7. doi: 10.1007/s11606-020-05882-3
15. Mackey, K, Ayers, CK, Kondo, KK, Saha, S, Advani, SM, Young, S, et al. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: a systematic review. Ann Intern Med. (2021) 174:362–73. doi: 10.7326/m20-6306
16. Rozenfeld, Y, Beam, J, Maier, H, Haggerson, W, Boudreau, K, Carlson, J, et al. A model of disparities: risk factors associated with COVID-19 infection. Int J Equity Health. (2020) 19:126. doi: 10.1186/s12939-020-01242-z
17. Lieberman-Cribbin, W, Tuminello, S, Flores, RM, and Taioli, E. Disparities in COVID-19 testing and positivity in new York City. Am J Prev Med. (2020) 59:326–32. doi: 10.1016/j.amepre.2020.06.005
18. Reitsma, MB, Goldhaber-Fiebert, JD, and Salomon, JA. Quantifying and benchmarking disparities in COVID-19 vaccination rates by race and ethnicity. JAMA Netw Open. (2021) 4:e2130343. doi: 10.1001/jamanetworkopen.2021.30343
19. Boehmer, TK, Koumans, EH, Skillen, EL, Kappelman, MD, Carton, TW, Patel, A, et al. Racial and ethnic disparities in outpatient treatment of COVID-19 - United States, January-July 2022. MMWR Morb Mortal Wkly Rep. (2022) 71:1359–65. http://dx.doi.org/10.15585/mmwr.mm7143a2.
20. Ladds, E, Rushforth, A, Wieringa, S, Taylor, S, Rayner, C, Husain, L, et al. Persistent symptoms after COVID-19: qualitative study of 114 "long COVID" patients and draft quality principles for services. BMC Health Serv Res. (2020) 20:1144. doi: 10.1186/s12913-020-06001-y
21. Maclean, A, Hunt, K, Brown, A, Evered, JA, Dowrick, A, Fokkens, A, et al. Negotiation of collective and individual candidacy for long COVID healthcare in the early phases of the COVID-19 pandemic: validated, diverted and rejected candidacy. SSM Qual Res Health. (2023) 3:100207. doi: 10.1016/j.ssmqr.2022.100207
22. Bergmans, RS, Chambers-Peeple, K, Yu, C, Xiao, LZ, Wegryn-Jones, R, Martin, A, et al. I'm still here, I'm alive and breathing': the experience of Black Americans with long COVID. J Clin Nurs. (2023) 33:162–77. doi: 10.1111/jocn.16733
23. Bergmans, RS, Chambers-Peeple, K, Aboul-Hassan, D, Dell’Imperio, S, Martin, A, Wegryn-Jones, R, et al. Opportunities to improve long COVID care: implications from semi-structured interviews with Black patients. Patient. (2022) 15:715–28. doi: 10.1007/s40271-022-00594-8
24. Baz, SA, Fang, C, Carpentieri, JD, and Sheard, L. I don't know what to do or where to go'. Experiences of accessing healthcare support from the perspectives of people living with long COVID and healthcare professionals: a qualitative study in Bradford, UK. Health Expect. (2023) 26:542–54. doi: 10.1111/hex.13687
25. Hsieh, HF, and Shannon, SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15:1277–88. doi: 10.1177/1049732305276687
26. Hirschtick, JL, Titus, AR, Slocum, E, Power, LE, Hirschtick, RE, Elliot, MR, et al. Population-based estimates of post-acute sequelae of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (PASC) prevalence and characteristics. Clin Infect Dis. (2021) 73:2055–64. doi: 10.1093/cid/ciab408
27. Cutler, DM, and Summers, LH. The COVID-19 pandemic and the $16 trillion virus. JAMA. (2020) 324:1495–6. doi: 10.1001/jama.2020.19759
28. Tsampasian, V, Elghazaly, H, Chattopadhyay, R, Debski, M, Naing, TKP, Garg, P, et al. Risk factors associated with post-COVID-19 condition: a systematic review and meta-analysis. JAMA Intern Med. (2023) 183:566–80. doi: 10.1001/jamainternmed.2023.0750
29. Antonelli, M, Penfold, RS, Merino, J, Sudre, CH, Molteni, E, Berry, S, et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID symptom study app: a prospective, community-based, nested, case-control study. Lancet Infect Dis. (2022) 22:43–55. doi: 10.1016/S1473-3099(21)00460-6
30. Xie, Y, Choi, T, and Al-Aly, Z. Association of treatment with nirmatrelvir and the risk of post-COVID-19 condition. JAMA Intern Med. (2023) 183:554–64. doi: 10.1001/jamainternmed.2023.0743
31. Gaffney, A, Himmelstein, DU, McCormick, D, and Woolhandler, S. Disparities in COVID-19 vaccine booster uptake in the USA: December 2021-February 2022. J Gen Intern Med. (2022) 37:2918–21. doi: 10.1007/s11606-022-07648-5
32. Lu, PJ, Srivastav, A, Vashist, K, Black, CL, Kriss, JL, Hung, MC, et al. COVID-19 booster dose vaccination coverage and factors associated with booster vaccination among adults, United States, march 2022. Emerg Infect Dis. (2023) 29:133–40. doi: 10.3201/eid2901.221151
33. Centers for Disease Control and Prevention . (2023). COVID data tracker. Available at: https://covid.cdc.gov/covid-data-tracker/#vaccination-demographics-trends (Accessed July 20, 2023).
34. Cooper, E, Lound, A, Atchison, CJ, Whitaker, M, Eccles, C, Cooke, GS, et al. Awareness and perceptions of long COVID among people in the REACT programme: early insights from a pilot interview study. PLoS One. (2023) 18:e0280943. doi: 10.1371/journal.pone.0280943
35. Au, L, Capotescu, C, Eyal, G, and Finestone, G. Long covid and medical gaslighting: dismissal, delayed diagnosis, and deferred treatment. SSM Qual Res Health. (2022) 2:100167. doi: 10.1016/j.ssmqr.2022.100167
36. Stephenson, J . Report on long COVID urges actions to address needs of patients, caregivers. JAMA Health Forum. (2022) 3:e225254. doi: 10.1001/jamahealthforum.2022.5254
37. Department of Health and Human Services, Office of the Assistant Secretary for Health . (2022). Health+ long COVID human-centered design report. Available at: https://www.hhs.gov/sites/default/files/healthplus-long-covid-report.pdf
38. Landhuis, EW . How primary care physicians can recognize and treat long COVID. JAMA. (2023) 329:1727–9. doi: 10.1001/jama.2023.6604
Keywords: COVID-19, long COVID, health disparities, awareness, national survey
Citation: Fisher KA, Mazor KM, Epstein MM, Goldthwait L, Abu Ghazaleh H, Zhou Y, Crawford S, Marathe J and Linas BP (2024) Long COVID awareness and receipt of medical care: a survey among populations at risk for disparities. Front. Public Health. 12:1360341. doi: 10.3389/fpubh.2024.1360341
Edited by:
César Fernández-de-las-Peñas, Rey Juan Carlos University, SpainReviewed by:
Randal A. Serafini, Boston University, United StatesJuan Sebastian Izquierdo-Condoy, University of the Americas, Ecuador
Kokouvi Kassegne, Shanghai Jiao Tong University, China
Copyright © 2024 Fisher, Mazor, Epstein, Goldthwait, Abu Ghazaleh, Zhou, Crawford, Marathe and Linas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kimberly A. Fisher, Kimberly.Fisher2@umassmed.edu
 Kimberly A. Fisher
Kimberly A. Fisher Kathleen M. Mazor1
Kathleen M. Mazor1 Mara M. Epstein
Mara M. Epstein Lydia Goldthwait
Lydia Goldthwait