- 1Department of Statistics, Injibara University, Injibara, Ethiopia
- 2Department of Statistics, Bahir Dar University, Bahir Dar, Ethiopia
Objective: The purpose of this study was to evaluate the spatio-temporal pattern of Ethiopia’s childhood diarrheal disease and identify its contributing factors.
Methods: We conducted analyses on secondary data from four Ethiopian Demographic and Health Surveys conducted between 2000 and 2016. Moran’s I was used to determine spatial dependence and spatial models were used to evaluate variables associated with diarrhea in under-five children at the zonal level.
Results: Childhood diarrhea showed spatial clustering in Ethiopia (Moran’s I; p < 0.05). The spatial regression model revealed significant factors at the zonal level: children born at home (
Conclusion: The prevalence of diarrhea among under-five children varied over time by zone, with the Assosa, Hundene, and Dire Diwa zones having the highest rates. Home births and low birth weight contributed to the prevalence of childhood diarrhea. In high-risk zones of Ethiopia, reducing childhood diarrhea requires integrated child health interventions and raising awareness about the potential hazards associated with unimproved water sources.
Introduction
Diarrhea is the second leading cause of death and morbidity in children under five years worldwide and is primarily caused by contaminated food and water sources. The World Health Organization (WHO) defines diarrheal disease as the passage of three or more loose or liquid stools per day, or more frequent passage than is normal for the individual (1). In countries with lower incomes, it is more common and widespread due to its infectious nature (1, 2). In the world, more than 1.7 billion cases of childhood diarrheal disease occur every year (1). As the WHO reported in 2019, diarrheal disease is the second leading cause of death in children under five years, next to pneumonia, and was responsible for the deaths of 370,000 children (3). According to United Nations International Children’s Emergency Fund (UNICEF) report in 2021, 9.1% of all under-five children deaths in the world are caused by diarrhea diseases (2). From a global perspective, the spatial pattern of diarrhea-related mortality was clustered worldwide during the study period from 2000 to 2017. Furthermore, the findings indicated that the world’s highest incidence of diarrhea-related mortality was found in Asian and African nations (4).
In Africa, diarrheal diseases are the leading cause of death in children under five, accounting for an estimated 30 million cases of severe diarrhea and 330,000 deaths in 2015 (5). The highest mortality rate is in sub-Saharan Africa, where rates typically range between 50 and 150 per 100,000 population (6) depending on various factors such as mother’s age, wealth index, mother’s education, mother’s occupation, the age of the children, time of initiation of breastfeeding, and time to fetch water were significantly associated with diarrhea (7).
In Ethiopia, diarrhea was the major contributor to the deaths of children under the age of five years. The Ethiopian Demography and Health Surveys (EDHS) in 2000, 2005, 2011, and 2016 indicate that childhood diarrheal disease experienced by 24.72, 18.04, 16.1, and 11.79%, respectively, of children at some time in the two weeks before the survey (8–11).
In Ethiopia, childhood diarrhea remains public health problem and had a spatial variation across the regions. Although there was a decline in diarrhea rates nationally from 2000 to 2011, morbidity remained high in regions such as Gambella, Benshangul-Gumuz, and Somali (12). Childhood diarrheal disease is more common among children under five years of age, particularly in the Southern Nation and Nationality People (SNNP), Gambella, Oromia, and Benshangul-Gumuz regions (13). In a research setting, analyzing disease trends over time and space provides context that can be associated with potential risk factors. Scanning statistics have been extensively used in studying the spatial, temporal, and spatiotemporal variation of infectious diseases such as diarrhea (14).
Morbidity due to diarrhea has been found to be influenced by socio-demographic factors such as sex, age, family size, place of residence, wealth index, parental education, mothers’ age, and child’s age (7, 15–18), child-caring factors include immunization status, birth place, birth order, the child’s birth weight, and the child’s nutritional status (17, 19, 20). Housing and sanitation factors include drinking water sources, waste disposal, and toilet facilities (15, 21, 22), and meteorological factors include precipitation and temperature across the globe, including Ethiopia (23–25).
It is important to explain how diarrheal diseases occur in temporal and spatial variations to enable health professionals at different levels to make informed decisions and improve disease surveillance. Nevertheless, there are not many studies in Ethiopia that examined zonal diversity in diarrhea from a geographical and temporal perspective. Few studies that are now available used a variety of data sources for a spatio-temporal study of the spread of diarrhea, but they were only able to look at local rather than national data. Therefore, the aim of this study was to examine the variability of diarrhea in children in different geographical and temporal zones of Ethiopia. The study adds to the body of information and identifies risk zones to enable the development of effective intervention techniques to reduce pediatric diarrhea in Ethiopia.
Methods
Description of study area and study setting
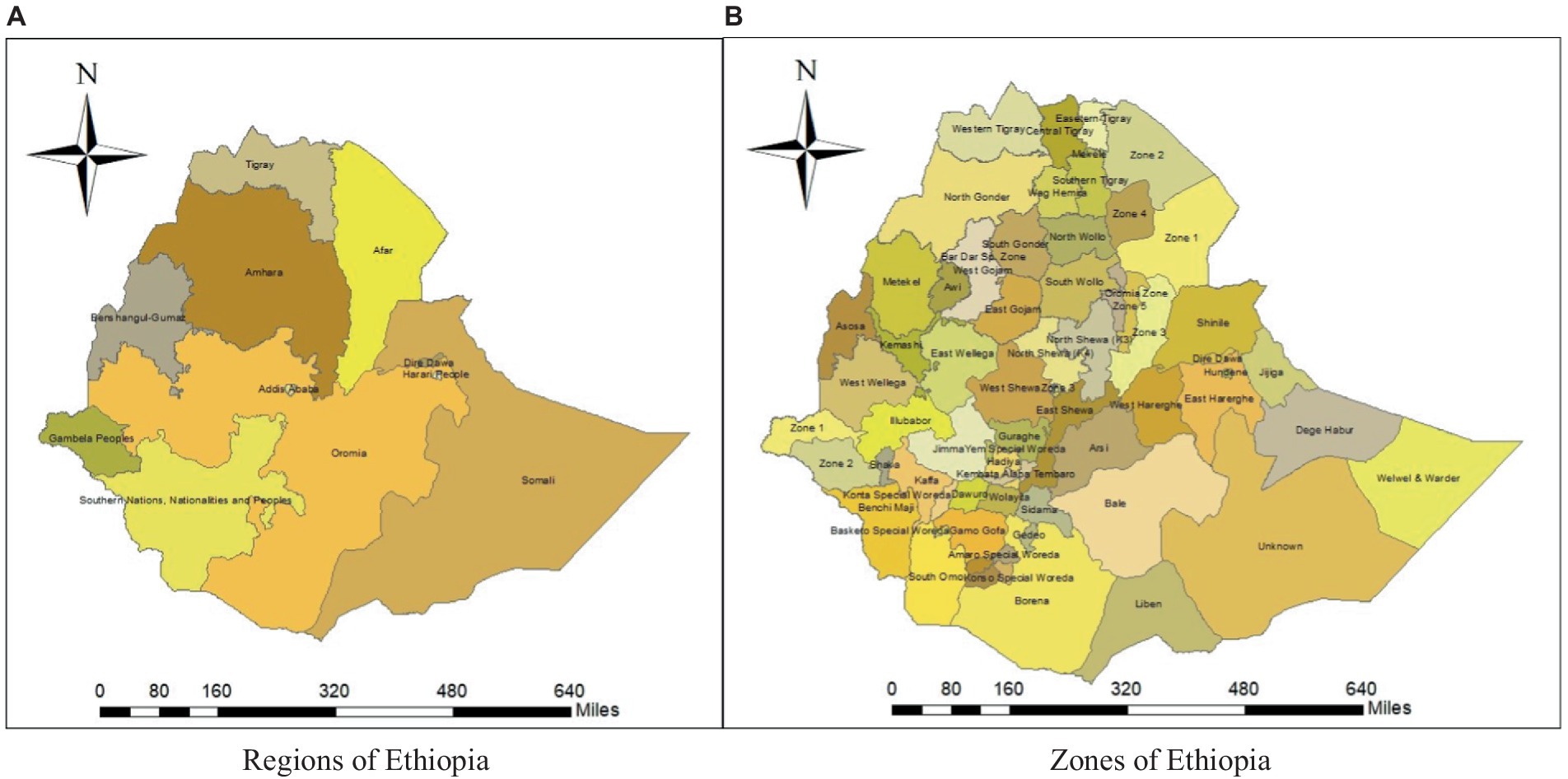
This study was conducted in Ethiopia, which is situated in eastern Africa. It is a landlocked country in the Horn of Africa, located between 3° and 15° north latitude and 33° and 48° east longitude (EDHS, 2000). The country has 11 regional states and two administrative cities, Addis Ababa and Dire Diwa (Figure 1).
Data collection and sampling procedure
The data was obtained from the Ethiopian Demographic and Health Survey (EDHS). The DHS results are available for many nations, particularly those with low incomes. The DHS data is readily accessible and publically available at: https://dhsprogram.com. In order to offer the most accurate data on indicators related to maternal and child health, the EDHS data is generated from a series of nationally representative demographic and health surveys conducted in the country every five years. This study took into account four EDHSs that were completed in 2000 along with those in 2005, 2011, and 2016, allowing for a summary of the results for the entire nation. A stratified two-stage cluster sampling procedure was used to select the nationally representative sample in all the four surveys. In the first stage, clusters or enumeration areas (EAs) were selected with probability proportional to population size. A total of 540, 540, 624 and 645 EAs (clusters) were selected in 2000, 2005, 2011, and 2016, respectively. The second stage involved the stratified sampling of households in each selected cluster. The study was conducted on a sample of 64,449 children: 18,060 from 2016; 17,817 from 2011; 14,500 from 2005; and 14,072 from the 2000 EDHS, respectively.
The dependent variable for the childhood diarrheal status was represented by a random variable with two possible values coded as 1 and 0. The occurrence of diarrhea was classified as “yes” or “no” by asking mothers whether their children had an incidence of diarrhea in the last two weeks before the survey. It needs some clarification, such the number of under-five children with diarrheal disease within two weeks before the survey is undertaken. Therefore, the response variable of the childhood diarrhea occurrence in space (zone) was measured as a count variable.
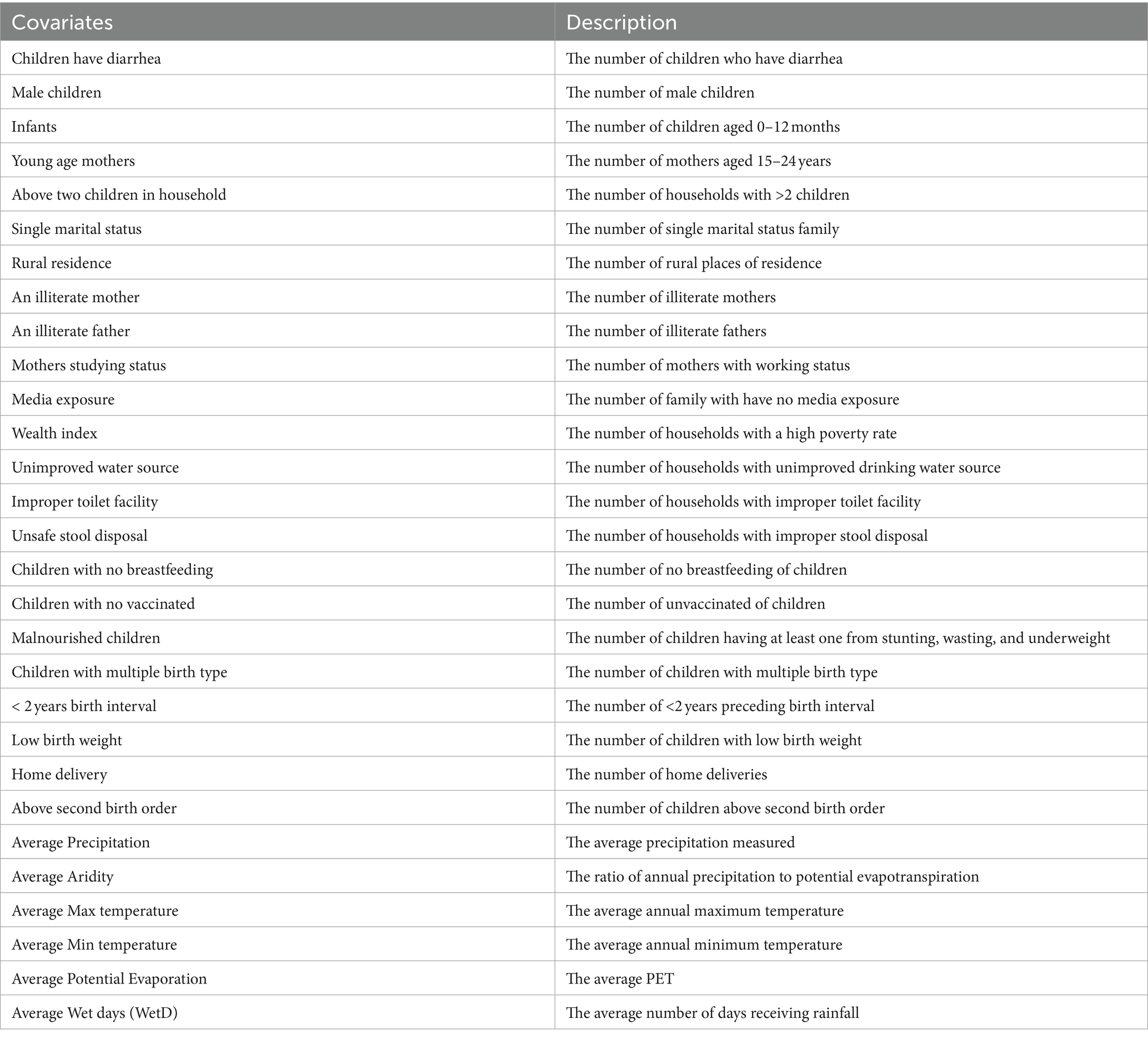
Childhood diarrheal status is expected to be influenced by several factors. Therefore, the predictor variables that were analyzed in this study as possible determinants of diarrhea among under-five children were grouped into socio-economic and socio-demographic factors, child-caring practice, geographical covariate, and housing and sanitation related factors (Table 1).
Data analysis
Global spatial autocorrelation is a measure of the overall clustering of the data, providing a correlation value to summarize the entire study area using the Moran I statistic. The Moran’s I values, which is found in the interval of , indicate the disease dispersed, whereas Moran’s I values found in indicate disease clustered and disease distributed randomly if Moran’s I value is zero. Moran’s I statistic of spatial autocorrelation has the form described in equation given below (26).
In this study, the spatial interpolation technique was used to predict unsampled from sampled measurements and ordinary Kriging spatial interpolation method was used for predictions and to generate smooth surfaces of the variables of interest (27).
The Scan statistics are used to detect and evaluate clusters of cases in either a purely temporal, purely spatial or space–time setting. This is done by incrementally scanning a window across time and/or space, noting the number of observed and expected observations within the window at each location (28). It is preferred among software programs capable of space–time disease surveillance analysis, also found to be the best-equipped package for use in surveillance system (29). In this study, the number of diarrheal cases, the number of under-five children population, and the coordinates of the study areas were used as input variables for the discrete Poisson model, assuming that the cases in each district have a Poisson distribution with a known population of under-five children that are at risk for diarrhea.
To detect and analyze the spatial clusters of childhood diarrhea, a purely spatial analysis was carried out using spatial scan statistics without taking time into account. This spatial statistical analysis method imposes a circular window on the map. The recommended choice is to express the upper limit as a percentage of the population at risk and use 50% as the value (28). Therefore, in this study, the maximum spatial cluster size of the population at risk is set at 50% as an upper limit, which allowed both small and large clusters to be detected and clusters that contained more than the maximum limit to be ignored.
Spatial regression models allow us to account for dependencies between observations, which often occur when collecting observations from points or regions in space (30, 31). Let denote column vector of observations on the response variable, denote matrix of observations on the independent variables, and is vector of the error term.
Let be a spatial weight matrix with a dimension of , denote the interaction effects among the independent variables with the spatial components, and denote the interaction effects among the error terms of different observations with the spatial components, and represent the spatial lag vector. As regards the parameters of the model, is the spatial dependence parameter, is the parameter of lagged independent variables, λ is the spatial correlation effect of errors (spatial autocorrelation).
The number of childhood diarrheal cases in zone , , were assumed to follow a Poisson distribution with mean ,
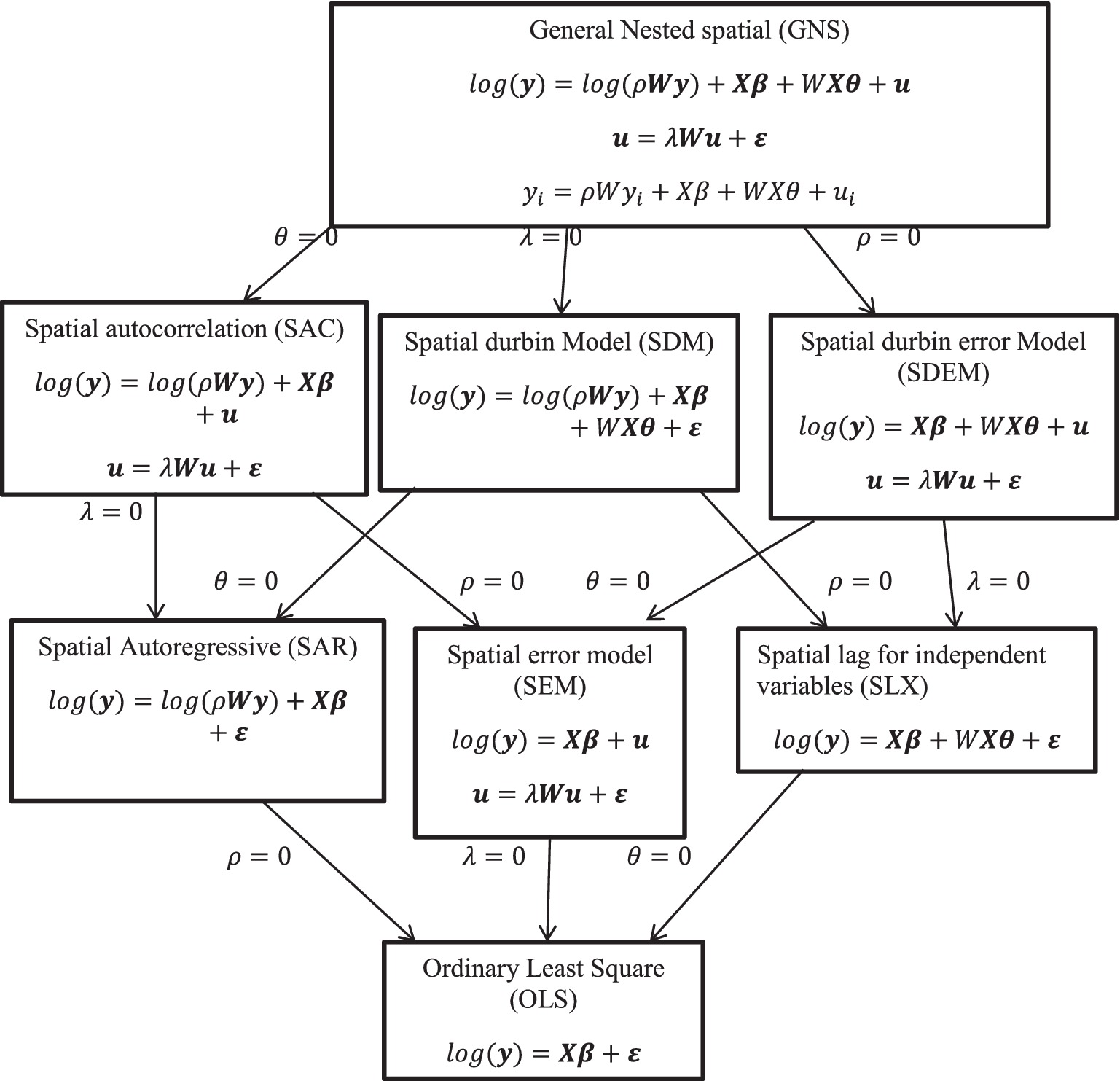
Different spatial models were used with the addition of different covariates to determine the best and appropriate model for this study (Figure 2).
Results
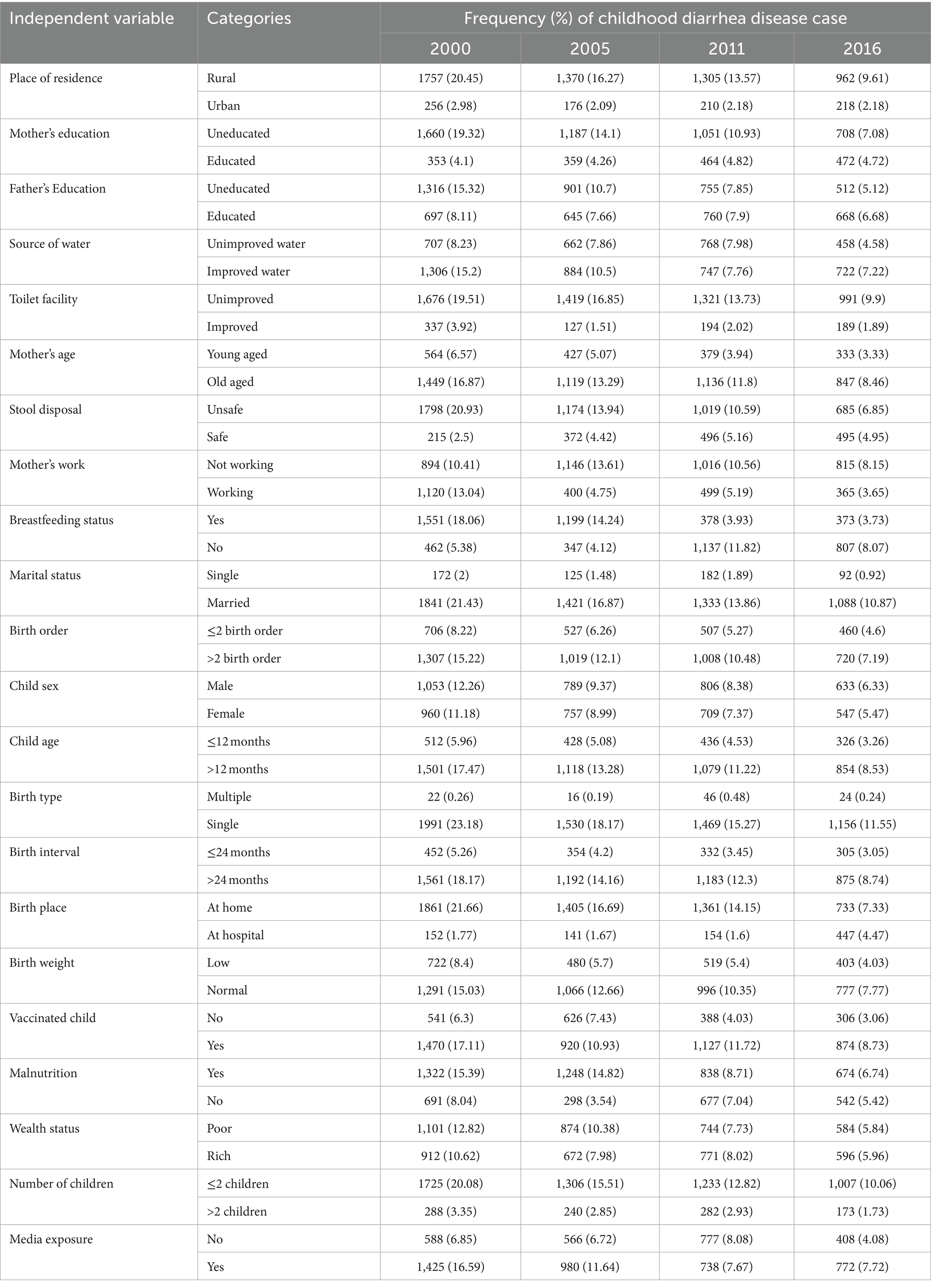
The prevalence of diarrhea among children under five years in Ethiopia was 24.72, 18.04, 16.10, and 11.79% in 2000, 2005, 2011, and 2016, respectively. Its was higher in rural areas (20.45, 16.27, 13.57 and 9.61%) over the four EDHS in 2000, 2005, 2011, and 2016, respectively, compared to urban areas. In a similar way, the prevalence of diarrheal case was higher in boys (12.26% in 2000, 9.37% in 2005, 8.38% in 2011 and 6.33% in 2016) compared to girl under-five children over those four-survey time periods. From this result, the prevalence of the childhood diarrhea disease decreased over time in the four EDHS phases (Table 2).
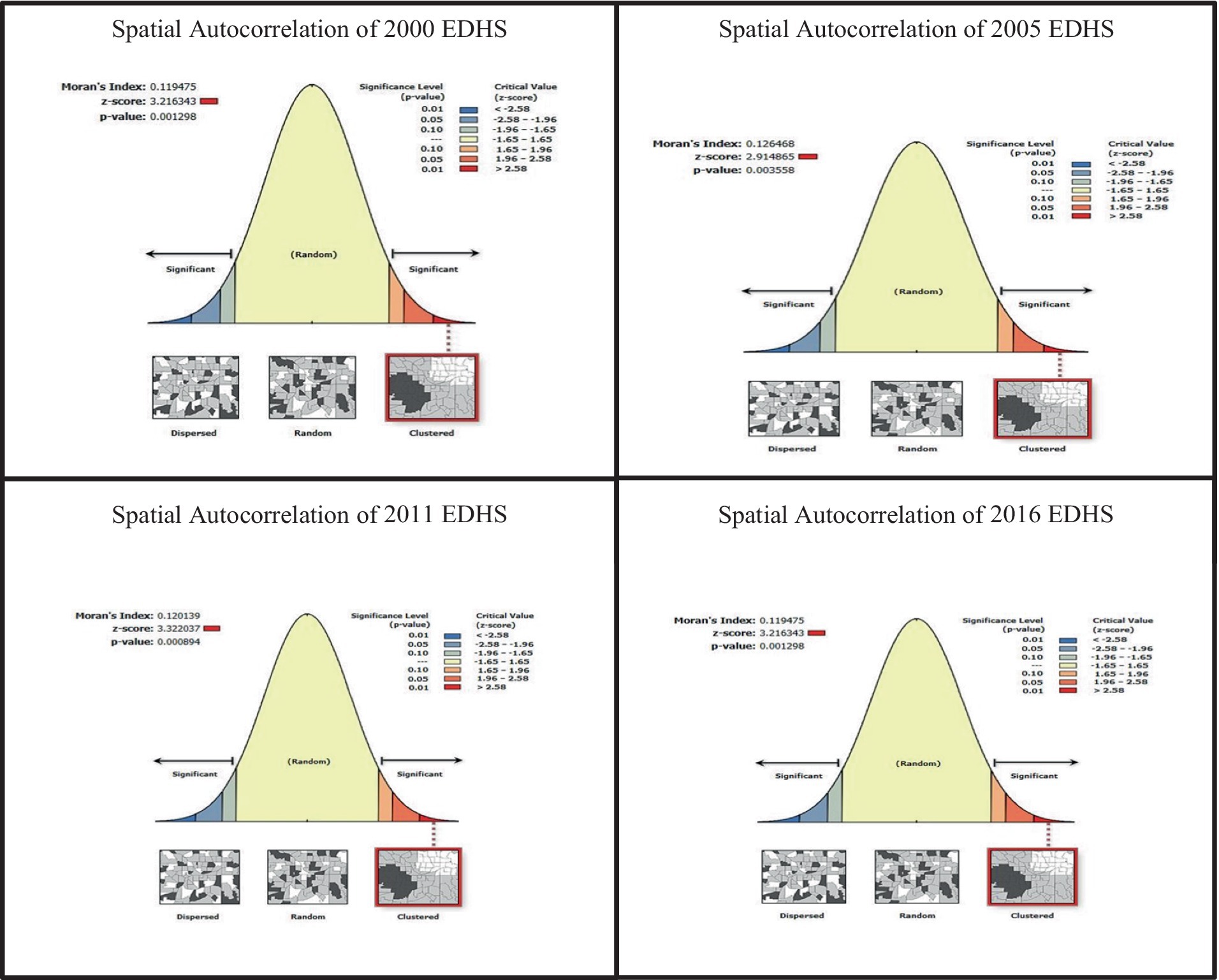
All four Moran’s I p-values of childhood diarrhea were less than 0.05 for all the EDHS data; it implies that there exists a significant spatial autocorrelation in risk of childhood diarrhea disease between zones of the country (Figure 3). All Moran’s I index values were positive and indicate that the spatial distribution of childhood diarrhea disease was significantly clustered between zones of the country .
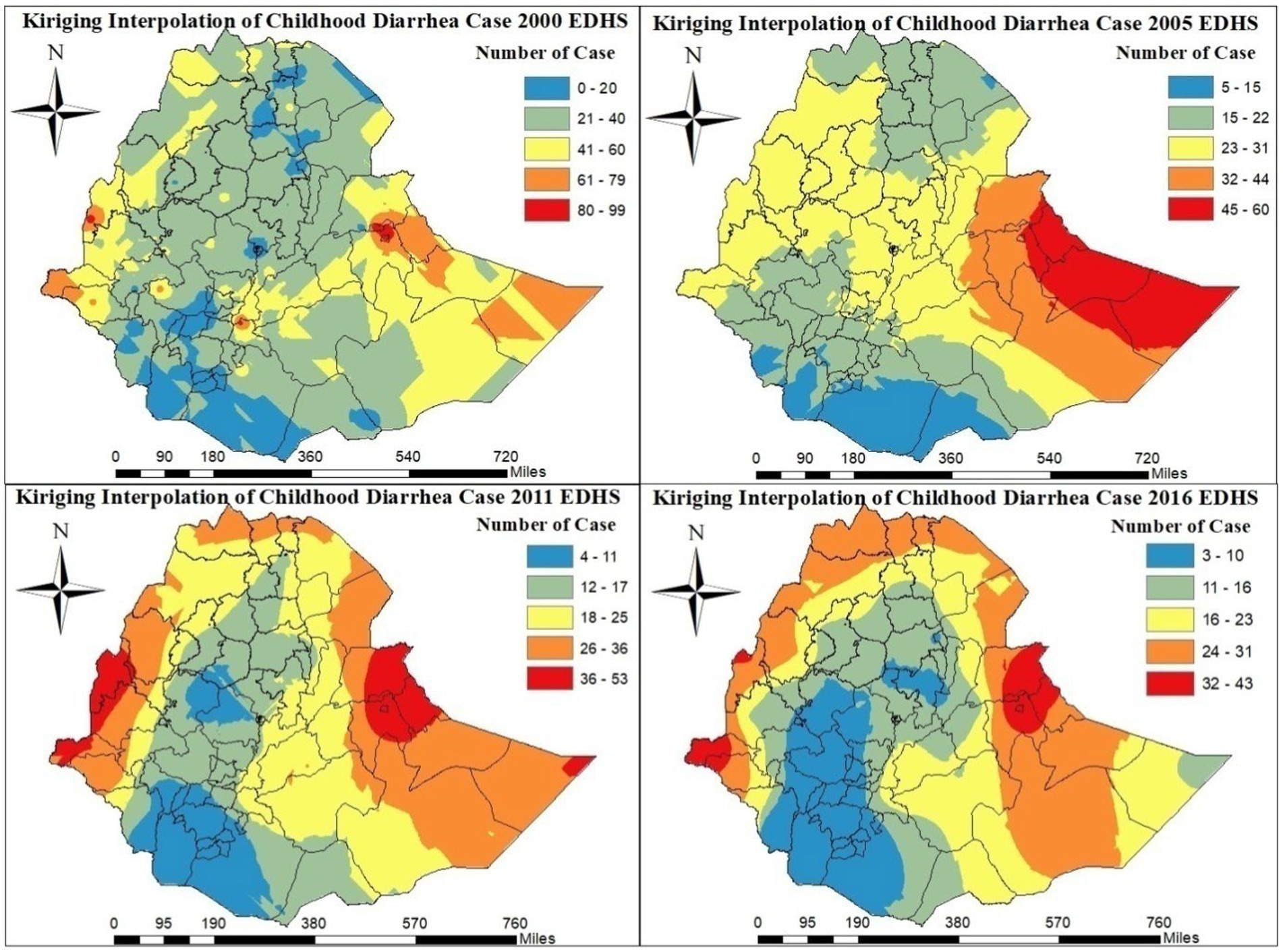
Kriging interpolation shows that the western and eastern areas of the country were heavily affected by childhood diarrhea in the 2000–2016 EDHS. In addition, in the 2011 and 2016 EDHSs, the northern part zones of the country were heavily affected by childhood diarrheal disease (Figure 4). Conversely, as shown in Figure 4, according to the EDHS 2000–2016, there are few cases of childhood diarrhea in most zones in the central and southern parts of the country.
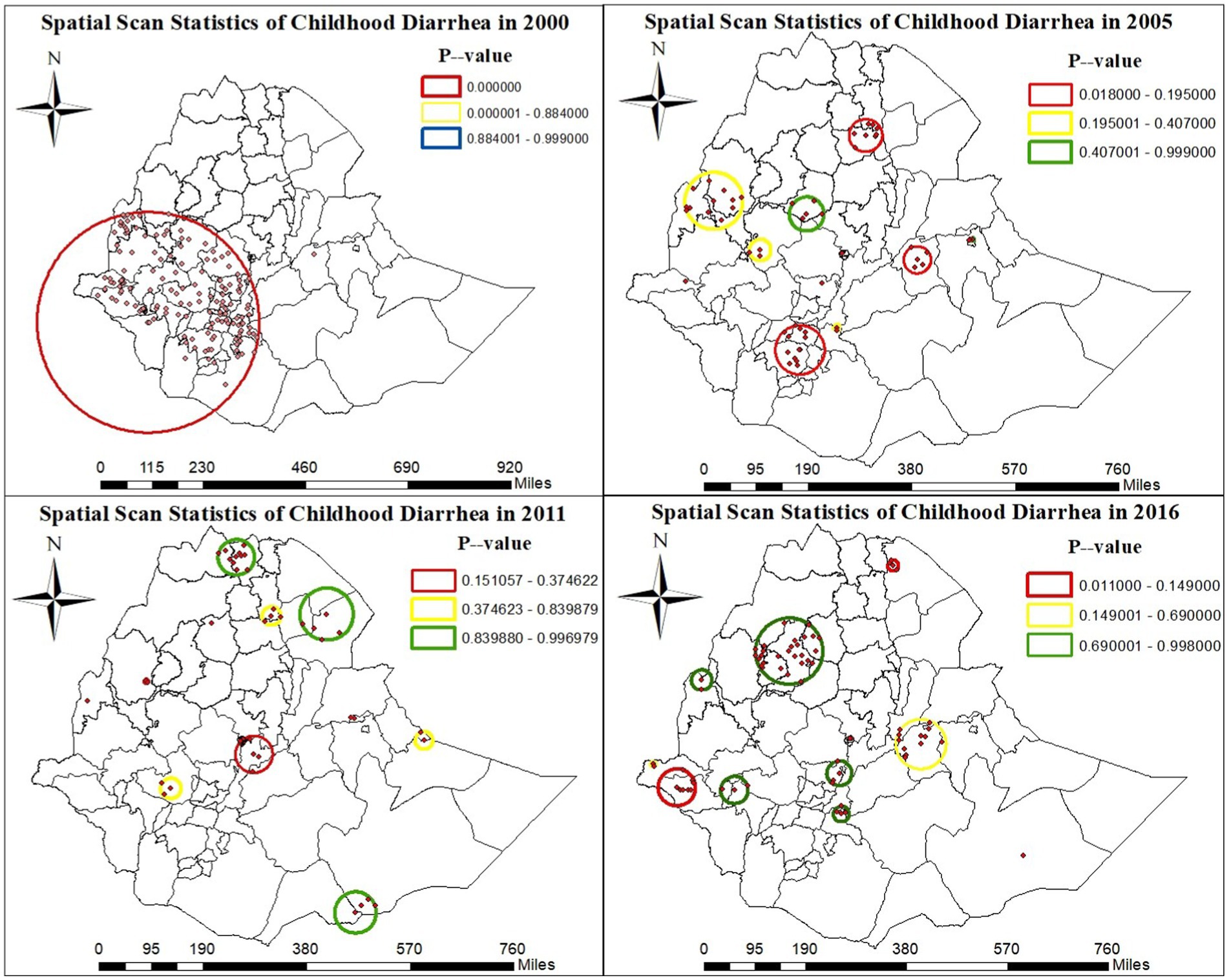
A total of 186 significant clusters (164 in 2000 EDHS, 18 in 2005 EDHS, and 4 in 2016 EDHS) were identified. Of the overall significant clusters, 173 clusters were primary clusters: 164 in the 2000 EDHS survey and the remaining clusters were in the 2005 and 2016 EDHS. Thirteen clusters were secondary clusters in the 2005 EDHS survey. The primary and secondary spatial cluster windows in the 2000 EDHS were found in the west and south-west zones of the country. In the 2005 EDHS, these windows were found in West Hararge, around the Wolayita, Gedeo, Dawro, Sidama, and GamoGofa zones, and in the 2016 EDHS, they were found in Afar Zone 2 (Figure 5).
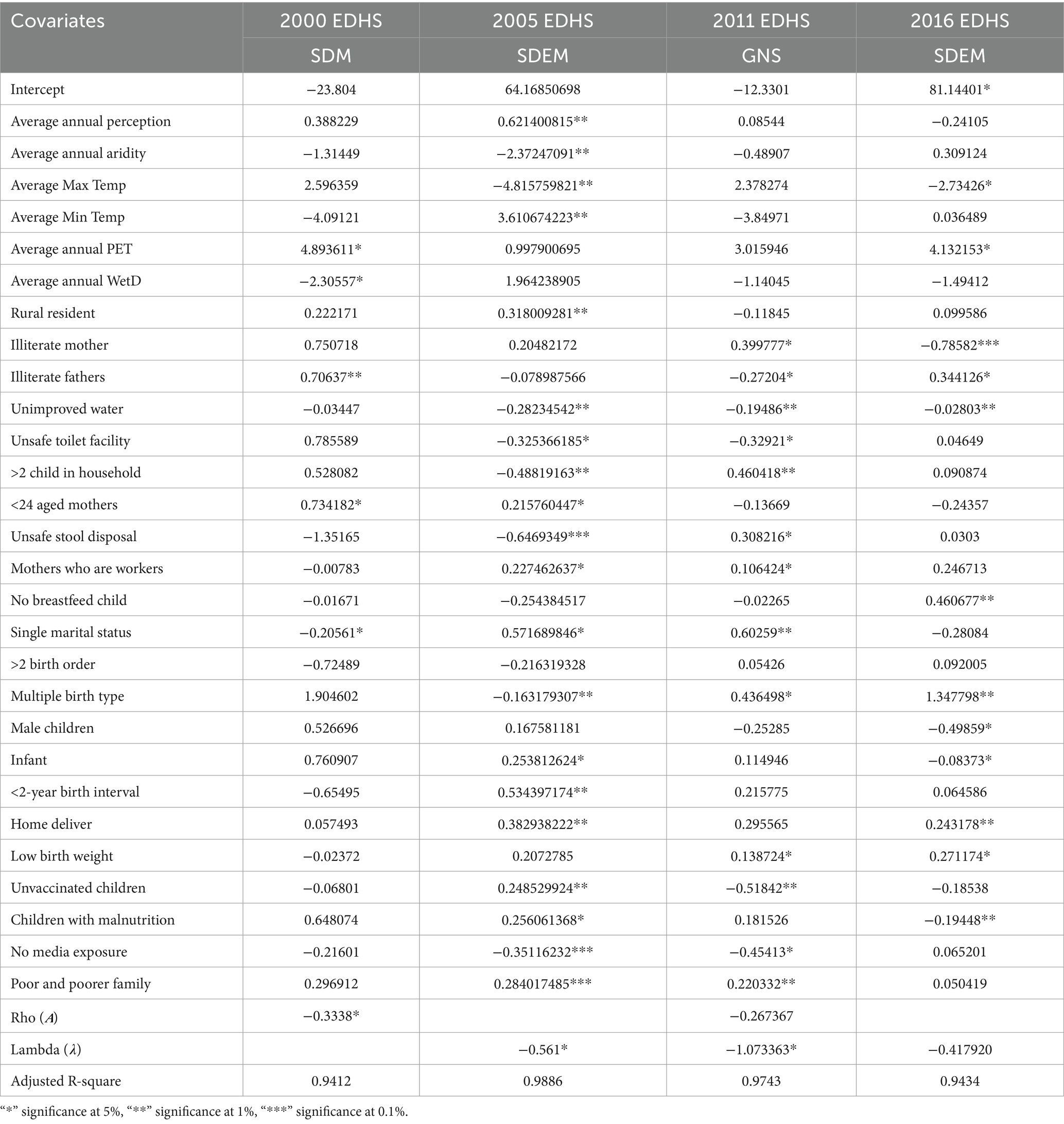
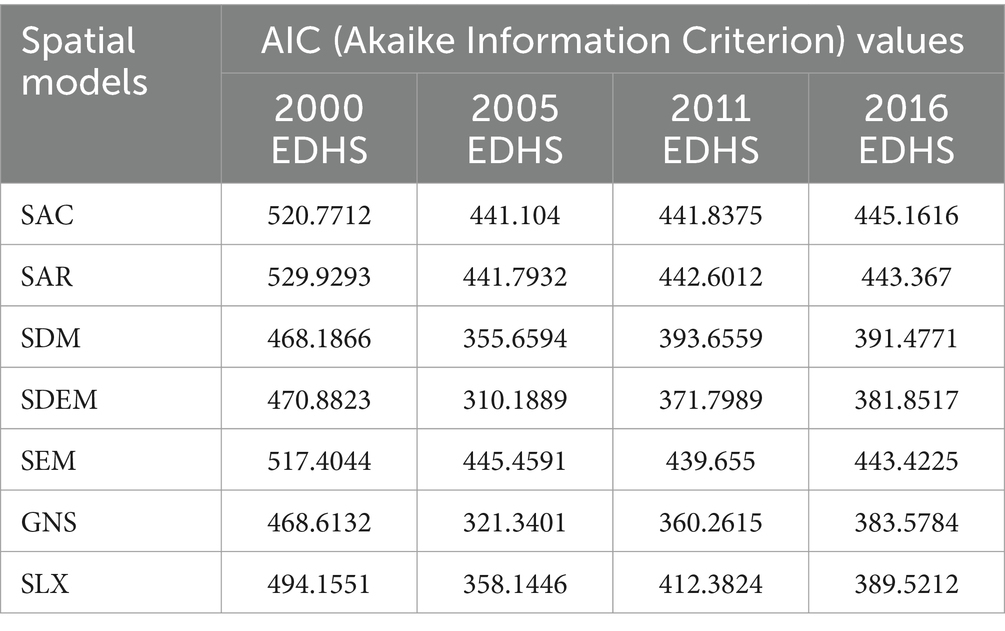
The model with the smallest Akaike Information Criterion (AIC) value was the best model. The spatial Durbin model was the best model for the 2000 EDHS data and the general nested spatial model was the best model for 2011 EDHS data (Table 3). In the same table, the spatial Durbin error model was the best for the 2005 and 2016 EDHS data (AIC = 310.1889 and AIC = 381.8517) respectively (Table 4).
The adjusted R-squared values in the four EDHS phases showed how the prevalence of diarrhea in children was explained by the set of explanatory variables. All adjusted R-square values of the four EDHS data were above 90%, indicating that more than 90% of the covariates at different levels were good at explaining the cases of diarrhea in under-five children (Table 3).
From the results of Table 3, the geographical covariates such as maximum temperature, potential evaporation, and annual perception are significant factors for childhood diarrheal cases. In the 2005 EDHS data, zones with a higher average precipitation are positively associated with a higher mean number of diarrheal cases among children under-five ( ).
Some socio-demographic factors have a significant influence on the number of cases of diarrhea in children under-five (Table 3). In the 2005 EDHS data, zones with a higher number of children from rural zones are positively associated with a higher average number of diarrheal cases among children under five years ( ).
As shown in Table 3, some socio-economic factors such as illiterate mothers, illiterate fathers and working mothers are important contributing factors for diarrhea in children under-five. The zones with a higher number of illiterate mothers are positively associated with a higher mean number of diarrheal cases in children under-five in the 2011 EDHS data and negatively in the 2016 EDHS data ( ). In the 2011 EDHS data, zones with a higher number of illiterate fathers are negatively associated with a higher mean number of diarrheal cases among children under-five ( ).
In child-caring practice, some factors are significant for the number of childhood diarrheal cases as shown in Table 3. In the 2016 EDHS data, the zones with a higher number of low-birth-weight children are positively associated with a higher mean number of childhoods diarrheal cases ). The zones with a higher number of children born at home are negatively associated in the 2005 EDHS data and positively associated in the 2016 EDHS data with a higher mean number of childhoods diarrheal cases ).
Unimproved water supply, unimproved toilet facilities, and unsafe stool disposal are factors listed in Table 3 that are also significant in sanitation and hygiene practices for diarrheal disease in children under five years of age. Zones with a higher number of households with unimproved water supply are negatively associated with a higher mean number of diarrheal cases in under-five children in the 2011 and 2016 EDHS data ( ).
In the 2005 and 2011 EDHS data ( ), the increase in the mean number of childhood diarrheal cases is negatively associated with the increasing number of households that have unimproved toilet facilities. The increasing the number of households with unsafe stool disposal is negatively associated in the 2005 EDHS and positively associated in the 2011 EDHS with the increasing mean incidence of childhood diarrhea .
The spatial coefficient rho ( ) was statistically significant ( ) in the 2000 EDHS data. This indicates that childhood diarrhea was significantly influenced by the adjacent zones. In the 2005–2011 EDHS data, areas with a higher number of unobserved variables ) are negatively associated with a higher mean number of diarrheal cases in children under the age of five ( ) (Table 3).
Discussion
Nationally, the number of children under-five exposed to diarrheal disease fell from 2,360 in 2000 to 1,180 in 2016. Although the general trend of reducing diarrheal disease in children under-five in Ethiopia over time is good, local trends show obvious heterogeneity. This study finding is similar with the study conducted in Ethiopia and India (12, 17, 32, 33) while the finding is different from the study conducted in Ghana (34). This could be because each county has different knowledge about the causes of diarrhea, the study environment is different, and there are differences in the study area.
The results of this study showed that childhood diarrheal diseases have a statistically significant and positive spatial autocorrelation in all zones of the country during the EDHS period 2000–2016. This study result is similar to the results of the study conducted in Ethiopia, India, Brazil, Rwanda, Nigeria, Ghana, and Tanzania (12, 13, 15, 16, 34–42) while this finding is different from the study conducted in Nepal (43). The possible reason for this difference could be the sample size, temperature, and lack of access to drinking water, especially in remote areas.
Furthermore, the results of this study showed that the Dire Diwa, Hundene, Jijiga, Dege Habour, and Welwel and Warder zones were highly affected by childhood diarrhea. This finding is also similar to the findings of the study conducted in Ethiopia (12) but different from the results of the study conducted in Ethiopia (13). This difference was probably due to Dire Diwa, Harari, and Somali regions lying in the low land part of the country. Conversely, zones in Addis Ababa, Jimma, Wolayita, Gamo Gofa, North Shewa, South Gondar, West Gojjam, and South Wollo zones areas with a low risk of childhood diarrhea, which is different from the results of the study conducted in Ethiopia (12, 13). The risks were lower in middle part of the country, which might be due to urbanization, improved drinking water sources, and high land areas of the country.
The scan statistics of spatial cluster showed that children inside the windows located in Gambela zone 1 and zone 2, Kamashi, Ilubabor, West Wellega, Kamashi, Shaka, Benchi Maji, Jimma, Hadiya, Wolayita, Assosa, West Harerge, Wolayita, Gedeo, Dawro, Sidama, Gamo Gofa, and Afar Zone 2 zones are more than once at the risk of diarrhea than children outside windows, according to 2000–2016 EDHS data. This study finding is similar with study findings that were reported from Ethiopia (12, 13).
In our study, some socio-demographic and socio-economic factors are significant for the childhood diarrhea. Based on the results of the spatial model, the illiteracy of both father and mother are directly proportional to the increase in the mean number of diarrhea of childhood diarrheal cases in children under the age of five. This result is in line with the previous studies conducted in Sub-Saharan Africa and Ethiopia (7, 17, 44) while this result is different from the previous studies conducted in East Africa and Nigeria (13, 15, 21, 45). This could be because the sample data taken from administrative zones of the country is different in different years and also due to the difference in study settings.
The study finding revealed that in spatial models, increasing number of illiterate fathers leads to an increase in the mean number of childhood diarrheal cases. This result is different from the result of the study conducted in India (32). This could be because the illiterate father does not have enough knowledge about the cause of diarrheal disease and its prevention.
In this study, some child-caring practices are significant for childhood diarrheal disease. This study results, based on a spatial model, showed that the increasing number of children who are twins and are born with low birth weight lead to an increase in the mean number of diarrheal cases among children under five years of age. Our study result is in line with the previous study results that were reported from Ethiopia and India (17, 18, 32). The possible reason might be due to mothers not caring for twin children properly and could be due to the fact that children with low birth weight have infant health problems or maternal health problems. Furthermore, children whose birth was at home increases the mean number of diarrheal cases, because of there is no safety at delivery time and initiation of breastfeeding and mothers did not get any advice from a nurse or a doctor about child care practices when they had birth at home. This finding agrees with the study conducted in Ethiopia (46).
The present study finding confirmed that children, who did not get breastfed, had higher mean number of diarrheal cases. The possible reason might be children who did not get breastfed miss out on the protective antibodies and immune factors present in breast milk. Lack of breastfeeding for children compromises their immune system, making them more vulnerable to pathogen invasion, which can lead to an increased risk of developing the diarrheal disease. Moreover, breast milk plays a crucial role in providing natural defenses against pathogens, promoting a healthier immune response, and reducing the likelihood of diarrhea in infants. This finding is similar to study results reported from Germany and Saudi Arabia (47, 48).
Limitations of the study
Since this study used EDHS data from 2000 to 2016, the results could not accurately reflect the current state of affairs in Ethiopia. Additionally, other significant variables like respondents’ cultural, behavioral, and other health-related aspects were not included in the data set. We looked at a lot of potential causes of diarrhea in children in our study, but we might have missed other unrecognized or unidentified diverse contributors in the spatial dimensions.
Conclusion
Although diarrhea has occasionally occurred in children under five years of age, its incidence is still high. Despite a falling pattern of childhood diarrhea at the national level, the prevalence remained high in the Assosa, Hundene, and Dire Diwa zones and displayed spatial and temporal variations throughout the country’s zones. Moreover, the eastern regions of the nation, including Jijiga, Dege Habour, Afar zones 1, Afar zone 3, Afar zone 4 and Hundene were hotspot areas of child diarrheal cases. Increases in the number of children due to multiple births, home births, children living in rural areas, low-birth-weight infants, unvaccinated children, households with unsafe stool disposal practices, malnourished children, both fathers and mother being illiterate were associated with an increase in the mean number of diarrheal cases among under-five children. Furthermore, use of unimproved water, unimproved toilet facilities, and unsafe stool disposal had significant effect for the high prevalence of diarrheal disease in under-five children. Thus, this study suggests that in order to prevent and control diarrheal, attention should be given for the above mentioned risk factors and appropriate intervention mechanisms should be applied. Moreover, the results of this study emphasizes public health education, vaccination program, provision of safe drinking water, and constant surveillance to find out the etiological agents causing diarrhea.
Data availability statement
The data sets used for this study are available at the DHS program, in the DHS repository (https://www.dhsprogram.com/data/dataset/Ethiopia_Standard-DHS_2016.cfm?flag=0) for all four surveys.
Ethics statement
Ethical approval for this research was obtained from ethical approval committee of postgraduate and research office, the College of Science, Bahir Dar University, Ethiopia. In the time of data collection there was no verbal consent from study participants because of the data was taken from secondary source from Ethiopian Demographic Health Survey data (EDHS from 2000 to 2016).
Author contributions
MT: Conceptualization, Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing. MZ: Conceptualization, Formal analysis, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. DB: Formal analysis, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to express our sincere appreciation and gratitude to the Ethical Approval Committee of the Postgraduate and Research Office, College of Science, Bahir Dar University, for their valuable support and guidance throughout the research process. We would also like to acknowledge and extend our gratitude to the Ethiopian Demographic Health Survey (EDHS) for providing us with the valuable data used in this research. We are grateful to the EDHS for their commitment to collecting and sharing high-quality data, which has greatly contributed to the validity and reliability of our findings.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
EDHS, Ethiopian Demographic and Health Survey; WHO, World Health Organization; UNICEF, United Nations International Children’s Emergency Fund; SNNP, Southern Nation and Nationality People; GNS, General nested spatial; SAC, Spatial autocorrelation model; SDM, Spatial Durbin model; SDEM, Spatial Durbin error model; SAR, Spatial autoregressive; SEM, Spatial error model; SLX, Spatial lag model for independent variables; OLS, Ordinal least square; AIC, Akaike information criterion.
References
4. Almasi, A, Zangeneh, A, Ziapour, A, Saeidi, S, Teimouri, R, Ahmadi, T, et al. Investigating global spatial patterns of diarrhea-related mortality in children under five. Front Public Health. (2022) 10:861629. doi: 10.3389/fpubh.2022.861629
5. Naghavi, M, Abajobir, AA, Abbafati, C, Abbas, KM, Abd-Allah, F, Abera, SF, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the global burden of disease study 2016. Lancet. (2017) 390:1151–210. doi: 10.1016/S0140-6736(17)32152-9
7. Demissie, GD, Yeshaw, Y, Aleminew, W, and Akalu, Y. Diarrhea and associated factors among under five children in sub-Saharan Africa: evidence from demographic and health surveys of 34 sub-Saharan countries. PLoS One. (2021) 16:e0257522. doi: 10.1371/journal.pone.0257522
12. Bogale, GG, Gelaye, KA, Degefie, DT, and Gelaw, YA. Spatial patterns of childhood diarrhea in Ethiopia: data from Ethiopian demographic and health surveys (2000, 2005, and 2011). BMC Infect Dis. (2017) 17:1–10. doi: 10.1186/s12879-017-2504-8
13. Atnafu, A, Sisay, MM, Demissie, GD, and Tessema, ZT. Geographical disparities and determinants of childhood diarrheal illness in Ethiopia: further analysis of 2016 Ethiopian demographic and health survey. Trop Med Health. (2020) 48:1–12. doi: 10.1186/s41182-020-00252-5
14. Wu, W, Guo, J, Guan, P, Sun, Y, and Zhou, B. Clusters of spatial, temporal, and space-time distribution of hemorrhagic fever with renal syndrome in Liaoning Province, northeastern China. BMC Infect Dis. (2011) 11:1–8. doi: 10.1186/1471-2334-11-229
15. Bolarinwa, OA, Tessema, ZT, Frimpong, JB, Seidu, A-A, and Ahinkorah, BO. Multi-level analysis and spatial interpolation of distributions and predictors of childhood diarrhea in Nigeria. Environ Health Insights. (2021) 15:11786302211045286. doi: 10.1177/11786302211045286
16. Onyambu, P., and Rutayisire, E., Diarrhoeal diseases in children under five years exhibits space-time disparities and priority areas for control interventions in Rwanda. (2020).
17. Fenta, SM, and Nigussie, TZ. Individual-and community-level risk factors associated with childhood diarrhea in Ethiopia: a multilevel analysis of 2016 Ethiopia demographic and health survey. Int J Pediatr. (2021) 2021:1–8. doi: 10.1155/2021/8883618
18. Saha, J, Mondal, S, Chouhan, P, Hussain, M, Yang, J, and Bibi, A. Occurrence of diarrheal disease among under-five children and associated sociodemographic and household environmental factors: an investigation based on National Family Health Survey-4 in rural India. Children. (2022) 9:658. doi: 10.3390/children9050658
19. Wolde, D, Tilahun, GA, Kotiso, KS, Medhin, G, and Eguale, T. The burden of diarrheal diseases and its associated factors among under-five children in Welkite town: A community based cross-sectional study. Int J Public Health. (2022) 67:1604960. doi: 10.3389/ijph.2022.1604960
20. Ugboko, HU, Nwinyi, OC, Oranusi, SU, and Fagbeminiyi, FF. Risk factors of diarrhoea among children under five years in Southwest Nigeria. Int J Microbiol. (2021) 2021:1–9. doi: 10.1155/2021/8868543
21. Tareke, AA, Enyew, EB, and Takele, BAJPO. Pooled prevalence and associated factors of diarrhea among under-five years children in East Africa: a multilevel logistic regression analysis. PLoS One. (2022) 17:e0264559. doi: 10.1371/journal.pone.0264559
22. Workie, GY, Akalu, TY, and Baraki, AGJBID. Environmental factors affecting childhood diarrheal disease among under-five children in Jamma district, south Wello zone, Northeast Ethiopia. BMC Infect Dis. (2019) 19:804–7. doi: 10.1186/s12879-019-4445-x
23. Kulinkina, AV, Mohan, VR, Francis, MR, Kattula, D, Sarkar, R, Plummer, JD, et al. Seasonality of water quality and diarrheal disease counts in urban and rural settings in South India. Sci Rep. (2016) 6:20521. doi: 10.1038/srep20521
24. Bandyopadhyay, S, Kanji, S, and Wang, LJAG. The impact of rainfall and temperature variation on diarrheal prevalence in sub-Saharan Africa. Appl Geogr. (2012) 33:63–72. doi: 10.1016/j.apgeog.2011.07.017
25. Phung, D, Huang, C, Rutherford, S, Chu, C, Wang, X, Nguyen, M, et al. Temporal and spatial patterns of diarrhoea in the Mekong Delta area. Vietnam. (2015) 143:3488–97. doi: 10.1017/S0950268815000709
26. Legros, D, and Dubé, J. Spatial econometrics using microdata. Hoboken, NJ: John Wiley & Sons (2014).
27. Blossom, JC, Finkelstein, JL, Guan, WW, and Burns, B. Applying GIS methods to public health research at Harvard University. J Map Geography Lib. (2011) 7:349–76. doi: 10.1080/15420353.2011.599770
29. Robertson, C, and Nelson, TA. Review of software for space-time disease surveillance. Int J Health Geogr. (2010) 9:16–8. doi: 10.1186/1476-072X-9-16
30. LeSage, JP . An introduction to spatial econometrics. Rev Econ Ind. (2008) 123:19–44. doi: 10.4000/rei.3887
31. Elhorst, JP . Spatial econometrics: From cross-sectional data to spatial panels, vol. 479. Berlin: Springer (2014).
32. Paul, P . Socio-demographic and environmental factors associated with diarrhoeal disease among children under five in India. BMC Public Health. (2020) 20:1–11. doi: 10.1186/s12889-020-09981-y
33. Nilima,, Kamath, A, Shetty, K, Unnikrishnan, B, Kaushik, S, Rai, SN, et al. Prevalence, patterns, and predictors of diarrhea: a spatial-temporal comprehensive evaluation in India. BMC Public Health. (2018) 18:1–10. doi: 10.1186/s12889-018-6213-z
34. Osei, FB, and Stein, A. Spatial variation and hot-spots of district level diarrhea incidences in Ghana: 2010–2014. BMC Public Health. (2017) 17:1–10. doi: 10.1186/s12889-017-4541-z
35. Edwin, P, and Azage, M. Geographical variations and factors associated with childhood diarrhea in Tanzania: a national population based survey 2015-16. Ethiop J Health Sci. (2019) 29:13. doi: 10.4314/ejhs.v29i4.13
36. Asare, EO, Warren, JL, and Pitzer, VE. Spatiotemporal patterns of diarrhea incidence in Ghana and the impact of meteorological and socio-demographic factors. Front Epidemiol. (2022) 2:4. doi: 10.3389/fepid.2022.871232
37. Ghosh, K, Chakraborty, AS, and Mog, M. Prevalence of diarrhoea among under five children in India and its contextual determinants: a geo-spatial analysis. Clin Epidemiol Global Health. (2021) 12:100813. doi: 10.1016/j.cegh.2021.100813
38. Lima, DDS, da Paz, WS, Lopes de Sousa, ÁFL, de Andrade, D, Conacci, BJ, Damasceno, FS, et al. Space–time clustering and socioeconomic factors associated with mortality from diarrhea in Alagoas, northeastern Brazil: a 20-year population-based study. Trop Med Infect Dis. (2022) 7:312. doi: 10.3390/tropicalmed7100312
39. Azage, M, Kumie, A, Worku, A, and Bagtzoglou, AC. Childhood diarrhea exhibits spatiotemporal variation in Northwest Ethiopia: a SaTScan spatial statistical analysis. PLoS One. (2015) 10:e0144690. doi: 10.1371/journal.pone.0144690
40. Gelan, E, Worku, M, Misganaw, A, Wongel, T, and Alemayehu, Y. Spatial disparities and associated factors of under-five diarrhea disease in Ilubabore zone, Oromia regional state, Ethiopia. Int J Clin Med Educ Res. (2022) 1:1–9.
41. Beyene, H, Deressa, W, Kumie, A, and Grace, D. Spatial, temporal, and spatiotemporal analysis of under-five diarrhea in southern Ethiopia. Trop Med Health. (2018) 46:1–12. doi: 10.1186/s41182-018-0101-1
42. Alemayehu, B, Ayele, BT, Valsangiacomo, C, and Ambelu, A. Spatiotemporal and hotspot detection of U5-children diarrhea in resource-limited areas of Ethiopia. Sci Rep. (2020) 10:10997. doi: 10.1038/s41598-020-67623-0
43. Li, R, Lai, Y, Feng, C, Dev, R, Wang, Y, and Hao, Y. Diarrhea in under five year-old children in Nepal: a spatiotemporal analysis based on demographic and health survey data. Int J Environ Res Public Health. (2020) 17:2140. doi: 10.3390/ijerph17062140
44. Sahiledengle, B, Teferu, Z, Tekalegn, Y, Zenbaba, D, Seyoum, K, Atlaw, D, et al. A multilevel analysis of factors associated with childhood diarrhea in Ethiopia. Environ Health Insights. (2021) 15:11786302211009894. doi: 10.1177/11786302211009894
45. Workie, GY, Akalu, TY, and Baraki, AG. Environmental factors affecting childhood diarrheal disease among under-five children in Jamma district, south Wello zone, Northeast Ethiopia. BMC Infect Dis. (2019) 19:1–7.
46. Gizaw, Z, Woldu, W, and Bitew, BD. Child feeding practices and diarrheal disease among children less than two years of age of the nomadic people in Hadaleala District, Afar region, Northeast Ethiopia. Int Breastfeed J. (2017) 12:24–10. doi: 10.1186/s13006-017-0115-z
47. Lokossou, GA, Kouakanou, L, Schumacher, A, and Zenclussen, AC. Human breast milk: from food to active immune response with disease protection in infants and mothers. Front Immunol. (2022) 13:849012. doi: 10.3389/fimmu.2022.849012
Keywords: childhood, diarrhea, spatio-temporal, zones, Ethiopia
Citation: Tiku M, Zeru MA and Belay DB (2024) Spatio-temporal distributions and determinants of diarrhea among under-five children in Ethiopia. Front. Public Health. 12:1369872. doi: 10.3389/fpubh.2024.1369872
Edited by:
Reda Elwakil, Ain Shams University, EgyptReviewed by:
Hemant Khuntia, Siksha O Anusandhan University, IndiaReda Elbadawy, Benha University, Egypt
Copyright © 2024 Tiku, Zeru and Belay. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melkamu A. Zeru, melkamu.ayana@gmail.com
 Meskerem Tiku1
Meskerem Tiku1 Melkamu A. Zeru
Melkamu A. Zeru Denekew Bitew Belay
Denekew Bitew Belay