Abstract
Background:
Stroke survivor's goals reflect their individual priorities and hopes for the future. Person-centred goal setting is recommended in rehabilitation clinical guidelines, but evidence-based training to support its implementation in practice is limited. We aimed to develop, describe and evaluate a new Goal setting and Action Planning (G-AP) rehabilitation training resource to support person-centred goal setting practice in community neuro-rehabilitation settings.
Methods:
A clinical-academic team, advisory group and web-design company were convened to co-develop the G-AP training resource. G-AP training was then delivered to multi-disciplinary staff (n = 48) in four community neuro-rehabilitation teams. A mixed methods evaluation utilising a staff questionnaire and focus group discussion was conducted to investigate staff experiences of G-AP training and their early G-AP implementation efforts. Questionnaire data were analysed descriptively; focus group data were analysed using a Framework approach. An integrated conceptual overview of data was developed to illustrate findings.
Results:
A fully online G-AP training resource comprising a training website and two interactive webinars was developed. Following training, 41/48 (85%) staff completed the online questionnaire and 8/48 (17%) participated in the focus group. Nearly all staff rated the training website as excellent (n = 25/40; 62%) or good (n = 14/40; 35%) and the webinars as excellent (n = 26/41; 63%) or good (n = 14/41; 34%). Following training, staff agreed they were knowledgeable about G-AP (37/41; 90%) and had the confidence (35/40; 88%) and skills (35/40; 88%) to use it in practice. Within one month of training, staff described implementing G-AP individually, but transitioning to implementation at a team level required more time to develop new working practices. Team context including staff beliefs about G-AP, leadership support and competing demands impacted (positively and negatively) on staff training engagement, learning experience and implementation efforts.
Conclusions:
The new G-AP training resource was positively evaluated and supported early G-AP implementation efforts. This study advances our understanding of training evaluation by highlighting the training—context interaction the temporal nature of training effects. A follow up study evaluating longer term G-AP implementation is underway.
1 Introduction
Person-centred goal setting is a cornerstone of good neurological rehabilitation practice (1) and is recommended in rehabilitation policy (2, 3) and clinical guidelines (4, 5). Working in partnership with patients who have neurological conditions to identify and pursue their personal goals optimises their motivation and involvement in the goal setting process (6, 7) and ensures that rehabilitation addresses their needs, preferences and priorities (8–10). However, evidence suggests that routine goal setting practice is sub-optimal (11–13) and that rehabilitation staff would like targeted training to support their goal setting practice (13, 14).
Evidence and theory based (15–17), the Goal setting and Action Planning (G-AP) framework informs a person-centred approach to the setting and pursuit of rehabilitation goals. G-AP is delivered by multidisciplinary community rehabilitation teams and its implementation tailored to individual patients within local contexts. A G-AP record provides patients with a copy of their personal goals, plans and progress (17); an accessible version (Access G-AP) is available for patients with communication difficulties (18).
A G-AP training prototype including both online and face-to-face components has been developed to support person-centred goal-setting practice (19). To enhance G-AP-related knowledge, skills, confidence, and practice, behaviour change techniques including role play, information provision, feedback, and modelling are incorporated (20, 21). The training has been positively evaluated by rehabilitation staff (19); however, additional training content was recommended to support planning for G-AP implementation in local contexts and provision of accessible resources to support patients with communication difficulties throughout the G-AP process. Additionally, the onset of COVID-19 required a fully online training resource to comply with social distancing restrictions.
Whilst staff training is the primary strategy used to support implementation of new rehabilitation interventions (
22), training development and evaluation is consistently under reported (
23). We sought to address this evidence-practice gap by developing, describing and conducting an initial evaluation of a new online G-AP training resource (based on the protype) to support delivery of person-centred goal setting practice in community neuro-rehabilitation settings. The research questions we sought to answer were:
RQ1 What are staff opinions and experiences of the new online G-AP training resource?
RQ2 To what extent does the new online G-AP training resource prepare staff to deliver G-AP in practice?
2 Methods
2.1 Phase 1: development of the online G-AP training resource
2.1.1 Co-production approach
A clinical-academic project team (n = 5) and advisory group (n = 8) were convened to develop the new online G-AP training resource. The clinical-academic team comprised of five practicing neuro-rehabilitation clinicians including three speech and language therapists (SB, EC, LG), one occupational therapist (LS) and one physiotherapist (II). In addition to their clinical role, LS and SB were academics with expertise in G-AP research. The advisory group comprised of two carers and three people with neurological conditions, including one with a communication difficulty. Three rehabilitation staff members completed the advisory group (See Supplementary File S1). A web design company with video production and graphic design expertise worked alongside the project team to create the new G-AP training website.
2.1.2 Development of new training content
Research evidence, clinical experience, rehabilitation policy and advisory group feedback informed updates and additions to the online G-AP training prototype, including new content and resources to support local G-AP implementation and delivery of G-AP to patients with communication difficulties (see Supplementary File S2). Webinars were introduced to replace the face-to-face training but retain the interactive and peer learning component of the training.
2.1.3 Use of implementation strategies
Implementation strategies defined as “methods or techniques used to improve adoption, implementation, sustainment, and scale-up of interventions” (24) informed the project set up and the development and delivery of the training materials and resources. The specific implementation strategies used, described using the Expert Recommendations for Implementing Change (ERIC) compilation (25), are summarised in Figure 1.
Figure 1

Strategies used to support G-AP implementation (ERIC compilation; Powell et al., 2015).
A content overview of the developed online G-AP training resource, including the training website and interactive webinars is presented in Table 1.
Table 1
| G-AP training website: freely available: https://g-apframework.scot/ |
|
| Interactive G-AP webinars: 2 × 2-hour interactive sessions delivered on MS teams |
|
Overview of the developed online G-AP training resource.
2.2 Phase 2: delivery and evaluation of the online G-AP training resource
An overview of the study participants and procedure is summarised in Figure 2.
Figure 2
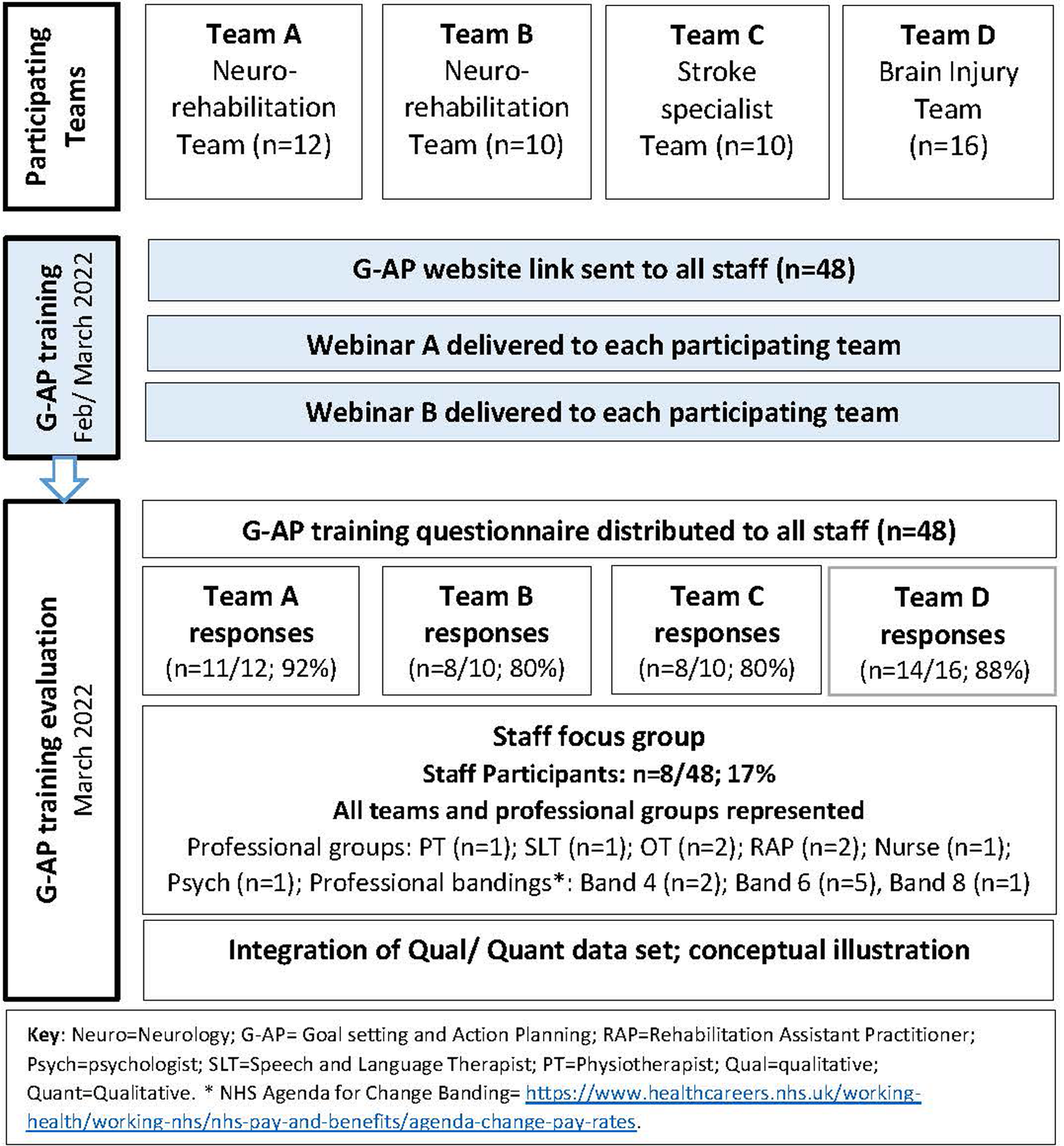
Study participants and procedure.
2.2.1 Participating community teams
Two neuro-rehabilitation teams (Team A and B) supported by a specialist stroke team (Team C) and one brain injury team (Team D) in NHS Lanarkshire, Scotland took part. Teams comprised a total of 48 multi-disciplinary staff members. See Supplementary File S3 for a descriptor of each participating team and usual goal setting practice pre-training delivery.
2.2.2 Delivery of the online G-AP training resource
The G-AP website link was emailed to all rehabilitation staff who were asked to dedicate three hours to complete the training within a four-week period. Staff were then invited to take part in webinar 1 then webinar 2, one week later. Webinars were led by LS supported by one other project group member (SB, II or LG). Webinars were recorded and made available to staff for review or catch up. The G-AP training website remained available to staff throughout the study period.
2.2.3 Evaluation design and procedure
A mixed methods evaluation using a convergent design (26, pg. 52) was conducted to evaluate the G-AP training resource and its impact on early (one month post training) G-AP implementation. Informed by the convergent design, qualitative and quantitative data were collected then combined to provide different insights about staff opinions of the G-AP training and their experiences of implementing G-AP in practice. Combining these data sets provided a more complete training evaluation. All rehabilitation staff from participating teams were eligible to take part. The criteria for describing and evaluating training interventions in healthcare professions—CRe-DEPTH (27) were used to inform the conduct and reporting of this study (see Supplementary File S4).
2.2.4 Data collection
2.2.4.1 G-AP training questionnaire
Building on a previous questionnaire (19), a G-AP training questionnaire was developed and emailed to staff within one week of completing the training website and webinars (see Supplementary File S5).
2.2.4.2 Staff focus group
A one hour focus group was conducted following the training period to explore staff opinions and experiences of the G-AP online training and webinars and the extent to which they had prepared them to implement G-AP in practice. Staff were purposively sampled to ensure all professional groups and levels of experience across the three teams were represented.
2.2.5 Data analysis
Informed by our mixed methods convergent design (26), each data set was analysed separately then combined to address the research questions. G-AP training questionnaire data were analysed using descriptive statistics; open ended responses were categorised and described. Focus group data were analysed using a five stage Framework approach (28, 29) (see Supplementary File S6). A conceptual overview was developed [KE, LS] to illustrate the combined data set.
2.2.6 Approvals
Ethical approval was obtained from the Glasgow Caledonian University Nursing Department Research Ethics Committee (ref: HLS/NCH/21/010). No NHS ethics approval was required as no patient participants were included in this study.
3 Results
3.1 Participants
Eighty five percent of staff (41/48) responded to the G-AP training questionnaire, of which 8/48 (17%) participated in the focus group (see Figure 2). All 41 respondents completed the online training and 40 attended both webinars.
3.2 Staff opinions and experiences of the G-AP training resource
Quantitative and qualitative data are combined and reported under the main themes of staff engagement with the training, learning experience and readiness for G-AP implementation. Illustrative quotes for themes and related sub-themes are referenced within the text (e.g., Quote 1) and presented in Table 2. A conceptual thematic overview incorporating contextual factors, is presented in Figure 3.
Table 2
| Theme | Subtheme | Illustrative quotes |
|---|---|---|
| Staff engagement with the training | Contextual factors influencing staff engagement | Q1 “Busy caseload and lots of competing development projects on the go within the team at the moment.” (*QR 4; Question 5) Q2 “Obviously you've got the external issues you won't always have like the Covid aspect, the amount of staff that are maybe off and the extra pressures that are there that hopefully in the future you're not going to have to deal with.” [Focus Group; P1] Q3 “We are always fire-fighting with regards to clinical time and we are always really busy, but as long as we know it's [G-AP training] so important, related to our work and it's going to make things better in the long run, then it's about managing it. So, I was happy to fit it in and work round as best I could.” [Focus Group; P8] Q4 “[My] manager was supportive to schedule a half day working from home to allow training without distraction which was helpful.” (Response 12, Question 5). Q5 “What was helpful was having plenty of notice about the training, therefore I could book the training into my diary a good few weeks in advance.” (QR 16, Question 5). |
| Delivery of the online G-AP training and webinars: pros and cons | Q6 “I thought it [the G-AP training website] flowed really well. It was easy to navigate. You could dip in and out of the sections—they were self-explanatory.” [Focus Group, P6] Q7 “Because it was online, it didn't take you all day. If you were going to a course, by the time you get there and by the time you get back. I thought that was a bit easier as well. It wasn't as time consuming.” [Focus Group; P2] Q8 “It [the website training] has pros and cons. I guess it depends on your own learning style as well, doesnt it? What you prefer to do.” [Focus Group; P7]. Q9 “Getting peoples opinions is a bit harder when you're online than when you are face-to-face, maybe people open up a bit more [face-to-face].” [Focus group; P4] Q10 “It was helpful to have that time to go through it [the G-AP training website] all yourself and do all the reading and have that understanding of what it [G-AP] is and then go into the discussion groups [webinars].” [Focus Group; P7] Q11 “It would be helpful to have trialled G-AP with a few patients prior to webinar [B], then we could bring to discussions what worked well/what didn't more, as it's the practical side of implementing it that's the challenge.” (QR 9, Question 33). | |
| Staff learning experience | G-AP website content | Q12 “I think the content of it [the G-AP training website] was really comprehensive. It covered everything that you wanted to hear about. But it was quite a lot to tackle in one go so you do need to split it up.” [Focus Group; P3] Q13 “For staff experienced in goal setting, I did not feel this [videos] added to my learning; several videos also increased time spent completing training.” (QR 8, Question 12). Q14 “I think the videos were very good and very helpful. I think practically you can understand, well I can, a lot easier if you can see it being played out rather than just reading lots of scrolls of writing.” (Focus Group; P4) |
| G-AP webinar content | Q15 “It was good to interact with all members of rehabilitation team [in the webinars]” (QR 3, Question 33) Q16 “[The webinars were] informal enough to feel safe to ask questions” (QR 4, Question 38). Q17 “It was really helpful to have that discussion [in webinar A] of what it [G-AP] actually looks like in everyday working life and the practicalities around it. The different patients it might work well with, and the patients it might be more challenging with.” [Focus group, P7] Q18 “I definitely thought the implementation webinar [webinar B] was really useful to gather the information [about local implementation].” [Focus group, P4] Q19 “I think the whole point about goal setting with your patients is that it is really steeped in communication, in good communication. When you're not a speech and language therapist, I’ll put my hands up, I find those patients [with communication difficulties] really, really challenging. So to have the ability to be able to discuss that [how to support people with communication difficulties] … to focus on that specific kind of patient was really helpful for me.” [Focus group, P4] Q20 “The patients that are really lacking in insight, that aren't quite there yet in terms of setting effective kind of person-centred goals. So, it [webinar A] was getting to some of those more tricky bits that you might come up against.” [Focus group, P3] | |
| Staff readiness for G-AP implementation | Feeling prepared for G-AP implementation at an individual level | Q21 “I do think it [the training] gave you the skills and confidence to go off and use it individually with a patient. I used it with a patient last week and it felt comfortable using it and it worked really well. I used Access G-AP [accessible version of the G-AP record] with an aphasic man and I felt the training prepared me to do that.” [Focus Group; P7] Q22 “I think when somethings new it's almost like we need permission. Because there was lots of ‘can we make that suggestion? Is that when we step in?’ We need to know that that's OK to do that, so it [webinar A] was useful for that.” [Focus Group, P6] Q23 “One of my colleagues [and I], were working jointly with a patient who has communication difficulties, and today we're going to use the G-AP toolkit. It's actually encouraged us to go back and look at some of the other resources. For this patient I think this [Talking Mats] will be a really good tool to use in conjunction with G-AP.” [Focus Group; P6] |
| Transitioning to G-AP implementation at a team level | Q24 “There is nobody that is not on-board [with G-AP implementation].” [Focus Group; P8] Q25 “The implementation is the hard bit. That's the bit that has us scratching our heads about how we are going to make this work logistically, how open people [staff] are to change, how ready are they [the teams] to adopt this kind of practice. We all have the knowledge and the understanding and it's what we do with that now.” [Focus Group; P6] Q26 “I started using it [G-AP] with my own patients and liaising colleagues who have had the same patients, so there's been a bit of multi-disciplinary use as well.” [Focus Group; P4] Q27 “I guess the challenge is using it [G-AP] alongside other professionals … so physio, OT, stroke nurses and using it not just for the speech therapy goals but as a joint goal setting resource. Just as everyone was saying, it needs more conversations of how that would look.” [Focus Group; P7]. Q28 “Our kind of end point from the implementation one [webinar B] was ‘right, we need to set up a G-AP implementation working group within our team to figure out how to get through all these things .. we're just setting up our implementation team at the minute.” [Focus Group; P3] Q29 “We were talking about an implementation champion and having someone who's got that time to invest. I think that's going to be our main challenge moving forward. We actually really want to use it [G-AP] and we want to invest a time but whether that's realistic, I don't know.” [Focus Group; P7] |
Themes, sub-themes and illustrative quotes.
*QR, questionnaire response.
Figure 3

Conceptual thematic overview incorporating contextual factors.
3.2.1 Overall ratings
The vast majority of staff rated the G-AP online training and webinars as either excellent or good (see Figure 4) and reported that the content of the online training (n = 36/41; 87%) and webinars (n = 31/40; 78%) was ‘very relevant’ to their work with patients. Ninety percent of staff (37/41) agreed that the combination of G-AP website and webinars offered the best learning experience.
Figure 4
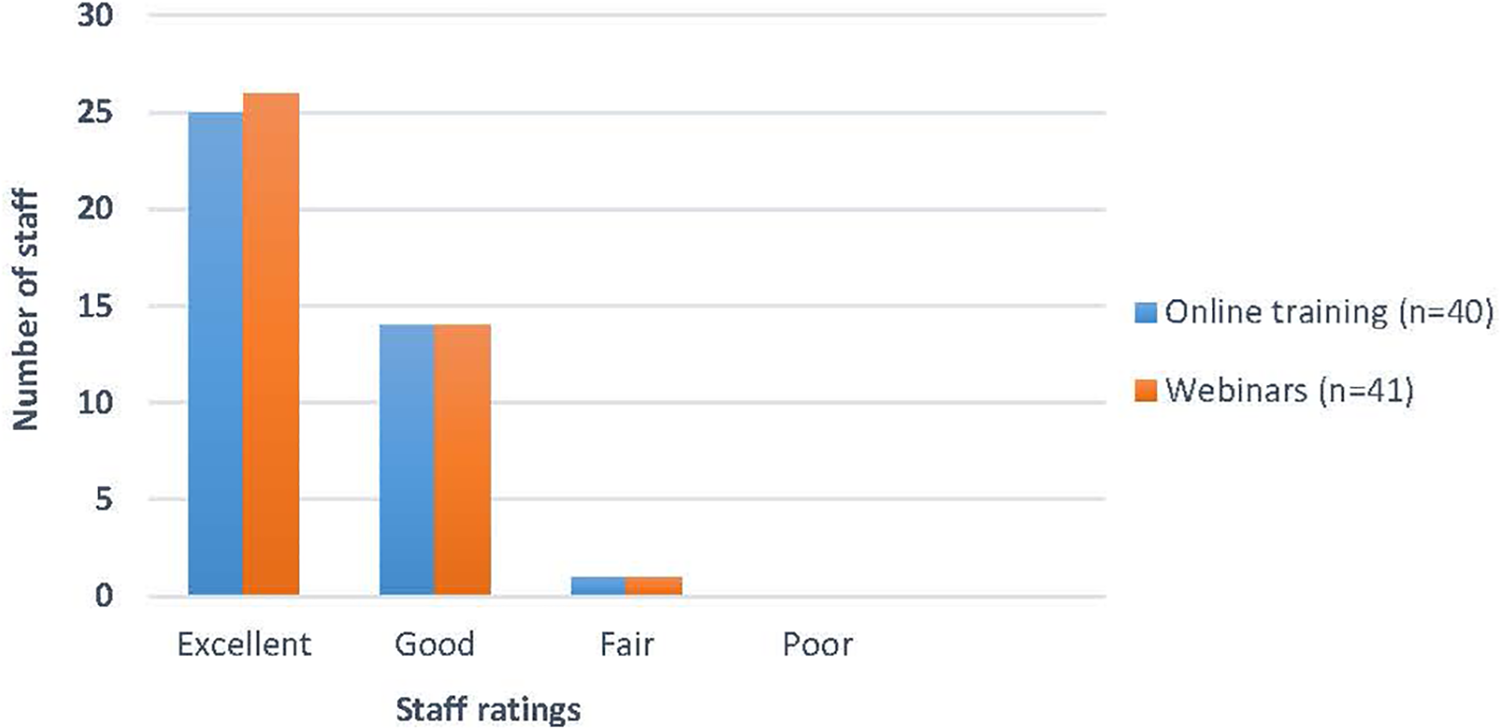
Overall ratings of G-AP training resource.
3.2.2 Staff engagement with the training
3.2.2.1 Time spent on G-AP training website
The majority of staff (28/40; 70%) spent the recommended three hours or more engaging with the G-AP training website (see Figure 5).
Figure 5
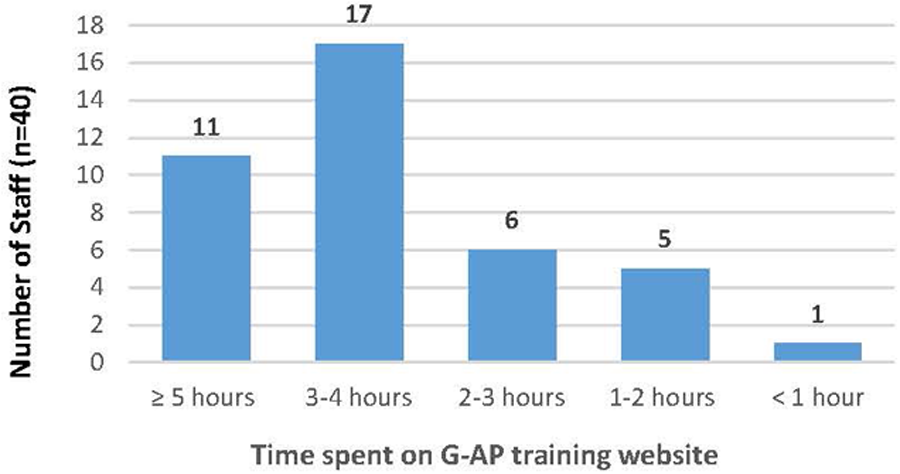
Time spent on G-AP training website.
3.2.2.2 Contextual factors influencing staff engagement
Sixty-two percent of staff (25/40) reported that setting time aside to complete the online training could be difficult. Local contextual factors such as competing demands, caseload commitments, part-time hours and staffing issues challenged staff engagement (Quote 1). Whilst perceived as a temporary barrier, Covid-19 created an additional challenge to training engagement (Quote 2). Staff beliefs that the training was relevant to their work and would lead to efficiencies in the longer term motivated training engagement (Quote 3). Supportive managers and advanced notice of training were highly valued (Quote 4–5).
3.2.2.3 Pros and cons of online format and delivery of the online G-AP training and webinars
The vast majority of staff reported the G-AP training website was either extremely easy (21/40; 52%) or somewhat easy (n = 18/40; 45%) to navigate through (Quote 6) and supported efficient use of time (Quote 7). However, staff acknowledged online training was not everyone's preferred option (Quote 8). The vast majority of staff agreed the webinars were well delivered (40/41; 97%), but 45% (18/41) agreed face to face webinars would have been preferable (Quote 9). Most staff reported that having two webinars of two hour duration was about right (n = 35/41; 86%; n = 34/41; 83% respectively). Staff liked the combination of the G-AP website and webinars; the majority (n = 35/40; 88%) reporting the former was good preparation for the later (Quote 10). However, staff recommended more time between webinar A and B would have supported informed discussions about local G-AP implementation (Quote 11).
3.2.3 Staff learning experience
3.2.3.1 G-AP website content
All sections of the G-AP training website were rated highly (see Table 3). There was consensus that the content was comprehensive, largely pitched at the right level and the amount of information was about right (Quote 12).
Table 3
| Training section | Excellent n (%) |
Good n (%) |
Fair n (%) |
Poor n (%) |
N/A n (%) |
Total responses n/41 (%) |
|---|---|---|---|---|---|---|
| About G-AP | 22 (55) | 17 (43) | 1 (2) | 0 (0) | 0 (0) | 40 (98) |
| G-AP training | 20 (50) | 18 (45) | 1 (2) | 0 (0) | 1 (2) | 40 (98) |
| Role play videos | 23 (58) | 12 (30) | 3 (8) | 1 (2) | 1 (2) | 40 (98) |
| Rights, barriers and ramps | 23 (58) | 15 (37) | 0 (0) | 0 (0) | 2 (5) | 40 (98) |
| Implementation | 15 (38) | 23 (59) | 1 (3) | 0 (0) | 0 (0) | 39 (95) |
Staff ratings of G-AP training website.
N/A, not accessed.
Although not everyone agreed the role-play videos provided added value (Quote 13), most staff reported they positively influenced their learning and practice by providing a different training format and illustrating use of G-AP in practice scenarios (Quote 14). Downloadable versions of the G-AP record (including the accessible version—Access G-AP) were rated as ‘very useful’ by 88% (n = 35/40) of staff.
3.2.3.2 G-AP webinar content
Staff reported that the webinars were interactive and resulted in a positive learning experience (see Table 4; Quotes 15–16).
Table 4
| Strongly agree n (%) |
Agree n (%) |
Disagree n (%) |
Strongly disagree n (%) |
Total responses n/41 (%) |
|
|---|---|---|---|---|---|
| Webinar discussions supported my learning | 25 (62) | 14 (35) | 1 (2) | 0 (0) | 40 (98) |
| I was able to ask questions in the webinars | 31 (77) | 9 (22) | 0 (0) | 0 (0) | 40 (98) |
| I found the webinars enjoyable | 27 (67) | 11 (27) | 2 (5) | 0 (0) | 40 (98) |
| The webinars were interactive | 25 (61) | 15 (38) | 0 (0) | 0 (0) | 40 (98) |
Staff opinions about G-AP webinars.
Webinars supported important discussions that enhanced staff knowledge and confidence to deliver G-AP to individual patients (webinar A) and implement G-AP locally (webinar B) (Quotes 17–18). Staff appreciated opportunities to discuss common clinical dilemmas that impede person-centred practice, for example, supporting patients with communication difficulties and those who may lack insight (Quotes 19–20).
3.2.4 Staff readiness for G-AP implementation
Two main sub-themes captured the extent to which the G-AP training resource supported early G-AP implementation—Feeling prepared for G-AP implementation at an individual level and Transitioning to G-AP implementation at a team level. Staff felt prepared to initiate G-AP individually. However, implementing G-AP at the team level was perceived to be more challenging and likely to take time for teams to make adaptations to staff roles to action the implementation process and strategies.
3.2.4.1 G-AP implementation at an individual level
Following training, the vast majority of staff agreed they had the knowledge, motivation, skills and confidence to use G-AP in practice, including supporting patients with communication difficulties and those with potentially unachievable goals (see Figure 6).
Figure 6
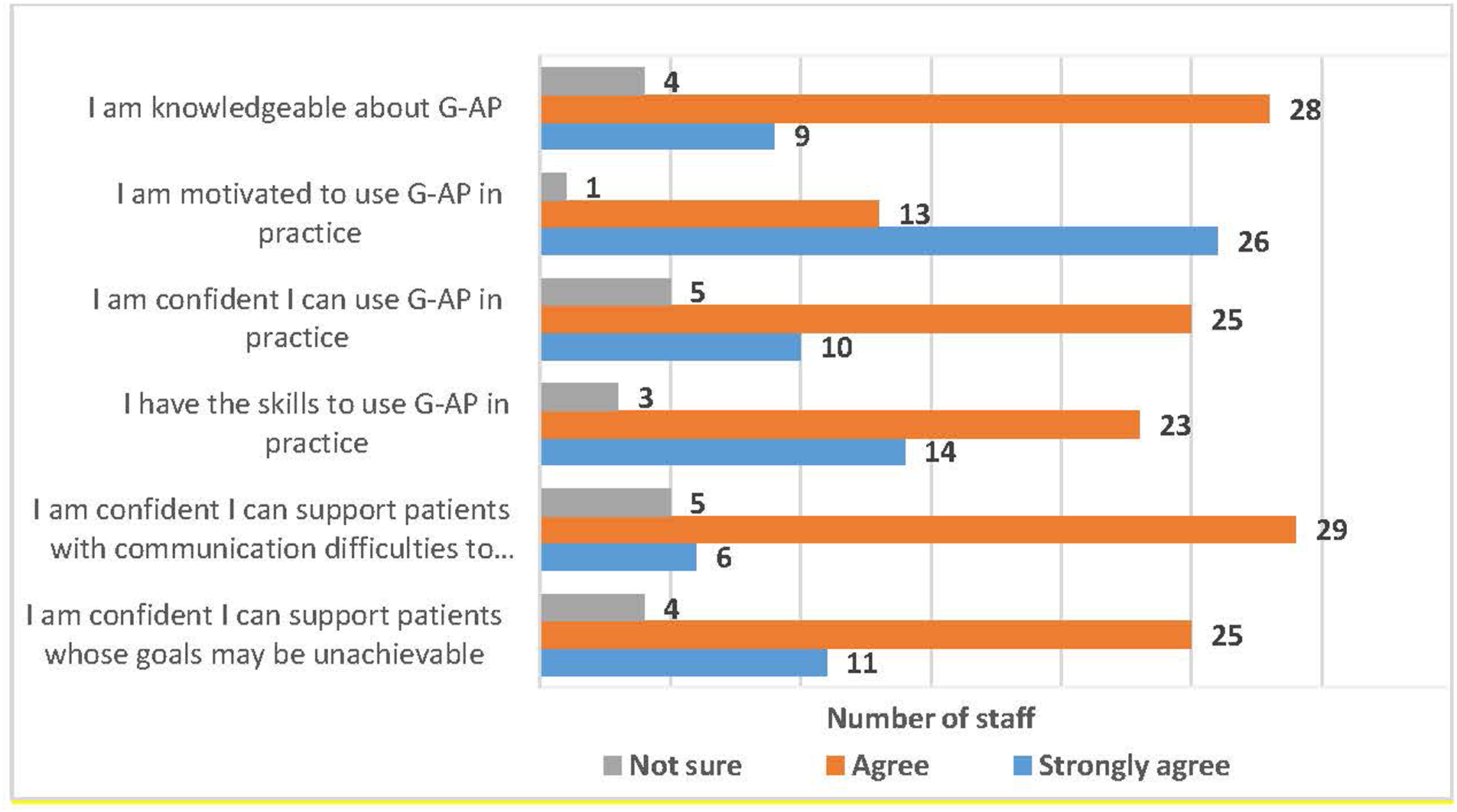
Staff self-ratings of preparedness to used G-AP in practice.
Almost all agreed (39/40; 98%) that webinar A supported helpful discussions about use of G-AP with individual patients and had given them the ‘go-ahead’ to try G-AP out in practice. Staff provided examples of implementing G-AP with individual patients, including to those with communication difficulties (Quotes 21–22). G-AP was also used in joint sessions with other staff and viewed as compatible with existing rehabilitation resources (Quote 23).
3.2.4.2 Transitioning to G-AP implementation at a team level
Whilst the vast majority of staff (38/40; 95%) agreed they felt prepared for G-AP implementation, this did not automatically translate into enacting implementation at a team level (Quotes 24–25). Staff recognised that this would require interdisciplinary team work which would take more time to embed (Quotes 26–27). Whilst not yet actioned, staff had taken on board suggested implementation strategies, including setting up a local implementation group and identifying G-AP champions, however having the time to commit to these implementation efforts was a concern (Quotes 28–29).
4 Discussion
A fully online G-AP training resource, incorporating a training website and two interactive webinars, has been developed, described and evaluated. The delivery and content of the G-AP training resource were rated highly. The majority of staff felt confident and prepared to deliver G-AP at an individual level and shared examples of practice change. Transitioning to G-AP implementation at a team level was at a preliminary stage and perceived as more challenging and requiring more time. An ongoing interplay existed between local contextual factors and staff engagement with the training, their learning experience and local implementation efforts.
4.1 Implementation strategies and temporal considerations
Informed by Expert Recommendations for Implementing Change (25) we used a range of implementation strategies to build a multi-component training resource to support G-AP implementation. Our findings suggest that within one month of training completion, some strategies had yielded positive results. Through our clinical academic partnership, we developed a G-AP training resource of high relevance to clinical practice. Positive staff opinions and experiences of the G-AP training and high ratings of G-AP related skills, confidence and motivation suggests our range of educational materials, resources and delivery methods were highly beneficial to multi-disciplinary staff. However, other implementation strategies needed more time to exert their influence. Whilst local G-AP implementation groups (led by G-AP champions) were planned, more time was needed to convene these groups. Furthermore, G-AP implementation at a team level required some reconfiguration of staff roles and team processes that would take more time to organise. The importance of understanding implementation as a staged process that evolves over time, rather than a one off event, has been highlighted (30, 31). The Stages of Implementation Completion tool (32) tracks implementation across three main stages: pre-implementation (engagement and planning), implementation (staff training, programme start up, monitoring) and sustainment (establishing competency, embedding practice). This study was situated within the pre-implementation and early implementation stage of the process. Evaluation at this stage is critical to pro-actively identify problems or challenges to optimise the chances of later implementation success (32). We are pleased this early evaluation was positive. How G-AP training supports ongoing G-AP implementation and sustainment will be reported in a follow up study.
4.2 Training—context interplay
Rehabilitation is a complex process involving delivery of multi-component interventions (23) many of which will rely on staff training as the primary implementation strategy to support their delivery (22). Our results highlighted the influence of local team contexts on staff engagement with the training, their learning experience and subsequent implementation efforts. Evaluations of health care staff training that focus solely on “does it work” are over simplistic and do not take account of this complex training-context interplay (30; pg14). Staff work patterns, beliefs about training relevance (33), high workloads, understaffing and complex workflows (34) are reported contextual factors that have diminished or negated the impact of health care staff training on learning and practice change. Whilst staff training can enhance the requisite knowledge, skills, confidence and motivation required to support practice change and implementation efforts, the training—context interaction will inevitably influence implementation success or failure.
4.3 Strengths and limitations
The NHS spends over £4 billion a year on training (35). Reporting the development and evaluation of rehabilitation staff training to support implementation of evidence-based practice is essential to ensure this money is well spent. However, details of training provided to support delivery of rehabilitation interventions is often absent or unclear (23), thus compromising the integrity of the evaluation. Our research has resulted in a G-AP training resource that has been evaluated and can be fully described for both clinical and research purposes. Furthermore, our co-production approach has supported development of a resource that is methodologically sound, clinically relevant and cognisant of patient and carer priorities.
However, this evaluation was conducted in one NHS Scotland board. A large-scale implementation evaluation with more participating NHS sites across the UK is necessary to enhance the generalisability of our findings. The short evaluation time frame and absence of patient data also limit in the extent to which we can report on longer term G-AP implementation and impacts (if any) on patient experiences of care. These limitations are being addressed in our follow up study.
5 Conclusions
The co-developed G-AP training resource, incorporating a training website (freely available) and two interactive webinars, has been well received by staff and shows promise in supporting person-centred goal setting practice in community neuro-rehabilitation settings. Implementation was facilitated by training materials that were relevant to clinical practice with clear benefits reflected in improvements to staff skills, confidence and motivation. It is important to recognise that implementation is a staged process that unfolds over time and strategies such as local implementation groups and team reconfiguration take time. Our findings also demonstrate the ongoing interplay between local contextual factors and staff engagement with training, their learning experience and local implementation efforts. Both the temporal nature of training effects and training—context interaction should be factored in when designing rehabilitation training evaluations.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by Glasgow Caledonian University Nursing Department Research Ethics Committee (ref: HLS/NCH/21/010). The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual (s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. KE: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. SB: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. LG: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. EC: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. II: Conceptualization, Data curation, Methodology, Project administration, Writing – original draft, Writing – review & editing. MB: Conceptualization, Formal analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing. RF: Conceptualization, Formal analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by funding form the Scottish Government Neurological framework fund. LS (first author) was supported by a Stroke Association Clinical Lectureship award (TSA LECT2016/02) for the duration of the study. KE was funded by a Glasgow Caledonian University PhD studentship.
Acknowledgments
We would like to thank all staff participants and members of the advisory group for their involvement in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fresc.2025.1505188/full#supplementary-material
References
1.
British Society of Rehabilitation Medicine. BSRM Standards for Specialist Rehabilitation for Community Dwelling Adults – Update of 2002 Standards. London: British Society of Rehabilitation Medicine C/o Royal College of Physicians (2021).
2.
National Advisory Committee for Stroke (NACS). A Progressive Stroke Pathway. Edinburgh: The Scottish Government (2022).
3.
NHS England and NHS Improvement. National Service Model for an Integrated Community Stroke Service. London: NHS England and NHS Improvement (2022). Available online at:https://www.england.nhs.uk/wp-content/uploads/2022/02/stroke-integrated-community-service-february-2022.pdf (accessed March 6, 2024)
4.
National Clinical Guideline for Stroke for the UK and Ireland. London: Intercollegiate Stroke Working Party (2023). Available at:www.strokeguideline.org(Accessed March 17, 2025).
5.
Scottish Intercollegiate Guidelines Network (SIGN). Brain Injury Rehabilitation in Adults.(SIGN publication no. 130). Edinburgh: SIGN (2013).
6.
Knutti K Björklund Carlstedt A Clasen R Green D . Impacts of goal setting on engagement and rehabilitation outcomes following acquired brain injury: a systematic review of reviews. Disabil Rehabil. (2022) 44(12):2581–90. 10.1080/09638288.2020.1846796
7.
Scobbie L Brady MC Duncan EAS Wyke S . Goal attainment, adjustment and disengagement in the first year after stroke: a qualitative study. Neuropsychol Rehabil. (2021) 31(5):691–709. 10.1080/09602011.2020.1724803
8.
Rosewilliam S Roskell C Pandyan A . A systematic review and synthesis of the quantitative and qualitative evidence behind patient-centred goal setting in stroke rehabilitation. Clin Rehabil. (2011) 25:501–14. 10.1177/0269215510394467
9.
Plant SE Tyson SF Kirk S Parsons J . What are the barriers and facilitators to goal-setting during rehabilitation for stroke and other acquired brain injuries? A systematic review and meta-synthesis. Clin Rehabil. (2016) 30(9):921–30. 10.1177/0269215516655856
10.
Gray SC Grudniewicz A Armas A Mold J Im J Boeckxstaens P . Goal-oriented care: a catalyst for person-centred system integration. Int J Integr Care. (2020) 20(4):8. 10.5334/ijic.5520
11.
Scobbie L Duncan EAS Brady MC Wyke S . Goal setting practice in services delivering community-based stroke rehabilitation: a United Kingdom (UK) wide survey. Disabil Rehabil. (2015) 37(14):1291–8. 10.3109/09638288.2014.961652
12.
Crawford L Maxwell J Colquhoun H Kingsnorth S Fehlings D Zarshenas S et al Facilitators and barriers to patient-centred goal-setting in rehabilitation: a scoping review. Clin Rehabil. (2022) 36(12):1694–704. 10.1177/02692155221121006
13.
Brown SE Scobbie L Worrall L Brady MC . A multinational online survey of the goal setting practice of rehabilitation staff with stroke survivors with aphasia. Aphasiology. (2023) 37(3):479–503. 10.1080/02687038.2022.2031861
14.
Rose A Rosewilliam S Soundy A . Shared decision making within goal setting in rehabilitation settings: a systematic review. Patient Educ Couns. (2017) 100(1):65–75. 10.1016/j.pec.2016.07.030
15.
Scobbie L Wyke S . Identifying and applying psychological theory to setting and achieving rehabilitation goals. Clin Rehabil. (2009) 23:321. 10.1177/0269215509102981
16.
Scobbie L Dixon D Wyke S . Goal setting and action planning in the rehabilitation setting: development of a theoretically informed practice framework. Clin Rehabil. (2011) 25(5):468–82. 10.1177/0269215510389198
17.
Scobbie L McLean D Dixon D Duncan E Wyke S . Implementing a framework for goal setting in community based stroke rehabilitation: a process evaluation. BMC Health Serv Res. (2013) 13:190–203. 10.1186/1472-6963-13-190
18.
Brown SE Scobbie L Worrall L Mc Menamin R Brady MC . Access G-AP: development of an accessible goal setting and action planning resource for stroke survivors with aphasia. Disabil Rehabil. (2023) 45(13):2107–17. 10.1080/09638288.2022.2085331
19.
Scobbie L Duncan EAS Brady MC Thomson K Wyke S . Facilitators and “deal breakers”: a mixed methods study investigating implementation of the goal setting and action planning (G-AP) framework in community rehabilitation teams. BMC Health Serv Res. (2020) 20(1):791. 10.1186/s12913-020-05651-2
20.
Michie S Johnston M Abraham C Lawton R Parker D Walker A et al Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. (2005) 14(1):26–33. 10.1136/qshc.2004.011155
21.
Michie S Johnston M Francis J Hardeman W Eccles M . From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol Meas. (2008) 57:660–80. 10.1111/j.1464-0597.2008.00341.x
22.
Flynn R Cassidy C Dobson L Al-Rassi J Langley J Swindle J et al Knowledge translation strategies to support the sustainability of evidence-based interventions in healthcare: a scoping review. Implement Sci. (2023) 18(1):69. 10.1186/s13012-023-01320-0
23.
Goodwin VA Hill JJ Fullam JA Finning K Pentecost C Richards DA . Intervention development and treatment success in UK health technology assessment funded trials of physical rehabilitation: a mixed methods analysis. BMJ Open. (2019) 9(8):e026289–026289. 10.1136/bmjopen-2018-026289
24.
Fernandez ME ten Hoor GA van Lieshout S Rodriguez SA Beidas RS Parcel G et al Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. (2019) 7:158. 10.3389/fpubh.2019.00158
25.
Powell BJ Waltz TJ Chinman MJ Damschroder LJ Smith JL Matthieu MM et al A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci. (2015) 10:21. 10.1186/s13012-015-0209-1
26.
Creswell JW . A Concise Introduction to Mixed Methods Research. 2nd ednThousand Oaks, CA: Sage Publications, Inc. (2022).
27.
Van Hecke A Duprez V Pype P Beeckman D Verhaeghe S . Criteria for describing and evaluating training interventions in healthcare professions—CRe-DEPTH. Nurse Educ Today. (2020) 84:104254. 10.1016/j.nedt.2019.104254
28.
Richie J Spencer L . Qualitative data analysis for applied policy research. Anal Qual Data. (1994) 1:173–94. 10.4324/9780203413081_chapter_9
29.
Gayle NK Heath G Cameron E Rashid S Redwood S . Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. (2013) 13:117. 10.1186/1471-2288-13-117
30.
Illing J Corbett S Kehoe A Carter M Hesselgreaves H Crampton P et al How Does the Education and Training of Health and Social Care Staff Transfer to Practice and Benefit Patients? A Realist Approach. London: Department of Health (2019). p. 183.
31.
Wong DR Schaper H Saldana L . Rates of sustainment in the universal stages of implementation completion. Implement Sci Commun. (2022) 3(1):2. 10.1186/s43058-021-00250-6
32.
Saldana L Chamberlain P Wang W Hendricks Brown C . Predicting program start-up using the stages of implementation measure. Adm Policy Ment Health. (2012) 39(6):419–25. 10.1007/s10488-011-0363-y
33.
Clarke DJ Godfrey M Hawkins R Sadler E Harding G Forster A et al Implementing a training intervention to support caregivers after stroke: a process evaluation examining the initiation and embedding of programme change. Implement Sci. (2013) 23(8):96–96. 10.1186/1748-5908-8-96
34.
Greenhalgh T Payne R Hemmings N Leach H Hanson I Khan A et al Training needs for staff providing remote services in general practice: a mixed-methods study. Br J Gen Pract. (2024) 74(738):e17–26. 10.3399/BJGP.2023.0251
35.
NHS England. NHS education funding guide: 2024 – 2025 financial year. (2025). Available at:https://www.england.nhs.uk/long-read/nhs-education-funding-guide-2024-2025-financial-year/(Accessed March 24, 2025).
Summary
Keywords
training, rehabilitation, goal setting, person-centred, implementation, evaluation, mixed methods
Citation
Scobbie L, Elliott K, Boa S, Grayson L, Chesnet E, Izat I, Barber M and Fisher R (2025) Development and evaluation of Goal setting and Action Planning (G-AP) training to support person-centred rehabilitation practice. Front. Rehabil. Sci. 6:1505188. doi: 10.3389/fresc.2025.1505188
Received
02 October 2024
Accepted
10 March 2025
Published
31 March 2025
Volume
6 - 2025
Edited by
Maria Gabriella Ceravolo, Marche Polytechnic University, Italy
Reviewed by
Alessandro Giustini, University San Raffaele, Italy
Christina Papadimitriou, Oakland University, United States
Updates
Copyright
© 2025 Scobbie, Elliott, Boa, Grayson, Chesnet, Izat, Barber and Fisher.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Lesley Scobbie Lesley.Scobbie@gcu.ac.uk
ORCID Rebecca Fisher orcid.org/0000-0001-6866-6341
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.