- 1Centro Paraplegici Ostia, UOC Riabilitazione e Centro Spinale, Asl Roma 3, Rome, Italy
- 2Ordine TSRM PSTRP Roma e Provincia, CdA Logopedisti, Rome, Italy
- 3Rehabilitation Health Care Professionals, Asl Roma 3, Rome, Italy
- 4Homecare Assistance and Home Artificial Nutrition Unit, Asl Roma 3, Rome, Italy
- 5Dipartimento Salute Mentale, UOC TSMREE, Asl Roma 3, Rome, Italy
The Home Artificial Nutrition Unit (HANU) deals with both dysphagic patients receiving enteral and parenteral nutrition and patients who can eat orally with restrictions. In the Lazio Region, the HANU prescribes water gels and thickeners, supplied by the National Health Service (NHS), for safe hydration. Before the employment of a Speech and Language Pathologist (SLP) in the HANU (January 2023), prescriptions were standardized, regardless of the swallowing impairment severity: four jars of thickeners per patient/month and six water gels daily. The Clinical Swallowing Evaluation (CSE) made by the SLP allowed to customize the amount of thickeners and water gels based on the actual needs of the patient. The aim of this study is to investigate the cost savings resulting from the employment of an SLP in the HANU. A descriptive retrospective study was conducted, which analyzed the SLP activity in the HANU of ASL Roma 3 (January–December 2023). The study group consisted of 149 patients (61 males, 88 females with a mean age of 76.2 years) with different pathologies. The cost of each product (thickeners and gelified water) was provided by the Regional Pharmacy. The annual savings were calculated as the difference between the standardized prescription of products (as usual care in our department) and personalized prescription after SLP assessment. Since January 2023, there has been an increasing trend in requests for SLP assessments. The employment of an SLP in the HANU resulted in an annual economic saving of €30,278.67. This preliminary study shows how the employment of an SLP in the HANU can reduce inappropriate prescriptions of thickeners and water gels, thus ensuring cost savings.
Introduction
The Home Artificial Nutrition Unit (HANU) deals with both dysphagic patients receiving enteral and parenteral nutrition and patients who can eat orally but with restrictions. These methods can improve clinical and quality of life (QoL) outcomes, but determining the most effective and safe methods can involve complex decision-making: healthcare professionals should consider using oral, enteral, or parenteral nutrition support, alone or in combination, for people who are either at risk of malnutrition or dehydration or for subjects who are unable to fully satisfy their nutritional needs (1). Artificial nutrition (AN) is often started during hospitalization and continues as long-term home therapy. Typically, there are only minor differences in the indication for Home AN (HAN) and for in-hospital AN. In HAN, additional criteria need to be considered carefully, such as prognosis, health-related QoL, and any ethical aspect of a treatment. To start HAN, the guiding principle is that without AN, the nutritional status of the patient is expected to deteriorate significantly, impacting their prognosis and QoL (2).
With regard to the Italian national prevalence, the most recent national survey carried out by the Italian Society for Artificial Nutrition and Metabolism shows that the number of recorded cases of HAN was 14,441 (90.3% adult and 9.7% pediatric patients) and the prevalence was 325.5/per million inhabitants. Among the disease categories in adult patients, oncological diseases accounted for 19.4% of the total HAN, neurological diseases 64.8%, gastrointestinal diseases (GI) 6.5%, and other diseases 9.3%. In pediatric patients, the main disease category distribution was GI disease (49.7%) and neurological pathologies (63.4%) (3).
Impaired swallowing can cause increased anxiety and fear: many patients avoid oral intake, leading to malnutrition, isolation, and depression, worsening their QoL. Understanding and balancing the risks and the potential benefits of continuing oral intake without restrictions or choosing to activate the HANU makes this a challenging area of healthcare (4).
In this regard, the importance of speech therapy–related activities such as assessment, intervention for safe swallowing, follow-up, and possible weaning practices of dysphagic patients should be highlighted (5). However, it should be underlined that regarding the presence and intervention of a Speech and Language Pathologist (SLP) in the HANU, scientific literature still struggles to show evidence on speech therapy intervention techniques and their effectiveness on the level of swallowing in the HAN service.
In a home setting, together with a multidisciplinary team, the SLP provides personalized support to the caregiver in acquiring skills, competence, and familiarity with the new indications for AN, especially to facilitate a continuation of oral intake, as appropriate. In fact, many patients need modified diet textures; for example, liquids may need to be thickened and/or foods may need to be pureed to prevent the patient from choking or contracting aspiration pneumonia (6, 7).
The healthcare costs related to dysphagia and its complications are substantial. Several studies have shown that individuals with dysphagia experience longer hospital stays, higher hospital readmission rates, increased mortality within a year of admission, and overall greater utilization of healthcare services (8, 9).
In the Lazio Region, the HANU prescribes water gels and thickeners, supplied by the National Health Service (NHS) (10), for safe hydration. The HANU of Local Health Unit “Roma 3” that covers an area of 605,534 inhabitants handles 1,570 patients. Before the employment of an SLP in the HANU (January 2023), prescriptions were standardized, regardless of the swallowing impairment severity: four jars of thickeners per patient/month and six water gels daily. The Clinical Swallowing Evaluation (CSE) made by the SLP allowed to customize the number of thickeners and water gels based on the actual needs of the patient.
The aim of this study is to investigate the cost savings resulting from the employment of an SLP in the HANU.
Materials and methods
A descriptive retrospective study was conducted analyzing SLP activity in the HANU of Local Health Unit “Roma 3” from January to December 2023.
At first, we analyzed the different characteristics of patients for whom CSE was performed, such as age, sex, and pathologies; then the trend was determined and the total number of requests of SLP assessments in the HANU in 2023 was calculated.
There were no exclusion criteria for the selection of patients, since all patients assessed by a speech therapist through the HANU were included in the study. Therefore, the sample was also completely representative of each patient referred to this service, and it was not a convenience sample. The comparison method was therefore purely descriptive.
The cost of each product (thickeners and water gels) was provided by the Territorial Pharmacy, and from this cost was calculated the annual savings accruing from personalized prescription after SLP assessment.
Results
The study group consisted of 149 patients: 61 males – 41%; 88 females – 59%, with a mean age of 76.2 years (minimum age 31, maximum age 100) with different pathologies.
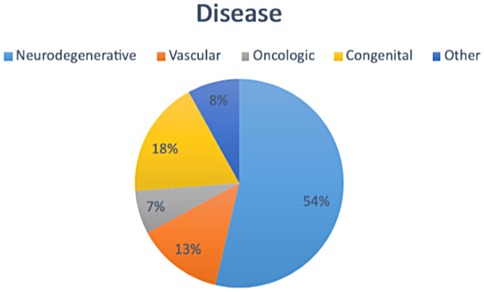
In Figure 1, we report the most common pathologies found in patients evaluated by the SLP. There were neurodegenerative diseases in 54% of them (amyotrophic lateral sclerosis, multiple sclerosis, Alzheimer's, Parkinson's disease and parkinsonism, cognitive impairment), followed by 18% of congenital diseases (PCI, Down Syndrome, and Rett Syndrome); 13% of vascular diseases (ischemic and hemorrhagic stroke); 7% of oncological diseases (head/neck tumors); and 8% of other etiologies (cranioencephalic trauma, respiratory infections, and cardiac pathologies).
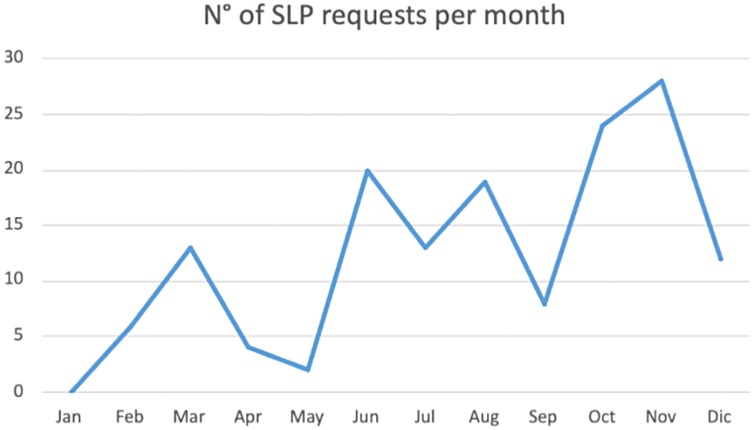
Since January 2023, there has been an increasing trend in requests for SLP assessments with a peak in November 2023, as can be seen in Figure 2.
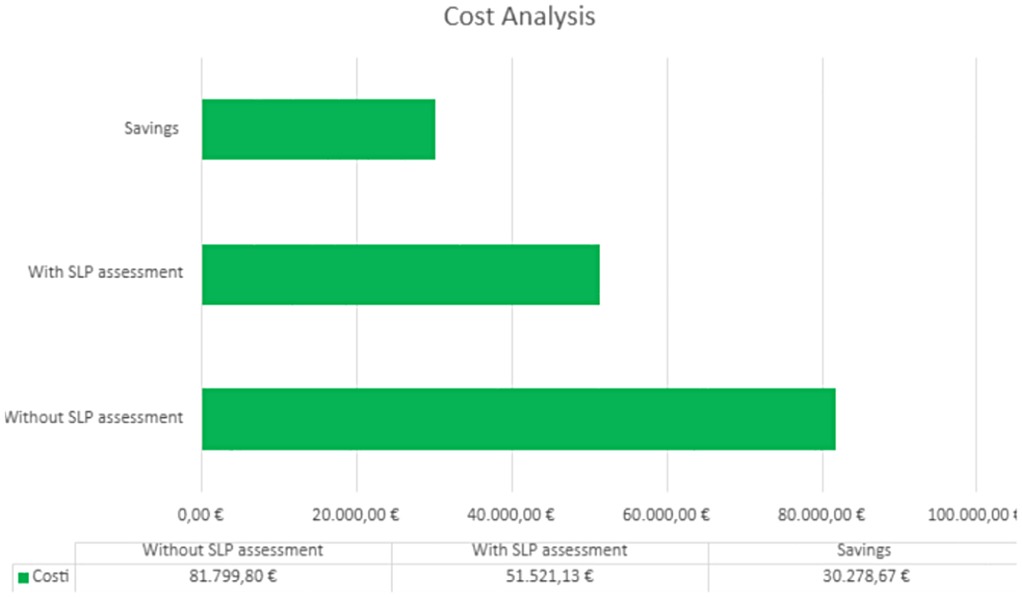
The annual savings were calculated as the difference between the standardized prescription of products (as usual care in our department) and personalized prescription after SLP assessment in the 149 patients who were evaluated. Considering that the cost of the standardized prescription for each patient, before the introduction of the speech therapist in the HANU, was approximately €1221 per month for thickeners and €183 per day for water gels (the cost of each product was provided by the Territorial Pharmacy), from a comparison of these expenses with those actually incurred after speech therapy assessments and related personalized prescriptions, an annual saving of €30,278.67 was recorded (Figure 3).
Discussion
This preliminary study shows how the employment of an SLP in the HANU can reduce inappropriate prescriptions of thickeners and water gels, thus ensuring cost savings.
Before the employment of an SLP in the HANU team, the dosage of thickeners and water gels was standardized for every patient (four jars of thickeners per month, six water gels daily). After the employment of the SLP, the prescription began to be personalized according to the real needs of each patient. The SLP can suggest 0–6 jars of thickeners per month and 0–8 water gels daily. This variability in dosage is due to differences among patients; for instance, some have mixed hydration needs, requiring smaller amounts of these products. In addition, the required quantity of thickening agents varies depending on the severity of dysphagia. In this way, a controlled prescription of thickeners and water gels results in waste reduction and significant economic savings.
Furthermore, since the beginning of this project, there has been a positive trend in requests for SLP assessments. This phenomenon was correlated both to a structured and a constant SLP intervention in a home setting and to an active collaboration with General Practitioners who have shown to be sensitive to the problem of swallowing and responsive to this new service offered.
Finally, there is a cost-effectiveness saving arising from the role of the SLP in preventing dysphagia complications and hospitalization. Patients with mobility impairments receive SLP assessments directly at home. The possibility of receiving treatments directly at home indicates a significant improvement in QoL for both the patient and the caregiver. During dysphagia evaluation, the SLP gives instructions to the patient and the caregiver about correct feeding and hydration methods; this allows the prevention of dysphagia complications; also, the risk of hospitalization for aspiration pneumonia is reduced.
This study has some limitations that need to be considered when interpreting the results. First, the sample size is relatively small (149 patients), although it is representative of the users actually followed by the HANU during the observation period. A larger number of patients could have ensured greater statistical power and generalizability of the results.
A second limitation is the lack of a control group. The study includes only patients with dysphagia who were prescribed thickeners and water gels, making it methodologically irrelevant to establish a comparison group with nondysphagic subjects, to whom these products are not prescribed. As a result, it was not possible to directly compare costs with an untreated population. This limits the possibility of exclusively attributing the observed cost reduction to the intervention of speech therapists, although it suggests a significant role.
Finally, potential confounding factors, such as variations within different local health units in the Lazio region in prescribing patterns, product availability, or clinical practices, must be considered.
Although these aspects may influence economic analysis, detailed public data on regional average costs for thickeners and water gels are not available, which prevents a more in-depth comparative analysis and adjustment for these variables.
Despite these limitations, the results obtained offer useful insights into the possible impact of speech intervention in a HANU setting and open the way for larger, controlled future studies.
Data availability statement
The datasets presented in this article are not readily available because of restrictions. Requests to access the datasets should be directed to Alice Di Battista,YWxpY2UuZGliYXR0aXN0YUBhc2xyb21hMy5pdA==.
Ethics statement
Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients’/participants’ legal guardian/next of kin was not required for participation in this study in accordance with the national legislation and institutional requirements.
Author contributions
AD: Writing – original draft, Writing – review & editing. YD: Writing – original draft, Writing – review & editing. LD: Writing – original draft, Writing – review & editing. CN: Writing – original draft, Writing – review & editing. LG: Writing – review & editing, Supervision. AV: Supervision, Writing – review & editing. AM: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Shen Z, Hou Y, Huerman A, Ma A. Patients with dysphagia: how to supply nutrition through non-tube feeding. Front Nutr. (2022) 9:1060630. doi: 10.3389/fnut.2022.1060630
2. National Collaborating Centre for Acute Care (UK). Nutrition Support for Adults: Oral Nutrition Support, Enteral Tube Feeding and Parenteral Nutrition. London: National Collaborating Centre for Acute Care (UK) (2006).
3. Pironi L, Regional Coordinators of SINPE. Development of home artificial nutrition in Italy over a seven-year period: 2005–2012. BMC Nutr. (2017) 3:6. doi: 10.1186/s40795-016-0118-y
4. Lisiecka D, Kearns Á, Bonass A. A qualitative systematic review of family caregivers’ experiences of artificial nutrition and hydration at home: a meta-ethnography. Int J Lang Commun Disord. (2022) 57(4):717–36. doi: 10.1111/1460-6984.12726
5. Bai AV, Agostini F, Bernetti A, Mangone M, Fidenzi G, D'Urzo R, et al. State of the evidence about rehabilitation interventions in patients with dysphagia. Eur J Phys Rehabil Med. (2021) 57(6):900–11. doi: 10.23736/S1973-9087.21.06716-2
6. Giles M, Barker M, Hayes A. The role of the speech-language pathologist in home care. Home Healthc Nurse. (2014) 32(6):349–53. doi: 10.1097/NHH.0000000000000079
7. Duncan S, Menclova A, Huckabee ML, Cadilhac DA, Ranta A. How much does dysphagia cost? Understanding the additional costs of dysphagia for New Zealand in patients hospitalised with stroke. Neuroepidemiology. (2024) 59(1):1–11. doi: 10.1159/000539133
8. Patel DA, Krishnaswami S, Steger E, Conover E, Vaezi MF, Ciucci MR, et al. Economic and survival burden of dysphagia among inpatients in the United States. Dis Esophagus. (2018) 31(1):1–7. doi: 10.1093/dote/dox131
9. Attrill S, White S, Murray J, Hammond S, Doeltgen S. Impact of oropharyngeal dysphagia on healthcare cost and length of stay in hospital: a systematic review. BMC Health Serv Res. (2018) 18(1):594. doi: 10.1186/s12913-018-3376-3
Keywords: speech language pathologist (SLP), artificial nutrition (AN), home artificial nutrition, thickener, water gel
Citation: Di Battista A, Di Giancaterino Y, Di Palma L, Nunziata C, Gigli L, Vivenzio A and Matano A (2025) Effectiveness and cost savings of employing speech therapists in a home artificial nutrition unit. Front. Rehabil. Sci. 6:1553818. doi: 10.3389/fresc.2025.1553818
Received: 12 February 2025; Accepted: 31 July 2025;
Published: 20 August 2025.
Edited by:
Niccolo Persiani, University of Florence, ItalyReviewed by:
Claudia Oliveira, University of Algarve, PortugalSusana Arranhado, Atlântica University, Portugal
Copyright: © 2025 Di Battista, Di Giancaterino, Di Palma, Nunziata, Gigli, Vivenzio and Matano. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alice Di Battista, YWxpY2UuZGliYXR0aXN0YUBhc2xyb21hMy5pdA==
 Alice Di Battista
Alice Di Battista Ylenia Di Giancaterino
Ylenia Di Giancaterino Lucia Di Palma
Lucia Di Palma Claudia Nunziata
Claudia Nunziata Loredana Gigli3
Loredana Gigli3 Alessandra Matano
Alessandra Matano