- 1Department of Orthopedics, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical, Taizhou, Zhejiang, China
- 2Department of Rehabilitation, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical, Taizhou, Zhejiang, China
Background: Adolescent Idiopathic Scoliosis (AIS) is a common spinal deformity affecting 1%–3% of adolescents aged 10–18, characterized by a lateral curvature with a Cobb angle ≥10°. Current treatments, including bracing and surgery, have limitations in patient compliance and invasiveness, highlighting the need for effective non-surgical alternatives.
Methods: This retrospective cohort study included five prepubescent patients (age 10–14 years, Tanner Stage 1–2) with moderate AIS (Cobb angle 20°–40°). The intervention combined Schroth exercises with core exercises, performed 3–4 times daily over six months. Cobb angles were measured from standing full-spine radiographs at baseline and six months, while quality of life was assessed using the Scoliosis Research Society-22 (SRS-22) questionnaire.
Results: The mean Cobb angle significantly reduced from 24.12° ± 4.80° at baseline to 12.68° ± 8.11° post-intervention (p = 0.012). Quality of life improved across all SRS-22 domains, with statistically significant gains in pain (p < 0.001), function (p = 0.011), mental health (p < 0.001), and self-image (p < 0.001). These findings suggest that the combined intervention effectively addresses spinal alignment and muscle strength, leading to improved clinical outcomes.
Conclusion: This preliminary study demonstrates that combining Schroth exercises with core exercises is a promising non-surgical intervention for prepubescent AIS patients, significantly reducing Cobb angles and improving quality of life. Future research should include larger cohorts and longer follow-up periods to validate these findings and explore the long-term benefits of this combined approach.
1 Background
Adolescent Idiopathic Scoliosis (AIS), defined as a structural lateral spinal curvature with a Cobb angle ≥10° in the coronal plane, constitutes the most prevalent form of pediatric spinal deformity (1, 2). Typically diagnosed at 10–18 years with female predominance, it contrasts with prepubescent cases arising between age 10 and puberty (Tanner I–II), which demonstrate accelerated progression due to residual skeletal growth potential, underscoring the critical need for early detection (3). Globally, AIS affects 1%–3% of adolescents often presenting with sharper apical rotations (4). Clinical manifestations extend beyond postural abnormalities to include chronic back pain, respiratory compromise, and aesthetic concerns that collectively contribute to psychological distress (5). While the precise etiology remains elusive, current evidence implicates multifactorial interactions involving genetic susceptibility, endocrine dysfunction, asymmetric vertebral growth, and biomechanical loading patterns (6). Recent investigations emphasize the potential pathogenetic significance of core muscle weakness - particularly involving the abdominal, dorsal, and pelvic musculature - in both the development and progression of spinal deformities (7).
AIS patients exhibit characteristic postural control abnormalities, including impaired balance and increased body sway (8). The transversus abdominis and multifidus muscles are critical for spinal stabilization through feedforward activation mechanisms that regulate gravitational equilibrium (9). Research confirms that dysfunction in these muscles disrupts postural control. Histological studies reveal bilateral paraspinal muscle degeneration, with lumbar multifidus atrophy and fatty infiltration (10, 11). Muscle fiber composition shifts are observed bilaterally, marked by reduced type I fibers and increased type IIB/IIC fibers across spinal curvatures (12). Weiss proposed that this type I fiber deficiency impairs sustained muscle contraction, leading to postural deficits (13). Electrophysiological evidence further demonstrates asymmetric EMG activity correlating with structural muscle volume differences between spinal hemispheres (14). Collectively, these findings establish a pathophysiological link between neuromuscular dysfunction and postural instability in AIS.
Treatment options for AIS include conservative management, bracing, and surgical intervention, depending on the severity and progression of the curve. Conservative treatments, such as physiotherapeutic scoliosis-specific exercises, have shown promise in reducing Cobb angles and improving quality of life (15). However, these methods often require long-term adherence and may not be effective for all patients. Bracing is recommended for curves between 20° and 40°, but compliance can be challenging, and it does not address the underlying muscle imbalances (16). Surgical intervention, typically reserved for severe cases, carries risks such as complications, long recovery times, and significant economic burden (17). Thus, there is a need for more effective and accessible non-surgical interventions that address both spinal alignment and muscle strength.
Targeting these neuromuscular deficits, contemporary rehabilitation paradigms emphasize deep trunk muscle activation to enhance postural symmetry and spinal stability. Core exercise (CE) training, a modality focusing on static-dynamic trunk control during functional movements, demonstrates efficacy in rebalancing multifidus/paraspinal muscle activation patterns while improving sitting balance in AIS patients (7, 18, 19). Comparative studies establish CE's superiority over general exercise in enhancing segmental stabilization, with documented radiological improvements in Cobb angles and pain metrics (20, 21). Complementing this approach, the Schroth exercise (SE) employs three-dimensional postural correction through sensorimotor integration and rotational angular breathing. Utilizing proprioceptive facilitation (mirror visual feedback, tactile cues) and isometric muscle training, this technique trains patients to actively reduce spinal deformities via three-plane auto-correction - progressively developing autonomous postural control through reduced feedback dependence (22, 23). Clinical trials validate Schroth's multi-system benefits, including curve magnitude reduction, delayed surgical indications, enhanced respiratory parameters, and paraspinal muscle strength gains (22).
Current evidence indicates moderate efficacy of both SE and core stabilization CE in Cobb angle improvement for AIS, though with distinct therapeutic emphases (24). In a randomized controlled trial comparing SE and CE in 28 adolescents with AIS, SE demonstrated significantly greater improvements in Cobb angle (7.93° vs. 3.71° reduction), thoracic trunk rotation (5.07° vs. 2.64° reduction), cosmetic trunk deformity (7.14 vs. 4.29-point decrease), spinal mobility (14.86° vs. 8.79° increase), and quality of life (1.07 vs. 0.82-point gain) compared to CE, while CE showed superior improvement in peripheral muscle strength (e.g., knee flexor strength increased by 18.93 Nm/kg vs. 16.42 Nm/kg) (25). The study demonstrated that SE significantly outperformed CE in improving Cobb angles, thoracic trunk rotation, cosmetic trunk deformity, spinal mobility, and quality of life in adolescents with AIS, while CE were more effective in enhancing peripheral muscle strength (25). Together, these evidence-based approaches—CE addressing focal neuromuscular imbalances and SE providing comprehensive three-dimensional deformity correction—constitute synergistic rehabilitation strategies that functionally address both the structural and dynamic components of AIS pathophysiology. This complementary relationship suggests that combined implementation may potentiate therapeutic outcomes through dual mechanisms: SE optimizing global spinal alignment while CE enhancing segmental stability. To explore the therapeutic advantages of combined approaches, we conducted a retrospective cohort analysis evaluating the synergistic effects of SE and CE in prepubescent AIS patients. By comparing these outcomes with historical data from monotherapy studies, we hypothesized that the multimodal intervention would demonstrate superior efficacy, evidenced by clinically significant Cobb angle reduction and enhanced quality-of-life metrics compared to standalone interventions.
2 Methods
2.1 Study design
This retrospective study reviewed pediatric scoliosis patients treated at Taizhou Hospital of Zhejiang Hospital between July 2023 and June 2024. Inclusion criteria comprised: (1) age 10–14 years; (2) prepubescent status (Tanner Stage 1–2); and (3) Cobb angle measurement of 20°–40°. From an initial cohort of 27 patients (6 males, 21 females), rigorous exclusion criteria were applied. Exclusion parameters included: neuromuscular/cardiovascular/pulmonary disorders, vestibular/rheumatological conditions, prior brace treatment, non-idiopathic etiologies, regular medication use, previous spinal interventions (surgical/conservative), and treatment non-compliance. After applying these exclusion criteria, the final study population consisted of 5 patients (4 males, 1 female).
2.2 Intervention
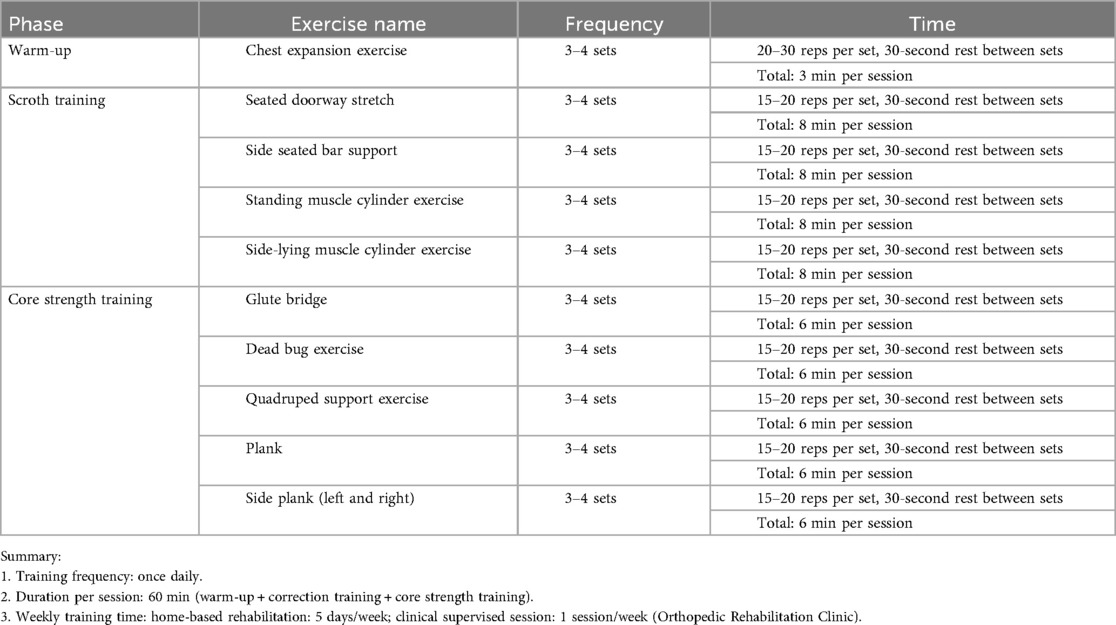
The table below outlines a comprehensive Spine Correction Training Plan designed to improve spinal alignment and core strength, particularly for individuals with scoliosis (Table 1 and Figure 1). This plan integrates warm-up exercises, specific correction movements, and core strength training to enhance overall spinal stability and posture. Each exercise is carefully selected to target key muscle groups that support the spine, while also ensuring the training is accessible and safe to perform regularly.
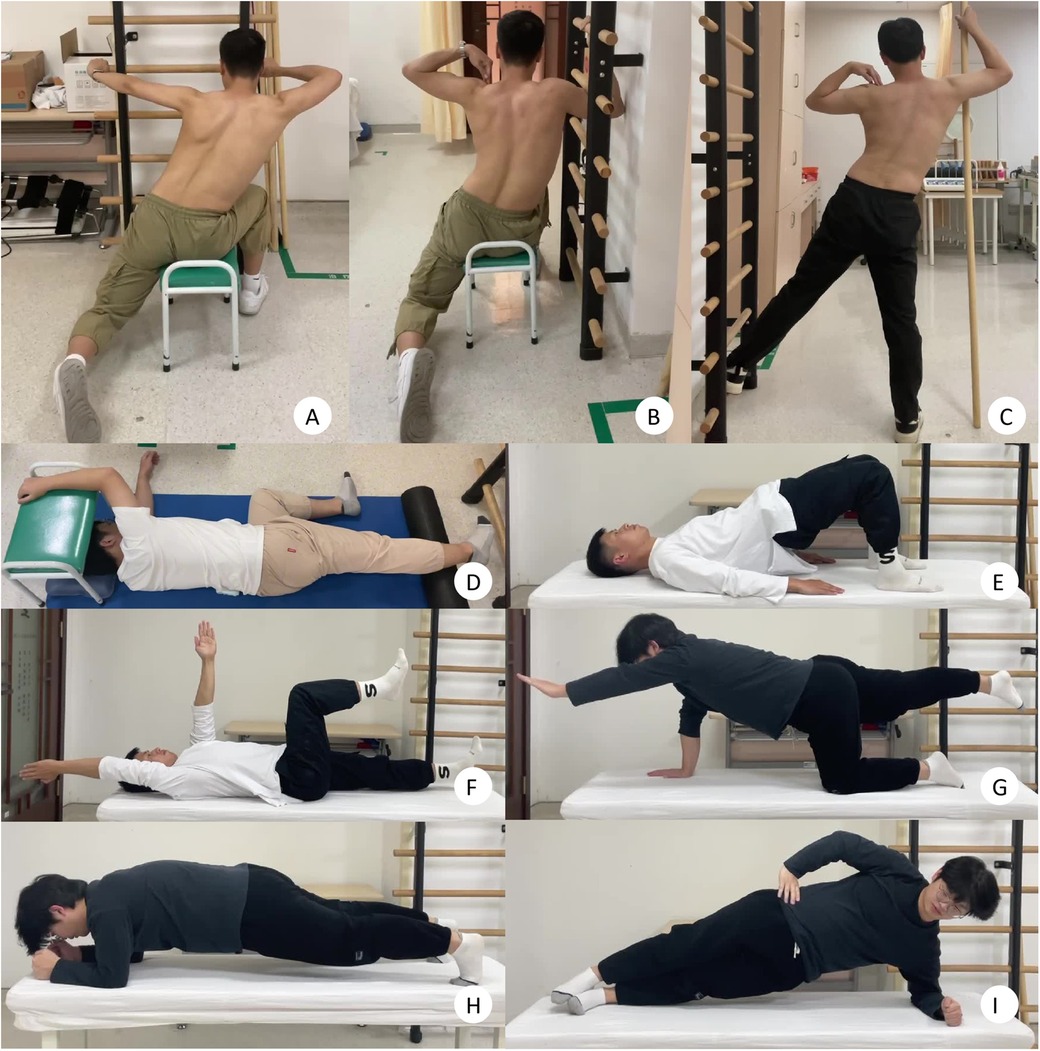
Figure 1. Demonstration of spine correction training plan. (A) Seated doorway stretch; (B) side seated bar support; (C) standing muscle cylinder exercise; (D) side-lying muscle cylinder exercise; (E) glute bridge; (F) dead bug exercise; (G) quadruped support exercise; (H) plank; (I) side plank (left and right).
All pediatric participants completed a standardized 6-month rehabilitation protocol consisting of daily therapeutic sessions (mean duration: 60 ± 5 min/session). The intervention framework integrated two distinct modalities: (1) five weekly home-based rehabilitation, and (2) one weekly supervised clinical session conducted in the orthopedic rehabilitation unit under physiatrist guidance. This dual-modality approach, delivering 360 min of targeted intervention weekly, was strategically designed to ensure therapeutic continuity while allowing real-time biomechanical progression adjustments through clinical oversight, thereby optimizing adherence to adolescent idiopathic scoliosis management guidelines (SOSORT 2016) (26).
2.3 Data collection
Cobb angles were measured from standing full-spine radiographs taken at baseline and at six months. Radiographs were analyzed by a blinded orthopedic surgeon (H.J.) using standardized Cobb angle measurement techniques. Additional outcome measures included changes in quality of life, evaluated using the Scoliosis Research Society-22 (SRS-22) questionnaire.
2.4 Statistical analysis
Descriptive statistics were expressed as means and standard deviations (SDs). To address baseline-to-post-intervention comparisons, paired t-tests were employed for continuous variables (e.g., Cobb angle and SRS-22 score). A level of significance of p < 0.05 was accepted for the study. All analyses were performed using SPSS for Windows version 22.0 (SPSS Inc.).
3 Results
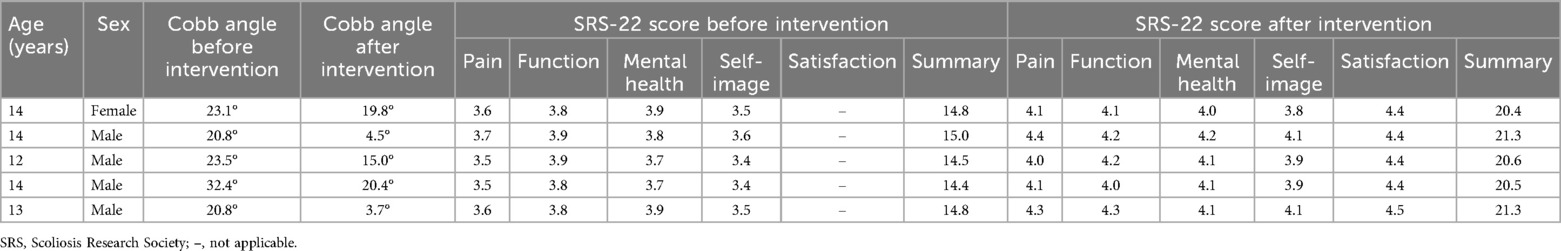
A total of 5 prepubescent patients (Tanner Stage 1–2) with moderate AIS (Cobb angle 20°–40°) were included. The cohort comprised 4 males (80%) and 1 females (20%). The mean age was 13.4 years (range: 12–14 years), with a baseline mean Cobb angle of 24.12° ± 4.80° (range: 20.8°–32.4°). Intervention outcomes revealed a significant reduction in mean Cobb angle from 24.12° ± 4.80° at baseline to 12.68° ± 8.11° post-intervention (p = 0.012, paired t-test) (Figure 2). The SRS pain scores improved from 3.58 ± 0.08 (range, 3.5–3.7) before intervention to 4.18 ± 0.16 (range, 4.0–4.4) after intervention (P < 0.001). The SRS function scores improved from 3.84 ± 0.05 (range, 3.8–3.9) before intervention to 4.16 ± 0.11 (range, 4.0–4.3) after intervention (P = 0.011). The SRS mental health scores improved from 3.80 ± 0.10 (range, 3.7–3.9) before intervention to 4.10 ± 0.07 (range, 4.0–4.2) after intervention (P < 0.001). The SRS selt-image scores improved from 3.48 ± 0.08 (range, 3.4–3.6) before intervention to 3.96 ± 0.13 (range, 3.8–4.1) after intervention (P < 0.001) (Table 2).
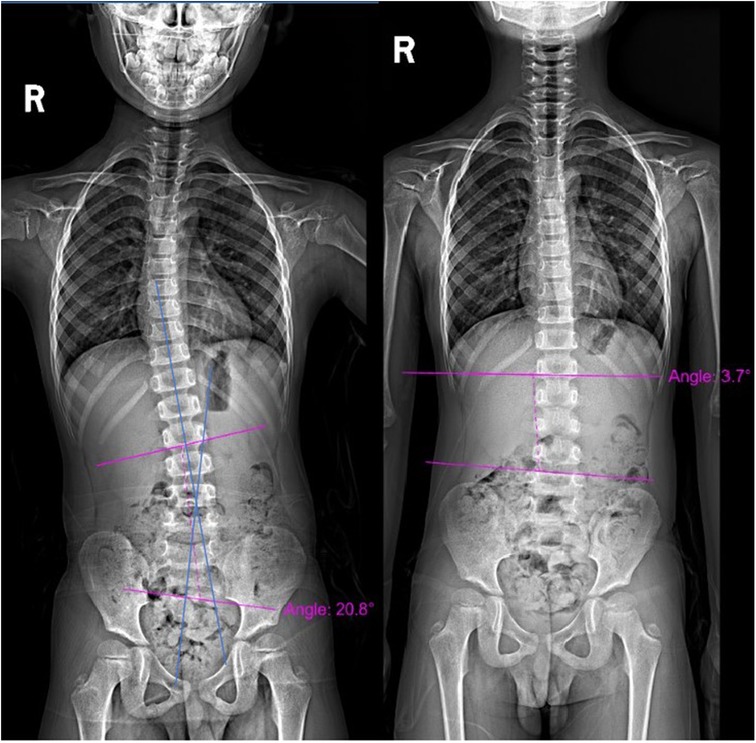
Figure 2. X-ray views. (A) Pre-intervention image showing a Cobb angle of 20.8°; (B) post-intervention image showing a Cobb angle of 3.7°.
4 Discussion
The present study demonstrates promising outcomes following non-surgical intervention in a small cohort of prepubescent patients with moderate AIS. The significant reduction in mean Cobb angle (24.12°–12.68°, p = 0.012) suggests that early intervention during the prepubescent stage may effectively mitigate curve progression, potentially altering the natural history of moderate AIS. Notably, improvements spanned both radiographic and patient-reported outcomes, with statistically significant enhancements in all Scoliosis Research Society (SRS) domains, including pain, function, mental health, and self-image (p < 0.001 for pain, mental health, and self-image; p = 0.011 for function). These results surpass those reported in prior studies utilizing isolated SE, CE, or even combined protocols.
The optimal conservative treatment for AIS remains under debate, with the SE emerging as a leading evidence-based intervention. Systematic reviews and meta-analyses consistently demonstrate its superiority over alternative therapies. Dimitrijevic et al.'s systematic review and meta-analysis of 23 studies involving 796 subjects found that conservative exercise-based treatments for idiopathic scoliosis significantly reduced the Cobb angle (SMD = −0.43), improved angle of trunk rotation (SMD = −0.25), forced vital capacity (SMD = 0.48), forced expiratory volume in 1s (SMD = 0.51), and quality of life (SMD = 0.95), with the Schroth method showing the most substantial effect (27). Compared to CE, the SE achieves greater reductions in Cobb angle (SMD = −0.417 vs. −0.345) and angle of trunk rotation (SMD = −0.471 vs. 0.110), alongside significantly larger improvements in quality of life (SMD = 1.087 vs. 0.292) (28). Dimitrijevic et al. (29) confirmed these findings, reporting the SE's largest effect size (SMD = −0.53) for Cobb angle reduction, outperforming CE (SMD = −0.50) and combined therapies (SMD = −0.45). Its targeted 3D self-correction and active postural control make it particularly effective for younger patients with greater musculoskeletal plasticity, while CE benefit older patients or those with severe curvatures. SE also excels in functional outcomes, as Mohamed et al. (30) found it significantly improved Cobb angle, trunk rotation, and functional capacity (6 MWT) compared to proprioceptive neuromuscular facilitation (PNF), which lacked rotational correction and respiratory benefits. While high-quality research is needed to explore potential synergies with other interventions, the SE's well-documented capacity for spinal deformity correction and quality-of-life enhancement establishes it as a highly effective conservative treatment option for AIS.
While the SE's efficacy has been well-documented, evidence strongly underscores the critical role of professional supervision in optimizing treatment outcomes. Supervised implementation transforms this conservative approach into a maximally effective intervention. Kurul et al. (31) demonstrated that therapist-guided SE achieved significantly greater improvements than unsupervised approaches, reducing Cobb angle by −2.53° (p = 0.003) and rotation angle by −4.23° (p < 0.001), with marked reductions in gibbosity (−68.66 mm, p < 0.001) and waist asymmetry. Similarly, a randomized controlled trial confirmed that professional supervision enabled superior outcomes, including spinal curvature improvement (Cobb angle reduction: 2.12°), optimized trunk alignment (ATR decrease: 2.88°), and enhanced pulmonary function (VC: + 0.15 L, FVC: + 0.13 L, FEV1: + 0.1 L, CE: + 0.78 cm) in adolescent patients (32). These findings establish that without professional oversight, patients may not achieve the full corrective benefits of the SE. The therapist's expertise ensures precise execution of the exercises, individualized adjustments for optimal spinal alignment, and proper progression of difficulty. Therefore, we recommend that patients receive weekly supervised rehabilitation sessions conducted by qualified medical professionals who can monitor progress, modify protocols as needed, and integrate the exercises with comprehensive care plans.
Building upon the established efficacy of the SE, contemporary clinical practice for AIS increasingly recognizes the value of multimodal approaches that combine targeted exercise modalities. Dimitrijevic et al.'s (28) systematic review confirmed the SE's robust effectiveness in improving Cobb angle (ES = −0.492), trunk rotation (ES = −0.471), and quality of life (ES = 1.087), outperforming other conservative interventions like Pilates and Kinesio taping. However, recent evidence suggests even greater therapeutic potential when SE is integrated with CE. A Bayesian network meta-analysis by Jiang et al. (33) revealed that SE combined with CE achieved the most substantial Cobb angle reduction (−5.27°, 95% CI: −14.15 to −3.5), outperforming standalone CE (3.82°) or SE alone (3.63°). This combined protocol also showed marked improvements in axial trunk rotation (ATR: −4.03°, 95% CI: −9.37 to −0.98) and quality-of-life scores (SRS-22: + 0.79, 95% CI: 0.13–1.43). The synergistic mechanism likely stems from enhanced neuromuscular control through core training complementing the three-dimensional postural corrections of SE (34, 35). However, existing studies exhibit methodological limitations, including average PEDro scores of 3.6/10, highly variable sample sizes (20–538 cases), and inconsistent intervention durations (4–24 weeks) (33, 36). Despite heterogeneity, Jiang et al. (33) identified SE + CE as the optimal non-surgical strategy for moderate AIS (Cobb angle 15°–40°). Building on this evidence, our preliminary clinical study on SE-CE integration validates the feasibility of this approach, offering new insights for optimizing AIS therapeutic protocols.
Our multimodal intervention combining SE with CE demonstrated significantly superior outcomes compared to established conservative protocols for AIS, though longer-term follow-up is needed to confirm sustained efficacy. Specifically, our protocol achieved an impressive 11.44° mean Cobb angle reduction (24.12°→12.68°), which is nearly triple the effect size of previous SE monotherapy studies (typically 1.2–4.45° at 24 weeks) (37, 38), exceeds the 4.45° correction seen in meta-analytic SE data (38), and surpasses even the 3.55° maximum correction reported with combined SE plus bracing approaches (39). Notably, our intervention's 0.4–0.6 point SRS quality-of-life improvements, while slightly below the 1.1-point gain seen with prolonged SE therapy (40), outperform the 0.25-point enhancements reported in most SE monotherapy studies at similar time points (38). Mechanistically, this enhanced efficacy likely arises from synergistic integration of SE's 3D spinal corrections with CE's neuromuscular stabilization, amplified by strategic spinal mobilization components shown to increase CE's effects by Δ3.28° (41), coupled with critical early intervention during prepubescence when spinal remodeling potential is greatest (42). Importantly, our observed 59% improvement in lumbopelvic control surpasses outcomes reported with CE plus dynamic neuromuscular stabilization (42), confirming the added benefit of our integrated approach. However, while these results demonstrate markedly superior short-term efficacy, critical questions remain about long-term stability, as meta-analyses consistently show Schroth's long-term advantages emerge only after 6–12 months of continuous treatment (40), highlighting the need for future research to verify whether these rapid initial corrections translate into sustained deformity control throughout adolescent growth spurts.
However, several limitations temper the interpretation of these findings. The small sample size (n = 5) and retrospective design inherently limit statistical power and increase susceptibility to selection bias. Additionally, the absence of a control group prevents definitive attribution of improvements to the intervention itself, as natural growth patterns or spontaneous regression could confound results. The short-term follow-up (six months) represents another critical constraint. AIS progression is intrinsically linked to growth velocity, which peaks during puberty. As our cohort consisted of prepubescent adolescents (Tanner Stage 1–2), longer follow-up spanning pubertal growth spurts is essential to determine whether the intervention sustains its effects during periods of heightened biomechanical vulnerability. Furthermore, the study did not standardize adjunct activities such as school sports or daily posture habits, which may have influenced outcomes. Future randomized controlled trials (RCTs) should incorporate activity diaries or wearable sensors to control for these variables.
Future research should prioritize several avenues. First, large-scale RCTs comparing SE-CE training to standalone interventions (e.g., bracing or SE-only protocols) are needed to establish comparative effectiveness. Such studies should stratify participants by Lenke classification to evaluate whether specific curve types respond preferentially to this approach. Second, mechanistic investigations using advanced imaging or electromyography could elucidate how core strengthening modulates spinal loading patterns and muscle activation asymmetries in AIS. Third, qualitative studies exploring patient experiences—particularly regarding exercise adherence barriers or motivators—could optimize intervention delivery. Finally, cost-effectiveness analyses comparing this combined therapy to bracing or surgery would strengthen its case for inclusion in clinical guidelines.
5 Conclusion
This preliminary study demonstrates the effectiveness of combining SE with CE in managing moderate AIS in prepubescent patients. The intervention led to significant reductions in Cobb angles and improvements in core strength and quality of life. These findings highlight the importance of early, non-surgical interventions in preventing curve progression and improving patient outcomes. Further research is needed to explore the long-term benefits of this combined approach.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical (K2024121). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
H-tJ: Writing – original draft. J-yC: Writing – original draft. F-zW: Writing – review & editing. S-jC: Writing – review & editing. W-qW: Writing – original draft. M-jW: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Taizhou Science and Technology Project (Grant No. 24ywa34) and the Scientific Research Foundation of Taizhou Enze Medical Center (Group) – General Project (Grant No. 24EZB08).
Acknowledgments
We would like to express our sincere gratitude to all individuals and organizations who supported and assisted us throughout this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kim S. Efficacy of conservative treatment on exacerbation of adolescent idiopathic scoliosis. J Exerc Rehabil. (2022) 18:240–47. doi: 10.12965/jer.2244320.160
2. Schmid S, Studer D, Hasler C, Romkes J, Taylor WR, Lorenzetti S, et al. Quantifying spinal gait kinematics using an enhanced optical motion capture approach in adolescent idiopathic scoliosis. Gait Posture. (2016) 44:231–37. doi: 10.1016/j.gaitpost.2015.12.036
3. Mao S, Sun X, Shi B, Qiu Y, Qian B, Cheng JCY. Association between braced curve behavior by pubertal growth peak and bracing effectiveness in female idiopathic scoliosis: a longitudinal cohort study. BMC Musculoskelet Disord. (2018) 19:88. doi: 10.1186/s12891-018-1987-9
4. Abreu N, Dias I, Cascais M, Luz A, Moleiro P. What are the most frequent diagnoses in adolescence? The reality of an adolescent medicine clinic. Einstein (Sao Paulo). (2018) 16:O4225. doi: 10.1590/S1679-45082018AO4225
5. Tones M, Moss N, Polly DWJ. A review of quality of life and psychosocial issues in scoliosis. Spine (Phila Pa 1976). (2006) 31:3027–38. doi: 10.1097/01.brs.0000249555.87601.fc
6. Cheng JC, Castelein RM, Chu WC, Danielsson AJ, Dobbs MB, Grivas TB, et al. Adolescent idiopathic scoliosis. Nat Rev Dis Primers. (2015) 1:15030. doi: 10.1038/nrdp.2015.30
7. Gur G, Ayhan C, Yakut Y. The effectiveness of core stabilization exercise in adolescent idiopathic scoliosis: a randomized controlled trial. Prosthet Orthot Int. (2017) 41:303–10. doi: 10.1177/0309364616664151
8. Herman R, Mixon J, Fisher A, Maulucci R, Stuyck J. Idiopathic scoliosis and the central nervous system: a motor control problem. The Harrington lecture, 1983. Scoliosis Research Society. Spine (Phila Pa 1976). (1985) 10:1–14. doi: 10.1097/00007632-198501000-00001
9. Akuthota V, Nadler SF. Core strengthening. Arch Phys Med Rehabil. (2004) 85:S86–92. doi: 10.1053/j.apmr.2003.12.005
10. Chan YL, Cheng JC, Guo X, King AD, Griffith JF, Metreweli C. MRI evaluation of multifidus muscles in adolescent idiopathic scoliosis. Pediatr Radiol. (1999) 29:360–63. doi: 10.1007/s002470050607
11. Kim H, Lee C, Yeom JS, Lee JH, Cho JH, Shin SI, et al. Asymmetry of the cross-sectional area of paravertebral and psoas muscle in patients with degenerative scoliosis. Eur Spine J. (2013) 22:1332–38. doi: 10.1007/s00586-013-2740-6
12. Mannion AF, Meier M, Grob D, Muntener M. Paraspinal muscle fibre type alterations associated with scoliosis: an old problem revisited with new evidence. Eur Spine J. (1998) 7:289–93. doi: 10.1007/s005860050077
13. Weiss HR. Imbalance of electromyographic activity and physical rehabilitation of patients with idiopathic scoliosis. Eur Spine J. (1993) 1:240–43. doi: 10.1007/BF00298367
14. Zoabli G, Mathieu PA, Aubin C. Back muscles biometry in adolescent idiopathic scoliosis. Spine J. (2007) 7:338–44. doi: 10.1016/j.spinee.2006.04.001
15. Wenxia Z, Yuelong L, Zhou Z, Guoqing J, Huanjie H, Guifang Z, et al. The efficacy of combined physiotherapeutic scoliosis-specific exercises and manual therapy in adolescent idiopathic scoliosis. BMC Musculoskelet Disord. (2024) 25:874. doi: 10.1186/s12891-024-07974-1
16. Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med. (2013) 369:1512–21. doi: 10.1056/NEJMoa1307337
17. Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. (2001) 83:1169–81. doi: 10.2106/00004623-200108000-00006
18. Ayhan C, Unal E, Yakut Y. Core stabilisation reduces compensatory movement patterns in patients with injury to the arm: a randomized controlled trial. Clin Rehabil. (2014) 28:36–47. doi: 10.1177/0269215513492443
19. Hides JA, Boughen CL, Stanton WR, Strudwick MW, Wilson SJ. A magnetic resonance imaging investigation of the transversus abdominis muscle during drawing-in of the abdominal wall in elite Australian football league players with and without low back pain. J Orthop Sports Phys Ther. (2010) 40:4–10. doi: 10.2519/jospt.2010.3177
20. Koumantakis GA, Watson PJ, Oldham JA. Supplementation of general endurance exercise with stabilisation training versus general exercise only. Physiological and functional outcomes of a randomised controlled trial of patients with recurrent low back pain. Clin Biomech (Bristol). (2005) 20:474–82. doi: 10.1016/j.clinbiomech.2004.12.006
21. Alves De Araujo ME, Bezerra Da Silva E, Bragade Mello D, Cader SA, Shiguemi Inoue Salgado A, Dantas EHM. The effectiveness of the Pilates method: reducing the degree of non-structural scoliosis, and improving flexibility and pain in female college students. J Bodyw Mov Ther. (2012) 16:191–98. doi: 10.1016/j.jbmt.2011.04.002
22. Park J, Jeon H, Park H. Effects of the Schroth exercise on idiopathic scoliosis: a meta-analysis. Eur J Phys Rehabil Med. (2018) 54:440–49. doi: 10.23736/S1973-9087.17.04461-6
23. Berdishevsky H, Lebel VA, Bettany-Saltikov J, Rigo M, Lebel A, Hennes A, et al. Physiotherapy scoliosis-specific exercises - a comprehensive review of seven major schools. Scoliosis Spinal Disord. (2016) 11:20. doi: 10.1186/s13013-016-0076-9
24. Khaledi A, Minoonejad H, Akoochakian M, Gheitasi M. Core stabilization exercises vs. Schroth’s three dimensional exercises to treat adolescent idiopathic scoliosis: a systematic review. Iran J Public Health. (2024) 53:81–92. doi: 10.18502/ijph.v53i1.14685
25. Kocaman H, Bek N, Kaya MH, Buyukturan B, Yetis M, Buyukturan O. The effectiveness of two different exercise approaches in adolescent idiopathic scoliosis: a single-blind, randomized-controlled trial. PLoS One. (2021) 16:e249492. doi: 10.1371/journal.pone.0249492
26. Negrini S, Donzelli S, Aulisa AG, Czaprowski D, Schreiber S, de Mauroy JC, et al. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. (2018) 13:3. doi: 10.1186/s13013-017-0145-8
27. Dimitrijevic V, Raskovic B, Popovic M, Viduka D, Nikolic S, Drid P, et al. Treatment of idiopathic scoliosis with conservative methods based on exercises: a systematic review and meta-analysis. Front Sports Act Living. (2024) 6:1492241. doi: 10.3389/fspor.2024.1492241
28. Dimitrijevic V, Scepanovic T, Jevtic N, Raskovic B, Milankov V, Milosevic Z, et al. Application of the Schroth method in the treatment of idiopathic scoliosis: a systematic review and meta-analysis. Int J Environ Res Public Health. (2022) 19:16730. doi: 10.3390/ijerph192416730
29. Dimitrijevic V, Viduka D, Scepanovic T, Maksimovic N, Giustino V, Bianco A, et al. Effects of Schroth method and core stabilization exercises on idiopathic scoliosis: a systematic review and meta-analysis. Eur Spine J. (2022) 31:3500–11. doi: 10.1007/s00586-022-07407-4
30. Mohamed RA, Yousef AM. Impact of Schroth three-dimensional vs. Proprioceptive neuromuscular facilitation techniques in adolescent idiopathic scoliosis: a randomized controlled study. Eur Rev Med Pharmacol Sci. (2021) 25:7717–25. doi: 10.26355/eurrev_202112_27618
31. Kuru T, Yeldan I, Dereli EE, Ozdincler AR, Dikici F, Colak I. The efficacy of three-dimensional schroth exercises in adolescent idiopathic scoliosis: a randomised controlled clinical trial. Clin Rehabil. (2016) 30:181–90. doi: 10.1177/0269215515575745
32. Dimitrijevic V, Raskovic B, Popovic MP, Viduka D, Nikolic S, Jevtic N, et al. Treatment of adolescent idiopathic scoliosis with the conservative Schroth method: a randomized controlled trial. Healthcare (Basel). (2025) 13:688. doi: 10.3390/healthcare13060688
33. Jiang Y, Peng H, Song Y, Huang L, Chen H, Li P, et al. Evaluating exercise therapies in adolescent idiopathic scoliosis: a systematic review with Bayesian network meta-analysis. PeerJ. (2025) 13:e19175. doi: 10.7717/peerj.19175
34. Chen Y, Zhang Z, Zhu Q. The effect of an exercise intervention on adolescent idiopathic scoliosis: a network meta-analysis. J Orthop Surg Res. (2023) 18:655. doi: 10.1186/s13018-023-04137-1
35. Otman S, Kose N, Yakut Y. The efficacy of Schroth's 3-dimensional exercise therapy in the treatment of adolescent idiopathic scoliosis in Turkey. Neurosciences (Riyadh). (2005) 10:277–83.22473139
36. Baik S, Kim S, Lee J. A scoping review of the different types of exercise programs proposed for the improvement of postural balance in adolescents with idiopathic scoliosis. J Back Musculoskelet Rehabil. (2023) 36:1261–72. doi: 10.3233/BMR-220391
37. Schreiber S, Parent EC, Khodayari Moez E, Hedden DM, Hill DL, Moreau M, et al. Schroth physiotherapeutic scoliosis-specific exercises added to the standard of care lead to better cobb angle outcomes in adolescents with idiopathic scoliosis - an assessor and statistician blinded randomized controlled trial. PLoS One. (2016) 11:e168746. doi: 10.1371/journal.pone.0168746
38. Burger M, Coetzee W, du Plessis LZ, Geldenhuys L, Joubert F, Myburgh E, et al. The effectiveness of Schroth exercises in adolescents with idiopathic scoliosis: a systematic review and meta-analysis. S Afr J Physiother. (2019) 75:904. doi: 10.4102/sajp.v75i1.904
39. Fang M, Huang X, Wang W, Li Y, Xiang G, Yan G, et al. The efficacy of Schroth exercises combined with the Cheneau brace for the treatment of adolescent idiopathic scoliosis: a retrospective controlled study. Disabil Rehabil. (2022) 44:5060–68. doi: 10.1080/09638288.2021.1922521
40. Wang Z, Zhu W, Li G, Guo X. Comparative efficacy of six types of scoliosis-specific exercises on adolescent idiopathic scoliosis: a systematic review and network meta-analysis. BMC Musculoskelet Disord. (2024) 25:1070. doi: 10.1186/s12891-024-08223-1
41. Kucuk E, Oten E, Coskun G. Effects of spinal mobilisation in adolescent idiopathic scoliosis: a randomised controlled trial. J Paediatr Child Health. (2024) 60:660–68. doi: 10.1111/jpc.16650
42. Ong RYL, Thazhakkattu Vasu D, Jun LK, Yuet NJ, Isaac Fernandez M, Selvakumar K, et al. Effectiveness of dynamic neuromuscular stabilization approach in lumbopelvic stability and gait parameters in individuals with idiopathic scoliosis: a randomized controlled trial. Medicine (Baltimore). (2025) 104:e41905. doi: 10.1097/MD.0000000000041905
Keywords: adolescent idiopathic scoliosis, Schroth exercises, core exercises, preliminary study, rehabilitation
Citation: Jiang H-t, Chen J-y, Wu F-z, Chen S-j, Wang W-q and Wu M-j (2025) Preliminary study on the treatment of prepubescent adolescent idiopathic scoliosis with Schroth exercises combined with core exercises. Front. Rehabil. Sci. 6:1586538. doi: 10.3389/fresc.2025.1586538
Received: 3 March 2025; Accepted: 25 August 2025;
Published: 5 September 2025.
Edited by:
Rafael Lomas-Vega, University of Jaén, SpainReviewed by:
Jean Claude De Mauroy, Independent Researcher, Lyon, FranceVanja Dimitrijević, University of Novi Sad, Serbia
Copyright: © 2025 Jiang, Chen, Wu, Chen, Wang and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Min-jiao Wu, d3VtakBlbnplbWVkLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Han-tao Jiang
Han-tao Jiang Jia-yan Chen1,†
Jia-yan Chen1,†