Abstract
Objective:
This systematic review and synthesis aimed to describe the frequency and characteristics of knee extensor exercise prescriptions within patellofemoral pain (PFP) interventions and to assess the extent to which key training variables are reported. By doing so, it sought to inform and support more transparent and standardized reporting practices in exercise-based rehabilitation for individuals with PFP.
Method:
This systematic review was conducted following PRISMA guidelines. A literature search was performed in January 2024 across Web of Science, PubMed, Scopus, CINAHL, and SportDiscus. Studies were included if they investigated interventions incorporating knee extensor exercises for PFP.
Results:
Seventy-nine studies met the inclusion criteria. The most commonly prescribed exercises were the straight leg raise, squat, and open-chain knee extension, typically performed as three sets of ten repetitions with bodyweight resistance. However, key training variables such as range of motion and intensity were often inadequately reported, limiting reproducibility and clinical applicability.
Conclusion:
Knee extensor training for PFP predominantly consists of low-load, moderate-volume exercises, differing from conventional strength training recommendations. The lack of detailed reporting on critical variables, such as intensity and range of motion, reduces the clarity and applicability of rehabilitation protocols. Standardized reporting and further research are needed to optimize exercise prescription for PFP management.
Introduction
Patellofemoral pain (PFP) is one of the most common knee disorders in adolescents and younger adults (1, 2). PFP has a prevalence between 8% and 25% depending on the population and is usually twice as common in females (3). Individuals diagnosed with PFP often have activity-induced pain around or inside the kneecap, which limits their participating in physical activities and sports (4). A reduced muscle strength of the knee extensors is often seen in these individuals, but it is discussed whether this is a cause of the disorder or a consequence of it (5, 6). The etiology of PFP is still unknown but has been suggested to be multifactorial. Factors such as patellar maltracking, excessive patellofemoral joint pressure, reduction in muscle strength of the hip and knee extensors and imbalances of activation patterns of the M. Quadriceps seem to cause the problem (1, 7).
Despite the high prevalence of PFP, consensus on the most effective treatment remains limited. Current evidence suggests that exercise therapy targeting the knee, hip, and core muscles may be beneficial (1, 8). Among these, hip and core exercises are frequently used in rehabilitation because they typically avoid directly loading the knee joint and thus pose minimal risk of aggravating symptoms (9). In contrast, prescribing knee extensor training presents a more complex clinical challenge. Quadriceps weakness is a common and clinically significant impairment in individuals with PFP, closely associated with abnormal joint mechanics, movement dysfunction, and persistent pain (5, 6). Strengthening the knee extensors is therefore essential for restoring joint function and improving long-term outcomes. However, because such exercises inherently involve loading the patellofemoral joint, they carry a higher risk of inducing pain, creating a tension between therapeutic necessity and symptom management (1, 7, 8).
Adding to this complexity, the recommended treatment “exercise therapy” can be perceives as a broad and somewhat vague term, requiring practitioners to navigate through a wide range of training variables (10). Within the scope of exercise therapy, various variables can be adjusted, such as type of exercise, range of motion (ROM), training volume (sets and repetitions), and external load (intensity) (11). The manipulation of these factors significantly influences outcomes related to muscle strength gains and hypertrophy (11). However, increased ROM and intensity in patients with PFP appear to negatively affect the risk of pain due to increased forces in the patellofemoral joint (12–15).
While previous systematic reviews have highlighted the benefits of knee extensor strengthening in PFP rehabilitation, indicating that this training may significantly enhance both short- and long-term rehabilitation outcomes (8, 16), there remains limited guidance on how to prescribe these exercises in practice. Specifically, reporting on key training parameters such as intensity, volume, and ROM is often inconsistent or insufficient, making it difficult for clinicians to apply existing evidence with precision. This lack of standardization also limits the ability to compare interventions across studies, replicate effective protocols, or understand common clinical practices. As a result, translating general recommendations into structured, individualized exercise programs can be difficult. More consistent and detailed reporting of exercise prescriptions is needed to support evidence-informed, patient-specific rehabilitation strategies.
Given these challenges, there is a clear need to investigate how knee extensor training is currently utilized and prescribed in the management of PFP. This synthesis aims to describe the characteristics and frequency of knee extensor exercise prescriptions within PFP interventions and to assess the extent to which key training variables are reported. By doing so, it seeks to provide clinicians with clearer insights to inform evidence-aligned decision-making in the management of PFP and support more transparent and standardized reporting in exercise-based rehabilitation.
Methods
Study selection and eligibility criteria
The review was conducted and reported following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and in accordance with the guidelines for implementing PRISMA in Exercise, Rehabilitation, Sport medicine and SporTs science (17, 18). The inclusion criteria were: (a) Full text, original and peer review articles published up to and the date the search was conducted and (b) exercise interventions, both random and non-random as well as controlled and non-controlled, which included training of the knee extensor muscles for treating PFP. Interventions could include other forms of treatment besides knee extensor training.
Exclusion criteria were: (a) article not available in English, (b) interventions that did not include exercises for the knee extensors muscles, (c) intervention with other diagnoses than PFP and (d) if the intervention had not yet been taken place, such as protocol papers.
Search strategy and review process
To find relevant literature an electronic search was initiated and finished in the end of January of 2024 in the following five databases: Web of Science, Pubmed, Scopus, CINAHL and SportDiscus. The following search string (with variation depending on the database) was used: Patellofemoral joint pain OR patellofemoral pain syndrome OR anterior knee pain OR OR plica syndrome AND resistance training OR knee musc* OR knee stren* OR knee exerc* OR knee resis* OR quadriceps resis* OR quadriceps exerc* OR quadriceps stren* OR quadriceps musc*. The entire search with queries in the different databases can be found in Supplementary S1.
The first author (TG) exported all identified studies to the reference manager system Endnote (EndNote, Version EndNote20, Philadelphia, PA) where duplicates were removed. The remaining studies were screened by title and non-relevant were removed (e.g., not exercise intervention, no PFP) by the first author. The abstracts of the remaining studies were then read independently by the three authors to further screen for relevant studies and remove non-relevant studies (e.g., no knee joint exercise, protocols). The relevant studies were then compared and discussed to reach consensus of studies eligible for this systematic review.
Data extraction
Following final selection, the first author independently extracted data by thoroughly reviewing all included articles and entering relevant information into a standardized Excel spreadsheet, which was collaboratively developed by all three authors. The following data items were identified and extracted from the included studies: (a) exercises targeting the knee extensor muscles—defined as any exercise that primarily involves activation of the quadriceps muscle group, including open and closed chain exercises as well as all types of muscle activation (concentric, eccentric, isometric); (b) number of repetitions and sets; (c) exercise intensity, classified as reported in the study (d) ROM during the exercise, if specified; (e) whether and how exercise progression was implemented, with progression recorded only when explicitly reported (e.g., increase in load, sets/reps, or complexity); (f) duration and training frequency of the intervention (e.g., sessions per week and overall intervention length); (g) type of training, categorized by modality (e.g., resistance training, neuromuscular training, functional strengthening); and (h) outcome measures used in each study. All classifications and definitions were applied consistently during data extraction, based on a predefined extraction template developed prior to the review.
Due to the considerable variation in factors such as duration, number of exercises employed, total training volume, and the possible inclusion of additional interventions alongside knee extensor training in the studies, a synthesis of outcome effects such as a meta-analysis was not pursued.
Risk of bias
We evaluated the risk of bias in randomised clinical trials using the Revised Cochrane Risk-of-Bias Tool for Randomised Trials (RoB2) (19). RoB2 assesses bias across five key domains: the randomisation process, deviations from intended interventions, missing outcome data, outcome measurement, and selection of reported results. We categorised studies as having low, some, or high risk of bias: low risk if there was low risk in all five domains, some risk if there was some risk in at least one domain but no high risk in any domain, and high risk if there was high risk in one or more domains.
For non-randomised trials, we used the Risk Of Bias In Non-randomised Studies of Interventions (ROBINS-I) tool, to assess controlled intervention studies (20). ROBINS-I includes a seven-domain checklist to evaluate risk of bias, covering (a) bias due to confounding, (b) bias in participant selection, (c) bias in intervention classification, (d) bias due to deviations from intended interventions, (e) bias due to missing data, (f) bias in outcome measurement, and (g) bias in selection of reported results. Each domain was rated as low, moderate, or serious risk of bias. Studies were summarised as having low risk (low risk across all domains), moderate risk (low or moderate risk in all domains), or serious risk (serious risk in one or more domains).
The three authors independently conducted the RoB2 assessments, while two (TG and HP) independently performed the ROBINS-I assessments. Any grading disagreements were resolved through discussion until a consensus was reached on the final grading.
Statement of equity, diversity and inclusion
All eligible studies were included in the systematic review regardless of participant characteristics such as sex, gender, race/ethnicity, socioeconomic status, or representation from marginalised groups, as these factors were not specified in our data analysis forms. The author group consists of two male and one female researcher, representing a combination of PhD candidate (one author) and senior researchers (two authors), all affiliated with a single academic institution in Sweden. Two authors have clinical backgrounds while one author has experience in exercise science.
Registration
This systematic review has not been registered in PROSPERO because it has not been aimed to report health related outcomes and effects. In this review we aimed only to describe and report only training variables of selected and analysed intervention studies.
Results
A total of 1,609 studies were initially found through the search strategy. After screening and analysis, 79 studies (21–99) were deemed eligible by the inclusion criteria and included in this systematic review. The flow chart of this process can be seen in Figure 1.
Figure 1

PRISMA flow diagram of the screening process.
Exercises for the knee extensors
A total of 240 exercises for the knee muscles were identified in the included studies. The exercises used in the included studies could through naming, illustration, or description of how they were performed, be summarised to a total of 19 different types of exercises. As the majority of studies incorporated multiple exercises for knee extensor training, Table 1 provides a summary of their implementation. This includes the frequency of use for each exercise, and details on the number of repetitions and sets, ROM and training intensity. In summary, the most frequently used exercises were straight leg raises, squats, and open chain knee extension. The most common training structure consisted of three sets of ten repetitions using only body weight, without additional resistance.
Table 1
| Exercise | Used in studies (n) | Number of repetitions: median (min-max) | Number of sets: median (min-max) | ROM: median (min-max)a | Intensity: median (min-max) |
|---|---|---|---|---|---|
| Straight leg raises | 33 | 10 (5–30) | 3 (1–6) | Isometric 0° | BW (BW—75% 1 RM) |
| Squat | 29 | 10 (5–25) | 3 (1–4) | 0–45° (0–90°) | BW (BW—80% 1 RM) |
| Knee extension (sitting) | 28 | 10 (3–30) | 3 (1–6) | 90–45° (90–0°) | 70% 1 RM (BW—80% 1 RM) |
| Terminal knee extension | 26 | 10 (5–55) | 3 (1–5) | 10° (0–30°) | BW (BW—10 RM) |
| Wall squat | 22 | 10 (10–20) | 3 (1–3) | 0–45° (0–90°) | BW (BW—BW + 10%) |
| Step downs | 22 | 20–10 | 3 (1–3) | 20 cm (3,6–25 cm) | BW (BW—BW + 10%) |
| Single leg squat | 17 | 10 (6–20) | 3 (1–3) | 0–90° (0–90°) | BW (BW—70% 1 RM) |
| Quad Set | 15 | 10 (10–15) | 3 (1–3) | Isometric 0° | BW (BW—BW + Resistance band) |
| Leg press | 13 | 10 (7–20) | 3 (2–4) | 0–45° (0–90°) | 70% 1 RM (50%–80% 1 RM) |
| Lunges | 13 | 10 (6–25) | 3 (3–3) | 0–90° (0–90°) | BW (BW—70% 1 RM) |
| Isometric contraction | 10 | 10 (10–10) | 3 (1–3) | 0° (0–90°) | NA |
| Hip thrust | 4 | 10 (6–20) | 3 (2–3) | ? | BW (BW—70% 1 RM) |
| Sit to stand | 2 | 10 (6–20) | 1 (1–1) | 0–90° (0–90°) | BW |
| Cross-ski in water | 1 | 2 min | 2 | ? | NA |
| Frontal kick in the water | 1 | 2 min | 2 | ? | NA |
| Hopping activities | 1 | 2 min | 2 | ? | NA |
| Single leg step jump | 1 | 15–10 | 3 | ? | BW |
| Single leg wall squat | 1 | 60 s | 3 | 0–60° (−) | BW |
| Wingate sprint | 1 | 30 s | 6 | NA | 1 kp |
Descriptives of the knee extensor exercises, including their implementation.
Degrees of knee flexion.
BW, body weight; ?, was not specified; NA, not applicable; 1RM, one repetition maximum; kp, kilopond; ROM, range of motion.
Study characteristics
A total of 296 outcome measures (82 different) were identified in the included studies. To make this data comprehensible, the 82 different outcome measures used were synthesised and categorised into 9 different categories that can be seen in Table 2. The Strength Tests category included outcomes like isometric knee extensor strength and trunk endurance. The Pain Questionnaires category encompassed assessments such as the Anterior Knee Pain Scale (AKPS) and the PFP Severity Scale, whereas the Pain category included measures like the Visual Analog Scale (VAS) and the Numeric Pain Rating Scale. Functional Tests featured performance-based measures, including the single-leg hop and eccentric knee control tests, while Functional Questionnaires involved tools such as the Tegner Activity Scale. The Anatomy Tests category covered outcomes like M. Quadriceps length and muscle thickness, and Movement Analysis included various kinematic measures. The Quality of Life Questionnaire category featured instruments like Short Form Health Survey (SF-36), and the Compliance category included measures of feasibility and adherence.
Table 2
| Type of training (n of the studies) |
Outcomes measures used (n of the studies) |
Progression used (n of the studies) |
Duration: median (min-max) |
Training frequency: median (min-max) |
|||
|---|---|---|---|---|---|---|---|
| Strength training | (41) | Strength tests | (67) | Did not use progression | (52) | 6 weeks (2a–21 weeks) | 3 sessions/week (1 session/week- 2 sessions/day) |
| Exercise therapy | (14) | Pain questionnaire | (63) | Increased intensity | (12) | ||
| Physiotherapy | (9) | Pain | (62) | Used multiple types of progression | (7) | ||
| Conservative treatment | (7) | Functional tests | (45) | Increase volume (sets and reps) | (5) | ||
| Functional stabilisation | (3) | Functional questionnaires | (27) | Increased range of motion | (2) | ||
| Blood flow restriction | (1) | Anatomy tests | (17) | Progression of exercises | (1) | ||
| Low load resistance | (1) | Movement analysis | (6) | ||||
| McConnel regime | (1) | Quality of life questionnaire | (5) | ||||
| Neurofeedback | (1) | Compliance | (4) | ||||
| Task specific | (1) | ||||||
Descriptive characteristics of exercise protocol and outcomes the studies.
1 study was cross sectional for 1 session.
The authors categorised the types of training as described in the various interventions into ten distinct categories, with strength training being the most prevalent used in 41 of the 79 included studies. Additionally, method by which progression was implemented, the duration of the interventions, and the training frequency are presented in Table 2. A full description of the included studies regarding title, author, year, population, country, results, and setting can be found in Supplementary S2.
Completeness of description
Out of the 79 included studies, 25 provided comprehensive information on the data items investigated in this research. Details of the number of studies that specified the exercises used and whether they included descriptions of training progression are presented in Figure 2. Additionally, the figure indicates whether the ROM, number of repetitions and sets, and the load used were described for the total of 240 exercises extracted from the studies.
Figure 2
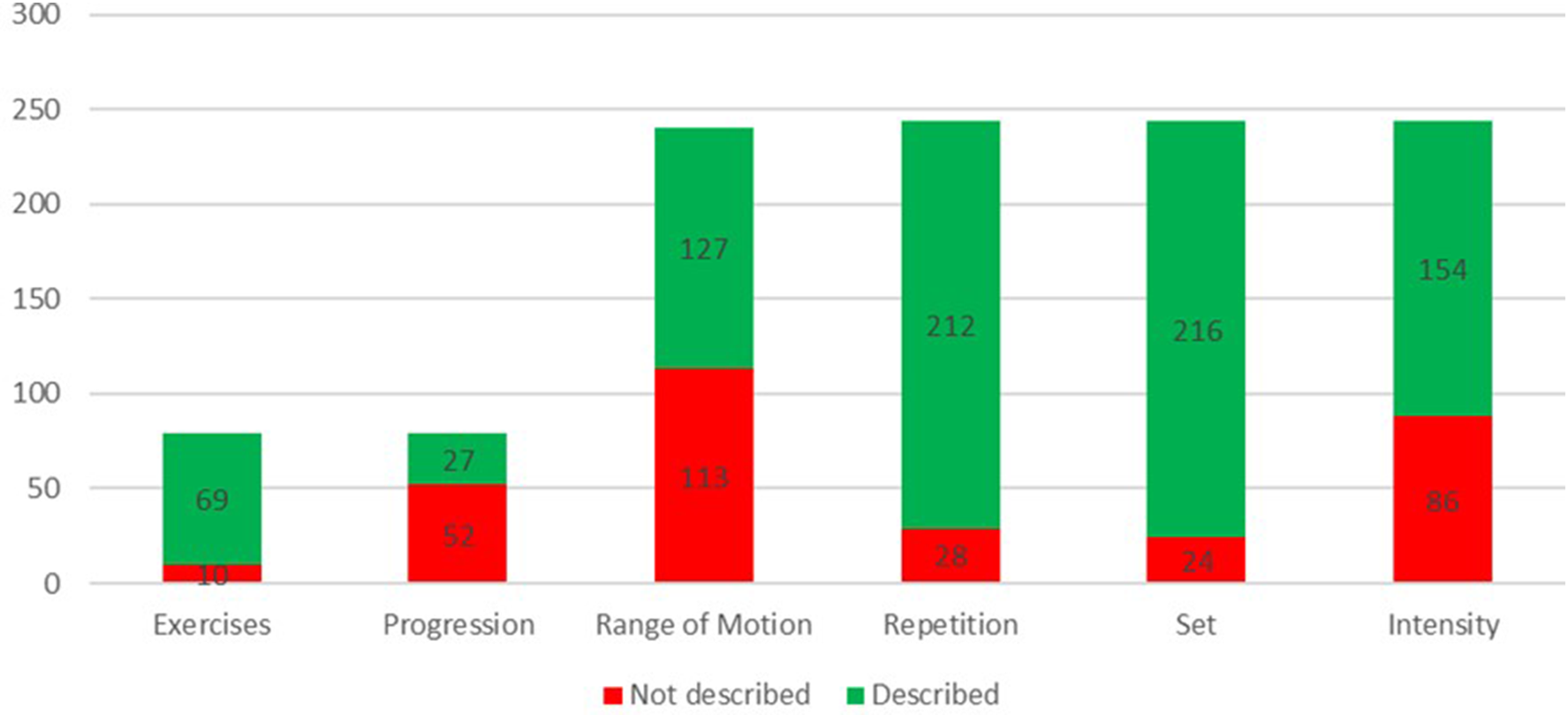
Reporting of exercise and training variables across studies.
Risk of bias
Out of the 79 included studies 61 where randomised controlled trials (RCT) and 18 were non-randomised. Of the 61 RCT assessed in regard of risk of bias, 28 exhibited some concerns while 33 raised high risk regarding potential bias. The overall risk of bias was largely consistent across the studies, with high risk primarily stemming from how outcomes were measured. In training interventions, when participants evaluate their own outcomes without blinding, it typically results in a high-risk rating in this area. Additionally, 30 of the 61 studies failed to clearly outline their randomisation process, and only 15 of the 61 had a preregistered study protocol in a clinical trial registry.
All 18 non-randomised studies included in this review had serious concerns regarding bias. When participants assessed outcomes, such as pain of function, without being blinded, it constituted a serious risk of bias in the measurement of outcomes domain. If this factor were not considered, 7 out of the 18 studies would still be classified as having a serious risk of bias, primarily due to confounding issues (5 out of 18).
A complete documentation of the Rob2 and ROBINS-I assessment can be found as Supplementary S3, S4.
Discussion
The key findings from this study are: (1) the most common training regimen for knee extensor training involves the exercises straight leg raise, squat, and open chain knee extension, typically performed in three sets of ten repetitions using body weight as resistance, and (2) higher reporting standards for training interventions to improve clarity and applicability of training interventions to clinical practice are warranted. Despite limited descriptions of exercise execution, these findings can still provide clinicians with valuable guidance when prescribing knee extensor training for patients with PFP.
Outcomes
The included studies utilised a total of 82 different outcomes. The most frequently used were VAS, AKPS, and knee extensor strength, appearing 54, 43, and 31 times, respectively. However, among the 82 different outcomes used in the included studies, the majority were only utilised once. This wide variation in outcomes poses a challenge for comparing and synthesizing results across studies, limiting the ability to draw clear conclusions and assess the effectiveness of interventions for PFP. Standardising outcomes ensures that the interventions effectively target and improve the intended qualities, and secondly, enables future meta-analyses and synthesis studies to accurately compare outcomes across different intervention studies (100).
Strength training
The majority of the studies included in this review described their intervention as “strength training”. According to the American College of Sports Medicine, recommended strength training should be performed such as 8–12 repetitions, 2–4 sets with a resistance equivalent of 70%–100% of one repetition maximum (1RM) (101). An alternative to training at or above 70% of 1RM is to train close to muscular failure on lower loads, which also seems to positively affects strength (102). Most included studies used a training regime where the exercises were performed within this range regarding repetitions and sets. However, the intensity used in the different exercises, in relation to the number of repetitions performed, does not reflect the recommended training regime aimed to improve strength (101). If the purpose of the “strength training” interventions was to increase the strength of the participants, another training regime might be more suitable, where the load stands in relation to the given repetition and set scheme. When high-intensity training with fewer repetitions is not feasible, low-intensity training should include a sufficiently high number of repetitions to induce muscular fatigue, which is essential for stimulating strength adaptations (103).
Although the progression of training variables has a critical role in improving physical abilities (104), most of the included studies lacked or did not describe if a progression was used in the intervention. The ACSM emphasizes the importance of progressive overload to elicit continued strength gains (101). Without sufficient load and progression, the physiological stimulus required for strength development is likely inadequate. As such, several interventions labeled as “strength training” in the included studies may be more accurately described as low-intensity muscle activation or general exercise routines. This cautious approach, likely aimed at minimizing the risk of pain exacerbation, often resulted in conservative training volumes and intensities. However, if the goal is to improve strength while managing pain risk, the use of individualized progression or periodized loading models could offer a more effective and safer alternative. Gradual increases in training load allow for strength gains while potentially maintaining tolerability in populations with pain or physical limitations (105).
Range of motion
ROM was the least reported training variable in this systematic review, despite its crucial role in muscle development and strength gains through enhanced muscle activation, mechanical tension, and stretch stimulus (106, 107). Furthermore, none of the included studies utilised a ROM greater than 90 degrees of knee flexion. This limitation was likely influenced by recommendations suggesting that PFP patients may benefit from limiting knee flexion to 45–60 degrees during closed-chain exercises to minimise patellofemoral joint forces and, consequently, reduce pain (12, 14, 15). These guidelines, however, are primarily based on biomechanical research conducted in healthy populations, leaving a gap in understanding the specific impact of larger ROM on patellofemoral joint stress among PFP patients. Further investigation is needed to establish whether the increased patellofemoral joint forces associated with higher ROM could have adverse effects on this population, emphasising the importance of evidence-based ROM guidelines that directly pertain to individuals with PFP.
Limited reporting
This systematic review included 79 articles that evaluated the effectiveness of rehabilitation protocols for PFP, specifically through interventions involving knee extensor strengthening exercises. The results indicate that the exercise regimes were generally reported inadequately, lacking the necessary details for accurate replication in future studies. This finding is in accordance with Holden et al. in 2018 (10) and Yamato et al. (108) in 2016 which found that the exercise regimes used in interventions are often poorly reported. Only 25 out of 79 studies included in this review had a complete description of the training variables in their intervention. This limited reporting restricts the ability to provide thorough recommendations and treatment guidelines for practitioners. Enhanced transparency in reporting would enable more effective replication of successful protocols and facilitate the development of standardised treatment guidelines (109).
Risk of bias
More than half of the 61 randomized controlled trials were rated as high risk of bias, primarily due to unblinded outcome assessment and poorly described randomisation methods, issues particularly relevant in studies relying on self-reported measures like pain and function. However, this review was designed as a descriptive analysis of exercise characteristics, not as an evaluation of intervention effectiveness. As such, while risk of bias affects the internal validity of individual studies, its impact on our primary aim—summarizing how knee extensor training has been implemented—is likely limited. Nevertheless, the consistent presence of bias underscores the need for higher-quality, transparently reported trials in this area.
Study designs
This systematic review was aimed to summarise and describe the utilisation of knee extensor exercises within training interventions for PFP, and to do so comprehensively, we included both randomised and non-randomised studies. This inclusive approach allowed us to capture a broader spectrum of interventions, often incorporating additional treatments alongside knee extensor exercises, thereby providing a more complete picture of the current research landscape. However, because of the variability in study designs and the diversity of interventions included, it was impossible to quantitatively assess the separate effects of knee extensor exercises alone. Consequently, this review does not determine the comparative efficacy of different knee extensor exercises. Instead, it offers clinicians an overview of standard practices in knee extensor exercise prescriptions, which may inform and support clinical decision-making.
Moving forward
Given that factors such as training volume, load, and ROM play a crucial role in promoting muscle hypertrophy and strength (102–104, 110), these variables should be carefully considered when designing training interventions, and detailed in research articles to improve the quality of patient treatment. To address these issues, future research should prioritize standardized reporting of exercise protocols, including clear definitions of exercise type and training parameters. Using structured frameworks and explicitly detailing prescription decisions can enhance transparency, improve study quality, and support more evidence-aligned clinical decision-making. Ultimately, better reporting will help bridge the gap between research and practice, enabling more tailored and informed rehabilitation strategies for individuals with PFP.
Strengths and limitations
This is the first study of its kind to systematically describe which exercises and training variables researchers prescribed for the knee joint muscles as treatment for PFP. From these results, practitioners can find some support in which exercises, training volume, load, and ROM to use in treating of patients with PFP. However, some limitations in the present study need to be acknowledged. First, the findings of this study are limited to being descriptive in nature. They provide information on the exercises used and how they have been applied to treat patients with PFP. Consequently, since the effect sizes of the included studies and exercises have not been investigated, no conclusions can be drawn about whether one exercise or method of prescribing an exercise is superior to another. However, assessing effect sizes was beyond the intended aim of this research.
Secondly, even though the authors of this study have experience as clinicians and researchers and the expertise of librarians was used to find correct search terms and construct a search string, relevant studies might have been missed in the search for literature. Extensive efforts were made to ensure the search was as comprehensive as possible by systematically incorporating keywords, concepts, and terminology identified in prior studies and related reviews, but some relevant literature may still have been overlooked.
Thirdly, the initial screening and exclusion of studies by title was conducted solely by the first author, which may introduce a risk of selection bias. However, in cases where there was any uncertainty regarding a study's relevance, it was retained for further evaluation. Additionally, all abstracts were independently reviewed by all three authors to further assess relevance and remove non-eligible studies. This collaborative process likely mitigated the risk of bias and improved the reliability of study selection.
Conclusion
In conclusion, this systematic review highlights common exercise regimes prescribed for PFP, primarily involving knee extensor exercises like straight leg raise, squat, and open-chain knee extension. However, key training variables, especially intensity and ROM, are insufficiently addressed, despite their importance for strength development and PFP-related pain. Enhancing transparency in reporting training variables would support more effective, evidence-based interventions and the development of standardised treatment guidelines for PFP. Furthermore, a notable discrepancy exists between the described interventions as strength training and the recommended load and volume parameters for optimal strength development. Despite these limitations, this review offers a clinically relevant overview of how knee extensor training is currently being implemented for PFP. While practitioners should be cautious about drawing conclusions regarding efficacy, the compiled data may still inform exercise selection and structuring decisions in clinical practice.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
TG: Visualization, Data curation, Formal analysis, Methodology, Writing – review & editing, Conceptualization, Writing – original draft. HP: Data curation, Writing – original draft, Investigation, Supervision, Writing – review & editing, Methodology. SA: Data curation, Methodology, Writing – review & editing, Writing – original draft, Investigation, Supervision.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fresc.2025.1641054/full#supplementary-material
References
1.
Crossley KM Stefanik JJ Selfe J Collins NJ Davis IS Powers CM et al 2016 patellofemoral pain consensus statement from the 4th international patellofemoral pain research retreat, Manchester. Part 1: terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med. (2016) 50(14):839–43. 10.1136/bjsports-2016-096384
2.
Willy RW Hoglund LT Barton CJ Bolgla LA Scalzitti DA Logerstedt DS et al Patellofemoral pain. J Orthop Sports Phys Ther. (2019) 49(9):Cpg1–cpg95. 10.2519/jospt.2019.0302
3.
Smith BE Selfe J Thacker D Hendrick P Bateman M Moffatt F et al Incidence and prevalence of patellofemoral pain: a systematic review and meta-analysis. PLoS One. (2018) 13(1):e0190892. 10.1371/journal.pone.0190892
4.
Rathleff MS Rathleff CR Olesen JL Rasmussen S Roos EM . Is knee pain during adolescence a self-limiting condition?: prognosis of patellofemoral pain and other types of knee pain. Am J Sports Med. (2016) 44(5):1165–71. 10.1177/0363546515622456
5.
Rathleff MS Rathleff CR Crossley KM Barton CJ . Is hip strength a risk factor for patellofemoral pain? A systematic review and meta-analysis. Br J Sports Med. (2014) 48(14):1088. 10.1136/bjsports-2013-093305
6.
Duffey MJ Martin DF Cannon DW Craven T Messier SP . Etiologic factors associated with anterior knee pain in distance runners. Med Sci Sports Exerc. (2000) 32(11):1825–32.
7.
Neal BS Lack SD Lankhorst NE Raye A Morrissey D van Middelkoop M . Risk factors for patellofemoral pain: a systematic review and meta-analysis. Br J Sports Med. (2019) 53(5):270–81. 10.1136/bjsports-2017-098890
8.
van der Heijden RA Lankhorst NE van Linschoten R Bierma-Zeinstra SM van Middelkoop M . Exercise for treating patellofemoral pain syndrome. Cochrane Database Syst Rev. (2015) 1:Cd010387. 10.1002/14651858.CD010387.pub2
9.
Pereira PM Baptista JS Conceição F Duarte J Ferraz J Costa JT . Patellofemoral pain syndrome risk associated with squats: a systematic review. Int J Environ Res Public Health. (2022) 19(15):9241. 10.3390/ijerph19159241
10.
Holden S Rathleff MS Jensen MB Barton CJ . How can we implement exercise therapy for patellofemoral pain if we don't know what was prescribed? A systematic review. Br J Sports Med. (2018) 52(6):385. 10.1136/bjsports-2017-097547
11.
Kraemer WJ Ratamess NA . Fundamentals of resistance training: progression and exercise prescription. Med Sci Sports Exerc. (2004) 36(4):674–88. 10.1249/01.MSS.0000121945.36635.61
12.
Hart HF Patterson BE Crossley KM Culvenor AG Khan MCM King MG et al May the force be with you: understanding how patellofemoral joint reaction force compares across different activities and physical interventions-a systematic review and meta-analysis. Br J Sports Med. (2022) 56(9):521–30. 10.1136/bjsports-2021-104686
13.
Wallace DA Salem GJ Salinas R Powers CM . Patellofemoral joint kinetics while squatting with and without an external load. J Orthop Sports Phys Ther. (2002) 32(4):141–8. 10.2519/jospt.2002.32.4.141
14.
Escamilla RF Zheng NQ Macleod TD Imamura R Wilk KE Wang SC et al Patellofemoral joint loading during the performance of the wall squat and ball squat with heel-to-wall-distance variations. Med Sci Sports Exerc. (2023) 55(9):1592–600. 10.1249/MSS.0000000000003185
15.
Powers CM Ho KY Chen YJ Souza RB Farrokhi S . Patellofemoral joint stress during weight-bearing and non-weight-bearing quadriceps exercises. J Orthop Sports Phys Ther. (2014) 44(5):320–7. 10.2519/jospt.2014.4936
16.
Kooiker L Van De Port IG Weir A Moen MH . Effects of physical therapist-guided quadriceps-strengthening exercises for the treatment of patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther. (2014) 44(6):391–402. 10.2519/jospt.2014.4127
17.
Page MJ McKenzie JE Bossuyt PM Boutron I Hoffmann TC Mulrow CD et al The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. 10.1136/bmj.n71
18.
Ardern CL Büttner F Andrade R Weir A Ashe MC Holden S et al Implementing the 27 PRISMA 2020 statement items for systematic reviews in the sport and exercise medicine, musculoskeletal rehabilitation and sports science fields: the PERSiST (implementing prisma in exercise, rehabilitation, sport medicine and sports science) guidance. Br J Sports Med. (2022) 56(4):175–95. 10.1136/bjsports-2021-103987
19.
Sterne JAC Savović J Page MJ Elbers RG Blencowe NS Boutron I et al Rob 2: a revised tool for assessing risk of bias in randomised trials. Br Med J. (2019) 366:l4898. 10.1136/bmj.l4898
20.
Sterne JAC Hernán MA Reeves BC Savović J Berkman ND Viswanathan M et al ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Br Med J. (2016) 355:i4919. 10.1136/bmj.i4919
21.
Herrington L Al-Sherhi A . A controlled trial of weight-bearing versus non-weight-bearing exercises for patellofemoral pain. J Orthop Sports Phys Ther. (2007) 37(4):155–60. 10.2519/jospt.2007.2433
22.
Salsich GB Yemm B Steger-May K Lang CE Van Dillen LR . A feasibility study of a novel, task-specific movement training intervention for women with patellofemoral pain. Clin Rehabil. (2018) 32(2):179–90. 10.1177/0269215517723055
23.
Barton CJ de Oliveira Silva D Patterson BE Crossley KM Pizzari T Nunes GS . A proximal progressive resistance training program targeting strength and power is feasible in people with patellofemoral pain. Phys Ther Sport. (2019) 38:59–65. 10.1016/j.ptsp.2019.04.010
24.
Silva NC Silva MC Tamburús NY Guimarães MG Nascimento MBO Felicio LR . Adding neuromuscular training to a strengthening program did not produce additional improvement in clinical or kinematic outcomes in women with patellofemoral pain: a blinded randomised controlled trial. Musculoskelet Sci Pract. (2023) 63:102720. 10.1016/j.msksp.2023.102720
25.
Halabchi F Mazaheri R Mansournia MA Hamedi Z . Additional effects of an individualized risk factor-based approach on pain and the function of patients with patellofemoral pain syndrome: a randomized controlled trial. Clin J Sport Med. (2015) 25(6):478–86. 10.1097/JSM.0000000000000177
26.
Kannus P Natri A Paakkala T Järvinen M . An outcome study of chronic patellofemoral pain syndrome: seven-year follow-up of patients in a randomized, controlled trial. J Bone Joint Surg Am. (1999) 81(3):355–63. 10.2106/00004623-199903000-00007
27.
Roush MB Sevier TL Wilson JK Jenkinson DM Helfst RH Gehlsen GM et al Anterior knee pain: a clinical comparison of rehabilitation methods. Clin J Sport Med. (2000) 10(1):22–8. 10.1097/00042752-200001000-00005
28.
Almeida GPL Rodrigues H Coelho BAL Rodrigues CAS Lima POP . Anteromedial versus posterolateral hip musculature strengthening with dose-controlled in women with patellofemoral pain: a randomized controlled trial. Phys Ther Sport. (2021) 49:149–56. 10.1016/j.ptsp.2021.02.016
29.
Yip SLM Ng GYF . Biofeedback supplementation to physiotherapy exercise programme for rehabilitation of patellofemoral pain syndrome: a randomized controlled pilot study. Clin Rehabil. (2006) 20(12):1050–7. 10.1177/0269215506071259
30.
Hamada HA Draz AH Koura GM Saab IM . Carryover effect of hip and knee exercises program on functional performance in individuals with patellofemoral pain syndrome. J Phys Ther Sci. (2017) 29(8):1341–7. 10.1589/jpts.29.1341
31.
Ismail MM Gamaleldein MH Hassa KA . Closed kinetic chain exercises with or without additional hip strengthening exercises in management of patellofemoral pain syndrome: a randomized controlled trial. Eur J Phys Rehabil Med. (2013) 49(5):687–98.
32.
Constantinou A Mamais I Papathanasiou G Lamnisos D Stasinopoulos D . Comparing hip and knee focused exercises versus hip and knee focused exercises with the use of blood flow restriction training in adults with patellofemoral pain. Eur J Phys Rehabil Med. (2022) 58(2):225–35. 10.23736/S1973-9087.22.06691-6
33.
Verma C Krishnan V . Comparison between mc connell patellar taping and conventional physiotherapy treatment in the management of patellofemoral pain syndrome - A randomised controlled trial. J Krishna Inst Med Sci Univ. (2012) 1(2):95–104.
34.
Razeghi M Etemadi Y Taghizadeh S Ghaem H . Could hip and knee muscle strengthening alter the pain intensity in patellofemoral pain syndrome?Iran Red Crescent Med J. (2010) 12(2):104–10.
35.
Syme G Rowe P Martin D Daly G . Disability in patients with chronic patellofemoral pain syndrome: a randomised controlled trial of VMO selective training versus general quadriceps strengthening. Man Ther. (2009) 14(3):252–63. 10.1016/j.math.2008.02.007
36.
Lee JH Rhim HC Jang KM . Effect of adding kinesio taping to exercise therapy in the treatment of patellofemoral pain syndrome. Medicina (Lithuania). (2023) 59(4). 10.3390/medicina59040754
37.
Eapen C Nayak CD Pazhyaottyil Zulfeequer C . Effect of eccentric isotonic quadriceps muscle exercises on patellofemoral pain syndrome: an exploratory pilot study. Asian J Sports Med. (2011) 2(4):227–34. 10.5812/asjsm.34747
38.
Liu Y Wu L . Effect of instrument-assisted soft tissue mobilization combined with blood flow restriction training on function, pain and strength of patients with patellofemoral joint pain. BMC Musculoskelet Disord. (2023) 24(1). 10.1186/s12891-023-06701-6
39.
Kannus P Natri A Niittymaki S Jarvinen M . Effect of intraarticular glycosaminoglycan polysulfate treatment on patellofemoral pain syndrome - a prospective, randomized double-blind trial comparing glycosaminoglycan polysulfate with placebo and quadriceps muscle exercises. Arthritis Rheum. (1992) 35(9):1053–61. 10.1002/art.1780350910
40.
Villafañe JH Bissolotti L La Touche R Pedersini P Negrini S . Effect of muscle strengthening on perceived pain and static knee angles in young subjects with patellofemoral pain syndrome. J Exerc Rehabil. (2019) 15(3):454–9. 10.12965/jer.1938224.112
41.
Naidu SK Kage V . Effect of weight and non-weight bearing quadriceps exercises versus weight-bearing quadriceps exercises on patellofemoral pain, quadriceps strength and functional ability: a randomized clinical trial. Int J Med Res Health Sci. (2018) 7(3):35–9.
42.
Hott A Brox JI Pripp AH Juel NG Paulsen G Liavaag S . Effectiveness of isolated hip exercise, knee exercise, or free physical activity for patellofemoral pain: a randomized controlled trial. Am J Sports Med. (2019) 47(6):1312–22. 10.1177/0363546519830644
43.
Peeler J Anderson JE . Effectiveness of static quadriceps stretching in individuals with patellofemoral joint pain. Clin J Sport Med. (2007) 17(4):234–41. 10.1097/JSM.0b013e3180f60afc
44.
Albornoz-Cabello M Barrios-Quinta CJ Barrios-Quinta AM Escobio-Prieto I de los Angeles Cardero-Durán M Espejo-Antunez L . Effectiveness of tele-prescription of therapeutic physical exercise in patellofemoral pain syndrome during the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18(3):1–11. 10.3390/ijerph18031048
45.
De Marche Baldon R Serrão FV Silva RS Piva SR . Effects of functional stabilization training on pain, function, and lower extremity biomechanics in women with patellofemoral pain: a randomized clinical trial. J Orthop Sports Phys Ther. (2014) 44(4):240–51. 10.2519/jospt.2014.4940
46.
Fang B Kim YH Choi MY . Effects of high-intensity aquatic or bicycling training in athletes with unilateral patellofemoral pain syndrome. Int J Environ Res Public Health. (2022) 19(8). 10.3390/ijerph19084675
47.
Ali L Hafeez S Hafeez Z Riaz S Khan RR Khalid H . Effects of hip and hip core muscles strengthening versus knee muscle strengthening for the management of anterior knee pain. Pak J Med Health Sci. (2021) 15(2):539–41.
48.
Begum R Tassadaq N Ahmad S Qazi WA Javed S Murad S . Effects of McConnell taping combined with strengthening exercises of vastus medialis oblique in females with patellofemoral pain syndrome. J Pak Med Assoc. (2020) 70(4):728–30. 10.5455/JPMA.28469
49.
Albornoz-Cabello M Ibáñez-Vera AJ Barrios-Quinta CJ Lara-Palomo IC Cardero-Durán M Espejo-Antúnez L . Effects of radiofrequency diathermy plus therapeutic exercises on pain and functionality of patients with patellofemoral pain syndrome: a randomized controlled trial. J Clin Med. (2023) 12(6). 10.3390/jcm12062348
50.
Lee JH Jang KM Kim E Rhim HC Kim HD . Effects of static and dynamic stretching with strengthening exercises in patients with patellofemoral pain who have inflexible hamstrings: a randomized controlled trial. Sports Health. (2021) 13(1):49–56. 10.1177/1941738120932911
51.
Fatimah I Waqqar S . Effects of tibiofemoral mobilization in patients of patellofemoral pain syndrome. J Pak Med Assoc. (2021) 71(11):2506–10. 10.47391/JPMA.04-585
52.
Corum M Basoglu C Yakal S Sahinkaya T Aksoy C . Effects of whole body vibration training on isokinetic muscular performance, pain, function, and quality of life in female patients with patellofemoralpain: a randomized controlled trial. J Musculoskelet Neuronal Interact. (2018) 18(4):473–84.
53.
Wu Z Zou Z Zhong J Fu X Yu L Wang J et al Effects of whole-body vibration plus hip-knee muscle strengthening training on adult patellofemoral pain syndrome: a randomized controlled trial. Disabil Rehabil. (2022) 44(20):6017–25. 10.1080/09638288.2021.1954703
54.
Alonazi A Hasan S Anwer S Jamal A Parvez S Alfaiz FAS et al Efficacy of electromyographic-biofeedback supplementation training with patellar taping on quadriceps strengthening in patellofemoral pain syndrome among young adult male athletes. Int J Environ Res Public Health. (2021) 18(9). 10.3390/ijerph18094514
55.
Nouri F Raeissadat SA Eliaspour D Rayegani SM Rahimi MS Movahedi B . Efficacy of high-power laser in alleviating pain and improving function of patients with patellofemoral pain syndrome: a single-blind randomized controlled trial. J Lasers Med Sci. (2019) 10(1):37–43. 10.15171/jlms.2019.06
56.
Talbot LA Solomon Z Webb L Morrell C Metter EJ . Electrical stimulation therapies for active duty military with patellofemoral pain syndrome: a randomized trial. Mil Med. (2020) 185(7-8):E963–E71. 10.1093/milmed/usaa037
57.
Baldon RD Piva SR Silva RS Serrao FV . Evaluating eccentric hip torque and trunk endurance as mediators of changes in lower limb and trunk kinematics in response to functional stabilization training in women with patellofemoral pain. Am J Sports Med. (2015) 43(6):1485–93. 10.1177/0363546515574690
58.
Riel H Matthews M Vicenzino B Bandholm T Thorborg K Rathleff MS . Feedback leads to better exercise quality in adolescents with patellofemoral pain. Med Sci Sports Exercise. (2018) 50(1):28–35. 10.1249/MSS.0000000000001412
59.
Collins N Crossley K Beller E Darnell R McPoil T Vicenzino B . Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. Br J Sports Med. (2009) 43(3):169–71. 10.1136/bmj.a1735
60.
Fukuda TY Melo WP Zaffalon BM Marcondes FR Magalhaes E Bryk FF et al Hip posterolateral musculature strengthening in sedentary women with patellofemoral pain syndrome: a randomized controlled clinical trial with 1-year follow-up. J Orthop Sports Phys Ther. (2012) 42(10):823–30. 10.2519/jospt.2012.4184
61.
Dolak K Silkman C Medina MJ Hosey RG Lattermann C Uhl T . Hip-Strengthening exercises before functional exercises reduced pain in women with patellofemoral pain syndrome. J Orthop Sports Phys Ther. (2012) 94(10):940. 10.2519/jospt.2011.3499
62.
Evcik D Kuru I Ay S Maralcan G . Home-based exercise and patellar bracig in the treatment of patellofemoral pain syndrome. Turkiye Fiziksel Tip ve Rehabilitasyon Dergisi. (2010) 56(3):100–4. 10.4274/tftr.56.100
63.
Hong QM Wang HN Liu XH Zhou WQ Zhang X Luo XB . Home-based exercise program and health education in patients with patellofemoral pain: a randomized controlled trial. BMC Musculoskelet Disord. (2023) 24(1):896. 10.1186/s12891-023-07027-z
64.
Greaves H Comfort P Liu A . How effective is an evidence-based exercise intervention in individuals with patellofemoral pain?Phys Ther Sport. (2021) 51:92–101. 10.1016/j.ptsp.2021.05.013
65.
Keays SL Mason M Newcombe PA . Individualized physiotherapy in the treatment of patellofemoral pain. Physiother Res Int. (2015) 20(1):22–36. 10.1002/pri.1593
66.
Saad MC de Vasconcelos RA Mancinelli LVD Munno MSD Liporaci RF Grossi DB . Is hip strengthening the best treatment option for females with patellofemoral pain? A randomized controlled trial of three different types of exercises. Braz J Phys Ther. (2018) 22(5):408–16. 10.1016/j.bjpt.2018.03.009
67.
Paoloni M Fratocchi G Mangone M Murgia M Santilli V Cacchio A . Long-term efficacy of a short period of taping followed by an exercise program in a cohort of patients with patellofemoral pain syndrome. Clin Rheumatol. (2012) 31(3):535–9. 10.1007/s10067-011-1883-2
68.
Korakakis V Whiteley R Giakas G . Low load resistance training with blood flow restriction decreases anterior knee pain more than resistance training alone. A pilot randomised controlled trial. Phys Ther Sport. (2018) 34:121–8. 10.1016/j.ptsp.2018.09.007
69.
Hamada HA Fawaz HE Koura G Elbehary NA Elhafez SM . Mechanical response of hip and knee muscles following randomized crossover trials in patellofemoral pain syndrome. Fizjoterapia Polska. (2020) 20(1):160–8.
70.
Zemadanis K Sykaras E Athanasopoulos S Mandalidis D . Mobilization-with-movement prior to exercise provides early pain and functionality improvements in patients with patellofemoral pain syndrome. Int Musculoskelet Med. (2015) 37(3):101–7. 10.1179/1753615415Y.0000000009
71.
Boling MC Bolgla LA Mattacola CG Uhl TL Hosey RG . Outcomes of a weight-bearing rehabilitation program for patients diagnosed with patellofemoral pain syndrome. Arch Phys Med Rehabil. (2006) 87(11):1428–35. 10.1016/j.apmr.2006.07.264
72.
Bolgla LA Earl-Boehm J Emery C Hamstra-Wright K Ferber R . Pain, function, and strength outcomes for males and females with patellofemoral pain who participate in either a hip/core- or knee-based rehabilitation program. Int J Sports Phys Ther. (2016) 11(6):926–35.
73.
Hott A Brox JI Pripp AH Juel NG Liavaag S . Patellofemoral pain: one year results of a randomized trial comparing hip exercise, knee exercise, or free activity. Scand J Med Sci Sports. (2020) 30(4):741–53. 10.1111/sms.13613
74.
Cowan SM Bennell KL Crossley KM Hodges PW McConnell J . Physical therapy alters recruitment of the vasti in patellofemoral pain syndrome. Med Sci Sports Exerc. (2002) 34(12):1879–85. 10.1097/00005768-200212000-00004
75.
Vinaya Kumar MV Subramanian NB Sreelatha S Kotamraju S Krishnan M . Physiotherapeutic interventions on quadriceps muscle architecture in patello-femoral pain syndrome. Bioinformation. (2023) 19(4):454–9. 10.6026/97320630019454
76.
Clark DI Downing N Mitchell J Coulson L Syzpryt EP Doherty M . Physiotherapy for anterior knee pain: a randomised controlled trial. Ann Rheum Dis. (2000) 59(9):700–4. 10.1136/ard.59.9.700
77.
Abyaneh HM Mosallanezhad Z Mohammadalizade H Bakhshi E Vahedi G Nourbakhsh MR . Physiotherapy with and without superficial dry needling affects pain and muscle strength in patients with patellofemoral pain syndrome. Iran Rehab J. (2016) 14(1):23–30. 10.15412/J.IRJ.08140104
78.
Khayambashi K Fallah A Movahedi A Bagwell J Powers C . Posterolateral hip muscle strengthening versus quadriceps strengthening for patellofemoral pain: a comparative control trial. Arch Phys Med Rehabil. (2014) 95(5):900–7. 10.1016/j.apmr.2013.12.022
79.
Giles L Webster K McClelland J Cook J . Quadriceps strengthening with and without blood-flow restriction in the treatment of patellofemoral pain – A double blind randomised trial. J Sci Med Sport. (2017) 20:e100. 10.1136/bjsports-2016-096329
80.
Fukuda TY Rossetto FM Magalhaes E Bryk FF Lucareli PRG Carvalho NAD . Short-Term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther. (2010) 40(11):736–42. 10.2519/jospt.2010.3246
81.
Lee JH Jang KM Kim E Rhim HC Kim HD . Static and dynamic quadriceps stretching exercises in patients with patellofemoral pain: a randomized controlled trial. Sports Health. (2021) 13(5):482–9. 10.1177/1941738121993777
82.
Ferber R Bolgla L Earl-Boehm JE Emery C Hamstra-Wright K . Strengthening of the hip and core versus knee muscles for the treatment of patellofemoral pain: a multicenter randomized controlled trial. J Athl Train. (2015) 50(4):366–77. 10.4085/1062-6050-49.3.70
83.
van Linschoten R van Middelkoop M Berger MY Heintjes EM Verhaar JAN Willemsen SP et al Supervised exercise therapy versus usual care for patellofemoral pain syndrome: an open label randomised controlled trial. BMJ. (2010) 120(3):101–11. 10.1136/bmj.b4074
84.
Telles G Cristovão DR Belache FA Santos MR Almeida RS Nogueira LA . The effect of adding myofascial techniques to an exercise programme for patients with anterior knee pain. J Bodyw Mov Ther. (2016) 20(4):844–50. 10.1016/j.jbmt.2016.02.007
85.
Monika R Joginder Y Sheetal K . The effect of adding specific hip strengthening exercises to conventional knee exercises in patients with patello-femoral pain syndrome. Int J Physiother. (2016) 3(1):15–21. 10.15621/ijphy/2016/v3i1/88902
86.
Nakagawa TH Muniz TB Baldon RD Maciel CD Reiff R Serrao FV . The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. Clin Rehabil. (2008) 22(12):1051–60. 10.1177/0269215508095357
87.
Şahin M Ayhan FF Borman P Atasoy H . The effect of hip and knee exercises on pain, function, and strength in patients with patellofemoral pain syndrome: a randomized controlled trial. Turk J Med Sci. (2016) 46(2):265–77. 10.3906/sag-1409-66
88.
Yelvar GD Y Baltaci G Bayrakci Tunay V Atay AÖ . The effect of postural stabilization exercises on pain and function in females with patellofemoral pain syndrome. Acta Orthop Traumatol Turc. (2015) 49(2):166–74. 10.3944/AOTT.2015.13.0118
89.
Mason M Keays SL Newcombe PA . The effect of taping, quadriceps strengthening and stretching prescribed separately or combined on patellofemoral pain. Physiother Res Int. (2011) 16(2):109–19. 10.1002/pri.486
90.
Ahmadi M Yalfani A Gandomi F Rashid K . The effect of twelve-week neurofeedback training on pain, proprioception, strength and postural balance in men with patellofemoral pain syndrome: a double-blind randomized control trial. J Rehabil Sci Res. (2020) 7(2):66–74. 10.30476/jrsr.2020.84868.1067
91.
Celik D Argut SK Türker N Kilicoglu OI . The effectiveness of superimposed neuromuscular electrical stimulation combined with strengthening exercises on patellofemoral pain: a randomized controlled pilot trial. J Back Musculoskelet Rehabil. (2020) 33(4):693–9. 10.3233/BMR-181339
92.
Esculier JF Bouyer LJ Dubois B Frémont P Moore L Roy JS . Effects of rehabilitation approaches for runners with patellofemoral pain: protocol of a randomised clinical trial addressing specific underlying mechanisms. BMC Musculoskelet Disord. (2016) 17(1). 10.1186/s12891-015-0859-9
93.
Chiu JK Wong YM Yung PS Ng GY . The effects of quadriceps strengthening on pain, function, and patellofemoral joint contact area in persons with patellofemoral pain. Am J Phys Med Rehabil. (2012) 91(2):98–106. 10.1097/PHM.0b013e318228c505
94.
Avraham F Aviv S Ya'akobi P Faran H Fisher Z Goldman Y et al The efficacy of treatment of different intervention programs for patellofemoral pain syndrome - A single blinded randomized clinical trial. Pilot study. TheScientificWorldJournal. (2007) 7:1256–62. 10.1100/tsw.2007.167
95.
Eburne J Bannister G . The McConnell regimen versus isometric quadriceps exercises in the management of anterior knee pain. A randomised prospective controlled trial. Knee. (1996) 3(3):151–3. 10.1016/0968-0160(96)00214-1
96.
Akarcali I Tugay N Kaya D Atay A Doral MN . The role of high voltage electrical stimulation in the rehabilitation of patellofemoral pain. Pain Clin. (2002) 14(3):207–12. 10.1163/156856902320761397
97.
Prieto-García LF Cortés-Reyes E Lara-Cotacio G Rodríguez-Corredor LC . Therapeutic effect of two muscle strengthening programs in patients with patellofemoral pain syndrome. A randomized controlled clinical trial. Revista de la Facultad de Medicina. (2021) 69(2):e85599. 10.15446/revfacmed.v69n2.85599
98.
Keays SL Mason M Newcombe PA . Three-year outcome after a 1-month physiotherapy program of local and individualized global treatment for patellofemoral pain followed by self-management. Clin J Sport Med. (2016) 26(3):190–8. 10.1097/JSM.0000000000000226
99.
Kannus P Niittymaki S . Which factors predict outcome in the nonoperative treatment of patellofemoral pain syndrome? A prospective follow-up study. Med Sci Sports Exercise. (1994) 26(3):289–96. 10.1249/00005768-199403000-00004
100.
Liao Z Quintana Y . Challenges to global standardization of outcome measures. AMIA Jt Summits Transl Sci Proc. (2021) 2021:404–9.
101.
American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. (2009) 41(3):687–708. 10.1249/MSS.0b013e3181915670
102.
Schoenfeld BJ Grgic J Ogborn D Krieger JW . Strength and hypertrophy adaptations between low- vs. High-load resistance training: a systematic review and meta-analysis. J Strength Cond Res. (2017) 31(12):3508–23. 10.1519/jsc.0000000000002200
103.
Nuzzo JL Pinto MD Nosaka K Steele J . Maximal number of repetitions at percentages of the one repetition Maximum: a meta-regression and moderator analysis of sex, age, training Status, and exercise. Sports Med. (2024) 54(2):303–21. 10.1007/s40279-023-01937-7
104.
Moesgaard L Beck MM Christiansen L Aagaard P Lundbye-Jensen J . Effects of periodization on strength and muscle hypertrophy in volume-equated resistance training programs: a systematic review and meta-analysis. Sports Med. (2022) 52(7):1647–66. 10.1007/s40279-021-01636-1
105.
Hoover DL VanWye WR Judge LW . Periodization and physical therapy: bridging the gap between training and rehabilitation. Phys Ther Sport. (2016) 18:1–20. 10.1016/j.ptsp.2015.08.003
106.
Pallarés JG Hernández-Belmonte A Martínez-Cava A Vetrovsky T Steffl M Courel-Ibáñez J . Effects of range of motion on resistance training adaptations: a systematic review and meta-analysis. Scand J Med Sci Sports. (2021) 31(10):1866–81. 10.1111/sms.14006
107.
Schoenfeld BJ . The mechanisms of muscle hypertrophy and their application to resistance training. J Strength Cond Res. (2010) 24(10):2857–72. 10.1519/JSC.0b013e3181e840f3
108.
Yamato TP Maher CG Saragiotto BT Hoffmann TC Moseley AM . How completely are physiotherapy interventions described in reports of randomised trials?Physiotherapy. (2016) 102(2):121–6. 10.1016/j.physio.2016.03.001
109.
Nosek BA Hardwicke TE Moshontz H Allard A Corker KS Dreber A et al Replicability, robustness, and reproducibility in psychological science. Annu Rev Psychol. (2022) 73:719–48. 10.1146/annurev-psych-020821-114157
110.
Garber CE Blissmer B Deschenes MR Franklin BA Lamonte MJ Lee IM et al American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. (2011) 43(7):1334–59. 10.1249/MSS.0b013e318213fefb
Summary
Keywords
rehabilitation, physical therapy, resistance training, quadriceps, range of motion
Citation
Gunhamn T, Pojskic H and Augustsson SR (2025) Knee extensor training in patients with patellofemoral pain: a systematic review and synthesis. Front. Rehabil. Sci. 6:1641054. doi: 10.3389/fresc.2025.1641054
Received
04 June 2025
Accepted
16 July 2025
Published
11 August 2025
Volume
6 - 2025
Edited by
Simona Portaro, University Hospital A.O.U. "G. Martino", Italy
Reviewed by
Frane Grubišić, Sisters of Charity Hospital, Croatia
Widi Arti, Universitas Muhammadiyah Sidoarjo, Indonesia
Updates
Copyright
© 2025 Gunhamn, Pojskic and Augustsson.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Ted Gunhamn ted.olssongunhamn@lnu.se
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.