Abstract
Recent years have seen an increase in recognition of the important impact that mental health, wellbeing, and stigma have on the quality of life of people affected by neglected tropical diseases (NTDs), including the publication of global normative guidance and policy frameworks. However, systematic collation of the evidence that can guide greater clarity of thinking for research and practical application of effective interventions is lacking. We used systematic mapping methodology to review the state of the evidence around mental health, stigma, and NTDs in low- and middle-income countries, applying a simple theoretical framework to explore intersections between these areas. We built on existing reviews on the links between each domain, bringing the reviews up to date, across the NTDs identified by the WHO (minus recent additions). After systematic searching of major databases, and exclusions, we identified 190 papers. Data extraction was done to inform key topics of interest, namely, the burden of mental distress and illness/stigma associated with NTDs, the mechanisms by which NTDs add to mental distress and illness/stigma, how mental distress and illness/stigma affect the outcome and treatment of NTDs, and efficacy of interventions to address these domains. We also document the recommendations given by the authors of included studies for research and interventions. We found that there has been a substantial increase in research, which remains very heterogeneous. It was dominated by skin conditions, especially leprosy and, less so, lymphatic filariasis. Few studies had a comparative and even fewer had an intervention design. Our findings were however consistent with existing reviews, pointing to a high prevalence of mental conditions, substantially mediated by stigma and exclusion and a lack of sufficient access to support for mental wellbeing in programmes, despite the existence of effective interventions. These interventions cut across mental health services, stigma reduction, community engagement, and empowerment of people affected. We conclude that the evidence justifies increased investment in practical and integrated interventions to support the wellbeing of people affected by NTDs but that there remains a need for implementation research of consistent quality, and basic science around the impact of mental health interventions on NTD outcomes (including on elimination efforts) needs to be strengthened.
1 Introduction
In addition to the considerable suffering and disability associated with neglected tropical diseases (NTDs), affected people often face social exclusion and have high rates of mental illness.
Traditional methods of estimating the burden of disease may not adequately capture adverse mental health effects and broader societal impacts (1, 2). For example, the burden of disease associated with lymphatic filariasis (LF) is around twice as high if a co-morbid depressive illness is taken into account (3). The isolation of physical manifestations of these conditions from emotional and social consequences underestimates not only the impact on people’s lives but also accurate formal measurement, including Global Burden of Disease estimates (4). This has major implications in policy and investment around service provision, though the World Health Organization (WHO) Roadmap for NTDs (2021–2030) has made substantial advances in calling for appropriate integration of comprehensive approaches in NTD programming (5).
Many of the consequences of NTDs are chronic, irreversible, and difficult to hide. They impact key life areas of social salience, such as the ability to work, marry, or meet social role expectations (6) and touch on popular concerns about the etiology, heredity, or transmission of the condition. People affected by NTDs describe emotional consequences such as mental distress and cite a major cause as social exclusion associated with stigma and discrimination, for example, preventing people from playing a full role in society (7–9). This has an impact on people affected and, by association, their families (3). Stigma and mental illness may impact negatively the uptake and effectiveness of NTD treatments, potentially reducing the effectiveness of investment in elimination efforts (9, 10). Recognizing the links between NTDs, stigma, and mental health is therefore important, both to ensure that health programmes adequately meet the expressed needs of those affected and to ensure that comprehensive NTD programming is maximally impactful.
1.1 Conceptual framework guiding the review
In this paper, we review and summarize the existing evidence on the links between NTDs, stigma, and mental health and derive recommendations for research and lessons for effective interventions to address mental health and stigma-related problems in NTD programmes and community interventions. The nature of these intersecting domains is that there are often mutually reinforcing, complex interactions between multiple social and personal factors. In order to address this, we propose a conceptual framework that clarifies relationships between different elements that we wish to explore, which we hope will also be helpful to guide research and action at several levels and by a range of stakeholders (Figure 1). This review itself also enables an examination of the utility of the conceptual frame in understanding these areas.
Figure 1
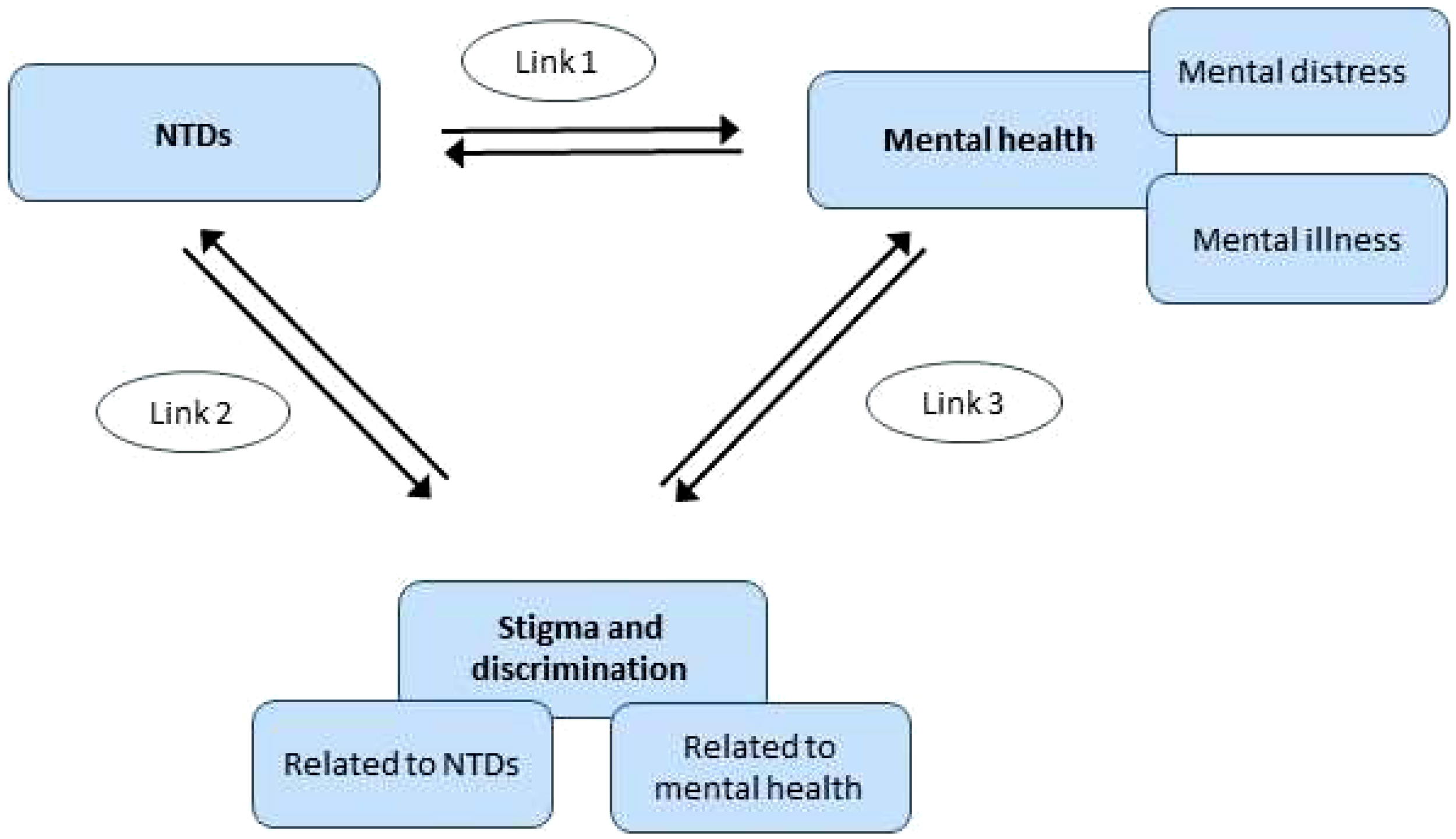
Initial conceptual framework for review.
1.2 Previous work guiding the review
Existing review articles cover some elements of this conceptual framework. For example, for Link 1 (NTDs and mental health), a review by Litt and colleagues (11) includes evidence up to and including 2010. This review, which our review served to update, highlighted the links between NTDs and mental health, including depression, suicide, and reduced quality of life. A more recent systematic review by Somar et al. (2020) (12) consolidated evidence on the mental health impacts and determinants of leprosy. The review identified depression, anxiety, and suicide (thoughts and/or attempts) as well as fear, shame, low self-esteem, loneliness, sadness, anger, and reduced quality of life are associated with leprosy. In addition, children (including adolescents) of leprosy-affected individuals were found to have poor mental health outcomes such as depression and low self-esteem.
For Link 2 (NTDs and stigma and discrimination), a seminal systematic review by Hofstraat and van Brakel published in 2016 covers the evidence up to and including 2014 for NTDs other than leprosy (9), and another review summarizes the evidence on leprosy and stigma up to and including 2012, with one study from 2013 included (13). The review by Hofstraat and van Brakel (2016) (9) found that the stigma associated with NTDs causes an enormous social and psychological burden in terms of social exclusion, reduced quality of life, and poor mental health. Leprosy-related stigmatization has been relatively well-researched compared to other NTDs (13–16). People with NTDs are prone to social stigmatization and discrimination, due to the physical impairments and disfigurements that accompany some of the NTDs (17). The reasons why NTDs are stigmatized vary, but the types of stigma, the impact on affected persons and their families, and potential interventions to reduce stigma share many characteristics (9).
Finally, several recent reviews cover the evidence on anti-stigma interventions in the field of mental illness-related stigma (Link 3) up to and including 2012 (18–21). However, due to the main focus of this paper on NTDs, Link 3 was not explored further as part of this review.
2 Methods
The review work carried out for this paper therefore focused on i) the evidence published since these reviews for Links 1 and 2 [using NTD-related search terms of the Hofstraat and van Brakel review (9) and stigma and mental health-related search terms of Thornicroft et al. (19)] and ii) integrates and summarizes both recent and previously reviewed evidence to answer the review questions.
Within the conceptual framework outlined above, we were particularly interested in certain research questions for Links 1 and 2, which served as categories for data summarizing in the data extraction phase of the review (see below). These questions were as follows: i) What is the burden of mental distress and illness/stigma associated with NTDs? ii) What are the mechanisms by which NTDs add to mental distress and illness/stigma? iii) How do mental distress and illness/stigma affect the outcome and treatment of NTDs? iv) What interventions have been employed to address the burden of mental distress and illness/stigma associated with NTDs and which have proven effective? v) What are the recommendations given by the authors of included studies for research and interventions?
2.1 Search strategy
The search strategy employed systematic literature mapping techniques as recommended in published guidelines (22, 23) to provide a broad overview of the literature in the field of NTDs, mental health, social exclusion, and stigma (24–26). Mapping reviews aim to map out existing research on a given subject or subject area rather than address one specific review question alone. Articles are not appraised for quality; instead, the aim is to describe and categorize the existing evidence base, identify gaps in the evidence, and derive recommendations. A broad set of search terms were used for each of 1) neglected tropical diseases (as subject heading or text word), 2) mental illness and wellbeing (as the subject heading or text word), and 3) social exclusion/inclusion and stigma (as the subject heading or text word) (see Appendix 1 for search terms used). The search terms were based on earlier seminal reviews in the field (9, 11, 19) and were expanded to include further terms describing wider aspects of mental health and wellbeing, such as (mental health/psychological/emotional aspects of) quality of life (see Appendix 1 for details). We searched Medline, Embase, PsycINFO, and Global Health databases to cover the literature published since the above key reviews, i.e., the search on NTDs and mental health (Link 1) covered the time span 2011–2018 [update to the review by Litt et al., 2012 (11)], whilst the search on NTDs and stigma (Link 2) covered the time frame 2015–2018 for NTDs other than leprosy [update to the review by Hofstraat and van Brakel (2016) (9)] and 2013–2018 for stigma and leprosy [update to the review by Sermrittirong and van Brakel 2014 (13)]. We further searched the repository of NTD-related studies listed under infoNTD.org (27) and infolep.org (28) with the search terms “mental” and “stigma”. All searches were conducted in July 2018.
2.2 Neglected tropical diseases
We applied the WHO definition of neglected tropical diseases valid in 2016 (29), which was also used in the systematic review by Hofstraat and van Brakel (2016) (9) and was described as follows (p.1): “According to WHO, the group of NTDs comprises 17 disease entities, caused by either viruses: dengue/chikungunya and rabies; bacteria: Buruli ulcer, leprosy, trachoma and endemic treponematoses (e.g., yaws); protozoa: Chagas disease, human African trypanosomiasis (HAT or sleeping sickness) and leishmaniasis; or helminths: dracunculiasis (guinea-worm disease), echinococcosis, foodborne trematodiases, lymphatic filariasis (LF), onchocerciasis (river blindness), schistosomiasis, soil-transmitted helminthiasis (STH) and taeniasis/cysticercosis. In addition to this list of 17 disease entities, podoconiosis is also highlighted by WHO as a neglected tropical condition” (9). Recent changes, notably the addition of snake bite envenoming and scabies, are not included here. Given its likely association with onchocerciasis and our aim to map the evidence available as broadly as possible, nodding syndrome was also included in the list of NTDs examined in our review, though we recognize that it is an associated symptom, not a disease per se (30). We analyzed findings separately for cutaneous and visceral leishmaniasis.
2.3 Mental distress and illness
The field of global mental health has increasingly come to view mental health on a continuum from distress through to diagnosable mental conditions, with increasing levels of functional impact (31). In looking at the intersection of mental illness with NTDs, we took this broad view that the impact on people affected may be at any point on this continuum. Even where distress does not reach diagnostic criteria, this remains a concern of the field and is amenable to appropriate interventions. We have also used diagnoses where relevant, based on findings in the papers, and recognized their value in research and clinical work. In this, we hope to capture the diversity of experiences related to mental health, wellbeing, and disability associated with NTDs. The list of search terms used to capture this domain is accessible in Appendix 1. Epilepsy was not included as a mental health outcome, as we considered neurological conditions to be beyond the scope of this review.
2.4 Stigma, discrimination, and social exclusion
Stigma can be conceptualized as a construct consisting of problems of knowledge (ignorance), problems of attitudes (prejudice), and problems of behavior (discrimination) (32). Discrimination, the behavioral consequence of stigma, contributes to the disability of people affected and leads to social exclusion and disadvantage. In this review, we examine both public stigma (i.e., stereotypes, negative attitudes and discriminatory behavior amongst community members, health staff, or even family members who may stigmatize a person affected by NTDs) and experienced stigma (i.e., the subjective experience of discrimination, exclusion, and devaluation faced by people affected by NTDS and sometimes their family members). The term experienced stigma here also includes the experience of internalized stigma, which is created when people affected accept the discrediting beliefs and prejudices held against them and lose self-esteem (33), leading to feelings of shame, feelings of hopelessness, feelings of depression, a sense of alienation, and social withdrawal (34). This also includes the distress created by anticipated stigma, i.e., the worry about potential negative social reactions, concerns about disclosing the illness, and attempts to prevent this. A further construct is the notion of perceived stigma, which refers to being aware of stigma and discrimination existing in one’s community, without necessarily having experienced it directly. We applied a broad selection of search terms in this review to capture the range of descriptions of stigma in the literature (see Appendix 1).
2.5 Participants/population
Studies included were those involving people affected by NTDs as defined above and their family members/caregivers who were living in low-and-middle-income countries (LMICs) [defined by the World Bank (35)]. We also included studies on community members or health professionals exhibiting stigma towards people with NTDs or their family members/caregivers in those countries. The focus on LMICs was chosen since our mapping review aimed to help inform future interventions in those countries, which carry the great majority of disease burden because of NTDs.
2.6 Types of studies included
The review included all types of original peer-reviewed research studies (including intervention studies and descriptive studies) published in the time frames specified for the search on each link, provided their main focus was on the outcomes specified below. The specified time frame for the search on Link 2 (NTDs and stigma) was shorter than for the search on Link 1 (NTDs and mental health), and chance findings on stigma outcomes identified outside this time frame within the searches on mental health were not included in our findings for reasons of consistency. Review papers were also searched for, and key findings were referred to in the “Introduction” and “Discussion” sections of this article. Only publications in the English language and with an abstract were included.
2.7 Study outcomes and selection of studies
A two-stage process was followed in order to determine whether a study addressed the study outcomes in question.
Firstly, we screened abstracts to examine whether the main focus of a study was related to one or both of the following two key study outcomes:
-
1. Mental health and wellbeing amongst people living with NTDs or
-
2. Stigma, discrimination, and social exclusion are faced by people living with NTDs.
Articles that simply performed an evaluation of treatments for NTDs were excluded unless the treatments included mental health or social component or measured an outcome that was related to either mental health and wellbeing (mental health components within the quality of life measures were also included as mental health outcomes) or stigma, human rights, and social exclusion (such as social relations, social functioning, or employment). Articles that investigated outcomes solely in relation to, for example, clinical symptoms of NTDs (including neuropsychiatric symptoms) or the acceptability, compliance with, and success of mass drug administration programmes, were excluded. We also excluded papers on knowledge, attitudes, and practices relating to NTDs if they did not specifically relate to the concept of stigma in the sense of social devaluation.
Where an abstract was found to meet the initial criteria, we then reviewed the full paper and included for final selection any paper where the primary or secondary outcome or the main determinant focused on 1) mental health and wellbeing or 2) stigma or social exclusion/inclusion.
Two reviewers (MK and YAH) participated in the selection of abstracts for full-text review. Both independently screened an initial set of 400 abstracts, at which point agreement for study exclusion between them was over 96%. Because of this high level of agreement, the remaining abstracts were divided between the two reviewers. The full texts of the selected articles were then divided amongst a team of five reviewers (EA, MK, MS, PCH, and YAH) to establish whether each retrieved paper met the inclusion criteria on the basis of the full text of the paper. Disparities in inclusion decisions were resolved through discussion. The reviewers did not contribute to inclusion decisions regarding studies in which they were involved. EndNote was used to store all selected studies.
A total of 190 articles were selected for inclusion (see also Figure 2). Data were extracted (by EA, MK, MS, PCH, and YAH) using categories derived from the research questions of the study, for example, “Burden and frequency of mental distress and illness amongst people affected by NTDs”. The first set of 25 studies was coded by two reviewers independently and then discussed in the group until agreement on the level of detail and type of information to be extracted had been achieved. Data were then extracted from the remaining papers separately. Coded data were summarized to identify key cross-cutting findings as well as important differences between diseases and countries for each research question.
Figure 2
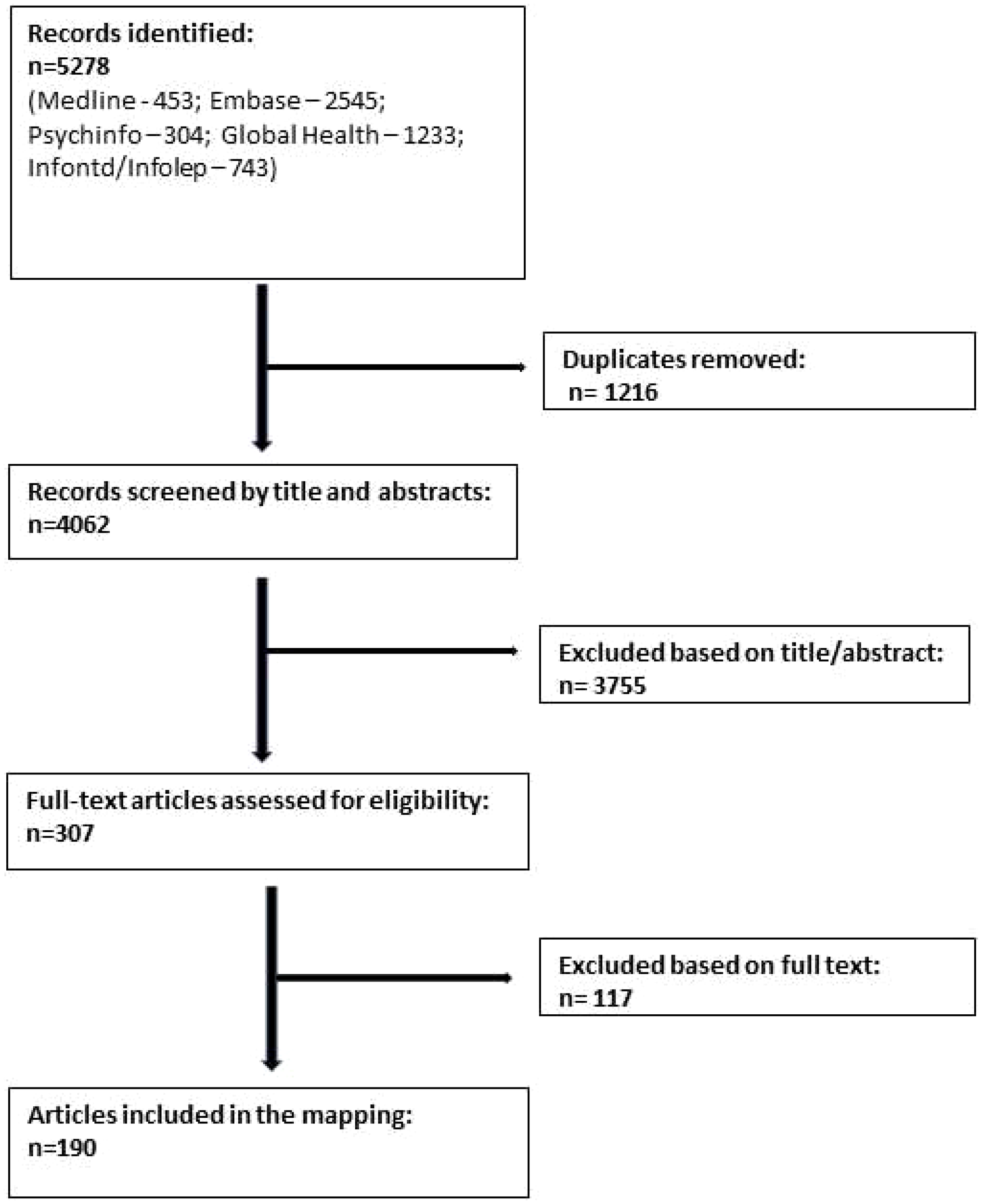
Flow diagram of study selection process.
3 Results
Findings are presented separately for each of Links 1 and 2 as shown in Figure 1. In each case, we also provide evidence for the interactions in both directions, as we found interactions between the domains to be bi-directional.
3.1 Neglected tropical diseases and mental health (Link 1)
3.1.1 Overview of evidence included as part of the systematic mapping review
In the review period for the link between NTDs and mental health (1 January 2011 to 22 July 2018), we found 66 studies (with 62 samples) from 26 countries (plus one global study) that reported on the mental health burden or mental distress/disorder associated with 14 of the included NTDs other than leprosy. These studies most commonly used a cross-sectional quantitative design (38 studies), some of which included a comparative element (for example, a control group). A further 12 studies were qualitative, seven were cohort studies, four were case–control studies, two were mixed-methods, one was a case series, one was a pre–post study, and only one was a randomized controlled trial (RCT). We found 53 studies from 13 countries in the review period that reported on the mental health link with leprosy.
Figure 3 shows those LMICs where we found published studies on the link between NTDs and mental health for both leprosy and other NTDs during the review period. There were over 100 LMICs that are endemic for at least one NTD, for which we did not find any relevant study during the review period.
Figure 3
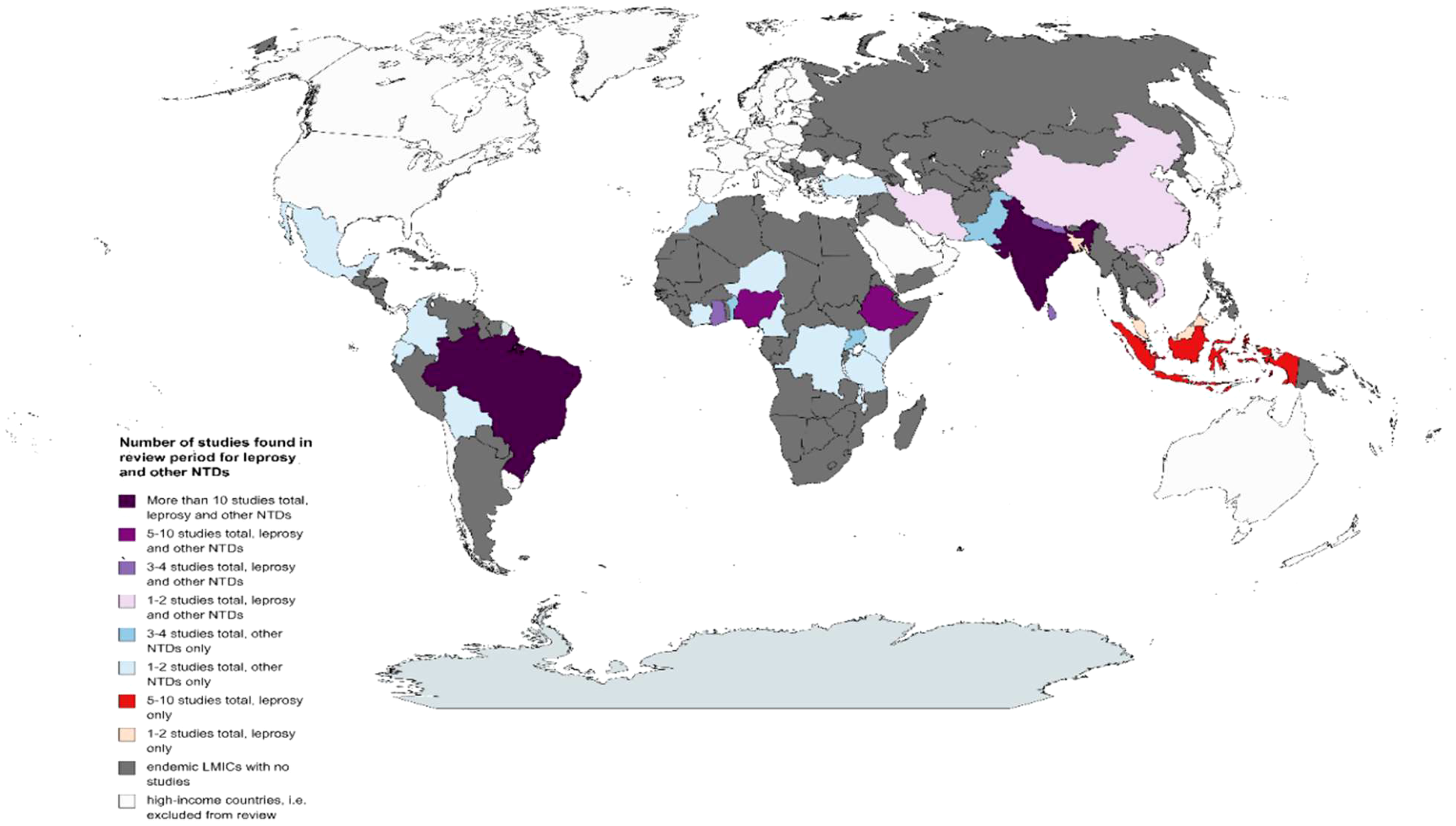
Map showing countries for which studies were found during the review period on the link between NTDs and mental health. NTDs, neglected tropical diseases.
For NTDs other than leprosy, the region with the most studies conducted in the review period was Africa with 28 studies (nine NTDs), followed by Asia with 20 studies (five NTDs), and the Americas with 17 studies (five NTDs), and there was one global study (see Figure 3). For nine of the included NTDs (other than leprosy), studies came from one region only in the review period, either Africa or the Americas. For five other included NTDs (other than leprosy), studies came from several regions: chikungunya (Americas and Asia), cutaneous leishmaniasis (Africa, Americas, and Asia), dengue (Americas and Asia), lymphatic filariasis (Africa, Asia, and global study), and schistosomiasis (Africa and Asia).
For leprosy, the region with the most studies conducted in the review period was Asia with 30 studies, followed by the Americas with 18 studies (all from Brazil) and then Africa (five studies, see Figure 3).
There was no relevant published study found on the link between NTDs and mental health in the review period for dracunculiasis (guinea-worm disease), echinococcosis, endemic treponematoses, foodborne trematodiases, human African trypanosomiasis, rabies, or soil-transmitted helminthiasis.
3.1.2 Burden and types of mental distress and illness associated with neglected tropical diseases
Findings across studies and NTDs were remarkably consistent in their trend, with poor mental health outcomes reported for all of the NTDs. The outcomes that were particularly salient (i.e. many studies, across different diseases) were mental health components of quality of life (23 studies reported on this outcome during the review period for 11 NTDs other than leprosy and 15 studies on leprosy), depression/depressive symptoms (20 studies for 11 NTDs other than leprosy and 13 on leprosy), and anxiety disorder/anxiety symptoms (13 studies for seven NTDs other than leprosy and five on leprosy).
When looking at each disease separately, the evidence was generally patchy, and for most NTDs only a few studies (five or fewer) were identified within the review period that assessed the burden and/or types of mental health outcomes. Slightly more substantial evidence was available for dengue and lymphatic filariasis (10 studies with nine participant samples each), and many more for leprosy, during the review period.
Table 1 shows the outcomes relating to mental health that were identified in this review, along with the relevant NTDs, and a summary of findings.
Table 1
| Sub-themes/outcome categories of mental health burden | Found for which NTDs | NTDs other than leprosy | Leprosy1 | All NTDs Summary of findings |
|---|---|---|---|---|
| Main findings | Mapping of the evidence identified in this review using a data saturation approach, supplemented by key findings of a recent systematic review on the impact of leprosy on mental wellbeing that that that that that included the same review period (12) | (this review) | ||
| (Quality of life) in mental health/psychological/emotional domains | ||||
| QoL (mental health/psychosocial subscales) | Chagas disease, chikungunya, dengue, leishmaniasis (cutaneous and visceral), leprosy, lymphatic filariasis (LF), neurocysticercosis, podoconiosis, schistosomiasis, trachoma, tungiasis | - Studies on prevalence rates² of impaired QoL reported these to be between approximately 60% and 100% [for Chagas disease (36) and cutaneous leishmaniasis (CL) (37) in Brazil, dengue fever in Vietnam (38), and tungiasis in Kenya (39)] - Chagas disease: impaired QoL reported, including role-emotional (40) and psychological domains (41) (Brazil) - Chikungunya: QoL (including mental and emotional domains) reported to be impaired compared to healthy controls, both during active illness and also for several months (>1 year) after clinical recovery (Colombia) (42) - CL: lower QoL (including mental health domain) found amongst adults (Iran) (43) compared to controls (India) (44), and amongst children and adolescents and their mothers (Turkey) (45) compared to controls - Visceral leishmaniasis (VL): lower QoL reported amongst patients with the disease and HIV compared to those with HIV only (46); taking ART drugs led to improvements in the psychological health QoL domain (47) (Ethiopia) - LF: QoL (including mental health/psychological health domains) found to be poorer compared to matched controls [India (48), Malawi (49)]; chronic lymphoedema had a negative impact on QoL (Sri Lanka) (50) - Neurocysticercosis: QoL (including emotional wellbeing and mental health domains) were lower compared to controls [Brazil (51, 52), Mexico (53)] - Podoconiosis: low QoL reported compared to healthy controls overall and in all domains, including the psychological one; controls were seven times more likely to have high (above median) QoL than cases (Ethiopia) (54) - Schistosomiasis: QoL (incl. emotional, psychosocial, and psychological) lower compared to healthy controls amongst affected adults [Cote d’Ivoire (55)], adolescents [Kenya (56)] and children [Kenya (56), Tanzania (57)] - Trachoma: reduced QoL reported amongst affected persons [Ethiopia (58), Niger (59)], including the psychological domain (Ethiopia) (58) |
This review: studies on QoL associated with leprosy were conducted during the review period in Bangladesh (60), Brazil (61–68), Ghana (69), India (70, 71), Nepal (72), and Vietnam (73). Review by Somar et al. (2020): leprosy-affected persons were found to have scored lower in the psychological domains of QoL than their healthy counterparts (12). |
For affected persons, impaired QoL in the mental health/psychological/emotional domains has been consistently reported by a wide range of studies across NTDs and countries. |
| Depression/depressive symptoms | ||||
| Depression/depressive symptoms | Buruli ulcer, Chagas disease, chikungunya, dengue, leishmaniasis (cutaneous and visceral), leprosy, LF, neurocysticercosis, nodding syndrome, podoconiosis, schistosomiasis | - Studies on prevalence rates² of depression/depressive symptoms reported these to be between 12.6% and over 80% [for Buruli ulcer in Benin (74), Chagas disease in Brazil (36, 75), chikungunya in India (76), dengue in Pakistan (77, 78) and Sri Lanka (79), LF in Nigeria (80, 81), neurocysticercosis in Brazil (51, 52), podoconiosis in Ethiopia (82), and schistosomiasis in China (83)]; these prevalence rates were much higher than in the general population [dengue in Pakistan (77), LF in Nigeria (80, 81), podoconiosis in Ethiopia (82)]; prevalence rates may still be elevated post-disease [Buruli ulcer in Benin (74), dengue in Sri Lanka (79)] - Chagas disease: affected persons were found to be more likely to experience depression/depressive symptoms (Brazil) (36, 75) - CL: depression was reported amongst affected adults (Iran) (43), and was reported to be higher amongst affected children and adolescents than healthy matched controls (Turkey) (45) - VL: depression was common amongst patients with both the disease and HIV; depressive symptoms were higher amongst HIV patients with the disease than those without (Ethiopia) (46, 84) - LF: depression was found to contribute twice the burden of morbidity of the disease compared to the physical health consequences globally (3) - Nodding syndrome: depression reported amongst affected children, which contributed to them missing or dropping out from school (Uganda) (85) |
This review: studies on this outcome were conducted in Brazil (86–89), India (71, 90–92), Indonesia (93, 94), and Nigeria (95–97) during the review period Review by Somar et al. (2020): Depression was the most frequently identified psychiatric condition amongst persons affected by leprosy. The prevalence of depression varied between countries but remained high. Several studies found that depression was significantly more likely in those with leprosy compared with healthy controls (12) |
Depression/depressive symptoms have been consistently reported to be high or elevated amongst affected persons, across a wide range of NTDs and countries. All studies that compared depression rates amongst affected people to a control group found depression to be higher amongst affected persons. The burden of depression associated with LF has been estimated to be twice that of the physical health consequences of LF globally. |
| Feelings that could be associated with depression/depressive symptoms | Buruli ulcer, chikungunya, dengue, leishmaniasis (cutaneous and visceral), leprosy, LF | - Buruli ulcer: severe and persistent fatigue reported amongst affected adults and children in Ghana, which also interfered with their activities of daily living (98); low mood common amongst former patients in Benin (adolescents: 52.4%, adults: 48.9%) (74) - Chikungunya: 15% of affected persons had neurasthenia (fatigue syndrome) (India) (76) - Dengue: fatigue/tiredness, lack of energy, and sadness reported by affected persons (99–101) - CL: 86% of high school students in endemic areas expressed in a survey that the disease possibly or definitely has psychological effects, including symptoms of depression (Morocco) (102); sadness reported by affected persons (Iran) (43) - VL: sadness reported by affected persons (84) - LF: sadness and hopelessness reported by affected persons (Nigeria) (80); 73.4% of affected persons reported low self-esteem (Nigeria) (81); low self-esteem and feeling weak were reported in Nepal (103) |
This review: the following outcomes were reported for leprosy: sadness/depressive feelings [Brazil (86, 104, 105), Indonesia (94, 106), Malaysia (107), Nepal (72)]; no or little meaning to life, negative feelings (Brazil) (86); hopelessness/despair [Brazil (105), India (108), Iran (109), Nepal (72)]; feeling like it is the end of their life (India) (108); lack of enthusiasm (Indonesia) (94); low self-esteem [Bangladesh (110), Indonesia (106, 111)]. Review by Somar et al. (2020): leprosy-affected persons experience low self-esteem, insecurity and a loss of confidence (12). |
Reported feelings that could be associated with depression/depressive symptoms include fatigue (syndrome)/tiredness, lack of energy, sadness, low self-esteem, low mood, life being meaningless/finished, hopelessness, and lack of enthusiasm. |
| Shame | Leishmaniasis (cutaneous), leprosy, onchocerciasis | - CL: 86% of high school students in endemic areas expressed in a survey that the disease possibly or definitely has psychological effects, including shame, e.g., to show face (Morocco) (102) - Onchocerciasis: shame mentioned by affected persons as a consequence of avoidance by others in a mixed-methods study in Cameroon, DRC, Nigeria, and Uganda (112) |
This review: studies were conducted during the review period in Bangladesh (110), Brazil (89, 105, 113), Indonesia (106, 111, 114), Iran (109), and Sri Lanka (115). Review by Somar et al. (2020): shame was reported as common amongst leprosy-affected individuals (12). |
Shame has been reported as an outcome by several studies (see also stigma section). |
| Anxiety/symptoms of anxiety | ||||
| (General) anxiety (disorder)/symptoms of anxiety | Buruli ulcer, Chagas disease, chikungunya, dengue, leishmaniasis (cutaneous), LF, leprosy, schistosomiasis | - Studies on prevalence rates² of anxiety/symptoms of anxiety reported these to be between 15% and approximately 60% (Buruli ulcer in Benin (74) and Ghana (116), Chagas disease in Brazil (75), chikungunya in India (76), dengue in Pakistan (78), schistosomiasis in China) (83) - Dengue: anxiety was common during the acute stage (which decreased after recovery) (Pakistan) (100); anxiety was common amongst people with prior diagnosis of dengue fever (Sri Lanka) (79) - CL: no significant difference in anxiety between those with and without the disease amongst affected children and adolescents (Turkey) (45) - LF: anxiety reported by affected persons (Nepal) (103) |
This review: studies were conducted during the review period in India (91, 92, 117) and Nigeria (95, 97). Review by Somar et al. (2020): anxiety conditions were the second most commonly reported mental health concern, with prevalence ranging from 10% to 20% amongst leprosy-afflicted individuals (12.) |
Elevated anxiety has been reported by several studies across various NTDs and countries. Of studies comparing anxiety rates amongst affected people to a control group, only one study found no significant effects (CL in Turkey). |
| Other forms of anxiety or feelings that could be associated with anxiety | Buruli ulcer, Chagas disease, chikungunya, dengue, leishmaniasis (cutaneous and visceral), leprosy, LF, nodding syndrome | - Buruli ulcer: amongst affected adults and children, the greatest worry was the fear of the ulcer recurring and the need to prevent this, which often led to anxiety and panic, which then affected participants’ daily routines and social activities (Ghana) (98); 60% of people with pre-ulcer conditions and 71.7% of respondents with ulcers reported feeling anxious and worried about their illness condition on family well-being (Ghana) (116); 20% of those with pre-ulcer conditions had fear of surgery vs. 18.7% of those with ulcers (Ghana) (116) - Chagas disease: 52% of people with the disease and/or HIV had agoraphobia (Brazil) (75); 31.7% of affected persons (n = 20) felt frightened, worried, or emotionally devastated when they were diagnosed with the disease, but 47.6% (n = 30) conveyed a current sense of acceptance and peace with their diagnosis (“tranquilidad”), and half of the respondents who initially felt upset upon receiving a diagnosis described a shift where they took control of their feelings and became “tranquilos” (Bolivia) (118) - Chikungunya: 10% of affected persons had general anxiety disorder with panic attacks and 5% had phobic disorder (claustrophobia) (India) (76) - Dengue: 90% of affected persons suffered from very severe fear of death during the acute stage of illness, which decreased after recovery (Pakistan) (100); 23% of affected persons (mostly female) had panic attacks (Pakistan) (100); symptoms associated with anxiety, such as insomnia, tremors, dryness of mouth and palpitations, were reported for affected persons (Pakistan) (100) - CL: women reported anxious feelings due to facial scars, including young single women, and those with children worried that it would affect their children or possible transformation of the scars into skin cancers, whilst some men considered the disease as a benign problem, as it is not contagious and not fatal (Morocco) (119); 86% of high school students in endemic areas expressed in a survey that the disease has psychological effects, including fear, e.g., to meet others or go out due to scars (Morocco) (102) - VL: all male participants co-infected with this disease and HIV reported that they were fearful (including fear of death), shocked, and worried about the concurrent diagnosis (Ethiopia) (84) - LF: affected persons reported various psychological problems, including anxiety, worry, fear of being abandoned, and fear of transmitting the disease to their children (Nepal) (103); worry was one of the most commonly reported emotional reactions amongst affected people in Nigeria (80) - Nodding syndrome: PTSD reported amongst affected children, which contributed to them not going to school or dropping out (Uganda) (85) |
This review: the following outcomes were reported for leprosy: feelings of anxiousness [Brazil (104), India (90, 108, 120, 121), Nepal (72)]; worry [Brazil (105), Malaysia (107)]; nervousness [Brazil (105)]; fear, e.g., of death or of experiencing disease sequelae [Brazil (86), India (90), Indonesia (106, 111, 114)]. Review by Somar et al. (2020): feelings of fear featured heavily in the studies cited by the review; this included fear of death or disease sequelae, fear of receiving confrontational questions, fear of infecting others, fear of rejection, isolation, and prejudice. In addition to generalized anxiety disorder, obsessive-compulsive disorder, panic, and agoraphobia were identified (12). |
Other reported forms of anxiety or feelings that could be associated with anxiety include panic or panic attacks, agoraphobia, claustrophobia, PTSD, worry, anxiousness, fear (e.g., fear of death, surgery, of experiencing disease sequelae or transmitting the disease to their children), and nervousness. |
| Mental distress/wellbeing | ||||
| Mental/psychological distress | Buruli ulcer, dengue, chikungunya or Zika (DCZ) infection, leprosy, podoconiosis | - Buruli ulcer: patients with chronic ulcers reported high levels of distress, due to uncertainty and not knowing the identity of their illness or duration of treatment (Benin) (122) - Dengue, chikungunya, or Zika (DCZ): people with suspected DCZ infections reported more psychological distress symptoms (58.1% prevalence) than those without suspected DCZ infections, following a large earthquake in one of four study sites near the epicentre (Ecuador) (123, 124) - Podoconiosis: mental distress was higher in affected persons compared to healthy controls, even when adjusted for gender, income, alcohol use, age, place of residence, and family history of mental illness (Ethiopia) (125) |
This review: studies were conducted during the review period in Brazil (126), Ethiopia (127), Indonesia (106, 128), and Iran (109). Review by Somar et al. (2020): the review found high prevalence of mental distress in leprosy-affected persons (12). |
High/elevated distress levels have been consistently reported across several NTDs and countries. |
| Reduced mental/emotional wellbeing | Buruli ulcer, leishmaniasis (cutaneous), LF | - Buruli ulcer: mental wellbeing was significantly lower amongst affected persons healed from the disease compared to controls (Benin) (129) - CL: women reported reduced emotional wellbeing due to facial scars (Morocco) (119) - LF: the mental and emotional wellbeing of healthy controls was significantly better (67%) than that of affected persons (37%) (Sri Lanka) (130) |
This review: no studies on leprosy found during the review period on this specific outcome. Review by Somar et al. (2020): no studies on this specific outcome reported (12). |
Mental/emotional wellbeing has been consistently found to be reduced across several NTDs and countries. |
| Stress | Buruli ulcer, dengue, leprosy, LF | - Buruli ulcer: patients with chronic ulcers reported high levels of stress, due to uncertainty and lack of knowledge of the identity of their illness and the duration of treatment (Benin) (122) - Dengue: people with prior diagnosis of dengue fever had significantly higher stress levels than controls (Sri Lanka) (79) - LF: affected persons reported various psychological problems, including stress (Nepal) (103) |
This review: studies were found in Indonesia (128) and Sri Lanka (115). during the the review period. Review by Somar et al. (2020): no studies on this outcome reported (12). |
Stress appears to be elevated/high amongst persons affected by several NTDs. |
| Mental health problems by family members/caregivers of affected persons | ||||
| Mental health problems by caregivers | LF, nodding syndrome | - LF: emotional toll was reported on caregivers and families of affected people (Nigeria) (80); family members of affected persons expressed significant distress at the physical pain and suffering that the patients experience (India) (131) - Nodding syndrome: caregivers of affected children reported signs of apathy, limited caring or coping capacity, helplessness as a reflection of actual powerlessness, and depression because they were multiply traumatized and living below the poverty line (Uganda) (132) |
This review: no studies found during the review period. Review by Somar et al. (2020): no studies on this outcome reported (12). |
The following issues have been reported for family members/caregivers: depression, emotional toll, distress, signs of apathy, limited caring or coping capacity, trauma, and helplessness. |
| Mental health problems by children of affected parents | Leprosy | No study found during the review period outside of leprosy. |
This review: lower emotional wellbeing and self-esteem was reported amongst adolescents with affected parents, as well as reduced QoL and depression in those with two affected parents (Nepal) (133). Review by Somar et al. (2020): review found that children of leprosy-affected parents worried about contracting the disease and had a negative self-concept (12). |
Lower emotional wellbeing and self-esteem, reduced QoL, and depression have been reported for adolescents with parents affected by leprosy in Nepal. |
| Suicide | ||||
| Suicide attempts, suicidal ideation, suicide risk, or (for leprosy) death wish | Chagas disease, leprosy, LF, podoconiosis | - Chagas disease: 56.8% of people with the disease and/or HIV were at risk of suicide (Brazil) (75) - LF: depression (20% prevalence in the sample) was associated with expressions of suicidal ideation amongst affected persons, though no suicidal attempts were reported (Nigeria) (80) - Podoconiosis: risk of suicide was 5.2% amongst affected persons compared to 0.4% amongst their healthy neighbors, which was a significant difference (Ethiopia) (82); over half of persons affected by podoconiosis had considered suicide in response to discrimination and prejudice, and 54% had attempted suicide (Ethiopia) (134) |
This review: studies were conducted in China (135), India (120, 136), and Iran (109) (the last-mentioned reported on death wish) during the review period. Review by Somar et al. (2020): several studies found that suicide, suicidal thoughts, and suicide attempts in those with leprosy were fairly common (12). |
Suicide attempts, suicidal ideation, suicide risk, or having a death wish have been reported for affected persons of several NTDs and across various countries. |
| Other | ||||
| Other outcomes not included in any of the rows above | Buruli ulcer, Chagas disease, chikungunya, leprosy, LF | - Buruli ulcer: the average psychological and social functional limitation scores (in a sample of affected adults and children) were 52% and 38%, respectively (scores ranging from no functional limitation [0%] to total limitation [100%] (Ghana) (98); 20% of those with pre-ulcer conditions were embarrassed about the condition vs. 49.4% of those with ulcers (Ghana) (116) - Chagas disease: 20.8% of people with the disease and/or HIV showed alcohol abuse/dependence, and 13.6% showed other substance (not alcohol) abuse/dependence (Brazil) (75) - Chikungunya: 15% of affected persons had somatoform disorder, and 10% had vague somatic complaints, which did not fit into any of the diagnostic categories (India) (76) - LF: most people with the disease experienced emotional trauma (Nigeria) (137); affected persons reported various psychological problems, including engaging in sexual intercourse (Nepal) (103) |
This review: the following other mental health related outcomes were reported for leprosy: embarrassment [Bangladesh (110), Sri Lanka (115)]; denial [Brazil (104), Indonesia (111)]; revolt/disgust (Indonesia) (111); anger, including at self (Brazil) (89, 105); concern, distrust, and resistance to accepting the diagnosis (Brazil) (113); rejection and deep hurt (India) (90); feelings of isolation/loneliness [India (90), Indonesia (111), Iran (109)]; guilt [India (120), Indonesia (111), Iran (109)]; drug/alcohol abuse (Nigeria) (97); mental difficulties (India) (138); number of psychiatric co-morbidities (Brazil) (139); and psychotic disorders (India) (92). Review by Somar et al. (2020): other conditions linked to leprosy included sleep disorders, delusional disorders, dementia, hysteria, hyperactivity, hypochondria, and premenstrual dysphoric disorder. Emotions such as loneliness, sadness, and anger were commonly found in leprosy-affected persons. Prevalence of schizophrenia was found to be low, at approximately 1% (12). |
Other outcomes that have been reported include substance abuse/dependence; somatoform disorder/somatic complaints; psychological and social functional limitation; embarrassment; emotional trauma; difficulties in sexual intercourse; denial; disgust; anger; concern, distrust, and resistance to accepting diagnosis; rejection and deep hurt; feelings of isolation/loneliness; guilt; mental difficulties; psychiatric co-morbidities; dementia; and psychotic disorders. |
Mental health outcomes and findings reported during the review period.
LF, lymphatic filariasis; CL, cutaneous leishmaniasis; VL, visceral leishmaniasis; PTSD, post-traumatic stress disorder; QoL, quality of life.
1 We employed a data saturation approach here for leprosy; i.e., we have only provided details in this column where studies on leprosy reported additional outcomes compared to other NTDs. We used this approach since a systematic review that included our review period was recently published on the impact of leprosy on mental wellbeing (see Somar et al., 2020 (12)]. Key findings of the review by Somar et al. (2020) (12) are also included here for the readers’ reference.
2 Note that some of the variances in reported prevalence rates are likely to be due to differences in study designs and measurement tools used.
3.1.3 Postulated mechanisms by which neglected tropical diseases add to mental distress and illness
Based on our review, the postulated mechanisms (i.e. factors for which there is a plausible yet unproven causal relationship with mental distress/illness) and other associated factors that may lead to mental distress or illness for people affected by NTDs can be categorized into five broad themes: biological factors including disability, scarring or severity of disease (11 NTDs); demographic factors, including age and gender (10 studies, seven NTDs); psychological factors, i.e., pre-existing mental health issues (seven NTDs); socio-economic factors including education and employment status (four studies, six NTDs); and social factors such as stigma and relationships (six NTDs). See these in Table 2.
Table 2
| Themes | Mechanisms/factors | Further information | NTDs |
|---|---|---|---|
| Postulated mechanisms | |||
| Biological factors | Disability and severity of physical symptoms | Buruli ulcer, chikungunya, dengue, leprosy, podoconiosis | |
| Stage of disease and duration of illness | Later stages of disease and longer duration of illness | Buruli ulcer, dengue, leishmaniasis (visceral), leprosy, LF, podoconiosis, trachoma | |
| Physical changes (including scarring) | Buruli ulcer, leishmaniasis (cutaneous and visceral), leprosy | ||
| Co-morbidities | HIV in those with leishmaniasis (visceral), and epilepsy in those with neurocysticercosis | Chagas disease, leishmaniasis (visceral), neurocysticercosis, podoconiosis | |
| Social factors | Stigma1 | Leishmaniasis (visceral), leprosy, LF, onchocerciasis, podoconiosis, trachoma | |
| Marriage | Leprosy, trachoma | ||
| Social obligations | Leprosy, trachoma | ||
| Other associated factors | |||
| Demographic factors | Age | Older age | Chikungunya, dengue, leishmaniasis (cutaneous), neurocysticercosis, podoconiosis, leprosy |
| Gender | Female gender | Dengue, leishmaniasis (cutaneous), leprosy, LF, neurocysticercosis, podoconiosis | |
| Socio-economic factors | Education | Lower educational attainment levels | Buruli ulcer, leishmaniasis (cutaneous), leprosy |
| Labor and unemployment | Lack of consistent work | Dengue, leishmaniasis (visceral), LF, leprosy | |
| Psychological factors | Pre-existing mental health issues | Obsessive-compulsive disorder, trauma, history and family history of mental disorder, self-esteem | Buruli ulcer, chikungunya, dengue, leprosy, LF, nodding syndrome, podoconiosis |
Postulated mechanisms and associated factors by which NTDs influence mental distress and illness.
NTDs, neglected tropical diseases; LF, lymphatic filariasis.
1 This section on stigma as a potential mechanism influencing mental health outcomes only includes studies in the review period that measured both a mental health outcome and a stigma-related outcome and investigated the relationship between the two. Further studies on stigma-related outcomes are described in the section on “Link 2: neglected tropical diseases and stigma”.
By far, the most salient mechanism that has been reported as adding to the reduced mental wellbeing of individuals with NTDs was the biological factors, which were reported for 11 NTDs (including leprosy). The scarring, pain, and physical attributes of the diseases were amongst the most noted factors contributing to distress and mental illness. In addition, across several NTDs, the stage of disease and duration of illness was important. A striking finding by one study was that over half of persons with podoconiosis reported that they had considered suicide in response to discrimination (134).
3.1.4 Link 1 reversed: Impact of poor mental health on neglected tropical disease-related outcomes
Most of the evidence reviewed on the link between NTDs and mental health outcomes was cross-sectional in nature, making it difficult to ascertain the directionality of any association. Nevertheless, wherever studies found a causal association to be plausible (see the section on postulated mechanisms above), the assumed direction of causality was that NTD-related factors led to poorer mental health outcomes. At the same time, it is likely that some of the correlational factors mentioned in the section on postulated mechanisms may actually be bi-directional (e.g., disability, stigma, and unemployment). We therefore looked out for evidence that may support a different direction of causality in Link 1 than the one generally assumed (“Link 1 reversed”), and we examined evidence on the impact of poor mental health on NTD-related physical outcomes, which has been reported for many other physical conditions, like HIV and non-communicable diseases (NCDs) (140, 141). Overall, it can be said that there is a clear gap in the literature surrounding how mental illness impacts NTD outcomes, with much fewer studies published over the review period compared to those looking at the impact of NTDs on mental health.
By far, the most commonly reported NTD-related outcome was reduced overall quality of life, with nine studies on six NTDs (of which over half were from Latin America) reporting a correlation between poor mental health and overall quality of life (though it is worth noting the point about reverse causality and reinforcing interactions here).
We found one study in the review period demonstrating that mental illness (substance abuse) may be associated with delayed help-seeking behavior and treatment. This study from Iran on cutaneous leishmaniasis (142) showed that those experiencing opium addictions were more likely to delay treatment for fear of withdrawal if hospitalized. Larger lesions were associated with higher drug dependency.
Substance abuse was also found to negatively affect NTD outcomes in a study from Ethiopia, where chewing khat and drinking alcohol were associated with visceral leishmaniasis relapses (resulting in 20% of interviewees changing their substance use habits due to frequent relapses) (84).
In a further study, children with nodding syndrome in Uganda were found to be more likely to drop out of school owing to social, psychological, and physical reasons associated with the illness (85).
In an ethnographic study from Bolivia (118), Chagas disease patients reported the need to be calm (“tranquilo”) for their emotional wellbeing and to lessen the effects of the disease. Even otherwise positive emotions (e.g., excitement associated with going to a party) could be detrimental to their illness if they impact the tranquilidad of an affected person.
In Pakistan, researchers found that depression, anxiety, and stress negatively predicted the self-efficacy of dengue patients (101). In Brazil, pathological hoarding was found to pose a threat to the increasing proliferation of the dengue mosquito Aedes aegypti by putting people at risk owing to poor sanitation and trash accumulation (143).
3.1.5 Evidence for interventions to address mental illness associated with neglected tropical diseases
Table 3 provides an overview of studies conducted during the review period that evaluated interventions to address mental illness associated with NTDs or that measured mental health outcomes.
Table 3
| Outcome category | NTD/country | Study design | Intervention | Main findings |
|---|---|---|---|---|
| Quality of life (QoL) in psychological domains | Buruli ulcer/Ghana (144) | RCT | Full course (8 weeks) of antibiotic treatment 3-6 years (median = 5 years) prior | Good QoL in the psychological domain amongst former patients. No or only small effect of the disease on their current life. |
| Leprosy/Indonesia (145) | Cluster RCT (randomization of sub-districts) | Three stigma reduction interventions evaluated: (peer) counselling (5 sessions), socio-economic development (loans, business development, and/or other livelihood assistance), contact between community members and affected persons (“contact events” in the community); two interventions implemented in each sub-district (3 variations) vs. a control sub-district (SARI project) | No significant change in the psychological domain of QoL in intervention sites at 2-year follow-up compared to baseline (though there was a significant change in the environment domain of QoL and other outcomes) | |
| Leprosy/Indonesia (146) | Pre–post, mixed-methods | Stigma reduction counselling intervention (rights-based, underlying cognitive behavioral model, three types of counselling, incl. lay/peer counselling) (SARI project) | Significant improvement between baseline and 2-year follow-up in the psychological health domain of QoL | |
| Leprosy/Brazil (87) | Pre–post, quantitative | Three types of therapeutic workshops (arts, music, and recreational activities/games) on a weekly basis (2 hours long each) amongst institutionalized persons with leprosy (almost all elderly) over 6 months | Improved QoL in the psychological domain (also see depression outcome below) | |
| LF/India (147) | Pre–post, quantitative | 6-month-long simplified self-care integrative treatment | No improvement from baseline to 6 months in the psychological health domain of QoL (even when LF improved). 12.4% (n = 53) of affected persons were unable to regularly comply with treatment at home. | |
| Tungiasis/Kenya (39) | Cohort study (indirect evaluation of intervention) | Effective treatment for tungiasis amongst children | Improved QoL (sleep disturbance and concentration difficulties domains) | |
| Depression/depressive symptoms | Leprosy/Indonesia (93) | Pre–post, quantitative (poor study quality) | Cognitive behavioral therapy (CBT) | Depression rates significantly reduced (i.e., proportion of people with different severity levels of depression) |
| Leprosy/Brazil (87) | Pre–post, quantitative | Three types of therapeutic workshops (arts, music, and recreational activities/games) on a weekly basis (2 hours long each) amongst institutionalized persons with leprosy (almost all elderly) over a period of 6 months | Symptoms of depression reduced significantly after intervention: 21% did not have depression pre vs. 53.2% post; proportion of affected persons with moderate depression decreased from 54.8% to 17.7% (also see QoL outcome above). | |
| Anxiety | Leprosy/India (117) | Pre–post, mixed methods | Good nursing strategies and staff for female persons with leprosy admitted to a leprosy hospital for the first time | Significant reductions in anxiety levels in all age groups (pre: 18% had mild anxiety, 72% moderate anxiety, and 10% severe anxiety; post: 65% had mild anxiety, 30% moderate anxiety, and 5% severe) |
| General mental health outcomes | Leprosy/Nepal (148) | Pre–post, mixed methods | Empowerment project using self-help groups (RECLAIM project) (also see row below) | Improved self-efficacy overall (363 people reported higher self-efficacy, 90 no difference, and 29 lower self-efficacy) |
| Leprosy/Nepal (149) | Qualitative | Counselling (plus group meetings, self-care, raising social awareness, identification and referral of cases, access to government resources, home visits, advocacy for rights, follow-up, securing disability cards, and activities to reduce stigma) as part of RECLAIM project | Reported by facilitators of self-help groups to be one of the activities that had a direct impact on the burden of leprosy in their local communities | |
| Leprosy/Mexico (150) | Pre–post | Techniques with a cognitive behavioral focus, such as the directed imagination technique | Adaptation level score for self-concept improved | |
| Cognitive disability | LF/India (151) | Prospective cohort | Community-based lymphoedema management program | From baseline to 24 months: 13% decrease (statistically significant) in cognitive disability; reduced disability in domains: “getting along with others”, “life activities”, “difficulty participating in society”, and composite disability. 2.5 fewer work days lost per month on average at 12 months. |
| Patient information and concerns; staff interactions | Buruli ulcer/Benin (122) | Qualitative | A) Weekly education sessions, B) weekly open forum and bi-weekly follow-up ward meetings, C) individual patient counselling and therapy facilitation | A and C: increased information and reduced concerns for patients about their treatment and healing process; positive changes in staff-patient interactions, including communication B: improved problem-solving; patients with non-Buruli ulcer felt like they were being treated unfairly |
| Improved mood | Nodding syndrome/Uganda (85) | Case series | Antidepressants (imipramine), family and play therapy, supervised feedings and anticonvulsant therapy | Improvements, including in mood |
Studies evaluating interventions to address mental illness associated with NTDs or that measured mental health outcomes.
NTDs, neglected tropical diseases; RCT, randomized controlled trial; LF, lymphatic filariasis.
In total, 14 studies involved some evaluation of a relevant intervention—eight of these were for leprosy, two each for Buruli ulcer and lymphatic filariasis, and one each for nodding syndrome and tungiasis. Eight studies were from Asia, four were from Africa, and two were from the Americas. There were no studies for the other 16 NTDs that were included in this review, indicating that there is a very large gap in the evidence on interventions, almost certainly demonstrating a gap in actual services in place.
There were only two RCTs during the review period (1 January 2011 to 22 July 2018 for studies on mental health outcomes), both of which included assessments of the psychological health domain of quality of life: a long-term follow-up in Ghana of persons affected by Buruli ulcer with small lesions 3 to 6 years after a full course of antibiotic treatment (144), and a cluster RCT evaluating three different stigma reduction interventions for people with leprosy in Indonesia, counselling, socio-economic development, and contact (145). Whilst the RCT in Ghana reported good quality of life scores (significantly higher than healthy controls) on the psychological domain of the WHOQOL-BREF, the cluster RCT in Indonesia found no significant improvement in the psychological domain of the WHOQOL-BREF between baseline and 2-year follow-up (though it did show improvements in other outcomes). Other studies employed a pre–post design (n = 7) or were cohort studies (n = 2), qualitative studies (n = 2), or case series (n = 1).
There were few universal findings, mainly because of the scarcity of studies conducted and the variety in the types of interventions and outcomes employed. However, all but two of the 14 studies reported positive mental health outcomes, including improvements in the psychological domains of quality of life for leprosy (87, 146), Buruli ulcer (144), and tungiasis (39) [though two studies reported no improvements in the psychological aspects of quality of life (145, 147)]; reduced depression symptoms for leprosy (87, 93); reductions in anxiety levels and improvements in self-efficacy and self-concept for leprosy (117, 148, 150); lessened burden of leprosy (149); decreased cognitive and other disabilities for LF (151); improvements in patient information, patient–staff interactions, problem-solving, and reduced patient concerns for Buruli ulcer (122); and improvements in mood for nodding syndrome (85).
The only two outcomes that were assessed by more than one study were quality of life in psychological domains (n = 6) and depression/depressive symptoms (n = 2). Four studies found improvements in psychological quality of life: the RCT mentioned above on Buruli ulcer in Ghana (144); one from Indonesia that evaluated a stigma reduction counselling intervention for people affected by leprosy (146); one from Brazil that assessed arts, music, and recreation/games workshops amongst institutionalized leprosy patients (87) (150); and one that reported improved quality of life following effective treatment for tungiasis amongst children in Kenya (39). However, two studies found no improvements in the psychological health domain of quality of life: the cluster RCT from Indonesia mentioned above (145) and a pre–post study on a simplified self-care integrative treatment for persons affected by LF in India (147). Both studies that included depression/depressive symptoms as an outcome were on leprosy and reported positive results in Brazil (87) and Indonesia (93).
3.1.6 Implications of studies and recommendations made by their authors
Here we summarize some of the implications and recommendations on the link between NTDs and mental health made by the authors of the studies that were included in this review. Our own interpretations of the results are included in the “Discussion” section.
Within the authors’ reflections, the intervention topic was covered the most. With seven studies capturing information on interventions for lymphatic filariasis and a further six for dengue alone, this clearly is a topic that authors feel should have attention paid to. Most studies fit broadly across two categories. Firstly, early intervention was seen as core to reducing the impact of NTDs; this was found across studies for Buruli ulcer, dengue, leprosy, and trachoma. Secondly, the impact of integrating psychosocial care into healthcare more widely was reported as a key intervention to consider for six NTDs: Buruli ulcer, dengue, leprosy, lymphatic filariasis, nodding syndrome, and podoconiosis. The authors asked those designing interventions to include standardized measures such as quality of life to monitor the progress of affected persons. A leprosy study from Nigeria noted that the need for psychiatric evaluation cannot be overemphasized, which was confirmed by a study in China that found that focusing on mental health throughout leprosy treatment was a way to reduce suicidal thoughts in almost a quarter of affected persons. However, the authors clearly stated that whilst integrating psychosocial care is key, the wellbeing of affected persons also depends on the consistent distribution of medication, where appropriate.
Conclusions on implications for research were significantly fewer. Broadly, the authors highlighted the need to standardize measures in NTD and mental health research whilst expanding the scope of study techniques to include quasi-experimental or longitudinal studies and to broaden study populations. Additionally, authors researching chikungunya highlighted the need for further research into health-related quality of life, whereas objective measures of mobility for those with lymphatic filariasis were touted as a useful supplement to self-assessed quality-of-life questionnaires.
No study included in our review made recommendations on how to improve policies relevant to those with NTDs. This is a notable oversight and is an area that future research could focus on, both on the evidence needed to inform policy engagement and on the most effective ways of carrying out such engagement.
3.2 Neglected tropical diseases and stigma (Link 2)
3.2.1 Evidence included as part of the systematic mapping review
The review period for articles on NTDs and stigma was limited to articles published from 1 January 2015 to 22 July 2018 for NTDs other than leprosy and to articles published from 1 January 2013 to 22 July 2018 for leprosy, given that the evidence published previously has been summarized in other systematic reviews (9, 13).
After abstract and full-text review, we included 23 articles on the stigma associated with NTDs other than leprosy: six each on cutaneous leishmaniasis and lymphatic filariasis, five on podoconiosis, two each on Buruli ulcer and visceral leishmaniasis, and one each on Chagas disease and nodding syndrome. There were 16 studies from Africa, five from Asia, and two from the Americas.
We included 81 articles on the stigma associated with leprosy: nine studies from Africa, 56 studies from Asia, and 15 studies from the Americas. There was one multi-country study that included Bangladesh and DR Congo.
No articles were found during the review period on stigma for chikungunya, dengue, dracunculiasis (guinea-worm disease), echinococcosis, endemic treponematoses (e.g., yaws), foodborne trematodiases, human African trypanosomiasis (HAT or sleeping sickness), neurocysticercosis, rabies, schistosomiasis, soil-transmitted helminthiasis (STH), trachoma, or tungiasis.
The articles were coded according to different aspects of stigma, such as experiences of stigma faced by people with NTDs or their family caregivers, and stereotypes and attitudes towards people with NTDs; not all studies included had information on all these aspects of stigma.
3.2.2 Extent and burden of stigma associated with neglected tropical diseases
3.2.2.1 Experiences of stigma, discrimination, or social exclusion faced by people with neglected tropical diseases
Just over half of the articles contained information on how people affected by NTDs experienced stigma. There was a wide range of experiences reported, with most evidence available for leprosy (45 papers) and a small number of papers on stigma experience in people with lymphatic filariasis (six), cutaneous leishmaniasis (five), podoconiosis (four), Buruli ulcer (two), visceral leishmaniasis (two), or Chagas disease (one).
The findings on NTDs other than leprosy were analyzed firstly to identify sub-themes of stigma experience present across various diseases (marked in italics in the paragraphs below). These themes were then cross-checked for saturation against the themes present in the much larger literature on stigma experiences amongst people with leprosy. Table 4 outlines sub-themes identified on stigma experience and key findings across NTDs.
Table 4
| Sub-themes of stigma experience and outcome categories | Found for which disorders | NTDs other than leprosy | Leprosy |
|---|---|---|---|
| (types of experiences) | (number of studies in brackets) | Main findings including references | Main findings including sample references |
|
Experiences of stigma and discrimination enacted by others
Negative reactions from others, social exclusion and violation of rights (devaluing comments, mocking, labelling, teasing, exclusion and avoidance, including from family members; violation of human rights) |
Cutaneous leishmaniasis (CL) (3), lymphatic filariasis (LF) (2), nodding syndrome (1), podoconiosis (3), leprosy (34) | CL: social exclusion, broken relationships, interpersonal conflict (152, 153), isolation, rejection (43), “stigma worse than the disease itself” (154) LF: social isolation, called names, being excluded from family meals, etc. (131), shunned, embarrassing stares, reduced social interactions (80) Nodding syndrome: mocking and avoidance (132) Podoconiosis: widespread discrimination from community (155–157), excluded from social gatherings, school, and church; being denied house rental (156), exclusion, avoidance, pointing/gesturing (157) |
Types of experiences: avoidance/isolation (very common), physical distancing due to fear of contagion, exclusion, abandonment, forced to leave the family, and forced to move to a leprosy colony; losing friendships; labelling (even when cured),being identified as “different”, treated with less respect, criticism; negative reactions from family members: avoidance, not allowed to share rooms with family, refrained from touching others, separate eating utensils, refrained from cooking, opinion not counted in family discussions, considered untouchable by family members (India) (158); not taken for treatment by family members, expulsion from the family; being prohibited from leaving home; discrimination; abusive behavior from school teachers and peers at school, violation of personal rights: forced removal from homes (mandatory admissions) (Brazil) (89), right to access to medical care, work, and education frequently disrespected and violated (111); forced deportation from Kuwait (159); social participation restrictions such as not participating in major festivals, barred access to public services; affected children denied admission to schools |
| Impact on marriage (reduced marriage prospects or impact on existing marriage; impact on intimate relationships) | Buruli ulcer (1), CL (2), LF (3), leprosy (9) | Buruli ulcer: difficulties engaging in intimate relationships (particularly in those with higher physical, social, and psychological limitation scores) (98) CL: reduced marriage prospects particularly affecting young women and those with facial scars (119, 153) LF: reduced marriage prospects (80, 131, 160), reduced quality of marital relationships (80, 160) |
Types of experiences: perception of reduced marital prospects (161): very common Anticipated stigma and marriage (109): not even considering marriage due to anticipation that no one would accept them Remarriage: most people affected remarried after moving to leprosy colony and started a new family (India) (158) Impact on intimate relationships (described mostly for affected women) (136, 162): being teased for changed appearance due to steroid medication by husband, negative consequences for sexual relationship, sleeping in separate beds, rude behavior by husband, being abandoned by husband, being sexually abused by husband |
| Impact on work | CL (1), LF (1), podoconiosis (2), leprosy (16) | CL: reduced chances of getting employment (153) LF: earnings of people with LF less than half compared to controls (49) Podoconiosis: discrimination from employers (156), refusal of marketing in various settings (157) |
Types of experiences: difficulties finding employment; job loss (93, 110, 161, 163): having to change jobs, particularly those with deformity, pushed into poverty due to job loss. Discrimination at work (89, 161), e.g., verbal abuse at work; internalized stigma (136, 164): anticipated stigma so almost all participants hiding their illness from work colleagues; low self-esteem and insecurity about being able to perform at work; children also affected (158) by their parent’s disease in the field of employment; being forced to practice begging as their sole means of livelihood |
| Discrimination in healthcare | Buruli ulcer (1), leprosy (4) | Buruli ulcer: hospital inpatients given very little information about their illness, feeling treated disrespectfully, staff experienced as unsympathetic and unapproachable (122) | Types of experiences: stigmatizing behavior by health professionals, e.g., medical staff labelling patients as non-compliant or uncooperative (107), fearful attitudes towards those affected, telling those affected to hide diagnosis even from other health professionals (Brazil) (113); structural aspects, e.g., no counselling services available for people with leprosy. Several studies found that healthcare workers’ stigmatization was impactful (Ghana) (164, 165) |
| Experiences of internalized stigma (including stereotypes applied to the self, anticipated discrimination, concerns about others finding out and consequences such as attempts to hide the illness, social withdrawal, shame, and low self-esteem) | Buruli ulcer (1), CL (4), LF (3), nodding syndrome (1), podoconiosis (1), leprosy (32) | Buruli ulcer: avoidance of certain social situations, recreational pursuits and leisure due to anticipated stigma (98) CL: hiding lesions for fear of stigma and reduced marriage prospects (43, 119); loss of self-esteem, feelings of inferiority, shame (153); “psychological stigma” (154), avoiding places and keeping a distance (152) LF: social withdrawal (80); 73% reporting low self-esteem (81), concerns about others finding out; embarrassment (160) Nodding syndrome: anticipated discrimination leading to children avoiding school (132) Podoconiosis: internalized stigma and anticipated discrimination due to beliefs about contagion; avoiding social events (166) |
Types of experiences: internalized negative beliefs (110): thinking less of oneself, holding beliefs that leprosy has to do with past sins, adopting a posture of self-punishment (Brazil) (105) Shame; low self-esteem and feelings of inferiority (161, 167), also affect access to education and confidence at work, feeling like a burden to the family; feelings of inferiority attributed to forced isolation in a sanatorium in China (167) Anticipated stigma (146, 168): worries about losing job if illness disclosed; consequences of anticipated stigma: hiding the illness, including from close family members; avoiding meeting friends; self-isolation from family members, friends, avoidance of social gatherings (169) or keeping away from workplace for fear of transmission, anticipated stigma or shame; avoidance of touching others. Stigma attached to leprosy-related disabilities motivating people affected to carry out plantar ulcer care (170) |
| Perceived stigma (being aware of societal stigma without necessarily having experience) | Leprosy (10) | No studies during review period | Perception that people with leprosy are stigmatized and discriminated against (89, 90, 127, 171–173), for example, that employers do not offer them work or that people dislike buying food from them; perception of high societal stigma impeding confidence to look for work, despite lower levels of restrictions experienced; perception that people with leprosy are neglected because others believe they have not been cured |
| Social participation restrictions, weakening of social bonds | Buruli ulcer (1), leprosy (3) | Buruli ulcer: ability to socialize and enjoy leisure activities adversely affected because of immobility, social stigma, and isolation (98) LF: lower social participation scores than unaffected peers (49) |
Children affected by leprosy discontinuing their studies or staying at home (China) (174); in two studies in India, 25% (175) and 53% (90) of people with leprosy suffered participation restrictions |
| Reduced quality of Life (QoL) in the social domain | LF (2), leprosy (2) | LF: lower overall QoL than unaffected peers (49); poorer social functioning than healthy controls (130) | Lower QoL in the social domain in those with visible deformity in India (70); lower QoL in those affected found in a study in Brazil (65) |
| No stigma or stigma a relatively minor problem | Chagas disease (1), CL (2), leprosy (4) | Chagas disease: people affected had relatively good social support (41) CL: lowest impact on QoL observed for the personal relationship domain (India) (44). 84% of participants did not experience enacted stigma, but some experienced anticipated stigma (Suriname); attributed to CL in Suriname rarely causing facial disfigurations; most of the sample was male (152) |
Examples:
- In Malaysian study, no evidence that Orang Asli leprosy patients (indigenous community) had been stigmatized or excluded by their communities (107) - In one Indonesian study, internalized stigma was a minor but relevant challenge only for a few participants (176) In one Indian study, most children and adolescents had a positive attitude towards having leprosy (177). In Brazil, three-quarters of the sample presented no effective restrictions (178) |
| Courtesy stigma (caregivers’ own experiences of stigma by association with person affected by the NTD) | Nodding syndrome (1), leprosy (5) | Nodding syndrome: family caregivers worried about being blamed for bringing disease to the area (132) | Types of experiences: children of people affected by leprosy facing social problems in the community (161), being denied admission to regular schools (158), or feeling stigmatized, which led to self-isolation (179); adult family caregivers in Ghana being labelled and having limited opportunities for social interactions outside the leprosarium and limited opportunities for getting jobs (163); less than 6% of family caregivers experiencing discrimination in one Indian study (180) |
| Impact of stigma experiences on mental health, wellbeing and social outcomes | LF, CL, visceral leishmaniasis (VL), nodding syndrome, leprosy | LF: hurtful experiences of discrimination: “My family members don’t take meals with me. I have to eat separately. This is really hurting me” (131); stigma and exclusion culminated in difficulties with social participation and reduced aspirations (80) CL: social limitations due to stigma contributed to mental impact (43) VL: having no social support associated with low QoL in psychological, social, and environmental domains of HIV–VL-coinfected patients (47) Nodding syndrome: children often being absent from school due to experienced and anticipated discrimination (132) |
Examples of experiences reported:
- “I am denied respect, and the community’s behavior robs me of my self-esteem. The community wrenches me out of my network of relationships and compels me to live a life of desolation and solitude.” (India) (181) - “The consequences of stigma can be indeed brutal and subtle. They are brutal, in particular, when self-isolation, self-mutilation or suicidal thoughts are encountered; subtle, when things are less visible” (Indonesia) (106) - Contemplation of suicide due to stigma and discrimination (Ghana) (165) - Impact of leprosy stigma on behavior (169): feelings of pessimism and a lack of motivation - Concealment as “coping strategy increasing negative feelings and emotions (sadness, shame, fear) and internalized stigma” (106) |
Experiences of stigma and discrimination faced by people with NTDs or their family members.
NTDs, neglected tropical diseases.
One of the most salient themes identified (in terms of presence across different diseases and the number of studies describing it) pertained to experiences of stigma and discrimination of people affected by NTDs reported having experienced from others, for example, in the form of exclusion and avoidance, devaluing comments, mocking, labelling, teasing, and violation of human rights. A few studies directly measured social participation restrictions.
Experiences of stigma were common and burdensome to people with NTDs; for example, a study amongst people with lymphatic filariasis in Nigeria found that nearly all respondents revealed emotionally burdensome experiences of stigma such as being shunned, receiving embarrassing stares and insults, or being viewed as inferior (80). Particularly salient across studies was the impact of stigma on work opportunities and marital relationships and marital prospects.
Sources of enacted stigma were members of the general public, and also people close to the person with the NTD, often their family members. A small number of studies looked at discrimination in healthcare, which was described for leprosy and Buruli ulcer.
Strikingly, internalized stigma with manifestations such as internalized stereotypes, anticipated discrimination, concealment of illness, shame, low self-esteem, and self-isolation was equally salient as experienced stigma in the studies we examined. A few studies on leprosy also described perceived stigma amongst people affected by leprosy, i.e., the degree to which they were aware of population attitudes being negative towards them due to their conditions.
Reduced quality of life in the social domain was another outcome measured in a few studies on leprosy and lymphatic filariasis. A small number of studies also reported that they found no or very little evidence of stigma; for example, one study found leprosy stigma to be virtually absent in an indigenous community in Malaysia (107). Six articles described courtesy stigma, i.e., experiences of stigma faced by the family members of those affected by NTDs.
Many studies reported directly or indirectly on the impact of stigma experiences on mental health, wellbeing, and social outcomes. They illustrated, for example, how emotionally hurtful experiences of exclusion and discrimination were, particularly when enacted by family members, and how stigma drove people into isolation, shame, low self-esteem, and depression. They reported how stigma led to feelings of pessimism, lack of motivation, and, often, contemplation of suicide. Concealment as an attempt to cope with stigma in turn reinforces negative emotions such as sadness, shame, and fear and leads to increased isolation.
3.2.2.2 Stereotypes and negative attitudes towards people affected by neglected tropical diseases
Articles further described stereotypes and negative attitudes towards people with NTDs found amongst community members or health staff. We found slightly less information on this than on experienced stigma faced by those affected, which is partly due to the fact that we excluded papers on knowledge, attitudes, and practices relating to NTDs if they did not specifically relate to the concept of stigma in the sense of social devaluation (for example, articles examining illness beliefs and attitudes with the aim of improving the acceptability of mass drug administration (MDA) programmes).
A total of 65 articles contained information on stigmatizing stereotypes and attitudes towards people with NTDs. Most evidence was available for leprosy (45 papers) and a small number of papers on stigma experience in people with lymphatic filariasis (6), cutaneous leishmaniasis (5), podoconiosis (4), Buruli ulcer (2), visceral leishmaniasis (2), or Chagas disease (1).
As for experienced stigma, the findings on NTDs other than leprosy were analyzed firstly, and sub-themes were then cross-checked against the larger literature on stigma towards people with leprosy. Table 5 outlines the sub-themes identified and key findings across NTDs.
Table 5
| Sub-themes of public stigma identified | Categories | Found for which disorders | NTDs other than leprosy | LeprosyMain findings |
|---|---|---|---|---|
| (numbers of studies) | Main findings | Main findings | ||
| Stereotypes held about the condition or the people affected | a) Fears of contagion, infectious b) Dirty, unclean, foul smelling, unattractive c) Scary, poorly understood d) Incurable e) Caused by supernatural causes/divine curse (leprosy) f) Dependence on charity, not contributing (leprosy) |
Cutaneous leishmaniasis (CL) (1), lymphatic filariasis (LF) (1), nodding syndrome (1), podoconiosis (1), leprosy (7) | a) Fears of contagion, seen as infectious disease: CL (102), nodding syndrome (132), podoconiosis (166) b) People affected viewed as dirty or foul smelling: LF (80) c) Scary, poorly understood illness: LF (80), podoconiosis (166) d) Incurable: LF (80) |
People affected viewed as unclean, unattractive, and dependent on charity. Presence considered disruptive (181) Incorrect beliefs relating to incurability or heredity (182) Beliefs that the illness is caused by supernatural causes or a divine curse (163, 180). This view held more commonly in low-endemic areas (145) Healthcare providers held the view that food was a specific cause of leprosy in Suriname (183) |
| Negative attitudes towards people affected | a) Desire for social distance b) Negative attitudes towards marriage of people affected c) Shame or incrimination d) Unwillingness to participate in healthcare education amongst health staff (leprosy) |
CL (1), LF (2), podoconiosis (1), leprosy (5) | a) Desire for social distance: LF (80), podoconiosis b) Negative attitudes towards marriage of people affected: podoconiosis (166), CL (119), LF (160) c) Shame or incrimination: CL (119), LF (160) |
High scores of stigmatizing attitudes towards those affected by leprosy (161), people maintaining a social distance from them Family members not allowing leprosy patients to share the room with other members of the family (180) Healthcare staff unwilling to participate in healthcare education (184) |
| Perceived stigma towards people affected by NTDs | CL (1), visceral leishmaniasis (VL) (1), LF (1), leprosy (3) | CL: perceived to lead to stigma and social isolation and avoidance by family members (119) VL: seen as associated with stigma (185) LF: perceived as leading to avoidance, marital and relationships |
Perceptions that leprosy would cause marital problems for those affected, or that those affected would make other community members feel uncomfortable and avoid them (160) Awareness that leprosy-afflicted people undergo a double burden: the condition and the attitudes of community members (186) Perceptions that people with leprosy and their families face difficulties getting employment, admission to school, or getting married themselves; bringing shame to the family (187) |
|
| No or little community stigma | CL (2), LF (1), leprosy (1) | Strong reactions seen as natural and not indicative of stigma: CL (152) Stigma in the community reported to have improved: LF (131), CL (119) |
Community members also showed their concerns and expressed their sympathies towards people with leprosy in different ways (170) |
Stereotypes and negative attitudes towards people affected by NTDs held by community members or healthcare workers.
NTDs, neglected tropical diseases.
Articles across several diseases (leprosy, cutaneous leishmaniasis, lymphatic filariasis, nodding syndrome, and podoconiosis) described stereotypes or stigmatizing beliefs held about the illness or people affected, such as the notion that people affected were contagious, unclean, or not contributing to society or that the illness was incurable, scary, or caused by supernatural forces. The number of articles found was too small to compare stereotypes held on each disease, but several stereotypes were found for several of the NTDs mentioned above.
Similarly, negative attitudes towards people with NTDs were reported for cutaneous leishmaniasis, lymphatic filariasis, podoconiosis, and leprosy. This manifested in a desire for social distance, negative attitudes towards marriage of people with NTDs, feelings of shame and incrimination, or negative attitudes towards attending respective health education, for example. A number of papers reported attitude scores rather than qualitative information on attitudes.
A small number of studies (for leishmaniasis (cutaneous and visceral), lymphatic filariasis, and leprosy) reported on perceived stigma, i.e., community members being aware of people affected by NTDs being avoided, excluded, and discriminated against. Two studies on cutaneous leishmaniasis, one on lymphatic filariasis, and one on leprosy found no or little evidence of public stigma.
3.2.3 Postulated mechanisms by which neglected tropical diseases may lead to stigma
The postulated mechanisms (factors for which there is a plausible yet unproven causal relationship with stigma) and other associated factors that may lead to experienced stigma and public stigma are summarized in Tables 6, 7, respectively.
Table 6
| Themes | Mechanisms | NTD | Main findings | Summary | Additional information |
|---|---|---|---|---|---|
| Experienced stigma (subjective experience of stigma amongst people affected by NTDs) | |||||
| Biological factors | Visible illness manifestations | Leprosy, cutaneous leishmaniasis, Buruli ulcer, lymphatic filariasis | Three quantitative studies and one mixed-method study reported strong evidence, concerning leprosy (110, 188, 189) and cutaneous leishmaniasis (152). Seven qualitative studies supported the association, concerning cutaneous leishmaniasis (102, 119), Buruli ulcer (98), lymphatic filariasis (80), and leprosy (164, 165, 190). No study reported conflicting findings or no association | More disfigured appearance and unpleasant characteristics led to higher levels of experienced stigma, in all studies identified, including quantitative and qualitative studies | Facial involvement, particularly, more commonly resulted in experienced stigma, which could be explained through Goffman’s theory of “spoiled identity” as face stands for one’s identity (152) |
| Level of disability | Leprosy, Buruli ulcer, Chagas disease, lymphatic filariasis, podoconiosis, chikungunya | One cluster randomized controlled trial on leprosy reported strong evidence (191). Six quantitative studies and one mixed-method study reported strong evidence concerning leprosy (136, 172, 173, 175), Chagas disease (41), and podoconiosis (70). Six qualitative studies supported the association, concerning leprosy (165, 169, 170, 190),lymphatic filariasis (80), and chikungunya (192). Social participation restriction is caused by physical disability and flare-up frequency (36, 41, 70, 80, 90, 134, 137, 173, 175, 190, 192–194), including vitality loss as in case of chikungunya (192). A study on Chagas disease hypothesized that restriction is reflected in the ability to eat, with social salience for sharing meals (41). A qualitative study on leprosy suggested wound care facilitated social participation (170) |
Higher levels of disability led to higher level of stigma and social participation restriction, supported by all studies identified, including both quantitative and qualitative studies | Persisted self-image as a “sick person” amongst the leprosy-affected individuals even after the declaration of being cured, which resulted in feeling discomfort and having deformities No study reported conflicting findings or no association (169) |
|
| Psychological factors | Fear of transmission | Leprosy | One quantitative study on leprosy reported strong evidence (188) | Fear of transmission led to higher levels of experienced stigma. Only one study identified | |
| Knowledge | Leprosy, cutaneous leishmaniasis | Three quantitative studies reported strong evidence (172, 188, 189) and one qualitative study supported the association (169). All focused on leprosy. A quantitative study on cutaneous leishmaniasis favored no association (153) | Studies on leprosy supported that lack of knowledge of the disease led to higher level of experienced stigma | Studies on other NTDs are scant | |
| Public stigma (stereotypes and negative attitudes towards people with NTDs) | |||||
| Psychological factors | Fear of transmission | Podoconiosis, cutaneous leishmaniasis, leprosy | One quantitative study on podoconiosis in Ethiopia reported strong evidence (155). Seven qualitative studies supported the association, in cutaneous leishmaniasis (119, leprosy (133, 195–197), and podoconiosis (156, 166) | Fear of transmission led to more stigmatizing attitudes, supported by predominant qualitative evidence | Frequently reported beliefs in transmission mechanisms include saliva, air, or skin contact (132) No study reported conflicting findings or no association |
| Poor knowledge about the illness | Leprosy | One quantitative study reported strong evidence (198), and two qualitative studies supported the association (184, 190). All focused on leprosy. No study reported conflicting findings or no association | Studies on leprosy found that lack of knowledge surrounding the disease led to more stigmatizing attitudes | No study on other NTDs identified | |
| Social factors | Illness beliefs | Leprosy, podoconiosis | One quantitative study reported strong evidence (198), and two qualitative studies supported the association (165, 184). All focused on leprosy. Local beliefs investigated include God’s punishment, witchcraft, curses, or evil spirits For belief in the hereditary nature of podoconiosis, one quantitative study reported strong evidence (155) |
Different NTDs have their own specific local beliefs linked to stigmatizing attitudes For leprosy, God’s punishment, witchcraft, curses, or evil spirits led to stigmatizing attitudes, whilst for podoconiosis, it is the belief in the hereditary nature |
|
| Contact duration | Leprosy, leishmaniasis, podoconiosis | One quantitative study on leprosy reported strong evidence (198). One qualitative study on cutaneous leishmaniasis supported the association (119). In a study on podoconiosis, no association found between the length of the community–NGO relationship and stigma (155) | Longer contact duration by the public with people affected is associated with less stigmatizing attitudes | ||
Postulated mechanisms leading to experienced stigma and public stigma.
NTD, neglected tropical disease; NGO, non-governmental organization.
Table 7
| Themes | Mechanisms | NTD | Main findings | Summary | Additional information |
|---|---|---|---|---|---|
| Experienced stigma | |||||
| Demographic factors | Age | Leprosy, cutaneous leishmaniasis, LF | Four quantitative studies reported strong evidence of leprosy (136, 175), cutaneous leishmaniasis (153), and lymphatic filariasis (130). Two quantitative studies on leprosy reported limited evidence (178, 188) | Advanced age is associated with higher levels of stigma | |
| Gender | Lymphatic filariasis, Buruli ulcer, podoconiosis, leprosy | Three quantitative studies reported strong evidence of gender links concerning lymphatic filariasis (130), Buruli ulcer (193), and podoconiosis (155), as did one mixed-method study (152). One qualitative study (119) on cutaneous leishmaniasis supported an association Five quantitative studies on leprosy reported limited evidence (136, 172, 173, 178, 188) One cluster randomized controlled trial on leprosy reported strong evidence for larger improvement in stigma scores after an intervention amongst female participants (191) |
Female gender is likely to be associated with higher levels of stigma, whilst evidence is weaker for leprosy and Buruli ulcer Female participants may benefit more from stigma reduction interventions |
Disproportionally fewer female participants were proposed as the explanation for the lack of statistical evidence (136, 152). For diseases with visible involvement, particularly the face, stigmatization amongst female participants may be more prominent, resulting in further impacts such as marriage rejection in certain cultures (119) | |
| Socio-economic status | Education | Leprosy, lymphatic filariasis, cutaneous leishmaniasis, chikungunya | Four quantitative studies reported strong evidence for the association between lower educational levels and higher levels of leprosy stigma (136, 172, 199) and lymphatic filariasis (130). Three quantitative studies favored no association between leprosy (178, 188) and cutaneous leishmaniasis (153). One qualitative study on chikungunya supported the association | Conflicting findings exist | Most of the studies reporting little association were conducted with highly homogeneous groups regarding gender or educational level |
| Employment and finance | leprosy | Three quantitative studies reported strong evidence (188, 189, 199), whilst one reported no association (172). All focused on leprosy A qualitative study assessing the effectiveness of a socio-economic intervention for persons with leprosy reported beliefs in the reduction of stigma levels and stigmatizing attitudes by socio-economic status improvement (114) |
Unemployment or occupational change due to the disease is associated with higher levels of stigma Socio-economic status improvement may reduce stigma levels |
||
| Occupational variation | Leprosy | One quantitative study on leprosy reported occupational variation (188) | Occupational variation existed | ||
| Psychological factors | Mental disorder | Leprosy, Chagas disease | A quantitative study on leprosy reported weak evidence (200) The researcher of a study on Chagas disease suggested depressive symptoms may explain the association between gastrointestinal discomfort and social isolation (41) |
Weak evidence supported association between depressive symptoms and stigma Depressive symptoms may contribute to gastrointestinal discomfort |
|
| Social factors | Regional or institutional variation | Leprosy | One quantitative study on leprosy reported regional or institutional variation (189) | Regional or institutional variation existed | |
| Stigmatizing attitudes | |||||
| Demographic factors | Age | Leprosy | A quantitative study on leprosy reported strong evidence for more stigmatizing attitudes amongst older participants (198) | Conflicting findings exist | |
| Gender | Leprosy, onchocerciasis | A quantitative study focusing on health workers for leprosy reported strong evidence for less stigmatizing attitudes amongst male participants (196) A quantitative study on onchocerciasis reported limited evidence (153) |
Male health workers showed less stigmatizing attitudes. Evidence for general populations is limited | ||
| Socio-economic status | Education | Leprosy | Two quantitative studies on leprosy reported strong evidence (196, 198). No study reported conflicting findings or no association | Lower educational level associated with more stigmatizing attitudes in all studies | |
| Occupational variation | Leprosy | For leprosy, one quantitative study (198) and one qualitative study (180) reported variation | Occupational variation existed | ||
| Social factors | Regional or institutional variation | Leprosy | One quantitative study (196) and one qualitative study on leprosy (180) reported regional or institutional variation | Regional or institutional variation existed | |
Other factors associated with experienced stigma and public stigma.
NTD, neglected tropical disease; LF, lymphatic filariasis.
Most research on postulated mechanisms and associated factors concerned demographic factors and socio-economic status, followed by psychological factors. Social factors were little investigated. Leprosy is the most studied disease, but the findings were inconsistent. For postulated mechanisms leading to higher experienced stigma, the strongest evidence was found for biological factors, including a more disfigured appearance and a higher level of disability. A higher level of disability was also associated with higher social participation restrictions. The findings were consistent across various NTDs, with no study reporting conflicting results. For psychological factors, studies focused mostly on leprosy, supporting the association between a lack of knowledge and higher levels of stigma.
Advanced age and female gender were associated with higher levels of experienced stigma. However, several studies on leprosy reported limited evidence of association, and the findings on associations with socio-economic status, particularly education, were also inconsistent.
For postulated mechanisms leading to public stigma, the strongest evidence found concerned psychological factors, including lack of knowledge and fear of transmission. Different NTDs have their own specific local beliefs linked to more stigmatizing attitudes, surrounding religious or magical topics such as punishment by God or witchcraft in leprosy in several countries, or a focus on heredity in podoconiosis in Ethiopia. Longer contact duration reduced stigmatizing attitudes. Some evidence supported the role of lower educational levels in public stigma. The findings for demographic factors such as age and gender are more inconsistent.
3.2.4 Link 2 reversed: Impact of stigma on the treatment and outcome of neglected tropical diseases
As in the section on NTDs and mental health, a substantial limitation in our endeavor to better understand the association between NTDs and stigma outcomes was that several studies were cross-sectional in nature, making it difficult to ascertain the directionality of any association. Nevertheless, given that most of the research reported (see the section under postulated mechanisms) assumed or described an association where NTD-related factors led to stigma and discrimination, we thought it useful to examine evidence on how stigma may influence NTD-related outcomes. Overall, we identified 16 studies that looked at the impact of stigma on leprosy outcomes and six studies across four other NTDs (Buruli ulcer, podoconiosis, cutaneous leishmaniasis, and visceral leishmaniasis) on the impact of stigma on the treatment and outcome of those NTDs.
Stigma was found to have a negative effect on health seeking and treatment uptake in several studies on leprosy, one study on Buruli ulcer, and one on podoconiosis. It was defined as a limiting factor in willingness to seek care for leprosy in Ghana (184) and amongst people with leprosy in Indonesia (169). Relating to Buruli ulcer, a study from Ethiopia (156) found that stigma led to barriers to attendance for treatment mediated by failure to access accommodation and basic services, such as water supplies. Behind this was a popular belief that the disease was contagious and discomfort about the smell. The study reported that “some family members prevented children or other dependents from using the treatment supplies they collected from the (…) outreach clinics because of the discomfort they feel about the smell.” In another study from Ethiopia, on podoconiosis (166), internalized illness beliefs emphasizing heredity and not acknowledging the role of the environment and preventability were found to lessen the likelihood of people wearing protective shoe wear.
Stigma was also found to delay treatment and affect treatment adherence. In a study from Brazil, participants who suspected they had leprosy but feared community isolation were 10 times more likely to wait longer before consulting a doctor for their symptoms (197), meaning that often patients presented later before getting treatment. Majumder (158) came to a similar conclusion in India. Highlighting a similar point, an Indonesian study found that social capital could increase treatment adherence (128).
However, stigma may also act as a motivating factor for treatment, as suggested by a study by Bennis et al. (2017) (102). This found a clear demand for better treatment amongst people affected by cutaneous leishmaniasis, which was attributed to fears about scar-related stigma. The loss of social support and social engagement, for example, as a result of stigma was found to affect the overall quality of life of people affected by visceral leishmaniasis in two studies in Ethiopia (46, 47).
3.2.5 Evidence for interventions to reduce neglected tropical disease-related stigma
For leprosy, 19 studies investigating interventions to reduce stigma and discrimination were identified, of which 11 were conducted in Indonesia. Two studies were identified for podoconiosis (166, 201) and one for Buruli ulcer (122). No study on interventions to reduce stigma and discrimination were found for Chagas disease, chikungunya, dengue, leishmaniasis (cutaneous and visceral), lymphatic filariasis, neurocysticercosis, onchocerciasis/nodding syndrome, schistosomiasis, trachoma, or tungiasis. See Table 8 for an overview of the interventions aiming to reduce stigma for persons affected by NTDs identified in our review.
Table 8
| Invention | NTD/country | Study design | Main findings |
|---|---|---|---|
| Interventions using multiple strategies simultaneously | |||
| 1. Peer and lay counsellors applied cognitive behavioral therapy using a Rights-Based Counselling Module (RBCM) (146) 2. The SED intervention addressed financial situation improvement, self-esteem establishment, skills acquisition, and access to public regions with microloans, business training or other support 3. Contact events were organized for interactions between community members and individuals affected (186) |
Leprosy/Indonesia | Cluster randomized controlled trial (145), with quantitative, qualitative (168, 176, 202) and mixed-method (146, 186) evaluations | 1. Stigma and participation restrictions were reduced in all intervention arms (either two of the three interventions) of the cluster randomized controlled trial (145) 2. Statistical evidence supported reduction in stigma domains by peer and lay counselling, including experienced stigma, disclosure concerns, internalized stigma, and anticipated stigma (146). Knowledge sharing was most effective through peer and lay counselling (168). The process of conscientization promoted transformation at individual, family, and community levels (146, 202) 3. Social distance and social stigma were reduced by contact intervention (145, 186). The events also formed new social identities and promoted focus on helping others (176) |
| Leprosy eradication project conducted by the Danish International Development Agency’s Leprosy Unit (DANLEP): 1) festivalization of health: incorporate information and messages into cultural and religious events; 2) trialogue strategy: engaging three main stakeholders with a mixed-group residential camp: persons with leprosy, leprosy workers, and community members; 3) a 3-month volunteer campaign for stigma reduction and treatment of leprosy | Leprosy/India | Field experience | 1) Data from the field essential for identifying social issues and community interests. 2) Actions required flexible and open plans. 3) Support from the health department and authorities was critical. 4) Project team comprised “leprologists, medical doctors, behavioral scientists, communications, leprosy workers and persons released from treatment (RFT)”. 5) Social and human resources actively identified and mobilized. 6) Field workers should be equipped with good “social engineering skills”. 7) The service should be delivered based on the principles of “Show, Do and Tell”. 8) New vocabularies diminished stigma and conveyed novel and positive meanings (181) |
| Perspectives obtained from semi-structured face-to-face interviews | Leprosy/Brazil | Qualitative | The following factors improved the attitudes towards leprosy: 1) abolition of compulsory isolation, 2) the introduction of MDT and vaccination, and 3) contact tracing and public health campaigns on media such as television adverts The use of “Hansen’s disease” as official name helped separate it as a treatable dermatological illness rather than a biblical one The advance in medical care promoted the belief that the illness was curable and thus reduced the fear in the population (89) |
| A pilot project consisting of three interventions: 1) education sessions, 2) weekly open-forum and bi-weekly follow-up ward meetings, and 3) patient counselling and therapy facilitation | Buruli ulcer/Benin | Qualitative | 1) Individual counselling and weekly education sessions. 2) Individual counselling for the affected individuals and therapy facilitation for the medical professionals. 3) Open forums and patient representative meetings facilitated understanding, communication, and constructive problem solving (122) |
| Information, education, and communication/health education/awareness raising | |||
| Teenager health multipliers on leprosy awareness with the five culture circles based on Paulo Freire method: 1) definition and transmission of leprosy; 2) characteristics and diagnosis of leprosy; 3) treatment of leprosy; 4) aesthetics, prejudice, and mental health related to leprosy; and 5) planning of educational activities for teenagers as health multipliers on leprosy awareness | Leprosy/Brazil | Qualitative | This active methodology encouraged teenagers in self-perception, dissemination of the knowledge surrounding leprosy, and political actions in the development of culture circles, ensuring the autonomy and major roles of teenagers in the reduction of stigmatization (203) |
| Health education provided by the National Leprosy Eradication Programme | Leprosy/India | Descriptive data, quantitative | 91.1% of participants possessed adequate knowledge after receiving the health education provided by the National Leprosy Eradication Programme (162) |
| Information and knowledge sources: NGOs, including auxiliary nurse midwife (ANM) and accredited social health activist (ASHA), and media such as television | Leprosy/India | Qualitative | People in highly prevalent regions obtained information from ANM and ASHA. Stigma and discrimination were reduced, and knowledge was disseminated through NGOs and the government health system. Where less prevalent, people obtained information from television, and the level of stigma was high. Information, education, and communication are required (180) |
| Providing a pocketbook to local traditional healers, “Tabibs”, which contains information about the identification, management, and treatment of leprosy and a training programme | Leprosy/Indonesia | Quasi-experimental | This approach was found to be effective in raising knowledge, improving attitudes, and reforming the self-image of the traditional healers who could take a potential role in healthcare and control of leprosy (204). |
| Three intervention arms: 1) usual care health education (UC), 2) household-based skills training (HB) and community awareness campaign (CAC), or 3) HB and CAC plus a genetics education module (GE) | Podoconiosis/Ethiopia | Cluster randomized control trial, with both qualitative and quantitative evaluations | 1) Usual health education alone may be as effective in experienced and enacted stigma reduction as HB and CAC at 3 and 12 months (201). 2) Only marginal evidence supported GE to be superior in enacted stigma reduction at 12 months in a cluster RCT conducted with caregivers (201). 3) Lay health educator (LHE)-delivered inherited susceptibility education module (ISEM) boosted confidence and social participation of families (166) |
| Disease management—reconstructive surgery | |||
| Reconstruction surgery | Leprosy/India | Mixed methods | More than 85% of participants were very satisfied with the acceptance of their family, friends, relatives, and society. Self-esteem increased (205) |
| Personal support interventions—counselling | |||
| The SCARED programme was designed to give a set of skills: REACHOUT; Reassurance, Effort to appear interested, Assertiveness, Courage to take small steps, Humor, Out There for attention shifting, Understanding the feelings of others, Try Again (206) | Leprosy/India | Qualitative | All participants built self-esteem and improved social interaction with the community. Group training rather than individual one was found to be more successful and less time-consuming. The recruitment of leprosy-affected individuals as role models appeared to be powerful (206) |
| Personal support interventions—peer groups | |||
| SCGs (self-care groups), focusing on wound healing and disability worsening, self-esteem promotion, and economic activities development | Leprosy/Mozambique | Descriptive data, quantitative | Perceived benefits reported by the majority of the participants (>70%) included “better care of disabilities and wounds”, “ability to fight for rights”, and “socializing and meeting with friends”. Others included “economic benefits”, “to have fun and enjoy together”, “to receive sandals”, “better care of the eyes” and “an opportunity to go out of the house”. Income generation and transportation are main challenges (207) |
| Integrated self-help groups | Leprosy/Nepal | Descriptive data, quantitative | Study (160) found that in relation to the integration of services, most participants affected by LF (78.8%) stated that they would attend a community-based self-help group that also provides services to people affected by leprosy. This is a positive finding and could potentially be extrapolated to other NTDs with good effect, though more research is needed to evaluate these groups and integration strategies |
| The RECLAIM project: self-help groups running literacy programmes, managed revolving loans, and micro-enterprises | Leprosy/Nepal | Qualitative | Self-efficacy was developed through sustained self-care and group support. Both literacy skills per se and non-formal adult literacy classes reduced stigma. The group members gained respect through advocacy for justice and rights of populations (149) |
| Personal support—financial support | |||
| Livelihood Empowerment Against Poverty (LEAP): providing financial support to caregivers | Leprosy/Ghana | Qualitative | Financial support was believed to be helpful, but not enough for coverage of daily living (164) |
Interventions to reduce NTD-related stigma.
NTD, neglected tropical disease; MDT, multidrug therapy; NGOs, non-governmental organizations; RCT, randomized controlled trial.
A cluster randomized controlled trial examined the effectiveness of three combined stigma-reduction interventions—peer and lay counselling, socio-economic development (SED), and contact events—conducted in the SARI project in Indonesia. Six studies reported findings of the interventions based on the SARI project (145, 146, 168, 176, 186, 202). The SARI project supported the effectiveness of two stigma-reduction strategies: personal support (peer and lay counselling and socio-economic development) and contact intervention, providing qualitative and quantitative evidence.
A cluster randomized controlled trial was found for podoconiosis in Ethiopia (201), investigating three intervention arms: 1) usual care health education, 2) household-based skills training (HB) and community awareness campaign (CAC), or 3) HB and CAC plus a genetics education module (GE). This study supported the effectiveness of a health education intervention. Usual care health education alone was reported to be as effective in experienced and enacted stigma reduction as HB and CAC at 3 and 12 months (166, 201).
Of the other studies, the effective domains of interventions included 1) information, education and communication (IEC)/health education interventions, 2) contact interventions, 3) disease management, 4) personal support, and 5) advocacy.
Most IEC/health education interventions provided education around general knowledge of the disease (162, 180, 203, 204), etiology (166, 201), transmission mechanisms (166, 203), available treatments (122, 166, 203, 204), prevention (166), and related issues including stigma, discrimination, and mental health (203).
For personal support interventions, peer groups fostered self-esteem, self-efficacy, and sense of control (149, 160, 207). Financial support and employment (145, 149, 164, 207) reduced poverty, encouraged health-seeking behaviors, and prevented social isolation. Knowledge (90, 168), personal experience, psychological support (90, 146, 206), human rights awareness, coping skills (90), and solutions to problems (90, 122) were the main focusses of counselling. Lay or peer counsellors were found to promote rapport and to be effective and empowering (168).
One study investigated reconstruction surgery for leprosy as disease management, which was found to be effective in the improvement of self-esteem and acceptance amongst family and community (205).
Contact interventions promoted mutual understanding and normalized the relationships between the affected individuals and their communities (89, 122, 145, 176, 181, 186). This set of interventions has been found to be effective in other areas of health-related stigma, such as mental health. These interventions reduced misconceptions and prejudice (146, 149, 181, 202).
There has been a lack of attention paid in research to specific populations including women, children, and the elderly, for whom general intervention approaches may not be applicable. Only two cluster randomized controlled trials were identified during our review, and few studies reported quantitative findings, which were often based on small sample sizes. Strong evidence was only available for leprosy, with some other evidence for podoconiosis and Buruli ulcer, which causes skin lesions or ulcers. Diseases causing impairment in other parts of the body and wider aspects of disabilities were little investigated.
3.2.6 Implications of studies and recommendations made by their authors
As in the mental health section, here we report on the implications and recommendations provided by the authors of the stigma studies identified.
Whilst thematic differences between NTDs other than leprosy and leprosy are quite small, the difference in the strength of association and level of detail is stark. We found that 20 studies across seven NTDs other than leprosy included reflections on implications for interventions, whereas leprosy alone had nearly 50 studies that made a recommendation for interventions to reduce stigma in those affected.
Across all NTDs (including leprosy), authors noted health education to be a useful intervention tactic to reduce stigmatization through multiple routes, firstly, through patient education of the disease in order to identify early cases and reduce the severity and chronicity of diseases. Secondly, IEC should be provided to a wider community. Education interventions recognize that incorrect beliefs about disease and disability exist, especially around leprosy. Hence, clear and accurate communication detailing that leprosy is non-contagious, curable, and preventable is a beneficial way to prevent community stigmatization. Additionally, work that seeks to enable, empower, and educate healthcare professionals can increase the chances of early diagnosis, therefore reducing stigma from advanced disease stages.
Integration of psychosocial care and the need for multi-disciplinary actors in the care of those with NTDs was also considered important. For those with lymphatic filariasis, authors highlighted that care should focus on encouraging social participation. Similarly, leprosy researchers suggested that schools and families should be involved in care to ensure that leprosy-affected individuals can overcome feelings of alienation and be able to better navigate negative societal reactions.
The authors called for future research on stigma and NTDs to focus on how societal constructs of gender can act as a stigmatizing factor, exploring interactions between psychological distress, infectious agents, and natural disasters, for example.
Eleven papers on leprosy made recommendations for policies, and only three studies did the same for all other NTDs; and this area requires greater research attention. The authors proposed policy changes such as optimizing resource allocation and water availability to endemic areas, increasing social and economic inclusion, and taking a rights-based approach to the challenges that those with NTDs face. The policies recommended for leprosy could extend to encompass all other NTDs, considering that the overarching themes (as referred to in the mechanisms sections) tend to align.
For information relevant to the impact of stigma on those affected by NTDs, the only information available was from leprosy studies. Author recommendations included the benefit of monitoring patients, self-care groups, and bringing together people with different stigmatized conditions to share the challenges they face. They also recommended prioritizing children’s mental health and physical care.
4 Discussion
4.1 Synthesis of findings with previous evidence
Our review was designed to update existing reviews in the field (9, 11, 13, 14), which means that its findings are not representative of the overall literature on their own but need to be considered in conjunction with previous evidence. The following sections on Links 1 and 2 therefore summarize the findings of previous research and the additional evidence provided by our review, covering all research questions posed at the outset of this article.
4.1.1 Link 1: Neglected tropical diseases and mental distress and illness
Overall, there is a growing body of evidence illustrating the high levels of co-morbidity between NTDs and poor mental health; however, there has been a heavy focus on leprosy so far, and many other NTDs have received little or no attention. Consistent with previous reviews (11, 12), our review found evidence corroborating that depression/depressive symptoms, anxiety, and reduced (mental health/psychosocial components of) quality of life are the most commonly reported mental health outcomes amongst NTD-affected persons (of which more than one can be present in individuals), followed by a wide range of other issues such as mental distress, suicidal tendencies, and negative feelings like shame, fear, and stress.
Despite this, the emotional and psychosocial consequences of NTDs are still usually not included in conventional estimates of the burden of NTDs (2, 11); to our knowledge, only two studies have attempted to rectify this so far—one of them found that the disability-adjusted life years (DALY) burden of cutaneous leishmaniasis was seven times higher than the previous burden of disease estimates when associated major depressive disorder was included (208), and the other estimated that the global burden attributable to depressive illness in persons affected by lymphatic filariasis was around twice that than the burden attributed to lymphatic filariasis alone and was also substantial for their caregivers (3); much of this falls disproportionately on women (11).
There are various mechanisms through which NTDs add to mental distress and illness. Our review substantiated previous evidence (11, 12) that physical symptoms associated with NTDs like pain, disability, stage, and duration of illness; demographic factors (female gender and age); socio-economic mechanisms including lower income and unemployment; and stigma, discrimination, and participation restriction/exclusion can all contribute to poor mental health outcomes. We identified pre-existing mental health issues as a further possible factor. Prior research has also reported that disease processes for some NTDs (e.g., African trypanosomiasis, Chagas disease, dengue, neurocysticercosis, and schistosomiasis) can directly affect the brain in ways that lead to mental and neurological consequences like epilepsy, reduced cognitive function, dementia, depression, anxiety, agitation, or even manic symptoms or psychosis (209); additionally, it has been noted that drugs commonly used to treat NTDs may impair mood and cause anxiety, agitation, or psychosis (12, 209). Other mediating factors for which there is some evidence for leprosy include lifestyle factors such as a weak social network or inactivity, and—more inconsistently—marital status (being single, separated, or divorced) and living environment (12).
Conversely, there is not much specific evidence on how poor mental health may impact NTD-related outcomes, though similar mechanisms have been documented from research in HIV (210) and mental health (20). Early evidence from our review and other related research suggests that this may include reduced help-seeking behavior and uptake of and adherence to treatment in children dropping out from school and links with the overall quality of life and substance abuse as well as other mechanisms of co-morbidity (e.g., depression as a risk factor for chronic pain) (209). Furthermore, the negative impact of stigma and participation restrictions on mental wellbeing can be mutually enforcing; not only can stigma and discrimination contribute to poor mental health outcomes, but depression and anxiety can in turn aggravate stigma and further diminish participation. Studies on interventions to improve the mental wellbeing of persons affected by NTDs are still sparse and inconsistent in their methodologies and the measures used. Nevertheless, several studies have reported positive outcomes (12) for psychological interventions such as therapeutic workshops, cognitive behavioral therapy, reminiscence group therapy, empowerment projects, and counselling (particularly when peers are involved), as well as physical interventions like surgical correction or drug treatment or in combination. We note again that our review only included studies up to 2018 and that we are aware that other relevant intervention projects have been conducted since then.
4.1.2 Link 2: Neglected tropical diseases and stigma
Reviewing the literature up to 2015 in 52 studies, Hofstraat and van Brakel (9) found evidence of widespread stigma related to lymphatic filariasis, podoconiosis, Buruli ulcer, onchocerciasis, and leishmaniasis and less firm evidence for Chagas disease, schistosomiasis, trachoma, and STH. Leprosy stigma, however, is documented widely, to the extent that it is seen by many as emblematic of health-related stigma overall. Several systematic reviews, including the two reviews by Sermrittirong et al. (13, 14), which our review served to update, describe aspects of leprosy stigma, such as its causes and determinants (13), or interventions to combat leprosy stigma (14). Nevertheless, comparatively little systematic research has attempted to measure the level or intensity of leprosy stigma (211).
Our review adds to evidence from another 23 studies on stigma related to NTDs other than leprosy (leishmaniasis, lymphatic filariasis, podoconiosis, Buruli ulcer, Chagas disease, and nodding syndrome) and 82 studies on leprosy stigma. Consistent with previous reviews, we found that stigma affects those living with NTDs and also family members (“courtesy stigma”) and can be experienced in many different ways. Particularly salient across diseases were experiences of enacted stigma and discrimination such as avoidance and exclusion, verbal insults and stares, critical comments, blaming and distancing from family members, and violation of personal rights and social participation restrictions. Stigma had a negative impact on people with NTDs’ ability to work and complete education, and their marital prospects and marital relationships (9). Strikingly, we found internalized stigma to be similarly common and impactful as experiences of enacted stigma in the studies we reviewed: across the disease groups for which studies had been done, there were reports of feelings of inferiority, feelings of shame, feelings of low self-esteem, anticipated stigma, attempts to hide the illness, or self-isolation, which also greatly affected social participation. Both enacted stigma and internalized stigma were directly linked to mental health, wellbeing, and social outcomes in many of the studies reviewed, which is also consistent with previous research (9, 13, 212).
Several reviews—mostly in the field of leprosy—have aimed to categorize the reasons or mechanisms by which NTDs are stigmatized and identify risk factors for stigma (9, 13, 213). Sermrittirong et al. (13), for example, distinguished external illness manifestations (physical appearance, odour, etc.), religious and cultural beliefs, and fear of transmission as key causes of leprosy stigma. In addition, the review by Hofstraat et al. (9) described the inability to fulfil a certain gender role, being a burden on family or society, low levels of knowledge about the illness, and advanced disease stage, leading to stigma. The studies included in our review strengthen the evidence base suggesting that visible illness manifestations, higher disability levels, poor knowledge about the illness, and fear of transmission act as mechanisms enhancing NTD-related stigma.
Previous research has also found that stigma affects structural issues such as political commitment to disease management and treatment, priorities and policymaking (9, 10), financial resources, and the way health systems work, including supervision and training levels of health workers. We found little information on these overarching issues of structural stigma; however, we found evidence of health workers holding stereotypes and stigmatizing attitudes towards patients (for Buruli ulcer and leprosy), which is in line with previous research documenting that health worker stigma negatively affects the quality of care, leading to reduced access to diagnosis and treatment (9, 214).
It is not surprising, therefore, that stigma has been found to impact the treatment and outcome of NTDs in areas such as health-seeking behavior, treatment uptake, and adherence (9, 10). Our review also found stigma to have a negative effect on these domains in a small number of studies on Buruli ulcer, podoconiosis, and leprosy, but research evidence in this domain is still scarce and is a priority for further research.
There has been a growing interest in interventions to address NTD-related stigma, yet the evidence on NTDs other than leprosy is still limited, and there are very few intervention studies or evaluations of programmes seeking to address stigma. However, the evidence base for interventions addressing leprosy-related stigma has grown significantly in the last decade and has been summarized in relevant systematic reviews (14, 215–217). Our review adds findings from 19 intervention studies on leprosy, two on podoconiosis, and one on Buruli ulcer. The most rigorous and recent evidence comes from the SARI Project in Indonesia, which was a randomized controlled trial of stigma interventions for leprosy, suggesting the effectiveness of comprehensive, multi-pronged approaches.
Key strategies and related interventions for reduction of NTD-related stigma include i) information, education, and communication (IEC)/health education interventions for patients and the community (9, 14) and also health staff, which aim to raise awareness, reduce stigma, and foster early detection and treatment [the importance of contextualization has been emphasized by several authors (14, 184)]; ii) contact interventions using testimonies and participatory video, which have been shown to improve knowledge and attitudes amongst community members and health staff (145, 186); iii) disease management interventions aiming to lessen the visible impact of NTDs to reduce stigma (9, 205); iv) disease prevention/early treatment interventions aiming to reduce the likelihood of stigmatization through early diagnosis and treatment, for example, in the case of Buruli ulcer, dengue fever, and nodding syndrome (in onchocerciasis) (132, 218, 219); and v) personal support interventions to achieve empowerment, improve self-esteem, and increase participation and community support (9, 14). Personal support interventions may focus on, for example, empowerment, community-based rehabilitation, and peer groups (16); socio-economic development (220); and participatory learning and action or counselling (168) to reduce stigma. vi) Advocacy provides another strategy to address structural stigma and ensure that the rights of people with NTDs are met. Overall, multi-level multi-targeted interventions have been found to have the best chances of success (221).
Our review adds evidence from 22 studies supporting the effectiveness of some of these strategies, particularly health education interventions [found for leprosy (162, 180, 203, 204), podoconiosis (166, 201), and Buruli ulcer (122)], contact interventions [found for leprosy (89, 145, 176, 181, 186) and Buruli ulcer (122)], disease management [found for leprosy (205)], personal support interventions [found for leprosy (90, 145, 146, 149, 160, 164, 168, 206, 207) and Buruli ulcer (122)], and advocacy interventions [in leprosy (146, 149, 181, 202)].
4.2 A negative cycle of stigma affecting mental, social inclusion, and treatment outcomes
Based on the above synthesis of our review findings with existing research, we postulate a revised framework to describe the relationships between NTD outcomes, stigma, and mental health (see Figure 4). This goes beyond the simple triangular relationship described in our original research framework (see Figure 1) to take account of the cyclical nature of these interconnected and mutually reinforcing aspects of health. The links (arrows) in the diagram in Figure 4 are based on our synthesis of the findings above and other established evidence. However, given the scarcity of research on NTD stigma overall, particularly for diseases other than leprosy, further research should examine the complex relationships that the framework aims to depict in a very simplified way. This applies particularly to the links between stigma experience and mental distress with reduced treatment adherence and uptake (arrows 3 and 4) and links between societal stigma, poor resource allocation, health worker stigma, and low quality of care (arrows 7, 8, and 9).
Figure 4
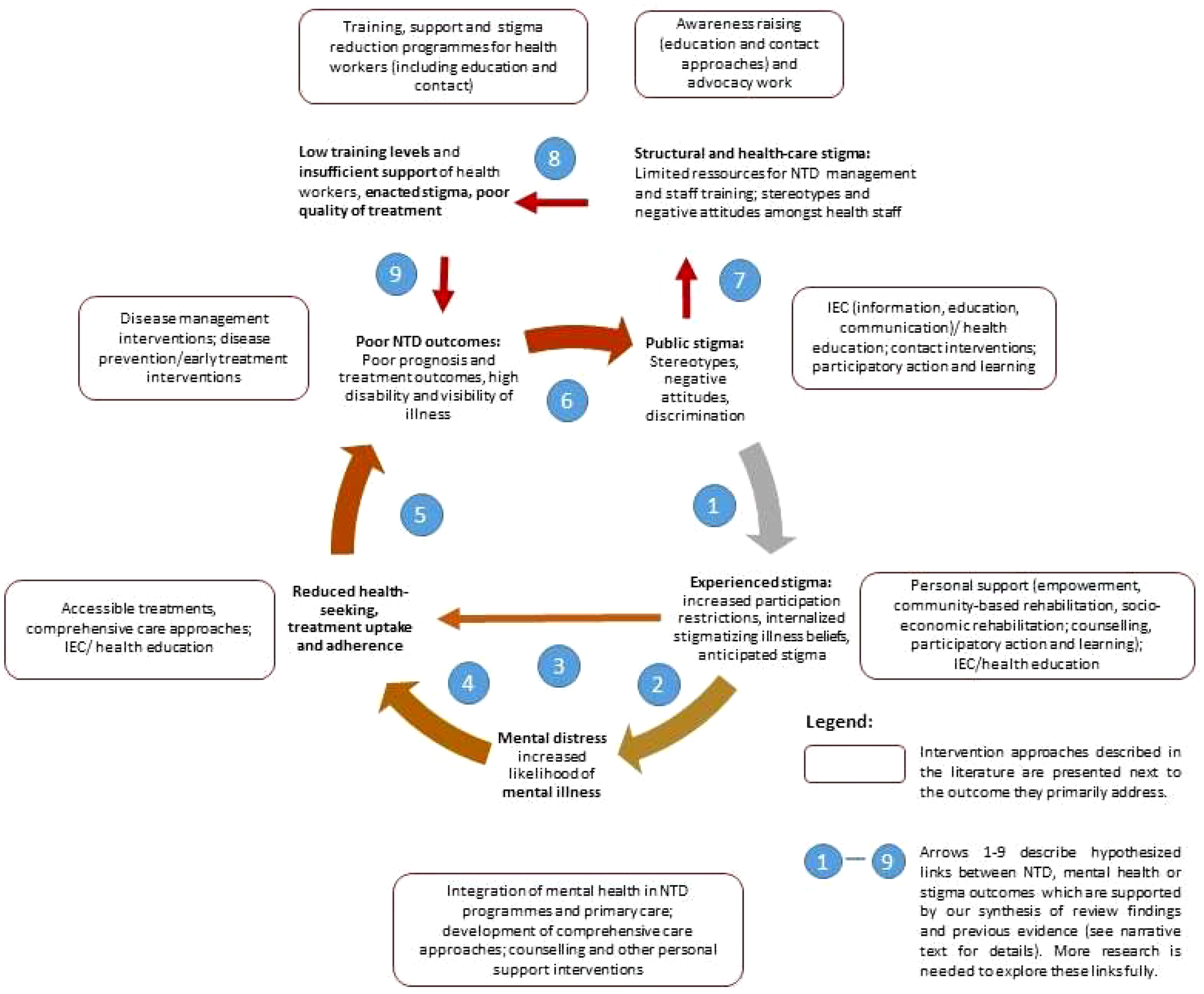
A negative cycle of stigma affecting mental health, social inclusion, and treatment outcomes.
Nevertheless, we hope that the framework will serve to summarize key points of the evidence reviewed here and help to inform future work in the field. It is briefly described in the following.
Stigma triggers a vicious cycle that leads to disadvantages in many aspects of life, reducing social participation and increasing disability (see Figure 4, arrow 1). Stigmatizing attitudes are often internalized by those affected, leading to feelings of shame and low self-esteem, which—along with social restrictions—cause mental distress and increase the likelihood of depression, anxiety, and other mental disorders (arrow 2). Poor mental health (arrow 3), feelings of shame, and anticipated stigma (arrow 4) reduce self-efficacy and act as a barrier to health-seeking and treatment adherence. All these factors adversely influence the effectiveness of treatments leading to poor recovery rates and maintaining disability levels and visibility of the illness (arrow 5), thereby further reinforcing negative attitudes and discrimination (arrow 6).
In addition to the direct effects of societal stigma, persons suffering from NTDs face several forms of structural stigma, manifested, for example, in the lack of resources allocated to this “neglected” group (arrow 7) and low training levels and negative attitudes amongst healthcare staff (arrow 8). This in turn affects the availability, quality, and uptake of treatments offered (arrow 9), feeding back into the cycle of poor treatment outcomes, persistent stigma, and poor mental health.
Each part of the cycle offers access points for interventions. Based on our synthesis of the research evidence above, we have overlaid potential intervention strategies in Figure 4 below. As pointed out earlier, it is often the case in complex systems that using multiple and complementary interventions can be more effective in bringing effective and sustained change. However, some studies suggest additional risks of the stigma associated with skin NTDs, where there is greater disfigurement (especially of the face), and in women, so there would be value in programmes recognizing the additional needs for these groups and target interventions accordingly. Interventions should also consider and address the specific local beliefs associated with different NTDs, such as ideas around punishment by God or witchcraft in leprosy in several countries, or a focus on heredity in podoconiosis in Ethiopia. Similarly, in relation to mental health, there is value in specifically focusing efforts to identify and respond appropriately to at-risk groups. Some mechanisms may be appropriate to address in specific NTDs, for example, addressing chronic itch in onchocerciasis or neuropathic pain in leprosy or considering anti-epileptic medication for nodding syndrome.
4.3 Limitations and learning about methods
This systematic mapping review covered a complex subject area, given the range of diseases covered under the definition of NTDs, and a broad range of outcomes pertaining to stigma and mental distress and illness. Hence, the review was carried out over a long period, which means that papers less than 3 years old are not included (other than key reviews). The selection of studies was limited in that it only considered scientific papers published in English. No grey literature or doctoral theses were included.
The pragmatic decision to make use of existing reviews for parts of the conceptual framework avoided repetition of work, but even though we attempted to be as consistent as possible in the use of search terms, definitions, etc., there are inevitably some differences in approach between different parts of the framework, for example, in terms of the time frames applied in the literature search. We attempted to incorporate the findings of the other reviews in our conclusions but have not re-analyzed raw data, so we were reliant on the results and conclusions drawn by the other review authors.
We felt that the simple conceptual framework adopted served its purpose well, giving a logical structure to our enquiry. We found that the links between the elements of the framework were relevant; each had rich information to populate them, none were redundant, and we did not identify factors in our review that did not fit into this frame. The complexity and interacting nature of many of the relevant factors affecting people’s lives were difficult to fully outline in this simple framework, and we have now proposed a more complex cyclical framework (Figure 4). Some additional factors (such as the intersection between NTD-related stigma and mental-health-related stigma) certainly warrant greater examination. We further acknowledge the role of context and the effect of social determinants on all parts of the framework (acting in a syndemic manner), which has been omitted here due to the limited scope of the review.
We found that there were a disproportionate number of small, uncontrolled studies, and a great heterogeneity in methods and measurements. Most studies were cross-sectional in nature, and greater use of longitudinal studies would enrich our understanding of course and mechanisms of interaction in particular. In accordance with systematic mapping methodology (22, 23), no quality appraisal of studies was carried out, and therefore, poorer-quality studies were considered on the same level as higher-quality evidence. However, the high level of overall concordance of the findings suggests that a different approach would not have altered the main findings and conclusions.
5 Conclusions
The studies identified in this review contain rich insights into the way that the mental health and wellbeing of people affected by a variety of NTDs are impacted by their conditions. The prevalence of mental conditions amongst people affected by NTDs is far higher than that of the general population, and stigma and social exclusion seem to be the major mechanisms through which this manifests, with obvious disfigurement, particularly to the face, being of particular importance. Disability, functional restrictions, and physical symptoms like chronic pain are also key factors, and means of reducing mental distress and illness must include comprehensive attention to physical treatment in addition to specific mental healthcare.
Many of the social determinants that influence mental health and stigma cannot be addressed in immediate service provision but require more profound and structural reform to reduce inequity. The well-described mutually reinforcing cycle of poverty and mental illness (or disability) is a good example of the need to intervene in multiple ways to break such cycles (222). As with mental health more broadly, there was less evidence for the role of addressing more upstream structural factors like poverty and other forms of marginalization, even though these were identified as major risk factors for mental illness and populations affected by NTDs tend to be part of the “bottom billion”.
There is strong evidence that stigma and mental illness result in poorer access to healthcare and worse outcomes in other conditions, but this relationship needs to be better characterized for NTDs if investment in mental healthcare and stigma reduction is to be further justified. This is of particular interest to national NTD programmes at the country level, and funders of global efforts to control and eliminate NTDs must be a focus of further research. In order to achieve a substantial improvement in mental health and wellbeing in the lives of people affected by NTDs, mental health and stigma must be core components of NTD strategies, so that the effective approaches identified in this review can be accessed routinely.
Funding
MS is supported by the Global Health Research Unit for NTDs at the Brighton and Sussex Medical School, which is funded by the National Institute for Health and Care Research (NIHR). JE is part-funded through the SUCCEED programme, funded by the UK Foreign, Commonwealth and Development Office. This research was supported by the National Institute for Health and Care Research (NIHR) using Official Development Assistance funding [grant number: NIHR 200140].
Acknowledgments
The need for a paper that summarized evidence on these issues arose from discussions in the Mental Wellbeing and Stigma Working Group of the Disease Management, Disability and Inclusion (DMDI) cross-cutting group of the NTD NGO Network (NNN), and we are grateful for the commitment of this group and those who work in NNN to raise the profile of inclusion and wellbeing in the NTD sector. We thank Emily Armstrong (EA) for her work in manuscript reviewing and Sara Evans for her methodological guidance. We would like to acknowledge CBM for their support of the lead authors’ time on the study.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further enquiries can be directed to the corresponding author.
Author contributions
MK and JE conceived the research and developed the methodology, which was refined in collaboration with MS, P-CT, and YHA-H. MK, MS, P-CT, and YHA-H screened and extracted data from the papers. All authors contributed to the writing of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fitd.2022.808955/full#supplementary-material
References
1
Bailey F Eaton J Jidda M van Brakel WH Addiss DG Molyneux DH . Neglected tropical diseases and mental health: Progress, partnerships, and integration. Trends Parasitol (2019) 35(1):23–31. doi: 10.1016/j.pt.2018.11.001
2
Hotez PJ Alvarado M Basáñez M Bolliger I Bourne R Boussinesq M et al . The global burden of disease study 2010: interpretation and implications for the neglected tropical diseases. PLoS Negl Trop Diseases (2014) 8(7):e2865. doi: 10.1371/journal.pntd.0002865
3
Ton TGN Mackenzie C Molyneux DH . The burden of mental health in lymphatic filariasis. Infect Dis Poverty (2015) 4:34. doi: 10.1186/s40249-015-0068-7
4
Bailey F Mondragon-Shem K Hotez P Ruiz-Postigo JA Al-Salem W Acosta-Serrano A et al . A new perspective on cutaneous leishmaniasis–implications for global prevalence and burden of disease estimates. PLoS Negl Trop Dis (2017) 11(8):e0005739. doi: 10.1371/journal.pntd.0005739
5
World Health Organization . Ending the neglect to attain the sustainable development goals: a road map for neglected tropical diseases 2021–2030. Geneva: World Health Organization (2020).
6
Yang LH Kleinman A Link BG Phelan JC Lee S Good B . Culture and stigma: Adding moral experience to stigma theory. Soc Sci Med (2007) 1(7):1524–35. doi: 10.1016/j.socscimed.2006.11.013
7
Tsutsumi A Izutsu T Islam AM Maksuda AN Kato H Wakai S . The quality of life, mental health, and perceived stigma of leprosy patients in Bangladesh. Soc Sci Med (2007) 64(12):2443–53. doi: 10.1016/j.socscimed.2007.02.014
8
Person B Addiss D Bartholomew L . Can it be that god does not remember me": a qualitative study on the psychological distress, suffering, and coping Dominican women with chronic filarial lymphedema and elephantiasis of the leg. Health Care Women Int (2008) 29:349–65. doi: 10.1080/07399330701876406
9
Hofstraat K van Brakel WH . Social stigma towards neglected tropical diseases: a systematic review. Int Health (2016) 8:53–70. doi: 10.1093/inthealth/ihv071
10
Weiss MG . Stigma and the social burden of neglected tropical diseases. PLoS Med (2008) 2(5): e237. doi: 10.1371/journal.pntd.0000237
11
Litt E Baker MC Molyneux D . Neglected tropical diseases and mental health: a perspective on comorbidity. Trends Parasitol (2012) 28:195–201. doi: 10.1016/j.pt.2012.03.001
12
Somar P Waltz M van Brakel W . The impact of leprosy on the mental wellbeing of leprosy-affected persons and their family members–a systematic review. Global Ment Health (2020) 7:e15. doi: 10.1017/gmh.2020.3
13
Sermrittirong S van Brakel W . Stigma in leprosy: concepts, causes and determinants. Leprosy Review (2014) 85:29–35. doi: 10.47276/lr.85.1.36
14
Sermrittirong S Van Brakel WH Bunbers-Aelen JFG . How to reduce stigma in leprosy - a systematic literature review. Leprosy Review (2014) 85(3):149–57. doi: 10.47276/lr.85.3.149
15
Stevelink S van Brakel W Augustine V . Stigma and social participation in southern India: Differences and commonalities among persons affected by leprosy and persons living with HIV/AIDS. Psychology Health Med (2011) 16:695–707. doi: 10.1080/13548506.2011.555945
16
Cross H Choudhary R . STEP: an intervention to address the issue of stigma related to leprosy in southern Nepal. Leprosy Review (2005) 76(4):316–24. doi: 10.47276/lr.76.4.316
17
Hotez P . Stigma: The stealth weapon of the NTD. PloS Negl Trop Diseases (2008) 2(4):e230. doi: 10.1371/journal.pntd.0000230
18
Semrau M Evans-Lacko S Koschorke M Ashenafi L Thornicroft G . Stigma and discrimination related to mental illness in low- and middle-income countries. Epidemiol Psychiatr Sci (2015), 24(5):382–94. doi: 10.1017/S2045796015000359
19
Thornicroft G Mehta N Clement S Evans-Lacko S Doherty M Rose D et al . Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet (2015) 207(5):377–84. doi: 10.1016/S0140-6736(15)00298-6
20
Henderson C Noblett J Parke H Clement S Caffrey A Gale-Grant O et al . Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry (2014) 1(6):467–82. doi: 10.1016/S2215-0366(14)00023-6
21
Mehta N Clement S Marcus E Stona A-C Bezborodovs N Evans-Lacko S et al . Evidence for effective interventions to reduce mental health-related stigma and discrimination in the medium and long term: systematic review. Br J Psychiatry (2015) 207(5):377–84. doi: 10.1192/bjp.bp.114.151944
22
Clapton J Rutter D Sharif N . Systematic mapping guidance. London: Social Care Institute for Excellence (2009).
23
Grant MJ Booth A . A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info. Libr. J (2009) 26(2):91–108. doi: 10.1111/j.1471-1842.2009.00848.x
24
Evans-Lacko S Courtin E Fiorillo A Knapp M Luciano M Park AL et al . The state of the art in European research on reducing social exclusion and stigma related to mental health: a systematic mapping of the literature. Eur Psychiatry (2014) 29(6):381–9. doi: 10.1016/j.eurpsy.2014.02.007
25
Craig GM Daftary A Engel N O'Driscoll S Ioannaki A . Tuberculosis stigma as a social determinant of health: a systematic mapping review of research in low incidence countries. Int J Infect Dis (2017) 56:90–100. doi: 10.1016/j.ijid.2016.10.011
26
Iemmi V . Sustainable development for global mental health: a typology and systematic evidence mapping of external actors in low-income and middle-income countries. BMJ Glob Health (2019) 4(6):e001826. doi: 10.1136/bmjgh-2019-001826
27
InfoNTD . (2018). Available at: https://www.infontd.org/ (Accessed 22/07/2018).
28
Infolep . (2018). Available at: https://www.infolep.org/ (Accessed 22/07/2018).
29
World Health Organization . Neglected tropical diseases (2018). Geneva: World Health Organisation. Available at: https://www.who.int/neglected_diseases/diseases/en/ (Accessed 22 July 2018).
30
Colebunders R Mandro M Njamnshi A Boussinesq M Hotterbeekx A Kamgno J et al . Report of the first international workshop on onchocerciasis-associated epilepsy. Infect Dis Poverty (2018) 7(1):23. doi: 10.1186/s40249-018-0400-0
31
Patel V Saxena S Lund C Thornicroft G Baingana F Bolton P et al . The Lancet commission on global mental health and sustainable development. Lancet (2018) 10157:1553–98. doi: 10.1016/S0140-6736(18)31612-X
32
Thornicroft G . Shunned: Discrimination against people with mental illness. Oxford: Oxford University Press (2006).
33
Link BG Struening EL Neese-Todd S Asmussen S Phelan JC . Stigma as a barrier to recovery: The consequences of stigma for the self-esteem of people with mental illnesses. Psychiatr Services (2001) 52(12):1621–6. doi: 10.1176/appi.ps.52.12.1621
34
Ritsher JB Otilingam PG Grajales M . Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res (2003) 121(1):31–49. doi: 10.1016/j.psychres.2003.08.008
35
World Bank . (2017). Available at: http://data.worldbank.org/income-level/low-and-middle-income (Accessed 24 March 2017).
36
Ozaki Y Guariento ME de Almeida EA . Quality of life and depressive symptoms in chagas disease patients. Qual Life Research: Int J Qual Life Aspects Treatment Care Rehabilitation (2011) 20:133–8. doi: 10.1007/s11136-010-9726-1
37
Toledo Jr.AC da Silva RE Carmo RF Amaral TA Luz ZM Rabello A . Assessment of the quality of life of patients with cutaneous leishmaniasis in belo horizonte, Brazil, 2009-2010. A Pilot Study Trans R Soc Trop Med Hygiene (2013) 107:335–6. doi: 10.1093/trstmh/trt021
38
Tran BX Vu GT Nguyen LH Nguyen ATL Tran TT Nguyen BT et al . Cost-of-illness and the health-related quality of life of patients in the dengue fever outbreak in Hanoi in 2017. International J Environmental Research and Public Health (2018) 15(6):1174.
39
Wiese S Elson L Feldmeier H . Tungiasis-related life quality impairment in children living in rural Kenya. PloS Negl Trop Diseases (2018) 12(1): e0005939. doi: 10.1371/journal.pntd.0005939
40
Oliveira BG Abreu MNS Abreu CDG da Costa Rocha MO Ribeiro AL . Health-related quality of life in patients with chagas disease TT - qualidade de vida relacionada a saude na doenca de chagas. Rev da Sociedade Bras Medicina Tropical (2011) 44:150–6. doi: 10.1590/S0037-86822011005000002
41
Ozaki Y Dias ELF Almeida E Guariento ME . Quality of life in adults and older adults with chagas disease. Rev Cienc Medicas (2015) 24:93–104. doi: 10.24220/2318-0897v24n3a2654
42
Rodriguez-Morales AJ Restrepo-Posada VM Acevedo-Escalante N Rodriguez-Munoz ED Valencia-Marin M Castrillon-Spitia JD et al . Impaired quality of life after chikungunya virus infection: A 12-months follow-up study of its chronic inflammatory rheumatism in la Virginia, risaralda, Colombia. Value Health (2016) 19(7):A420–A1. doi: 10.1016/j.jval.2016.09.428
43
Khatami A Emmelin M Talaee R Mohammadi AM Aghazadeh N Firooz A et al . Lived experiences of patients suffering from acute old world cutaneous leishmaniasis: A qualitative content analysis study from Iran. J Arthropod-Borne Diseases (2018) 12(2):180–95. doi: 10.18502/jad.v12i2.44
44
Pal B Murti K Siddiqui NA Das P Lal CS Babu R et al . Assessment of quality of life in patients with post kalaazar dermal leishmaniasis. Health Qual Life Outcomes (2017) 15(1):148. doi: 10.1186/s12955-017-0720-y
45
Turan E Kandemir H Yesilova Y Ekinci S Tanrikulu O Kandemir SB et al . Assessment of psychiatric morbidity and quality of life in children and adolescents with cutaneous leishmaniasis and their parents. Postepy Dermatologii. i Alergologii (2015) 32:344–8. doi: 10.5114/pdia.2015.54744
46
Alemayehu M Wubshet M Mesfin N Tamiru A Gebayehu A . Health-related quality of life of HIV infected adults with and without visceral leishmaniasis in Northwest Ethiopia. Health Qual Life Outcomes (2017) 15:65. doi: 10.1186/s12955-017-0636-6
47
Alemayehu M Wubshet M Mesfin N Gebayehu A . Effect of health care on quality of life among human immunodeficiency virus infected adults with and without visceral leishmaniasis in northwest Ethiopia: A longitudinal follow-up study. Am J Trop Med Hygiene (2018) 98(3): 747–52. doi: 10.4269/ajtmh.17-0458
48
Harichandrakumar KT Kumaran M . Health related quality of life (HRQoL) among patients with lymphatic filariasis. Int J Health Sci Res (2017) 7(3):256–68. Available at: https://www.ijhsr.org/IJHSR_Vol.7_Issue.3_March2017/IJHSR_Abstract.037.html
49
Stanton MC Yamauchi M Mkwanda SZ Ndhlovu P Matipula DE Mackenzie C et al . Measuring the physical and economic impact of filarial lymphoedema in chikwawa district, Malawi: a case-control study. Infect Dis Poverty (2017) 6:28. doi: 10.1186/s40249-017-0241-2
50
Wijesinghe R . Quality of life in filarial lymphoedema patients in Colombo, Sri Lanka. Trop Med Int Health (2011) 227. doi: 10.1016/j.trstmh.2009.08.005
51
de Almeida SM Gurjao SA . Is the presence of depression independent from signs of disease activity in patients with neurocysticercosis? J Community Health (2011) 36(5):693–7. doi: 10.1007/s10900-011-9362-x
52
de Almeida SM Gurjao SA . Quality of life assessment in patients with neurocysticercosis. J Community Health (2011) 36(4):624–30. doi: 10.1007/s10900-010-9351-5
53
Bhattarai R Budke CM Carabin H Proano JV Flores-Rivera J Corona T et al . Quality of life in patients with neurocysticercosis in Mexico. Am J Trop Med Hygiene (2011) 84:782–6. doi: 10.4269/ajtmh.2011.10-0646
54
Mousley E Deribe K Tamiru A Davey G . The impact of podoconiosis on quality of life in northern Ethiopia. Health Qual Life Outcomes (2013) 11:122. doi: 10.1186/1477-7525-11-122
55
Furst T Silue KD Ouattara M N'Goran DN Adiossan LG N'Guessan Y et al . Schistosomiasis, soil-transmitted helminthiasis, and sociodemographic factors influence quality of life of adults in cote d'Ivoire. PloS Negl Trop Dis [electronic resource] (2012) 6:e1855. doi: 10.1371/journal.pntd.0001855
56
Terer CC Bustinduy AL Magtanong RV Muhoho N Mungai PL Muchiri EM et al . Evaluation of the health-related quality of life of children in schistosoma haematobium-endemic communities in Kenya: a cross-sectional study. PloS Negl Trop Dis (2013) 7:e2106. doi: 10.1371/journal.pntd.0002106
57
Kinung'hi S Magnussen P Kaatano G Olsen A . Infection with schistosoma mansoni has an effect on quality of life, but not on physical fitness in schoolchildren in mwanza region, north-Western Tanzania: A cross-sectional study. PloS Negl Trop Diseases (2016) 10(12):e0005257. doi: 10.1371/journal.pntd.0005257
58
Esmael H Tariku W Sintayehu A Zerihun T Mulat Z Zebideru Z et al . The impact of trachomatous trichiasis on quality of life: a case control study. PloS Negl Trop Dis (2015) 9(11):e0004254. doi: 10.1371/journal.pntd.0004254
59
Palmera SL Winskell K Patterson AE Boubacar K Ibrahim F Namata I et al . 'A living death': a qualitative assessment of quality of life among women with trichiasis in rural Niger. Int Health (2014) 6:291–7. doi: 10.1093/inthealth/ihu054
60
Bowers B Butlin CR Alam K Lockwood DNJ Walker SL . Health-related quality of life amongst people affected by erythema nodosum leprosum in Bangladesh: a cross sectional study. Leprosy Review (2017) 88:488–98. doi: 10.47276/lr.88.4.488
61
Borges-de-Oliveira R Rocha-Leite CI Araujo-de-Freitas L Queiroz DA Machado PR Quarantini LC . Perception of social exclusion, neuropathy, and quality of life among hansen's disease patients. Int J Psychiatry Med (2015) 49:176–86. doi: 10.1177/0091217415582173
62
Bottene IMC dos Reis VMS . Quality of life of patients with paucibacillary leprosy TT - qualidade de vida em pacientes com hanseniase paucibacilar. Anais Brasileiros Dermatologia (2012) 87:408–11. doi: 10.1590/S0365-05962012000300009
63
Costa MD Terra Fde S Costa RD Lyon S Costa AM Antunes CM . Assessment of quality of life of patients with leprosy reactional states treated in a dermatology reference center. Anais Brasileiros Dermatologia (2012) 87:26–35. doi: 10.1590/S0365-05962012000100003
64
Lustosa AA Nogueira LT Pedrosa JIS Teles JBM Campelo V . The impact of leprosy on health-related quality of life. Rev da Sociedade Bras Medicina Trop (2011) 44(5):621–6. doi: 10.1590/S0037-86822011000500019
65
Reis FJJ Cunha AJLA Gosling AP Fontana AP Gomes MK . Quality of life and its domains in leprosy patients after neurolysis: a study using WHOQOL-BREF. Leprosy Review (2013) 84:119–23. doi: 10.47276/lr.84.2.119
66
Sales AM Illarramendi X Walker SL Lockwood D Sarno EN Nery J . The impact of erythema nodosum leprosum on health related quality of life in Rio de Janeiro. Leprosy Review (2017) 88:499–509. doi: 10.47276/lr.88.4.499
67
Santos VS Oliveira LS Castro FDN Gois-Santos VT Lemos LMD MdCO R et al . Functional activity limitation and quality of life of leprosy cases in an endemic area in northeastern Brazil. PloS Negl Trop Dis (2015) 9(7):e0003900. doi: 10.1371/journal.pntd.0003900
68
Santos VS Castro FDN Oliveira LS Santana JCV Feitosa VLC Gurgel RQ et al . Pain and quality of life in leprosy patients in an endemic area of northeast Brazil: A cross-sectional study. Infect Dis Poverty (2016) 5(1):18. doi: 10.1186/s40249-016-0113-1
69
Bello AI Dengzee SA Iyor FT . Health related quality of life amongst people affected by leprosy in south Ghana: a needs assessment. Leprosy Review (2013) 84:76–84. doi: 10.47276/lr.84.1.76
70
Govindharaj P Srinivasan S Darlong J . Quality of life of people affected with leprosy disability living in purulia, West Bengal. International J Health Sci Res (2018) 8(2):221–25.
71
Kosaraju S Reddy K Vadlamani N Sandhya L Kalasapati L Maganti S et al . Psychological morbidity among dermatological patients in a rural setting. Indian J Dermatol (2015) 60(6):635. doi: 10.4103/0019-5154.169140
72
Brouwers C van Brakel W Cornielje HCN-B . Quality of life, perceived stigma, activity and participation of people with leprosy-related disabilities in south-East Nepal. Disability CBR Inclusive Dev (2011) 22:16–34. doi: 10.5463/dcid.v22i1.15
73
Hunt WTN Thanh H Ton N Nikolaou V Dang K Hong L . A case-control study comparing the dermatology life quality index (DLQI) ratings of patients undergoing leprosy treatment, people cured of leprosy, and controls in Vietnam. Leprosy Rev (2018) 89(1):46–55. doi: 10.47276/lr.89.1.46
74
Kpadonou TG Alagnide E Azanmasso H Fiossi-Kpadonou E Moevi HAA Niama D et al . Psychosocioprofessional and familial becoming of formers buruli ulcer patients in Benin. Ann Phys Rehabil Med (2013) 56:7–8. doi: 10.1016/j.rehab.2013.07.785
75
Guimaraes PMQ Passos SR Calvet GA Hokerberg YH Lessa JL de Andrade CA . Suicide risk and alcohol and drug abuse in outpatients with HIV infection and chagas disease. Rev Bras Psiquiatria (2014) 36(2):131–7. doi: 10.1590/1516-4446-2013-1219
76
Bhatia MS Gautam P Jhanjee A . Psychiatric morbidity in patients with chikungunya fever: First report from India. J Clin Diagn Res (2015) 9:VC01–VC3. doi: 10.7860/JCDR/2015/14569.6586
77
Ali S Shaikh S Chaudhry RA . A study on post-dengue depression. Pakistan J Med Health Sci (2017) 11:12–3. Available at: https://www.pjmhsonline.com/2017/jan_march/pdf/12.pdf
78
Hashmi AM Butt Z Idrees Z Niazi M Yousaf Z Haider S et al . Anxiety and depression symptoms in patients with dengue fever and their correlation with symptom severity. Int J Psychiatry Med (2012) 44(3):199–210. doi: 10.2190/PM.44.3.b
79
Gunathilaka N Chandradasa M Champika L Siriwardana S Wijesooriya L . Delayed anxiety and depressive morbidity among dengue patients in a multi-ethnic urban setting: First report from Sri Lanka. Int J Ment Health Syst (2018) 12:ArtID 20. doi: 10.1186/s13033-018-0202-6
80
Abdulmalik J Nwefoh E Obindo J Dakwak S Ayobola M Umaru J et al . Emotional difficulties and experiences of stigma among persons with lymphatic filariasis in plateau state, Nigeria. Health Hum rights J (2018) 20(1):27–40.
81
Obindo J Abdulmalik J Nwefoh E Agbir M Nwoga C Armiya'u A et al . Prevalence of depression and associated clinical and socio-demographic factors in people living with lymphatic filariasis in plateau state, Nigeria. PloS Negl Trop Dis (2017) 11(6):e0005567. doi: 10.1371/journal.pntd.0005567
82
Bartlett J Deribe K Abreham T Tsige A Girmay M Malik M et al . Depression and disability in people with podoconiosis: a comparative cross-sectional study in rural northern Ethiopia. Int Health (2016) 8(2):124–31. doi: 10.1093/inthealth/ihv037
83
Jia TW Utzinger J Deng Y Yang K Li YY Zhu JH et al . Quantifying quality of life and disability of patients with advanced schistosomiasis japonica. PloS Negl Trop Dis [electronic resource] (2011) 5(2):e966. doi: 10.1371/journal.pntd.0000966
84
Alemayehu M Wubshet M Mesfin N Gebayehu A . Perceived quality of life among visceral leishmaniasis and HIV coinfected migrant male-workers in Northwest Ethiopia: a qualitative study. BMC Public Health (2017) 17(1):204. doi: 10.1186/s12889-017-4132-z
85
Musisi S Akena D Nakimuli-Mpungu E Abbo C Okello J . Neuropsychiatric perspectives on nodding syndrome in northern Uganda: a case series study and a review of the literature. Afr Health Sci (2013) 13:205–18. doi: 10.4314/ahs.v13i2.3
86
Garbin CA Garbin AJ Carloni ME Rovida TA Martins RJ . The stigma and prejudice of leprosy: influence on the human condition. Rev Da Sociedade Bras Medicina Tropical (2015) 48:194–201.
87
Leite SCC Caldeira AP . Therapeutic workshops and psychosocial rehabilitation for institutionalised leprosy patients. Ciencia Saude Coletiva (2015) 20(6):1835–42. doi: 10.1590/1413-81232015206.16412014
88
Moura SHL Grossi MAF Lehman LF Salgado SP Almeida CA Lyon DT et al . Epidemiology and assessment of the physical disabilities and psychosocial disorders in new leprosy patients admitted to a referral hospital in belo horizonte, minas gerais, Brazil. Leprosy Review (2017) 88:244–57. doi: 10.47276/lr.88.2.244
89
Sillo S Lomax C de Wildt G Da Silva Fonseca M . And sociocultural exploration of the stigma experiences of leprosy patients in Brazil. Leprosy Review (2016) 87:378–95. doi: 10.47276/lr.87.3.378
90
Bense N Das P Rao PS John AS . Enhancing counselling strategies for leprosy patients through the participation scale. Leprosy Review (2013) 84:199–208. doi: 10.47276/lr.84.3.199
91
Lasry-Levy E Hietaharju A Pai V Ganapati R Rice ASC Haanpaa M et al . Neuropathic pain and psychological morbidity in patients with treated leprosy: A cross-sectional prevalence study in Mumbai. PLoS Negl Trop Dis (2011) 5(3):e981. doi: 10.1371/journal.pntd.0000981
92
Nagargoje A Mundhada GR Deshmukh SB Saboo AVCN-N . Psychiatric Co-morbidity in persons with hansen’s disease. J Evidence based Med Healthcare (2015) 2:2872–81. doi: 10.18410/jebmh/2015/418
93
Rahmawati I Yuniarti EV . The influence of cognitive behaviour therapy to decrease the level of depression for leprosy sufferer. Int J Nurs midwifery (2017) 1:69–73. doi: 10.29082/IJNMS/2017/Vol1/Iss1/41
94
Utami R Haryanto J Sajidin M . Path analysis of the factors that influence the prevention of leprosy clients depression in leprosy hospital sumberglagah mojokerto, East Java, Indonesia. Int J Sci Res (2017) 6:431–5. doi: 10.21275/ART20174228
95
Bakare AT Yusuf AJ Habib ZG Obembe A . Anxiety and depression: A study of people with leprosy. Sokoto, North- Western Nigeria: J psychiatry -previously: African J psychiatry (2015).
96
Enwereji E . Assessing psychological rehabilitation of leprosy patients discharged home in abia and ebonyi states of Nigeria. Eur J Gen Med (2011) 8(2):110–6. doi: 10.29333/ejgm/82710
97
Attama CM Uwakwe R Onyeama GM Igwe MN . Psychiatric morbidity among subjects with leprosy and albinism in south East Nigeria: A comparative study. Ann Med Health Sci Res (2015) 5(3):197–204. doi: 10.4103/2141-9248.157503
98
Effah A Ersser SJ Hemingway A . Support needs of people living with mycobacterium ulcerans (Buruli ulcer) disease in a Ghana rural community: a grounded theory study. Int J Dermatol (2017) 56:1432–7. doi: 10.1111/ijd.13785
99
Martelli CM Nascimento NE Suaya JA Siqueira JB Souza WV Turchi MD et al . Quality of life among adults with confirmed dengue in Brazil. Am J Trop Med Hygiene (2011) 85:732–8. doi: 10.4269/ajtmh.2011.11-0067
100
Gill KU Ahmad W Irfan M . A clinical study to see the psychological effects of dengue fever. Pakistan J Med Health Sci (2011) 5:101–4.
101
Mushtaq M Zahir M . Depression, anxiety, stress and their effect upon the self-efficacy in dengue patients. J Postgraduate Med Institute (2016) 30:62–5. Available at: https://jpmi.org.pk/index.php/jpmi/article/view/1783
102
Bennis I Thys S Filali H de Brouwere V Sahibi H Boelaert M . Psychosocial impact of scars due to cutaneous leishmaniasis on high school students in errachidia province, Morocco. Infect Dis Poverty (2017) 6:46. doi: 10.1186/s40249-017-0267-5
103
Adhikari RK Sherchand JB Mishra SR Ranabhat K Pokharel A Devkota P et al . Health-seeking behaviors and self-care practices of people with filarial lymphoedema in Nepal: A qualitative study. J Trop Med (2015) 2015:260359. doi: 10.1155/2015/260359
104
Silva CAB Albuquerque VLM Antunes MFR . Leprosy as a neglected disease and its stigma in the northeast of Brazil. Indian J Leprosy (2014) 86:53–9.
105
Silva R Vieira M Mistura C Carvalho e Lira M Sarmento S . [Stigmata and prejudice: reality of carriers of leprosy in prisional units.] TT - estigma e preconceito: realidade de portadores de hanseníase em unidades prisionais. Rev Pesquisa: Cuidado é Fundam Online (2014) 6:493–506. doi: 10.9789/2175-5361.2014.v6i2.493-506
106
Peters RMH Hofker ME Van Brakel W Zweekhorst MBM Seda FSSE Irwanto et al . Narratives around concealment and agency for stigma-reduction: A study of women affected by leprosy in cirebon district, Indonesia. Disability CBR Inclusive Dev (2014) 25:5–21. doi: 10.5463/dcid.v25i4.389
107
Bedford J . Perceptions of leprosy in the orang asli (Indigenous minority) of peninsular Malaysia. In: When Culture Impacts Health: Global Lessons for Effective Health Research. Amsterdam: Elsevier (2013).
108
Verma DK Katoch VM Katoch K Gupta SC Jain P Tomar S et al . A study of social stigma by the neighbours among leprosy patients of Agra and kanpur districts of UP. Indian J Community Health (IJCH) (2012) 1:2:8–12.
109
Abedi H Javadi A Naji S . An exploration of health, family and economic experiences of leprosy patients, Iran. Pakistan J Biol Sciences: PJBS (2013) 16(18):927–32. doi: 10.3923/pjbs.2013.927.932
110
Azad-uz-zaman Q Hossain Q Hadi M Boiragee J Parvin M . Psychosocial consequences of leprosy and the related deformity in Bangladesh. Asian Pacific J Trop Disease (2016) 7(1):25–29. doi: 10.12980/apjtd.7.2017D6-326
111
Lusli M Peters R Bunders J Irwanto I Zweekhorst M . Development of a rights-based counselling practice and module to reduce leprosy-related stigma and empower people affected by leprosy in cirebon district, Indonesia. Leprosy Review (2017) 88(3):318–33. doi: 10.47276/lr.88.3.318
112
Tchounkeu YFL Onyeneho NG Wanji S Kabali AT Manianga C Amazigo UV et al . Changes in stigma and discrimination of onchocerciasis in Africa. Trans R Soc Trop Med Hygiene (2012) 106:340–7. doi: 10.1016/j.trstmh.2012.02.009
113
Pelizzari é Arruda G Marcon ôS Fernandes CAM . Perceptions of people with leprosy about disease and treatment. TT - percepções de pessoas com hanseníase acerca da doença e tratamento. Rev da Rede Enfermagem. do Nordeste (2016) 17(4):466–74. doi: 10.15253/2175-6783.2016000400005
114
Dadun D Peters R Lusli M Miranda-Galarza B Van Brakel W Zweekhorst M et al . Exploring the complexities of leprosy-related stigma and the potential of a socio-economic intervention in a public health context in Indonesia. Disability CBR Inclusive Dev (2016) 27(3):5–23. doi: 10.5463/dcid.v27i3.551
115
Arachchi MM Wickramasinghe R Kuruppu NR . Stigmatization in leprosy: A descriptive study from patients’ perspective in Sri Lanka. Sci Res J (2017) 5(9):10–13.
116
Ackumey MM Gyapong M Pappoe M Kwakye-Maclean C Weiss MG . Illness meanings and experiences for pre-ulcer and ulcer conditions of buruli ulcer in the Ga-West and Ga-south municipalities of Ghana. BMC Public Health (2012) 12:264. doi: 10.1186/1471-2458-12-264
117
George A Khora T Das P Rao PS . Nursing interventions to manage anxiety levels of female inpatients admitted first time in a leprosy hospital. Indian J Leprosy (2013) 85:19–25.
118
Forsyth CJ . "I cannot be worried": Living with chagas disease in tropical Bolivia. PloS Negl Trop Dis [electronic resource] (2017) 11:e0005251. doi: 10.1371/journal.pntd.0005251
119
Bennis I Belaid L de Brouwere V Filali H Sahibi H Boelaert M . "The mosquitoes that destroy your face". social impact of cutaneous leishmaniasis in south-eastern Morocco, a qualitative study. PLoS One (2017) 12(12):e0189906. doi: 10.1371/journal.pone.0189906
120
Divya S Khaitan BK Neena K Rajesh S . Dehabilitation in the era of elimination and rehabilitation: a study of 100 leprosy patients from a tertiary care hospital in India. Leprosy Review (2015) 86:62–74. doi: 10.47276/lr.86.1.62
121
Thwaites V Anjum V Rao M . Sources of anxiety amongst leprosy patients in urban treatment setting in Hyderabad, India. Leprosy Review (2014) 85:328–31. doi: 10.47276/lr.85.4.328
122
Amoussouhoui AS Johnson RC Sopoh GE Agbo IE Aoulou P Houezo JG et al . Steps toward creating a therapeutic community for inpatients suffering from chronic ulcers: Lessons from allada buruli ulcer treatment hospital in Benin. PLoS Negl Trop Dis [electronic resource] (2016) 10(7):e0004602. doi: 10.1371/journal.pntd.0004602
123
Diaz AR Stewart A Hargrave A Kenneson-Adams A Molina JP Gonzales A et al . Psychological distress and zika, dengue, and chikungunya infections following 2016 earthquake in coastal Ecuador. Am J Trop Med Hygiene (2017) 97:468.
124
Stewart-Ibarra AM Hargrave A Diaz A Kenneson A Madden D Romero MM et al . Psychological distress and zika, dengue and chikungunya symptoms following the 2016 earthquake in bahia de caraquez, Ecuador. Int J Environ Res Public Health [Electronic Resource] (2017) 14:5. doi: 10.3390/ijerph14121516
125
Mousley E Deribe K Tamiru A Tomczyk S Hanlon C Davey G . Mental distress and podoconiosis in northern Ethiopia: A comparative cross-sectional study. International Health (2015) 7(1):16–25.
126
de Souza Cunha MA Antunes DE Machado da Silveira RW Goulart IMB . Application of the SRQ20 and the protocol of psychological assessment in patients with leprosy in a reference centre in Brazil. Leprosy Review (2015) 86:229–39. doi: 10.47276/lr.86.3.229
127
Damte A Berihun Berhe H Hiwot HG . Prevalence and associated factors of mental distress among leprosy patients at alert hospital out patient clinic Addis Ababa, Ethiopia, 2011. Int J Pharm Sci Res (2013) 4:1176–82. doi: 10.13040/IJPSR.0975-8232.4(3).1176-82
128
Nahrowi S Munawar S . Influenced social capital related to stigma, psychological stress and treatment adherence of leprosy. Int J Epidemiol Infection (2014) 2:92–6.
129
Kpadonou T Houngbédji G Alagnidé E Gouton E Azanmasso H Niama D et al . Health-related quality of life of adult patients healed from buruli ulcer in Benin. Br J Med Med Res (2015) 6(1):88–98. doi: 10.9734/BJMMR/2015/14187
130
Wijesinghe RS Wickremasinghe AR . Physical, psychological, and social aspects of quality of life in filarial lymphedema patients in Colombo, Sri Lanka. Asia Pacific J Public Health (2015) 27(2):NP2690–701. doi: 10.1177/1010539511434140
131
Cassidy T Worrell CM Little K Aishya P Inakhi P Rout J et al . Experiences of a community-based lymphedema management program for lymphatic filariasis in odisha state, India: an analysis of focus group discussions with patients, families, community members and program volunteers. PloS Negl Trop Dis (2016) 10(2):e0004424. doi: 10.1371/journal.pntd.0004424
132
Buchmann K . 'These nodding people': Experiences of having a child with nodding syndrome in postconflict northern Uganda. Epilepsy Behavior (2015) 42:71–7. doi: 10.1016/j.yebeh.2014.10.027
133
Yamaguchi N Poudel KC Jimba M . Health-related quality of life, depression, and self-esteem in adolescents with leprosy-affected parents: results of a cross-sectional study in Nepal. BMC Public Health (2013) 13:22. doi: 10.1186/1471-2458-13-22
134
Tora A Franklin H Kebede D Reda AA Davey G . Extent of podoconiosis-related stigma in wolaita zone, southern Ethiopia: a cross-sectional study. SpringerPlus (2014) 3:647. doi: 10.1186/2193-1801-3-647
135
Shen J Liu M Zhou M Li W . Causes of death among active leprosy patients in China. Int J Dermatol (2011) 50:57–60. doi: 10.1111/j.1365-4632.2010.04593.x
136
Seshadri D Khaitan BK Khanna N Sagar R . Dehabilitation in the era of elimination and rehabilitation: a study of 100 leprosy patients from a tertiary care hospital in India. Leprosy Review (2015) 86:62–74. doi: 10.47276/lr.86.1.62
137
Akogun OB Akogun MK Apake E Kale OO . Rapid community identification, pain and distress associated with lymphoedema and adenolymphangitis due to lymphatic filariasis in resource-limited communities of north-eastern Nigeria. Acta Tropica (2011) 120(SUPPL. 1):S62–68. doi: 10.1016/j.actatropica.2011.03.008
138
Major S . A study of psychological strengths and weaknesses of children and adolescents from leprosy Community:A case study of south Delhi. Indian J Health & Wellbeing (2017) 8(7):611–13.
139
Rocha-Leite CI Borges-De-Oliveira R Machado PRL Pettersen KM Trinchao M Morais-De-Jesus M et al . Mental disorders in leprosy: High prevalence and low psychiatric care. Eur Psychiatry Conference: 21st Eur Congress Psychiatry EPA (2013) 28.
140
Antelman G Kaaya S Wei R Mbwambo J Msamanga G Fawzi W et al . Depressive symptoms increase risk of HIV disease progression and mortality among women in Tanzania. J Acquir Immune Defic Syndr (2007) 44:470–7. doi: 10.1097/QAI.0b013e31802f1318
141
Stein D Benjet C Gureje O Lund C Scott K Poznyak V et al . Integrating mental health with other non-communicable diseases. BMJ (2019) 28:364. doi: 10.1136/bmj.l295
142
Aflatoonian MR Sharifi I Parizi HM Fekri AR Aflatoonian B Sharifi M et al . A prospective cohort study of cutaneous leishmaniasis risk and opium addiction in south eastern Iran. PLoS One [Electronic Resource] (2014) 9(2):e89043. doi: 10.1371/journal.pone.0089043
143
Caixeta L Azevedo PV Caixeta M Reimer CH . Psychiatry disorders and dengue: is there a relationship? Arquivos Neuro-Psiquiatria (2011) 69:920–3. doi: 10.1590/S0004-282X2011000700014
144
Klis S Ranchor A Phillips RO Abass KM Tuah W Loth S et al . Good quality of life in former buruli ulcer patients with small lesions: Long-term follow-up of the BURULICO trial. PLoS Negl Trop Dis (2014) 8(7):e2964. doi: 10.1371/journal.pntd.0002964
145
Dadun D Van Brakel WH Peters RMH Lusli M Zweekhorst MBM Bunders JGF et al . Impact of socio-economic development, contact and peer counselling on stigma against persons affected by leprosy in cirebon, Indonesia - a randomised controlled trial. Leprosy Review (2017) 88:2–22. doi: 10.47276/lr.88.1.2
146
Lusli M Peters R van Brakel W Zweekhorst M Iancu S Bunders J et al . The impact of a rights-based counselling intervention to reduce stigma in people affected by leprosy in Indonesia. PloS Negl Trop Dis (2016) 10(12):e0005088. doi: 10.1371/journal.pntd.0005088
147
Aggithaya MG Narahari SR Sudha V Mohammed S Jacob NK Sushma KV . Self care integrative treatment demonstrated in rural community setting improves health related quality of life of lymphatic filariasis patients in endemic villages. Acta Tropica (2013) 126(3):198–204. doi: 10.1016/j.actatropica.2013.02.022
148
Cross H Beise K Choudhary R . A study of the linkage of poverty alleviation with self-care in south central Nepal. Leprosy Rev (2017) 88:306–17. doi: 10.47276/lr.88.3.306
149
Cross H Kumar Sah A . The experiences and attitudes of people affected by leprosy who voluntarily undertake leprosy services in Nepal. Leprosy Review (2014) 85:224–31. doi: 10.47276/lr.85.3.224
150
Pérez-Hernández MG Velasco-Rodríguez R Mora-Brambila AB Vázquez-Espinoza JA Maturano-Melgoza JA . Directed imagination: A procedure for improving self-concept in persons with leprosy. J Nurs Care JNC (2015) 4:4. doi: 10.4172/2167-1168.1000273
151
Budge PJ Little KM Mues KE Kennedy ED Prakash A Rout J et al . Impact of community-based lymphedema management on perceived disability among patients with lymphatic filariasis in orissa state, India. PLoS Negl Trop Dis (2013) 7(3):e2100. doi: 10.1371/journal.pntd.0002100
152
Sahienshadebie R Geest S Schallig HDFH . Nuancing stigma through ethnography: the case of cutaneous leishmaniasis in Suriname. Soc Sci Med (2016) 151:139–46. doi: 10.1016/j.socscimed.2015.12.044
153
Chahed MK Bellali H Ben Jemaa S Bellaj T . Psychological and psychosocial consequences of zoonotic cutaneous leishmaniasis among women in Tunisia: Preliminary findings from an exploratory study. PloS Negl Trop Dis [electronic resource] (2016) 10:e0005090. doi: 10.1371/journal.pntd.0005090
154
Al-Kamel M . Stigmata in cutaneous leishmaniasis: Historical and new evidence-based concepts. Our Dermatol Online (2017) 8(1):81–90. doi: 10.7241/ourd.20171.21
155
Ayode D Tora A Farrell D Tadele G Davey G McBride CM . Dual perspectives on stigma: reports of experienced and enacted stigma by those affected and unaffected by podoconiosis. J Public Health Research (2016) 5(2):689.
156
Tsegay G Wubie M Degu G Tamiru A Cooper M Davey G . Barriers to access and re-attendance for treatment of podoconiosis: a qualitative study in northern Ethiopia. Int Health (2015) 7:285–92. doi: 10.1093/inthealth/ihu085
157
Bekele K Deribe K Amberbir T Tadele G Davey G Samuel A . Burden assessment of podoconiosis in wayu tuka woreda, East wollega zone, Western Ethiopia: a community-based cross-sectional study. BMJ Open (2016) 6:e012308. doi: 10.1136/bmjopen-2016-012308
158
Majumder N . Socio-economic and health status of leprosy affected person: A study in Jharkhand. Indian J Leprosy (2015) 87:145–54.
159
Lambert SM Walker SL . The deportation of two Ethiopian migrant workers with leprosy. Leprosy Review (2015) 86:108–11. doi: 10.47276/lr.86.1.108
160
Pryce J Mableson HE Ramesh C Pandey BD Aley D Betts H et al . Assessing the feasibility of integration of self-care for filarial lymphoedema into existing community leprosy self-help groups in Nepal. BMC Public Health (2018) 18:201. doi: 10.1186/s12889-018-5099-0
161
Hossain QZ Hadi AA Boiragee J Parvin M Azad- Q . Demographic and psychological life of leprosy affected people in Bangladesh. Int J perceptions Public Health (2016) 1:25–34.
162
Kolay S Bisai S Pal R Mohanta P Sarbapalli D . Knowledge, attitude and stigma experienced by leprosy patients in tribal concentrated bastar district of chhattisgarh, India. Turkish J Public Health (2016) 14(3):178–187.
163
Dako-Gyeke M . Courtesy stigma: A concealed consternation among caregivers of people affected by leprosy. Soc Sci Med (2018) 196:190–6. doi: 10.1016/j.socscimed.2017.11.030
164
Asampong E Dako-Gyeke M Oduro R . Caregivers' views on stigmatization and discrimination of people affected by leprosy in Ghana. PLoS Negl Trop Diseases (2018) 12(1):e0006219. doi: 10.1371/journal.pntd.0006219
165
Dako-Gyeke M Asampong E Oduro R . Stigmatisation and discrimination: Experiences of people affected by leprosy in southern Ghana. Leprosy Review (2017) 88:58–74. doi: 10.47276/lr.88.1.58
166
Tora A Desta A Getnet T Farrell D Davey G McBride CM . Interpretations of education about gene-environment influences on health in rural Ethiopia: the context of a neglected tropical disease. Int Health (2016) 8(4):253–60. doi: 10.1093/inthealth/ihw016
167
Chen I Cheng S Sheu S . The meaning of physical activity for older adults with leprosy: a life story inside the wall. Leprosy Review (2017) 88:399–409. doi: 10.47276/lr.88.3.399
168
Lusli M Peters RMH Zweekhorst MBM Brakel WH Seda FSSE Bunders JFG . Lay and peer counsellors to reduce leprosy-related stigma–lessons learnt in cirebon, Indonesia. Leprosy Rev (2015) 86(1):37–53. doi: 10.47276/lr.86.1.37
169
Lusli M Zweekhorst M Miranda-Galarza B Peters R Cummings S Seda F et al . Dealing with stigma: experiences of persons affected by disabilities and leprosy. BioMed Res Int (2015) 28:261329. doi: 10.1155/2015/261329
170
Win LL Shwe S Myint K Ishidas Y Tun TM Mar KK et al . Factors influencing proper plantar ulcer care of leprosy patients: Experience from Mon-ywa township of disabilities survey project, Myanmar. Global J Dermatol Venereology (2013) 1:37–40. doi: 10.12970/2310-998X.2013.01.02.4
171
Loures LF Mármora CHC Barreto J Duppre NC . Perception of stigma and social impacts on individuals with hansen's disease. Psicologia em Estudo (2016) 21:665–75. doi: 10.4025/psicolestud.v21i4.30037
172
Astutik E Gayatri D . Perceived stigma in people affected by leprosy in leprosy village of sinatala, tangerang district, banten province, Indonesia. Kesmas: Natl Public Health J (2018) 12(4):187. doi: 10.21109/kesmas.v12i4.1756
173
Dadun Peters RMH Van Brakel WH Lusli M Damayanti R Bunders JFG et al . Cultural validation of a new instrument to measure leprosy-related stigma: the SARI stigma scale. Leprosy Review (2017) 88:23–42. doi: 10.47276/lr.88.1.23
174
Yan L Shen J Zhou M Zhang G . Survey on child leprosy patients and problems resulted from the disease in China. Leprosy Review (2015) 86:75–9. doi: 10.47276/lr.86.1.75
175
Ramasamy S Govindharaj P Panneerselvam S Kumar A . Factors associated with social participation of women affected with leprosy reporting at a referral centre in chhattisgarh, India. Leprosy Review (2018) 89:56–64. doi: 10.47276/lr.89.1.56
176
Peters R Zweekhorst M van Brakel W Bunders J Irwanto . People like me don't make things like that': Participatory video as a method for reducing leprosy-related stigma. Global Public Health: Int J Research Policy Practice (2016) 11:666–82. doi: 10.1080/17441692.2016.1153122
177
Pitchaimani G Joydeepa D John AS Suresh M . Children and adolescents' attitude towards having leprosy in a high endemic district of India. Leprosy Review (2016) 87:42–52. doi: 10.47276/lr.87.1.42
178
Reis BM Fernandes LFRM de Castro SS . Limitation of activity and restriction of social participation in relation to age range, gender, and education in people with leprosy. Anais Brasileiros Dermatologia (2017) 92:335–9. doi: 10.1590/abd1806-4841.20175216
179
Costa Pinheiro MG Rodrigues Monteiro B Rodrigues de Medeiros E de Souza Silva F Albino Simpson C Nunes de Miranda FA et al Repercussion of segregation in the lives of children separated by leprosy. International Archives of Medicine (2016) 9(75):1–9. doi: 10.3823/1946
180
Mandal NK Saha G . A qualitative assessment of current perception of different social groups about leprosy in high & low prevalent districts of West Bengal. J Compr Health (2015) 3(2):1–58. doi: 10.53553/JCH.v03i02.004
181
Sangeeta S . Using campaigns to de-stigmatize leprosy in India: stories from the field. (Special Issue: Health communication.) J Creative Commun (2014) 9:1–21. doi: 10.1177/0973258613517434
182
Katoch K Aggarwal A Yadav V Pandey A . National sample survey to assess the new case disease burden of leprosy in India. Indian J Med Res (2017) 146(5):585–605. doi: 10.4103/ijmr.IJMR_1496_16
183
Van Haaren MAC Reyme M Lawrence M Menke J Kaptein AA . Illness perceptions of leprosy-cured individuals in Surinam with residual disfigurements - "i am cured, but still i am ill". Chronic. Illness (2017) 13:117–27. doi: 10.1177/1742395316657398
184
Bergman L Britton A Kneck Å . Health-related stigma related to leprosy: What can be learned from nurses in Ghana? Nordic J Nurs Res (2017) 38(2):96–102. doi: 10.1177/2057158517719603
185
Okindo EG Kutima HL Mutai J Kasili S . Attitude and practices of household heads towards leishmaniases infections in marigat sub-county, baringo county, Kenya. East Afr Med J (2017) 94:86–94.
186
Peters RM Dadun Zweekhorst MB Bunders JF Irwanto van Brakel WH . A cluster-randomized controlled intervention study to assess the effect of a contact intervention in reducing leprosy-related stigma in Indonesia. PLoS Negl Trop Dis [electronic resource] (2015) 9:e0004003. doi: 10.1371/journal.pntd.0004003
187
Tabah EN Nsagha DS Bissek ACZK Njamnshi TN Njih INN Pluschke G et al . Community knowledge, perceptions and attitudes regarding leprosy in rural Cameroon: The case of ekondotiti and mbonge health districts in the south-west region. PLoS Negl Trop Dis (2018) 12(2):e0006233. doi: 10.1371/journal.pntd.0006233
188
Kaehler N Adhikari B Chapman R . Risk factors of perceived stigma in leprosy affected persons in non sombon leprosy colony, khon khaen province Vol. 27. . Thailand: J Health Research (2013).
189
Adhikari B Kaehler N Chapman RS Raut S Roche P . Factors affecting perceived stigma in leprosy affected persons in Western Nepal. PloS Negl Trop Diseases (2014) 8(6):e2940. doi: 10.1371/journal.pntd.0002940
190
Peters R Lusli M Zweekhorst M Miranda-Galarza B Brakel Wv Bunders I et al . Learning from a leprosy project in Indonesia: making mindsets explicit for stigma reduction. Dev Pract (2015) 25:1105–19. doi: 10.1080/09614524.2015.1081155
191
Dadun D Van Brakel WH Peters RMH Lusli M Zweekhorst MBM Bunders JGF et al . Impact of socio-economic development, contact and peer counselling on stigma against persons affected by leprosy in cirebon, Indonesia – a randomised controlled trial. Leprosy Review (2017) 88:2–22. doi: 10.47276/lr.88.1.2
192
Elsinga J Grobusch MP Tami A Gerstenbluth I Bailey A . Health-related impact on quality of life and coping strategies for chikungunya: a qualitative study in curacao. PLoS Negl Trop Diseases (2017) 11(10):e0005987. doi: 10.1371/journal.pntd.0005987
193
Zeeuw Jd Omansen TF Douwstra M Barogui YT Agossadou C Sopoh GE et al . Persisting social participation restrictions among former buruli ulcer patients in Ghana and Benin. PLoS Negl Trop Dis (2014) 8(12):e3418. doi: 10.1371/journal.pntd.0003303
194
Deribe K Tomczyk S Mousley E Tamiru A Davey G . Stigma towards a neglected tropical disease: felt and enacted stigma scores among podoconiosis patients in northern Ethiopia. BMC Public Health (2013) 13:1178. doi: 10.1186/1471-2458-13-1178
195
van’t Noordende AT van Brakel WH Banstola N Dhakal KP . The impact of leprosy on marital relationships and sexual health among married women in Eastern Nepal. J Trop Med (2016) 2016:4230235. doi: 10.1155/2016/4230235
196
Abeje T Negera E Kebede E Hailu T Hassen I Lema T et al . Performance of general health workers in leprosy control activities at public health facilities in amhara and oromia states, Ethiopia. BMC Health Serv Res (2016) 16:122. doi: 10.1186/s12913-016-1329-2
197
Henry M GalAn N Teasdale K Prado R Amar H Rays MS et al . Factors contributing to the delay in diagnosis and continued transmission of leprosy in Brazil–an explorative, quantitative, questionnaire based study. PLoS Negl Trop Dis [electronic resource] (2016) 10(3):e0004542. doi: 10.1371/journal.pntd.0004542
198
Kaehler N Adhikari B Raut S Marahatta SB Chapman RS . Perceived stigma towards leprosy among community members living close to nonsomboon leprosy colony in Thailand. PloS One (2015) 10(6):e0129086. doi: 10.1371/journal.pone.0129086
199
Marahatta S Ghimire A Jha N Pokhrel SM Rayamajhi S Jirel S . Social stigma in leprosy. J Chitwan Med College (2015) 5:6. doi: 10.3126/jcmc.v5i2.13148
200
Cunha MA Antunes DE Da Silveira RW Goulart IM . Application of the SRQ20 and the protocol of psychological assessment in patients with leprosy in a reference centre in Brazil. Leprosy Review (2015) 86:229–39. doi: 10.47276/lr.86.3.229
201
McBride CM Price CS Ayode D . A cluster randomized intervention trial to promote shoe use by children at high risk for podoconiosis. Int J Health Sci Res (2015) 5(6):518–28.
202
Miranda-Galarza B Lusli M Dedding CWM Budge FM Zweekhorst MBM . The power of personal knowledge: reflecting on conscientization in lives of disabled people and people affected by leprosy in cirebon, Indonesia. Knowledge Manage Dev J (2013) 9:85–104.
203
Monteiro EMLM Merces A Cavalcanti A Cavalcanti A Lacerda A Silva R et al . Culture circle as a teaching approach in the education of teenager health multipliers on leprosy awareness. (Special issue: Health education and promotion initiatives.). Health (2015) 7:1813–23. doi: 10.4236/health.2015.714199
204
Alamsyah T Usman S Yusuf M Elvin SD . Effectiveness of traditional healers in program to control leprosy in nagan raya district in aceh. Dermatol Res Practice (2018) 2018:3176762. doi: 10.1155/2018/3176762
205
Lenka D Mahapatra A . Role of reconstructive surgery (RCS) in improving the quality of life of leprosy afflicted persons. Indian J leprosy (2016) 88(1):7–12.
206
Valsa A Longmore M Mannam E Richard J . Effectiveness of social skills training for reduction of self-perceived stigma in leprosy patients in rural India - a preliminary study. Leprosy Review (2012) 83:80–92. doi: 10.47276/lr.83.1.80
207
Deepak S Hansine PE Braccini C . Self-care groups of leprosy-affected people in Mozambique. Leprosy Review (2013) 84:283–91. doi: 10.47276/lr.84.4.283
208
Bailey F Mondragon-Shem K Haines LR Olabi A Alorfi A Ruiz-Postigo JA et al . Cutaneous leishmaniasis and co-morbid major depressive disorder: A systematic review with burden estimates. PloS Negl Trop Diseases (2019) 13(2):e0007092. doi: 10.1371/journal.pntd.0007092
209
Morys JM Jezewska M Korzeniewski K . Neuropsychiatric manifestations of some tropical diseases. Int Marit Health (2015) 66(1):30–5. doi: 10.5603/IMH.2015.0009
210
Das S Leibowitz G . Mental health needs of people living with HIV/AIDS in India: a literature review. AIDS Care (2011) 23(4):417–25. doi: 10.1080/09540121.2010.507752
211
Van Brakel WH . Measuring health-related stigma–a literature review. Psychol Health Med (2006) 11(3):307–34. doi: 10.1080/13548500600595160
212
Sharma D Joshi A Kumar P . Stigma and psychological problems encountered by people with leprosy and how counselling helps: A systematic review. Int J Indian Psychol (2017) 4:176–86. doi: 10.25215/0404.039
213
Adhikari B Kaehler N Raut S Marahatta S Gyanwali K Chapman R . Risk factors of stigma related to leprosy. A systematic review JMMIHS (2013) 1:1–9.
214
Alonso L . Stigmatizing neglected tropical diseases: a systematic review. Soc Med (2010) 5(4):218–27.
215
Castro C . Reducing stigmatisation of leprosy: What is being done? J Tradi Med Clin Natur (2016) 5:194. doi: 10.4172/2573-4555.1000194
216
Marcela Castro C Erazo L Gunturiz ML . Strategies for reducing leprosy stigma. Mycobact. Dis (2018) 8(1):253. doi: 10.4172/2161-1068.1000253
217
Rao PSSS . Perspectives on the impact of stigma in leprosy: strategies to improve access to health care. Res Rep Trop Med (2015) 6:49–57. doi: 10.2147/RRTM.S55903
218
Abass K van der Werf T Phillips R Sarfo F Abotsi J Mireku S et al . Buruli ulcer control in a highly endemic district in Ghana: role of community-based surveillance volunteers. Am J Trop Med hygiene (2015) 92(1):115. doi: 10.4269/ajtmh.14-0405
219
Arellano C Castro L Díaz-Caravantes R Ernst K Hayden M Reyes-Castro P . Knowledge and beliefs about dengue transmission and their relationship with prevention practices in hermosillo, Sonora. Front Public Health (2015) 3:142. doi: 10.3389/fpubh.2015.00142
220
Ebenso B Fashona A Ayuba M Idah M Adeyemi G S-Fada S . Impact of socio-economic rehabilitation on leprosy stigma in northern Nigeria: findings of a retrospective study. Asia Pacific Disability Rehabil J (2007) 18(2):98–119.
221
Heijnders M van der Meij S . The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychology Health Med (2006) 11(3):353–63. doi: 10.1080/13548500600595327
222
Lund C De Silva M Plagerson S Cooper S Chisholm D Das J et al . Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. Lancet (2011) 378(9801):1502–14. doi: 10.1016/S0140-6736(11)60754-X
Summary
Keywords
wellbeing, neglected tropical diseases, stigma, leprosy, mental health
Citation
Koschorke M, Al-Haboubi YH, Tseng P-C, Semrau M and Eaton J (2022) Mental health, stigma, and neglected tropical diseases: A review and systematic mapping of the evidence. Front. Trop. Dis 3:808955. doi: 10.3389/fitd.2022.808955
Received
04 November 2021
Accepted
24 August 2022
Published
11 October 2022
Volume
3 - 2022
Edited by
Maria Teresa Ochoa, University of Southern California, United States
Reviewed by
Charles D. Mackenzie, Task Force for Global Health, United States; Wim H. van Brakel, NLR International, Netherlands
Updates
Copyright
© 2022 Koschorke, Al-Haboubi, Tseng, Semrau and Eaton.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julian Eaton, julian.eaton@lshtm.ac.uk
This article was submitted to Neglected Tropical Diseases, a section of the journal Frontiers in Tropical Diseases
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.