- 1College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
- 2Disease Control Unit, Ghana Health Service, Accra, Ghana
- 3Cancer and Infectious Diseases Epidemiology Research Unit (CIDERU), University of KwaZulu-Natal, Durban, KwaZulu-Natal, South Africa
- 4Institute of Health Research, University of Health and Allied Sciences, Ho, Ghana
Background: Addressing the knowledge gaps for female genital schistosomiasis (FGS) among healthcare professionals and community members in endemic areas to improve early detection and management is crucial. In Ghana, limited knowledge, entrenched socio-cultural beliefs, and inadequate healthcare resources hinder effective FGS management. This study utilized a systematic intervention mapping (IM) approach to design targeted health promotion interventions in Ghana’s Lower Manya-Krobo and Shai Osudoku Municipalities.
Methods: The five IM steps are as follows:1) Conducting needs assessment and identifying implementation adopters; 2) developing program objectives and outlining the desired outcome and performance objectives; 3) selecting theoretical methods and designing implementation strategies; 4) developing implementation materials, and tools, and protocols; and 5) evaluate implementation outcome. During the needs assessment, surveys and focused group discussions with 856 women and 252 healthcare workers and discussions with community members highlighted widespread misinformation and gaps in knowledge, attitudes, and practices related to FGS. Stakeholders’ engagement then guided the mapping of context-specific interventions and the development of program objectives. Intervention materials, including FGS posters, jingles in four languages, screening tools, and reporting forms, were created and distributed through accessible local channels. Training sessions were also conducted to build healthcare workers’ diagnostic and management capacities.
Results: The study revealed that Implementation mapping (IM), grounded in needs assessment and stakeholder involvement, facilitated the creation of tailored, evidence-based strategies. These strategies reached the intended population and improved awareness and attitudes among healthcare workers and community members. The findings emphasized the need for adaptive intervention that accounts for varying healthcare settings and community contexts to effectively address FGS knowledge gaps. It also revealed that the provision of adequate system support and needed logistics enhances FGS case diagnosis and management.
Conclusion: The intervention in Lower Manya-Krobo Municipal enhanced public health outcomes by improving community awareness, case detection, and management of FGS, demonstrating its potential for broader application in endemic regions. The study highlighted the need for tailored approaches to address varying healthcare dynamics and resource constraints. Continued monitoring and evaluation are crucial to ensure the long-term sustainability and effectiveness of such interventions, offering valuable insights for policymakers, clinicians, and public health practitioners.
Introduction
Female genital schistosomiasis (FGS) is a neglected tropical disease caused by the parasitic trematode, Schistosoma haematobium (S. haematobium), which poses a significant yet often overlooked threat to women’s reproductive health, particularly in sub-Saharan Africa (SSA) (1, 2). Over 100 million women of childbearing age are at risk, and an estimated 56 million are infected with FGS in the SSA (3, 4). Women and young girls become infected when the larval forms of the parasite, released by freshwater snails, penetrate the skin during contact with infested freshwater (1, 5). FGS is characterized by grainy, sandy patches in the mucosa, homogenous yellow sandy patches, abnormal blood vessels, and rubbery papules on the cervix of the female reproductive system (6–8). These changes occur when dead or viable ova of S. haematobium lodges in the genital tissues, resulting in lesions (2, 6–9). Infected women experience irregular vaginal bleeding often combined with purulent discharge (which can be stigmatizing), pelvic discomfort, genital itch, and dyspareunia (coital pain/general discomfort and pain during sex), often misdiagnosed as a sexually transmitted infection (STI) (6–8, 10, 11). Subfertility or infertility, ectopic pregnancy, spontaneous abortion, premature birth, low birth weight, and maternal death become the resulting outcome if FGS is left untreated (2, 6, 7, 10, 11).
Ghana is endemic for 14 of the 20 neglected tropical diseases (NTDs) that overlap geographically across the country. The country is ranked among the first five schistosomiasis-endemic countries in SSA, with approximately 20 million people at risk (12–15). The national prevalence of schistosomiasis is estimated at 23% but ranges between <1% and >50%, despite three decades of implementation of schistosomiasis mass drug administration (MDA) interventions among the at-risk population (15). Continuous transmission is attributed to localized drivers such as dam construction and irrigation, agricultural practices, and contact with surface water for domestic chores or economic gains, among others (14, 15). Currently, 18 districts with over 400 communities along the Volta Lake are classified among the highly endemic areas in the country (16, 17). The current FGS burden in Ghana is unknown, but a study conducted along the Volta Lake reported an estimated 10% prevalence (18).
The complexity of FGS lies not only in its complicated pathophysiology but also in the pervasive knowledge gap surrounding its causes, transmission, diagnosis, and management among healthcare professionals and community members (19–23). A study by Kukula et al. demonstrated a gross lack of FGS knowledge among healthcare workers and community members in Ghana, which poses a challenge to case detection and management (22). Similar findings were reported by Yirenya-Tawiah et al. in a study conducted in the Afram basin of Ghana (23). These findings align with what Mazigo et al. discovered in Tanzania among community members and healthcare professionals (19–21). Most respondents knew about schistosomiasis or bilharzia that affects boys but did not know of FGS. Some respondents believed FGS was transmitted sexually. Thus, infested adolescents were mocked by their peers (19–22).
As studies have acknowledged the urgent need for targeted interventions to address these identified FGS gaps, this study explores the application of Implementation Mapping (IM) using Intervention Mapping (IM) as a robust framework for developing and implementing context-specific strategies (24–27). By combining evidence-based research, stakeholder engagement, and a tailored approach to diverse settings (24, 26–30), Implementation Mapping and Intervention Mapping provides a systematic methodology to bridge the knowledge gap of FGS. Intervention Mapping has been employed in immunization and different disease areas such as non-communicable diseases, cancer, and NTDs, and has proven its usefulness and robustness in addressing complex issues (28, 30). As our baseline study has revealed the knowledge, attitudes, and practices (KAP) gap and the influencing factors, Implementation mapping (IM) emerges as a promising avenue to design interventions that are not only grounded in scientific rigor but are also sensitive to context. Hence, we advocate for a targeted and evidence-driven approach to empower communities, healthcare professionals, and policymakers in addressing this often-neglected aspect of women’s health.
For Ghana to advance towards the 2030 roadmap to end NTDs (31, 32), improving the knowledge, attitudes, and practices towards schistosomiasis and FGS through context-specific improvement strategies in endemic areas cannot be overlooked (31). This study aims to underscore the process of selecting context-specific strategies that are designed and implemented to improve FGS knowledge and awareness among healthcare workers and community members in the Lower Manya-Krobo Municipal in the Eastern region of Ghana.
Methods
Study design
A cross-sectional study based on a mixed-method approach was conducted at baseline involving 432 women of reproductive age from 10 communities and 126 healthcare professionals from 14 health facilities reported elsewhere. The study assessed FGS knowledge, attitudes, and practices among community members and healthcare professionals. Based on our reported findings, we employed the Implementation mapping (IM) framework to inform the intervention content/package, design, implementation, and evaluation to address the knowledge gaps identified.
Study area and settings
The Lower Manya-Krobo Municipality (LMK) is one of the 18 schistosomiasis-endemic districts along the Volta Lake in the eastern region of Ghana. It covers an area of 1,476 square km, and Odumase Krobo is the district capital (33). Geographically, parts of the district stretch along Volta Lake while the other areas have streams, ponds, and rivers within the municipality that serve as the common source of water for inhabitants (33). Most inhabitants are farmers and traders, predominantly engaged in fishing and fish farming on Volta Lake, predisposing them to a high risk of schistosomiasis (33).
Sampling strategy
A purposive sampling strategy was employed to recruit 40 frontline healthcare workers (HCWs) involved in sexual and reproductive health (SRH) and health promotion (HP) services from 14 health facilities in the Lower Manya-Krobo Municipality (Appendix Table 1).
Implementation mapping using intervention mapping
Merging the insights from the field of implementation science and Intervention Mapping results in Implementation Mapping (27). This framework incorporates and builds on step 5 of Intervention Mapping by adding four tasks. Intervention mapping (IM) is a systematic process or framework for developing a concept and evidence-based health promotion interventions and establishing their implementation (24–28, 30). The Intervention Mapping (IM) process is a valuable tool that has been proven to increase behavioral change, cancer screening, vaccination uptake, and uptake of MDA for lymphatic filariasis across the globe (24–30). Here, the Implementation Mapping (IM) framework consists of five iterative steps with distinct tasks that direct the modification of significant personal characteristics and environmental factors into the health promotion program (25, 27, 34). The process is practical based on the stakeholder engagements and the theories employed to formulate context-based interventions and strategies to address identified health problems. The steps are: 1) conduct needs assessment and identify implementation team and adopters, 2) develop program objective and outline the desired outcome and performance objectives, 3) select theoretical methods and design implementation strategies, 4) develop implementation material, tools and protocols, and 5) evaluate the implementation outcomes (27). We briefly describe each step of the Implementation Mapping (IM) as follows.
Step 1 - Conduct needs assessment and identify implementation teams and adopters
Program designers often lack adequate understanding of the context and implementation requirements from the outset (27, 35, 36). Planners perform a needs assessment as part of task 1 of Implementation mapping (IM) to determine the facilitators and bottlenecks that affect program implementation. This step is required to carry out the program successfully and comprehend the factors influencing its success, hence, it entails involving all stakeholders, including adopters, implementers, and those in charge of maintaining the intervention (28, 37, 38). This step of Intervention Mapping (IM) is like Intervention Mapping Step 1.
Step 2 - Develop program objectives and outline the desired outcome and performance objectives
Adoption and implementation outcomes, performance goals, determinants, and change objective matrices are all defined by implementation planners (27, 35). The result explicitly outlines the objectives pertaining to adoption, implementation, or maintenance and is customized for adopters and implementers. For participants to successfully adopt, implement, and maintain the program, performance objectives specify “who has to do what” in order to accomplish these goals (24, 27, 35). These goals are focused on action, proposing specific actions for the duties and tasks required to guarantee the program’s effective implementation and ongoing viability.
Step 3 - Select theoretical methods and design implementation strategies
This step employs the use of theory-based methods aimed at influencing implementation determinants (24). These theoretical methods can influence both individual or organizational level change that fosters commitments. The impulse of this step is further explained by Elderege et al. and Fernansez et al. (24, 27).
Step 4 – Develop implementation materials, tools, and protocols
This stage requires program planners to design and produce implementation materials, tools, and protocols that will address the expected change (24, 27, 30). These materials go through team reviews of the draft content, pretest, refinement, and final product. The material development takes into account the purpose of the material, intended audience, determinants, and change objectives.
Step 5 – Evaluate the implementation outcome
This step ensures that the implemented strategies to address identified gaps are evaluated to assess the adoption and effectiveness of the implemented health promotion strategies.
Theoretical underpinning of the study
The need to identify the bottlenecks associated with the FGS intervention and gain an in-depth understanding of participants’ knowledge, attitudes, and practices towards FGS was based on the literature. Afterwards, the Reach Effectiveness Adoption Implementation and Maintenance (RE-AIM) framework was adopted for the design and evaluation of the intervention outcome (39). Using the RE-AIM framework we identified and addressed the reach, effectiveness, adoption, implementation, and maintenance, which will be fully addressed in another article (40).
Data analysis
Descriptive statistics and content analysis were computed using the data gathered for this study.
Results
Background characteristics
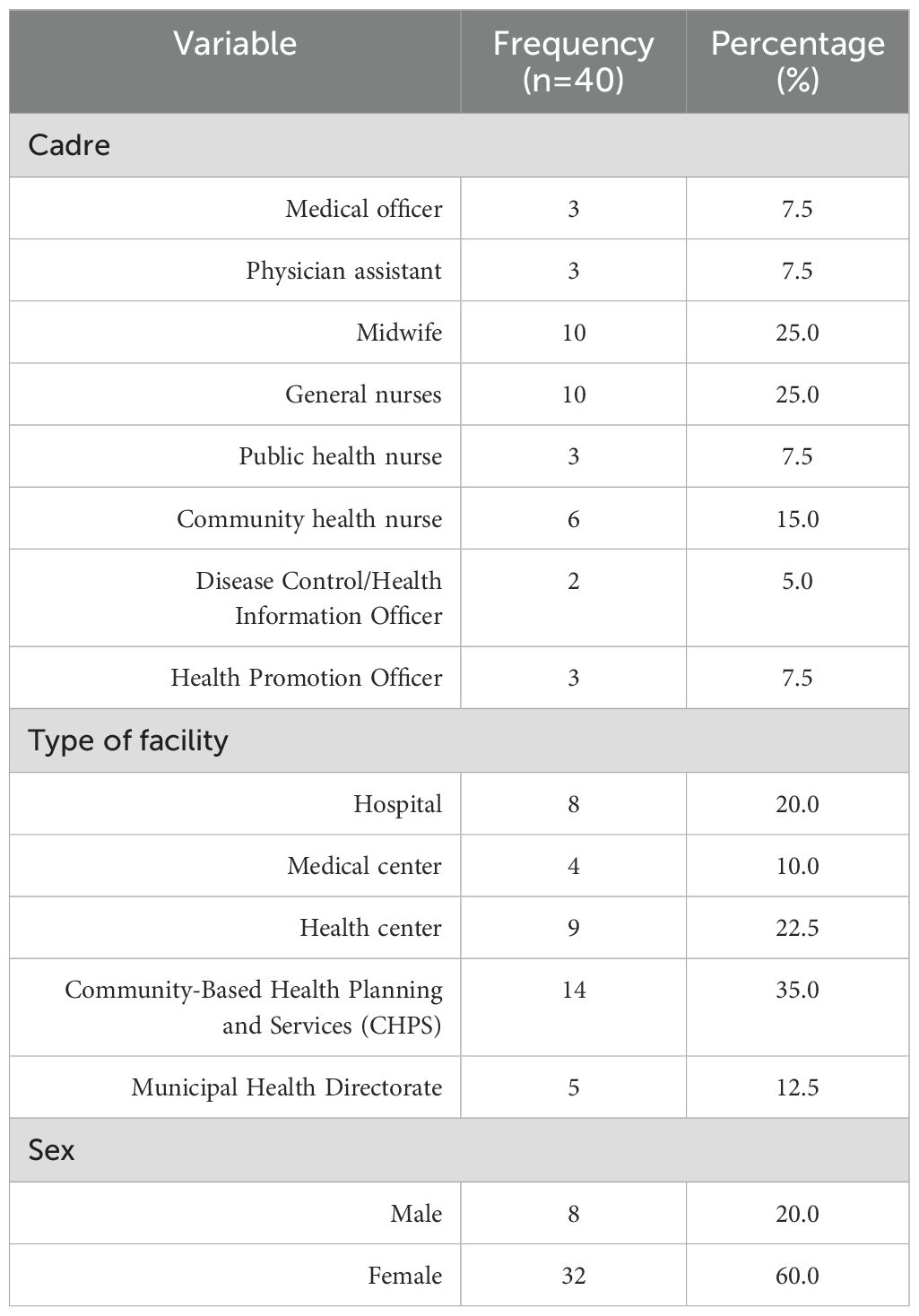
Among HCWs, there were 112 (88.9%) and 107 (84.9%) female participants in the Lower Manya-Krobo and Shai Osudoku, respectively. The majority of the participants in Lower Manya-Krobo Municipality were younger than 31 years (71, 56.4%), and 85 (67.5%) had practiced for less than 5 years. In contrast, in the Shai Osudoku District, 29 (23.0%) were younger than 31 years, and 94 (74.6%) had practiced for more than 5 years (Table 1A).
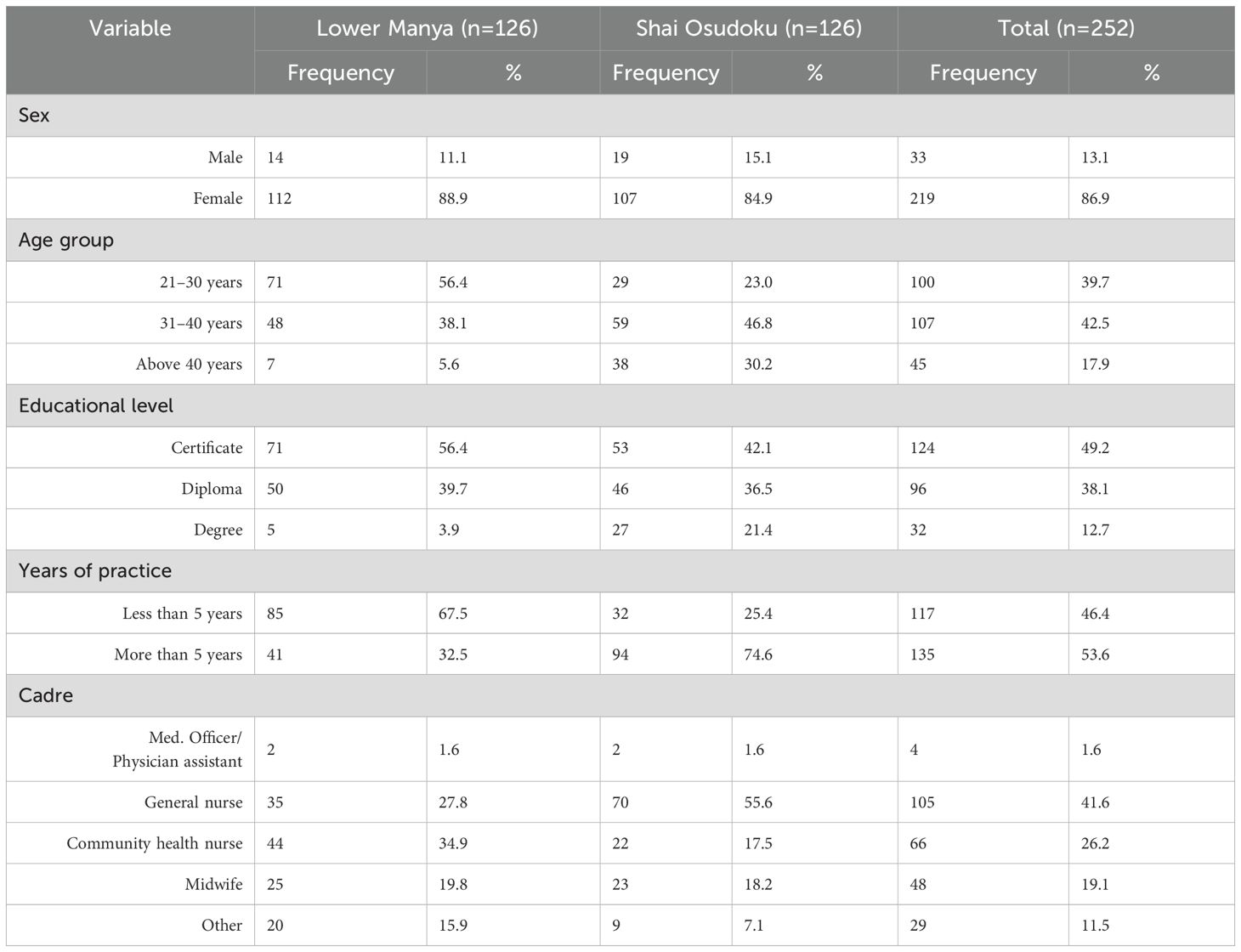
Table 1A. Characteristics of healthcare workers in the Lower Manya-Krobo and Shai Osudoku districts.
As shown in Table 1B, the mean age of the women was 29.4 (± 7.2) years. Furthermore, 225 (52.6%) and 238 (55.6%) respondents had received a primary education in the Lower Manya-Krobo and Shai Osudoku districts, respectively. Moreover 175 (40.9%) and 179 (41.8%) respondents had resided for more than 10 years in the LMK and SOD districts, respectively.
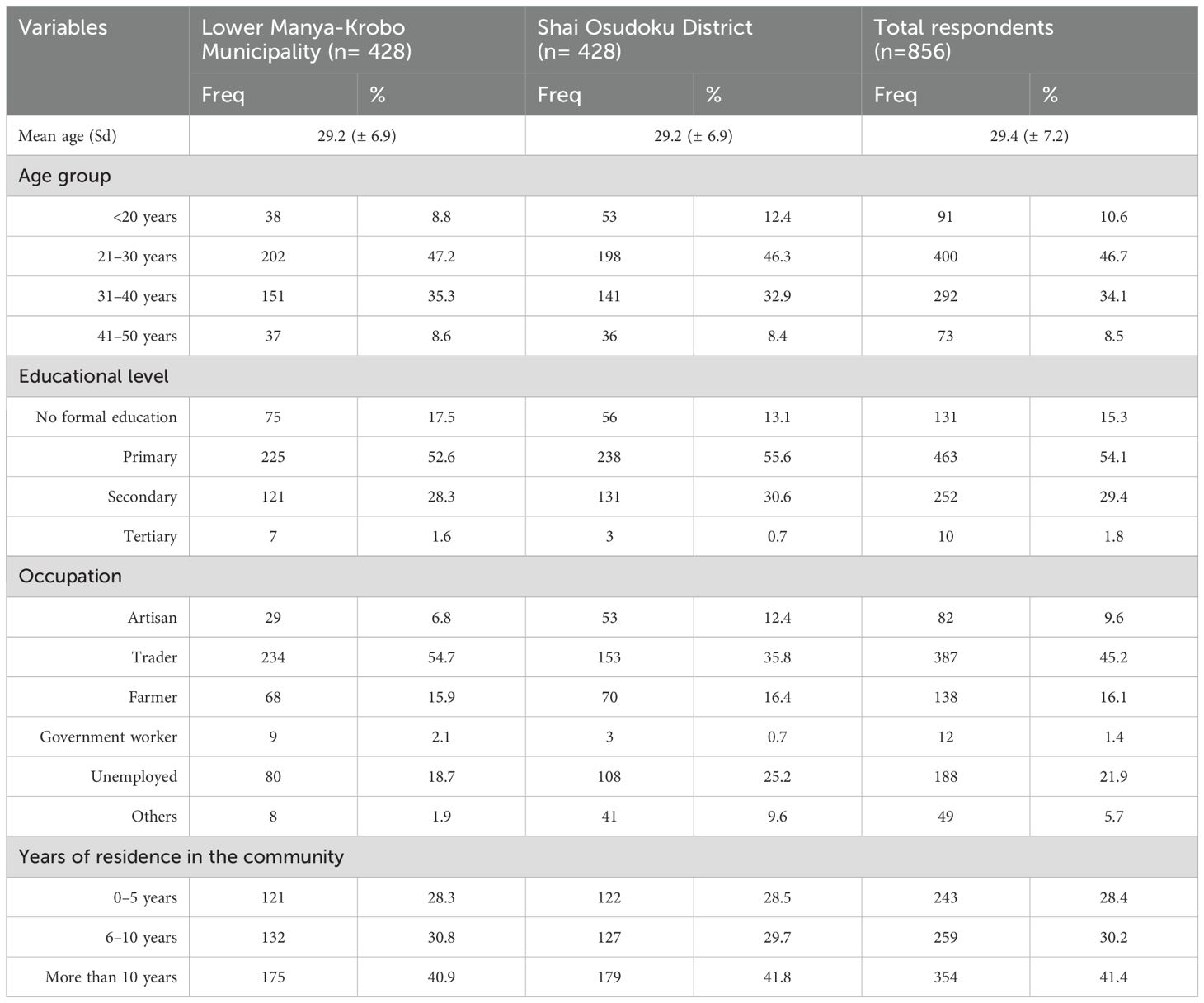
Table 1B. Characteristics of women of reproductive age in the Lower Manya-Krobo and Shai Osudoku districts.
Step 1 (Needs assessment): An initial needs assessment of knowledge, attitude, and practices towards FGS among healthcare workers and women of reproductive age using a mixed-method approach was conducted in the Lower Manya-Krobo Municipality and the Shai Osudoku District. We interviewed 856 women of reproductive age and 252 healthcare workers, with 8 focused group discussions (FGD) with women and adolescent girls, 20 key informant interviews (KIIs) among opinion leaders, and 36 KIIs among healthcare workers in 14 health facilities and 2 NTD focal persons from the district and regional health directorate respectively. The background characteristics of these healthcare workers have been described in Tables 1A and B.
The complexities of FGS and the influencing factors were discovered, gaining understanding and insight into the poor knowledge, attitudes, and practices among the service providers and women of reproductive age. Moreover, we engaged stakeholders from the national, regional, and district levels. The assessment revealed the lack of systemic support, skills, capacity, tools, and resources to diagnose and manage FGS in both districts, but these were worse in the Lower Manya-Krobo. The choice to implement an intervention in the Lower Manya-Krobo municipality was based on the outcome of the survey (Tables 2A, B), where a total score was generated for knowledge, attitudes, and practices. Correct responses were scored 1 point and 0 for a wrong response, with the responses summed upon completion. Knowledge, attitudes, and practices were categorized as “poor” if the score was below the mean and “good” if above the mean score.
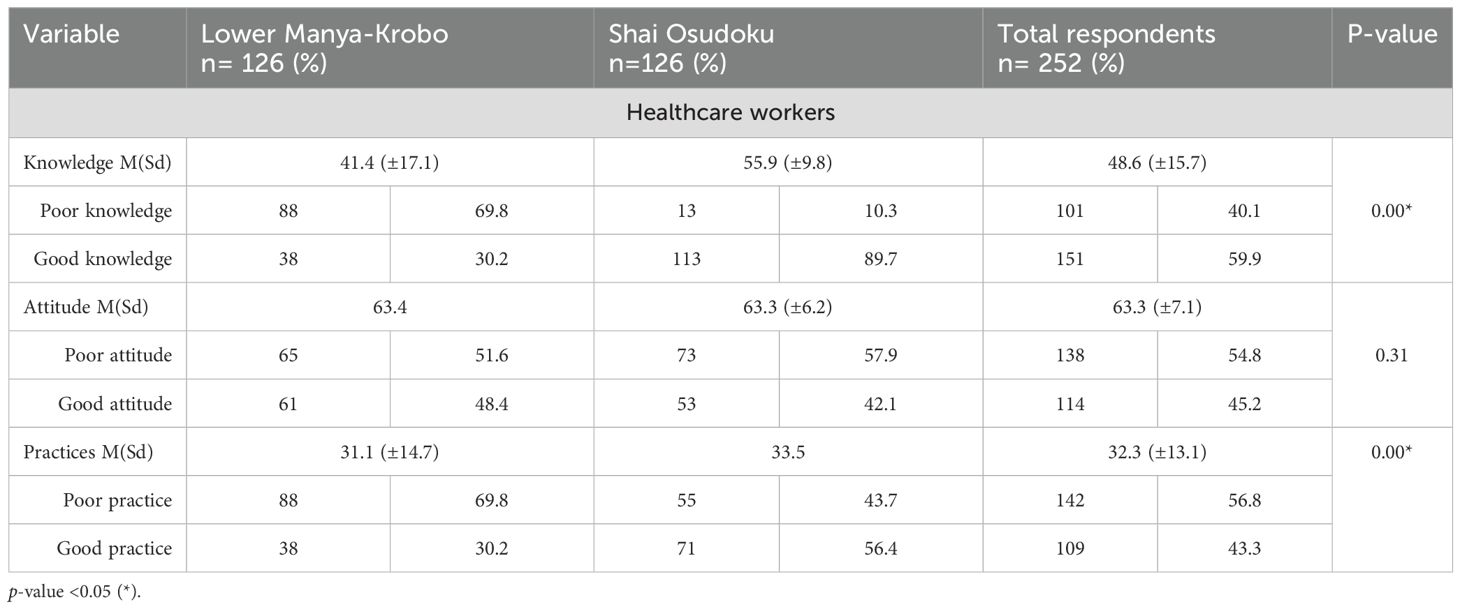
Table 2A. Description and categorization of mean score for healthcare workers’ (HCWs) knowledge, attitude, and practices towards FGS.
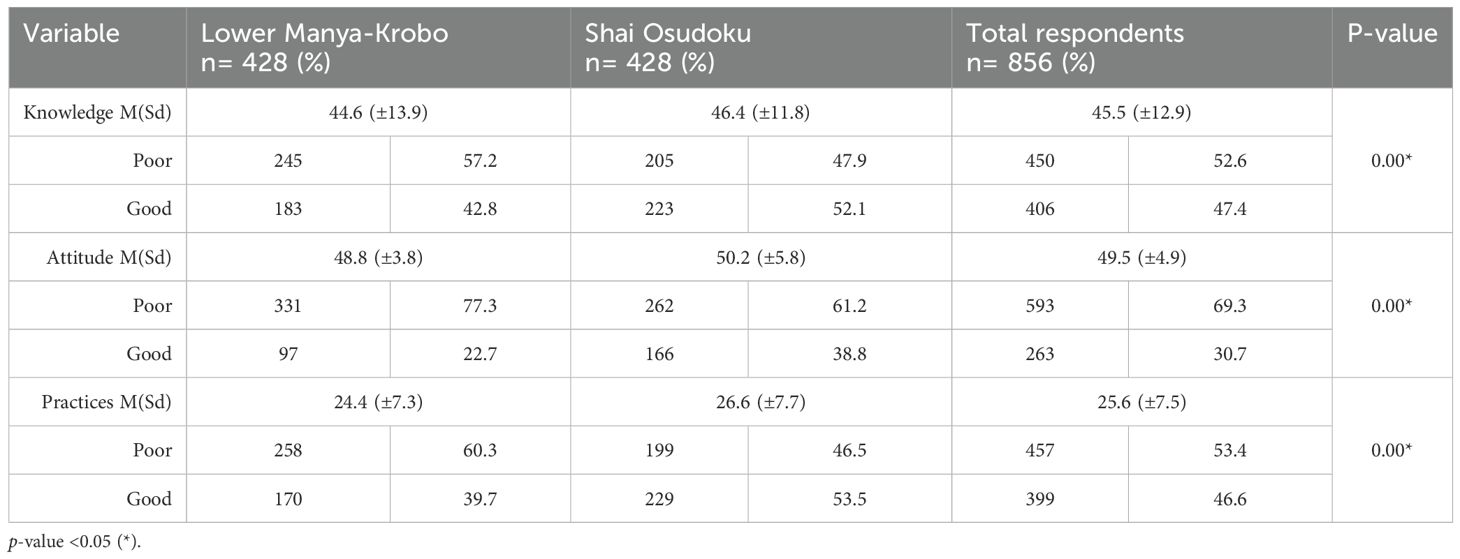
Table 2B. Description and categorization of the mean scores for women of reproductive age’s knowledge, attitude, and practices towards FGS.
Based on the outcome of the needs assessment, we identified the program adopters (physicians, clinical and public health nurses, and community members), implementors (nurses, health promotion officers, disease control officers, and opinion leaders), and other stakeholders (head of the facility, administrators, and NTD focal person at different levels) (24, 26, 27).
Step 2 (Develop program objective and implementation outcomes): After exploring the FGS KAPs through the needs assessment, the aim was to develop the program objective and outline the desired outcome and performance objectives required for behavior changes. Stakeholders were engaged at this stage of the Implementation mapping (IM) process to discuss the findings of the needs assessment. The included stakeholders were the 2 regional NTD focal persons (Greater Accra and Eastern regions), 2 District Directors of Health Services (Lower Manya-Krobo and Shai Osudoku Districts), 2 District Health Promotion Officers, 2 District Disease Control Officers, 2 District Public Health Nurses, 12 clinicians (Head of sub-districts), and 2 Health Information Officers. We also engaged two local government representatives, six community leaders, and a journalist from a television and radio station. During the session, specific contextual gaps identified during the needs assessment were discussed and addressed by developing evidence-based, context-specific strategies in concert with one another. Involving stakeholders in the process guarantees that the implementation techniques are applicable, realistic, and tailored to the requirements of the situation. The stakeholders then defined the program components, connected objectives, and created practical applications to implement the methods. Stakeholders were divided into three groups to brainstorm, discuss, and develop context-specific strategies to address the identified gaps (Table 3). An implementation team comprising seven members of district and sub-district staff was instituted. The team then identified the determinants for the implementers, adopters, and facilitators and the barriers to the project (41–43). Metrics of change objectives were then created across performance objectives and determinants to achieve the desired change objectives (Table 4) (35).
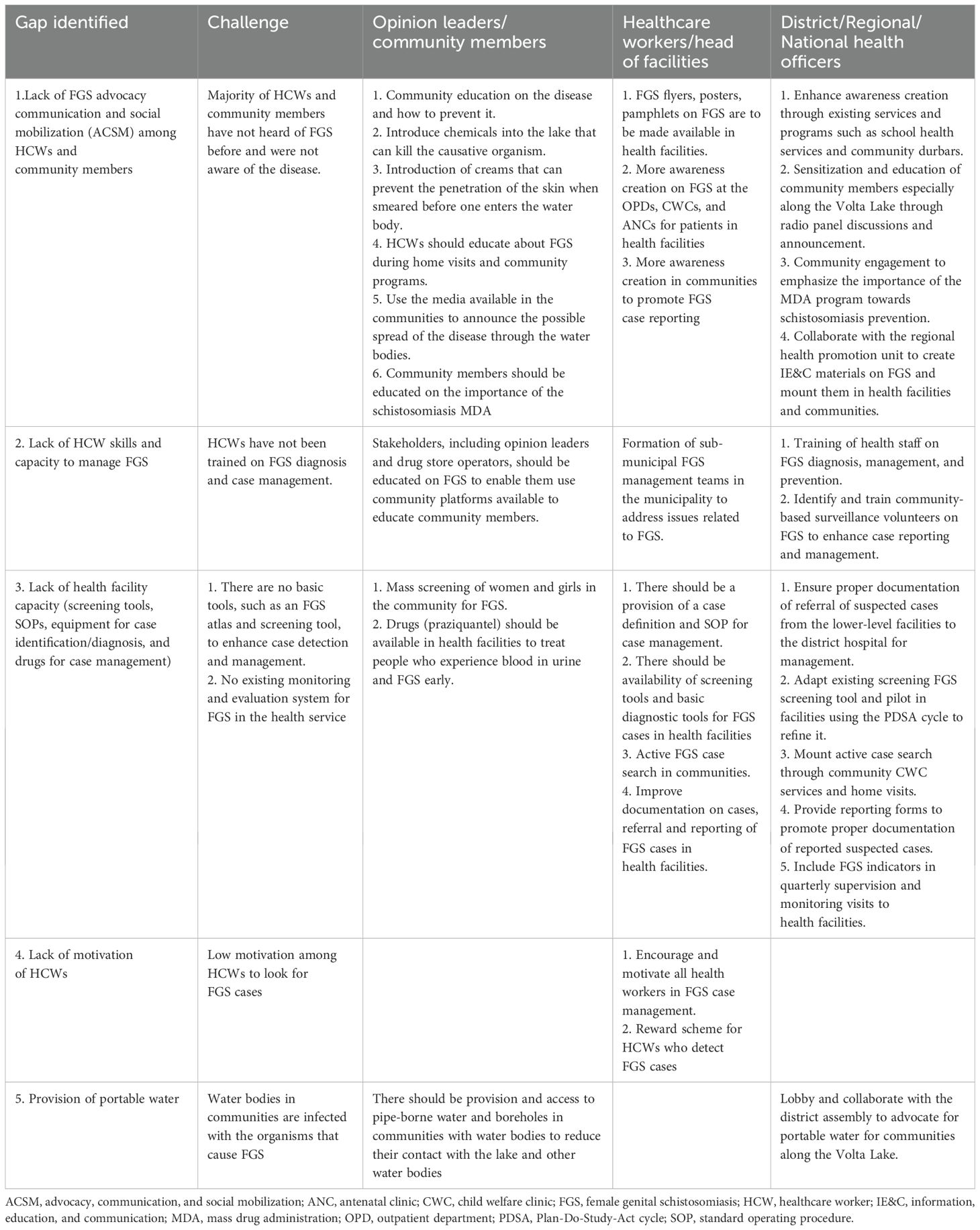
Table 3. Outcome of stakeholder group discussion to address gaps identified during the needs assessment.
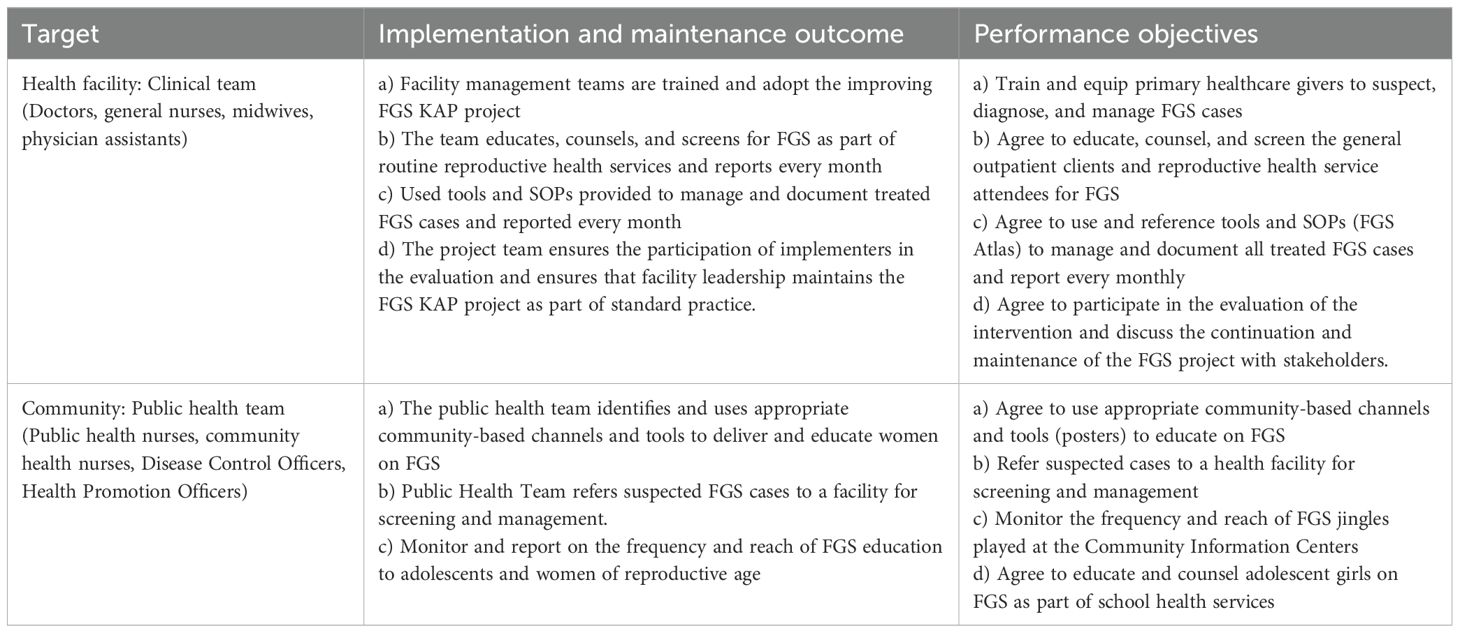
Table 4. Implementation outcomes and performance objectives to improve FGS KAP among healthcare workers and community members in the Lower Manya-Krobo Municipality.
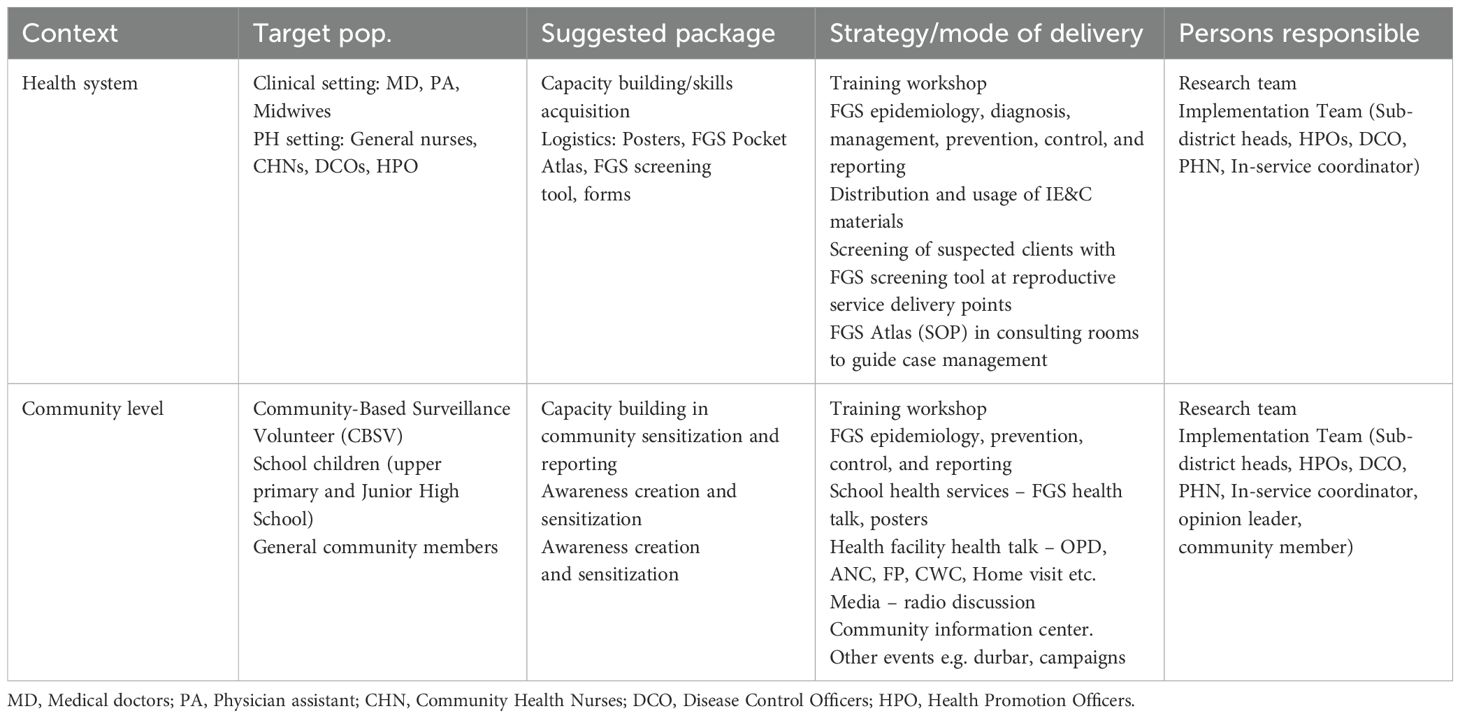
Step 3 (Select theoretical methods and design implementation strategies): The implementation team consolidated the ideas into two broad categories based on the target population, i.e., healthcare workers and community members, to develop the implementation strategies, addressing the mode of delivery and implementers (Table 5) (24, 44). The team considered both individual and organizational level expected changes for the implementation of the project and the role of facility leadership (44).
Step 4 (Develop implementation materials, tools, and protocols): The research team mobilized resources and consulted the National NTD program for FGS educational materials and the WHO FGS Pocket Atlas. The team developed a training package by adopting a training manual developed by Liberia (31). The FGS intervention included a training workshop for 40 healthcare workers from 14 facilities at different levels and the directorate team. The topics covered included general information on FGS, symptoms and risk factors, screening and examination, treatment guide, and clinical pathway. Based on the WHO FGS Pocket Atlas, diagnosis of FGS in this intervention was done through visual inspection of the genital tract using a speculum and flashlight, since there was no colposcopy in the district (6, 7, 45).
The training was facilitated by a member of the National Schistosomiasis Expert Committee, a medical doctor, a health information officer, and a health promotion expert within the municipality.
Through iteration, the team developed an FGS poster that presented basic information about FGS that was to be posted in consulting rooms, outpatient departments, and the communities. The team developed a synopsis and produced FGS educational messages in four local languages (Krobo, Ewe, Twi, and English), which were aired on 16 community information centers at dawn and dusk from February to April 2024 in the Lower Manya-Krobo Municipality. Screening, reporting, and monitoring forms were developed to ensure proper documentation of every activity. This was to ensure that the adoption, implementation, and maintenance were considered at every stage of the Implementation Mapping process. Every intervention package was piloted to ensure it achieved the intended purpose.
Step 5 (Evaluate the implementation outcomes): We completed steps 1 to 4 with our target population in mind and conducted monitoring and evaluation of the FGS KAP intervention, which helped us to assess both the process and implementation outcomes (46). A common social media platform, WhatsApp, was used by the implementation team to enhance information sharing, review bottlenecks, and reinforce adherence to the intervention. A weekly meeting allowed sub-district representatives to present implementation reports. The implementation team also conducted monthly visits to facilities using a checklist, which helped to reinforce adherence to the protocols of intervention. Avenues included the outpatient departments (OPDs), schools, and the community information center (CIC).
Figure 1 shows the start of screening, which yielded suspected cases that were examined, and four positive FGS cases that were treated. Females who reported to the OPD, antenatal care, and the family and reproductive care unit with symptoms related to FGS were screened using the FGS screening tool and examined if required. The channels used for awareness creation included one-on-one education, OPD health talks, group meetings, community information center (CIC) publicity, durbar, home visits, school health services, child welfare clinics, family planning services, antenatal services, and market visits. By the end of June 2024, 17,002 women, 6,349 men, and 3,234 adolescents were reached with FGS education and awareness creation across the district.
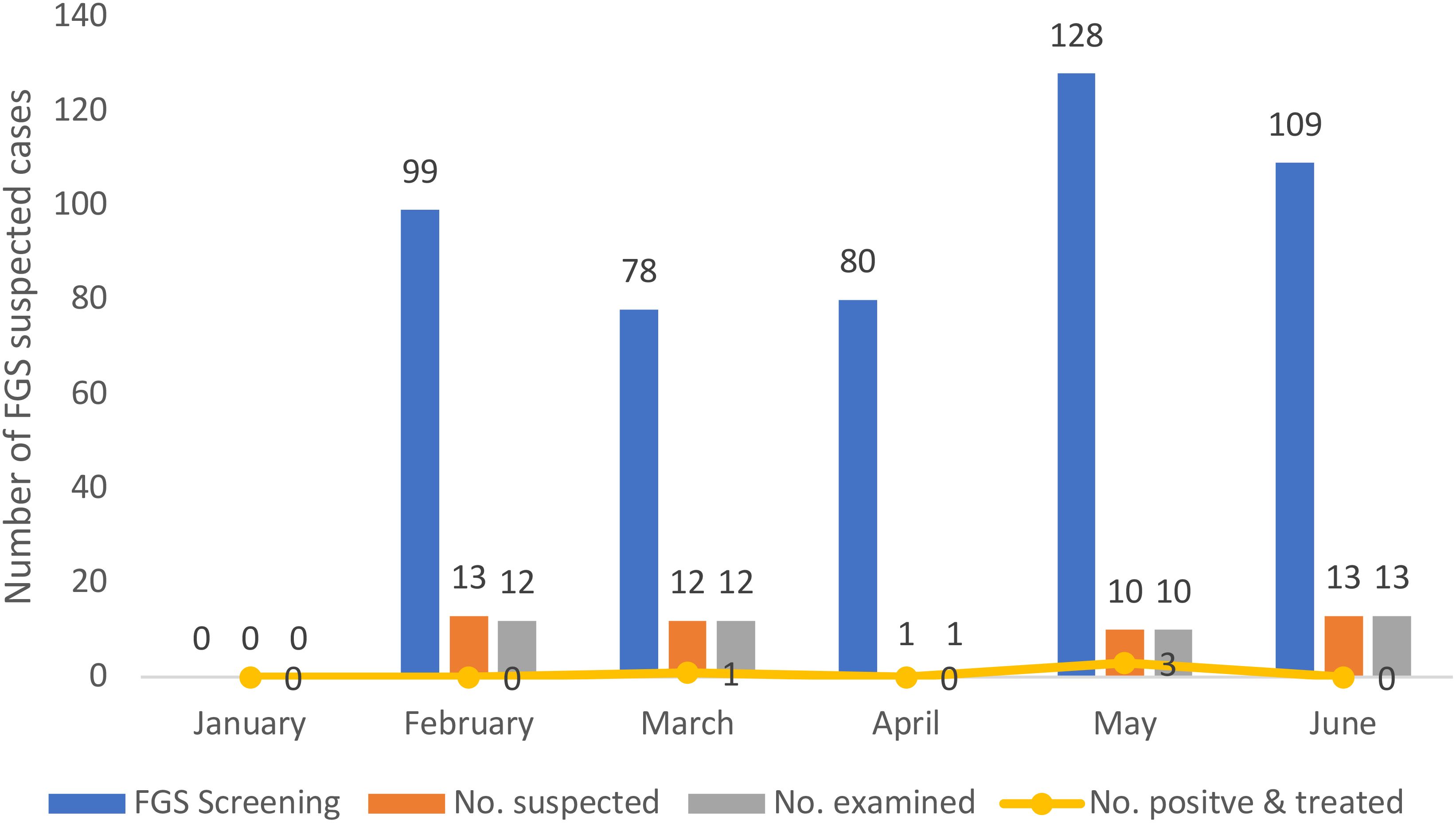
Figure 1. Screening outcome of suspected FGS cases in the Lower Manya-Krobo District from February to June 2024.
The evaluation of KAP after the intervention implemented in the Lower Manya-Krobo Municipal will be assessed and the results shared in the future. Between January to June 2024, the progressive outcome of the screening, management, and community sensitization are presented in Figure 1.
Discussion
This article presents an intervention plan to improve the awareness, case detection, and management of FGS among healthcare workers and women of reproductive age in the Lower Manya-Krobo Municipality. It also provides a foundation for addressing the FGS gaps identified through the needs assessment and provides future researchers with an intervention plan for FGS in endemic areas. Given the complications that could arise from FGS among affected populations, it is crucial to address the poor knowledge, attitudes, and practices towards FGS among healthcare workers and women of reproductive age. Therefore, the adoption of Implementation Mapping to systematically design and implement interventions in the Lower Manya-Krobo Municipal to address gaps in knowledge, attitudes, and practices regarding FGS showed potential benefits across several key areas. Since the implementation is ongoing, step five (evaluation of the intervention) will be described separately after completion of the intervention implementation.
Improved knowledge and awareness of FGS
The initial needs assessment revealed significant gaps in knowledge, attitudes, and practices about FGS among both healthcare workers and women of reproductive age, with poor knowledge, attitudes, and practices rates, especially in the Lower Manya-Krobo Municipality. The intervention targeted capacity building, skill development, and resource provision for healthcare workers and awareness creation among women of reproductive age to address the gaps. By engaging stakeholders at multiple levels and launching community awareness campaigns, including CIC broadcast in four local languages and educational materials such as posters, health talks at school services, and OPDs, the intervention aimed to raise awareness and encourage early reporting. Additionally, the provision of the FGS Pocket Atlas by the National NTD program and training of healthcare workers built capacity to detect and manage FGS cases. These efforts reached over 26,000 individuals, including women, men, and adolescents, suggesting that the initiative may have significantly expanded the community’s and healthcare workers’ understanding of FGS symptoms, transmission, and prevention and the need to detect and manage FGS early.
Reach and effectiveness—integration with community services and stakeholder engagement
The use of the various community-based channels, such as school health services, child welfare clinics, and local media, facilitated widespread dissemination of FGS information. By involving opinion leaders, local government representatives, and community members, the intervention ensured that educational activities were tailored to the specific needs and context of the Lower Manya-Krobo community. This participatory approach likely enhanced the acceptability and sustainability of the interventions.
Adoption—enhanced healthcare capacity and skills
The lack of healthcare workers trained to diagnose and manage FGS was identified as a critical challenge. Through training workshops that covered FGS epidemiology, diagnosis, management, prevention, and control, the intervention equipped healthcare workers with the necessary skills. This training was supplemented with logistical support, including screening tools, protocols, and educational materials, ensuring that health facilities were better prepared to identify and manage FGS cases.
The intervention led to the screening of 494 individuals for FGS over a 5-month period, identifying 48 suspected cases and confirming four positive diagnoses. This suggests that increased awareness and training may have directly contributed to a higher rate of case detection, which is critical for managing and reducing the prevalence of FGS.
Limitation and future evaluation
Due to the step-by-step insight this article revealed and its applicability in other primary healthcare and low-resource settings, the Implementation Mapping and implemented interventions showed improvement in FGS case detection, management, and awareness creation. While the intervention successfully laid the groundwork for addressing FGS, the full impact on long-term changes in KAP remains to be assessed. Due to resource constraints, the intervention could not include the radio program and training of community-based surveillance volunteers. Furthermore, due to time constraints, the researchers were not able to extend the implementation of the intervention beyond the time used in this study. Future evaluations will determine if the observed improvements in awareness and case detection translate into sustained behavior changes and a reduction in disease prevalence.
Conclusion
The implementation of the intervention in the Lower Manya-Krobo Municipal using Implementation Mapping demonstrated significant public health benefits, including enhanced community awareness, improved case detection, and better management of FGS cases. This finding underscores the feasibility of adapting this approach in other FGS-endemic areas guided by localized needs assessments. Scientifically, the study provides valuable insights into the adaptability and challenges of implementing interventions across varied healthcare settings.
Clinicians and healthcare policy makers are informed of the necessity to customize intervention packages to fit the unique dynamics and resource availability of each setting. For facilities with high patient load, the intervention highlighted the critical need for additional workforce and logistical support to prevent overburdening existing staff and to minimize patient waiting time. From a public health perspective, this work emphasizes the importance of sustained monitoring and evaluation to ensure long-term impact and sustainability of such interventions. These insights serve as a resource for public health practitioners, healthcare administrators, and researchers aiming to enhance the control and management of neglected tropical diseases such as FGS in resource-constrained settings.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical clearance was given by the Biomedical Research Ethics Committee (BREC) of the University of KwaZulu-Natal (BREC/00005309/2023) and the Ethics Review Committee of the Ghana Health Service (GHS-ERC:008/02/23). Participants consent was sort and information sheet given before commencement of the study.
Author contributions
CT: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. TG: Conceptualization, Methodology, Supervision, Writing – review & editing, Validation. JN: Conceptualization, Methodology, Supervision, Writing – review & editing, Validation. AM: Conceptualization, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. However, this research was made possible through a HEARD PhD scholarship at the University of KwaZulu-Natal (UKZN), funded by the Swedish International Development Agency (SIDA).
Acknowledgments
We are thankful to the Lower Manya-Krobo Health Directorate and staff for their cooperation and participation in the study implementation. We also thank the Ghana NTD Control Program, Eastern and Greater Accra Regional Health Directorates, and Shai Osudoku Health Directorates for their support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the view of HEARD, UKZN, and SIDA.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fitd.2025.1566451/full#supplementary-material
Abbreviations
CIC, Community information center; FGD, Focused group discussion; FGS, Female genital schistosomiasis; IM, Implementation Mapping; IM, Intervention Mapping; KAP, Knowledge, attitudes, and practices; KII, Key informant interview; MDA, Mass drug administration; NTD, Neglected tropical diseases; OPD, Outpatient department; S. haematobium, Schistosoma haematobium; SSA, sub-Saharan Africa; STI, Sexually transmitted infections.
References
1. WHO. Schistosomiasis Fact sheet (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/schistosomiasis (Accessed May 18, 2022).
2. Kjetland EF, Poggensee G, Helling-Giese G, Richter J, Sjaastad A, Chitsulo L, et al. Female genital schistosomiasis due to Schistosoma haematobium Clinical and parasitological findings in women in rural Malawi. Acta Trop. (1996) 62:239–55. doi: 10.1016/S0001-706X(96)00026-5
3. Gyapong M and Theobald S. “The sexual and reproductive health issue you’ve probably never heard of…,” in Open Democracy. London, United Kingdom: OpenDemocracy (2015) p. 50.
4. Ursini T, Scarso S, Mugassa S, Othman JB, Yussuph AJ, Ndaboine E, et al. Assessing the prevalence of Female Genital Schistosomiasis and comparing the acceptability and performance of health worker-collected and self-collected cervical-vaginal swabs using PCR testing among women in North-Western Tanzania: The ShWAB study. PloS Negl Trop Dis. (2023) 17:e0011465. doi: 10.1371/journal.pntd.0011465
5. Ekpo U, Odeyemi OM, Sam-Wobo SO, Onunkwor OB, Mogaji HO, Oluwole AS, et al. Female genital schistosomiasis (FGS) in Ogun State, Nigeria: a pilot survey on genital symptoms and clinical findings. Parasitol Open. (2017) 3:e10. doi: 10.1017/pao.2017.11
6. WHO. FEMALE GENITAL SCHISTOSOMIASIS: A pocket atlas for clinical health-care professional. Geneva, Switzerland: World Health Organization (2015). p. 49.
7. Norseth HM, Ndhlovu PD, Kleppa E, Randrianasolo BS, Jourdan PM, Roald B, et al. The colposcopic atlas of schistosomiasis in the lower female genital tract based on studies in Malawi, Zimbabwe, Madagascar and South Africa. PLoS Negl Trop Dis. (2014) 8:e3229. doi: 10.1371/journal.pntd.0003229
8. Kjetland EF, Leutscher PD, and Ndhlovu PD. A review of female genital schistosomiasis. Trends Parasitol. (2012) 28:58–65. doi: 10.1016/j.pt.2011.10.008
9. Helling-Giese G, Kjetland EF, Gundersen SG, Poggensee G, Richter J, Krantz I, et al. Schistosomiasis in women: manifestations in the upper reproductive tract. Acta Trop. (1996) 62:225–38. doi: 10.1016/S0001-706X(96)00025-3
10. USAID. No more neglect, Female genital schistosomiasis and HIV: Integrating sexual and reproductive health interventions to improve women’s lives. Geneva, Switzerland: USAID (2019) p. 1–44.
11. Hegertun IE, Sulheim Gundersen KM, Kleppa E, Zulu SG, Gundersen SG, Taylor M, et al. S. haematobium as a common cause of genital morbidity in girls: a cross-sectional study of children in South Africa. PLoS Negl Trop Dis. (2013) 7:e2104. doi: 10.1371/journal.pntd.0002104
12. Kulinkina AV, Walz Y, Koch M, Biritwum NK, Utzinger J, Naumova EN, et al. Improving spatial prediction of Schistosoma haematobium prevalence in southern Ghana through new remote sensors and local water access profiles. PLoS Negl Trop Dis. (2018) 12:e0006517. doi: 10.1371/journal.pntd.0006517
13. Adenowo AF, Oyinloye BE, Ogunyinka BI, and Kappo AP. Impact of human schistosomiasis in sub-Saharan Africa. Braz J Infect Dis. (2015) 19:196–205. doi: 10.1016/j.bjid.2014.11.004
14. Lai YS, Biedermann P, Ekpo UF, Garba A, Mathieu E, Midzi N, et al. Spatial distribution of schistosomiasis and treatment needs in sub-Saharan Africa: a systematic review and geostatistical analysis. Lancet Infect Dis. (2015) 15:927–40. doi: 10.1016/S1473-3099(15)00066-3
15. Hotez PJ and Kamath A. Neglected tropical diseases in sub-Saharan Africa: review of their prevalence, distribution, and disease burden. PLoS Neglect Trop Dis. (2009) 3:e412. doi: 10.1371/journal.pntd.0000412
16. Authority PHDVR. Summary of prevalence of Bilhazia for all districts (VRA Data). Accra, Ghana: Volta River Authority (2020). 2pg.
17. Volta River Authority. Corporate Social Responsibility (2024). Available online at: https://www.vra.com/csr/index.php.
18. Yirenya-Tawiah D, Amoah C, Apea-Kubi KA, Dade M, Ackumey M, Annang T, et al. A survey of female genital schistosomiasis of the lower reproductive tract in the volta basin of Ghana. Ghana Med J. (2011) 45:16–21. doi: 10.4314/gmj.v45i1.68917
19. Mazigo HJ, Samson A, Lambert VV, Kosia A, Ngoma DV, Murphy R, et al. We know about schistosomiasis but we know nothing about FGS”: A qualitative assessment of knowledge gaps about female genital schistosomiasis among communities living in Schistosoma haematobium endemic districts of Zanzibar and Northwestern Tanzania. PLoS Neglect Trop Dis. (2021) 15:1–25. doi: 10.1371/journal.pntd.0009789
20. Mazigo HD, Samson A, Lambert VJ, Kosia AL, Ngoma DD, Murphy R, et al. Healthcare workers’ Low knowledge of female genital schistosomiasis and proposed interventions to prevent, control, and manage the disease in zanzibar. Int J Public Health. (2022) 67:1604767. doi: 10.3389/ijph.2022.1604767
21. Mazigo HD, Samson A, Lambert VJ, Kosia AL, Ngoma DD, Murphy R, et al. Female genital schistosomiasis is a sexually transmitted disease”: Gaps in healthcare workers’ knowledge about female genital schistosomiasis in Tanzania. PLoS Global Public Health. (2022) 2:1–19. doi: 10.1371/journal.pgph.0000059
22. Kukula VA, MacPherson EE, Tsey IH, Stothard JR, Theobald S, Gyapong M, et al. A major hurdle in the elimination of urogenital schistosomiasis revealed: Identifying key gaps in knowledge and understanding of female genital schistosomiasis within communities and local health workers. PLoS Negl Trop Dis. (2019) 13:e0007207. doi: 10.1371/journal.pntd.0007207
23. Yirenya-Tawiah DR, Ackumey MM, and Bosompem KM. Knowledge and awareness of genital involvement and reproductive health consequences of urogenital schistosomiasis in endemic communities in Ghana: a cross-sectional study. Reprod Health. (2016) 13:117. doi: 10.1186/s12978-016-0238-5
24. Eldredge LKB, Markham CM, Ruiter RAC, Fernández ME, Kok G, Parcel GS, et al. Planning health promotion programs: an intervention mapping approach. New Jersey, USA: John Wiley & Sons (2016).
25. Scarinci IC, Bandura L, Hidalgo B, and Cherrington A. Development of a theory-based (PEN-3 and health belief model), culturally relevant intervention on cervical cancer prevention among Latina immigrants using intervention mapping. Health Promot Pract. (2012) 13:29–40. doi: 10.1177/1524839910366416
26. Bartholomew LK, Markham C, Mullen P, and Fernandez ME. Planning models for theory-based health promotion interventions. Health Behav: Theory Res Pract. (2015) 5:359–88.
27. Fernandez ME, Ten Hoor GA, Van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, et al. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. (2019) 7:158. doi: 10.3389/fpubh.2019.00158
28. Garba RM and Gadanya MA. The role of intervention mapping in designing disease prevention interventions: A systematic review of the literature. PLoS One. (2017) 12:e0174438. doi: 10.1371/journal.pone.0174438
29. Manyeh AK, Ibisomi L, Baiden F, Chirwa T, and Ramaswamy R. Using intervention mapping to design and implement quality improvement strategies towards elimination of lymphatic filariasis in Northern Ghana. PLoS Negl Trop Dis. (2019) 13:e0007267. doi: 10.1371/journal.pntd.0007267
30. Durks D, Fernandez-Llimos F, Hossain LN, Franco-Trigo L, Benrimoj SI, Sabater-Hernández D, et al. Use of intervention mapping to enhance health care professional practice: A systematic review. Health Educ Behav. (2017) 44:524–35. doi: 10.1177/1090198117709885
31. COUNTDOWN, Liberia, Ministry of Health Liberia, UKaid, PIRE, and LSTM. “Female Genital Schistosomiasis Intervention Training Manual”. In: Ministry of Health Liberia, editor. Liberia: Countdown & MoH Liberia (2021) p. 1–122.
32. NTD C. COUNTDOWN calling time on Neglected Tropical Diseases (2015). Available online at: https://countdown.lstmed.ac.uk/publications-resources.
33. Ghana Statistical Service. 2010 Population and housing census: District Report Lower Manya Krobo Municipality. Accra, Ghana: Ghana Statistical Service (2014) p. 1–97.
34. Green LW and Kreuter MW. Health program planning: An educational and ecological approach, ed. t. edition. New York: McGraw Hill (2005).
35. Highfield L, Valerio MA, Fernandez ME, and Eldridge-Bartholomew LK. Development of an implementation intervention using intervention mapping to increase mammography among low income women. Front Public Health. (2018) 6:300. doi: 10.3389/fpubh.2018.00300
36. Walker TJ, Kohl HW, Bartholomew JB, Green C, and Fernández ME. Using Implementation Mapping to develop and test an implementation strategy for active learning to promote physical activity in children: a feasibility study using a hybrid type 2 design. Implement Sci Commun. (2022) 3:26. doi: 10.1186/s43058-022-00271-9
37. Austin JD, Rodriguez SA, Savas LS, Megdal T, Ramondetta L, Fernandez ME, et al. Using intervention mapping to develop a provider intervention to increase HPV vaccination in a federally qualified health center. Front Public Health. (2020) 8:530596. doi: 10.3389/fpubh.2020.530596
38. Crawford CA, Shegog R, Savas LS, Frost EL, Healy CM, Coan SP, et al. Using intervention mapping to develop an efficacious multicomponent systems-based intervention to increase human papillomavirus (HPV) vaccination in a large urban pediatric clinic network. J Appl Res Child. (2019) 10:1–35.
39. King DK, Glasgow RE, and Leeman-Castillo B. Reaiming RE-AIM: using the model to plan, implement, and evaluate the effects of environmental change approaches to enhancing population health. Am J Public Health. (2010) 100:2076–84. doi: 10.2105/AJPH.2009.190959
40. Holtrop JS, Estabrooks PA, Gaglio B, Harden SM, Kessler RS, King DK, et al. Understanding and applying the RE-AIM framework: Clarifications and resources. J Clin Transl Sci. (2021) 5:e126. doi: 10.1017/cts.2021.789
41. Bandura A. Health promotion by social cognitive means. Health Educ Behav. (2004) 31:143–64. doi: 10.1177/1090198104263660
42. Ajzen I. The theory of planned behaviour: Reactions and reflections. Abingdon, Oxfordshire, UK: Taylor & Francis (2011) p. 1113–27.
43. Rosenstock IM, Strecher VJ, and Becker MH. Social learning theory and the health belief model. Health Educ Q. (1988) 15:175–83. doi: 10.1177/109019818801500203
44. Parcel GS, Simons-Morton BG, and Kolbe LJ. Health promotion: Integrating organizational change and student learning strategies. Health Educ Q. (1988) 15:435–50. doi: 10.1177/109019818801500405
45. Martinez SG, Mbabazi PS, Sebitloane MH, Vwalika B, Mocumbi S, Galaphaththi-Arachchige HN, et al. The WHO atlas for female-genital schistosomiasis: Co-design of a practicable diagnostic guide, digital support and training. PLoS Global Public Health. (2024) 4:e0002249. doi: 10.1371/journal.pgph.0002249
46. Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Admin Policy Ment Health Ment Health Serv Res. (2011) 38:65–76. doi: 10.1007/s10488-010-0319-7
Appendix
Keywords: female genital schistosomiasis, implementation mapping, Ghana, knowledge, attitudes, practices
Citation: Tetteh CD, Ginindza TG, Ncayiyana JR and Manyeh AK (2025) Tailoring interventions for impact: implementing evidence-based strategies for female genital schistosomiasis knowledge gaps in selected districts in Ghana. Front. Trop. Dis. 6:1566451. doi: 10.3389/fitd.2025.1566451
Received: 28 January 2025; Accepted: 22 April 2025;
Published: 19 June 2025.
Edited by:
Koert Ritmeijer, Médecins Sans Frontières, NetherlandsReviewed by:
Charles Abongomera, Swiss Tropical and Public Health Institute, SwitzerlandYabo Josiane Honkpehedji, Centre de Recherche Médicales de Lambaréné, Gabon
Copyright © 2025 Tetteh, Ginindza, Ncayiyana and Manyeh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Comfort Dede Tetteh, Y2RlZGV0ZXR0ZWhAZ21haWwuY29t
 Comfort Dede Tetteh
Comfort Dede Tetteh Themba G. Ginindza
Themba G. Ginindza Jabulani R. Ncayiyana
Jabulani R. Ncayiyana Alfred Kwesi Manyeh
Alfred Kwesi Manyeh