- 1Field Epidemiology and Laboratory Training Program, Moi University/Center for Disease Control and Prevention (CDC), Eldoret, Kenya
- 2Ministry of Health, Directorate of Health Policy, Monitoring and Evaluation, Nairobi, Kenya
- 3School of Nursing, Kibabii University, Bungoma, Kenya
- 4Moi University, Department of Epidemiology and Medical Statistics, School of Public Health, Eldoret, Kenya
Introduction: By 2023, HIV will have claimed 40.4 million lives, posing a significant global public health risk, with youth at the highest risk of new infections. Pre-exposure prophylaxis (PrEP) reduces HIV transmission by 48.9% when combined with other prevention strategies. Despite increased PrEP programs in sub-Saharan Africa since 2015, uptake remains low due to various barriers. This study aims to validate a model identifying demographic, economic, social, behavioral, and structural factors influencing PrEP use in Turbo Sub-County, where uptake is among the lowest.
Methods: The study will employ a descriptive cross-sectional design using both quantitative and qualitative methods to gather data from youths aged 15–24 in Turbo Sub-County. Participants will be selected through multistage random sampling based on Wards and villages. Data will be collected via self-administered questionnaires, interviews, and Focus Group Discussions (FGDs). Analysis will include thematic methods for qualitative data and Structural Equation Modeling (SEM) will be used to validate the relationships predicting PrEP uptake at 95% confidence intervals and α < 0.05.
Results: The study is expected to provide insights into factors influencing PrEP uptake among youths in Turbo Sub-County. The validated model will highlight key demographic, economic, and behavioral determinants, offering actionable data for enhancing HIV prevention strategies tailored to this population.
Discussion: The discussion will interpret the interplay of factors affecting PrEP uptake and compare findings with regional studies. It will emphasize community-specific barriers and enablers, informing targeted interventions and strategies to improve PrEP accessibility and acceptance.
Conclusions: The study aims to provide a validated framework for predicting PrEP uptake, guiding stakeholders in addressing barriers and strengthening interventions. The findings will support optimizing PrEP programs to reduce HIV transmission among at-risk youth.
1 Introduction
HIV remains a significant global public health threat, with an estimated 40.4 million deaths by 2023. In 2022, 1.3 million people contracted HIV, and 630,000 died from AIDS-related causes, with two-thirds of HIV-positive individuals living in Sub-Saharan Africa (1). The region continues to face a heavy burden, with 1.4 million of the 1.65 million HIV-positive youths aged 10–19 residing in Sub-Saharan Africa (2). Efforts to end the AIDS epidemic by 2030 are lagging behind, as the rise in new infections is particularly notable in Sub-Saharan Africa, accounting for 60% of new infections (3–5). Pre-Exposure Prophylaxis (PrEP) is recognized as a key biomedical strategy to prevent new infections in high-risk populations. By 2021, around 144 countries had adopted WHO guidelines for oral PrEP (1), with approximately 1.6 million people having used PrEP globally. PrEP uptake has notably increased in Sub-Saharan Africa, where nearly 91% of users in the region were recorded (6), though adolescents still face challenges (7). In Kenya, there were 1.4 million people living with HIV in 2022, and 12,000 new infections were among young people aged 15-24 (8). The number of new infections among adolescents increased by 16% in Uasin Gishu County, with Turbo and Kapseret sub-counties accounting for 50% of the newly diagnosed cases (9). PrEP uptake in Turbo stands at 26.7%, leading to this study, which seeks to understand the factors influencing PrEP use among youths aged 15–24 in Turbo Sub-County, Uasin Gishu, Kenya, with the goal of developing targeted interventions to improve PrEP uptake as well as validate a proposed model of determinants of PrEP uptake (10).
1.1 Problem statement
As of 2021, Kenya had 1.43 million HIV-positive individuals, with a prevalence of 4.3% (8). The country reported 32,027 new HIV infections, a 68.5% decline from 2013. Among individuals aged 15-24, there were 7,307 new infections and 145,142 living with HIV (MOH, 2021). Alarmingly, 47% of youths experience sexual and gender-based violence, which heightens their risk of HIV transmission. Pre-exposure prophylaxis (PrEP) has proven to be an effective intervention for preventing HIV when taken consistently, particularly for individuals at high risk (11). While globally PrEP uptake varies, with high levels of acceptability among men who have sex with men in the U.S. and Europe (12), Sub-Saharan Africa, including Kenya, has seen limited PrEP uptake among youths aged 15-24. Despite free access to PrEP in Kenya, uptake remains lower than expected, particularly in Turbo Sub County, Uasin Gishu, where uptake is only 26.7% (13). In comparison, Kapsaret has a slightly better PrEP uptake at 35.9% (13). Various factors contribute to this low uptake, including limited awareness, stigma, and socio-economic barriers (12). However, there is a lack of context-specific research in Turbo Sub County, which this study seeks to address. By identifying the determinants of PrEP uptake among youths aged 15–24 and validating model proposed to explain the interaction of these factors, the study aims to inform strategies to reduce HIV incidence and enhance PrEP usage within this vulnerable population.
1.2 Justification
PrEP is available for free in public hospitals to individuals at high risk of contracting HIV (14). However, the uptake among youths remains low with a typical example being Turbo Sub County at 26.9%, compared to higher rates in other areas like Kapsaret, where uptake stands at 35.9% (13). Despite its proven effectiveness, this disparity highlights the need for a deeper understanding of the factors influencing PrEP uptake. This research aims to inform the design and implementation of targeted interventions to increase PrEP utilization and reduce HIV incidence among youths in Turbo. The study’s findings will provide policymakers and healthcare providers with evidence-based insights necessary to develop effective interventions, such as educational campaigns, community engagement, and healthcare improvements tailored to youths’ needs in Turbo Sub County (15). Addressing these determinants will empower young people with knowledge and tools for HIV prevention, fostering a more informed generation. Additionally, this research will contribute to the broader body of knowledge, offering data and insights for future studies.
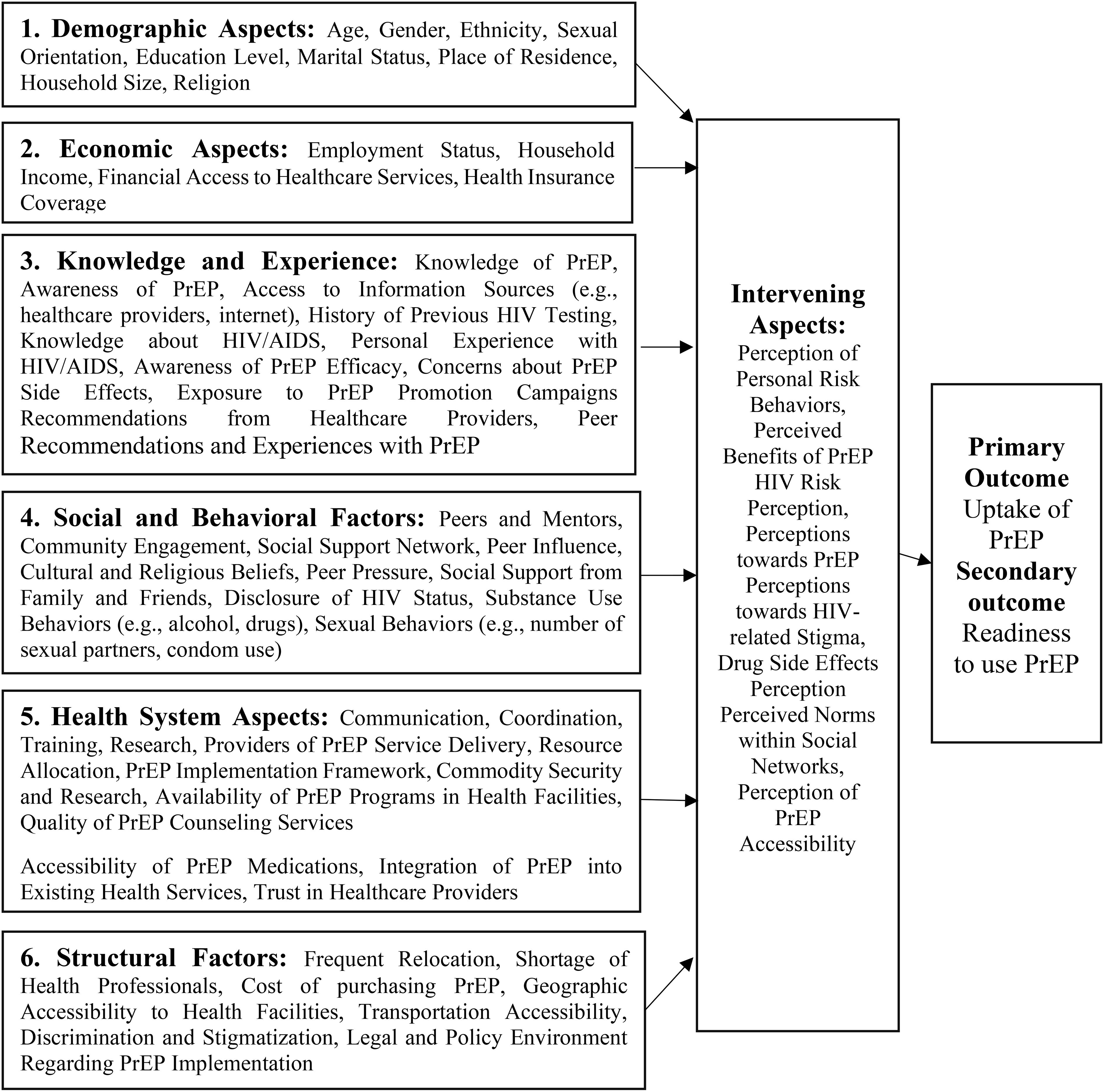
1.3 Model for predicting HIV pre-exposure prophylaxis uptake
The proposed model for predicting the uptake of HIV Pre-Exposure Prophylaxis (PrEP) is structured around independent factors, intervening factors, and the resulting outcomes, with its constructs rooted in empirical evidence from previous research. This model integrates key insights from existing literature, focusing on various demographic, economic, knowledge-based, social, behavioral, and health system-related factors has the independent predictors, and perception factors as the intervening variables in predicting intent to use PrEP.
1.3.1 Independent factors
Demographic factors such as age, gender, race/ethnicity, sexual orientation, education level, and marital status significantly influence HIV PrEP uptake. Younger individuals often have lower awareness and risk perception, leading to reduced uptake, while older individuals may be more motivated to use PrEP due to perceived higher risk (16, 17). Gender norms and cultural beliefs can create barriers, particularly for women and LGBTQ+ populations, who may face stigma and discrimination that deter them from seeking PrEP (7, 18, 19). Racial and ethnic minorities also experience disparities in healthcare access and quality, contributing to lower PrEP uptake (20, 21). Additionally, educational attainment and health literacy play critical roles in understanding and accessing PrEP, with higher education levels associated with greater uptake (16). Marital and relationship status further influences PrEP decisions, with those in non-monogamous or high-risk relationships more likely to seek PrEP, particularly when supported by partners and family (22, 23).
Economic factors such as income, employment, insurance coverage, and overall economic conditions play a crucial role in determining HIV PrEP uptake. Lower income and financial instability often prevent individuals from affording PrEP and related healthcare services, creating significant barriers to access (17, 24). Employment status also influences access, with stable jobs often providing health insurance that covers PrEP, while those in precarious employment face greater challenges (25). Insurance coverage is critical, as inadequate or absent coverage can lead to high out-of-pocket costs that deter individuals from seeking PrEP (21). Additionally, broader economic conditions, including national economic stability and government health spending, affect the availability and affordability of PrEP services, with economically unstable regions often facing reduced access (26).
A person’s knowledge and experience with HIV/AIDS and PrEP are pivotal in shaping their attitudes toward PrEP usage. Awareness of PrEP, personal experience with HIV, concerns about side effects, and recommendations from peers and healthcare providers all influence an individual’s decision to use PrEP. Effective education and awareness programs have been shown to drive PrEP uptake by addressing concerns and building trust in its efficacy (18). Furthermore, studies emphasize the importance of educating healthcare providers to ensure they are well-prepared to guide patients in PrEP-related decisions (27).
Peer support and positive social influences play a vital role in HIV Pre-Exposure Prophylaxis (PrEP) uptake by encouraging individuals to consider and use PrEP through shared experiences, information exchange, and the reduction of stigma. Peers who advocate for PrEP can significantly increase an individual’s confidence in its use, making it easier to navigate healthcare systems and manage any concerns (22, 23). Social networks also shape norms and behaviors, where acceptance of PrEP within a group can lead to higher uptake, particularly when PrEP is seen as a normal and positive health choice (7). Additionally, community engagement and collective action amplify these effects by creating broader supportive environments, further enhancing PrEP adoption (28). Leveraging these social dynamics is crucial for effective public health interventions aimed at increasing PrEP use, especially among young and high-risk populations.
Health system factors significantly influence HIV Pre-Exposure Prophylaxis (PrEP) uptake by shaping the accessibility, quality, and sustainability of services. Key aspects include the integration of PrEP into existing health services, the competence and attitudes of healthcare providers, and the coordination and resource allocation within health systems. Integrating PrEP into routine health services and ensuring geographic coverage are crucial for making PrEP accessible, particularly in underserved areas (23, 29). The training and attitudes of healthcare providers are vital for patient education and adherence, with supportive, well-informed providers playing a key role in encouraging PrEP use (30). Effective coordination between health programs and adequate resource allocation, including ensuring a steady supply of PrEP, are essential for maintaining service quality and access (26). Moreover, patient-centered care, which tailors services to individual needs, enhances the acceptability of PrEP and supports adherence, while flexible service delivery models help reach diverse populations (31). Robust health information systems that monitor and track PrEP uptake and outcomes are critical for identifying gaps and improving service delivery (32).
Structural factors play a crucial role in determining HIV Pre-Exposure Prophylaxis (PrEP) uptake by shaping the environment in which individuals make health decisions. Key structural aspects include healthcare infrastructure, policy and legal frameworks, geographic accessibility, socioeconomic inequalities, and cultural norms. The availability and quality of healthcare services, as well as the integration of PrEP into existing health programs, directly impact access and adherence (23, 26, 33). Supportive policies, regulatory approval, and adequate funding are essential for ensuring widespread access to PrEP, while legal protections can reduce stigma and discrimination against marginalized groups (7, 21). Geographic accessibility, including the proximity of healthcare facilities and reliable transportation, significantly influences PrEP uptake, particularly in rural or underserved areas (29). Socioeconomic factors such as financial constraints, employment, and education levels also affect individuals’ ability to access and afford PrEP services (17, 24). Housing stability and mobility further influence continuity of care, with housing insecurity and frequent relocation posing significant barriers to consistent PrEP use (22, 25). Cultural norms and societal attitudes, including gender roles and HIV-related stigma, can either facilitate or hinder PrEP adoption. Negative cultural beliefs and discrimination discourage individuals from seeking PrEP, while supportive community engagement and social networks can promote its uptake (18, 31). Effective public health messaging and information dissemination are critical for raising awareness and addressing misconceptions about PrEP (15).
1.3.2 Intervening factors
Intervening factors play a pivotal role in the proposed model by mediating the relationship between the independent factors (such as demographic, economic, knowledge, social, behavioral, and health system aspects) and the ultimate outcomes of PrEP uptake and readiness to use PrEP. These intervening factors primarily involve various perceptions that significantly influence an individual’s decision-making process regarding PrEP. One of the most critical intervening factors is an individual’s perception of their own risk behaviors related to HIV. The perceived risk of contracting HIV directly influences whether a person considers PrEP as a necessary preventive measure. Studies have shown that individuals who perceive themselves to be at high risk of HIV infection are more likely to seek out and use PrEP (30). This perception is often shaped by several factors, including sexual behavior, history of sexually transmitted infections (STIs), and knowledge of HIV transmission routes. For instance, people who engage in high-risk behaviors such as unprotected sex with multiple partners or those who have a partner with unknown or positive HIV status are more likely to perceive themselves as being at higher risk and, therefore, more likely to consider PrEP (12, 34).
The perceived benefits of PrEP, particularly its efficacy in preventing HIV, are another crucial intervening factor. Individuals who believe that PrEP offers significant protection against HIV are more inclined to use it. This perception is influenced by awareness campaigns, healthcare provider recommendations, and personal or community experiences with PrEP. Research indicates that individuals who are well-informed about PrEP’s benefits and efficacy are more likely to adopt it as part of their HIV prevention strategy (Bor et al., 2021). However, this perception can be undermined by misinformation or lack of trust in the healthcare system, which can lead to lower uptake rates.
Closely related to personal risk behaviors is the broader perception of HIV risk within an individual’s environment. This includes the perceived prevalence of HIV within one’s community, social network, or peer group. If a person perceives that HIV is a significant threat in their surroundings, they are more likely to adopt preventive measures, including PrEP (16). Conversely, individuals who perceive a low risk of HIV in their community may not see the need for PrEP, even if they themselves are at risk. This broader risk perception is influenced by community norms, media representations of HIV, and public health messaging.
General attitudes toward PrEP, including beliefs about its safety, side effects, and the ease of adherence, significantly affect its uptake. Negative perceptions, such as fears about potential side effects (e.g., nausea, dizziness) or the inconvenience of daily medication, can deter individuals from starting or continuing PrEP (23). Additionally, misconceptions about PrEP, such as the belief that it might encourage risky sexual behavior or that it is only for certain groups (e.g., men who have sex with men), can limit its acceptance among broader populations. Overcoming these negative perceptions through education and counseling is essential for increasing PrEP uptake (19).
Stigma is a powerful intervening factor that can significantly reduce the likelihood of PrEP uptake. HIV-related stigma, including the association of HIV with immoral behavior or the belief that those who use PrEP must be HIV-positive or at high risk due to risky behaviors, can discourage individuals from seeking PrEP (28, 31). In many communities, the fear of being labeled or judged for using PrEP can outweigh the perceived benefits, leading to low uptake. Addressing stigma through community engagement, education, and normalization of PrEP as a preventive health measure is crucial for improving its adoption.
The perception of how accessible PrEP is—whether in terms of availability at local clinics, affordability, or the ease of obtaining a prescription—also mediates PrEP uptake. Individuals who perceive PrEP as easily accessible are more likely to use it. On the other hand, if PrEP is perceived as difficult to obtain due to cost, lack of nearby clinics, or bureaucratic barriers within the healthcare system, individuals may be less likely to pursue it as an option (12, 26). Improving the actual and perceived accessibility of PrEP through policy changes, subsidized programs, and decentralized distribution channels can significantly increase its uptake.
The perceived norms within an individual’s social network or community can also influence PrEP uptake. If PrEP use is seen as acceptable and supported within a person’s peer group or community, they are more likely to consider and use it. Conversely, if there is a strong social norm against PrEP, due to stigma or misinformation, individuals may avoid it even if they recognize its benefits. Social networks play a critical role in either facilitating or hindering health behaviors, and leveraging positive social influences can be an effective strategy for increasing PrEP uptake (7).
Fear of side effects can deter individuals from starting PrEP or lead to discontinuation if side effects are experienced. Addressing these concerns through proper counseling and providing information about managing side effects is essential to maintaining adherence to PrEP (29). Clear communication about the nature and prevalence of side effects, as well as reassurance that they can often be managed, is vital for encouraging continued use.
Cultural and religious beliefs can significantly influence perceptions and attitudes toward PrEP. In some communities, cultural norms or religious teachings may conflict with the use of PrEP, either by promoting abstinence-only approaches or by associating PrEP with promiscuity. These beliefs can serve as powerful intervening factors that discourage PrEP use. Engaging with community leaders and tailoring public health messages to align with cultural and religious values can help mitigate these barriers and promote PrEP uptake in diverse settings (25). Understanding and addressing these intervening factors is essential for the successful implementation and scale-up of PrEP programs, particularly in high-risk populations where these perceptions can significantly influence health behaviors.
The integrated approach forestalled by the proposed model tries to predict the complex interplay between demographic, economic, knowledge, social, behavioral, and health system factors that influence PrEP uptake as shown in Figure 1. It emphasizes the importance of addressing individual perceptions, such as risk behaviors and stigma, as critical mediators between these factors and the ultimate outcome of PrEP adoption. To validate this framework, the current research explores how each of these factors impacts the uptake of PrEP thus providing a basis for designing interventions aimed at enhancing PrEP coverage, especially among vulnerable populations. The model aims to validate factors that lead to two primary outcomes: increased uptake of PrEP and readiness to use PrEP. The successful validation of this model will provide a comprehensive understanding of the factors influencing PrEP uptake, thus guiding the design of targeted interventions to enhance PrEP coverage, especially among vulnerable populations, like the youth in Turbo Sub-County.
2 Methodology
2.1 Study area
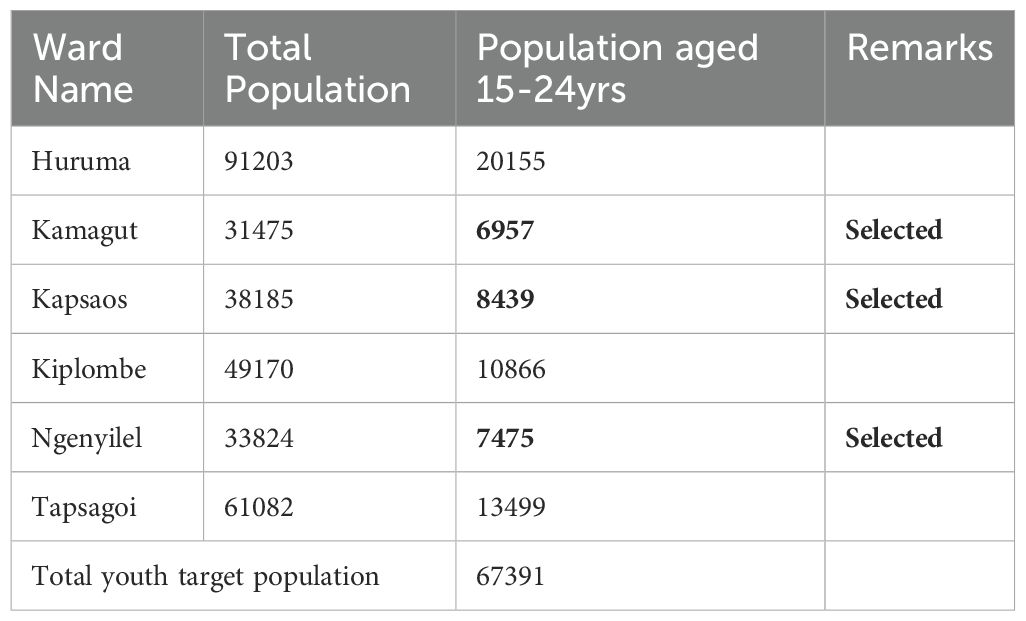
Turbo Subcounty has twenty-one health facilities out of which 8 are offering PrEP services. The total number of clients undergoing PrEP services as of September 2023 was 193, with females being the majority (115) than males (78). Turbo is located approximately 34 kilometers northwest of Eldoret town, the capital of the county. Its main town is situated along the Nairobi-Malaba Road. As per the Kenya National Bureau of Statistics (KNBS), the town has a total population of 302,629, and 67,391 of its residents belong to the youth age group of 15–24 years. The predominant ethnic group in Turbo is the Kalenjin tribe, although there is also a presence of Tachoni, Luhya, Kikuyu, and Somali communities (35). The study will be conducted in the households within the randomly sampled wards in the Sub County.
2.2 Study design
This will be a cross-sectional study where both quantitative and qualitative methods will be applied. The concurrent mixed methods design will help develop a better understanding of the circumstances that prompt youth (15–24 years old) in Turbo Sub County, Uasin Gishu County, to take up HIV-PrEP. Triangulating the results from quantitative and qualitative approaches might offer greater insight into factors that affect the adoption and use of PrEP. This design allows for the simultaneous collection and analysis of both quantitative and qualitative data.
2.3 Study population
This study will be carried out among youths aged 15–24 years residing in Turbo Sub County who are approximately 67,391 as per the National census report of 2019.
2.4 Inclusion and exclusion criteria
Participants will be eligible if they are between the ages of fifteen and twenty-four years, have resided in Turbo Sub County, Uasin Gishu County, Kenya, for more than three months immediately preceding data collection, and provide voluntary and informed consent to participate in the research. To confirm that participants have resided in Turbo Sub-County for more than three months, the research team will include screening questions in the questionnaire. For example: “How long have you lived in Turbo Sub-County?” “Have you changed residence in the past 3 months?” Participants who indicate residency for less than 3 months will be excluded. Additionally, for further verification (especially in cases of doubt), participants may be asked to provide a supporting document, such as a clinic attendance card, school ID with a local address, or any document showing residence. Community Health Promoters (CHPs) will assist in verifying residency through their knowledge of local households. Additionally, for participants aged 15–18 years, parental or caregiver assent must be obtained. Further, we also recognize the sensitivity and ethical implications of including vulnerable adolescents like those without guardians, in informal care, or experiencing housing instability and homeless youth. To uphold ethical standards, the following steps will be taken: Those adolescents without identifiable guardians, the study team will work with the local Children’s Officer and Community Health Volunteers to determine legal and ethical eligibility for participation, in line with the Kenyan guidelines on research with minors. Vulnerable adolescents (e.g., street-connected youth or those in child-headed households) will be approached only with approval from the County Children’s Department and will be provided with counseling and support prior to and during participation. Safeguards and referrals for those in vulnerable circumstances, will be provided with confidential referral mechanisms for counseling, social support, or health services when necessary. The research team will also include a trained counselor or social worker to support youth participants during data collection. The study will exclude individuals who are not eligible for PrEP based on existing medical criteria, such as those who are HIV positive, as this is a contraindication to PrEP.
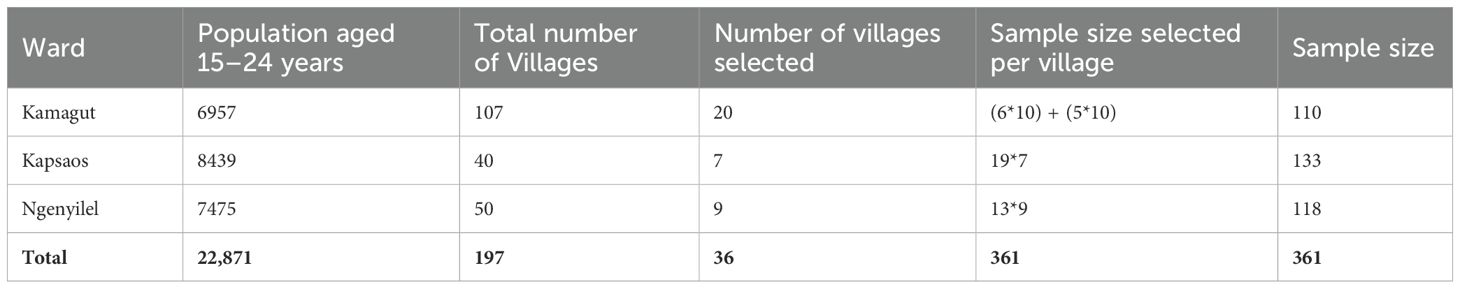
2.5 Sample size determination
Fisher’s formula for calculating sample size in a survey will be used. Fisher’s formula: n=[Z2 *p*(1-p)/E2. Where n is the required sample size, Z is the Z-score (the critical value for the desired confidence level 95% CI is 1.96), p is the estimated prevalence or proportion of the study population who uses Prep in Turbo sub-County, estimated at 26.7% according to Kenya Health Information System (36), E as the margin of error set at 5% (0.05). Therefore, n=1.962x0.267x (1-0.267)]/0.052. n= (3.8416*0.267*0.733)/0.0025 = 300.74 = 301 With an addition of sampling error and non-response of 10% each (37), the sample size will be 1.2*301 = 361.
2.6 Sampling technique
The sampling technique will be a multistage sampling method. Three out of the six wards in Turbo Sub-County were sampled using a simple random sampling technique. This was achieved using the Generated OpenEPI Random Program, where the six wards within the Sub- County were assigned numbers, three numbers were randomly drawn, and the wards listed against the selected numbers were included in the study. Table 1 shows the three wards selected for the study.
The next step is to determine the number of villages for each ward and select the villages to be included in the study. The number of villages for each ward will be allocated proportionately to the sample size and the population of youths aged 15-24. A total of 36 villages have been generated (Table 2). The names of the villages for each ward will then be selected using computer-generated random numbers.
The final step involves selecting households with potential participants (youths aged 15–24 years) to visit, which will also be done using simple random sampling technique. Names of all households with eligible potential participants (youths aged 15–24 years) will be generated per village through the help of Community Health Promoters (CHPs) and assigned different numbers from the first to the last. The lottery method will then be applied using computer excel software to generate numbers (household) which will take part in the study. If a selected household decline to participate, the nearest neighboring household with an eligible potential participant will be chosen as a replacement. If there is more than one eligible participant in a household, one youth will be randomly selected for the study.
2.7 Development of instruments
The data collection tools will be designed to collect quantitative and qualitative data, aligning with the variables outlined in the proposed model for predicting HIV pre-exposure prophylaxis (PrEP) uptake. The data collection tools for this study should systematically capture information related to the identified independent and dependent variables. These encompass demographic factors, including gender, age, level of education, marital status, socioeconomic standing, and religion. The tools should also capture structural and health facility factors, including transportation logistics, appointment timing, availability time off from work or schooling, the presumed charges of PrEP, adherence aid, the ease of PrEP, and access to a PrEP provider. Structured questionnaires will incorporate Likert scales or categorical response options for quantitative assessment, while qualitative exploration through interviews will delve into individual experiences and perceptions. PrEP uptake will be quantitatively assessed through structured questionnaires that include questions use or non-use and reasons for either. Qualitative data gathered from interviews will complement these quantitative findings, providing deeper insights into the motivations behind PrEP uptake or barriers preventing its adoption. Throughout the development process of these data collection tools, literature review, including insights other relevant sources, will guide the selection and framing of questions for each variable. Expert consultation with professionals in HIV prevention, public health, and social sciences will ensure the relevance and appropriateness of the questions, enriching the tools with expert insights. Ethical considerations will be paramount, ensuring that questions are sensitive and respectful, particularly when addressing potentially stigmatized or personal topics, thereby promoting participant well-being and fostering an environment conducive to candid and accurate responses.
2.8 Validity
The first draft of the questionnaire will undergo pilot testing to identify ambiguities, inconsistencies, or potential comprehension challenges, with feedback from a small sample guiding refinement. The pilot study will be carried out in the neighboring Soy Sub County. During this stage, parameters for measuring different constructs will be assessed for validity using Cronbach’s alpha with >0.70 being acceptable. The finalized tools will undergo a validation process to ensure they effectively measure the intended constructs, providing reliable and valid data for subsequent analysis. Construct and content validity will be assured by using Muhumuza et al. (2021) validated conceptual framework to develop the questionnaire.
2.9 Reliability
The consistency of actual application of the tools and methods of this research will be ensured by the researcher using thoroughly trained data collectors. This will strengthen interrater reliability by reducing bias introduced by the data collectors. Cronbach’s alpha of 0.7 was considered appropriate for the Likert scale questions, and internal consistency will be established by piloting the tools and improving them to make sure they capture the essence of what they were intended to collect.
2.10 Data collection procedure
A mix of quantitative and qualitative data collection techniques will be used in this study to thoroughly look into the factors that affect PrEP (HIV Pre-Exposure Prophylaxis) adoption. Being that the study employs dual methods, the qualitative data collection methods will be applied first so that the questionnaire can be enriched by the questions being asked. For qualitative data, key informant interviews will be contacted to explore the factors influencing PrEP utilization. Eight (8-12) key informants will be identified based on their relevance to the research objectives, their potential to provide diverse perspectives, and their involvement in the community or professional field related to HIV prevention and PrEP, their willingness to participate and that their insights contribute meaningfully to the research goals. The six Key Informant Interviews (KIIs) will be purposively drawn from Clinical Team and managers (County Pharmacist/Nurse/Clinical Officer), a representative from Non-Governmental Organization (NGO), a peer educator, religious leaders (from church mosque, others), parent and a community health promoter. Two focus group discussions will be done per ward, for the three wards so as to get detailed opinion and perceptions of the youths regarding their uptake of HIV PrEP. The youths taking part in the FGD will be mobilized through their respective youth champions per each ward. Each FGD session will involve 8–10 participants (youths aged 15-24), with the researcher taking the active role of a moderator. FGD guide will be employed, allowing for probing questions for deeper understanding of individual experiences and opinions. This will be recorded and transcribed for analysis, facilitating the identification of shared perspectives and diverse opinions within the sampled population. Structured questionnaires will then be administered as a primary tool for quantitative data collection after it has been enriched by the outcome of the qualitative methods.
2.11 Data management
The data will be password protected: only authorized users were allowed access to the data. In addition, the collected information will be stored safely; hardcopies will be stored in lockable cabinets and soft copies secured by password. Data transmission will be encrypted to ensure data integrity and confidentiality of participants. The quantitative data will be exported from Kobo Collect into MS Excel, data cleaning will be done in Excel and the imported into Stata for data analysis.
2.12 Variables in the study
Independent variables in the study are divided into the following categories; participants’ demographic characteristics, social and behavioral factors, health facility factors, and clinical factors. The dependent variable in this study will be PrEP uptake. The participant demographic variables include; age, gender, education level, marital status, and religion. This aspect will be measured by questions 1–9 in the sociodemographic section of the questionnaire. Economic status of the participants is measured by questions 1–4 under the economic status section of the questionnaire. Knowledge and experience is measured by parameters under the knowledge and experience section of the questionnaire with questions ranging from 1-11. Particularly, knowledge of PrEP and HIV/AIDS as constructs will be measured by question 1 and 5, respectively, under the knowledge and experience section of the questionnaire which are 4 point parameters that are ordinal variables. Experience will be measured by questions 4, and 6 in particular. Health system factors will be assessed in section 4. The study explores social and behavioral factors, including HIV-related stigma, relationship dynamics, sexual risk behaviors, cultural influence, and peer support that are assessed by questions in section 5 of the questionnaire with social support aspects measured by questions 1–7 and behavioral aspects measured by questions 8-10. The structural factors will be assessed by parameters in section 6 of the questionnaire using questions 1–7 to include transportation logistics, appointment timing, availability of time off from work or school, perceived costs of PrEP, and adherence counseling.
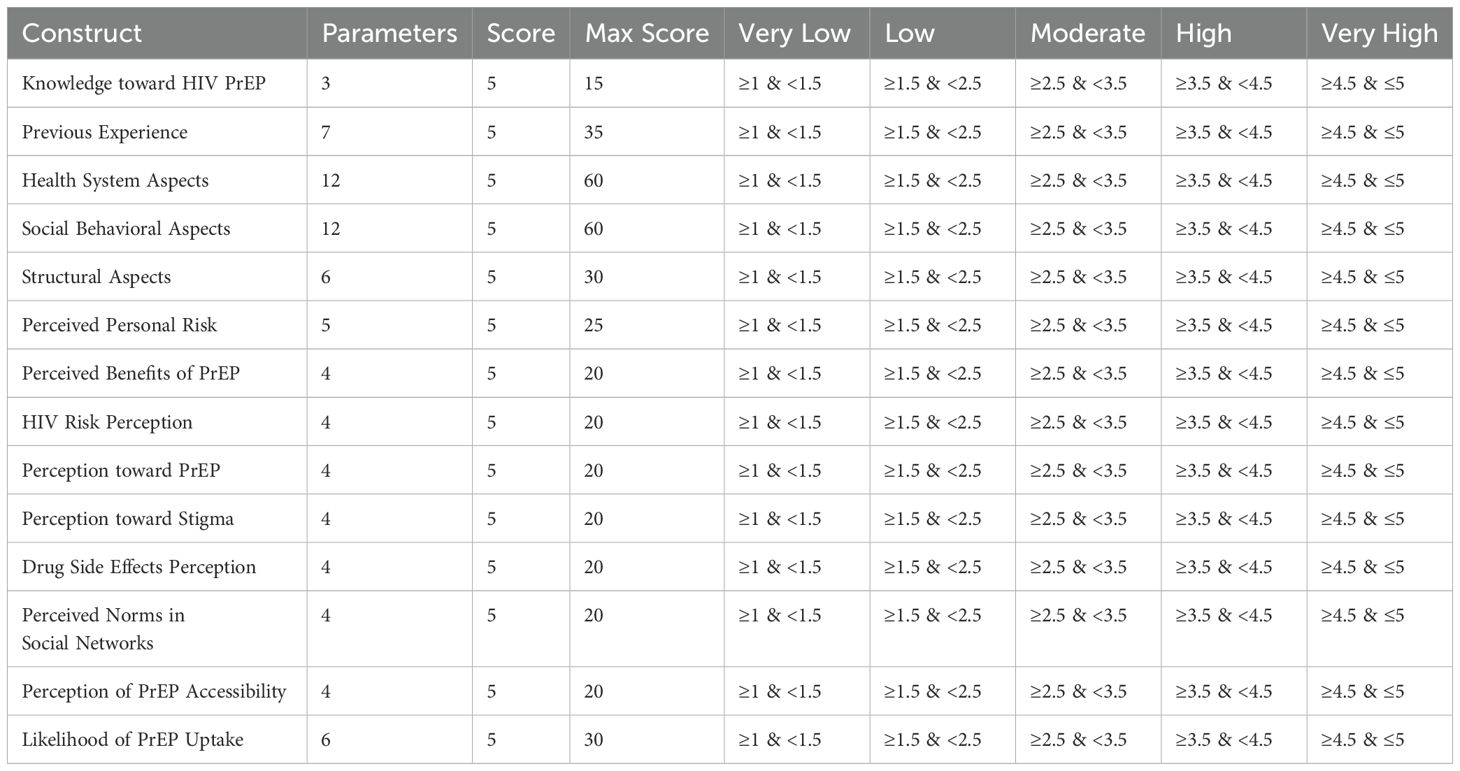
Knowledge toward HIV PrEP will be assessed using 3 parameters, each a 5-point Likert scale. Therefore, the knowledge toward HIV PrEP will be converted to a continuous variable by adding all the scores for the three parameters, with the maximum score being 15. This will be subsequently converted to an interval scale by dividing the total by 3 parameters. The Knowledge toward HIV PrEP will be rated as: very low: ≥1<1.5, low: ≥1.5<2.5, moderate: ≥2.5<3.5, high: ≥3.5<4.5, very high: ≥4.5 ≤ 5.
Previous experience will be assessed using seven parameters, each a 5-point Likert scale. Therefore, the previous experience will be converted to a continuous variable by adding all the scores for the seven parameters, with the maximum score being 35. This will be subsequently converted to an interval scale by dividing the total by 7 parameters. The rating of previous experience will be categorized as follows: very low: ≥1<1.5, low: ≥1.5<2.5, moderate: ≥2.5<3.5, high: ≥3.5<4.5, very high: ≥4.5 ≤ 5.
Health system aspects will be assessed using twelve parameters, each a 5-point Likert scale. Therefore, the health system aspects will be converted to a continuous variable by adding all the scores for the twelve parameters, with the maximum score being 60. This will be subsequently converted to an interval scale by dividing the total by 12 parameters. The rating of health system aspects will be categorized as follows: very low: ≥1<1.5, low: ≥1.5<2.5, moderate: ≥2.5<3.5, high: ≥3.5<4.5, very high: ≥4.5 ≤ 5.
Social behavioral aspects will be assessed using twelve parameters, each a 5-point Likert scale. Therefore, the social behavioral aspects will be converted to a continuous variable by adding all the scores for the twelve parameters, with the maximum score being 60. This will be subsequently converted to an interval scale by dividing the total by 12 parameters. The rating of social behavioral aspects will be categorized as follows: very low: ≥1<1.5, low: ≥1.5<2.5, moderate: ≥2.5<3.5, high: ≥3.5<4.5, very high: ≥4.5 ≤ 5.
Structural aspects will be assessed using six parameters, each a 5-point Likert scale. Therefore, the structural aspects will be converted to a continuous variable by adding all the scores for the six parameters, with the maximum score being 30. This will be subsequently converted to an interval scale by dividing the total by 6 parameters. The rating of structural aspects will be categorized as follows: very low: ≥1<1.5, low: ≥1.5<2.5, moderate: ≥2.5<3.5, high: ≥3.5<4.5, very high: ≥4.5 ≤ 5.
Perceptions variables will be classified into 8 aspects; perceived personal risk to risky behavior, perceived benefits of PrEP, HIV risk perception, perception toward PrEP, perception toward HIV related stigma, drug side effects perception, perceived norms related to PrEP within social networks, and perception of PrEP accessibility. Perception of personal risk behaviors will be assessed using three parameters each a 5-point Likert scale. Therefore, perception of personal risk will be converted to continuous variable by adding all the scores for the five parameters with the maximum score being 20. This will be subsequently converted to an interval Scale by dividing the total by 5 parameters thus perception of personal risk behaviors will be rated as Very Low if it is ≥1<1.5, Low: ≥1.5<2.5, Moderate: ≥2.5<3.5, High: ≥3.5<4.5 and Very High: ≥4.5 ≤ 5. Perceived benefits of PrEP will be assessed using four parameters, each a 5-point Likert scale. Therefore, the perception of benefits will be converted to a continuous variable by adding all the scores for the four parameters, with the maximum score being 20. This will be subsequently converted to an interval scale by dividing the total by 4 parameters. The perception of benefits will be rated as: Very Low: ≥1<1.5; Low: ≥1.5<2.5; Moderate: ≥2.5<3.5; High: ≥3.5<4.5; and Very High: ≥4.5 ≤ 5. HIV risk perception will be assessed using four parameters, each a 5-point Likert scale. Therefore, the perception of risk will be converted to a continuous variable by adding all the scores for the four parameters, with the maximum score being 20. This will be subsequently converted to an interval scale by dividing the total by 4 parameters. The perception of risk will be rated as: Very Low: ≥1<1.5; Low: ≥1.5<2.5; Moderate: ≥2.5<3.5; High: ≥3.5<4.5; and Very High: ≥4.5 ≤ 5. Perceptions toward PrEP will be assessed using four parameters, each a 5-point Likert scale. Therefore, the perception toward PrEP will be converted to a continuous variable by adding all the scores for the four parameters, with the maximum score being 20. This will be subsequently converted to an interval scale by dividing the total by 4 parameters. The perception toward PrEP will be rated as: Very Low: ≥1<1.5; Low: ≥1.5<2.5; Moderate: ≥2.5<3.5; High: ≥3.5<4.5; and Very High: ≥4.5 ≤ 5. Perceptions toward HIV-related stigma will be assessed using four parameters, each a 5-point Likert scale. Therefore, the perception toward stigma will be converted to a continuous variable by adding all the scores for the four parameters, with the maximum score being 20. This will be subsequently converted to an interval scale by dividing the total by 4 parameters. The perception toward stigma will be rated as: Very Low: ≥1<1.5; Low: ≥1.5<2.5; Moderate: ≥2.5<3.5; High: ≥3.5<4.5; and Very High: ≥4.5 ≤ 5. Drug side effects perception will be assessed using four parameters, each a 5-point Likert scale. Therefore, the perception of side effects will be converted to a continuous variable by adding all the scores for the four parameters, with the maximum score being 20. This will be subsequently converted to an interval scale by dividing the total by 4 parameters. The perception of side effects will be rated as: Very Low: ≥1<1.5; Low: ≥1.5<2.5; Moderate: ≥2.5<3.5; High: ≥3.5<4.5; and Very High: ≥4.5 ≤ 5. Perceived norms within social networks will be assessed using four parameters, each a 5-point Likert scale. Therefore, the perception of social norms will be converted to a continuous variable by adding all the scores for the four parameters, with the maximum score being 20. This will be subsequently converted to an interval scale by dividing the total by 4 parameters. The perception of social norms will be rated as: Very Low: ≥1<1.5; Low: ≥1.5<2.5; Moderate: ≥2.5<3.5; High: ≥3.5<4.5; and Very High: ≥4.5 ≤ 5. Perception of PrEP accessibility will be assessed using four parameters, each a 5-point Likert scale. Therefore, the perception of accessibility will be converted to a continuous variable by adding all the scores for the four parameters, with the maximum score being 20. This will be subsequently converted to an interval scale by dividing the total by 4 parameters. The perception of accessibility will be rated as: Very Low: ≥1<1.5; Low: ≥1.5<2.5; Moderate: ≥2.5<3.5; High: ≥3.5<4.5; and Very High: ≥4.5 ≤ 5.
As for the outcome variable, uptake of PrEP, actual use of PrEP will be assessed, such that the former will be assessed by 1 question seeking to know whether the youth has used PrEP. Secondly, being an intervention that is rarely utilized, uptake was assessed by likelihood to use PrEP measured by six parameters aligned with the constructs of the Health Belief Model will be used to measure it. The first parameter seeks to understand the client’s likelihood of using PrEP in the future. This assesses the intention to use PrEP and embodies cues to action and perceived benefits. The second parameter, Adherence Readiness, evaluates self-efficacy by asking how willing the individual is to take PrEP daily as prescribed, focusing on their confidence in maintaining a treatment regimen. The third, Healthcare Communication, relates to cues to action, measuring the likelihood of discussing PrEP with a healthcare provider, which reflects proactive health-seeking behavior. The fourth parameter, Provider Influence, assesses both cues to action and perceived benefits, querying comfort with starting PrEP if recommended by a healthcare provider, thus gauging trust in professional advice and the perceived effectiveness of PrEP. The fifth, Continuation in the Face of Adversity, examines perceived barriers and self-efficacy by determining the likelihood of continuing PrEP amidst minor side effects, addressing the resilience to maintain usage under potential challenges. Lastly, the sixth parameter, Accessibility and Readiness, combines self-efficacy and perceived barriers, asking about readiness to use PrEP if available, focusing on both the accessibility of the treatment and the individual’s preparedness to begin and sustain its use. Therefore, 6 parameters, each of a 5-point Likert scale are used to assess likelihood of PrEP uptake. Where uptake of PrEP will be converted to continuous variable by adding all the scores for the six parameters, with the maximum score being 30. This will be subsequently converted to an interval scale by dividing the total by the six parameters. Likelihood of Uptake of PrEP will be rated as: Very Low: ≥1<1.5; Low: ≥1.5<2.5; Moderate: ≥2.5<3.5; High: ≥3.5<4.5; and Very High: ≥4.5 ≤ 5. The conversion of parameter measures into construct variables is as shown in the Table 3.
2.13 Analysis
The analysis will focus on validating the proposed model for HIV Pre-Exposure Prophylaxis (PrEP) uptake using Structural Equation Modeling (SEM) by IBM SPSS AMOS Version 21. This approach will allow for the simultaneous examination of multiple relationships between observed and latent variables based on the constructs outlined in the proposed model. The constructs include demographic factors, economic factors, knowledge and experience, social and behavioral factors, health system factors, structural factors, and intervening perception-related factors.
2.13.1 Data preparation and summary of participants’ characteristics
The analysis will begin with data cleaning and preparation, including addressing missing values, outliers, and inconsistencies. During data preparation, all variables will be assessed for the presence and extent of missing data. We will apply a multi-step strategy for handling missing values. Descriptive Analysis will ascertain frequency and pattern of missing data. Variables with more than 10% missing data will be critically reviewed. Statistical tests such as Little’s Missing Completely at Random (MCAR) test will be done to determine whether the data are missing completely at random. Quantitative variables with missing values less than 5%, mean or median imputation will be used depending on the variable’s distribution. Categorical variables, mode imputation will be used if the missing values are minimal. If missing data exceeds 10% and is not MCAR, Multiple Imputation (MI) techniques will be applied to minimize bias, especially in key variables involved in SEM analysis. Sensitivity analyses will be done where appropriate, to assess the impact of imputation on the results. Categorical variables will be numerically coded, and a master dataset incorporating all relevant variables will be created. Descriptive statistics will summarize participants’ characteristics, with continuous variables like age described using measures of central tendency (mean, median) and dispersion (standard deviation). Categorical variables, such as gender, education level, and marital status, will be summarized into proportions and displayed in frequency tables.
2.13.2 Bivariate analysis for preliminary insights
Before SEM, bivariate analyses will be conducted to explore the relationships between individual variables. Chi-square tests for categorical variables and appropriate correlation coefficients for continuous variables will be utilized to assess the associations between demographic, economic, knowledge, social, behavioral, health system, and structural variables and PrEP utilization.
2.13.3 Exploratory and confirmatory factor analysis
Before applying SEM, exploratory factor analysis (EFA) will be conducted to identify the underlying structure of the constructs and to confirm that the observed variables load onto the expected latent constructs. Confirmatory factor analysis (CFA) will then be used to test the measurement model and confirm the factor structure, ensuring that the constructs are valid and reliable. The internal consistency of the scales will be assessed using Cronbach’s alpha, with a threshold of ≥0.7 considered acceptable. Parameters with low factor loadings will be removed or appropriate correlation of error terms will be applied on the most affected parameters to optimize the model following known theoretical and empirical recommendation. As such, Exploratory Factor Analysis (EFA) will be conducted to identify the underlying structure of latent constructs and examine how observed variables cluster. Principal Component Analysis (PCA) with varimax rotation will be used, and the suitability of data for factor analysis will be assessed using the Kaiser-Meyer-Olkin (KMO) measure, with a threshold of ≥ 0.6, and Bartlett’s Test of Sphericity, which should yield a significant result (p < 0.05). Factors will be extracted based on eigenvalues ≥ 1.0, and items with factor loadings of ≥ 0.40 will be retained. Items loading below this threshold will be considered for removal or revision unless there is strong theoretical justification for their inclusion. Cross-loading items will be assessed for both statistical significance and conceptual coherence.
Confirmatory Factor Analysis (CFA) will then be used to validate the factor structure identified in EFA, ensuring that observed variables appropriately reflect their intended latent constructs. CFA will be conducted using I|BM SPSS AMOS. Model fit will be evaluated using established indices, including the Chi-square statistic, Comparative Fit Index (CFI > 0.90), Tucker-Lewis Index (TLI > 0.90), Root Mean Square Error of Approximation (RMSEA < 0.08), and Standardized Root Mean Square Residual (SRMR < 0.08). Items with standardized factor loadings below 0.40 will be reviewed for exclusion, unless retained for strong theoretical reasons. Any modifications to the model—such as the removal of items or correlating error terms—will be guided by empirical evidence (e.g., modification indices) and theoretical justification to maintain the integrity and interpretability of the constructs.
2.13.4 Structural equation modeling for model validation
2.13.4.1 Model specification:
The SEM will be specified based on the proposed conceptual framework, where latent variables (constructs) include demographic factors, economic factors, knowledge and experience, social and behavioral factors, health system factors, structural factors, and intervening perception-related factors. Each latent variable will be measured by multiple observed indicators derived from the data.
2.13.4.2 Model estimation:
Structural Equation Modeling (SEM) will be used to estimate the direct, indirect, and total effects of latent and observed variables on the outcome of PrEP uptake. These effects will be interpreted in terms of both statistical significance (e.g., standardized path coefficients, p-values <0.05, confidence intervals) and practical significance—that is, the strength and direction of relationships will be contextualized based on their implications for real-world application. For example, a strong and significant indirect effect of health system factors mediated through perceived accessibility will be interpreted as evidence for prioritizing improvements in service delivery and outreach as a strategy to enhance PrEP uptake. Similarly, a meaningful direct effect of perceived HIV risk on uptake will be taken to suggest the value of targeted awareness campaigns that personalize HIV vulnerability among youth. Interpretation will also be informed by effect sizes (e.g., standardized coefficients ≥ 0.30 will be considered moderate to strong), and key pathways will be highlighted for their policy and intervention relevance. These findings will be triangulated with qualitative data to provide a nuanced understanding of the mechanisms influencing PrEP use, ensuring that statistical outcomes translate into actionable recommendations for public health programming.
2.13.4.3 Model fit evaluation:
The model’s fit will be evaluated using various fit indices, including the Chi-square statistic, Root Mean Square Error of Approximation (RMSEA), Comparative Fit Index (CFI), and Tucker-Lewis Index (TLI). A good model fit will be indicated by a non-significant Chi-square (p > 0.05), RMSEA < 0.06, CFI > 0.95, and TLI > 0.95.
2.13.4.4 Mediation analysis:
Mediation analysis will be conducted within the SEM framework to assess the mediating role of perception-related factors (e.g., perception of personal risk behaviors, perceived benefits of PrEP, HIV risk perception, stigma, and PrEP accessibility) on the relationship between the independent variables (demographic, economic, and social factors) and PrEP uptake. To rigorously test the significance of mediation pathways, the bias-corrected bootstrapping method will be used. This non-parametric resampling technique will involve generating 5,000 bootstrap samples to estimate 95% confidence intervals for indirect effects. A mediation effect will be considered significant if the bootstrap confidence interval does not include zero. Both partial and full mediation pathways will be interpreted, and results will be contextualized to identify leverage points for programmatic interventions—particularly focusing on modifiable perceptions and attitudes that mediate the effect of structural and contextual factors on PrEP uptake.
2.13.4.4.1 Model optimization and validation:
The final step will involve optimizing the SEM by adjusting the model based on the fit indices and theoretical considerations. The validated model will then be used to identify the most significant factors influencing PrEP uptake, providing insights for targeted interventions and policy recommendations. The optimized model will be cross-validated using a split-sample approach or bootstrapping techniques to ensure its robustness.
Ultimately, this study will employ Covariance-Based Structural Equation Modeling (CB-SEM) to validate the hypothesized model of PrEP uptake. CB-SEM is preferred in this context because the study aims to confirm a theoretically grounded model and assess the relationships among latent constructs based on empirical data. Unlike PLS-SEM, which is more suitable for exploratory or prediction-focused models, CB-SEM is ideal for theory testing and model confirmation. The analysis will be conducted using IBM SPSS AMOS, which supports CB-SEM and allows for detailed model specification, estimation, and evaluation of model fit using a range of goodness-of-fit indices. Assumptions such as multivariate normality and adequate sample size will be checked prior to conducting SEM to ensure robustness and validity of the results.
2.13.4.4.2 Integration of quantitative and qualitative data:
Qualitative data from interviews will undergo thematic analysis to identify recurring themes related to facilitators and barriers influencing PrEP utilization. These qualitative findings will be integrated with the quantitative results from SEM to provide a comprehensive explanation of the factors influencing PrEP uptake. This integration will help identify convergent or divergent patterns between the two data types and offer a holistic interpretation of the results.
2.14 Ethical considerations
The study has been approved by the Moi University School of Graduate Studies (SGS). The MTRH’s Institutional Ethics Review Committee (IERC) provided ethical clearance on 9th August 2024, IREC 889/2024, Approval No 0004877, with data collection expected to commence on 12th February 2025 and end on 30th March 2025. Data collection will start after research authorization and permit have been acquired from NACOSTI. The Director of Public Health Services (DPHS) Uasin Gishu County will provide an official letter of permission for data collection. Before data collection, respondents will be informed about the study’s purpose and procedures, and their consent will be obtained through signing an informed consent form. They will be assured that their participation is voluntary and that they can withdraw at any time if they choose. For youths below 18 years, permission will first be obtained from their respective guardians by having them sign assent forms. Both the guardians and the participants will be informed that there will be no harm likely to arise from the study and that the study will only gear toward improving the overall health of youths aged 15–24 years in Turbo Sub County. Data confidentiality will be maintained by ensuring that no information is disclosed to third parties. Personal identifiers of participants will be excluded during data analysis.
3 Organization and rigor of a research project
The dedicated study core team for this cross-sectional study on HIV Pre-Exposure Prophylaxis (PrEP) uptake among youths in Turbo Sub-County, Uasin Gishu County, Kenya, will consist of the Principal Investigator (PI) and two Co-Principal Investigators (Co-PIs). This core team will ensure adherence to study-specific procedures and standard operating protocols to guarantee accurate data collection and high-quality results.
To maintain quality, consistency, and harmonization of study procedures, standardized training, supervision, and oversight will be provided. This includes regular monitoring and support to ensure all team members understand and follow the established protocols.
The core team will oversee finalizing the study title, securing funding, managing protocol amendments, and overseeing data collection processes. They will ensure proper data management, implement recommendations from the data management team, and set and monitor recruitment start and end dates. The team will track actual recruitment rates against projections, manage the consenting process for participants, and summarize and address protocol deviations. Additionally, they will conduct site visits and report any organizational issues or study-related problems.
The data management team, including the PI, enumerators at study sites, and Community Health Promoters (CHPs), will be responsible for establishing the acceptance rate by comparing participants with those sampled, monitoring data completeness from recruitment through data collection, and providing weekly forecasts on data collection progress. They will oversee data management metrics, such as the rate of electronic data capture, track the number of completed surveys and questionnaires, and ensure data fidelity through monitoring by the enumerators or CHPs. Additionally, they will conduct data quality checks and review results via a dashboard. To reduce social desirability bias, anonymity of responses will be assured and reiterated to respondents, emphasizing the confidentiality of responses, and creating a nonjudgmental environment during data collection and if possible privacy for those who are able to respond to the questions without an assistant the Kobo link will be send to their phones for them to respond to the questionnaire.
4 Dissemination plans
Upon completion of data analysis, the core research team will develop manuscripts for submission to peer-reviewed journals and presentations at international conferences, specifically targeting professionals involved in HIV prevention and youth health services, as well as policymakers and advisors. Additionally, a comprehensive report will be compiled by the PI and archived in relevant institutional repositories.
Feedback sessions will be organized with healthcare professionals, both at operational and strategic levels, within the regions where the study was conducted. The findings will also be disseminated through popular media platforms such as Twitter, Facebook, and local newspapers to reach a broader audience.
While the study protocols will be published in peer-reviewed journals, participant-level data sets and analysis code will be made available upon reasonable written request to ensure transparency and foster further research.
5 Limitations of the study design
This cross-sectional study, like any research, is subject to limitations, including those related to measurement, estimation, assumptions, and strategies. A specific limitation and potential source of bias for this study is selection bias. The study targets youths who are accessible within the selected villages, which may negatively affect the generalization of the findings to the broader population of youths in Turbo Sub-County. Equally, cross-sectional design is not strong in imputing causality, however, the causal relationship between constructs in the model under validation has been widely studied and explained in studies referenced in this protocol.
6 Amendments to the study
As much as major amendments are not foreseeable, the PI will be responsible for communicating any significant protocol modifications, such as changes to eligibility criteria, outcomes, or analyses, to all relevant parties, including study implementers, the Moi University Institutional Ethics Review Committee (IERC), the journal where the study is published, and the National Commission for Science, Technology, and Innovation (NACOSTI).
Author contributions
MS: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. EK: Conceptualization, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing. JS: Methodology, Supervision, Conceptualization, Funding acquisition, Writing – review & editing. NG: Methodology, Supervision, Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. HIV and AIDS. HIV and AIDS (2024). Available online at: https://www.who.int/news-room/fact-sheets/detail/hiv-aids (Accessed August 11, 2024).
2. WHO. HIV and AIDS. Fact Sheets (2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/hiv-aids?gad_source=1&gclid=CjwKCAjw4ri0BhAvEiwA8oo6F7QLONmk9rplCKVc1fg9fU2zUMENuNacFCvj_UX-ySJGyybWkLitjxoCfS0QAvD_BwE (Accessed August 11, 2024).
3. Bekker LG, Alleyne G, Baral S, Cepeda J, Daskalakis D, Dowdy D, et al. Advancing global health and strengthening the HIV response in the era of the Sustainable Development Goals: the International AIDS Society—Lancet Commission. Lancet. (2018) 392:312. doi: 10.1016/S0140-6736(18)31070-5
4. Lung VPKSKMTHDW. Global goal to end HIV/AIDS is off track: Here’s how we can catch up. World Bank Blogs (2022).
5. UNAIDS. 90-90–90 treatment target. UNAIDS (2018). Available online at: https://www.unaids.org/en/90-90-90 (Accessed August 23, 2020).
6. Roberts ST, Mancuso N, Williams K, Nabunya HK, Mposula H, Mugocha C, et al. How a menu of adherence support strategies facilitated high adherence to HIV prevention products among adolescent girls and young women in sub-Saharan Africa: a mixed methods analysis. J Int AIDS Soc. (2023) 26:e26189–9. doi: 10.1002/JIA2.26189
7. Barnabee G, Billah I, Ndeikemona L, Silas L, Ensminger A, MacLachlan E, et al. PrEP uptake and early persistence among adolescent girls and young women receiving services via community and hybrid community-clinic models in Namibia. PloS One. (2023) 18:e0289353. doi: 10.1371/JOURNAL.PONE.0289353
10. Ogolla M, Nyabiage OL, Musingila P, Gachau S, Odero TMA, Odoyo-June E, et al. Uptake and continuation of HIV pre-exposure prophylaxis among women of reproductive age in two health facilities in Kisumu County, Kenya. J Int AIDS Soc. (2023) 26. doi: 10.1002/JIA2.26069
11. Tanner MR, Miele P, Carter W, Valentine SS, Dunville R, Kapogiannis BG, et al. Preexposure prophylaxis for prevention of HIV acquisition among adolescents: clinical considerations, 2020. MMWR Recommendations Rep. (2020) 69:1–12. doi: 10.15585/MMWR.RR6903A1
12. Camlin CS, Koss CA, Getahun M, Owino L, Itiakorit H, Akatukwasa C, et al. Understanding demand for prEP and early experiences of prEP use among young adults in rural Kenya and Uganda: A qualitative study. AIDS Behav. (2020) 24:2149–62. doi: 10.1007/S10461-020-02780-X
14. Were D, Musau A, Mutegi J, Ongwen P, Manguro G, Kamau M, et al. Using a HIV prevention cascade for identifying missed opportunities in PrEP delivery in Kenya: results from a programmatic surveillance study. J Int AIDS Soc. (2020) 23 Suppl 3:e25537. doi: 10.1002/JIA2.25537
15. Vega-Ramirez H, Torres TS, Guillen-Diaz C, Pimenta C, Diaz-Sosa D, Konda KA, et al. Awareness, knowledge, and attitudes related to HIV pre-exposure prophylaxis and other prevention strategies among physicians from Brazil and Mexico: cross-sectional web-based survey. BMC Health Serv Res. (2022) 22:532–2. doi: 10.1186/S12913-022-07900-Y
16. Shamu S, Shamu P, Khupakonke S, Farirai T, Chidarikire T, Guloba G, et al. Pre-exposure prophylaxis (PrEP) awareness, attitudes and uptake willingness among young people: gender differences and associated factors in two South African districts. Glob Health Action. (2021) 14:1886455. doi: 10.1080/16549716.2021.1886455
17. Marcus JL, Hurley LB, Dentoni-Lasofsky D, Ellis CG, Silverberg MJ, Slome S, et al. Barriers to preexposure prophylaxis use among individuals with recently acquired HIV infection in northern california. AIDS Care. (2019) 31:536. doi: 10.1080/09540121.2018.1533238
18. Nakasone SE, Young I, Estcourt CS, Calliste J, Flowers P, Ridgway J, et al. Risk perception, safer sex practices and PrEP enthusiasm: barriers and facilitators to oral HIV pre-exposure prophylaxis in Black African and Black Caribbean women in the UK. Sex Transm Infect. (2020) 96:349–54. doi: 10.1136/SEXTRANS-2020-054457
19. She B, Lu F, Zhao R, Lin S, Sun J, He S, et al. Examining the Effects of PrEP Use on Sexual Behaviors and Sexually Transmitted Infections Among Chinese Men who have Sex with Men: A Cross-Sectional Study. AIDS Behav. (2024). 28:3128–38. doi: 10.1007/s10461-024-04398-9
20. Krakower DS and Mayer KH. Pre-exposure prophylaxis to prevent HIV infection: current status, future opportunities and challenges. Drugs. (2015) 75:243–51. doi: 10.1007/s40265-015-0355-4
21. Mayer KH, Agwu A, and Malebranche D. Barriers to the wider use of pre-exposure prophylaxis in the United States: A narrative review. Adv Ther. (2020) 37:1778–811. doi: 10.1007/S12325-020-01295-0
22. Rogers Z, Pintye J, Kinuthia J, O’Malley G, Abuna F, Escudero J, et al. Key influences on the decision to initiate PrEP among adolescent girls and young women within routine maternal child health and family planning clinics in Western Kenya. AIDS Care. (2022) 34:363. doi: 10.1080/09540121.2021.1981217
23. Jackson-Gibson M, Ezema AU, Orero W, Were I, Ohiomoba RO, Mbullo PO, et al. Facilitators and barriers to HIV pre-exposure prophylaxis (PrEP) uptake through a community-based intervention strategy among adolescent girls and young women in Seme Sub-County, Kisumu, Kenya. BMC Public Health. (2021) 21:1–13. doi: 10.1186/S12889-021-11335-1/TABLES/1
24. Masyuko S, Mukui I, Njathi O, Kimani M, Oluoch P, Wamicwe J, et al. Pre-exposure prophylaxis rollout in a national public sector program: The Kenyan case study. Sex Health. (2018) 15:578–86. doi: 10.1071/SH18090
25. Kayesu I, Mayanja Y, Nakirijja C, Machira YW, Price M, Seeley J, et al. Uptake of and adherence to oral pre-exposure prophylaxis among adolescent girls and young women at high risk of HIV-infection in Kampala, Uganda: A qualitative study of experiences, facilitators and barriers. BMC Womens Health. (2022) 22:440. doi: 10.1186/S12905-022-02018-Z
26. Atkins K, Musau A, Mugambi M, Odhyambo G, Tengah SA, Kamau M, et al. Health system opportunities and challenges for PrEP implementation in Kenya: A qualitative framework analysis. PloS One. (2022) 17:e0259738. doi: 10.1371/JOURNAL.PONE.0259738
27. Przybyla S, Fillo J, Kamper-DeMarco K, Bleasdale J, Parks K, Klasko-Foster L, et al. HIV pre-exposure prophylaxis (PrEP) knowledge, familiarity, and attitudes among United States healthcare professional students: A cross-sectional study. Prev Med Rep. (2021) 22:101334. doi: 10.1016/J.PMEDR.2021.101334
28. Graham SM, Okall DO, Mehta SD, Obondi E, Ng’ety G, Ochieng E, et al. Challenges with prEP uptake and adherence among gay, bisexual, and other men who have sex with men in Kisumu, Kenya. AIDS Behav. (2023) 27:1234. doi: 10.1007/S10461-022-03860-W
29. Muhumuza R, Ssemata AS, Kakande A, Ahmed N, Atujuna M, Nomvuyo M, et al. Exploring perceived barriers and facilitators of prEP uptake among young people in Uganda, Zimbabwe, and South Africa. Arch Sex Behav. (2021) 50:1729. doi: 10.1007/S10508-020-01880-Y
30. Rotsaert A, Reyniers T, Jacobs BKM, Vanbaelen T, Burm C, Kenyon C, et al. PrEP user profiles, dynamics of PrEP use and follow-up: a cohort analysis at a Belgian HIV centre (2017–2020). J Int AIDS Soc. (2022) 25:25953. doi: 10.1002/JIA2.25953
31. Shaw G, Schaefer R, Schmidt HMA, Madden A, Chang J, Mozalevskis A, et al. Pre-exposure prophylaxis (PrEP) for HIV prevention among people who inject drugs: a global mapping of service delivery. Harm Reduct J. (2023) 20:1–8. doi: 10.1186/S12954-023-00729-6/TABLES/1
32. Irungu EM, Mugwanya KK, Mugo NR, Bukusi EA, Donnell D, Odoyo J, et al. Integration of pre-exposure prophylaxis services into public HIV care clinics in Kenya: a pragmatic stepped-wedge randomised trial. Lancet Glob Health. (2021) 9:e1730–9. doi: 10.1016/S2214-109X(21)00391-0
33. Irungu EM and Baeten JM. PrEP rollout in Africa: status and opportunity. Nat Med. (2020) 26:655–64. doi: 10.1038/s41591-020-0872-x
34. Moussa AB, Badahdah AM, Hidous K, Barakad R, Diallo F, Traoré M, et al. Barriers to oral prEP: A qualitative study of female sex workers, prEP prescribers, policymakers, and community advocates in Morocco. J Int Assoc Provid AIDS Care. (2024) 23:23259582241266692. doi: 10.1177/23259582241266691
Keywords: HIV prevention and control, validated model, pre-exposure prophylaxis (PrEP), Structural Equation Modeling (SEM), Kenya
Citation: Kileku EN, Sitienei J, Shisanya MS and Gitahi N (2025) Validation of a model for predicting HIV pre-exposure prophylaxis uptake: a study protocol. Front. Trop. Dis. 6:1571116. doi: 10.3389/fitd.2025.1571116
Received: 05 February 2025; Accepted: 22 April 2025;
Published: 06 June 2025.
Edited by:
Stanis Okitotsho Wembonyama, University of Lubumbashi, Democratic Republic of CongoReviewed by:
David Eugene Vance, University of Alabama at Birmingham, United StatesDimas Setyadi Putra, Padjadjaran University, Indonesia
Copyright © 2025 Kileku, Sitienei, Shisanya and Gitahi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Morris Senghor Shisanya, bXNoaXNhbnlhQGtpYnUuYWMua2U=;, c2VuZ2hvcm1vcnJpc0BnbWFpbC5jb20=
 Elizabeth Nailantei Kileku
Elizabeth Nailantei Kileku Joseph Sitienei2
Joseph Sitienei2 Morris Senghor Shisanya
Morris Senghor Shisanya