- 1Office of the Research Innovation & Commercialization, Khyber Medical University, Peshawar, Pakistan
- 2Primary Care and Mental Health, Institute of Population Health, University of Liverpool, Liverpool, United Kingdom
- 3School of Nursing and Midwifery and the Applied Health Research Hub (AHRh), University of Central Lancashire, Preston, United Kingdom
- 4Ulverscroft Eye Unit, Institute of Precision Health, University of Leicester, Leicester, United Kingdom
- 5Stroke Research Team, School of Nursing & Midwifery, University of Central Lancashire, Preston, United Kingdom
Tuberculosis (TB) is a preventable, curable disease but still impacts people in high-burden countries, who face challenges, including stigma, in accessing and engaging with healthcare services. The Nuttall's review examined the quality of existing TB-stigma intervention studies and developed a conceptual framework of pathways to stigma reduction. We critically appraised the methods used and expanded upon these findings in the context of the WHO End TB Strategy. The included studies showed significant heterogeneity in design, aims, populations, type of TB-stigma targeted and took place across diverse countries. Only three of 11 studies were rated as high quality. This systematic review synthesized existing interventions and outcomes into a conceptual framework outlining pathways to reduce TB-stigma. The conceptual framework highlights the need for educational, emotional, and psychosocial support for TB patients, Health Care Workers, and Communities, and provides a useful guide of pathways needed in TB-stigma reduction interventions. However, to be effective, stigma reduction interventions must be part of a well-organized, and committed multi-sectoral collaboratives, which extend beyond national and global TB programs, including mental health services, social support systems, and public health programs.
Introduction
Each year, approximately 10 million people contract tuberculosis (TB), a preventable and curable disease (1). The World Health Organization (WHO) End TB Strategy's goal is to reduce the global TB epidemic by 2035 (2). Half of all High Burden Countries (HBC) for TB, as defined by WHO, are listed as low- and middle-income countries (LMICs) (1). People with TB still face challenges in accessing, and engaging with healthcare services (3).
Stigma is described by the WHO as a “hidden” burden of disease (4) and a major barrier to ending TB globally (5). People with TB often face different types of stigmas as defined in Box 1. These stem from cultural fears and misconceptions, which significantly hinder testing, contact tracing, treatment linkage, and medication adherence (6, 7). However, the process and impact evaluation of TB-stigma interventions are limited. A 2017 review focusing on stigma-reduction interventions highlighted the complexity of measuring and addressing stigma (9). Recently, Nuttall et al. (10) examined the quality of existing TB-stigma intervention studies and created a novel conceptual framework of pathways to TB-stigma reduction (10). In this perspective we critically analyse Nuttall et al. (10) and apply their findings in the context and the aims of the WHO End TB Strategy. We ask the question can this conceptual framework help HBC for TB to operationalise effective TB-stigma reduction programs. The Nuttall et al. (10) review aimed to examine the quality of existing TB-stigma intervention studies and create a novel conceptual framework of pathways to TB-stigma reduction (10). We critically appraised the methods used in this review and expanded upon the findings in the context of WHO End TB Strategy (1, 2, 11). In addition, we have examined the continuing challenges for TB-stigma interventions and how they can be refined for future implementation and scale-up.
Box 1. TB-Stigma definitions (8).
Enacted (or experienced) stigma encompasses the range of behaviors directly experienced by a person with TB.
Anticipated stigma is the expectation and fear of discrimination and behavior of others toward a person if they are diagnosed and/or unwell with TB, which has an impact on health-seeking behavior, whether enacted stigma occurs or not.
Internalized (or self) stigma is when those diagnosed and/or unwell with TB may accept a negative stereotype about people with TB and potentially act in a way that endorses this stereotype.
Secondary or external stigma is the negative attitude toward family members, caregivers, friends, or TB healthcare workers because they are associated with, live with, or have close contact with people with TB.
Critical appraisal of the methods in Nuttall et al.
Nuttall et al. (10) included studies that reported the implementation and evaluation of TB-stigma reduction interventions amongst people with TB and their households, healthcare workers (HCWs) and the public. This included a wide range of study designs, with all studies importantly measuring TB-stigma. The Joanna Briggs Institute critical appraisal tool for systematic review and research synthesis (12) was used to appraise Nuttall et al. (10). The appraisal purpose was to assess methodological quality and the possibility of bias in design, conduct, and analysis of this review; following an independent process and consensus discussion two of the 11 criteria were not achieved (Table 1).
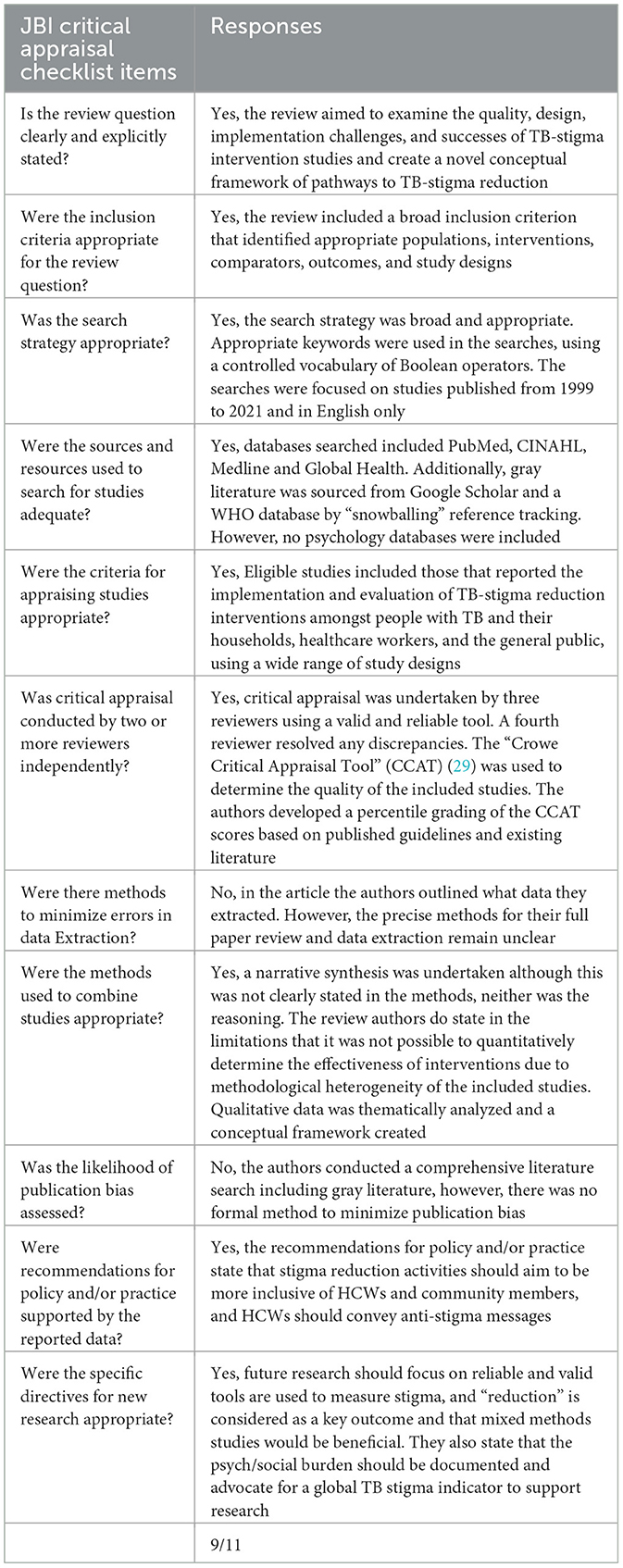
Table 1. Critical appraisal using the JBI critical appraisal checklist for systematic reviews and research syntheses (12).
It is important to note that the following criteria was not met: no information that outlined any methods to minimize errors in data extraction; or evidence of a formal assessment of publication bias. The former is an important consideration to minimize bias or systematic errors in the conduct of the review. Clarity is needed to know what efforts were made by authors, for example, if data extraction was done in duplicate and independently, or evidence of training/piloting of their extraction tools (12). We can mitigate publication bias by having a comprehensive search strategy, which can best capture all relevant studies. The authors reported a detailed strategy and also looked at the gray literature, however no psychology databases were included. Publication bias was acknowledged as a potential limitation by the authors. Undertaking a meta-analysis looking at TB stigma intervention effect measurements would have been useful to test for publication bias and potential bias in outcome reporting (12). However, this may have not been possible because of the limited number of studies identified with quantitative stigma measurement tools (<10) plus the heterogeneity of the tests undertaken. Nevertheless, this influence was not discussed within the review. Overall, despite the two concerns, 1 provides a comprehensive summary of the available data that address the question of interest. However, there were no clear recommendations for their implementation.
Results of the review by Nuttall et al.
The 11 included studies showed significant heterogeneity in design, aims, populations, type of TB-stigma targeted and regions, spanning low-income (n = 1), middle-income (n = 9), and high-income (n = 1) countries, respectively. Study populations varied between people with TB and their households (n = 5), healthcare workers (HCWs) (n = 3), and the public (n = 3). The study quality varied, with a median CCAT score of 24/40; issues such as lack of methodological detail and protocols affected lower scores. Only three studies were of high quality and review authors describe paper quality as “moderate.” Five studies measured anticipated stigma, two enacted stigma and five focused on internalized stigma. The findings showed that TB-stigma affects patients, their families, HCWs, and the public stemming from the illness, diagnosis, and treatment. There were three studies focusing on the public, three with TB HCWs and five targeting people with TB.
Interventions, like TB clubs, home visits, and psychosocial support groups significantly reduced “internalized” stigma, empowerment and changes to norms and behavior, and improved TB knowledge. However, home visits in areas with high TB-stigma, may have unintentionally triggered “anticipated” or “internalized” stigma. In addition, TB educational efforts enhanced confidence, and reduced myths.
Training for TB HCWs improved their knowledge, attitudes, and practices toward patients, contributing to better TB care. Nonetheless, TB-related HCWs frequently faced stigma from their peers. While the training did not reduce “secondary or external” stigma, TB-related HCWs could potentially utilize campaign materials to educate their local communities. However, in public health interventions, the failure to deliver a clear health message, through educational material, allowed TB-stigma misconceptions to persist or worsen.
Some studies employed quantitative questionnaires to measure TB-stigma, with the number of questions varying from 3 to 14. Half of these studies used validated TB-stigma tools. The others used adapted tools, and one piloted a new tool in six different African communities. Some studies utilized qualitative methods, such as focus groups, interviews, and observations, to assess stigma. These focused on exploring how TB patients coped with “internalized” stigma, “anticipated” stigma from others, and one study focused on, “secondary or external,” how HCWs working with TB patients experienced stigmatization from their colleagues. Challenges related to implementation, delivery, and process indicators (e.g., fidelity, acceptability, and feasibility) were rarely addressed in the studies.
By synthesizing the interventions and outcomes of these studies, Nutall et al. (10), designed a conceptual framework with pathways to reduce TB-stigma based on targeted populations (10). In this, they highlighted mechanisms for intended outcomes, which included improving understanding, removing misconceptions, attitude and behaviors change among public via educational material, mass gathering (health talks) and health education programs. They also highlighted intended impacts in terms of reducing stigma among people with TB, toward TB-HCWs, TB “internalized” stigma, improving TB treatment adherence, completion, success and minimizing the economic consequences of TB. However, the authors did not make recommendations on how to use this framework.
Discussion
In global efforts and strategies to prevent and control tuberculosis, stigma has historically been a low-priority issue (13). At its inception the WHO End TB strategy did not explicitly talk about stigma but emphasized addressing social determinants of TB via stakeholder involvement at individual, community, and government levels through patient-centered care approaches, and health education and awareness (2). Combating stigma and discrimination was included in the updated “Implementing the End of TB Strategy” (11). TB-Stigma was the sixth priority recommendation but still failed to emphasize how to introduce mechanisms to report, address and evaluate the stigma status among tuberculosis patients at a system level.
TB stigma not being a primary objective of policy has led to gaps in the literature. Systematic reviews in this field predominantly feature qualitative evidence (9, 10, 14, 15) consisting of studies majorly from Africa, although most HBC for TB, including Pakistan, are found in Asia (1). Nuttall et al. (10) reviewed the literature and created a conceptual framework that provides a useful guide to understanding the pathways needed in TB-stigma reduction interventions. Decreasing TB stigma requires a multi-level, holistic approach, with community-informed, person-centered interventions prioritized by TB programs (16). However, Nuttall et al. make no explicit mention of how TB stigma-reduction efforts should be integrated within existing health systems.
Empowering people with TB, and communities
Nuttall et al. (10) emphasized intellectual and emotional empowerment. In high-risk populations, the framework effectively highlights the need for educational, emotional, and psychosocial support for TB patients, HCWs, and the community. TB-stigma interventions seem to lean heavily on informational interventions such as pamphlets, health talks and workshops. These methods alone may not fully address deep-rooted stigma, particularly where poverty and cultural beliefs or systemic issues are involved (17, 18). For example, though the framework includes public education, it doesn't explicitly mention adapting interventions to local cultural contexts, particularly in LMICs (19). Few interventions have engaged patients and communities effectively at each step of the care process, highlighting the need for further research on prioritizing patient-centered care in resource-constrained settings (20).
Addressing the social determinants of TB
The framework touches on misconceptions and psychosocial factors but does not fully address structural barriers like poverty, healthcare access, and discrimination. Addressing TB-stigma requires tackling these broader determinants of health, especially in resource-constrained settings (19). While Nuttall et al. (10) addresses capability through knowledge and emotional support, it overlooked the critical aspect of financial empowerment. Providing financial empowerment is essential to ensure opportunity, which enables patients to access and utilize TB care services. For example, asking patients to wear masks or attend clinics is ineffective if they lack the financial means to buy masks or cover transportation costs. Without financial support, even well-informed patients may struggle to engage in care. Therefore, offering both knowledge and the means to act on that knowledge is equally important for successful TB stigma reduction and treatment adherence.
Health system integration and strengthening
There is a need for greater emphasis on strengthening health systems in HBC for TB, which currently lag due to limited focus and resources. Anticipated, internal, and enacted stigma are significant barriers to TB care, directly affecting patient wellbeing, yet targeted stigma interventions remain limited (5). Understanding stigma drivers is essential to enhance timely diagnosis and treatment for people living with TB, with stigma reduction being critical to advancing care engagement (21). To this end measuring all forms of stigma is important. System-level enhancements such as routine stigma monitoring mechanisms, integration of stigma indicators into patient records, and structured monitoring and evaluation processes contribute to sustained health system strengthening. However, validated tools to measure TB-stigma remain scarce (22) and those used lack cultural and linguistic validation, highlighting the critical need for reliable and valid tools to measure TB stigma in LMICs most affected by the disease (7).
In addition, stigma from healthcare workers who don't work in TB facilities not only impacts patient care but also health-seeking behavior, necessitating workforce stigma-reduction strategies to improve patient outcomes (23). Nuttall et al. (10) highlighted the stigma faced by HCWs, highlighting the need to make HCWs feel safe while undergoing clinical training and psychosocial support. To be effective, stigma reduction interventions must be part of a larger health system response, including mental health services, social support systems and public health programs. Furthermore, workplace protections and gender-sensitive support are added to ensure equitable, non-discriminatory environments that acknowledge social and gender-based vulnerabilities (24, 25). However, confidentiality safeguards and mental health support for both healthcare workers and people with TB should be included to foster trust, psychological wellbeing, and a stigma-free care environment (26).
Navigating emerging, operationalising, and future interventions
The recent WHO report highlights progress in European and African countries, (1) demonstrating that targeted efforts can yield results. However, there is a need for greater emphasis on strengthening systems and research activities in other HBC for TB, like Pakistan, which currently lag due to limited focus and resources. In addition, research should aim to characterize TB stigma across diverse populations, using validated tools to assess its impact on time to diagnosis, treatment adherence, morbidity, and mortality, while also developing new strategies to mitigate TB stigma.
Current interventions focus on raising community awareness, providing patient counseling on problem-solving and emotional skills, creating culturally sensitive and scientifically accurate media messages, incentives, and enhancing healthcare professionals' empathy, respect, concern, and cultural sensitivity (13). TB stigma in communities can be reduced through shared commitment to TB prevention and supportive environments at home, in the community, and within healthcare services (23).
With most of the studies, in Nuttall et al. (10), being reported from Africa and earlier than 2021, it is highly recommended to search for recent and contextual interventions to take insights for developing innovative and context-based solutions. For example, a communication intervention based on self-efficacy and social support theories at Thai high schools (27) and “Jaga rasa Jaga tangga” (take care of your neighbors as well as take care of their feelings) community for HCWs (23). The diverse contexts, health infrastructure, and HBC for TB require tailored approaches to effectively address TB prevention and control efforts in different settings (19).
Limitations
We followed the steps outlined in the Rapid Conversion of Evidence Summaries (RaCES) developed by the NIHR Applied Research Collaboration North West Coast (28). Through this approach we aim to answer an important health and social care question to help inform policy and practice and aid implementation. Therefore, we acknowledge that our perspective does not present findings from an original systematic review or a formal literature update, but is a critical reflection based primarily on existing evidence in a recently published systematic review. This approach is focused on implementing the best current knowledge in the real world, supported and substantiated through relevant and credible references to ensure conceptual validity and evidence-based interpretation.
Conclusions
In this perspective, we examined the continuing challenges and outlined potential changes to this framework making it a better guide for future implementation and scale-up in HBC for TB. To move closer to eradicating TB, we require urgent, well-organized, and committed multi-sectoral actions to reducing TB stigma, that extend beyond national and global TB programs. This effort must be supported by substantial investments in research and the equitable, rapid implementation of innovations worldwide. Few TB stigma reduction interventions have been rigorously evaluated, and replication of effective studies has been rare. The conceptual framework by Nuttall et al. (10) is a useful guide helping HBC for TB to operationalise effective TB-stigma reduction programs.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
BB: Writing – review & editing, Writing – original draft, Conceptualization. MG: Writing – original draft, Writing – review & editing, Conceptualization. IR: Writing – review & editing, Conceptualization, Writing – original draft. SJ: Conceptualization, Writing – review & editing, Writing – original draft. CM: Writing – original draft, Conceptualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was partly-funded by the National Institute for Health and Care Research Applied Research Collaboration North West Coast (NIHR ARC NWC).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
References
1. WHO. Global Tuberculosis Report 2024. (2024). Available online at: https://www.who.int/publications/i/item/9789240101531 (Accessed November 4, 2024).
3. Maynard C, Tariq S, Sotgiu G, Migliori GB, van den Boom M, Field N. Psychosocial support interventions to improve treatment outcomes for People living with tuberculosis: a mixed methods systematic review and meta-analysis. EClinicalMedicine. (2023) 61:102057. doi: 10.1016/j.eclinm.2023.102057
4. Kane JC, Elafros MA, Murray SM, Mitchell EM, Augustinavicius JL, Causevic S, et al. A scoping review of health-related stigma outcomes for high-burden diseases in low-and middle-income countries. BMC Med. (2019) 17:1–40. doi: 10.1186/s12916-019-1250-8
5. Hayward SE, Vanqa N, Makanda G, Tisile P, Ngwatyu L, Foster I, et al. “As a patient I do not belong to the clinic, I belong to the community.” Co-developing a multi-level, person-centred tuberculosis stigma intervention in Cape Town, South Africa. Res Sq. (2024) rs.3.rs-3921970. doi: 10.21203/rs.3.rs-3921970/v1
6. Villar-Hernández R, Ghodousi A, Konstantynovska O, Duarte R, Lange C, Raviglione M. Tuberculosis: current challenges and beyond. Breathe. (2023) 19:220166. doi: 10.1183/20734735.0166-2022
7. Bergman A, McNabb K, Farley JE. A systematic review and psychometric appraisal of instruments measuring tuberculosis stigma in Sub-Saharan Africa. Stigma Health. (2024) 9:81. doi: 10.1037/sah0000328
8. The Stop TB Partnership. TB Stigma Assessment - Implementation Handbook. Geneva, Switzerland: Stop TB Partnership (2019).
9. Sommerland N, Wouters E, Mitchell E, Ngicho M, Redwood L, Masquillier C, et al. Evidence-based interventions to reduce tuberculosis stigma: a systematic review. Int J Tuberc Lung Dis. (2017) 21:S81–6. doi: 10.5588/ijtld.16.0788
10. Nuttall C, Fuady A, Nuttall H, Dixit K, Mansyur M, Wingfield, T. Interventions pathways to reduce tuberculosis-related stigma: a literature review and conceptual framework. Infect Dis Poverty. (2022) 11:101. doi: 10.1186/s40249-022-01021-8
11. WHO. Implementing the End TB Strategy: The Essentials, 2022 Update. (2022). Available online at: https://www.who.int/publications/i/item/9789240065093 (Accessed November 3, 2024).
12. Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Health. (2015) 13:132–40. doi: 10.1097/XEB.0000000000000055
13. Yadav S. Stigma in tuberculosis: time to act on an important and largely unaddressed issue. Cureus. (2024) 16:e61964. doi: 10.7759/cureus.61964
14. Faraade MH, Jeffree MS, LIN, LJ, Fiidow OA, Avoi R, et al. Intervention approaches of stigma related to tuberculosis in developing countries: a systematic review. Malays J Public Health Med. (2022) 22:197–204. doi: 10.37268/mjphm/vol.22/no.2/art.1753
15. Foster I, Galloway M, Human W, Anthony M, Myburgh H, Vanqa N, et al. Analysing interventions designed to reduce tuberculosis-related stigma: a scoping review. PLOS Glob Public Health. (2022) 2:e0000989. doi: 10.1371/journal.pgph.0000989
16. Myburgh H, Baloyi D, Loveday M, Meehan S.-A, Osman M, Wademan D, et al. A scoping review of patient-centred tuberculosis care interventions: gaps and opportunities. PLOS Glob Public Health. (2023) 3:e0001357. doi: 10.1371/journal.pgph.0001357
17. Rocha C, Montoya R, Zevallos K, Curatola A, Ynga W, Franco J, et al. The innovative socio-economic interventions against tuberculosis (ISIAT) project: an operational assessment. Int J Tuberc Lung Dis. (2011) 15:S50–7. doi: 10.5588/ijtld.10.0447
18. Wingfield T, Boccia D, Tovar MA, Huff D, Montoya R, Lewis JJ, et al. Designing and implementing a socioeconomic intervention to enhance TB control: operational evidence from the CRESIPT project in Peru. BMC Public Health. (2015) 15:1–16. doi: 10.1186/s12889-015-2128-0
19. Islam MS, Chughtai AA, Banu S, Seale H. Context matters: examining the factors impacting the implementation of tuberculosis infection prevention and control guidelines in health settings in seven high tuberculosis burden countries. J Infect Public Health. (2021) 14:588–97. doi: 10.1016/j.jiph.2021.01.014
20. Junaid SA, Kanma-Okafor OJ, Olufunlayo TF, Odugbemi BA, Ozoh OB. Tuberculosis stigma: assessing tuberculosis knowledge, attitude and preventive practices in surulere, Lagos, Nigeria. Ann Afr Med. (2021) 20:184–92. doi: 10.4103/aam.aam_40_20
21. Sabin LL, Thulasingam M, Carwile M, Babu SP, Knudsen S, Dong L, et al. ‘People listen more to what actors say': a qualitative study of tuberculosis-related knowledge, behaviours, stigma, and potential interventions in Puducherry, India. Glob Public Health. (2022) 17:2898–910. doi: 10.1080/17441692.2021.1990372
22. Fuady A, Arifin B, Yunita F, Rauf S, Fitriangga A, Sugiharto A, et al. Stigma towards people with tuberculosis: a cross-cultural adaptation and validation of a scale in Indonesia. BMC Psychol. (2023) 11:112. doi: 10.1186/s40359-023-01161-y
23. Purwanti NS, Ghofur A, Khairani W, Sasmito P. Introducing Jaga-rasa Jaga-tangga: a community program that can reduce tuberculosis stigma in Sleman, Indonesia. Int J Public Health Excell. (2024) 3:713–20. doi: 10.55299/ijphe.v3i2.829
24. Ringwald B, Mwiine AA, Chikovore J, Makanda G, Amoah-Larbi J, Millington KA, et al. Ending TB means responding to socially produced vulnerabilities of all genders. BMJ Glob Health. (2023) 8:e014151. doi: 10.1136/bmjgh-2023-014151
25. Brüggemann R, Schlumberger F, Chinshailo F, Willis M, Kadyrov A, Kalmambetova G, et al. Stigmatization and discrimination of female tuberculosis patients in Kyrgyzstan – a phenomenological study. Int J Equity Health. (2025) 24:185. doi: 10.1186/s12939-025-02566-4
26. van der Westhuizen HM, Dorward J, Roberts N, Greenhalgh T, Ehrlich R, Butler CC, et al. Health worker experiences of implementing TB infection prevention and control: a qualitative evidence synthesis to inform implementation recommendations. PLOS Glob Public Health. (2022) 2:e0000292. doi: 10.1371/journal.pgph.0000292
27. Moonsarn S, Kasetjaroen Y, Bettex-Baars A.-M, Phanumartwiwath A. A communication-based intervention study for reducing stigma and discrimination against tuberculosis among Thai high-school students. Int J Environ Res Public Health. (2023) 20:4136. doi: 10.3390/ijerph20054136
28. Clegg AH, Harrison J, Benedetto V. Rapid Conversion of Evidence Summaries (RaCES), ARCNWC MIDAS. (2019). Available online at: https://arc-nwc.nihr.ac.uk/midas/rapid-conversion-of-evidence-summaries/ (Accessed November 4, 2025).
29. Crowe M. Crowe Critical Appraisal Tool (CCAT). (2013). Available online at: https://conchra.com.au/wp-content/uploads/2015/12/CCAT-form-v1.4.pdf (Accessed November 3, 2024).
Keywords: tuberculosis, stigma, intervention, conceptual framework, implementation
Citation: Bibi B, Goodall M, Ranjit I, Jones S and Miller C (2025) Implementing TB-Stigma reduction interventions in High Burden Countries: a perspective on a conceptual framework. Front. Tuberc. 3:1721361. doi: 10.3389/ftubr.2025.1721361
Received: 09 October 2025; Revised: 07 November 2025; Accepted: 07 November 2025;
Published: 28 November 2025.
Edited by:
Kirankumar Rade, World Health Organisation, IndiaReviewed by:
Alcione Basílio De Abreu, Fiocruz Mato Grosso do Sul, BrazilCopyright © 2025 Bibi, Goodall, Ranjit, Jones and Miller. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bushra Bibi, YnVzaHJhc2hhaC5vcmljQGttdS5lZHUucGs=
 Bushra Bibi
Bushra Bibi Mark Goodall
Mark Goodall Injety Ranjit
Injety Ranjit Stephanie Jones5
Stephanie Jones5