- 1Department of Pediatrics, Mie University Graduate School of Medicine, Tsu, Japan
- 2Department of Pediatric Cardiology, National Cerebral and Cardiovascular Center, Suita, Japan
- 3Division of Clinical Research Planning, Department of Development Strategy and Cardiology, Center for Clinical Research and Development, National Center for Child Health and Development, Tokyo, Japan
- 4Department of Regional Pediatrics and Perinatology, Ehime University Graduate School of Medicine, Toon, Japan
- 5Department of Pediatrics, Jikei University School of Medicine, Tokyo, Japan
- 6Department of Pediatrics, Nippon Medical School, Tokyo, Japan
- 7Department of Forensic Medicine, Tokai University School of Medicine, Isehara, Japan
- 8Department of Public Health, Jichi Medical University, Shimotsuke, Japan
- 9Department of Pathology, Toho University Medical Center, Ohashi Hospital, Tokyo, Japan
- 10Department of Pediatrics and Child Health, Nihon University School of Medicine, Tokyo, Japan
- 11Department of Pediatrics, Toyama University School of Medicine, Toyama, Japan
- 12Department of Pediatric Cardiology, Chukyo Hospital, Nagoya, Japan
- 13Department of Pediatric Cardiology, Hiroshima City Hiroshima Citizens Hospital, Hiroshima, Japan
- 14Department of Pediatrics and Child Health, Kurume University, Kurume, Japan
- 15Department of Cardiology, Dokkyo Medical University Koshigaya Hospital, Koshigaya, Japan
- 16Department of Pediatrics, Kurashiki Central Hospital, Kurashiki, Japan
- 17Department of Cardiology, Toyota Kosei Hospital, Toyota, Japan
- 18Department of Cardiology, Japanese Red Cross Kumamoto Hospital, Kumamoto, Japan
- 19Cardiovascular Center, Fukuoka Sanno Hospital, Fukuoka, Japan
- 20Department of Pediatric Cardiology and Nephrology, Graduate School of Medical Science, Kyoto Prefectural University of Medicine, Kyoto, Japan
Background: Acute coronary syndrome (ACS), which is emerging in adults long after confirmed (followed-up or lost-to-follow), or missed Kawasaki disease (KD), is poorly characterized.
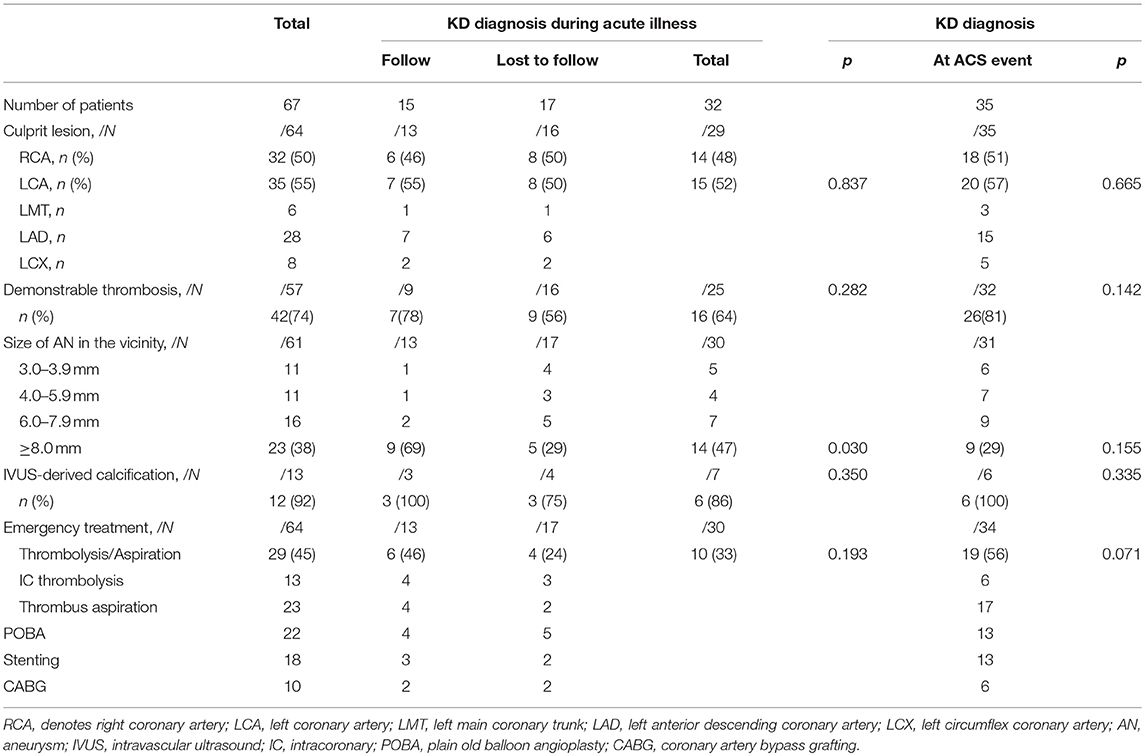
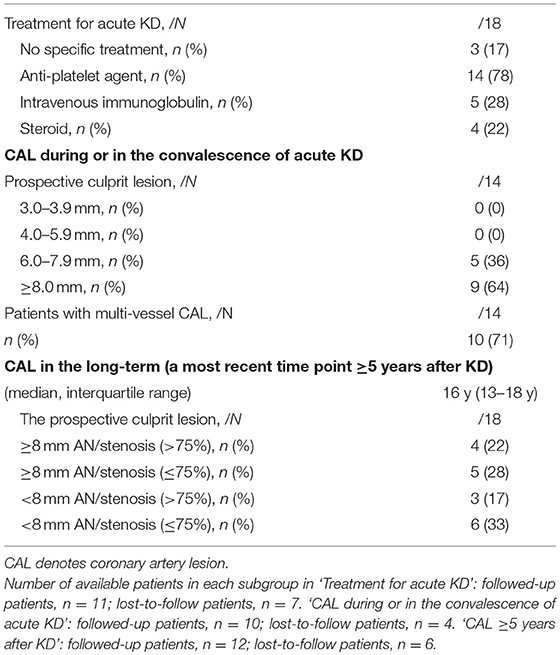
Methods and Results: A Japanese retrospective nationwide hospital-based questionnaire survey of ACS during 2000–09 was conducted to characterize such patients. Among a total of 67 patients (median age 35, male 76%) recruited, low conventional coronary risks (≤1/6) was noted in 75%, a diagnosis of ST-elevation and myocardial infarction or cardiac arrest in 66%, medication before ACS in 22% (warfarin in 4%), and no prior history of acute myocardial infarction in 94%. One-month mortality was 19%. KD diagnosis was made in 32 during acute illness (Group A), in which 17 were lost to follow, and retrospectively in the other 35 from coronary imaging at ACS (Group B). Group A developed ACS at lower coronary risks (≤2/5 in 87 vs. 65% in group B, p = 0.043) at a younger age (26.5 vs. 40 yo, p < 0.001). In group A, followed-up patients developed ACS under medication before ACS (87 vs. 0% in lost-to-follow patients, p < 0.001) for giant aneurysm in culprit lesions (69 vs. 29%, p = 0.030). One-month mortality was comparable between groups A and B, and between patients followed-up and lost-to-follow in group A. The culprit lesion in group A was characterized by the association of an aneurysm ≥6 mm in acute KD (100%), lack of significant stenosis (61%) or giant aneurysm (50%) in the long-term (median interval 16 y), and the presence of intravascular ultrasound-derived calcification at ACS (86%).
Conclusions: The present retrospective nationwide questionnaire survey demonstrated nationwide emergence of initial ACS in young adults at low coronary risks, who are followed-up or lost-to-follow after confirmed KD and initial coronary aneurysms ≥6 mm.
Introduction
Kawasaki disease (KD) is a common acute febrile disorder of unknown etiology in young children, which is associated with systemic vasculitis especially in coronary circulation (1, 2). Previously, up to 25% of KD patients develop coronary aneurysms leading to lethal coronary vascular events, which occurs typically early after the acute illness in infants associated with giant aneurysms (1, 2). Recently, this disease is a great concern to cardiologists as well as pediatricians, because grown-up KD patients with coronary sequelae exhibit functional and structural alterations in the coronary arteries (3–7). Such patients, in fact, seem to have a coronary event long after the acute illness in adulthood, which is poorly characterized (8–12).
It has been 50 years since the initial report of KD was published in 1967, with the first English version of the same report in 1974 (13, 14). As of Dec 2010, >272,000 patients were affected by KD in Japan, among whom >117,000 reached adulthood; it is estimated that there are >24,000 young adults with a history of KD in the United States (9, 15). Reports of acute coronary events in young adults after a missed history of KD began to emerge as early as in 1980s after Kawasaki's original publication (8, 10, 16, 17). Recently, case review reports showed that young adults mainly long after missed KD developed acute events mimicking acute coronary syndrome (ACS), which includes acute myocardial infarction (AMI), unstable angina and sudden cardiac arrest (10, 17, 18). However, a significant knowledge gap exists between the onset of acute KD, the initial coronary involvement and the occurrence of KD-associated ACS in adulthood. Limitations in retrospective diagnosis of missed KD and the lack of recognition of coronary involvement even in patients with a confirmed KD diagnosis in early decades, which may have resulted in loss of follow-up, hampered the investigation of this condition (8, 10, 19). In fact, after Kato's study on adult population with a missed history of KD in 1992, no subsequent survey from Japan has been reported to characterize this condition (16).
Recently in Japan, there was a 3.5-fold increase in the adult population with registered KD diagnosis during the acute illness from 1998 to 2010 (15, 20). It is >20 years, as of the year 2000, after the first diagnostic criteria of KD was released for the first nationwide survey of acute KD in 1970 and the first angiographic and ultrasound findings of coronary artery lesions after KD were reported in 1975 and1979, respectively (21–25). Accordingly, a substantial population with registered KD diagnosis and coronary sequelae should have begun to reach adulthood in 2000s in Japan. We therefore conducted a Japanese nationwide survey to characterize ACS, which is emerging in adults with a confirmed (whether followed-up or lost to follow-up) as well as missed history of KD.
Methods
Study Design
This was a retrospective, nationwide hospital-based questionnaire survey of ACS occurring during 2000–2009 in adults (≧ 20 years of age) after a confirmed or missed KD in Japan. This was an official research project, which was endorsed by the Japanese Society of Kawasaki Disease and was conducted by members in the subcommittee on ACS in adult KD patients in the Society. The ethics committee in the Mie University Graduate School of Medicine approved this study. A confirmed diagnosis of KD was defined as the KD diagnosis at the acute illness by medical doctors, which was verified in accordance with medical documents (medical record or medical referral letter) or interview with the patients or family members about KD diagnosis by medical doctors during the acute illness (24, 26, 27). A missed KD diagnosis was defined as the KD diagnosis at ACS or other time points, according to findings in coronary imaging, including coronary aneurysm, ring-like calcification, recanalization, or localized severe intimal thickening, or autopsy findings, not by KD-like symptoms retrospectively obtained from interviews with parents (26, 27). Study setting was described in detail in the Supplemental Material.
Data Collection
Questionnaires were sent to the directors in the department of pediatric cardiology or cardiology in 644 hospitals across Japan during 2010–2011 (28, 29), including (1) all hospitals registered as teaching hospitals by the Japanese Society for Pediatric Cardiology and Cardiac Surgery or to which any councilor of the society belonged, (2) all hospitals, from which any doctor in any scientific meeting reported web-searchable cases that met the criteria for inclusion, and (3) all hospitals, in which ≥200 coronary interventional procedures were performed in 2009. Registry data were collected retrospectively by doctors in charge of the patients in each hospital. Inclusion criteria was an adult patient (≥20 years of age) with acute coronary events consistent with ACS, including acute myocardial infarction, unstable angina and sudden cardiac arrest during January 2000-December 2009 (30, 31), the final diagnosis with ACS made clinically with the use of any investigations, at least including coronary angiography or autopsy (30, 31), and the presence of prospective or retrospective diagnosis of KD by medical doctors. Exclusion criteria included any cases diagnosed finally with effort angina, other cardiovascular disorders including arrhythmia, cases for elective coronary interventions, or acute coronary events without diagnosis using coronary angiography or autopsy. Duplication of the reported cases was avoided by investigators through carefully checking the demography (the birthdate and gender), KD diagnosis at acute illness (age and calendar year) and various clinical information at ACS onset, including age, calendar year, the address of the hospital, angiographic findings and follow-up information. Detailed questionnaire forms were shown in the Supplemental Material.
Statistical Analysis
All statistical analyses were performed with IBM SPSS statistics, version 22. Continuous data are reported as median and interquartile ranges. The significance of any differences among two groups was assessed by the Mann-Whitney U test. Categorical data are expressed as a value or frequency of occurrence. The difference of the proportions of categorical variables among groups was assessed by chi-square analysis. All tests were 2-tailed, and P < 0.05 was considered to indicate statistical significance. YM has full access to all the data in the study and takes responsibility for its integrity and the data analysis.
Results
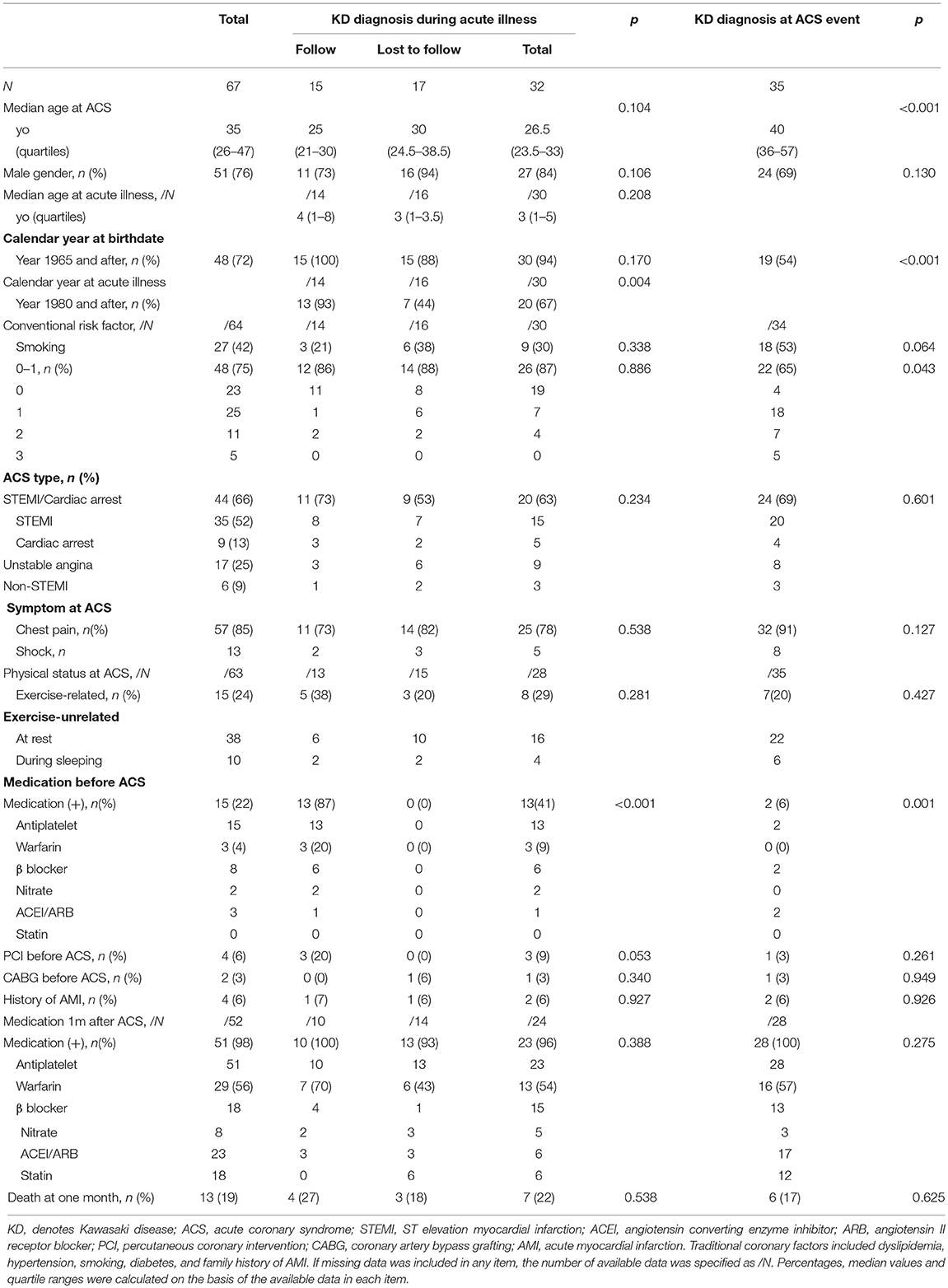
The primary response rate in the present survey was 46.3%. A total of 67 patients (median age 35, male 76%) were recruited (Table 1). A confirmed diagnosis of KD was made by medical doctors in 32 during acute illness (Group A, verified by medical documents in 22; obtained by interview with family members in 10), among which 17 were lost to follow up at ACS. A missed KD diagnosis was made retrospectively in the other 35 patients in accordance with coronary imaging (n = 35) (n = 34 at the registered ACS events, n = 1 at previous AMI in adulthood) and autopsy (n = 0) at ACS (Group B), in which episodes suggestive of acute KD during childhood were also obtained in the parent interviews for 2 patients. Demography and clinical characteristics by the group were shown (Table 1; Figure 1). All the patients, except one Korean and two of unknown ethnicity in group B, were Japanese. Among overall patients, low conventional coronary risks (≤1/6) was noted in 75%, a diagnosis of ST-elevation and myocardial infarction (STEMI) or cardiac arrest in 66%, chest pain in 85%, exercise-related events in 24%, medication before ACS in 22% (warfarin in 4%), and no prior history of AMI in 94%. One-month mortality was 19%. Compared with group B, group A was characterized by younger age at ACS (26.5 vs. 40 yo, p < 0.001), a more recent birthdate (birth in 1965 or after, 94 s. 54%, < 0.001), lower conventional coronary risks (≤1/6 in 87 s. 65%, p = 0.043) (smoking, 30 vs. 53%, p = 0.064) and higher percentage of medication before ACS (41 vs. 6%, p = 0.001). In group A, patients who were followed up before ACS were characterized by a more recent onset (1980 and after) of the acute illness (93 vs. 44% in KD patients lost to follow up, p = 0.004), higher percentage of medication (87 vs. 0%, p < 0.001) before ACS, and a tendency to have a history of percutaneous coronary intervention (PCI) before registered ACS (20 vs. 0%, P = 0.053). One-month mortality was comparable between Groups A and B, and between patients followed-up and lost to follow in group A (Figure 1; Table 1).
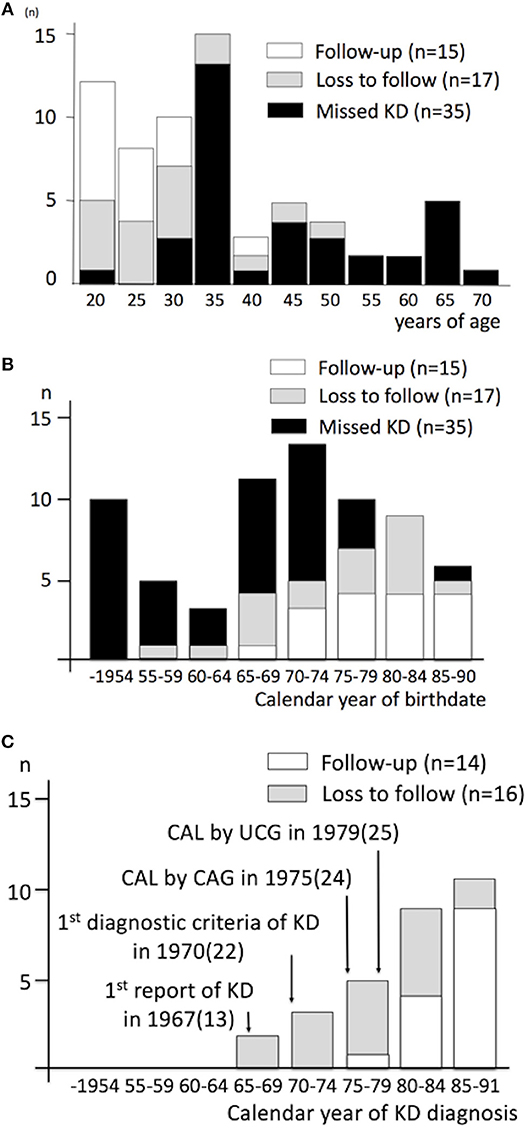
Figure 1. Age at ACS and calendar year of birthdate and KD diagnosis, by the type of KD diagnosis and the follow-up status. (A) Age at acute coronary syndrome, (B) Calendar year of birthdate, (C) Calendar year of KD diagnosis. ACS denotes acute coronary syndrome; KD, Kawasaki disease; CAL, coronary artery lesion; CAG, coronary angiography; UCG, ultrasound cardiography; n, number of patients. Number in parenthesis indicates reference number.
Of the culprit lesions, 67 patients were characterized by demonstrable thrombosis (74%), as well as the presence of persistent giant aneurysms (≥8 mm) (38%) and intravascular ultrasound (IVUS)-derived calcification (92%) (Table 2). In group A, patients who were followed up before ACS represented a higher proportion of persistent giant aneurysms in culprit lesions (69 vs. 29%, p = 0.030) than those lost to follow. In group A, 28% received intravenous immunoglobulin (IVIG) treatment during the acute illness (Table 3). The vessel size of prospective culprit lesion was 6.0–7.9 mm in 36% and ≥8 mm in 64%, and patients with multi-vessel coronary involvement accounted for 71% in the convalescence of acute KD. Prospective culprit lesions were associated with significant stenosis in 39% and giant aneurysm in 50% in the long-term follow-up period (16 y, 13–18 y, after the acute illness).
Discussion
The present Japanese nationwide survey demonstrated that ACS in young adults, with a confirmed as well as a missed history of KD, is emerging in Japan. Patients after confirmed KD usually had initial events long after acute KD; culprit lesions were characterized by large or giant AN in the convalescence of acute KD, the lack of giant aneurysms or severe stenosis in more than a half of patients in the long-term, and IVUS-derived calcification at ACS. Compared with lost-to-follow patients, followed-up patients were more likely to have persistent giant aneurysm in the culprit lesions and had an initial ACS even under conventional medication. Compared with patients after confirmed KD, adults after missed KD also had an initial ACS at higher coronary risks at more advanced age. The present findings may give an insight into the natural history of coronary sequelae as well as the emerging ACS in patients after KD in adulthood.
The present study uniquely characterized young adult population who usually developed an initial ACS long after a confirmed diagnosis of KD and initial coronary sequelae in a nationwide manner in Japan. Recruitment of patients with a confirmed KD diagnosis and coronary sequelae in the convalescence of the acute illness in the present study complied with the chronological order of events in KD research in Japan, including the reports of the first diagnostic criteria of KD and the first angiographic and ultrasound findings of coronary artery lesions after KD (Figure 1C) (21, 22, 24, 25). Present findings in confirmed KD cases may not be confounded by the lack of coronary risks, as in missed KD cases in previous literature (8, 10, 11, 17). Correlation of coronary sequelae in the convalescence of acute KD to the culprit lesion at ACS and the absence of patients with normal coronary arteries at the acute KD in group A underlines the contribution of initial coronary sequelae to this condition. ACS in patients lost to follow or ACS in patients after missed KD were not necessarily associated with persistent giant aneurysm in the present study, in contrast to previous reports in adults (10). Such difference in the former may be related to better recognition of KD patients, which is explained by the emergence of population with KD diagnosis during the acute illness in the present study (18); the difference in the latter may be related to the publication bias in the literature, including inclusion criteria of patients (10).
Initial occurrence of ACS in patients with persistent giant aneurysm who were followed up under medication and/or PCI may indicate that such severe cases might become resistant to the conventional anti-thrombotic therapy in adulthood. The gap between ACS events in followed-up patients with persistent giant aneurysms in the present study and the uneventful outcome in long-term pediatric cohort studies could be explained by the larger background population and the longer time interval until adulthood in the present study, as well as the expertise in KD centers in previous studies (32). Conventional coronary risks or the aging may have additional roles in the development of ACS, because patients after missed history of KD had an initial ACS and more coronary risks at a more advanced age (10). These findings are collectively in line with the functional and/or morphological abnormality in the coronary vessel wall in the development of adult ACS (3–7, 33). Since IVUS-derived calcification in the culprit lesions, a parameter for vessel wall morphology was in fact demonstrated in any subgroup of KD adult patients at ACS, and vessel wall changes culminating in IVUS-derived calcification may play a role in the development of ACS. The potential mechanisms underlying these findings include ongoing remodeling of the coronary arteries mediated by endothelial dysfunction, inflammatory process, myofibroblast proliferation and matrix remodeling of the coronary arteries, which is subjected to progressive calcifications located at the subendothelial surface of any sequelae in the long term (6, 33–35). In addition, potentially superimposed atherogenesis might play a role in a subset of patients with coronary aneurysms long after KD, especially in group B, which requires further research (6, 36, 37).
Implications
Firstly, although the population in which KD-related coronary artery lesion was evaluated during the acute illness in or after 1980 is limited (Figure 1C), the lack of KD patients with normal coronary arteries from the disease onset in the present study may reassure such patients in their 20 s. Secondly, the current AHA and Japanese guidelines recommend anti-platelet therapy for persistent coronary aneurysms or stenosis, but not necessarily for regressed aneurysms (1, 27). Since patients with regressed aneurysms in fact account for a half of the entire KD population with coronary sequelae and may rarely have ACS in early adulthood (2), how to stratify patients at risk is important in an evidence-based approach for this subgroup. Since IVUS-derived coronary calcification was detected in a majority of ACS patients investigated, the present findings suggest that KD patients with regressed aneurysms, especially in case of the original aneurysm ≥6 mm, may be screened by plain MDCT for calcification in adulthood (38). Thirdly, although the presence of persistent giant aneurysms or induced myocardial ischemia has been regarded as an important indicator for poor prognosis in KD, the lack of persistent giant aneurysms or severe stenosis in more than a half of patients in the long-term, in the present study, may uniquely alert cardiologists to the risk of ACS in adulthood (1, 9, 27, 39). Fourthly, since group B is characterized by increased conventional coronary risks and a tendency for an increase in smoking at an advanced age, it may be reasonable to recommend life style modification in KD patients in adulthood (10). Together with the vessel wall alterations in coronary arteries in the long term and initial ACS in followed-up patients under conventional medication, any additional compounds with anti-inflammatory property, such as statins, may be of theoretical benefit in KD patients who are at risk in adulthood (40).
Limitations
Firstly, there are issues (including recall bias and potential duplication of patients) related to the retrospective nature of the study, as well as issues of a low response rate (46.3%) and missing data, especially during the acute illness and convalescence in this nationwide questionnaire survey. Prospective long-term registry from the KD onset would be required to uncover the natural history of this disorder in adulthood. However, considering the rarity of the events, the long observation period required, and the issue of loss-to-follow in adult KD, a nationwide retrospective survey as in the present study may play a role in characterizing this condition. Secondly, the proportion of regressed aneurysms in culprit lesions at ACS might be undervalued in the loss-to-follow patients after KD or in patients after missed KD in adulthood. A cohort of adult KD population, if any, including patients with regressed aneurysms will be warranted in this regard. Thirdly, KD diagnosis from the coronary imaging at ACS is uncertain in group B and could be biased by the presence of giant aneurysm or the lack of multiple coronary risks. However, this group in this study may be of clinical relevance, because this group exhibits characteristics consistent with the other subgroup: this group and lost-to-follow patients in group A had a reasonably similar proportion of persistent giant aneurysm at ACS; this group is still at more coronary risks than group A. Fourthly, as with all retrospective questionnaire surveys, the integrity and validity of the data are potential limitations of our study.
Conclusions
The present Japanese retrospective nationwide questionnaire survey uniquely characterized emerging ACS in young adults with a confirmed as well as missed diagnosis of KD, which complies with the chronology of KD research for half a century in Japan. The present findings may alert pediatricians and general practitioners to the risk of ACS in adults long after the acute illness and the transition issues of KD, and warrant a prospective registry study of adults with a confirmed KD diagnosis and the information of initial coronary sequelae.
Data Availability
The datasets for this manuscript are not publicly available because it is not approved by the ethics committee in Mie University Graduate School of Medicine. Requests to access the datasets should be directed toeW1pdGFuaUBjbGluLm1lZGljLm1pZS11LmFjLmpw.
Ethics Statement
The study conformed to the principles of the Helsinki Declaration, and the study protocol was approved by the Ethics Committee of the Mie University Graduate School of Medicine. The requirement for individual informed consent was waived.
Author Contributions
YM, HK, KH, and HY design, methodology, investigation, supervision, funding acquisition, data curation, formal analysis, resources, writing, final approval of the manuscript. ET design, methodology, investigation, supervision, acquisition, data curation, formal analysis, resources, writing, final approval of the manuscript. TH, SO, KT, MA, ToK, FI, and HY design, methodology, investigation, supervision, data curation, formal analysis, resources, writing, final approval of the manuscript. MF design, methodology, investigation, data curation, resources, writing, final approval of the manuscript. FS design, methodology, investigation, acquisition, data curation, formal analysis, resources, writing, final approval of the manuscript. YN design, methodology, investigation, supervision, data curation, formal analysis, writing, final approval of the manuscript. MM, MK, KS, HO, HS, TaK, KW, MS, and RT design, methodology, investigation, data curation, formal analysis, resources, writing, final approval of the manuscript.
Funding
This work is supported in part by Research grant for child health and development 24–14 (Development of diagnosis and treatment for IVIG-resistant Kawasaki disease), Ministry of Health, Labor and Welfare, Tokyo, Japan (HK); by Grants-in-Aid for Scientific Research, JSPS KAKENHI Grant 15K09908, The Ministry of Education, Culture, Sports, Science and Technology, Tokyo, Japan (KS).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the participating physicians for graciously enrolling their patients.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2019.00275/full#supplementary-material
References
1. Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on rheumatic fever, endocarditis and kawasaki disease, council on cardiovascular disease in the young, American heart association. Circulation. (2004) 110:2747–71. doi: 10.1161/01.CIR.0000145143.19711.78
2. Newburger JW, Takahashi M, Burns JC. Kawasaki disease. J Am Coll Cardiol. (2016) 67:1738–49. doi: 10.1016/j.jacc.2015.12.073
3. Mitani Y, Okuda Y, Shimpo H, Uchida F, Hamanaka K, Aoki K, et al. Impaired endothelial function in epicardial coronary arteries after Kawasaki disease. Circulation. (1997) 96:454–61.
4. Yamakawa R, Ishii M, Sugimura T, Akagi T, Eto G, Iemura M, et al. Coronary endothelial dysfunction after Kawasaki disease: evaluation by intracoronary injection of acetylcholine. J Am Coll Cardiol. (1998) 31:1074–80. doi: 10.1016/S0735-1097(98)00033-3
5. Mitani Y, Sawada H, Hayakawa H, Aoki K, Ohashi H, Matsumura M, et al. Elevated levels of high-sensitivity C-reactive protein and serum amyloid-A late after Kawasaki disease: association between inflammation and late coronary sequelae in Kawasaki disease. Circulation. (2005) 111:38–43. doi: 10.1161/01.CIR.0000151311.38708.29
6. Mitani Y, Ohashi H, Sawada H, Ikeyama Y, Hayakawa H, Takabayashi S, et al. In vivo plaque composition and morphology in coronary artery lesions in adolescents and young adults long after Kawasaki disease: a virtual histology-intravascular ultrasound study. Circulation. (2009) 119:2829–36. doi: 10.1161/CIRCULATIONAHA.108.818609
7. Suda K, Tahara N, Kudo Y, Yoshimoto H, Iemura M, Ueno T, et al. Persistent coronary arterial inflammation in a patient long after the onset of Kawasaki disease. Int J Cardiol. (2012) 154:193–4. doi: 10.1016/j.ijcard.2011.10.078
8. Burns JC, Shike H, Gordon JB, Malhotra A, Schoenwetter M, Kawasaki T. Sequelae of Kawasaki disease in adolescents and young adults. J Am Coll Cardiol. (1996) 28:253–7. doi: 10.1016/0735-1097(96)00099-X
9. Gordon JB, Kahn AM, Burns JC. When children with Kawasaki disease grow up: myocardial and vascular complications in adulthood. J Am Coll Cardiol. (2009) 54:1911–20. doi: 10.1016/j.jacc.2009.04.102
10. Tsuda E, Abe T, Tamaki W. Acute coronary syndrome in adult patients with coronary artery lesions caused by Kawasaki disease: review of case reports. Cardiol Young. (2011) 21:74–82. doi: 10.1017/S1047951110001502
11. Daniels LB, Tjajadi MS, Walford HH, Jimenez-Fernandez S, Trofimenko V, Fick DB Jr, et al. Prevalence of Kawasaki disease in young adults with suspected myocardial ischemia. Circulation. (2012) 125:2447–53. doi: 10.1161/CIRCULATIONAHA.111.082107
12. Rizk SR, El Said G, Daniels LB, Burns JC, El Said H, Sorour KA, et al. Acute myocardial ischemia in adults secondary to missed Kawasaki disease in childhood. Am J Cardiol. (2015) 115:423–7. doi: 10.1016/j.amjcard.2014.11.024
13. Kawasaki T. Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children. Arerugi. (1967) 16:178–222.
14. Kawasaki T, Kosaki F, Okawa S, Shigematsu I, Yanagawa H. A new infantile acute febrile mucocutaneous lymph node syndrome (MLNS) prevailing in Japan. Pediatrics. (1974) 54:271–6.
15. Nakamura YYM. Epidemiology of fatal cases with Kawasaki disease. Cardioangiography. (2011) 69:412–20.
16. Kato H, Inoue O, Kawasaki T, Fujiwara H, Watanabe T, Toshima H. Adult coronary artery disease probably due to childhood Kawasaki disease. Lancet. (1992) 340:1127–9. doi: 10.1016/0140-6736(92)93152-D
17. Daniels LB, Gordon JB, Burns JC. Kawasaki disease: late cardiovascular sequelae. Curr Opin Cardiol. (2012) 27:572–7. doi: 10.1097/HCO.0b013e3283588f06
18. Negoro N, Nariyama J, Nakagawa A, Katayama H, Okabe T, Hazui H, et al. Successful catheter interventional therapy for acute coronary syndrome secondary to kawasaki disease in young adults. Circ J. (2003) 67:362–5. doi: 10.1253/circj.67.362
19. Angelini P, Monge J. Newer concepts regarding adults with coronary artery aneurysms: are they all Kawasaki? Does it make a difference? Circulation. (2012) 125:3076–8. doi: 10.1161/CIRCULATIONAHA.112.106880
20. Yanagawa H. Editorial comments: two adults of acute myocardial infarction after Kawasaki disease. Shinzo. (1999) 31:422–3.
21. Kato H, Koike S, Yamamoto M, Ito Y, Yano E. Coronary aneurysms in infants and young children with acute febrile mucocutaneous lymph node syndrome. J Pediatr. (1975) 86:892–8. doi: 10.1016/S0022-3476(75)80220-4
22. Yoshikawa J, Yanagihara K, Owaki T, Kato H, Takagi Y, Okumachi F, et al. Cross-sectional echocardiographic diagnosis of coronary artery aneurysms in patients with the mucocutaneous lymph node syndrome. Circulation. (1979) 59:133–9. doi: 10.1161/01.CIR.59.1.133
23. Nakamura Y, Yanagawa H, Kawasaki T. Mortality among children with Kawasaki disease in Japan. N Engl J Med. (1992) 326:1246–9. doi: 10.1056/NEJM199205073261903
24. Ayusawa M, Sonobe T, Uemura S, Ogawa S, Nakamura Y, Kiyosawa N, et al. Revision of diagnostic guidelines for Kawasaki disease (the 5th revised edition). Pediatr Int. (2005) 47:232–4. doi: 10.1111/j.1442-200x.2005.02033.x
26. Ogawa S. Overview of the JCS 2008 guidelines for diagnosis and management of cardiovascular sequelae in Kawasaki disease. Nihon Rinsho. (2011) 69(Suppl. 9):529–35.
27. Group JCSJW. Guidelines for diagnosis and management of cardiovascular sequelae in Kawasaki disease (JCS 2013). Digest version Circ J. (2014) 78:2521–62. doi: 10.1253/circj.CJ-66-0096
28. Jspccs. Home page, Japanese Society of Pediatric Cardiology and Cardiac Surgery. Available online at: http://jspccs.jp/english/ (accessed March 1, 2019).
29. Therapeutics J.a.O.C.I.A. Homepage, Japanese Association of Cardiovascular Interventions and Therapeutics. Available online at: http://www.cvit.jp/ (accessed March 1, 2019).
30. Krumholz HM, Anderson JL, Bachelder BL, Fesmire FM, Fihn SD, Foody JM, et al. ACC/AHA 2008 performance measures for adults with ST-elevation and non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to develop performance measures for ST-elevation and non-ST-elevation myocardial infarction): developed in collaboration with the American Academy of Family Physicians and the American College of Emergency Physicians: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, Society for Cardiovascular Angiography and Interventions, and Society of Hospital Medicine. Circulation. (2008) 118:2596–648. doi: 10.1161/CIRCULATIONAHA.108.191099
31. Fuster V, Kovacic JC. Acute coronary syndromes: pathology, diagnosis, genetics, prevention, and treatment. Circ Res. (2014) 114:1847–51. doi: 10.1161/CIRCRESAHA.114.302806
32. Suda K, Iemura M, Nishiono H, Teramachi Y, Koteda Y, Kishimoto S, et al. Long-term prognosis of patients with Kawasaki disease complicated by giant coronary aneurysms: a single-institution experience. Circulation. (2011) 123:1836–42. doi: 10.1161/CIRCULATIONAHA.110.978213
33. Sugimura T, Kato H, Inoue O, Fukuda T, Sato N, Ishii M, et al. Intravascular ultrasound of coronary arteries in children. Assessment of the wall morphology and the lumen after Kawasaki disease. Circulation. (1994) 89:258–65. doi: 10.1161/01.CIR.89.1.258
34. Suzuki A, Miyagawa-Tomita S, Komatsu K, Nishikawa T, Sakomura Y, Horie T, et al. Active remodeling of the coronary arterial lesions in the late phase of Kawasaki disease: immunohistochemical study. Circulation. (2000) 101:2935–41. doi: 10.1161/01.CIR.101.25.2935
35. Orenstein JM, Shulman ST, Fox LM, Baker SC, Takahashi M, Bhatti TR, et al. Three linked vasculopathic processes characterize Kawasaki disease: a light and transmission electron microscopic study. PLoS ONE. (2012) 7:e38998. doi: 10.1371/journal.pone.0038998
36. Takahashi K, Oharaseki T, Naoe S. Pathological study of postcoronary arteritis in adolescents and young adults: with reference to the relationship between sequelae of Kawasaki disease and atherosclerosis. Pediatr Cardiol. (2001) 22:138–42. doi: 10.1007/s002460010180
37. Shiraishi J, Yashige M, Hyogo M, Shima T, Sawada T, Kohno Y. Lipid-rich plaque in possible coronary sequelae of Kawasaki disease detected by optical frequency domain imaging. Cardiovasc Interv Ther. (2015) 30:367–71. doi: 10.1007/s12928-014-0305-1
38. Tsujii N, Tsuda E, Kanzaki S, Ishizuka J, Nakashima K, Kurosaki K. Late wall thickening and calcification in patients after Kawasaki disease. J Pediatr. (2016) 181:167–71.e2. doi: 10.1016/j.jpeds.2016.10.026
39. Dajani AS, Taubert KA, Takahashi M, Bierman FZ, Freed MD, Ferrieri P, et al. Guidelines for long-term management of patients with Kawasaki disease. Report from the committee on rheumatic fever, endocarditis, and kawasaki disease, council on cardiovascular disease in the young, American heart association. Circulation. (1994) 89:916–22. doi: 10.1161/01.CIR.89.2.916
40. Suda K, Tahara N, Honda A, Yoshimoto H, Kishimoto S, Kudo Y, et al. Statin reduces persistent coronary arterial inflammation evaluated by serial (1)(8)fluorodeoxyglucose positron emission tomography imaging long after Kawasaki disease. Int J Cardiol. (2015) 179:61–2. doi: 10.1016/j.ijcard.2014.10.057
Keywords: Kawasaki disease, coronary aneurysm, acute coronary syndrome, transition, long-term issue
Citation: Mitani Y, Tsuda E, Kato H, Higaki T, Fujiwara M, Ogawa S, Satoh F, Nakamura Y, Takahashi K, Ayusawa M, Kobayashi T, Ichida F, Matsushima M, Kamada M, Suda K, Ohashi H, Sawada H, Komatsu T, Waki K, Shinoda M, Tsunoda R, Yokoi H and Hamaoka K (2019) Emergence and Characterization of Acute Coronary Syndrome in Adults After Confirmed or Missed History of Kawasaki Disease in Japan: A Japanese Nationwide Survey. Front. Pediatr. 7:275. doi: 10.3389/fped.2019.00275
Received: 22 March 2019; Accepted: 17 June 2019;
Published: 09 July 2019.
Edited by:
Umberto Morbiducci, Polytechnic University of Turin, ItalyReviewed by:
Fabrizio D'Ascenzo, San Giovanni Battista Molinette, ItalyZiyad M. Hijazi, Rush University, United States
Copyright © 2019 Mitani, Tsuda, Kato, Higaki, Fujiwara, Ogawa, Satoh, Nakamura, Takahashi, Ayusawa, Kobayashi, Ichida, Matsushima, Kamada, Suda, Ohashi, Sawada, Komatsu, Waki, Shinoda, Tsunoda, Yokoi and Hamaoka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yoshihide Mitani, eW1pdGFuaUBjbGluLm1lZGljLm1pZS11LmFjLmpw
 Yoshihide Mitani
Yoshihide Mitani Etsuko Tsuda2
Etsuko Tsuda2 Yoshikazu Nakamura
Yoshikazu Nakamura Mamoru Ayusawa
Mamoru Ayusawa Masahiro Kamada
Masahiro Kamada Hiroyuki Ohashi
Hiroyuki Ohashi Takaaki Komatsu
Takaaki Komatsu