- 1National Institute on Drug Dependence and Beijing Key Laboratory of Drug Dependence, Peking University, Beijing, China
- 2School of Public Health, Peking University, Beijing, China
- 3National Drug and Alcohol Research Centre, University of New South Wales, Sydney, NSW, Australia
- 4Key Laboratory of Mental Health and Peking University Sixth Hospital, National Clinical Research Center for Mental Disorders, Institute of Mental Health, Peking University, Beijing, China
- 5Peking-Tsinghua Center for Life Sciences and IDG/McGovern Institute for Brain Research, Peking University, Beijing, China
Objective: To explore the epidemiological characteristics and the risk factors for methamphetamine (MA)—associated psychotic symptoms among MA users in China.
Methods: A cross-sectional study was conducted between April, 2012 and October, 2015 among individuals for whom MA was the principal drug of use in a Compulsory Drug Detoxification Center in Beijing, Guangdong Province. Demographic, drug use and psychological characteristics were examined using a specifically-designed questionnaire, the Positive and Negative Syndrome Scale, Barratt Impulsive Scale, Hamilton Anxiety Scale and Beck Depression Inventory. Logistic regression was performed to explore the risk factors for MA-associated psychotic symptoms.
Results: A total of 1685 participants were included. Participants were predominantly aged 30 or above, unemployed, and were unmarried Han Chinese men, with limited education. The duration of MA use was more than 3 months in 72.3%. 47.8% reported that the dose of MA use was ≥ 0.2 g per occasion of use. 11.5% had used two or more synthetic drugs. The prevalence of MA-associated psychotic symptoms was 17.0% among MA users during periods of abstinence. Multiple logistic regression analyses showed that a higher dose (≥0.2 g per time), a longer duration of MA use (>3 months) a history of heroin use and a history of tobacco use were associated with MA-associated psychotic symptoms, with adjusted odds ratios (ORs) of 1.96 (95% confidence interval [CI]: 1.40–2.76), 1.98 (95% CI: 1.33–2.96) and 2.45 (95% CI: 1.67–3.60), 1.78 (95% CI: 1.27–2.49) respectively. MA-associated psychotic symptoms were less common among married/cohabitating than unmarried (OR = 0.56; 95% CI: 0.39–0.81), and unemployed than employed (OR = 0.65; 95% CI: 0.47–0.92) individuals. MA users with anxiety and depression symptoms had significantly greater risk for MA-associated psychotic symptoms by 9.70 (6.92–13.59) and 1.90 (1.36–2.65) times respectively. Individuals with higher impulsivity were more likely to have MA-associated psychotic symptoms than those with lower (OR = 2.19; CI:1.50–3.20).
Conclusion: MA-associated psychotic symptoms occurred frequently among MA users in China. The efforts that facilitate drug users' attempts to reduce MA use, abstain from poly-drug use, and control associated psychiatric symptoms and impulsivity should be supported because of their potential contribution to MA-associated psychotic symptoms in this population.
Introduction
Amphetamine-type stimulants (ATS) comprising predominantly methamphetamine (MA) are the second most commonly used illicit drug globally after cannabis. Their use is associated with health problems globally, and particularly in East and South-East Asia (1, 2). The United Nations Office on Drugs and Crime reported that an estimated 37 million individuals have used amphetamines in the past year and that MA was the most consumed drug in China (3). Data from the Annual Report on Drug Control in China indicated that the number of registered synthetic drug users exceeded users of traditional drugs such as heroin. At the end of 2016, the number of registered synthetic drugs users reached 1.52 million, accounting for 60.5% of all drug users (4–6). The use of MA contributes to a wide range of physical and mental health disorders.
It is well established that MA can induce both prolonged and transient psychosis, which is characterized typically by persecutory delusions and auditory hallucinations, but also delusions of reference, visual hallucinations, and thought broadcasting (7–9). MA-associated psychotic symptoms give rise to a variety of adverse consequences that are considerable public health concerns, including negatively impacting on the individual's quality of life and increasing the burden on their family and society (10, 11). Studies conducted internationally provide evidence that MA-associated psychotic symptoms increase risk for suicidality (10–12).
The increasing use of MA and associated harms globally raise questions regarding the prevalence of MA-associated psychotic symptoms in MA users. The reported prevalence of psychotic symptoms among MA users varies widely in different countries, ranging between 13 and 46% (9, 13–18). A Chinese study reported 17.4% prevalence of psychotic symptoms in MA users from detoxification centers (19). Studies have shown that earlier, longer and heavier use of MA was associated with increased risk for MA-associated psychotic symptoms (19–21). MA dependence, too, may increase the risk for MA-associated psychotic symptoms (9, 13–16). There is also an association between increased prevalence of co-occurring anxiety and depressive symptoms in individuals with MA-related psychotic symptoms (22, 23). Most studies to date have been conducted in developed countries, however, and evidence from developing country populations is scant and interpretation limited by small sample size. This study aimed to examine the prevalence of psychotic symptoms among MA users in China, and to systematically analyze the risk factors for MA-associated psychotic symptoms among Chinese MA users.
Materials and Methods
Participants
A cross-sectional study of MA–associated psychotic symptoms and risk behavior among MA users was conducted in compulsory drug detoxification centers in Beijing and Guangdong Province, China. MA users who only or primarily used MA in the past year (prior to enrollment) were recruited from April, 2012 to October, 2015 by convenient sampling method. Inclusion criteria were: age 18 years or above; MA as primary drug ever used, and positive urine test for MA at time of entry to the treatment center. Subjects were excluded if they had significant physical illnesses, such as cerebrovascular disease, cardiovascular disease, or stroke which had been diagnosed by doctors previously. The participants who declined to participate or otherwise did not participate were not disadvantaged in any way. Written informed consent was obtained from all the study participants. The study was approved by the Institutional Ethics Board of Peking University. A total of 1685 MA users who reported that MA was their primary drug ever used and completed the psychotic symptoms assessment were included in the present study.
Measures
Sociodemographic and Drug Use Questionnaire
A self-designed structured questionnaire that collected information on demographic characteristics and drug use history was administered in face-to-face interviews by trained interviewers. Demographic variables included geographical area of survey, age, gender, ethnicity, employment, education, and marital status. Information about drug use included: synthetic drug ever used, other substance ever used, two or more synthetic drugs ever used, main route, source, cause, sites of MA administration, dose, frequency and duration of MA use, concurrent use of other drugs and MA dependence in the past year before entering the treatment center. MA dependence was defined as present if there were two or more of the following symptoms: craving, tolerance, withdrawal, out-of-control drug use, preoccupation with drug, and use despite significant impairment (based on the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (24).
The Positive and Negative Syndrome Scale (PANSS)
The Positive and Negative Syndrome Scale (PANSS) was used to assess psychotic symptoms (25). The 30-item scale assesses the severity of positive syndrome (7 items), negative syndrome (7 items), and general psychopathology (16 items). Each item rated on a 7-point scale (1=absent, 2=minimal, 3=mild, 4=moderate, 5=moderate severe, 6=severe, and 7=extreme), with cumulative scores ranging from 30 to 210. Clinically significant psychotic symptoms corresponded to a PANSS total score of 58 and above (26). The validity and reliability of PANSS (Chinese version) both meet the requirements of psychometrics for assessing psychotic symptoms in Chinese patients, with internal consistency reliability of 0.87 (27).
The Beck Depression Inventory (BDI)
Symptoms of depression were measured using the short 13-item Beck Depression Inventory (BDI). Each item is scored from 0 to 3 with total scores ranging from 0 to 39. A score of ≥8 was classified as indicative of having depressive symptoms (28). Previous research demonstrates that the BDI can be reliably used to assess depression symptoms in Chinese populations (29).
The Hamilton Anxiety Scale (HAMA)
Anxiety symptoms were measured using the Hamilton Anxiety Scale (HAMA). The scale comprises 14 items each rated from 0 to 4, with cumulative scores ranging from 0 to 56. A cut-off value of ≥14 was used to define presence of anxiety symptoms (30). HAMA has been demonstrated to have good reliability and validity in Chinese individuals (31).
The Barratt Impulsive Scale (BIS-11)
The Barratt Impulsive Scale (BIS-11) was used to measure impulsiveness and comprises 30 items (32). In the adapted Chinese version, each of the 30 items is scored from 1 to 5, with total scores ranging from 30 to 150 (33). The higher the total questionnaire score, the higher the individual's level of impulsiveness (34). Reliability and validity in Chinese populations are acceptable (33).
Statistical Analysis
EpiData software (Odense, Denmark) was used to verify consistency of the double-entered data. Descriptive analysis was conducted for the demographic and drug use characteristics, psychotic symptoms, depressive symptoms, and anxiety symptoms of the study participants with the estimated means and proportions. Univariate logistic regression was used to examine the association of variables with risk for MA-associated psychotic symptoms. Multiple logistic regression was conducted using a stepwise backward sequence. Significant variables from univariate analysis were included for multiple logistic regression analysis. All the statistical tests were completed using Stata version 13.1 (35). Statistical significance was set at 0.05 in two-sided tests for all analyses.
Results
Sample Characteristics and Pattern of Drug Use
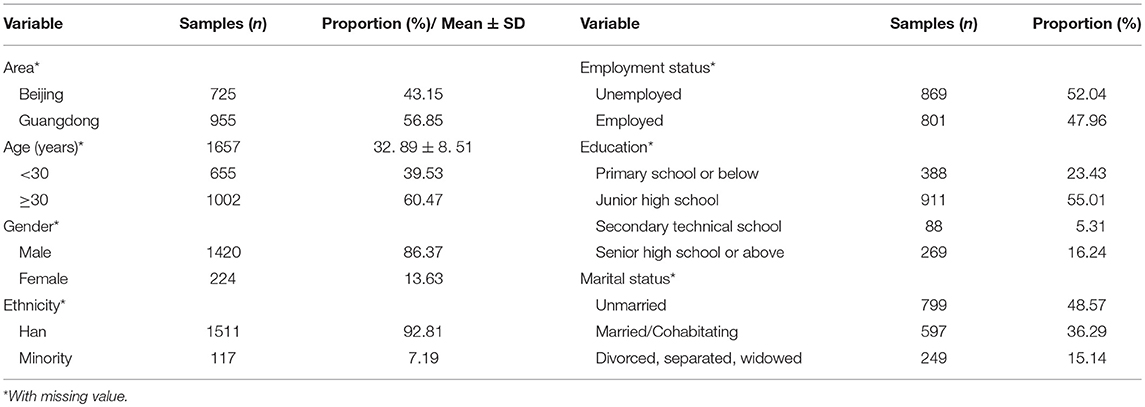
1685 MA users participated in the study, from Beijing (43.2%) and Guangdong (56.9%) Province, China. Tables 1, 2 show the demographic and drug use characteristics of the subjects respectively. Age ranged from 18 to 57 years (mean, 32.9 years) and 655 participants (39.5%) were < 30 years old. The majority were male (86.4%), of Han ethnicity (92.8%), 52.0% were unemployed, and 48.6% unmarried. The level of education was mainly junior high school or below (78.4%).
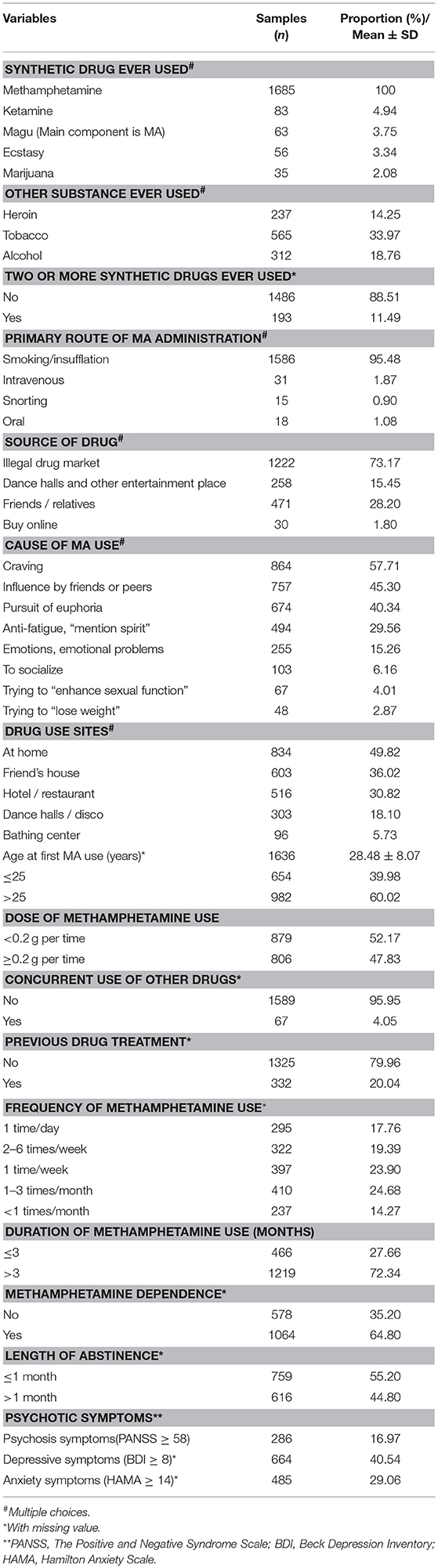
Among the 1685 MA users, 14.3% had a history of heroin use, 18.8 and 34.0% reported alcohol use and cigarette smoking respectively. The majority (95.5%) used MA by smoking or insufflation. Craving (57.7%), influence by friends or peers (45.3%), and pursuit of euphoria (40.3%) were the main reasons given for drug use. The average age at onset of MA use was 28.5 years, 40.0% of the MA users' age at first MA use was ≤ 25 years. 72.3% had used MA for more than 3 months, 61.1% had used MA every week. 64.8% were MA-dependent. 55.2% of MA users were abstinent for 1 month or less. Almost half (47.8%) had used ≥0.2 g per time. 20.0% had received prior treatment for drug use.
Prevalence and Profiles of Psychotic and Affective Symptoms
286 (17.0%) had MA-associated psychotic symptoms. Table 3 also shows the proportion to which each item psychotic symptom on the PANSS was rated as present among MA users who met criteria for psychosis (PANSS> = 58). The top three psychotic symptoms were somatic concern (G1, 36.7%), guilt feelings (G3, 36.7%), and excitement (P4, 33.9%), respectively. The other three noteworthy psychotic symptoms were hallucinations (P3, 27.3%), suspiciousness/persecution (P6, 26.6%), and delusions (P1, 17.8%).
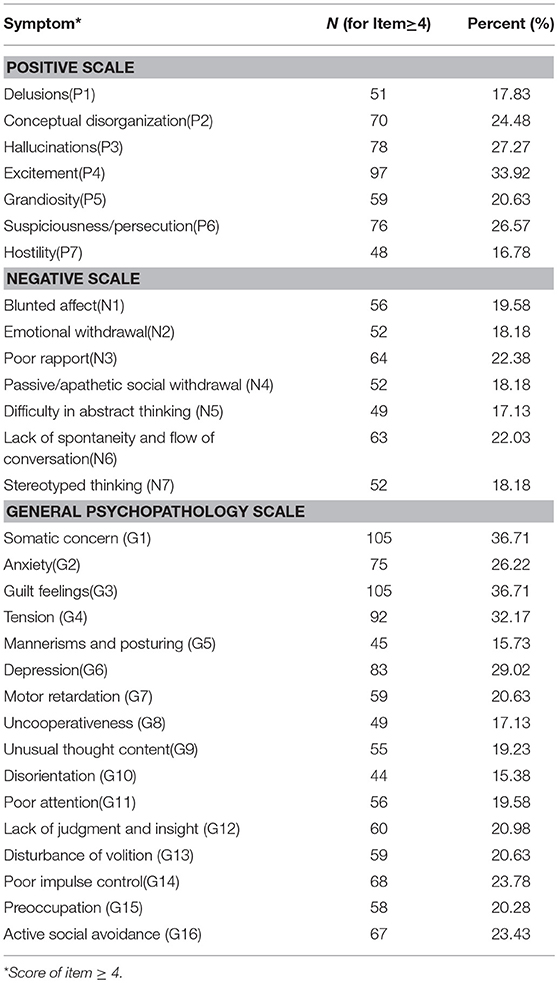
Table 3. Prevalence of PANSS symptoms reported by methamphetamine users who met criteria for psychosis (PANSS > = 58).
Predictors of MA-Associated Psychotic Symptoms
The multiple logistic regression (Table 4) showed that a higher dose (≥0.2 g per time), and a longer duration of MA use (>3 months) were both associated with increased odds of psychotic symptoms: adjusted odds ratio (OR) = 1.96 (95% confidence interval [CI]: 1.40–2.76), and 1.98 (95% CI: 1.33–2.96), respectively. Subjects who reported a history of heroin or tobacco use had higher odds of MA—associated psychotic symptoms than those without (OR = 2.45, 95% CI: 1.67–3.60; OR = 1.78, 95% CI: 1.27–2.49, respectively). Being married/cohabitating, or unemployed had lower odds of MA-associated psychotic symptoms: OR = 0.56 (95% CI: 0.39–0.81) and 0.65 (95% CI: 0.47–0.92), respectively. MA users with anxiety symptoms or depression symptoms had significantly increased odds of having MA-associated psychotic symptoms by 9.70 (95% CI: 6.92–13.59) and 1.90 (95% CI: 1.36–2.65) times. Based on the average score of BIS-11 (75.79 ± 21.24), we divided the subjects into high impulsivity group (BIS-11>75) and low impulsivity group (BIS-11≤75). Individuals with high impulsivity were more likely to have MA-associated psychotic symptoms than those with low impulsivity: OR = 2.19 (95% CI: 1.50–3.20).
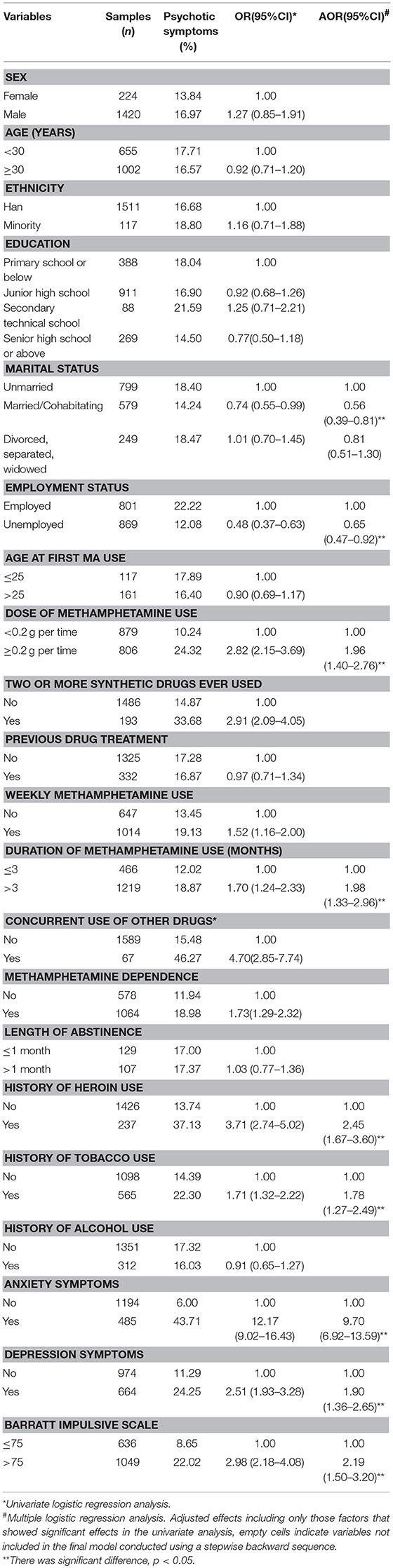
Table 4. Logistic regression analysis of the risk factors for psychotic symptoms (PANSS total score ≥ 58) in methamphetamine users.
Discussion
The present study found that MA-associated psychotic symptoms were common (17%) among abstinent MA users in detention centers in Beijing and Guangdong Province, China. Factors that increased risk for MA-associated psychotic symptoms included both longer duration and a higher typical dose of MA use. Other factors included a history of heroin or tobacco use, comorbid depression or anxiety symptoms, and higher impulsivity. Though this study cannot demonstrate a causal link, important next steps include examination of the effects of comprehensive interventions to assist in reducing the use of MA, actively treating depression and anxiety comorbidity, and relieving impulsivity through psychological and behavioral interventions in reducing the risk for MA-associated psychotic symptoms in this population.
The prevalence of MA-associated psychotic symptoms reported here is similar to the rate reported in an Australian study, which excluded MA users with pre-morbid psychotic symptoms (17.0% vs. 18%) (17). Prior research showed that the risk of experiencing psychotic symptoms in MA users who were abstinent ranged from 12.7 to 26.4% (21). The nature of psychotic symptoms has been remarkably consistent across previous studies, with high frequency of hallucinations, delusions of persecution, thought broadcasting, and suicidal ideation (7, 9, 20, 21).
Regular use of a higher dose of MA was associated with higher risk for MA-associated psychotic symptoms, consistent with earlier studies that indicated that heavier MA users are at higher risk of psychosis (17, 36–38). Similarly, MA users with a longer duration of drug use were more likely to have MA-associated psychotic symptoms, concordant with findings from a longitudinal prospective cohort study that showed a strong dose-response effect between number of days of MA use and psychotic symptoms (20). A similar of a dose-response relationship between the duration of MA use and risk of psychiatric symptoms was observed in our previous study (19). Higher dose and longer duration of MA use represent greater severity of exposure to MA. These findings suggest that reducing MA use may be helpful to reduce the risk of psychosis among this population. Our study found that history of heroin and tobacco use each is associated with higher risk for occurring MA-associated psychotic symptoms. Although heroin use is rarely reported as a risk factor in MA-associated psychotic symptoms, previous research has demonstrated that mental health among heroin users is poorer than in the general population (39). Smoking as a risk factor for MA-associated psychotic symptoms has been reported by a Chinese study conducted in a Compulsory Drug Detoxification Center (19).
Being of married or cohabitating status was associated with reduced risk for psychotic symptoms, findings which concur with our previous study. It may be that being in a longterm relationship is a protective factor against MA-associated psychotic symptoms. Alternatively, it may be that those who can sustain a relationship have different characteristics that render them less likely to be vulnerable to the development of psychotic symptoms. Being unemployed was also a protective factor but this finding was contrary to previous research results (40). Future study is necessary to further examine this issue. High prevalence of anxiety symptoms and depressive symptoms were reported in the study, and users with comorbid anxiety symptoms or depressive symptoms were more likely to experience MA-associated psychotic symptoms than users without, consistent with previous studies (19, 38).
MA users with high impulsivity were more likely to experience MA-associated psychotic symptoms than those with low impulsivity. Impulsivity has been shown previously to be associated with earlier initiation of substance use and greater MA consumption (41, 42). MA use itself is associated with heightened impulsivity in animal models (43). Impulsivity is a multidimensional construct, and studies have shown that impulsivity may be related to damage to dopamine and serotonin axons, dopamine D2/D3 receptor and polymorphism of COMT (Catechol-O- methyltransferase), DAT (Dopamine transporter), and DRD4 (Dopamine D4 receptor) genes (44–46), which may be implicated in the risk for MA-associated psychotic symptoms (9, 47–50). Further research of the relationship between MA-associated psychotic symptoms and impulsivity is needed. The association with impulsivity is important when considering interventions aimed at the prevention and treatment of MA-associated psychotic symptoms: presence of impulsivity is likely to indicate additional risk for psychosis, but its presence is likely to be associated with poorer adherence to treatment and irregular engagement and help-seeking.
Previous studies have reported that psychotic symptoms largely resolved within a week of cessation of MA among MA-dependent participants (51), but the data from this study did not support those findings. The reason may be that the participants of this study were recruited from the Compulsory Drug Detoxification Center where all individuals entered after staying in detention centers for a few days and thus had longer abstinence periods than participants recruited in other study designs. We did not find a statistically significant association between the age of onset of MA use and MA-associated psychotic symptoms. Evidence on onset of MA use and risk for psychotic symptoms varies across studies, and further research is required (52, 53). Interestingly, the symptoms and some risk factors of MA-associated psychotic symptoms are similar to those observed in cocaine-induced psychosis (54, 55). Both MA and cocaine belong to the psychostimulants class, and are highly related, so the findings in this study possibly could be extrapolated to other psychostimulant-related psychoses.
This study included a large sample that was drawn from compulsory drug detoxification centers in Beijing and Guangdong Province, China. The extent to which the findings reported here are generalizable to users of MA within the community is unclear. The present study relied on retrospective self-reports of drug use history. This may have resulted in recall bias. The assessment of psychiatric symptoms was not based on DSM-based structured interviews, which may have affected the accuracy of the prevalence of psychotic symptoms. We did not collect information on psychiatric histories, particularly past history of psychotic illness, which may be an important confounding factor in the relationship between MA use and psychotic symptoms (17, 56). In addition, other potentially relevant risk factors such as family history of psychosis or psychiatric illness, personality traits, and adverse childhood experiences were not assessed in this study. In spite of these limitations, we reported the prevalence of and risk factors for MA-associated psychotic symptoms among MA users in a large population in China. The finding that higher impulsivity is associated with greater risk for psychotic symptoms is novel and warrants further research. Given the widespread use of methamphetamine in China in recent years, greater awareness is needed about the potential effect of this drug on mental health issues. There is a need to provide integrated care for patients who suffer from substance use disorders and psychiatric disorders to enable better prevention and treatment.
Conclusion
This study found that MA-associated psychotic symptoms were common in MA users, and identified that higher dose and longer duration of MA use, history of heroin or tobacco use, depression or anxiety symptoms, and higher impulsivity were each associated with higher risk for psychotic symptoms. These findings highlight the need to develop prevention and treatment strategies for psychiatric symptoms, and psychotic symptoms in particular, among MA users.
Author Contributions
LL and YB designed the study and oversaw data collection. M-FS and M-XL designed the data analytic plan, performed literature review, and wrote the manuscript and tables. J-QL conducted analyses and made contributions to the content of the manuscript. JL, SL, PW, Z-ML and JS revised the manuscript and approve the final manuscript.
Funding
This work was supported by the Thirteenth Five-Year Program of the Chinese Ministry of Science and Technology (No. 2016YFC0800907), Twelfth Five-Year Program of the Chinese Ministry of Science and Technology (No. 2012ZX10001001) and the State Scholarship Fund of China (No. 201706015001).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. United Nations Office on Drugs and Crime. World Drug Report 2014. Vienna: United Nations Office on Drugs and Crime (2014).
2. United Nations Office on Drugs and Crime. World Drug Report 2016. Vienna: United Nations Office on Drugs and Crime (2016).
3. United Nations Office on Drugs and Crime. World Drug Report 2017. Vienna: United Nations Office on Drugs and Crime (2017).
4. Office of China National Narcotics Control Commission. Annual Report on Drug Control in China (2015). Beijing: Office of China National Narcotics Control Commission (2015).
5. Office of China National Narcotics Control Commission. Annual Report on Drug Control in China (2017). Beijing: Office of China National Narcotics Control Commission (2017).
6. China Food and Drug Administration. National Drug Abuse Monitoring Annual Report 2016. Beijing: China Food and Drug Administration (CFDA), National Surveillance Center on Drug Abuse (2017).
7. Akiyama K. Longitudinal clinical course following pharmacological treatment of methamphetamine psychosis which persists after long-term abstinence. Ann N Y Acad Sci. (2006) 1074:125–34. doi: 10.1196/annals.1369.012
8. Harris D, Batki SL. Stimulant psychosis: symptom profile and acute clinical course. Am J Addict. (2000) 9:28–37. doi: 10.1080/10550490050172209
9. Grant KM, LeVan TD, Wells SM, Li M, Stoltenberg SF, Gendelman HE, et al. Methamphetamine-associated psychosis. J Neuroimmune Pharmacol. (2012) 7:113–39. doi: 10.1007/s11481-011-9288-1
10. Glasner-Edwards S, Mooney LJ, Marinelli-Casey P, Hillhouse M, Ang A, Rawson R. Risk factors for suicide attempts in methamphetamine-dependent patients. Am J Addict. (2008) 17:24–7. doi: 10.1080/10550490701756070
11. Kittirattanapaiboon P, Mahatnirunkul S, Booncharoen H, Thummawomg P, Dumrongchai U, Chutha W. Long-term outcomes in methamphetamine psychosis patients after first hospitalisation. Drug Alcohol Rev. (2010) 29:456–61. doi: 10.1111/j.1465-3362.2010.00196.x
12. Artenie AA, Bruneau J, Zang G, Lesperance F, Renaud J, Tremblay J, et al. Associations of substance use patterns with attempted suicide among persons who inject drugs: can distinct use patterns play a role? Drug Alcohol Depend. (2015) 147:208–14. doi: 10.1016/j.drugalcdep.2014.11.011
13. ShoptawS P, Reback FJ. Psychiatric and susbstance dependence comorbidities, sexually transmitted diseases, and r isk behaviors among methamphetamine-dependenct gay and bisexual men seeking outpatient drug abuse treatment. Psychoact Drugs (2003) 35 (Suppl. 1):161–8. doi: 10.1080/02791072.2003.10400511
14. Grant KM, Kelley SS, Agrawal S, Meza JL, Meyer JR, Romberger DJ. Methamphetamine use in rural Midwesterners. Am J Addict. (2007) 16:79–84. doi: 10.1080/10550490601184159
15. Wallace C, Galloway T, McKetin R, Kelly E, Leary J. Methamphetamine use, dependence and treatment access in rural and regional North Coast of New South Wales, Australia. Drug Alcohol Rev. (2009) 28:592–9. doi: 10.1111/j.1465-3362.2008.00016.x
16. Leamon MH, Flower K, Salo RE, Nordahl TE, Kranzler HR, Galloway GP. Methamphetamine and paranoia: the methamphetamine experience questionnaire. Am J Addict. (2010) 19:155–68. doi: 10.1111/j.1521-0391.2009.00014.x
17. McKetin R, McLaren J, Lubman DI, Hides L. The prevalence of psychotic symptoms among methamphetamine users. Addiction (2006) 101:1473–8. doi: 10.1111/j.1360-0443.2006.01496.x
18. Lecomte T, Dumais A, Dugre JR, Potvin S. The prevalence of substance-induced psychotic disorder in methamphetamine misusers: a meta-analysis. Psychiatry Res. (2018) 268:189–92. doi: 10.1016/j.psychres.2018.05.033
19. Ma J, Sun XJ, Wang RJ, Wang TY, Su MF, Liu MX, et al. Profile of psychiatric symptoms in methamphetamine users in China: greater risk of psychiatric symptoms with a longer duration of use. Psychiatry Res. (2018) 262:184–92. doi: 10.1016/j.psychres.2018.02.017
20. McKetin R, Lubman DI, Baker AL, Dawe S, Ali RL. Dose-related psychotic symptoms in chronic methamphetamine users: evidence from a prospective longitudinal study. JAMA Psychiatry (2013) 70:319–24. doi: 10.1001/jamapsychiatry.2013.283
21. Chen CK, Lin SK, Sham PC, Ball D, Loh EW, Hsiao CC, et al. Pre-morbid characteristics and co-morbidity of methamphetamine users with and without psychosis. Psychol Med. (2003) 33:1407–14. doi: 10.1017/S0033291703008353
22. McKetin R, Gardner J, Baker AL, Dawe S, Ali R, Voce A, et al. Correlates of transient versus persistent psychotic symptoms among dependent methamphetamine users. Psychiatry Res. (2016) 238:166–71. doi: 10.1016/j.psychres.2016.02.038
23. Lecomte T, Mueser KT, MacEwan W, Thornton AE, Buchanan T, Bouchard V, et al. Predictors of persistent psychotic symptoms in persons with methamphetamine abuse receiving psychiatric treatment. J Nerv Ment Dis. (2013) 201:1085–9. doi: 10.1097/nmd.0000000000000059
24. Uosukainen H, Tacke U, Winstock AR. Self-reported prevalence of dependence of MDMA compared to cocaine, mephedrone and ketamine among a sample of recreational poly-drug users. Int J Drug Policy (2015) 26:78–83. doi: 10.1016/j.drugpo.2014.07.004
25. Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. (1987) 13:261–76.
26. Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel RR. What does the PANSS mean? Schizophr Res. (2005) 79:231–8. doi: 10.1016/j.schres.2005.04.008
27. Si TM, Shu L. The reliability and validity of the positive and negative symptom scale (PANSS, Chinese version). Chin J Psychiatry (2004) 18:45–7.
28. Bao YP, Qiu Y, Yan SY, Jia ZJ, Li SX, Lian Z, et al. Pattern of drug use and depressive symptoms among amphetamine type stimulants users in Beijing and Guangdong province, China. PloS ONE (2013) 8:e60544. doi: 10.1371/journal.pone.0060544
29. Zhang YX, Wang Y, Qian MY. Reliability and validity of Beck Depression Inventory (BDI) examined in Chinese samples. Chin Ment Health J. (1990) 4:164–8.
30. Eslami-Shahrbabaki M, Fekrat A, Mazhari S. A study of the prevalence of psychiatric disorders in patients with methamphetamine-induced psychosis. Addict Health (2015) 7:37–46.
32. Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. (1995) 51:768–74.
33. Li X, Phillips MR, Xu D, Niu Y. Reliability and validity of an adapted Chinese version of Barratt Impulsiveness Scale. Chin Ment Health J (2011) 25:610–5. doi: 10.3969/j.issn.1000-6729.2011.08.013
34. Yang HQ, Yao SQ, Zhu XZ. The Chinese version of the barratt impulsiveness scale, 11th version (BIS-11) in adolescents: its reliability and validity. Chin J Clin Psychol. (2007) 15:4–6. doi: 10.16128/j.cnki.1005-3611.2007.01.003
36. Hall W, Hando J, Darke S, Ross J. Psychological morbidity and route of administration among amphetamine users in Sydney, Australia. Addiction (1996) 91:81–7.
37. Farrell M, Boys A, Bebbington P, Brugha T, Coid J, Jenkins R, et al. Psychosis and drug dependence: results from a national survey of prisoners. Br J Psychiatry (2002) 181:393–8. doi: 10.1192/bjp.181.5.393
38. Sulaiman AH, Said MA, Habil MH, Rashid R, Siddiq A, Guan NC, et al. The risk and associated factors of methamphetamine psychosis in methamphetamine-dependent patients in Malaysia. Compr Psychiatry (2014) 55 (Suppl. 1):S89–94. doi: 10.1016/j.comppsych.2013.01.003
39. Teesson M, Marel C, Darke S, Ross J, Slade T, Burns L, et al. Long-term mortality, remission, criminality and psychiatric comorbidity of heroin dependence: 11-year findings from the Australian Treatment Outcome Study. Addiction (2015) 110:986–93. doi: 10.1111/add.12860
40. Kendler KS, Gallagher TJ, Abelson JM, Kessler RC. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry (1996) 53:1022–31.
41. de Wit H. Impulsivity as a determinant and consequence of drug use: a review of underlying processes. Addict Biol. (2009) 14:22–31. doi: 10.1111/j.1369-1600.2008.00129.x
42. Semple SJ, Zians J, Grant I, Patterson TL. Impulsivity and methamphetamine use. J Subst Abuse Treat. (2005) 29:85–93. doi: 10.1016/j.jsat.2005.05.001
43. Richards JB, Sabol KE, de Wit H. Effects of methamphetamine on the adjusting amount procedure, a model of impulsive behavior in rats. Psychopharmacology (1999) 146:432–9.
44. Eliza Congdon TC. The endophenotype of impulsivity: reaching consilience through behavioral, genetic, and neuroimaging approaches. Behav Cogn Neurosci Rev. (2006) 4:262–81. doi: 10.1177/1534582305285980
46. Lee B, London ED, Poldrack RA, Farahi J, Nacca A, Monterosso JR, et al. Striatal dopamine d2/d3 receptor availability is reduced in methamphetamine dependence and is linked to impulsivity. J Neurosci. (2009) 29:14734–40. doi: 10.1523/jneurosci.3765-09.2009
47. Kuhn DM, Francescutti-Verbeem DM, Thomas DM. Dopamine disposition in the presynaptic process regulates the severity of methamphetamine-induced neurotoxicity. Ann N Y Acad Sci. (2008) 1139:118–26. doi: 10.1196/annals.1432.026
48. Sekine Y, Minabe Y, Ouchi Y, Takei N, Iyo M, Nakamura K, et al. Association of dopamine transporter loss in the orbitofrontal and dorsolateral prefrontal cortices with methamphetamine-related psychiatric symptoms. Am J Psychiatry (2003) 160:1699–701. doi: 10.1176/appi.ajp.160.9.1699
49. Yui K, Goto K, Ikemoto S, Ishiguro T, Kamada Y. Increased sensitivity to stress and episode recurrence in spontaneous recurrence of methamphetamine psychosis. Psychopharmacology (1999) 145:267–72.
50. Nohesara S, Ghadirivasfi M, Barati M, Ghasemzadeh MR, Narimani S, Mousavi-Behbahani Z, et al. Methamphetamine-induced psychosis is associated with DNA hypomethylation and increased expression of AKT1 and key dopaminergic genes. Am J Med Genet B (2016) 171:1180–9. doi: 10.1002/ajmg.b.32506
51. Zorick T, Nestor L, Miotto K, Sugar C, Hellemann G, Scanlon G, et al. Withdrawal symptoms in abstinent methamphetamine-dependent subjects. Addiction (2010) 105:1809–18. doi: 10.1111/j.1360-0443.2010.03066.x
52. Arunogiri S, Foulds JA, McKetin R, Lubman DI. A systematic review of risk factors for methamphetamine-associated psychosis. Aust N Z J Psychiatry (2018) 52:514–29. doi: 10.1177/0004867417748750
53. Ding Y, Lin H, Zhou L, Yan H, He N, Shin EJ, et al. Adverse childhood experiences and interaction with methamphetamine use frequency in the risk of methamphetamine-associated psychosis. Drug Alcohol Depend. (2014) 142:295–300. doi: 10.1016/j.drugalcdep.2014.06.042
54. Roncero C, Daigre C, Grau-Lopez L, Barral C, Perez-Pazos J, Martinez-Luna N, et al. An international perspective and review of cocaine-induced psychosis: a call to action. Subst Abus. (2014) 35:321–7. doi: 10.1080/08897077.2014.933726
55. Roncero C, Daigre C, Grau-Lopez L, Rodriguez-Cintas L, Barral C, Perez-Pazos J, et al. Cocaine-induced psychosis and impulsivity in cocaine-dependent patients. J Addict Dis. (2013) 32:263–73. doi: 10.1080/10550887.2013.824330
Keywords: MA-associated psychotic symptoms, risk factors, prevalence, MA users, China
Citation: Su M-F, Liu M-X, Li J-Q, Lappin JM, Li S, Wu P, Liu Z-M, Shi J, Lu L and Bao Y (2018) Epidemiological Characteristics and Risk Factors of Methamphetamine—Associated Psychotic Symptoms. Front. Psychiatry 9:489. doi: 10.3389/fpsyt.2018.00489
Received: 30 July 2018; Accepted: 19 September 2018;
Published: 12 October 2018.
Edited by:
Carlos Roncero, Complejo Hospitalario de Salamanca, SpainReviewed by:
Raul Felipe Palma-Alvarez, Hospital Universitari Vall d'Hebron, SpainMercedes Lovrecic, National Institute for Public Health, Slovenia
Copyright © 2018 Su, Liu, Li, Lappin, Li, Wu, Liu, Shi, Lu and Bao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanping Bao, YmFveXBAYmptdS5lZHUuY24=
Lin Lu, bGlubHVAYmptdS5lZHUuY24=
†These authors have contributed equally to this work
 Meng-Fan Su
Meng-Fan Su Mo-Xuan Liu1,2†
Mo-Xuan Liu1,2† Julia M. Lappin
Julia M. Lappin Su-xia Li
Su-xia Li Jie Shi
Jie Shi Yanping Bao
Yanping Bao