- 1Department of Psychiatry and Psychotherapy, University of Regensburg, Regensburg, Germany
- 2LWL Hospital Paderborn, Psychiatry-Psychotherapy-Psychosomatics, Ruhr University of Bochum, Bochum, Germany
A causal relationship between sleep disturbances and suicidal behavior has been previously reported. Insomnia and nightmares are considered as hallmarks of posttraumatic stress disorder (PTSD). In addition, patients with PTSD have an increased risk for suicidality. The present article gives an overview about the existing literature on the relationship between sleep disturbances and suicidality in the context of PTSD. It aims to demonstrate that diagnosing and treating sleep problems as still underestimated target symptoms may provide preventive strategies with respect to suicidality. However, heterogeneous study designs, different samples and diverse outcome parameters hinder a direct comparison of studies and a causal relationship cannot be shown. More research is necessary to clarify this complex relationship and to tackle the value of treatment of sleep disturbances for suicide prevention in PTSD.
Introduction
Suicide is a leading cause of death worldwide with at least 788,000 annual deaths from suicide around the world in 2015 according to WHO data (1). Sleep disturbances have been shown to be a risk factor for mental disorders for decades, and are an independent risk factor for suicidal behavior (2). However, not only sleep problems in general have evolved as an evidence-based risk factor for suicide (3, 4), but short sleep duration also seems to be associated with suicidality (5, 6). Moreover, insomnia has also been proposed to be an independent risk factor for suicidality (7, 8). However, the association is weaker after controlling for depression (9, 10). Further, there is also evidence for an association between nightmare disorder and suicidality (11–13). However, the specific contributions of nightmare disorder to suicidality remain unclear (14). Unfortunately, nightmares are under-reported, therefore detection and treatment are often insufficient (15).
PTSD and Sleep Disturbances
The lifetime prevalence of posttraumatic stress disorder (PTSD) is estimated to be about 8.0% in the general population (16, 17), and sleep disturbances are considered as a core feature of PTSD (18). There is a high prevalence of nightmares (up to 70%) in patients with PTSD (19), and the rate of sleep disturbances in PTSD is estimated to be in the same range as that of nightmares and insomnia at about 40% (20). A bidirectional relationship between PTSD and sleep disturbances has been purported (21, 22). This is in line with the hypothesis that it is biologically plausible for sleep disturbance to be mechanistically transdiagnostic, suggesting that sleep disturbances are related to the onset and course of several psychiatric disorders. Specifically, increased activity of the noradrenergic system during rapid-eye-movement-(REM)-sleep, REM-sleep fragmentation and reduced activity of the medial prefrontal cortex during REM-sleep may play a pivotal role with respect to sleep fragmentation and emotion dysregulation in PTSD (23).
Apart from sleep disturbances and nightmares being an integral diagnostic criteria of PTSD, specific sleep disorders such as obstructive sleep apnea syndrome (OSAS), REM-sleep behavior disorder, and periodic limb movement disorder have been reported to be disproportionately frequent in PTSD patients (24). Several studies have shown a high prevalence of OSAS in PTSD patients, and it is suggested that OSAS plays a role in the pathophysiology of PTSD symptoms (25–27). There is also evidence for a positive correlation between effective OSAS treatment and reduced PTSD severity (28, 29). Sleep terrors, nocturnal panic attacks, and simple and complex motor behaviors including vocalizations and acting out dreams may also occur during sleep in patients with PTSD (23). These features were recently described as “Trauma Associated Sleep Disorder” which may also occur without the presence of other typical PTSD symptoms (30, 31).
PTSD and Suicidality
Numerous studies have shown that PTSD represents a risk factor for suicidal thoughts and behaviors (32, 33). In addition, there is evidence for a mediating role of depression in the association of PTSD and suicidality (34). Comorbid depression may amplify the suicide risk synergistically beyond an additive effect (35). Indeed, there is evidence of an increased risk of death by suicide in PTSD patients in general (36, 37) even compared to trauma-exposed people (38, 39). Considering suicide risk, it is noteworthy that PTSD is one of the few psychiatric disorders that distinguish those who think about suicide from those who make suicide attempts (40). A meta-analysis has shown that PTSD is reliably more common in attempters than ideators, but these effects seem to be modest rather than strong (41).
PTSD, Sleep Disturbances and Suicidality
There are only few studies reporting on the relationship between PTSD, sleep disturbances, and suicidality. A meta-analysis of sleep disturbances and suicidal thoughts and behaviors including studies on mixed samples (42) identified only one study on their relationship to PTSD (43); another meta-analysis and systematic review about the association between sleep disturbances and suicidal behaviors in patients with psychiatric diagnoses (44) also found the same study by Krakow et al. (43). Moreover, a systematic review of the relationship between sleep disturbance, suicidal ideation, suicide attempts, and suicide among adults (45) provided three studies for PTSD (46–48) and seven studies for veterans in consideration of a possible PTSD diagnosis (49–55).
Literature Search and Results
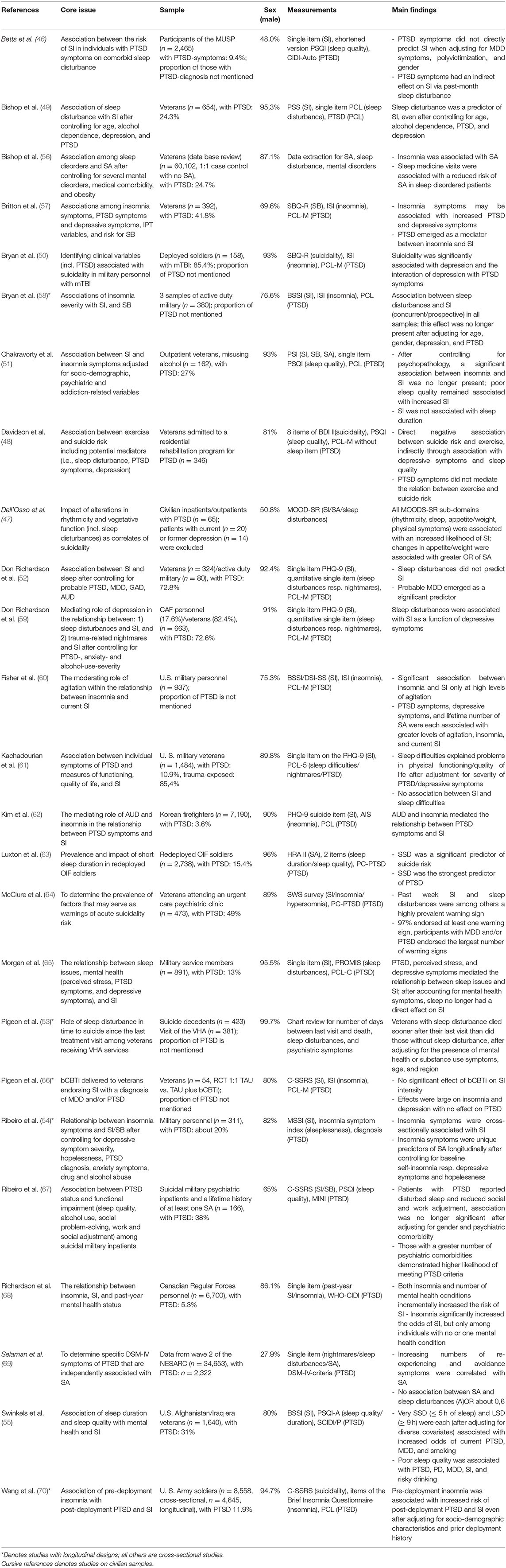
We conducted a comprehensive search of MEDLINE/PubMed databases using Medical Subject Headings terms in various combinations to identify studies that examined aspects of sleep disorders, suicidality and PTSD. Furthermore, we identified several studies by searching through references of identified studies, reviews and meta-analyses. In total, we identified 30 studies (Tables 1–3).
Sleep Disturbances (Insomnia)
The respective studies are listed in Table 1. One study in military personnel investigated the relationship between insomnia symptoms and suicidal ideation and behavior after controlling for depressive symptom severity, hopelessness, PTSD diagnosis, anxiety symptoms, and drug and alcohol abuse in a cross-sectional as well as longitudinal design (54). It was shown that insomnia symptoms were cross-sectionally associated with suicidal ideation. Using a longitudinal design, insomnia symptoms were unique predictors of suicide attempts after controlling for baseline self-insomnia, depressive symptoms and hopelessness (54). The study is often cited as the prime example of a close link between sleep disturbances and suicidality independent of the presence of depression in PTSD. In addition, another study in veterans found that the association of sleep disturbance with suicidal ideations remained significant after controlling for age, alcohol dependence, depression, and PTSD (49). This was replicated in another study on veterans for poor sleep quality in general, but not for insomnia symptoms (51). A chart review provided evidence for a longitudinal relationship between sleep and suicidality; veterans with sleep disturbance died sooner after their last visit compared to those without sleep disturbance, even after adjusting for the presence of mental health or substance use symptoms (53).
New findings with respect to the longitudinal relationship revealed that pre-deployment insomnia was associated with increased risk of post-deployment PTSD and suicidal ideation even after adjusting for sociodemographic characteristics and prior deployment history (70). This is in line with prior findings. Sleep disturbance is not only a symptom of PTSD, but when existing prior to trauma they may also be a risk factor for developing PTSD in civilians (74) and in military personnel (75–77).
Consistent with these findings, an analysis of a large suicide attempt database from the U.S. Department of Veterans Affairs also revealed an independent association between insomnia and suicide attempts even after controlling for several socio-demographic factors and diverse psychiatric disorders. Furthermore, sleep medicine visits 180 days prior to the index date were associated with a decreased likelihood of suicide attempt for individuals with sleep disorders. Thus, the assessment and treatment of sleep disorders should be considered in context of strategies to augment suicide prevention efforts (56).
A proof-of-concept randomized clinical trial investigated the effects of a brief cognitive behavioral therapy for insomnia in primary care patients with suicidal ideation and insomnia in addition to either major depressive disorder and/or PTSD. The effect size of brief cognitive behavioral therapy for insomnia on suicidal ideation intensity was not significant. Effects were large on insomnia and depression with no effect on PTSD (66).
A birth cohort study in young Australians (the only study with non-veterans in this context) showed that PTSD symptoms indirectly predicted suicidal ideation via comorbid sleep disturbances even when adjusting for major depression symptoms, poly-victimization and gender. Notably, poly-victimization predicted sleep disturbances and suicidal ideation independently of PTSD or major depression (46).
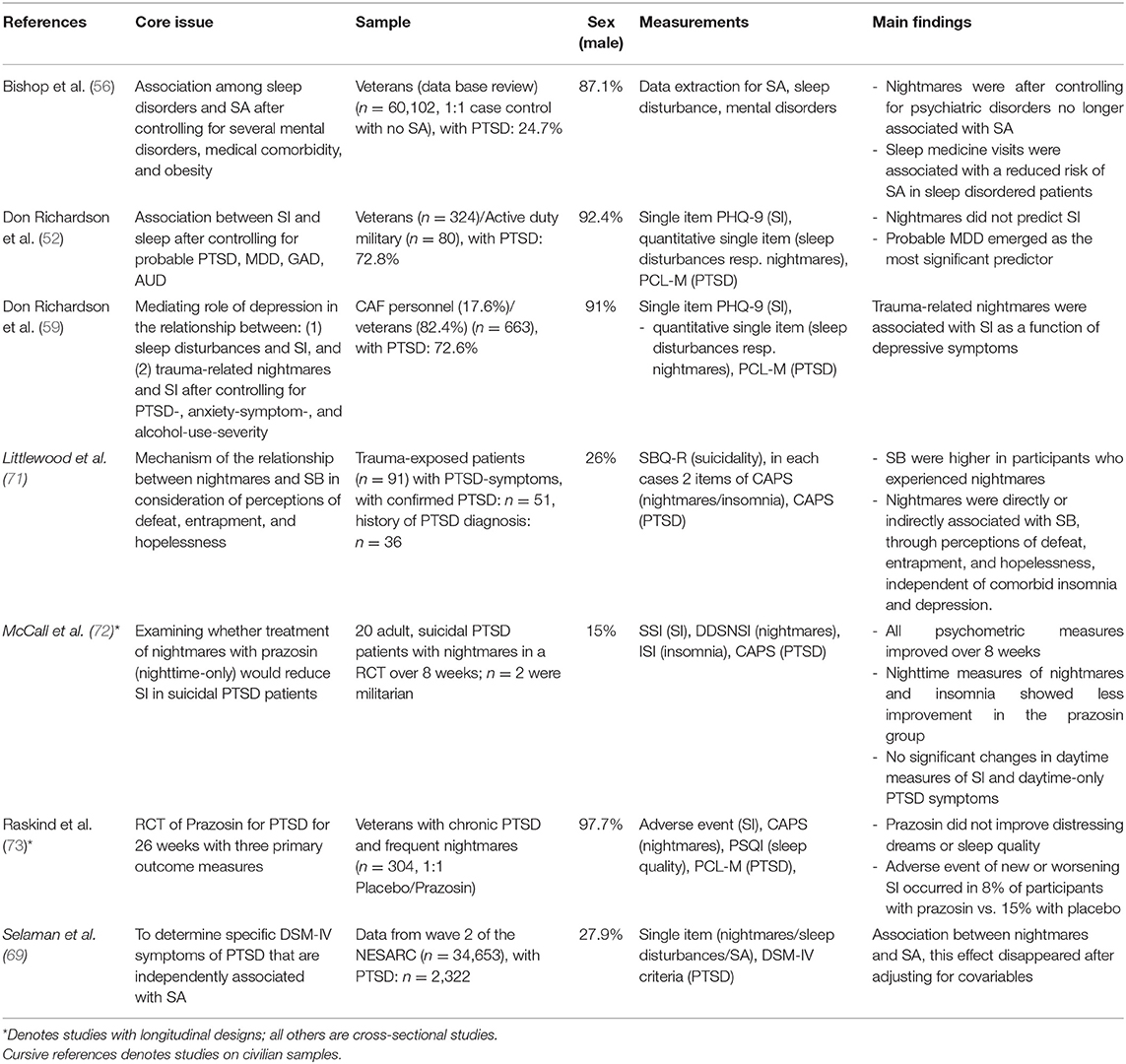
Nightmares
The studies focusing on nightmares are listed in Table 2. Two studies focused on the association between suicidality and nightmares in the context of PTSD. In the first study, the authors reported that trauma-related nightmares were highly prevalent (67.9%) but not associated with suicidal ideations. However, in a regression model, the presence of probable PTSD was significantly associated with suicidal ideations, indicating a mediating role of PTSD in the association between nightmares and suicidal ideations. Probable major depressive disorder emerged as the strongest predictor of suicidal ideation (52). These results were confirmed in a subsequent study by the same authors (59). Recently, corresponding results regarding the association between suicide attempts and nightmares were reported in a sample with veterans. After controlling for psychiatric disorders, nightmares were no longer significant associated with suicidal attempts (56).
In contrast to these findings, in a sample of trauma-exposed civilians with PTSD symptoms, nightmares were both directly and indirectly associated with suicidal behavior, through perceptions of defeat, entrapment, and hopelessness, independent of comorbid insomnia and depression (71). Further analyses supported that the relationship between nightmares and suicidal behavior was partially mediated by a multistep pathway via defeat, entrapment, and hopelessness (71).
Prazosin, an α1-adrenergic receptor antagonist, has been effective in alleviating nightmares associated with PTSD in military veterans (78, 79). However, in a randomized clinical trial of prazosin in suicidal PTSD patients there was no significant improvement of suicidal ideation or day time-only PTSD symptoms. In addition, nightmares and insomnia showed significantly less improvement in the prazosin group (72). These findings are in line with a recent multi-center randomized trial on the effect of prazosin in veterans with chronic PTSD, which revealed no effects of prazosin on nightmares or sleep quality (73). Of note, fewer patients in the prazosin group reported suicidal ideation compared with the placebo group.
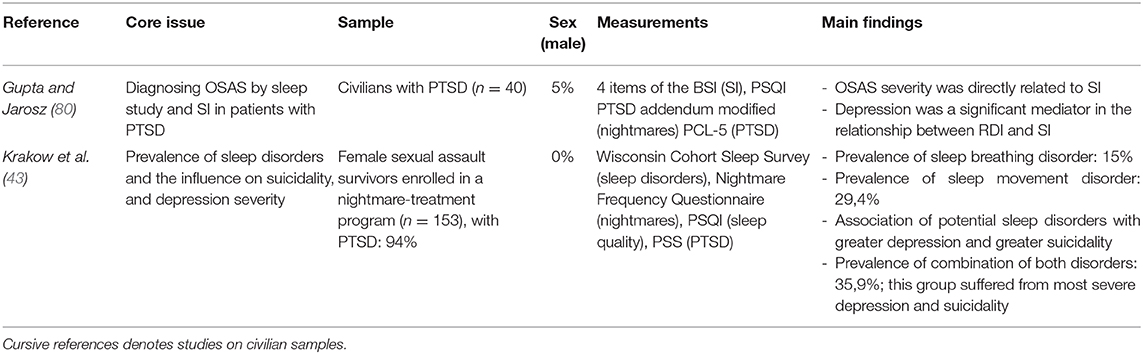
Sleep-Related Breathing Disorders
The studies focused on sleep-related breathing disorders are listed in Table 3. A sample of female sexual assault survivors with PTSD was assessed for subjectively determined sleep related breathing and movement disorders and 80% of the participants presented with such disorders (43). Participants with potential sleep disorders suffered from a higher degree of depression and suicidality in comparison to those without any potential sleep disorder. It was hypothesized that this effect could be mediated through chronic sleep fragmentation. The study was limited insofar as the participants were recruited through a nightmare-treatment program. Nightmares are estimated as a marker for other sleep disorders, therefore nightmares could increase the total prevalence of sleep disorders (43). In a study performed to elucidate the association between suicidal ideations and OSAS, it was found that OSAS severity was directly related to suicidal ideation in (predominately female) PTSD patients who underwent a home sleep apnea monitoring. Depression was a significant mediator in the relationship between respiratory disturbance index and suicidal ideation (80).
Sleep Duration
Sleep duration itself is purported to have an effect on suicidality (5, 6, 81). In redeployed soldiers, after controlling for combat exposure, short sleep duration was associated with symptoms of depression, PTSD, and panic syndrome, and with high-risk health behaviors such as abuse of tobacco and alcohol products, as well as suicide attempts. Short sleep duration emerged as a significant predictor of suicide risk; conversely, short sleep was the strongest predictor of PTSD symptoms (63). Another study in veterans corroborated an association between sleep duration, very short sleep duration (≤5 h of sleep) as well as long sleep duration (≥9 h): after adjusting for covariates, both conditions were associated with increased odds of current PTSD and major depression, but not with suicidal ideation. However, poor sleep quality was associated with PTSD and suicidal ideation as well as with panic disorder, major depressive disorder, and risky drinking (55).
Circadian Aspects
We identified one study in civilian patients with PTSD investigating the effect of alterations in rhythmicity and vegetative function including sleep disturbances as correlates of suicidality. As a result, all lifetime mood spectrum sub-domains (rhythmicity, sleep, appetite/weight, sexual function, physical symptoms) were associated with an increased likelihood of suicidal ideation. Interestingly, another study reported that an eveningness chronotype in PTSD was associated with an increased likelihood of suicidal ideations, but not suicide attempts (47).
Mediating Factors
Various mediating factors may have an influence on the association between sleep disturbances, suicidality, and PTSD symptoms.
Depression
A study on deployed soldiers with mild trauma brain injury showed a significant association between increased suicidality and depression as well as the interaction of depression with PTSD symptoms. Interestingly, longer duration of loss of consciousness was associated with decreased likelihood for any suicidality (50). Another study found an association between sleep disturbances with concurrent and prospective suicide ideation in three active military samples. When adjusting for age, gender, depression, and PTSD, insomnia severity was no longer directly associated with suicidal ideation either concurrently or prospectively, whereby depression mediated the relation of insomnia severity with suicide risk (58). One study examined the association of suicidal ideation and sleep disturbances after controlling for probable PTSD, depression, alcohol use disorder (AUD) and generalized anxiety disorder. Neither sleep disturbances nor nightmares significantly predicted suicidal ideation; instead, major depression emerged as the most significant predictor (52). Depression also mediated the relationship between insomnia and nightmares and suicidal ideations (59). Another study investigated the associations among insomnia symptoms, PTSD, and depressive symptoms, interpersonal theory of suicide variables, and risk for suicidal behavior in community veterans and confirmed a mediating effect of depression. In extension to this, PTSD emerged also as a mediator between insomnia and suicidal ideation. The interpersonal theory of suicide variables of thwarted belongingness and perceived burdensomeness mediated the association of depressive and PTSD symptoms with risk for suicidal behavior, indicating a sequential association (57).
Other Mediators
In military service members with PTSD, perceived stress mediated the relationship between sleep issues and suicidal ideation; however, after accounting for mental health symptoms (depression, perceived stress, PTSD symptoms) sleep no longer had a significant direct effect on suicidal ideation (65). In outpatient veterans misusing alcohol the relationship between insomnia symptoms and suicidal ideation was no longer significant after controlling for other mental disorders. However, poor sleep quality remained significantly associated with increased suicidal ideation even after controlling for other risk factors (51). Among suicidal military inpatients, those with PTSD reported more disturbed sleep and reduced social and work adjustment. Still, this association between functionality and PTSD status was no longer significant after adjusting for gender and psychiatric comorbidity as individuals. Patients with a higher number of psychiatric comorbidities demonstrated a higher likelihood of meeting PTSD criteria (67).
Beyond mental health conditions in general, some studies also investigated specific mediators, i.e., AUD (62), agitation (60), and exercise (48) in the context of PTSD, suicidality, and sleep disturbances. Given that AUD und PTSD frequently co-occur (82), evidence for a mediating role of AUD and insomnia in the relationship between PTSD symptoms and suicidal ideation derived from a large sample of Korean firefighters (62). With respect to a moderating role of agitation within the relationship between insomnia and current suicidal ideations, a study on U.S. military personnel showed significant effects only at high levels of agitation. PTSD symptoms, depressive symptoms, and lifetime number of suicide attempts were each associated with greater levels of agitation, insomnia, and current suicidal ideation (60).
PTSD Symptom Clusters and Suicidality
A burgeoning approach to determine suicide risk in the context of PTSD is the analysis of specific PTSD symptom clusters (69, 83–90) yielding conflicting results. Considering sleep disturbances and nightmares as diagnostic criteria for PTSD, a within-cluster item analysis would be necessary. So far, only one study meets this requirement: reporting that an increased number of re-experiencing and avoidance symptoms significantly correlated with suicide attempts. In addition, a significant association between nightmares and suicide attempts was found; however, this effect was no longer present after controlling for covariates (69). In this study, sleep disturbances (85.0%) and nightmares (77.8%) were highly prevalent, but were evaluated by using a single, dichotomous question only, indicating a possible lack of selectivity. To date, only three studies examined the relationship between PTSD symptom clusters and suicidality in a prospective design (88, 90, 91), with two of them pointing at a unique relationship between alterations in arousal and reactivity and higher suicidality (90, 91). Unfortunately, sleep disturbance as a feature of the cluster “alterations in arousal and reactivity” was not separately considered in these studies. Thus, it is not possible to state, whether sleep disturbances had a significant influence on these results.
A more tailored approach on individual PTSD symptoms a priori has been provided by the use of a more detailed method for the assessment, monitoring, and treatment of PTSD symptoms (61). This study of predominantly trauma-exposed military veterans investigated the association between individual symptoms of PTSD and measures of functioning, quality of life, and suicidal ideation. Among others, sleep difficulties explained problems in physical functioning and quality of life. These findings persisted after adjustment for lifetime trauma burden and severity of PTSD and depressive symptoms. No association was found between suicidal ideations and sleep difficulties (61). However, it should be emphasized that only about 10% of the sample met full PTSD criteria.
Discussion
The present studies revealed heterogeneous and partially contradictory results. A direct association between sleep disturbances and suicidal behavior in patients with PTSD has been reported by a few studies (49, 51, 53, 54, 70),while others found no association after controlling for covariates such as depression (50, 52, 57–59). In a sample of veterans with PTSD and two or more comorbid disorders there was a higher risk of suicidal ideation compared to veterans with PTSD only (92).
The study results should be interpreted with caution because differences in approach and samples, as well as different applied measurements and outcome parameters, hinder direct comparisons. In particular, due to the studies available, various types of sleep disturbances, measured by using different methodologies, were included. Some studies focused on specific sleep disorders such as insomnia, nightmares or sleep related breathing disorders (57, 80, 93) while others measured only sleep quality or sleep duration in a more general approach (43, 48) or used a single sleep item only (59, 69) limiting the comparability. In addition, almost all studies used self-report instruments to assess sleep variables. However, subjective and objective measurements of sleep may differ also in PTSD patients and do not necessarily co-vary (94, 95). The use of sleep diaries could be a more reliable measurement in order to assess prospectively sleep disorders compared to a selective survey (96). The vast majority of studies used a cross-sectional design, a major limitation for drawing causal conclusions. With respect to suicidality, it can be stated that the outcome parameters vary between suicidal ideation (60), suicidal behavior (57), suicide attempts (56), death by suicide (53), and through combinations of those (51). Thus, “suicidality” does not always carry the same meaning and precludes comparability.
Of importance, an explicit PTSD diagnosis was a primary inclusion criterion only in five studies (27, 47, 48, 72, 73), whereas in all other studies a “possible” PTSD diagnosis was recorded and considered in data analysis with prevalence rates between 3.6% (62) and 94% (43). Therefore, the absolute number of subjects with PTSD was considerably lower than the absolute number of study participants, mitigating the statistical validity. In military samples, the vast majority of participants were men with a proportion of at least 69.6% (57) up to 99.7% (53). In civilian samples, women were overrepresented by trend with a proportion of at least 49.2% (47) up to 100% (43). This remarkable disproportion in gender ratios should be taken into account in light of gender differences in suicidal behavior among persons with PTSD. For example, among veterans with PTSD, women have a lower risk of dying by suicide compared with men (97).
In addition, most studies have included military personnel and veterans. A large cohort study, for example, revealed an association between type and number of traumata with suicidal ideation and suicide attempts in patients with PTSD (98). Among others, peacekeeping traumata had the highest rates of suicidal ideation and suicidal behavior. In the civilian population, however, a broader spectrum of trauma types may occur. Moreover, it remains questionable whether results obtained from veterans can be transferred to the civilian population. Evaluating the risk of death by suicide in military personnel, some specific aspects have to be noted; historically, soldiers have had a markedly lower suicide rate than civilians (99, 100). However, since 2005 the incidence of suicide in Army and Marine personnel has nearly doubled and remained elevated (101, 102). Several studies showed an increased risk of people with PTSD dying by suicide (103–106), while others revealed a decreased risk of death by suicide in military personnel (107–110). The background of these confusing results is discussed in detail in a recently published review (111).
The current overview has some limitations. Most importantly, it does not meet the requirements of a systematic review because we did not perform a systematic literature research. In addition, we had no strict inclusion/exclusion criteria to identify relevant studies. In many studies, the relationship between sleep disturbances, suicidality, and PTSD was a minor issue and evaded a literature search using Medical Subject Headings terms. Therefore, the overview may not cover all studies in the field. Nevertheless, diagnosing and treating sleep disturbances early in the context of trauma exposition may provide preventive strategies regarding the development of PTSD. For example, non-drug interventions such as cognitive behavioral therapy for insomnia has been shown to reduce sleep disturbances and, subsequently, PTSD symptoms (112). It remains to be clarified whether or not suicidal behavior in PTSD can also be improved by treating impaired sleep.
Conclusion
Heterogeneous study approaches, different samples and applied measurements, and diverse outcome parameters hinder a direct comparison of studies examining sleep disturbances, suicidality, and PTSD. In addition, due to limited study methodologies, a causal relationship in these entities cannot be shown. Future research including adequately designed studies is necessary to clarify the complex relationship between these parameters. Particularly, more studies in the civilian population are needed also to tackle the value of treatment of sleep disturbances for suicide prevention in PTSD.
Author Contributions
FW and TW have made substantial contributions to conception and design of the study and analyzed the data. FW executed the acquisition of data. FW, CN, and TW have been involved in the interpretation of data, drafting and revising the manuscript for important intellectual content. All authors have read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer RG declared a past co-authorship with the authors to the handling editor.
Abbreviations
AIS, Athens Insomnia Scale; AOR, Adjusted odds ratio; AUD, Alcohol use disorder; bCBTi, Brief cognitive behavioral therapy for insomnia; BDI II, Beck Depression Inventory, 2. Edition; BSSI, Beck Scale for Suicidal Ideation; CAF, Canadian Armed Force; CAPS, Clinician-Administered PTSD Scale for DSM-IV; CIDI-Auto, Composite International Diagnostic Interview, version 2.4; C-SSRS, Columbia Suicide Severity Rating Scale; DDNSI, Disturbing Dreams and Nightmare Severity Index; DSI-SS, Depressive Symptom Index-Suicidality Subscale; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, 4. Version; GAD, Generalized anxiety disorder; HRA II, Health Risk Appraisal; IPT, Interpersonal Theory of Suicide; ISI, Insomnia Severity Index; LSD, Long sleep duration; MDD, Major depressive disorder; MINI, Mini International Neuropsychiatric Screen and Interview; MOODS-SR, Mood Spectrum-Self Report; MSSI, Modified Scale for Suicidal Ideationl; mTBI, Mild traumatic brain injury; MUSP, Mater University Study of Pregnancy; NESARC, National Epidemiologic Survey on Alcohol and Related Conditions; OIF, Operation Iraqi Freedom; OR, Odds ratio; OSAS, Obstructive sleep apnea syndrome; PCL, Posttraumatic Stress Disorder Symptoms Checklist; PCL-5, Posttraumatic Stress Disorder Checklist for DSM-5; PCL-C, Posttraumatic Stress Disorder Symptoms Checklist—Civilian version; PCL-M, Posttraumatic Stress Disorder Symptoms Checklist—Military version; PC-PTSD, Primary Care PTSD Screen; PD, Panic disorder; PHQ-9, Patient Health Questionnaire 9; PROMIS, Patient-Reported Outcomes Measurement Information System; PSI, Paykel Suicide Items; PSQI, Pittsburgh Sleep Quality Index; PSQI-A, Pittsburgh Sleep Quality Index-Addendum; PSS, PTSD Symptom Scale; PTSD, Posttraumatic stress disorder; RCT, Randomized clinical trial; RDI, Respiratory disturbance index; REM, Rapid eye movement; SA, Suicide attempt; SB, Suicidal behavior; SBQ-R, Suicidal Behaviors Questionnaire-Revised; SCIDI/P, Structured Clinical Interview for DSMIV-TR Axis I Disorders; SI, Suicidal ideation; SSD, Short sleep duration; SSI, Scale for Suicide Ideation; SWS, Suicide warning signs survey; TAU, Treatment as usual; VHA, Veterans Health Administration.
References
1. WHO Mental Health. Prevention of Suicidal Behaviours: A Task for All. (2015). Available online at: http://www.who.int/mental_health/prevention/suicide/background (accessed January 30, 2020).
2. McCall WV, Black CG. The link between suicide and insomnia: theoretical mechanisms. Curr Psychiatry Rep. (2013) 15:389. doi: 10.1007/s11920-013-0389-9
3. Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep. (2015) 17:15. doi: 10.1007/s11920-015-0554-4
4. Liu JW, Tu YK, Lai YF, Lee HC, Tsai PS, Chen TJ, et al. Associations between sleep disturbances and suicidal ideation, plans, and attempts in adolescents: a systematic review and meta-analysis. Sleep Med Rev. (2019) 42:119–26. doi: 10.1093/sleep/zsz054
5. Lee J, Jang H, Kim J, Min S. Development of a suicide index model in general adolescents using the South Korea 2012-2016 national representative survey data. Sci Rep. (2019) 9:1846. doi: 10.1038/s41598-019-38886-z
6. Littlewood DL, Kyle SD, Carter LA, Peters S, Pratt D, Gooding P. Short sleep duration and poor sleep quality predict next-day suicidal ideation: an ecological momentary assessment study. Psychol Med. (2019) 49:403–11. doi: 10.1017/S0033291718001009
7. Rössler W, Angst J, Ajdacic-Gross V, Haker H, Berrouiguet S, Ujeyl M, et al. Sleep disturbances and suicidality-a longitudinal analysis from a representative community study over 30 years. Front Psychiatry. (2018) 9:320. doi: 10.3389/fpsyt.2018.00320
8. Russell K, Rasmussen S, Hunter SC. Insomnia and nightmares as markers of risk for suicidal ideation in young people: investigating the role of defeat and entrapment. J Clin Sleep Med. (2018) 14:775–84. doi: 10.5664/jcsm.7104
9. Bernert RA, Joiner TE, Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. (2005) 28:1135–41. doi: 10.1093/sleep/28.9.1135
10. Tae H, Jeong BR, Chae JH. Sleep problems as a risk factor for suicide: Are certain specific sleep domains associated with increased suicide risk? J Affect Disord. (2019) 252:182–9. doi: 10.1016/j.jad.2019.04.053
11. Sjöström N, Hetta J, Waern M. Persistent nightmares are associated with repeat suicide attempt: a prospective study. Psychiatry Res. (2009) 170:208–11. doi: 10.1016/j.psychres.2008.09.006
12. Tanskanen A, Tuomilehto J, Viinamäki H, Vartiainen E, Lehtonen J, Puska P. Nightmares as predictors of suicide. Sleep. (2001) 24:844–7. doi: 10.1093/sleep/24.7.845
13. Sandman N, Valli K, Kronholm E, Vartiainen E, Laatikainen T, Paunio T. Nightmares as predictors of suicide: an extension study including war veterans. Sci Rep. (2017) 7:44756. doi: 10.1038/srep44756
14. Titus CE, Speed KJ, Cartwright PM, Drapeau CW, Heo Y, Nadorff MR. What role do nightmares play in suicide? A brief exploration. Curr Opin Psychol. (2018) 22:59–62. doi: 10.1016/j.copsyc.2017.08.022
15. Nadorff MR, Nadorff DK, Germain A. Nightmares: under-reported, undetected, and therefore untreated. J Clin Sleep Med. (2015) 11:747–50. doi: 10.5664/jcsm.4850
16. Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen H-U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. (2012) 21:169–84. doi: 10.1002/mpr.1359
17. Kessler RC, Ruscio AM, Shear K, Wittchen HU. Epidemiology of anxiety disorders. Curr Top Behav Neurosci. (2010) 2:21–35. doi: 10.1007/7854_2009_9
18. Ross RJ, Ball WA, Sullivan KA, Caroff SN. Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry. (1989) 146:697–707. doi: 10.1176/ajp.146.1.128-a
19. Wittmann L, Schredl M, Kramer M. Dreaming in posttraumatic stress disorder: a critical review of phenomenology, psychophysiology and treatment. Psychother Psychosom. (2007) 76:25–39. doi: 10.1159/000096362
20. Ohayon MM, Shapiro CM. Sleep disturbances and psychiatric disorders associated with posttraumatic stress disorder in the general population. Compr Psychiatry. (2000) 41:469–78. doi: 10.1053/comp.2000.16568
21. Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev. (2008) 12:169–84. doi: 10.1016/j.smrv.2007.08.008
22. Miller KE, Brownlow JA, Gehrman PR. Sleep in PTSD: treatment approaches and outcomes. Curr Opin Psychol. (2019) 34:12–7. doi: 10.1016/j.copsyc.2019.08.017
23. Germain A, Buysse DJ, Nofzinger E. Sleep-specific mechanisms underlying posttraumatic stress disorder: integrative review and neurobiological hypotheses. Sleep Med Rev. (2008) 12:185–95. doi: 10.1016/j.smrv.2007.09.003
24. Miller KE, Brownlow JA, Woodward S, Gehrman PR. Sleep and dreaming in posttraumatic stress disorder. Curr Psychiatry Rep. (2017) 19:74. doi: 10.1007/s11920-017-0827-1
25. El-Solh AA, Riaz U, Roberts J. Sleep disorders in patients with posttraumatic stress disorder. Chest. (2018) 154:427–39. doi: 10.1016/j.chest.2018.04.007
26. Krakow BJ, Ulibarri VA, Moore BA, McIver ND. Posttraumatic stress disorder and sleep-disordered breathing: a review of comorbidity research. Sleep Med Rev. (2015) 24:37–45. doi: 10.1016/j.smrv.2014.11.001
27. Gupta MA, Simpson FC. Obstructive sleep apnea and psychiatric disorders: a systematic review. J Clin Sleep Med. (2015) 11:165–75. doi: 10.5664/jcsm.4466
28. Orr JE, Smales C, Alexander TH, Stepnowsky C, Pillar G, Malhotra A, et al. Treatment of OSA with CPAP is associated with improvement in PTSD symptoms among veterans. J Clin Sleep Med. (2017) 13:57–63. doi: 10.5664/jcsm.6388
29. El-Solh AA, Adamo D, Kufel T. Comorbid insomnia and sleep apnea in Veterans with post-traumatic stress disorder. Sleep Breath. (2018) 22:23–31. doi: 10.1007/s11325-017-1618-y
30. Mysliwiec V, O'Reilly B, Polchinski J, Kwon HP, Germain A, Roth BJ. Trauma associated sleep disorder: a proposed parasomnia encompassing disruptive nocturnal behaviors, nightmares, and REM without atonia in trauma survivors. J Clin Sleep Med. (2014) 10:1143–8. doi: 10.5664/jcsm.4120
31. Brock MS, Powell TA, Creamer JL, Moore BA, Mysliwiec V. Trauma associated sleep disorder: clinical developments 5 years after discovery. Curr Psychiatry Rep. (2019) 21:80. doi: 10.1007/s11920-019-1066-4
32. Bernal M, Haro JM, Bernert S, Brugha T, Graaf R, de Bruffaerts R, et al. Risk factors for suicidality in Europe: results from the ESEMED study. J Affect Disord. (2007) 101:27–34. doi: 10.1016/j.jad.2006.09.018
33. Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med. (2009) 6:e1000123. doi: 10.1371/journal.pmed.1000123
34. Panagioti M, Gooding PA, Tarrier N. A meta-analysis of the association between posttraumatic stress disorder and suicidality: the role of comorbid depression. Compr Psychiatry. (2012) 53:915–30. doi: 10.1016/j.comppsych.2012.02.009
35. Panagioti M, Gooding P, Tarrier N. Post-traumatic stress disorder and suicidal behavior: a narrative review. Clin Psychol Rev. (2009) 29:471–82. doi: 10.1016/j.cpr.2009.05.001
36. Gradus JL. Prevalence and prognosis of stress disorders: a review of the epidemiologic literature. Clin Epidemiol. (2017) 9:251–60. doi: 10.2147/CLEP.S106250
37. Krysinska K, Lester D. Post-traumatic stress disorder and suicide risk: a systematic review. Arch Suicide Res. (2010) 14:1–23. doi: 10.1080/13811110903478997
38. Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. (1999) 56:617–26. doi: 10.1001/archpsyc.56.7.617
39. Gradus JL, Qin P, Lincoln AK, Miller M, Lawler E, Sørensen HT, et al. Posttraumatic stress disorder and completed suicide. Am J Epidemiol. (2010) 171:721–7. doi: 10.1093/aje/kwp456
40. Bryan CJ, Grove JL, Kimbrel NA. Theory-driven models of self-directed violence among individuals with PTSD. Curr Opin Psychol. (2017) 14:12–7. doi: 10.1016/j.copsyc.2016.09.007
41. May AM, Klonsky ED. What distinguishes suicide attempters from suicide ideators? A meta-analysis of potential factors. Clin Psychol Sci Pract. (2016) 23:5–20. doi: 10.1111/cpsp.12136
42. Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. (2012) 73:e1160–7. doi: 10.4088/JCP.11r07586
43. Krakow B, Artar A, Warner TD, Melendrez D, Johnston L, Hollifield M, et al. Sleep disorder, depression, and suicidality in female sexual assault survivors. Crisis. (2000) 21:163–70. doi: 10.1027//0227-5910.21.4.163
44. Malik S, Kanwar A, Sim LA, Prokop LJ, Wang Z, Benkhadra K, et al. The association between sleep disturbances and suicidal behaviors in patients with psychiatric diagnoses: a systematic review and meta-analysis. Syst Rev. (2014) 3:18. doi: 10.1186/2046-4053-3-18
45. Pigeon WR, Bishop TM, Titus CE. The relationship between sleep disturbance, suicidal ideation, suicide attempts, and suicide among adults: a systematic review. Psychiatr Ann. (2016) 46:177–86. doi: 10.3928/00485713-20160128-01
46. Betts KS, Williams GM, Najman JM, Alati R. The role of sleep disturbance in the relationship between post-traumatic stress disorder and suicidal ideation. J Anxiety Disord. (2013) 27:735–41. doi: 10.1016/j.janxdis.2013.09.011
47. Dell'Osso L, Massimetti G, Conversano C, Bertelloni CA, Carta MG, Ricca V, et al. Alterations in circadian/seasonal rhythms and vegetative functions are related to suicidality in DSM-5 PTSD. BMC Psychiatry. (2014) 14:352. doi: 10.1186/s12888-014-0352-2
48. Davidson CL, Babson KA, Bonn-Miller MO, Souter T, Vannoy S. The impact of exercise on suicide risk: examining pathways through depression, PTSD, and sleep in an inpatient sample of veterans. Suicide Life Threat Behav. (2013) 43:279–89. doi: 10.1111/sltb.12014
49. Bishop TM, Pigeon WR, Possemato K. Sleep disturbance and its association with suicidal ideation in veterans. Mil Behav Health. (2013) 1:81–4. doi: 10.1080/21635781.2013.830061
50. Bryan CJ, Clemans TA, Hernandez AM, Rudd MD. Loss of consciousness, depression, posttraumatic stress disorder, and suicide risk among deployed military personnel with mild traumatic brain injury. J Head Trauma Rehabil. (2013) 28:13–20. doi: 10.1097/HTR.0b013e31826c73cc
51. Chakravorty S, Grandner MA, Mavandadi S, Perlis ML, Sturgis EB, Oslin DW. Suicidal ideation in veterans misusing alcohol: relationships with insomnia symptoms and sleep duration. Addict Behav. (2014) 39:399–405. doi: 10.1016/j.addbeh.2013.09.022
52. Don Richardson J, St. Cyr K, Nelson C, Elhai JD, Sareen J. Sleep disturbances and suicidal ideation in a sample of treatment-seeking Canadian Forces members and veterans. Psychiatry Res. (2014) 218:118–23. doi: 10.1016/j.psychres.2014.04.008
53. Pigeon WR, Britton PC, Ilgen MA, Chapman B, Conner KR. Sleep disturbance preceding suicide among veterans. Am J Public Health. (2012) 102 (Suppl. 1):S93–7. doi: 10.2105/AJPH.2011.300470
54. Ribeiro JD, Pease JL, Gutierrez PM, Silva C, Bernert RA, Rudd MD, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord. (2012) 136:743–50. doi: 10.1016/j.jad.2011.09.049
55. Swinkels CM, Ulmer CS, Beckham JC, Buse N, Calhoun PS. The association of sleep duration, mental health, and health risk behaviors among US Afghanistan/Iraq Era veterans. Sleep. (2013) 36:1019–25. doi: 10.5665/sleep.2800
56. Bishop TM, Walsh PG, Ashrafioun L, Lavigne JE, Pigeon WR. Sleep, suicide behaviors, and the protective role of sleep medicine. Sleep Med. (2019) 66:264–70. doi: 10.1016/j.sleep.2019.07.016
57. Britton PC, McKinney JM, Bishop TM, Pigeon WR, Hirsch JK. Insomnia and risk for suicidal behavior: a test of a mechanistic transdiagnostic model in veterans. J Affect Disord. (2019) 245:412–8. doi: 10.1016/j.jad.2018.11.044
58. Bryan CJ, Gonzales J, Rudd MD, Bryan AO, Clemans TA, Ray-Sannerud B, et al. Depression mediates the relation of insomnia severity with suicide risk in three clinical samples of U. S military personnel Depress Anxiety. (2015) 32:647–55. doi: 10.1002/da.22383
59. Don Richardson J, King L, St Cyr K, Shnaider P, Roth ML, Ketcheson F, et al. Depression and the relationship between sleep disturbances, nightmares, and suicidal ideation in treatment-seeking Canadian Armed Forces members and veterans. BMC Psychiatry. (2018) 18:204. doi: 10.1186/s12888-018-1782-z
60. Fisher K, Houtsma C, Assavedo BL, Green BA, Anestis MD. Agitation as a moderator of the relationship between insomnia and current suicidal ideation in the military. Arch Suicide Res. (2017) 21:531–43. doi: 10.1080/13811118.2016.1193077
61. Kachadourian LK, Harpaz-Rotem I, Tsai J, Southwick SM, Pietrzak RH. Posttraumatic stress disorder symptoms, functioning, and suicidal ideation in, U. S, Military Veterans: a symptomics approach. Prim Care Companion CNS Disord. (2019) 21:18m02402. doi: 10.4088/PCC.18m02402
62. Kim JI, Park H, Kim J-H. Alcohol use disorders and insomnia mediate the association between PTSD symptoms and suicidal ideation in Korean firefighters. Depress Anxiety. (2018) 35:1095–103. doi: 10.1002/da.22803
63. Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. (2011) 34:1189–95. doi: 10.5665/SLEEP.1236
64. McClure JR, Criqui MH, Macera CA, Ji M, Nievergelt CM, Zisook S. Prevalence of suicidal ideation and other suicide warning signs in veterans attending an urgent care psychiatric clinic. Compr Psychiatry. (2015) 60:149–55. doi: 10.1016/j.comppsych.2014.09.010
65. Morgan JK, Hourani L, Tueller S, Strange L, Lane ME, Lewis GF. Effects of sleep issues on suicidal ideation in a military sample: the mediating role of mental health. Mil Behav Health. (2018) 6:234–42. doi: 10.1080/21635781.2017.1406415
66. Pigeon WR, Funderburk JS, Cross W, Bishop TM, Crean HF. Brief CBT for insomnia delivered in primary care to patients endorsing suicidal ideation: a proof-of-concept randomized clinical trial. Transl Behav Med. (2019) 9:1169–77. doi: 10.1093/tbm/ibz108
67. Ribeiro SP, LaCroix JM, Oliveira F, de Novak LA, Lee-Tauler SY, Darmour CA, et al. The link between posttraumatic stress disorder and functionality among united states military service members psychiatrically hospitalized following a suicide crisis. Healthcare. (2018) 6:1–13. doi: 10.3390/healthcare6030095
68. Richardson JD, Thompson A, King L, Corbett B, Shnaider P, St Cyr K, et al. Insomnia, psychiatric disorders and suicidal ideation in a national representative sample of active Canadian forces members. BMC Psychiatry. (2017) 17:211. doi: 10.1186/s12888-017-1372-5
69. Selaman ZMH, Chartrand HK, Bolton JM, Sareen J. Which symptoms of post-traumatic stress disorder are associated with suicide attempts? J Anxiety Disord. (2014) 28:246–51. doi: 10.1016/j.janxdis.2013.12.005
70. Wang HE, Campbell-Sills L, Kessler RC, Sun X, Heeringa SG, Nock MK, et al. Pre-deployment insomnia is associated with post-deployment post-traumatic stress disorder and suicidal ideation in, US, Army soldiers. Sleep. (2019) 42:1–9. doi: 10.1093/sleep/zsy229
71. Littlewood DL, Gooding PA, Panagioti M, Kyle SD. Nightmares and suicide in posttraumatic stress disorder: the mediating role of defeat, entrapment, and hopelessness. J Clin Sleep Med. (2016) 12:393–9. doi: 10.5664/jcsm.5592
72. McCall WV, Pillai A, Case D, McCloud L, Nolla T, Branch F, et al. A pilot, randomized clinical trial of bedtime doses of prazosin versus placebo in suicidal posttraumatic stress disorder patients with nightmares. J Clin Psychopharmacol. (2018) 38:618–21. doi: 10.1097/JCP.0000000000000968
73. Raskind MA, Peskind ER, Chow B, Harris C, Davis-Karim A, Holmes HA, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. (2018) 378:507–17. doi: 10.1056/NEJMoa1507598
74. Bryant RA, Creamer M, O'Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. (2010) 33:69–74. doi: 10.1093/sleep/33.1.69
75. Milanak ME, Zuromski KL, Cero I, Wilkerson AK, Resnick HS, Kilpatrick DG. Traumatic event exposure, posttraumatic stress disorder, and sleep disturbances in a national sample of US adults. J Traumatic Stress. (2019) 32:14–22. doi: 10.1002/jts.22360
76. Gehrman P, Seelig AD, Jacobson IG, Boyko EJ, Hooper TI, Gackstetter GD, et al. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep. (2013) 36:1009–18. doi: 10.5665/sleep.2798
77. van Liempt S, van Zuiden M, Westenberg H, Super A, Vermetten E. Impact of impaired sleep on the development of PTSD symptoms in combat veterans: a prospective longitudinal cohort study. Depress Anxiety. (2013) 30:469–74. doi: 10.1002/da.22054
78. Raskind MA, Peterson K, Williams T, Hoff DJ, Hart K, Holmes H, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. (2013) 170:1003–10. doi: 10.1176/appi.ajp.2013.12081133
79. Khachatryan D, Groll D, Booij L, Sepehry AA, Schütz CG. Prazosin for treating sleep disturbances in adults with posttraumatic stress disorder: a systematic review and meta-analysis of randomized controlled trials. Gen Hosp Psychiatry. (2016) 39:46–52. doi: 10.1016/j.genhosppsych.2015.10.007
80. Gupta MA, Jarosz P. Obstructive sleep apnea severity is directly related to suicidal ideation in posttraumatic stress disorder. J Clin Sleep Med. (2018) 14:427–35. doi: 10.5664/jcsm.6992
81. Goodwin RD, Marusic A. Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep. (2008) 31:1097–101. doi: 10.5665/sleep/31.8.1097
82. Petrakis IL, Simpson TL. Posttraumatic stress disorder and alcohol use disorder: a critical review of pharmacologic treatments. Alcohol Clin Exp Res. (2017) 41:226–37. doi: 10.1111/acer.13297
83. Davis MT, Witte TK, Weathers FW, Blevins CA. The role of posttraumatic stress disorder symptom clusters in the prediction of passive suicidal ideation. Psychol Trauma. (2014) 6:S82–91. doi: 10.1037/a0035966
84. Bell JB, Nye EC. Specific symptoms predict suicidal ideation in Vietnam combat veterans with chronic post-traumatic stress disorder. Mil Med. (2007) 172:1144–7. doi: 10.7205/MILMED.172.11.1144
85. Boffa JW, Stanley IH, Hom MA, Norr AM, Joiner TE, Schmidt NB. PTSD symptoms and suicidal thoughts and behaviors among firefighters. J Psychiatr Res. (2017) 84:277–83. doi: 10.1016/j.jpsychires.2016.10.014
86. Zuromski KL, Davis MT, Witte TK, Weathers F, Blevins C. PTSD symptom clusters are differentially associated with components of the acquired capability for suicide. Suicide Life Threat Behav. (2014) 44:682–97. doi: 10.1111/sltb.12098
87. Guerra VS, Calhoun PS. Examining the relation between posttraumatic stress disorder and suicidal ideation in an OEF/OIF veteran sample. J Anxiety Disord. (2011) 25:12–8. doi: 10.1016/j.janxdis.2010.06.025
88. Horwitz AG, Miron L, Maieritsch KP. Prospective associations between DSM-5 PTSD symptom clusters and suicidal ideation in treatment-seeking veterans. Psychol Serv. (2019) 16:321–8. doi: 10.1037/ser0000215
89. Brown LA, Contractor A, Benhamou K. Posttraumatic stress disorder clusters and suicidal ideation. Psychiatry Res. (2018) 270:238–45. doi: 10.1016/j.psychres.2018.09.030
90. Panagioti M, Angelakis I, Tarrier N, Gooding P. A prospective investigation of the impact of distinct posttraumatic (PTSD) symptom clusters on suicidal ideation. Cognit Ther Res. (2017) 41:645–53. doi: 10.1007/s10608-016-9829-2
91. Stanley IH, Rogers ML, Hanson JE, Gutierrez PM, Joiner TE. PTSD symptom clusters and suicide attempts among high-risk military service members: a three-month prospective investigation. J Consult Clin Psychol. (2019) 87:67–78. doi: 10.1037/ccp0000350
92. Jakupcak M, Cook J, Imel Z, Fontana A, Rosenheck R, McFall M. Posttraumatic stress disorder as a risk factor for suicidal ideation in Iraq and Afghanistan War veterans. J Trauma Stress. (2009) 22:303–6. doi: 10.1002/jts.20423
93. Littlewood DL, Gooding PA, Panagioti M, Kyle SD. Investigating psychological mechanisms in relation to sleep problems and suicide. J Clin Sleep Med. (2016) 12:931. doi: 10.5664/jcsm.5910
94. Woodward SH, Friedman MJ, Bliwise DL. Sleep and depression in combat-related PTSD inpatients. Biol Psychiatry. (1996) 39:182–92. doi: 10.1016/0006-3223(95)00104-2
95. Werner KB, Griffin MG, Galovski TE. Objective and subjective measurement of sleep disturbance in female trauma survivors with posttraumatic stress disorder. Psychiatry Res. (2016) 240:234–40. doi: 10.1016/j.psychres.2016.04.039
96. Gehrman PR, Harb GC, Cook JM, Barilla H, Ross RJ. Sleep diaries of Vietnam War veterans with chronic PTSD: the relationships among insomnia symptoms, psychosocial stress, and nightmares. Behav Sleep Med. (2015) 13:255–64. doi: 10.1080/15402002.2014.880344
97. Ronzitti S, Loree AM, Potenza MN, Decker SE, Wilson SM, Abel EA, et al. Gender differences in suicide and self-directed violence risk among veterans with post-traumatic stress and substance use disorders. Women's Health Issues. (2019) 29(Suppl. 1):S94–102. doi: 10.1016/j.whi.2019.04.010
98. LeBouthillier DM, McMillan KA, Thibodeau MA, Asmundson Gordon JG. Types and number of traumas associated with suicidal ideation and suicide attempts in PTSD: findings from a US Nationally representative sample J Traumatic Stress. (2015) 28:183–90. doi: 10.1002/jts.22010
99. Eaton KM, Messer SC, Garvey Wilson AL, Hoge CW. Strengthening the validity of population-based suicide rate comparisons: an illustration using US military and civilian data. Suicide Life Threat Behav. (2006) 36:182–91. doi: 10.1521/suli.2006.36.2.182
100. Rothberg JM, Bartone PT, Holloway HC, Marlowe DH. Life and death in the, U. S, army in corpore sano JAMA. (1990) 264:2241–4. doi: 10.1001/jama.1990.03450170089028
101. Kuehn BM. Soldier suicide rates continue to rise: military, scientists work to stem the tide. JAMA. (2009) 301:1111–3. doi: 10.1001/jama.2009.342
102. Hoge CW, Castro CA. Preventing suicides in, U. S, service members and veterans: concerns after a decade of war. JAMA. (2012) 308:671–2. doi: 10.1001/jama.2012.9955
103. Conner KR, Bohnert AS, McCarthy JF, Valenstein M, Bossarte R, Ignacio R, et al. Mental disorder comorbidity and suicide among 2.96 million men receiving care in the Veterans Health Administration health system. J. Abnorm. Psychol. (2013) 122:256–63. doi: 10.1037/a0030163
104. Hyman J, Ireland R, Frost L, Cottrell L. Suicide incidence and risk factors in an active duty, U. S, military population. Am J Public Health. (2012) 102(Suppl. 1):S138–46. doi: 10.2105/AJPH.2011.300484
105. Ilgen MA, Bohnert ASB, Ignacio RV, McCarthy JF, Valenstein MM, Kim HM, et al. Psychiatric diagnoses and risk of suicide in veterans. Arch Gen Psychiatry. (2010) 67:1152–8. doi: 10.1001/archgenpsychiatry.2010.129
106. LeardMann CA, Powell TM, Smith TC, Bell MR, Smith B, Boyko EJ, et al. Risk factors associated with suicide in current and former, U. S, military personnel. JAMA. (2013) 310:496–506. doi: 10.1001/jama.2013.65164
107. Bullman T, Schneiderman A, Gradus JL. Relative importance of posttraumatic stress disorder and depression in predicting risk of suicide among a cohort of vietnam veterans. Suicide Life Threat Behav. (2019) 49:838–45. doi: 10.1111/sltb.12482
108. Conner KR, Bossarte RM, He H, Arora J, Lu N, Tu XM, et al. Posttraumatic stress disorder and suicide in 5.9 million individuals receiving care in the veterans health administration health system. J Affect Disord. (2014) 166:1–5. doi: 10.1016/j.jad.2014.04.067
109. Shen YC, Cunha JM, Williams TV. Time-varying associations of suicide with deployments, mental health conditions, and stressful life events among current and former, US military personnel: a retrospective multivariate analysis. Lancet Psychiatry. (2016) 3:1039–48. doi: 10.1016/S2215-0366(16)30304-2
110. Zivin K, Kim HM, McCarthy JF, Austin KL, Hoggatt KJ, Walters H, et al. Suicide mortality among individuals receiving treatment for depression in the Veterans Affairs health system: associations with patient and treatment setting characteristics. Am J Public Health. (2007) 97:2193–8. doi: 10.2105/AJPH.2007.115477
111. Gradus JL. Posttraumatic stress disorder and death from suicide. Curr Psychiatry Rep. (2018) 20:98. doi: 10.1007/s11920-018-0965-0
Keywords: sleep, sleep disorders, suicidality, PTSD (post-traumatic stress disorder), insomnia, nightmares
Citation: Weber FC, Norra C and Wetter TC (2020) Sleep Disturbances and Suicidality in Posttraumatic Stress Disorder: An Overview of the Literature. Front. Psychiatry 11:167. doi: 10.3389/fpsyt.2020.00167
Received: 08 November 2019; Accepted: 21 February 2020;
Published: 10 March 2020.
Edited by:
Anastasia Theodoridou, Psychiatric University Hospital Zurich, SwitzerlandReviewed by:
Leonardo Afonso Dos Santos, University of São Paulo, BrazilRobert Göder, University Medical Center Schleswig-Holstein, Germany
Copyright © 2020 Weber, Norra and Wetter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thomas C. Wetter, dGhvbWFzLndldHRlckBtZWRiby5kZQ==
 Franziska C. Weber
Franziska C. Weber Christine Norra2
Christine Norra2 Thomas C. Wetter
Thomas C. Wetter