- Department of Biomedical Sciences, University of North Dakota, Grand Forks, ND, United States
Background: Immunology is a complex subject that students and instructors often find challenging. Active learning (AL) strategies, particularly patient-centered learning (PCL) within a team-based learning (TBL) framework, may enhance student engagement and conceptual understanding while fostering clinical reasoning and empathy development.
Methods: This study examines the effectiveness of PCL case studies in an undergraduate immunology course at a public R1 university. Students engaged in multi-day case studies, analyzing patient histories, symptoms, diagnostic results, and treatment plans while integrating foundational immunology concepts. Data were collected through end-of-course evaluations, including a Likert-scale item (quantitative) and two open-ended questions (qualitative).
Results: Students reported high agreement (mean = 4.72, SD = 0.74) that PCL enhanced their understanding of immunology. Thematic analysis of open-ended responses revealed six key learning outcomes, including real-world application, critical thinking, preparation for medical careers, and patient connection. Additionally, students identified diagnostic reasoning, problem-solving, and teamwork as skills gained. However, empathy was not explicitly mentioned, suggesting a need for more structured reflection-based activities in undergraduate coursework.
Conclusion: PCL improves concept mastery, clinical reasoning, and diagnostic skills in undergraduate immunology education. However, while case studies introduced patient-centered elements, students did not self-report increased empathy. Future course designs should incorporate intentional scaffolding of empathy development, such as guided reflections and interprofessional discussions, to better integrate scientific knowledge with humanistic awareness.
Introduction
Immunology has long been regarded by students as a difficult subject to understand (Bansal, 1997). This sentiment is mirrored by instructors who often describe immunology as a particularly challenging subject to teach (Siani et al., 2024). A combination of intricate networks, multiple components, and lack of an understanding of the basics, all make for a course that can quickly become overwhelming for many medical and pre-health students. Even more challenging for students and educators alike is the content for undergraduate immunology courses having swelled in the last decade to include emerging topics and a deeper understanding of foundational immunology topics (Bauer et al., 2024). Regardless, immunology is a constantly evolving, critical subject for future healthcare professionals to grasp. Undergraduate immunology guidelines outline the importance of students understanding the foundational biochemical underpinnings of the discipline (Pandey et al., 2024; Porter et al., 2021), while the Infectious Disease Society of America (IDSA) highlights the need of this knowledge when developing differential diagnoses, ordering diagnostic tests, and developing treatment plans (Southwick et al., 2010). Nearly every clinical discipline integrates immunology concepts, whether in the context of pathophysiology, diagnostic testing, or immunotherapy.
With advancements in teaching and learning methodologies, approaches to teaching immunology have evolved. The complexity of the human body necessitates interdisciplinary learning, where students must synthesize knowledge from multiple fields to solve real-world clinical problems. This creates an opportunity to embed active learning (AL) strategies that encourage critical thinking and collaborative problem-solving (Amarilla et al., 2022). AL, particularly through social construction of knowledge, has been shown to help students grasp complex immunological concepts more effectively (Stranford et al., 2020). When instructors design activities that connect basic immunological principles with clinical applications, students not only enhance their immunological literacy but also improve their ability to apply these concepts in practical, patient scenarios (Haidaris and Frelinger, 2019).
This article describes an AL approach that integrates patient-centered learning (PCL) within a team-based learning (TBL) framework to enhance students’ understanding of immunology while simultaneously fostering the development of empathy. Traditional case-based learning (CBL) originated, and is still widely used, in medical education to connect basic science concepts to clinical applications (Svinicki, 2004). However, this PCL-TBL approach extends beyond standard CBL by intentionally embedding patient perspectives throughout the case, allowing students to engage not only with scientific clinical reasoning but also with the human experience of illness. The PCL approach described herein is adapted from a well-established PCL model at the same institution that has been a core component of the medical curriculum since 2010, now applied to the undergraduate immunology course.
In this model, students work in teams to progressively analyze patient histories, clinical symptoms, laboratory results, and treatment decisions while also considering the emotional, ethical, and social dimensions of patient care. By engaging in PCL, students are encouraged to approach immunology not as a purely mechanistic science but as a discipline deeply connected to real-world patient experiences. The overarching goal of using PCL is to extend the grasp of immunologic concepts beyond the textbook to increase comprehension of immunology and its ubiquitous presence in the world, specifically in healthcare. This integration of empathy-building exercises within case-based immunology instruction represents an innovative pedagogical approach that supports both scientific competency and humanistic awareness—two essential qualities for future healthcare professionals. Additionally, a passion for helping others is often a driving force behind pursuing a career in medicine, and this approach helps to nurture that desire by emphasizing the human side of healthcare.
Despite the widespread use of CBL and TBL, limited research has explored their impact on conceptual comprehension and the development of empathy in undergraduate immunology education. This article examines how a structured, patient-centered approach to immunology instruction influences student engagement, perceptions of conceptual mastery, and their ability to connect immunological principles to patient care. By presenting a method for integrating empathy into CBL, this work offers an adaptable model for improving both scientific understanding and patient-centered thinking in pre-health education.
Pedagogical framework
The constructivist learning theory, championed by educational theorists such as John Dewey, Jean Piaget, and Lev Vygotsky, describes that learners actively build knowledge through experiences rather than passively absorbing information (Brooks and Brooks, 1993). In a constructivist classroom, students engage in problem-solving within meaningful contexts and construct understanding by integrating prior knowledge with new information. For difficult subjects like immunology, students enjoy thinking critically when content is clinically relevant (Bansal, 1997).
AL is a core instructional strategy that facilitates knowledge construction by engaging students in learning activities that promotes interaction with content, collaboration with peers, and knowledge application. Extensive research supports the success of AL particularly in STEM disciplines (Freeman et al., 2014). Incorporating content within clinically relevant scenarios is a widely adopted method to enhance active learning in health professional education. This technique effectively integrates structured and guided learning, leading to improved student outcomes (Smith et al., 2014; Thistlethwaite et al., 2012). In immunology education, AL methods such as case-based discussions, team-based problem-solving, and inquiry-driven exploration provide students with opportunities to contextualize theoretical knowledge and develop an understanding of underlying mechanisms. Additionally, innovative teaching methods that move away from traditional immunology lectures can have a positive influence on students’ future interest in infectious disease specialties (Cervantes, 2020).
One structured approach to AL that has been particularly effective in health sciences education is TBL. TBL is a highly structured, collaborative, constructive strategy designed to promote engagement, critical thinking, and retention (James et al., 2019). A critical element of TBL is the facilitation of discussion, which requires a balance of allowing students to have independent discussions and integrating faculty perspective. Students need the space to grapple with the content and fit it into their existing schema, yet guidance needs to be available to avoid frustration and bring clarity to why particular answers are right or wrong. This often creates engaging, high-energy, interactive classroom environments that are less predictable and more dynamic than traditional lecture courses (Kibble et al., 2016).
While TBL provides a structured, collaborative framework for AL, CBL further enhances student engagement by grounding basic science concepts in clinically relevant scenarios. The primary goal of CBL is to prepare students for clinical practice by linking theory to method through the application of knowledge in real-world contexts (Thistlethwaite et al., 2012). When basic science content is delivered in a clinically meaningful way, students are more likely to retain and apply this knowledge in future clinical settings (Anderson et al., 2020; Yang et al., 2024; Zhang and Hu, 2024). This is particularly relevant in immunology education, where understanding cellular pathways and processes, immune system dysfunction, and disease pathology is essential for diagnosing and treating patients.
Effective case design is crucial for maximizing the benefits of CBL. When developing a case, utilizing Backward design principles (UbD) ensure that content and related questions are aligned with defined learning outcomes (Wiggins and McTighe, 2005). Novack (2020) recommends that cases should be designed to encourage students to begin with foundational concepts, then progressively work through more complex clinical reasoning tasks. Incorporating questions about molecular mechanisms helps students make connections between basic immunological principles and patient clinical presentations, reinforcing reasoning skills. The IDSA further emphasizes the importance of incorporating questions to foster the understanding of pathogenesis, organ-specific effects, and diagnostic approaches (Southwick et al., 2010). Additionally, learning progressions in CBL should incorporate systems thinking and mechanistic reasoning, guiding students toward a comprehensive understanding of immune function in health and disease (Siani et al., 2024).
PCL epitomizes these strategies while also aiming to cultivate empathy, a critical competency for future healthcare professionals. Empathy in healthcare is defined as the ability to identify and understand a patient’s perspective without losing objectivity, as well as to recognize patients’ emotions and respond appropriately (Zhou et al., 2021). While traditional CBL focuses primarily on clinical reasoning, PCL embeds personal patient narratives within case studies. This provides students with opportunities to engage with the human experience of illness, fostering deeper emotional and ethical awareness. Empathy in clinicians contributes to greater wellbeing, stronger doctor-patient relationships, and improved clinical competence (Del Canale et al., 2012; Hojat et al., 2011). This is further exemplified from the patient’s perspective, where empathetic healthcare interactions have been linked to higher satisfaction and improved adherence to therapy, underscoring the importance of empathy in healthcare (Noordman et al., 2019; Zhou et al., 2021). Traditional pre-health science curricula often focus solely on technical knowledge, while leaving out the development of interpersonal skills. Ultimately, students may not be well-rounded and fully prepared for real-world patient interactions.
Used in conjunction, these techniques—AL, TBL, and CBL—form the foundation of the PCL approach described in this study. Furthermore, by incorporating patient narratives and ethical considerations, PCL extends beyond traditional case-based methods to foster empathy and patient-centered thinking, ensuring that students not only understand immunological mechanisms but also appreciate the human impact of immune-related diseases.
Learning environment
Course description
Introduction to Immunology is a 300-level lecture-based undergraduate course at an R1, public research university. The course covers fundamentals of the human immune system including innate immunity, humoral and cellular response, hypersensitivity, immunodeficiency, immunogenetics, tolerance, and immunodiagnostics. It meets face-to-face three times per week for 50-min sessions. By the end of the course, students are expected to demonstrate a basic, yet comprehensive understanding of the human immune system. Specific to this article, the following course learning objectives are most relevant:
• Identify the organs of the immune system and their functions.
• Analyze real-world problems related to immunology.
• Formulate conclusions related to immunological diseases/disorders.
Student profile
This course primarily enrolls junior and senior biology majors, most of whom are pursuing a pre-health track. These students typically have strong foundational knowledge in biology and chemistry, having completed prerequisite coursework in general biology, genetics, and biochemistry. The course serves as an upper-level biology elective and is particularly relevant for students preparing for professional programs in medicine, dentistry, optometry, and other health sciences fields.
Instructors
The course section specific to this article was held in the fall semester of 2024 and led by a faculty member in the Department of Biomedical Sciences (Instructor). The instructor was responsible for course design, content development, and primary instruction. Additionally, a graduate teaching assistant (GTA) assisted in content delivery and grading. The GTA played a central role in facilitating student engagement during AL activities. The instructor utilized a hybrid lecture-AL approach, dedicating approximately one-third of each class period to traditional lecture and the remaining two-thirds to student-centered learning activities. The GTA supported these activities by interacting with student groups, clarifying concepts, and reinforcing immunological principles.
Pedagogical format
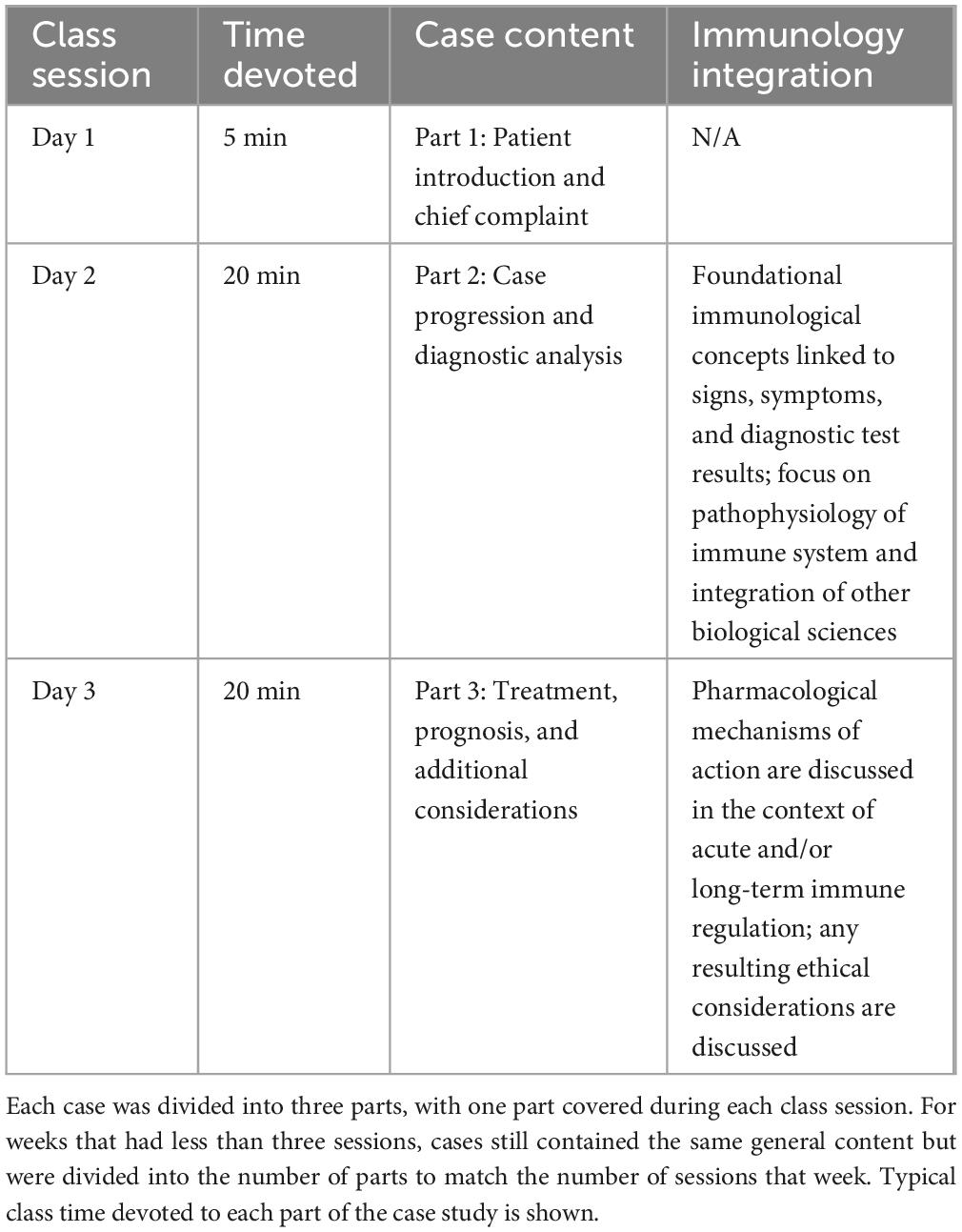
The course employed a PCL case study approach, integrating CBL with traditional lecture content to reinforce immunological concepts in a clinically relevant context. Each week, student teams of 5–6 explored a new patient case, designed using UbD that aligned with the immunological topics covered in the corresponding chapter and addressed the course learning objectives. Throughout the semester there were 15 case studies completed (see Supplementary Materials). Table 1 displays a breakdown of the case progression on a typical week.
Each week at the end of the first class session (day 1) students were introduced to a patient in part 1 of the case study (see Figure 1). They learned the patient’s name, a little about their background, and their chief complaint. There was also a picture of the patient included in this introductory information. This brief introduction was designed to help students get to know the patient and begin to develop empathy. Without prompting, students naturally engaged in group discussions about possible underlying conditions and began to develop a differential diagnosis.
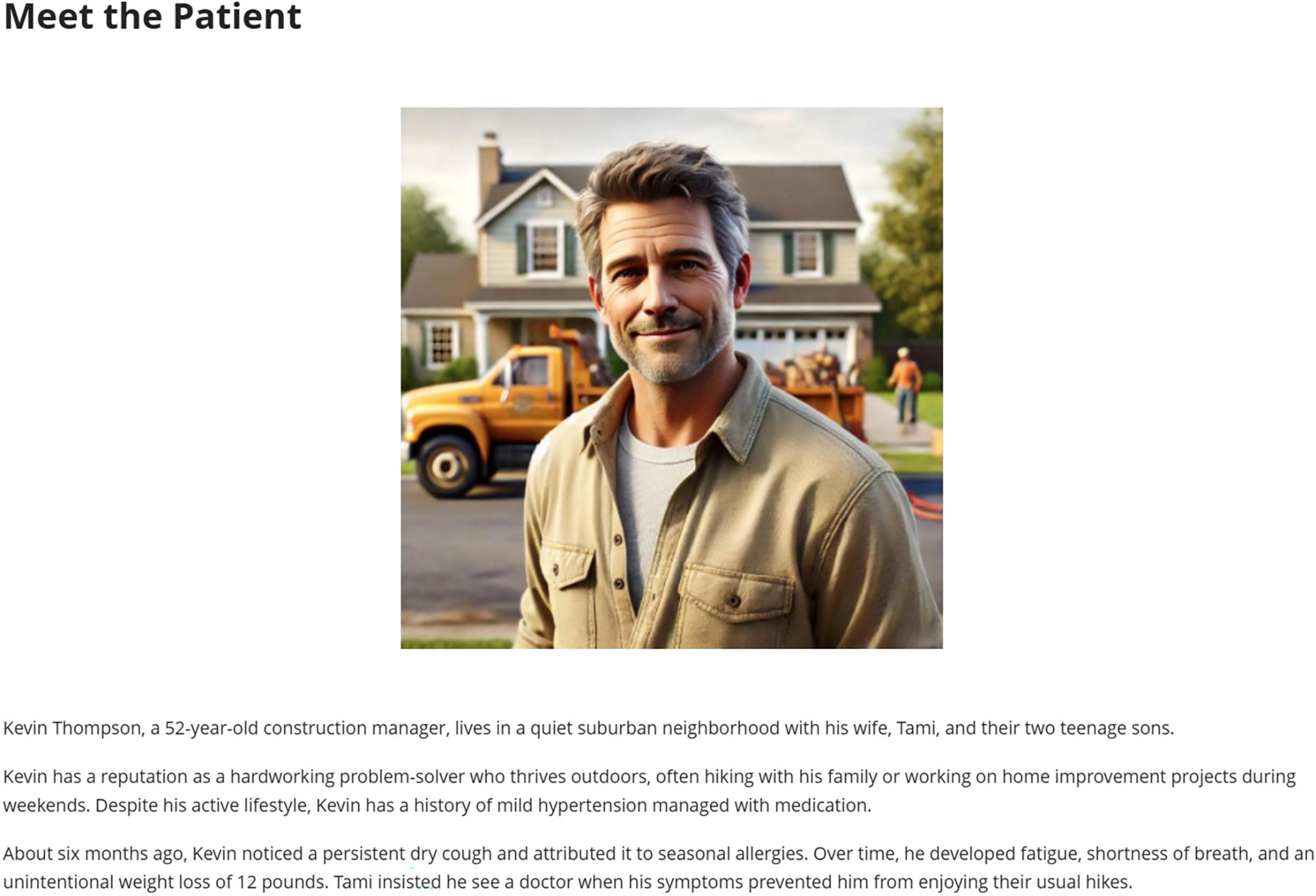
Figure 1. Part 1 of case study. On the first day of a case study students were introduced to the patient, saw an AI-generated picture of them, learned a little about their background, and heard their chief complaint in a Blackboard module.
On day 2, students worked through part 2 of the case study, learning additional clinical details, including signs, symptoms, and diagnostic test results. Embedded questions guided students in connecting clinical findings to foundational immunological mechanisms, utilizing both new information learned that week and building on knowledge from previous chapters. Collaboratively, students worked toward determining a final diagnosis for their patient and understanding the immunological underpinnings of the case.
Students wrapped up the case study on day 3 by exploring treatment options and potential long-term management. The integration of immunology concepts focused on the mechanism of action of therapeutics specifically related to immunological processes and clinical outcomes. When applicable, Part 3 also included ethical considerations for the students to discuss in their groups, aimed to garner empathy for the patient and their families. The denouement of this multi-session PCL case study was to help students grasp the broader, ubiquitous impact of immunology on society and the importance of responsible decision-making in healthcare.
Students used the course LMS (Blackboard) to answer embedded questions in all three parts of the case. Although students discussed the case in teams, each student submitted their own responses. These scored questions provided immediate feedback without revealing the correct answers, allowing re-attempts to reinforce learning, and encourage discussion among teams.
Data collection and measures
At the end of the semester, 36 students (28 seniors, 7 juniors, and 1 sophomore) completed the university’s standard Student Evaluation of Learning and Feedback for Instruction (SELFI), administered by the institution. As part of this evaluation, three additional questions were incorporated to assess the impact of the patient-centered case studies on student learning. These questions included both quantitative and qualitative measures.
Quantitative analysis
The quantitative measure consisted of a Likert-scale item, where students rated their agreement (Strongly Agree = 5 to Strongly Disagree = 1) with the statement:
“The patient-centered case studies each chapter helped me better understand complex immunologic concepts.”
Responses were analyzed by calculating the percentage breakdown for each of the five response categories. The mean score and standard deviation were computed to summarize overall agreement with the statement.
In addition to the Likert-scale question, one open-ended question, “Describe some aspects of this course that promoted your learning,” was analyzed quantitatively using a content analysis approach. Student responses were examined to determine the frequency of mentions of three instructional strategies: AL, TBL, and CBL. Each response was reviewed, and a tally was recorded for the number of students who explicitly referenced each strategy. The total counts for each category were calculated to assess the prominence of these themes in student reflections.
Qualitative analysis
The qualitative component included two open-ended questions to capture students’ perspectives on the effectiveness of the case studies:
1. “In what ways did the patient-centered case studies enhance or challenge your understanding of immunology concepts?”
2. “What skills do you feel you gained or improved upon by working through the patient-centered case studies?”
A thematic analysis was conducted for these questions. Each student response was independently coded by the two authors, who reviewed the data separately to identify overarching themes. After independent coding, the authors compared their themes to resolve discrepancies and establish consensus on key findings. Comprehensive theme identification was achieved, ensuring that major concepts were well-represented in the final analysis.
Results
Quantitative results
Of the 36 students who responded to the Likert-scale question regarding the effectiveness of patient-centered case studies, the mean response was 4.72 (SD = 0.74), indicating a high level of agreement with the statement that case studies enhanced their understanding of immunologic concepts. Corresponding percent distribution of responses are displayed in Figure 2.
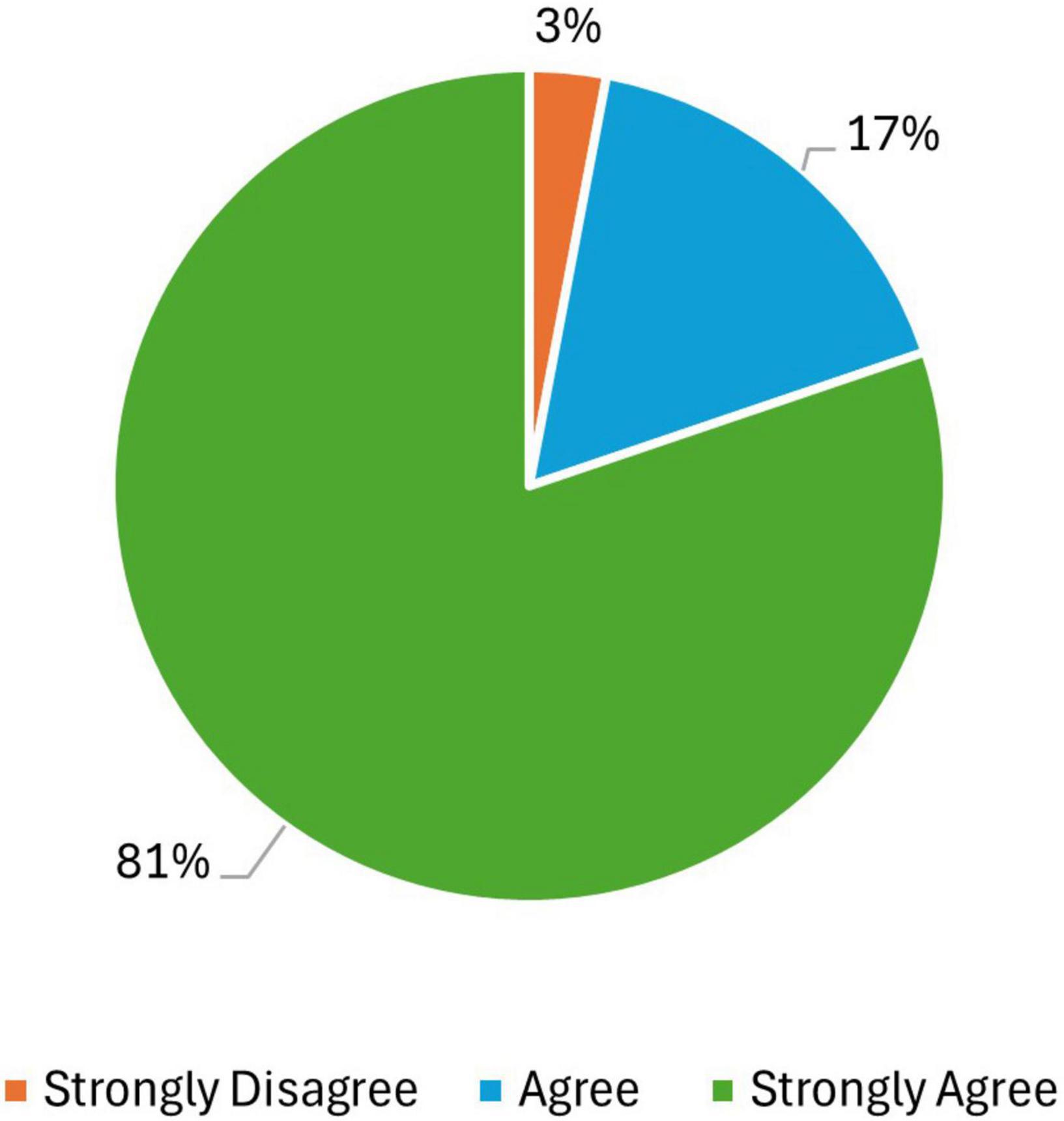
Figure 2. Distribution of student responses to the Likert-scale question: “The patient-centered case studies in each chapter helped me better understand complex immunologic concepts.” The majority of students (81%) selected Strongly Agree, followed by 17% selecting Agree, and 3% selecting Strongly Disagree. No students selected Neutral or Disagree.
Students were asked to describe aspects of the course that promoted their learning, and the frequency of instructional strategy mentions was recorded. The results are depicted in Figure 3. CBL emerged as the most frequently referenced approach, accounting for 61% (N = 22). Students highlighted its effectiveness in contextualizing immunologic concepts within real-world clinical scenarios.
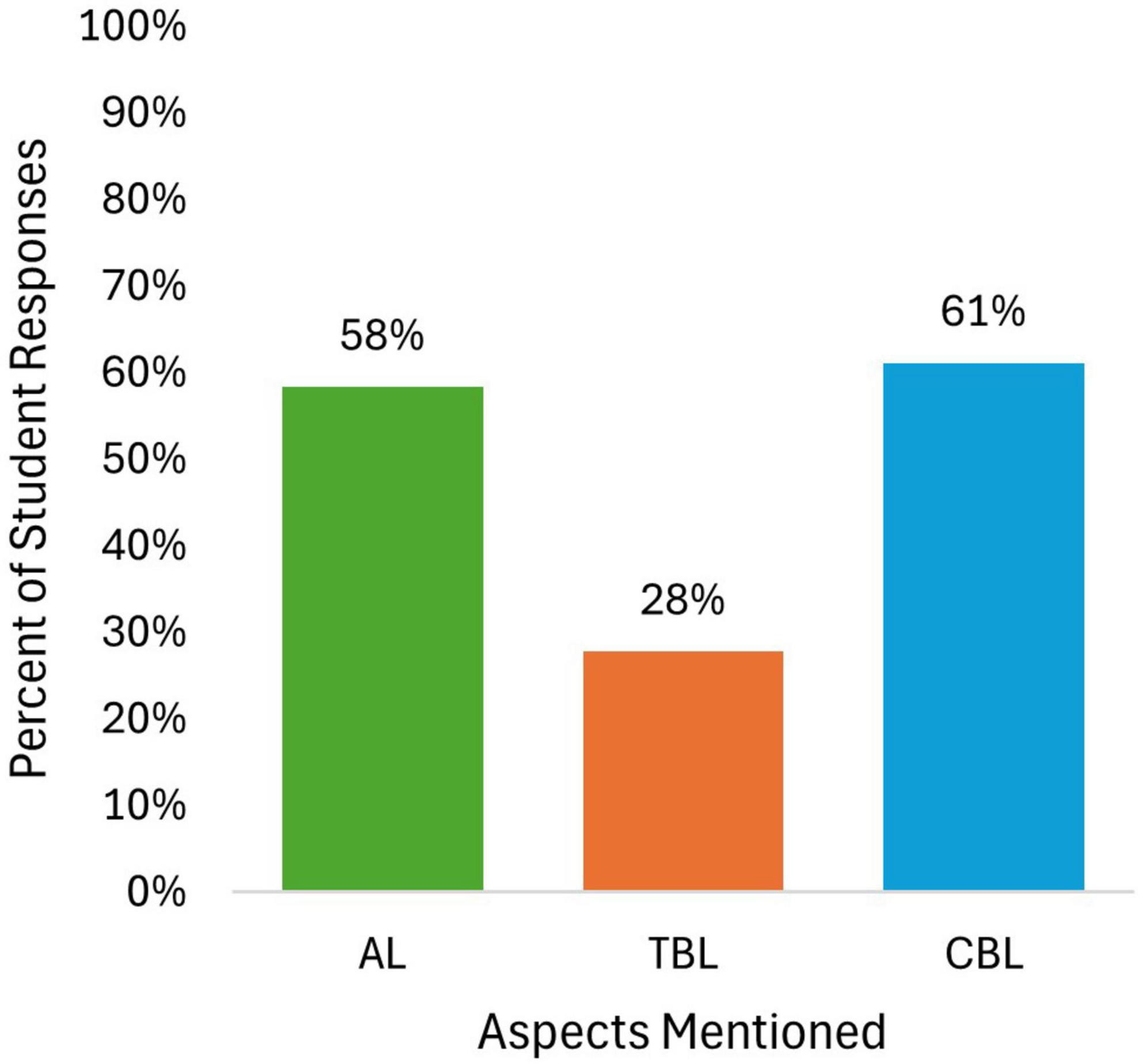
Figure 3. Percentage of student responses mentioning key instructional strategies in response to the question, “Describe some aspects of this course that promoted your learning.” Case-Based Learning (CBL) was the most frequently mentioned (61%), followed by Active Learning (AL; 58%) and Team-Based Learning (TBL; 28%).
“The case studies really helped me apply the information learned in a real world, clinical setting.”
AL was also commonly mentioned, constituting 58% (N = 21), with students noting its role in fostering engagement and deepening their understanding of key concepts.
“We also did in class activities that were creative and helped to visualize the concepts we were learning in class.”
TBL was less frequently referenced, at 28% (N = 10), although students who mentioned it described the benefits of peer collaboration and discussion in reinforcing fundamental concepts.
“I enjoyed the group learning format of the class. I like to bounce ideas off of others, so this definitely helped me learn.”
These findings indicate that students found case-based and active learning strategies particularly effective in enhancing their comprehension of immunology.
Qualitative results
Understanding of immunology concepts
Student responses to the question, “In what ways did the patient-centered case studies enhance or challenge your understanding of immunology concepts?” were analyzed to understand their perceptions of learning. Through thematic analysis, six major themes emerged: (1) Real-world Application; (2) Critical Thinking and Problem Solving; (3) Enhanced Understanding and Desire to Learn; (4) Preparation for Medical Careers; (5) Connection of Concepts; and (6) Patient Connection. A visual representation of the code frequency is shown in Figure 4A.
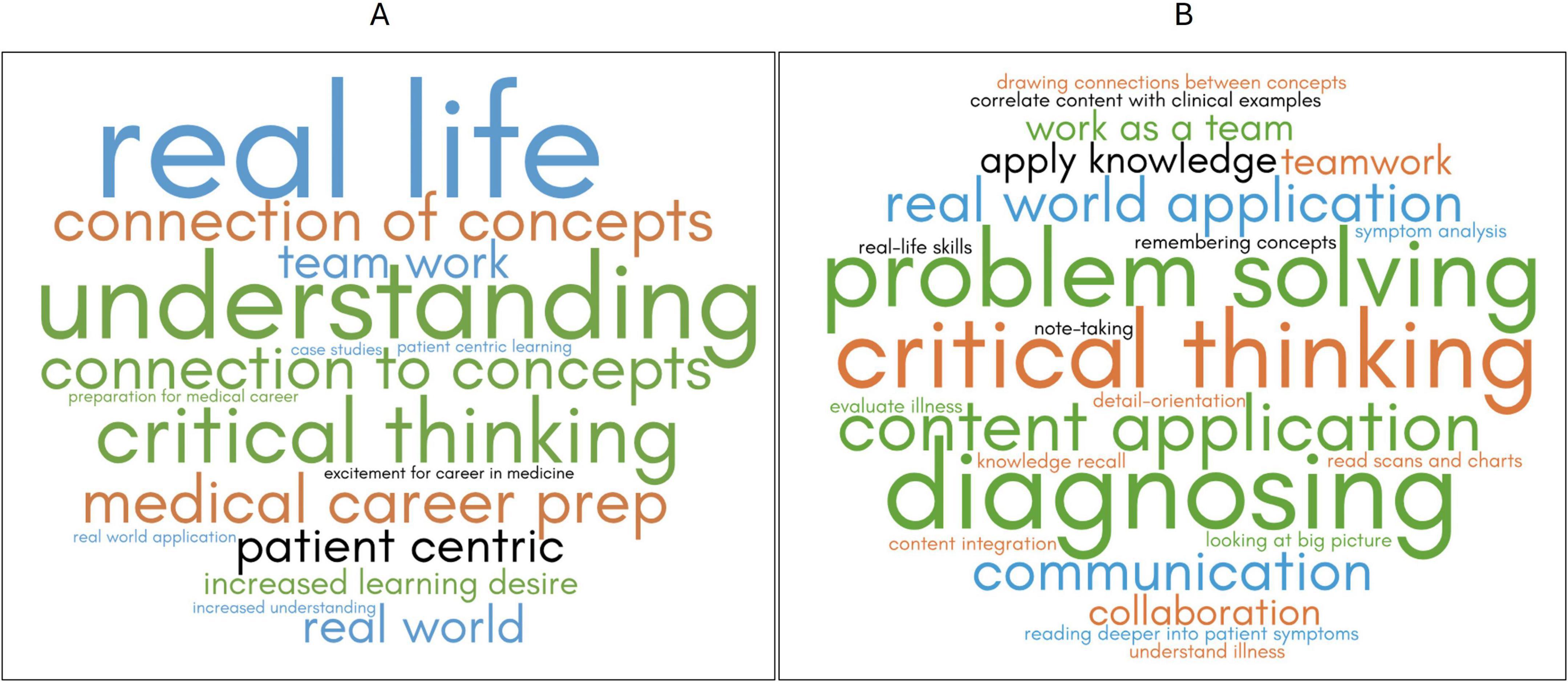
Figure 4. Word clouds representing student responses to qualitative questions about PCL. The larger the word, the more often the idea was mentioned. The size of each word corresponds to the frequency of its mention by students, while colors are used for visual distinction and do not carry specific meaning. (A) Codes from responses to the question, “In what ways did the patient-centered case studies enhance or challenge your understanding of immunology concepts?” (B) represents codes from responses to the question, “What skills do you feel you gained or improved upon by working through the patient-centered case studies?”
Real-world application
Over half of the students expressed that the case studies helped them connect immunological concepts to real-world scenarios. They highlighted how engaging with clinical cases allowed them to see how theoretical knowledge is applied in practice:
“These case studies enhanced my understanding by connecting it to the real world.”
“I enjoyed the case studies since they show how the material learned in the chapters is seen in real life. I think we learned a lot more and understood the content more through case studies.”
This theme suggests that students found value in bridging the gap between classroom learning and practical application, reinforcing the importance of contextualized learning.
Critical thinking and problem solving
One-third of students described how the case studies challenged them to think critically and problem-solve, often requiring them to analyze symptoms, make differential diagnoses, and synthesize multiple concepts:
“The case studies helped us learn to work as a team and use problem solving and critical thinking skills to come to a diagnosis. It was interesting to learn about the different ways diseases can present in a patient. It made me excited because it felt like we were treating patients and not just in a classroom.”
“I think they were often challenging, but I enjoyed that as it enhanced my learning and allowed me to apply the concepts learned in lecture to realistic scenarios. They also had images and explanations imbedded in them that made it easy to follow and helped me when I was stuck on a question.”
By engaging in these exercises, students demonstrated higher-order cognitive skills aligned with the upper levels of Bloom’s Taxonomy (Anderson and Krathwohl, 2001), moving beyond rote memorization toward meaningful knowledge integration.
Enhanced understanding and desire to learn
While closely related to other themes, half specifically noted that the case studies deepened their understanding and sparked curiosity and a greater desire to learn more about immunology:
“I felt like the case studies both enhanced and challenged my understanding of immunology concepts. Some things we did not know because we are not trained professionals so that is how it challenges us, but it also helped me better understand some of the topics that we were working on that week because it was able to bring all of the concepts together.”
“The patient-centered case studies helped enhance my learning by bringing up things that we didn’t necessarily cover in lecture, but we could ask questions and learn more about it.”
This finding suggests that CBL can enhance students’ grasp of immunological principles and motivation to learn more about case-related topics.
Preparation for medical careers
Nearly half of the students noted that the case studies provided valuable preparation for future medical training by simulating real patient scenarios:
“The case studies brought real word instances to life in this classroom. It made me look forward to my future medical career path.”
“I found these to be beneficial because they were relevant to the career I want to go into in the future, so they helped me stay engaged with class and apply what I learned to more relevant concepts.”
This theme underscores the importance of active learning in connecting undergraduate education with professional practice.
Connection of concepts
Students indicated that the case studies helped them integrate multiple immunological concepts, making learning more cohesive:
“We needed to apply immunological concepts that we learned in the lectures to real–world problems. This was helping in grasping how abnormal functioning of different components of the immune system manifest as a variety of physical symptoms.”
“The case studies enhanced my learning because they combined multiple aspects of the concepts we learned in a real–life situation, which helped me understand how the concepts come together in real life.”
This suggests that CBP facilitates knowledge retention by reinforcing the relationships between key immunological principles.
Patient connection
Although less frequently mentioned, some students emphasized the patient-centered nature of the case studies and its impact on their learning:
“Provided good real world understanding of how the immune system impacts people and changes.”
“They made me want to be knowledgeable and know everything about each patient so I could find the right cure.”
While not as dominant as other themes, this insight highlights the potential for CBL to foster a more patient-focused approach in medical education.
Skills gained or improved
Student responses to the question, “What skills do you feel you gained or improved upon by working through the patient-centered case studies?” were analyzed to evaluate student perceptions regarding the impact on their learning skills. Through thematic analysis, four primary themes emerged: (1) Critical Thinking and Problem Solving; (2) Content Application; (3) Diagnosing and Clinical Skills; and (4) Teamwork and Communication. A visual representation of the code frequency is shown in Figure 4B.
Critical thinking and problem solving
Half of the students explicitly described how the case studies challenged them to engage in deeper analysis, problem-solving, and decision-making. Many responses emphasized the necessity of interpreting symptoms and integrating multiple pieces of information to determine possible diagnoses:
“Although these case studies are already solved and I know what is going on by the end, I gained experience with trying to integrate all of the information and variables I am given and try to figure out what is going on.”
“I feel that I gained problem solving and detail–oriented skills when completing the case studies. They forced me to look at symptoms and clues and make a diagnosis.”
These findings suggest that CBL fosters critical thinking by requiring students to assess complex problems rather than passively absorb information.
Content application
A similar proportion of students highlighted that the case studies facilitated the application of immunological concepts to real-world scenarios. They noted that working through cases allowed them to bridge the gap between theoretical knowledge and practical use:
“I think I gained skills on reading deeper into patient symptoms and being able to apply the symptoms to what I learned in class.”
“Being able to correlate what we went over in class with clinical examples definitely helped me remember more content. It forced me to recall and implement my knowledge in a practical way that I wish other courses regarding complicated science concepts follow.”
This theme underscores the role of CBL in reinforcing content comprehension and helping students see the relevance of immunology beyond the classroom.
Diagnosing and clinical skills
Related to critical thinking and problem solving, one-third of students acknowledged that the case studies helped them develop diagnostic reasoning and clinical evaluation skills. They gained a better understanding of how to interpret patient data and recognize disease patterns:
“I think these case studies helped me analyze the symptoms and synthesize them to come up with a resulting diagnosis.”
“I learned a lot more about different immunological disorders that improved my ability to read all the facts and narrow down what the disorder was.”
This theme suggests that case studies serve as an early introduction to clinical reasoning, helping students practice skills that will be critical in their future medical careers.
Teamwork and communication
Students also emphasized the collaborative nature of the case studies, noting that working in teams allowed them to refine their communication skills and learn from peers:
“I think I gained teamwork and problem-solving skills. It helped open my mind to different possibilities when diagnosing.”
“Teamwork and communication are some skills that I have gained as I often completed the case studies with my group. We were able to share ideas and guide each other with remembering concepts that were just discussed in class.”
The responses indicate that case-based learning fosters an interactive learning environment, encouraging students to engage in discussion, share insights, and problem-solve collectively.
The results suggest that patient-centered case studies effectively enhance students’ ability to apply immunology content, develop critical thinking skills, practice clinical reasoning, and collaborate effectively. The findings support the role of PCL in preparing students for real-world medical scenarios, reinforcing both conceptual knowledge and essential professional competencies.
Discussion
This study demonstrates that students perceive the use of PCL in an undergraduate immunology course as enhancing their comprehension of immunologic concepts, critical thinking, and diagnostic reasoning skills. The results indicate that CBL and AL were the most frequently cited instructional strategies that contributed to students’ learning, reinforcing the importance of student engagement and contextualized learning, which is consistent with adult learning theory (Knowles, 1984). While TBL was mentioned less frequently, those who referenced it recognized the value of peer collaboration and group discussion, supporting findings that team-based activities help solidify conceptual knowledge (James et al., 2019; Kibble et al., 2016).
Through qualitative analysis, students identified six major themes related to how PCL impacted their learning, including real-world application, critical thinking, preparation for medical careers, connection of concepts, enhanced understanding, and patient connection. Importantly, students described gains in problem solving abilities, diagnostic reasoning, and teamwork, indicating that patient-centered cases provide an early introduction to clinical reasoning skills essential for future healthcare providers. These findings align with prior research emphasizing that when basic science content is delivered in a clinically relevant manner, it is more readily retained and applied to clinical practice (Anderson et al., 2020).
Expanding the role of empathy in patient-centered case studies
This study presents a versatile model of CBL that enhances scientific comprehension and patient-centered thinking in pre-health education. CBL facilitates interprofessional learning (Thistlethwaite et al., 2012), which is particularly beneficial in undergraduate courses where students from various health professions attend classes together. Furthermore, cases provide opportunities to integrate multiple subjects across the health sciences, allowing students to connect foundational knowledge in the basic sciences with clinical applications, thus promoting deeper and more holistic understanding (Novack, 2020).
Although the goal of designing case studies in a patient-centric format was to expand and promote students’ empathy for patients, a surprising result was a distinct lack of “empathy” in students’ responses to open-ended questions. While students readily detailed how patient-centered case studies increased their critical thinking and problem solving, teamwork and communication, and diagnostic skills, there were no direct mentions of increased empathy. This suggests that while students recognized the real-world application of immunological concepts, they may not have consciously reflected on the emotional and humanistic dimensions of patient care or considered it a skill. This may be that empathy on the path to medical education is impressed upon far less than harder, more tangible skills. Laughey et al. (2021) hypothesize that empathy originates from inherent sentiments and is nurtured through both formal and informal medical curricula. Furthermore, there are various events within the hidden curriculum that enhance empathy, often without the explicit awareness of the students.
This absence of explicit empathy-related responses may reflect a gap in pre-health undergraduate education and preparation for future medical careers where technical skills are prioritized over interpersonal and emotional competencies. Empathy can be more difficult to imbue in students than more tangible attributes like being able to work in a team environment or applying immunology concepts to diagnose patients in a case study. However, the increasing need for empathy to balance technical, statistical treatments is becoming more apparent (Laughey et al., 2021). Patient-centered case studies lay the groundwork for students flexing and developing their empathy muscles, but everything takes practice and time. If more undergraduate courses implement exercises styled like the case studies described herein, students will have more opportunities to hone their empathy.
Implications for future course design
While patient-centered case studies lay the groundwork for developing empathy in undergraduate students, this study suggests that more deliberate scaffolding is necessary to ensure that students actively engage with the humanistic aspects of patient care. One potential strategy is to explicitly integrate reflection exercises alongside case studies, prompting students to consider patient emotions, ethical dilemmas, and the psychosocial aspects of disease. Guided discussions, role-playing exercises, and reflective writing prompts could further enhance students’ ability to connect scientific reasoning with human experience.
Furthermore, incorporating interprofessional education (IPE) activities can enhance students’ understanding of the collaborative nature of patient care (Thistlethwaite et al., 2012). This method is particularly advantageous for undergraduate immunology courses, given the diverse range of pre-health majors that may participate. Encouraging students to discuss case studies with peers from different health-related disciplines could foster a deeper appreciation for patient-centered, team-based decision-making.
Limitations
While this study provides valuable insights into the effectiveness of PCL in undergraduate immunology education, a few limitations should be acknowledged. First, the findings rely on self-reported student perceptions collected through course evaluations. While these data provide meaningful reflections on student experiences, they are inherently subjective and may not fully capture actual learning gains. Future research could benefit from incorporating direct assessments of immunology knowledge and clinical reasoning skills before and after case study implementation. Second, although one of the goals of PCL was to foster empathy, the study did not include a validated empathy assessment tool. The absence of explicit references to empathy in student responses suggests that targeted survey items may be necessary to measure changes in students’ patient-centered thinking. Lastly, this study was conducted within a single undergraduate immunology course at one institution, which may limit the generalizability of the findings. Students’ experiences and perceptions of PCL may differ across institutions, disciplines, and course structures. Expanding this approach to other health science courses and diverse educational settings would help determine its broader applicability and effectiveness.
Conclusion
Ultimately, this study highlights the effectiveness of PCL in reinforcing conceptual learning, diagnostic reasoning, and collaborative problem-solving, while also revealing an opportunity to better integrate explicit empathy-building components into undergraduate immunology education. As the demand for holistic, patient-centered clinicians continues to grow, integrating structured empathy development activities into pre-health curricula will be essential in shaping both scientifically competent and compassionate healthcare professionals.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation, upon reasonable request.
Ethics statement
The studies involving humans were approved by the University of North Dakota Office of Research Compliance & Ethics. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because this study utilized existing data collected through the standard, university facilitated student evaluation system. The authors received the data in an aggregated, deidentified format at the end of the semester after grades had been entered. This study applied for and received formal IRB approval: IRB0006553; Exempt Category 4.
Author contributions
SS: Conceptualization, Project administration, Methodology, Supervision, Data curation, Writing – original draft, Writing – review & editing. DC: Writing – review & editing, Data curation, Writing – original draft, Methodology, Formal Analysis, Investigation.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We utilized ChatGPT-4, an AI language model developed by OpenAI, for assistance with editing and refining this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor TV declared a past co-authorship with the author SS.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2025.1598286/full#supplementary-material
References
Amarilla, N. S., Revuelta, M. J. C., and Martínez, A. I. M. (2022). Systematic review: Flipped classrooms in the performance of undergraduate science students. J. Sci. Educ. Technol. 31:594. doi: 10.1007/s10956-022-09979-8
Anderson, H., Sweeney, C., Perry, R., Vaquero, J., and Ison, H. (2020). Patient-centered team-based learning in pre-clinical curriculum supporting the application of knowledge to real-world clinical experience. Med. Sci. Educ. 30, 65–68. doi: 10.1007/s40670-019-00872-5
Anderson, L. W., and Krathwohl, D. R. (2001). A Taxonomy for Learning, Teaching, and Assessing: A Revision of Bloom’s Taxonomy of Educational Objectives: Complete Edition. Saddle River, NJ: Addison Wesley Longman, Inc.
Bauer, M. E., Akbar, S., Bauler, T. J., Chacon, J., McClelland, E. E., Staudaher, S., et al. (2024). Exploration of the integration of microbiology and immunology emerging topics into undergraduate medical education. Med. Educ. Online 29, 2336331. doi: 10.1080/10872981.2024.2336331
Brooks, J. G., and Brooks, M. G. (1993). In Search of Understanding: The Case for Constructivist Classrooms. Arlington, VA: ASCD.
Cervantes, J. (2020). The future of infectious diseases education. Med Sci Educ. 30, 1783–1785. doi: 10.1007/s40670-020-01023-x
Del Canale, S., Louis, D., Maio, V., Wang, X., Rossi, G., Hojat, M., et al. (2012). The relationship between physician empathy and disease complications: An empirical study of primary care physicians and their diabetic patients in Parma, Italy. Acad. Med. 87, 1243–1249. doi: 10.1097/ACM.0b013e3182628fbf
Freeman, S., Eddy, S. L., McDonough, M., Smith, M. K., Okoroafor, N., Jordt, H., et al. (2014). Active learning increases student performance in science, engineering, and mathematics. Proc. Natl. Acad. Sci. U S A. 111:8410. doi: 10.1073/pnas.1319030111
Haidaris, C. G., and Frelinger, J. G. (2019). Inoculating a new generation: immunology in medical education [Perspective]. Front. Immunol. 10:2548. doi: 10.3389/fimmu.2019.02548
Hojat, M., Louis, D., Markham, F., Wender, R., Rabinowitz, C., and Gonnella, J. (2011). Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 86, 359–364. doi: 10.1097/ACM.0b013e3182086fe1
James, S., Cogan, P., and McCollum, M. (2019). Team-based learning for immunology courses in allied health programs. Front. Immunol. 10:2477. doi: 10.3389/fimmu.2019.02477
Kibble, J. D., Bellew, C., Asmar, A., and Barkley, L. (2016). Team-based learning in large enrollment classes. Adv. Physiol. Educ. 40, 435–442. doi: 10.1152/advan.00095.2016
Knowles, M. (1984). Andragogy in action: Applying modern principles of adult learning, 1st Edn. Jossey-Bass.
Laughey, W. F., Atkinson, J., Craig, A. M., Douglas, L., Brown, M. E., Scott, J. L., et al. (2021). Empathy in medical education: Its nature and nurture - A qualitative study of the views of students and tutors. Med. Sci. Educ. 31, 1941–1950. doi: 10.1007/s40670-021-01430-8
Noordman, J., Post, B., van Dartel, A., Slits, J., and Olde Hartman, T. (2019). Training residents in patient-centred communication and empathy: Evaluation from patients, observers and residents. BMC Med Educ. 19:128. doi: 10.1186/s12909-019-1555-5
Novack, J. P. (2020). Designing cases for case-based immunology teaching in large medical school classes [perspective]. Front. Immunol. 11:995. doi: 10.3389/fimmu.2020.00995
Pandey, S., Elliott, S. L., Liepkalns, J., Taylor, R. T., Vanniasinkam, T., Kleinschmit, A. J., et al. (2024). The immunoskills guide: Competencies for undergraduate immunology curricula. PLoS One 19:e0313339. doi: 10.1371/journal.pone.0313339
Porter, E., Amiel, E., Bose, N., Bottaro, A., Carr, W. H., Swanson-Mungerson, M., et al. (2021). American association of immunologists recommendations for an undergraduate course in immunology. Immunohorizons 5, 448–465. doi: 10.4049/immunohorizons.2100030
Siani, M., Dubovi, I., Borushko, A., and Haskel-Ittah, M. (2024). Teaching immunology in the 21st century: A scoping review of emerging challenges and strategies. Int. J. Sci. Educ. 46, 1826–1847. doi: 10.1080/09500693.2023.2300380
Smith, M. A., Mohammad, R. A., and Benedict, N. (2014). Use of virtual patients in an advanced therapeutics pharmacy course to promote active, patient-centered learning. Am. J Pharm. Educ. 78:125. doi: 10.5688/ajpe786125
Southwick, F., Katona, P., Kauffman, C., Monroe, S., Pirofski, L.-A., del Rio, C., et al. (2010). Commentary: IDSA guidelines for improving the teaching of preclinical medical microbiology and infectious diseases. Acad. Med. 85, 19–22. doi: 10.1097/ACM.0b013e3181c485c5
Stranford, S. A., Owen, J. A., Mercer, F., and Pollock, R. R. (2020). Active learning and technology approaches for teaching immunology to undergraduate students. Front. Public Health 8:114. doi: 10.3389/fpubh.2020.00114
Svinicki, M. D. (2004). Learning and Motivation in the Postsecondary Classroom. Hoboken, NJ: Jossey-Bass.
Thistlethwaite, J. E., Davies, D., Ekeocha, S., Kidd, J. M., MacDougall, C., Matthews, P., et al. (2012). The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Med. Teach. 34, e421–e444. doi: 10.3109/0142159x.2012.680939
Yang, W., Zhang, X., Chen, X., Lu, J., and Tian, F. (2024). Based case based learning and flipped classroom as a means to improve international students’ active learning and critical thinking ability. BMC Med. Educ. 24:759. doi: 10.1186/s12909-024-05758-8
Zhang, M., and Hu, W. (2024). Application of PBL combined with CBL teaching method in clinical teaching of vascular surgery. PLoS One 19:e0306653. doi: 10.1371/journal.pone.0306653
Keywords: case-based learning (CBL), patient-centered learning (PCL), case studies, active learning, empathy, undergraduate, immunology
Citation: Cleveland DW and Sletten S (2025) Integrating patient-centered learning strengthens concept mastery, problem-solving, and patient awareness in undergraduate immunology. Front. Educ. 10:1598286. doi: 10.3389/feduc.2025.1598286
Received: 22 March 2025; Accepted: 15 May 2025;
Published: 16 June 2025.
Edited by:
Thiru Vanniasinkam, Charles Sturt University, AustraliaReviewed by:
Andrea Bottaro, Cooper Medical School of Rowan University, United StatesSean T. Coleman, Wartburg College, United States
Holly Basta, Rocky Mountain College, United States
Copyright © 2025 Cleveland and Sletten. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sarah Sletten, c2FyYWguc2xldHRlbkB1bmQuZWR1
 Dawn W. Cleveland
Dawn W. Cleveland Sarah Sletten
Sarah Sletten