- 1Department of Restorative Dental Sciences, Endodontic Division, College of Dentistry, King Saud University, Riyadh, Saudi Arabia
- 2Department of Prosthetic Dental Sciences, College of Dentistry, King Saud University, Riyadh, Saudi Arabia
- 3Molecular and Cell Biology Laboratory, Prince Naif bin Abdulaziz Health Research Center, King Saud University Medical City, Riyadh, Saudi Arabia
- 4Department of Oral Medicine and Diagnostic Sciences, College of Dentistry, King Saud University, Riyadh, Saudi Arabia
Background: Regenerative endodontic procedures require effective disinfection and preservation of stem cell viability, which are essential for successful tissue regeneration. Conventional intracanal medicaments possess antibacterial properties but may negatively impact stem cell survival. Benzyl isothiocyanate (BITC) is a bioactive compound with known antibacterial properties and favorable biocompatibility.
Methods: This study evaluated the antibacterial efficacy of BITC against Fusobacterium nucleatum in both planktonic and biofilm forms and assessed its biocompatibility on human bone marrow mesenchymal stem cells (hBMMSCs) in comparison to calcium hydroxide (Ca(OH)2). Minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) were determined using microdilution and agar culture methods. Biofilm biomass was quantified using the crystal violet assay, viability was visualized through live/dead imaging, and microstructure was examined using scanning electron microscopy. Stem cell viability was evaluated using the Alamar Blue™ assay, and cell morphology was examined using inverted microscopy.
Results: BITC exhibited MIC and MBC values of 0.2% and 0.4%, respectively. At 0.2%, BITC demonstrated comparable antibacterial activity to Ca(OH)2, whereas 0.4% and 0.8% showed enhanced bactericidal effects. Notably, 0.2% and 0.4% BITC maintained hBMMSCs viability and morphology, while 0.8% BITC and Ca(OH)2 significantly reduced cell survival.
Conclusion: These findings suggest that BITC could serve as a potential antimicrobial agent in regenerative endodontic treatment and future therapeutic applications.
1 Introduction
Regenerative endodontic procedures (REPs) were first introduced by Banchs and Trope in 2004 to treat necrotic permanent immature teeth (Banchs and Trope, 2004). The primary goal of REPs is to eliminate symptoms, promote apical bone healing, continue root development, and close the root apex (Kim et al., 2018). To achieve these goals, three important biological factors must be present: stem cells, growth factors, and scaffolds (Hargreaves et al., 2013). Recently, the role of disinfection has received more attention in regard to the success of regeneration, with an emphasis on additional detoxification that clears infections and maintains stem cell viability through intracanal medicaments (Diogenes and Hargreaves, 2017). The most commonly used intracanal medicaments in REPs are antibiotic pastes and calcium hydroxide (Ca(OH)2) (Kontakiotis et al., 2015). Several studies have reported successful outcomes after using various antibiotic mixtures in REPs (Chan et al., 2017; Lin et al., 2017). However, potential side effects such as tooth discoloration, the development of antibiotic resistance, and negative effects on stem cell proliferation have been major concerns (Sedgley et al., 2008; Torabinejad et al., 2017).
As a result, Ca(OH)2 has been widely favored for its proven antimicrobial properties and successful regenerative outcomes (Desai and Chandler, 2009; Glynis et al., 2021). These properties are primarily due to its high alkalinity and the ability to release hydroxyl ions, which create an unfavorable environment for bacterial growth (Mohammadi and Dummer, 2011). However, the antimicrobial effect of Ca(OH)2 remains limited in some cases, particularly in persistent infections and against certain resistant bacteria such as Fusobacterium nucleatum (F. nucleatum) (Sathorn et al., 2007; Ferreira et al., 2015). This limitation is critical in REPs, since F. nucleatum is frequently detected in necrotic immature permanent teeth and endodontic abscesses and often persists after instrumentation and chemical disinfection (Zandi et al., 2018; Fouad, 2019). In addition to the microbial limitation of Ca(OH)2, its effect on host stem cells remains controversial. While some studies reported that Ca(OH)2 promotes the proliferation and osteogenic differentiation of dental pulp stem cells (DPSCs) in certain conditions (Chen et al., 2016), other studies suggest unfavorable effects on DPSCs proliferation (Alghilan et al., 2017). Given these limitations and conflicting outcomes, the need to develop an antimicrobial agent that can effectively eradicate bacterial infections while maintaining stem cell viability, promoting cell proliferation, and ultimately enhancing the outcome of REPs remains important in regenerative endodontic research.
Natural products have been used in medicine for centuries due to their relatively minimal side effects and notable antimicrobial properties (Garg et al., 2014). Benzyl isothiocyanate (BITC) is a naturally occurring bioactive compound found in various plants, including Salvadora persica, Carica papaya, and Tropaeolum majus (Sofrata et al., 2011; Kaiser et al., 2017; Zhang and Chen, 2017). This metabolite is synthesized by plants in reaction to disruption, mainly via glucosinolate and myrosinase hydrolysis (Romeo et al., 2018b). BITC has been recognized for its significant antibacterial effects against a wide range of gram-positive and gram-negative bacterial pathogens. It has been shown to downregulate virulence gene expression in Staphylococcus aureus and inhibit Salmonella typhimurium motility and biofilm growth (Wang et al., 2019; Niu et al., 2020). It was also reported to have an antimicrobial efficacy comparable to that of gentamycin sulfate in treating Pseudomonas aeruginosa infections, with minimal toxicity and lower inflammatory responses (Yang et al., 2024). Additionally, extracts containing BITC have been shown to inhibit oral biofilm formation, reduce periodontal pathogens, and promote gingival wound healing (Aljarbou et al., 2022; Harun et al., 2023). These antibacterial properties are attributed to the ability of BITC to protrude bacterial membranes, disrupt metabolic activity, and induce oxidative stress, ultimately leading to cell death (Hoch et al., 2024). However, the antibacterial effects of BITC against F. nucleatum have yet to be explored.
In cancer research, BITC has been studied for its anticancer properties, exhibiting a promising capacity to induce apoptosis, cell cycle arrest, and oxidative stress in cancer cells (Dinh et al., 2021). BITC downregulates Mcl-1, an anti-apoptotic protein, in leukemia cells, triggering apoptosis via caspase activation. In contrast, it exhibits minimal toxic effects on normal human peripheral blood mononuclear cells (Zhou et al., 2013). Furthermore, BITC has demonstrated cytotoxic effects against canine lymphoma and leukemia cells by inducing caspase-dependent apoptosis through the upregulation of reactive oxygen species (ROS), causing DNA damage (Henklewska et al., 2021).
Despite extensive research on the anticancer effects of BITC, its effects on normal mesenchymal stem cells remain poorly understood. Several studies on moringin, in which BITC is the main bioactive compound, have demonstrated that it has positive effects on cell survival and proliferation of human periodontal ligament stem cells (hPDLSCs) and human gingival mesenchymal stem cells (hGMSCs) (Romeo et al., 2018a; Chiricosta et al., 2019). However, the effects of BITC on the viability of human bone marrow stem cells (hBMMSCs) have not been investigated. Therefore, the present study aimed to evaluate the antibacterial properties of BITC against F. nucleatum in both planktonic and biofilm states and to assess its effect on the viability of hBMMSCs in comparison to Ca(OH)2.
2 Materials and methods
2.1 Bacterial strain and culture preparation
Before each experiment, F. nucleatum ATCC 25586 (Cat. No. 0328K, Microbiologics KWIK-STIK™, Saint Cloud, MN, USA) was cultured on tryptic soy agar (TSA) plates supplemented with hemin and vitamin K (Watin-Biolife Factory, Riyadh, Saudi Arabia) under anaerobic conditions at 37 °C for 72 h using an anaerobic jar and generator pack (AnaeroPack™, Mitsubishi Gas Chemical Co., Tokyo, Japan). Single isolated bacterial colonies were then inoculated in 10 mL tryptic soy broth (TSB) (Watin-Biolife Factory) supplemented with 5 µg/mL hemin and 1 µg/mL menadione and incubated anaerobically in an Excella E24 incubator shaker (New Brunswick Scientific, Edison, NJ, USA) for 24 h. After incubation, the bacterial concentrations were standardized to an optical density (OD600) of approximately 0.5-0.6 (mid-log phase) using a spectrophotometer (Libra S22, Biochrom Ltd., Cambridge, UK) before subsequent experiments were performed, unless otherwise noted (Casasanta et al., 2020).
2.2 Chemicals and experimental groups
BITC (98% purity) in liquid form was obtained from Sigma-Aldrich (Cat. No. 252492, St. Louis, MO, USA) and freshly dissolved in dimethyl sulfoxide (DMSO, 0.2%, Sigma-Aldrich) immediately prior to the experiments. Based on preliminary evaluation, the following concentrations were selected: 0.05%, 0.1%, 0.2%, 0.4%, 0.8%, and 1.6%. As a positive control group, calcium hydroxide was purchased in the form of UltraCal™ XS (35% Ca(OH)2, Ultradent, South Jordan, UT, USA).
2.3 Determination of minimum inhibitory concentration and minimum bactericidal concentration
To determine the MIC, a modified resazurin microplate-based assay method was used (Franzblau et al., 1998). Briefly, a BITC stock solution was prepared in DMSO and serially diluted using TSB to obtain the concentration range. A sterile 96-well U-bottom microtiter plate was prepared by adding 150 μL of 1.6% BITC into Column 8, and 150 μL of TSB to Columns 3-7, followed by two-fold serial dilutions using a multi-channel pipette to generate descending concentrations ranging from 1.6% to 0.05%. Ca(OH)2 and DMSO served as positive controls, TSB with a bacterial inoculate as a bacteria growth control, and TSB alone served as a negative control. Fifty microliters of the standardized F. nucleatum suspension were added to the appropriate wells, reaching the final working volume to 200 μL. Plates were incubated anaerobically at 37 °C for 24 h. After the incubation period, 20 μL 0.015% resazurin indicator solution (Sigma-Aldrich) was added to all wells and incubated for 2 h. A color change from blue to pink indicates metabolic activity, whereas no color change indicates bacterial growth inhibition. The MIC was determined as the lowest concentration at which no change in color was observed (Dias et al., 2014; Elshikh et al., 2016).
For MBC determination, 20 µL aliquots from the MIC-related wells in the 96-well plates were cultured on Brucella blood agar plates supplemented with hemin and vitamin K (Watin-Biolife Factory, Riyadh, Saudi Arabia) and incubated overnight at 37 °C under anaerobic conditions. The MBC was identified as the lowest concentration with no visible bacterial colony growth (Sabrah et al., 2013). All experiments were conducted in triplicates from three independent biological replicates.
2.4 pH measurements
The pH of the experimental solutions was measured using a calibrated pH meter (Jenway 3540 pH & Conductivity meter, Bibby Scientific, Staffordshire, UK). Calibration was performed before each reading using standard buffer solutions at pH 4.0, 7.0, and 9.0 (Honeywell Fluka™, Seelze, Germany). Samples were prepared in 15 mL conical tubes (TPP®, Trasadingen, Switzerland), each containing 10 mL of supplemented tryptic soy broth. All tubes were incubated at 37 °C, and pH measurements were recorded at 1, 3, and 7 days.
2.5 Planktonic bacterial viability assessment
Following MIC determination, the same experimental setup was used to evaluate the viability of planktonic F. nucleatum. The fluorescence readings (FI) were recorded on days 1, 3, and 7 using a Synergy HT microplate reader (BioTek Instruments, Winooski, VT, USA) at excitation and emission wavelengths of 530 and 590 nm, respectively (Niazy et al., 2024). The percentage of bacterial viability was calculated using the following equation:
2.6 Reactive oxygen species production
The intracellular production of reactive oxygen species (ROS) in F. nucleatum following BITC treatment was assessed using a fluorescence-based assay (Nowicki et al., 2016). Bacteria were cultured in TSB to an OD600 = 0.5, then harvested and washed three times with phosphate-buffered saline (PBS). The fluorogenic probe 2',7'-dichlorofluorescein diacetate (DCFH-DA; Santa Cruz Biotechnology, Heidelberg, Germany) was added to a final concentration of 30 μM, and the cells were incubated anaerobically at 37 °C for 60 min in the dark with shaking. After incubation, cells were centrifuged and washed twice with PBS and resuspended in fresh TSB. Bacterial suspensions were then treated with different BITC concentrations for 6 h at 37 °C under anaerobic conditions. For controls, untreated samples and groups treated with DMSO or Ca(OH)2 were included under the same conditions. Fluorescence intensity was measured using a Synergy HT microplate reader (BioTek Instruments, Winooski, VT, USA) at an excitation wavelength of 488 nm and emission wavelength of 535 nm. ROS levels were expressed as relative fluorescence units (RFU).
2.7 Biofilm biomass quantification
To quantify biofilm formation, a crystal violet biofilm assay was used as described by haney et al (Haney et al., 2018). Briefly, BITC concentrations and control groups were prepared as previously described. After bacterial culturing was carried out, each well of the 96-well plate was inoculated with 150 μL of bacterial suspension at an OD of 0.5 at 600 nm. Untreated bacterial growth controls served as negative controls, and the experiment was conducted at two time points: days 3 and 7. At each time point, non-adherent bacteria were removed by gently washing the 96-well plates thrice using distilled water. The plates were left to air-dry for 20 mins, and then 150 μL of 0.5% crystal violet solution (Sigma-Aldrich) was added to each well. After staining, the wells were washed with distilled water to remove excess dye and dried at 37°C for 15 min. Absolute ethanol was added to each well, and the wells were incubated for 15 mins. Then, the absorbances were read spectrophotometrically at 570 nm using a BioTek Synergy HT microplate reader. Biofilm inhibition was calculated as a percentage relative to the untreated bacterial control. The experiments were all performed in triplicate.
2.8 Biofilm viability assessment
The effects of experimental groups on F. nucleatum biofilms were further assessed using live/dead fluorescent imaging and viewed under confocal laser scanning microscopy (CLSM). Bacterial cells were inoculated into 2 mL of supplemented TSB at (OD600 = 0.5) initial turbidity and cultured on coverslips in 6-well culture plates at 37°C in an anaerobic chamber for 3 and 7 days. BITC stock solutions and control groups were prepared as previously described. For the live/dead staining of biofilms, any remaining broth was removed from each well, and the coverslips were washed gently three times with PBS and transferred to a new 6-well plate. About 200 µL of working solution (LIVE/DEAD® BacLight Bacterial Viability kit, Invitrogen, Eugene, OR, USA) was added to each biofilm sample, following the manufacturer's instructions, and then incubated for 30 min at room temperature, protected from light. The stained surface was placed face down onto a clean microscope slide and imaged using a Nikon C2 CLSM (Nikon Instruments Inc., Tokyo, Japan) with a 20×/0.75 NA air objective using (λexc) 488 nm/(λem)<550 nm for SYTO® 9 (BacLight™ Component A) and (λexc) 568 nm/(λem) >600 nm for propidium iodide (BacLight™ Component B). Image analysis was carried out using ImageJ software (version 1.50i, NIH, Bethesda, USA) (Niazy et al., 2024). The green fluorescence represents live cells, and red represents dead cells. The percentages of bacterial cell death were calculated as previously described using the following equation.
2.9 Bacterial morphology analysis
Bacterial samples were grown for 48 h and then cultured for 7 days, as described above. The culture broth in each well was removed, and the cover slips were washed with PBS. The scanning electron microscopy (SEM) sample preparation method was conducted as previously described by Diarra et al (Diarra et al., 2023). Cover slip samples were fixed with 2.5% glutaraldehyde solution at 4°C for 2 h, washed with PBS three times, and dehydrated serially with increasing concentrations of ethanol (30 to 95%) for 10 mins each, followed by two 15 min washes with absolute ethanol. Finally, each coverslip was critically point-dried and coated with gold using a JEOL JFC1100 sputter instrument (JEOL Ltd., Tokyo, Japan) and then viewed using a JEOL JSM-6360LV scanning electron microscope (JEOL Ltd., Tokyo, Japan).
2.10 Cell culture
Immortalized human bone marrow-derived mesenchymal stem cells (hMSC-TERT20) were used as an experimental model for in vitro biocompatibility studies (Liu et al., 2015). Immortalization with human telomerase reverse transcriptase was performed for the mesenchymal stem cells following protocols described previously (Simonsen et al., 2002; Abdallah et al., 2005). The hMSC-TERT20 cell line was kindly provided by the Molecular and Cell Biology (MCB) Laboratory of the College of Dentistry, in collaboration with the Prince Naif Bin Abdulaziz Health Research Center (King Saud University, Riyadh, Saudi Arabia).
The cell line was cultured in a T-75 culture flask (NEST Scientific, Woodbridge, NJ, USA) with Dulbecco's Modified Eagle's medium (DMEM) with 4 mM glutamine, 1 mM sodium pyruvate, and 4500 mg/L of glucose supplemented with 10% fetal bovine serum (FBS), 1% non-essential amino acids, and 1% antibiotic–antimycotic solution (all Gibco, Invitrogen, Carlsbad, CA, USA) and was maintained at 37°C in a 5% CO2 humidified NU-4850E incubator (NuAire® Inc., Plymouth, MN, USA) until ~80% confluence was reached. The medium was replaced every 48 h to maintain stable growth conditions for the cell culture.
2.11 Stem cell viability assessment
The viability and proliferation of hBMMSCs was examined by using Alamar Blue™ (Invitrogen™, Eugene, OR, USA) according to the manufacturer's instructions (Cassiano et al., 2022). Each experiment was performed on cells from three independent passages and included two negative controls (untreated cells in basal media and cells treated with 0.2% DMSO). Similar to previous bacterial assessments, BITC concentrations used for all the cell experiments are (0.05% to 0.8%) and Ca(OH)2 served as a positive control group. Before use and following UV sterilization, all the test groups were diluted with DMEM immediately before treatment in order to dilute the final concentration of DMSO to 0.2% to eliminate the influence of DMSO. All experimental procedures were performed under aseptic conditions under a Class II laminar flow hood (NU-425-400G Biological Safety Cabinet; NuAire® Inc.).
In brief, the cells were cultured in 96-well flat-bottom culture plates (NEST Scientific, Woodbridge, NJ, USA) using supplemented DMEM at a seeding density of 1×104 cells/well in a volume of 200 μL and allowed to adhere overnight. The culture medium was then removed, and the cells were exposed to 200 µL of experimental and control groups for 1, 2, 4, and 7 days. After the exposure period, the treated medium was removed from the plates, a 1/10th volume of Alamar Blue™ reagent solution was mixed with serum-free DMEM and added to each well, and the plates were incubated in the dark at 37 °C for 4 h. The fluorescence readings of each well were measured at an excitation wavelength of 530 nm and an emission wavelength of 590 nm using a Synergy HT fluorescence microplate reader. Cell viability was calculated using the following formula:
The results are presented as percentages of cell viability in comparison to the control group, and the fluorescence values of the untreated cells were considered to have 100% viability based on ISO 10993–5 guidelines (ISO 10993-5, 2009). The experiment was performed in six wells per condition and repeated three different times.
2.12 Cellular morphology assessment
For the observation of any morphological changes, the cells were cultivated (1.5×105 cells/well) on 12-well culture plates (Greiner Bio-One GmbH, Frickenhausen, Germany) and grown until 80% confluency (Ahmed et al., 2016). Subsequently, the cells were treated experimental and control groups. The cellular morphology was observed, and multiple representative fields (in at least 4 replicates) were photographed at different intervals during the 7-day incubation period using an inverted light microscope (Carl Zeiss Axiovert 40C Imaging Microscope, Göttingen, Germany).
2.13 Statistical analysis
All data are presented as means ± standard deviations. All the group values were obtained by averaging at least three or more biological replicates. Statistical differences were analyzed using one-way or two-way ANOVA according to the variables analyzed, followed by Tukey's post hoc test to test statistical differences among the treatment groups. The statistical analysis was performed using GraphPad Prism (version 6.00 for Windows, La Jolla, CA, USA; https://www.graphpad.com). p ≤ 0.05 was considered to be statistically significant.
3 Results
3.1 Minimum inhibitory concentration and minimum bactericidal concentration
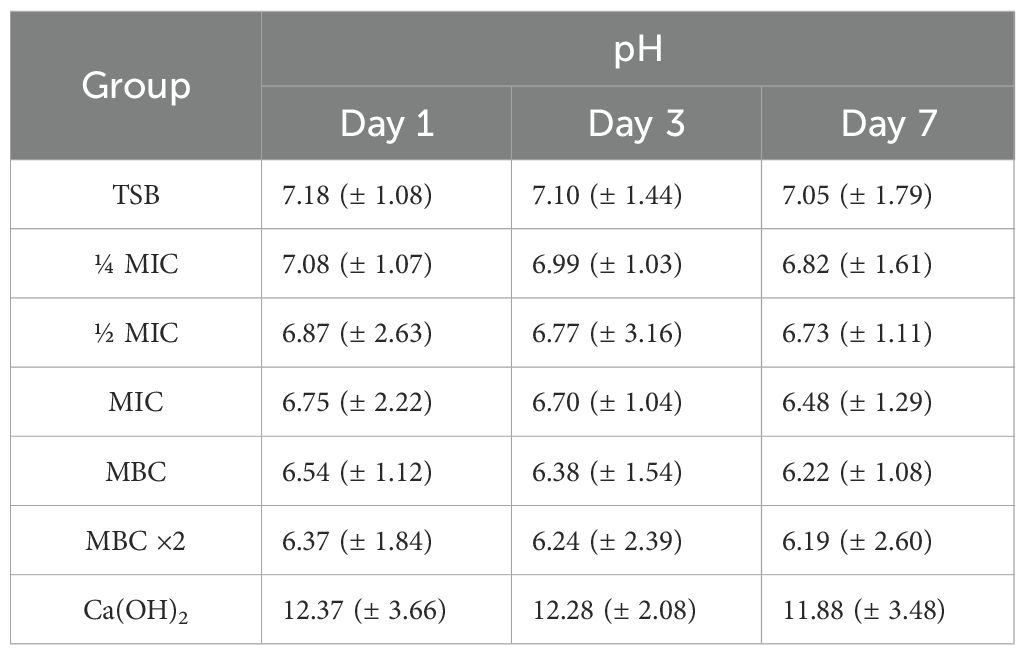
BITC at 0.2% exhibited the first observable color shift, indicating bacterial growth inhibition, and was thus identified as the MIC (Figure 1A). In agar plate cultures (Figure 1B), BITC at 0.4% was identified as the MBC, being the lowest concentration to achieve complete bacterial eradication. Subinhibitory concentrations of ¼ MIC (0.05%), ½ MIC (0.1%), along with MIC (0.2%), MBC (0.4%), and MBC ×2 (0.8%) were selected for further microbiological and cellular analysis.
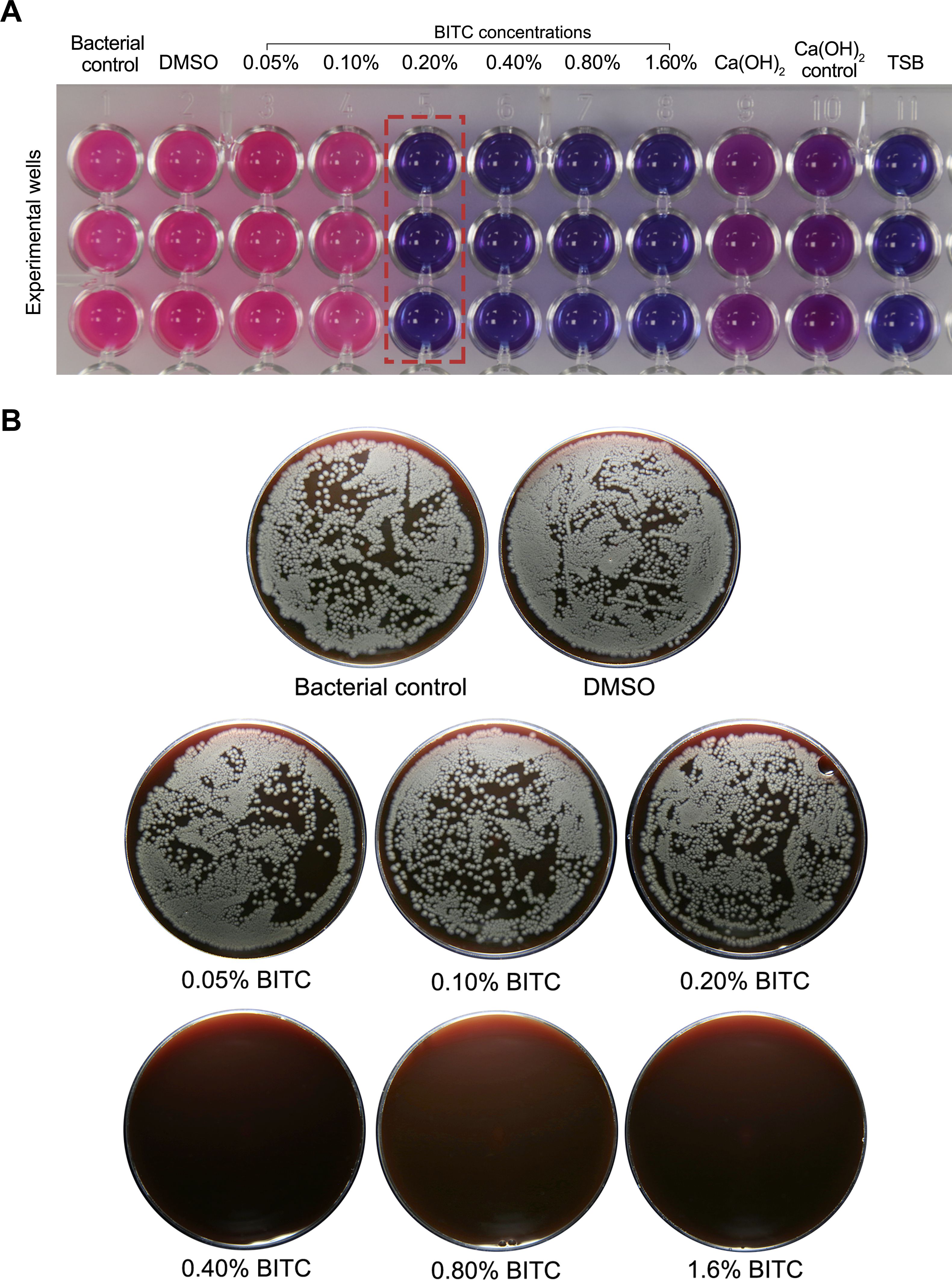
Figure 1. (A) Microplate resazurin-based assay showing F. nucleatum viability. BITC at 0.2% marked the initial indication of bacterial inhibition (highlighted in red), which was determined to be the MIC. (B) Agar plate cultures showing visible bacterial colonies in the control and BITC up to 0.2%, while BITC at 0.4% achieved the first visible bacterial elimination, which was identified as the MBC.
3.2 pH measurements
The pH values of the experimental groups are summarized in Table 1. BITC solutions showed slight acidity, exhibiting a minimal decrease in pH over time. In contrast, Ca(OH)2 maintained a strongly alkaline pH throughout the incubation period, whereas the TSB control remained near neutral.
3.3 Planktonic bacterial viability assessment
The bacterial control and DMSO groups maintained high bacterial viability at all time points. On day 1, BITC at ¼ MIC, ½ MIC, and MBC significantly reduces viability compared to bacterial control (p≤0.05), while the Ca(OH)2 group showed greater reduction (p≤0.05). In contrast, BITC at MBC and MBC x2 showed significantly greater bacterial reduction than the Ca(OH)2 group (p≤0.05). On day 3, BITC at ½ MIC and MIC remained effective (p≤0.05), but was notably lower than MBC, MBC ×2, and Ca(OH)2 groups (p≤0.05). By day 7, all tested groups demonstrated a significant reduction in bacterial viability when compared to bacterial control (p≤0.05). However, MBC ×2 and Ca(OH)2 showed the highest antibacterial effects, almost eliminating all F. nucleatum planktonic cells, with no statistically significant difference observed (p = 0.99) (Figure 2).
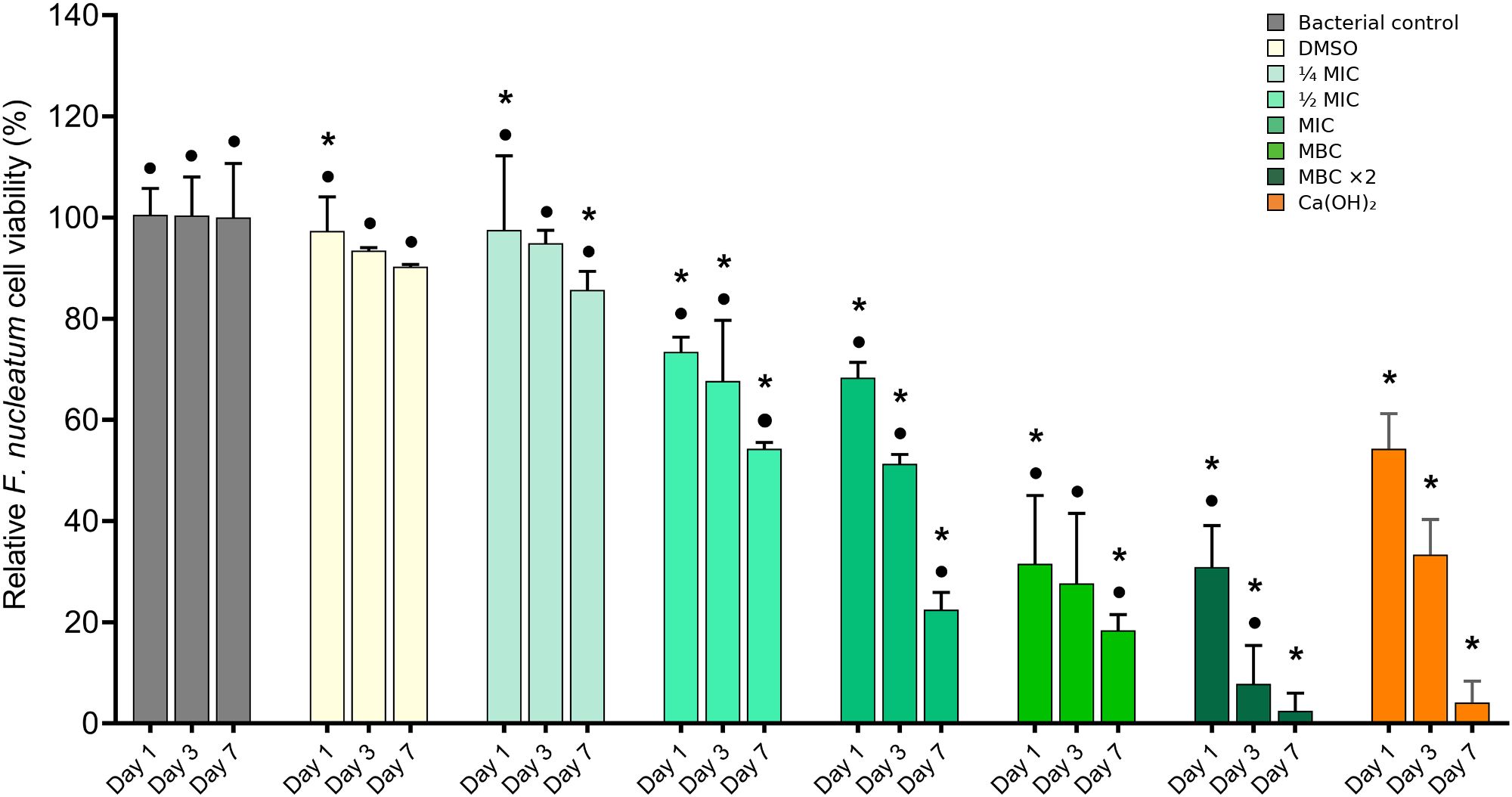
Figure 2. Assessment of planktonic F. nucleatum viability using a resazurin-based assay on days 1, 3, and 7. Quantification of the bacterial viability percentage is shown in the bar graph as the mean ± standard deviation (SD). Asterisks (*) indicate p ≤ 0.05 compared with the bacterial control at each time point. Dots (•) indicate p ≤ 0.05 compared with Ca(OH)2 at each time point.
3.4 Reactive oxygen species production
BITC exposure led to increased ROS production in F. nucleatum, as reflected by elevated fluorescence levels across all treated groups (Figure 3). The highest ROS activity was observed in the MBC ×2 group, suggesting greater oxidative stress with higher concentrations. However, with Ca(OH)2 treatment, no significant change in ROS levels relative to the control was noted.
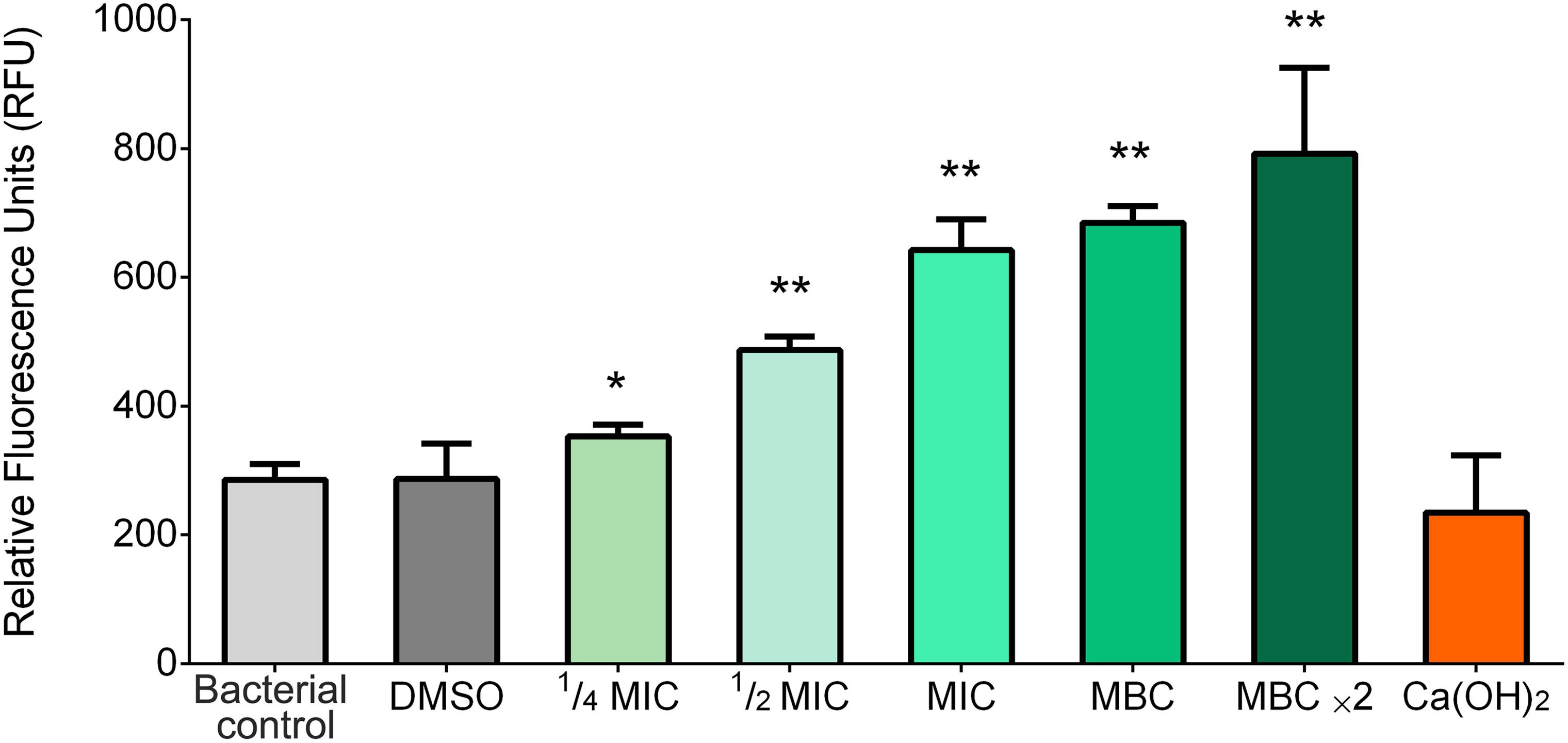
Figure 3. Intercellular ROS levels in F. nucleatum following 6 h exposure to experimental groups. Bars represent mean RFU ± SD, (p ≤ 0.05) (*) and (p ≤ 0.01) (**) compared to the bacterial control group.
3.5 Biofilm biomass quantification
Biofilm biomass formation was quantified using the crystal violet biofilm assay (Figure 4). On day 3, BITC at ¼ MIC and ½ MIC exhibited minimal biofilm reduction with no significant difference in comparison to the bacterial control group (p >0.05). The Ca(OH)2 group showed a significant reduction in biofilm formation compared with the bacterial control group (p ≤ 0.05). However, the BITC at MIC, MBC, and MBC ×2 demonstrated a more significant reduction compared to the Ca(OH)2 group (p ≤ 0.05). By day 7, all experimental groups showed significant biofilm reduction compared to the bacterial control group (p ≤ 0.05). The BITC at ≤ MIC showed no significant difference in biofilm reduction compared with the Ca(OH)2 group (p >0.05). However, BITC at MBC and MBC ×2 exhibited significantly greater biofilm reduction than the Ca(OH)2 group (p ≤ 0.05).

Figure 4. Crystal violet assay showing biofilm formation (%) on days 3 and 7 following treatment. Bars represent the mean ± SD of biofilm formation. The stained wells are displayed above each bar. Asterisks (*) indicate p ≤ 0.05 compared with the bacterial control at each time point. Dots (•) indicate p ≤ 0.05 compared with Ca(OH)2 at each time point.
3.6 Biofilm viability assessment
Live/dead fluorescent imaging revealed a significant increase in biofilm cell death in all experimental groups compared to the untreated bacterial control at both time points (p ≤ 0.05). CLSM images demonstrated strong green fluorescence intensity in the bacterial control group at both time points, indicating a high proportion of live bacteria. In contrast, experimental groups showed an increased red fluorescence supporting bactericidal efficacy (Figure 5A). On day 3, BITC at ¼ MIC and ½ MIC demonstrated significantly less biofilm cell death compared to the Ca(OH)2 group (p ≤ 0.05), while no significant difference was observed between the MIC and Ca(OH)2 groups (p >0.05). However, BITC at MBC and MBC ×2 led to significantly greater bactericidal effects than the Ca(OH)2 group (p ≤ 0.05). By day 7, BITC at ≤ MIC were significantly less effective than the Ca(OH)2 group (p ≤ 0.05). On the contrary, MBC and MBC ×2 exhibited significantly higher levels of biofilm cell death than the Ca(OH)2 group (p ≤ 0.05) (Figure 5B).
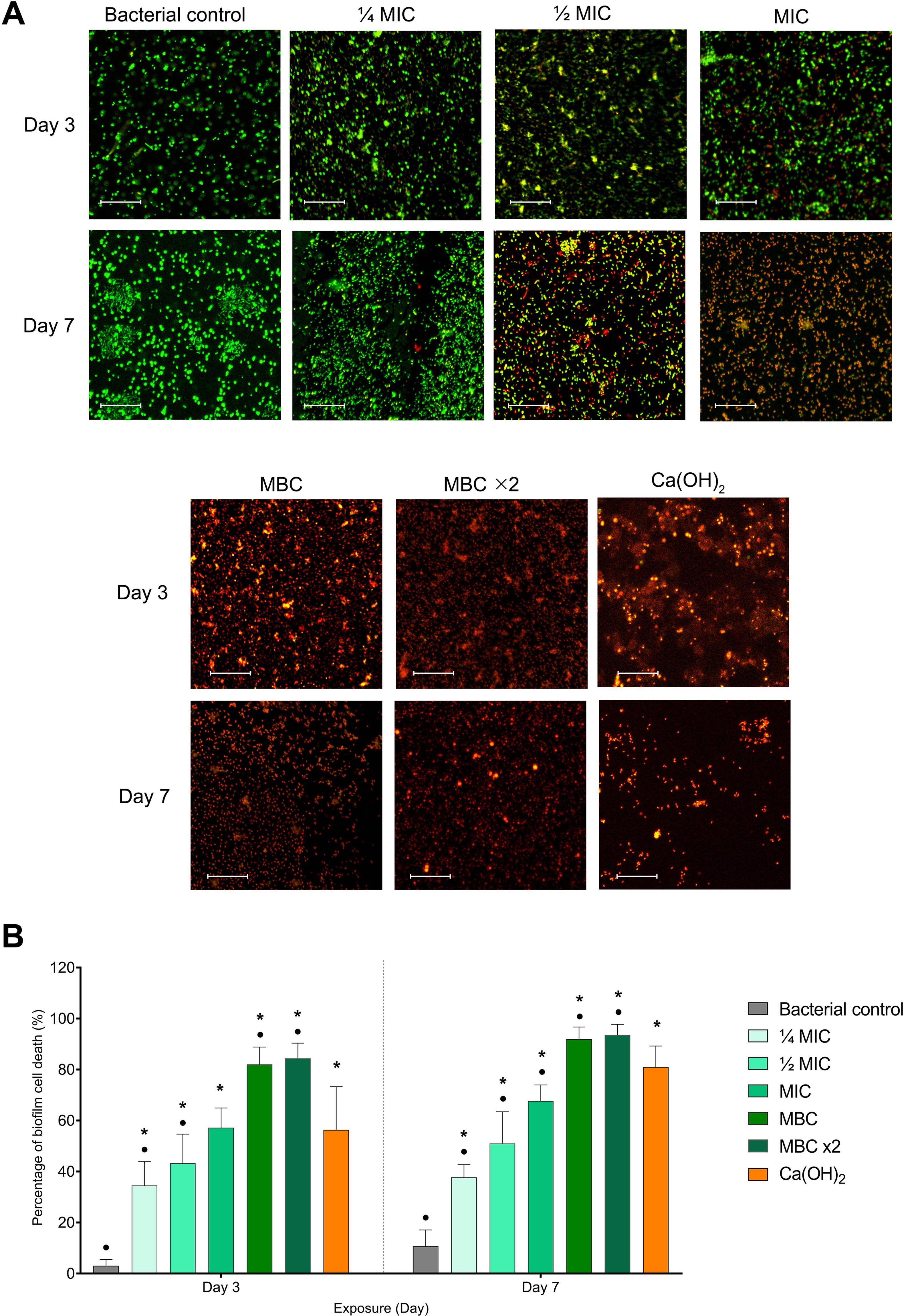
Figure 5. (A) Representative fluorescence images of F. nucleatum biofilm cells stained for viability (green=live, red=dead). (B) Quantification of bacterial cell death percentage is shown in the bar graph as means ± SD. Asterisks (*) indicate p ≤ 0.05 compared with the bacterial control at each time point. Dots (•) indicate p ≤ 0.05 compared with Ca(OH)2 at each time point.
3.7 Biofilm morphology analysis
SEM analysis of biofilm morphology demonstrated notable structural differences across examined groups (Figure 6). The bacterial control group exhibited a dense, well-organized biofilm with abundant extracellular matrix. In BITC at ¼ MIC and ½ MIC groups, bacterial clusters remained visible with slight disruption noted. However, MIC and MBC led to noticeable structural damage, with deformed cells and extracellular matrix breakdown. Notably, treatment with MBC ×2 and Ca(OH)2 caused extensive biofilm disruption, scattered cellular debris, and loss of structural integrity.
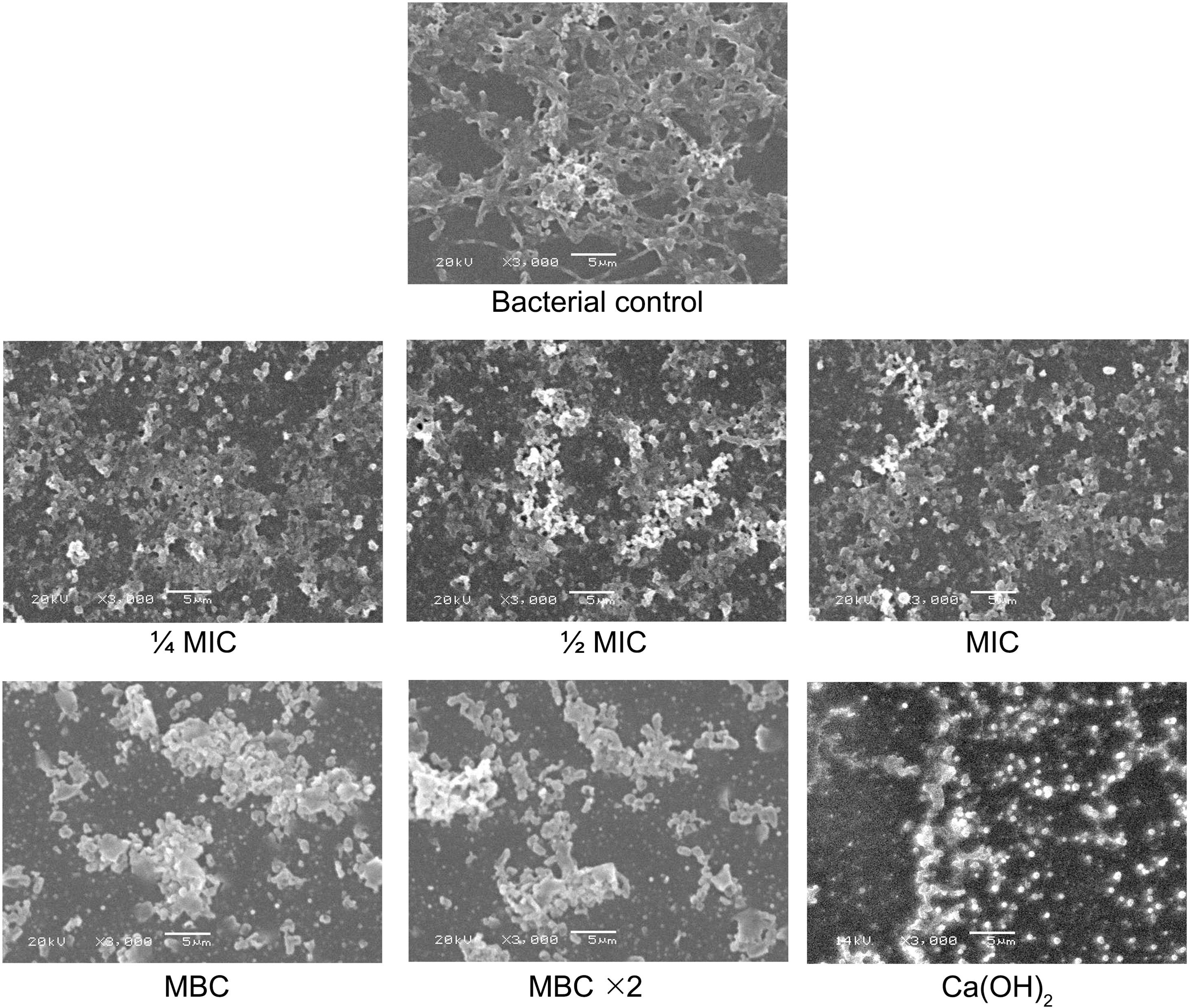
Figure 6. SEM images of F. nucleatum biofilm morphology after exposure to experimental groups. Scale bar = 5 μm.
3.8 Stem cell viability assessment
Alamar Blue™ viability assay was used to evaluate the effects of experimental groups on the viability of hBMMSCs. The results are presented as percentages of cell viability relative to the untreated control group (Figure 7). According to ISO 10993-5:2009 guidelines for the biological evaluation of medical devices, a reduction in viability below 70% is considered indicative of cytotoxicity (ISO 10993-5, 2009).

Figure 7. hBMMSCs following exposure to experimental groups over a 7-day time period using the Alamar Blue™ assay. According to the ISO 10993–5 guidelines, the cell viability threshold was set at 70% (dashed line). Bars represent the mean ± SD of cell viability. Asterisks (*) indicate p ≤ 0.05 compared with DMEM control at each time point. The phi symbol (Φ) indicates p ≤ 0.05 compared with Ca(OH)2 at each time point.
The DMSO-treated stem cells exhibited minimal reductions in viability, suggesting that DMSO, as a vehicle, exerted a negligible effect on cell survival. In the BITC 0.05% and 0.1% groups, an initial proliferative response was noted at days 1 and 2, respectively. This increase was statistically significant only in the 0.05% group compared to the negative control group (DMEM). Over time, both groups exhibited a gradual decline in proliferation, with significant reductions observed at day 7. In contrast, higher concentrations (0.2% and 0.4%) caused a decrease in cell counts over the exposure period. For the 0.2% group, the decline became significant by days 4 and 7, while the 0.4% group showed a significant reduction at all time points. Despite these trends, cell viability remained relatively stable in the previously mentioned groups over the 7-day period. However, the BITC 0.8% group displayed a clear decline in cell viability starting as early as day 2, with cell counts continuing to decline significantly over time. Similarly, cells exposed to Ca(OH)2 also experienced a significant drop in viability across the exposure period. When comparing treatment groups, cells exposed to the Ca(OH)2 had significantly lower cell counts than the BITC 0.05%, 0.1%, and 0.2% groups at all time points (p ≤ 0.05). No significant difference was found between Ca(OH)2 and BITC 0.4% (p >0.05), while BITC 0.8% induced significantly greater cytotoxicity than the Ca(OH)2 group (p ≤ 0.05).
3.9 Cellular morphology assessment
The hBMMSCs morphology was monitored microscopically at baseline, 24 h, 48 h, and day 7 following exposure to experimental groups (Figure 8). The control group and DMSO-treated cells maintained a normal spindle-shaped appearance with consistent confluency and proliferation throughout the observation period. BITC at concentrations of 0.05%, 0.1%, 0.2%, and 0.4% maintained a normal confluent spindle-shaped appearance for the first 48 h, with a slight reduction in confluency by day 7. However, the 0.8% BITC group showed evident morphological changes, including cell shrinkage and detachment. Similarly, Ca(OH)2 demonstrated dark granulation regions and changes in cell morphology at the 24 h mark, with substantial cellular detachment and loss of confluency by day 7.
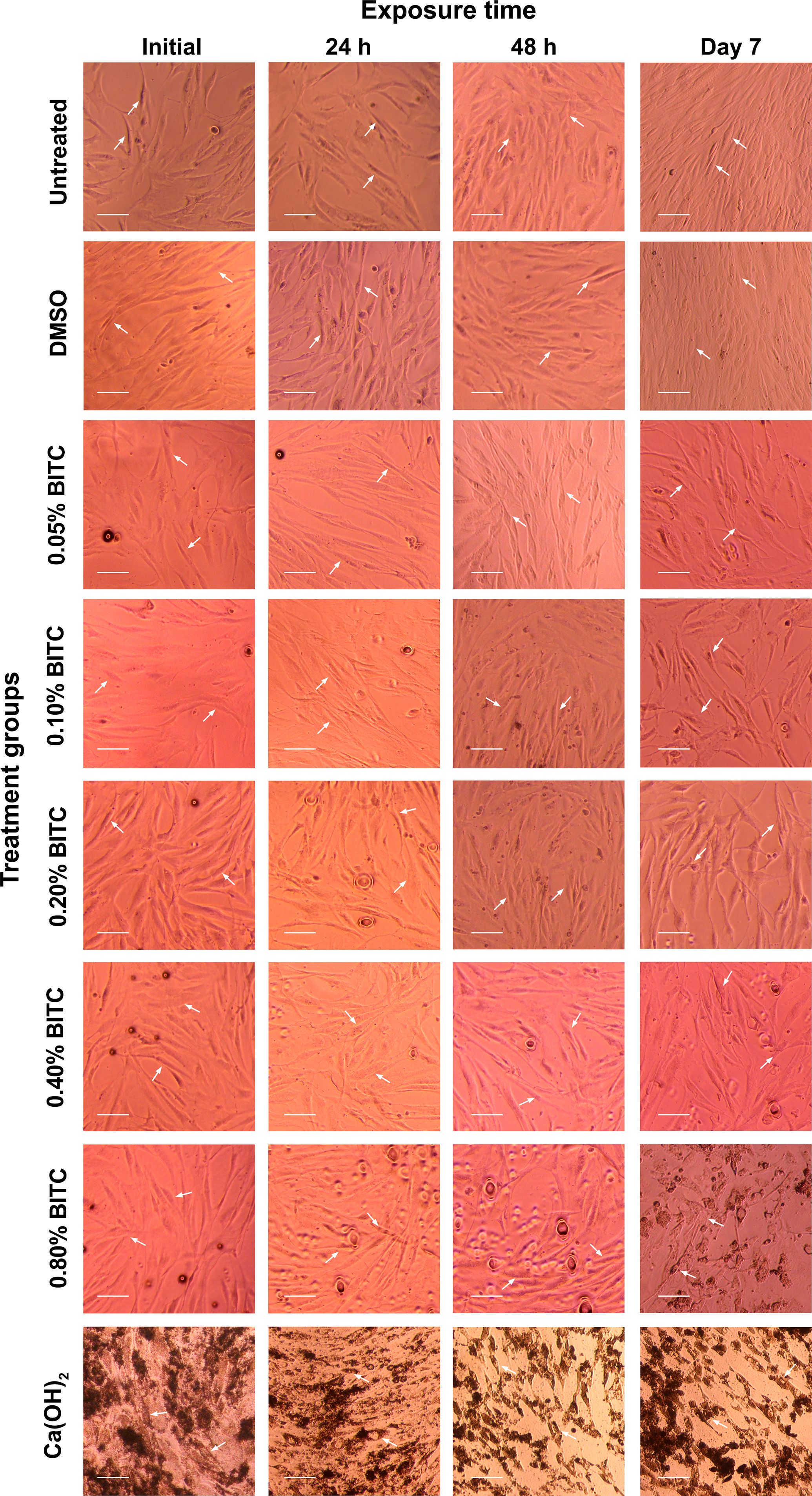
Figure 8. Representative phase-contrast microscopic images showing the morphology of hBMMSCs at the initial stage, 24 h, 48 h, and day 7 in untreated control and experimental treatment groups. White arrows indicate characteristic cell morphology. All images were captured at 10× magnification. Scale bar = 50 µm.
4 Discussion
In REPs, chemical disinfection is critical not only for eradicating pathogens but also for creating an environment that supports stem cell survival and conduction (Diogenes and Hargreaves, 2017). Improper disinfection of bacterial biofilms can compromise the differentiation potential of stem cells during treatment (Vishwanat et al., 2017). Therefore, the intracanal medicaments used in REPs must strike a balance between potent antibacterial activity and minimal cytotoxicity towards stem cells (Murray et al., 2007).
Although endodontic infections are polymicrobial in nature (Siqueira and Rôças, 2022), F. nucleatum was selected in this study due to its high prevalence in root canals before and after chemo-mechanical preparation, and is one of the most frequently detected bacteria in immature permanent teeth with necrotic pulps (Zandi et al., 2018; Fouad, 2019). The antibacterial evaluation revealed that BITC exhibits potent inhibitory activity against F. nucleatum, with an MIC of 0.2% and an MBC of 0.4% which is higher than the MIC values reported for other bacterial species in previous studies (Song et al., 2019; Alhandal et al., 2022; Vrca et al., 2023). This might be due to its anaerobic nature, its ability to form a robust dense biofilm, and the upregulation of specific genes that might enhance biofilm resistance (Zhao et al., 2022; Ciani et al., 2024). Notably, BITC effectively eliminated F. nucleatum planktonic cells within the first 24 h and disrupted established biofilms by 48 h at MBC concentrations. Moreover, BITC was observed to have a concentration-dependent antibacterial effect on F. nucleatum biofilms, with significant reductions in viability observed at 0.4% and 0.8% concentrations. This finding aligns with previous studies reporting similar dose-dependent activity against Staphylococcus aureus and Salmonella typhimurium (Wang et al., 2019; Niu et al., 2020).
The mechanism of action of BITC is believed to be multifactorial, involving the disruption of cell membranes, suppression of virulence factors, oxidative stress induction, bacterial morphology alteration, and impairment of biofilm adhesion capabilities (Kaiser et al., 2017; Liu et al., 2021; Hoch et al., 2024). In our study, SEM analysis demonstrated an alteration in F. nucleatum morphology and biofilm detachment. Crystal violet staining further confirmed a significant reduction in biofilm biomass following treatment, particularly at concentrations corresponding to the MIC and higher. In addition, BITC treatment led to a marked increase of intracellular ROS in F. nucleatum, supporting previously reported evidence of oxidative stress induction.
To assess clinical relevance, BITC was compared to calcium hydroxide (CaOH2), in the form of UltraCal XS (Ultradent, South Jordan, UT, USA), in accordance with previous in vitro and ex vivo regenerative endodontic studies (Althumairy et al., 2014; Latham et al., 2016; Bilvinaite et al., 2024). Our results demonstrated that BITC concentrations corresponding to MIC and higher exhibited a rapid antibacterial effect, resulting in a high proportion of dead bacterial cells and a marked reduction in biofilm formation at early experimental stages. In contrast, Ca(OH)2 showed minimal antibacterial effects during the first 72 h. However, by day 7, Ca(OH)2 exerted a potent effect, increasing bacterial cell death and reducing biofilm formation. Although this delayed effect was notable, its efficacy remained significantly lower than 0.4% and 0.8% BITC concentrations. This delayed antibacterial action was supported earlier by Sjögren et al., who reported that Ca(OH)2 requires at least 7 days for optimal bacterial elimination (Sjögren et al., 1991). The antimicrobial action of Ca(OH)2 is mainly attributed to its ability to release hydroxyl ions creating an alkaline environment capable of disrupting bacterial cell membranes (Mohammadi and Dummer, 2011). In the present study, pH evaluation showed that Ca(OH)2 maintained high alkalinity throughout the 7-day period.
In addition to the importance of proper microbial disinfection, an antimicrobial agent must also preserve stem cell viability for successful regeneration (Parchami et al., 2024). Various types of mesenchymal stem cells have been identified in REPs, including dental pulp stem cells (DPSCs), apical papilla stem cells (SCAP), periodontal ligament stem cells (PDLSCs), alveolar-bone-derived mesenchymal stem cells (ABSMCs), stem cells from human exfoliated deciduous teeth (SHEDs), and human bone marrow mesenchymal stem cells (hBBMSCs) (Huang et al., 2009; Ayoub et al., 2020). Moreover, studies have validated the use of immortalized human bone marrow mesenchymal stem cells in regenerative research (AlMobarak et al., 2025). In our study, immortalized hBMMSCs was selected to evaluate the viability responses to the experimental materials. The BITC concentrations (≤0.4%) maintained stem cell viability. In fact, low BITC concentrations (0.05% and 0.1%) enhanced cell proliferation, increasing the cell count to a greater extent than that for the control group. In contrast, 0.8% BITC showed cytotoxic effects after 48 h and continued to reduce cell counts throughout the observation period. Consistent with the viability findings, morphological assessment showed that BITC groups at (≤0.2%), maintained normal spindle-shaped cellular morphology with firm attachment. However, 0.4% BITC exhibited mild alterations such as reduced cellular spreading. Although the current evidence on the effects of BITC on stem cell viability remains limited, findings from structurally related compounds such as moringin suggest positive regeneration potential. In hPDLSCs, moringin increases stem cell proliferation and promotes neural differentiation, while in human gingival mesenchymal stem cells (GMSCs), it maintains cell viability and promotes regenerative responses (Romeo et al., 2018a; Chiricosta et al., 2019). Moreover, isothiocyanates as a class demonstrated a similar behavior, where low concentrations protected mesenchymal stem cells (MSCs) from oxidative injuries, while higher concentrations led to DNA damage and cytotoxicity (Zanichelli et al., 2012), supporting the dose-dependent effect observed in our study.
On the other hand, Ca(OH)2 demonstrated a significantly higher cytotoxicity towards hBMMSCs, with cell viability initially maintained but declined as exposure progressed. Morphological analysis confirmed this unfavorable effect by showing evident signs of cell stress, including rounding, detachment, and shrinkage. Comparable findings have been reported previously, in which Ca(OH)2 significantly reduced the viability and proliferation of bone marrow-derived mesenchymal stem cells (Khosropanah et al., 2018). The cytocompatibility of BITC compared to Ca(OH)2 suggests that BITC is a potential candidate for REPs, where preserving stem cell function is critical. Furthermore, its natural origin and known safety profile add to its translational appeal for clinical application.
This study has several limitations, which should be acknowledged. First, the antibacterial evaluation and cell viability assessments were limited to in vitro models, which do not fully represent the complex biological reactions present in biological systems. Secondly, the antibacterial evaluation was only conducted on mono-species F. nucleatum; although one of the most prevalent bacteria in endodontic infections, it does not represent the diverse microbial species detected in clinical settings (Siqueira and Rôças, 2022). Lastly, the stem cell assessment was limited to viability and morphology effects over a 7-day observation period. It did not evaluate the long-term effects on stem cell function, including differentiation potential, migration, mineralization capabilities, and gene expression. Future studies should also explore the efficacy of BITC in multispecies biofilm models, co-culture systems, and in vivo models. In addition, exploring controlled delivery systems or sustained-release formulations for intracanal use may optimize BITC's clinical utility.
5 Conclusions
In conclusion, benzyl isothiocyanate demonstrated promising antibacterial and antibiofilm activity against Fusobacterium nucleatum compared to calcium hydroxide. Moreover, benzyl isothiocyanate preserved the viability and morphology of human bone marrow mesenchymal stem cells, whereas calcium hydroxide showed cytotoxic effects and caused notable morphological alterations. These preliminary findings suggest that benzyl isothiocyanate may serve as a potential bioactive antimicrobial agent relevant for regenerative endodontic applications. However, further research is needed to evaluate its efficacy against a broader range of pathogens and to optimize concentrations that balance intracanal disinfection with biological compatibility.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the studies on humans in accordance with the local legislation and institutional requirements because only commercially available established cell lines were used.
Author contributions
AAA: Formal Analysis, Writing – original draft, Methodology, Investigation, Visualization, Validation, Resources, Data curation, Funding acquisition, Writing – review & editing, Conceptualization. AA: Project administration, Supervision, Writing – review & editing, Funding acquisition. AB: Supervision, Funding acquisition, Project administration, Conceptualization, Methodology, Writing – review & editing. RL: Investigation, Visualization, Validation, Writing – review & editing, Formal Analysis, Data curation. AN: Writing – review & editing, Supervision, Methodology, Resources, Funding acquisition, Project administration. FA: Project administration, Supervision, Methodology, Validation, Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Acknowledgments
The authors thank Terrence Suministrado Sumague and the Molecular and Cell Biology Laboratory of Prince Naif Bin AbdulAziz Health Research Center for their assistance with confocal microscopy, image acquisition, and scientific illustrations.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcimb.2025.1683203/full#supplementary-material
Glossary
ABSMCs: Alveolar bone-derived mesenchymal stem cells
BITC: Benzyl isothiocyanate
Ca(OH)2: Calcium hydroxide
CLSM: Confocal laser scanning microscopy
DMEM: Dulbecco's Modified Eagle's medium
DMSO: Dimethyl sulfoxide
DPSCs: Dental pulp stem cells
F. nucleatum: Fusobacterium nucleatum
hBMMSCs: Human bone marrow mesenchymal stem cells
hGMSCs: Human gingival mesenchymal stem cells
hPDLSCs: Human periodontal ligament stem cells
MIC: Minimum inhibitory concentration
MBC: Minimum bactericidal concentration
REPs: Regenerative endodontic procedures
ROS: Reactive oxygen species
SCAP: Stem cells of apical papilla
SEM: Scanning electron microscopy
SHEDs: Stem cells from human exfoliated deciduous teeth
TSA: Tryptic soy agar
TSB: Tryptic soy broth
References
Abdallah, B. M., Haack-Sørensen, M., Burns, J. S., Elsnab, B., Jakob, F., Hokland, P., et al. (2005). Maintenance of differentiation potential of human bone marrow mesenchymal stem cells immortalized by human telomerase reverse transcriptase gene despite of extensive proliferation. Biochem. Biophys. Res. Commun. 326, 527–538. doi: 10.1016/j.bbrc.2004.11.059
Ahmed, NE-MB, Murakami, M., Kaneko, S., and Nakashima, M. (2016). The effects of hypoxia on the stemness properties of human dental pulp stem cells (DPSCs). Sci. Rep. 6, 35476. doi: 10.1038/srep35476
Alghilan, M., Windsor, L. J., Palasuk, J., and Yassen, G. H. (2017). Attachment and proliferation of dental pulp stem cells on dentine treated with different regenerative endodontic protocols. Int. endodontic J. 50, 667–675. doi: 10.1111/iej.12669
Alhandal, H., Almesaileikh, E., Bhardwaj, R. G., Al Khabbaz, A., and Karched, M. (2022). The effect of benzyl isothiocyanate on the expression of genes encoding NADH oxidase and fibronectin-binding protein in oral streptococcal biofilms. Front. Oral. Health 3, 863723. doi: 10.3389/froh.2022.863723
Aljarbou, F., Almobarak, A., Binrayes, A., and Alamri, H. M. (2022). Salvadora persica’s biological properties and applications in different dental specialties: A narrative review. Evidence-Based Complementary Altern. Med. 2022, 8667687. doi: 10.1155/2022/8667687
AlMobarak, S., AlMadi, E., Almohaimede, A., Badran, M., and Lambarte, R. A. (2025). The effect of commiphora molmol nanoparticles as an endodontic irrigant on the morphology, viability, migration, and proliferation of human bone marrow mesenchymal stem cells: an in vitro study. Int. J. Mol. Sci. 26, 1412. doi: 10.3390/ijms26041412
Althumairy, R. I., Teixeira, F. B., and Diogenes, A. (2014). Effect of dentin conditioning with intracanal medicaments on survival of stem cells of apical papilla. J. endodontics. 40, 521–525. doi: 10.1016/j.joen.2013.11.008
Ayoub, S., Cheayto, A., Bassam, S., Najar, M., Berbéri, A., and Fayyad-Kazan, M. (2020). The effects of intracanal irrigants and medicaments on dental-derived stem cells fate in regenerative endodontics: an update. Stem Cell Rev. Rep. 16, 650–660. doi: 10.1007/s12015-020-09982-9
Banchs, F. and Trope, M. (2004). Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J. endodontics 30, 196–200. doi: 10.1097/00004770-200404000-00003
Bilvinaite, G., Drukteinis, S., Simoliunas, E., Widbiller, M., and Sakirzanovas, S. (2024). Effect of calcium silicate-based intracanal medicament and calcium hydroxide on growth factor TGF-β1 release from root canal dentine. J. Funct. Biomaterials. 15, 139. doi: 10.3390/jfb15060139
Casasanta, M. A., Yoo, C. C., Udayasuryan, B., Sanders, B. E., Umaña, A., Zhang, Y., et al. (2020). Fusobacterium nucleatum host-cell binding and invasion induces IL-8 and CXCL1 secretion that drives colorectal cancer cell migration. Sci. Signaling 13, eaba9157. doi: 10.1126/scisignal.aba9157
Cassiano, A. F. B., Coaguila-Llerena, H., Santos, C. S., da Silva, L. R., Nogueira, L. F. B., Ciancaglini, P., et al. (2022). The effect of octenidine on proliferation, migration, and osteogenic differentiation of human dental pulp and apical papilla stem cells. J. Endodontics. 48, 1502–10.e1. doi: 10.1016/j.joen.2022.09.010
Chan, E. K. M., Desmeules, M., Cielecki, M., Dabbagh, B., and Dos Santos, B. F. (2017). Longitudinal cohort study of regenerative endodontic treatment for immature necrotic permanent teeth. J. endodontics. 43, 395–400. doi: 10.1016/j.joen.2016.10.035
Chen, L., Zheng, L., Jiang, J., Gui, J., Zhang, L., Huang, Y., et al. (2016). Calcium hydroxide–induced proliferation, migration, osteogenic differentiation, and mineralization via the mitogen-activated protein kinase pathway in human dental pulp stem cells. J. endodontics. 42, 1355–1361. doi: 10.1016/j.joen.2016.04.025
Chiricosta, L., Silvestro, S., Pizzicannella, J., Diomede, F., Bramanti, P., Trubiani, O., et al. (2019). Transcriptomic analysis of stem cells treated with moringin or cannabidiol: analogies and differences in inflammation pathways. Int. J. Mol. Sci. 20, 6039. doi: 10.3390/ijms20236039
Ciani, L., Libonati, A., Dri, M., Pomella, S., Campanella, V., and Barillari, G. (2024). About a possible impact of endodontic infections by Fusobacterium nucleatum or Porphyromonas gingivalis on oral carcinogenesis: A literature overview. Int. J. Mol. Sci. 25, 5083. doi: 10.3390/ijms25105083
Desai, S. and Chandler, N. (2009). Calcium hydroxide–based root canal sealers: a review. J. endodontics. 35, 475–480. doi: 10.1016/j.joen.2008.11.026
Diarra, C., Goetz, C., Gagnon, M., Roy, D., and Jean, J. (2023). Biofilm formation by heat-resistant dairy bacteria: multispecies biofilm model under static and dynamic conditions. Appl. Environ. Microbiol. 89, e00713–e00723. doi: 10.1128/aem.00713-23
Dias, C., Aires, A., and Saavedra, M. J. (2014). Antimicrobial activity of isothiocyanates from cruciferous plants against methicillin-resistant Staphylococcus aureus (MRSA). Int. J. Mol. Sci. 15, 19552–19561. doi: 10.3390/ijms151119552
Dinh, T. N., Parat, M.-O., Ong, Y. S., and Khaw, K. Y. (2021). Anticancer activities of dietary benzyl isothiocyanate: A comprehensive review. Pharmacol. Res. 169, 105666. doi: 10.1016/j.phrs.2021.105666
Diogenes, A. and Hargreaves, K. M. (2017). Microbial modulation of stem cells and future directions in regenerative endodontics. J. Endodontics. 43, S95–S101. doi: 10.1016/j.joen.2017.07.012
Elshikh, M., Ahmed, S., Funston, S., Dunlop, P., McGaw, M., Marchant, R., et al. (2016). Resazurin-based 96-well plate microdilution method for the determination of minimum inhibitory concentration of biosurfactants. Biotechnol. letters. 38, 1015–1019. doi: 10.1007/s10529-016-2079-2
Ferreira, N. S., Martinho, F. C., Cardoso, F. G., Nascimento, G. G., Carvalho, C. A., and Valera, M. C. (2015). Microbiological profile resistant to different intracanal medications in primary endodontic infections. J. endodontics. 41, 824–830. doi: 10.1016/j.joen.2015.01.031
Fouad, A. F. (2019). Microbiological aspects of traumatic injuries. J. endodontics. 45, S39–S48. doi: 10.1016/j.joen.2019.05.011
Franzblau, S. G., Witzig, R. S., McLaughlin, J. C., Torres, P., Madico, G., Hernandez, A., et al. (1998). Rapid, low-technology MIC determination with clinical Mycobacterium tuberculosis isolates by using the microplate Alamar Blue assay. J. Clin. Microbiol. 36, 362–366. doi: 10.1128/JCM.36.2.362-366.1998
Garg, P., Tyagi, S. P., Sinha, D. J., Singh, U. P., Malik, V., and Maccune, E. R. (2014). Comparison of antimicrobial efficacy of propolis, Morinda citrifolia, Azadirachta indica, triphala, green tea polyphenols and 5.25% sodium hypochlorite against Enterococcus fecalis biofilm. Saudi endodontic J. 4, 122–127. doi: 10.4103/1658-5984.138141
Glynis, A., Foschi, F., Kefalou, I., Koletsi, D., and Tzanetakis, G. N. (2021). Procedures for the treatment of necrotic mature teeth with apical periodontitis: A systematic review and meta-analysis of randomized controlled trials. J. OF ENDODONTICS. 47, 873–882. doi: 10.1016/j.joen.2021.03.015
Haney, E. F., Trimble, M. J., Cheng, J. T., Vallé, Q., and Hancock, R. E. (2018). Critical assessment of methods to quantify biofilm growth and evaluate antibiofilm activity of host defence peptides. Biomolecules 8, 29. doi: 10.3390/biom8020029
Hargreaves, K. M., Diogenes, A., and Teixeira, F. B. (2013). Treatment options: biological basis of regenerative endodontic procedures. J. Endodontics. 39, S30–S43. doi: 10.1016/j.joen.2012.11.025
Harun, N. A., Ramli, N., Azli, A. R. K., Hassan, H., Adam, K. B. C., and Halil, M. H. M. (2023). The effect of Salvadora persica ethanolic extract on oral tissue healing in rats: An in vivo study. Saudi Dental J. 35, 663–667. doi: 10.1016/j.sdentj.2023.05.019
Henklewska, M., Pawlak, A., Li, R.-F., Yi, J., Zbyryt, I., and Obmińska-Mrukowicz, B. (2021). Benzyl isothiocyanate, a vegetable-derived compound, induces apoptosis via ROS accumulation and DNA damage in canine lymphoma and leukemia cells. Int. J. Mol. Sci. 22, 11772. doi: 10.3390/ijms222111772
Hoch, C. C., Shoykhet, M., Weiser, T., Griesbaum, L., Petry, J., Hachani, K., et al. (2024). Isothiocyanates in medicine: A comprehensive review on phenylethyl-, allyl-, and benzyl-isothiocyanates. Pharmacol. Res. 201, 107107. doi: 10.1016/j.phrs.2024.107107
Huang, G.-J., Gronthos, S., and Shi, S. (2009). Critical reviews in oral biology & medicine: mesenchymal stem cells derived from dental tissues vs. those from other sources: their biology and role in regenerative medicine. J. Dental Res. 88, 792. doi: 10.1177/0022034509340867
ISO 10993-5 (2009). Biological evaluation of medical devices — Part 5: tests for in vitro cytotoxicity. Available online at: https://www.iso.org/standard/36406.html.
Kaiser, S. J., Mutters, N. T., Blessing, B., and Günther, F. (2017). Natural isothiocyanates express antimicrobial activity against developing and mature biofilms of Pseudomonas aeruginosa. Fitoterapia 119, 57–63. doi: 10.1016/j.fitote.2017.04.006
Khosropanah, H., Lashkarizadeh, N., Ayatollahi, M., Kaviani, M., and Mostafavipour, Z. (2018). The impact of calcium hydroxide on the osteoinductive capacity of demineralized freeze-dried bone allograft: an in-vitro study. J. Dentistry. 19, 19. doi: 10.30476/dentjods.2018.41787
Kim, S., Malek, M., Sigurdsson, A., Lin, L., and Kahler, B. (2018). Regenerative endodontics: a comprehensive review. Int. endodontic J. 51, 1367–1388. doi: 10.1111/iej.12954
Kontakiotis, E. G., Filippatos, C. G., Tzanetakis, G. N., and Agrafioti, A. (2015). Regenerative endodontic therapy: A data analysis of clinical protocols. J. Endodontics. 41, 146–154. doi: 10.1016/j.joen.2014.08.003
Latham, J., Fong, H., Jewett, A., Johnson, J. D., and Paranjpe, A. (2016). Disinfection efficacy of current regenerative endodontic protocols in simulated necrotic immature permanent teeth. J. endodontics. 42, 1218–1225. doi: 10.1016/j.joen.2016.05.004
Lin, J., Zeng, Q., Wei, X., Zhao, W., Cui, M., Gu, J., et al. (2017). Regenerative endodontics versus apexification in immature permanent teeth with apical periodontitis: a prospective randomized controlled study. J. endodontics. 43, 1821–1827. doi: 10.1016/j.joen.2017.06.023
Liu, J., Yu, F., Sun, Y., Jiang, B., Zhang, W., Yang, J., et al. (2015). Concise reviews: characteristics and potential applications of human dental tissue-derived mesenchymal stem cells. Stem Cells 33, 627–638. doi: 10.1002/stem.1909
Liu, J., Zhang, K., Song, J., Wu, H., Hao, H., Bi, J., et al. (2021). Bacteriostatic effects of benzyl isothiocyanate on Vibrio parahaemolyticus: Transcriptomic analysis and morphological verification. BMC Biotechnol. 21, 56. doi: 10.1186/s12896-021-00716-4
Mohammadi, Z. and Dummer, P. M. H. (2011). Properties and applications of calcium hydroxide in endodontics and dental traumatology. Int. endodontic J. 44, 697–730. doi: 10.1111/j.1365-2591.2011.01886.x
Murray, P. E., Garcia-Godoy, F., and Hargreaves, K. M. (2007). Regenerative endodontics: a review of current status and a call for action. J. endodontics. 33, 377–390. doi: 10.1016/j.joen.2006.09.013
Niazy, A. A., Lambarte, R. N. A., Sumague, T. S., Vigilla, M. G. B., Bin Shwish, N. M., Kamalan, R., et al. (2024). FTY720 reduces the biomass of biofilms in pseudomonas aeruginosa in a dose-dependent manner. Antibiotics 13, 621. doi: 10.3390/antibiotics13070621
Niu, T.-X., Wang, X.-N., Wu, H.-Y., Bi, J.-R., Hao, H.-S., Hou, H.-M., et al. (2020). Transcriptomic analysis, motility and biofilm formation characteristics of Salmonella typhimurium exposed to benzyl isothiocyanate treatment. Int. J. Mol. Sci. 21, 1025. doi: 10.3390/ijms21031025
Nowicki, D., Rodzik, O., Herman-Antosiewicz, A., and Szalewska-Pałasz, A. (2016). Isothiocyanates as effective agents against enterohemorrhagic Escherichia coli: insight to the mode of action. Sci. Rep. 6, 22263. doi: 10.1038/srep22263
Parchami, K., Dastorani, M., and Barati, M. (2024). What is the impact of Endodontic Irrigant Solutions on the Viability of Stem Cells from Apical Papilla in an in-vitro setting: A Systematic Review. Saudi Dental J. 36, 1170–1178. doi: 10.1016/j.sdentj.2024.07.006
Romeo, L., Diomede, F., Gugliandolo, A., Scionti, D., Lo Giudice, F., Lanza Cariccio, V., et al. (2018a). Moringin induces neural differentiation in the stem cell of the human periodontal ligament. Sci. Rep. 8, 9153. doi: 10.1038/s41598-018-27492-0
Romeo, L., Iori, R., Rollin, P., Bramanti, P., and Mazzon, E. (2018b). Isothiocyanates: An overview of their antimicrobial activity against human infections. Molecules 23, 624. doi: 10.3390/molecules23030624
Sabrah, A. H., Yassen, G. H., and Gregory, R. L. (2013). Effectiveness of antibiotic medicaments against biofilm formation of Enterococcus faecalis and Porphyromonas gingivalis. J. endodontics. 39, 1385–1389. doi: 10.1016/j.joen.2013.05.003
Sathorn, C., Parashos, P., and Messer, H. (2007). Antibacterial efficacy of calcium hydroxide intracanal dressing: a systematic review and meta-analysis. Int. endodontic J. 40, 2–10. doi: 10.1111/j.1365-2591.2006.01197.x
Sedgley, C. M., Lee, E. H., Martin, M. J., and Flannagan, S. E. (2008). Antibiotic resistance gene transfer between Streptococcus gordonii and Enterococcus faecalis in root canals of teeth ex vivo. J. endodontics. 34, 570–574. doi: 10.1016/j.joen.2008.02.014
Simonsen, J. L., Rosada, C., Serakinci, N., Justesen, J., Stenderup, K., Rattan, S. I., et al. (2002). Telomerase expression extends the proliferative life-span and maintains the osteogenic potential of human bone marrow stromal cells. Nat. Biotechnol. 20, 592–596. doi: 10.1038/nbt0602-592
Siqueira, J. F., Jr. and Rôças, I. N. (2022). Present status and future directions: Microbiology of endodontic infections. Int. endodontic J. 55, 512–530. doi: 10.1111/iej.13677
Sjögren, U., Figdor, D., Spångberg, L., and Sundqvist, G. (1991). The antimicrobial effect of calcium hydroxide as a short-term intracanal dressing. Int. endodontic J. 24, 119–125. doi: 10.1111/j.1365-2591.1991.tb00117.x
Sofrata, A., Santangelo, E. M., Azeem, M., Borg-Karlson, A.-K., Gustafsson, A., and Pütsep, K. (2011). Benzyl isothiocyanate, a major component from the roots of Salvadora persica is highly active against Gram-negative bacteria. PloS One 6, e23045. doi: 10.1371/journal.pone.0023045
Song, J., Hou, H.-M., Wu, H.-Y., Li, K.-X., Wang, Y., Zhou, Q.-Q., et al. (2019). Transcriptomic analysis of Vibrio parahaemolyticus reveals different virulence gene expression in response to benzyl isothiocyanate. Molecules 24, 761. doi: 10.3390/molecules24040761
Torabinejad, M., Nosrat, A., Verma, P., and Udochukwu, O. (2017). Regenerative endodontic treatment or mineral trioxide aggregate apical plug in teeth with necrotic pulps and open apices: a systematic review and meta-analysis. J. endodontics. 43, 1806–1820. doi: 10.1016/j.joen.2017.06.029
Vishwanat, L., Duong, R., Takimoto, K., Phillips, L., Espitia, C. O., Diogenes, A., et al. (2017). Effect of bacterial biofilm on the osteogenic differentiation of stem cells of apical papilla. J. endodontics. 43, 916–922. doi: 10.1016/j.joen.2017.01.023
Vrca, I., Jug, B., Fredotović, Ž, Vuko, E., Brkan, V., Šestić, L., et al. (2023). Significant benefits of environmentally friendly hydrosols from Tropaeolum majus L. seeds with multiple biological activities. Plants 12, 3897. doi: 10.3390/plants12223897
Wang, X., Wu, H., Niu, T., Bi, J., Hou, H., Hao, H., et al. (2019). Downregulated expression of virulence factors induced by benzyl isothiocyanate in Staphylococcus aureus: a transcriptomic analysis. Int. J. Mol. Sci. 20, 5441. doi: 10.3390/ijms20215441
Yang, J., Hediyal, T. A., Chidambaram, S. B., Kaul-Ghanekar, R., and Sakharkar, M. K. (2024). Benzyl isothiocyanate as an alternative to antibiotics? a comparative in vivo study using Pseudomonas aeruginosa infection as a model. PloS One 19, e0303490. doi: 10.1371/journal.pone.0303490
Zandi, H., Kristoffersen, A. K., Ørstavik, D., Rôças, I. N., Siqueira, J. F., Jr., and Enersen, M. (2018). Microbial analysis of endodontic infections in root-filled teeth with apical periodontitis before and after irrigation using pyrosequencing. J. Endodontics. 44, 372–378. doi: 10.1016/j.joen.2017.11.019
Zanichelli, F., Capasso, S., Di Bernardo, G., Cipollaro, M., Pagnotta, E., Cartenì, M., et al. (2012). Low concentrations of isothiocyanates protect mesenchymal stem cells from oxidative injuries, while high concentrations exacerbate DNA damage. Apoptosis 17, 964–974. doi: 10.1007/s10495-012-0740-3
Zhang, T. and Chen, W. (2017). The Candida albicans inhibitory activity of the extract from papaya (Carica papaya L.) seed relates to mitochondria dysfunction. Int. J. Mol. Sci. 18, 1858. doi: 10.3390/ijms18091858
Zhao, T., Chen, J., Liu, S., Yang, J., Wu, J., Miao, L., et al. (2022). Transcriptome analysis of Fusobacterium nucleatum reveals differential gene expression patterns in the biofilm versus planktonic cells. Biochem. Biophys. Res. Commun. 593, 151–157. doi: 10.1016/j.bbrc.2021.11.075
Keywords: benzyl isothiocyanate, Fusobacterium nucleatum, antimicrobial, antibiofilm, calcium hydroxide, regenerative endodontics, stem cells, viability
Citation: Almobarak AA, Alqedairi A, Binrayes A, Lambarte RA, Niazy AA and Aljarbou F (2025) Benzyl isothiocyanate exhibits antibacterial and antibiofilm activity against Fusobacterium nucleatum while preserving viability of human bone marrow mesenchymal stem cells: an in vitro study. Front. Cell. Infect. Microbiol. 15:1683203. doi: 10.3389/fcimb.2025.1683203
Received: 10 August 2025; Accepted: 24 September 2025;
Published: 24 October 2025.
Edited by:
J. Christopher Fenno, University of Michigan, United StatesReviewed by:
Riham H. Ahmed, Misr International University, EgyptFasiha Moin Kazi, Dow University of Health Sciences, Pakistan
Copyright © 2025 Almobarak, Alqedairi, Binrayes, Lambarte, Niazy and Aljarbou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdulaziz A. Almobarak, YWxtb2JhcmFrLmFhQGdtYWlsLmNvbQ==; Fahd Aljarbou, ZmFsamFyYm91QGtzdS5lZHUuc2E=
 Abdulaziz A. Almobarak
Abdulaziz A. Almobarak Abdullah Alqedairi1
Abdullah Alqedairi1 Abdulaziz Binrayes
Abdulaziz Binrayes Rhodanne A. Lambarte
Rhodanne A. Lambarte Abdurahman A. Niazy
Abdurahman A. Niazy