- 1Behavioural Science Institute, Radboud University, Nijmegen, Netherlands
- 2Academy for Engineering and Information Technology, Avans University of Applied Science, Breda, Netherlands
- 3Kentalis Academy, Royal Dutch Kentalis, Sint-Michielsgestel, Netherlands
Background: In persons with combined intellectual and sensory disabilities, mood disorders, stress reactions, and attachment problems are more prevalent. This study assessed the presence of these problems within this target population and the effects of an additional Autism Spectrum Disorder (ASD).
Methods: Participants were 60 persons with combined intellectual and sensory disabilities, all participants had visual impairments, 16 were deafblind. ASD was assessed with Observation of Autism in people with Sensory and Intellectual Disabilities. Additionally the Anxiety, Depression and Mood Scale, The list of Disturbed Attachment Behaviors and the Stress Survey Schedule were used.
Results: Almost every participant showed signs of a disturbed attachment. Stress and mood disorders were not prevalent. An additional ASD resulted in more disturbed attachment, manic and hyperactive behavior and social avoidance.
Conclusion: Only for disturbed attachment a relatively high prevalence was found. The presence of ASD sometimes led to a different profile of the assessed problems.
Introduction
Mental health and behavioral problems are very common in persons with a combination of sensory and intellectual disabilities (ID). Examples are depression or mood disorders (Hurley, 2006) and strong reactions to stress (Bloeming-Wolbrink et al., 2012). Behaviors indicative of insecure attachment, such as stereotyped behaviors or aggressive behaviors, are also shown often (Janssen et al., 2002; Poppes et al., 2010). In addition, both people with sensory and people with intellectual disabilities often show symptoms that are also seen in people with Autism Spectrum Disorder (ASD) (De Bildt et al., 2005; Dammeyer, 2011). Note that according to Russell et al. (2019) global estimates suggest the proportion of the population with ASD who have additional ID is approximately 50%. However, in most studies people with ID are excluded from participation. Russell et al. (2019) found that 80% of the studies demonstrated a selection bias against participants with ID. As a result a keen follower of the literature might get the impression ASD and ID are completely discrete phenomena, whereas in reality there is large overlap. ASD in itself is also associated with more mental health problems (e.g., Corbett et al., 2006; Stewart et al., 2006). Therefore, ASD in addition to sensory and intellectual disabilities is also related to high rates of mental health problems in people with multiple disabilities. This makes the diagnosis of mental health problems very complex, since symptoms, such as stereotyped behavior, are not only indications of mental health problems, they are also core characteristics of ASD (American Psychiatric Association, 2013) and are also often shown by persons with multiple disabilities without ASD (Hoevenaars-van den Boom et al., 2009; De Vaan et al., 2016b).
The goal of the current study is to describe the range of mental health problems in a group of people with moderate to profound intellectual disability combined with a visual impairment or deafblindness, with and without symptoms of ASD. Mild intellectual disabilities were disregarded because previous research showed that level of visual impairment is strongly correlated with moderate to profound levels of intellectual disability, with persons with severe intellectual disabilities showing more profound visual disabilities (van Splunder et al., 2003, 2006; Evenhuis et al., 2009).
People with sensory and intellectual disabilities can encounter problems in developing a secure attachment style (Fraiberg, 1977; Janssen et al., 2002; Stor and Storsbergen, 2006). This is similar to children with ASD, who are generally less securely attached to their caregivers, especially when the ASD is combined with an intellectual disability (Rutgers et al., 2004, 2007; van IJZendoorn et al., 2007). An insecure attachment relationship has severe consequences, such as disturbances in emotional well-being, the occurrence of externalizing behavior problems and inadequate reactions to stress (Stor and Storsbergen, 2006; Fearon et al., 2010).
Persons with sensory impairments and intellectual disabilities are also thought to be more susceptible to stress. Because of their impairments, sensory information is often missed, making their everyday lives more unpredictable and thus more stressful (Dickerson and Kemeny, 2004; Corbett et al., 2006; Bloeming-Wolbrink et al., 2012). Furthermore, for people with disabilities it may be more difficult to cope with these stressors, especially when they cannot seek comfort with an attachment figure (Janssen et al., 2002; Schuengel and Janssen, 2006). When there is an additional diagnosis of ASD, persons are even more susceptible to stress, for example in new and unfamiliar situations (Corbett et al., 2006) or in social situations (Dickerson and Kemeny, 2004).
Finally, both persons with disabilities and persons with ASD have been shown to be susceptible to develop mood disorders (Hurley, 2006; Stewart et al., 2006). In turn, mood disorders, anxiety, and stress can lead to social withdrawal and an increase in stereotyped behaviors (Kraijer, 2004; Stewart et al., 2006; Rubin et al., 2013), which are all also symptoms of ASD (American Psychiatric Association, 2013). Mental health problems such as these could thus increase the severity of ASD symptoms. This is supported by Ghaziuddin et al. (2002) who stated that curing mood disorders could also reduce the ASD symptoms. Insight in prevalent mental health issues in this population is therefore helpful for treatment.
A rationale for the co-occurrence of disorders in affect regulation, attachment behaviors and stress reactions has been given by Janssen et al. (2002) and Schuengel and Janssen (2006) in their stress-attachment model of challenging behaviors in people with intellectual disability. According to this model there is evidence that people with ID are more vulnerable to stress and use less effective coping strategies once they are confronted with stressful situations. In addition, they claim that studies on attachment indicate that people with intellectual disability are at risk for developing insecure, especially disorganized, attachment. Stress and insecure or disorganized attachment in combination with less effective coping styles is thought to put people with intellectual disabilities at risk for developing behavior problems.
The symptoms of ASD and mental health problems overlap in the population of persons with combined intellectual and sensory disabilities. This makes it rather difficult to assess the etiology of their behaviors. A consequence is that this may lead to an overdiagnosis as well as an underdiagnosis of mental health problems in this target group. This phenomenon, where behaviors are unfairly attributed to the most notable disability, is called diagnostic overshadowing (Mason and Scior, 2004). ASD in addition to the intellectual and sensory disabilities complicates both diagnosis and treatment. To prevent inaccurate diagnoses and treatments it is important to create a complete profile of mental health problems and behaviors related to experiencing and coping with stress and insecure attachment. For the population of people with combined sensory and intellectual disabilities this has not been done yet. Because both the combinations of sensory and intellectual disabilities as well as ASD and intellectual disabilities increase the risk for mental health problems, it is likely that the combination of intellectual disability, sensory impairments and ASD puts people at an even higher risk of developing mental health problems, stress reactions, and insecure attachment styles.
Firstly, conditions that might cause behavioral problems: insecure attachment and stress reactions, are studied, next to the presence of some of the most common mental health problems that have been described for this population: mood disorders, anxiety, and manic and hyperactive behavior. Secondly, this study will assess whether the presence of ASD symptoms in this population is related to a different profile of mental health problems, stress reactions and attachment styles in people with combined sensory and intellectual disabilities.
Materials and Methods
Participants
Participants were recruited in four locations of three residential institutions and in three schools for people with sensory and intellectual disabilities within the Netherlands. We believe a representative sample was reached by recruiting in locations of all of the institutions and schools specialized in our target population within the Netherlands. Inclusion criteria were (1) a moderate to profound intellectual disability, (2) a visual impairment according to the ICD-10 version 2016 criteria (World Health Organization [WHO], 2019), (3) between 6 and 60 years of age. Participants were selected by a contact person from each facility to maintain anonymity until consent for participation was given. Because of this procedure there was no information about response rate.
Participants were 60 people aged between 6 and 55 years old (M = 31.6, SD = 14.9). The sample consisted of 42 males and 18 females. Participants were diagnosed with moderate (n = 11), severe (n = 24), or profound (n = 25) intellectual disabilities. All participants had a visual impairment (n = 30) or were blind with or without light perception (n = 30). There were 16 participants with additional auditory impairments. According to the definitions of Dammeyer (2012) and Ask Larsen and Damen (2014) they were deafblind. ASD symptoms were determined as part of an earlier study using the instrument “Observation of Autism in people with Sensory and Intellectual Disabilities” (OASID) (De Vaan et al., 2016a, 2018). This instrument was designed specifically for this target population. OASID is an ASD screening instrument that can be used as part of the assessment of presumed ASD in people with multiple disabilities (De Vaan et al., 2016a). In the current study OASID was used to split the group of participants in half. A group with many ASD symptoms (N = 32) and a group with few symptoms (N = 28). Sensory impairments and intellectual disabilities were diagnosed prior to and independent of this study by licensed psychologists or physicians. For this study, this information was retrieved directly from the participants’ records of their residential facility or school.
Materials
List of Disturbed Attachment Behaviors
The list of disturbed attachment behaviors (Boris and Zeanah, 2005) is a screening instrument that gives an indication of how securely attached persons are to their caregivers. The questionnaire consists of eight behavior descriptions on a 5-point Likert scale. A total score is calculated by adding scores on the eight individual questions. Higher scores are indicative of more disturbed attachment behaviors (Stor and Storsbergen, 2006).
Anxiety, Depression, and Mood Scale
The Dutch translation (Hermans et al., 2008) of the Anxiety Depression and Mood Scale (ADAMS; Esbensen et al., 2003a) was used. The ADAMS consists of 28 multiple choice questions, in which the prevalence or severity of behaviors are rated on a scale from 0 (not a problem) to 3 (severe problem). The 28 items are divided over five scales: “manic/hyperactive behavior,” “depressed mood,” “social avoidance,” “general anxiety,” and “compulsive behavior.” The ADAMS is a psychometrically valid and reliable screening tool for anxiety, depression and mood disorders in individuals with an intellectual disability (Esbensen et al., 2003b).
Stress Survey Schedule
The Stress Survey Schedule for Autism and Other Developmental Disabilities (SSS; Groden, 2001) is a 62-items questionnaire that can be used to measure stress and identify specific stressors for individuals with ASD and other developmental disabilities (Groden et al., 2001). All items are rated on 5-point scales of stress intensity, ranging from “none to mild” to “severe.” A score can be calculated for 10 potential problem areas: “changes,” “anticipation,” “unpleasant,” “positive,” “sensory/personal,” “food related,” “social/environmental,” “rituals,” “fears,” and “life stressors.” The SSS was found to be valid and reliable for its purpose (Groden et al., 2001).
Procedure
This study was approved by the Committee on Research Involving Human Subjects, Arnhem-Nijmegen, and was in line with the Ethical Principles for Medical Research Involving Human Subjects of the World Medical Association declaration of Helsinki (World Medical Association, 2013). Participants were recruited through their residential facility or school. Because of ethical and legal requirements parents or legal representatives were asked for informed consent. After consent was given, a caregiver from the residential facility, who was most familiar to the participant, filled in the questionnaires.
In order to assess whether the participants had scores within the clinical ranges, we compared scores of our participants to norms or cut-off scores of these questionnaires when available. When cut-off scores or norms were not published, scores of participants were compared to mean scores of similar populations.
Results
Attachment
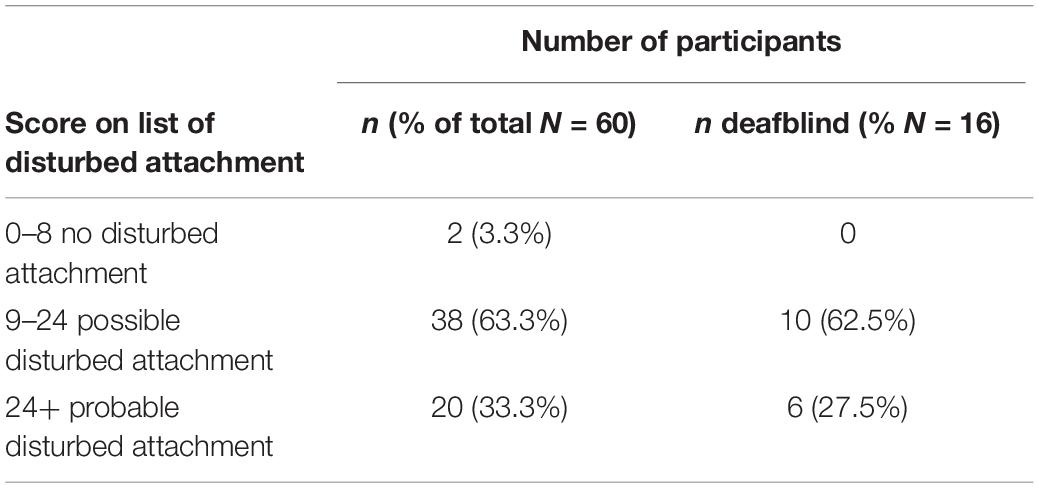
For the list of disturbed attachment behaviors, scores ranging from 0 to 8 indicate no disturbed attachment, scores ranging from 8 to 24 indicate possible disturbed attachment, and scores of 24 and above indicate a probable disturbed attachment (Stor and Storsbergen, 2006). Table 1 shows how many participants fell into each category.
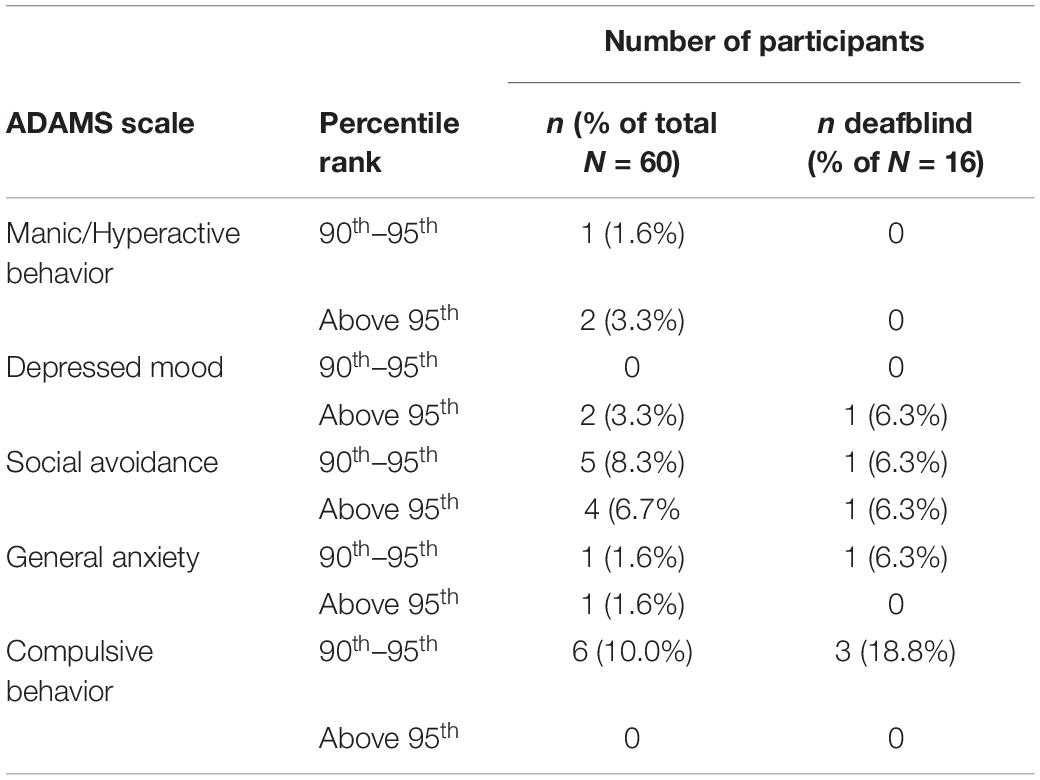
Anxiety, Depression, and Mood
For the ADAMS, cut-off scores have only been reported for the Depressed Mood and General Anxiety subscale. These cut-off scores are meant for screening purposes (Hermans et al., 2012). For people with moderate to profound intellectual disabilities, the Depressed Mood cut-off is a score of 11. Two participants scored above the cut-off (3.3%), one of them was deafblind. In addition, Esbensen et al. (2003b) reported percentile ranks for a large group of participants. Table 2 shows how many participants from the current study scored above the 90th and 95th percentile rank.
Stress Survey Schedule
For the Stress Survey Schedule, mean scores were reported as a function of sex, verbal ability or age (Goodwin et al., 2007). Since the larger part of our group consisted of non-verbal participants or participants with very limited verbal skills, we compared our participants to the non-verbal group that was reported by Goodwin et al. (2007). Table 3 shows this comparison. Reported are how many participants scored two SD’s or more above the mean.
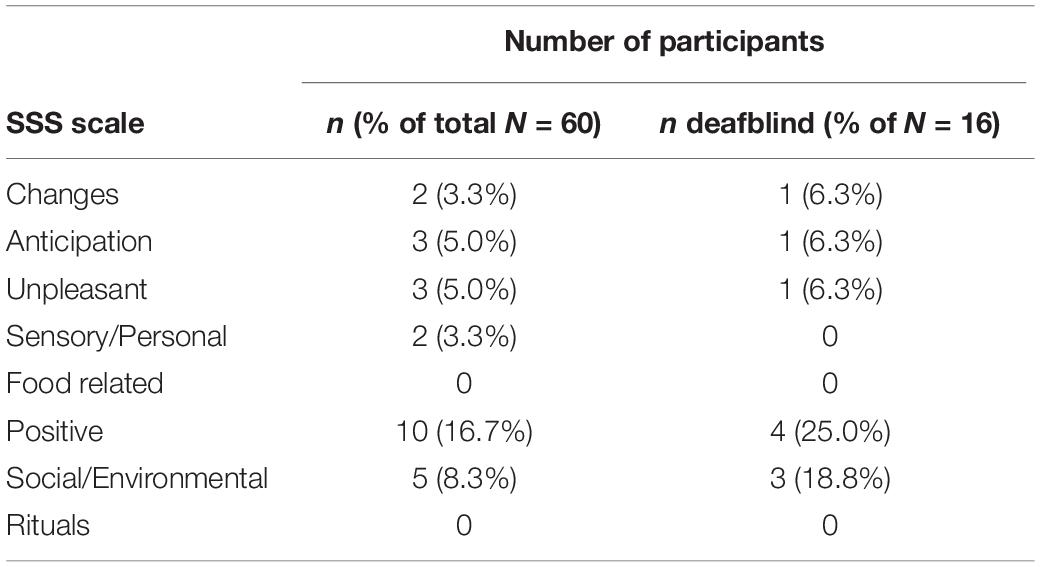
Table 3. Number of participants with two SD’s or more above the mean for the SSS scale compared to non-verbal persons.
Differences Between Few and Many ASD Symptoms
Differences between participants with few and many ASD symptoms (based on OASID scores, see De Vaan et al., 2018) were compared using non-parametric Mann-Whitney U tests. Corresponding effect sizes were calculated by the following formula r = z/√N (Pallant, 2010). All medians and significant differences between the two groups on the List of Disturbed Attachment, ADAMS and SSS are presented in Table 4. Participants with many ASD symptoms scored significantly higher than participants without ASD symptoms on the list of disturbed attachment and on the ADAMS scales Manic and Hyperactive behavior and Social Avoidance. Participants with few ASD symptoms scored higher on the SSS scale “Unpleasant” than people with many ASD symptoms. All effect sizes were medium. Within the group of participants with many ASD symptoms, five participants were deafblind. The remaining 11 participants with deafblindness showed few ASD symptoms.
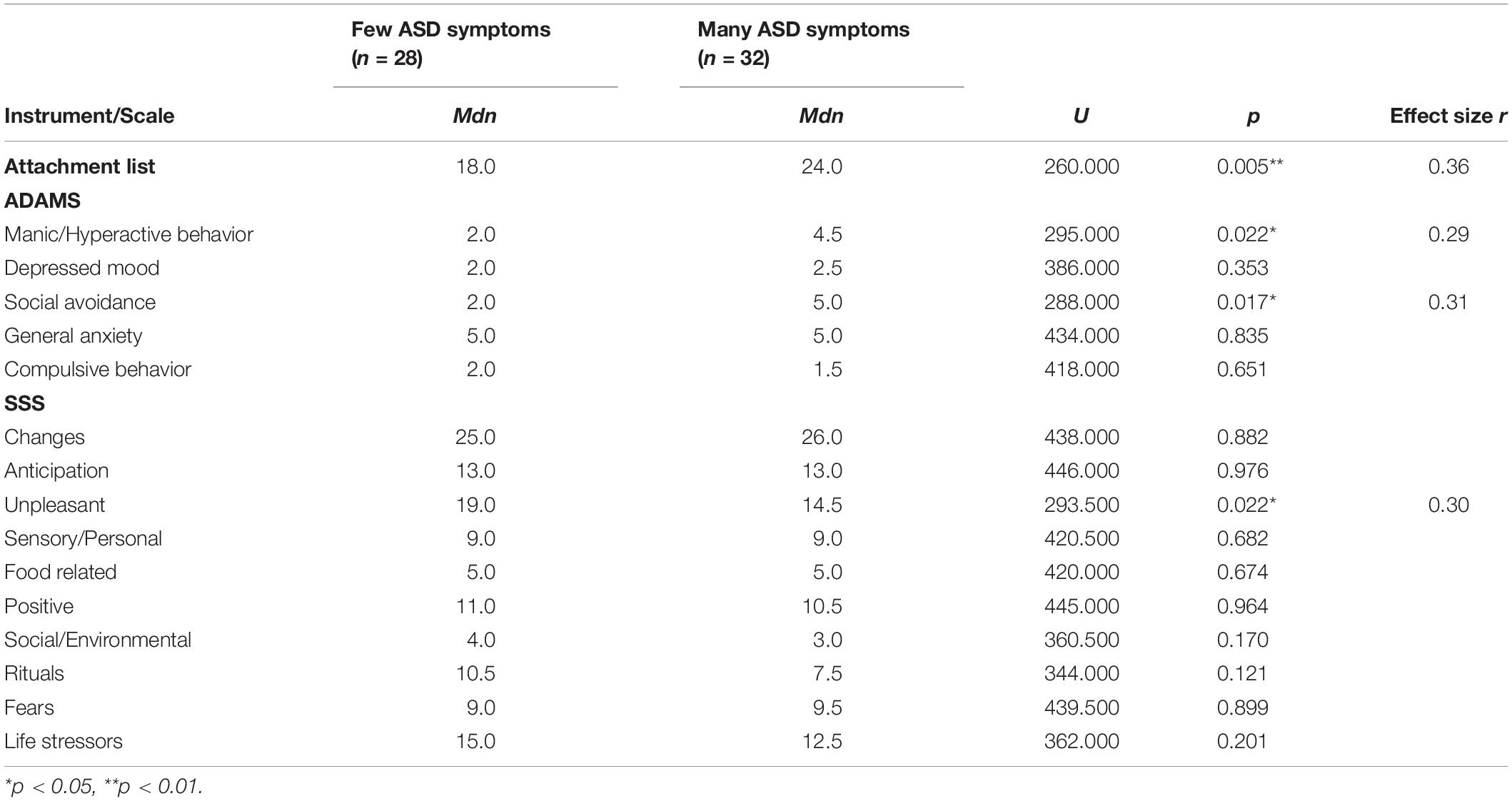
Table 4. Differences between groups with few and many symptoms of ASD on attachment, anxiety, depression and mood, and stress.
With regard to IQ, age, and physical disabilities of the participants we found no correlation between age, visual and auditory impairments with OASID scores. There were slightly more participants with severe and profound intellectual disability with high OASID scores.
Discussion
The current study investigated the presence of mental health problems, insecure attachment, and stress reactions in persons with a combination of sensory and intellectual disabilities. First, the attachment style, stress reactions and presence of anxiety, depression, and mood disorders were studied in the target population by comparing them to norm scores or cut-off scores. Secondly, the effect of the number of ASD symptoms on these mental health problems and behaviors was assessed by looking at the differences in scores between participants with few and many ASD symptoms.
On the list of disturbed attachment signals, only a very small proportion of the study sample did not show signs of a disturbed attachment. The larger part of the participants scored within the range of a “possible disturbed attachment.” A quarter of the sample had a score that indicated a “probable disturbed attachment.” Though the literature suggests that disabilities as well as ASD can both contribute to the development of a less secure attachment style (e.g., Janssen et al., 2002; Rutgers et al., 2004; Stor and Storsbergen, 2006), these numbers are still quite high. The stress-attachment model of challenging behaviors in people with intellectual disability of Janssen et al. (2002) and Schuengel and Janssen (2006), mentioned in the introduction, accounts for the link between attachment, ID and problematic behavior, that is inadequate coping. A treatment based on this model was designed by Sterkenburg (2008), who has shown that an attachment based treatment (i.e., first working on the therapist client relation before using applied behavior analysis techniques for treating discrete behavior) in persons with sensory and intellectual disabilities can help to regulate stress and reduce challenging behavior. In line with this intervention it is therefore recommended to screen for attachment related problems in persons from this population and that behavioral treatment is adjusted in the case that disturbed attachment is encountered. There is, however, still the possibility that the prevalence of attachment problems in the current study is slightly overestimated. The list of disturbed attachment signals is not specifically developed for this population and some signals may have been unfairly attributed to attachment problems when they are in fact part of their intellectual or sensory disability. Nevertheless, it is important to remain vigilant for signs of an insecure attachment style within this population.
The results on the ADAMS revealed that only a few participants scored above the 90th percentile on any of the scales. Based on the ADAMS’ results there is no reason to believe that the participants showed clinically concerning manic/hyperactive behaviors, general anxiety, depressed mood, or compulsive behaviors. For social avoidance high scores were found. Fifteen percent of the participants scored above the 90th percentile. This figure is not surprising given the fact that ASD symptoms were also highly prevalent in the study group and social problems, including social avoidance, is one of the key characteristics of ASD (American Psychiatric Association, 2013).
With the SSS stressful situations for the participants were identified. The norm group used for comparison were non-verbal participants from an earlier study by Groden et al. (2001). Since the larger part of the current sample was non-verbal, this was the most appropriate group to compare the participants to. On most of the scales of the SSS less than 10% of the group scored more than two SD’s above the mean of the non-verbal control group.
In the second part of the study the differences between participants with few and many ASD symptoms were assessed. It was found that participants with many ASD symptoms scored higher on the disturbed attachment list and the ADAMS scales “manic/hyperactive behavior” and “social avoidance.” This result is in line with earlier research that persons with ASD show less secure attachment styles than persons without ASD (Rutgers et al., 2004, 2007; van IJZendoorn et al., 2007). It is also related to another finding in the current study, namely that participants with many ASD symptoms show more social avoidance. In itself, this finding makes sense, as social avoidance is a symptom of ASD (Richer, 1976; American Psychiatric Association, 2013), and additional impairments in social skills can also lead to a less secure attachment style (Rutgers et al., 2007). The finding that participants with many ASD symptoms scored higher on manic and hyperactive behaviors is in line with expectations, because hyperactivity is frequently observed in persons with ASD (Aman and Langworthy, 2000; American Psychiatric Association, 2013). Participants with few ASD symptoms scored higher on the SSS scale “unpleasant.” This indicates that persons with few ASD symptoms show stronger stress reactions to unpleasant events than persons with many ASD symptoms. There might be a logical explanation for this. Items on this scale include questions related to receiving criticism from others (Groden, 2001). Impairments in the social domain and their level of cognitive impairment make it difficult for persons with many ASD symptoms to understand criticism, and thus, they experience it as less stressful. On the other SSS scales no significant differences were found between participants with few and many ASD symptoms.
All of our participants had an intellectual disability and a visual impairment. Sixteen participants had an additional auditory impairment, meaning that they were deafblind. Although it was not statistically confirmed because it was not a part of our main focus, our results showed no striking over- or underrepresentation of deafblind participants in any of the analyses. This indicates that the results that were found are representative for a broad group of persons with combined intellectual and sensory impairments, and that having an additional auditory impairment does not appear to make one more sensitive for developing any of the mental health problems described in this study.
The profiles of participants with many ASD symptoms were slightly different from profiles of participants with few ASD symptoms, much of which could be due to attributing ASD symptoms either to attachment style, stress reactions, anxiety and mood disorders instead of ASD. It is therefore recommended that when these symptoms occur, especially problems related to an insecure attachment style, manic and hyperactive behaviors and social avoidance, to always also consider the presence of ASD. When ASD is likely present, any intervention should keep into account typical ASD behavior. However, when ASD is absent, these same symptoms may be caused by another mental health problem such as a mood disorder or ADHD and treatment should be tailored to these disorders.
This study has some limitations. First, there are only a few instruments that are specifically developed for the population of people with combined sensory and intellectual disabilities. A recent study has shown that instruments that were not specifically developed for this populations items are not always valid (De Vaan et al., 2016b). In addition, because of the specific target population, norms, or cut-off scores for this population are often not available and it is difficult to decide which group is most appropriate for comparison. In this study, the list of disturbed attachment behaviors did not have separate norms for specific populations and the ADAMS only for persons with intellectual disabilities without sensory impairments. For the SSS our best comparison group were non-verbal persons. More research is needed to develop new instruments or at least norms for this specific target population so that mental health problems can be assessed validly.
A second limitation is that in ASD several severity levels can be distinguished (American Psychiatric Association, 2013). The diagnosis of ASD for this study was done with the OASID that distinguishes three severity levels of ASD (De Vaan et al., 2018), besides a no ASD level. However, because of small numbers of participants in each ASD severity level, all participants with ASD were combined to form the group with many ASD symptoms. By categorizing this variable the variation in severity of ASD symptoms got lost. For future studies, it would be interesting to see whether the severity of ASD is positively correlated to the number of mental health problems, stress reactions and attachment style.
Persons with multiple disabilities show behaviors that could be interpreted as symptoms of several mental health problems, including ASD, depression, anxiety, and to symptoms as a result of stress or an insecure attachment. Depending on the diagnostic instruments that are used, one or more of these behaviors could be diagnosed. Traditionally, this is seen as comorbidity, with each symptom having its own underlying pathological process, similar to somatic diseases. An alternative view, network analysis, was presented more recently. Network analyses have shown that symptoms interact and influence each other, creating a new network of symptoms that are not necessarily linked to one specific diagnosis but may be activated by other symptoms (Borsboom and Cramer, 2013; Bringmann et al., 2013; Boschloo et al., 2015; Epskamp et al., 2018). It is argued that in mental health, symptoms can be the result of many different processes, causes and even symptoms of other disorders. Disorders are often diagnosed together because several symptoms are part of different disorders; they are not unique for one disorder. These are the bridging symptoms (Fried et al., 2017). From the point of view of network analysis the presence of a large number of ASD symptoms and insecure attachment diagnoses in the population described in the current study is completely understandable, since ASD and insecure attachment, stress and sensory disorders share several symptoms.
Concluding, the current study explored the presence of mental health problems in persons with combined sensory and intellectual disabilities. It showed that most participants with sensory and intellectual disabilities showed signs of a disturbed attachment and these problems are largest in the ASD group. This finding is important for clinical practice and we recommend that in this population everyone is screened for attachment related problems and treatment is adjusted to these findings. In addition, it was found that participants with ASD show more disturbed attachment behaviors, manic and hyperactive behavior and more social avoidance than persons without ASD. The presence of ASD led to a different profile of mental health problems as compared to persons without ASD. When these mental health problems occur in persons with sensory and intellectual disabilities, it is always recommended to assess the presence of an ASD and adjust treatment to the presence or absence of ASD.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Committee on Research Involving Human Subjects, Arnhem-Nijmegen. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
GV conducted the study, analyzed the data, and wrote the first draft of the manuscript. MV designed the study, supervised the analyses, and edited the manuscript. HK and LV supervised the study, commented on the results and conclusions, and edited the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by the ZonMw (Grant No. 60-00635-98-0081), the Royal Dutch Kentalis, and the Behavioral Science Institute, Radboud University Nijmegen. Funding sources were not involved in study design, data collection, writing of reports, or decisions regarding publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Aman, M. G., and Langworthy, K. S. (2000). Pharmacotherapy for hyperactivity in children with autism and other pervasive developmental disorders. J. Autism. Dev. Disord. 30, 451–459. doi: 10.1023/a:1005559725475
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders, DSM-5, 5th Edn. Washington, DC: American Psychiatric Publishing.
Ask Larsen, F., and Damen, S. (2014). Definitions of deafblindness and congenital deafblindness. Res. Dev. Disabil. 35, 2568–2576. doi: 10.1016/j.ridd.2014.05.029
Bloeming-Wolbrink, K. A., Janssen, M. J., de Weerth, C., Ruijssenaars, W. A., Sweep, F. C., Eijsbouts, A., et al. (2012). Stress in adults with congenital deafblindness and an intellectual disability: Information from their cortisol curves. Br. J. Vis. Impairment 30, 149–159. doi: 10.1177/0264619612456375
Boris, N. W., and Zeanah, C. H. (2005). Practice parameter for the assessment and treatment of children and adolescents with reactive attachment disorder of infancy and early childhood. J. Am. Acad. Child Adoles. Psychiatry 44, 1206–1219. doi: 10.1097/01.chi.0000177056.41655.ce
Borsboom, D., and Cramer, A. O. J. (2013). Network Analysis: an integrative approach to the structure of psychopathology. Aannu. Rev. Clin. Psychol. 9, 91–121. doi: 10.1146/annurev-clinpsy-050212-185608
Boschloo, L., van Borkulo, C. D., Rhemtulla, M., Keyes, K. M., Borsboom, D., and Schoevers, R. A. (2015). The network structure of symptoms of the diagnostic and statistical manual of mental disorders. PLoS One 10:e0137621. doi: 10.1371/journal.pone.0137621
Bringmann, L. F., Vissers, N., Wichers, M., Geschwind, N., Kuppens, P., Peeters, F., et al. (2013). A network approach to psychopathology: new insights into clinical longitudinal data. PLoS One 8:e60188. doi: 10.1371/journal.pone.0060188
Corbett, B. A., Mendoza, S., Abdullah, M., Wegelin, J. A., and Levine, S. (2006). Cortisol circadian rhythms and response to stress in children with autism. Psychoneuroendocrinology 31, 59–68. doi: 10.1016/j.psyneuen.2005.05.011
Dammeyer, J. (2011). Mental and behavioral disorders among people with congenital deafblindness. Res. Dev. Disabil. 32, 571–575. doi: 10.1016/j.ridd.2010.12.019
Dammeyer, J. (2012). Identification of congenital deafblindness. Br. J. Vis. Impair. 30, 101–107. doi: 10.1177/0264619612443882
De Bildt, A., Sytema, S., Kraijer, D., and Minderaa, R. (2005). Prevalence of pervasive developmental disorders in children and adolescents with mental retardation. J. Child Psychol. Psychiatry 46, 275–286. doi: 10.1111/j.1469-7610.2004.00346.x
De Vaan, G., Vervloed, M., Hoevenaars-van den Boom, M. A. A., Antonissen, A. C. F. M., Knoors, H., and Verhoeven, L. (2016a). A critical review of screening and diagnostic instruments for autism spectrum disorders in people with sensory impairments in addition to intellectual disabilities. J. Ment. Health Res. Intell. Disabil. 9, 36–59. doi: 10.1080/19315864.2015.1119917
De Vaan, G., Vervloed, M., Peters-Scheffer, N. C., van Gent, T., Knoors, H., and Verhoeven, L. (2016b). Behavioural assessment of autism spectrum disorders in people with multiple disabilities. J. Intellect. Disabil. Res. 60, 101–112. doi: 10.1111/jir.12206
De Vaan, G., Vervloed, M. P. J., Peters-Scheffer, N. C., Van Gent, T., Knoors, H., and Verhoeven, L. (2018). Assessing autism spectrum disorder in people with sensory impairments combined with intellectual disabilities. J. Dev. Phys. Disabil. 30, 471–487. doi: 10.1007/s10882-018-9597-x
Dickerson, S. S., and Kemeny, M. E. (2004). Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychol. Bull. 130, 355–391. doi: 10.1037/0033-2909.130.3.355
Epskamp, S., Borsboom, D., and Fried, E. I. (2018). Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res. 50, 195–212. doi: 10.3758/s13428-017-0862-1
Esbensen, A. J., Rojahn, J., Aman, M. G., and Ruedrich, S. (2003a). Anxiety, Depression and Mood Scale (ADAMS). Columbus: The Ohio State University.
Esbensen, A. J., Rojahn, J., Aman, M. G., and Ruedrich, S. (2003b). Reliability and validity of an assessment instrument for anxiety, depression, and mood among individuals with mental retardation. J. Autism. Dev. Disord. 33, 617–629. doi: 10.1023/b:jadd.0000005999.27178.55
Evenhuis, H. M., Sjoukes, L., Koot, H. M., and Kooijman, A. C. (2009). Does visual impairment lead to additional disability in adults with intellectual disabilities? J. Intell. Disabil. Res. 53, 19–28. doi: 10.1111/j.1365-2788.2008.01114.x
Fearon, R. P., Bakermans-Kranenburg, M. J., Van IJzendoorn, M. H., Lapsley, A.-M., and Roisman, G. I. (2010). The significance of insecure attachment and disorganization in the development of children’s externalizing behavior: a meta-analytic study. Child Dev. 81, 435–456. doi: 10.1111/j.1467-8624.2009.01405.x
Fried, E. I., van Borkulo, C. D., Cramer, A. O. J., Boschloo, L., Schoevers, R. A., and Borsboom, D. (2017). Mental disorders as networks of problems: a review of recent insights. Soc. Psychiatry Psychiatr. Epidemiol. 52, 1–10. doi: 10.1007/s00127-016-1319-z
Ghaziuddin, M., Ghaziuddin, N., and Greden, J. (2002). Depression in persons with autism: implications for research and clinical care. J. Autism. Dev. Disord. 32, 299–306. doi: 10.1023/a:1016330802348
Goodwin, M. S., Groden, J., Velicer, W. F., and Diller, A. (2007). Brief Report: validating the stress survey schedule for persons with autism and other developmental disabilities. Focus Autism Other Dev. Disabil. 22, 183–189. doi: 10.1177/10883576070220030501
Groden, J. (2001). The Stress Survey Schedule for Individuals with Autism and Other Pervasive Developmental Disabilities. Available online at: https://www.kmsd.edu/cms/lib/WI01919005/Centricity/Domain/257/Groden%20Stress%20Survey.pdf (accessed September 25, 2020).
Groden, J., Diller, A., Bausman, M., Velicer, W., Norman, G., and Cautela, J. (2001). The Development of a Stress Survey Schedule for Persons with Autism and Other Developmental Disabilities. J. Autism. Dev. Disord 31, 207–217. doi: 10.1023/a:1010755300436
Hermans, H., Jelluma, N., and Evenhuis, H. M. (2008). Angst, Depressie en Stemming Schaal (ADESS). Rotterdam: Erasmus MC.
Hermans, H., Jelluma, N., van der Pas, F. H., and Evenhuis, H. M. (2012). Feasibility, reliability and validity of the dutch translation of the anxiety, depression and mood scale in older adults with intellectual disabilities. Res. Dev. Disabil. 33, 315–323. doi: 10.1016/j.ridd.2011.09.018
Hoevenaars-van den Boom, M. A. A., Antonissen, A. C. F. M., Knoors, H., and Vervloed, M. P. J. (2009). Differentiating characteristics of deafblindness and autism in people with congenital deafblindness and profound intellectual disability. J. Intellect. Disabil. Res. 53, 548–558. doi: 10.1111/j.1365-2788.2009.01175.x
Hurley, A. D. (2006). Mood disorders in intellectual disability. Current Opinion in Psychiatry 19, 465–469. doi: 10.1097/01.yco.0000238471.84206.0a
Janssen, C. G. C., Schuengel, C., and Stolk, J. (2002). Understanding challenging behaviour in people with severe and profound intellectual disability: a stress-attachment model. J. Intellect. Disabil. Res. 46, 445–453. doi: 10.1046/j.1365-2788.2002.00430.x
Kraijer, D. (2004). Handboek autismespectrumstoornissen en verstandelijke beperking [handbook autism spectrum disorders and intelectual disability]. Lisse: Harcourt.
Mason, J., and Scior, K. (2004). ‘Diagnostic Overshadowing’ Amongst Clinicians Working with People with Intellectual Disabilities in the UK. J. Appl. Res. Intell. Disabil. 17, 85–90. doi: 10.1111/j.1360-2322.2004.00184.x
Poppes, P., van der Putten, A. J. J., and Vlaskamp, C. (2010). Frequency and severity of challenging behaviour in people with profound intellectual and multiple disabilities. Res. Dev. Disabil. 31, 1269–1275. doi: 10.1016/j.ridd.2010.07.017
Richer, J. (1976). The social-avoidance behaviour of autistic children. Anim. Behav. 24, 898–906. doi: 10.1016/S0003-3472(76)80020-6
Rubin, K. H., Coplan, R. J., and Bowker, J. C. (2013). Social withdrawal in childhood. Annu. Rev. Psychol. 60, 141–171. doi: 10.1146/annurev.psych.60.110707.163642
Russell, G., Mandy, W., Elliott, D., White, R., Pittwood, T., and Ford, T. (2019). Selection bias on intellectual ability in autism research: a cross-sectional review and meta-analysis. Mol. Autism 10:9. doi: 10.1186/s13229-019-0260-x
Rutgers, A. H., Bakermans-Kranenburg, M. J., van IJzendoorn, M. H., and van Berckelaer-Onnes, I. A. (2004). Autism and attachment: a meta-analytic review. J. Child Psychol. Psychiatry 45, 1123–1134. doi: 10.1111/j.1469-7610.2004.t01-1-00305.x
Rutgers, A. H., van IJzendoorn, M. H., Bakermans-Kranenburg, M. J., Swinkels, S. H. N., van Daalen, E., Dietz, C., et al. (2007). Autism, attachment and parenting: a comparison of children with autism spectrum disorder, mental retardation, language disorder, and non-clinical children. J. Abnorm. Child Psychol. 35, 859–870. doi: 10.1007/s10802-007-9139-y
Schuengel, C., and Janssen, C. G. C. (2006). People with mental retardation and psychopathology: stress, affect regulation and attachment: a review. Int. Rev. Res. Ment. Retard. 32, 229–260. doi: 10.1016/s0074-7750(06)32008-3
Sterkenburg, P. S. (2008). Intervening in Stress, Attachment and Challenging Behaviour. Effects in Children with Multiple Disabilities (Unpublished doctoral dissertation). Netherlands: Vrije Universiteit Amsterdam.
Stewart, M. E., Barnard, L., Pearson, J., Hasan, R., and O’Brien, G. (2006). Presentation of depression in autism and Asperger syndrome. Autism 10, 103–116. doi: 10.1177/1362361306062013
Stor, P., and Storsbergen, H. (2006). Onveilig Gehecht of een Hechtingsstoornis, Het Onderkennen Van Hechtingsproblematiek Bij Mensen Met Een Verstandelijke Beperking [unsecurely attached or attachment disorder, assessment of attachment problems in people with intellectual disability]. Utrecht. Netherlands: LEMMA.
van IJZendoorn, M. H., Rutgers, A. H., Bakermans-Kranenburg, M. J., Swinkels, S. H. N., Van Daalen, E., Dietz, C., et al. (2007). Parental sensitivity and attachment in children with autism spectrum disorder: comparison with children with mental retardation, with language delays, and with typical development. Child Dev. 78, 597–608. doi: 10.1111/j.1467-8624.2007.01016.x
van Splunder, J., Stilma, J. S., Bernsen, R. M. D., Arentz, T. G. M. H. J., and Evenhuis, H. M. (2003). Refractive errors and visual impairment in 900 adults with intellectual disabilities in the Netherlands. Acta Ophthalmol. Scand. 81, 123–129. doi: 10.1034/j.1600-0420.2003.00035.x
van Splunder, J., Stilma, J. S., Bernsen, R. M. D., and Evenhuis, H. M. (2006). Prevalence of visual impairment in adults with intellectual disabilities in the Netherlands: cross-sectional study. Eye 20, 1004–1010.. doi: 10.1038/sj.eye.6702059
World Health Organization [WHO] (2019). International Statistical Classification of Diseases and Related Health Problems 10th Revision. Geneva: WHO.
World Medical Association (2013). Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects.: Adopted and amended by the World Medical Association’s 64th General Assembly, Fortaleza, Brazil. Available online at: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed September 25, 2020).
Keywords: stress, mood, attachment, autism spectrum disorder, multiple disabilities, sensory impairments, deafblindness
Citation: de Vaan G, Vervloed MPJ, Knoors H and Verhoeven L (2020) Stress, Affect Regulation and Attachment of People With Sensory and Intellectual Disabilities. Front. Educ. 5:539792. doi: 10.3389/feduc.2020.539792
Received: 02 March 2020; Accepted: 16 September 2020;
Published: 22 October 2020.
Edited by:
Marleen J. Janssen, University of Groningen, NetherlandsReviewed by:
Meredith Imoguen Prain, The University of Melbourne, AustraliaAndrea Wanka, Heidelberg University of Education, Germany
Copyright © 2020 de Vaan, Vervloed, Knoors and Verhoeven. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mathijs P. J. Vervloed, bS52ZXJ2bG9lZEBwd28ucnUubmw=
 Gitta de Vaan
Gitta de Vaan Mathijs P. J. Vervloed
Mathijs P. J. Vervloed Harry Knoors
Harry Knoors Ludo Verhoeven
Ludo Verhoeven