- 1Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, Shenyang, China
- 2Department of Urology, Shengjing Hospital of China Medical University, Shenyang, China
- 3Center of Reproductive Medicine, Shengjing Hospital of China Medical University, Shenyang, China
The development of Multimodal Large Language Model (MLLMs) offers new technological support for cultivating design thinking and innovation capability in medical education. However, the current training of medical professionals remains predominantly centered on knowledge memorization and one-way didactic instruction. The systematic integration of artificial intelligence and innovation methodologies is still insufficient, while challenges such as limited interdisciplinary integration and inefficient teaching iteration have constrained the cultivation of innovative literacy. To address these challenges, this study constructs the “MLLM+EDIPT” integration framework, which deeply couples the design thinking model from Stanford University's D.school with MLLM technology. It systematically elucidates the cognitive support mechanisms of MLLM across the stages of empathy, definition, ideation, prototyping, and testing. Targeting diverse stakeholders, including hospitals, universities, educators, and students, this study proposes a phased cultivation strategy and competency framework based on school-clinician collaboration. This framework emphasizes the full integration of the “human-centered” philosophy, leveraging AI to enhance situational awareness, feedback timeliness, and methodological rigor, thereby driving the transformation of teaching models from experience-driven to intelligent collaboration. Ultimately, this research aims to provide a theoretically grounded and practically viable pathway reference for the cultivation of top-tier innovative medical talents in the AI era.
1 Background
In recent years, artificial intelligence technologies represented by deep learning and cross-modal perception have advanced rapidly, propelling Multimodal Large Language Models (MLLMs) to become pivotal vehicles for cognitive computing and intelligence augmentation (Mohammad-Rahimi et al., 2023; Stahlschmidt et al., 2022; Vakalopoulou et al., 2023; Sofia and John, 2024; Yin et al., 2024; Truhn et al., 2024; Ferber et al., 2024; AlSaad et al., 2024). Trained on massive multi-source heterogeneous data, including text, images, audio, and video, MLLM possesses ultra-large-scale parameters and cross-modal semantic understanding capabilities. It can simulate human cognitive processes that integrate visual, auditory, and linguistic information, aligning with Paivio's Dual Coding Theory, where visual and linguistic representations synergistically promote knowledge construction. Simultaneously, its dynamic reasoning mechanism embodies the core tenets of embodied cognition—cognition is not isolated symbol manipulation within the brain, but rather emerges dynamically through the coupling of perception and action during human-environment interaction (Ianı̀, 2021; Reali et al., 2024). Compared to traditional single-mode models, MLLM demonstrates significant improvements in generalization ability, contextual adaptability, and cross-modal alignment. It is progressively evolving from “instrumental assistance” toward “cognitive collaboration”, offering new technical pathways for the intelligent transformation of education based on Dual Coding Theory (Stout, 2021; Dubova et al., 2022; Elabd et al., 2025). In the medical field, MLLM has demonstrated broad potential in clinical decision support, medical education, patient interaction, and drug discovery (Yu et al., 2024; Meng et al., 2024; Lucas et al., 2024; Hobensack et al., 2024; Lu et al., 2024). Statistics indicate that over 100 healthcare-specific large models were released globally between 2022 and 2024, covering scenarios such as diagnosis, teaching, and science popularization (Lee, 2024; Gu et al., 2025; Yazdani et al., 2025; Wu et al., 2024). As MLLMs progressively replace repetitive, procedural knowledge processing tasks, the core competitiveness of future medical professionals must shift toward advanced cognitive activities—particularly the development of innovative thinking(Wang and Chow, 2023; Houssaini et al., 2024; Wiggins, 2020). Innovative thinking refers to an individual's ability to identify problems, reconstruct cognitive frameworks, and propose original solutions within complex and uncertain contexts. It represents a critical quality for addressing future healthcare challenges (Esmaeilzadeh, 2024; He et al., 2025; Mudgal et al., 2022; Bidenko et al., 2025). How to reshape the medical student training paradigm—shifting away from reliance on rote memorization and knowledge reproduction toward developing capabilities in problem discovery, cross-disciplinary integration, and prototype creation—has become a core issue in medical education reform for the new era (Fahrner et al., 2025; Gautam et al., 2024; Denecke and Gabarron, 2021).
Against this backdrop, Design Thinking—as a human-centered, iterative innovation methodology—is increasingly recognized as an effective approach for cultivating innovation capabilities (Bravo, 2023; Lorusso et al., 2021; Madson, 2021; van Velzen et al., 2024). This concept, jointly advocated and developed by IDEO and Stanford University's d.school, traces its theoretical roots to Schön's “reflective practitioner” model and Kolb's experiential learning cycle theory, emphasizing knowledge construction and meaning generation through “learning by doing” (Quilty and Murphy, 2022; Karnieli-Miller, 2020; Chen et al., 2022). Design thinking typically comprises five stages—Empathize, Define, Ideate, Prototype, and Test—forming the EDIPT model. This framework has been widely applied to solving complex social problems and service innovation practices. Research indicates that this model not only provides a structured process but also stimulates individual creative potential through immersive scenarios, empathy training, and rapid trial-and-error mechanisms, serving as a crucial bridge connecting abstract innovative thinking with concrete practical outcomes (Guo et al., 2024). However, current design thinking education remains predominantly experience-driven and reliant on human feedback, commonly suffering from excessive cognitive load, prolonged iteration cycles, and insufficient personalized guidance. While prior research has attempted to integrate AI technologies into innovation teaching processes, most efforts remain confined to text generation or single-modal information support, failing to achieve the systematic embedding and cognitive augmentation of MLLM across the entire design process (Vykhrushch et al., 2021; Alqahtani et al., 2023). This landscape reveals a critical research gap: How can the cognitive enhancement capabilities of multimodal large models be deeply integrated into the classical design thinking framework to establish a new intelligent paradigm for cultivating medical students' innovation competencies? This study aims to bridge this theoretical void by proposing an intelligent upgrade pathway based on the EDIPT model, propelling design thinking education from an “experience paradigm” to an “intelligence paradigm.” Constructing a “new paradigm” with MLLM as its technological foundation, this approach achieves cognitive expansion and innovation empowerment throughout the entire process by:—Deepening understanding of patient needs during the empathy phase through real-time perception of multimodal clinical contexts, integration of cross-domain knowledge, and generation of visual feedback;—Precisely refining core problems during the definition phase; —Stimulating interdisciplinary associations during the ideation phase;—Accelerating solution iteration and validation during the prototyping and testing phase.
In summary, this study aims to integrate the technical advantages of Multimodal Large Language Models (MLLMs) with the educational logic of the EDIPT design thinking model to construct a theoretically sound, structurally clear, and scalable intelligent framework for cultivating medical students' innovation capabilities. Specific objectives include: establishing cognitive support mechanisms for MLLMs across the stages of empathy, definition, ideation, prototyping, and testing; proposing a new paradigm for innovation capability development centered on “human-centered, intelligent collaboration”; and designing an actionable cultivation strategy system applicable to university-clinic collaborative scenarios. The theoretical significance of this research lies in expanding the connotation and boundaries of design thinking in the AI era. Its practical value manifests in providing a feasible pathway for the systematic cultivation of top-tier innovative medical talent. Its innovation primarily lies in the first systematic realization of the deep integration between MLLM and classical innovation methodologies, propelling medical education toward a paradigm shift from “experience-driven” to “intelligent collaboration.” The full text comprises six sections: Part One outlines the research background and necessity; Part Two introduces research methods and data sources; Part Three analyzes the theoretical foundation of the EDIPT model and its feasibility for integration with MLLM; Part Four proposes a phased implementation pathway and target competency framework for the “MLLM+EDIPT” integrated framework; Part Five explores teaching strategies for collaborative advancement by multiple stakeholders including hospitals, universities, faculty, and students; Part Six summarizes the study's contributions, limitations, and future research directions. Through theoretical construction and strategic design, this paper aims to provide a forward-looking and practical reference framework for medical innovation education in the AI era.
2 Research methods and data sources
To ensure scientific rigor and reproducibility, this study employed the following research methods:
2.1 Literature search and screening process
We conducted systematic searches using keyword combinations across databases, including PubMed, Web of Science, IEEE Xplore, and CNKI:
keywords: Design thinking, Medical education, Multimodal AI, Innovation Thinking, EDIPT model. The timeframe was restricted to 2020-2025, yielding 369 relevant articles. After initial screening of titles/abstracts, full-text reading, and quality assessment (using PRISMA standards), 89 high-quality articles were ultimately included, covering three major categories: theoretical research, teaching practice, and technological application.
2.2 Data analysis method
Thematic analysis was employed to categorize and extract the following four key dimensions:
(1) Current state and bottlenecks of medical students' innovation capabilities
(2) Application models of design thinking in medical education
(3) Role of AI technology in innovative teaching
(4) Competency assessment indicator systems
3 The main body and reform challenge of the cultivation of medical students' design thinking and innovation ability under the wave of multimodal large model
3.1 Helping hospital diagnosis and treatment innovation: breakthroughs and challenges in innovation
A large amount of multimodal data, including medical records, laboratory results, medical pictures, audio, and various other types of data (such as genetic data), is produced during hospital diagnosis and treatment. Consequently, extensive models whether commercial or open-source models, are perpetually simulated and trained to develop a comprehensive medical model infused with medical information. The introduction of extensive multimodal medical models like Med-PaLMM, LLaVA-Med, and XrayGPT has delivered unparalleled assistance and precision in administrative oversight, medical diagnosis and treatment, clinical management, and medical research, underscoring their significant application potential and value within the entire medical process (Li et al., 2023; Samaan et al., 2023; Tekcan Sanli et al., 2025; Ayers et al., 2023).
In terms of diagnosis and clinical nursing, the large medical model can reduce the workload of medical service providers from complex case management and routine diagnosis. More and more scientific and technological companies and hospitals are training their general large model into a large medical model that can assist clinical diagnosis and nursing. Among them, the multimodal model Med-PaLM-2, from Google Research, is designed specifically for the medical field, which is also the first AI system to exceed the passing score (>60%) in the United States Medical Licensing Examination (USMLE) (Khalpey et al., 2024). In medical research, the application of large models can greatly shorten the research and development process, process a large amount of genetic data, clinical trial design, data collection, and mining of the laws and associations behind the data in a short time, so that medical research has changed from the traditional experience-driven and small experiment mode to the data-driven and large analysis mode. In online diagnosis and treatment, the large model uses its powerful data processing ability, language understanding, and decision support ability. With deep learning and natural language processing technology, the large model can understand the symptoms described by patients, provide preliminary health assessment suggestions, assist doctors in disease analysis, and even help identify the vital signs of patients in an emergency, and guide family members and doctors in first aid.
The training of large models requires strong computing power, which demands significant financial commitment for support. For example, the computational cost of training ChatGPT-3 has exceeded hundreds of millions or billions of dollars. In practice, the majority of hospitals are unable to implement extensive medical deployment and training owing to limitations in computational capacity and financial resources; thus, the optimization of big medical models for efficiency is a critical focus for future advancements. Although we can obtain a lightweight medical model by compressing the large model through model pruning, quantification, and multiple rounds of training, the compression process is prone to large model illusion, which refers to the phenomenon that the generated output contains inaccurate or nonfactual information (Metze et al., 2024). Large model illusion is not only a technical debugging problem but also a bridge for interdisciplinary dialogue. It connects many disciplines such as computer science, medicine, ethics, etc. Owing to the sensitivity of data, stringent professionalism, elevated risk, and other attributes of the medical sector, the lightweight training of big models frequently encounters difficulties in the acquisition of high-quality training samples, particularly when addressing rare diseases or uncommon situations. The core of the challenge is the scarcity of interdisciplinary innovative talents. There is a shortage of innovative talents who are familiar with medical professional knowledge and proficient in information technology, which seriously restricts the development and application of lightweight medical models.
3.2 Promoting the upgrading of school education: educational innovation and transformation challenges
In April 2024, the National Education Digitization Strategy Action 2024 Working Points released by China's Ministry of Education explicitly proposed the implementation of a demonstration initiative for the application of AI large models in the education system and promoted the application of AI large models in relevant professional fields with higher education as the entry point. The large model facilitates precise assessment of students‘ learning behavior and teachers' teaching quality through its powerful multimodal content generation capabilities such as text, pictures, audio, and images, as well as its efficient context dialogue, logical reasoning, data calculation, and task processing capabilities, providing a scientific basis for educational decision-making, and promoting the comprehensive upgrading of campus, teaching, scientific research, and employment services.
Campus management: We will implement comprehensive and dynamic intelligent management of the campus utilizing a multimodal large model, achieving digital transformation and intelligent enhancement across various scenarios, including teacher-student governance, educational administration, intelligent oversight, support for teacher-student development, smart office operations, logistics services, campus security, and collaborative education. This initiative aims to elevate the standard of intelligent management and enhance the efficiency of educational governance, ultimately fostering efficiency, intelligence, and humanization in educational management services (Gallagher et al., 2021).
Teaching resources: The classroom can be extended to multiple times and spaces, including digital cyberspace, virtual world, and meta-universe, through intelligent education platforms and virtual teaching assistants. This expansion allows educational resources and services to reach a broader audience of educators and learners, thereby enhancing the accessibility of educational materials. Through the analysis of massive data, the large model can provide more comprehensive and enlightening knowledge content, accurately monitor and analyze each medical student's learning habits and career planning, and create an exclusive training plan (Gordon et al., 2024).
Scientific research: Generate new data, hypotheses, models, or solutions with the help of multimodal large models, predict the trend of medical research, and provide new tools and perspectives for addressing complicated challenges and investigating uncharted domains. Combined with the multimodal content generation capability of large models, complex simulation environments can be built for high-precision scientific experiments, thereby diminishing reliance on costly physical equipment and resources while simultaneously enhancing security (Mashraqi and Allehyani, 2022).
Career planning guidance: To ensure alignment between educational trajectories and societal human resource demands, the employment guidance department of colleges and universities, through the big data analysis ability of the big model, has a real-time understanding of the current social employment situation, salary, and career development trend, and timely coordinates with the teaching management department to refine professional curricula and facilitate effective career planning for college students (Godoi et al., 2024).
According to a UNESCO survey, less than 10% of the 450 schools surveyed have issued guidance on AI. Numerous medical universities still lag in the reform and innovation of the medical education system and resource integration, especially in terms of interdisciplinary vision and cooperative spirit (Yánez Benítez et al., 2023). The cultivation of cooperative innovation, empathy, and adaptability is seriously insufficient. The application cases and related knowledge of large model technology in disease prevention, diagnosis, and treatment have not been fully incorporated into the curriculum system. The extensive use of massive models in the medical domain has highlighted issues related to humanistic treatment, privacy protection, equity, and accountability.
3.3 Helping teachers' Teaching Reform: mode reform and transformation challenges
The multimodal large models, using the capabilities of diverse data types including text, images, video, and audio, have been thoroughly integrated into various aspects of education, like teaching design, teaching resource development, teaching implementation, and assessment, thereby introducing unparalleled innovations in teaching and research tools for university educators. It has not only changed the traditional teaching mode but also deepened the potential of medical research, providing students with more high-quality, efficient, and personalized educational services.
Teaching design: With the help of the large model, teachers can quickly complete the collection and analysis of multimodal data such as academic performance, learning behaviors, and emotional response, depict students‘ portraits, analyze their learning situation, and provide a strong basis for teachers to formulate personalized teaching plans. At the same time, the large models can intelligently recommend appropriate teaching objectives and diversified teaching strategies for teachers according to curriculum standards and students' learning situations (Tolentino et al., 2024).
Teaching materials: The large models can automatically generate relevant course content, including courseware, pictures, videos, and other types of teaching materials according to the teaching themes and objectives provided by teachers. Simultaneously, the large model can monitor developments in educational research and practice in real time, dynamically updating teaching cases and reference materials. This ensures that the resources available to instructors remain aligned with both disciplinary advances and evolving industry standards (Xu et al., 2024).
Classroom teaching: The large model can build diversified classroom interaction scenes such as ubiquitous learning and situational learning, act as an intelligent teaching assistant, alleviate the burden of teachers‘ answering questions, and collect students' learning state, expression, and interaction data in real-time with intelligent devices. The large model can analyze the deficiencies in the instructional process and optimize it in real-time through recognition training (Abd-Alrazaq et al., 2023).
Teaching evaluation: The teaching evaluation involves a thorough analysis of students' academic performance, classroom engagement, learning attitudes, and various multimodal factors. The extensive model assesses the effectiveness of teaching, produces a visual evaluation report, and graphically represents the strengths and weaknesses of the instructional process. Teachers can contemplate the instructional process, adjust teaching strategies, and continuously improve the teaching quality based on these evaluation results (Guo et al., 2021).
With the in-depth application of multimodal large models and related technologies in the field of medical education, the lack of dual-qualified teachers with both medical knowledge and experience in the development and application of large-scale models has become increasingly prominent. Certain educators struggle to swiftly adjust to the creative pedagogical approaches introduced by large-scale models, lack the corresponding innovative teaching ability, and find it challenging to address the diverse learning needs of students.
3.4 Promoting students' learning and upgrading: knowledge explosion and Innovation Challenge
Contemporary medical students grow up in an era of vigorous development of high technology and deep penetration of the Internet and social media, and are highly sensitive to emerging technologies. The multimodal large model accurately generates multiple resources, including text, images, audio and video derived from knowledge learning, social experiences, and the accumulation of clinical practice, ultimately facilitating the comprehensive development of medical students through career guidance.
Knowledge learning: Multimodal large models can intelligently recommend suitable learning resources, including online courses and practice question banks, by analyzing the learning habits, capabilities, and interests of medical students, thereby enhancing the precision and efficiency of the learning process. Multimodal large models can also continuously track and provide the latest medical research reports and results, ensuring the timeliness and competitiveness of medical students' knowledge (Zhang et al., 2025).
Social life: Multimodal large models provide medical students with richer and more diverse social experiences, such as virtual reality socializing and online games, by creating virtual characters and scenes. By intelligently analyzing the interests and preferences of medical students, we propose appropriate entertainment content, including music, movies, and literature (Alonso-Bastarreche and Vargas, 2021).
Clinical practice: Multimodal large models provide personalized learning paths by assisting in the design and simulation of patient diagnosis and treatment cases, assisting medical students in understanding complex medical theories, and closely integrating theoretical knowledge with practical clinical scenarios. Enable medical students to practice diagnosis and develop treatment plans within a secure environment, improve their practical skills, and enhance their communication and teamwork skills with patients (Liu et al., 2023).
Career guidance: The multimodal large models, through deep learning and multimodal data analysis, can predict employment prospects in different medical majors, assist medical students in optimizing their resumes and simulating interviews, and improve job success rates. Currently, multimodal large models have given rise to a series of emerging professions, such as medical language engineers and medical AI engineers, hence providing more employment opportunities and development space for medical students (Chen et al., 2025).
The growing utilization of large models by medical students is amplifying concerns regarding academic honesty among certain individuals in the field. Driven by a lazy mentality, attempts to use artificial intelligence to cheat, plagiarize papers, and do homework on behalf of others have been repeatedly banned, and medical students' ability for independent thought and exploring innovation has gradually deteriorated due to their lack of consideration for big models. Therefore, the cultivation of innovative thinking, complex problem-solving abilities, human-machine collaboration, self-regulated learning, and other abilities for medical students is becoming increasingly important.
4 A new paradigm for design thinking EDIPT modeling in the context of multimodal models
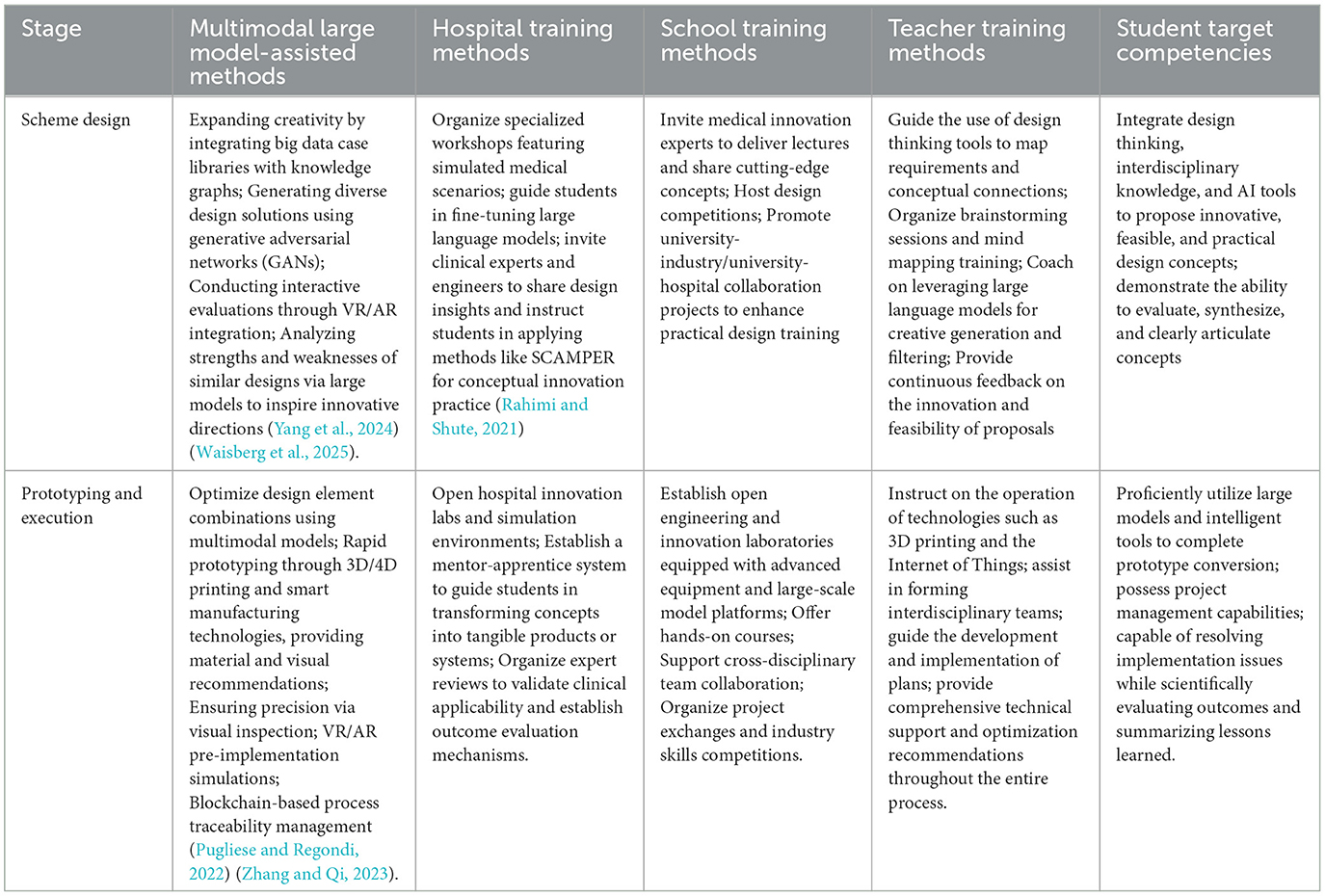
Verganti et al. asserted that design thinking is a paradigm, methodology, process, or cognitive framework that is future-oriented, user-centric, and innovatively solves problems. The objective is to devise innovative solutions for current or prospective issues, with a focus on user needs and process efficiency. The EDIPT approach is derived from the results of the development of the design innovation course at Stanford D.school, which delineated the design thinking process into five phases: Empathy, Define, Ideate, Prototype, and Test. Brown and Katz emphasize that design thinking is a people-oriented design philosophy and methodology, prioritizing human needs and behaviors, emphasizing team collaboration, and promoting innovation (Triplett et al., 2024). Utilizing techniques such as empathetic insight, prototype iteration, and testing optimization, corresponding development tools are employed to pursue systematic innovation methods that pursue innovative problem-solving through structured processes. Concurrently, with the increasingly powerful and widely used functions of multimodal large models, the EDIPT design thinking model has also ushered in a new opportunity to integrate with multimodal large models. The significant benefits empowering value of multimodal large models in various aspects of the model, such as understanding needs, stimulating creativity, and testing and verification, are becoming increasingly prominent. It injects new intelligent power into the EDIPT design thinking model, opens up a new paradigm of human-machine collaboration, and greatly improves the efficiency of cultivating innovation among medical students (Table 1).
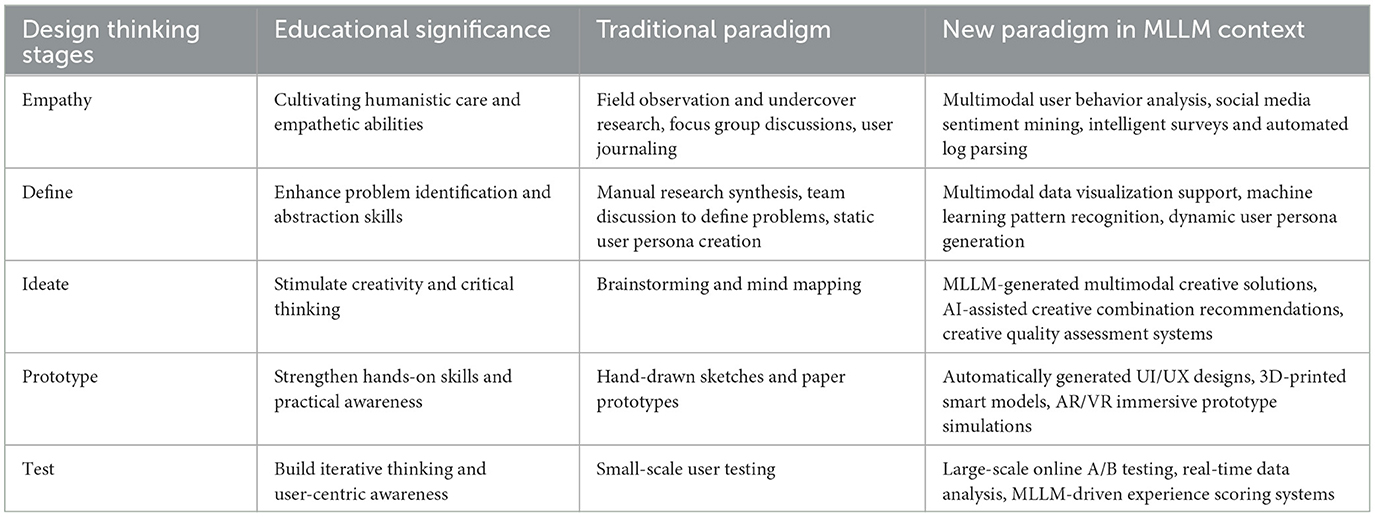
Table 1. Differences between traditional paradigm and multimodal large models at the design thinking stage.
4.1 Empathy integration
The initial phase of the EDIPT design thinking model is “Empathize”, highlighting the importance of understanding the genuine requirements of users, which coincides with the spirit of humanistic care that medical students need to master during the innovation process (Buchheit and Allen, 2022). With the advancement of medical technology, medical students need to focus on utilizing these innovations to improve the quality of life of patients, rather than just treating physical ailments. By understanding the psychological and physical requirements of patients, medical students can design innovative treatment regimens that are more relevant and practical.
4.2 Problem-oriented
The EDIPT design thinking model emphasizes the process of the “Define” and “imagining”, which involve elucidating specific problems and engaging in diverse creative thinking. In the era of AI large models, medical students will encounter many challenges, such as unfamiliar experimental design, massive data processing, large-scale disease management, and the realization of personalized treatment. Medical students need to use brainstorming, user portraits, participation in design, and other methodologies to innovate and conceive corresponding solutions from multiple dimensions and perspectives, utilizing AI large model platforms such as ALphaFold and RoseTTAFold (Abramson et al., 2024; Krishna et al., 2024).
4.3 Practice and iteration
During the “Prototype” and “Test” phases, the EDIPT design thinking model emphasizes “Learning by Doing” and encourages swift practice and iterative improvement (Annan et al., 2023). In the age of large models, medical problems are complex and changeable. Innovation in the medical field also needs to explore optimal solutions through rapid design and repeated experiments. This iterative process enables medical students to accumulate experience through trial and error, improve problem-solving skills, and accelerate the innovative research and development of personalized treatment schemes, drugs, or devices.
4.4 Interdisciplinary cooperation
The EDIPT design thinking model advocates interdisciplinary teams collaborating closely to transcend the constrains of individual specializations, using tools such as brainstorming and participatory design to stimulate more innovative sparks. Medical innovation in the era of AI large models frequently arises from interdisciplinary integration, involving knowledge and skills in biotechnology, information technology, artificial intelligence, ethics, and other fields (Huber, 2022).
4.5 Continuous learning
The EDIPT design thinking model emphasizes openness and adaptability. The rapid development of technology in the era of AI large models renders lifelong learning essential. In the process of innovation, medical students need to constantly absorb new knowledge and skills. The capacity for continual learning is crucial for monitoring the latest medical progress and implementing innovation in practice (Olasoji, 2016).
5 Cultivation of medical students' design thinking based on the new paradigm of design thinking edit model
With the rapid advancement of artificial intelligence technology, hospitals, universities, educators, and medical students must collaborate to address emerging challenges. In the context of multimodal large model, and drawing on both classical design thinking process and new paradigm, all stakeholders should actively engage in various stages of the EDIPT model to comprehensively cultivate design thinking of medical students in an all-around way, to forge the innovative thinking of medical students. This approach seeks to cultivate innovative thinking, stimulate creativity, and equip medical students with the skills needed to thrive in the face of future societal challenges.
5.1 Cultivation of medical students' design thinking in the empathy stage
Medical students are assigned to hospitals or community service centers through the school-doctor collaboration to engage with the medical needs of diverse populations (Ong et al., 2024). Medical students are encouraged to engage in discussions of clinical cases, articulate personal reflections and emotional responses, and facilitate debates on controversial medical issues. This approach aims to foster a multifaceted understanding of diverse perspectives.
Integrate the concept of empathy into compulsory educational curricula, including social studies, literature, and ethics education. Utilize VR and AR devices to create immersive scenarios that enable medical students to confront the emotional dilemmas inherent in medical decision-making. This approach fosters empathy, teaches the balance between innovation and ethical standards, and instills a respect for the value of life through pre-programmed emotional and discursive scripts.
Educators ought to establish role models and foster emotional connections with medical students through effective communication, active listening, and compassion. They should refine teaching objectives, content, and task analysis, while prioritizing empathy in the learning environment. Additionally, creating a multicultural educational setting and promoting engagement in public welfare activities will enhance students' social awareness and empathy (Martinsone and ŽydŽiunaite, 2023).
Students require training in trans-personal thinking to comprehend the emotions and needs of others across various contexts. This training aims to improve their capacity for divergent thinking and to enrich their empathetic experiences through storytelling, role-playing, and group discussions. Additionally, employing multimodal large model tools for the analysis of expressive observation, body language, and intonation is essential (Lin et al., 2024).
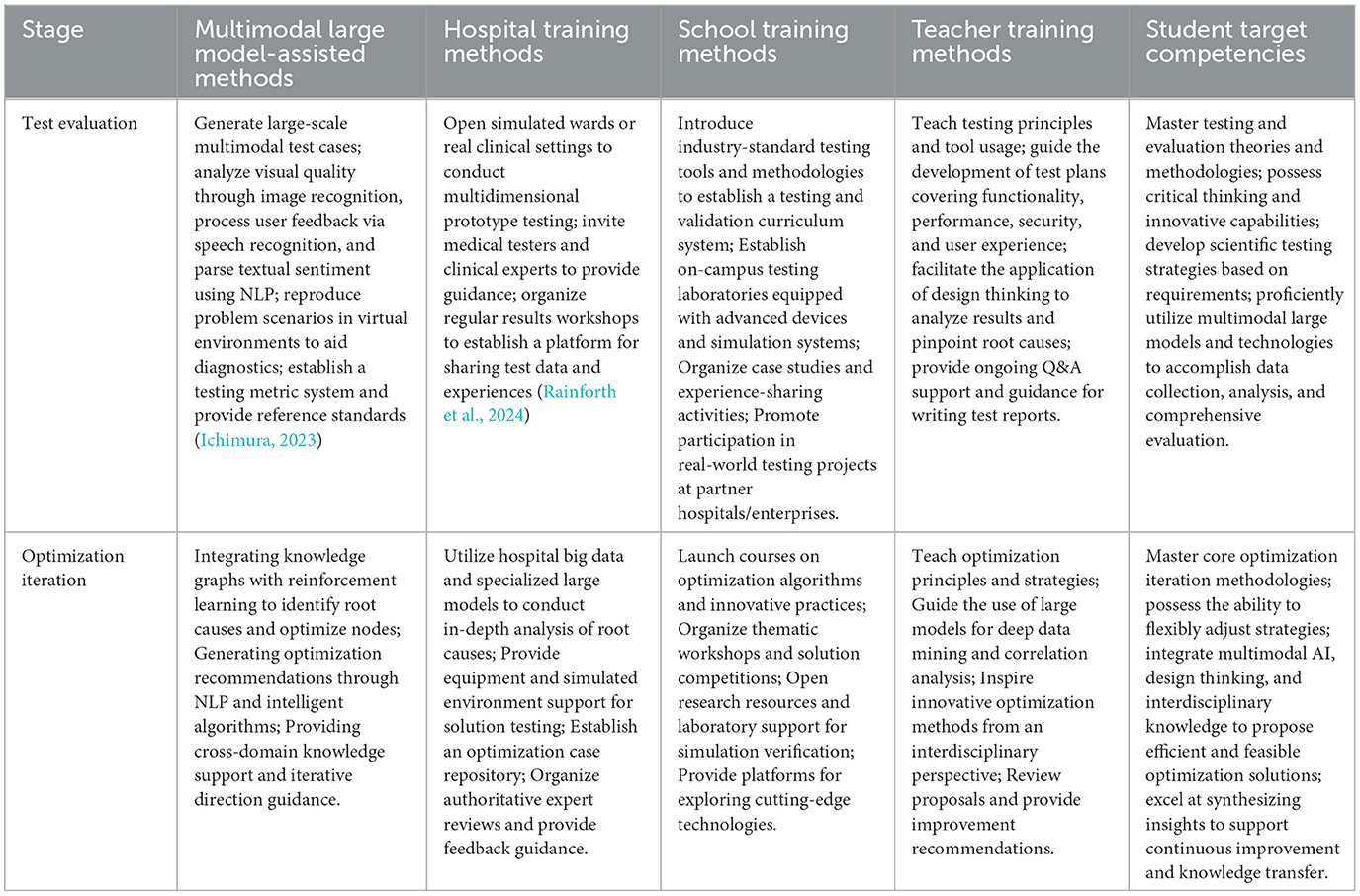
5.2 Cultivation of medical students' design thinking in the define and ideate stage
The definition and conception of needs/problems is the key starting point for the implementation of design thinking. The traditional methods of definition and conception of needs/problems mainly rely on small-scale patient interviews and field research, which can only obtain one-sided user feedback. With the advent of artificial intelligence, multimodal large model technology is fundamentally transforming how medical students understand and address the needs of various stakeholders. From the collection and analysis of massive data to the generation of profound insight, the multimodal large model has injected unprecedented power into the design thinking of medical students. Although the multimodal large model is powerful, it often lacks empathy and humanistic insight and is prone to hallucinations (Li and Wu, 2025). Based on the new paradigm of design thinking, this paper takes empathy and humanistic care as the core and a multimodal large model as the support platform to build a systematic training path from the four-dimensional relationship of hospital school teacher-student, to stimulate innovative ideas, enrich the conception dimension, improve the scientificity and innovation of demand/problem definition and conception, use human emotional wisdom to control model analysis, and capture the temperature of human nature in the cold data (Table 2).
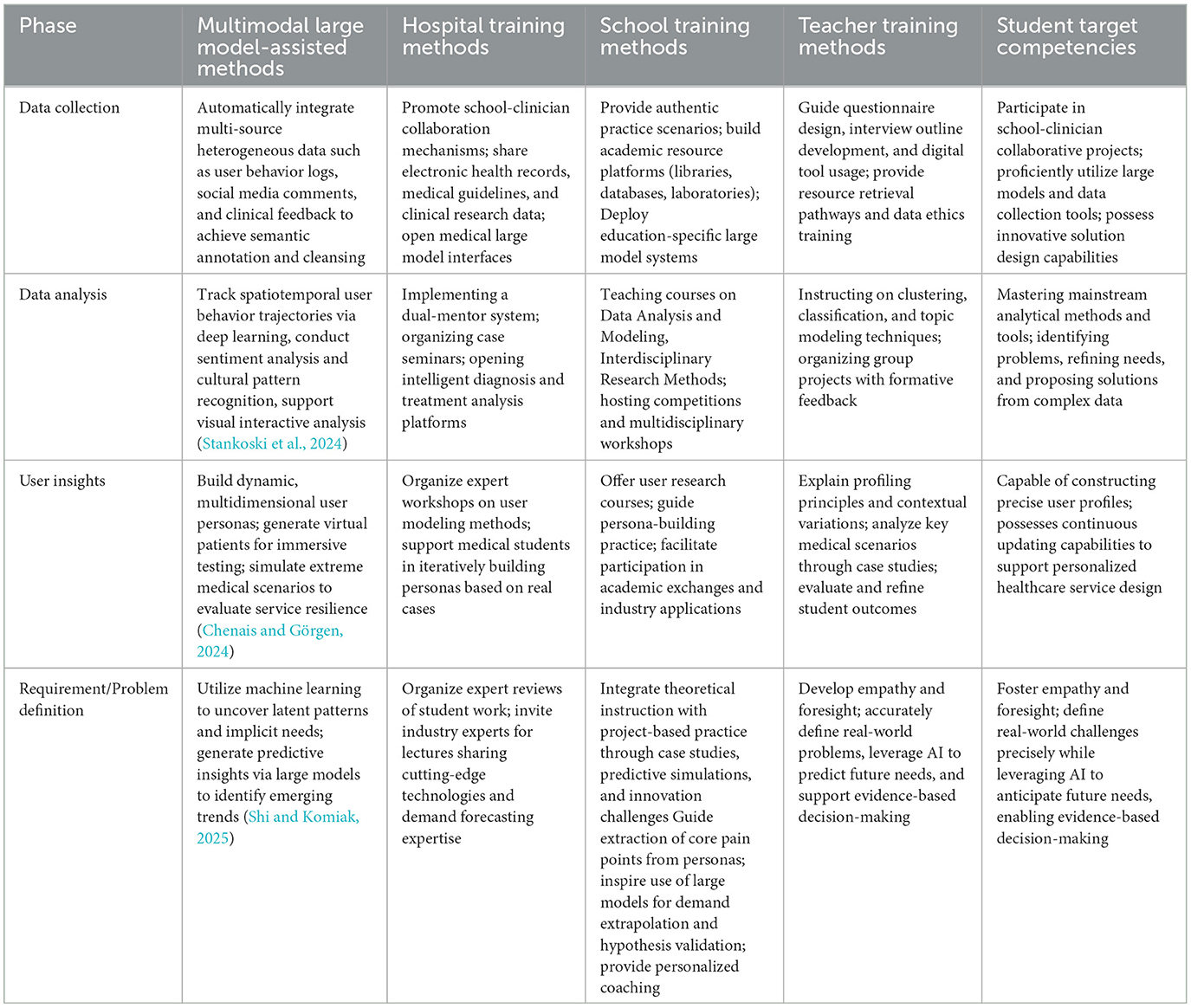
Table 2. Methods and objectives of cultivation of each subject in the definition and conceptualization phase.
5.3 Training of medical students' design thinking in the prototype stage
Prototype production is the core link of design thinking and the stage for medical students to show their talents. Multimodal large-scale model technology is injecting new vitality into this process. Multimodal large-scale model realizes the batch and personalized generation of creative resources and can automatically recommend and generate relevant creative elements based on a vast database, which greatly expands the boundary of medical students' creativity (Shah, 2024). However, with the in-depth application of multimodal and multimodal models, problems such as the homogenization tendency of generated content and the lack of fit with the real environment have become increasingly apparent (Kilintzis et al., 2024). Hospitals, schools, and teachers, as key players in fostering innovative thinking, should always be vigilant to supplement their shortcomings. Simultaneously, they should prioritize empathy and use design thinking as a foundation to enhance their innovation, enabling medical students to cultivate their strengths, overcome their weaknesses in human-computer collaboration, and appreciate the beauty of intelligence with a craftsman's mindset (Table 3).
5.4 Training of medical students' design thinking in the test stage
Test evaluation and optimization iteration is the core hub of design thinking from theory to practice, which has a decisive impact on the effectiveness and adaptability of the solution. Traditional methods mainly rely on small-scale user testing and subjective judgment, which makes it difficult to deal with complex and changeable user needs and dynamic problem scenarios, and restricts the practical effect of design thinking. With the breakthrough development of multimodal large model technology, test evaluation, and optimization iteration are undergoing fundamental changes (Chao et al., 2025; Gan et al., 2024) (Table 4). This technological innovation provides strong intelligent support for design thinking, which not only significantly improves the coverage and accuracy of test and evaluation, but also realizes the intellectualization and systematization of optimization iteration. Especially in the field of medical education, this change has provided unprecedented practical tools for medical students, greatly enhanced the ability of design thinking to solve complex problems and develop innovative solutions, and made it more efficient and accurate in dealing with practical challenges.
6 Conclusion
This study presents an integrated framework combining the “Multimodal Large Language Model (MLLM)” with the EDIPT Design Thinking Model, proposing a new intelligent paradigm for fostering innovation in medical education. Research has shown that MLLM not only serves as an information-generation tool but also offers cross-modal perceptual support, real-time feedback, and cognitive enhancement throughout the stages of empathy, definition, ideation, prototyping, and testing (Kang et al., 2024). This significantly improves the scientific rigor, efficiency, and personalization of design thinking instruction. Compared to traditional experience-driven teaching models, this approach facilitates a shift from the “experience paradigm” to an “intelligent paradigm,” effectively addressing issues such as high cognitive load, lengthy iteration cycles, and resource disparities. Unlike previous studies that limited AI to text generation or single-task assistance (e.g., Al-Johany et al., 2023; Reali et al., 2024), this study overcomes the limitations of “tool-based” applications by embedding MLLM as a cognitive collaborator throughout the EDIPT process. It highlights the dynamic coupling of multimodal inputs-such as clinical images, patient voices and electronic medical records- with contextual outputs, expanding MLLM's role in developing of higher-order thinking. The findings support and extend the applicability of Schön's “reflective practice” and Kolb's “experiential practice” theories in intelligent environments, validating the cognitive enhancement effects of technology-enabled “learning by doing” models. This provides new theoretical foundations and practical pathways for the deep integration of AI into medical innovation education. The main innovations of this study are threefold: First, it introduces the “MLLM+EDIPT” integrated framework, creating an intelligent pathway for medical innovation education; Second, it establishes the core concept of “human-machine co-intelligence,” redefining medical students' irreplaceable value in the AI era; Third, it develops a replicable and scalable university-clinic collaborative training strategy system, driving a fundamental shift in educational objectives from knowledge transmission to innovation capability development. The theoretical contribution of this study lies in bridging gap between multimodal large models and classical innovation methodologies, while its practical value provides medical schools with an actionable framework for designing AI-integrated curricula and building collaborative education mechanisms. However, this study has some limitations: First, it remains in the theoretical development and small-scale pilot stage, and its long-term effects require further large-scale empirical validation. Second, risks related to medical data privacy, algorithmic bias, and ethical compliance need additional assessment. Third, disparities in digital literacy between faculty and students may impact the successful implementation of this paradigm, necessitating improved faculty training and technical support systems. Future research should focus on three areas: First, conducting longitudinal studies to quantify MLLM's dynamic impact on various dimensions of innovative thinking; Second, exploring lightweight local deployment options to enhance security and accessibility; Third, establishing ethical guidelines for human-machine collaboration to ensure that technology serves the “student-centered” nature of education.
In summary, this study offers new theoretical perspectives and practical pathways for cultivating top-tier innovative medical talent in the era of artificial intelligence, propelling medical education toward a new phase of high-quality development characterized by “human-machine co-intelligence and innovation-driven learning.”
Author contributions
JL: Writing – review & editing, Writing – original draft. QL: Writing – original draft, Methodology. WX: Writing – review & editing, Project administration. LM: Writing – review & editing, Funding acquisition. YZ: Supervision, Writing – review & editing, Visualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the 2024 China Medical University Undergraduate Teaching Reform Research Project (YDJG20240055, LBM).
Acknowledgments
The authors are grateful for the opportunity to conduct this study and write this paper, and the authors appreciate the kind support and encouragement received from the academic and research community.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abd-Alrazaq, A., AlSaad, R., Alhuwail, D., Ahmed, A., Healy, P. M., Latifi, S., et al. (2023). Large language models in medical education: opportunities, challenges, and future directions. JMIR Med. Educ. 9:e48291. doi: 10.2196/48291
Abramson, J., Adler, J., Dunger, J., Evans, R., Green, T., Pritzel, A., et al. (2024). Accurate structure prediction of biomolecular interactions with AlphaFold 3. Nature 630, 493–500. doi: 10.1038/s41586-024-07487-w
Al-Johany, N. A., Eassa, F. E., Sharaf, S. A., Noaman, A. Y., and Ahmed, A. (2023). Prediction and correction of software defects in message-passing interfaces using a static analysis tool and machine learning. IEEE Access 11, 60668–60680. doi: 10.1109/ACCESS.2023.3285598
Alonso-Bastarreche, G., and Vargas, A. I. (2021). Gift game metatheory: social interaction and interpersonal growth. Front. Psychol. 12:687617. doi: 10.3389/fpsyg.2021.687617
Alqahtani, T., Badreldin, H. A., Alrashed, M., Alshaya, A. I., Alghamdi, S. S., Bin Saleh, K., et al. (2023). The emergent role of artificial intelligence, natural learning processing, and large language models in higher education and research. Res. Social Adm. Pharm. 19, 1236–1242. doi: 10.1016/j.sapharm.2023.05.016
AlSaad, R., Abd-Alrazaq, A., Boughorbel, S., Ahmed, A., Renault, M. A., Damseh, R., et al. (2024). Multimodal large language models in health care: applications, challenges, and future outlook. J. Med. Internet Res. 26:e59505. doi: 10.2196/59505
Annan, H. G., Do, V., and MacLeod, A. (2023). Learning by doing: a phenomenological study of medical student leaders. Med. Educ. 57, 753–760. doi: 10.1111/medu.15025
Ayers, J. W., Poliak, A., Dredze, M., Leas, E. C., Zhu, Z., Kelley, J. B., et al. (2023). Comparing physician and artificial intelligence chatbot responses to patient questions posted to a public social media forum. JAMA Intern. Med. 183, 589–596. doi: 10.1001/jamainternmed.2023.1838
Bidenko, N. V., Stuchynska, N. V., Palamarchuk, Y. V., and Matviienko, M. M. (2025). Integrating artificial intelligence in healthcare practice: challenges and future prospects. Wiad. Lek. 78, 1199–1205. doi: 10.36740/WLek/205397
Bravo, K. (2023). Design thinking in nursing education and health sciences education. Nurs. Educ. Perspect. 44, 164–168. doi: 10.1097/01.NEP.0000000000001055
Buchheit, M., and Allen, S. V. (2022). To Optimize? First, empathize. Int. J. Sports Physiol. Perform. 17, 505–506. doi: 10.1123/ijspp.2022-0036
Chao, C. Y., Lin, T. K., Hung, N. Y., Hsu, C. L., and Kao, L. T. (2025). Advancing pharmacy students' communication skills through real-time feedback in innovative simulations. Am. J. Pharm. Educ. 89:101414. doi: 10.1016/j.ajpe.2025.101414
Chen, H., Van Reyk, D., and Oliver, B. G. (2025). The use of AI large language models by university students for assignment preparation. Adv. Physiol. Educ. 49, 517–525. doi: 10.1152/advan.00181.2024
Chen, L., Jiang, W. J., and Zhao, R. P. (2022). Application effect of Kolb's experiential learning theory in clinical nursing teaching of traditional Chinese medicine. Digit. Health 8:20552076221138313. doi: 10.1177/20552076221138313
Chenais, N., and Görgen, A. (2024). Immersive interfaces for clinical applications: current status and future perspective. Front. Neurorobot. 18:1362444. doi: 10.3389/fnbot.2024.1362444
Denecke, K., and Gabarron, E. (2021). How artificial intelligence for healthcare look like in the future? Stud. Health Technol. Inform. 281, 860–864. doi: 10.3233/SHTI210301
Dubova, M., Galesic, M., and Goldstone, R. L. (2022). Cognitive science of augmented intelligence. Cogn. Sci. 46:e13229. doi: 10.1111/cogs.13229
Elabd, N., Rahman, Z. M., Abu Alinnin, S. I., Jahan, S., Campos, L. A., and Baltatu, O. C. (2025). Designing personalized multimodal mnemonics with AI: a medical student's implementation tutorial. JMIR Med. Educ. 11:e67926. doi: 10.2196/67926
Esmaeilzadeh, P. (2024). Challenges and strategies for wide-scale artificial intelligence (AI) deployment in healthcare practices: a perspective for healthcare organizations. Artif. Intell. Med. 151:102861. doi: 10.1016/j.artmed.2024.102861
Fahrner, L. J., Chen, E., Topol, E., and Rajpurkar, P. (2025). The generative era of medical AI. Cell 188, 3648–3660. doi: 10.1016/j.cell.2025.05.018
Ferber, D., Wölflein, G., Wiest, I. C., Ligero, M., Sainath, S., Ghaffari Laleh, N., et al. (2024). In-context learning enables multimodal large language models to classify cancer pathology images. Nat. Commun. 15:10104. doi: 10.1038/s41467-024-51465-9
Gallagher, S., Gladman, T., Macfarlane, E., Hallman, S., Hutton, J., and Paterson, H. (2021). Student use of common online resources in a multi-campus medical school. MedEdPublish. 10:56. doi: 10.15694/mep.2021.000056.1
Gan, W., Ouyang, J., Li, H., Xue, Z., Zhang, Y., Dong, Q., et al. (2024). Integrating ChatGPT in orthopedic education for medical undergraduates: randomized controlled trial. J. Med. Intern. Res. 26:e57037. doi: 10.2196/57037
Gautam, A., Sakthivel, J., and Rahman, F. A. (2024). Impact of international medical graduates on the UK healthcare system: current contributions and future challenges. Kathmandu Univ. Med. J. 22, 112–116.
Godoi, A., Casteleyn, C., Virk, F., McDade-Kumar, M., Byrne, M. H. V., Moussa, A., et al. (2024). Construction and validation of a medical career readiness inventory. Clin. Teach. 21:e13733. doi: 10.1111/tct.13733
Gordon, M., Daniel, M., Ajiboye, A., Uraiby, H., Xu, N. Y., Bartlett, R., et al. (2024). A scoping review of artificial intelligence in medical education: BEME guide No. 84. Med. Teach. 46, 446-470. doi: 10.1080/0142159X.2024.2314198
Gu, Z., Chen, J., Liu, F., Yin, C., and Zhang, P. (2025). MedVH: toward systematic evaluation of hallucination for large vision language models in the medical context. Adv. Intell. Syst. 10:1002. doi: 10.1002/aisy.202500255
Guo, J., Bai, L., Yu, Z., Zhao, Z., and Wan, B. (2021). An AI-application-oriented in-class teaching evaluation model by using statistical modeling and ensemble learning. Sensors 21:s21010241. doi: 10.3390/s21010241
Guo, Y., Wang, X., Gao, Y., Yin, H., Ma, Q., and Chen, T. (2024). Flipped online teaching of histology and embryology with design thinking: design, practice and reflection. BMC Med. Educ. 24:388. doi: 10.1186/s12909-024-05373-7
He, Y., Huang, F., Jiang, X., Nie, Y., Wang, M., Wang, J., et al. (2025). Foundation model for advancing healthcare: challenges, opportunities and future directions. IEEE Rev. Biomed. Eng. 18, 172–191. doi: 10.1109/RBME.2024.3496744
Hobensack, M., von Gerich, H., Vyas, P., Withall, J., Peltonen, L. M., Block, L. J., et al. (2024). A rapid review on current and potential uses of large language models in nursing. Int. J. Nurs. Stud. 154:104753. doi: 10.1016/j.ijnurstu.2024.104753
Houssaini, M. S., Aboutajeddine, A., and Toughrai, I. (2024). Development of a data-centric design thinking process for innovative care delivery. Herd 17, 146–165. doi: 10.1177/19375867231215071
Huber, C. (2022). Interprofessional Collaboration in Health Care. Praxis (Bern 1994) 110, 3–4. doi: 10.1024/1661-8157/a003808
Ianì, F. (2021). Embodied cognition: so flexible as to be “disembodied”? Conscious. Cogn. 88:103075. doi: 10.1016/j.concog.2021.103075
Ichimura, K. (2023). Effects of virtual reality's viewing medium and the environment's spatial openness on divergent thinking. PLoS ONE 18:e0283632. doi: 10.1371/journal.pone.0283632
Kang, K., Yang, Y., Wu, Y., and Luo, R. (2024). Integrating large language models in bioinformatics education for medical students: opportunities and challenges. Ann. Biomed. Eng. 52, 2311–2315. doi: 10.1007/s10439-024-03554-5
Karnieli-Miller, O. (2020). Reflective practice in the teaching of communication skills. Patient Educ. Couns. 103, 2166–2172. doi: 10.1016/j.pec.2020.06.021
Khalpey, Z., Kumar, U., King, N., Abraham, A., and Khalpey, A. H. (2024). Large language models take on cardiothoracic surgery: a comparative analysis of the performance of four models on American board of thoracic surgery exam questions in 2023. Cureus 16:e65083. doi: 10.7759/cureus.65083
Kilintzis, V., Kalokyri, V., Kondylakis, H., Joshi, S., Nikiforaki, K., Díaz, O., et al. (2024). Public data homogenization for AI model development in breast cancer. Eur. Radiol. Exp. 8:42. doi: 10.1186/s41747-024-00442-4
Krishna, R., Wang, J., Ahern, W., Sturmfels, P., Venkatesh, P., Kalvet, I., et al. (2024). Generalized biomolecular modeling and design with RoseTTAFold All-Atom. Science 384:eadl2528. doi: 10.1126/science.adl2528
Lee, H. (2024). The rise of ChatGPT: exploring its potential in medical education. Anat. Sci. Educ. 17, 926–931. doi: 10.1002/ase.2270
Li, H., Moon, J. T., Purkayastha, S., Celi, L. A., Trivedi, H., and Gichoya, J. W. (2023). Ethics of large language models in medicine and medical research. Lancet Digit. Health 5, e333–e335. doi: 10.1016/S2589-7500(23)00083-3
Li, R., and Wu, T. (2025). Delving into the practical applications and pitfalls of large language models in medical education: narrative review. Adv. Med. Educ. Pract. 16, 625–636. doi: 10.2147/AMEP.S497020
Lin, H. L., Wang, Y. C., Huang, M. L., Yu, N. W., Tang, I., Hsu, Y. C., et al. (2024). Can virtual reality technology be used for empathy education in medical students: a randomized case-control study. BMC Med. Educ. 24:1254. doi: 10.1186/s12909-024-06009-6
Liu, J., Wang, C., and Liu, S. (2023). Utility of ChatGPT in clinical practice. J. Med. Internet Res. 25:e48568. doi: 10.2196/48568
Lorusso, L., Lee, J. H., and Worden, E. A. (2021). Design thinking for healthcare: transliterating the creative problem-solving method into architectural practice. Herd 14, 16–29. doi: 10.1177/1937586721994228
Lu, Z., Peng, Y., Cohen, T., Ghassemi, M., Weng, C., and Tian, S. (2024). Large language models in biomedicine and health: current research landscape and future directions. J. Am. Med. Inform. Assoc. 31, 1801–1811. doi: 10.1093/jamia/ocae202
Lucas, H. C., Upperman, J. S., and Robinson, J. R. (2024). A systematic review of large language models and their implications in medical education. Med. Educ. 58, 1276–1285. doi: 10.1111/medu.15402
Madson, M. J. (2021). Making sense of design thinking: a primer for medical teachers. Med. Teach. 43, 1115–1121. doi: 10.1080/0142159X.2021.1874327
Martinsone, B., and ŽydŽiunaite, V. (2023). Teachers' contributions to the school climate and using empathy at work: implications from qualitative research in two European countries. Front. Psychol. 14:1160546. doi: 10.3389/fpsyg.2023.1160546
Mashraqi, A. M., and Allehyani, B. (2022). Current trends on the application of artificial intelligence in medical sciences. Bioinformation 18, 1050–1061. doi: 10.6026/973206300181050
Meng, X., Yan, X., Zhang, K., Liu, D., Cui, X., Yang, Y., et al. (2024). The application of large language models in medicine: a scoping review. iScience 27:109713. doi: 10.1016/j.isci.2024.109713
Metze, K., Morandin-Reis, R. C., Lorand-Metze, I., and Florindo, J. B. (2024). Bibliographic research with large language model ChatGPT-4: instability, hallucinations and sometimes alerts. Clinics 79:100409. doi: 10.1016/j.clinsp.2024.100409
Mohammad-Rahimi, H., Rokhshad, R., Bencharit, S., Krois, J., and Schwendicke, F. (2023). Deep learning: a primer for dentists and dental researchers. J. Dent. 130:104430. doi: 10.1016/j.jdent.2023.104430
Mudgal, S. K., Agarwal, R., Chaturvedi, J., Gaur, R., and Ranjan, N. (2022). Real-world application, challenges and implication of artificial intelligence in healthcare: an essay. Pan. Afr. Med. J. 43:3. doi: 10.11604/pamj.2022.43.3.33384
Olasoji, H. O. (2016). Feedback after continuous assessment: an essential element of students' learning in medical education. Niger. J. Clin. Pract. 19, 692–694. doi: 10.4103/1119-3077.188696
Ong, C. Y., Lai, J., Lee, D. W. C., and Lee, J. M. H. (2024). Bridging hospital and nursing home: collaboration for smoother transitions and reduced hospitalizations. J. Am. Med. Dir. Assoc. 25:104924. doi: 10.1016/j.jamda.2023.12.012
Pugliese, R., and Regondi, S. (2022). Artificial intelligence-empowered 3D and 4D printing technologies toward smarter biomedical materials and approaches. Polymers 14:14142794. doi: 10.3390/polym14142794
Quilty, T., and Murphy, L. (2022). Time to review reflective practice? Int. J. Qual. Health Care 34:052. doi: 10.1093/intqhc/mzac052
Rahimi, S., and Shute, V. J. (2021). First inspire, then instruct to improve students' creativity. Comput. Educ. 174:104312. doi: 10.1016/j.compedu.2021.104312
Rainforth, C., John, A., and Brown, A. (2024). Augmented reality in ward round-based simulation: exploring student experiences and impact on confidence. Cureus 16:e73847. doi: 10.7759/cureus.73847
Reali, F., Cevasco, J., and Marmolejo-Ramos, F. (2024). Some contributions from embodied cognition to psychonarratology. J. Psycholinguist. Res. 53:74. doi: 10.1007/s10936-024-10110-8
Samaan, J. S., Yeo, Y. H., Rajeev, N., Hawley, L., Abel, S., Ng, W. H., et al. (2023). Assessing the accuracy of responses by the language model ChatGPT to questions regarding bariatric surgery. Obes. Surg. 33, 1790–1796. doi: 10.1007/s11695-023-06603-5
Shah, M. H. (2024). Expanding boundaries: the synergy of creative writing and reflective learning in medicine. Med. Teach. 46, 426–427. doi: 10.1080/0142159X.2023.2239454
Shi, Y. V., and Komiak, S. (2025). Unveiling patient-centric interactions in virtual consultation: a comprehensive text mining approach. Health Inform. J. 31:14604582251327093. doi: 10.1177/14604582251327093
Sofia, R. C., and John, S. (2024). “AI-driven service and slice orchestration,” in Shaping the Future of IoT with Edge Intelligence: How Edge Computing Enables the Next Generation of IoT Applications, eds. R. C., Sofia, S. John (Abingdon, UK: River Publishers), 15–36.
Stahlschmidt, S. R., Ulfenborg, B., and Synnergren, J. (2022). Multimodal deep learning for biomedical data fusion: a review. Brief. Bioinform. 23:569. doi: 10.1093/bib/bbab569
Stankoski, S., Kiprijanovska, I., Gjoreski, M., Panchevski, F., Sazdov, B., Sofronievski, B., et al. (2024). Controlled and real-life investigation of optical tracking sensors in smart glasses for monitoring eating behavior using deep learning: cross-sectional study. JMIR Mhealth Uhealth 12:e59469. doi: 10.2196/59469
Stout, D. (2021). The cognitive science of technology. Trends Cogn. Sci. 25, 964–977. doi: 10.1016/j.tics.2021.07.005
Tekcan Sanli, D. E., Sanli, A. N., Yildirim, D., and Dogan, I. (2025). Can ChatGPT detect breast cancer on mammography? J. Med. Screen. 32, 172–175. doi: 10.1177/09691413251334587
Tolentino, R., Baradaran, A., Gore, G., Pluye, P., and Abbasgholizadeh-Rahimi, S. (2024). Curriculum frameworks and educational programs in AI for medical students, residents, and practicing physicians: scoping review. JMIR Med. Educ. 10:e54793. doi: 10.2196/54793
Triplett, N. S., Mbwayo, A., Kiche, S., Sackey, E., AlRasheed, R., Okoth, D. A., et al. (2024). A problem shared is a problem solved: integrating human-centered design and implementation science to optimize lay counselor supervision in Western Kenya. SSM Ment. Health 5:100319. doi: 10.1016/j.ssmmh.2024.100319
Truhn, D., Eckardt, J. N., Ferber, D., and Kather, J. N. (2024). Large language models and multimodal foundation models for precision oncology. NPJ Precis. Oncol. 8:72. doi: 10.1038/s41698-024-00573-2
Vakalopoulou, M., Christodoulidis, S., Burgos, N., Colliot, O., and Lepetit, V. (2023). “Deep learning: basics and Convolutional Neural Networks (CNNs),” in Machine Learning for Brain Disorders, ed. O. Colliot. (New York, NY: Humana)77-115. doi: 10.1007/978-1-0716-3195-9_3
van Velzen, M., Boru, A., Sarton, E., and de Beaufort, A. J. (2024). Design thinking in medical education to tackle real world healthcare problems: the masterminds challenge. Med. Teach. 46, 611–613. doi: 10.1080/0142159X.2024.2305713
Vykhrushch, A. V., Khvalyboha, T. I., Fedchyshyn, N. O., Bagriy, M. A., Fedoniuk, L. Y., Protsyk, H. M., et al. (2021). Development of medical students creativity as a priority of modern higher education. Wiad. Lek. 74, 3204–3213. doi: 10.36740/WLek202112115
Waisberg, E., Ong, J., Kamran, S. A., Masalkhi, M., Paladugu, P., Zaman, N., et al. (2025). Generative artificial intelligence in ophthalmology. Surv. Ophthalmol. 70, 1–11. doi: 10.1016/j.survophthal.2024.04.009
Wang, P., and Chow, S. C. (2023). Innovative thinking of clinical investigation for rare disease drug development. Orphanet J. Rare Dis. 18:299. doi: 10.1186/s13023-023-02909-w
Wiggins, G. A. (2020). Creativity, information, and consciousness: the information dynamics of thinking. Phys. Life Rev. 34, 1–39. doi: 10.1016/j.plrev.2018.05.001
Wu, C., Lin, W., Zhang, X., Zhang, Y., Xie, W., and Wang, Y. (2024). PMC-LLaMA: toward building open-source language models for medicine. J. Am. Med. Inform. Assoc. 31, 1833–1843. doi: 10.1093/jamia/ocae045
Xu, X., Chen, Y., and Miao, J. (2024). Opportunities, challenges, and future directions of large language models, including ChatGPT in medical education: a systematic scoping review. J. Educ. Eval. Health Prof. 21:6. doi: 10.3352/jeehp.2024.21.6
Yánez Benítez, C., Tilsed, J., Weinstein, E. S., Caviglia, M., Herman, S., Montán, C., et al. (2023). Education, training and technological innovation, key components of the ESTES-NIGHTINGALE project cooperation for mass casualty incident preparedness in Europe. Eur. J. Trauma Emerg. Surg. 49, 653–659. doi: 10.1007/s00068-022-02198-1
Yang, J., Zhuang, X., Li, Z., Xiong, G., Xu, P., Ling, Y., et al. (2024). CPMKG: a condition-based knowledge graph for precision medicine. Database (Oxford) 2024:base102. doi: 10.1093/database/baae102
Yazdani, S., Henry, R. C., Byrne, A., and Henry, I. C. (2025). Utility of word embeddings from large language models in medical diagnosis. J. Am. Med. Inform. Assoc. 32, 526–534. doi: 10.1093/jamia/ocae314
Yin, S., Fu, C., Zhao, S., Li, K., Sun, X., Xu, T., et al. (2024). A survey on multimodal large language models. Natl. Sci. Rev. 11:nwae403. doi: 10.1093/nsr/nwae403
Yu, H., Fan, L., Li, L., Zhou, J., Ma, Z., Xian, L., et al. (2024). Large language models in biomedical and health informatics: a review with bibliometric analysis. J. Healthc. Inform. Res. 8, 658–711. doi: 10.1007/s41666-024-00171-8
Zhang, F., Li, J., Li, Y. C., Zhang, Z., Yu, Y., and Ye, D. (2025). Improving sample efficiency of reinforcement learning with background knowledge from large language models. IEEE Trans. Neural. Netw. Learn. Syst. doi: 10.1109/TNNLS.2025.3590731 [Epub ahead of print].
Keywords: multimodal large models, innovative thinking, design thinking, EDIPT model new paradigm, innovation enhancement
Citation: Liu Q, Xue W, Meng L, Zhu Y and Li J (2025) Research on the training strategy of college students' design thinking and innovation ability based on multimodal large model. Front. Educ. 10:1640684. doi: 10.3389/feduc.2025.1640684
Received: 04 June 2025; Accepted: 09 October 2025;
Published: 22 October 2025.
Edited by:
Fauziah Sulaiman, Universiti Malaysia Sabah, MalaysiaReviewed by:
Tianyi Sui, Tianjin University, ChinaMuhammad Kristiawan, University of Bengkulu, Indonesia
Erikson Saragih, Universitas Sumatera Utara, Indonesia
Copyright © 2025 Liu, Xue, Meng, Zhu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jixin Li, ZHJsaWppeGluQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Qing Liu1†
Qing Liu1† Lingbo Meng
Lingbo Meng Jixin Li
Jixin Li