- 1The University of Jordan School of Medicine, Amman, Jordan
- 2Hunter–New England Health, New Lambton, NSW, Australia
- 3Division of Internal Medicine, MedStar Georgetown University Hospital/Washington Hospital Center, Washington, DC, United States
- 4Department of Internal Medicine, The University of Jordan School of Medicine, Amman, Jordan
Objective: We aimed to investigate the effect of dosage reduction of four hypoglycemic multidrug regimens on the incidences of acute glycemic complications in people with type 2 diabetes who fast during Ramaḍān.
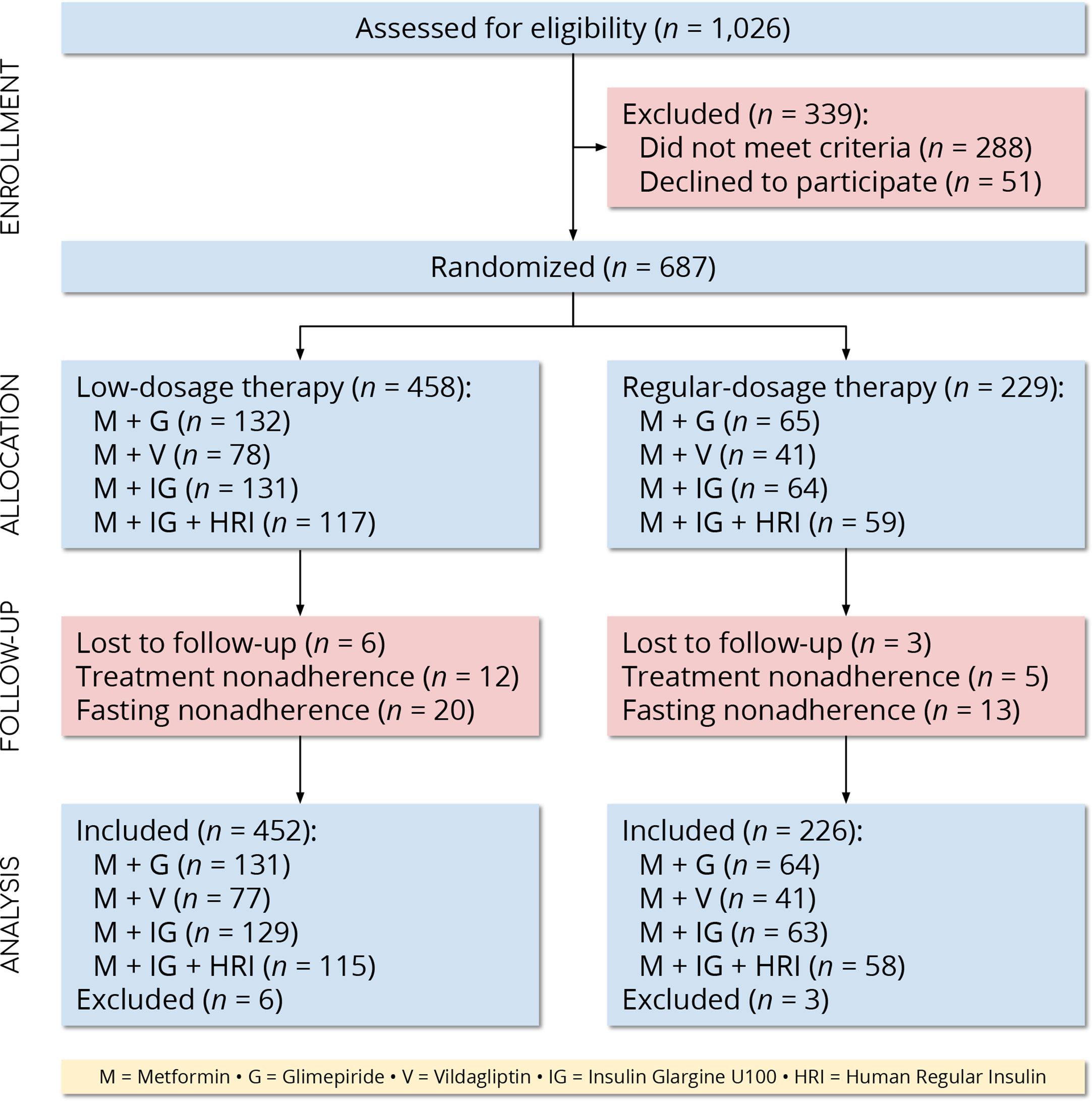
Methods: We conducted an open-label, parallel-group, randomized controlled trial at a tertiary care center in Amman, Jordan. We recruited adults with type 2 diabetes who expressed an intention to fast during Ramaḍān and were adherent to one of four regimens—namely: metformin and glimepiride; metformin and vildagliptin; metformin and insulin glargine U100; or, metformin, insulin glargine U100, and human regular insulin. We randomly assigned participants in a 2:1 ratio to low- or regular-dosage therapy. The primary outcomes were the incidences of hypoglycemia and hyperglycemia during the 29 days of Ramaḍān 2017, and the secondary outcomes were the incidences of diabetic ketoacidosis and hyperosmolar hyperglycemic state during the same period.
Results: We randomly assigned 687 participants to low-dosage therapy (n = 458) or regular-dosage therapy (n = 229) and included 678 (452 and 226, respectively) in the final analysis. The incidence of hypoglycemia was lower in the low-dosage group compared with the regular-dosage group (19 [4.2%] vs. 52 [23.0%], respectively; OR, 0.15 [95% CI, 0.08–0.26]; P < 0.001). The incidence of hyperglycemia did not differ between the low- and regular-dosage groups (319 [70.6%] vs. 154 [68.1%], respectively; OR, 1.12 [95% CI, 0.79–1.58]; P = 0.5). No participants experienced diabetic ketoacidosis or hyperosmolar hyperglycemic state. Each 1% decrease in the baseline HbA1c concentration was associated with a 19.9-fold (95% CI, 9.6–41.5; P < 0.001) increase in the odds of hypoglycemia, and each 1% increase in the baseline HbA1c concentration was associated with a 15.7-fold (95% CI, 10.0–24.6; P < 0.001) increase in the odds of hyperglycemia.
Conclusion: Dosage reduction decreases the incidence of hypoglycemia without a concomitant increase in the incidences of hyperglycemia, diabetic ketoacidosis, and hyperosmolar hyperglycemic state in people with type 2 diabetes who fast during Ramaḍān.
Clinical Trial Registration: www.ClinicalTrials.gov, identifier NCT04237493.
Introduction
Every lunar year, during the month of Ramaḍān, Muslims abstain from food and drink between dawn and nightfall. People who fast usually consume a meal after nightfall (ifār), another before dawn (suūr), and multiple snacks in between (1). Muslims with a chronic disease, such as type 2 diabetes, are exempt from fasting, but many choose to fast despite the health risks. According to a population-based study, 79% of Muslims with type 2 diabetes (~80 million people worldwide) observe the fast (2). People with type 2 diabetes who fast during Ramaḍān are at increased risk of acute glycemic complications—namely: hypoglycemia, hyperglycemia, diabetic ketoacidosis, and hyperosmolar hyperglycemic state (3).
One strategy to prevent acute glycemic complications is dosage reduction of hypoglycemic drug therapy (4). Ideally, dosage reduction should produce a decrease in the incidence of hypoglycemia without a concomitant increase in the incidence of hyperglycemia. Currently, evidence for or against the safety and efficacy of dosage reduction in people with type 2 diabetes who fast during Ramaḍān is scarce (1, 4, 5). Some randomized controlled trials (RCTs) have investigated the effect of dosage reduction of one or two hypoglycemic drugs on the incidence of hypoglycemia in people with type 2 diabetes who fast during Ramaḍān (6–8). However, many common hypoglycemic multidrug regimens have not been investigated, and the incidences of other important acute glycemic complications have not been measured.
Therefore, we aimed to investigate the effect of dosage reduction of four hypoglycemic multidrug regimens on the incidences of acute glycemic complications in people with type 2 diabetes who fast during Ramaḍān.
Materials and Methods
Trial Design and Participants
We conducted an open-label, parallel-group, randomized controlled trial at a tertiary care center in Amman, Jordan. We recruited people with type 2 diabetes from the endocrinology outpatient clinics between February and April 2017. Eligible participants were adults (≥18 years) who expressed an intention to fast during Ramaḍān 2017 (between May 27 and June 24, 2017) and were adherent to one of four hypoglycemic multidrug regimens for at least the past three months. The four regimens are outlined in Table 1. We selected these four regimens because they were the most commonly used by people who attended our clinics during the study period. Newer drug classes, such as sodium–glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists, were not commonly used by our patients. We defined treatment adherence as use of ≥80% of prescribed medication (by pill and/or vial count).
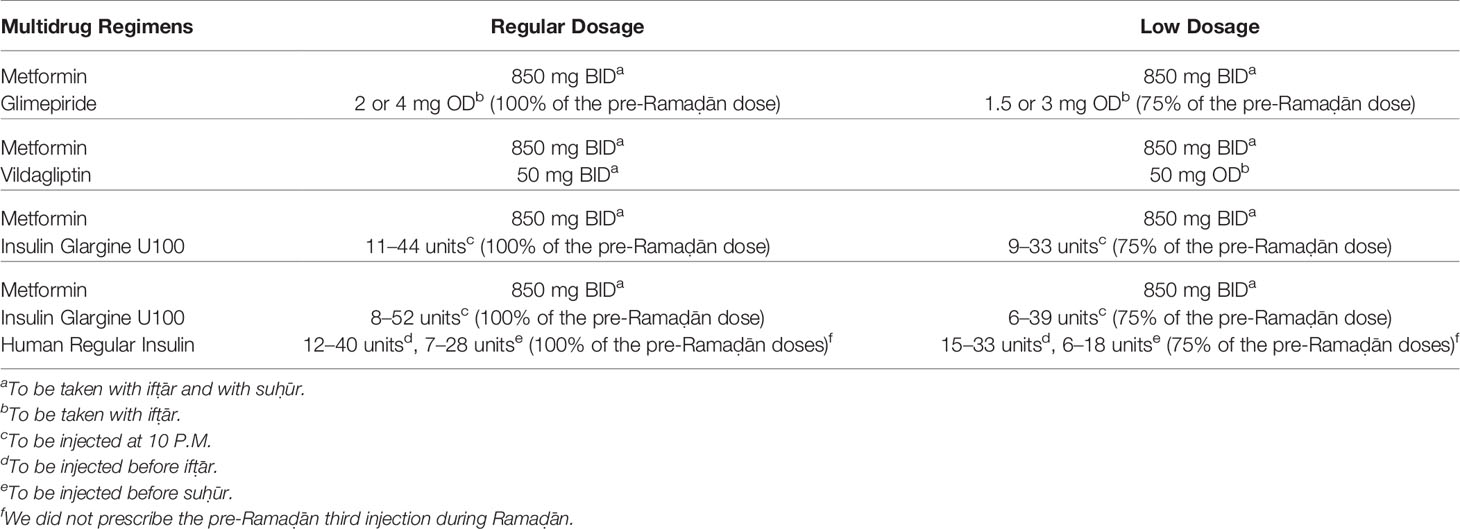
Table 1 The hypoglycemic multidrug regimens used during Ramaḍān by our participants, who we randomly allocated to low- or regular-dosage therapy (N = 678 participants).
We excluded people with type 1 diabetes, latent autoimmune diabetes in adults, secondary diabetes, or autonomic neuropathy. In addition, we excluded pregnant, postpartum, breastfeeding, and eumenorrheic women. Pregnant, postpartum, and breastfeeding women are exempt from fasting, and eumenorrheic women do not fast during menstruation. We also excluded participants who experienced diabetic ketoacidosis or hyperosmolar hyperglycemic state within three months and those who received niacin or corticosteroids within one month. In addition, we excluded participants with a baseline hemoglobin A1c (HbA1c) concentration below 6.0% (42 mmol/mol) or exceeding 11.0% (97 mmol/mol). Finally, we reviewed the medical records and excluded participants who had a history of recurrent hypoglycemia, hypoglycemia unawareness, chronic renal insufficiency (stages IV or V), liver cirrhosis, uncontrolled epilepsy, depressive disorder, bipolar disorder, psychotic disorder, or cognitive dysfunction.
Procedures
A research assistant, who was otherwise not involved in the study, generated the allocation sequence and enclosed the assignments in sequentially numbered, opaque, sealed envelopes. We enrolled participants and randomly assigned them (2:1 ratio) to low- or regular-dosage therapy. We stratified randomization by treatment regimen and used unequal allocation to obtain more safety data for low-dosage therapy. We determined the extent of dosage reduction (Table 1) based on our experience from a previous study (9).
We asked participants to attend a clinic visit before Ramaḍān and another after Ramaḍān. During the pre-Ramaḍān clinic visit, we prescribed the treatment dosage to be taken during Ramaḍān and asked participants to self-monitor their blood glucose concentration four times a day—namely, before suūr (the meal before dawn), at noon, before ifār (the meal after nightfall), and two hours after ifār—and if they developed any symptoms of hypoglycemia or hyperglycemia. We also offered participants the option to continue using their own glucometer and test strips if the device met the ISO 15197:2013 standard. Otherwise, we offered participants a new glucometer and test strips. We advised participants to break the fast and seek medical attention if they experienced any symptom of hypoglycemia or hyperglycemia or recorded a blood glucose concentration ≤70 mg/dL (3.9 mmol/L). Finally, we recorded nine baseline characteristics—namely: age, biologic sex, years since diagnosis, baseline HbA1c concentration, body mass index (BMI), polypharmacy, β1-blocker use, angiotensin-converting enzyme (ACE) inhibitor use, and number of comorbidities. We classified BMI according to the standard World Health Organization classification system (10). We defined polypharmacy as the concurrent, long-term use of five or more drugs (11). During the post-Ramaḍān clinic visit, we assessed the treatment and fasting adherence of participants, and we measured the outcomes using interviews, chart reviews and glucometer readings. We defined fasting adherence as observance of the full Ramaḍān fast excluding per-protocol breaking of the fast.
Outcomes
The primary outcomes were the incidences of hypoglycemia and hyperglycemia during the 29 days of Ramaḍān 2017. We identified and classified hypoglycemia based on the definitions of the International Hypoglycaemia Study Group (12). Briefly, level 1 hypoglycemia corresponds to a blood glucose concentration ≤70 mg/dL (3.9 mmol/L), level 2 hypoglycemia corresponds to a blood glucose concentration ≤54 mg/dL (3.0 mmol/L), and level 3 hypoglycemia denotes hypoglycemia with severe cognitive impairment requiring external assistance for recovery. We defined hyperglycemia as a blood glucose concentration ≥200 mg/dL (11.1 mmol/L). The secondary outcomes were the incidences of diabetic ketoacidosis and hyperosmolar hyperglycemic state (defined according to a consensus report by the American Diabetes Association) during the same period (13).
Statistical Methods
We used R (version 4.0.2) to perform data analysis. To calculate the minimum number of participants required, we anticipated incidences of hypoglycemia of 7.5% and 15% in the low- and regular-dosage groups, respectively, for an overall incidence of 10% (14). The minimum target was 597 participants (α = 0.05, β = 0.2). We summarized categorical data as n (%) and continuous data as mean ± standard deviation. To measure the association between treatment dosage and the level of hypoglycemia, we used Pearson’s χ2 test. To compare the distribution of the number of episodes of hyperglycemia between the low- and regular-dosage groups, we used the Mann–Whitney U test. We used Pearson’s χ2 test to compare the primary outcomes between the low- and regular-dosage groups and binary logistic regression to model the primary outcomes as functions of treatment dosage, treatment regimen, age, biologic sex, years since diagnosis, BMI, baseline HbA1c concentration, and polypharmacy. We handled missing data according to the recommendations of Jakobsen et al. (15). We used the Benjamini–Hochberg method to correct for multiple testing and interpreted values of P < 0.05 (two-tailed) to indicate statistical significance.
Ethics
The Institutional Review Board of the Jordan University Hospital approved the trial (2017/35). We did not offer a financial incentive for participation, and all participants provided written informed consent. The trial is registered with ClinicalTrials.gov (NCT04237493).
Results
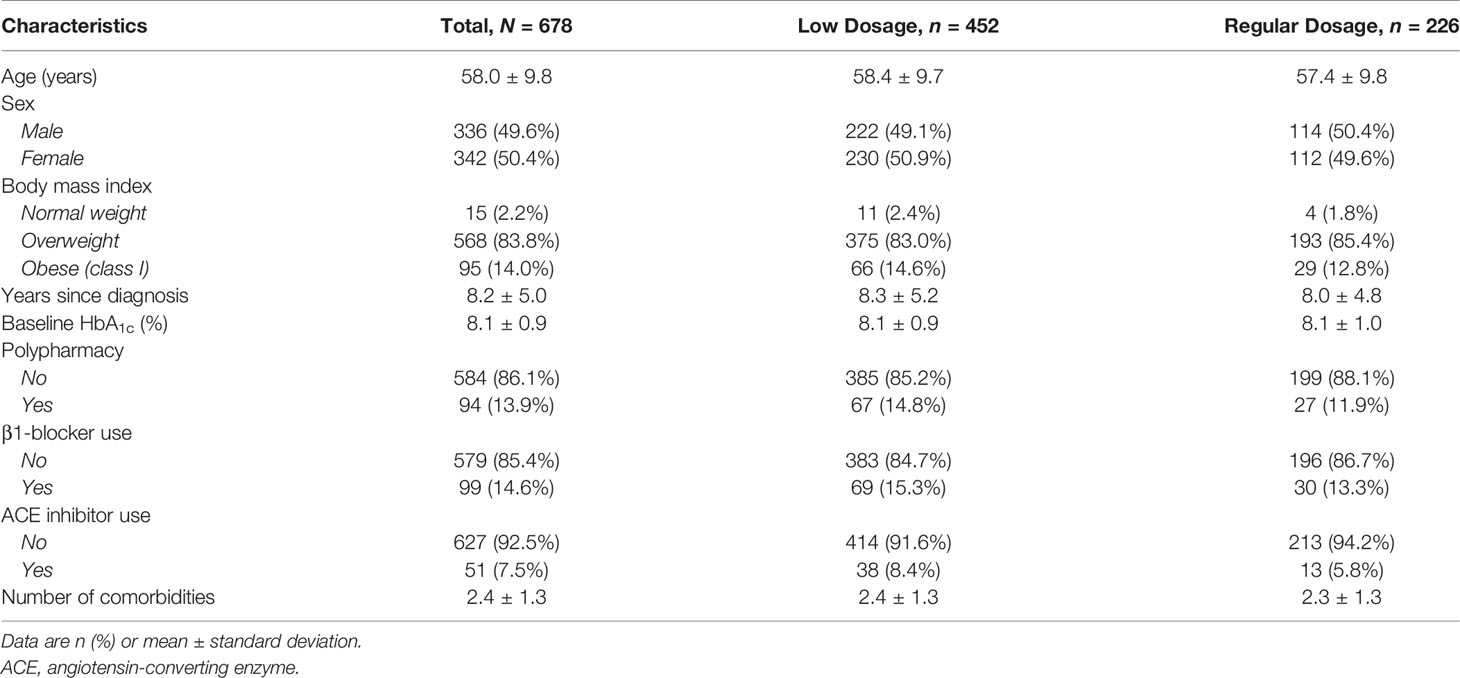
We screened 1,026 people for eligibility and 687 (67.0%) met the eligibility criteria. We excluded nine participants (1.3%) with missing outcomes and included the remaining 678 (98.7%) in the final analysis (Figure 1). The numbers of participants in the low- and regular-dosage groups were 452 (66.7%) and 226 (33.3%), respectively. In total, 195 participants (28.8%) were on metformin and glimepiride; 118 (17.4%) were on metformin and vildagliptin; 192 (28.3%) were on metformin and insulin glargine U100; and, 173 (25.5%) were on metformin, insulin glargine U100, and human regular insulin. We report the baseline characteristics of the study population in Table 2 (by-dosage and total) and Supplementary Table 1 (by-regimen and by-dosage).
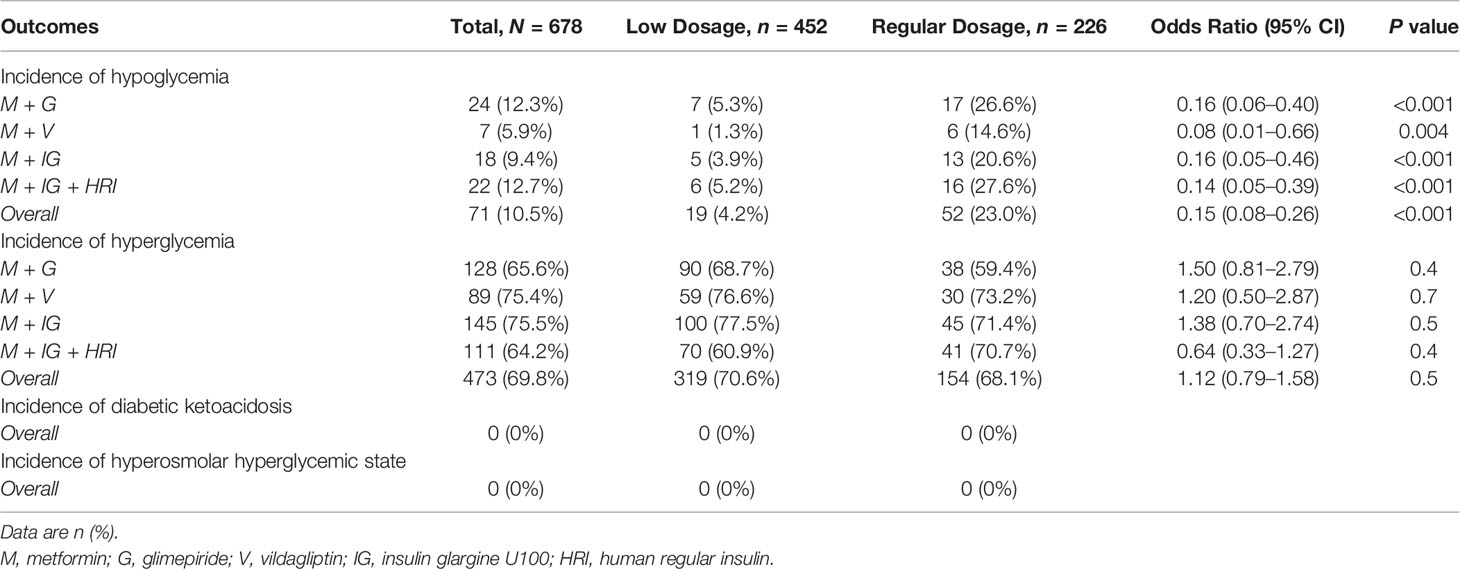
We report the outcomes of the study population in Table 3. Hypoglycemia occurred in 71 participants (10.5%), with a lower incidence in the low-dosage group compared with the regular-dosage group (19 [4.2%] vs. 52 [23.0%], respectively; P < 0.001). The difference in incidences was consistent across all four treatment regimens. Of the participants in the low-dosage group, 14 (73.7%) experienced level 1 hypoglycemia and the remaining five (26.3%) experienced level 2 hypoglycemia. Of the participants in the regular-dosage group, 32 (61.5%) experienced level 1 hypoglycemia and the remaining 20 (38.5%) experienced level 2 hypoglycemia. No participants experienced level 1 or 2 hypoglycemia more than once, and no participants experienced level 3 hypoglycemia. In participants who experienced level 1 or 2 hypoglycemia, treatment dosage was not associated with the level of hypoglycemia (P = 0.3). Hyperglycemia occurred in 473 participants (69.8%), with no statistically significant difference in the incidences between the low- and regular-dosage groups (319 [70.6%] vs. 154 [68.1%], respectively; P = 0.5). The distribution of the number of episodes of hyperglycemia did not differ between the groups (P = 0.5), and the incidences of hyperglycemia were not statistically significantly different between the groups across all four treatment regimens. No participants experienced diabetic ketoacidosis or hyperosmolar hyperglycemic state.
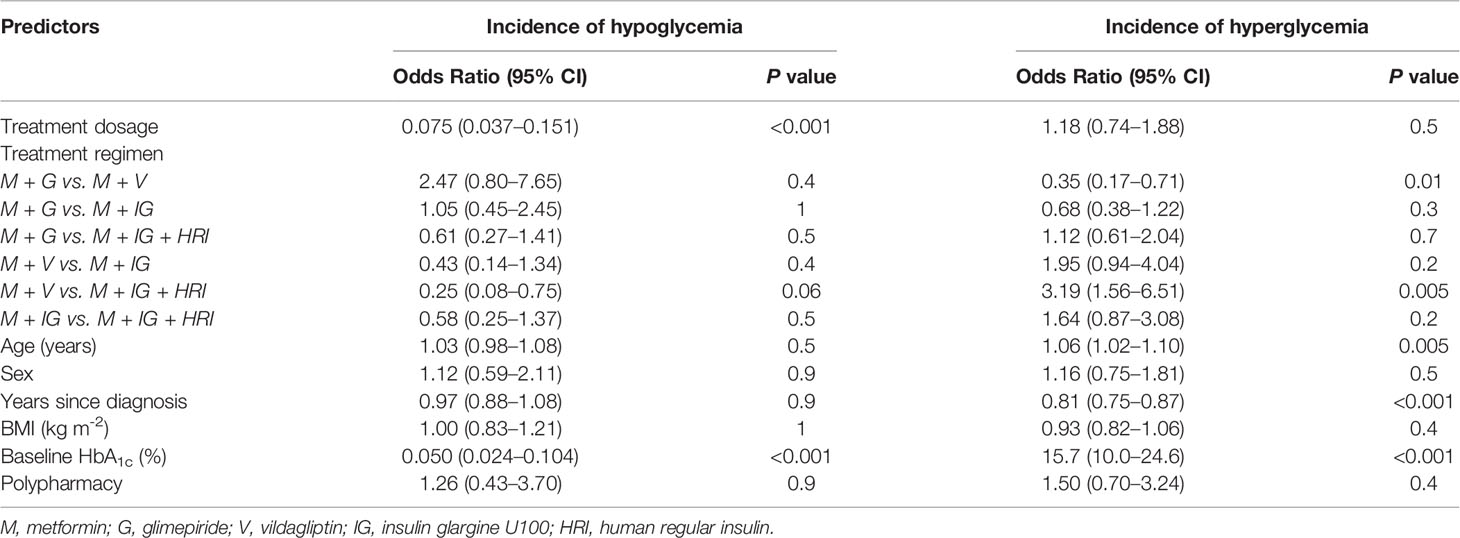
In multivariable analysis, treatment dosage and baseline HbA1c concentration were independent predictors of the incidence of hypoglycemia (Table 4). Each 1% (11 mmol/mol) decrease in the baseline HbA1c concentration predicted a 19.9-fold increase in the odds of hypoglycemia. Notably, treatment dosage was not an independent predictor of the incidence of hyperglycemia. However, the odds of hyperglycemia was higher in participants who were on metformin and vildagliptin compared with participants who were on metformin and glimepiride or metformin, insulin glargine U100, and human regular insulin. In addition, age, years since diagnosis, and baseline HbA1c concentration were also independent predictors of the incidence of hyperglycemia (Table 4). Each 1% (11 mmol/mol) increase in the baseline HbA1c concentration predicted a 15.7-fold increase in the odds of hyperglycemia.
Discussion
We conducted the first randomized controlled trial to investigate the effect of dosage reduction of four hypoglycemic multidrug regimens on the incidences of acute glycemic complications in people with type 2 diabetes who fast during Ramaḍān. We found that: (a) Dosage reduction was associated with a decrease in the incidence of hypoglycemia without a concomitant increase in the incidence of hyperglycemia; (b) Both effects were consistent across people on any one of four hypoglycemic multidrug regimens—namely: metformin and glimepiride; metformin and vildagliptin; metformin and insulin glargine U100; and, metformin, insulin glargine U100, and human regular insulin; (c) No participants experienced diabetic ketoacidosis or hyperosmolar hyperglycemic state, which suggests that dosage reduction is safe; and, (d) An increase in the baseline HbA1c concentration was independently associated with an increase in the odds of hyperglycemia but a decrease in the odds of hypoglycemia during Ramaḍān.
The incidence of hypoglycemia during Ramaḍān varies widely between different populations. Jabbar et al. reported that the incidence of hypoglycemia during Ramaḍān ranged from 4% in the Middle East to 13% in North Africa (16). In our sample, the incidence of hypoglycemia was 10.5% and ranged from 4.2% in the low-dosage group to 23.0% in the regular-dosage group. The difference in incidences was consistent across all four treatment regimens. For instance, we found that 25% dosage reduction of glimepiride was associated with a decrease in the incidence of hypoglycemia. In contrast, Belkhadir et al. reported that 25% dosage reduction of glyburide (another sulfonylurea compound) monotherapy was not associated with a decrease in the incidence of hypoglycemia during Ramaḍān (6). However, they did not identify episodes of hypoglycemia based on blood glucose concentrations. Rather, they rated the episodes on a “six point scale”, so the incidence of hypoglycemia they reported may be an underestimate.
Likewise, we found that dosage reduction of vildagliptin (in dual therapy with metformin) was associated with a decrease in the incidence of hypoglycemia. Current practice guidelines do not recommend dosage reduction of dipeptidyl-peptidase IV inhibitors in people with type 2 diabetes who fast during Ramaḍān (1, 4, 5). The recommendation is based on the finding that dipeptidyl-peptidase IV inhibitors are associated with a low risk of hypoglycemia in monotherapy and dual therapy with metformin (4, 17). In addition, Bosi et al. showed that the incidence of hypoglycemia does not differ between patients on metformin and 50 mg vildagliptin daily and those on metformin and 100 mg vildagliptin daily (18). The foregoing results seem likely to apply to people with type 2 diabetes who fast during Ramaḍān because dipeptidyl-peptidase IV inhibitors stimulate insulin secretion in a glucose-dependent manner (19). However, in our clinical experience, we observed that the incidence of hypoglycemia increases in people on metformin and 100 mg vildagliptin daily during Ramaḍān compared with the months before Ramaḍān. In support, Halimi et al. reported that the incidence of confirmed hypoglycemia in people on metformin and vildagliptin who fast during Ramaḍān was 24% (20). The discrepancy between these results remains unclear but we speculate that the increased incidence of hypoglycemia in people on metformin and 100 mg vildagliptin daily during Ramaḍān may be related to interindividual variability in the glucagon response to hypoglycemia (21, 22).
We also found that dosage reduction was not associated with hyperglycemia (overall and across all treatment regimens). Notably, the odds of hyperglycemia was higher in participants who were on metformin and vildagliptin compared with two other regimens (metformin and glimepiride; metformin, insulin glargine U100, and human regular insulin) independent of treatment dosage. To our knowledge, the effects of these regimens on the incidence of hyperglycemia in patients with type 2 diabetes who fast during Ramaḍān have not been compared in head-to-head trials. However, we speculate that the glucose-lowering effects of sulfonylureas and insulins are more potent than dipeptidyl-peptidase IV inhibitors during prolonged fasting because the latter stimulate insulin secretion in a glucose-dependent manner while the former are glucose-independent (19). Overall, the incidence of hyperglycemia in people with type 2 diabetes who fast during Ramaḍān is not well-established; compared with hypoglycemia, hyperglycemia is less often an outcome of interest. According to the EPIDIAR study—a population-based study of 11,173 people with type 2 diabetes—the incidence of hyperglycemia is higher in people who fast (2). However, according to the DAR–MENA T2DM study—a prospective, observational study of 1,749 people with type 2 diabetes—the incidence of hyperglycemia is lower in people who fast (14).
No participants experienced diabetic ketoacidosis or hyperosmolar hyperglycemic state, which supports the safety of dosage reduction. We observed similar results in a previous study on another group of people with type 2 diabetes who fast during Ramaḍān (9). Some authors have suggested that people with diabetes who fast during Ramaḍān are at increased risk of diabetic ketoacidosis (23). The suggested reasons are insulin insufficiency associated with excess counterregulatory hormones, excessive dosage reduction of hypoglycemic drugs, and compensatory overeating during the nighttime. However, the reasons are unsubstantiated, and a recent review showed that the risk of diabetic ketoacidosis is not higher in people who fast (24).
We also found that people with a higher baseline HbA1c concentration were less likely to experience hypoglycemia and more likely to experience hyperglycemia. In support, Loke et al. reported that an HbA1c concentration less than 8% is a risk factor for hypoglycemia during Ramaḍān (25). Therefore, people with well-controlled type 2 diabetes who fast during Ramaḍān require closer monitoring and may benefit from dosage reduction beyond what we have proposed.
Our study has some limitations. First, we recruited participants from a single center by consecutive sampling. Therefore, our conclusions may not be generalizable. However, our center provides tertiary care to people from all the governorates of Jordan, so our conclusions may apply to the general population of Jordan. Notably, the incidence of hypoglycemia in Ramaḍān varies widely between the populations of different countries, and so our investigation must be replicated in other populations (16). Second, glycemic control during Ramaḍān is an important outcome that we did not measure. Unlike HbA1c, serum fructosamine is a suitable marker of short-term glycemic control (less than one month). However, we did not have access to the test. In addition, our methods may be improved by the use of continuous glucose monitoring. We recommend the use of serum fructosamine and continuous glucose monitoring in future investigations of people with diabetes who fast during Ramaḍān. Third, we did not assess participants for β-cell failure. However, we anticipate that the likelihood of β-cell failure in our participants is low because the mean duration of diabetes was 8.2 years since diagnosis, which is relatively short. According to the Veterans Affairs Diabetes Trial, the mean blood C-peptide—a marker of β-cell failure—in patients with type 2 diabetes of 13–15 years duration was ~0.7 nmol/L, which is considerably higher than the cutoff value (<0.2 nmol/L) for β-cell failure (26).
In conclusion, dosage reduction decreases the incidence of hypoglycemia without a concomitant increase in the incidences of hyperglycemia, diabetic ketoacidosis, and hyperosmolar hyperglycemic state in people with type 2 diabetes who fast during Ramaḍān.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board of the Jordan University Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AZ and LZ designed the study. LZ, AB, AH, YH, and AQ performed the literature search. AZ conducted the trial. AZ and AB collected the data. AZ, LZ, JA, and AB interpreted the data. JA performed data analysis. JA, LZ, and AZ wrote the report, and RZ and MT reviewed the report. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2021.613826/full#supplementary-material
References
1. Al-Arouj M, Assaad-Khalil S, Buse J, Fahdil I, Fahmy M, Hafez S, et al. Recommendations for Management of Diabetes During Ramadan: Update 2010. Diabetes Care (2010) 33:1895–902. doi: 10.2337/dc10-0896
2. Salti I, Bénard E, Detournay B, Bianchi-Biscay M, Le Brigand C, Voinet C, et al. A Population-Based Study of Diabetes and Its Characteristics During the Fasting Month of Ramadan in 13 Countries: Results of the Epidemiology of Diabetes and Ramadan 1422/2001 (EPIDIAR) Study. Diabetes Care (2004) 27:2306–11. doi: 10.2337/diacare.27.10.2306
3. Hassan A, Meo SA, Usmani AM, Shaikh TJ. Diabetes During Ramadan – PRE-Approach Model: Presentation, Risk Stratification, Education. Eur Rev Med Pharmacol Sci (2014) 18:1798–805.
4. Bajaj HS, Abouhassan T, Ahsan MR, Arnaout A, Hassanein M, Houlden RL, et al. Diabetes Canada Position Statement for People With Types 1 and 2 Diabetes Who Fast During Ramadan. Can J Diabetes (2019) 43:3–12. doi: 10.1016/j.jcjd.2018.04.007
5. Hassanein M, Al-Arouj M, Hamdy O, Bebakar WMW, Jabbar A, Al-Madani A, et al. Diabetes and Ramadan: Practical Guidelines. Diabetes Res Clin Pract (2017) 126:303–16. doi: 10.1016/j.diabres.2017.03.003
6. Belkhadir J, el Ghomari H, Klöcker N, Mikou A, Nasciri M, Sabri M. Muslims With Non-Insulin Dependent Diabetes Fasting During Ramadan: Treatment With Glibenclamide. BMJ (1993) 307:292–5. doi: 10.1136/bmj.307.6899.292
7. Shehadeh N, Maor Y, Ramadan Study Group. Effect of a New Insulin Treatment Regimen on Glycaemic Control and Quality of Life of Muslim Patients With Type 2 Diabetes Mellitus During Ramadan Fast – An Open Label, Controlled, Multicentre, Cluster Randomised Study. Int J Clin Pract (2015) 69:1281–8. doi: 10.1111/ijcp.12695
8. Hassanein M, Echtay AS, Malek R, Omar M, Shaikh SS, Ekelund M, et al. Original Paper: Efficacy and Safety Analysis of Insulin Degludec/Insulin Aspart Compared With Biphasic Insulin Aspart 30: A Phase 3, Multicentre, International, Open-Label, Randomised, Treat-to-Target Trial in Patients With Type 2 Diabetes Fasting During Ramadan. Diabetes Res Clin Pract (2018) 135:218–26. doi: 10.1016/j.diabres.2017.11.027
9. Beano AM, Zmaili MA, Gheith ZH, Naser AM, Momani MS, Yousef AMF, et al. Predetermined Anti-Diabetic Drug Regimen Adjustments During Ramadan Fasting: An Observational Study of Safety. Endocrinol Metab (Seoul) (2017) 32:265–73. doi: 10.3803/EnM.2017.32.2.265
10. World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Geneva, Switzerland: World Health Organization (2000).
11. Shorr RI, Ray WA, Daugherty JR, Griffin MR. Incidence and Risk Factors for Serious Hypoglycemia in Older Persons Using Insulin or Sulfonylureas. Arch Intern Med (1997) 157:1681–6. doi: 10.1001/archinte.157.15.1681
12. International Hypoglycaemia Study Group. Glucose Concentrations of Less Than 3.0 mmol/L (54 mg/dL) Should Be Reported in Clinical Trials: A Joint Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care (2017) 40(1):155–7. doi: 10.2337/dc16-2215
13. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic Crises in Adult Patients With Diabetes. Diabetes Care (2009) 32(7):1335–43. doi: 10.2337/dc09-9032
14. Hassanein M, Al Awadi FF, El Hadidy KES, Ali SS, Echtay A, Djaballah K, et al. The Characteristics and Pattern of Care for the Type 2 Diabetes Mellitus Population in the MENA Region During Ramadan: An International Prospective Study (DAR-MENA T2DM). Diabetes Res Clin Pract (2019) 151:275–84. doi: 10.1016/j.diabres.2019.02.020
15. Jakobsen JC, Gluud C, Wetterslev J, Winkel P. When and How Should Multiple Imputation Be Used for Handling Missing Data in Randomised Clinical Trials – a Practical Guide With Flowcharts. BMC Med Res Methodol (2017) 17(1):162. doi: 10.1186/s12874-017-0442-1
16. Jabbar A, Hassanein M, Beshyah SA, Boye KS, Yu M, Babineaux SM. CREED Study: Hypoglycaemia During Ramadan in Individuals With Type 2 Diabetes Mellitus From Three Continents. Diabetes Res Clin Pract (2017) 132:19–26. doi: 10.1016/j.diabres.2017.07.014
17. Mishriky BM, Cummings DM, Tanenberg RJ. The Efficacy and Safety of DPP4 Inhibitors Compared to Sulfonylureas as Add-on Therapy to Metformin in Patients With Type 2 Diabetes: A Systematic Review and Meta-Analysis. Diabetes Res Clin Pract (2015) 109:378–88. doi: 10.1016/j.diabres.2015.05.025
18. Bosi E, Camisasca RP, Collober C, Rochotte E, Garber AJ. Effects of Vildagliptin on Glucose Control Over 24 Weeks in Patients With Type 2 Diabetes Inadequately Controlled With Metformin. Diabetes Care (2007) 30:890–5. doi: 10.2337/dc06-1732
19. Mest HJ, Mentlein R. Dipeptidyl Peptidase Inhibitors as New Drugs for the Treatment of Type 2 Diabetes. Diabetologia (2005) 48:616–20. doi: 10.1007/s00125-005-1707-5
20. Halimi S, Levy M, Huet D, Quéré S, Dejager S. Experience With Vildagliptin in Type 2 Diabetic Patients Fasting During Ramadan in France: Insights From the VERDI Study. Diabetes Ther (2013) 4:385–98. doi: 10.1007/s13300-013-0038-7
21. Israelian Z, Szoke E, Woerle J, Bokhari S, Schorr M, Schwenke DC, et al. Multiple Defects in Counterregulation of Hypoglycemia in Modestly Advanced Type 2 Diabetes Mellitus. Metabolism (2006) 55:593–8. doi: 10.1016/j.metabol.2005.11.013
22. Segel SA, Paramore DS, Cryer PE. Hypoglycemia-Associated Autonomic Failure in Advanced Type 2 Diabetes. Diabetes (2002) 51:724–33. doi: 10.2337/diabetes.51.3.724
23. Ahmad J, Pathan MF, Jaleel MA, Fathima FN, Raza SA, Khan AK, et al. Diabetic Emergencies Including Hypoglycemia During Ramadan. Indian J Endocrinol Metab (2012) 16:512–5. doi: 10.4103/2230-8210.97996
24. Beshyah SA, Chowdhury TA, Ghouri N, Lakhdar AA. Risk of Diabetic Ketoacidosis During Ramadan Fasting: A Critical Reappraisal. Diabetes Res Clin Pract (2019) 151:290–8. doi: 10.1016/j.diabres.2019.02.027
25. Loke SC, Rahim KF, Kanesvaran R, Wong TW. A Prospective Cohort Study on the Effect of Various Risk Factors on Hypoglycaemia in Diabetics Who Fast During Ramadan. Med J Malaysia (2010) 65:3–6.
Keywords: type 2 diabetes mellitus, hypoglycemic agents, hypoglycemia, hyperglycemia, fasting
Citation: Zaghlol LY, Beirat AF, Amarin JZ, Hassoun Al Najar AM, Hasan YY, Qtaishat A, Tierney ME, Zaghlol RY and Zayed AA (2021) Effect of Dosage Reduction of Hypoglycemic Multidrug Regimens on the Incidences of Acute Glycemic Complications in People With Type 2 Diabetes Who Fast During Ramaḍān: A Randomized Controlled Trial. Front. Endocrinol. 12:613826. doi: 10.3389/fendo.2021.613826
Received: 03 October 2020; Accepted: 18 June 2021;
Published: 07 July 2021.
Edited by:
Ernesto Maddaloni, Sapienza University of Rome, ItalyReviewed by:
Silvia Pieralice, Campus Bio-Medico University, ItalyLuca D’Onofrio, Sapienza University of Rome, Italy
Copyright © 2021 Zaghlol, Beirat, Amarin, Hassoun Al Najar, Hasan, Qtaishat, Tierney, Zaghlol and Zayed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ayman A. Zayed, YmFyYWFheW1hbkBnbWFpbC5jb20=
 Louay Y. Zaghlol
Louay Y. Zaghlol Amir F. Beirat
Amir F. Beirat Justin Z. Amarin
Justin Z. Amarin Amro M. Hassoun Al Najar
Amro M. Hassoun Al Najar Yazan Y. Hasan
Yazan Y. Hasan Abdallah Qtaishat
Abdallah Qtaishat Michael E. Tierney2
Michael E. Tierney2 Raja Y. Zaghlol
Raja Y. Zaghlol Ayman A. Zayed
Ayman A. Zayed