- 1International Thyroid Surgery Center, Department of Otolaryngology-Head and Neck Surgery, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
- 2Center for Liquid Biopsy and Cohort Research, and Faculty of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 3Department of Otolaryngology-Head and Neck Surgery, Kaohsiung Municipal Siaogang Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
- 4Department of Otolaryngology, Massachusetts Eye and Ear Infirmary, Boston, MA, United States
- 5Department of Surgery, Massachusetts General Hospital, Harvard Medical School, Boston, MA, United States
- 6Department of Endocrine Surgery, Third Chair of General Surgery, Jagiellonian University Medical College, Krakow, Poland
- 7Department of Surgery, University Hospital Halle, Martin-Luther-University, Halle-Wittenberg, Germany
- 8Department of Otolaryngology, E-Da Hospital, School of Medicine, College of Medicine, I-Shou University, Kaohsiung, Taiwan
- 9Division of Otolaryngology-Head and Neck Surgery, Department of Surgery, NorthShore University HealthSystem, Evanston, IL, United States
- 10Department of Surgery, Ospedale di Circolo, ASST Settelaghi, Varese, Italy
- 11Department of General, Visceral and Transplantation Surgery, University of Duisburg-Essen, Essen, Germany
- 12Department of Human Pathology in Adulthood and Childhood “G. Barresi”, University Hospital G. Martino, University of Messina, Messina, Italy
Intraoperative neural monitoring (IONM) is now an integral aspect of thyroid surgery in many centers. Interest in IONM and the number of institutions that perform monitored thyroidectomies have increased throughout the world in recent years. For surgeons considering the introduction of IONM in their practice, specific training in IONM devices and procedures can substantially shorten the learning curve. The International Neural Monitoring Study Group (INMSG) has been at the forefront of IONM technology and procedural adoption since the introduction of neural monitoring in thyroid and parathyroid surgery. The purpose of this document is to define the INMSG consensus on essential elements of IONM training courses. Specifically, this document describes the minimum training required for teaching practical application of IONM and consensus views on key issues that must be addressed for the safe and reliable introduction of IONM in surgical practice. The intent of this publication is to provide societies, course directors, teaching institutions, and national organizations with a practical reference for developing IONM training programs. With these guidelines, IONM will be implemented optimally, to the ultimate benefit of the thyroid and parathyroid surgical patients.
Introduction
Intraoperative neural monitoring (IONM) is now an integral aspect of thyroid surgery in many centers. Interest in IONM, the number of institutions that perform, and societies that recommended monitored thyroidectomies have increased throughout the world in recent years (1–16). A recent international survey (16) of over 1,000 surgeons revealed that IONM is highly prevalent with 83% of surgeons using IONM in some or all of their cases. Reasons for use included patient request, preoperative vocal cord palsy, thyroid cancer, substernal goiter and most notably for reoperative surgery where the rate of use was 95%. The body of knowledge in IONM has also rapidly evolved in recent years with the introduction of new, less invasive monitoring devices, as well as the publication of prospective randomized clinical trials, multi-center studies, cost analyses, studies of ethical/medicolegal issues, clinical guidelines, and standards for the recurrent laryngeal nerve (RLN) and external branch of the superior laryngeal nerve (EBSLN) monitoring (1–4, 11, 17–34). Additionally, current technology enables the use of continuous-IONM (C-IONM) to analyze nerve monitoring signal loss and recovery under periodic vagus nerve (VN) stimulation and to understand the relationship between signal loss and early postoperative vocal fold palsy (5, 35–38). Up-to-date structured courses are needed to introduce the clinical, legal and research implications of these developments, in order that monitoring be done at the highest optimal and most current standards.
As IONM use in thyroid/parathyroid surgery is increasing, surgical residency programs have begun including IONM courses in their core curricula. Competency in the use of IONM technology in thyroid/parathyroid surgery is being tested similar to the use of other technologies (e.g., laparoscopic technology) in other specialties such as neurosurgical spine surgery (39), the training evolution for implementation of basic and advanced IONM system (IONM needs, stages and benefits) will improve the surgical residency and surgeon’s practice and maturity of autonomous IONM operations (Figure 1).
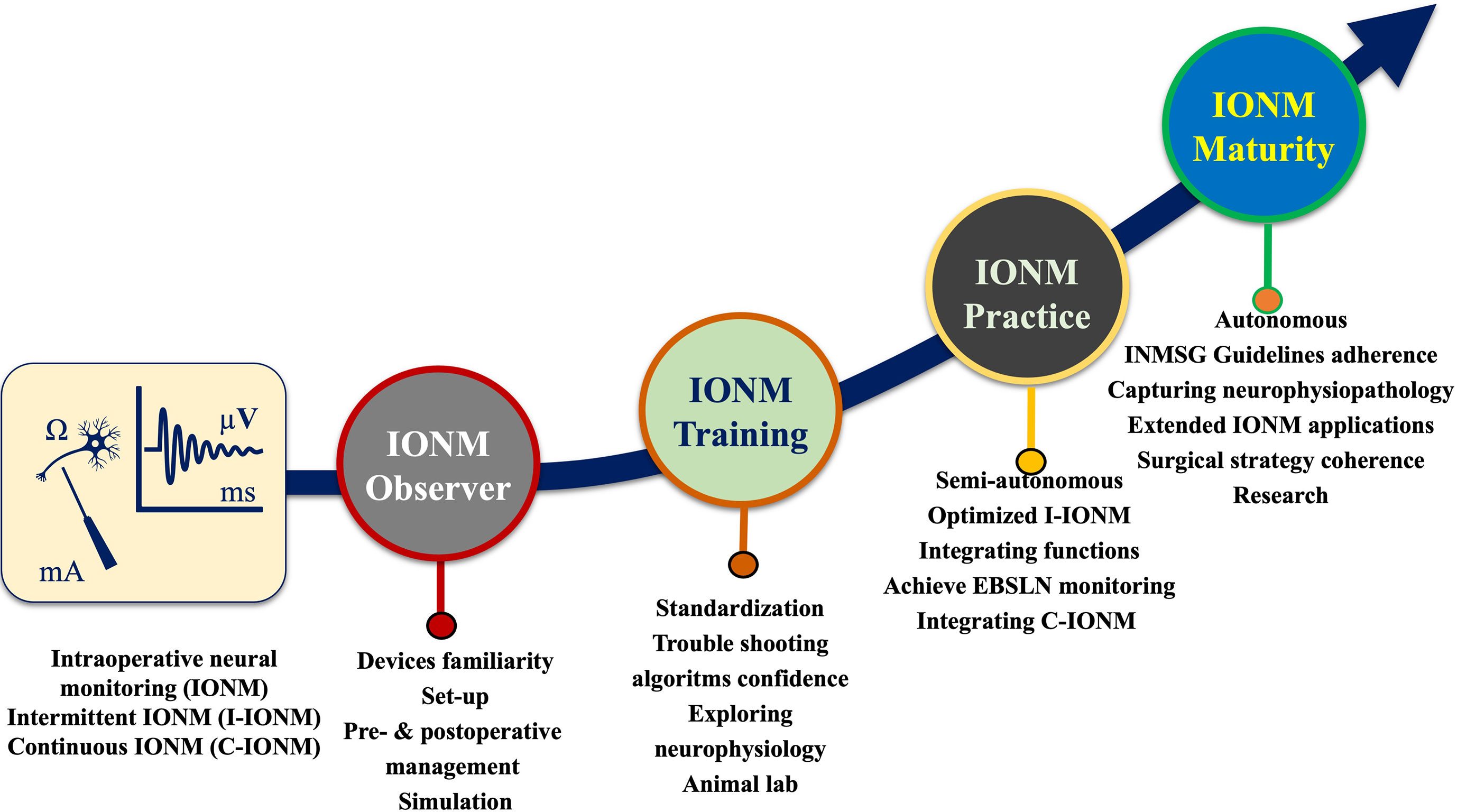
Figure 1 A journey to autonomous IONM operations. Training evolution for implementation of basic and advanced IONM system (IONM needs, stages and benefits).
Despite the growing need for and acceptance of IONM training, there remains a lack of professional certification by national or international thyroid societies (40). Currently, surgeons primarily receive IONM training through industry-sponsored courses that provide limited opportunities for certification and may be biased. Additionally, these non-standardized courses in IONM have not been vetted by professional groups and may not provide the optimal clinical education based on the most recent scientific literature.
The International Nerve Monitoring Study Group [INMSG(www.inmsg.org)] has been at the forefront of IONM technology and procedural adoption since the introduction of neural monitoring in thyroid/parathyroid surgery (1). Specifically, the INMSG has had leading roles in the development and evolution of international guidelines for laryngeal nerve monitoring (1–4). The INMSG has also addressed key issues in IONM training and specialization. The INMSG Board which is global and multidisciplinary in composition, has developed national and international training courses for general surgery and surgical specialties, including endocrine, head and neck, and Otolaryngologic or ENT surgery, in Europe, the US and Asia (Supplementary File 1). National IONM Study Groups have also developed IONM courses in collaboration with INMSG. The aims of training courses are (i) to address the increased interest in IONM and (ii) to discuss recent research in IONM as well as guidelines and standards for IONM practice. Since better clinical outcomes of IONM are associated with well-coordinated introduction to and training in new IONM technologies and procedures, consensus statements are needed to ensure an orderly process of incorporating these technologies in surgical practice (4, 41, 42). For surgeons considering the introduction of IONM in their practice, specific training in IONM devices and procedures can substantially shorten the learning curve (43). Notably, surgeons who adopt IONM tend to modify their surgical practices and dissection techniques and may have improved outcomes (43, 44).
The purpose of this document is to define the INMSG consensus on essential elements of IONM training courses. Specifically, this document describes the minimum training required for teaching practical application of IONM and consensus views on key issues that must be addressed for safe and reliable introduction of IONM in surgical practice. With these guidelines we feel IONM will be implemented optimally, to the ultimate benefit of thyroid/parathyroid surgical patients.
Consensus Statement and Implications
Training Course Requirements
Course Leadership Experience Level
General Requirements
Course leaders must have robust experience and have a national board qualification in general, endocrine, or otolaryngology-head and neck surgery (45, 46). By acting as a chair, the organizer of the IONM course should be able to provide expertise based on relevant experience and qualifications. A minimum of 50 cases per year, for no less than three years, should provide the course chair with sufficient experience for their role as the course director. Since the focus of the IONM Course is applying and managing IONM technology in thyroid/parathyroid surgery, course faculty and instructors require profound knowledge of endocrine neck surgery to provide the optimal environment for learning comprehensive implementation and management of IONM. The course should also emphasize patient safety and should ideally be enjoyable for participants.
IONM Requirements
Scope of Basic Course
Course faculty and instructors require full knowledge of laryngeal nerve anatomy/electrophysiology (VN, EBSLN, RLN) and profound experience in the standard use of IONM, including laryngeal examination before and after surgery(L1-L2), collaboration with the anesthesiologist (neuromuscular blockage agent selection and EMG endotracheal tube placement), standard equipment setup (Recording/Stimulation side electrodes, interface box and monitor connections), stimulating the EBSLN before and after upper thyroid pole dissection(S1-S2), and stimulating the VN and RLN before and after the dissection(V1-R1-R2-V2) (Figure 2).
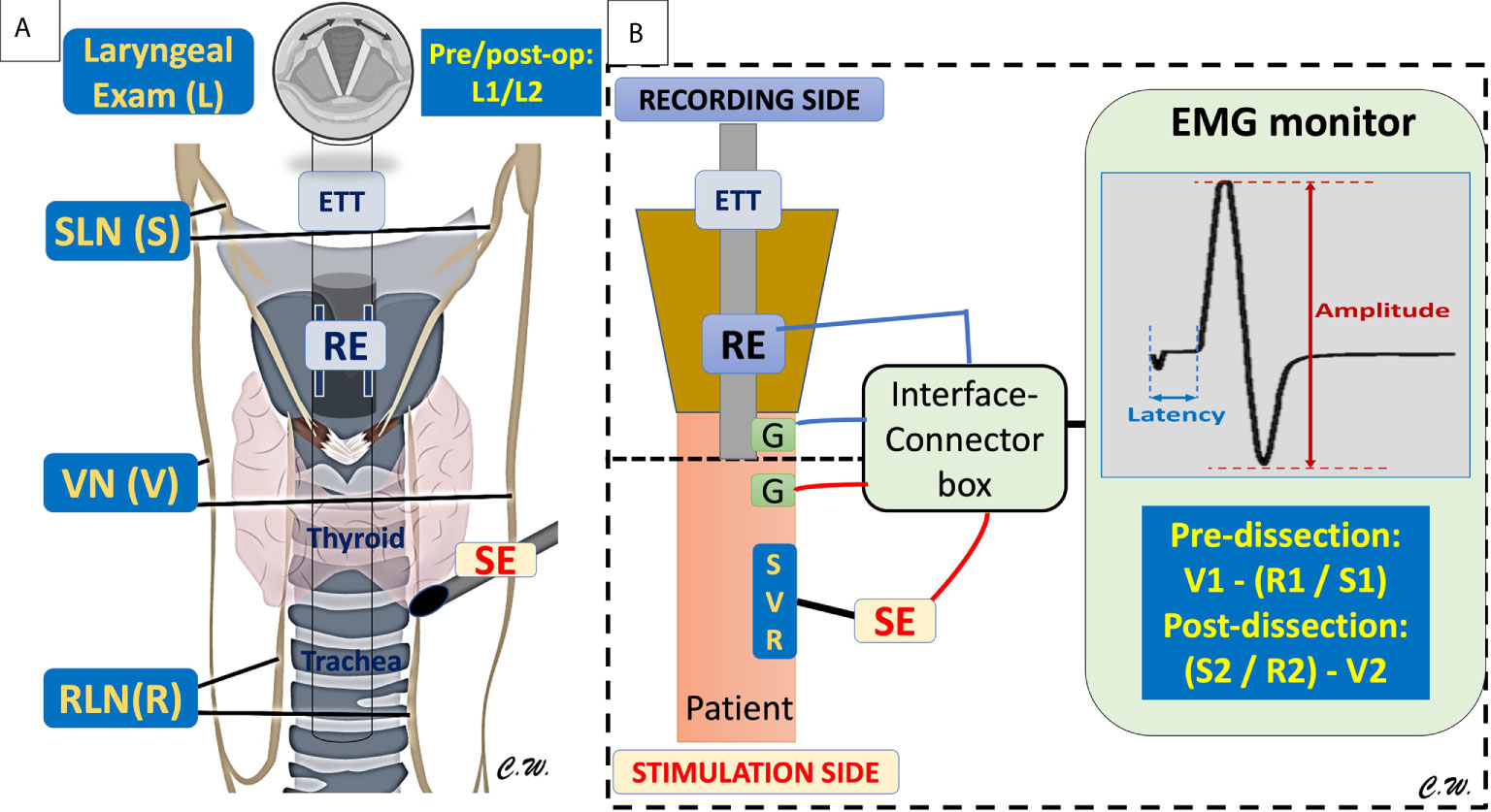
Figure 2 The Basic laryngeal nerve anatomy/electrophysiology and standard monitoring equipment setup/procedures. (A) The basic equipment included the recording electrodes (RE) connected to the endotracheal tube (ETT) to place in contact with the bilateral vocal fold, the neural stimulating electrodes (SE) to stimulate the external branch of superior laryngeal nerve (SLN)(S), the Vagus nerve (VN)(V), and the recurrent laryngeal nerve (RLN)(R) during thyroid and parathyroid surgery. The standard procedure for performing IONM should include the laryngeal examination (L) before and after surgery(L1-L2), stimulating the SLN(S) before and after upper thyroid pole dissection (S1-S2), and stimulating the VN(V) and RLN(R) before and after the dissection. (B) Standard equipment setup (Recording (RE)/Stimulation (SE) side, ground (G) electrodes, interface connector box and monitor connections. The stimulating electrode (SE) can be used for mapping, localization, and identification of the SLN (S), VN (V), and RLN (R), and the evoked laryngeal EMG waveform can be viewed on the EMG monitor screen, and the amplitude and latency changes can be monitored during surgery.
Knowledge of Common Pitfalls and Ability to Use Troubleshooting Algorithms
The course should clarify the limitations of IONM, demonstrate how to identify artifacts by applying algorithms and systematic troubleshooting procedures, foster the development of skills to optimize interaction with the anesthesiologist and manage LOS (Figure 3). It is for these reasons that a course leader have a strong foundation and sufficient experience as outlined above, as well as a clear understanding of how these limits impact surgical strategy.
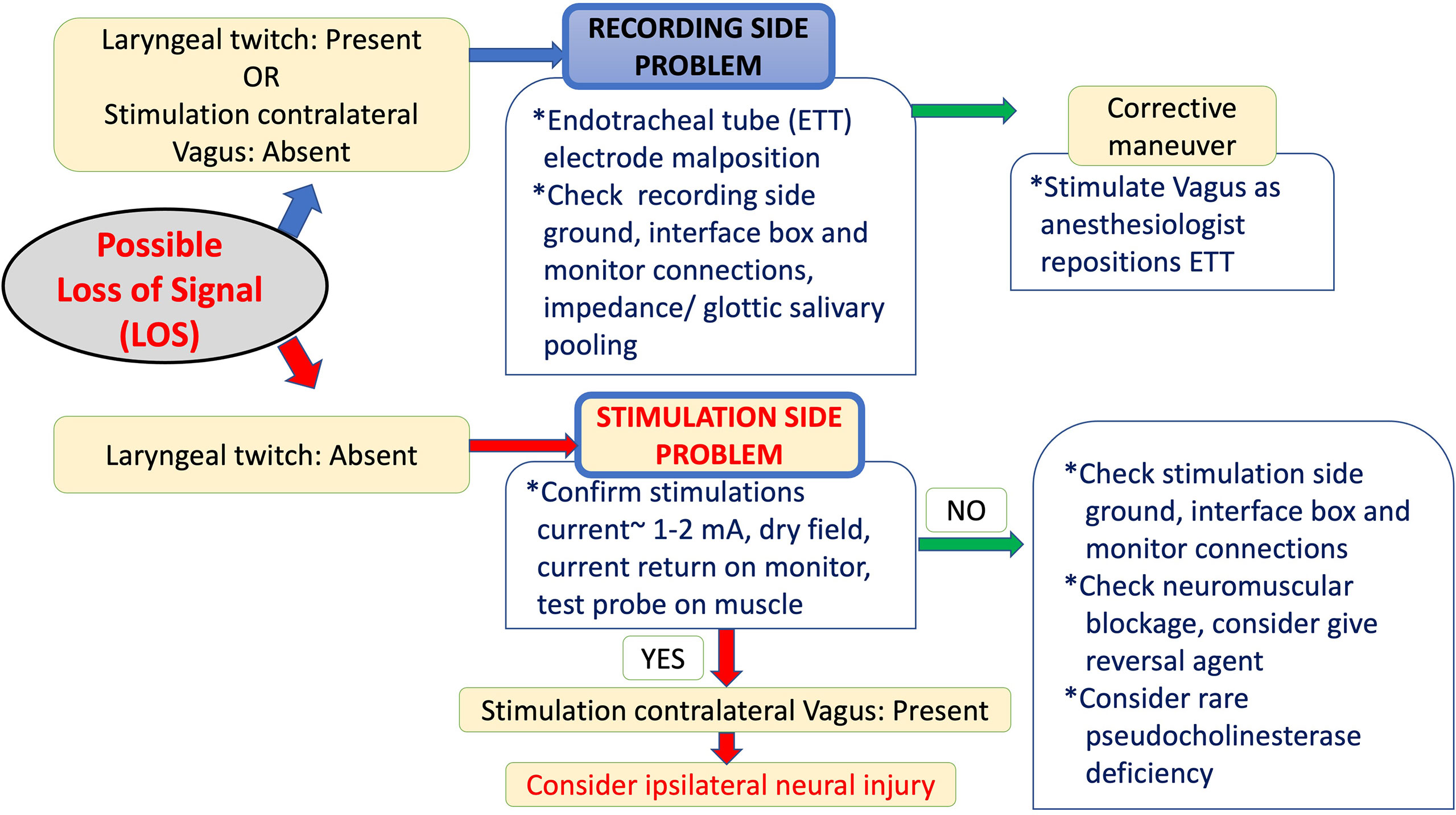
Figure 3 The International Neural Monitoring Study Group (INMSG) recommendation for loss of signal (LOS) evaluation and troubleshooting algorithms.
Adherence to IONM Guidelines
The INMSG has published guidelines (1–4) for using IONM to monitor the RLN and EBSLN in thyroid/parathyroid surgery. The INMSG has also provided guidelines for managing LOS and avoiding RLN injury. These guidelines should be discussed comprehensively in the course to train and improve the participants’ practice and maturity of autonomous IONM operations (Figure 1).
Anesthesiologist
When performing thyroid/parathyroid surgery, the surgeon shares the responsibility for implementing IONM. IONM training therefore must incorporate discussion of collaboration between the anesthesiologist and the surgeon (47, 48). The course should include an expert anesthesiologist, where possible, to provide training in maintaining optimal intraoperative communication between the anesthesiologist and the surgeon.
Basic and Advanced Courses
Courses offered by IONM training centers should include basic and advanced Courses.
Basic IONM Course
Basic course content should include basic knowledge of IONM, common errors in application, how IONM may assist in RLN identification and RLN mapping in both routine and difficult thyroid/parathyroid operations. Training should include standard IONM procedures, such as acquiring the essential dataset by “L1-V1-R1-S1-S2-R2-V2-L2” stimulation/laryngeal examination (Figure 2) and LOS evaluation and troubleshooting algorithms (Figure 3).
Advanced IONM Course
In addition to basic course content (which may be abbreviated depending on the audience), advanced course content should include C-IONM and EBSLN monitoring, quantitative and qualitative normative parameters for evaluating and interpreting EMG of the VN and RLN, and voice outcome analysis.
Course Setting and Additional Integrated Training Facilities
IONM Course Setting
The course should be delivered using modern IONM equipment and monitoring software with both audio and graphic monitoring documentation.
Live OR Demonstration
Demonstration of IONM applications in the OR may be done during live surgery or by video of live surgery. While in-person live format limits the number of attendees, it enables discussion of IONM techniques among individual participants in real time. Video format with interactive discussion is suitable for larger groups.
IONM Course Content, Implementing and Marketing
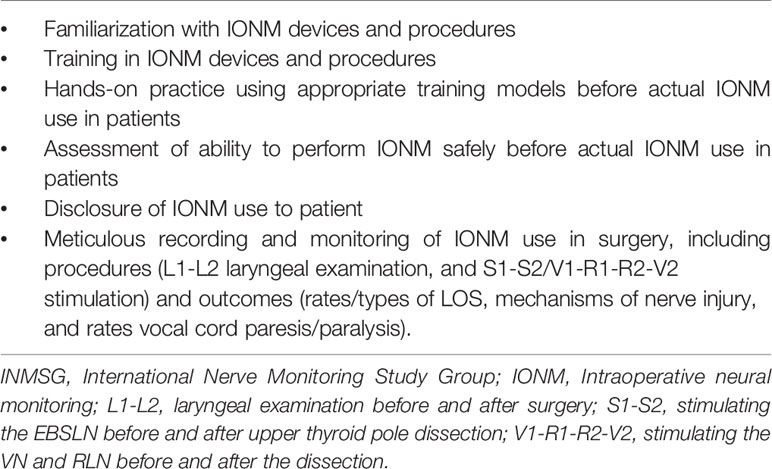
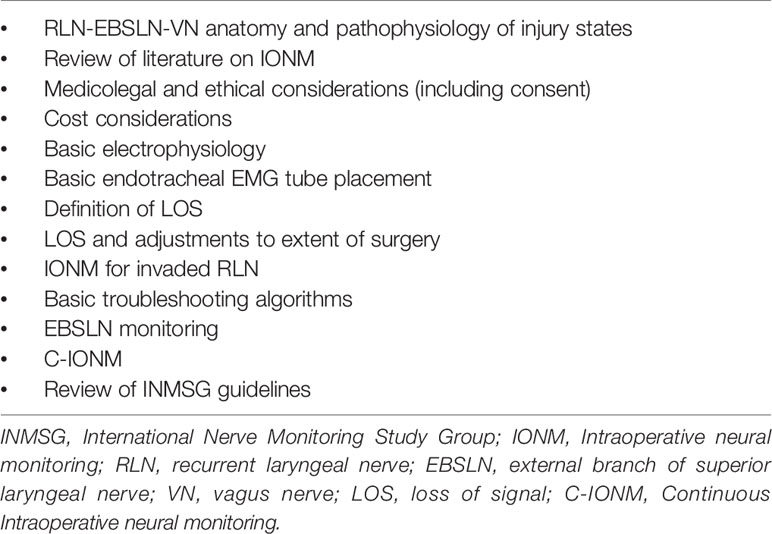
Course content should facilitate teaching both theoretical and practical skills in IONM so that participants who have completed the course should understand the fundamental steps and routine procedures (Table 1) for performing a safe IONM procedure.
Lectures on IONM in thyroid/parathyroid surgery should summarize basic knowledge in RLN anatomy and function, as well as advantages and limitations of IONM. Course learning objectives should be clearly stated to provide structure to the course and to inform participants on the content and level of the course. The optimal course content is listed in Table 2.
The Course can be marketed via the Internet, the INMSG website/member lists, the World Congress on Thyroid Cancer (WCTC), and individual medical technology companies (under the approval of and collaboration with INMSG).
Participants and Training Surgeons
Course Size
For adequate teaching efficiency, the number of participants should not exceed a number that can be accommodated optimally in the live OR. We have found that a small group of 8-10 participants enables in-depth discussion of diverse perspectives and enables an intimate experience and exchange of ideas. A small group also facilitates and encourages interaction among all participants and faculty and the development of personal relationships among the participants, which improves educational outcomes and may lead to future long-term professional collaboration.
Participants in IONM Training Courses
In recent years course participants have included surgeons with varying experience and backgrounds, including general surgery, otolaryngology-head and neck surgery, endocrine surgery, and thoracic surgery. Anesthesiologists often attend as well. Other potential participants include surgical nursing staff and IONM technicians. Participants with widely varying levels of knowledge, expertise and experience can benefit from the course, including currently practicing clinicians, residents, young surgical trainees, and medical students. The participant is recommended to select the appropriate course level (basic or advanced) however, extensive experience in IONM is not required to obtain a practical benefit from the course.
Syllabus
Course organizers should determine and make clear the expertise level at which the course is aimed. Less experienced participants may require pre-course training modules (online videos and/or required reading) in order to ensure the minimum working knowledge needed to benefit optimally from the course. The syllabus should contain information about the course program as well as pertinent recent literature on IONM. Literature summary materials may be provided to participants through an online link or on a USB flash drive. Ideally, the syllabus should be provided to participants at least one month before the course begins.
Surgical Procedures
Live Surgical Demonstration and Case Selection
Demonstration of surgical applications of IONM should be limited to thyroid/parathyroid surgery. Cases selected for demonstration in the course should be limited to routinely performed conventional thyroidectomies or routine parathyroidectomies. Patients should be selected carefully and should be limited to those with minor comorbidity to minimize risk of last minute cancellation. If possible, patients should be limited to those who previously follow-up or treated by the surgeon performing the live demonstration. Written informed consent to undergo “live” surgery for educational purposes must be obtained from the patient. A list of reserve patients should be prepared well in advance so that a replacement can be available on short notice.
Animal Models
The course leader must comply with the procedures for using experimental animal models at the animal laboratory where the course is delivered (see Actionable Recommendations).
Duration of the IONM Course
The complete course, including lectures, discussions, case studies, and/or demonstrations should ideally be designed for completion in 2 days.
Financing
Course financing should be responsibility of the institution sponsoring the course and/or an official society. Conflicts of interest of the course faculty and course sponsorship must be declared.
Feedback Method, Questionnaires, and Conclusion of the IONM Course
The Course should conclude with an interactive question-and-answer session moderated by the course leader. Feedback from participants at the conclusion of the course is important for quality control and further refinement of the course. Participants should complete a course evaluation form to document their assessments of the quality and utility of the Course and to provide feedback for future modifications and improvements in course content and/or structure. Administering a pre-/post-test can provide course directors with insight into the educational benefit of their course and how it can be improved. Participants should also complete the 37-item questionnaire developed by the INMSG for self-assessment of the benefit received from the course (Supplementary File 2).
Certificate of Attendance
Participants who successfully complete the post-test and evaluation should receive a certificate of attendance.
Actionable Recommendations
Improving Proficiency in IONM Procedures
Technology Applicable for IONM Simulation
Surgical simulation is an effective and sustainable adjunct to surgical training (49, 50). Implementation of surgical simulations in various surgical specialties has been discussed extensively, including effective designs, practical implementation issues, and analysis of simulation results (49–51). Use of surgical simulations for educational purposes is feasible in training courses and is enjoyable for trainees (52, 53). One currently available IONM simulation technology is NIM™SAM-T, a teaching and demonstration tool used to illustrate basic and advanced principles of nerve monitoring (54).
Online Courses and Outreach
The INMSG offers online training programs in accordance with recent e-learning trends. Online programs provide the capability to reach participants in widely dispersed geographic locations (without limitation to time and cost of travel), to deliver training courses under special conditions (e.g., the Covid19pandemic), to follow-up with participants, and to share IONM materials quickly and easily in various formats (e.g., videos, photographs, word/pdf processing files, presentation files, etc.). To provide IONM experts with updated knowledge of new developments, the INMSG is in the process of increasing its interaction with IONM experts through use of various communication formats and technologies, including webinars, chat applications, and internet forums/message boards.
IONM Training Courses in Animal Laboratories
In the past 20 years, INMSG has also implemented training courses in animal laboratories. Animal studies are an essential component of IONM research and are a crucial educational tool for disseminating basic IONM knowledge. Animal research has been instrumental in development of IONM standards and in the enormous advances in IONM quality in recent years (55).
Animal Models
Currently, most training programs and research use medium-sized animals for experimental models, most typically canine(dog) models (56–59) and porcine(swine/mini-pig) models (60–77). Dog models of laryngeal function and the RLN are well-established and closely mimic the anatomy, size, and physiology in humans. The porcine model was the earliest animal model used in RLN research. Its medium size enables easy handling, and experimental animals are widely available and relatively inexpensive.
Animal Course Format
Duration, Timing, and Preparation
The duration may be one half-or full day, optimally after the standard 1-to 2-day course of lectures with live surgical demonstration. Before the animal course, the instructors should briefly discuss the neck anatomy of the experimental model and the details of the procedures.
Animal Course Set Up and Purpose
Live animal surgery should include veterinarians and anesthesiologists for technical assistance in the animal preparation and anesthesia. Additionally, the protocol should be reviewed and approved in advance by the animal care and use committee of the host institution to ensure that the course complies with national/international regulations and with the 3Rs (“replacement, reduction and refinement”) principle of animal experiments (73). The main advantage of animal modeling is that, unlike human surgery, EMG correlates of RLN injury can be studied quantitatively. Therefore, for the IONM trainee, animals are useful for demonstrating the relationship between neural injury and EMG decrements (55, 64).
Animal Course Protocol
Animal Preparation/Anesthesia
During anesthesia induction and tracheal intubation, the instructors should discuss the effects of anesthetics and the principles of EMG tube placement and fixation (48, 78, 79).
Nerve Monitoring Setting
The instructors should introduce the key features of the stimulation/recording equipment, grounding electrodes, and associated connections at the interface-connector box and monitor. By the end of the course, participants should be familiar with electrode connections and stimuli/threshold settings for the monitoring system.
Nerve Preparation
Participants should learn basic IONM applications by using an I-IONM stimulation probe for mapping and localization before visual identification of target nerves, including EBSLN, RLN, and VN (34). Nerves can then be identified and exposed for the experiments.
Basic Electrophysiology Study
a. Baseline EMG Responses. Participants can learn normative EMG responses (different waveform/latencies, minimal/maximal stimulus levels, and stimulus-response relationships) by testing EMG responses in the EBSLN-RLN-VN (34, 69).
b. Stimulating Electrodes. If different I-IONM or C-IONM stimulation electrode types are available (e.g., monopolar probes, bipolar probes, stimulation probes/dissectors, and APS™ electrode), sensitivity can be tested and compared in different stimulation probes/dissectors used at different distances and in different fascia (69, 80). The procedures for APS™ vagal electrode placement and monitoring can be practiced repeatedly to enable participants to master clinical skills (73, 77).
c. Recording Electrodes. Participants can compare the effects of mispositioned or displaced EMG tubes that leads to false LOS due to rotation or upward/downward EMG tube displacement). Participants can also learn troubleshooting algorithms and corrective maneuvers for mispositioned EMG tubes (67).
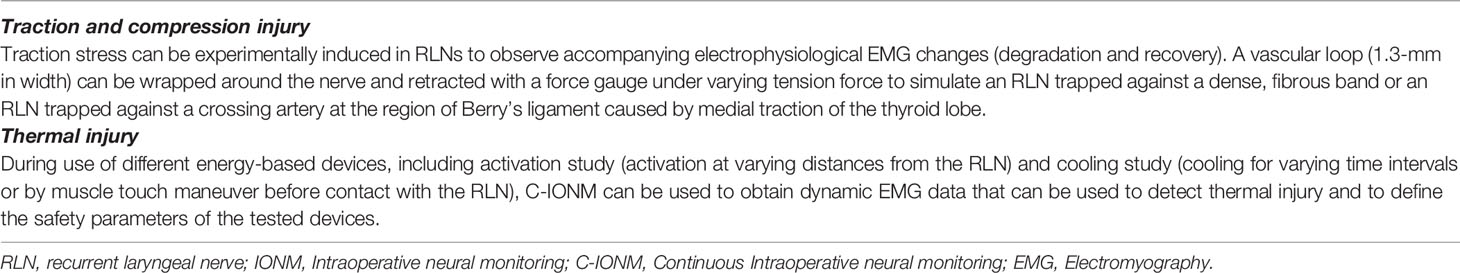
Advanced Nerve Injury Study
After completion of repeatable electrophysiology studies, participants can perform nerve injury experiments by testing the nerve segments from proximal to distal segments (e.g., caudal to cranial part of the RLN). A typical use of C-IONM is to confirm and compare patterns of change in real-time evoked laryngeal EMG signals during and after RLN injuries caused by different mechanisms [e.g., traction injuries (58, 59, 61, 64, 65) versus thermal injuries (62–64, 68, 74, 75)](Table 3). The I-IONM probe can be used to confirm and map the injury area and to compare proximal and distal EMG.
Discussion
Over the past decade, the use of IONM in thyroid and parathyroid surgery has become well established and is increasing accepted across the world. Recent data from UKRETS (13), SQRTPA (14), EUROCRINE (15) and international surveys (16) give incite into the current practices in IONM. These data show that IONM is performed by a large majority of thyroid surgeons and helps identify both the RLN anatomically and recognize injury in a higher percentage of cases than without IONM. In addition, IONM reduces the risk of RLN palsy, both temporary and permanent injury.
As IONM use in thyroid/parathyroid surgery is increasing, surgical residency programs have begun including IONM courses in their core curricula. An IONM training course aims to increase basic knowledge in IONM, including common errors in IONM application, and to increase competence in nerve identification, mapping, and functional preservation, not only in the routine management of the RLN and the EBSLN, but also in complex thyroid/parathyroid surgery. By the end of the course, participants should have practical knowledge in standard use of IONM, including positioning the endotracheal tube, interacting with the anesthesiologist, differentiating between electromyography(EMG) signals and artifacts, and applying troubleshooting algorithms. Additionally, participants should know the centrally important procedures for differentiating the key elements of technical/equipment failure in IONM from true loss of signal (LOS) during thyroid/parathyroid surgery (Figures 2, 3). This is a core IONM functionality and will guide the participants in future IONM practice and maturity (Figure 1).
The INMSG is the leading professional association in neurophysiological assessment and monitoring of laryngeal nerves in thyroid and parathyroid surgery (1–4). The group is comprised of a multidisciplinary international collection of surgeons and researchers selected according to their clinical experience and expertise in thyroid surgery, parathyroid surgery, neural monitoring, and related fields. The INMSG is dedicated to improving neurophysiologic monitoring quality and preventing laryngeal nerve injury during thyroid/parathyroid surgery and provides a forum for education and dissemination of up-to-date knowledge in the field (Table 1, Supplementary Files 1, 2). This consensus statement presents the views of the INMSG regarding the key recommendations for improving both the content and delivery of IONM surgical training and education with a goal to ensure the delivery of consistent high-quality up-to-date IONM surgical training courses from experienced leaders (Tables 2, 3). We believe this consensus statement can provide societies, course directors, teaching institutions, and national organizations with a practical reference for developing IONM training programs. The consensus statement was developed under the auspices of the INMSG and is scheduled for periodic review to enable incorporation of pertinent developments in IONM knowledge and practice. Notably, the consensus statement is intended to indicate the preferred approaches to IONM training, but not necessarily the only approaches. We suggest a training course should meet the requirements listed in this consensus statement and receive approval from the INMSG Steering Committee to qualified as an “INMSG Certified Basic IONM Course” or as an “INMSG Certified Advanced IONM Course”. Considering the dynamism and the continuous evolution in the thyroid/parathyroid surgical technigues and the IONM technologies, this expert opinion provides just outlines the essential elements and key recommendations of IONM training courses intending to stimulate further discussions among all those interested in the scientific, training, clinical, and experimental aspects of IONM and to provide some guidance and clarification for ongoing discussion.
Conclusion
This document describes the minimum training required for teaching practical application of IONM and consensus views on key issues that must be addressed for the safe and reliable introduction of IONM in surgical practice. The intent of this publication is to provide societies, course directors, teaching institutions, and national organizations with a practical reference for developing IONM training programs. With these guidelines, IONM will be implemented optimally, to the ultimate benefit of the thyroid and parathyroid surgical patients.
Author Contributions
C-WW, GR, MB, RS, F-YC, HD, and GD conceived and designed the study. Administrative support and provision of study materials were obtained by AKa, AKo, FF, and FW. Data collection, analysis and interpretation was done by T-YH and C-HL. All authors contributed to the article and approved the submitted version.
Funding
This study is supported partially by Ministry of Science and Technology grant (MOST 109-2628-B-037-014), and by Kaohsiung Municipal Siaogang Hospital/Kaohsiung Medical University Research Center grants (KMHK-DK(C)110009, I-109-04, H-109-05, I-108-02), Taiwan.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor declared a past co-authorship with one of the authors GR.
Acknowledgments
We acknowledge all members of the International Neural Monitoring Study Group (INMSG) and their collaborators for the generous and huge job.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2021.705346/full#supplementary-material
Supplementary File 1 | INMSG IONM Training Courses information and content.
Supplementary File 2 | Questionnaires for IONM Training Courses.
References
1. Randolph GW, Dralle H, Abdullah H, Barczynski M, Bellantone R, Brauckhoff M, et al. Electrophysiologic Recurrent Laryngeal Nerve Monitoring During Thyroid and Parathyroid Surgery: International Standards Guideline Statement. Laryngoscope (2011) 121 Suppl 1:S1–16. doi: 10.1002/lary.21119
2. Barczynski M, Randolph GW, Cernea CR, Dralle H, Dionigi G, Alesina PF, et al. External Branch of the Superior Laryngeal Nerve Monitoring During Thyroid and Parathyroid Surgery: International Neural Monitoring Study Group Standards Guideline Statement. Laryngoscope (2013) 123 Suppl 4:S1–14. doi: 10.1002/lary.24301
3. Schneider R, Randolph GW, Dionigi G, Wu CW, Barczynski M, Chiang FY, et al. International Neural Monitoring Study Group Guideline 2018 Part I: Staging Bilateral Thyroid Surgery With Monitoring Loss of Signal. Laryngoscope (2018)128(Suppl 3):S1–17. doi: 10.1002/lary.27359
4. Wu CW, Dionigi G, Barczynski M, Chiang FY, Dralle H, Schneider R, et al. International Neuromonitoring Study Group Guidelines 2018: Part II: Optimal Recurrent Laryngeal Nerve Management for Invasive Thyroid Cancer-Incorporation of Surgical, Laryngeal, and Neural Electrophysiologic Data. Laryngoscope (2018) 128(Suppl 3):S18–27. doi: 10.1002/lary.27360
5. Schneider R, Machens A, Lorenz K, Dralle H. Intraoperative Nerve Monitoring in Thyroid Surgery-Shifting Current Paradigms. Gland Surg (2020) 9(Suppl 2):S120–8. doi: 10.21037/gs.2019.11.04
6. Liu CH, Wang CC, Wu CW, Lin YC, Lu IC, Chang PY, et al. Comparison of Surgical Complications Rates Between LigaSure Small Jaw and Clamp-and-Tie Hemostatic Technique in 1,000 Neuro-Monitored Thyroidectomies. Front Endocrinol (Lausanne) (2021) 12:638608. doi: 10.3389/fendo.2021.638608
7. Horne SK, Gal TJ, Brennan JA. Prevalence and Patterns of Intraoperative Nerve Monitoring for Thyroidectomy. Otolaryngol Head Neck Surg (2007) 136(6):952–6. doi: 10.1016/j.otohns.2007.02.011
8. Sturgeon C, Sturgeon T, Angelos P. Neuromonitoring in Thyroid Surgery: Attitudes, Usage Patterns, and Predictors of Use Among Endocrine Surgeons. World J Surg (2009) 33(3):417–25. doi: 10.1007/s00268-008-9724-4
9. Ho Y, Carr MM, Goldenberg D. Trends in Intraoperative Neural Monitoring for Thyroid and Parathyroid Surgery Amongst Otolaryngologists and General Surgeons. Eur Arch Otorhinolaryngol (2013) 270(9):2525–30. doi: 10.1007/s00405-013-2359-6
10. Dralle H, Sekulla C, Lorenz K, Nguyen Thanh P, Schneider R, Machens A. Loss of the Nerve Monitoring Signal During Bilateral Thyroid Surgery. Br J Surg (2012) 99(8):1089–95. doi: 10.1002/bjs.8831
11. Dionigi G, Lombardi D, Lombardi CP, Carcoforo P, Boniardi M, Innaro N, et al. Intraoperative Neuromonitoring in Thyroid Surgery: A Point Prevalence Survey on Utilization, Management, and Documentation in Italy. Updates Surg (2014) 66(4):269–76. doi: 10.1007/s13304-014-0275-y
12. Zhang D, Pino A, Caruso E, Dionigi G, Sun H. Neural Monitoring in Thyroid Surgery Is Here to Stay. Gland Surg (2020) 9(Suppl 1):S43–6. doi: 10.21037/gs.2019.10.24
13. Abdelhamid A, Aspinall S. Intraoperative Nerve Monitoring in Thyroid Surgery: Analysis of United Kingdom Registry of Endocrine and Thyroid Surgery Database. Br J Surg (2021) 108(2):182–7. doi: 10.1093/bjs/znaa081
14. Bergenfelz A, Salem AF, Jacobsson H, Nordenström E, Almquist M. Risk of Recurrent Laryngeal Nerve Palsy in Patients Undergoing Thyroidectomy With and Without Intraoperative Nerve Monitoring. Br J Surg (2016) 103(13):1828–38. doi: 10.1002/bjs.10276
15. Staubitz JI, Watzka F, Poplawski A, Riss P, Clerici T, Bergenfelz A, et al. Effect of Intraoperative Nerve Monitoring on Postoperative Vocal Cord Palsy Rates After Thyroidectomy: European Multicentre Registry-Based Study. BJS Open (2020) 4(5):821–9. doi: 10.1002/bjs5.50310
16. Feng AL, Puram SV, Singer MC, Modi R, Kamani D, Randolph GW. Increased Prevalence of Neural Monitoring During Thyroidectomy: Global Surgical Survey. Laryngoscope (2020) 130(4):1097–104. doi: 10.1002/lary.28210
17. Dralle H, Sekulla C, Lorenz K, Brauckhoff M, Machens A. Intraoperative Monitoring of the Recurrent Laryngeal Nerve in Thyroid Surgery. World J Surg (2008) 32(7):1358–66. doi: 10.1007/s00268-008-9483-2
18. Schneider R, Randolph G, Dionigi G, Barczynski M, Chiang FY, Wu CW, et al. Prediction of Postoperative Vocal Fold Function After Intraoperative Recovery of Loss of Signal. Laryngoscope (2019) 129(2):525–31. doi: 10.1002/lary.27327
19. Schneider R, Randolph G, Dionigi G, Barczyński M, Chiang FY, Triponez F, et al. Prospective Study of Vocal Fold Function After Loss of the Neuromonitoring Signal in Thyroid Surgery: The International Neural Monitoring Study Group’s POLT Study. Laryngoscope (2016) 126(5):1260–6. doi: 10.1002/lary.25807
20. Musholt TJ, Clerici T, Dralle H, Frilling A, Goretzki PE, Hermann MM, et al. German Association of Endocrine Surgeons Practice Guidelines for the Surgical Treatment of Benign Thyroid Disease. Langenbecks Arch Surg (2011) 396(5):639–49. doi: 10.1007/s00423-011-0774-y
21. Barczynski M, Konturek A, Cichon S. Randomized Clinical Trial of Visualization Versus Neuromonitoring of Recurrent Laryngeal Nerves During Thyroidectomy. Br J Surg (2009) 96(3):240–6. doi: 10.1002/bjs.6417
22. Barczynski M, Konturek A, Stopa M, Honowska A, Nowak W. Randomized Controlled Trial of Visualization Versus Neuromonitoring of the External Branch of the Superior Laryngeal Nerve During Thyroidectomy. World J Surg (2012) 36(6):1340–7. doi: 10.1007/s00268-012-1547-7
23. Wang T, Kim HY, Wu CW, Rausei S, Sun H, Pergolizzi FP, et al. Analyzing Cost-Effectiveness of Neural-Monitoring in Recurrent Laryngeal Nerve Recovery Course in Thyroid Surgery. Int J Surg (2017) 48:180–8. doi: 10.1016/j.ijsu.2017.10.003
24. Dionigi G, Bacuzzi A, Boni L, Rausei S, Rovera F, Dionigi R. Visualization Versus Neuromonitoring of Recurrent Laryngeal Nerves During Thyroidectomy: What About the Costs? World J Surg (2012) 36(4):748–54. doi: 10.1007/s00268-012-1452-0
25. Dralle H, Lorenz K, Machens A. Verdicts on Malpractice Claims After Thyroid Surgery: Emerging Trends and Future Directions. Head Neck (2012) 34(11):1591–6. doi: 10.1002/hed.21970
26. Angelos P. Ethical and Medicolegal Issues in Neuromonitoring During Thyroid and Parathyroid Surgery: A Review of the Recent Literature. Curr Opin Oncol (2012) 24(1):16–21. doi: 10.1097/CCO.0b013e32834cd596
27. Angelos P. Recurrent Laryngeal Nerve Monitoring: State of the Art, Ethical and Legal Issues. Surg Clin North Am (2009) 89(5):1157–69. doi: 10.1016/j.suc.2009.06.010
28. Wu CW, Dionigi G, Chen HC, Chen HY, Lee KW, Lu IC, et al. Vagal Nerve Stimulation Without Dissecting the Carotid Sheath During Intraoperative Neuromonitoring of the Recurrent Laryngeal Nerve in Thyroid Surgery. Head Neck (2013) 35(10):1443–7. doi: 10.1002/hed.23154
29. Chiang FY, Lee KW, Chen HC, Chen HY, Lu IC, Kuo WR, et al. Standardization of Intraoperative Neuromonitoring of Recurrent Laryngeal Nerve in Thyroid Operation. World J Surg (2010) 34(2):223–9. doi: 10.1007/s00268-009-0316-8
30. Iwata AJ, Liddy W, Barczyński M, Wu CW, Huang TY, Van Slycke S, et al. Superior Laryngeal Nerve Signal Attenuation Influences Voice Outcomes in Thyroid Surgery. Laryngoscope (2021) 131(6):1436–42. doi: 10.1002/lary.29413
31. Fundakowski CE, Hales NW, Agrawal N, Barczynski M, Camacho PM, Hartl DM, et al. Surgical Management of the Recurrent Laryngeal Nerve in Thyroidectomy: American Head and Neck Society Consensus Statement. Head Neck (2018) 40(4):663–75. doi: 10.1002/hed.24928
32. Dionigi G, Kim HY, Randolph GW, Wu CW, Sun H, Liu X, et al. Prospective Validation Study of Cernea Classification for Predicting EMG Alterations of the External Branch of the Superior Laryngeal Nerve. Surg Today (2016) 46(7):785–91. doi: 10.1007/s00595-015-1245-9
33. Ferrari CC, Rausei S, Amico F, Boni L, Chiang FY, Wu CW, et al. Recurrent Laryngeal Nerve Injury in Thyroid Surgery: Clinical Pathways and Resources Consumption. Head Neck (2016) 38(11):1657–65. doi: 10.1002/hed.24489
34. Liddy W, Barber SR, Cinquepalmi M, Lin BM, Patricio S, Kyriazidis N, et al. The Electrophysiology of Thyroid Surgery: Electrophysiologic and Muscular Responses With Stimulation of the Vagus Nerve, Recurrent Laryngeal Nerve, and External Branch of the Superior Laryngeal Nerve. Laryngoscope (2017) 127(3):764–71. doi: 10.1002/lary.26147
35. Schneider R, Machens A, Randolph G, Kamani D, Lorenz K, Dralle H. Impact of Continuous Intraoperative Vagus Stimulation on Intraoperative Decision Making in Favor of or Against Bilateral Surgery in Benign Goiter. Best Pract Res Clin Endocrinol Metab (2019) 33(4):101285. doi: 10.1016/j.beem.2019.06.001
36. Phelan E, Schneider R, Lorenz K, Dralle H, Kamani D, Potenza A, et al. Continuous Vagal IONM Prevents Recurrent Laryngeal Nerve Paralysis by Revealing Initial EMG Changes of Impending Neuropraxic Injury: A Prospective, Multicenter Study. Laryngoscope (2014) 124(6):1498–505. doi: 10.1002/lary.24550
37. Schneider R, Randolph GW, Sekulla C, Phelan E, Thanh PN, Bucher M, et al. Continuous Intraoperative Vagus Nerve Stimulation for Identification of Imminent Recurrent Laryngeal Nerve Injury. Head Neck (2013) 35(11):1591–8. doi: 10.1002/hed.23187
38. Schneider R, Machens A, Sekulla C, Lorenz K, Elwerr M, Dralle H. Superiority of Continuous Over Intermittent Intraoperative Nerve Monitoring in Preventing Vocal Cord Palsy. Br J Surg (2020) 108(5):566–73. doi: 10.1002/bjs.11901
39. Sun H, Carcoforo P, Dionigi G. Prerequisites for Introducing Neural Monitoring in Thyroid Surgery. Eur Ann Otorhinolaryngol Head Neck Dis (2020) 137(1):91. doi: 10.1016/j.anorl.2018.05.015
40. Dionigi G, Bacuzzi A, Barczynski M, Biondi A, Boni L, Chiang FY, et al. Implementation of Systematic Neuromonitoring Training for Thyroid Surgery. Updates Surg (2011) 63(3):201–7. doi: 10.1007/s13304-011-0098-z
41. Lerner HP. SAGES Guidelines for the Introduction of New Technology and Techniques. Surg Endosc (2014) 28(8):2255–6. doi: 10.1007/s00464-014-3641-4
42. Perrier ND, Randolph GW, Inabnet WB, Marple BF, VanHeerden J, Kuppersmith RB. Robotic Thyroidectomy: A Framework for New Technology Assessment and Safe Implementation. Thyroid (2010) 20(12):1327–32. doi: 10.1089/thy.2010.1666
43. Duclos A, Lifante JC, Ducarroz S, Soardo P, Colin C, Peix JL. Influence of Intraoperative Neuromonitoring on Surgeons’ Technique During Thyroidectomy. World J Surg (2011) 35(4):773–8. doi: 10.1007/s00268-011-0963-4
44. Wojtczak B, Sutkowski K, Kaliszewski K, Głód M, Barczyński M. Experience With Intraoperative Neuromonitoring of the Recurrent Laryngeal Nerve Improves Surgical Skills and Outcomes of Non-Monitored Thyroidectomy. Langenbecks Arch Surg (2017) 402(4):709–17. doi: 10.1007/s00423-016-1449-5
45. Musholt TJ, Bränström R, Kaderli RM, Pérez NM, Raffaelli M, Stechman MJ. Accreditation of Endocrine Surgery Units. Langenbecks Arch Surg (2019) 404(7):779–93. doi: 10.1007/s00423-019-01820-y
46. Lorenz K, Raffaeli M, Barczyński M, Lorente-Poch L, Sancho J. Volume, Outcomes, and Quality Standards in Thyroid Surgery: An Evidence-Based Analysis-European Society of Endocrine Surgeons (ESES) Positional Statement. Langenbecks Arch Surg (2020) 405(4):401–25. doi: 10.1007/s00423-020-01907-x
47. Macias AA, Eappen S, Malikin I, Goldfarb J, Kujawa S, Konowitz PM, et al. Successful Intraoperative Electrophysiologic Monitoring of the Recurrent Laryngeal Nerve, A Multidisciplinary Approach: The Massachusetts Eye and Ear Infirmary Monitoring Collaborative Protocol With Experience in Over 3000 Cases. Head Neck (2016) 38(10):1487–94. doi: 10.1002/hed.24468
48. Lu IC, Lin IH, Wu CW, Chen HY, Lin YC, Chiang FY, et al. Preoperative, Intraoperative and Postoperative Anesthetic Prospective for Thyroid Surgery: What’s New. Gland Surg (2017) 6(5):469–75. doi: 10.21037/gs.2017.05.02
49. Reznick RK, MacRae H. Teaching Surgical Skills–Changes in the Wind. N Engl J Med (2006) 355(25):2664–9. doi: 10.1056/NEJMra054785
50. Gardner AK, Scott DJ, Pedowitz RA, Sweet RM, Feins RH, Deutsch ES, et al. Best Practices Across Surgical Specialties Relating to Simulation-Based Training. Surgery (2015) 158(5):1395–402. doi: 10.1016/j.surg.2015.03.041
51. Razavi CR, Tanavde V, Shaear M, Richmon JD, Russell JO. Simulations and Simulators in Head and Neck Endocrine Surgery. Ann Thyroid (2020) 5(3):1–6. doi: 10.21037/aot.2020.03.03
52. Pandian T, Khatib MME, Abdelsattar JM, Farley DR. Simulation for Endocrine Surgery Training: A Call to Action. Int J Endocr Oncol (2016) 3(2):109–14. doi: 10.2217/ije-2016-0003
53. Biffl WL, Spain DA, Reitsma AM, Minter RM, Upperman J, Wilson M, et al. Responsible Development and Application of Surgical Innovations: A Position Statement of the Society of University Surgeons. J Am Coll Surg (2008) 206(6):1204–9. doi: 10.1016/j.jamcollsurg.2008.02.011
54. Sun H, Wu CW, Zhang D, Makay Ö, Zhao Y, Carcofaro P, et al. New Paradigms for Neural Monitoring in Thyroid Surgery. Surg Technol Int (2019) 34:79–86.
55. Wu C-W, Randolph GW, Lu I-C, Chang P-Y, Chen Y-T, Hun P-C, et al. Intraoperative Neural Monitoring in Thyroid Surgery: Lessons Learned From Animal Studies. Gland Surg (2016) 5(5):473–80. doi: 10.21037/gs.2016.09.06
56. Scott AR, Chong PS, Brigger MT, Randolph GW, Hartnick CJ. Serial Electromyography of the Thyroarytenoid Muscles Using the NIM-Response System in a Canine Model of Vocal Fold Paralysis. Ann Otol Rhinol Laryngol (2009) 118(1):56–66. doi: 10.1177/000348940911800110
57. Scott AR, Chong PS, Hartnick CJ, Randolph GW. Spontaneous and Evoked Laryngeal Electromyography of the Thyroarytenoid Muscles: A Canine Model for Intraoperative Recurrent Laryngeal Nerve Monitoring. Ann Otol Rhinol Laryngol (2010) 119(1):54–63. doi: 10.1177/000348941011900111
58. Puram SV, Chow H, Wu CW, Heaton JT, Kamani D, Gorti G, et al. Posterior Cricoarytenoid Muscle Electrophysiologic Changes Are Predictive of Vocal Cord Paralysis With Recurrent Laryngeal Nerve Compressive Injury in a Canine Model. Laryngoscope (2016) 126(12):2744–51. doi: 10.1002/lary.25967
59. Puram SV, Chow H, Wu CW, Heaton JT, Kamani D, Gorti G, et al. Vocal Cord Paralysis Predicted by Neural Monitoring Electrophysiologic Changes With Recurrent Laryngeal Nerve Compressive Neuropraxic Injury in a Canine Model. Head Neck (2016) 38(Suppl 1):E1341–50. doi: 10.1002/hed.24225
60. Wu CW, Lu IC, Randolph GW, Kuo WR, Lee KW, Chen CL, et al. Investigation of Optimal Intensity and Safety of Electrical Nerve Stimulation During Intraoperative Neuromonitoring of the Recurrent Laryngeal Nerve: A Prospective Porcine Model. Head Neck (2010) 32(10):1295–301. doi: 10.1002/hed.21324
61. Wu CW, Dionigi G, Sun H, Liu X, Kim HY, Hsiao PJ, et al. Intraoperative Neuromonitoring for the Early Detection and Prevention of RLN Traction Injury in Thyroid Surgery: A Porcine Model. Surgery (2014) 155(2):329–39. doi: 10.1016/j.surg.2013.08.015
62. Lin YC, Dionigi G, Randolph GW, Lu IC, Chang PY, Tsai SY, et al. Electrophysiologic Monitoring Correlates of Recurrent Laryngeal Nerve Heat Thermal Injury in a Porcine Model. Laryngoscope (2015) 125(8):E283–90. doi: 10.1002/lary.25362
63. Wu CW, Chai YJ, Dionigi G, Chiang FY, Liu X, Sun H, et al. Recurrent Laryngeal Nerve Safety Parameters of the Harmonic Focus During Thyroid Surgery: Porcine Model Using Continuous Monitoring. Laryngoscope (2015) 125(12):2838–45. doi: 10.1002/lary.25412
64. Dionigi G, Wu CW, Kim HY, Rausei S, Boni L, Chiang FY. Severity of Recurrent Laryngeal Nerve Injuries in Thyroid Surgery. World J Surg (2016) 40(6):1373–81. doi: 10.1007/s00268-016-3415-3
65. Lee HY, Cho YG, You JY, Choi BH, Kim JY, Wu CW, et al. Traction Injury of the Recurrent Laryngeal Nerve: Results of Continuous Intraoperative Neuromonitoring in a Swine Model. Head Neck (2016) 38(4):582–8. doi: 10.1002/hed.23934
66. Lu IC, Wu CW, Chang PY, Chen HY, Tseng KY, Randolph GW, et al. Reversal of Rocuronium-Induced Neuromuscular Blockade by Sugammadex Allows for Optimization of Neural Monitoring of the Recurrent Laryngeal Nerve. Laryngoscope (2016) 126(4):1014–9. doi: 10.1002/lary.25577
67. Kim HY, Tufano RP, Randolph G, Barczynski M, Wu CW, Chiang FY, et al. Impact of Positional Changes in Neural Monitoring Endotracheal Tube on Amplitude and Latency of Electromyographic Response in Monitored Thyroid Surgery: Results From the Porcine Experiment. Head Neck (2016) 38 Suppl 1:E1004–8. doi: 10.1002/hed.24145
68. Dionigi G, Chiang FY, Kim HY, Randolph GW, Mangano A, Chang PY, et al. Safety of LigaSure in Recurrent Laryngeal Nerve Dissection-Porcine Model Using Continuous Monitoring. Laryngoscope (2017) 127(7):1724–9. doi: 10.1002/lary.26271
69. Wu CW, Liu X, Barczynski M, Kim HY, Dionigi G, Sun H, et al. Optimal Stimulation During Monitored Thyroid Surgery: EMG Response Characteristics in a Porcine Model. Laryngoscope (2017) 127(4):998–1005. doi: 10.1002/lary.26141
70. Lu IC, Chang PY, Randolph GW, Chen HY, Tseng KY, Lin YC, et al. Safety of High-Current Stimulation for Intermittent Intraoperative Neural Monitoring in Thyroid Surgery: A Porcine Model. Laryngoscope (2018) 128(9):2206–12. doi: 10.1002/lary.27086
71. Wu CW, Chiang FY, Randolph GW, Dionigi G, Kim HY, Lin YC, et al. Feasibility of Intraoperative Neuromonitoring During Thyroid Surgery Using Transcartilage Surface Recording Electrodes. Thyroid (2018) 28(11):1508–16. doi: 10.1089/thy.2017.0680
72. Wu CW, Chiang FY, Randolph GW, Dionigi G, Kim HY, Lin YC, et al. Transcutaneous Recording During Intraoperative Neuromonitoring in Thyroid Surgery. Thyroid (2018) 28(11):1500–7. doi: 10.1089/thy.2017.0679
73. Wu CW, Huang TY, Chen HC, Chen HY, Tsai TY, Chang PY, et al. Intra-Operative Neural Monitoring of Thyroid Surgery in a Porcine Model. J Vis Exp (2019) 11(144):1–12. doi: 10.3791/57919
74. Huang TY, Lin YC, Tseng HY, Dionigi G, Kim HY, Chai YJ, et al. Safety Parameters of Ferromagnetic Device During Thyroid Surgery: Porcine Model Using Continuous Neuromonitoring. Head Neck (2020) 42(10):2931–40. doi: 10.1002/hed.26334
75. Huang TY, Lin YC, Tseng HY, Dionigi G, Kim HY, Lu IC, et al. Safety of Ligasure Exact Dissector in Thyroidectomy With Continuous Neuromonitoring: A Porcine Model. Gland Surg (2020) 9(3):702–10. doi: 10.21037/gs.2020.03.17
76. Huang TY, Lin YC, Tseng HY, Kim HY, Dionigi G, Lu IC, et al. Full Percutaneous Intraoperative Neuromonitoring Technique in Remote Thyroid Surgery: Porcine Model Feasibility Study. Head Neck (2021) 43(2):505–13. doi: 10.1002/hed.26500
77. Wang T, Dionigi G, Zhao Y, Zhang D, Pino A, Dralle H, et al. Tensile Strength Analysis of Automatic Periodic Stimulation for Continuous Intraoperative Neural Monitoring in a Piglet Model. Sci Rep (2021) 11(1):5898. doi: 10.1038/s41598-021-84988-y
78. Lu IC, Chu KS, Tsai CJ, Wu CW, Kuo WR, Chen HY, et al. Optimal Depth of NIM EMG Endotracheal Tube for Intraoperative Neuromonitoring of the Recurrent Laryngeal Nerve During Thyroidectomy. World J Surg (2008) 32(9):1935–9. doi: 10.1007/s00268-008-9549-1
79. Lu IC, Wu SH, Wu CW. Neuromuscular Blockade Management for Intraoperative Neural Monitoring. Kaohsiung J Med Sci (2020) 36(4):230–5. doi: 10.1002/kjm2.12153
Keywords: intraoperative neural monitoring, vocal cord paralysis, vagus nerve, recurrent laryngeal nerve, external branch of superior laryngeal nerve, training courses, parathyroid surgery, thyroid surgery
Citation: Wu C-W, Randolph GW, Barczyński M, Schneider R, Chiang F-Y, Huang T-Y, Karcioglu AS, Konturek A, Frattini F, Weber F, Liu C-H, Dralle H and Dionigi G (2021) Training Courses in Laryngeal Nerve Monitoring in Thyroid and Parathyroid Surgery- The INMSG Consensus Statement. Front. Endocrinol. 12:705346. doi: 10.3389/fendo.2021.705346
Received: 05 May 2021; Accepted: 26 May 2021;
Published: 18 June 2021.
Edited by:
Laura Boucai, Memorial Sloan Kettering Cancer Center, United StatesReviewed by:
Ian Ganly, Memorial Sloan Kettering Cancer Center, United StatesStan Sidhu, Royal North Shore Hospital, Australia
Copyright © 2021 Wu, Randolph, Barczyński, Schneider, Chiang, Huang, Karcioglu, Konturek, Frattini, Weber, Liu, Dralle and Dionigi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gianlorenzo Dionigi, Z2lhbmxvcmVuem8uZGlvbmlnaUB1bmltZS5pdA==
 Che-Wei Wu
Che-Wei Wu Gregory W. Randolph
Gregory W. Randolph Marcin Barczyński
Marcin Barczyński Rick Schneider7
Rick Schneider7 Tzu-Yen Huang
Tzu-Yen Huang Aleksander Konturek
Aleksander Konturek Frank Weber
Frank Weber Cheng-Hsin Liu
Cheng-Hsin Liu Gianlorenzo Dionigi
Gianlorenzo Dionigi