- 1Department of Orthopedics, Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 2Beijing Bo’ai Hospital China Rehabilitation Research Center, School of Rehabilitation, Capital Medical University, Beijing, China
- 3Department of Rehabilitation, Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 4Department of Orthopedics, Yibin Hospital of Traditional Chinese Medicine, Yibin, Sichuan, China
- 5Department of Rehabilitation, The First People’s Hospital of Longquanyi District, Chengdu, China
- 6Traditional Chinese Medicine (TCM) Preventive Medical Center, Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, China
Introduction: Worldwide, there is a high frequency of chronic non-specific low back pain (CNLBP), which is a significant public health concern. The etiology is complicated and diverse, and it includes a number of risk factors such as diminished stability and weak core muscles. Mawangdui-Guidance Qigong has been employed extensively to bolster the body in China for countless years. However, the effectiveness of treating CNLBP has not been assessed by a randomized controlled trial (RCT). In order to verify the results of the Mawangdui-Guidance Qigong Exercise and examine its biomechanical mechanism, we intend to perform a randomized controlled trial.
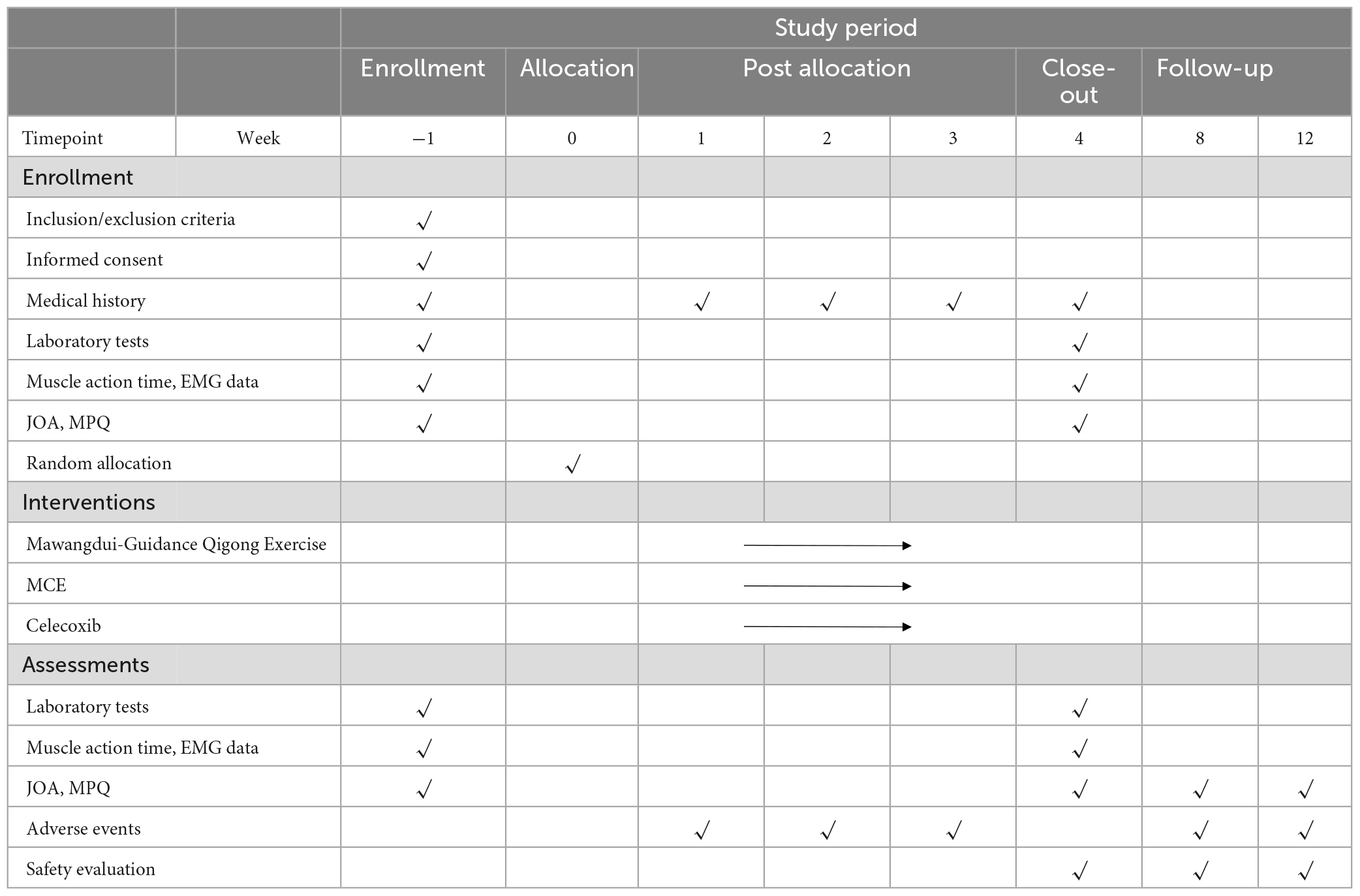
Methods and analysis: Over the course of 4 weeks, 84 individuals with CNLBP will be randomly assigned to receive either Mawangdui-Guidance Qigong Exercise, motor control exercise, or medication (celecoxib). Electromyographic data, including muscle activation time, iEMGs, root mean square value (RMS) and median frequency (MF), will be the main outcomes. The Japanese Orthopedic Association (JOA) Score, the Mcgill Pain Questionnaire (MPQ), beta-endorphin, and substance P are examples of secondary outcomes. At the start of treatment and 4 weeks later, all outcomes will be evaluated. SPSS version 20.0 (SPSS Inc., Chicago, IL, USA) will be used for all of the analysis.
Discussion: The prospective findings are anticipated to offer an alternative treatment for CNLBP and provide a possible explanation of the mechanism of Mawangdui-Guidance Qigong Exercise on CNLBP.
Ethics and dissemination: The Sichuan Regional Ethics Review Committee on Traditional Chinese Medicine has given the study approval (Approval No. 2020KL-067). It has also registered at the website of China Clinical Trial Center Registration. The application adheres to the Declaration of Helsinki’s tenets (Version Edinburgh 2000). Peer-reviewed papers will be used to publicize the trial’s findings.
Trial registration number: ClinicalTrials.gov, identifier ChiCTR2000041080.
Strengths and weaknesses of this research
1. The purpose of this study protocol is to conduct the first-ever single-blinded, randomized controlled trial to assess the effectiveness and potential mechanism of Mawangdui-Guidance Qigong Exercise for CNLBP.
2. Biological markers and EMG data are included in the primary and secondary outcomes. There has been no agreement achieved despite numerous EMG investigations that attempted to disclose the CNLBP with muscle activity sequence mechanism. Beta-endorphin levels and substance P, which are quick, safe, and effective markers to gauge pain relief will be tested.
3. Participants are limited by ages between 20 and 39 for easily identification of specific chronic LBP or CNLBP, further researches on differences of various ages are needed.
4. This is a single-center RCT with limited sample size, multi-center experiments can be conducted to get reproducible and stable results in the future.
5. The treatment duration keeps 4 weeks without longer-term observation, we plan to conduct a follow-up at the 8th and 12th weeks by phone after the trial finished.
Introduction
Pain between the costal margin and inferior gluteal fold is known as low back pain (LBP). Chronic non-specific low back pain (CNLBP) is defined as LBP for at least 12 weeks, which is not caused by a specific pathology such as a tumor, infection, fracture, structural deformity, radiculopathy, osteoporosis, inflammatory disorder, or cauda equina syndrome (Furlan et al., 2009). The literature reports a wide range of estimated prevalence rates for CNLBP, ranging from 4 to 14% (Parthan et al., 2006; van Tulder et al., 2006; Chou et al., 2007). One of the most prevalent musculoskeletal conditions in the world today is CNLBP (Maher et al., 2017). Effective therapies from drugs to surgery for CNLBP are widely used (Ma et al., 2019). NSAIDs, such as Celecoxib and other COX-2 inhibitors are frequently advised for the treatment of CNLBP (Birbara et al., 2003; Katz et al., 2003; Pallay et al., 2004; Airaksinen et al., 2006). The effectiveness of exercise therapy in CNLBP, including pilates, Tai Chi, yoga, and motor control exercise (MCE), has received greater attention in recent years (van Middelkoop et al., 2011; Holtzman and Beggs, 2013; Macedo et al., 2013; Eliks et al., 2019). For the treatment of persistent, nonspecific LBP, exercise therapy has been utilized extensively (Saragiotto et al., 2016).
Mawangdui-Guidance Qigong Exercise is an arising exercise therapy organized and created by the Fitness Qigong Management Center of the State General Administration of Sport of China (Fan, 2002). Traditional Chinese exercises, including Qigong and Tai Chi, are recommended to relieve pain intensity in patients with LBP (Zhang et al., 2019). Qigong may achieve the same efficacy as other exercise therapies in the treatment of CNLBP (Blödt et al., 2015). The pain intensity and back dysfunction are significantly regulated for people who practice Qigong (Phattharasupharerk et al., 2019), and it is safe in the treatment of musculoskeletal pain (Marks, 2019).
In order to assess internal and external postural interference in patients with LBP, the quick arm raise test and the falling ball test by surface electromyograph (sEMG) are frequently utilized (Hodges and Richardson, 1996; Tsao and Hodges, 2008; Jacobs et al., 2017; Xie and Wang, 2019; Larivière and Preuss, 2021; Yu et al., 2021). Although no consensus was established, numerous EMG studies attempted to shed light on the CNLBP with muscle activity sequence mechanism (Geisser et al., 2005; Marshall and Murphy, 2008; Falla and Hodges, 2017). The influence of adjusting posture on pain reduction and disability improvement may be observed by using EMG to examine the changes in muscle initiation time and iEMGs in patients with CNLBP (Yu et al., 2021). The management of spinal postural alignment and overall body balance are thought to depend mostly on the back muscles (Daggfeldt and Thorstensson, 2003; Christophy et al., 2012). The Chinese Association for the Study of Pain (Ma et al., 2019) advises sEMG y as an objective method of assessing the back muscles’ functionality (Akbari et al., 2015).
There is not enough solid evidence to support the high efficacy of Qigong when compared to other various nonoperative treatments. Mawangdui-Guidance Qigong Exercise has not been subjected to a randomized controlled trial (RCT) to determine the effectiveness in treating CNLBP. We strive to confirm the critical function in treating chronic CNLBP by contrasting Mawangdui-Guidance Qigong Exercise with MCE and medication.
Methods and design
Study design
This study is a randomized, single-blinded clinical trial to investigate the effectiveness of Mawangdui-Guidance Qigong Exercise for CNLBP. This study will be conducted at the Hospital of Chengdu University of Traditional Chinese Medicine (CDUTCM). For the duration of the 4-week course of therapy, 84 participants who meet the trial criteria will be assigned at random to the Mawangdui-Guidance Qigong Exercise group, the MCE group, or the medicine group. Participants in Qigong group and MCE group will receive different types of exercise therapies under the supervision of different professional coaches. Others in the medicine group will be given celecoxib orally on a regular basis. EMG data, including muscle activation time, iEMGs, root mean square value (RMS) and median frequency (MF), will be the main outcomes. The Japanese Orthopedic Association (JOA) Score, the Mcgill Pain Questionnaire (MPQ), beta-endorphin, and substance P will be the secondary outcomes. All outcomes will be evaluated at the start of treatment and 4 weeks later. We think Mawangdui-Guidance Qigong Exercise can produce an improvement in pain and lumbar function that is equal to or greater than what the other two groups can.
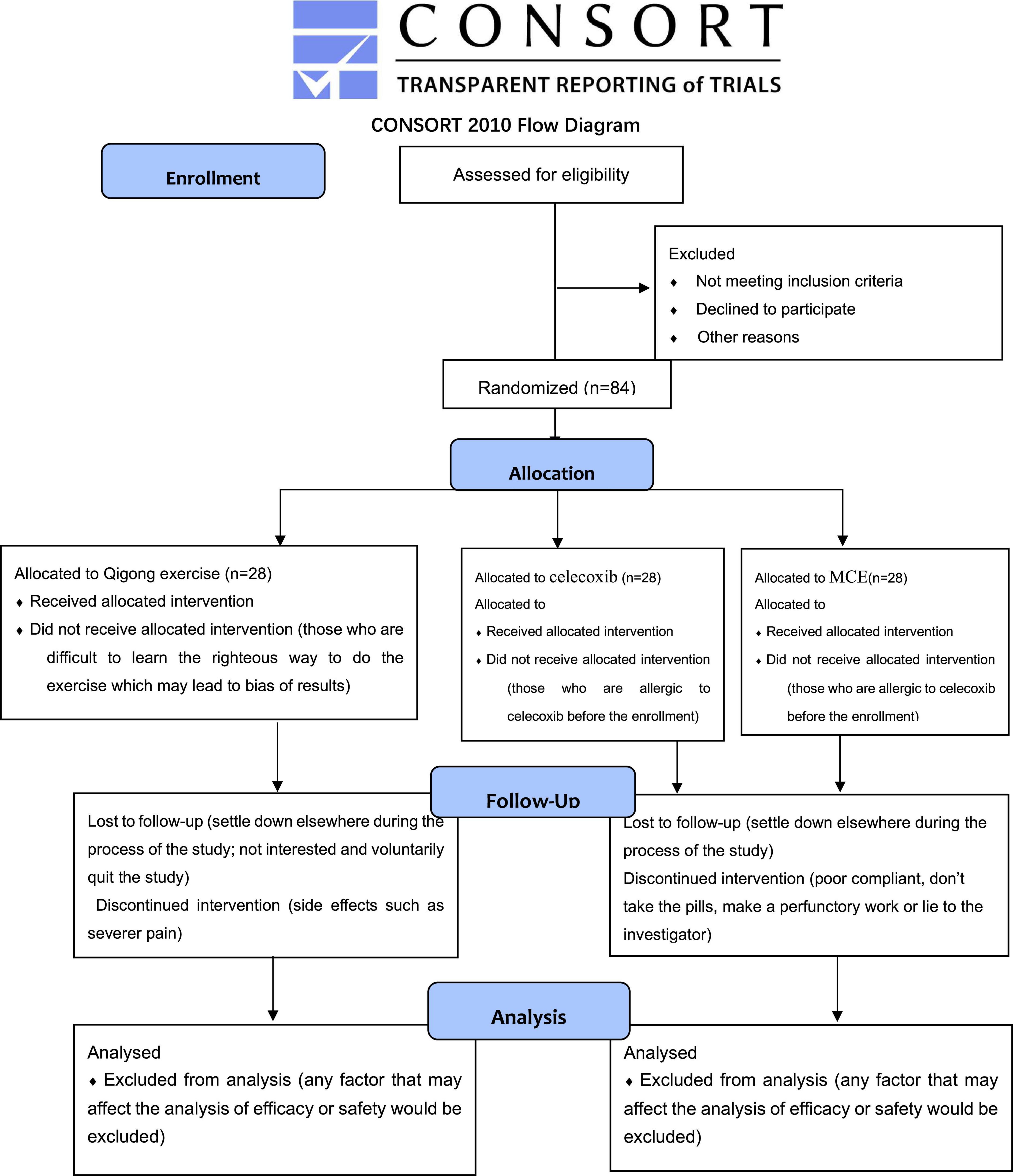
The study is approved by the Sichuan Regional Ethics Review Committee on Traditional Chinese Medicine (Approval No. 2020KL-067) and registered with China Clinical Trial Center Registration (ChiCTR2000041080). The implementation follows the principles of the Declaration of Helsinki (Version Edinburgh 2000). The SPIRIT guidelines and CONSORT flow diagram will be followed in this investigation. The whole study design will be illustrated as a flow chart in Figure 1 and the process timetable will be shown in Table 1.
Inclusion criteria
Eligible participants who met the following criteria will be included: (i) pain between the costal margin and inferior gluteal fold for at least 12 weeks which is not caused by a specific pathology, (ii) age between 20 and 39 years old, (iii) never received drug treatment, non-pharmacy, or surgical treatments for CNLBP during the previous 12 weeks, and (iv) agree to join the study and sign the written informed consent.
Exclusion criteria
Participants matching any of the following criteria will be excluded: (i) LBP with a specific diagnosis such as lumbar disc herniation, fracture of lumbar vertebra, spinal stenosis, severe osteoarthritis, or ankylosing spondylitis, (ii) be suffering from serious diseases of the heart, liver, kidney, or other organs, (iii) pregnant women, tumor patients, or those with serious disorders, (iv) structural deformity of the lumbar spine, (v) be suffering from other diseases that cause pain, such as migraine, angina, etc., and (vi) patients received surgery, acupuncture, massage, Tuina, spinal manipulation, and NSAIDs treatment in the past 12 weeks.
Interventions
Mawangdui-Guidance Qigong Exercise therapy
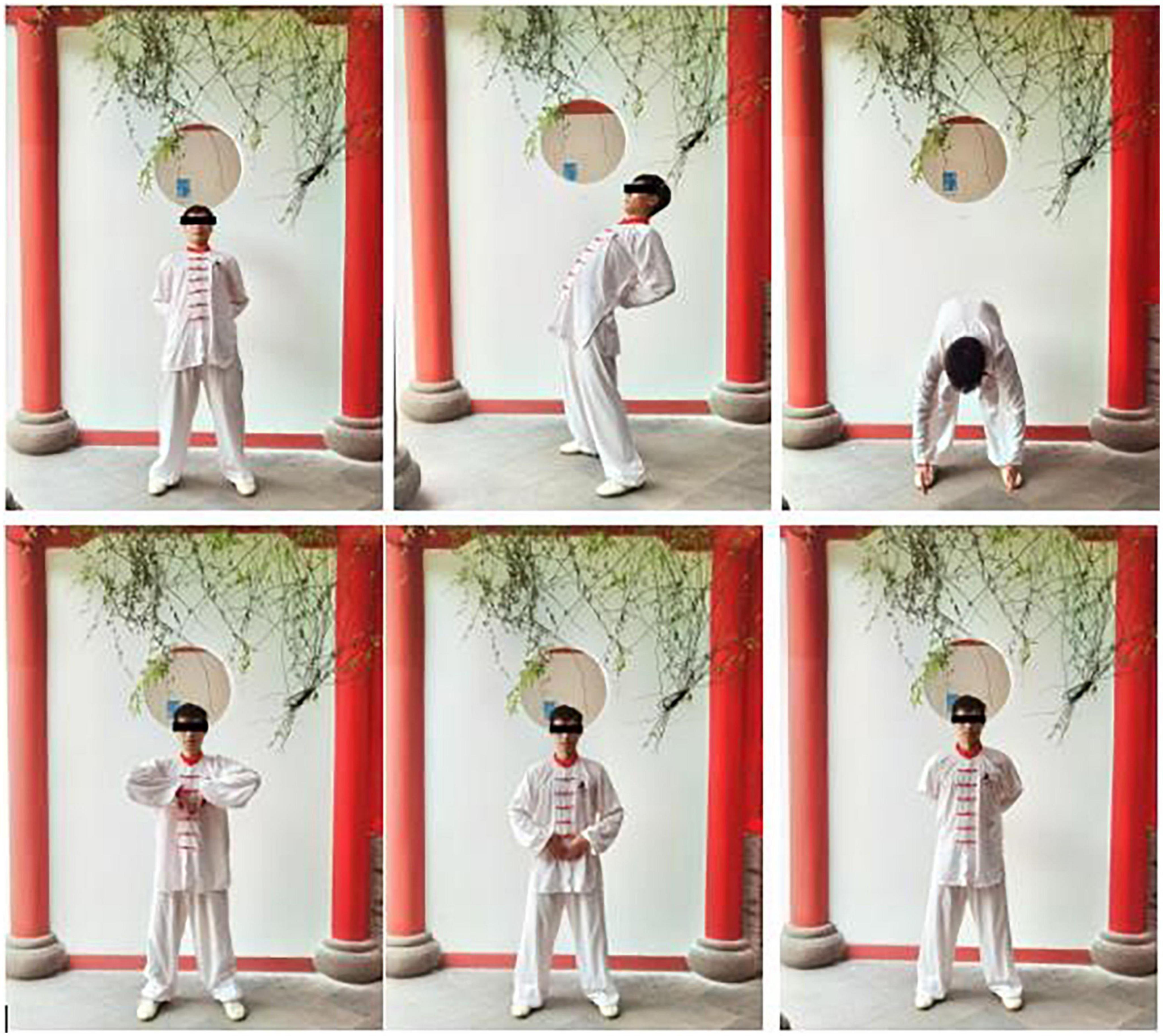
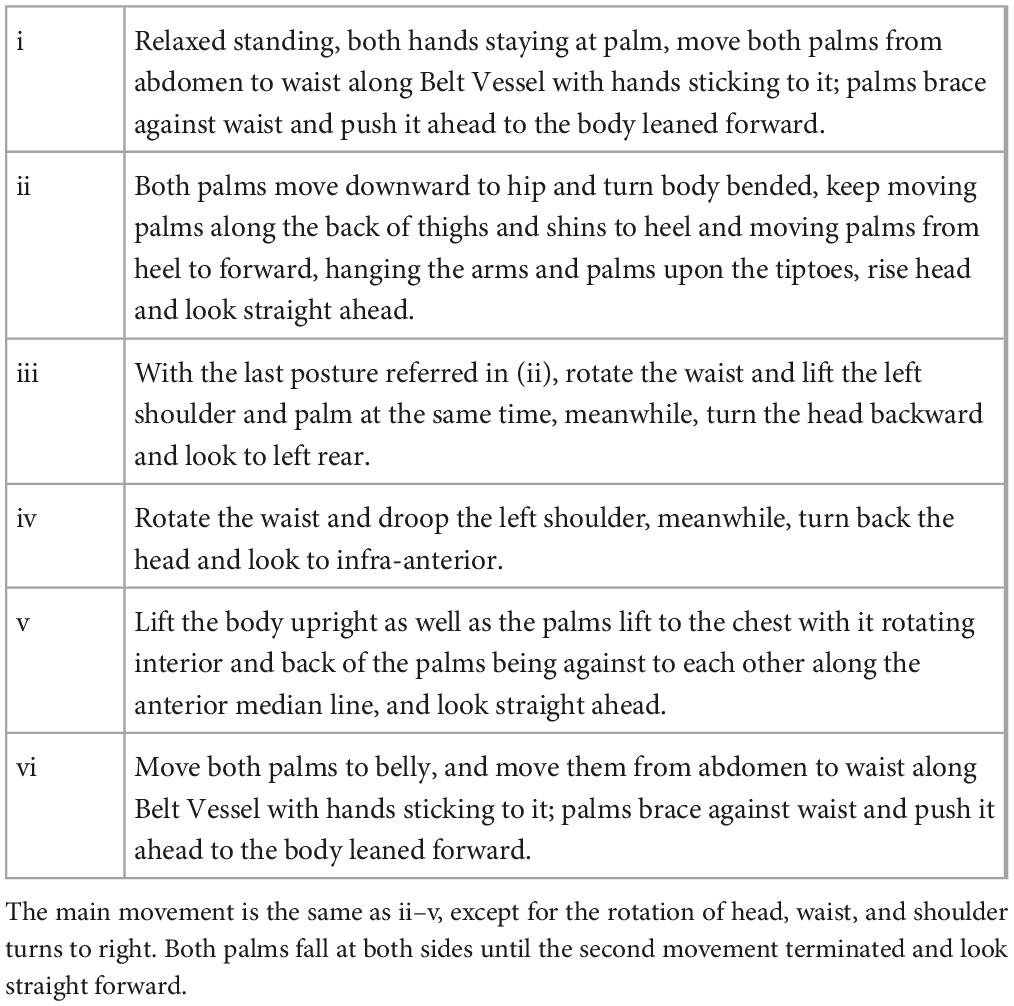
For a session of 4 weeks, participants in the experimental group will receive Mawangdui-Guidance Qigong Exercise therapy five times each week. Each exercise will continue for 30 min and be led by a particular coach who is equally skilled and experienced and has received training in how to manage a project. Figure 2, Table 2, and Supplementary video 1 show the program of the Mawangdui-Guidance Qigong Exercise’s “yinyao” movement.
Motor control exercise
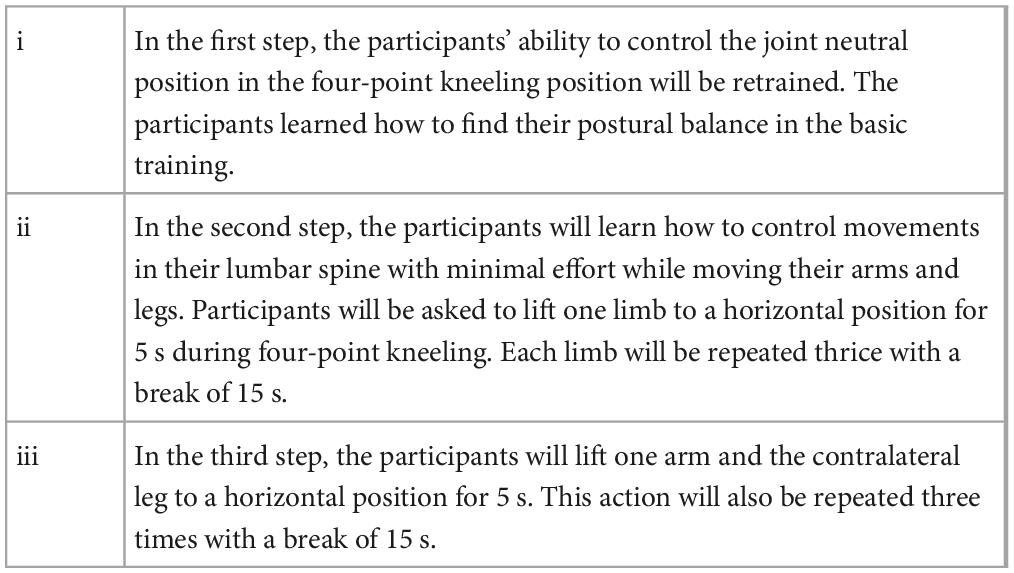
The main goal of these exercises in the MCE group is to normalize the significant motor abnormalities by teaching participants to maintain stable posture while properly contracting their muscles to lessen pain and intensity. Precious study helps to set the MCE strategy (Li et al., 2021). Participants will practice five times a week for 30 min each under the guidance of a specified experienced physiotherapist. Table 3 depicts the MCE process steps.
Drug treatment
A qualified and experienced doctor who has received the same training as the medicine group will evaluated and give oral celecoxib (Celebrex, Pfizer), 200 mg once daily, for 4 weeks to participant. The doctor will provide drug counseling throughout the duration of the experiment, as well.
To guarantee impartiality and rigor, participants with increased muscle pain after exercise and no obvious relief after rest will be treated with appropriate cryotherapy under the supervision of researchers. However, additional treatments including decoction, Chinese herbs, acupuncture, Tuina, and other painkillers will not be permitted.
Outcome measures
Primary outcomes
Primary outcomes include muscle activation sequence (Hodges, 2001; Suehiro et al., 2015), iEMG, RMS, and MF, generated from sEMG (Thomas et al., 2007; Aruin et al., 2015; Aruin, 2016). The EMG data will be gathered from the probe on the surface of deltoids, lumbar multifidus, transverse abdominis muscle (TrA), erector spinae muscle, gluteus maximus, and hamstrings. Each channel’s interelectrode distance will be 10 mm.
Secondary outcomes
The JOA Score (Oshima et al., 2020) and the McGill Pain Questionnaire (MPQ) (Main, 2016) are the secondary outcomes. JOA Score takes into account bladder function, daily activity, clinical indicators and subjective complaints, with the lowest score of 6 and the highest score of 29. Better functioning conditions are indicated by higher overall scores. MPQ is made up of 15 carefully chosen words, comprising 4 emotional and 11 sensory words. Each item is given a number from 0 to 3, with a higher score denotes a severer symptom (Choi et al., 2015). Biomarkers like substance P (Bhatia, 2015) and beta-endorphin (Choi and Lee, 2019) will also be tested.
All the primary and secondary outcomes will be assessed before and 1 week after treatment.
Adverse events
Researchers will keep track of adverse events and evaluate the correlation with therapies. Once relevant severe adverse event occurs (major damage to the heart, liver, kidneys, or other organs), the researchers will evaluate the participant can continue this trial or not. If serious adverse reactions occur, visits will continue after safety and treatment after the patient’s trial is suspended.
Sample size
By utilizing a two-sided 0.05 level t-test with >95% power and assuming a 10% dropout rate, the sample size was estimated to demonstrate the influence of the target muscles on MF (Zhou, 2018). To detect a target effect size of 0.44 (GPower 3.1) with 28 participants in each group, a sample size of 84 participants is needed.
Participants recruitment
Chronic non-specific low back pain is an exclusionary diagnosis. Patients with chronic LBP who do not have particular illnesses will be given this diagnosis (Koes et al., 2006). Eligible patients will be recruited from the Department of Orthopedics of Chengdu University of Traditional Chinese Medicine (CDUTCM). To ensure that recruitment messages are easily received by patients interested in the trial, recruitment posters and leaflets are placed in hospital lobbies and orthopedic clinics. Patients can also contact the staff through WeChat and the hospital website to sign up for the trial. In order to improve compliance, participants will be fully informed before signing informed consent. Researchers will keep track of participants’ compliance, including monitoring drug use and exercise on a regular basis. The participant recruiting process started on 23 October 2022, is still running, and it should be finished by 31 December 2022.
Allocation
Eligible patients will be randomly assigned to the Qigong group (n = 28), the MCE group (n = 28), or the medication group (n = 28) according to the inclusion and exclusion criteria with a ratio of 1:1:1. Prior to intervention, each patient will receive a random number in a sealed envelope. An automated random number generator created this random number, which is specific to each row in the table. A randomizer will assign patients to the experimental or control groups. An assessor who is unrelated to the study will maintain absolute confidentiality regarding the allocation list.
Blinding
In this study, a single blind approach will be used to execute the Mawangdui-Guidance Qigong Exercise. It is impossible to blind participants and researchers to the group assignment. The same unbiased, skilled evaluators who are blind to the allocation will measure each result.
Data collecting and monitoring
The Data Monitoring Committee (DMC) for Medical Data in this project is the Chengdu University of Traditional Chinese Medicine Evidence-based Medicine Center. Designated outcome assessors will record data on paper and computerized CRFs, and the DMC will keep an eye on it. Every 3 months, monitors will audit the data. During the evaluation process, coaches and statisticians will not have access to these data.
Statistical analysis
Test-retest reliability and content consistency reliability will be used to gauge the scale’s dependability (test-retest reliability). Cronbach’s coefficient is the most often used measure of internal consistency reliability. The better the homogeneity, the higher the Cronbach’s alpha coefficient. If the scale’s consistency is greater than 0.8, it is considered to be good, and if it is greater than 0.7, it is considered to be acceptable.
SPSS version 20.0 (SPSS Inc., Chicago, IL, USA) will be used for all of the analysis. The significance threshold will be set at 0.05, and the confidence interval will be 95%. The χ2 will be used to analyze categorical data. For continuous variables, mean ± SD will be recorded by using ANOVA test if they were normally distributed, or the median with interquartile range will be shown with Kruskal–Wallis H test. The Bonferroni correction and Tukey post-hoc test (for ANOVA) will be used to handle multiple comparisons (for Kruskal–Wallis). The Chi-square test will be used to verify the classification count data. Two-tailed test will be used in this study. The difference will be regarded as statistically significant when P < 0.05.
To handle missing data, we will evaluate the underlying cause, employ an imputation adjustment approach, and do a last observation carried forward analysis. Following the primary analysis, a sensitivity analysis will be carried out to determine the effect of missing data on the trial outcomes by contrasting the findings from the per-protocol analysis and the intention to treat analysis. Also planned are subgroup analysis by the center.
Quality assurance
Before agreeing to participate, it will be ensured that each participant meets tight eligibility requirements. All of the researchers have received professional training to understand how to carry out a typical research protocol and the operational requirements. Particularly, there will be individuals in charge of gathering and registering test information. Periodically, the data will be audited by the DMC monitors.
Discussion
The purpose of this study is to explore the effectiveness of Mawangdui-Guidance Qigong Exercise on CNLBP, and to further discuss the potential neuroelectrophysiology mechanism. Lumbar multifidus muscle has been proved crucial to the intersegmental stability of lumbar spine (Beimborn and Morrissey, 1988). Higher level of multifidus muscle activation observed in CNLBP patients is related to muscle spasm and the Pain Adaptation Model (Sherman, 1985; Ahern et al., 1988; Ansari et al., 2018). TrA primarily contributes to the dynamic stability of the lumbar spine by contracting the abdominal muscles to regulate various pain adaption models (van Dieën et al., 2003; Allison and Morris, 2008; da Silva et al., 2017). The data of lumbar multifidus muscle and TrA (Beneck et al., 2016; Shah et al., 2020) are usually collected using sEMG in the study of postural balance in patients with LBP. The relationship between neuromuscular control mechanisms and pain, however, is yet unclear.
Neurological system moderately activates the muscles at the proper time in the event of spinal injury, according to the “spinal stability model” (Panjabi, 1992). Feed-forward, feed-back, and voluntary control makes up of the basic central motor control modes of lumbar spinal stability muscles. According to visual, auditory, postural, and proprioceptive senses as well as feed-forward and feed-back control, the nervous system regulates the lumbar stability muscles to maintain lumbar stability or unconsciously protect the spine. The probable mechanism of Qigong may involve stretching and strengthening the core muscles in the waist. In patients with CNLBP, Mawangdui-Guidance Qigong Exercise, according to our hypothesis, preserves postural stability by altering the order of muscle activation.
Since the pathophysiology of CNLBP is unknown, LBP is frequently included in discussions about CNLBP illness management (Maher et al., 2017). Inflammation may continue throughout the entire course of LBP (Vucetic and Svensson, 1996; Vroomen et al., 2002) and is a key component of both pain and spinal degenerative processes (Wuertz and Haglund, 2013; Risbud and Shapiro, 2014). Beta-endorphin and substance P are also advised as alternatives to inflammatory markers as indicators of how well a treatment is working for patients with LBP (Bhatia, 2015; Choi and Lee, 2019). We believe that Mawangdui-Guidance Qigong Exercise can achieve the same or even more improvement in pain and lumbar function than the other two groups.
Prescription of Mawangdui-Guidance Qigong Exercise revolve limb opening and closing, rotation flexion and extension, stretching, and bone stretching, based on meridian guidance. It is a popular kind of Traditional Chinese Medicine (TCM) rehabilitation exercise therapy recently for cardiovascular, metabolic, and musculoskeletal system diseases (Wang et al., 2014; Sun and Wang, 2015; Chen, 2016; Ding et al., 2019). Though it is beneficial to the changes in the cellular level of elderly women (Wang et al., 2016), generally speaking, application of guidance still focuses on the observation of the overall effect on the body. The current research should focus on the therapeutic impact mechanism of Mawangdui guidance.
Compared with younger people, people over the age of 40 have a higher incidence of degenerative diseases such as lumbar disc herniation (Brinjikji et al., 2015). It is difficult to prove that LBP in patients over 40 years old is not caused by the above-mentioned specific causes. The specificity and non-specificity of LBP can be easily identified in younger people. That is why we designed this RCT with participants limited by ages between 20 and 39. As a result, the current study could not clearly explain the differentiation between various ages, and future researches on the effectiveness of multiple ages are needed. Secondly, since the single-center design with limited sample size may restrict the credibility of this trial, multi-center experiments in the future may help in enhancing the reproducibility and stability of the research. In addition, the treatment duration keeps 4 weeks without longer-term observation, we plan to conduct a follow-up at the 8th and 12th weeks by phone after the trial finished.
By contrasting the efficacy and safety of Mawangdui-Guidance Qigong Exercise in CNLBP treatment with MCE and oral medication, the prospective findings are anticipated to offer an alternative treatment for CNLBP and provide a possible explanation of the mechanism of Mawangdui-Guidance Qigong Exercise on CNLBP.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
GZ, LG, YS, ZZ, and YH participated in the conception and design of this trial. GZ, DZ, and HL were responsible for planning the draft and revising the manuscript. GZ was monitor of this study. All authors contributed to this work, read the manuscript, and approved the publication of this protocol.
Funding
This study was supported by the Sichuan Cadres Health Project: “Study on the biomechanical mechanism of Mawangdui guidance in the treatment of nonspecific low back pain” (grant number: Chuanganyan2020-501), Science and Technology Department of Sichuan Province Project: “Big data diagnosis and intelligent diagnosis of traditional Chinese and western medicine on orthopedic shoulder pain” (grant number: 23ZDYF2413), and Sichuan Provincial Administration of Traditional Chinese Medicine Project: “The biomechanical mechanism based on gait analysis to explore the application and popularization value of fitness Qigong Mawangdui guidance in the prevention and treatment of non-specific low back pain” (grant number: 2021MS156). These funding bodies did not have any role in the study design or the decision to submit the manuscript for publication.
Acknowledgments
We would like to express gratitude to YH from the Department of Orthopedic of Affiliated Hospital of Chengdu University of Traditional Chinese Medicine, for recruiting participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2023.1090138/full#supplementary-material
Abbreviations
CNLBP, chronic non-specific low back pain; RCT, randomized controlled trial; RMS, root mean square value; MF, median frequency; JOA, Japanese Orthopedic Association; MPQ, Mcgill Pain Questionnaire; LBP, low back pain; MCE, motor control exercise; sEMG, surface electromyograph; CDUTCM, Hospital of Chengdu University of Traditional Chinese Medicine; TrA, transverse abdominis muscle; DMC, Data Monitoring Committee.
References
Ahern, D., Follick, M., Council, J., Laser-Wolston, N., and Litchman, H. (1988). Comparison of lumbar paravertebral EMG patterns in chronic low back pain patients and non-patient controls. Pain 34, 153–160. doi: 10.1016/0304-3959(88)90160-1
Airaksinen, O., Brox, J., Cedraschi, C., Hildebrandt, J., Klaber-Moffett, J., Kovacs, F., et al. (2006). Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur. Spine J. 15, S192–S300. doi: 10.1007/s00586-006-1072-1
Akbari, M., Sarrafzadeh, J., Maroufi, N., and Haghani, H. (2015). Changes in postural and trunk muscles responses in patients with chronic nonspecific low back pain during sudden upper limb loading. Med. J. Islam. Repub. Iran 29:265.
Allison, G., and Morris, S. (2008). Transversus abdominis and core stability: Has the pendulum swung? Br. J. Sports Med. 42, 930–931. doi: 10.1136/bjsm.2008.048637
Ansari, B., Bhati, P., Singla, D., Nazish, N., and Hussain, M. (2018). Lumbar muscle activation pattern during forward and backward walking in participants with and without chronic low back pain: An electromyographic study. J. Chiropr. Med. 17, 217–225. doi: 10.1016/j.jcm.2018.03.008
Aruin, A. (2016). Enhancing anticipatory postural adjustments: A novel approach to balance rehabilitation. J. Nov. Physiother. 6:e144. doi: 10.4172/2165-7025.1000e144
Aruin, A., Kanekar, N., Lee, Y., and Ganesan, M. (2015). Enhancement of anticipatory postural adjustments in older adults as a result of a single session of ball throwing exercise. Exp. Brain Res. 233, 649–655. doi: 10.1007/s00221-014-4144-1
Beimborn, D., and Morrissey, M. (1988). A review of the literature related to trunk muscle performance. Spine (Phila Pa 1976) 13, 655–660.
Beneck, G., Story, J., and Donald, S. (2016). Postural cueing to increase lumbar lordosis increases lumbar multifidus activation during trunk stabilization exercises: Electromyographic assessment using intramuscular electrodes. J. Orthop. Sports Phys. Ther. 46, 293–299. doi: 10.2519/jospt.2016.6174
Bhatia, M. (2015). H2S and substance P in inflammation. Methods Enzymol. 555, 195–205. doi: 10.1016/bs.mie.2014.11.024
Birbara, C., Puopolo, A., Munoz, D., Sheldon, E., Mangione, A., Bohidar, N., et al. (2003). Treatment of chronic low back pain with etoricoxib, a new cyclo-oxygenase-2 selective inhibitor: Improvement in pain and disability–a randomized, placebo-controlled, 3-month trial. J. Pain 4, 307–315. doi: 10.1016/s1526-5900(03)00633-3
Blödt, S., Pach, D., Kaster, T., Lüdtke, R., Icke, K., Reisshauer, A., et al. (2015). Qigong versus exercise therapy for chronic low back pain in adults–a randomized controlled non-inferiority trial. Eur. J. Pain 19, 123–131. doi: 10.1002/ejp.529
Brinjikji, W., Luetmer, P., Comstock, B., Bresnahan, B., Chen, L., Deyo, R., et al. (2015). Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am. J. Neuroradiol. 36, 811–816. doi: 10.3174/ajnr.A4173
Chen, D. (2016). Effect of health qigong Mawangdui daoyinshu on blood pressure of individuals with essential hypertension. J. Am. Geriatr. Soc. 64, 1513–1515. doi: 10.1111/jgs.14218
Choi, H., and Lee, C. (2019). Can beta-endorphin be used as a biomarker for chronic low back pain? A meta-analysis of randomized controlled trials. Pain Med. 20, 28–36. doi: 10.1093/pm/pny186
Choi, S., Son, C., Lee, J., and Cho, S. (2015). Confirmatory factor analysis of the Korean version of the short-form McGill pain questionnaire with chronic pain patients: A comparison of alternative models. Health Qual. Life Outcomes 13:15. doi: 10.1186/s12955-014-0195-z
Chou, R., Qaseem, A., Snow, V., Casey, D., Cross, J. Jr., Shekelle, P., et al. (2007). Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American college of physicians and the American pain society. Ann. Intern. Med. 147, 478–491. doi: 10.7326/0003-4819-147-7-200710020-00006
Christophy, M., Faruk Senan, N., Lotz, J., and O’Reilly, O. (2012). A musculoskeletal model for the lumbar spine. Biomech. Model. Mechanobiol. 11, 19–34.
da Silva, A., Dos Santos, R., Coertjens, P., and Coertjens, M. (2017). Clinimetric properties of the pressure biofeedback unit method for estimating respiratory pressures. Physiother. Theory Pract. 33, 345–351. doi: 10.1080/09593985.2017.1289577
Daggfeldt, K., and Thorstensson, A. (2003). The mechanics of back-extensor torque production about the lumbar spine. J. Biomech. 36, 815–825. doi: 10.1016/s0021-9290(03)00015-0
Ding, H., Yu, C., Zhang, C., Wang, L., and Li, P. (2019). Application and prospect of fitness qigong Mawangdui guidance in rehabilitation nursing. J. Nurs. 26, 19–22. doi: 10.16460/j.issn1008-9969.2019.08.019
Eliks, M., Zgorzalewicz-Stachowiak, M., and Zeńczak-Praga, K. (2019). Application of pilates-based exercises in the treatment of chronic non-specific low back pain: State of the art. Postgrad. Med. J. 95, 41–45. doi: 10.1136/postgradmedj-2018-135920
Falla, D., and Hodges, P. (2017). Individualized exercise interventions for spinal pain. Exerc. Sport Sci. Rev. 45, 105–115.
Fan, X. (2002). A brief analysis of the partial function method of Mawangdui guide map. Clin. J. Tradit. Chin. Med. 5, 345–346. doi: 10.16448/j.cjtcm.2002.05.007
Furlan, A., Pennick, V., Bombardier, C., van Tulder, M., and Editorial Board, Cochrane Back Review Group (2009). 2009 updated method guidelines for systematic reviews in the Cochrane back review group. Spine (Phila Pa 1976) 34, 1929–1941. doi: 10.1097/BRS.0b013e3181b1c99f
Geisser, M., Ranavaya, M., Haig, A., Roth, R., Zucker, R., Ambroz, C., et al. (2005). A meta-analytic review of surface electromyography among persons with low back pain and normal, healthy controls. J. Pain 6, 711–726. doi: 10.1016/j.jpain.2005.06.008
Hodges, P. (2001). Changes in motor planning of feedforward postural responses of the trunk muscles in low back pain. Exp. Brain Res. 141, 261–266. doi: 10.1007/s002210100873
Hodges, P., and Richardson, C. (1996). Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine (Phila Pa 1976) 21, 2640–2650. doi: 10.1097/00007632-199611150-00014
Holtzman, S., and Beggs, R. (2013). Yoga for chronic low back pain: A meta-analysis of randomized controlled trials. Pain Res. Manag. 18, 267–272. doi: 10.1155/2013/105919
Jacobs, J., Lyman, C., Hitt, J., and Henry, S. (2017). Task-related and person-related variables influence the effect of low back pain on anticipatory postural adjustments. Hum. Mov. Sci. 54, 210–219. doi: 10.1016/j.humov.2017.05.007
Katz, N., Ju, W., Krupa, D., Sperling, R., Bozalis Rodgers, D., Gertz, B., et al. (2003). Efficacy and safety of rofecoxib in patients with chronic low back pain: Results from two 4-week, randomized, placebo-controlled, parallel-group, double-blind trials. Spine (Phila Pa 1976) 28, 851–858. doi: 10.1097/01.BRS.0000059762.89308.97
Koes, B., van Tulder, M., and Thomas, S. (2006). Diagnosis and treatment of low back pain. BMJ 332, 1430–1434. doi: 10.1136/bmj.332.7555.1430
Larivière, C., and Preuss, R. (2021). The effect of extensible and non-extensible lumbosacral orthoses on anticipatory postural adjustments in participants with low back pain and healthy controls. Musculoskelet Sci. Pract. 55:102421. doi: 10.1016/j.msksp.2021.102421
Li, Z., Yu, Q., Luo, H., Liang, W., Li, X., Ge, L., et al. (2021). The effect of virtual reality training on anticipatory postural adjustments in patients with chronic nonspecific low back pain: A preliminary study. Neural Plast. 2021:9975862. doi: 10.1155/2021/9975862
Ma, K., Zhuang, Z., Wang, L., Liu, X., Lu, L., Yang, X., et al. (2019). The Chinese association for the study of pain (CASP): Consensus on the assessment and management of chronic nonspecific low back pain. Pain Res. Manag. 2019:8957847. doi: 10.1155/2019/8957847
Macedo, L., Bostick, G., and Maher, C. (2013). Exercise for prevention of recurrences of nonspecific low back pain. Phys. Ther. 93, 1587–1591. doi: 10.2522/ptj.20120464
Maher, C., Vroomen, P., and Buchbinder, R. (2017). Non-specific low back pain. Lancet 389, 736–747. doi: 10.1016/S0140-6736(16)30970-9
Main, C. (2016). Pain assessment in context: A state of the science review of the McGill pain questionnaire 40 years on. Pain 157, 1387–1399. doi: 10.1097/j.pain.0000000000000457
Marks, R. (2019). Qigong and musculoskeletal pain. Curr. Rheumatol. Rep. 21:59. doi: 10.1007/s11926-019-0861-6
Marshall, P., and Murphy, B. (2008). Muscle activation changes after exercise rehabilitation for chronic low back pain. Arch. Phys. Med. Rehabil. 89, 1305–1313.
Oshima, Y., Takeshita, K., Kato, S., Doi, T., Matsubayashi, Y., Taniguchi, Y., et al. (2020). Comparison between the Japanese orthopaedic association (JOA) score and patient-reported JOA (PRO-JOA) score to evaluate surgical outcomes of degenerative cervical myelopathy. Global Spine J. 12, 795–800. doi: 10.1177/2192568220964167
Pallay, R., Seger, W., Adler, J., Ettlinger, R., Quaidoo, E., Lipetz, R., et al. (2004). Etoricoxib reduced pain and disability and improved quality of life in patients with chronic low back pain: A 3 month, randomized, controlled trial. Scand. J. Rheumatol. 33, 257–266. doi: 10.1080/03009740410005728
Panjabi, M. (1992). The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord. 5, 390–396. doi: 10.1097/00002517-199212000-00002
Parthan, A., Evans, C., and Le, K. (2006). Chronic low back pain: Epidemiology, economic burden and patient-reported outcomes in the USA. Expert Rev. Pharmacoecon. Outcomes Res. 6, 359–369. doi: 10.1586/14737167.6.3.359
Phattharasupharerk, S., Purepong, N., Eksakulkla, S., and Siriphorn, A. (2019). Effects of qigong practice in office workers with chronic non-specific low back pain: A randomized control trial. J. Bodyw. Mov. Ther. 23, 375–381. doi: 10.1016/j.jbmt.2018.02.004
Risbud, M., and Shapiro, I. (2014). Role of cytokines in intervertebral disc degeneration: Pain and disc content. Nat. Rev. Rheumatol. 10, 44–56. doi: 10.1038/nrrheum.2013.160
Saragiotto, B., Maher, C., Yamato, T., Costa, L., Menezes Costa, L., Ostelo, R., et al. (2016). Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst. Rev. 2016:CD012004. doi: 10.1002/14651858.CD012004
Shah, J., Tanwar, T., Iram, I., Aldabbas, M., and Veqar, Z. (2020). Effect of increased lumbar lordosis on lumbar multifidus and longissimus thoracis activation during quadruped exercise in patients with chronic low back pain: An EMG study. J. Appl. Biomech. 22, 1–8. doi: 10.1123/jab.2020-0040
Sherman, R. (1985). Relationships between strength of low back muscle contraction and reported intensity of chronic low back pain. Am. J. Phys. Med. 64, 190–200.
Suehiro, T., Mizutani, M., Ishida, H., Kobara, K., Osaka, H., and Watanabe, S. (2015). Individuals with chronic low back pain demonstrate delayed onset of the back muscle activity during prone hip extension. J. Electromyogr. Kinesiol. 25, 675–680. doi: 10.1016/j.jelekin.2015.04.013
Sun, Y., and Wang, H. (2015). Teaching exploration of fitness qigong Mawangdui guidance– clinical follow-up study based on ankylosing spondylitis. Wushu Stud. 12, 86–88. doi: 10.13293/j.cnki.wskx.005458
Thomas, J., France, C., Sha, D., Vander Wiele, N., Moenter, S., and Swank, K. (2007). The effect of chronic low back pain on trunk muscle activations in target reaching movements with various loads. Spine (Phila Pa 1976) 32, E801–E808. doi: 10.1097/BRS.0b013e31815d0003
Tsao, H., and Hodges, P. (2008). Persistence of improvements in postural strategies following motor control training in people with recurrent low back pain. J. Electromyogr. Kinesiol. 18, 559–567. doi: 10.1016/j.jelekin.2006.10.012
van Dieën, J., Selen, L., and Cholewicki, J. (2003). Trunk muscle activation in low-back pain patients, an analysis of the literature. J. Electromyogr. Kinesiol. 13, 333–351. doi: 10.1016/s1050-6411(03)00041-5
van Middelkoop, M., Rubinstein, S., Kuijpers, T., Verhagen, A., Ostelo, R., Koes, B., et al. (2011). A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur. Spine J. 20, 19–39. doi: 10.1007/s00586-010-1518-3
van Tulder, M., Becker, A., Bekkering, T., Breen, A., del Real, M., Hutchinson, A., et al. (2006). Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur. Spine J. 15(Suppl. 2) S169–S191. doi: 10.1007/s00586-006-1071-2
Vroomen, P., de Krom, M., Wilmink, J., Kester, A., and Knottnerus, J. (2002). Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J. Neurol. Neurosurg. Psychiatry 72, 630–634. doi: 10.1136/jnnp.72.5.630
Vucetic, N., and Svensson, O. (1996). Physical signs in lumbar disc hernia. Clin. Orthop. Relat. Res. 333, 192–201.
Wang, B., Wu, Z., Lu, S., and Ma, J. (2016). Effect of health qigong Mawangdui Daoyin on NK cell of old and middle-aged women. China Med. Herald 13, 69–72.
Wang, B., Wu, Z., Lu, S., Hu, Y., Wang, D., and Xu, Y. (2014). Effects of fitness qigong Mawangdui guided exercise on blood lipid metabolism and free radical metabolism in middle-aged and elderly women. Chin. J. Gerontol. 34, 3720–3722.
Wuertz, K., and Haglund, L. (2013). Inflammatory mediators in intervertebral disk degeneration and discogenic pain. Global Spine J. 3, 175–184. doi: 10.1055/s-0033-1347299
Xie, L., and Wang, J. (2019). Anticipatory and compensatory postural adjustments in response to loading perturbation of unknown magnitude. Exp. Brain Res. 237, 173–180. doi: 10.1007/s00221-018-5397-x
Yu, Q., Huo, Y., Chen, M., Zhang, Z., Li, Z., Luo, H., et al. (2021). A study on the relationship between postural control and pain-related clinical outcomes in patients with chronic nonspecific low back pain. Pain Res. Manag. 2021:9054152.
Zhang, Y., Loprinzi, P., Yang, L., Liu, J., Liu, S., and Zou, L. (2019). The beneficial effects of traditional Chinese exercises for adults with low back pain: A meta-analysis of randomized controlled trials. Medicina (Kaunas) 55:118. doi: 10.3390/medicina55050118
Keywords: Qigong, postural balance, paraspinal muscles, RCT, low back pain
Citation: Zhang G, Gao L, Zhang D, Li H, Shen Y, Zhang Z and Huang Y (2023) Mawangdui-Guidance Qigong Exercise for patients with chronic non-specific low back pain: Study protocol of a randomized controlled trial. Front. Neurosci. 17:1090138. doi: 10.3389/fnins.2023.1090138
Received: 04 November 2022; Accepted: 23 February 2023;
Published: 13 March 2023.
Edited by:
Xue-Qiang Wang, Shanghai University of Sport, ChinaReviewed by:
Yan Shao, Liaoning University of Traditional Chinese Medicine, ChinaFeifei Liu, Binzhou Medical University Hospital, China
Wanli Xu, Nanjing Medical University, China
Copyright © 2023 Zhang, Gao, Zhang, Li, Shen, Zhang and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong Huang, aHVhbmd5b25nY2R1dGNtQDEyNi5jb20=
†These authors have contributed equally to this work and share first authorship
 Guilong Zhang
Guilong Zhang Liang Gao2†
Liang Gao2† Di Zhang
Di Zhang Hongjian Li
Hongjian Li