- 1Department of Surgical Oncology, Taizhou Hospital of Zhejiang Province, Wenzhou Medical University, Linhai, China
- 2Department of Plastic Surgery, Enze Hospital of Taizhou Enze Medical Center (Group), Luqiao, China
Background: The value of prophylactic central neck dissection (PCND) for papillary thyroid carcinoma (PTC) with clinically evident lateral cervical lymph node metastases (cN1b) remains unclear. Therefore, a systematic review and meta-analysis was conducted to assess the efficacy and safety of PCND.
Methods: A comprehensive systematic search was conducted on PubMed, Web of Science, Cochrane library and Embase databases up to September 2021 to identify eligible studies. Controlled clinical trials assessing therapeutic effects and safety of PCND for cN1b PTC patients were included. The risk of bias for each cohort study was assessed using the Newcastle-Ottawa Scale (NOS). The primary outcomes were indexes related to the locoregional recurrence (LRR) and surgical complications. Review Manager software V5.4.0 was used for statistical analysis. A fixed effects model was adopted for the data without heterogeneity, otherwise a random effects model was used.
Results: We included 4 retrospective cohort studies, which comprised 483 PTC patients. There was no statistically significant difference in the central neck recurrence (CNR) (10.2% vs. 3.8%, relative risk (RR) = 1.82; 95%CI 0.90–3.67; P = 0.09), lateral neck recurrence (LNR) (5.1% vs. 7.7%, RR = 0.47; 95% CI 0.13–1.74; P = 0.26), and overall recurrence (OR) (18.9% vs. 16.9%, RR = 0.77; 95%CI 0.34–1.76; P = 0.54), between LND + PCND group and LND group. Simultaneously, PCND increased the risk of permanent hypoparathyroidism (11.4% vs. 4.5%, RR = 2.70, 95%CI 1.05–6.94; P = 0.04) and overall complications (17.0% vs. 5.3%, RR = 3.28; 95%CI 1.37–7.86; P = 0.008).
Conclusions: This meta-analysis showed that PCND did not have any advantage in preventing LRR for cN1b PTC. Meanwhile, PCND may result in the increased rate of surgical complications. However, the current evidence is limited and more clinical trials are still needed to further clarify the true role of PCND.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/, CRD42021281825.
Introduction
Thyroid cancer is the most common malignant tumor in the endocrine system and head and neck tumors, causing586,000 cases worldwide and ranking 9th in incidence in 2020 (1). Papillary thyroid carcinoma (PTC) accounts for the vast majority of thyroid cancers. Regional lymph node metastases (LNM) are very common in patients with PTC (up to 80%), especially in the central compartment of the neck (2, 3). LNM have been reported in association with a higher rate of locoregional recurrence (LRR) (4). Surgical resection of clinically nodal-positive disease (cN1) in PTC is considered to make improvement to the results of both recurrence and survival. Therefore, it is generally believed that therapeutic cervical lymph node dissection is indicated in PTC patients with cN1. However, the effect on long-term outcome of prophylactic central neck dissection (PCND) in PTC patients without clinically evident nodal metastasis (cN0) remains unclear, and the 2021 National Comprehensive Cancer Network (NCCN) and the 2015 American Thyroid Association (ATA) guidelines do not recommend that routine PCND should be performed in all these PTC patients with cN0 (5, 6).
There is a generally accepted assumption that cervical LNM in PTC patients follow the gradual progression of LNM from the central to lateral compartment and lymph nodes skip metastases to the lateral compartment are present only in a small number of PTC patients (7, 8). Therefore, some surgeons have advocated routine PCND in PTC patients with clinically evident lateral cervical LNM (cN1b) combined with total thyroidectomy (TT) and lateral neck dissection (LND) (9). Moreover, the 2021 NCCN and the 2015 ATA guidelines suggest that PCND should be taken into consideration in PTC patients with cN1b (5, 6). However, this suggestion is relatively weak and based on low quality evidence, and the value of PCND remains unclear.
Surgery in the central compartment of neck may result in some complications. The majority of these complications are injuries of the parathyroid glands and recurrent laryngeal nerves, which will lead to temporary or permanent hypoparathyroidism and hoarseness of voice. As is well known, the extent of initial surgery of thyroid and lymph nodes should be based on evidence of long-term benefits in terms of improvements of local control or survival, while minimizing the risk of complications. Hence, for these PTC patients with cN1b but no clinically evident central compartment LNM on preoperative imaging or intraoperative evaluation, we should weigh the potential benefits of PCND against the risks. This systematic review and meta-analysis was conducted to evaluate the LRR and complications rates of TT + LND versus TT + LND + PCND.
Methods
Study Protocol and Registration
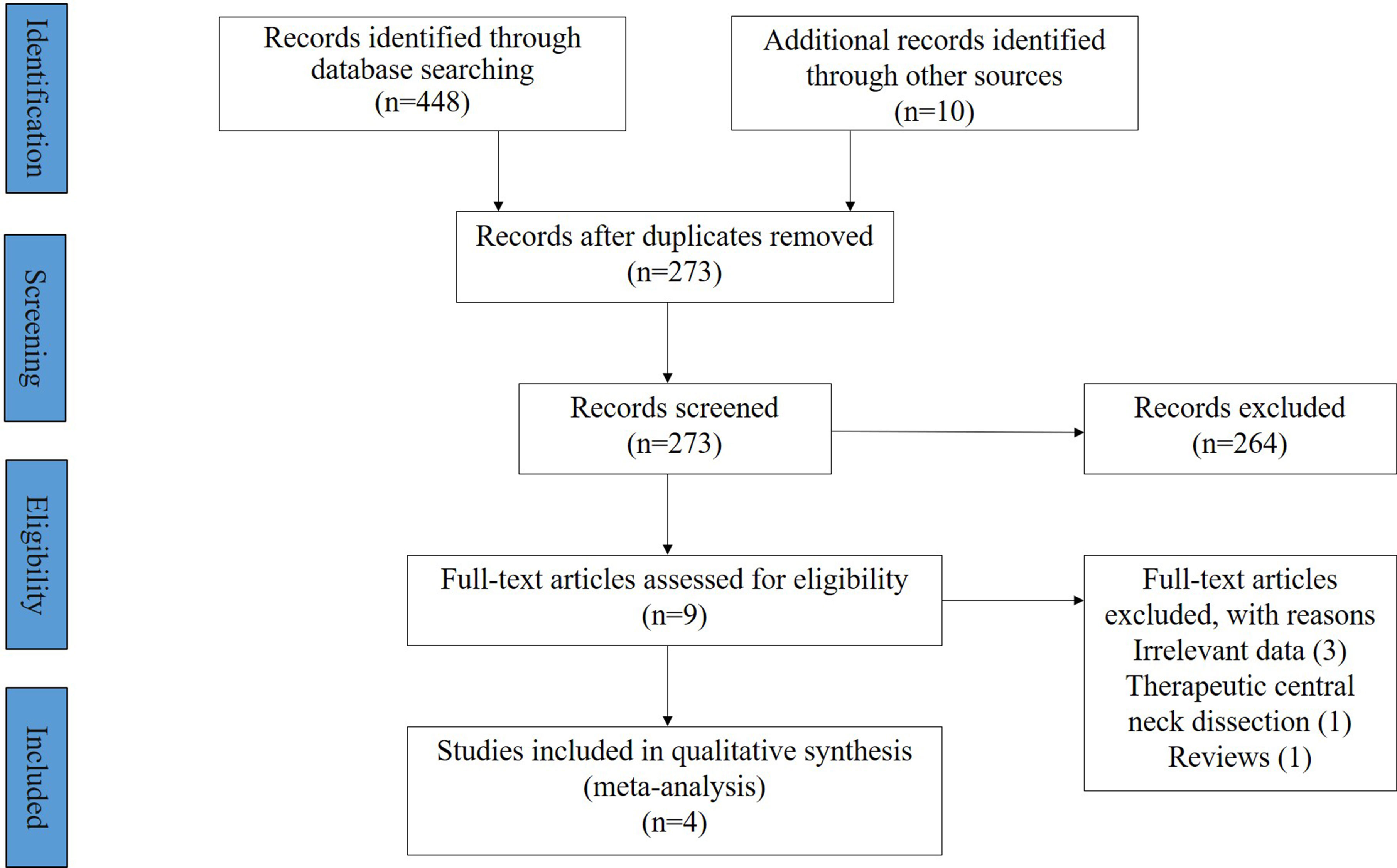
This systematic review and meta-analysis was performed in accordance with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Figure 1). The study protocol was registered on PROSPERO with No. CRD42021281825.
Search Strategy
Eligible studies were identified by a comprehensive systematic search on the PubMed, Web of Science, Cochrane library and Embase databases up to September 2021. The search strings used a combination of the terms “papillary thyroid cancer”, “well-differentiated thyroid carcinoma”, “lateral neck dissection”, “elective central neck dissection”, “prophylactic central neck dissection”, and logical word “OR” or “AND”.
Study Selection
Two investigators independently used search strategies to retrieve study titles and abstracts. The inclusion criteria for the articles were as follows (1): articles published in English, (2) PTC patients diagnosed with lateral compartment LNM, (3) two groups that compared TT + LND with TT + LND + PCND in study. The exclusion criteria were as follows: (1) lack of preoperative assessment of central compartment lymph nodes, (2) preoperative diagnosis of central compartment LNM, and (3) insufficient demographic and clinical data. Letters to editors, case reports, meeting abstracts, review articles and incomplete studies were also excluded. In addition, both investigators also reviewed the reference lists of included articles to identify additional relevant articles. All of the potentially eligible articles were identified, and any disagreements between the two investigators were resolved through a discussion and by consensus with a third investigator.
Data Extraction and Quality Assessment
Two investigators independently completed extraction of the following data from included articles based on a standardized template: first author, year, country, study design, study period, follow up, sample size, age, sex, tumor size, extrathyroidal extension, incidence of central LNM, radioactive iodine (RAI) treatment, number of LRR, site of LRR, and surgical complications. For cohort studies, quality assessment and analysis of risk of bias were conducted by Y-xQ and Z-zZ using Newcastle-Ottawa Scale (NOS) independently. This scale awards a maximum of nine points. A score of ≥7 is considered to indicate high quality.
Statistical Analysis
Review Manager software V5.4.0 (The Cochrane Collaboration, 2020) was used for statistical analysis. Heterogeneity among studies was assessed by the heterogeneity test with the I2 statistic. I2 >50% was considered significant heterogeneity. A fixed effects model was adopted for the data without heterogeneity in the meta-analysis, otherwise a random effects model was used for the significantly heterogeneous data. The difference between the two groups was quantified by the terms of relative risk (RR) along with 95% confidence interval (CI), and P <0.05 was considered to be significance.
Results
Study Selection
The detail of the article selection process is described as a flow chart (Figure 1). Our search strategy retrieved a total of 458 articles, and 273 unique articles were retained after removing the duplicates. After reviewing the titles and abstracts according to the inclusion and exclusion criteria, 9 potentially eligible articles were obtained and reviewed in full text. Of these 9 articles, 5 were subsequently excluded for various reasons, and finally 4 retrospective cohort studies involving 483 PTC cases were included in the meta-analysis (286 in the LND group and 197 in the LND + PCND group) (10–13).
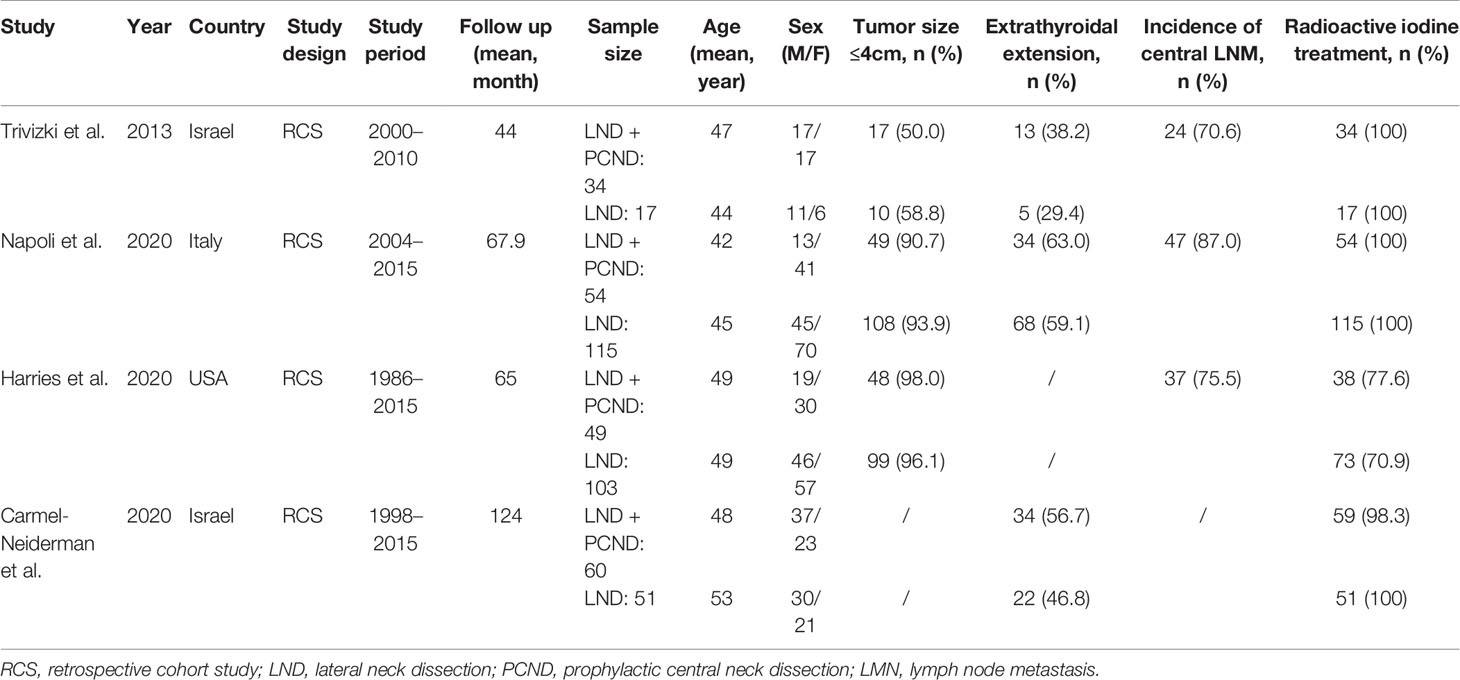
Study Characteristics and Quality
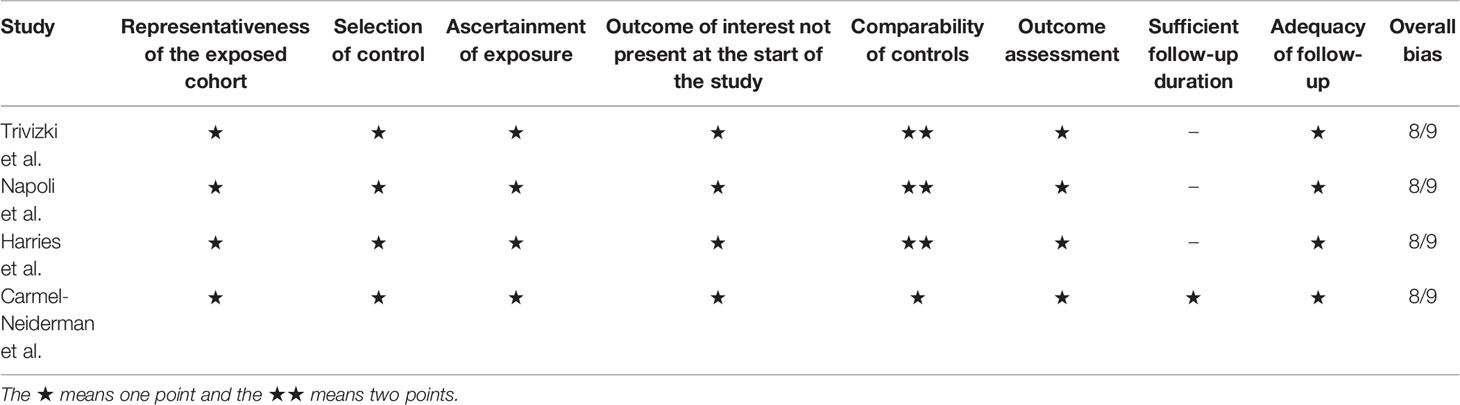
The characteristics of these included studies are summarized in Table 1. The years of publication of the included articles ranged from 2013 to 2020. Two studies were conducted in the Israel (10, 13), one in the USA (12), and one in Italy (11). All studies underwent a preoperative imaging procedure for central compartment lymph node assessment by ultrasonography, CT scan, or MRI scan, and two studies also performed an intraoperative evaluation. All studies made a comparison of gender ratio, age, tumor size, multifocality, extrathyroidal extension, metastatic lateral cervical lymph nodes, maximum size of metastatic lateral cervical lymph nodes, and RAI treatment between the two groups. Three studies showed a high incidence of central LNM ranging from 70.6 to 87.0%. The follow-up period ranged from 44 to 124 months. Recurrence of disease was determined by cervical imaging evaluation or serum thyroglobulin level and pathologically confirmed (if possible). Quality assessment is shown in Table 2. The exposed (patients underwent PCND) and nonexposed cohorts in all included studies were considered good representatives. The main outcomes of interest were LRR and complications. The distribution of preoperative clinical and demographic characteristics was comparable between these two groups, but the status of lateral cervical lymph nodes in each cohort was not compared in the Carmel‐Neiderman et al. study. The assessment of outcome was obtained from laboratory and imaging data. All studies provided the complete follow-up of all patients, but the mean follow-up period was less than 10 years in three studies, which was considered insufficient.
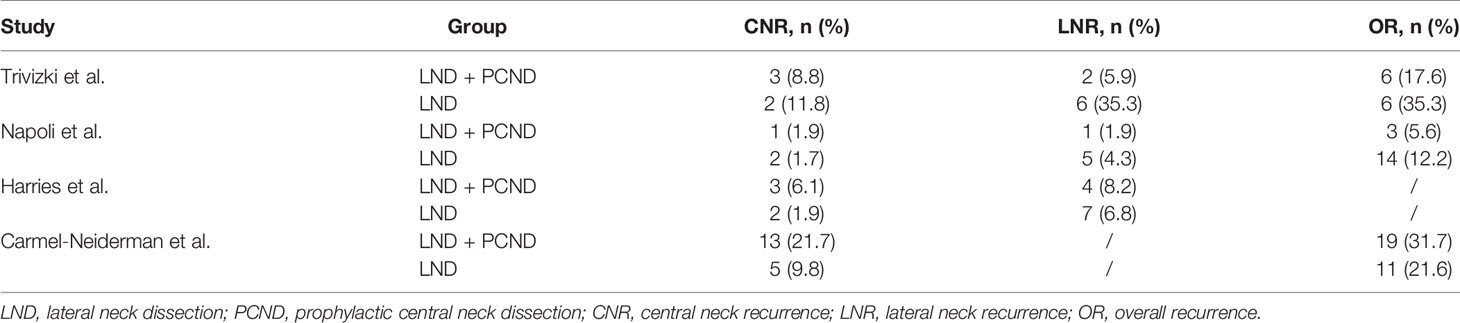
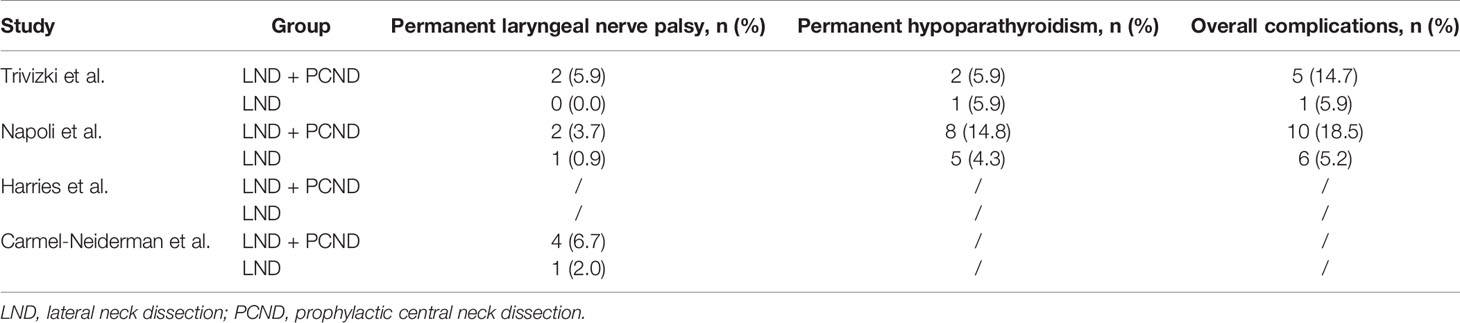
Recurrence
All studies reported data for central neck recurrence (CNR), 20 patients in the LND + PCND group and 11 patients in the LND group. There was no statistically significant difference between the two groups in the CNR (10.2% vs. 3.8%, RR = 1.82; 95%CI 0.90–3.67; P = 0.09; I2 = 0%). Three studies described lateral neck recurrence (LNR) (10–12), 7 patients in the LND + PCND group and 18 patients in the LND group. The rate of LRR in the lateral neck region was also similar between the two groups (5.1% vs. 7.7%, RR = 0.47; 95%CI 0.13–1.74; P = 0.26; I2 = 52%) (10–12). Moreover, we evaluated the overall recurrence (OR) in three studies involving 331 patients (148 received LND + PCND and 183 received LND). A total of 28 patients in total relapsed in the LND + PCND group and 31 patients in the LND group. There was no statistically significant difference between the two groups in OR (18.9% vs. 16.9%, RR = 0.77; 95%CI 0.34–1.76; P = 0.54; I2 = 59%) (10, 11, 13). Therefore, the outcomes of this meta-analysis suggested no statistically significant difference between the two groups in LRR and OR (Table 3 and Figure 2).
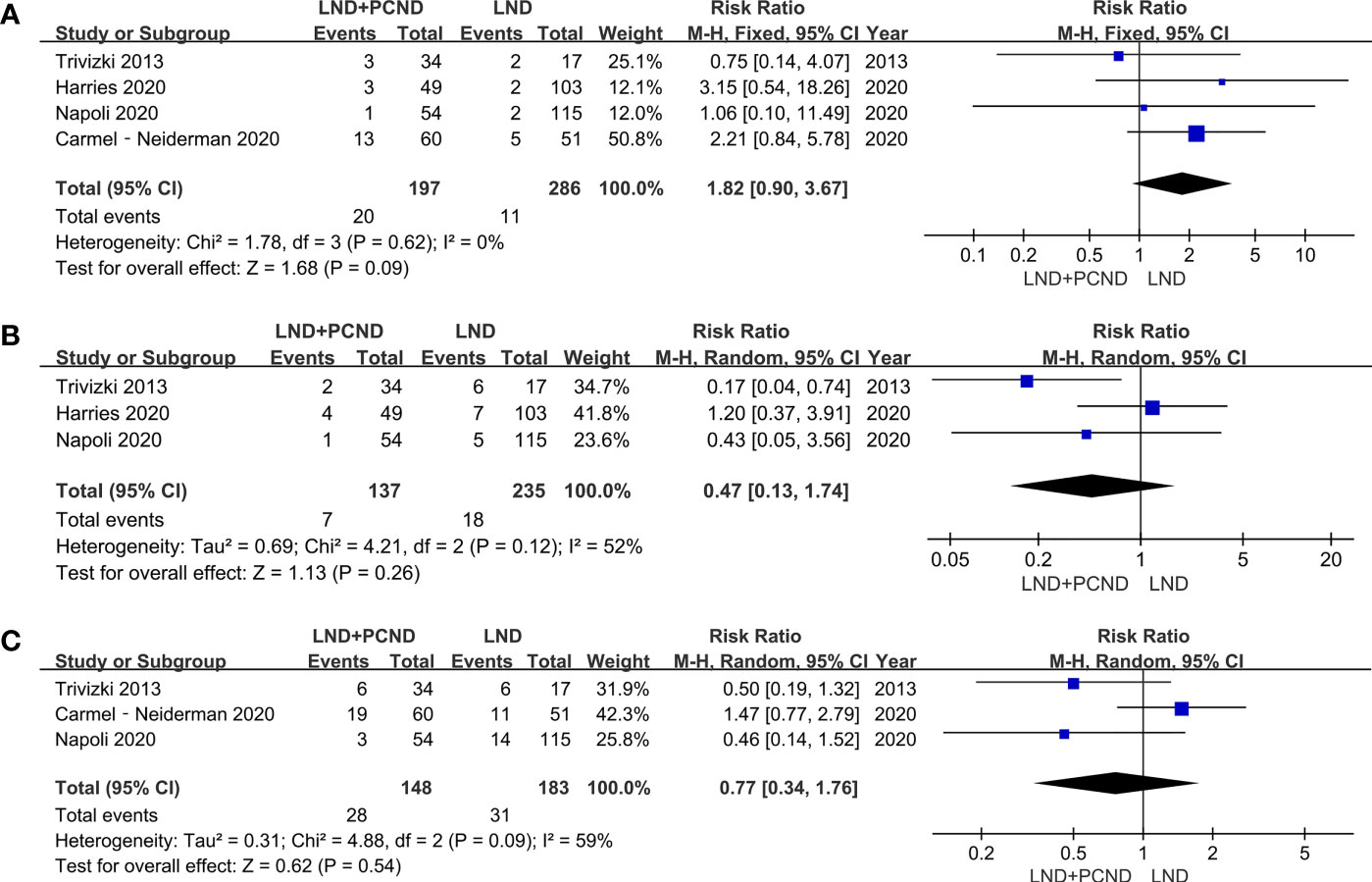
Figure 2 Forest plot showing a meta-analysis of locoregional recurrence (LRR) for included studies. (A) Central neck recurrence; (B) Lateral neck recurrence; (C) overall recurrence.
Surgical Complications
Data regarding to permanent laryngeal nerve palsy was reported in three studies, 8 patients in the LND + PCND group and 2 patients in the LND group. Prevalence of laryngeal nerve injury in the LND + PCND group and LND group was 5.4% (8/148) and 1.1% (2/183), respectively. Although the incidence of permanent laryngeal nerve palsy in the LND + PCND group was higher than that of the LND group, the outcome of this meta-analysis suggested no statistically significant difference (5.4% vs. 1.1%, RR = 3.40; 95%CI 0.83–13.94; P = 0.09; I2 = 0%). Data of permanent hypoparathyroidism and overall complications was reported in two studies (10, 11). A total of 10 patients presented permanent hypoparathyroidism in the LND + PCND group while 6 patients in the LND group, indicating a higher rate of permanent hypoparathyroidism in the LND + PCND group (11.4% vs. 4.5%, RR = 2.70, 95%CI 1.05–6.94; P = 0.04; I2 = 0%). A similar result was obtained for overall complications (17.0% vs. 5.3%, RR = 3.28; 95%CI 1.37–7.86; P = 0.008; I2 = 0%) (Table 4 and Figure 3).
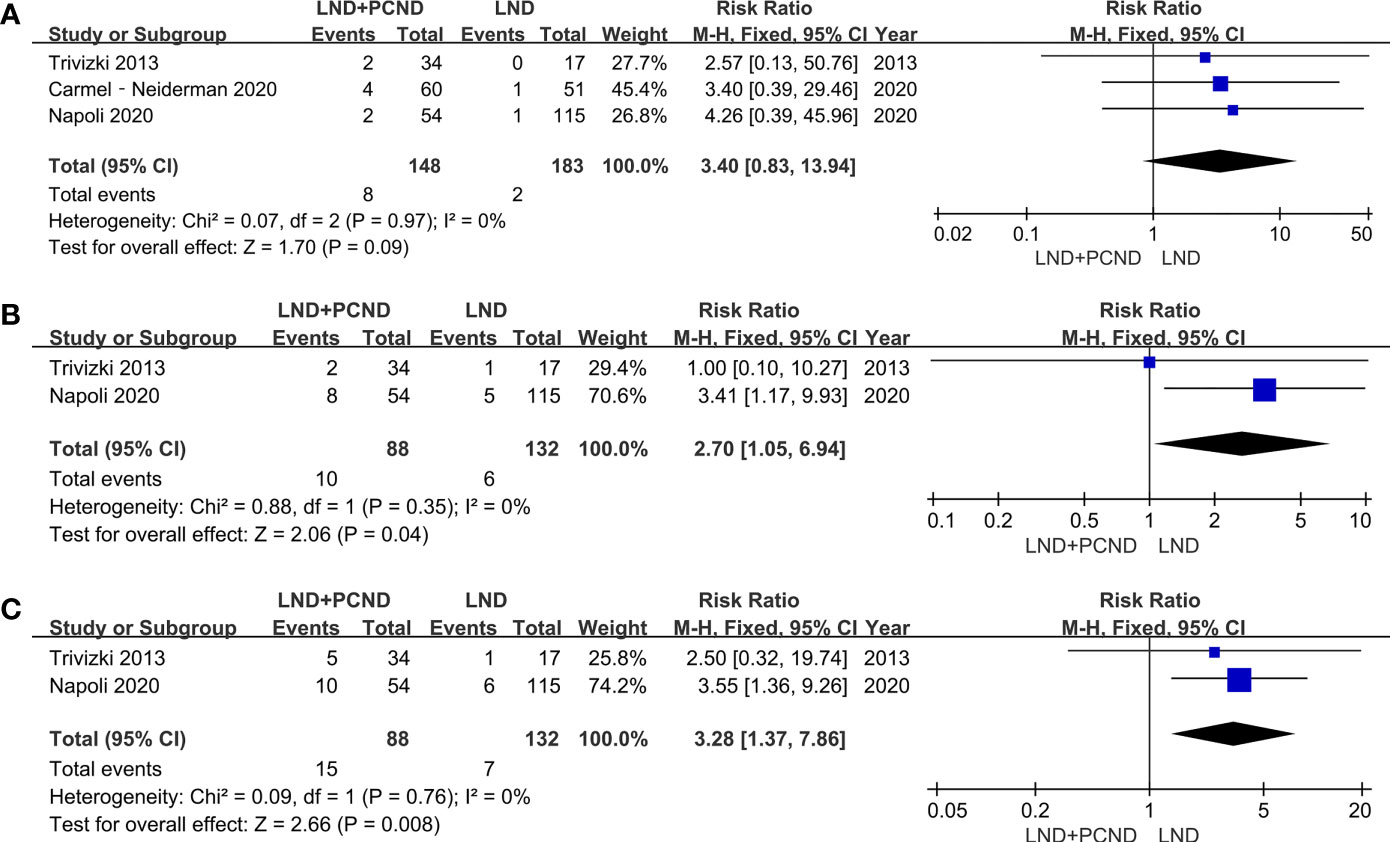
Figure 3 Forest plot showing a meta-analysis of postoperative complications for included studies. (A) Permanent laryngeal nerve palsy; (B) permanent hypoparathyroidism; (C) overall complications.
Discussion
Nowadays, the management of cervical lymph node dissection in the treatment of PTC is still one of most controversial issues. As everyone knows that therapeutic lymph node dissection for PTC patients will remove all metastatic lymphoid tissue and reduce the LRR rate. However, there is still a lack of sufficient evidence regarding the confirmation of the efficacy and benefit of PCND for PTC patients. Nowadays, the role of PCND in PTC patients with cN0 has been elaborately investigated. Some studies suggested that PCND in cN0 cases would make improvements to locoregional control and disease‐specific survival (14–18). Conversely, other studies suggested that PCND did not improve the long‐term prognosis, but increased the risk of complications (19–24). The difference between the same approach and the results of these studies, may be potentially settled in a prospective randomized controlled trial. However, the ATA investigation revealed that it was not feasible to conduct such a large prospective randomized controlled trial of PCND in PTC patients with cN0 (25). At present, the ATA and NCCN guidelines recommend that PCND should be considered in PTC patients with cN0 with advanced tumor or PTC patients with cN1b (5, 6). However, this recommendation is weak and the evidence is of low quality. The present study showed that a very select group of PTC patients with cN1b but no clinically evident central compartment lymph nodes involvement, might not require routine PCND. The additional procedure does not decrease the rate of LRR and OR, but it is accompanied by complications.
As we all know, regional LNM are very common in PTC patients. Studies have suggested that occult metastases can be found in the central compartment in 40–70% of cases (4, 11, 26). Due to the high rate of occult metastases, PCND may convert many patients from cN0 to pathologic N1a. However, occult metastases do not carry the similar recurrence risk compared with that of clinically detectable macro-metastases (2). The accurate staging information of lymph nodes may be helpful in the selection of adjuvant therapy in PTC patients with cN0, but it is almost useless for these PTC patients with cN1b. These patients will undergo adjuvant RAI treatment and suppression treatment followed surgery in accordance with the ATA guidelines (6). Adjuvant RAI treatment can improve the lymph node failure-free survival in all lymph node categories, and the greatest therapeutic benefits have been observed in patients with cN1b disease (27, 28). Clinically occult lymph node metastasis can also be successfully treated with adjuvant RAI treatment, with an improvement of 10-year lymph node failure-free survival rate from 82.3 to 95% and overall survival rate more than 90% in PTC patients with cN0 (27, 29). Therefore, adjuvant RAI treatment can contain the LRR and might be used as an alternative to PCND.
Additionally, the potential complications of PCND should not be overlooked. In this study, there was a significantly higher rate of permanent hypoparathyroidism in these patients treated with PCND. In fact, it is a quite common phenomenon that PCND leads to a high proportion of both transient and permanent hypoparathyroidism. The reason may be that the inferior parathyroid glands are removed or devascularized unintentionally during the procedure of PCND. Previous literatures also suggest that PTC patients who underwent PCND had a significantly higher incidence rate of permanent hypoparathyroidism compared with those patients managed without PCND (4.11–19.4% VS. 1.95–8%) (24, 30, 31). Although, there was no statistically significant difference in permanent laryngeal nerve palsy by the meta-analysis, the rate of permanent laryngeal nerve palsy following PCND is 3.7–6.7% compared with 0–2.0% in patients managed without PCND. Nowadays, intraoperative laryngeal nerve monitoring has been widely used for reducing the incidence of recurrent laryngeal nerve injury, and some intraoperative parathyroid identification techniques will be helpful to protect the parathyroid in surgery (32, 33). However, the extent of initial surgery should ultimately be determined by oncological benefit.
We acknowledge that there are several limitations in this meta-analysis. Firstly, only 4 articles were included in this meta-analysis and all studies were of retrospective design with small simple size, which limited our ability to draw firm conclusions from the data. Secondly, since PTC may relapse 10 to 20 years after initial treatment, long-term follow-up is necessary to compare the recurrence rate instead of only about 5 years follow-up. Thirdly, the quality of the included studies was not high. Selection bias or other confounding factors might be included and affect the reliability of the final results. Fourthly, because only articles in English were reviewed and included, some non-English articles may have been excluded from the present study.
Conclusions
In conclusion, this meta-analysis did not demonstrate any advantage in performing PCND in cN1b PTC patients without clinical evidence of central neck involvement for preventing LRR, even in the central region. Furthermore, PCND may result in the increased rate of surgical complications, including a higher rate of permanent hypoparathyroidism and overall complications. We recommend that PCND should not be routinely performed in PTC patients with cN1b, especially for these patients without any clinically evident central neck involvement. However, the current evidence is limited and we need more evidence from multicenter, prospective, randomized, controlled clinical trials to further clarify the true role of PCND in PTC patients with cN1b.
Data Availability Statement
The original contributions presented in the study are included in the article material. Further inquiries can be directed to the corresponding author.
Author Contributions
Study conception and design: B-jX and X-qY. Acquisition of data: X-qY, Z-zZ, and W-jY. Analysis and interpretation of data: Z-sM, M-lC and X-qY. Drafting of manuscript: X-qY, Z-zZ. Critical revision of manuscript: B-jX. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank Prof. Tao-Hsin Tung for his valuable suggestion that has helped improve the quality of the manuscript.
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: Cancer J Clin (2021) 71(3):209–49. doi: 10.3322/caac.21660
2. Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL, et al. The Prognostic Significance of Nodal Metastases From Papillary Thyroid Carcinoma can be Stratified Based on the Size and Number of Metastatic Lymph Nodes, as Well as the Presence of Extranodal Extension. Thyroid (2012) 22(11):1144–52. doi: 10.1089/thy.2012.0043
3. Thompson AM, Turner RM, Hayen A, Aniss A, Jalaty S, Learoyd DL, et al. A Preoperative Nomogram for the Prediction of Ipsilateral Central Compartment Lymph Node Metastases in Papillary Thyroid Cancer. Thyroid (2014) 24(4):675–82. doi: 10.1089/thy.2013.0224
4. Pereira JA, Jimeno J, Miquel J, Iglesias M, Munné A, Sancho JJ, et al. Nodal Yield, Morbidity, and Recurrence After Central Neck Dissection for Papillary Thyroid Carcinoma. Surgery (2005) 138(6):1095–100, discussion 100-1. doi: 10.1016/j.surg.2005.09.013
5. National Comprehensive Cancer Network. NCCN Clinicial Practice Guidelines in Oncology—Thyroid Carcinoma. Available at: https://wwwnccnorg/ (Accessed 1 September 2021).
6. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients With Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid (2016) 26(1):1–133. doi: 10.1089/thy.2015.0020
7. Lee YS, Shin SC, Lim YS, Lee JC, Wang SG, Son SM, et al. Tumor Location-Dependent Skip Lateral Cervical Lymph Node Metastasis in Papillary Thyroid Cancer. Head Neck (2014) 36(6):887–91. doi: 10.1002/hed.23391
8. Roh JL, Park JY, Rha KS, Park CI. Is Central Neck Dissection Necessary for the Treatment of Lateral Cervical Nodal Recurrence of Papillary Thyroid Carcinoma? Head Neck (2007) 29(10):901–6. doi: 10.1002/hed.20606
9. Likhterov I, Reis LL, Urken ML. Central Compartment Management in Patients With Papillary Thyroid Cancer Presenting With Metastatic Disease to the Lateral Neck: Anatomic Pathways of Lymphatic Spread. Head Neck (2017) 39(5):853–9. doi: 10.1002/hed.24568
10. Trivizki O, Amit M, Fliss DM, Gil Z. Elective Central Compartment Neck Dissection in Patients With Papillary Thyroid Carcinoma Recurrence. Laryngoscope (2013) 123(6):1564–8. doi: 10.1002/lary.23982
11. De Napoli L, Matrone A, Favilla K, Piaggi P, Galleri D, Ambrosini CE, et al. Role of Prophylactic Central Compartment Lymph Node Dissection on the Outcome Of Patients With Papillary Thyroid Carcinoma and Synchronous Ipsilateral Cervical Lymph Node Metastases. Endocr Pract (2020) 26(8):807–17. doi: 10.4158/EP-2019-0532
12. Harries V, McGill M, Wang LY, Tuttle RM, Wong RJ, Shaha AR, et al. Is a Prophylactic Central Compartment Neck Dissection Required in Papillary Thyroid Carcinoma Patients With Clinically Involved Lateral Compartment Lymph Nodes? Ann Surg Oncol (2021) 28(1):512–8. doi: 10.1245/s10434-020-08861-4
13. Carmel-Neiderman NN, Mizrachi A, Yaniv D, Vainer I, Muhanna N, Abergel A, et al. Prophylactic Central Neck Dissection has No Advantage in Patients With Metastatic Papillary Thyroid Cancer to the Lateral Neck. J Surg Oncol (2021) 123(2):456–61. doi: 10.1002/jso.26299
14. Popadich A, Levin O, Lee JC, Smooke-Praw S, Ro K, Fazel M, et al. A Multicenter Cohort Study of Total Thyroidectomy and Routine Central Lymph Node Dissection for Cn0 Papillary Thyroid Cancer. Surgery (2011) 150(6):1048–57. doi: 10.1016/j.surg.2011.09.003
15. Barczyński M, Konturek A, Stopa M, Nowak W. Prophylactic Central Neck Dissection for Papillary Thyroid Cancer. Br J Surg (2013) 100(3):410–8. doi: 10.1002/bjs.8985
16. Hartl DM, Mamelle E, Borget I, Leboulleux S, Mirghani H, Schlumberger M. Influence of Prophylactic Neck Dissection on Rate of Retreatment for Papillary Thyroid Carcinoma. World J Surg (2013) 37(8):1951–8. doi: 10.1007/s00268-013-2089-3
17. White ML, Gauger PG, Doherty GM. Central Lymph Node Dissection in Differentiated Thyroid Cancer. World J Surg (2007) 31(5):895–904. doi: 10.1007/s00268-006-0907-6
18. Lang BH, Ng SH, Lau LL, Cowling BJ, Wong KP, Wan KY. A Systematic Review and Meta-Analysis of Prophylactic Central Neck Dissection on Short-Term Locoregional Recurrence in Papillary Thyroid Carcinoma After Total Thyroidectomy. Thyroid (2013) 23(9):1087–98. doi: 10.1089/thy.2012.0608
19. So YK, Seo MY, Son YI. Prophylactic Central Lymph Node Dissection for Clinically Node-Negative Papillary Thyroid Microcarcinoma: Influence on Serum Thyroglobulin Level, Recurrence Rate, and Postoperative Complications. Surgery (2012) 151(2):192–8. doi: 10.1016/j.surg.2011.02.004
20. Moreno MA, Edeiken-Monroe BS, Siegel ER, Sherman SI, Clayman GL. In Papillary Thyroid Cancer, Preoperative Central Neck Ultrasound Detects Only Macroscopic Surgical Disease, But Negative Findings Predict Excellent Long-Term Regional Control and Survival. Thyroid (2012) 22(4):347–55. doi: 10.1089/thy.2011.0121
21. Roh JL, Park JY, Park CI. Total Thyroidectomy Plus Neck Dissection in Differentiated Papillary Thyroid Carcinoma Patients: Pattern of Nodal Metastasis, Morbidity, Recurrence, and Postoperative Levels of Serum Parathyroid Hormone. Ann Surg (2007) 245(4):604–10. doi: 10.1097/01.sla.0000250451.59685.67
22. Hughes DT, White ML, Miller BS, Gauger PG, Burney RE, Doherty GM. Influence of Prophylactic Central Lymph Node Dissection on Postoperative Thyroglobulin Levels and Radioiodine Treatment in Papillary Thyroid Cancer. Surgery (2010) 148(6):1100–6. doi: 10.1016/j.surg.2010.09.019
23. Zhao W, You L, Hou X, Chen S, Ren X, Chen G, et al. The Effect of Prophylactic Central Neck Dissection on Locoregional Recurrence in Papillary Thyroid Cancer After Total Thyroidectomy: A Systematic Review and Meta-Analysis: pCND for the Locoregional Recurrence of Papillary Thyroid Cancer. Ann Surg Oncol (2017) 24(8):2189–98. doi: 10.1245/s10434-016-5691-4
24. Viola D, Materazzi G, Valerio L, Molinaro E, Agate L, Faviana P, et al. Prophylactic Central Compartment Lymph Node Dissection in Papillary Thyroid Carcinoma: Clinical Implications Derived From the First Prospective Randomized Controlled Single Institution Study. J Clin Endocrinol Metab (2015) 100(4):1316–24. doi: 10.1210/jc.2014-3825
25. Carling T, Carty SE, Ciarleglio MM, Cooper DS, Doherty GM, Kim LT, et al. American Thyroid Association Design and Feasibility of a Prospective Randomized Controlled Trial of Prophylactic Central Lymph Node Dissection for Papillary Thyroid Carcinoma. Thyroid (2012) 22(3):237–44. doi: 10.1089/thy.2011.0317
26. Roh JL, Kim JM, Park CI. Central Lymph Node Metastasis of Unilateral Papillary Thyroid Carcinoma: Patterns and Factors Predictive of Nodal Metastasis, Morbidity, and Recurrence. Ann Surg Oncol (2011) 18(8):2245–50. doi: 10.1245/s10434-011-1600-z
27. Chow SM, Yau S, Kwan CK, Poon PC, Law SC. Local and Regional Control in Patients With Papillary Thyroid Carcinoma: Specific Indications of External Radiotherapy and Radioactive Iodine According to T and N Categories in AJCC 6th Edition. Endocrine-Related Cancer (2006) 13(4):1159–72. doi: 10.1677/erc.1.01320
28. Ruel E, Thomas S, Dinan M, Perkins JM, Roman SA, Sosa JA. Adjuvant Radioactive Iodine Therapy Is Associated With Improved Survival for Patients With Intermediate-Risk Papillary Thyroid Cancer. J Clin Endocrinol Metab (2015) 100(4):1529–36. doi: 10.1210/jc.2014-4332
29. Kelemen PR, Van Herle AJ, Giuliano AE. Sentinel Lymphadenectomy in Thyroid Malignant Neoplasms. Arch Surg (Chicago Ill 1960) (1998) 133(3):288–92. doi: 10.1001/archsurg.133.3.288
30. Giordano D, Valcavi R, Thompson GB, Pedroni C, Renna L, Gradoni P, et al. Complications of Central Neck Dissection in Patients With Papillary Thyroid Carcinoma: Results of a Study on 1087 Patients and Review of the Literature. Thyroid (2012) 22(9):911–7. doi: 10.1089/thy.2012.0011
31. Chen L, Wu YH, Lee CH, Chen HA, Loh EW, Tam KW. Prophylactic Central Neck Dissection for Papillary Thyroid Carcinoma With Clinically Uninvolved Central Neck Lymph Nodes: A Systematic Review and Meta-Analysis. World J Surg (2018) 42(9):2846–57. doi: 10.1007/s00268-018-4547-4
32. Barczyński M, Konturek A, Pragacz K, Papier A, Stopa M, Nowak W. Intraoperative Nerve Monitoring can Reduce Prevalence of Recurrent Laryngeal Nerve Injury in Thyroid Reoperations: Results of a Retrospective Cohort Study. World J Surg (2014) 38(3):599–606. doi: 10.1007/s00268-013-2260-x
Keywords: prophylactic central neck dissection (PCND), papillary thyroid carcinoma (PTC), lateral neck dissection (LND), lateral cervical lymph node metastases, locoregional recurrence, total thyroidectomy (TT)
Citation: Yan X-q, Zhang Z-z, Yu W-j, Ma Z-s, Chen M-l and Xie B-j (2022) Prophylactic Central Neck Dissection for cN1b Papillary Thyroid Carcinoma: A Systematic Review and Meta-Analysis. Front. Oncol. 11:803986. doi: 10.3389/fonc.2021.803986
Received: 28 October 2021; Accepted: 22 December 2021;
Published: 14 January 2022.
Edited by:
Gianlorenzo Dionigi, University of Milan, ItalyCopyright © 2022 Yan, Zhang, Yu, Ma, Chen and Xie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo-jian Xie, b25jb2xvZ3l5eHFAb3V0bG9vay5jb20=
†These authors have contributed equally to this work and share first authorship
 Xing-qiang Yan1†
Xing-qiang Yan1†